6b61a7c64e95e8f211f266e249c1c6b2.ppt
- Количество слайдов: 104


 DEFINITION
DEFINITION
 Paraneoplastic neurological disorders (PNDs) refer to an extensive group of syndromes that can affect any part of the nervous system by mechanisms that are primarily immune mediated.
Paraneoplastic neurological disorders (PNDs) refer to an extensive group of syndromes that can affect any part of the nervous system by mechanisms that are primarily immune mediated.
 INCIDENCE
INCIDENCE
 - Rare, < 1% patients with cancer - 3% in SCLC - 30% in thymoma and 50% in sclerotic myeloma - LEMS occurs in approximately 3% of patients with SCLC and 1/1000 in gynaecological tumours - Some specific cancers may have associations with certain disorders more frequently
- Rare, < 1% patients with cancer - 3% in SCLC - 30% in thymoma and 50% in sclerotic myeloma - LEMS occurs in approximately 3% of patients with SCLC and 1/1000 in gynaecological tumours - Some specific cancers may have associations with certain disorders more frequently
 In neuromyopathy - 4% of women with breast cancer - 16% of men with lung cancer - 66% of patients with all cancers
In neuromyopathy - 4% of women with breast cancer - 16% of men with lung cancer - 66% of patients with all cancers
 Age & Sex: - In UK M: F 1: 3. 2 - In USA 3: 1 - Median age 66 y (30 -77) - 11% below 50 y - lymphoproliferative diseases and testicular tumours in younger
Age & Sex: - In UK M: F 1: 3. 2 - In USA 3: 1 - Median age 66 y (30 -77) - 11% below 50 y - lymphoproliferative diseases and testicular tumours in younger
 - In 60% of patients, symptoms of PND develop before the presence of a tumor is known. - In 40% of patients, symptoms of PND develop after the tumor diagnosis or at tumor recurrence. - In 40% of patients, ther is no detected antibodies - In 15% of cancer patients showed antibodies without having neurologic syndromes.
- In 60% of patients, symptoms of PND develop before the presence of a tumor is known. - In 40% of patients, symptoms of PND develop after the tumor diagnosis or at tumor recurrence. - In 40% of patients, ther is no detected antibodies - In 15% of cancer patients showed antibodies without having neurologic syndromes.
 PATHOGENESIS
PATHOGENESIS
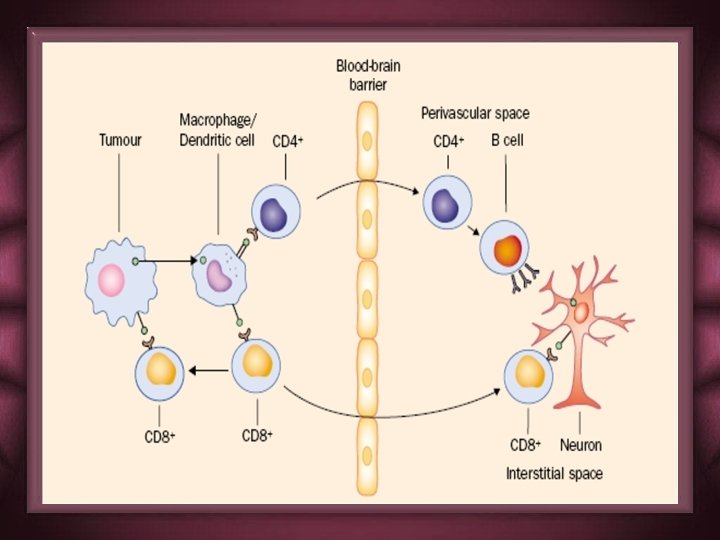
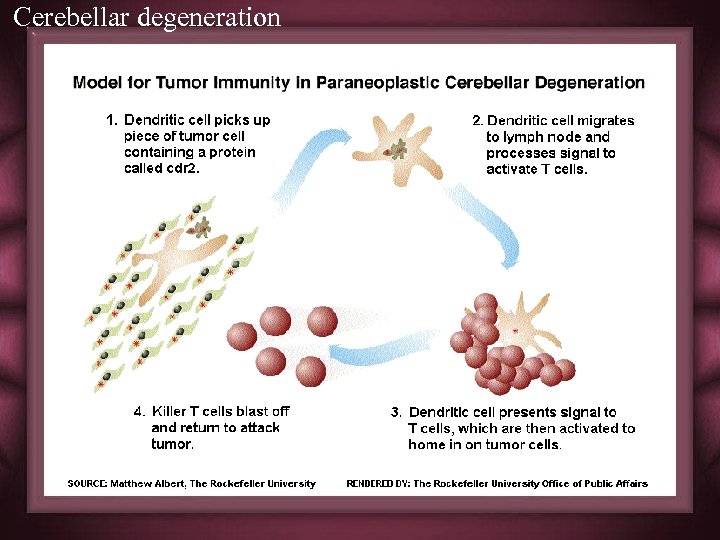
 Different etiologies postulated: Toxins, viruses, nutritional deficiency, autoimmune - Autoimmune theory strongest: “molecular mimicry” Antibodies react with shared protein antigens: - Not the cause of damage -Cytotoxic. T-cells involved
Different etiologies postulated: Toxins, viruses, nutritional deficiency, autoimmune - Autoimmune theory strongest: “molecular mimicry” Antibodies react with shared protein antigens: - Not the cause of damage -Cytotoxic. T-cells involved
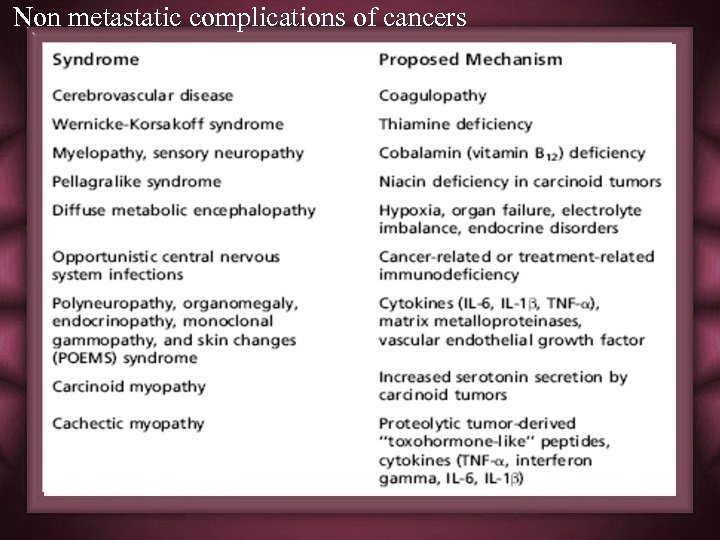 Non metastatic complications of cancers
Non metastatic complications of cancers
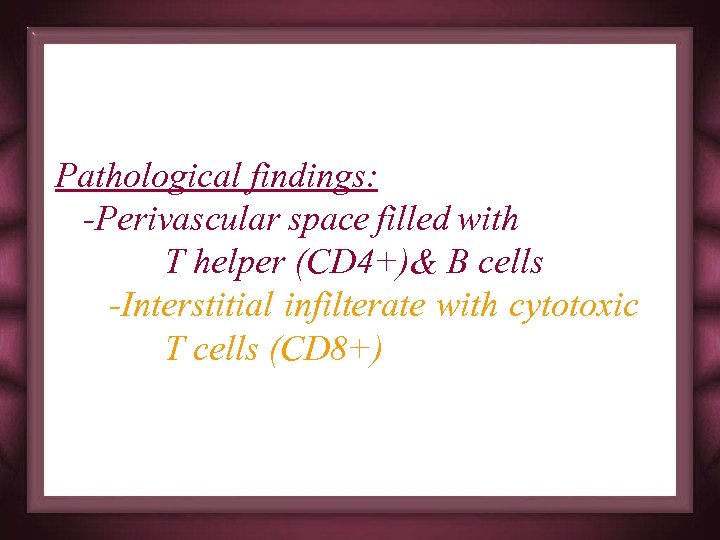 Pathological findings: -Perivascular space filled with T helper (CD 4+)& B cells -Interstitial infilterate with cytotoxic T cells (CD 8+)
Pathological findings: -Perivascular space filled with T helper (CD 4+)& B cells -Interstitial infilterate with cytotoxic T cells (CD 8+)
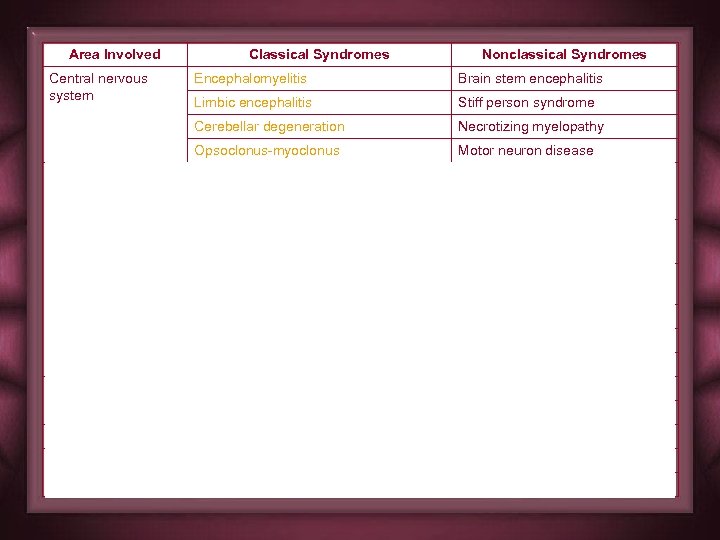
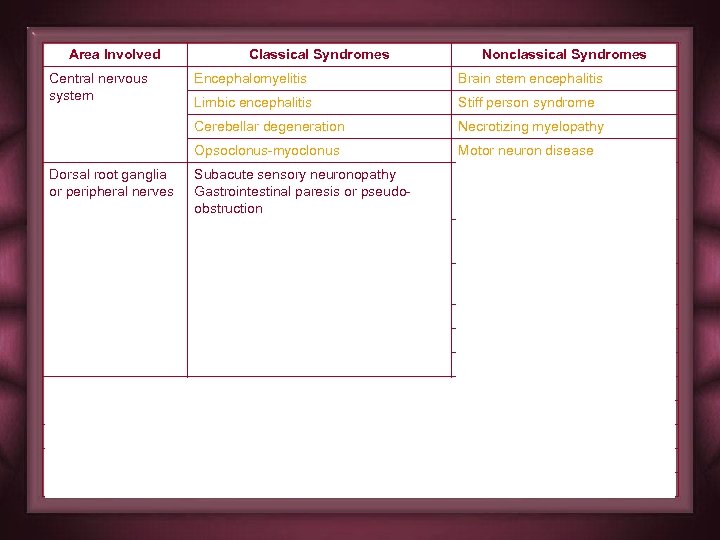
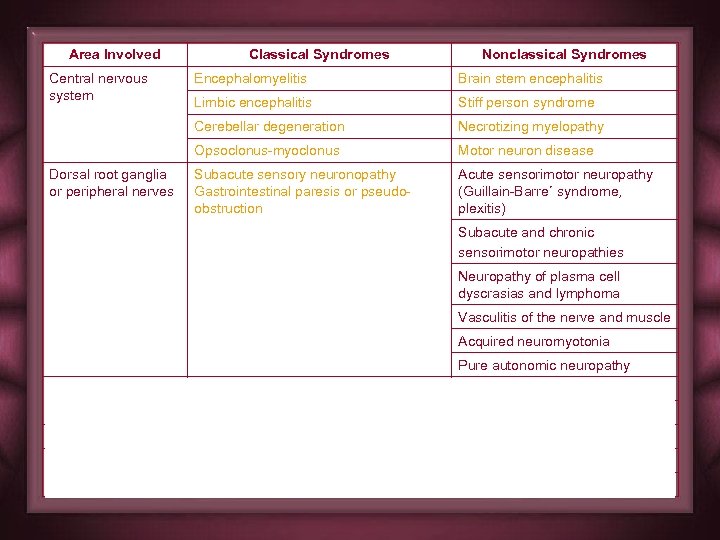
 CLSSIFICATION
CLSSIFICATION
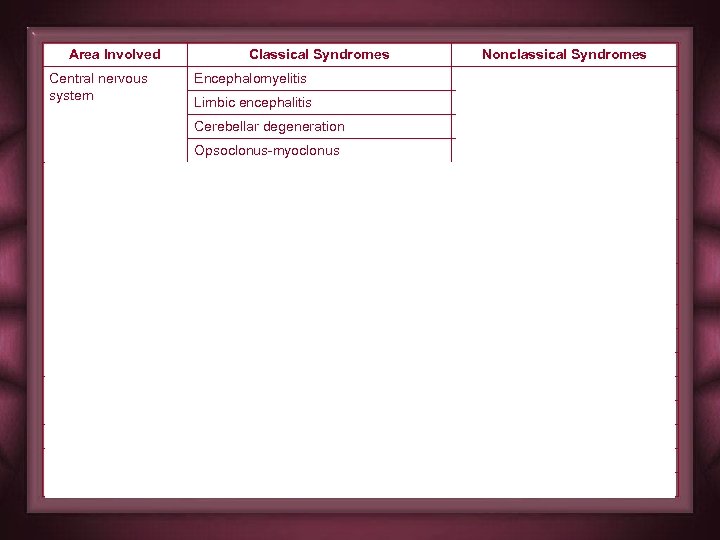 Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
 Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
 Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
 Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
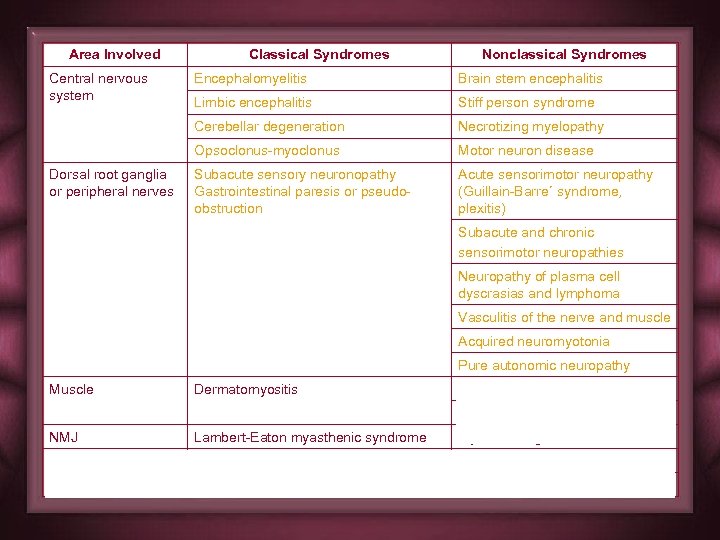 Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
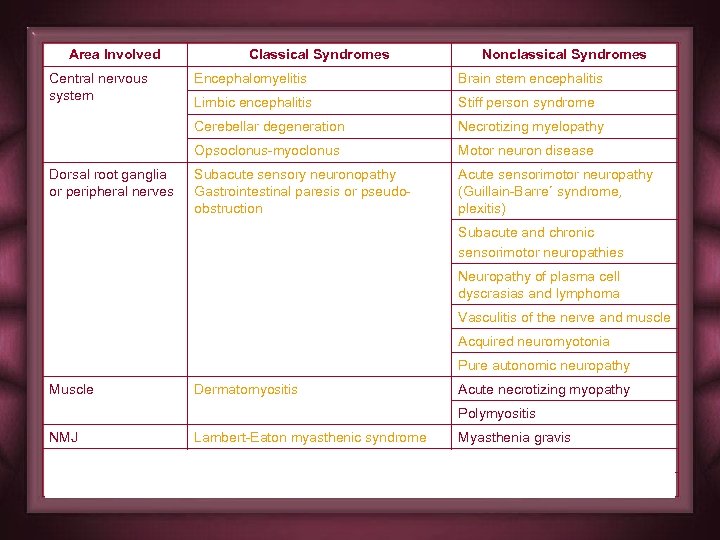 Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
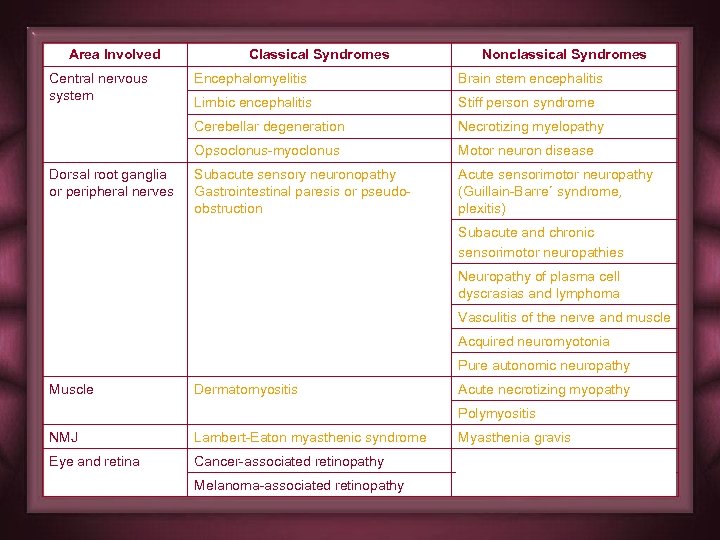 Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
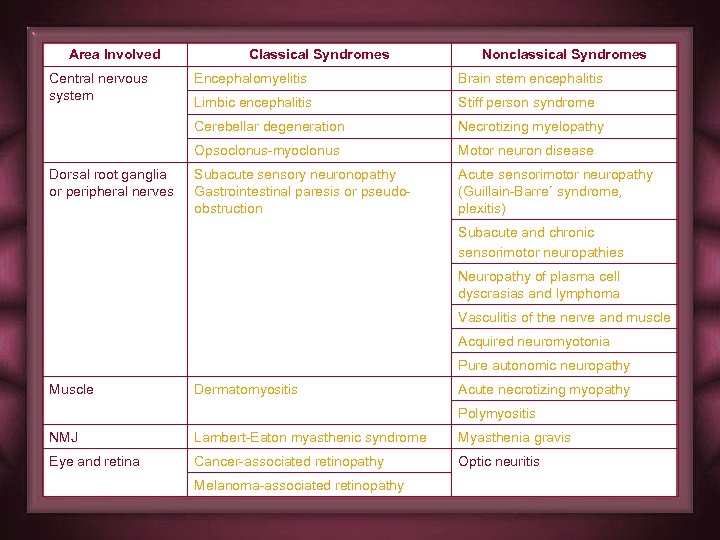 Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
 DIAGNOSIS
DIAGNOSIS
 Recognition of the paraneoplastic antibodies Recognition of the associated cancer Recognition of the Neurological Syndrome
Recognition of the paraneoplastic antibodies Recognition of the associated cancer Recognition of the Neurological Syndrome
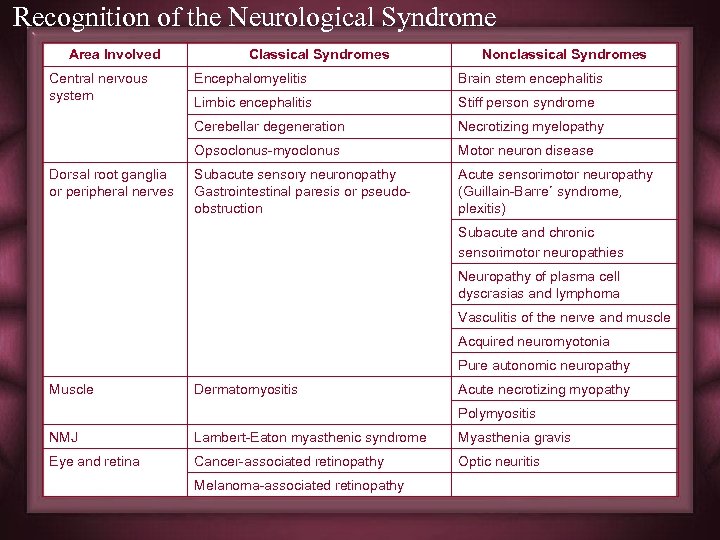 Recognition of the Neurological Syndrome Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
Recognition of the Neurological Syndrome Area Involved Central nervous system Classical Syndromes Nonclassical Syndromes Brain stem encephalitis Limbic encephalitis Stiff person syndrome Cerebellar degeneration Necrotizing myelopathy Opsoclonus-myoclonus Dorsal root ganglia or peripheral nerves Encephalomyelitis Motor neuron disease Subacute sensory neuronopathy Gastrointestinal paresis or pseudoobstruction Acute sensorimotor neuropathy (Guillain-Barre´ syndrome, plexitis) Subacute and chronic sensorimotor neuropathies Neuropathy of plasma cell dyscrasias and lymphoma Vasculitis of the nerve and muscle Acquired neuromyotonia Pure autonomic neuropathy Muscle Dermatomyositis Acute necrotizing myopathy Polymyositis NMJ Lambert-Eaton myasthenic syndrome Myasthenia gravis Eye and retina Cancer-associated retinopathy Optic neuritis Melanoma-associated retinopathy
