7dfda7a5e7588a125529d0e1f3fecb8e.ppt
- Количество слайдов: 53
 Decision Support as a Clinical Skill August 2008
Decision Support as a Clinical Skill August 2008
 Workshop Outline n Module 1: Context n n Shared decision making Preference sensitive care Difficult decisions Decisional conflict § Module 2: Decision support process § Ottawa Decision Support Framework § Decision Support § Ottawa Personal Decision Guide § Module 3: Communicating risk information § Module 4: Decision support tools § Decision aids § Other resources
Workshop Outline n Module 1: Context n n Shared decision making Preference sensitive care Difficult decisions Decisional conflict § Module 2: Decision support process § Ottawa Decision Support Framework § Decision Support § Ottawa Personal Decision Guide § Module 3: Communicating risk information § Module 4: Decision support tools § Decision aids § Other resources
 Key Concepts n Shared Decision Making n Effective vs. Preference Sensitive Care n Decisional Conflict n Decision Quality
Key Concepts n Shared Decision Making n Effective vs. Preference Sensitive Care n Decisional Conflict n Decision Quality
 Module 1: Context Shared decision making Values-sensitive care Difficult decisions Decisional conflict
Module 1: Context Shared decision making Values-sensitive care Difficult decisions Decisional conflict
 Shared Decision Making n An integrative process between patient and clinician that: Engages the patient in decision making Ø Provides the patient with information about alternative treatments Ø Facilitates the incorporation of patient preferences and values into the medical plan Ø (Charles C, Soc Sci Med 1997; 44: 681)
Shared Decision Making n An integrative process between patient and clinician that: Engages the patient in decision making Ø Provides the patient with information about alternative treatments Ø Facilitates the incorporation of patient preferences and values into the medical plan Ø (Charles C, Soc Sci Med 1997; 44: 681)
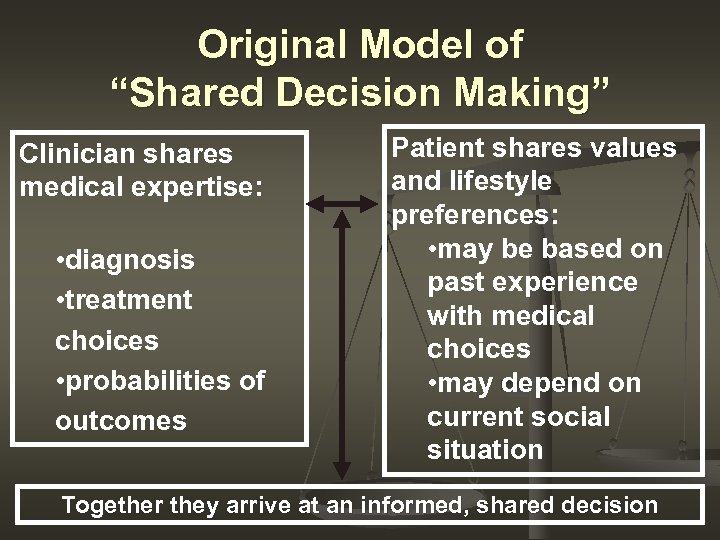 Original Model of “Shared Decision Making” Clinician shares medical expertise: • diagnosis • treatment choices • probabilities of outcomes Patient shares values and lifestyle preferences: • may be based on past experience with medical choices • may depend on current social situation Together they arrive at an informed, shared decision
Original Model of “Shared Decision Making” Clinician shares medical expertise: • diagnosis • treatment choices • probabilities of outcomes Patient shares values and lifestyle preferences: • may be based on past experience with medical choices • may depend on current social situation Together they arrive at an informed, shared decision
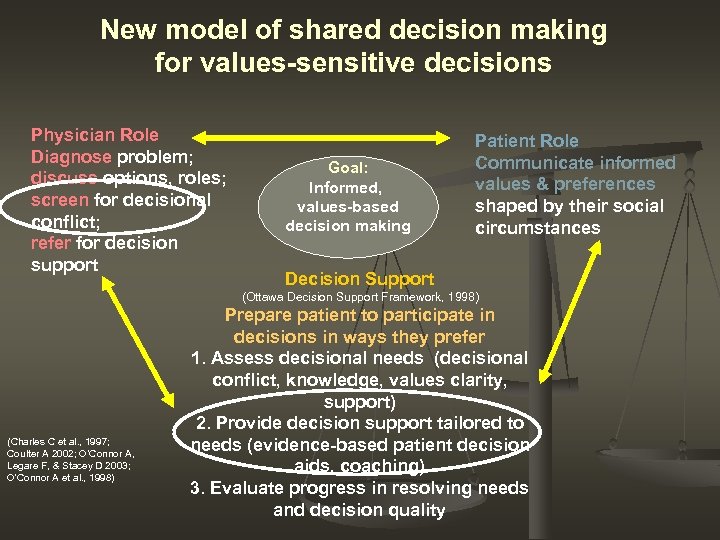 New model of shared decision making for values-sensitive decisions Physician Role Diagnose problem; discuss options, roles; screen for decisional conflict; refer for decision support Goal: Informed, values-based decision making Patient Role Communicate informed values & preferences shaped by their social circumstances Decision Support (Ottawa Decision Support Framework, 1998) (Charles C et al. , 1997; Coulter A 2002; O’Connor A, Legare F, & Stacey D 2003; O'Connor A et al. , 1998) Prepare patient to participate in decisions in ways they prefer 1. Assess decisional needs (decisional conflict, knowledge, values clarity, support) 2. Provide decision support tailored to needs (evidence-based patient decision aids, coaching) 3. Evaluate progress in resolving needs and decision quality
