dac98c1cea1ab0340fefebe1554413e1.ppt
- Количество слайдов: 55
 CRRT in Acute Liver Failure Akash Deep Director - PICU King’s College Hospital London Chair Renal/CRRT Section European Society of Pediatric and Neonatal Intensive Care (ESPNIC) 0
CRRT in Acute Liver Failure Akash Deep Director - PICU King’s College Hospital London Chair Renal/CRRT Section European Society of Pediatric and Neonatal Intensive Care (ESPNIC) 0
 DISCLOSURE • Research grant from Mallinckrodt Pharmaceuticals – Terlipressin in paediatric HRS • Taskforce member for ESPNIC/SCCM joint septic shock guidelines – Adjunctive therapies in septic shock 1
DISCLOSURE • Research grant from Mallinckrodt Pharmaceuticals – Terlipressin in paediatric HRS • Taskforce member for ESPNIC/SCCM joint septic shock guidelines – Adjunctive therapies in septic shock 1
 Overview • Hyperammonaemia – raised ICP in ALF • Controversies in CRRT in ALF – why, when, how ? • Role of MARS, SPAD and TPE in Liver failure • Anticoagulation in liver Patients 2
Overview • Hyperammonaemia – raised ICP in ALF • Controversies in CRRT in ALF – why, when, how ? • Role of MARS, SPAD and TPE in Liver failure • Anticoagulation in liver Patients 2
 Why patients with FHF die ? • Sepsis – MOSF • Cerebral edema /intracranial hypertension • SIRS at presentation associated with mortality - immune modulation