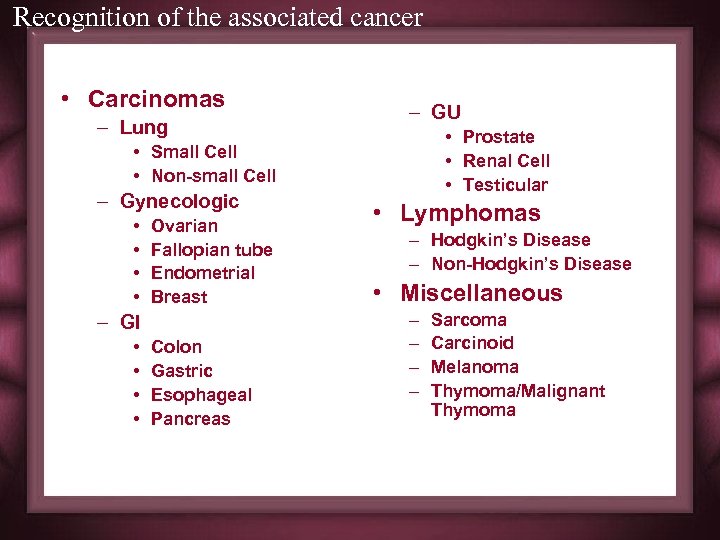 Recognition of the associated cancer • Carcinomas – Lung – GU • Prostate • Renal Cell • Testicular • Small Cell • Non-small Cell – Gynecologic • • Ovarian Fallopian tube Endometrial Breast – GI • • Colon Gastric Esophageal Pancreas • Lymphomas – Hodgkin’s Disease – Non-Hodgkin’s Disease • Miscellaneous – – Sarcoma Carcinoid Melanoma Thymoma/Malignant Thymoma
Recognition of the associated cancer • Carcinomas – Lung – GU • Prostate • Renal Cell • Testicular • Small Cell • Non-small Cell – Gynecologic • • Ovarian Fallopian tube Endometrial Breast – GI • • Colon Gastric Esophageal Pancreas • Lymphomas – Hodgkin’s Disease – Non-Hodgkin’s Disease • Miscellaneous – – Sarcoma Carcinoid Melanoma Thymoma/Malignant Thymoma
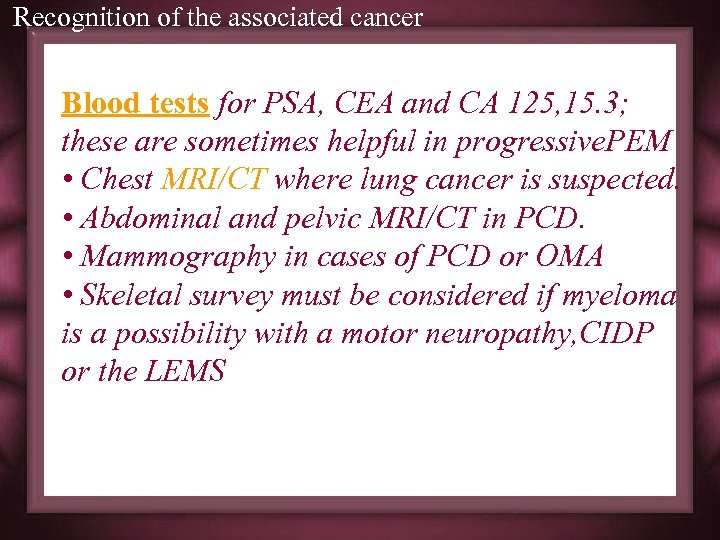 Recognition of the associated cancer Blood tests for PSA, CEA and CA 125, 15. 3; these are sometimes helpful in progressive. PEM • Chest MRI/CT where lung cancer is suspected. • Abdominal and pelvic MRI/CT in PCD. • Mammography in cases of PCD or OMA • Skeletal survey must be considered if myeloma is a possibility with a motor neuropathy, CIDP or the LEMS
Recognition of the associated cancer Blood tests for PSA, CEA and CA 125, 15. 3; these are sometimes helpful in progressive. PEM • Chest MRI/CT where lung cancer is suspected. • Abdominal and pelvic MRI/CT in PCD. • Mammography in cases of PCD or OMA • Skeletal survey must be considered if myeloma is a possibility with a motor neuropathy, CIDP or the LEMS
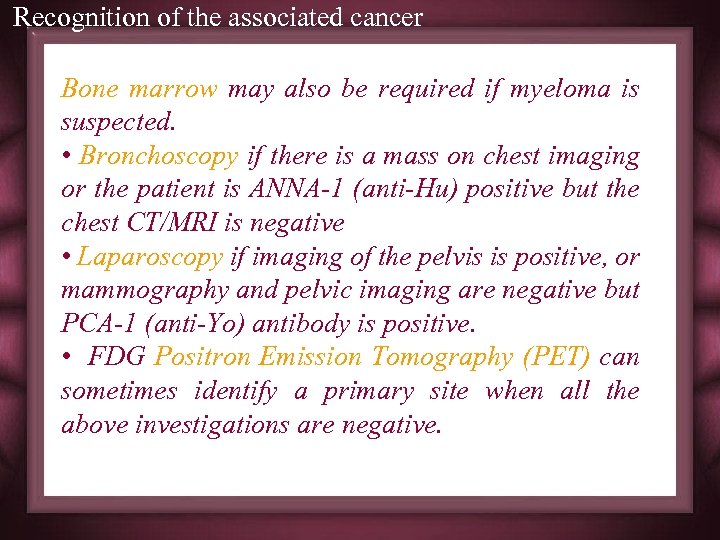 Recognition of the associated cancer Bone marrow may also be required if myeloma is suspected. • Bronchoscopy if there is a mass on chest imaging or the patient is ANNA-1 (anti-Hu) positive but the chest CT/MRI is negative • Laparoscopy if imaging of the pelvis is positive, or mammography and pelvic imaging are negative but PCA-1 (anti-Yo) antibody is positive. • FDG Positron Emission Tomography (PET) can sometimes identify a primary site when all the above investigations are negative.
Recognition of the associated cancer Bone marrow may also be required if myeloma is suspected. • Bronchoscopy if there is a mass on chest imaging or the patient is ANNA-1 (anti-Hu) positive but the chest CT/MRI is negative • Laparoscopy if imaging of the pelvis is positive, or mammography and pelvic imaging are negative but PCA-1 (anti-Yo) antibody is positive. • FDG Positron Emission Tomography (PET) can sometimes identify a primary site when all the above investigations are negative.
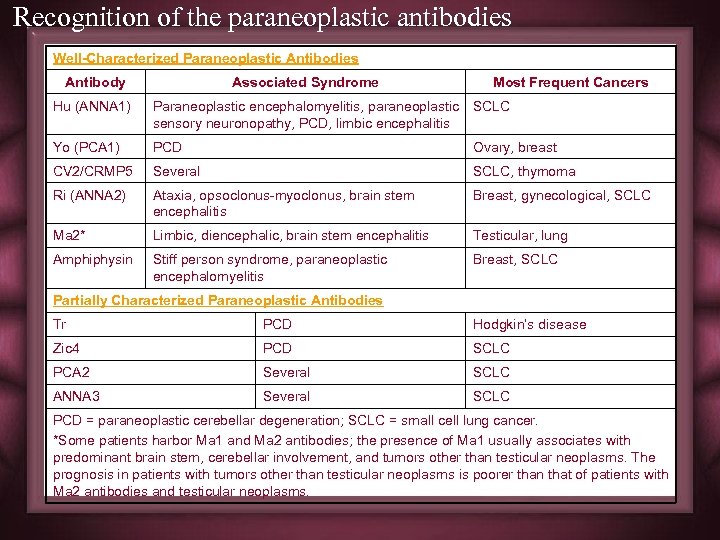 Recognition of the paraneoplastic antibodies Well-Characterized Paraneoplastic Antibodies Antibody Associated Syndrome Most Frequent Cancers Hu (ANNA 1) Paraneoplastic encephalomyelitis, paraneoplastic SCLC sensory neuronopathy, PCD, limbic encephalitis Yo (PCA 1) PCD Ovary, breast CV 2/CRMP 5 Several SCLC, thymoma Ri (ANNA 2) Ataxia, opsoclonus-myoclonus, brain stem encephalitis Breast, gynecological, SCLC Ma 2* Limbic, diencephalic, brain stem encephalitis Testicular, lung Amphiphysin Stiff person syndrome, paraneoplastic encephalomyelitis Breast, SCLC Partially Characterized Paraneoplastic Antibodies Tr PCD Hodgkin’s disease Zic 4 PCD SCLC PCA 2 Several SCLC ANNA 3 Several SCLC PCD = paraneoplastic cerebellar degeneration; SCLC = small cell lung cancer. *Some patients harbor Ma 1 and Ma 2 antibodies; the presence of Ma 1 usually associates with predominant brain stem, cerebellar involvement, and tumors other than testicular neoplasms. The prognosis in patients with tumors other than testicular neoplasms is poorer than that of patients with Ma 2 antibodies and testicular neoplasms.
Recognition of the paraneoplastic antibodies Well-Characterized Paraneoplastic Antibodies Antibody Associated Syndrome Most Frequent Cancers Hu (ANNA 1) Paraneoplastic encephalomyelitis, paraneoplastic SCLC sensory neuronopathy, PCD, limbic encephalitis Yo (PCA 1) PCD Ovary, breast CV 2/CRMP 5 Several SCLC, thymoma Ri (ANNA 2) Ataxia, opsoclonus-myoclonus, brain stem encephalitis Breast, gynecological, SCLC Ma 2* Limbic, diencephalic, brain stem encephalitis Testicular, lung Amphiphysin Stiff person syndrome, paraneoplastic encephalomyelitis Breast, SCLC Partially Characterized Paraneoplastic Antibodies Tr PCD Hodgkin’s disease Zic 4 PCD SCLC PCA 2 Several SCLC ANNA 3 Several SCLC PCD = paraneoplastic cerebellar degeneration; SCLC = small cell lung cancer. *Some patients harbor Ma 1 and Ma 2 antibodies; the presence of Ma 1 usually associates with predominant brain stem, cerebellar involvement, and tumors other than testicular neoplasms. The prognosis in patients with tumors other than testicular neoplasms is poorer than that of patients with Ma 2 antibodies and testicular neoplasms.
