adc0cd3368b5ed9a3c697b9a0f9b55be.ppt
- Количество слайдов: 38
 Cushings, Addisons and Acromegaly Dr J Storrow FY 2
Cushings, Addisons and Acromegaly Dr J Storrow FY 2
 Objectives Brief overview of the pituitary gland Brief overview of all three conditions Review: aetiology presentation investigations complications prognosis Brief case presentations Revision tips
Objectives Brief overview of the pituitary gland Brief overview of all three conditions Review: aetiology presentation investigations complications prognosis Brief case presentations Revision tips
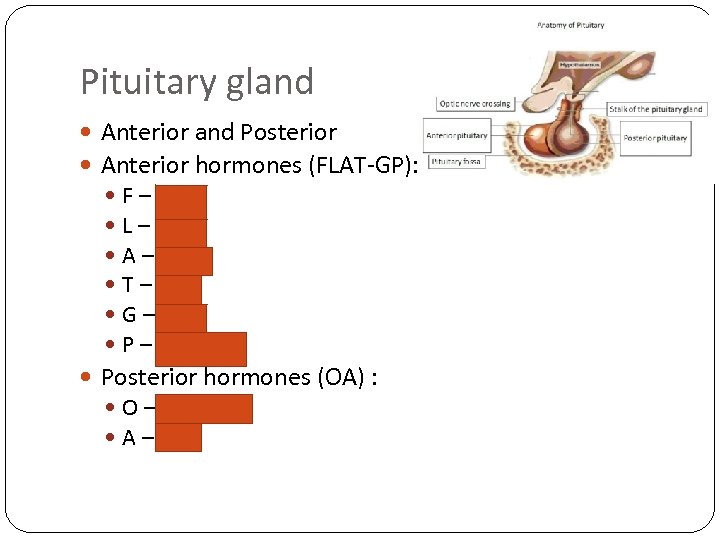 Pituitary gland Anterior and Posterior Anterior hormones (FLAT-GP): F – FSH L – LH A – ACTH T – TSH G – GH P – Prolactin Posterior hormones (OA) : O – Oxytocin A – ADH
Pituitary gland Anterior and Posterior Anterior hormones (FLAT-GP): F – FSH L – LH A – ACTH T – TSH G – GH P – Prolactin Posterior hormones (OA) : O – Oxytocin A – ADH
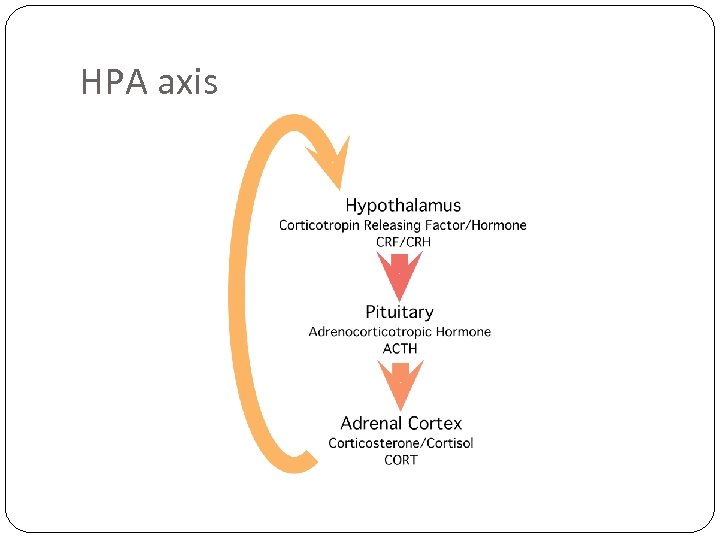 HPA axis
HPA axis
 Definitions Cushings Increased glucocorticoid exposure Addisons Chronic primary adrenocortical insufficiency Acromegaly Increased growth hormone production
Definitions Cushings Increased glucocorticoid exposure Addisons Chronic primary adrenocortical insufficiency Acromegaly Increased growth hormone production
 Cushings
Cushings
 Disease vs. Syndrome Cushings Disease is the result of a pituitary tumour secreting inappropriate ACTH Cushings Syndrome causes the same symptoms, but is caused by overproduction of adrenal hormones. It encompasses all other forms of Cushings Basically: Disease = increased cortisol from pituitary Syndrome = all other sources
Disease vs. Syndrome Cushings Disease is the result of a pituitary tumour secreting inappropriate ACTH Cushings Syndrome causes the same symptoms, but is caused by overproduction of adrenal hormones. It encompasses all other forms of Cushings Basically: Disease = increased cortisol from pituitary Syndrome = all other sources
 Aetiology Harvey Cushing in 1932 Endogenous Causes: 65% = pituitary 25% = adrenals = Females 5: 1 ratio and ages 25 -40 10% = ectopic source (small cell lung ca), non-pituitary, ACTH producing tumour Exogenous Causes: Iatrogenic Steroids (Asthma, RA, palliative) Higher incidence in people with: DM, HTN, Obesity and Osteoporosis
Aetiology Harvey Cushing in 1932 Endogenous Causes: 65% = pituitary 25% = adrenals = Females 5: 1 ratio and ages 25 -40 10% = ectopic source (small cell lung ca), non-pituitary, ACTH producing tumour Exogenous Causes: Iatrogenic Steroids (Asthma, RA, palliative) Higher incidence in people with: DM, HTN, Obesity and Osteoporosis