Why patients with FHF die ? • Sepsis – MOSF • Cerebral edema /intracranial hypertension • SIRS at presentation associated with mortality - immune modulation
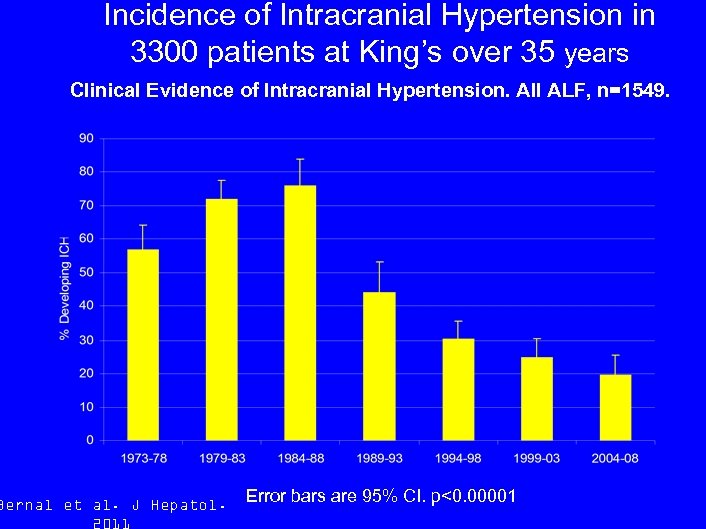 Incidence of Intracranial Hypertension in 3300 patients at King’s over 35 years Clinical Evidence of Intracranial Hypertension. All ALF, n=1549. Bernal et al. J Hepatol. Error bars are 95% CI. p<0. 00001
Incidence of Intracranial Hypertension in 3300 patients at King’s over 35 years Clinical Evidence of Intracranial Hypertension. All ALF, n=1549. Bernal et al. J Hepatol. Error bars are 95% CI. p<0. 00001
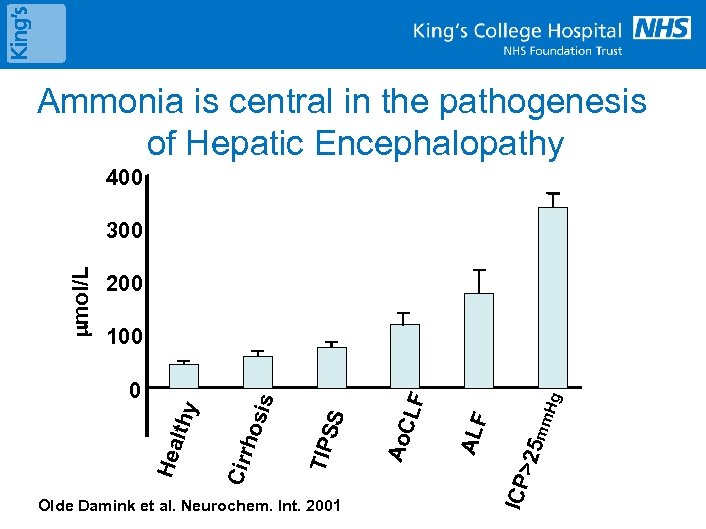 Ammonia is central in the pathogenesis of Hepatic Encephalopathy 400 200 Hg mm LF ALF >25 ICP Olde Damink et al. Neurochem. Int. 2001 Ao. C SS TIP Hea lthy 0 hos is 100 Cirr mol/L 300
Ammonia is central in the pathogenesis of Hepatic Encephalopathy 400 200 Hg mm LF ALF >25 ICP Olde Damink et al. Neurochem. Int. 2001 Ao. C SS TIP Hea lthy 0 hos is 100 Cirr mol/L 300
