8035a11ba8862bc0e370d70e8876bbd6.ppt
- Количество слайдов: 44

CRRT Protocol Continuous Renal Replacement Therapy 台大外科部 護理師 蔡壁如
Outline n History n Indication n CRRT Method n Ultrafiltration rates n Choice of replacement fluid n Set-up protocol
History n n n n 1861 Thomas Graham, etc. use a semi-permeable membrane to diffuse urea 1924 George Haas dialyse a patient during 15 minutes 1927 Heparin, an anticoagulant, is available 1937 Production of cellophane for filters 1943 Willem Kolff makes a rotating drum dialyser 1970 First artificial membrane 1975 -1985 Development of new techniques, i. e. adsorption, plasma exchange, filtration …
Extracorporeal depuration in ICU n n n 1977 : Peter Kramer performs first arterio-venous hemofiltration (CAVH) 1982 : FDA approves the CAVH 1984 : Blood pump circulated remove fluid 1994 : Clinical importance to control fluid balance 1994 The first « automatic » machine is available 2000 : higher flows machines becomes available

CAVH
Extracorporeal depuration in ICU n n n 1977 : Peter Kramer performs first arterio-venous hemofiltration (CAVH) 1982 : FDA approves the CAVH 1984 : Blood pump circulated remove fluid 1994 : Clinical importance to control fluid balance 1994 The first « automatic » machine is available 2000 : higher flows machines becomes available