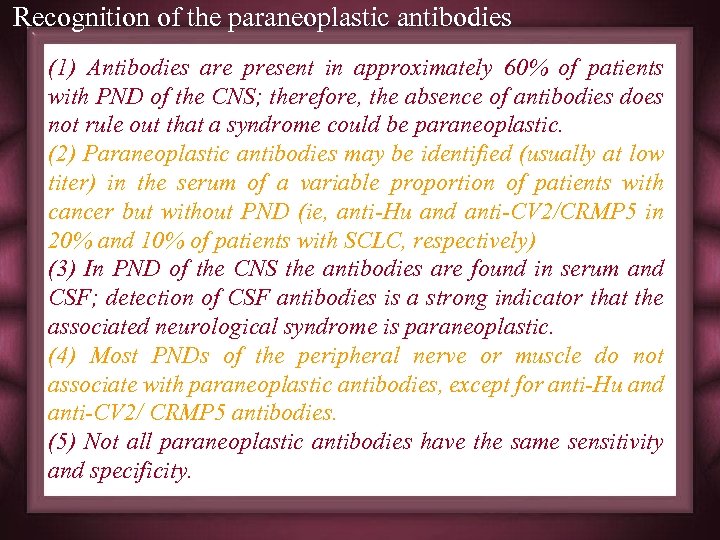 Recognition of the paraneoplastic antibodies (1) Antibodies are present in approximately 60% of patients with PND of the CNS; therefore, the absence of antibodies does not rule out that a syndrome could be paraneoplastic. (2) Paraneoplastic antibodies may be identified (usually at low titer) in the serum of a variable proportion of patients with cancer but without PND (ie, anti-Hu and anti-CV 2/CRMP 5 in 20% and 10% of patients with SCLC, respectively) (3) In PND of the CNS the antibodies are found in serum and CSF; detection of CSF antibodies is a strong indicator that the associated neurological syndrome is paraneoplastic. (4) Most PNDs of the peripheral nerve or muscle do not associate with paraneoplastic antibodies, except for anti-Hu and anti-CV 2/ CRMP 5 antibodies. (5) Not all paraneoplastic antibodies have the same sensitivity and specificity.
Recognition of the paraneoplastic antibodies (1) Antibodies are present in approximately 60% of patients with PND of the CNS; therefore, the absence of antibodies does not rule out that a syndrome could be paraneoplastic. (2) Paraneoplastic antibodies may be identified (usually at low titer) in the serum of a variable proportion of patients with cancer but without PND (ie, anti-Hu and anti-CV 2/CRMP 5 in 20% and 10% of patients with SCLC, respectively) (3) In PND of the CNS the antibodies are found in serum and CSF; detection of CSF antibodies is a strong indicator that the associated neurological syndrome is paraneoplastic. (4) Most PNDs of the peripheral nerve or muscle do not associate with paraneoplastic antibodies, except for anti-Hu and anti-CV 2/ CRMP 5 antibodies. (5) Not all paraneoplastic antibodies have the same sensitivity and specificity.
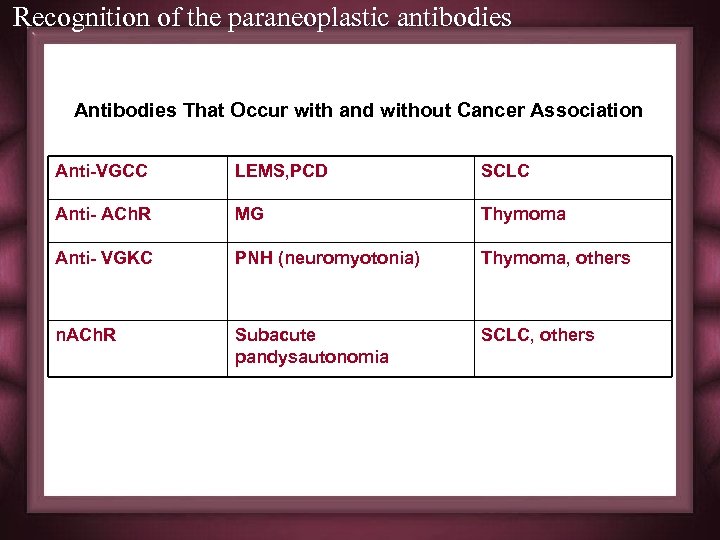 Recognition of the paraneoplastic antibodies Antibodies That Occur with and without Cancer Association Anti-VGCC LEMS, PCD SCLC Anti- ACh. R MG Thymoma Anti- VGKC PNH (neuromyotonia) Thymoma, others n. ACh. R Subacute pandysautonomia SCLC, others
Recognition of the paraneoplastic antibodies Antibodies That Occur with and without Cancer Association Anti-VGCC LEMS, PCD SCLC Anti- ACh. R MG Thymoma Anti- VGKC PNH (neuromyotonia) Thymoma, others n. ACh. R Subacute pandysautonomia SCLC, others
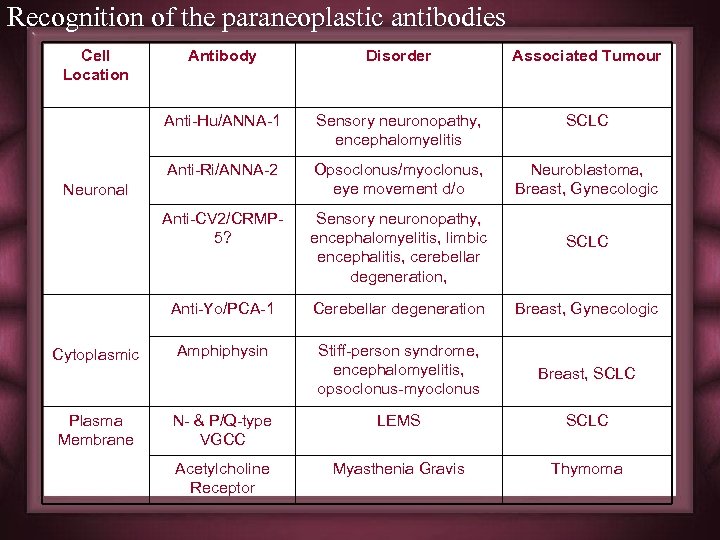 Recognition of the paraneoplastic antibodies Cell Location Antibody Disorder Associated Tumour Anti-Hu/ANNA-1 Sensory neuronopathy, encephalomyelitis SCLC Anti-Ri/ANNA-2 Opsoclonus/myoclonus, eye movement d/o Neuroblastoma, Breast, Gynecologic Anti-CV 2/CRMP 5? Sensory neuronopathy, encephalomyelitis, limbic encephalitis, cerebellar degeneration, SCLC Anti-Yo/PCA-1 Cerebellar degeneration Breast, Gynecologic Amphiphysin Stiff-person syndrome, encephalomyelitis, opsoclonus-myoclonus Breast, SCLC N- & P/Q-type VGCC LEMS SCLC Acetylcholine Receptor Myasthenia Gravis Thymoma Neuronal Cytoplasmic Plasma Membrane
Recognition of the paraneoplastic antibodies Cell Location Antibody Disorder Associated Tumour Anti-Hu/ANNA-1 Sensory neuronopathy, encephalomyelitis SCLC Anti-Ri/ANNA-2 Opsoclonus/myoclonus, eye movement d/o Neuroblastoma, Breast, Gynecologic Anti-CV 2/CRMP 5? Sensory neuronopathy, encephalomyelitis, limbic encephalitis, cerebellar degeneration, SCLC Anti-Yo/PCA-1 Cerebellar degeneration Breast, Gynecologic Amphiphysin Stiff-person syndrome, encephalomyelitis, opsoclonus-myoclonus Breast, SCLC N- & P/Q-type VGCC LEMS SCLC Acetylcholine Receptor Myasthenia Gravis Thymoma Neuronal Cytoplasmic Plasma Membrane
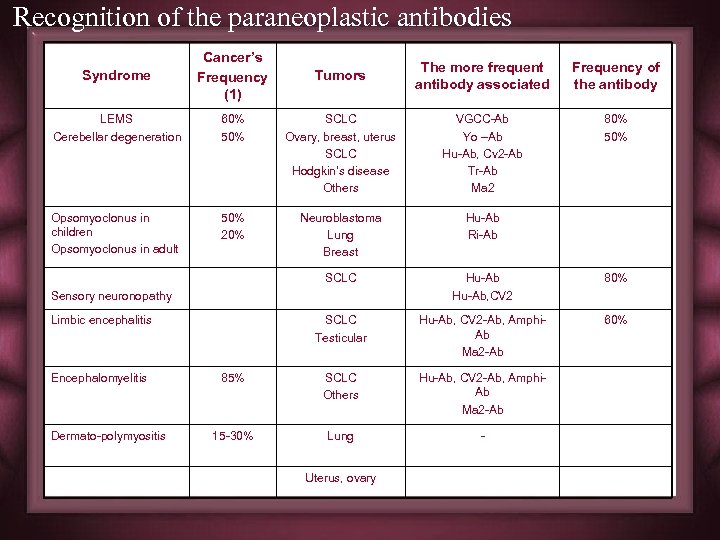 Recognition of the paraneoplastic antibodies Syndrome Cancer’s Frequency (1) LEMS Cerebellar degeneration Opsomyoclonus in children Opsomyoclonus in adult Tumors The more frequent antibody associated Frequency of the antibody 60% 50% SCLC Ovary, breast, uterus SCLC Hodgkin’s disease Others VGCC-Ab Yo –Ab Hu-Ab, Cv 2 -Ab Tr-Ab Ma 2 80% 50% 20% Neuroblastoma Lung Breast Hu-Ab Ri-Ab SCLC Hu-Ab, CV 2 80% SCLC Testicular Hu-Ab, CV 2 -Ab, Amphi. Ab Ma 2 -Ab 60% 85% SCLC Others Hu-Ab, CV 2 -Ab, Amphi. Ab Ma 2 -Ab 15 -30% Lung - Sensory neuronopathy Limbic encephalitis Encephalomyelitis Dermato-polymyositis Uterus, ovary
Recognition of the paraneoplastic antibodies Syndrome Cancer’s Frequency (1) LEMS Cerebellar degeneration Opsomyoclonus in children Opsomyoclonus in adult Tumors The more frequent antibody associated Frequency of the antibody 60% 50% SCLC Ovary, breast, uterus SCLC Hodgkin’s disease Others VGCC-Ab Yo –Ab Hu-Ab, Cv 2 -Ab Tr-Ab Ma 2 80% 50% 20% Neuroblastoma Lung Breast Hu-Ab Ri-Ab SCLC Hu-Ab, CV 2 80% SCLC Testicular Hu-Ab, CV 2 -Ab, Amphi. Ab Ma 2 -Ab 60% 85% SCLC Others Hu-Ab, CV 2 -Ab, Amphi. Ab Ma 2 -Ab 15 -30% Lung - Sensory neuronopathy Limbic encephalitis Encephalomyelitis Dermato-polymyositis Uterus, ovary
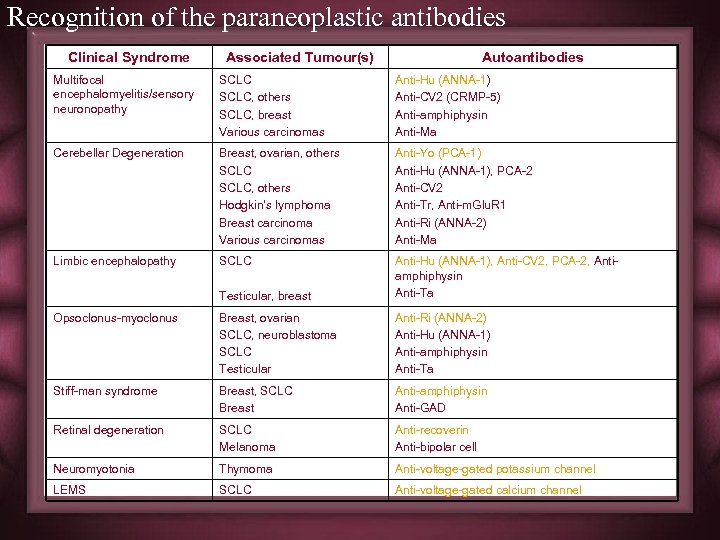 Recognition of the paraneoplastic antibodies Clinical Syndrome Associated Tumour(s) Autoantibodies Multifocal encephalomyelitis/sensory neuronopathy SCLC, others SCLC, breast Various carcinomas Anti-Hu (ANNA-1) Anti-CV 2 (CRMP-5) Anti-amphiphysin Anti-Ma Cerebellar Degeneration Breast, ovarian, others SCLC, others Hodgkin’s lymphoma Breast carcinoma Various carcinomas Anti-Yo (PCA-1) Anti-Hu (ANNA-1), PCA-2 Anti-CV 2 Anti-Tr, Anti-m. Glu. R 1 Anti-Ri (ANNA-2) Anti-Ma Limbic encephalopathy SCLC Testicular, breast Anti-Hu (ANNA-1), Anti-CV 2, PCA-2, Antiamphiphysin Anti-Ta Opsoclonus-myoclonus Breast, ovarian SCLC, neuroblastoma SCLC Testicular Anti-Ri (ANNA-2) Anti-Hu (ANNA-1) Anti-amphiphysin Anti-Ta Stiff-man syndrome Breast, SCLC Breast Anti-amphiphysin Anti-GAD Retinal degeneration SCLC Melanoma Anti-recoverin Anti-bipolar cell Neuromyotonia Thymoma Anti-voltage-gated potassium channel LEMS SCLC Anti-voltage-gated calcium channel
Recognition of the paraneoplastic antibodies Clinical Syndrome Associated Tumour(s) Autoantibodies Multifocal encephalomyelitis/sensory neuronopathy SCLC, others SCLC, breast Various carcinomas Anti-Hu (ANNA-1) Anti-CV 2 (CRMP-5) Anti-amphiphysin Anti-Ma Cerebellar Degeneration Breast, ovarian, others SCLC, others Hodgkin’s lymphoma Breast carcinoma Various carcinomas Anti-Yo (PCA-1) Anti-Hu (ANNA-1), PCA-2 Anti-CV 2 Anti-Tr, Anti-m. Glu. R 1 Anti-Ri (ANNA-2) Anti-Ma Limbic encephalopathy SCLC Testicular, breast Anti-Hu (ANNA-1), Anti-CV 2, PCA-2, Antiamphiphysin Anti-Ta Opsoclonus-myoclonus Breast, ovarian SCLC, neuroblastoma SCLC Testicular Anti-Ri (ANNA-2) Anti-Hu (ANNA-1) Anti-amphiphysin Anti-Ta Stiff-man syndrome Breast, SCLC Breast Anti-amphiphysin Anti-GAD Retinal degeneration SCLC Melanoma Anti-recoverin Anti-bipolar cell Neuromyotonia Thymoma Anti-voltage-gated potassium channel LEMS SCLC Anti-voltage-gated calcium channel
 DIAGNOSTIC CRITERIA
DIAGNOSTIC CRITERIA
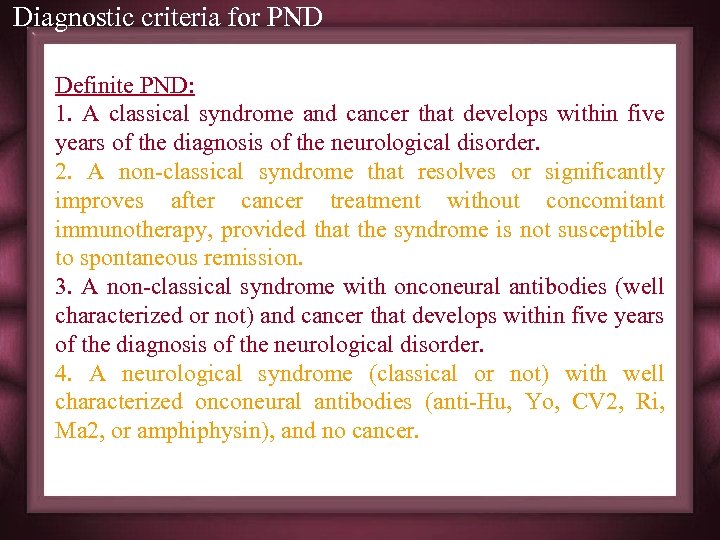 Diagnostic criteria for PND Definite PND: 1. A classical syndrome and cancer that develops within five years of the diagnosis of the neurological disorder. 2. A non-classical syndrome that resolves or significantly improves after cancer treatment without concomitant immunotherapy, provided that the syndrome is not susceptible to spontaneous remission. 3. A non-classical syndrome with onconeural antibodies (well characterized or not) and cancer that develops within five years of the diagnosis of the neurological disorder. 4. A neurological syndrome (classical or not) with well characterized onconeural antibodies (anti-Hu, Yo, CV 2, Ri, Ma 2, or amphiphysin), and no cancer.
Diagnostic criteria for PND Definite PND: 1. A classical syndrome and cancer that develops within five years of the diagnosis of the neurological disorder. 2. A non-classical syndrome that resolves or significantly improves after cancer treatment without concomitant immunotherapy, provided that the syndrome is not susceptible to spontaneous remission. 3. A non-classical syndrome with onconeural antibodies (well characterized or not) and cancer that develops within five years of the diagnosis of the neurological disorder. 4. A neurological syndrome (classical or not) with well characterized onconeural antibodies (anti-Hu, Yo, CV 2, Ri, Ma 2, or amphiphysin), and no cancer.