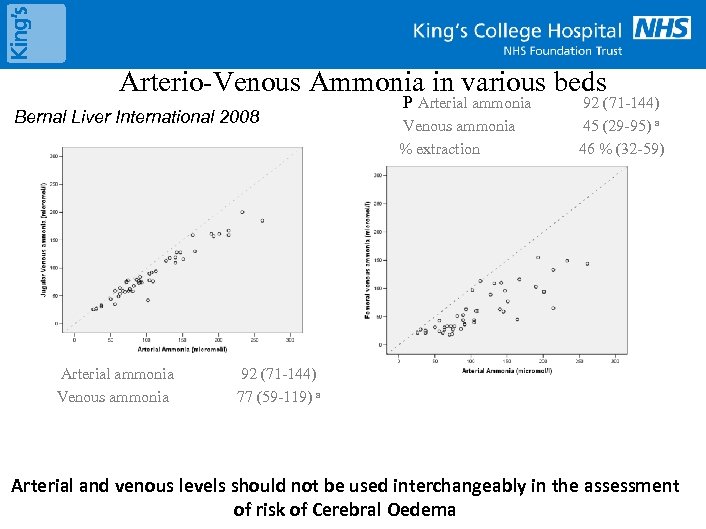 Arterio-Venous Ammonia in various beds Bernal Liver International 2008 Arterial ammonia Venous ammonia P Arterial ammonia Venous ammonia % extraction 92 (71 -144) 45 (29 -95) a 46 % (32 -59) 92 (71 -144) 77 (59 -119) a Arterial and venous levels should not be used interchangeably in the assessment of risk of Cerebral Oedema
Arterio-Venous Ammonia in various beds Bernal Liver International 2008 Arterial ammonia Venous ammonia P Arterial ammonia Venous ammonia % extraction 92 (71 -144) 45 (29 -95) a 46 % (32 -59) 92 (71 -144) 77 (59 -119) a Arterial and venous levels should not be used interchangeably in the assessment of risk of Cerebral Oedema
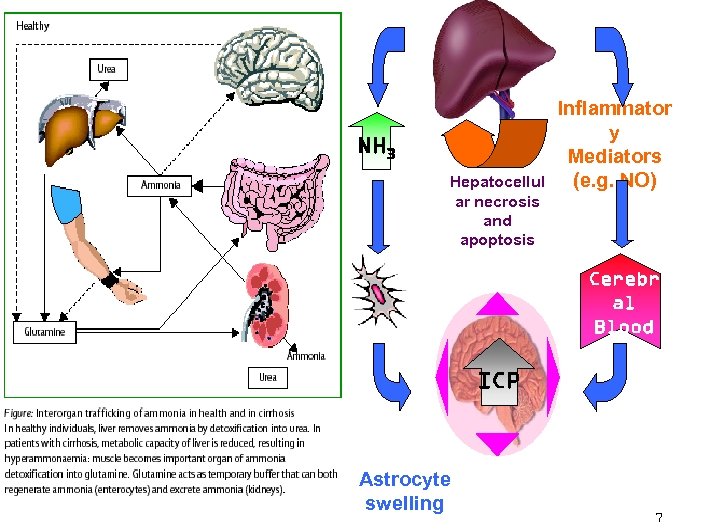 NH 3 Hepatocellul ar necrosis and apoptosis Inflammator y Mediators (e. g. NO) Cerebr al Blood Flow ICP Astrocyte swelling 7
NH 3 Hepatocellul ar necrosis and apoptosis Inflammator y Mediators (e. g. NO) Cerebr al Blood Flow ICP Astrocyte swelling 7
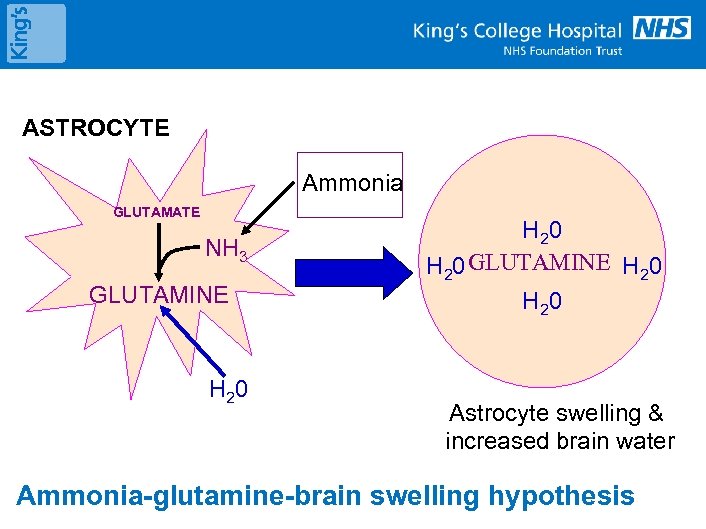 ASTROCYTE Ammonia GLUTAMATE NH 3 GLUTAMINE H 20 GLUTAMINE H 20 Astrocyte swelling & increased brain water Ammonia-glutamine-brain swelling hypothesis
ASTROCYTE Ammonia GLUTAMATE NH 3 GLUTAMINE H 20 GLUTAMINE H 20 Astrocyte swelling & increased brain water Ammonia-glutamine-brain swelling hypothesis