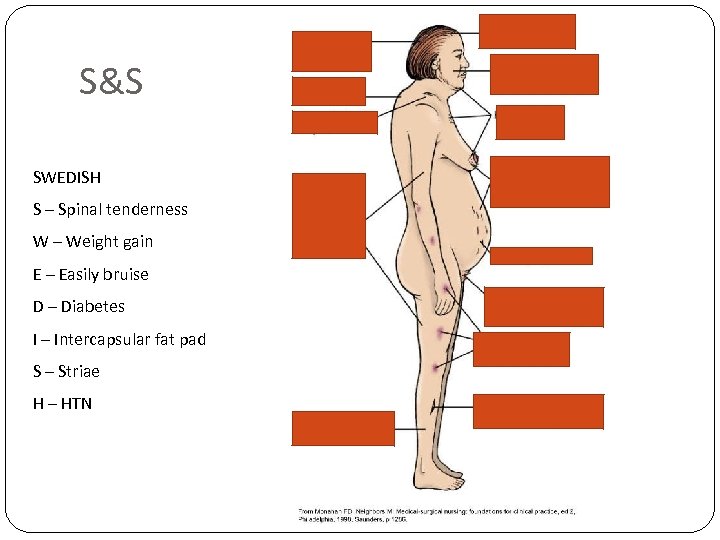 S&S SWEDISH S – Spinal tenderness W – Weight gain E – Easily bruise D – Diabetes I – Intercapsular fat pad S – Striae H – HTN
S&S SWEDISH S – Spinal tenderness W – Weight gain E – Easily bruise D – Diabetes I – Intercapsular fat pad S – Striae H – HTN
 Differential Diagnosis Pseudo-Cushingoid: Chronic severe anxiety and/or depression Prolonged excess alcohol consumption Obesity Poorly controlled diabetes HIV infection
Differential Diagnosis Pseudo-Cushingoid: Chronic severe anxiety and/or depression Prolonged excess alcohol consumption Obesity Poorly controlled diabetes HIV infection
 Investigations Bedside? Bloods tests – which and why? FBC – raised WCC U/E – low K Special tests: Cortisol at midnight and 0900 (loss of diurnal variation – should be low at midnight <550) – less reliable 24 hour urinary cortisol – 3 collections 24 hour salivary cortisol sampling Dexamethasone Suppression Test
Investigations Bedside? Bloods tests – which and why? FBC – raised WCC U/E – low K Special tests: Cortisol at midnight and 0900 (loss of diurnal variation – should be low at midnight <550) – less reliable 24 hour urinary cortisol – 3 collections 24 hour salivary cortisol sampling Dexamethasone Suppression Test
 Dexamethasone Suppression Test Overnight Low dose = Baseline reading, Dex 1 mg given at 11 pm, measure cortisol at 8 am If cortisol low (<50 nmol/L) = normal If cortisol high (>50 nmol/L) = investigate further – Cushings syndrome Localising the lesion: Plasma ACTH if undetectable = adrenal cause (as adrenal cause independent of ACTH) If detected – proceed to high dose dex suppression test High dose if >90% suppression – pituitary if less/no suppression – ectopic source
Dexamethasone Suppression Test Overnight Low dose = Baseline reading, Dex 1 mg given at 11 pm, measure cortisol at 8 am If cortisol low (<50 nmol/L) = normal If cortisol high (>50 nmol/L) = investigate further – Cushings syndrome Localising the lesion: Plasma ACTH if undetectable = adrenal cause (as adrenal cause independent of ACTH) If detected – proceed to high dose dex suppression test High dose if >90% suppression – pituitary if less/no suppression – ectopic source
 Investigations If any positive - imaging: CT of adrenals MRI pituitary If ? ectopic: CXR CT =/- MRI of neck, thorax, abdomen
Investigations If any positive - imaging: CT of adrenals MRI pituitary If ? ectopic: CXR CT =/- MRI of neck, thorax, abdomen
 Management Always split in to: Conservative Medical Surgical
Management Always split in to: Conservative Medical Surgical