CVVH
Extracorporeal depuration in ICU n n n 1977 : Peter Kramer performs first arterio-venous hemofiltration (CAVH) 1982 : FDA approves the CAVH 1984 : Blood pump circulated remove fluid 1994 : Clinical importance to control fluid balance 1994 The first « automatic » machine is available 2000 : higher flows machines becomes available

CRRT
Extracorporeal depuration in ICU n n n 1977 : Peter Kramer performs first arterio-venous hemofiltration (CAVH) 1982 : FDA approves the CAVH 1984 : Blood pump circulated remove fluid 1994 : Clinical importance to control fluid balance 1994 The first « automatic » machine is available 2000 : higher flows machines becomes available

Automatic CRRT
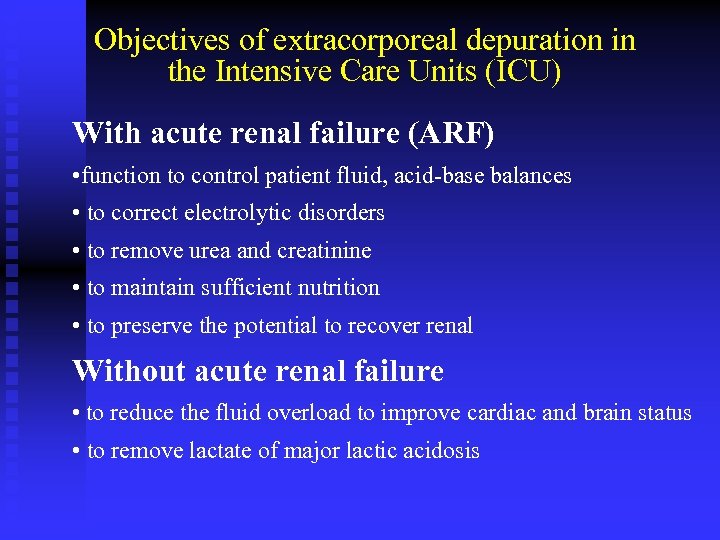
Objectives of extracorporeal depuration in the Intensive Care Units (ICU) With acute renal failure (ARF) • function to control patient fluid, acid-base balances • to correct electrolytic disorders • to remove urea and creatinine • to maintain sufficient nutrition • to preserve the potential to recover renal Without acute renal failure • to reduce the fluid overload to improve cardiac and brain status • to remove lactate of major lactic acidosis