New model of shared decision making for values-sensitive decisions Physician Role Diagnose problem; discuss options, roles; screen for decisional conflict; refer for decision support Goal: Informed, values-based decision making Patient Role Communicate informed values & preferences shaped by their social circumstances Decision Support (Ottawa Decision Support Framework, 1998) (Charles C et al. , 1997; Coulter A 2002; O’Connor A, Legare F, & Stacey D 2003; O'Connor A et al. , 1998) Prepare patient to participate in decisions in ways they prefer 1. Assess decisional needs (decisional conflict, knowledge, values clarity, support) 2. Provide decision support tailored to needs (evidence-based patient decision aids, coaching) 3. Evaluate progress in resolving needs and decision quality
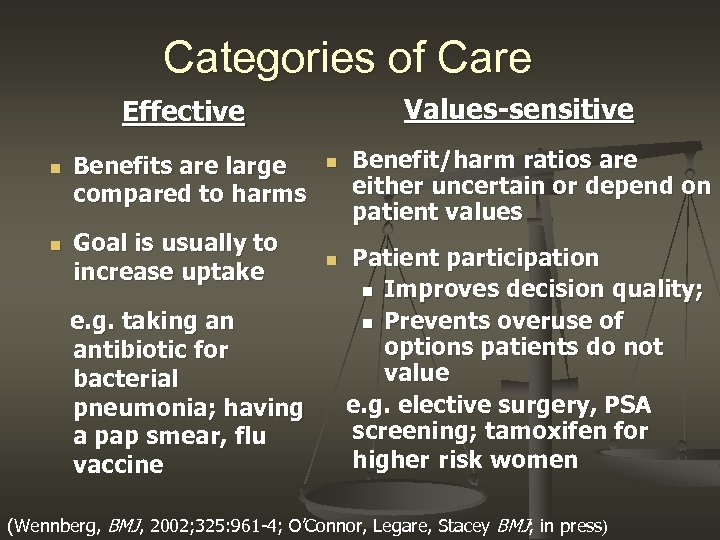 Categories of Care Values-sensitive Effective n n Benefits are large compared to harms Goal is usually to increase uptake e. g. taking an antibiotic for bacterial pneumonia; having a pap smear, flu vaccine n n Benefit/harm ratios are either uncertain or depend on patient values Patient participation n Improves decision quality; n Prevents overuse of options patients do not value e. g. elective surgery, PSA screening; tamoxifen for higher risk women (Wennberg, BMJ, 2002; 325: 961 -4; O’Connor, Legare, Stacey BMJ; in press)
Categories of Care Values-sensitive Effective n n Benefits are large compared to harms Goal is usually to increase uptake e. g. taking an antibiotic for bacterial pneumonia; having a pap smear, flu vaccine n n Benefit/harm ratios are either uncertain or depend on patient values Patient participation n Improves decision quality; n Prevents overuse of options patients do not value e. g. elective surgery, PSA screening; tamoxifen for higher risk women (Wennberg, BMJ, 2002; 325: 961 -4; O’Connor, Legare, Stacey BMJ; in press)
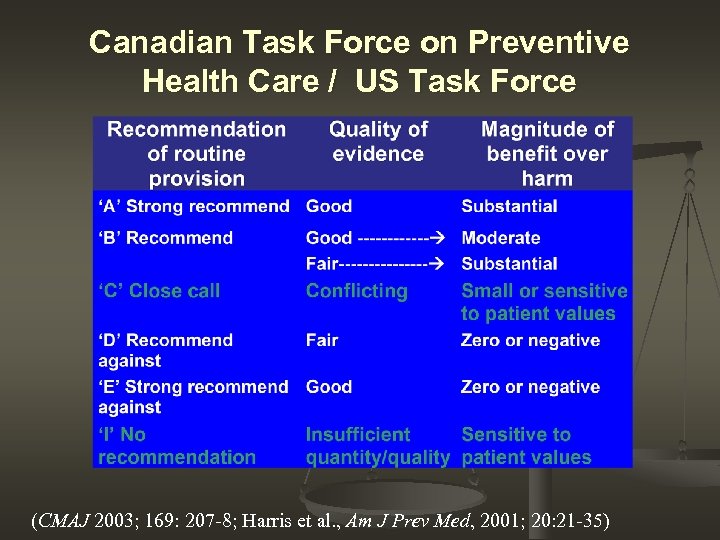 Canadian Task Force on Preventive Health Care / US Task Force (CMAJ 2003; 169: 207 -8; Harris et al. , Am J Prev Med, 2001; 20: 21 -35)
Canadian Task Force on Preventive Health Care / US Task Force (CMAJ 2003; 169: 207 -8; Harris et al. , Am J Prev Med, 2001; 20: 21 -35)
 Decision Making is… n n A Process of Choosing between courses of action (including inaction) We generally want to choose options that achieve valued outcomes and avoid undesirable outcomes
Decision Making is… n n A Process of Choosing between courses of action (including inaction) We generally want to choose options that achieve valued outcomes and avoid undesirable outcomes
 Difficult Decisions What are difficult decisions?
Difficult Decisions What are difficult decisions?
 Diagnosing Decisional Conflict Definition: § § Uncertainty about which course of action to take, resulting from… Simultaneous opposing tendencies to accept and reject a given course of action Janis & Mann, Decision Making, 1977
Diagnosing Decisional Conflict Definition: § § Uncertainty about which course of action to take, resulting from… Simultaneous opposing tendencies to accept and reject a given course of action Janis & Mann, Decision Making, 1977
 Signs and Symptoms n n unsure what to do unclear about best choice for them concern about bad results waver between choices n n delay decision question what is important distressed, anxious, tense preoccupied with decision