 Management Drug therapy remains very important for normalising cortisol levels. Medical treatment can also be used in patients who are unwilling or unfit for surgery. Metyrapone, ketoconazole, and mitotane can all be used to lower cortisol by directly inhibiting synthesis and secretion in the adrenal gland. The treatment of choice in most patients is surgical but the metabolic consequences increase the risk of surgery: increased tissue fragility poor wound healing HTN and DM
Management Drug therapy remains very important for normalising cortisol levels. Medical treatment can also be used in patients who are unwilling or unfit for surgery. Metyrapone, ketoconazole, and mitotane can all be used to lower cortisol by directly inhibiting synthesis and secretion in the adrenal gland. The treatment of choice in most patients is surgical but the metabolic consequences increase the risk of surgery: increased tissue fragility poor wound healing HTN and DM
 Surgical Treatment Pituitary tumours: trans-sphenoidal microsurgery. Radiation therapy may be used as an adjunct for patients who are not cured. Bilateral adrenalectomy may be necessary to control toxic cortisol levels. Adrenocortical tumours: require surgical removal – can develop Nelsons Syndrome Removal of neoplastic tissue is indicated for ectopic ACTH production. Metastatic spread makes a surgical cure unlikely or impossible. Bilateral adrenalectomy is indicated if necessary to control toxic cortisol levels.
Surgical Treatment Pituitary tumours: trans-sphenoidal microsurgery. Radiation therapy may be used as an adjunct for patients who are not cured. Bilateral adrenalectomy may be necessary to control toxic cortisol levels. Adrenocortical tumours: require surgical removal – can develop Nelsons Syndrome Removal of neoplastic tissue is indicated for ectopic ACTH production. Metastatic spread makes a surgical cure unlikely or impossible. Bilateral adrenalectomy is indicated if necessary to control toxic cortisol levels.
 Prognosis Patients with incompletely controlled Cushing's syndrome have a five-fold excess mortality. Premature death in untreated Cushing's syndrome are caused by vascular disease (MI/CVA), uncontrolled DM and infections. The usual course is chronic, with cyclical exacerbations and rare remissions. The prognosis is better with surgery. The rare adrenocortical carcinomas have a 5 -year survival rate of 30% or less.
Prognosis Patients with incompletely controlled Cushing's syndrome have a five-fold excess mortality. Premature death in untreated Cushing's syndrome are caused by vascular disease (MI/CVA), uncontrolled DM and infections. The usual course is chronic, with cyclical exacerbations and rare remissions. The prognosis is better with surgery. The rare adrenocortical carcinomas have a 5 -year survival rate of 30% or less.
