32ab4c6cc009589d38b53f644ed2ee10.ppt
- Количество слайдов: 1
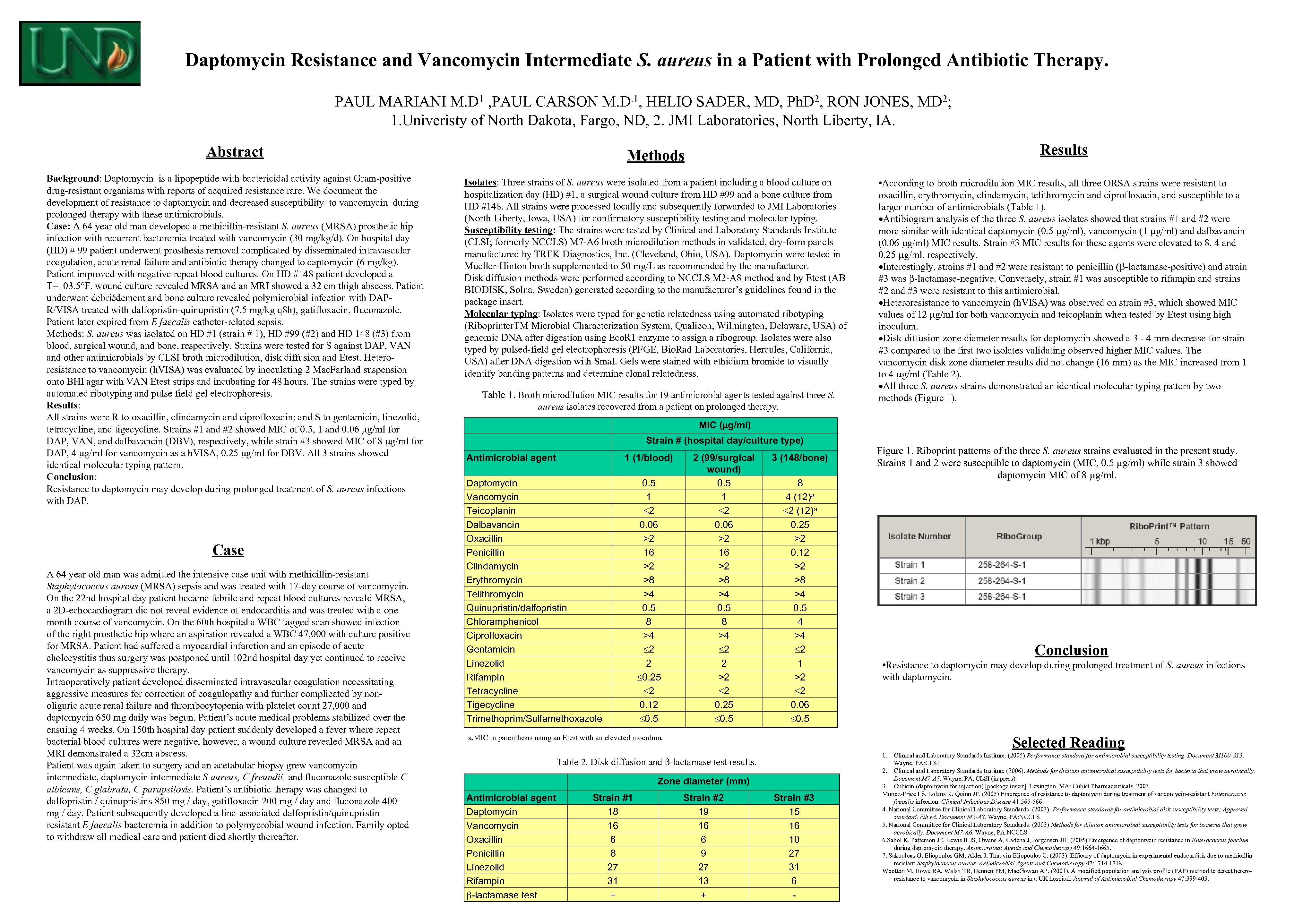 Daptomycin Resistance and Vancomycin Intermediate S. aureus in a Patient with Prolonged Antibiotic Therapy. PAUL MARIANI M. D 1 , PAUL CARSON M. D. 1, HELIO SADER, MD, Ph. D 2, RON JONES, MD 2; 1. Univeristy of North Dakota, Fargo, ND, 2. JMI Laboratories, North Liberty, IA. Results Abstract Methods Background: Daptomycin is a lipopeptide with bactericidal activity against Gram-positive drug-resistant organisms with reports of acquired resistance rare. We document the development of resistance to daptomycin and decreased susceptibility to vancomycin during prolonged therapy with these antimicrobials. Case: A 64 year old man developed a methicillin-resistant S. aureus (MRSA) prosthetic hip infection with recurrent bacteremia treated with vancomycin (30 mg/kg/d). On hospital day (HD) # 99 patient underwent prosthesis removal complicated by disseminated intravascular coagulation, acute renal failure and antibiotic therapy changed to daptomycin (6 mg/kg). Patient improved with negative repeat blood cultures. On HD #148 patient developed a T=103. 5°F, wound culture revealed MRSA and an MRI showed a 32 cm thigh abscess. Patient underwent debriédement and bone culture revealed polymicrobial infection with DAPR/VISA treated with dalfopristin-quinupristin (7. 5 mg/kg q 8 h), gatifloxacin, fluconazole. Patient later expired from E faecalis catheter-related sepsis. Methods: S. aureus was isolated on HD #1 (strain # 1), HD #99 (#2) and HD 148 (#3) from blood, surgical wound, and bone, respectively. Strains were tested for S against DAP, VAN and other antimicrobials by CLSI broth microdilution, disk diffusion and Etest. Heteroresistance to vancomycin (h. VISA) was evaluated by inoculating 2 Mac. Farland suspension onto BHI agar with VAN Etest strips and incubating for 48 hours. The strains were typed by automated ribotyping and pulse field gel electrophoresis. Results: All strains were R to oxacillin, clindamycin and ciprofloxacin; and S to gentamicin, linezolid, tetracycline, and tigecycline. Strains #1 and #2 showed MIC of 0. 5, 1 and 0. 06 μg/ml for DAP, VAN, and dalbavancin (DBV), respectively, while strain #3 showed MIC of 8 μg/ml for DAP, 4 μg/ml for vancomycin as a h. VISA, 0. 25 μg/ml for DBV. All 3 strains showed identical molecular typing pattern. Conclusion: Resistance to daptomycin may develop during prolonged treatment of S. aureus infections with DAP. Isolates: Three strains of S. aureus were isolated from a patient including a blood culture on hospitalization day (HD) #1, a surgical wound culture from HD #99 and a bone culture from HD #148. All strains were processed locally and subsequently forwarded to JMI Laboratories (North Liberty, Iowa, USA) for confirmatory susceptibility testing and molecular typing. Susceptibility testing: The strains were tested by Clinical and Laboratory Standards Institute (CLSI; formerly NCCLS) M 7 -A 6 broth microdilution methods in validated, dry-form panels manufactured by TREK Diagnostics, Inc. (Cleveland, Ohio, USA). Daptomycin were tested in Mueller-Hinton broth supplemented to 50 mg/L as recommended by the manufacturer. Disk diffusion methods were performed according to NCCLS M 2 -A 8 method and by Etest (AB BIODISK, Solna, Sweden) generated according to the