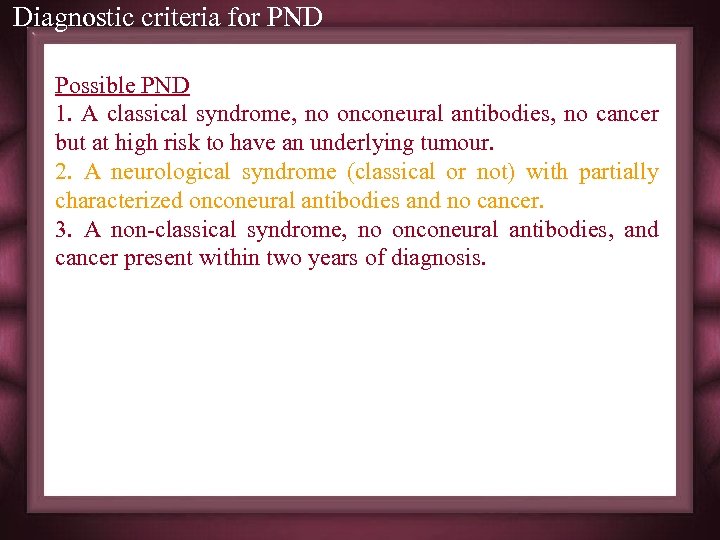 Diagnostic criteria for PND Possible PND 1. A classical syndrome, no onconeural antibodies, no cancer but at high risk to have an underlying tumour. 2. A neurological syndrome (classical or not) with partially characterized onconeural antibodies and no cancer. 3. A non-classical syndrome, no onconeural antibodies, and cancer present within two years of diagnosis.
Diagnostic criteria for PND Possible PND 1. A classical syndrome, no onconeural antibodies, no cancer but at high risk to have an underlying tumour. 2. A neurological syndrome (classical or not) with partially characterized onconeural antibodies and no cancer. 3. A non-classical syndrome, no onconeural antibodies, and cancer present within two years of diagnosis.
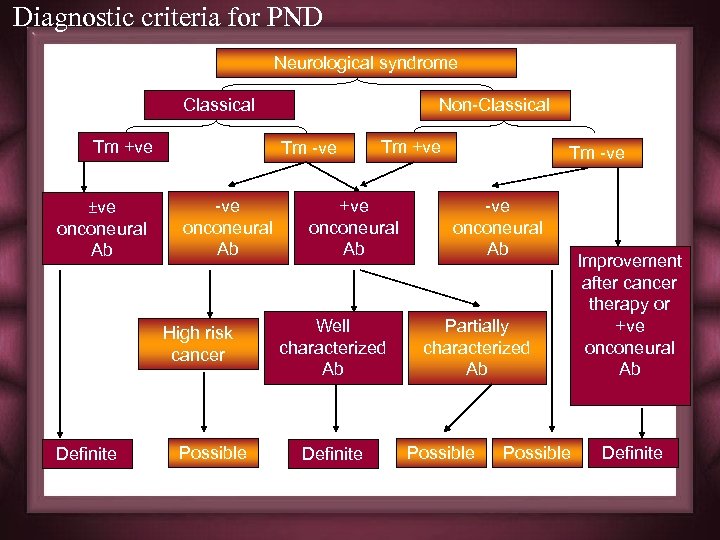 Diagnostic criteria for PND Neurological syndrome Classical Tm +ve ±ve onconeural Ab Tm -ve onconeural Ab High risk cancer Definite Non-Classical Possible Tm +ve onconeural Ab Well characterized Ab Definite Tm -ve onconeural Ab Partially characterized Ab Possible Improvement after cancer therapy or +ve onconeural Ab Definite
Diagnostic criteria for PND Neurological syndrome Classical Tm +ve ±ve onconeural Ab Tm -ve onconeural Ab High risk cancer Definite Non-Classical Possible Tm +ve onconeural Ab Well characterized Ab Definite Tm -ve onconeural Ab Partially characterized Ab Possible Improvement after cancer therapy or +ve onconeural Ab Definite
 PARANEOPLASTIC SYNDROMES
PARANEOPLASTIC SYNDROMES
 Historic context • First description – peripheral neuropathy in lung Ca patient, Oppenheim, 1888 • Myasthenia with thymoma – Weigert, 1901 • Cerebellar degeneration with ovarian and SCLC – Brain et al, 1951 • Lambert-Eaton myasthenic syndrome and SCLC – Lambert et al, 1956 • Cancer associated retinopathy – Sawyer et al, 1976 • Croft & Wilkinson 1965 Carcinomatous neuromyopathy Dr Edward H Lambert (1915 -2003)
Historic context • First description – peripheral neuropathy in lung Ca patient, Oppenheim, 1888 • Myasthenia with thymoma – Weigert, 1901 • Cerebellar degeneration with ovarian and SCLC – Brain et al, 1951 • Lambert-Eaton myasthenic syndrome and SCLC – Lambert et al, 1956 • Cancer associated retinopathy – Sawyer et al, 1976 • Croft & Wilkinson 1965 Carcinomatous neuromyopathy Dr Edward H Lambert (1915 -2003)
 Encephalomyelitis • Immune-mediated inflammatory disorder that can affect any part of the CNS, dorsal root ganglia, and autonomic nerves. • main areas involved include the hippocampus (limbic encephalitis), the Purkinje cells of the cerebellum cerebellar degeneration), the lower brain stem (brain stem encephalitis), dorsal root ganglia (sensory neuronopathy), spinal cord (myelitis) • Symptoms usually precede tumour detection (SCLC) • Brain MRI often normal, except limbic encephalitis • CSF - ↑ protein, mild pleocytosis; may be N • Most common antibodies: Anti-Hu (ANNA-1), antiamphiphysin, anti-CV 2 • Rare improvement despite tumour treatment – Immunosuppressive Rx, PLEX, IVIG rarely successful
Encephalomyelitis • Immune-mediated inflammatory disorder that can affect any part of the CNS, dorsal root ganglia, and autonomic nerves. • main areas involved include the hippocampus (limbic encephalitis), the Purkinje cells of the cerebellum cerebellar degeneration), the lower brain stem (brain stem encephalitis), dorsal root ganglia (sensory neuronopathy), spinal cord (myelitis) • Symptoms usually precede tumour detection (SCLC) • Brain MRI often normal, except limbic encephalitis • CSF - ↑ protein, mild pleocytosis; may be N • Most common antibodies: Anti-Hu (ANNA-1), antiamphiphysin, anti-CV 2 • Rare improvement despite tumour treatment – Immunosuppressive Rx, PLEX, IVIG rarely successful
 Limbic Encephalitis l Majority have SCLC, occ testicular, thymoma, other carcinoma l Usually part of encephalomyelitis syndrome l Symptoms: subacute amnestic syndrome, affective disorder, antero - and retrograde amnesia, hallucinations or delusions, seizures common, abnormal sleep/wake, labile BP, SIADH l MRI: increased T 2 signal medial temporal lobes/amygdala, occ hypothalamus, basal forebrain l CSF: N or mild pleocytosis, ↑ protein l Path: non-spec neuronal loss, gliosis, perivasc infiltrates, microglial nodules l Anti-Hu (ANNA-1) (other Ab’s occ) l Workup: Look for SCLC – CT Chest, other CT l Course variable: many may improve after tumour Rx, frequently stabilize at moderate/severe disability
Limbic Encephalitis l Majority have SCLC, occ testicular, thymoma, other carcinoma l Usually part of encephalomyelitis syndrome l Symptoms: subacute amnestic syndrome, affective disorder, antero - and retrograde amnesia, hallucinations or delusions, seizures common, abnormal sleep/wake, labile BP, SIADH l MRI: increased T 2 signal medial temporal lobes/amygdala, occ hypothalamus, basal forebrain l CSF: N or mild pleocytosis, ↑ protein l Path: non-spec neuronal loss, gliosis, perivasc infiltrates, microglial nodules l Anti-Hu (ANNA-1) (other Ab’s occ) l Workup: Look for SCLC – CT Chest, other CT l Course variable: many may improve after tumour Rx, frequently stabilize at moderate/severe disability
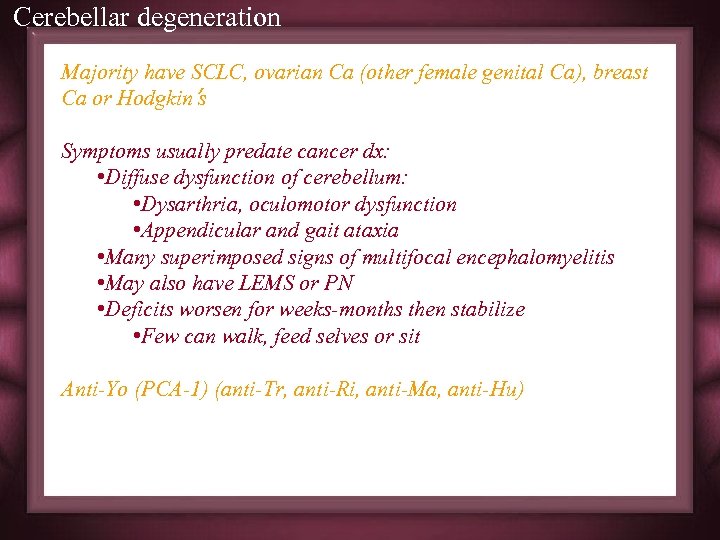 Cerebellar degeneration Majority have SCLC, ovarian Ca (other female genital Ca), breast Ca or Hodgkin’s Symptoms usually predate cancer dx: • Diffuse dysfunction of cerebellum: • Dysarthria, oculomotor dysfunction • Appendicular and gait ataxia • Many superimposed signs of multifocal encephalomyelitis • May also have LEMS or PN • Deficits worsen for weeks-months then stabilize • Few can walk, feed selves or sit Anti-Yo (PCA-1) (anti-Tr, anti-Ri, anti-Ma, anti-Hu)
Cerebellar degeneration Majority have SCLC, ovarian Ca (other female genital Ca), breast Ca or Hodgkin’s Symptoms usually predate cancer dx: • Diffuse dysfunction of cerebellum: • Dysarthria, oculomotor dysfunction • Appendicular and gait ataxia • Many superimposed signs of multifocal encephalomyelitis • May also have LEMS or PN • Deficits worsen for weeks-months then stabilize • Few can walk, feed selves or sit Anti-Yo (PCA-1) (anti-Tr, anti-Ri, anti-Ma, anti-Hu)
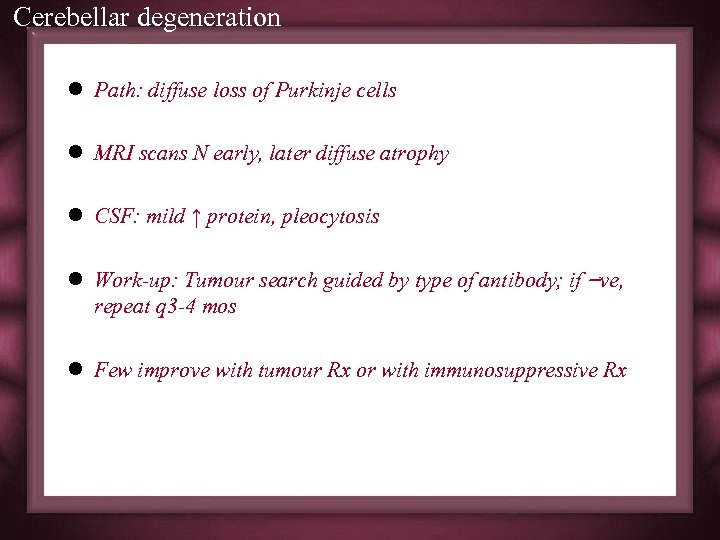 Cerebellar degeneration l Path: diffuse loss of Purkinje cells l MRI scans N early, later diffuse atrophy l CSF: mild ↑ protein, pleocytosis l Work-up: Tumour search guided by type of antibody; if –ve, repeat q 3 -4 mos l Few improve with tumour Rx or with immunosuppressive Rx
Cerebellar degeneration l Path: diffuse loss of Purkinje cells l MRI scans N early, later diffuse atrophy l CSF: mild ↑ protein, pleocytosis l Work-up: Tumour search guided by type of antibody; if –ve, repeat q 3 -4 mos l Few improve with tumour Rx or with immunosuppressive Rx
 Cerebellar degeneration
Cerebellar degeneration
 Cerebellar degeneration
Cerebellar degeneration
 Opsoclonous - myoclonus l l l l l Usually disorder of children, ½ have neuroblastoma Symptoms develop before or after tumour found, fluctuate Respond to tumour Rx and ACTH, profound deficits freq Adult syndrome also ass’d with ataxia/falls, precedes tumour Dx – SCLC, Ca breast Paraneoplastic clinically worse than idiopathic, does not respond as well to Rx, progresses more MRI normal, CSF protein ↑ Antibodies: Anti-Ri (ANNA-2), occ PCA-1, anti-Hu Adult work-up: mammo, pelvic exam & imaging, CEA, CA-125; smokers CT or MRI chest Better outcome than PCD or encephalomyelitis Rx with steroids, ACTH, tumour Rx
Opsoclonous - myoclonus l l l l l Usually disorder of children, ½ have neuroblastoma Symptoms develop before or after tumour found, fluctuate Respond to tumour Rx and ACTH, profound deficits freq Adult syndrome also ass’d with ataxia/falls, precedes tumour Dx – SCLC, Ca breast Paraneoplastic clinically worse than idiopathic, does not respond as well to Rx, progresses more MRI normal, CSF protein ↑ Antibodies: Anti-Ri (ANNA-2), occ PCA-1, anti-Hu Adult work-up: mammo, pelvic exam & imaging, CEA, CA-125; smokers CT or MRI chest Better outcome than PCD or encephalomyelitis Rx with steroids, ACTH, tumour Rx
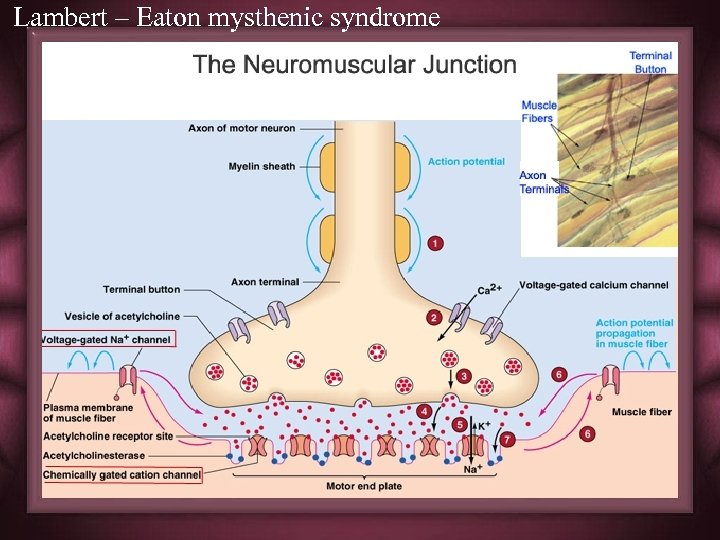
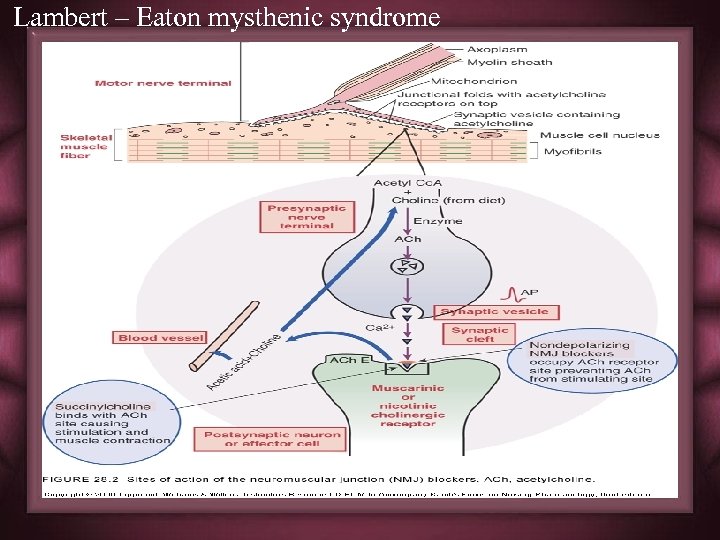
 Lambert – Eaton mysthenic syndrome l Associated with cancer in 40 -70%, SCLC l Presynaptic inhib release of quanta of ACh at NMJ l Syndrome precedes tumour discovery in most, by up to 5 y l fatigue, proximal weakness, muscle aches, autonomic dysfunction(dry mouth, constipation, impotence), paresthesias l Reflexes absent, improve after voluntary contraction (facilitation)
Lambert – Eaton mysthenic syndrome l Associated with cancer in 40 -70%, SCLC l Presynaptic inhib release of quanta of ACh at NMJ l Syndrome precedes tumour discovery in most, by up to 5 y l fatigue, proximal weakness, muscle aches, autonomic dysfunction(dry mouth, constipation, impotence), paresthesias l Reflexes absent, improve after voluntary contraction (facilitation)
 Lambert – Eaton mysthenic syndrome l Isolated ocular weakness virtually exclude the diagnosis l Reduced CMAP on rep stim, ↑ with facilitation, jitter on SFEMG l Antibody found, usually N- or P/Q-type Cachannel Ab’s (occ ANNA-1) l Indistinguishable from non- paraneoplastic but later may be in younger female l Non PN –LEMS associated with autoimmune Thyroiditis and IDDM l 3, 4 Diaminopyridine, or combination of pyrodistigmine and guanidine l IVIG, PE, Immunesuppression(azathioprine)
Lambert – Eaton mysthenic syndrome l Isolated ocular weakness virtually exclude the diagnosis l Reduced CMAP on rep stim, ↑ with facilitation, jitter on SFEMG l Antibody found, usually N- or P/Q-type Cachannel Ab’s (occ ANNA-1) l Indistinguishable from non- paraneoplastic but later may be in younger female l Non PN –LEMS associated with autoimmune Thyroiditis and IDDM l 3, 4 Diaminopyridine, or combination of pyrodistigmine and guanidine l IVIG, PE, Immunesuppression(azathioprine)
 Lambert – Eaton mysthenic syndrome
Lambert – Eaton mysthenic syndrome
 Lambert – Eaton mysthenic syndrome l D-Penicillamine should never be used l Following produce worsening of weakness in most. Use with caution a. Succinylcholine b. D-tubocurarine, other neuromuscular-blocking agents c. Quinine, quinidine, and procainamide d. Aminoglycoside Abx, particularly gentamicin e. Beta blockers f. Calcium-channel blockers g. Magnesium salts (incl. laxatives and antacids) h. Iodinated contrast
Lambert – Eaton mysthenic syndrome l D-Penicillamine should never be used l Following produce worsening of weakness in most. Use with caution a. Succinylcholine b. D-tubocurarine, other neuromuscular-blocking agents c. Quinine, quinidine, and procainamide d. Aminoglycoside Abx, particularly gentamicin e. Beta blockers f. Calcium-channel blockers g. Magnesium salts (incl. laxatives and antacids) h. Iodinated contrast
 Lambert – Eaton mysthenic syndrome
Lambert – Eaton mysthenic syndrome
 Stiff person syndrome l 3 similar syndromes – original “stiff-person syndrome” with anti-GAD antibodies – multifocal PREM affecting spinal interneurons l. SCLC, thymoma, Ca breast/colon laching/rigidity axial muscles, painful spasms – anti-amphiphysin stiff-person syndrome lbreast/SCLC lsimilar to multifocal PREM l Treatment with baclofen, clonazepam, diazepam in high doses and Often respond to steroids
Stiff person syndrome l 3 similar syndromes – original “stiff-person syndrome” with anti-GAD antibodies – multifocal PREM affecting spinal interneurons l. SCLC, thymoma, Ca breast/colon laching/rigidity axial muscles, painful spasms – anti-amphiphysin stiff-person syndrome lbreast/SCLC lsimilar to multifocal PREM l Treatment with baclofen, clonazepam, diazepam in high doses and Often respond to steroids
 Extrapyramidal symptoms • Although only reported as case reports or small series, extrapyramidal symptoms such as chorea, dystonia, and Parkinson’s disease can also be signs of paraneoplastic encephalitis. . Anti-Hu, anti-Ma, or anti. CRMP 5/CV 2 reactivity has been found in some of these patients.
