f59174a8285a06b8cf9133b699054538.ppt
- Количество слайдов: 34
 CRT 2011 Cool New Therapies for Cardiac Arrest: What you need to know to save lives Dr. Michael Mooney Director Interventional Cardiology Minneapolis Heart Institute Associate Professor of Clinical Medicine University of Minnesota
CRT 2011 Cool New Therapies for Cardiac Arrest: What you need to know to save lives Dr. Michael Mooney Director Interventional Cardiology Minneapolis Heart Institute Associate Professor of Clinical Medicine University of Minnesota
 Michael R. Mooney, MD I have no real or apparent conflicts of interest to report. I intend to reference off label or unapproved uses of drugs or devices in my presentation. I intend to discuss therapeutic hypmia which is not FDA approved, it is ILCOR and ACC indicated, however.
Michael R. Mooney, MD I have no real or apparent conflicts of interest to report. I intend to reference off label or unapproved uses of drugs or devices in my presentation. I intend to discuss therapeutic hypmia which is not FDA approved, it is ILCOR and ACC indicated, however.
 Cardiac Arrest • Out-of-hospital cardiac arrest (OOHCA) affects 295, 000 people annually in the US • 7. 9% median survival rate • Anoxic encephalopathy and neurologic deficits are common and disabling - among survivors • Modest gain with CPR advances, many failed clinical trials – BRCT - barbiturates • Enormous public health issue - personal, family & societal burdens • Growing awareness of needed cardio-cerebral protection Lloyd-Jones D, Adams R, Carnethon M et al. Heart disease and stroke statistics-2009 update. Circulation 2009; 119: e 21 -e 181.
Cardiac Arrest • Out-of-hospital cardiac arrest (OOHCA) affects 295, 000 people annually in the US • 7. 9% median survival rate • Anoxic encephalopathy and neurologic deficits are common and disabling - among survivors • Modest gain with CPR advances, many failed clinical trials – BRCT - barbiturates • Enormous public health issue - personal, family & societal burdens • Growing awareness of needed cardio-cerebral protection Lloyd-Jones D, Adams R, Carnethon M et al. Heart disease and stroke statistics-2009 update. Circulation 2009; 119: e 21 -e 181.