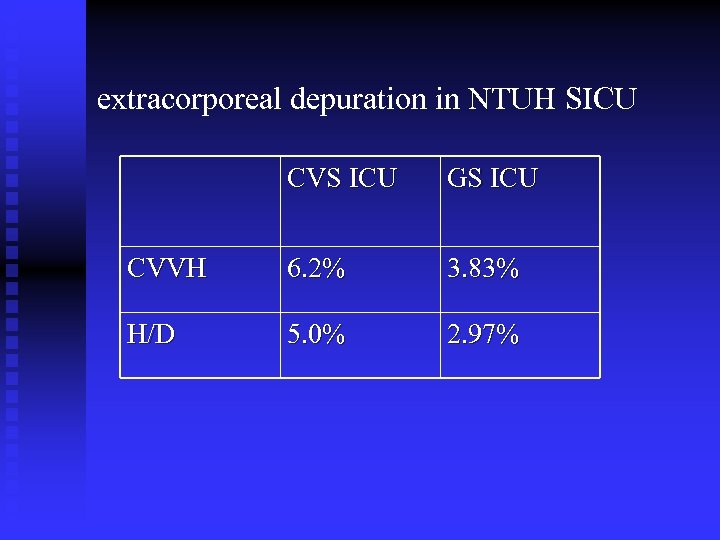
extracorporeal depuration in NTUH SICU CVS ICU GS ICU CVVH 6. 2% 3. 83% H/D 5. 0% 2. 97%
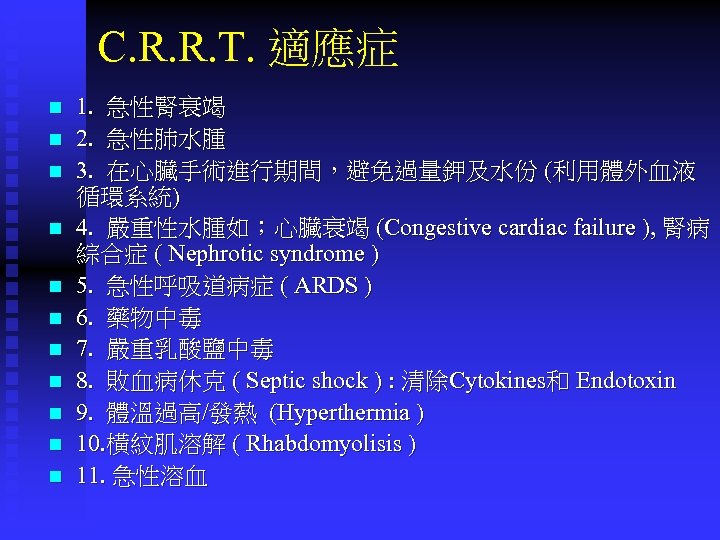
C. R. R. T. 適應症 n n n 1. 急性腎衰竭 2. 急性肺水腫 3. 在心臟手術進行期間,避免過量鉀及水份 (利用體外血液 循環系統) 4. 嚴重性水腫如;心臟衰竭 (Congestive cardiac failure ), 腎病 綜合症 ( Nephrotic syndrome ) 5. 急性呼吸道病症 ( ARDS ) 6. 藥物中毒 7. 嚴重乳酸鹽中毒 8. 敗血病休克 ( Septic shock ) : 清除Cytokines和 Endotoxin 9. 體溫過高/發熱 (Hyperthermia ) 10. 橫紋肌溶解 ( Rhabdomyolisis ) 11. 急性溶血
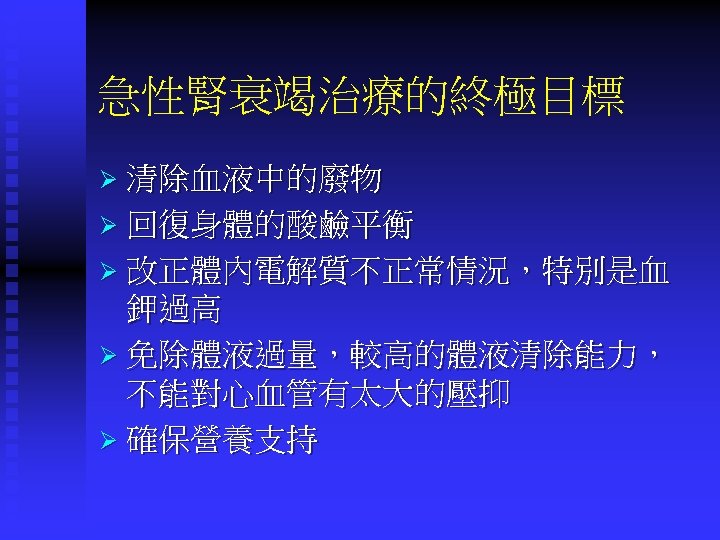
急性腎衰竭治療的終極目標 Ø 清除血液中的廢物 Ø 回復身體的酸鹼平衡 Ø 改正體內電解質不正常情況,特別是血 鉀過高 Ø 免除體液過量,較高的體液清除能力, 不能對心血管有太大的壓抑 Ø 確保營養支持
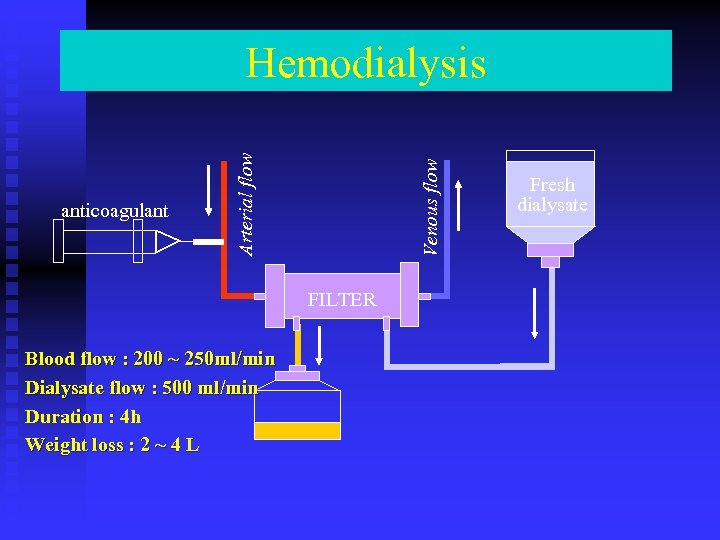
Venous flow anticoagulant Arterial flow Hemodialysis FILTER Blood flow : 200 ~ 250 ml/min Dialysate flow : 500 ml/min Duration : 4 h Weight loss : 2 ~ 4 L Fresh dialysate
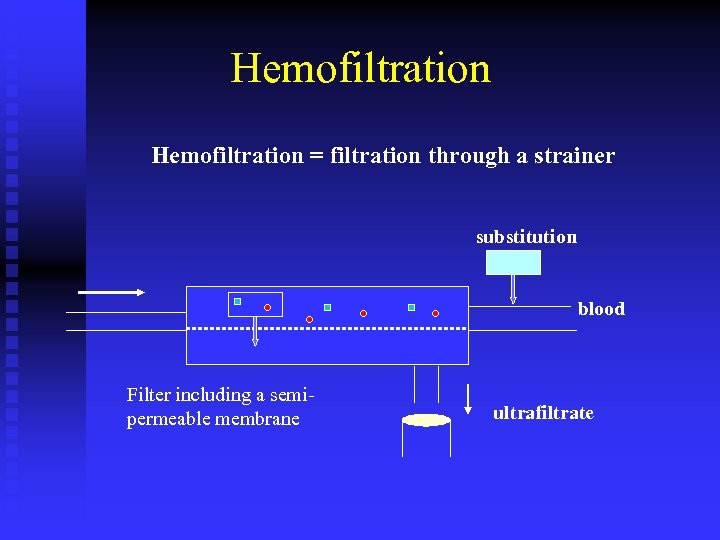
Hemofiltration = filtration through a strainer substitution blood Filter including a semipermeable membrane ultrafiltrate
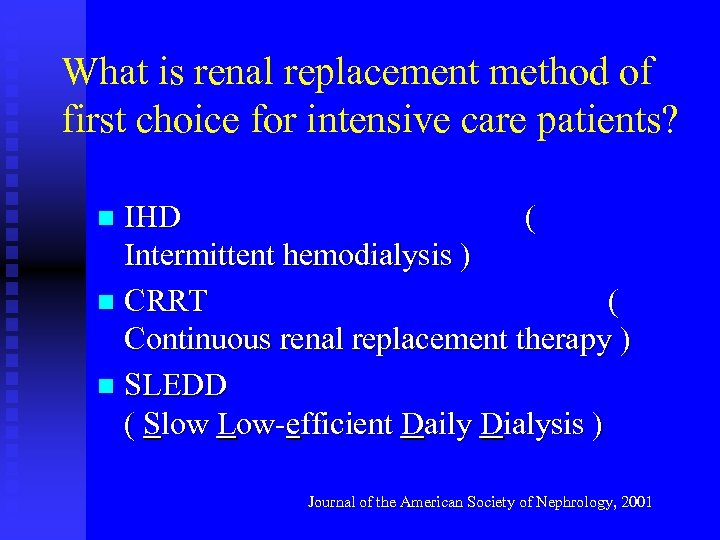