Signs and Symptoms n n unsure what to do unclear about best choice for them concern about bad results waver between choices n n delay decision question what is important distressed, anxious, tense preoccupied with decision
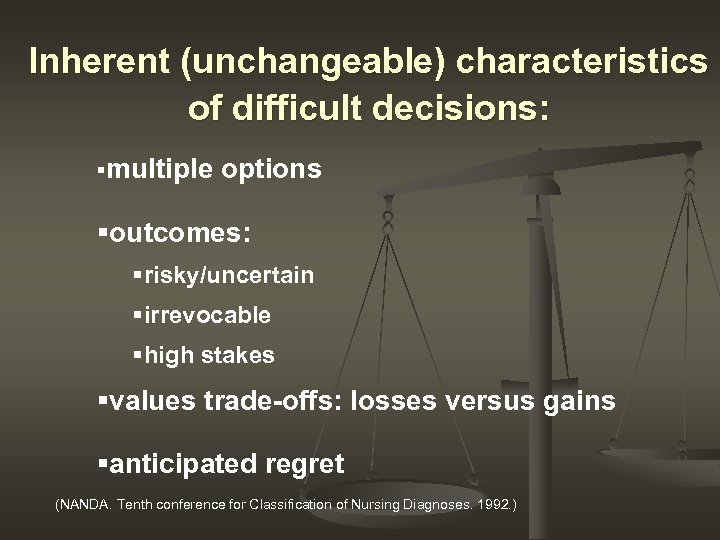 Inherent (unchangeable) characteristics of difficult decisions: §multiple options §outcomes: §risky/uncertain §irrevocable §high stakes §values trade-offs: losses versus gains §anticipated regret (NANDA. Tenth conference for Classification of Nursing Diagnoses. 1992. )
Inherent (unchangeable) characteristics of difficult decisions: §multiple options §outcomes: §risky/uncertain §irrevocable §high stakes §values trade-offs: losses versus gains §anticipated regret (NANDA. Tenth conference for Classification of Nursing Diagnoses. 1992. )
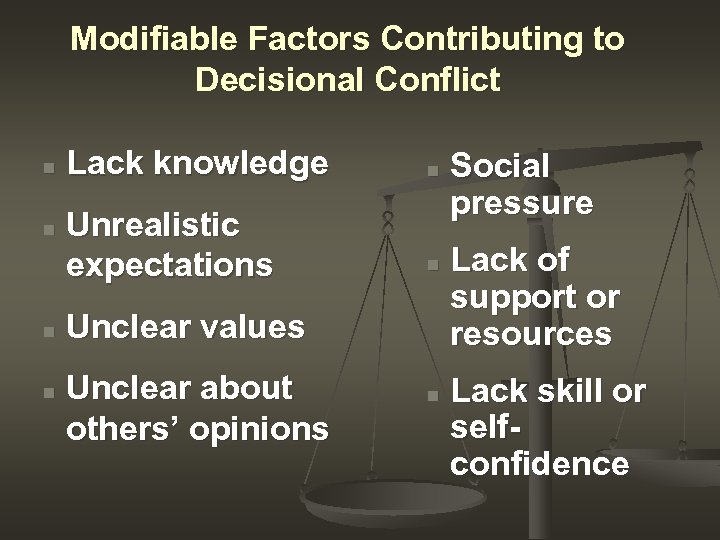 Modifiable Factors Contributing to Decisional Conflict n n Lack knowledge Unrealistic expectations n n Unclear values Unclear about others’ opinions n Social pressure Lack of support or resources Lack skill or selfconfidence
Modifiable Factors Contributing to Decisional Conflict n n Lack knowledge Unrealistic expectations n n Unclear values Unclear about others’ opinions n Social pressure Lack of support or resources Lack skill or selfconfidence
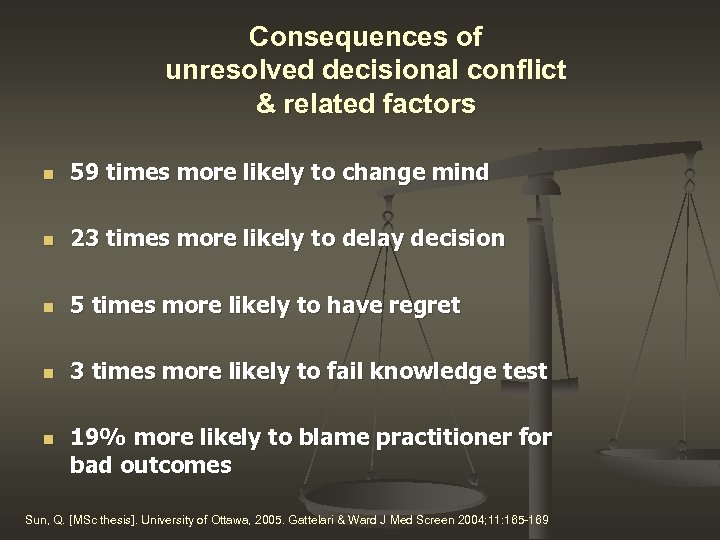 Consequences of unresolved decisional conflict & related factors n 59 times more likely to change mind n 23 times more likely to delay decision n 5 times more likely to have regret n 3 times more likely to fail knowledge test n 19% more likely to blame practitioner for bad outcomes Sun, Q. [MSc thesis]. University of Ottawa, 2005. Gattelari & Ward J Med Screen 2004; 11: 165 -169
Consequences of unresolved decisional conflict & related factors n 59 times more likely to change mind n 23 times more likely to delay decision n 5 times more likely to have regret n 3 times more likely to fail knowledge test n 19% more likely to blame practitioner for bad outcomes Sun, Q. [MSc thesis]. University of Ottawa, 2005. Gattelari & Ward J Med Screen 2004; 11: 165 -169
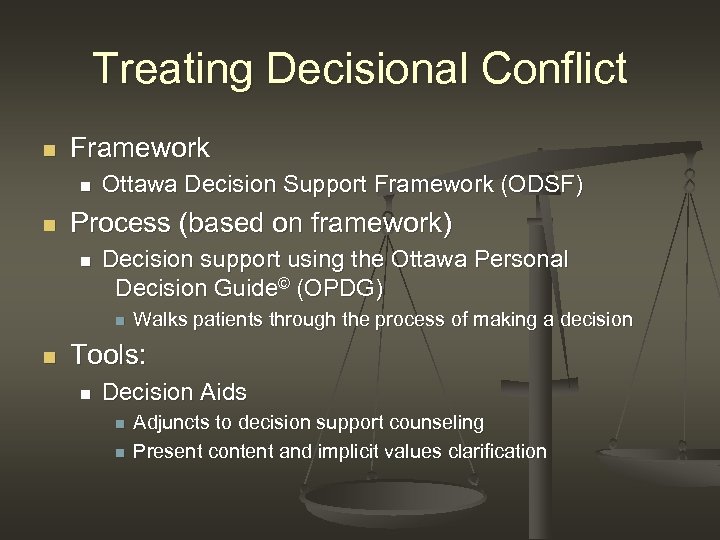 Treating Decisional Conflict n Framework n n Ottawa Decision Support Framework (ODSF) Process (based on framework) n Decision support using the Ottawa Personal Decision Guide© (OPDG) n n Walks patients through the process of making a decision Tools: n Decision Aids n n Adjuncts to decision support counseling Present content and implicit values clarification
Treating Decisional Conflict n Framework n n Ottawa Decision Support Framework (ODSF) Process (based on framework) n Decision support using the Ottawa Personal Decision Guide© (OPDG) n n Walks patients through the process of making a decision Tools: n Decision Aids n n Adjuncts to decision support counseling Present content and implicit values clarification
 Module 2: Decision support process Ottawa Decision Support Framework Decision Support Ottawa Personal Decision Guide
Module 2: Decision support process Ottawa Decision Support Framework Decision Support Ottawa Personal Decision Guide
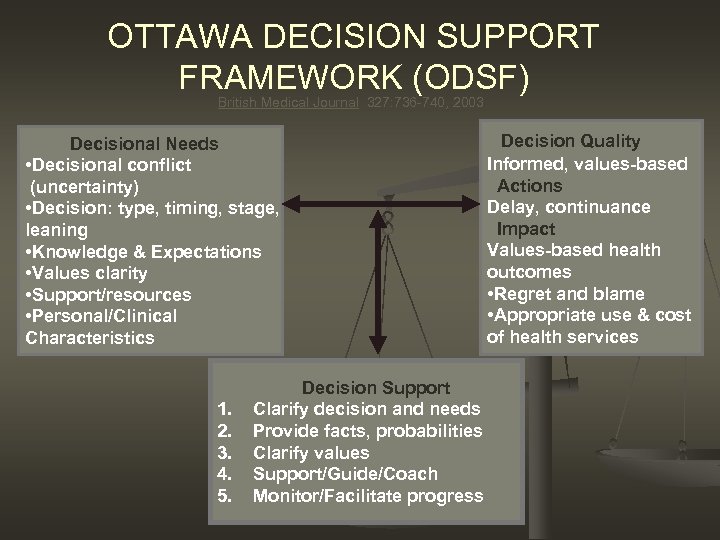 OTTAWA DECISION SUPPORT FRAMEWORK (ODSF) British Medical Journal 327: 736 -740, 2003 Decisional Needs • Decisional conflict (uncertainty) • Decision: type, timing, stage, leaning • Knowledge & Expectations • Values clarity • Support/resources • Personal/Clinical Characteristics 1. 2. 3. 4. 5. Decision Support Clarify decision and needs Provide facts, probabilities Clarify values Support/Guide/Coach Monitor/Facilitate progress Decision Quality Informed, values-based Actions Delay, continuance Impact Values-based health outcomes • Regret and blame • Appropriate use & cost of health services