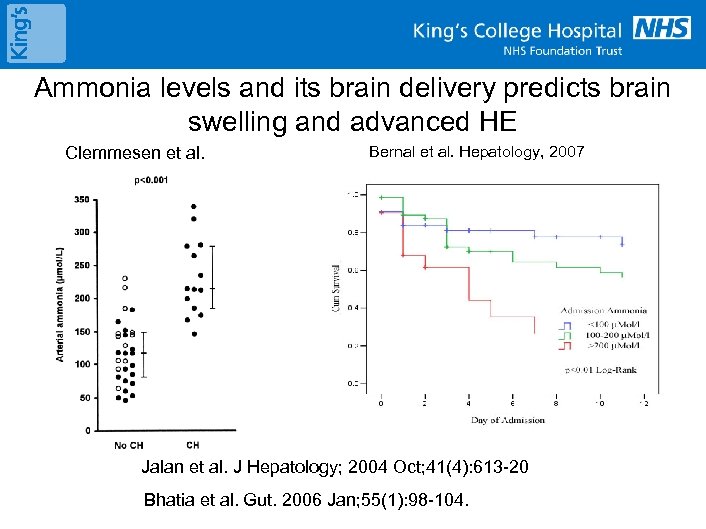 Ammonia levels and its brain delivery predicts brain swelling and advanced HE Clemmesen et al. Bernal et al. Hepatology, 2007 Jalan et al. J Hepatology; 2004 Oct; 41(4): 613 -20 Bhatia et al. Gut. 2006 Jan; 55(1): 98 -104.
Ammonia levels and its brain delivery predicts brain swelling and advanced HE Clemmesen et al. Bernal et al. Hepatology, 2007 Jalan et al. J Hepatology; 2004 Oct; 41(4): 613 -20 Bhatia et al. Gut. 2006 Jan; 55(1): 98 -104.
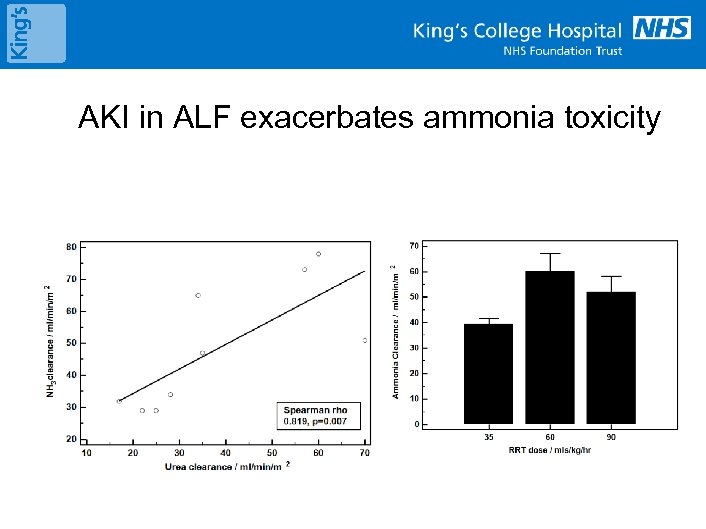 AKI in ALF exacerbates ammonia toxicity
AKI in ALF exacerbates ammonia toxicity
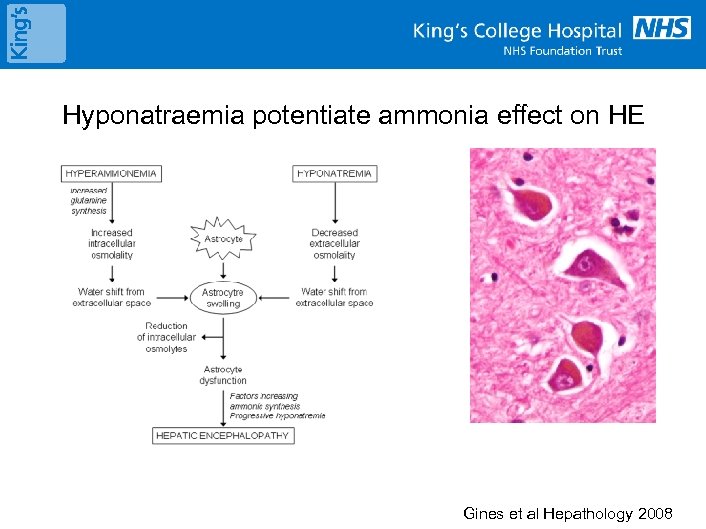 Hyponatraemia potentiate ammonia effect on HE Gines et al Hepathology 2008
Hyponatraemia potentiate ammonia effect on HE Gines et al Hepathology 2008
 Controversies in RRT in Liver Failure • Why do patients with Liver failure develop AKI and why do they need to go on CRRT? • What is the best time to initiate RRT in patients with ALF? - Elective versus standard CRRT • What dose of RRT is the best dose? • Anticoagulation in CRRT for ALF • Ideal Extracorporeal Liver Assist Device (ELAD) – excretory and synthetic function 12
Controversies in RRT in Liver Failure • Why do patients with Liver failure develop AKI and why do they need to go on CRRT? • What is the best time to initiate RRT in patients with ALF? - Elective versus standard CRRT • What dose of RRT is the best dose? • Anticoagulation in CRRT for ALF • Ideal Extracorporeal Liver Assist Device (ELAD) – excretory and synthetic function 12