 Hypothermia Pivotal Studies HACA, 2002 Bernard, 2002
Hypothermia Pivotal Studies HACA, 2002 Bernard, 2002
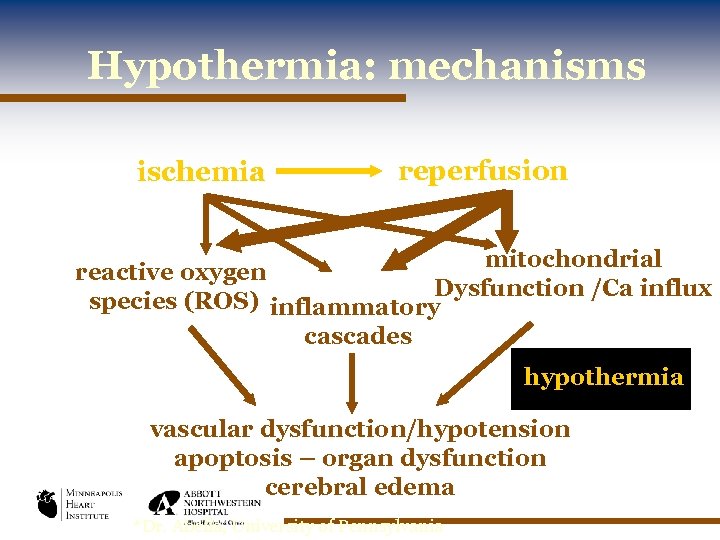 Hypothermia: mechanisms ischemia reperfusion mitochondrial reactive oxygen Dysfunction /Ca influx species (ROS) inflammatory cascades hypothermia vascular dysfunction/hypotension apoptosis – organ dysfunction cerebral edema *Dr. Abella, University of Pennsylvania
Hypothermia: mechanisms ischemia reperfusion mitochondrial reactive oxygen Dysfunction /Ca influx species (ROS) inflammatory cascades hypothermia vascular dysfunction/hypotension apoptosis – organ dysfunction cerebral edema *Dr. Abella, University of Pennsylvania
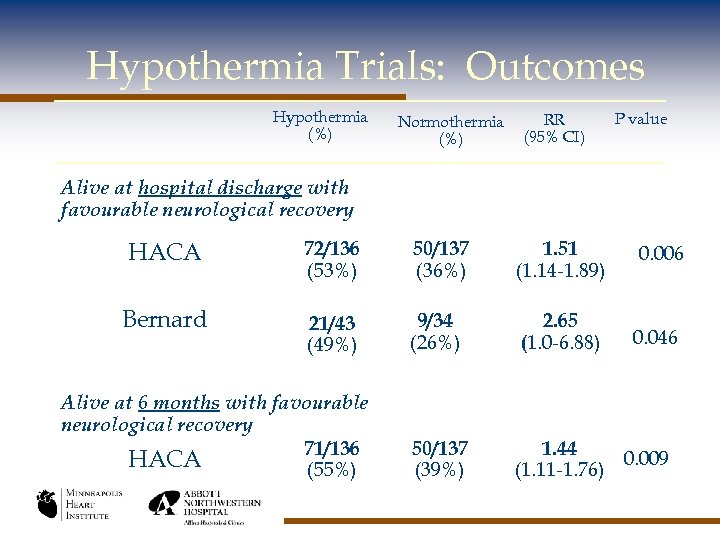 Hypothermia Trials: Outcomes Hypothermia (%) Normothermia (%) RR (95% CI) P value Alive at hospital discharge with favourable neurological recovery HACA 72/136 (53%) 50/137 (36%) 1. 51 (1. 14 -1. 89) 0. 006 Bernard 21/43 (49%) 9/34 (26%) 2. 65 (1. 0 -6. 88) 0. 046 50/137 (39%) 1. 44 0. 009 (1. 11 -1. 76) Alive at 6 months with favourable neurological recovery 71/136 HACA (55%)
Hypothermia Trials: Outcomes Hypothermia (%) Normothermia (%) RR (95% CI) P value Alive at hospital discharge with favourable neurological recovery HACA 72/136 (53%) 50/137 (36%) 1. 51 (1. 14 -1. 89) 0. 006 Bernard 21/43 (49%) 9/34 (26%) 2. 65 (1. 0 -6. 88) 0. 046 50/137 (39%) 1. 44 0. 009 (1. 11 -1. 76) Alive at 6 months with favourable neurological recovery 71/136 HACA (55%)
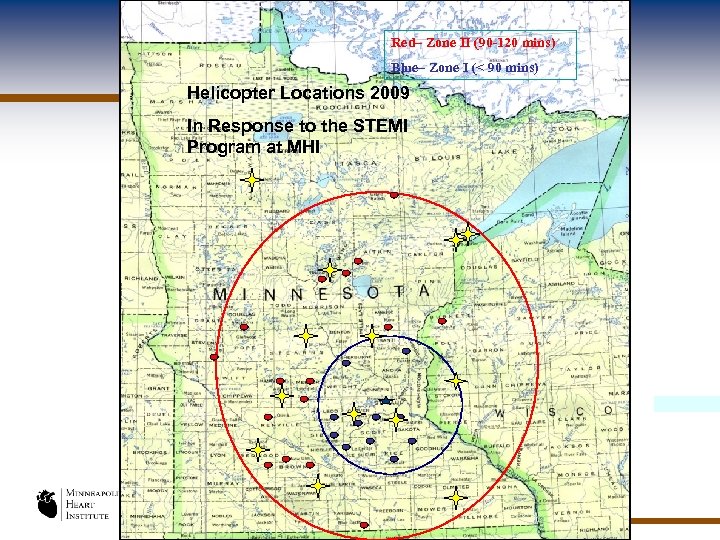 Red– Zone II (90 -120 mins) Blue– Zone I (< 90 mins) Helicopter Locations (90 -120 mins) Red– Zone II 2009 Blue– the I (< 9 mins) In Response to Zone STEMI Program at MHI .
Red– Zone II (90 -120 mins) Blue– Zone I (< 90 mins) Helicopter Locations (90 -120 mins) Red– Zone II 2009 Blue– the I (< 9 mins) In Response to Zone STEMI Program at MHI .
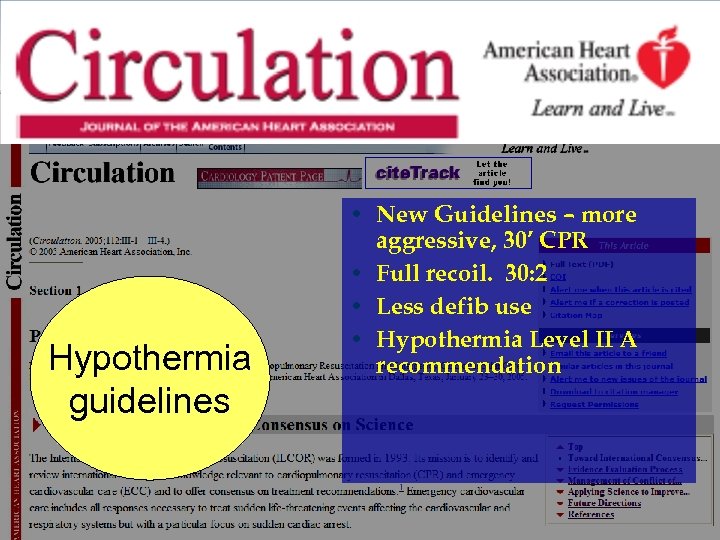 Hypothermia guidelines • New Guidelines – more aggressive, 30’ CPR • Full recoil. 30: 2 • Less defib use • Hypothermia Level II A recommendation