OTTAWA DECISION SUPPORT FRAMEWORK (ODSF) British Medical Journal 327: 736 -740, 2003 Decisional Needs • Decisional conflict (uncertainty) • Decision: type, timing, stage, leaning • Knowledge & Expectations • Values clarity • Support/resources • Personal/Clinical Characteristics 1. 2. 3. 4. 5. Decision Support Clarify decision and needs Provide facts, probabilities Clarify values Support/Guide/Coach Monitor/Facilitate progress Decision Quality Informed, values-based Actions Delay, continuance Impact Values-based health outcomes • Regret and blame • Appropriate use & cost of health services
 Health Decisions Best Suited to the ODSF • No clear “choice” that’s right for everyone • Stimulated by new circumstance, medical diagnosis, or developmental transition • Options have different benefit/harm profiles that clients value differently • Careful deliberation --- uncertain outcomes (scientific uncertainty) • More effort in deliberation than in implementation
Health Decisions Best Suited to the ODSF • No clear “choice” that’s right for everyone • Stimulated by new circumstance, medical diagnosis, or developmental transition • Options have different benefit/harm profiles that clients value differently • Careful deliberation --- uncertain outcomes (scientific uncertainty) • More effort in deliberation than in implementation
 Decision Support Process n Decision support is a process of: • assessing decisional needs: modifiable factors • intervening to address individual needs evaluating the progress and quality of decision making • n Quality decisions: • informed • congruent with personal values • acted upon (O’Connor, Jacobsen, Stacey, JOGNN, 2002)
Decision Support Process n Decision support is a process of: • assessing decisional needs: modifiable factors • intervening to address individual needs evaluating the progress and quality of decision making • n Quality decisions: • informed • congruent with personal values • acted upon (O’Connor, Jacobsen, Stacey, JOGNN, 2002)
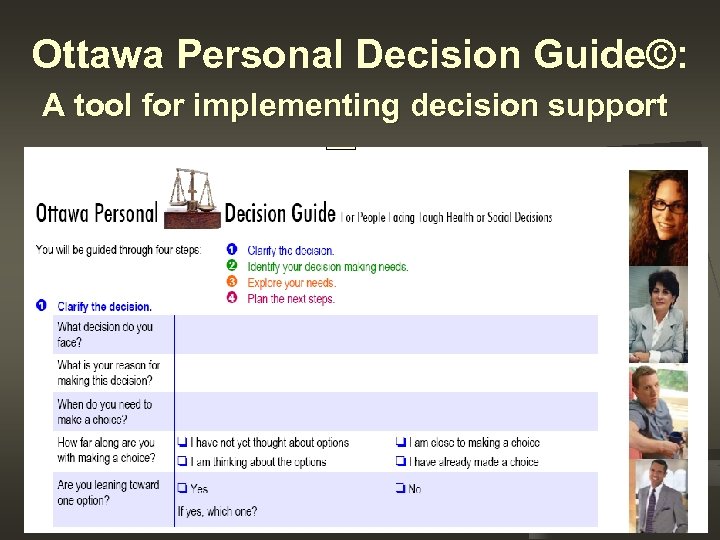 Ottawa Personal Decision Guide©: A tool for implementing decision support
Ottawa Personal Decision Guide©: A tool for implementing decision support
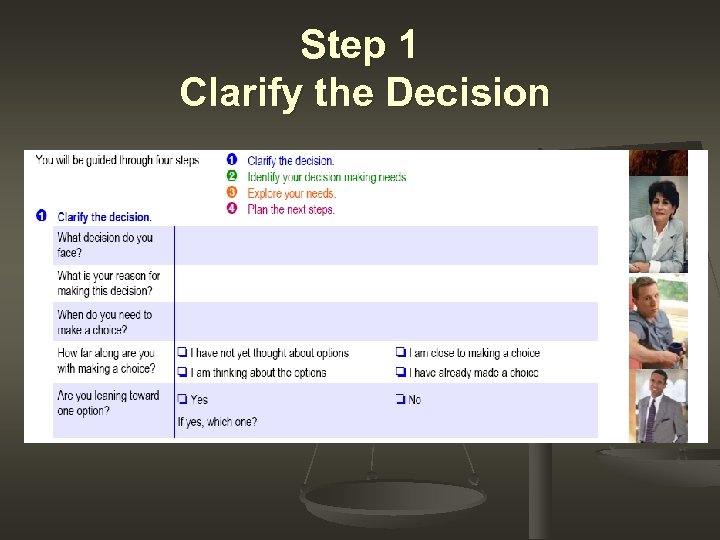 Step 1 Clarify the Decision
Step 1 Clarify the Decision
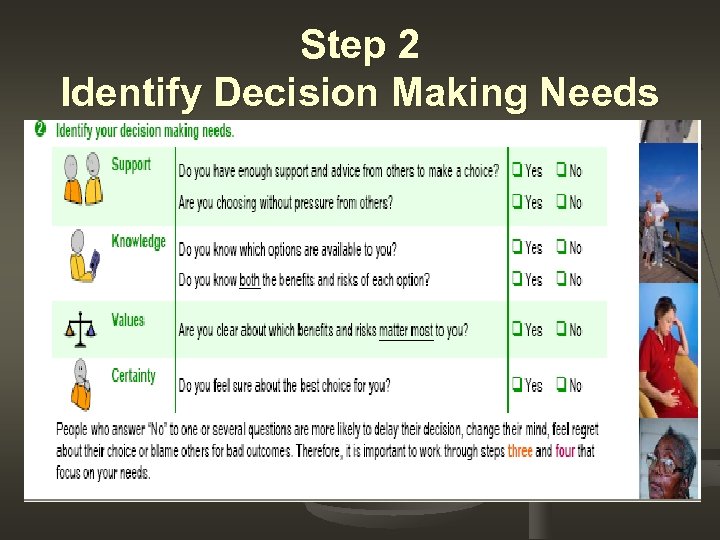 Step 2 Identify Decision Making Needs
Step 2 Identify Decision Making Needs
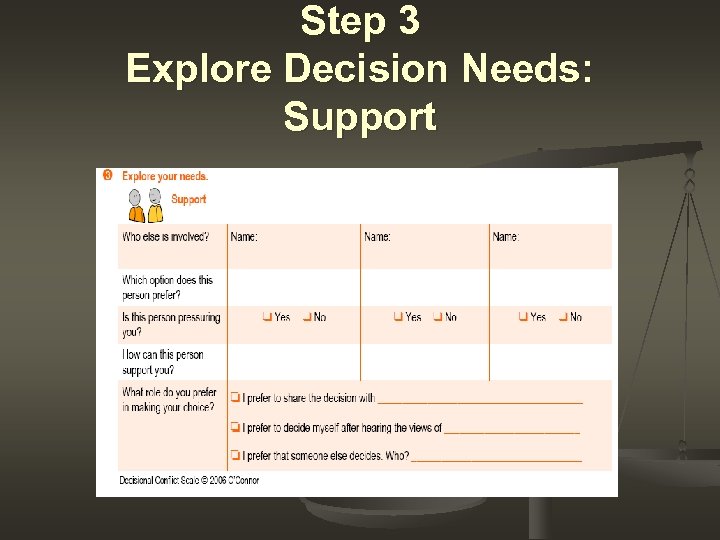 Step 3 Explore Decision Needs: Support
Step 3 Explore Decision Needs: Support
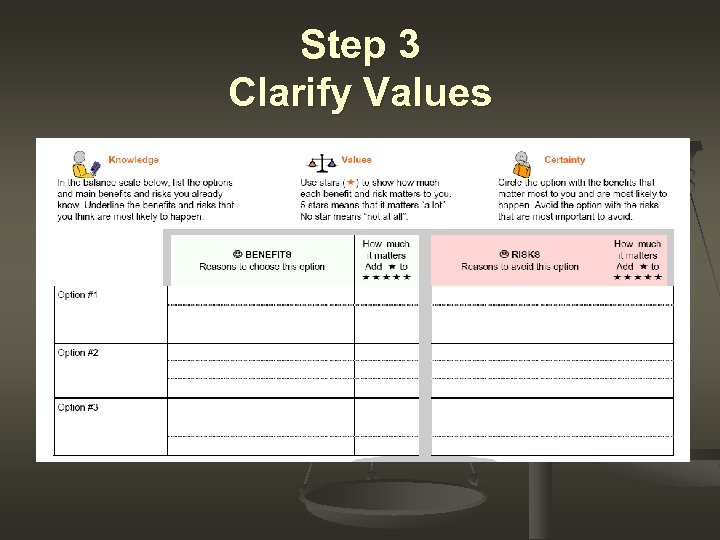 Step 3 Clarify Values
Step 3 Clarify Values
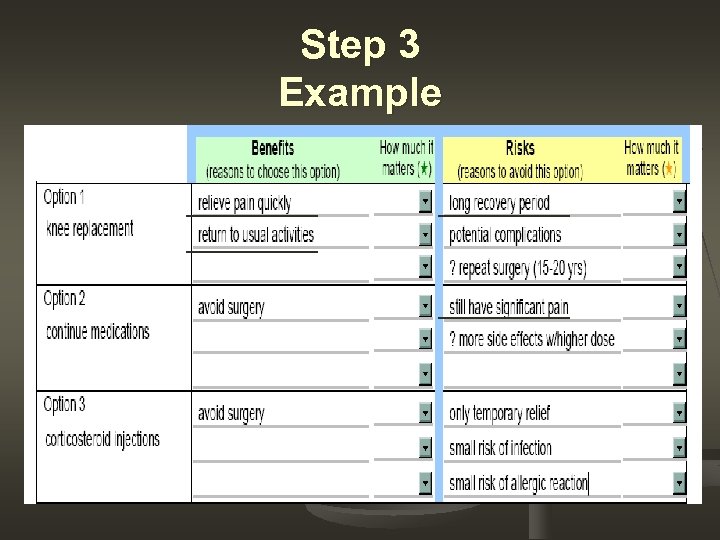 Step 3 Example
Step 3 Example
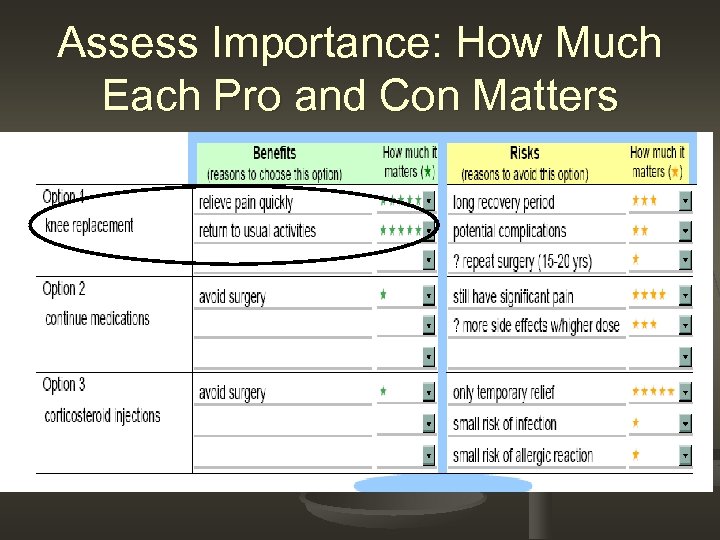 Assess Importance: How Much Each Pro and Con Matters
Assess Importance: How Much Each Pro and Con Matters
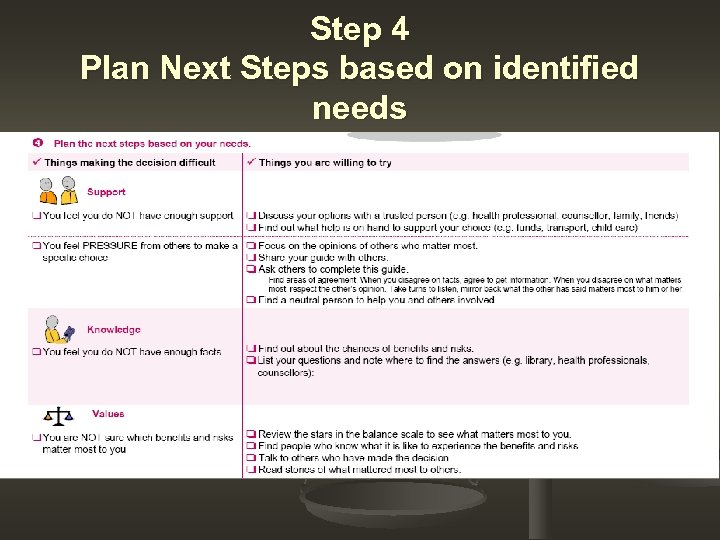 Step 4 Plan Next Steps based on identified needs
Step 4 Plan Next Steps based on identified needs
 Using the Ottawa Personal Decision Guide© 1. Form groups of two • • ‘Client’ making a difficult decision ‘Practitioner’ coaching 2. ‘Client’ choose a real decision (health, career, education, move, buy a car) 3. ‘Practitioner’ interviews patient & documents on the Ottawa Guide 4. Discussion