Extrapyramidal symptoms • Although only reported as case reports or small series, extrapyramidal symptoms such as chorea, dystonia, and Parkinson’s disease can also be signs of paraneoplastic encephalitis. . Anti-Hu, anti-Ma, or anti. CRMP 5/CV 2 reactivity has been found in some of these patients.
 Myelitis • An isolated myelitis is a very rare manifestation of PND. • Pathologically, mostly the grey matter is involved. • Clinically, a motor neuron syndrome, with both flaccid and spastic paresis, may occur. If a part of a paraneoplastic syndrome, most cases will show progression to involve other areas of the brain and peripheral nerves, and CSF testing will show an inflammatory
Myelitis • An isolated myelitis is a very rare manifestation of PND. • Pathologically, mostly the grey matter is involved. • Clinically, a motor neuron syndrome, with both flaccid and spastic paresis, may occur. If a part of a paraneoplastic syndrome, most cases will show progression to involve other areas of the brain and peripheral nerves, and CSF testing will show an inflammatory
 Autonomic neuropathy • Some patients showed progressive autonomic dysfunction with postural dizziness, abdominal pain, and diarrhoea. • Others show disturbances of intestinal motility, such as gastroparesis, intestinal pseudo-obstruction, or oesophageal achalasia. .
Autonomic neuropathy • Some patients showed progressive autonomic dysfunction with postural dizziness, abdominal pain, and diarrhoea. • Others show disturbances of intestinal motility, such as gastroparesis, intestinal pseudo-obstruction, or oesophageal achalasia. .
 Mononeuropathy - Mononeuropathies may also be the first signs of a paraneoplastic disorder, mainly associated with anti-Hu antibodies. Single cranial nerves, especially VIII, may be involved, but also others such as the ulnar nerve.
Mononeuropathy - Mononeuropathies may also be the first signs of a paraneoplastic disorder, mainly associated with anti-Hu antibodies. Single cranial nerves, especially VIII, may be involved, but also others such as the ulnar nerve.
 • Motor-neuron syndromes -According to Forsyth and colleagues, three groups of patients with motor-neuron syndromes and cancer may be distinguished. - The first group are anti-Hu positive, and the paraneoplastic aetiology is proven; their clinical symptoms will progress to involve other areas of the nervous system.
• Motor-neuron syndromes -According to Forsyth and colleagues, three groups of patients with motor-neuron syndromes and cancer may be distinguished. - The first group are anti-Hu positive, and the paraneoplastic aetiology is proven; their clinical symptoms will progress to involve other areas of the nervous system.
 • Motor-neuron syndromes -The second group is women with an upper motor-neuron disease, resembling primary lateral sclerosis, who have an associated breast cancer (but no associated antibodies have been described so far). -The third group is patients with cancer and a motor-neuron syndrome resembling amyotrophic lateral sclerosis, in whom the association is probably coincidental.
• Motor-neuron syndromes -The second group is women with an upper motor-neuron disease, resembling primary lateral sclerosis, who have an associated breast cancer (but no associated antibodies have been described so far). -The third group is patients with cancer and a motor-neuron syndrome resembling amyotrophic lateral sclerosis, in whom the association is probably coincidental.
 Paraneoplastic Immune mediated Disorders of the Muscle l Dermatomyositis/Polymyositis – Debated if more frequent in Ca patients – Dermatomyositis has 15 -20% incidence of Ca, polymyositis 9% • Lung adeno. Ca • all patients (particularly those older than 50 years) shouldundergo cancer screening. – proximal muscle weakness, myalgia, and muscle tenderness. Pharyngeal, esophageal, and neck flexor muscles – purplish discoloration of the eyelids (heliotrope rash) – edema, and erythematous, scaly lesions over the knuckles.
Paraneoplastic Immune mediated Disorders of the Muscle l Dermatomyositis/Polymyositis – Debated if more frequent in Ca patients – Dermatomyositis has 15 -20% incidence of Ca, polymyositis 9% • Lung adeno. Ca • all patients (particularly those older than 50 years) shouldundergo cancer screening. – proximal muscle weakness, myalgia, and muscle tenderness. Pharyngeal, esophageal, and neck flexor muscles – purplish discoloration of the eyelids (heliotrope rash) – edema, and erythematous, scaly lesions over the knuckles.
 Paraneoplastic Immune mediated Disorders of the Muscle Acute necrotizing myopathy • Rare paraneoplastic manifestation of cancer • acute and severe muscle weakness, markedly ↑ ↑ serum muscle enzymes, and extensive muscle necrosis with mild or absent inflammatory infiltrates.
Paraneoplastic Immune mediated Disorders of the Muscle Acute necrotizing myopathy • Rare paraneoplastic manifestation of cancer • acute and severe muscle weakness, markedly ↑ ↑ serum muscle enzymes, and extensive muscle necrosis with mild or absent inflammatory infiltrates.
 Lymphoproliferative disorders l. Myeloma associated with several PND – Most types of neuropathies l. Various forms – acute GBS, CIDP – Antibodies directed against myelin – CSF protein ↑ – Some respond to tumour therapy, but can remit spontaneously
Lymphoproliferative disorders l. Myeloma associated with several PND – Most types of neuropathies l. Various forms – acute GBS, CIDP – Antibodies directed against myelin – CSF protein ↑ – Some respond to tumour therapy, but can remit spontaneously
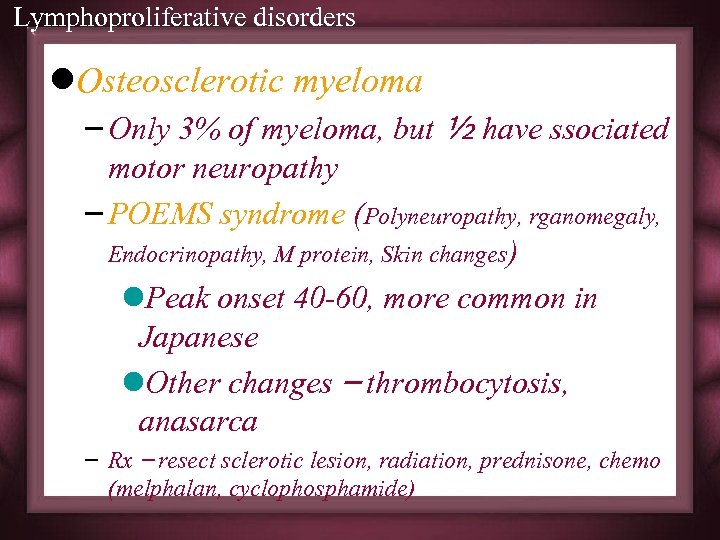 Lymphoproliferative disorders l. Osteosclerotic myeloma – Only 3% of myeloma, but ½ have ssociated motor neuropathy – POEMS syndrome (Polyneuropathy, rganomegaly, Endocrinopathy, M protein, Skin changes) l. Peak onset 40 -60, more common in Japanese l. Other changes – thrombocytosis, anasarca – Rx – resect sclerotic lesion, radiation, prednisone, chemo (melphalan, cyclophosphamide)
Lymphoproliferative disorders l. Osteosclerotic myeloma – Only 3% of myeloma, but ½ have ssociated motor neuropathy – POEMS syndrome (Polyneuropathy, rganomegaly, Endocrinopathy, M protein, Skin changes) l. Peak onset 40 -60, more common in Japanese l. Other changes – thrombocytosis, anasarca – Rx – resect sclerotic lesion, radiation, prednisone, chemo (melphalan, cyclophosphamide)
 Lymphoproliferative disorders – Paraprotein-associated, amyloid deposition – Dx through immunoelectrophoresis detection of paraprotein, skeletal survey (sclerotic lesion) – CSF protein ↑ – Pathology: mixed axonal/demyelinating
Lymphoproliferative disorders – Paraprotein-associated, amyloid deposition – Dx through immunoelectrophoresis detection of paraprotein, skeletal survey (sclerotic lesion) – CSF protein ↑ – Pathology: mixed axonal/demyelinating
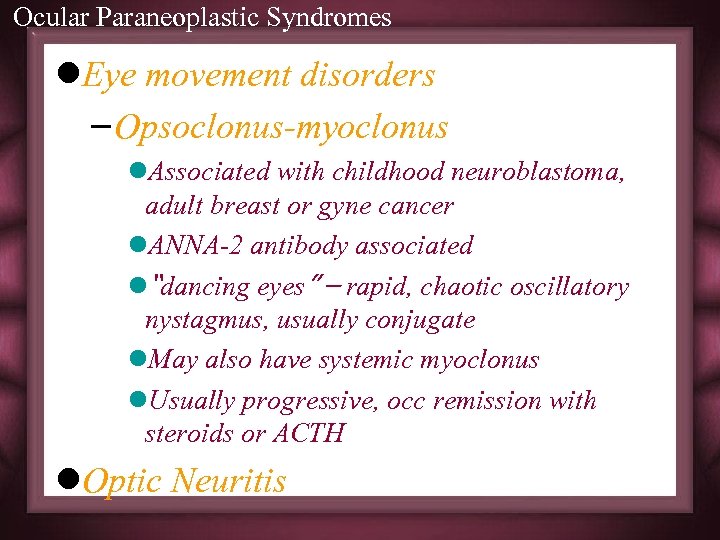 Ocular Paraneoplastic Syndromes l. Eye movement disorders – Opsoclonus-myoclonus l. Associated with childhood neuroblastoma, adult breast or gyne cancer l. ANNA-2 antibody associated l“dancing eyes” – rapid, chaotic oscillatory nystagmus, usually conjugate l. May also have systemic myoclonus l. Usually progressive, occ remission with steroids or ACTH l. Optic Neuritis
Ocular Paraneoplastic Syndromes l. Eye movement disorders – Opsoclonus-myoclonus l. Associated with childhood neuroblastoma, adult breast or gyne cancer l. ANNA-2 antibody associated l“dancing eyes” – rapid, chaotic oscillatory nystagmus, usually conjugate l. May also have systemic myoclonus l. Usually progressive, occ remission with steroids or ACTH l. Optic Neuritis
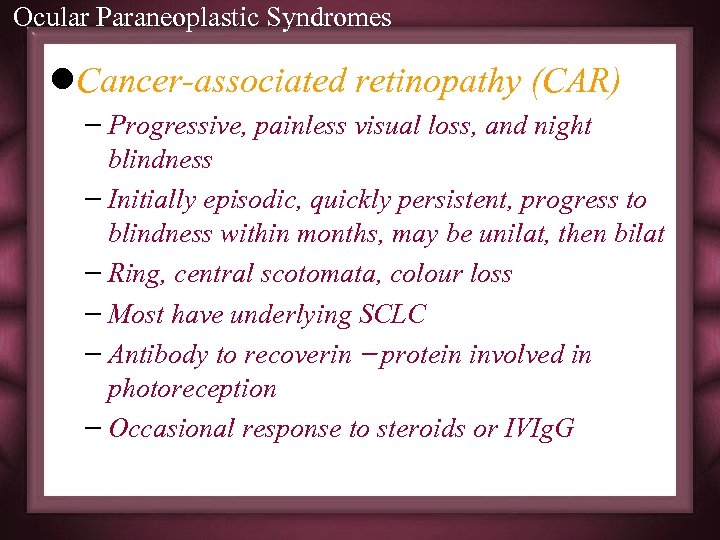 Ocular Paraneoplastic Syndromes l. Cancer-associated retinopathy (CAR) – Progressive, painless visual loss, and night blindness – Initially episodic, quickly persistent, progress to blindness within months, may be unilat, then bilat – Ring, central scotomata, colour loss – Most have underlying SCLC – Antibody to recoverin – protein involved in photoreception – Occasional response to steroids or IVIg. G
Ocular Paraneoplastic Syndromes l. Cancer-associated retinopathy (CAR) – Progressive, painless visual loss, and night blindness – Initially episodic, quickly persistent, progress to blindness within months, may be unilat, then bilat – Ring, central scotomata, colour loss – Most have underlying SCLC – Antibody to recoverin – protein involved in photoreception – Occasional response to steroids or IVIg. G
 DIFFERENTIAL DIAGNOSIS
DIFFERENTIAL DIAGNOSIS
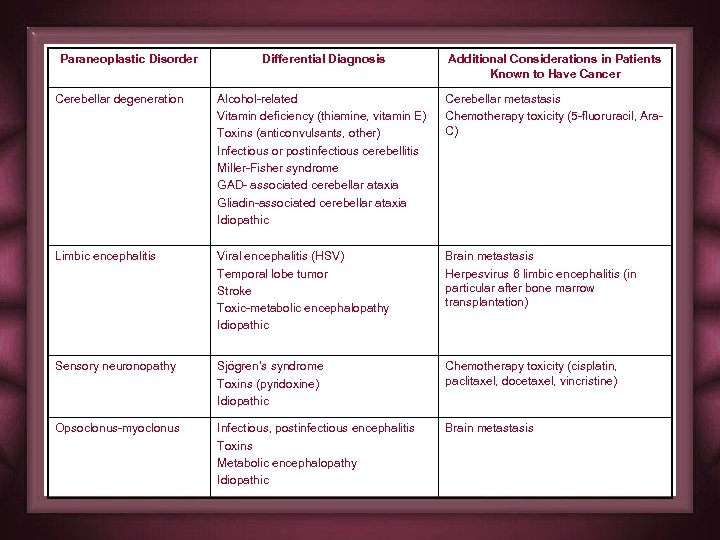 Paraneoplastic Disorder Differential Diagnosis Additional Considerations in Patients Known to Have Cancer Cerebellar degeneration Alcohol-related Vitamin deficiency (thiamine, vitamin E) Toxins (anticonvulsants, other) Infectious or postinfectious cerebellitis Miller-Fisher syndrome GAD- associated cerebellar ataxia Gliadin-associated cerebellar ataxia Idiopathic Cerebellar metastasis Chemotherapy toxicity (5 -fluoruracil, Ara. C) Limbic encephalitis Viral encephalitis (HSV) Temporal lobe tumor Stroke Toxic-metabolic encephalopathy Idiopathic Brain metastasis Herpesvirus 6 limbic encephalitis (in particular after bone marrow transplantation) Sensory neuronopathy Sjögren’s syndrome Toxins (pyridoxine) Idiopathic Chemotherapy toxicity (cisplatin, paclitaxel, docetaxel, vincristine) Opsoclonus-myoclonus Infectious, postinfectious encephalitis Toxins Metabolic encephalopathy Idiopathic Brain metastasis