What is renal replacement method of first choice for intensive care patients? IHD ( Intermittent hemodialysis ) n CRRT ( Continuous renal replacement therapy ) n SLEDD ( Slow Low-efficient Daily Dialysis ) n Journal of the American Society of Nephrology, 2001

Intermittent H/D
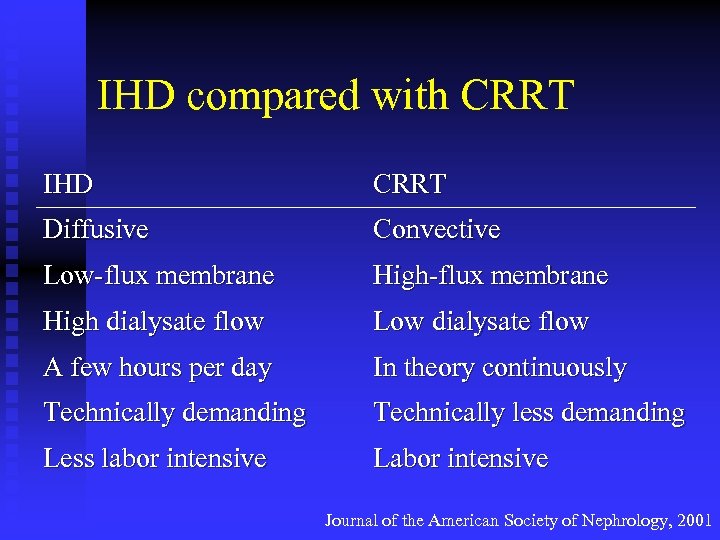
IHD compared with CRRT IHD CRRT Diffusive Convective Low-flux membrane High dialysate flow Low dialysate flow A few hours per day In theory continuously Technically demanding Technically less demanding Less labor intensive Labor intensive Journal of the American Society of Nephrology, 2001
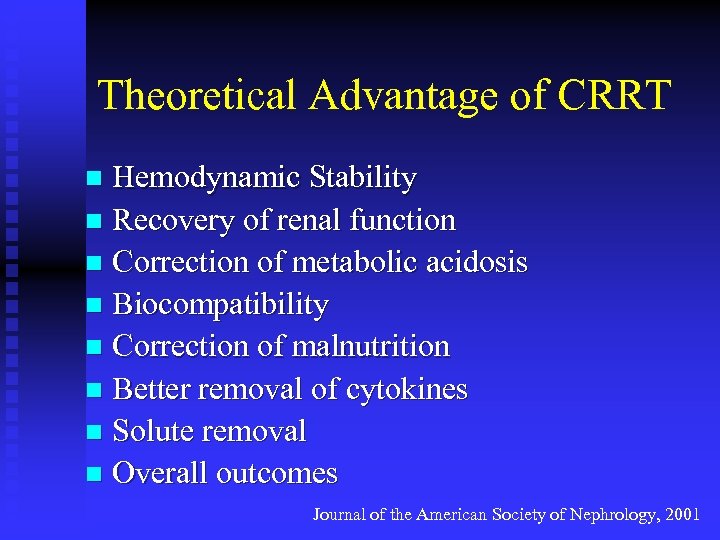
Theoretical Advantage of CRRT Hemodynamic Stability n Recovery of renal function n Correction of metabolic acidosis n Biocompatibility n Correction of malnutrition n Better removal of cytokines n Solute removal n Overall outcomes n Journal of the American Society of Nephrology, 2001
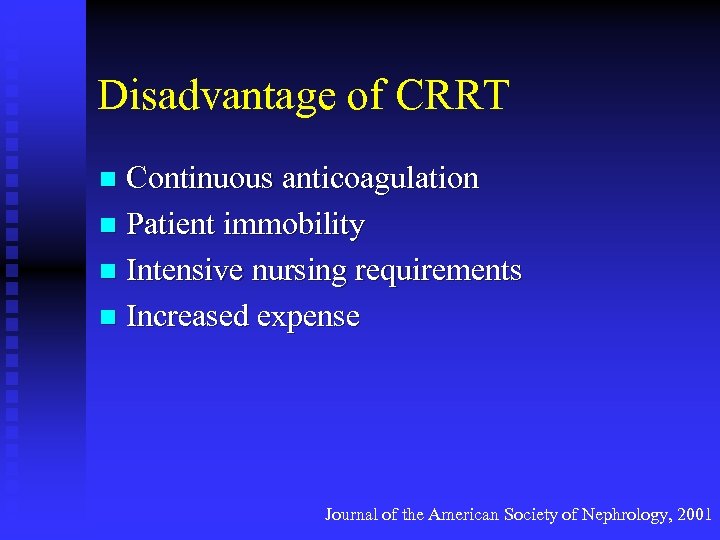
Disadvantage of CRRT Continuous anticoagulation n Patient immobility n Intensive nursing requirements n Increased expense n Journal of the American Society of Nephrology, 2001
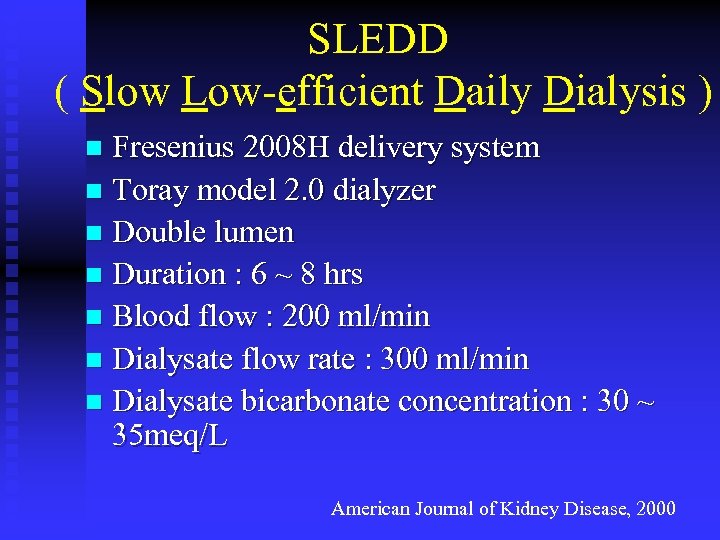