 Survival in patients treated by RRT according to diagnoses: pp. CRRT Registry Symons, Clin J Am Soc Nephrol, 2: 732, 2007 p. CCRT Rome 2010 13
Survival in patients treated by RRT according to diagnoses: pp. CRRT Registry Symons, Clin J Am Soc Nephrol, 2: 732, 2007 p. CCRT Rome 2010 13
 CRRT in ALF 14
CRRT in ALF 14
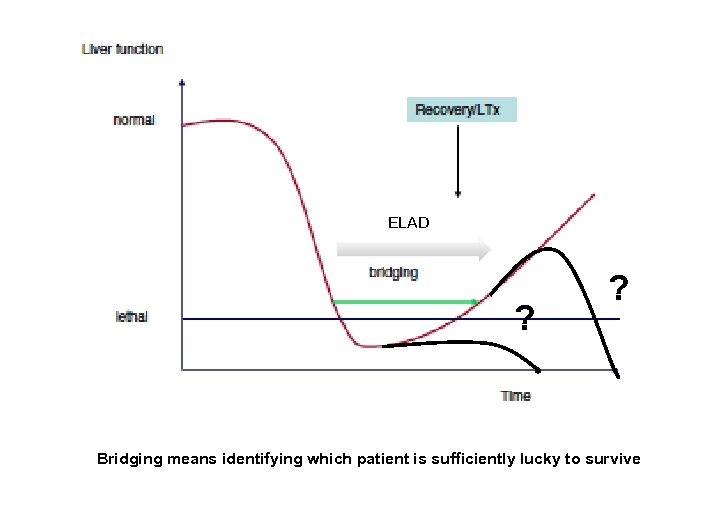 ELAD ? ? Bridging means identifying which patient is sufficiently lucky to survive
ELAD ? ? Bridging means identifying which patient is sufficiently lucky to survive
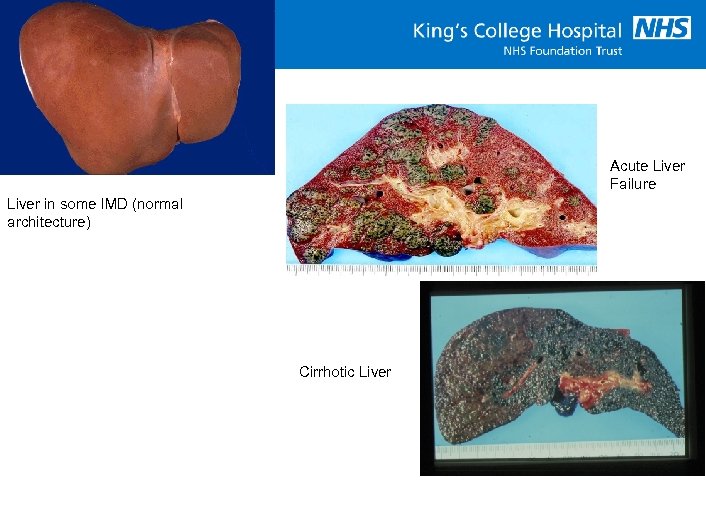 Acute Liver Failure Liver in some IMD (normal architecture) Cirrhotic Liver
Acute Liver Failure Liver in some IMD (normal architecture) Cirrhotic Liver
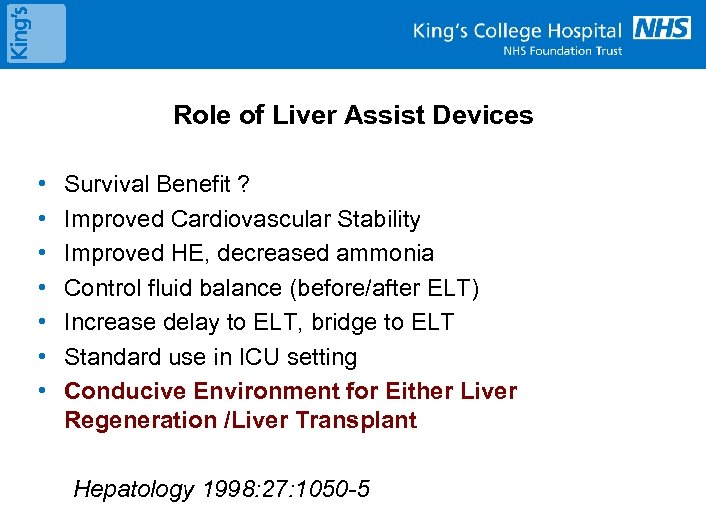 Role of Liver Assist Devices • • Survival Benefit ? Improved Cardiovascular Stability Improved HE, decreased ammonia Control fluid balance (before/after ELT) Increase delay to ELT, bridge to ELT Standard use in ICU setting Conducive Environment for Either Liver Regeneration /Liver Transplant Hepatology 1998: 27: 1050 -5