 Addisons
Addisons
 Aetiology Dr Thomas Addison in 1855 True Addisons: Affects 1 in 10000 in UK – rare Common presentation between 30 and 50 Affects women more 70 -90% have autoimmune basis – cytotoxic T cells Clinical and biochemical insufficiency only occurs once >90% of the gland is destroyed. Primary = adrenals Secondary = pituitary Tertiary = hypothalamus
Aetiology Dr Thomas Addison in 1855 True Addisons: Affects 1 in 10000 in UK – rare Common presentation between 30 and 50 Affects women more 70 -90% have autoimmune basis – cytotoxic T cells Clinical and biochemical insufficiency only occurs once >90% of the gland is destroyed. Primary = adrenals Secondary = pituitary Tertiary = hypothalamus
 Aetiology continued TB (most common worldwide) infections – AIDS, fungal Adrenal haemorrhage (caused by sepsis, meningitis) Metastatic spread to adrenals Amyloidosis Adrenalectomy Genetic/congenital defects Addsions = long term steroids leading to suppression of HPA axis
Aetiology continued TB (most common worldwide) infections – AIDS, fungal Adrenal haemorrhage (caused by sepsis, meningitis) Metastatic spread to adrenals Amyloidosis Adrenalectomy Genetic/congenital defects Addsions = long term steroids leading to suppression of HPA axis
 S&S
S&S
 Investigations Bedside? Blood tests: Low Na, low cortisol Low aldosterone causing high K, High adrenocorticotrophic hormone (ACTH) Low glucose High TSH – indicates what? Imaging? CXR – why? CT/MRI adrenals
Investigations Bedside? Blood tests: Low Na, low cortisol Low aldosterone causing high K, High adrenocorticotrophic hormone (ACTH) Low glucose High TSH – indicates what? Imaging? CXR – why? CT/MRI adrenals
 Investigations - Synacthen Test Nightmare for busy house officer! How do you perform it? Measures cortisol Short – no cortisol produced (no response) Long allows differentiation Primary – No cortisol produced (ACTH high) = adrenal Secondary – Cortisol produced (ACTH low) = pit If initial cortisol is >140 nmol/L and second cortisol is >400 -500 nmol/L, this excludes Addison's disease (most common finding!) The test can be performed at any time of day.
Investigations - Synacthen Test Nightmare for busy house officer! How do you perform it? Measures cortisol Short – no cortisol produced (no response) Long allows differentiation Primary – No cortisol produced (ACTH high) = adrenal Secondary – Cortisol produced (ACTH low) = pit If initial cortisol is >140 nmol/L and second cortisol is >400 -500 nmol/L, this excludes Addison's disease (most common finding!) The test can be performed at any time of day.
 Management C, M, S (no surgical) Conservative = lifestyle Medic. Alert bracelet and steroid card. Importance of not missing steroids. Intercurrent illness - if tolerating oral medication the dose should be doubled until better Medical = Replace steroids Glucocorticoid replacement - hydrocortisone is the mainstay of treatment; dose divided into two thirds in the morning and one third in the late afternoon (thus stimulating the normal diurnal adrenal rhythm). Mineralocorticoid replacement - this is usually required in primary adrenal insufficiency – Fludrocortisone (what else used for – clue = elderly who fall)
Management C, M, S (no surgical) Conservative = lifestyle Medic. Alert bracelet and steroid card. Importance of not missing steroids. Intercurrent illness - if tolerating oral medication the dose should be doubled until better Medical = Replace steroids Glucocorticoid replacement - hydrocortisone is the mainstay of treatment; dose divided into two thirds in the morning and one third in the late afternoon (thus stimulating the normal diurnal adrenal rhythm). Mineralocorticoid replacement - this is usually required in primary adrenal insufficiency – Fludrocortisone (what else used for – clue = elderly who fall)
 Complications – Addisonian Crisis severe dehydration pale, cold, clammy skin sweating rapid, shallow breathing dizziness severe vomiting and diarrhoea severe muscle weakness headache severe drowsiness or loss of consciousness coma and death
Complications – Addisonian Crisis severe dehydration pale, cold, clammy skin sweating rapid, shallow breathing dizziness severe vomiting and diarrhoea severe muscle weakness headache severe drowsiness or loss of consciousness coma and death
 Treatment of crisis Medical emergency Bloods, large bore cannula Seek help if you suspect Iv Hydrocortisone Iv fluids Iv glucose if needed
Treatment of crisis Medical emergency Bloods, large bore cannula Seek help if you suspect Iv Hydrocortisone Iv fluids Iv glucose if needed
 Prognosis Depends upon the underlying cause In those patients in whom the prognosis is not affected by the underlying pathology, replacement therapy should result in a return to health with a normal life expectancy.