Using the Ottawa Personal Decision Guide© 1. Form groups of two • • ‘Client’ making a difficult decision ‘Practitioner’ coaching 2. ‘Client’ choose a real decision (health, career, education, move, buy a car) 3. ‘Practitioner’ interviews patient & documents on the Ottawa Guide 4. Discussion
 What happened? What helped?
What happened? What helped?
 Module 3: Communicating risk information
Module 3: Communicating risk information
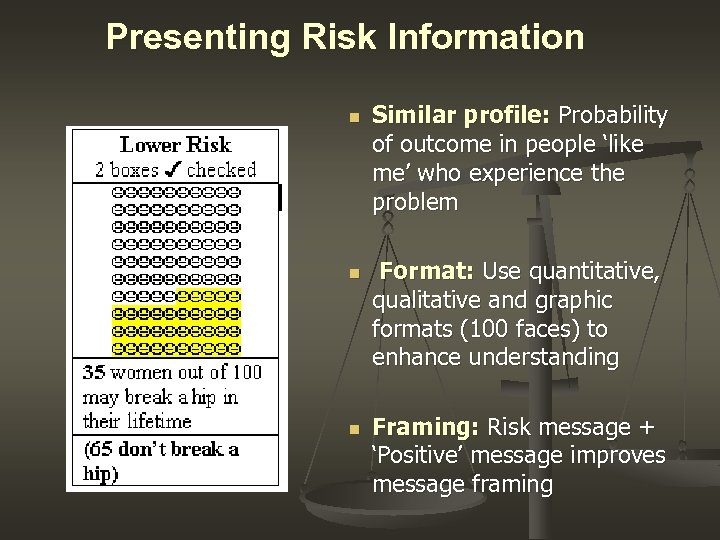 Presenting Risk Information n Similar profile: Probability of outcome in people ‘like me’ who experience the problem Format: Use quantitative, qualitative and graphic formats (100 faces) to enhance understanding Framing: Risk message + ‘Positive’ message improves message framing
Presenting Risk Information n Similar profile: Probability of outcome in people ‘like me’ who experience the problem Format: Use quantitative, qualitative and graphic formats (100 faces) to enhance understanding Framing: Risk message + ‘Positive’ message improves message framing
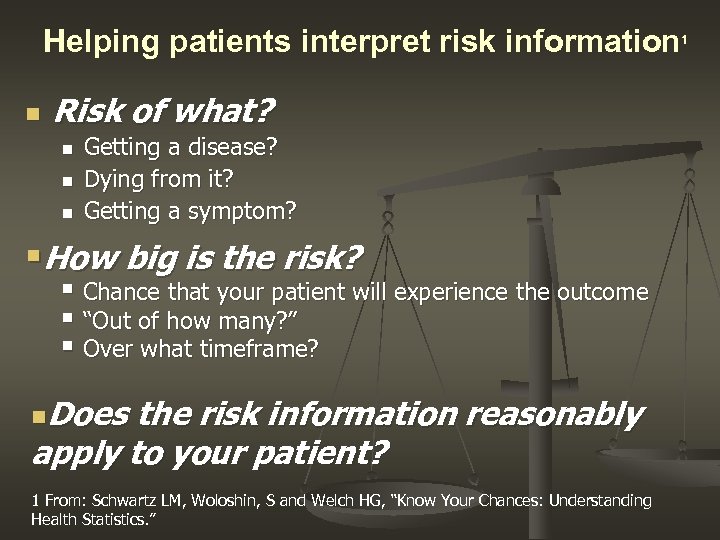 Helping patients interpret risk information 1 n Risk of what? n n n Getting a disease? Dying from it? Getting a symptom? §How big is the risk? § Chance that your patient will experience the outcome § “Out of how many? ” § Over what timeframe? n. Does the risk information reasonably apply to your patient? 1 From: Schwartz LM, Woloshin, S and Welch HG, “Know Your Chances: Understanding Health Statistics. ”
Helping patients interpret risk information 1 n Risk of what? n n n Getting a disease? Dying from it? Getting a symptom? §How big is the risk? § Chance that your patient will experience the outcome § “Out of how many? ” § Over what timeframe? n. Does the risk information reasonably apply to your patient? 1 From: Schwartz LM, Woloshin, S and Welch HG, “Know Your Chances: Understanding Health Statistics. ”
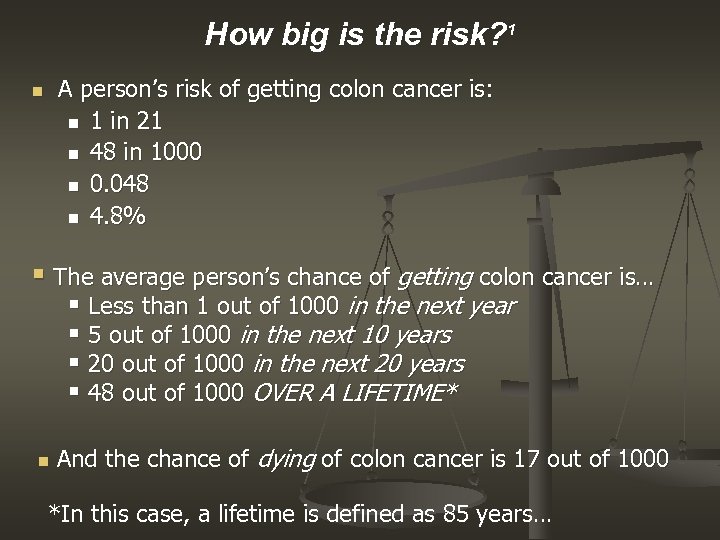 How big is the risk? 1 n A person’s risk of getting colon cancer is: n 1 in 21 n 48 in 1000 n 0. 048 n 4. 8% § The average person’s chance of getting colon cancer is… § Less than 1 out of 1000 in the next year § 5 out of 1000 in the next 10 years § 20 out of 1000 in the next 20 years § 48 out of 1000 OVER A LIFETIME* n And the chance of dying of colon cancer is 17 out of 1000 *In this case, a lifetime is defined as 85 years…
How big is the risk? 1 n A person’s risk of getting colon cancer is: n 1 in 21 n 48 in 1000 n 0. 048 n 4. 8% § The average person’s chance of getting colon cancer is… § Less than 1 out of 1000 in the next year § 5 out of 1000 in the next 10 years § 20 out of 1000 in the next 20 years § 48 out of 1000 OVER A LIFETIME* n And the chance of dying of colon cancer is 17 out of 1000 *In this case, a lifetime is defined as 85 years…
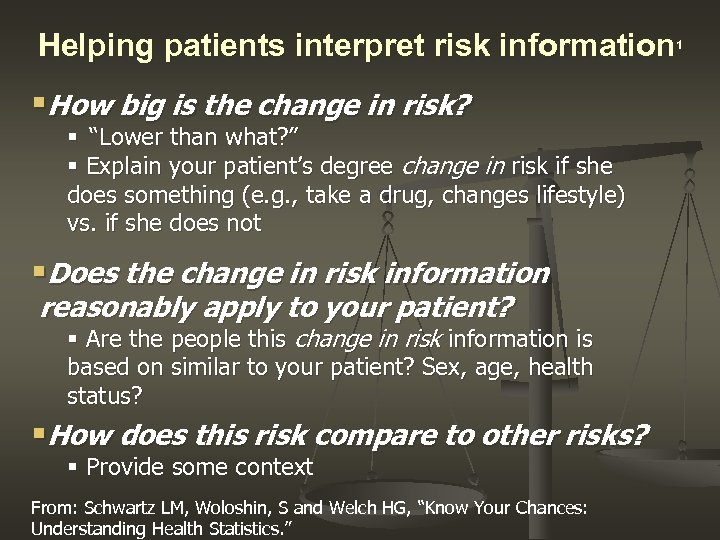 Helping patients interpret risk information 1 §How big is the change in risk? § “Lower than what? ” § Explain your patient’s degree change in risk if she does something (e. g. , take a drug, changes lifestyle) vs. if she does not §Does the change in risk information reasonably apply to your patient? § Are the people this change in risk information is based on similar to your patient? Sex, age, health status? §How does this risk compare to other risks? § Provide some context From: Schwartz LM, Woloshin, S and Welch HG, “Know Your Chances: Understanding Health Statistics. ”