Role of Liver Assist Devices • • Survival Benefit ? Improved Cardiovascular Stability Improved HE, decreased ammonia Control fluid balance (before/after ELT) Increase delay to ELT, bridge to ELT Standard use in ICU setting Conducive Environment for Either Liver Regeneration /Liver Transplant Hepatology 1998: 27: 1050 -5
 When to initiate ? 18
When to initiate ? 18
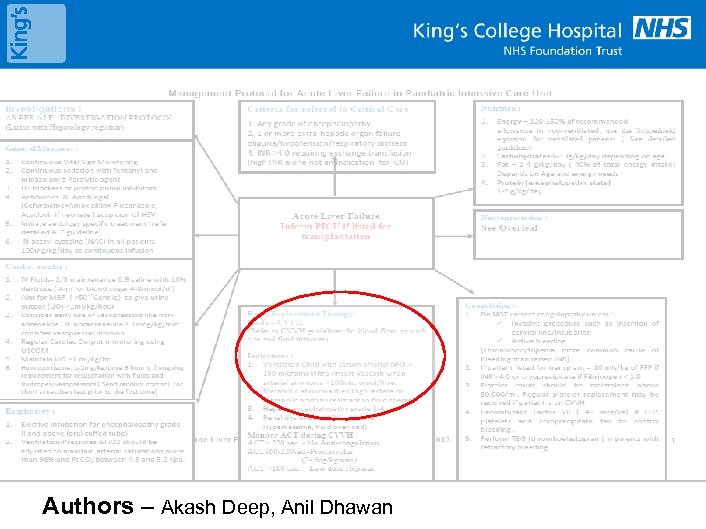 Authors – Akash Deep, Anil Dhawan
Authors – Akash Deep, Anil Dhawan
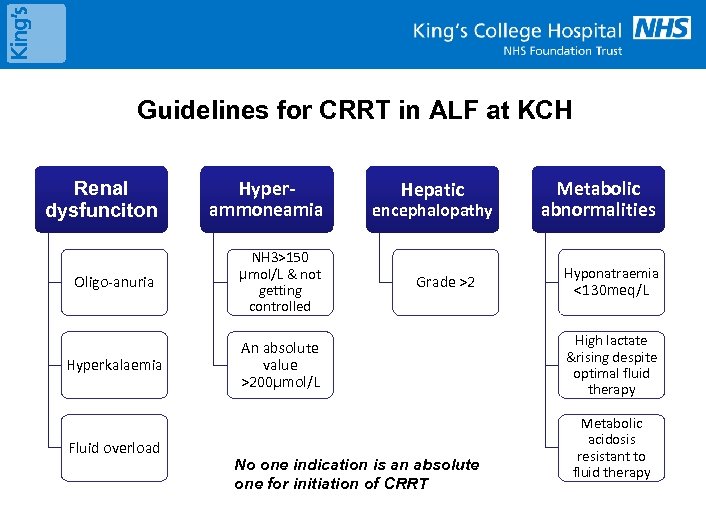 Guidelines for CRRT in ALF at KCH Renal dysfunciton Hyperammoneamia Oligo-anuria NH 3>150 µmol/L & not getting controlled Hyperkalaemia An absolute value >200µmol/L Fluid overload Hepatic encephalopathy Grade >2 No one indication is an absolute one for initiation of CRRT Metabolic abnormalities Hyponatraemia <130 meq/L High lactate &rising despite optimal fluid therapy Metabolic acidosis resistant to fluid therapy
Guidelines for CRRT in ALF at KCH Renal dysfunciton Hyperammoneamia Oligo-anuria NH 3>150 µmol/L & not getting controlled Hyperkalaemia An absolute value >200µmol/L Fluid overload Hepatic encephalopathy Grade >2 No one indication is an absolute one for initiation of CRRT Metabolic abnormalities Hyponatraemia <130 meq/L High lactate &rising despite optimal fluid therapy Metabolic acidosis resistant to fluid therapy