Paraneoplastic Disorder Differential Diagnosis Additional Considerations in Patients Known to Have Cancer Cerebellar degeneration Alcohol-related Vitamin deficiency (thiamine, vitamin E) Toxins (anticonvulsants, other) Infectious or postinfectious cerebellitis Miller-Fisher syndrome GAD- associated cerebellar ataxia Gliadin-associated cerebellar ataxia Idiopathic Cerebellar metastasis Chemotherapy toxicity (5 -fluoruracil, Ara. C) Limbic encephalitis Viral encephalitis (HSV) Temporal lobe tumor Stroke Toxic-metabolic encephalopathy Idiopathic Brain metastasis Herpesvirus 6 limbic encephalitis (in particular after bone marrow transplantation) Sensory neuronopathy Sjögren’s syndrome Toxins (pyridoxine) Idiopathic Chemotherapy toxicity (cisplatin, paclitaxel, docetaxel, vincristine) Opsoclonus-myoclonus Infectious, postinfectious encephalitis Toxins Metabolic encephalopathy Idiopathic Brain metastasis
 INVESTIGATIONS
INVESTIGATIONS
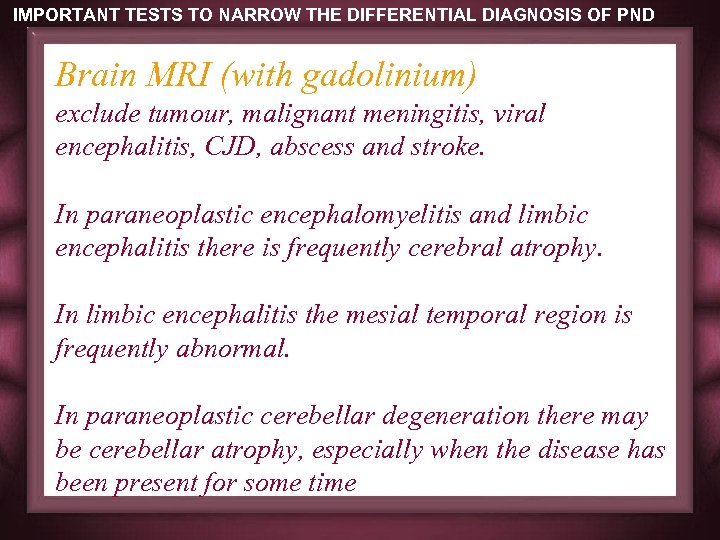 IMPORTANT TESTS TO NARROW THE DIFFERENTIAL DIAGNOSIS OF PND Brain MRI (with gadolinium) exclude tumour, malignant meningitis, viral encephalitis, CJD, abscess and stroke. In paraneoplastic encephalomyelitis and limbic encephalitis there is frequently cerebral atrophy. In limbic encephalitis the mesial temporal region is frequently abnormal. In paraneoplastic cerebellar degeneration there may be cerebellar atrophy, especially when the disease has been present for some time
IMPORTANT TESTS TO NARROW THE DIFFERENTIAL DIAGNOSIS OF PND Brain MRI (with gadolinium) exclude tumour, malignant meningitis, viral encephalitis, CJD, abscess and stroke. In paraneoplastic encephalomyelitis and limbic encephalitis there is frequently cerebral atrophy. In limbic encephalitis the mesial temporal region is frequently abnormal. In paraneoplastic cerebellar degeneration there may be cerebellar atrophy, especially when the disease has been present for some time
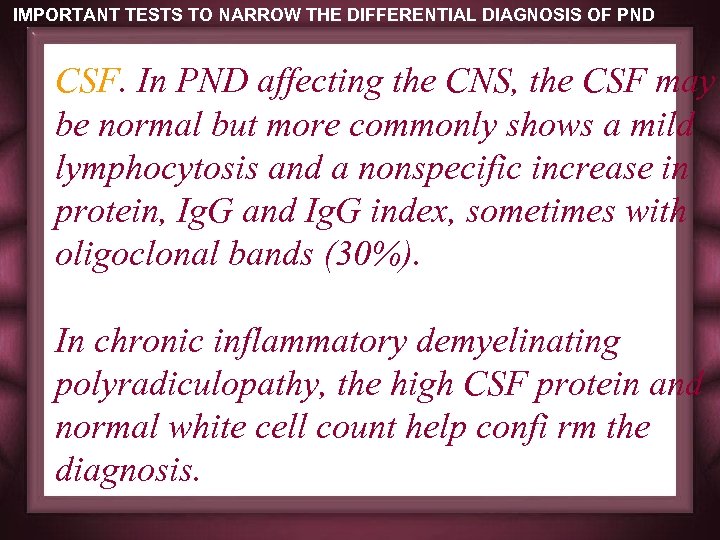 IMPORTANT TESTS TO NARROW THE DIFFERENTIAL DIAGNOSIS OF PND CSF. In PND affecting the CNS, the CSF may be normal but more commonly shows a mild lymphocytosis and a nonspecific increase in protein, Ig. G and Ig. G index, sometimes with oligoclonal bands (30%). In chronic inflammatory demyelinating polyradiculopathy, the high CSF protein and normal white cell count help confi rm the diagnosis.
IMPORTANT TESTS TO NARROW THE DIFFERENTIAL DIAGNOSIS OF PND CSF. In PND affecting the CNS, the CSF may be normal but more commonly shows a mild lymphocytosis and a nonspecific increase in protein, Ig. G and Ig. G index, sometimes with oligoclonal bands (30%). In chronic inflammatory demyelinating polyradiculopathy, the high CSF protein and normal white cell count help confi rm the diagnosis.
 IMPORTANT TESTS TO NARROW THE DIFFERENTIAL DIAGNOSIS OF PND Electroencephalogram exclude herpes simplex encephalitis, nonconvulsive status and CJD. It may show slowing over the temporal lobes or frontally in limbic encephalitis and PEM Electro-retinogram is flat in most cases of paraneoplastic retinopathy even though vision may be retained. In melanoma-associated retinopathy the dark adapted B wave has reduced amplitude.
IMPORTANT TESTS TO NARROW THE DIFFERENTIAL DIAGNOSIS OF PND Electroencephalogram exclude herpes simplex encephalitis, nonconvulsive status and CJD. It may show slowing over the temporal lobes or frontally in limbic encephalitis and PEM Electro-retinogram is flat in most cases of paraneoplastic retinopathy even though vision may be retained. In melanoma-associated retinopathy the dark adapted B wave has reduced amplitude.
 IMPORTANT TESTS TO NARROW THE DIFFERENTIAL DIAGNOSIS OF PND Neurophysiology. In paraneoplastic sensory neuropathy, nerve conduction usually confirms the sensory neuropathy with reduced amplitude of SNAP in the presence of normal motor amplitudes and conduction. In LEMS, will demonstrate reduced amplitude of the compound muscle action potential with single supramaximal stimulation; an increase after exercise (postexercise facilitation); a decremental response to repetitive stimulation at 3 Hz; an incremental response > 200% at > 30 Hz; and increased jitter on single fibre EMG
IMPORTANT TESTS TO NARROW THE DIFFERENTIAL DIAGNOSIS OF PND Neurophysiology. In paraneoplastic sensory neuropathy, nerve conduction usually confirms the sensory neuropathy with reduced amplitude of SNAP in the presence of normal motor amplitudes and conduction. In LEMS, will demonstrate reduced amplitude of the compound muscle action potential with single supramaximal stimulation; an increase after exercise (postexercise facilitation); a decremental response to repetitive stimulation at 3 Hz; an incremental response > 200% at > 30 Hz; and increased jitter on single fibre EMG
 IMPORTANT TESTS TO NARROW THE DIFFERENTIAL DIAGNOSIS OF PND Tensilon test is not usually necessary although it is sometimes positive in LEMS, but seldom dramatically. It may give some idea of how the patient might respond to pyridostigmine. Biopsies. Brain biopsy is seldom indicated except perhaps in some antibody negative cases to exclude cerebral vasculitis or intravascular lymphoma. Sural nerve biopsy is very rarely needed to exclude vasculitis, demyelination or lymphomatous infi ltration of the nerves. Muscle biopsy may exclude myositis or myopathy in the occasional diffi cult case.
IMPORTANT TESTS TO NARROW THE DIFFERENTIAL DIAGNOSIS OF PND Tensilon test is not usually necessary although it is sometimes positive in LEMS, but seldom dramatically. It may give some idea of how the patient might respond to pyridostigmine. Biopsies. Brain biopsy is seldom indicated except perhaps in some antibody negative cases to exclude cerebral vasculitis or intravascular lymphoma. Sural nerve biopsy is very rarely needed to exclude vasculitis, demyelination or lymphomatous infi ltration of the nerves. Muscle biopsy may exclude myositis or myopathy in the occasional diffi cult case.
 TREATMENT
TREATMENT
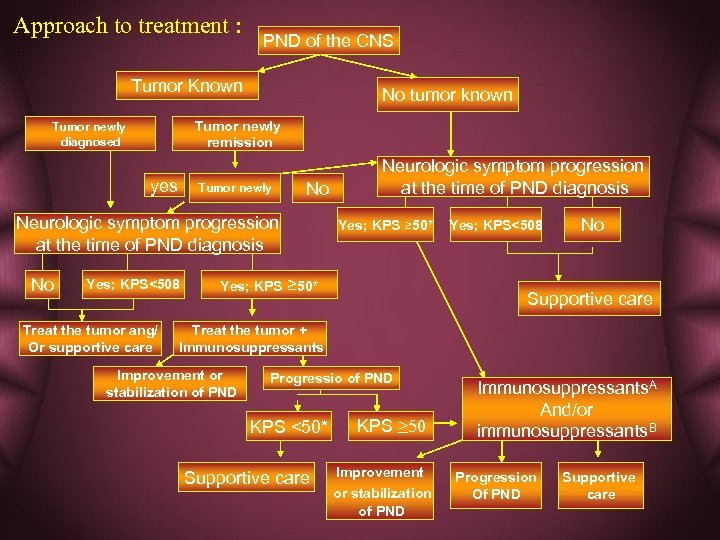 Approach to treatment : PND of the CNS Tumor Known No tumor known Tumor newly remission Tumor newly diagnosed yes Tumor newly No Neurologic symptom progression at the time of PND diagnosis No Yes; KPS<508 Treat the tumor ang/ Or supportive care Yes; KPS Neurologic symptom progression at the time of PND diagnosis Yes; KPS ≥ 50* Yes; KPS<508 No Supportive care Treat the tumor + Immunosuppressants Improvement or stabilization of PND Progressio of PND KPS <50* Supportive care KPS ≥ 50 Improvement or stabilization of PND Immunosuppressants. A And/or immunosuppressants. B Progression Of PND Supportive care
Approach to treatment : PND of the CNS Tumor Known No tumor known Tumor newly remission Tumor newly diagnosed yes Tumor newly No Neurologic symptom progression at the time of PND diagnosis No Yes; KPS<508 Treat the tumor ang/ Or supportive care Yes; KPS Neurologic symptom progression at the time of PND diagnosis Yes; KPS ≥ 50* Yes; KPS<508 No Supportive care Treat the tumor + Immunosuppressants Improvement or stabilization of PND Progressio of PND KPS <50* Supportive care KPS ≥ 50 Improvement or stabilization of PND Immunosuppressants. A And/or immunosuppressants. B Progression Of PND Supportive care
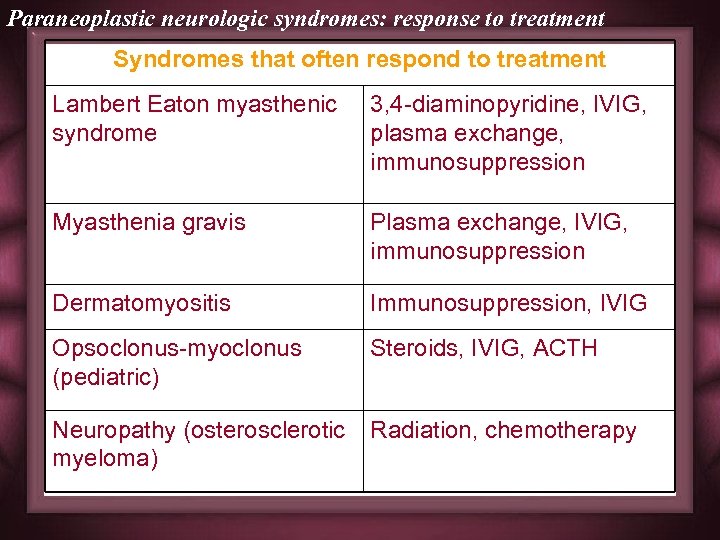 Paraneoplastic neurologic syndromes: response to treatment Syndromes that often respond to treatment Lambert Eaton myasthenic syndrome 3, 4 -diaminopyridine, IVIG, plasma exchange, immunosuppression Myasthenia gravis Plasma exchange, IVIG, immunosuppression Dermatomyositis Immunosuppression, IVIG Opsoclonus-myoclonus (pediatric) Steroids, IVIG, ACTH Neuropathy (osterosclerotic myeloma) Radiation, chemotherapy
Paraneoplastic neurologic syndromes: response to treatment Syndromes that often respond to treatment Lambert Eaton myasthenic syndrome 3, 4 -diaminopyridine, IVIG, plasma exchange, immunosuppression Myasthenia gravis Plasma exchange, IVIG, immunosuppression Dermatomyositis Immunosuppression, IVIG Opsoclonus-myoclonus (pediatric) Steroids, IVIG, ACTH Neuropathy (osterosclerotic myeloma) Radiation, chemotherapy
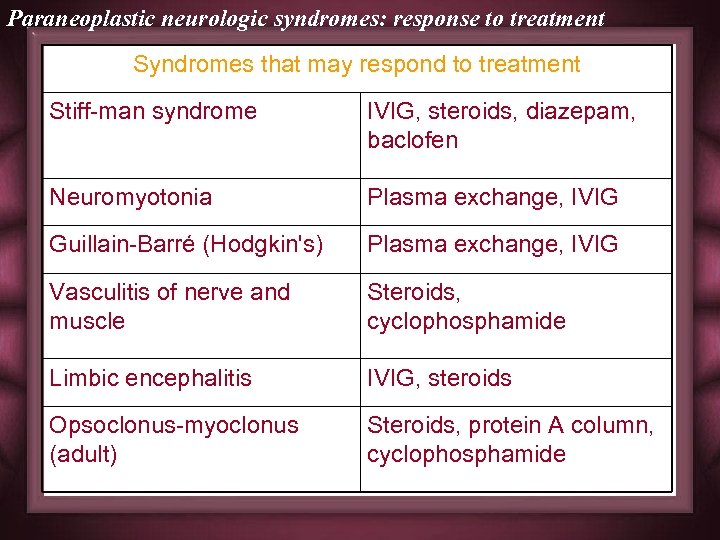 Paraneoplastic neurologic syndromes: response to treatment Syndromes that may respond to treatment Stiff-man syndrome IVIG, steroids, diazepam, baclofen Neuromyotonia Plasma exchange, IVIG Guillain-Barré (Hodgkin's) Plasma exchange, IVIG Vasculitis of nerve and muscle Steroids, cyclophosphamide Limbic encephalitis IVIG, steroids Opsoclonus-myoclonus (adult) Steroids, protein A column, cyclophosphamide
Paraneoplastic neurologic syndromes: response to treatment Syndromes that may respond to treatment Stiff-man syndrome IVIG, steroids, diazepam, baclofen Neuromyotonia Plasma exchange, IVIG Guillain-Barré (Hodgkin's) Plasma exchange, IVIG Vasculitis of nerve and muscle Steroids, cyclophosphamide Limbic encephalitis IVIG, steroids Opsoclonus-myoclonus (adult) Steroids, protein A column, cyclophosphamide
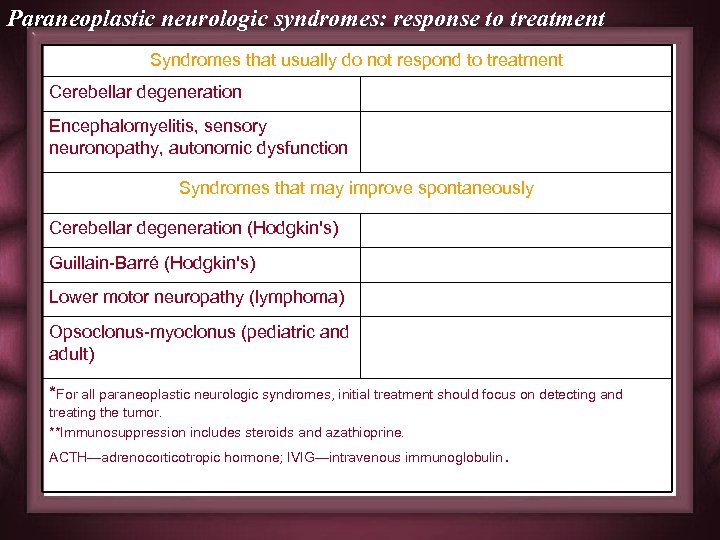 Paraneoplastic neurologic syndromes: response to treatment Syndromes that usually do not respond to treatment Cerebellar degeneration Encephalomyelitis, sensory neuronopathy, autonomic dysfunction Syndromes that may improve spontaneously Cerebellar degeneration (Hodgkin's) Guillain-Barré (Hodgkin's) Lower motor neuropathy (lymphoma) Opsoclonus-myoclonus (pediatric and adult) *For all paraneoplastic neurologic syndromes, initial treatment should focus on detecting and treating the tumor. **Immunosuppression includes steroids and azathioprine. ACTH—adrenocorticotropic hormone; IVIG—intravenous immunoglobulin.