Prognosis Depends upon the underlying cause In those patients in whom the prognosis is not affected by the underlying pathology, replacement therapy should result in a return to health with a normal life expectancy.
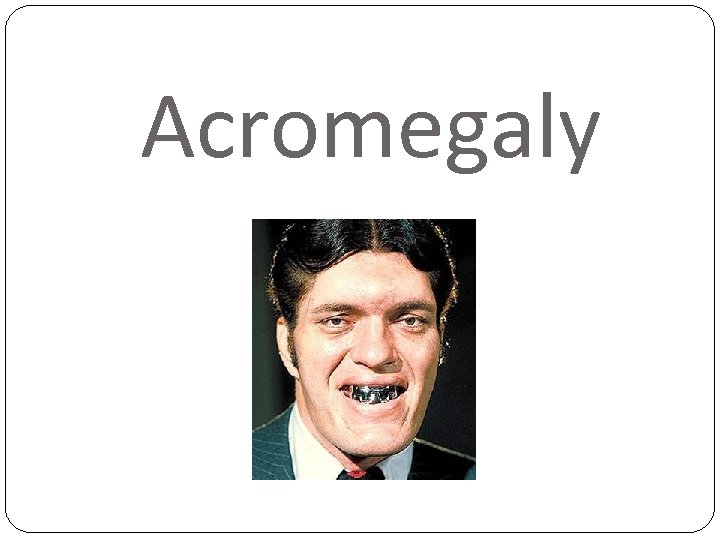 Acromegaly
Acromegaly
 Aetiology Pituitary tumour >99% (very rarely ectopic (carcinoid) M: F = 1: 1 30 -50 y old 5% genetic association with MEN 1 GH stimulates soft tissue and skeletal growth through increased secretion of IGF-1 and secretion inhibited by somatostatin
Aetiology Pituitary tumour >99% (very rarely ectopic (carcinoid) M: F = 1: 1 30 -50 y old 5% genetic association with MEN 1 GH stimulates soft tissue and skeletal growth through increased secretion of IGF-1 and secretion inhibited by somatostatin
 S&S A – Arthopathy B – BP high C – Carpal tunnel D – Diabetes & HF E – Enlarged tongue/heart F – Field defect - hemianopia
S&S A – Arthopathy B – BP high C – Carpal tunnel D – Diabetes & HF E – Enlarged tongue/heart F – Field defect - hemianopia
 Investigations Bedside? Bloods? Random GH levels – not helpful (stress/sleep/pregnancy) IGF-1 increased in 75% people Special tests: OGTT: Measure glucose and GH at 0, 30, 60, 90, 120, 150 mins Normally glucose causes GH suppression If Acromegaly – no GH suppression False +ves – puberty, pregnancy, hepato-renal disease, anorexia, DM
Investigations Bedside? Bloods? Random GH levels – not helpful (stress/sleep/pregnancy) IGF-1 increased in 75% people Special tests: OGTT: Measure glucose and GH at 0, 30, 60, 90, 120, 150 mins Normally glucose causes GH suppression If Acromegaly – no GH suppression False +ves – puberty, pregnancy, hepato-renal disease, anorexia, DM
 Investigations Imaging: MRI pituitary Visual fieds and acuity ECG/Echo
Investigations Imaging: MRI pituitary Visual fieds and acuity ECG/Echo
 Treatment – C, M, S Medical: Somatostatin analogues - Octreotide Inhibit GH secretion Monthly IM injection Controls GH and IGF 1 in 60% GH recpetor antagonists – Pegvisomant Supresses IGF 1 in 90% but GH levels rise Can cause tumour size to increase
Treatment – C, M, S Medical: Somatostatin analogues - Octreotide Inhibit GH secretion Monthly IM injection Controls GH and IGF 1 in 60% GH recpetor antagonists – Pegvisomant Supresses IGF 1 in 90% but GH levels rise Can cause tumour size to increase
 Surgical Trans-sphenoidal surgery Cures 80% microadenomas and 40% macroadenomas Can try radiotherapy if surgery inappropriate – can take years to work
Surgical Trans-sphenoidal surgery Cures 80% microadenomas and 40% macroadenomas Can try radiotherapy if surgery inappropriate – can take years to work
 Complications Impaired GT – 40% DM – 20% (GH counter regulates insulin) Vascular – HTN, LVH, IHD/CVA Malignancy – colonic polyps – controversial Mortality 2 -3 times (vascular risk)