manufacturer’s guidelines found in the package insert. Molecular typing: Isolates were typed for genetic relatedness using automated ribotyping (Riboprinter. TM Microbial Characterization System, Qualicon, Wilmington, Delaware, USA) of genomic DNA after digestion using Eco. R 1 enzyme to assign a ribogroup. Isolates were also typed by pulsed-field gel electrophoresis (PFGE, Bio. Rad Laboratories, Hercules, California, USA) after DNA digestion with Sma. I. Gels were stained with ethidium bromide to visually identify banding patterns and determine clonal relatedness. Case A 64 year old man was admitted the intensive case unit with methicillin-resistant Staphylococcus aureus (MRSA) sepsis and was treated with 17 -day course of vancomycin. On the 22 nd hospital day patient became febrile and repeat blood cultures reveald MRSA, a 2 D-echocardiogram did not reveal evidence of endocarditis and was treated with a one month course of vancomycin. On the 60 th hospital a WBC tagged scan showed infection of the right prosthetic hip where an aspiration revealed a WBC 47, 000 with culture positive for MRSA. Patient had suffered a myocardial infarction and an episode of acute cholecystitis thus surgery was postponed until 102 nd hospital day yet continued to receive vancomycin as suppressive therapy. Intraoperatively patient developed disseminated intravascular coagulation necessitating aggressive measures for correction of coagulopathy and further complicated by nonoliguric acute renal failure and thrombocytopenia with platelet count 27, 000 and daptomycin 650 mg daily was begun. Patient’s acute medical problems stabilized over the ensuing 4 weeks. On 150 th hospital day patient suddenly developed a fever where repeat bacterial blood cultures were negative, however, a wound culture revealed MRSA and an MRI demonstrated a 32 cm abscess. Patient was again taken to surgery and an acetabular biopsy grew vancomycin intermediate, daptomycin intermediate S aureus, C freundii, and fluconazole susceptible C albicans, C glabrata, C parapsilosis. Patient’s antibiotic therapy was changed to dalfopristin / quinupristins 850 mg / day, gatifloxacin 200 mg / day and fluconazole 400 mg / day. Patient subsequently developed a line-associated dalfopristin/quinupristin resistant E faecalis bacteremia in addition to polymycrobial wound infection. Family opted to withdraw all medical care and patient died shortly thereafter. Table 1. Broth microdilution MIC results for 19 antimicrobial agents tested against three S. aureus isolates recovered from a patient on prolonged therapy. • According to broth microdilution MIC results, all three ORSA strains were resistant to oxacillin, erythromycin, clindamycin, telithromycin and ciprofloxacin, and susceptible to a larger number of antimicrobials (Table 1). Antibiogram analysis of the three S. aureus isolates showed that strains #1 and #2 were more similar with identical daptomycin (0. 5 g/ml), vancomycin (1 g/ml) and dalbavancin (0. 06 g/ml) MIC results. Strain #3 MIC results for these agents were elevated to 8, 4 and 0. 