Helping patients interpret risk information 1 §How big is the change in risk? § “Lower than what? ” § Explain your patient’s degree change in risk if she does something (e. g. , take a drug, changes lifestyle) vs. if she does not §Does the change in risk information reasonably apply to your patient? § Are the people this change in risk information is based on similar to your patient? Sex, age, health status? §How does this risk compare to other risks? § Provide some context From: Schwartz LM, Woloshin, S and Welch HG, “Know Your Chances: Understanding Health Statistics. ”
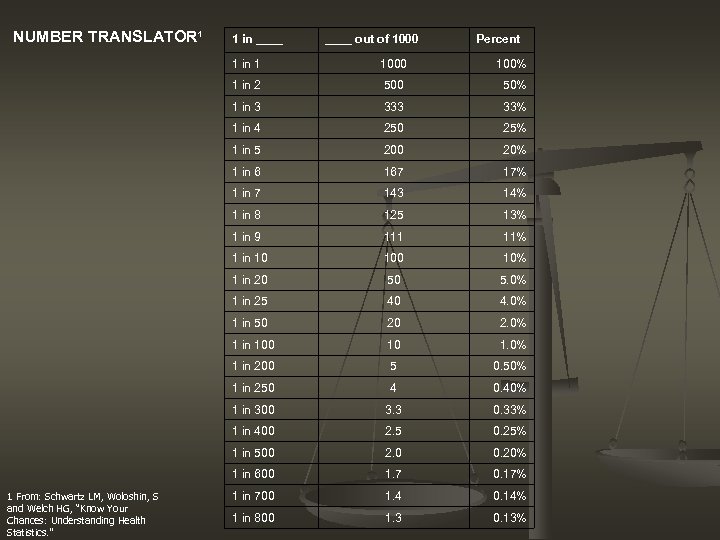 NUMBER TRANSLATOR 1 1 in ____ out of 1000 Percent 1 in 1 100% 1 in 2 500 50% 1 in 3 33% 1 in 4 250 25% 1 in 5 200 20% 1 in 6 167 17% 1 in 7 143 14% 1 in 8 125 13% 1 in 9 111 11% 1 in 10 10% 1 in 20 50 5. 0% 1 in 25 40 4. 0% 1 in 50 20 2. 0% 1 in 100 10 1. 0% 1 in 200 5 0. 50% 1 in 250 4 0. 40% 1 in 300 3. 3 0. 33% 1 in 400 2. 5 0. 25% 1 in 500 2. 0 0. 20% 1 in 600 1 From: Schwartz LM, Woloshin, S and Welch HG, “Know Your Chances: Understanding Health Statistics. ” 1000 1. 7 0. 17% 1 in 700 1. 4 0. 14% 1 in 800 1. 3 0. 13%
NUMBER TRANSLATOR 1 1 in ____ out of 1000 Percent 1 in 1 100% 1 in 2 500 50% 1 in 3 33% 1 in 4 250 25% 1 in 5 200 20% 1 in 6 167 17% 1 in 7 143 14% 1 in 8 125 13% 1 in 9 111 11% 1 in 10 10% 1 in 20 50 5. 0% 1 in 25 40 4. 0% 1 in 50 20 2. 0% 1 in 100 10 1. 0% 1 in 200 5 0. 50% 1 in 250 4 0. 40% 1 in 300 3. 3 0. 33% 1 in 400 2. 5 0. 25% 1 in 500 2. 0 0. 20% 1 in 600 1 From: Schwartz LM, Woloshin, S and Welch HG, “Know Your Chances: Understanding Health Statistics. ” 1000 1. 7 0. 17% 1 in 700 1. 4 0. 14% 1 in 800 1. 3 0. 13%
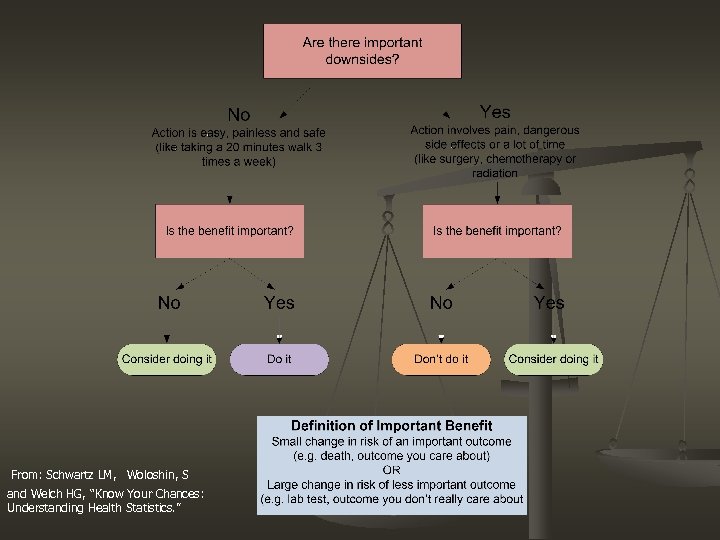 From: Schwartz LM, Woloshin, S and Welch HG, “Know Your Chances: Understanding Health Statistics. ”
From: Schwartz LM, Woloshin, S and Welch HG, “Know Your Chances: Understanding Health Statistics. ”
 Module 4: Decision Support Tools
Module 4: Decision Support Tools
 Decision Aids
Decision Aids
 Decision Aids adjunct to counseling n inform re options, benefits, risks n specify probabilities of outcomes n clarify personal values & norms n guide in deliberating & communicating n
Decision Aids adjunct to counseling n inform re options, benefits, risks n specify probabilities of outcomes n clarify personal values & norms n guide in deliberating & communicating n
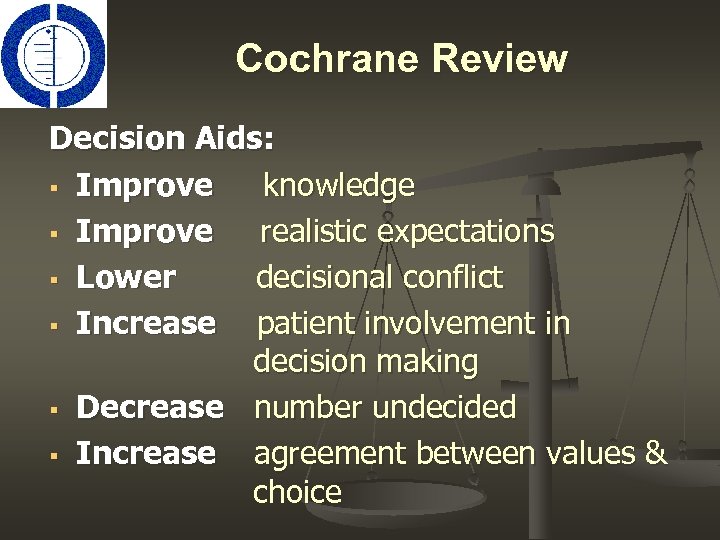 Cochrane Review Decision Aids: § Improve knowledge § Improve realistic expectations § Lower decisional conflict § Increase patient involvement in decision making § Decrease number undecided § Increase agreement between values & choice
Cochrane Review Decision Aids: § Improve knowledge § Improve realistic expectations § Lower decisional conflict § Increase patient involvement in decision making § Decrease number undecided § Increase agreement between values & choice
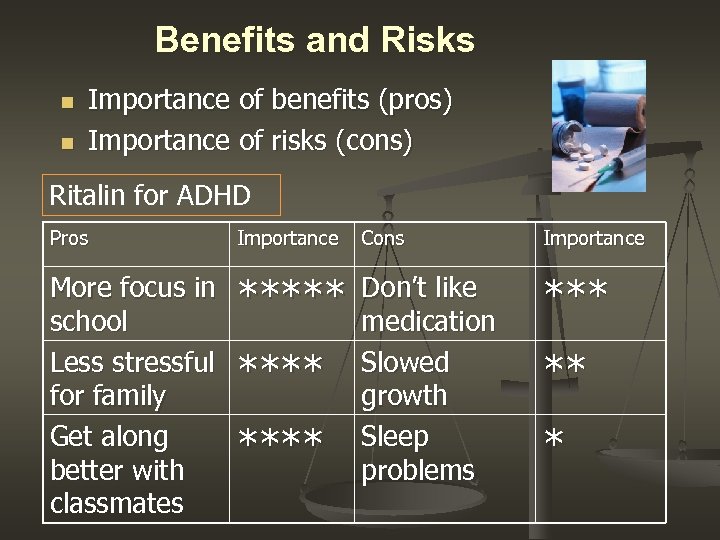 Benefits and Risks n n Importance of benefits (pros) Importance of risks (cons) Ritalin for ADHD Pros Importance Cons Importance More focus in school Less stressful for family Get along better with classmates ***** Don’t like medication Slowed growth Sleep problems **** ** *
Benefits and Risks n n Importance of benefits (pros) Importance of risks (cons) Ritalin for ADHD Pros Importance Cons Importance More focus in school Less stressful for family Get along better with classmates ***** Don’t like medication Slowed growth Sleep problems **** ** *