SLEDD ( Slow Low-efficient Daily Dialysis ) Fresenius 2008 H delivery system n Toray model 2. 0 dialyzer n Double lumen n Duration : 6 ~ 8 hrs n Blood flow : 200 ml/min n Dialysate flow rate : 300 ml/min n Dialysate bicarbonate concentration : 30 ~ 35 meq/L n American Journal of Kidney Disease, 2000
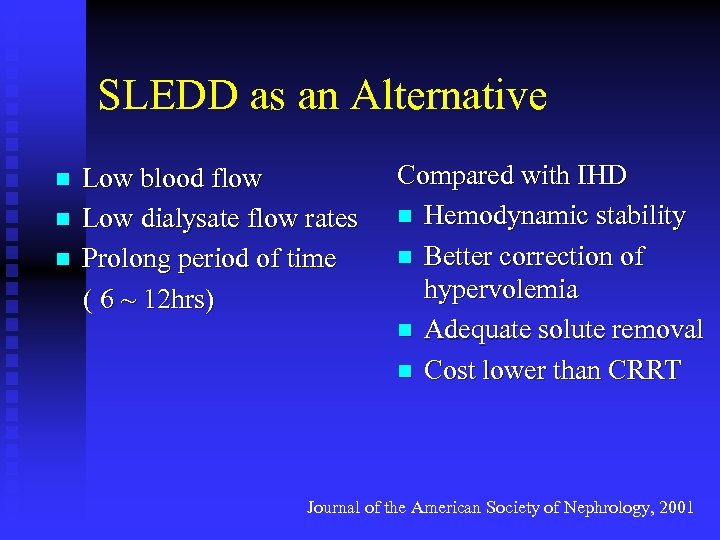
SLEDD as an Alternative Low blood flow n Low dialysate flow rates n Prolong period of time ( 6 ~ 12 hrs) n Compared with IHD n Hemodynamic stability n Better correction of hypervolemia n Adequate solute removal n Cost lower than CRRT Journal of the American Society of Nephrology, 2001
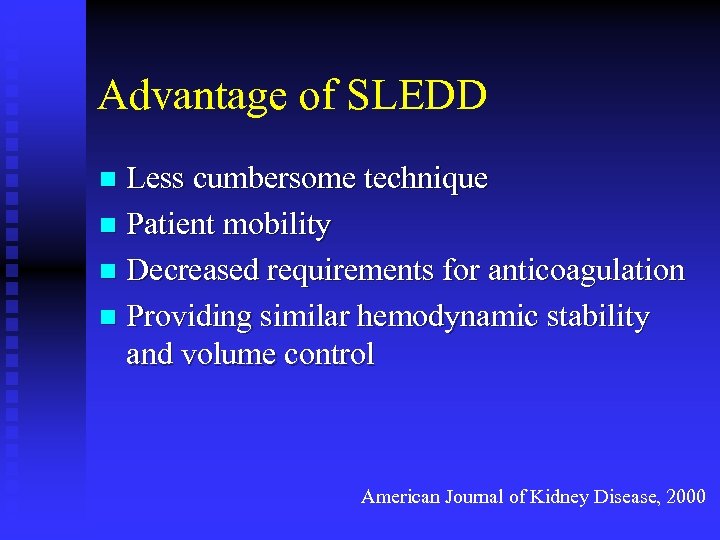
Advantage of SLEDD Less cumbersome technique n Patient mobility n Decreased requirements for anticoagulation n Providing similar hemodynamic stability and volume control n American Journal of Kidney Disease, 2000
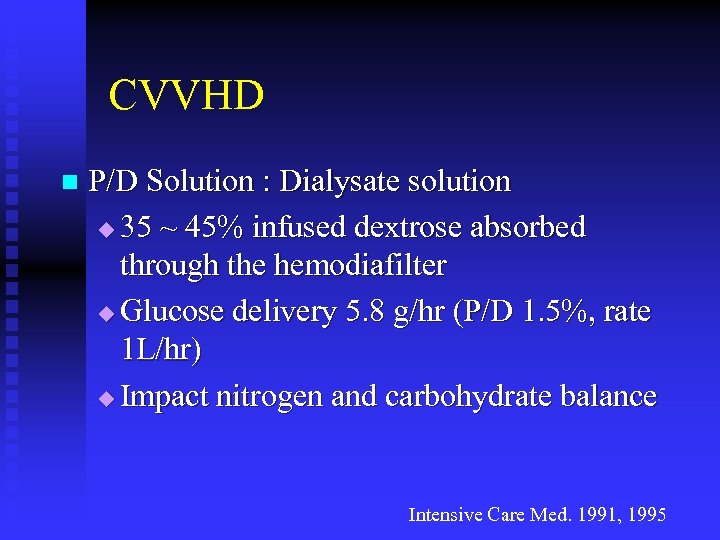
CVVHD n P/D Solution : Dialysate solution u 35 ~ 45% infused dextrose absorbed through the hemodiafilter u Glucose delivery 5. 8 g/hr (P/D 1. 5%, rate 1 L/hr) u Impact nitrogen and carbohydrate balance Intensive Care Med. 1991, 1995
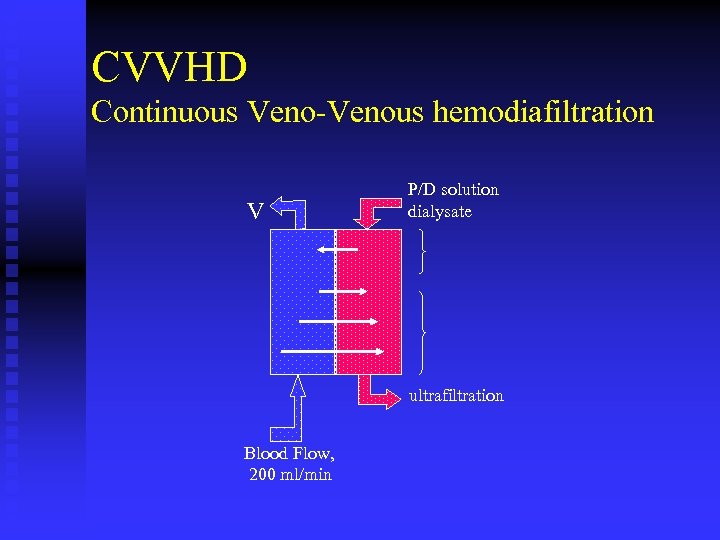
CVVHD Continuous Veno-Venous hemodiafiltration V P/D solution dialysate ultrafiltration Blood Flow, 200 ml/min