25 g/ml, respectively. Interestingly, strains #1 and #2 were resistant to penicillin ( -lactamase-positive) and strain #3 was -lactamase-negative. Conversely, strain #1 was susceptible to rifampin and strains #2 and #3 were resistant to this antimicrobial. Heteroresistance to vancomycin (h. VISA) was observed on strain #3, which showed MIC values of 12 g/ml for both vancomycin and teicoplanin when tested by Etest using high inoculum. Disk diffusion zone diameter results for daptomycin showed a 3 - 4 mm decrease for strain #3 compared to the first two isolates validating observed higher MIC values. The vancomycin disk zone diameter results did not change (16 mm) as the MIC increased from 1 to 4 g/ml (Table 2). All three S. aureus strains demonstrated an identical molecular typing pattern by two methods (Figure 1). MIC ( g/ml) Strain # (hospital day/culture type) Antimicrobial agent 1 (1/blood) Daptomycin Vancomycin Teicoplanin Dalbavancin Oxacillin Penicillin Clindamycin Erythromycin Telithromycin Quinupristin/dalfopristin Chloramphenicol Ciprofloxacin Gentamicin Linezolid Rifampin Tetracycline Tigecycline Trimethoprim/Sulfamethoxazole 0. 5 1 2 0. 06 >2 16 >2 >8 >4 0. 5 8 >4 2 2 0. 25 2 0. 12 0. 5 2 (99/surgical wound) 0. 5 1 2 0. 06 >2 16 >2 >8 >4 0. 5 8 >4 2 2 >2 2 0. 25 0. 5 3 (148/bone) 8 4 (12)a 2 (12)a 0. 25 >2 0. 12 >2 >8 >4 0. 5 4 >4 2 1 >2 2 0. 06 0. 5 Figure 1. Riboprint patterns of the three S. aureus strains evaluated in the present study. Strains 1 and 2 were susceptible to daptomycin (MIC, 0. 5 g/ml) while strain 3 showed daptomycin MIC of 8 g/ml. Conclusion • Resistance to daptomycin may develop during prolonged treatment of S. aureus infections with daptomycin. a. MIC in parenthesis using an Etest with an elevated inoculum. Selected Reading 1. Table 2. Disk diffusion and -lactamase test results. Zone diameter (mm) Antimicrobial agent Daptomycin Vancomycin Oxacillin Penicillin Linezolid Rifampin -lactamase test Strain #1 18 16 6 8 27 31 + Strain #2 19 16 6 9 27 13 + Strain #3 15 16 10 27 31 6 - Clinical and Laboratory Standards Institute. (2005) Performance standard for antimicrobial susceptibility testing. Document M 100 -S 15. Wayne, PA: CLSI. 2. Clinical and Laboratory Standards Institute (2006). Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Document M 7 -A 7. Wayne, PA, CLSI (in press). 3. Cubicin (daptomycin for injection) [package insert]. Lexington, MA: Cubist Pharmaceuticals, 2003. Munoz-Price LS, Lolans K, Quinn JP. (2005) Emergence of resistance to daptomycin during treatment of vancomycin-resistant Enterococcus faecalis infection. Clinical Infectious Disease 41: 565 -566. 4. National Committee for Clinical Laboratory Standards. (2003). Performance standards for antimicrobial disk susceptibility tests; Approved standard, 8 th ed. Document M 2 -A 8. Wayne, PA: NCCLS 5. National Committee for Clinical Laboratory Standards. (2003) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Document M 7 -A 6. Wayne, PA: NCCLS. 6. Sabol K, Patterson JE, Lewis II JS, Owens A, Cadena J, Jorgensen JH. (2005) Emergence of daptomycin resistance in Enterococcus faecium during daptomycin therapy. Antimicrobial Agents and Chemotherapy 49: 1664 -1665. 7. Sakouloas G, Eliopoulos GM, Alder J, Thauvin-Eliopoulos C. (2003). Efficacy of daptomycin in experimental endocarditis due to methicillinresistant Staphylococcus aureus. Antimicrobial Agents and Chemotherapy 47: 1714 -1718. Wootton M, Howe RA, Walsh TR, Bennett PM, Mac. Gowan AP. (2001). A modified population analysis profile (PAP) method to detect heteroresistance to vancomycin in Staphylococcus aureus in a UK hospital. Journal of Antimicrobial Chemotherapy 47: 399 -403.