Hypothermia guidelines • New Guidelines – more aggressive, 30’ CPR • Full recoil. 30: 2 • Less defib use • Hypothermia Level II A recommendation
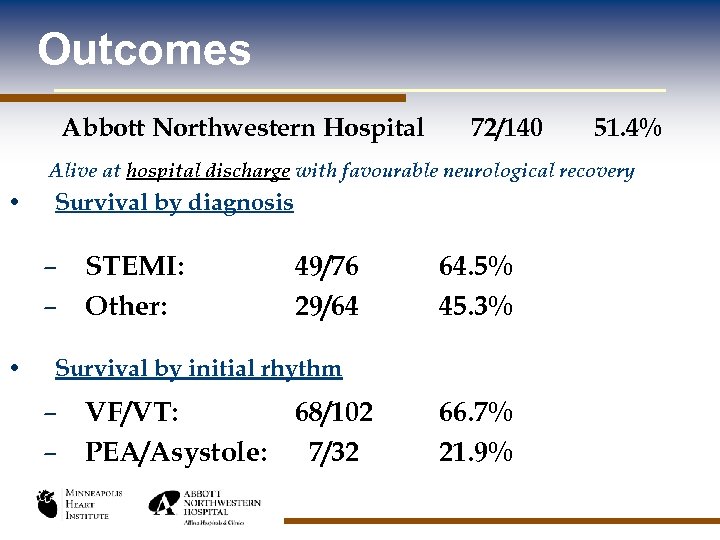 Outcomes Abbott Northwestern Hospital 72/140 51. 4% Alive at hospital discharge with favourable neurological recovery • Survival by diagnosis – STEMI: – Other: • 49/76 29/64 64. 5% 45. 3% Survival by initial rhythm – VF/VT: 68/102 – PEA/Asystole: 7/32 66. 7% 21. 9%
Outcomes Abbott Northwestern Hospital 72/140 51. 4% Alive at hospital discharge with favourable neurological recovery • Survival by diagnosis – STEMI: – Other: • 49/76 29/64 64. 5% 45. 3% Survival by initial rhythm – VF/VT: 68/102 – PEA/Asystole: 7/32 66. 7% 21. 9%
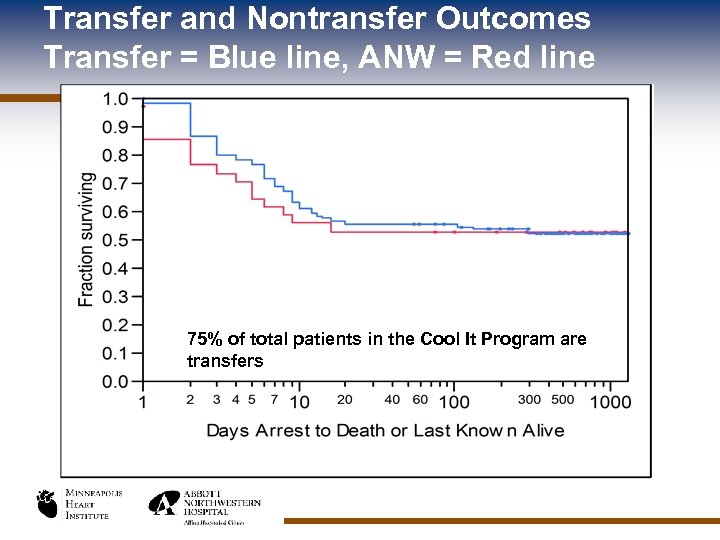 Transfer and Nontransfer Outcomes Transfer = Blue line, ANW = Red line 75% of total patients in the Cool It Program are transfers
Transfer and Nontransfer Outcomes Transfer = Blue line, ANW = Red line 75% of total patients in the Cool It Program are transfers
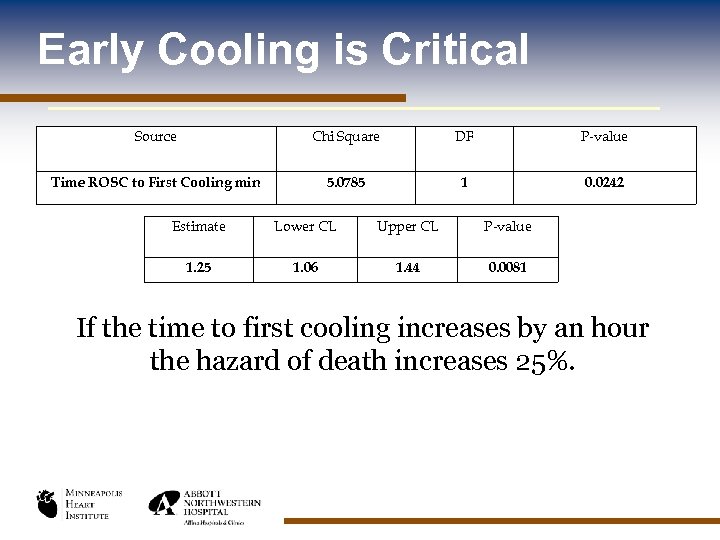 Early Cooling is Critical Source Chi Square DF P-value Time ROSC to First Cooling min 5. 0785 1 0. 0242 Estimate Lower CL Upper CL P-value 1. 25 1. 06 1. 44 0. 0081 If the time to first cooling increases by an hour the hazard of death increases 25%.
Early Cooling is Critical Source Chi Square DF P-value Time ROSC to First Cooling min 5. 0785 1 0. 0242 Estimate Lower CL Upper CL P-value 1. 25 1. 06 1. 44 0. 0081 If the time to first cooling increases by an hour the hazard of death increases 25%.
 Hypothermia – The Year in Review New Technology Randomized trials Rapid MI-ICE – Gotberg , Lund SW Prince – Bene. Chill
Hypothermia – The Year in Review New Technology Randomized trials Rapid MI-ICE – Gotberg , Lund SW Prince – Bene. Chill
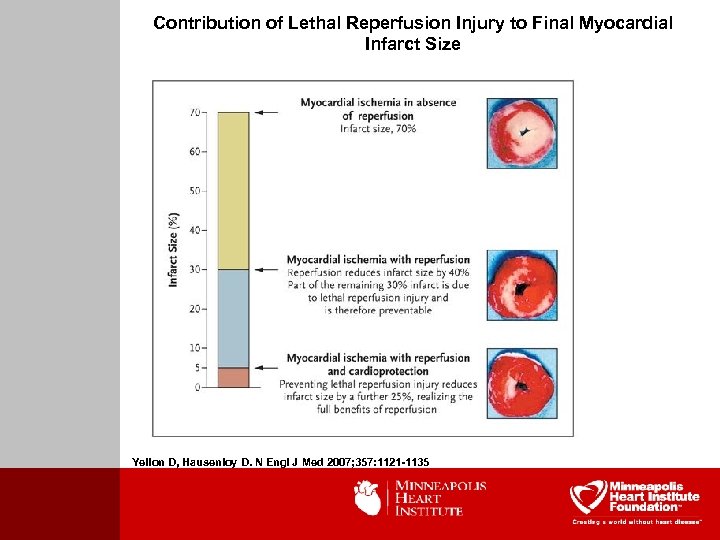 Contribution of Lethal Reperfusion Injury to Final Myocardial Infarct Size Yellon D, Hausenloy D. N Engl J Med 2007; 357: 1121 -1135
Contribution of Lethal Reperfusion Injury to Final Myocardial Infarct Size Yellon D, Hausenloy D. N Engl J Med 2007; 357: 1121 -1135