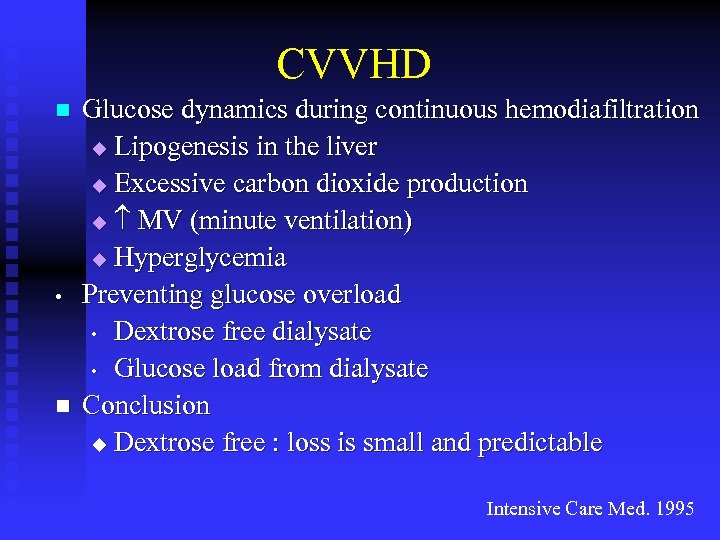
CVVHD n • n Glucose dynamics during continuous hemodiafiltration u Lipogenesis in the liver u Excessive carbon dioxide production u MV (minute ventilation) u Hyperglycemia Preventing glucose overload • Dextrose free dialysate • Glucose load from dialysate Conclusion u Dextrose free : loss is small and predictable Intensive Care Med. 1995
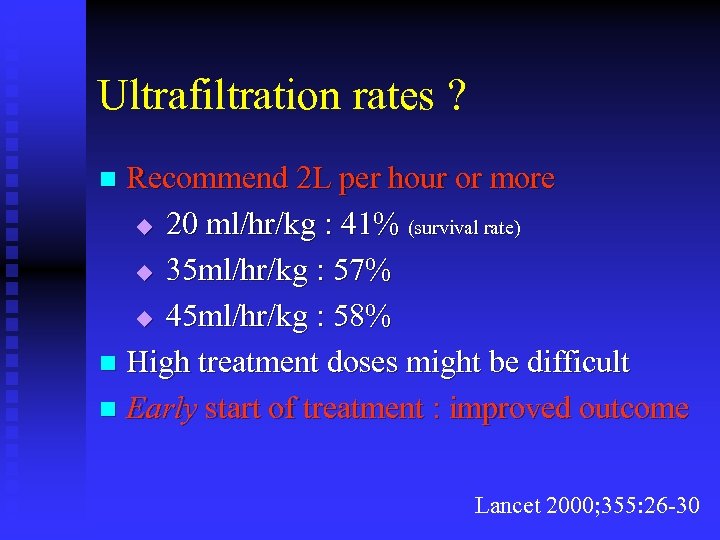
Ultrafiltration rates ? Recommend 2 L per hour or more u 20 ml/hr/kg : 41% (survival rate) u 35 ml/hr/kg : 57% u 45 ml/hr/kg : 58% n High treatment doses might be difficult n Early start of treatment : improved outcome n Lancet 2000; 355: 26 -30
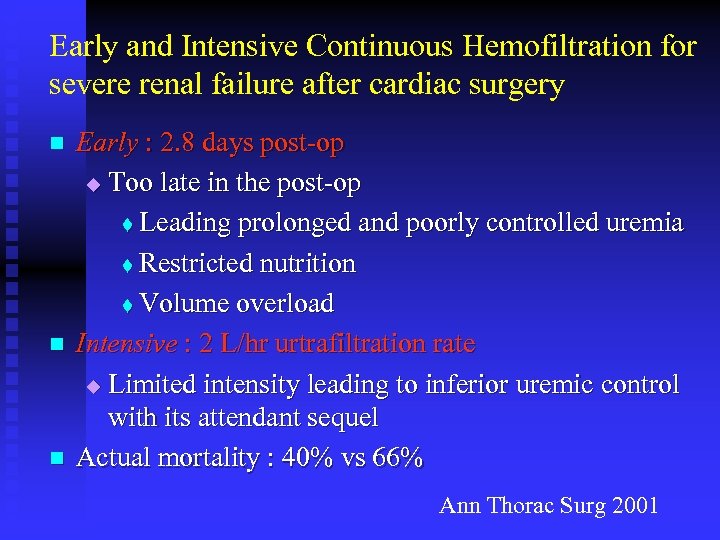
Early and Intensive Continuous Hemofiltration for severe renal failure after cardiac surgery n n n Early : 2. 8 days post-op u Too late in the post-op t Leading prolonged and poorly controlled uremia t Restricted nutrition t Volume overload Intensive : 2 L/hr urtrafiltration rate u Limited intensity leading to inferior uremic control with its attendant sequel Actual mortality : 40% vs 66% Ann Thorac Surg 2001
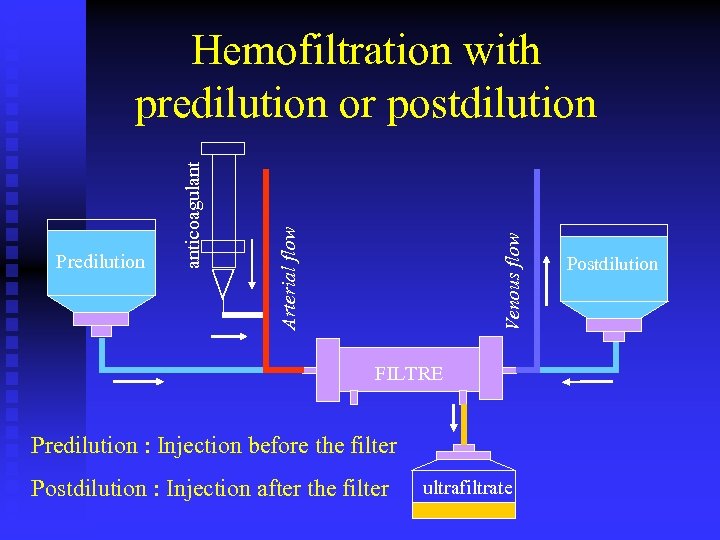