Daptomycin Resistance and Vancomycin Intermediate S. aureus in a Patient with Prolonged Antibiotic Therapy. PAUL MARIANI M. D 1 , PAUL CARSON M. D. 1, HELIO SADER, MD, Ph. D 2, RON JONES, MD 2; 1. Univeristy of North Dakota, Fargo, ND, 2. JMI Laboratories, North Liberty, IA. Results Abstract Methods Background: Daptomycin is a lipopeptide with bactericidal activity against Gram-positive drug-resistant organisms with reports of acquired resistance rare. We document the development of resistance to daptomycin and decreased susceptibility to vancomycin during prolonged therapy with these antimicrobials. Case: A 64 year old man developed a methicillin-resistant S. aureus (MRSA) prosthetic hip infection with recurrent bacteremia treated with vancomycin (30 mg/kg/d). On hospital day (HD) # 99 patient underwent prosthesis removal complicated by disseminated intravascular coagulation, acute renal failure and antibiotic therapy changed to daptomycin (6 mg/kg). Patient improved with negative repeat blood cultures. On HD #148 patient developed a T=103. 5°F, wound culture revealed MRSA and an MRI showed a 32 cm thigh abscess. Patient underwent debriédement and bone culture revealed polymicrobial infection with DAPR/VISA treated with dalfopristin-quinupristin (7. 5 mg/kg q 8 h), gatifloxacin, fluconazole. Patient later expired from E faecalis catheter-related sepsis. Methods: S. aureus was isolated on HD #1 (strain # 1), HD #99 (#2) and HD 148 (#3) from blood, surgical wound, and bone, respectively. Strains were tested for S against DAP, VAN and other antimicrobials by CLSI broth microdilution, disk diffusion and Etest. Heteroresistance to vancomycin (h. VISA) was evaluated by inoculating 2 Mac. Farland suspension onto BHI agar with VAN Etest strips and incubating for 48 hours. The strains were typed by automated ribotyping and pulse field gel electrophoresis. Results: All strains were R to oxacillin, clindamycin and ciprofloxacin; and S to gentamicin, linezolid, tetracycline, and tigecycline. Strains #1 and #2 showed MIC of 0. 5, 1 and 0. 06 μg/ml for DAP, VAN, and dalbavancin (DBV), respectively, while strain #3 showed MIC of 8 μg/ml for DAP, 4 μg/ml for vancomycin as a h. VISA, 0. 25 μg/ml for DBV. All 3 strains showed identical molecular typing pattern. Conclusion: Resistance to daptomycin may develop during prolonged treatment of S. aureus infections with DAP. Isolates: Three strains of S. aureus were isolated from a patient including a blood culture on hospitalization day (HD) #1, a surgical wound culture from HD #99 and a bone culture from HD #148. All strains were processed locally and subsequently forwarded to JMI Laboratories (North Liberty, Iowa, USA) for confirmatory susceptibility testing and molecular typing. Susceptibility testing: The strains were tested by Clinical and Laboratory Standards Institute (CLSI; formerly NCCLS) M 7 -A 6 broth microdilution methods in validated, dry-form panels manufactured by TREK Diagnostics, Inc. (Cleveland, Ohio, USA). Daptomycin were tested in Mueller-Hinton broth supplemented to 50 mg/L as recommended by the manufacturer. Disk diffusion methods were performed according to NCCLS M 2 -A 8 method and by Etest (AB BIODISK, Solna, Sweden) generated according to the manufacturer’s guidelines found in the package insert. Molecular