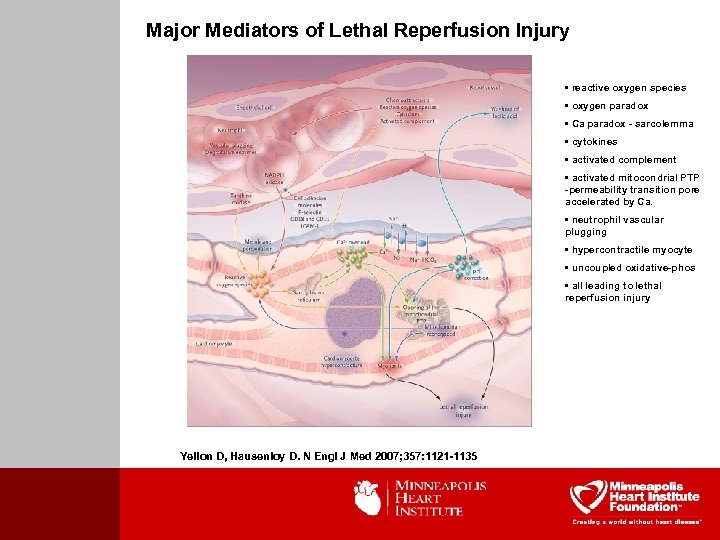 Major Mediators of Lethal Reperfusion Injury • reactive oxygen species • oxygen paradox • Ca paradox - sarcolemma • cytokines • activated complement • activated mitocondrial PTP -permeability transition pore accelerated by Ca. • neutrophil vascular plugging • hypercontractile myocyte • uncoupled oxidative-phos • all leading to lethal reperfusion injury Yellon D, Hausenloy D. N Engl J Med 2007; 357: 1121 -1135
Major Mediators of Lethal Reperfusion Injury • reactive oxygen species • oxygen paradox • Ca paradox - sarcolemma • cytokines • activated complement • activated mitocondrial PTP -permeability transition pore accelerated by Ca. • neutrophil vascular plugging • hypercontractile myocyte • uncoupled oxidative-phos • all leading to lethal reperfusion injury Yellon D, Hausenloy D. N Engl J Med 2007; 357: 1121 -1135
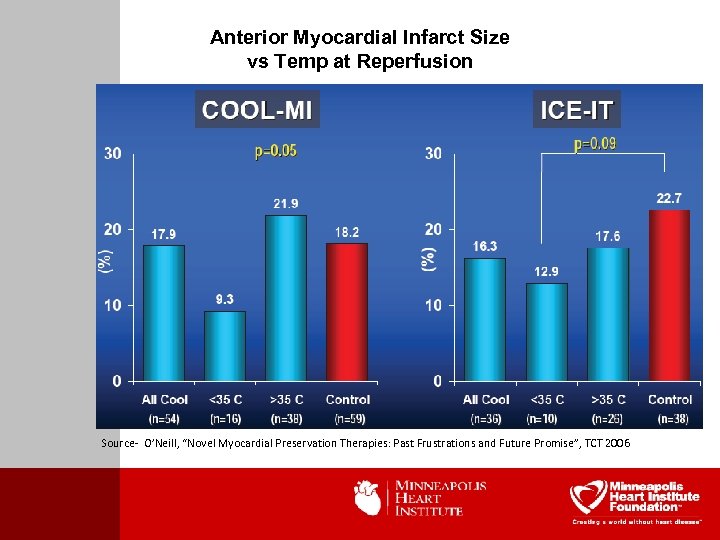 Anterior Myocardial Infarct Size vs Temp at Reperfusion Source- O’Neill, “Novel Myocardial Preservation Therapies: Past Frustrations and Future Promise”, TCT 2006
Anterior Myocardial Infarct Size vs Temp at Reperfusion Source- O’Neill, “Novel Myocardial Preservation Therapies: Past Frustrations and Future Promise”, TCT 2006
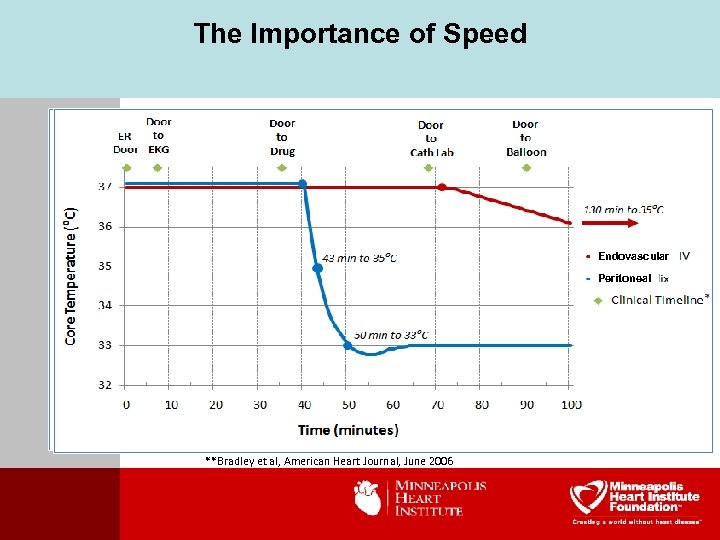 The Importance of Speed Endovascular Peritoneal * **Bradley et al, American Heart Journal, June 2006
The Importance of Speed Endovascular Peritoneal * **Bradley et al, American Heart Journal, June 2006
 Why Use the Peritoneal Cavity? • Efficient heat exchange • • • § > 50% of total blood flow § Large surface area Time to target (10 - 15 minutes to 34°C) Eliminates femoral access interference Eliminates upper chest and neck area interference
Why Use the Peritoneal Cavity? • Efficient heat exchange • • • § > 50% of total blood flow § Large surface area Time to target (10 - 15 minutes to 34°C) Eliminates femoral access interference Eliminates upper chest and neck area interference
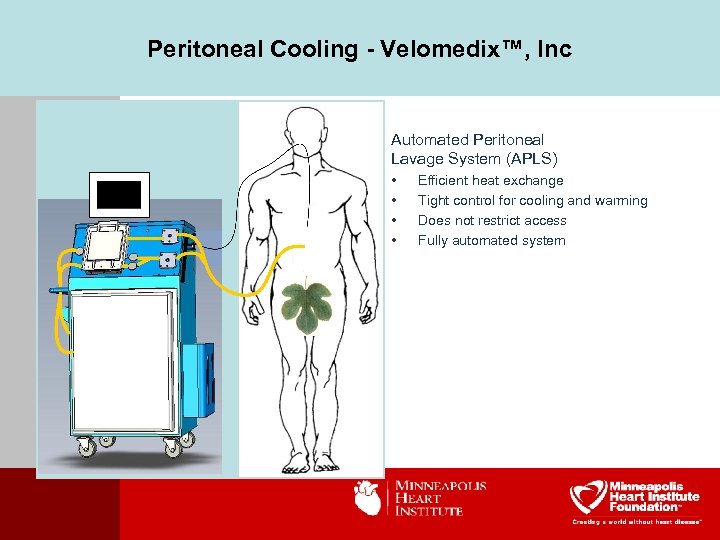 Peritoneal Cooling - Velomedix™, Inc Automated Peritoneal Lavage System (APLS) • • Efficient heat exchange Tight control for cooling and warming Does not restrict access Fully automated system