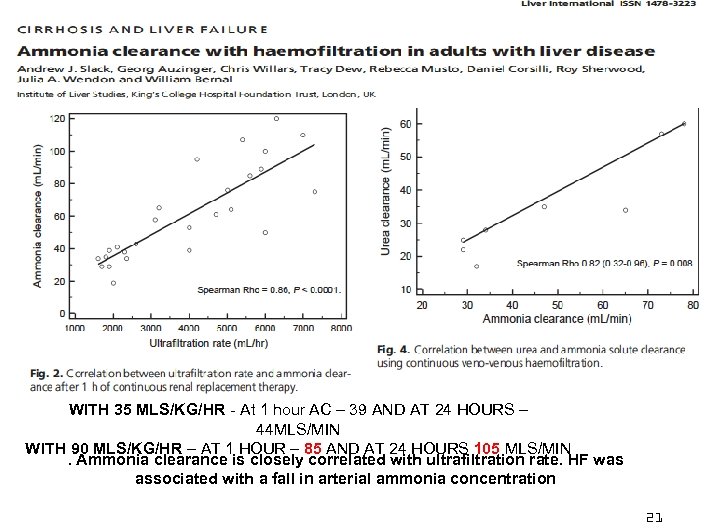 WITH 35 MLS/KG/HR - At 1 hour AC – 39 AND AT 24 HOURS – 44 MLS/MIN WITH 90 MLS/KG/HR – AT 1 HOUR – 85 AND AT 24 HOURS 105 MLS/MIN. Ammonia clearance is closely correlated with ultrafiltration rate. HF was associated with a fall in arterial ammonia concentration 21
WITH 35 MLS/KG/HR - At 1 hour AC – 39 AND AT 24 HOURS – 44 MLS/MIN WITH 90 MLS/KG/HR – AT 1 HOUR – 85 AND AT 24 HOURS 105 MLS/MIN. Ammonia clearance is closely correlated with ultrafiltration rate. HF was associated with a fall in arterial ammonia concentration 21
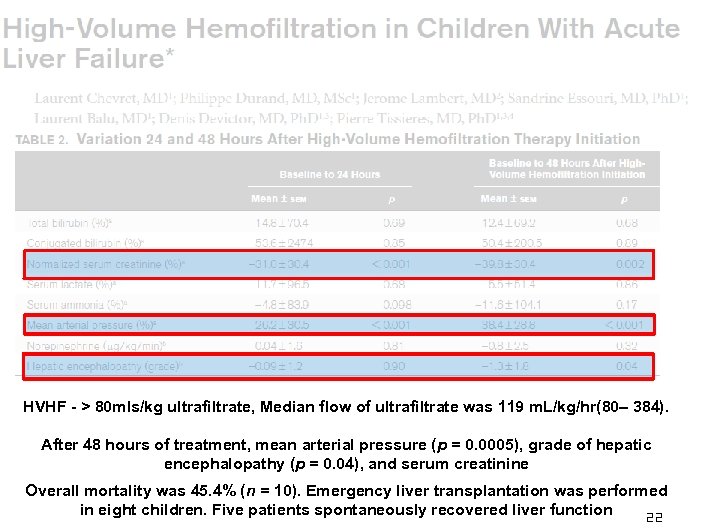 HVHF - > 80 mls/kg ultrafiltrate, Median flow of ultrafiltrate was 119 m. L/kg/hr(80– 384). After 48 hours of treatment, mean arterial pressure (p = 0. 0005), grade of hepatic encephalopathy (p = 0. 04), and serum creatinine Overall mortality was 45. 4% (n = 10). Emergency liver transplantation was performed in eight children. Five patients spontaneously recovered liver function 22
HVHF - > 80 mls/kg ultrafiltrate, Median flow of ultrafiltrate was 119 m. L/kg/hr(80– 384). After 48 hours of treatment, mean arterial pressure (p = 0. 0005), grade of hepatic encephalopathy (p = 0. 04), and serum creatinine Overall mortality was 45. 4% (n = 10). Emergency liver transplantation was performed in eight children. Five patients spontaneously recovered liver function 22