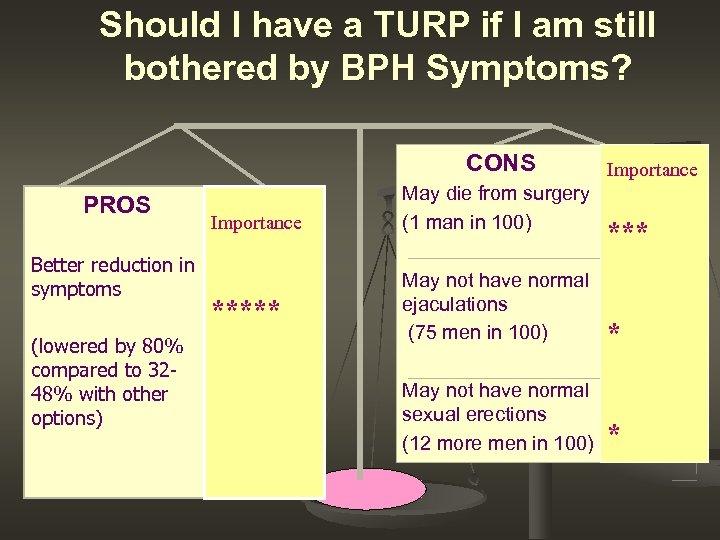 Should I have a TURP if I am still bothered by BPH Symptoms? CONS PROS Better reduction in symptoms (lowered by 80% compared to 3248% with other options) Importance ***** May die from surgery (1 man in 100) Importance *** May not have normal ejaculations (75 men in 100) * May not have normal sexual erections (12 more men in 100) *
Should I have a TURP if I am still bothered by BPH Symptoms? CONS PROS Better reduction in symptoms (lowered by 80% compared to 3248% with other options) Importance ***** May die from surgery (1 man in 100) Importance *** May not have normal ejaculations (75 men in 100) * May not have normal sexual erections (12 more men in 100) *
 Providers’ Perspectives “It is helpful to have my patients arrive at the consultation with familiarity of the options and knowledge of the risks and benefits” Richard Barth, MD, surgical oncologist "With this process, I can focus on helping each individual patient decide the best treatment for her. ” Kari Rosenkranz, MD, surgical oncologist
Providers’ Perspectives “It is helpful to have my patients arrive at the consultation with familiarity of the options and knowledge of the risks and benefits” Richard Barth, MD, surgical oncologist "With this process, I can focus on helping each individual patient decide the best treatment for her. ” Kari Rosenkranz, MD, surgical oncologist
 Patient Perspective “At first I wondered what this was all for? It didn't take long for me to understand. The videos were the most helpful tools! I felt peace for the first time in a while. The whole shared decision making concept is wonderful and empowering. Thank you!” Breast cancer patient
Patient Perspective “At first I wondered what this was all for? It didn't take long for me to understand. The videos were the most helpful tools! I felt peace for the first time in a while. The whole shared decision making concept is wonderful and empowering. Thank you!” Breast cancer patient
 Patients’ Perspectives: Herniated Disc n n n “Before watching the video I was prepared for surgery. Now after watching it I am going to try non-surgical treatments to see if it works. ” “I found the video very informative and helpful and because of it I am more inclined to consider surgery, which is a new position. ” “This video made me realize I need to be more in charge of myself. And that surgery should be a last resort and that other options should be explored. ” “Nothing can replace a question & answer visit with the doctor. The video made it very clear about how undependable the statistics were. ” “The video helps in that “real people” that actually have back issues talked about their own experiences and the choices they made. It helps you understand that you are not alone in your pain, decisions or hardships. ”
Patients’ Perspectives: Herniated Disc n n n “Before watching the video I was prepared for surgery. Now after watching it I am going to try non-surgical treatments to see if it works. ” “I found the video very informative and helpful and because of it I am more inclined to consider surgery, which is a new position. ” “This video made me realize I need to be more in charge of myself. And that surgery should be a last resort and that other options should be explored. ” “Nothing can replace a question & answer visit with the doctor. The video made it very clear about how undependable the statistics were. ” “The video helps in that “real people” that actually have back issues talked about their own experiences and the choices they made. It helps you understand that you are not alone in your pain, decisions or hardships. ”