typing: Isolates were typed for genetic relatedness using automated ribotyping (Riboprinter. TM Microbial Characterization System, Qualicon, Wilmington, Delaware, USA) of genomic DNA after digestion using Eco. R 1 enzyme to assign a ribogroup. Isolates were also typed by pulsed-field gel electrophoresis (PFGE, Bio. Rad Laboratories, Hercules, California, USA) after DNA digestion with Sma. I. Gels were stained with ethidium bromide to visually identify banding patterns and determine clonal relatedness. Case A 64 year old man was admitted the intensive case unit with methicillin-resistant Staphylococcus aureus (MRSA) sepsis and was treated with 17 -day course of vancomycin. On the 22 nd hospital day patient became febrile and repeat blood cultures reveald MRSA, a 2 D-echocardiogram did not reveal evidence of endocarditis and was treated with a one month course of vancomycin. On the 60 th hospital a WBC tagged scan showed infection of the right prosthetic hip where an aspiration revealed a WBC 47, 000 with culture positive for MRSA. Patient had suffered a myocardial infarction and an episode of acute cholecystitis thus surgery was postponed until 102 nd hospital day yet continued to receive vancomycin as suppressive therapy. Intraoperatively patient developed disseminated intravascular coagulation necessitating aggressive measures for correction of coagulopathy and further complicated by nonoliguric acute renal failure and thrombocytopenia with platelet count 27, 000 and daptomycin 650 mg daily was begun. Patient’s acute medical problems stabilized over the ensuing 4 weeks. On 150 th hospital day patient suddenly developed a fever where repeat bacterial blood cultures were negative, however, a wound culture revealed MRSA and an MRI demonstrated a 32 cm abscess. Patient was again taken to surgery and an acetabular biopsy grew vancomycin intermediate, daptomycin intermediate S aureus, C freundii, and fluconazole susceptible C albicans, C glabrata, C parapsilosis. Patient’s antibiotic therapy was changed to dalfopristin / quinupristins 850 mg / day, gatifloxacin 200 mg / day and fluconazole 400 mg / day. Patient subsequently developed a line-associated dalfopristin/quinupristin resistant E faecalis bacteremia in addition to polymycrobial wound infection. Family opted to withdraw all medical care and patient died shortly thereafter. Table 1. Broth microdilution MIC results for 19 antimicrobial agents tested against three S. aureus isolates recovered from a patient on prolonged therapy. • According to broth microdilution MIC results, all three ORSA strains were resistant to oxacillin, erythromycin, clindamycin, telithromycin and ciprofloxacin, and susceptible to a larger number of antimicrobials (Table 1). Antibiogram analysis of the three S. aureus isolates showed that strains #1 and #2 were more similar with identical daptomycin (0. 5 g/ml), vancomycin (1 g/ml) and dalbavancin (0. 06 g/ml) MIC results. Strain #3 MIC results for these agents were elevated to 8, 4 and 0. 