Venous flow Arterial flow Predilution anticoagulant Hemofiltration with predilution or postdilution FILTRE Predilution : Injection before the filter Postdilution : Injection after the filter ultrafiltrate Postdilution
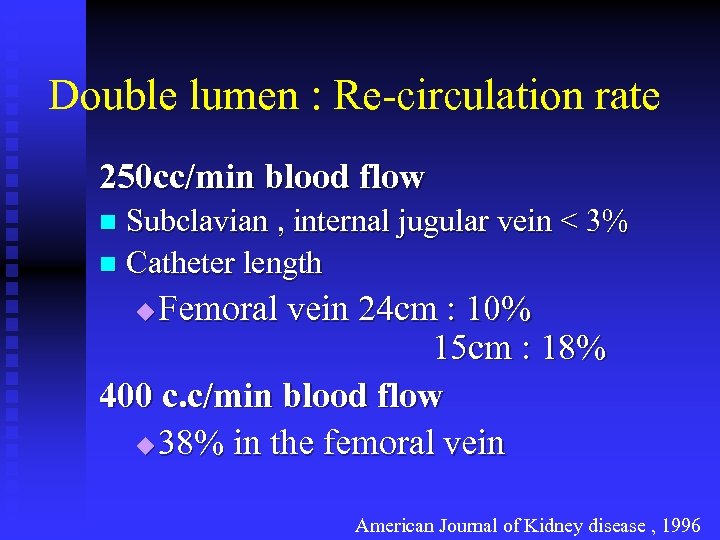
Double lumen : Re-circulation rate 250 cc/min blood flow Subclavian , internal jugular vein < 3% n Catheter length n Femoral vein 24 cm : 10% 15 cm : 18% 400 c. c/min blood flow u 38% in the femoral vein u American Journal of Kidney disease , 1996
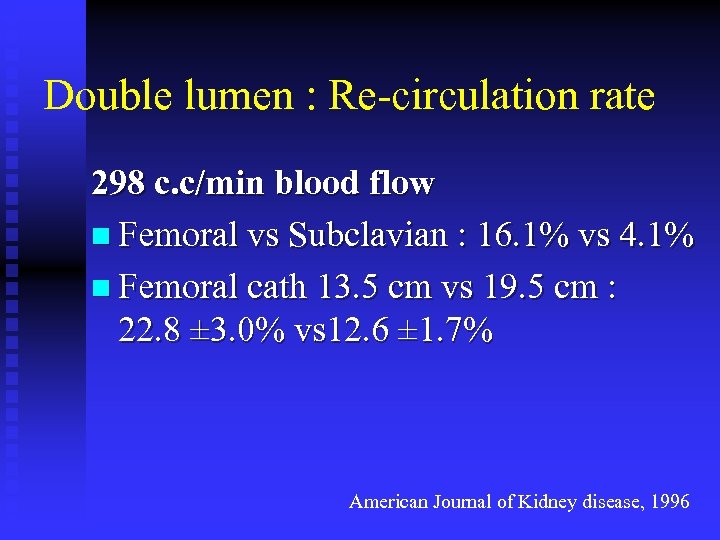
Double lumen : Re-circulation rate 298 c. c/min blood flow n Femoral vs Subclavian : 16. 1% vs 4. 1% n Femoral cath 13. 5 cm vs 19. 5 cm : 22. 8 ± 3. 0% vs 12. 6 ± 1. 7% American Journal of Kidney disease, 1996
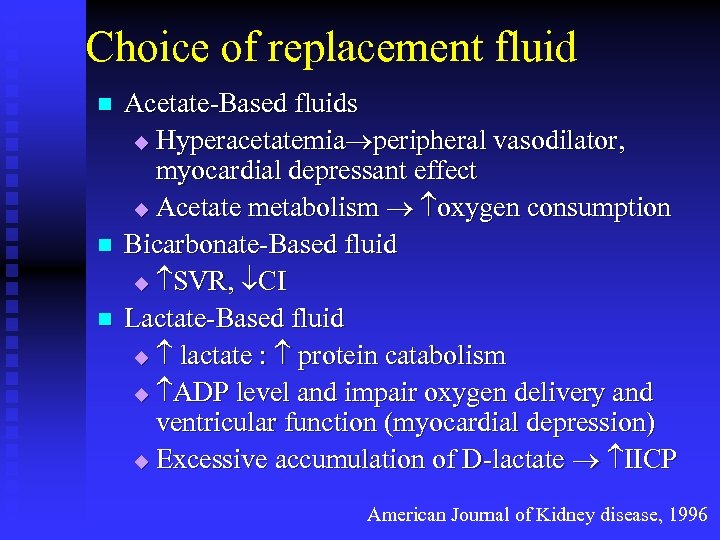
Choice of replacement fluid n n n Acetate-Based fluids u Hyperacetatemia peripheral vasodilator, myocardial depressant effect u Acetate metabolism oxygen consumption Bicarbonate-Based fluid u SVR, CI Lactate-Based fluid u lactate : protein catabolism u ADP level and impair oxygen delivery and ventricular function (myocardial depression) u Excessive accumulation of D-lactate IICP American Journal of Kidney disease, 1996