Peritoneal Cooling - Velomedix™, Inc Automated Peritoneal Lavage System (APLS) • • Efficient heat exchange Tight control for cooling and warming Does not restrict access Fully automated system
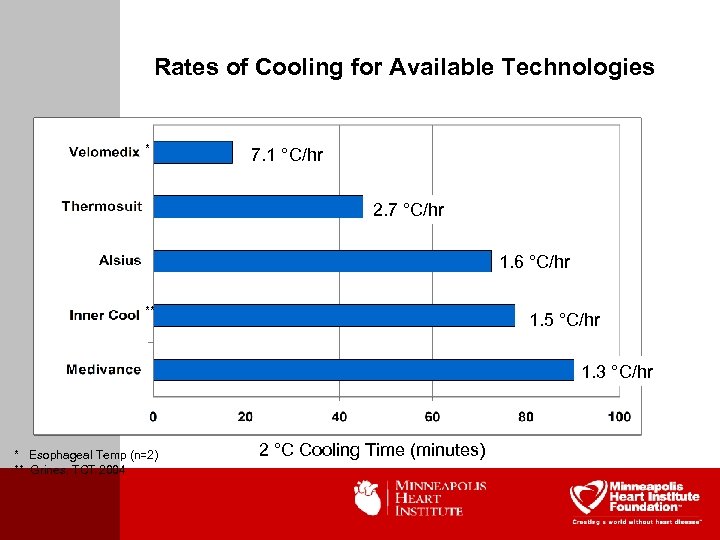 Rates of Cooling for Available Technologies * 7. 1 °C/hr 2. 7 °C/hr 1. 6 °C/hr ** 1. 5 °C/hr 1. 3 °C/hr * Esophageal Temp (n=2) ** Grines, TCT 2004 2 °C Cooling Time (minutes)
Rates of Cooling for Available Technologies * 7. 1 °C/hr 2. 7 °C/hr 1. 6 °C/hr ** 1. 5 °C/hr 1. 3 °C/hr * Esophageal Temp (n=2) ** Grines, TCT 2004 2 °C Cooling Time (minutes)
 Life Recovery Systems
Life Recovery Systems
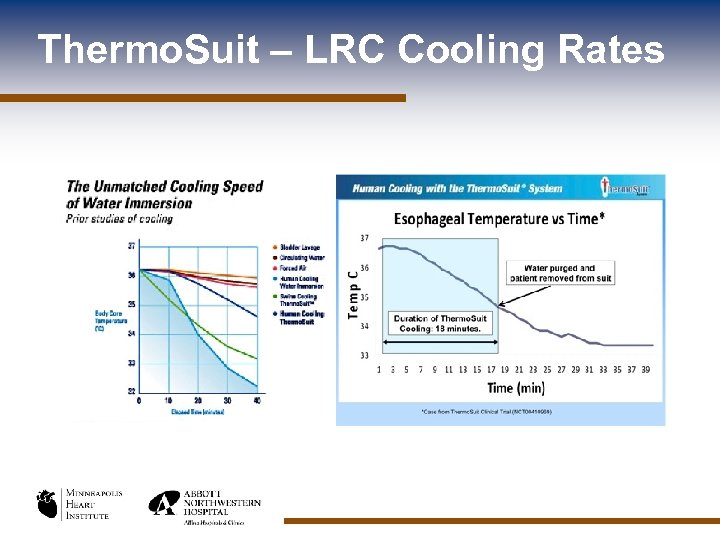 Thermo. Suit – LRC Cooling Rates
Thermo. Suit – LRC Cooling Rates
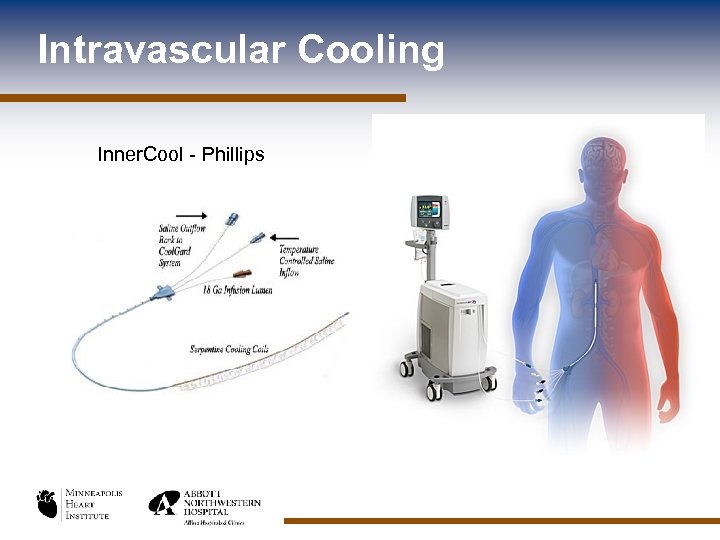 Intravascular Cooling Inner. Cool - Phillips
Intravascular Cooling Inner. Cool - Phillips
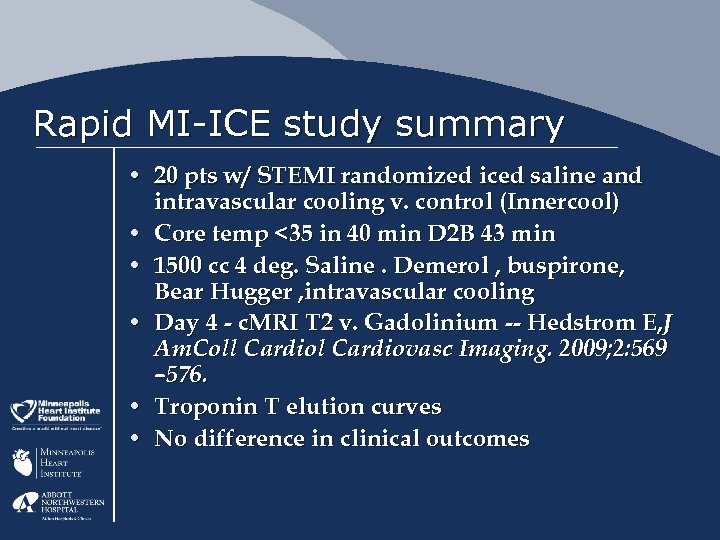 Rapid MI-ICE study summary • 20 pts w/ STEMI randomized iced saline and intravascular cooling v. control (Innercool) • Core temp <35 in 40 min D 2 B 43 min • 1500 cc 4 deg. Saline. Demerol , buspirone, Bear Hugger , intravascular cooling • Day 4 - c. MRI T 2 v. Gadolinium -- Hedstrom E, J Am. Coll Cardiovasc Imaging. 2009; 2: 569 – 576. • Troponin T elution curves • No difference in clinical outcomes
Rapid MI-ICE study summary • 20 pts w/ STEMI randomized iced saline and intravascular cooling v. control (Innercool) • Core temp <35 in 40 min D 2 B 43 min • 1500 cc 4 deg. Saline. Demerol , buspirone, Bear Hugger , intravascular cooling • Day 4 - c. MRI T 2 v. Gadolinium -- Hedstrom E, J Am. Coll Cardiovasc Imaging. 2009; 2: 569 – 576. • Troponin T elution curves • No difference in clinical outcomes
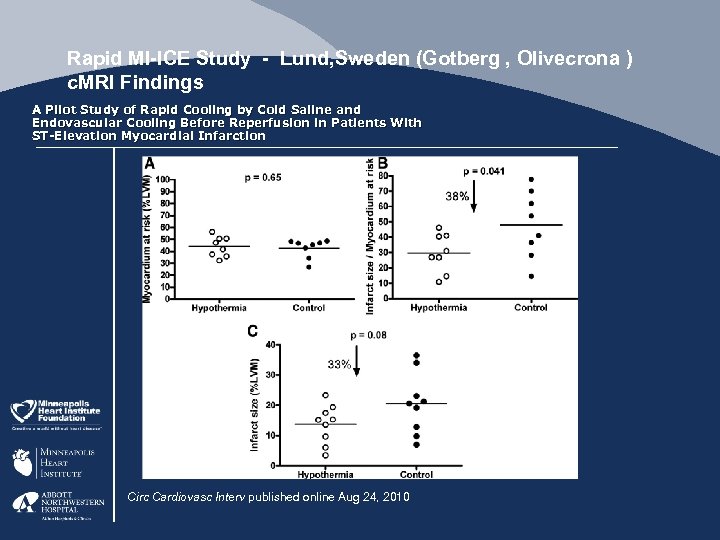 Rapid MI-ICE Study - Lund, Sweden (Gotberg , Olivecrona ) c. MRI Findings A Pilot Study of Rapid Cooling by Cold Saline and Endovascular Cooling Before Reperfusion in Patients With ST-Elevation Myocardial Infarction Circ Cardiovasc Interv published online Aug 24, 2010