25 g/ml, respectively. Interestingly, strains #1 and #2 were resistant to penicillin ( -lactamase-positive) and strain #3 was -lactamase-negative. Conversely, strain #1 was susceptible to rifampin and strains #2 and #3 were resistant to this antimicrobial. Heteroresistance to vancomycin (h. VISA) was observed on strain #3, which showed MIC values of 12 g/ml for both vancomycin and teicoplanin when tested by Etest using high inoculum. Disk diffusion zone diameter results for daptomycin showed a 3 - 4 mm decrease for strain #3 compared to the first two isolates validating observed higher MIC values. The vancomycin disk zone diameter results did not change (16 mm) as the MIC increased from 1 to 4 g/ml (Table 2). All three S. aureus strains demonstrated an identical molecular typing pattern by two methods (Figure 1). MIC ( g/ml) Strain # (hospital day/culture type) Antimicrobial agent 1 (1/blood) Daptomycin Vancomycin Teicoplanin Dalbavancin Oxacillin Penicillin Clindamycin Erythromycin Telithromycin Quinupristin/dalfopristin Chloramphenicol Ciprofloxacin Gentamicin Linezolid Rifampin Tetracycline Tigecycline Trimethoprim/Sulfamethoxazole 0. 5 1 2 0. 06 >2 16 >2 >8 >4 0. 5 8 >4 2 2 0. 25 2 0. 12 0. 5 2 (99/surgical wound) 0. 5 1 2 0. 06 >2 16 >2 >8 >4 0. 5 8 >4 2 2 >2 2 0. 25 0. 5 3 (148/bone) 8 4 (12)a 2 (12)a 0. 25 >2 0. 12 >2 >8 >4 0. 5 4 >4 2 1 >2 2 0. 06 0. 5 Figure 1. Riboprint patterns of the three S. aureus strains evaluated in the present study. Strains 1 and 2 were susceptible to daptomycin (MIC, 0. 5 g/ml) while strain 3 showed daptomycin MIC of 8 g/ml. Conclusion • Resistance to daptomycin may develop during prolonged treatment of S. aureus infections with daptomycin. a. MIC in parenthesis using an Etest with an elevated inoculum. Selected Reading 1. Table 2. Disk diffusion and -lactamase test results. Zone diameter (mm) Antimicrobial agent Daptomycin Vancomycin Oxacillin Penicillin Linezolid Rifampin -lactamase test Strain #1 18 16 6 8 27 31 + Strain #2 19 16 6 9 27 13 + Strain #3 15 16 10 27 31 6 - Clinical and Laboratory Standards Institute. (2005) Performance standard for antimicrobial susceptibility testing. Document M 100 -S 15. Wayne, PA: CLSI. 2. Clinical and Laboratory Standards Institute (2006). Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Document M 7 -A 7. Wayne, PA, CLSI (in press). 3. Cubicin (daptomycin for injection) [package insert]. Lexington, MA: Cubist Pharmaceuticals, 2003. Munoz-Price LS, Lolans K, Quinn JP. (2005) Emergence of resistance to daptomycin during treatment of vancomycin-resistant Enterococcus faecalis infection. Clinical Infectious Disease 41: 565 -566. 4. National Committee for Clinical Laboratory Standards. (2003). Performance standards for antimicrobial disk susceptibility tests; Approved standard, 8 th ed. Document M 2 -A 8. Wayne, PA: NCCLS 5. National Committee for Clinical Laboratory Standards. (2003) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Document M 7 -A 6. Wayne, PA: NCCLS. 6. Sabol K, Patterson JE, Lewis II JS, Owens A, Cadena J, Jorgensen JH. (2005) Emergence of daptomycin resistance in Enterococcus faecium during daptomycin therapy. Antimicrobial Agents and Chemotherapy 49: 1664 -1665. 7. Sakouloas G, Eliopoulos GM, Alder J, Thauvin-Eliopoulos C. (2003). Efficacy of daptomycin in experimental endocarditis due to methicillinresistant Staphylococcus aureus. Antimicrobial Agents and Chemotherapy 47: 1714 -1718. Wootton M, Howe RA, Walsh TR, Bennett PM, Mac. Gowan AP. (2001). A modified population analysis profile (PAP) method to detect heteroresistance to vancomycin in Staphylococcus aureus in a UK hospital. Journal of Antimicrobial Chemotherapy 47: 399 -403.