Effects of bicarbonate and lactate-buffered replacement fluids on cardiovascular outcome in CRRT patients Bicarbonate Replacement Fluid : recommended in patients with lactic acidemia and severe liver failure n Improve cardiovascular outcome in critically ill patients with acute renal failure n n International Society of Nephrology 2000
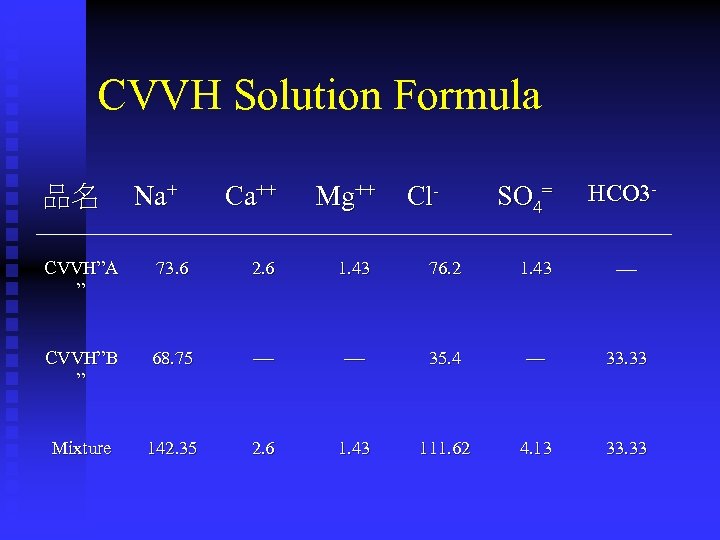
CVVH Solution Formula 品名 Na+ Ca++ Mg++ Cl- SO 4= HCO 3 - CVVH”A ” 73. 6 2. 6 1. 43 76. 2 1. 43 CVVH”B ” 68. 75 35. 4 — 33. 33 Mixture 142. 35 2. 6 1. 43 111. 62 4. 13 33. 33
Replacement Fluid : A, B Solution
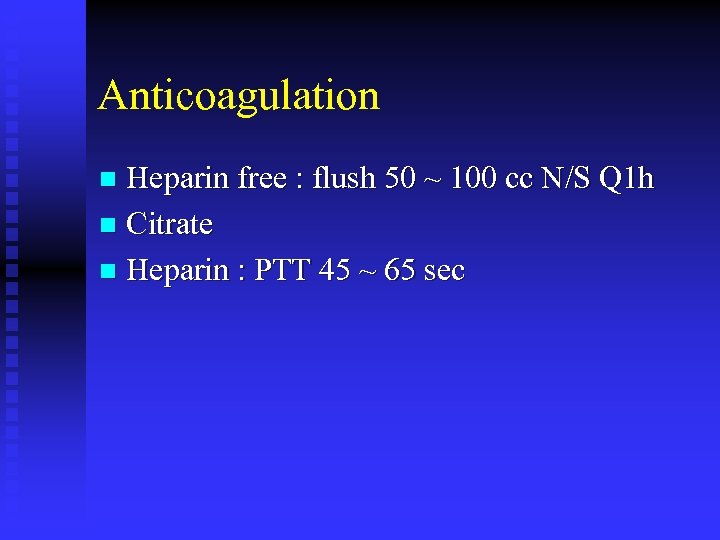
Anticoagulation Heparin free : flush 50 ~ 100 cc N/S Q 1 h n Citrate n Heparin : PTT 45 ~ 65 sec n
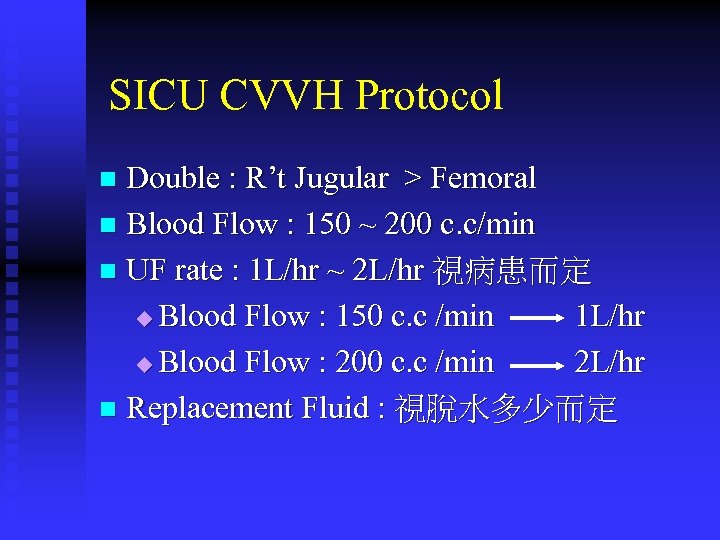
SICU CVVH Protocol Double : R’t Jugular > Femoral n Blood Flow : 150 ~ 200 c. c/min n UF rate : 1 L/hr ~ 2 L/hr 視病患而定 u Blood Flow : 150 c. c /min 1 L/hr u Blood Flow : 200 c. c /min 2 L/hr n Replacement Fluid : 視脫水多少而定 n

主機 加熱袋 Blood flow Power Roller pump
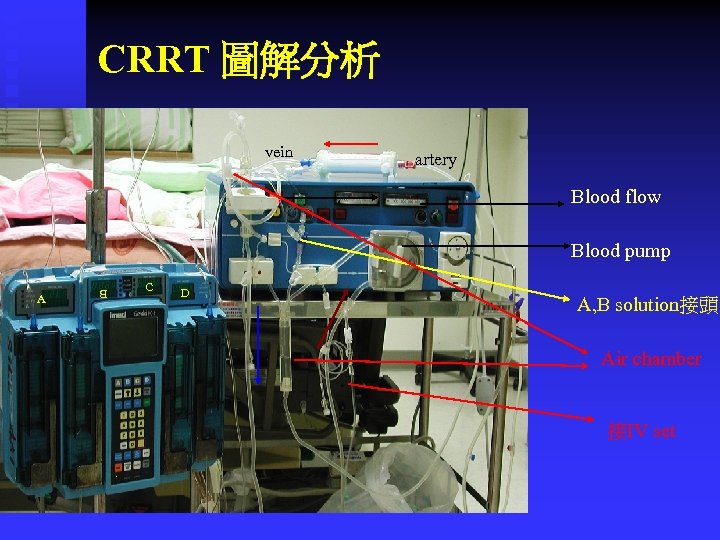
CRRT 圖解分析 vein artery Blood flow Blood pump A B C D A, B solution接頭 Air chamber 接IV set
CRRT

Automatic CRRT
8035a11ba8862bc0e370d70e8876bbd6.ppt