Complications Impaired GT – 40% DM – 20% (GH counter regulates insulin) Vascular – HTN, LVH, IHD/CVA Malignancy – colonic polyps – controversial Mortality 2 -3 times (vascular risk)
 Case presentations 30 year old woman presents feeling unwell and dizzy, loss of weight, decreased libido and darker skin but also some areas of very light skin. Treated for anorexia 2 years ago 50 year old man presents saying his rings are becoming tighter on his hands and he’s had to buy bigger shoes. Keeps walking into things 30 year old woman has noticed weight gain especially around face and abdomen, hair loss, bruises easily, urinating more often
Case presentations 30 year old woman presents feeling unwell and dizzy, loss of weight, decreased libido and darker skin but also some areas of very light skin. Treated for anorexia 2 years ago 50 year old man presents saying his rings are becoming tighter on his hands and he’s had to buy bigger shoes. Keeps walking into things 30 year old woman has noticed weight gain especially around face and abdomen, hair loss, bruises easily, urinating more often
 Revision Tips Look at the patient and around the patient’s bedside Think logically: S&S lead to what investigations which leads to management which leads to complications which leads to prognosis Management in to conservative, medical, surgical Investigations: start bedside then move to desk then walk to xray etc: Obs, urine dip, ECG, BM, clinical exam Bloods, Iv fluids, VTE (anti-coag? ), Kardex (meds) CXR, AXR, USS, CT/MRI If endocrine – consider bloods for other pituitary hormones Hyperprolactinaemia is most common disorder
Revision Tips Look at the patient and around the patient’s bedside Think logically: S&S lead to what investigations which leads to management which leads to complications which leads to prognosis Management in to conservative, medical, surgical Investigations: start bedside then move to desk then walk to xray etc: Obs, urine dip, ECG, BM, clinical exam Bloods, Iv fluids, VTE (anti-coag? ), Kardex (meds) CXR, AXR, USS, CT/MRI If endocrine – consider bloods for other pituitary hormones Hyperprolactinaemia is most common disorder
 Tips for finals/FY 1 Be nice to nurses/pharmacists/physios Always ask if you don’t know what to do (inc exams – shows safety and professionalism) Prioritise jobs THINK LOGICALLY – start with basic things Learn sepsis six Learn medical emergencies – you might just save a life Hyperkalaemia Massive UGI bleed Anaphylaxis DKA Meningitis Seizures + status Hypoglycaemia
Tips for finals/FY 1 Be nice to nurses/pharmacists/physios Always ask if you don’t know what to do (inc exams – shows safety and professionalism) Prioritise jobs THINK LOGICALLY – start with basic things Learn sepsis six Learn medical emergencies – you might just save a life Hyperkalaemia Massive UGI bleed Anaphylaxis DKA Meningitis Seizures + status Hypoglycaemia