Paraneoplastic neurologic syndromes: response to treatment Syndromes that usually do not respond to treatment Cerebellar degeneration Encephalomyelitis, sensory neuronopathy, autonomic dysfunction Syndromes that may improve spontaneously Cerebellar degeneration (Hodgkin's) Guillain-Barré (Hodgkin's) Lower motor neuropathy (lymphoma) Opsoclonus-myoclonus (pediatric and adult) *For all paraneoplastic neurologic syndromes, initial treatment should focus on detecting and treating the tumor. **Immunosuppression includes steroids and azathioprine. ACTH—adrenocorticotropic hormone; IVIG—intravenous immunoglobulin.
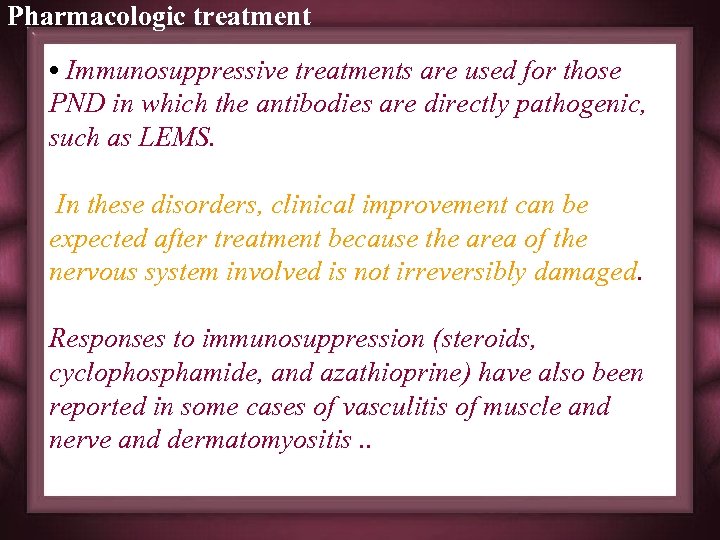 Pharmacologic treatment • Immunosuppressive treatments are used for those PND in which the antibodies are directly pathogenic, such as LEMS. In these disorders, clinical improvement can be expected after treatment because the area of the nervous system involved is not irreversibly damaged. Responses to immunosuppression (steroids, cyclophosphamide, and azathioprine) have also been reported in some cases of vasculitis of muscle and nerve and dermatomyositis. .
Pharmacologic treatment • Immunosuppressive treatments are used for those PND in which the antibodies are directly pathogenic, such as LEMS. In these disorders, clinical improvement can be expected after treatment because the area of the nervous system involved is not irreversibly damaged. Responses to immunosuppression (steroids, cyclophosphamide, and azathioprine) have also been reported in some cases of vasculitis of muscle and nerve and dermatomyositis. .
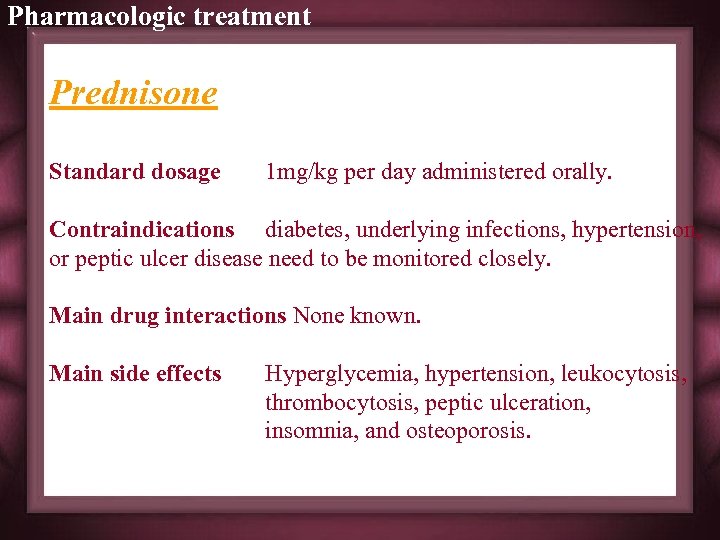 Pharmacologic treatment Prednisone Standard dosage 1 mg/kg per day administered orally. Contraindications diabetes, underlying infections, hypertension, or peptic ulcer disease need to be monitored closely. Main drug interactions None known. Main side effects Hyperglycemia, hypertension, leukocytosis, thrombocytosis, peptic ulceration, insomnia, and osteoporosis.
Pharmacologic treatment Prednisone Standard dosage 1 mg/kg per day administered orally. Contraindications diabetes, underlying infections, hypertension, or peptic ulcer disease need to be monitored closely. Main drug interactions None known. Main side effects Hyperglycemia, hypertension, leukocytosis, thrombocytosis, peptic ulceration, insomnia, and osteoporosis.
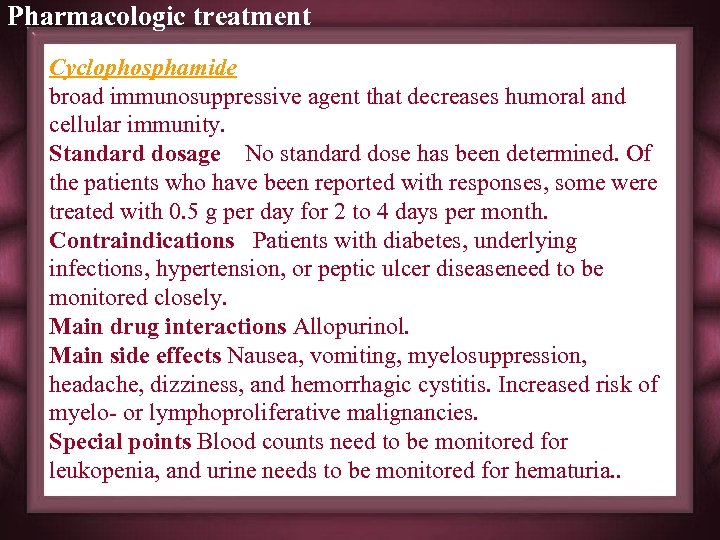 Pharmacologic treatment Cyclophosphamide broad immunosuppressive agent that decreases humoral and cellular immunity. Standard dosage No standard dose has been determined. Of the patients who have been reported with responses, some were treated with 0. 5 g per day for 2 to 4 days per month. Contraindications Patients with diabetes, underlying infections, hypertension, or peptic ulcer diseaseneed to be monitored closely. Main drug interactions Allopurinol. Main side effects Nausea, vomiting, myelosuppression, headache, dizziness, and hemorrhagic cystitis. Increased risk of myelo- or lymphoproliferative malignancies. Special points Blood counts need to be monitored for leukopenia, and urine needs to be monitored for hematuria. .
Pharmacologic treatment Cyclophosphamide broad immunosuppressive agent that decreases humoral and cellular immunity. Standard dosage No standard dose has been determined. Of the patients who have been reported with responses, some were treated with 0. 5 g per day for 2 to 4 days per month. Contraindications Patients with diabetes, underlying infections, hypertension, or peptic ulcer diseaseneed to be monitored closely. Main drug interactions Allopurinol. Main side effects Nausea, vomiting, myelosuppression, headache, dizziness, and hemorrhagic cystitis. Increased risk of myelo- or lymphoproliferative malignancies. Special points Blood counts need to be monitored for leukopenia, and urine needs to be monitored for hematuria. .
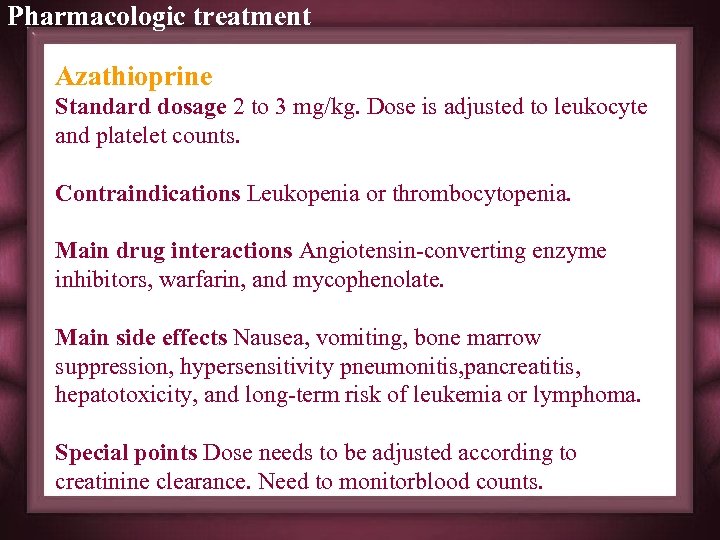 Pharmacologic treatment Azathioprine Standard dosage 2 to 3 mg/kg. Dose is adjusted to leukocyte and platelet counts. Contraindications Leukopenia or thrombocytopenia. Main drug interactions Angiotensin-converting enzyme inhibitors, warfarin, and mycophenolate. Main side effects Nausea, vomiting, bone marrow suppression, hypersensitivity pneumonitis, pancreatitis, hepatotoxicity, and long-term risk of leukemia or lymphoma. Special points Dose needs to be adjusted according to creatinine clearance. Need to monitorblood counts.
Pharmacologic treatment Azathioprine Standard dosage 2 to 3 mg/kg. Dose is adjusted to leukocyte and platelet counts. Contraindications Leukopenia or thrombocytopenia. Main drug interactions Angiotensin-converting enzyme inhibitors, warfarin, and mycophenolate. Main side effects Nausea, vomiting, bone marrow suppression, hypersensitivity pneumonitis, pancreatitis, hepatotoxicity, and long-term risk of leukemia or lymphoma. Special points Dose needs to be adjusted according to creatinine clearance. Need to monitorblood counts.
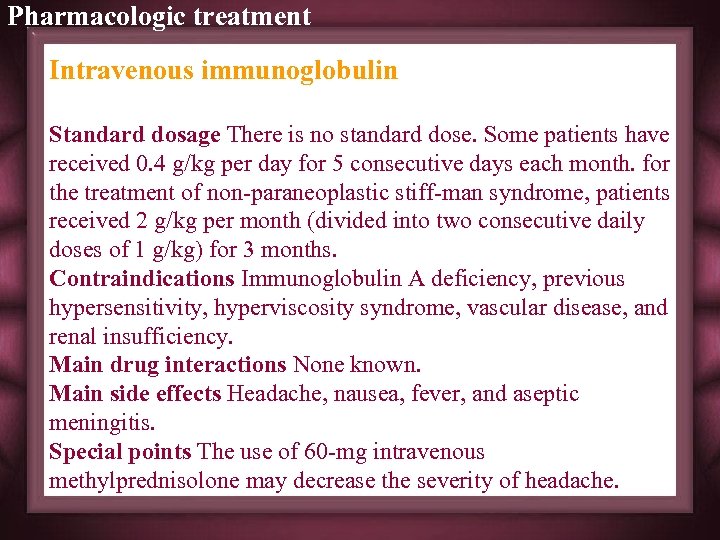 Pharmacologic treatment Intravenous immunoglobulin Standard dosage There is no standard dose. Some patients have received 0. 4 g/kg per day for 5 consecutive days each month. for the treatment of non-paraneoplastic stiff-man syndrome, patients received 2 g/kg per month (divided into two consecutive daily doses of 1 g/kg) for 3 months. Contraindications Immunoglobulin A deficiency, previous hypersensitivity, hyperviscosity syndrome, vascular disease, and renal insufficiency. Main drug interactions None known. Main side effects Headache, nausea, fever, and aseptic meningitis. Special points The use of 60 -mg intravenous methylprednisolone may decrease the severity of headache.
Pharmacologic treatment Intravenous immunoglobulin Standard dosage There is no standard dose. Some patients have received 0. 4 g/kg per day for 5 consecutive days each month. for the treatment of non-paraneoplastic stiff-man syndrome, patients received 2 g/kg per month (divided into two consecutive daily doses of 1 g/kg) for 3 months. Contraindications Immunoglobulin A deficiency, previous hypersensitivity, hyperviscosity syndrome, vascular disease, and renal insufficiency. Main drug interactions None known. Main side effects Headache, nausea, fever, and aseptic meningitis. Special points The use of 60 -mg intravenous methylprednisolone may decrease the severity of headache.