 Decision Support Resources
Decision Support Resources
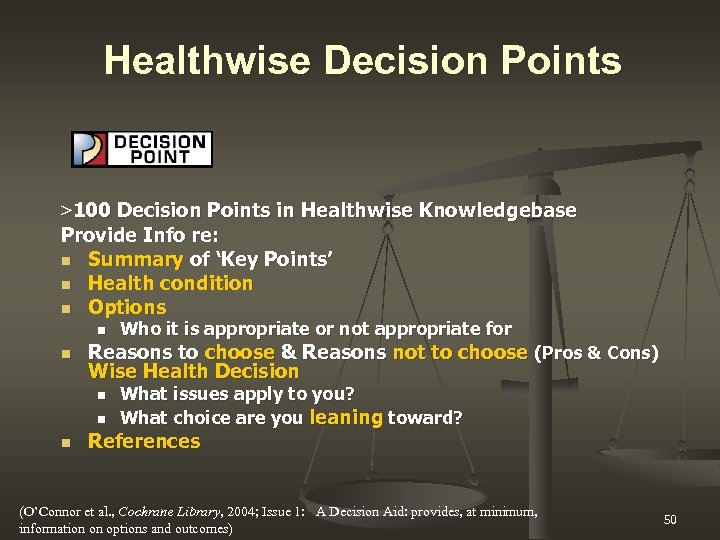 Healthwise Decision Points >100 Decision Points in Healthwise Knowledgebase Provide Info re: n Summary of ‘Key Points’ n Health condition n Options n n Reasons to choose & Reasons not to choose (Pros & Cons) Wise Health Decision n Who it is appropriate or not appropriate for What issues apply to you? What choice are you leaning toward? References (O’Connor et al. , Cochrane Library, 2004; Issue 1: A Decision Aid: provides, at minimum, information on options and outcomes) 50
Healthwise Decision Points >100 Decision Points in Healthwise Knowledgebase Provide Info re: n Summary of ‘Key Points’ n Health condition n Options n n Reasons to choose & Reasons not to choose (Pros & Cons) Wise Health Decision n Who it is appropriate or not appropriate for What issues apply to you? What choice are you leaning toward? References (O’Connor et al. , Cochrane Library, 2004; Issue 1: A Decision Aid: provides, at minimum, information on options and outcomes) 50
 Shared Decision Making Resources n DHMC Center for Shared Decision Making n n Ottawa Health Research Institute n n http: //www. webmd. com/ Foundation for Informed Medical Decision Making n n http: //www. healthwise. net/preferredcare Web. MD n n http: //decisionaid. ohri. ca/index. html Healthwise Preferred Care n n http: //www. dhmc. org/dept/csdm http: //www. informedmedicaldecisions. org Health News Review n http: //www. healthnewsreview. org
Shared Decision Making Resources n DHMC Center for Shared Decision Making n n Ottawa Health Research Institute n n http: //www. webmd. com/ Foundation for Informed Medical Decision Making n n http: //www. healthwise. net/preferredcare Web. MD n n http: //decisionaid. ohri. ca/index. html Healthwise Preferred Care n n http: //www. dhmc. org/dept/csdm http: //www. informedmedicaldecisions. org Health News Review n http: //www. healthnewsreview. org
 Conclusions Decision support is a process of: n assessing decisional needs n intervening to address individual needs n evaluating the quality of decision making A high quality decision is informed, -based, and acted upon values Decision quality improves with: n Patient decision aids n Personal health coaching using a structured decision guide
Conclusions Decision support is a process of: n assessing decisional needs n intervening to address individual needs n evaluating the quality of decision making A high quality decision is informed, -based, and acted upon values Decision quality improves with: n Patient decision aids n Personal health coaching using a structured decision guide
 Acknowledgements and Thanks n n n The Foundation for Informed Medical Decision Making Health Dialog, Inc. Annette O’Connor, MSc. N, Ph. D, FCAHS and the Ottawa Health Research Institute team John Wennberg, MD, MPH James N. Weinstein, DO, MS
Acknowledgements and Thanks n n n The Foundation for Informed Medical Decision Making Health Dialog, Inc. Annette O’Connor, MSc. N, Ph. D, FCAHS and the Ottawa Health Research Institute team John Wennberg, MD, MPH James N. Weinstein, DO, MS