Rapid MI-ICE Study - Lund, Sweden (Gotberg , Olivecrona ) c. MRI Findings A Pilot Study of Rapid Cooling by Cold Saline and Endovascular Cooling Before Reperfusion in Patients With ST-Elevation Myocardial Infarction Circ Cardiovasc Interv published online Aug 24, 2010
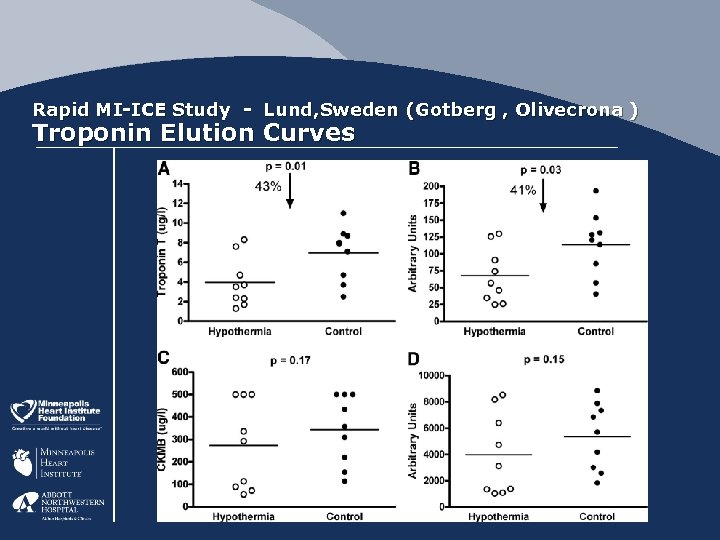 Rapid MI-ICE Study - Lund, Sweden (Gotberg , Olivecrona ) Troponin Elution Curves
Rapid MI-ICE Study - Lund, Sweden (Gotberg , Olivecrona ) Troponin Elution Curves
 Intra-Arrest Transnasal Evaporative Cooling: A Randomized, Prehospital, Multicenter Study (PRINCE: Pre-ROSC Intra. Nasal Cooling Effectiveness) - Study Outline • 200 pts witnessed arrest, intra-arrest cooling vs standard care no prehospital iced saline or cold packs • 18 adverse device events- 13 nasal discoloration, 2 periorbital bleed/emphysema, 3 epistaxis • No difference in ROSC 38% vs 42% control • Time to Target temp 102 vs 282 (P=. 03) • Survival 35 vs 41%% (P=. 26) • Neuro intact 34 vs 21% (P=. 21)
Intra-Arrest Transnasal Evaporative Cooling: A Randomized, Prehospital, Multicenter Study (PRINCE: Pre-ROSC Intra. Nasal Cooling Effectiveness) - Study Outline • 200 pts witnessed arrest, intra-arrest cooling vs standard care no prehospital iced saline or cold packs • 18 adverse device events- 13 nasal discoloration, 2 periorbital bleed/emphysema, 3 epistaxis • No difference in ROSC 38% vs 42% control • Time to Target temp 102 vs 282 (P=. 03) • Survival 35 vs 41%% (P=. 26) • Neuro intact 34 vs 21% (P=. 21)
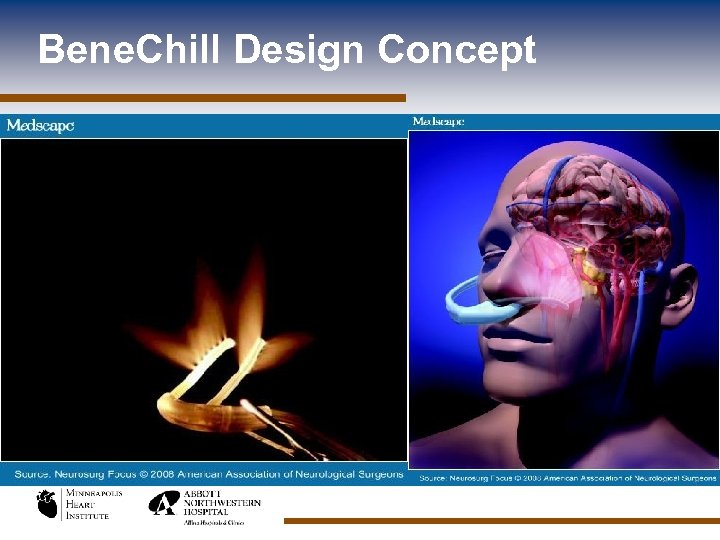 Bene. Chill Design Concept
Bene. Chill Design Concept
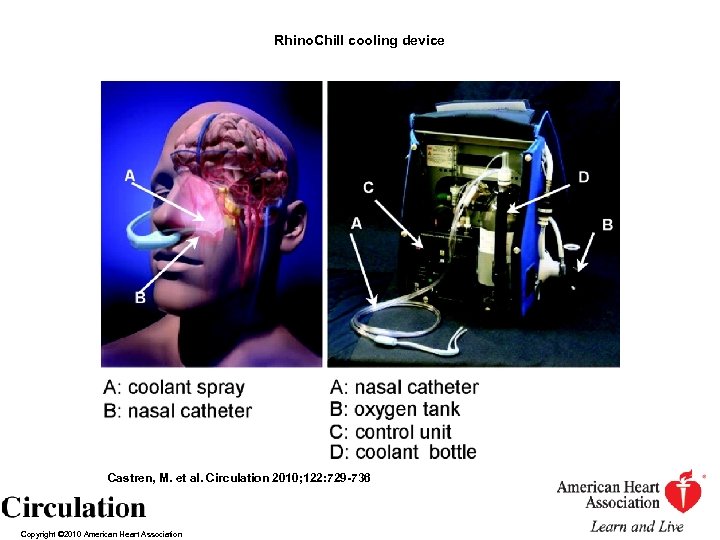 Rhino. Chill cooling device Castren, M. et al. Circulation 2010; 122: 729 -736 Copyright © 2010 American Heart Association
Rhino. Chill cooling device Castren, M. et al. Circulation 2010; 122: 729 -736 Copyright © 2010 American Heart Association
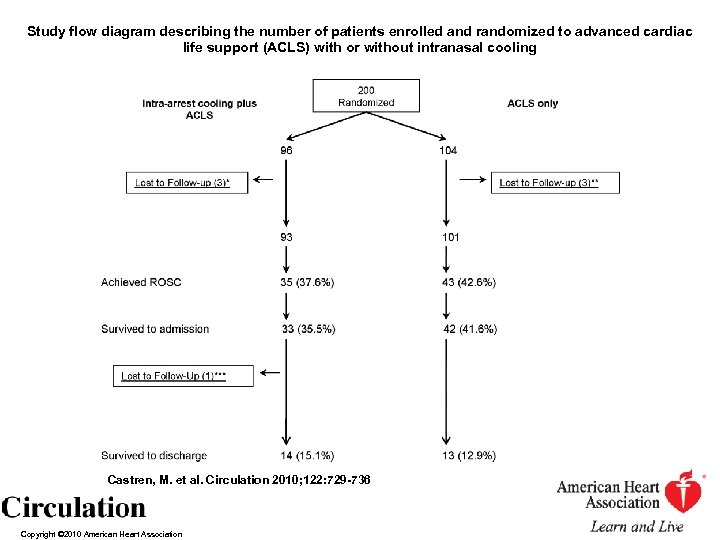 Study flow diagram describing the number of patients enrolled and randomized to advanced cardiac life support (ACLS) with or without intranasal cooling Castren, M. et al. Circulation 2010; 122: 729 -736 Copyright © 2010 American Heart Association