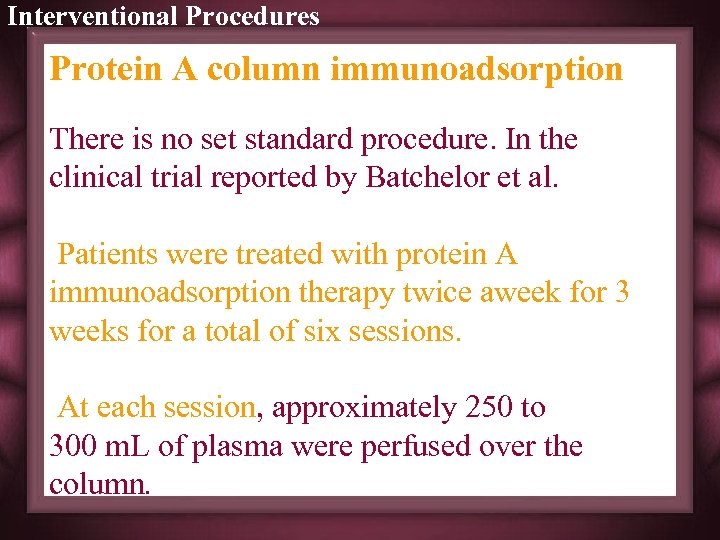 Interventional Procedures Protein A column immunoadsorption There is no set standard procedure. In the clinical trial reported by Batchelor et al. Patients were treated with protein A immunoadsorption therapy twice aweek for 3 weeks for a total of six sessions. At each session, approximately 250 to 300 m. L of plasma were perfused over the column.
Interventional Procedures Protein A column immunoadsorption There is no set standard procedure. In the clinical trial reported by Batchelor et al. Patients were treated with protein A immunoadsorption therapy twice aweek for 3 weeks for a total of six sessions. At each session, approximately 250 to 300 m. L of plasma were perfused over the column.
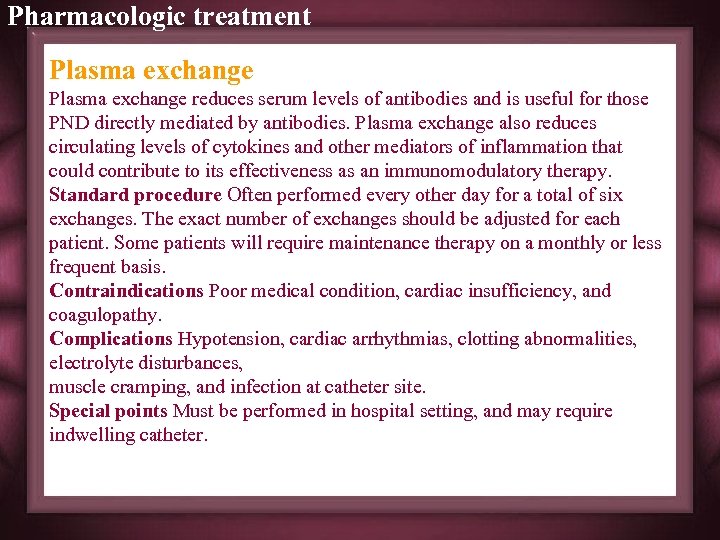 Pharmacologic treatment Plasma exchange reduces serum levels of antibodies and is useful for those PND directly mediated by antibodies. Plasma exchange also reduces circulating levels of cytokines and other mediators of inflammation that could contribute to its effectiveness as an immunomodulatory therapy. Standard procedure Often performed every other day for a total of six exchanges. The exact number of exchanges should be adjusted for each patient. Some patients will require maintenance therapy on a monthly or less frequent basis. Contraindications Poor medical condition, cardiac insufficiency, and coagulopathy. Complications Hypotension, cardiac arrhythmias, clotting abnormalities, electrolyte disturbances, muscle cramping, and infection at catheter site. Special points Must be performed in hospital setting, and may require indwelling catheter.
Pharmacologic treatment Plasma exchange reduces serum levels of antibodies and is useful for those PND directly mediated by antibodies. Plasma exchange also reduces circulating levels of cytokines and other mediators of inflammation that could contribute to its effectiveness as an immunomodulatory therapy. Standard procedure Often performed every other day for a total of six exchanges. The exact number of exchanges should be adjusted for each patient. Some patients will require maintenance therapy on a monthly or less frequent basis. Contraindications Poor medical condition, cardiac insufficiency, and coagulopathy. Complications Hypotension, cardiac arrhythmias, clotting abnormalities, electrolyte disturbances, muscle cramping, and infection at catheter site. Special points Must be performed in hospital setting, and may require indwelling catheter.
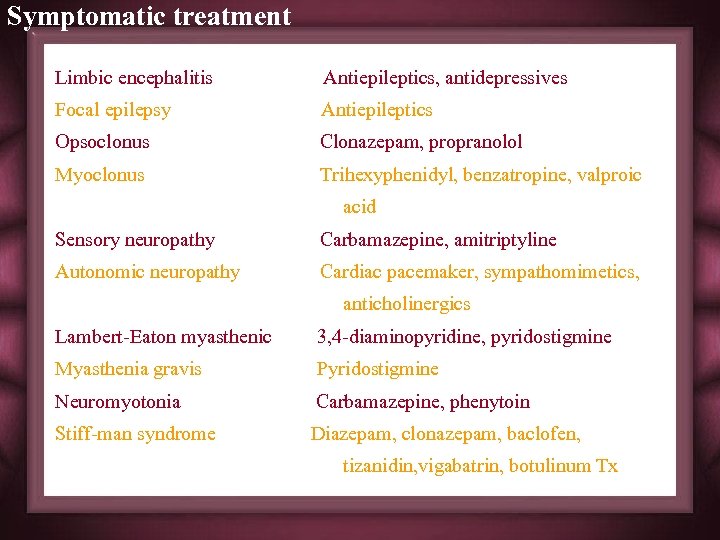 Symptomatic treatment Limbic encephalitis Antiepileptics, antidepressives Focal epilepsy Antiepileptics Opsoclonus Clonazepam, propranolol Myoclonus Trihexyphenidyl, benzatropine, valproic acid Sensory neuropathy Carbamazepine, amitriptyline Autonomic neuropathy Cardiac pacemaker, sympathomimetics, anticholinergics Lambert-Eaton myasthenic 3, 4 -diaminopyridine, pyridostigmine Myasthenia gravis Pyridostigmine Neuromyotonia Carbamazepine, phenytoin Stiff-man syndrome Diazepam, clonazepam, baclofen, tizanidin, vigabatrin, botulinum Tx
Symptomatic treatment Limbic encephalitis Antiepileptics, antidepressives Focal epilepsy Antiepileptics Opsoclonus Clonazepam, propranolol Myoclonus Trihexyphenidyl, benzatropine, valproic acid Sensory neuropathy Carbamazepine, amitriptyline Autonomic neuropathy Cardiac pacemaker, sympathomimetics, anticholinergics Lambert-Eaton myasthenic 3, 4 -diaminopyridine, pyridostigmine Myasthenia gravis Pyridostigmine Neuromyotonia Carbamazepine, phenytoin Stiff-man syndrome Diazepam, clonazepam, baclofen, tizanidin, vigabatrin, botulinum Tx
 GENERAL COMMENTS
GENERAL COMMENTS
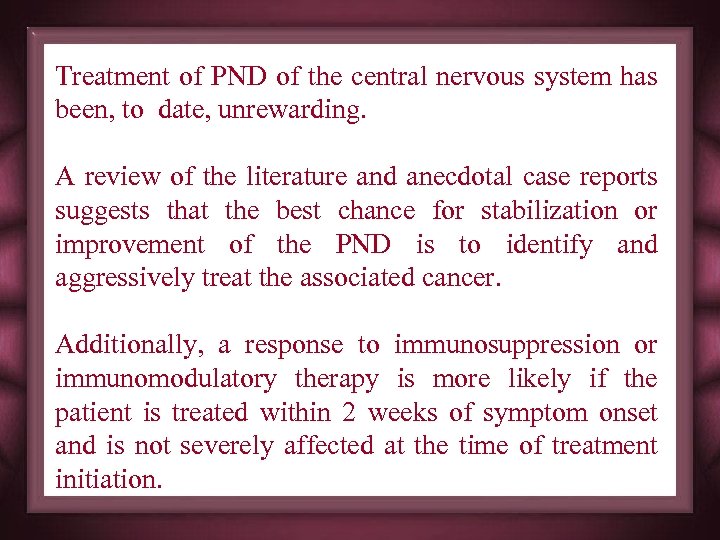 Treatment of PND of the central nervous system has been, to date, unrewarding. A review of the literature and anecdotal case reports suggests that the best chance for stabilization or improvement of the PND is to identify and aggressively treat the associated cancer. Additionally, a response to immunosuppression or immunomodulatory therapy is more likely if the patient is treated within 2 weeks of symptom onset and is not severely affected at the time of treatment initiation.
Treatment of PND of the central nervous system has been, to date, unrewarding. A review of the literature and anecdotal case reports suggests that the best chance for stabilization or improvement of the PND is to identify and aggressively treat the associated cancer. Additionally, a response to immunosuppression or immunomodulatory therapy is more likely if the patient is treated within 2 weeks of symptom onset and is not severely affected at the time of treatment initiation.
 CASES
CASES

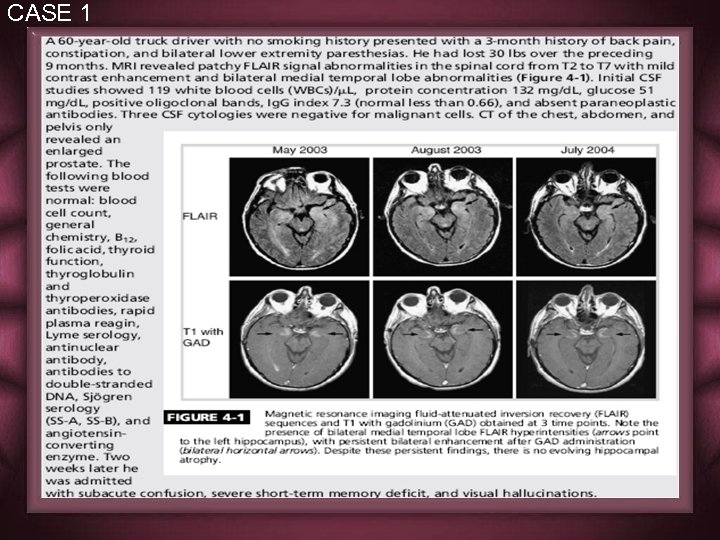 CASE 1
CASE 1
 CASE 1
CASE 1
 CASE 1
CASE 1
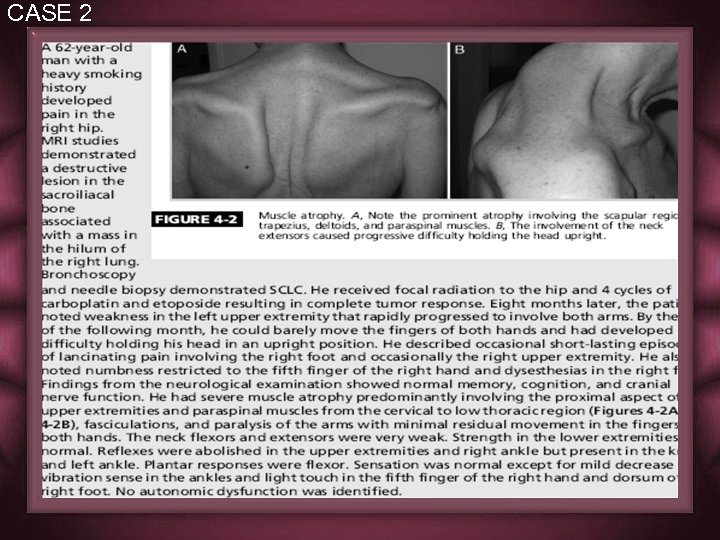 CASE 2
CASE 2
 CASE 2
CASE 2
 CASE 2
CASE 2
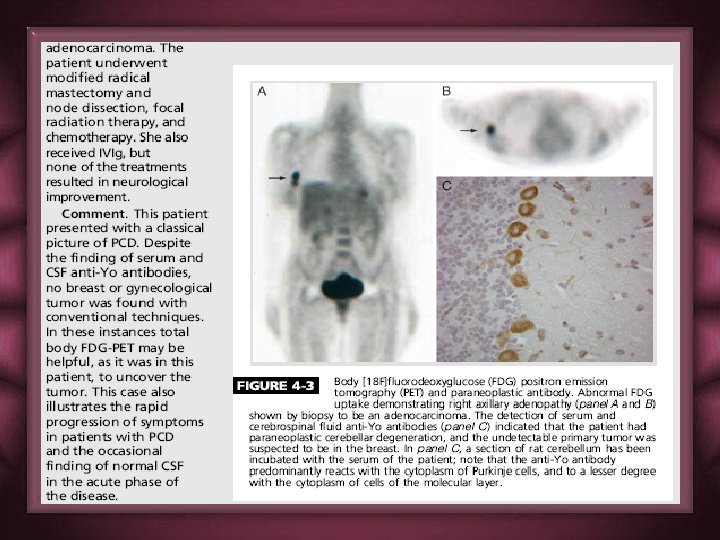
 CASE 3
CASE 3
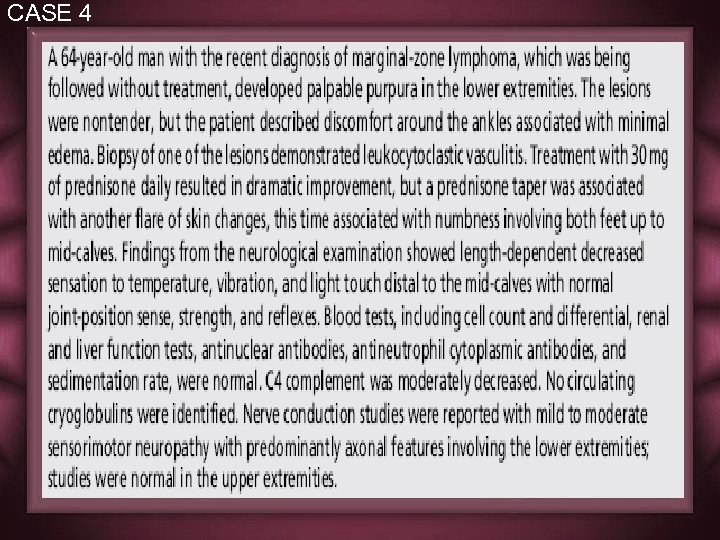 CASE 4
CASE 4
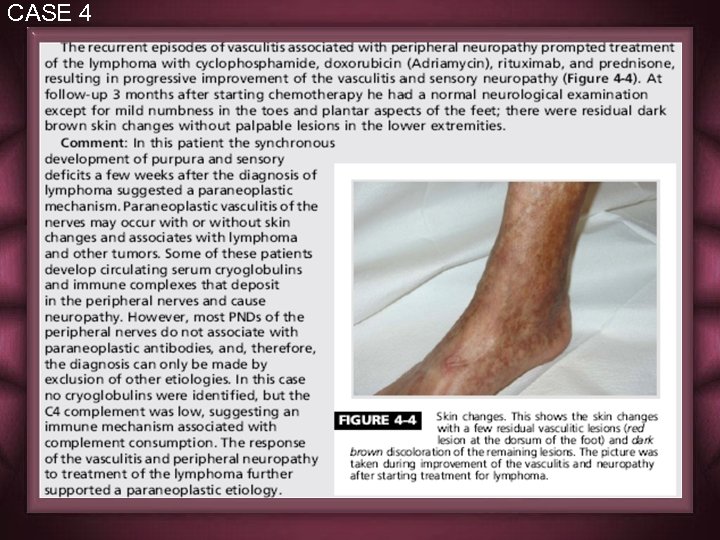 CASE 4
CASE 4