Study flow diagram describing the number of patients enrolled and randomized to advanced cardiac life support (ACLS) with or without intranasal cooling Castren, M. et al. Circulation 2010; 122: 729 -736 Copyright © 2010 American Heart Association
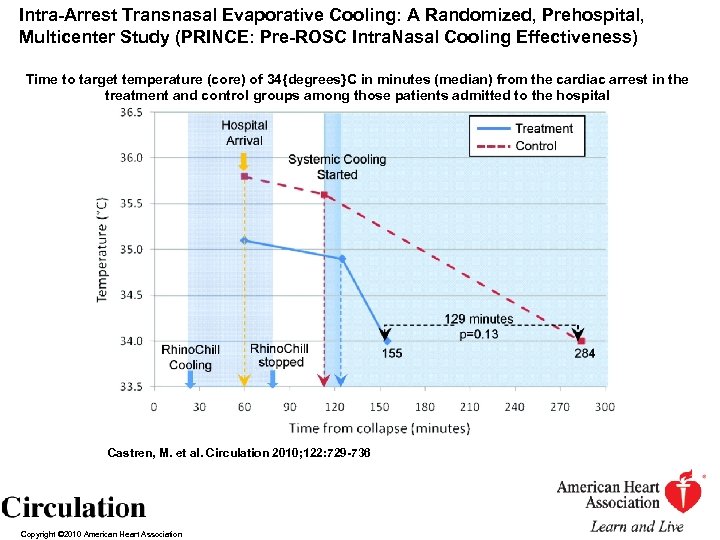 Intra-Arrest Transnasal Evaporative Cooling: A Randomized, Prehospital, Multicenter Study (PRINCE: Pre-ROSC Intra. Nasal Cooling Effectiveness) Time to target temperature (core) of 34{degrees}C in minutes (median) from the cardiac arrest in the treatment and control groups among those patients admitted to the hospital Castren, M. et al. Circulation 2010; 122: 729 -736 Copyright © 2010 American Heart Association
Intra-Arrest Transnasal Evaporative Cooling: A Randomized, Prehospital, Multicenter Study (PRINCE: Pre-ROSC Intra. Nasal Cooling Effectiveness) Time to target temperature (core) of 34{degrees}C in minutes (median) from the cardiac arrest in the treatment and control groups among those patients admitted to the hospital Castren, M. et al. Circulation 2010; 122: 729 -736 Copyright © 2010 American Heart Association
![Rates of neurologically intact survival (defined as having a cerebral performance category [CPC] of Rates of neurologically intact survival (defined as having a cerebral performance category [CPC] of](https://present5.com/presentation/f59174a8285a06b8cf9133b699054538/image-31.jpg) Rates of neurologically intact survival (defined as having a cerebral performance category [CPC] of 1 or 2) in the treatment and control groups among those patients admitted to the hospital for the entire group, those who received rescuer CPR within 10 minutes, and those with a presenting rhythm of VF Castren, M. et al. Circulation 2010; 122: 729 -736 Copyright © 2010 American Heart Association
Rates of neurologically intact survival (defined as having a cerebral performance category [CPC] of 1 or 2) in the treatment and control groups among those patients admitted to the hospital for the entire group, those who received rescuer CPR within 10 minutes, and those with a presenting rhythm of VF Castren, M. et al. Circulation 2010; 122: 729 -736 Copyright © 2010 American Heart Association

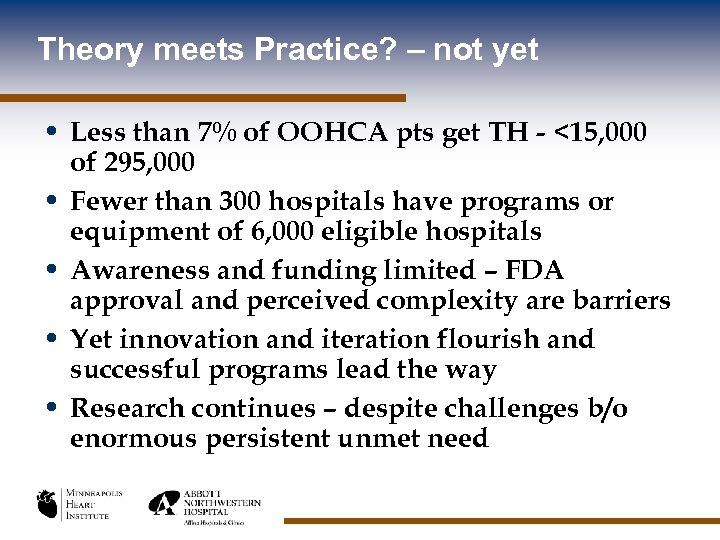 Theory meets Practice? – not yet • Less than 7% of OOHCA pts get TH - <15, 000 of 295, 000 • Fewer than 300 hospitals have programs or equipment of 6, 000 eligible hospitals • Awareness and funding limited – FDA approval and perceived complexity are barriers • Yet innovation and iteration flourish and successful programs lead the way • Research continues – despite challenges b/o enormous persistent unmet need
Theory meets Practice? – not yet • Less than 7% of OOHCA pts get TH - <15, 000 of 295, 000 • Fewer than 300 hospitals have programs or equipment of 6, 000 eligible hospitals • Awareness and funding limited – FDA approval and perceived complexity are barriers • Yet innovation and iteration flourish and successful programs lead the way • Research continues – despite challenges b/o enormous persistent unmet need
 Cardiovascular Emergency Centers To maximize benefits, cooling should be initiated as soon as possible. Survival benefits are dramatic. But, we under-deliver this lifesaving treatment Systems of Care Do Make a Difference TH capable Acute MI PCI centers should offer this lifesaving treatment, it is a public health care imperative. To achieve equivalent access and outcomes in rural and metro patients by providing one Standard of Care for an entire Region for the most complex cardiac emergencies including acute STEMI and cardiac arrest
Cardiovascular Emergency Centers To maximize benefits, cooling should be initiated as soon as possible. Survival benefits are dramatic. But, we under-deliver this lifesaving treatment Systems of Care Do Make a Difference TH capable Acute MI PCI centers should offer this lifesaving treatment, it is a public health care imperative. To achieve equivalent access and outcomes in rural and metro patients by providing one Standard of Care for an entire Region for the most complex cardiac emergencies including acute STEMI and cardiac arrest