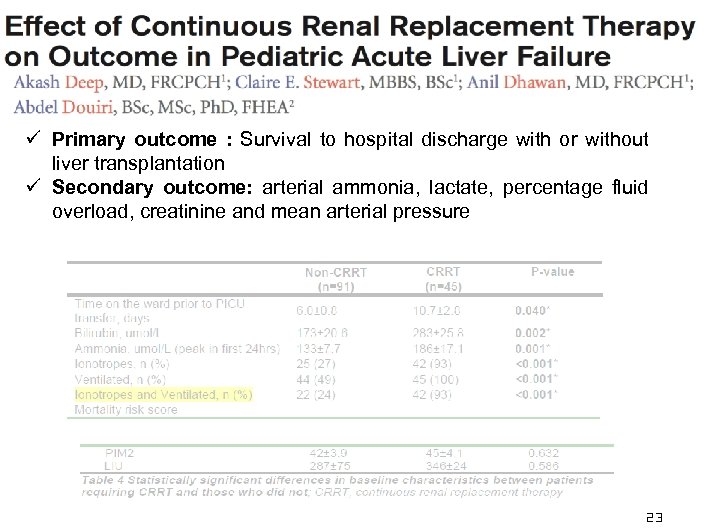 ü Primary outcome : Survival to hospital discharge with or without liver transplantation ü Secondary outcome: arterial ammonia, lactate, percentage fluid overload, creatinine and mean arterial pressure 23
ü Primary outcome : Survival to hospital discharge with or without liver transplantation ü Secondary outcome: arterial ammonia, lactate, percentage fluid overload, creatinine and mean arterial pressure 23
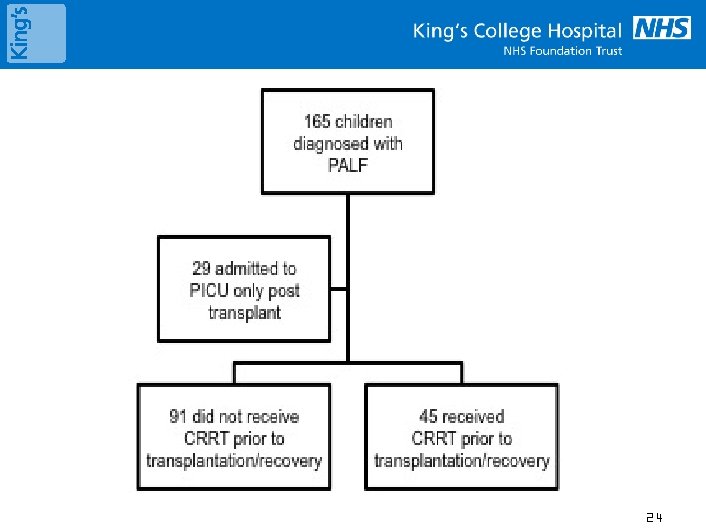 24
24
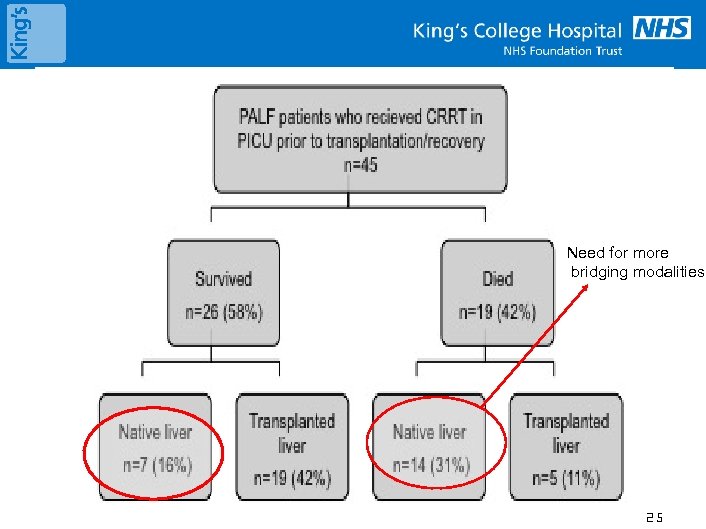 Need for more bridging modalities 25
Need for more bridging modalities 25
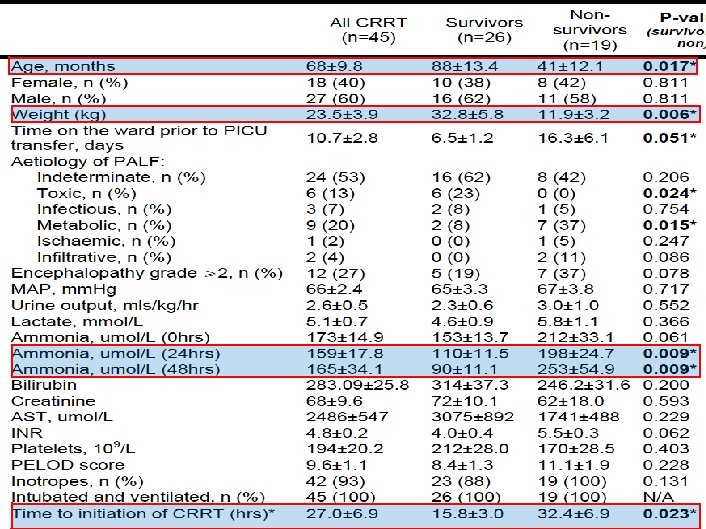 26
26
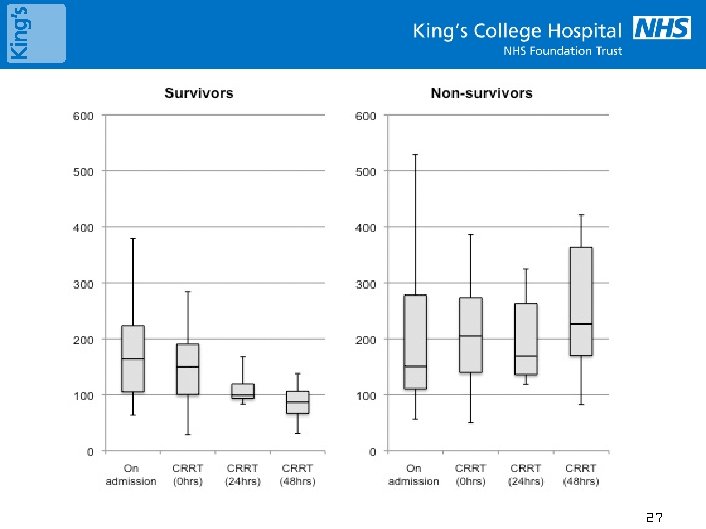 27
27
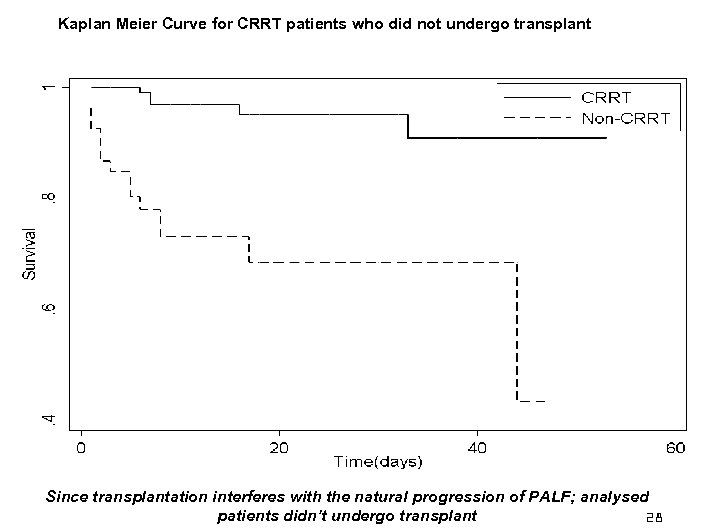 Kaplan Meier Curve for CRRT patients who did not undergo transplant Since transplantation interferes with the natural progression of PALF; analysed patients didn’t undergo transplant 28
Kaplan Meier Curve for CRRT patients who did not undergo transplant Since transplantation interferes with the natural progression of PALF; analysed patients didn’t undergo transplant 28
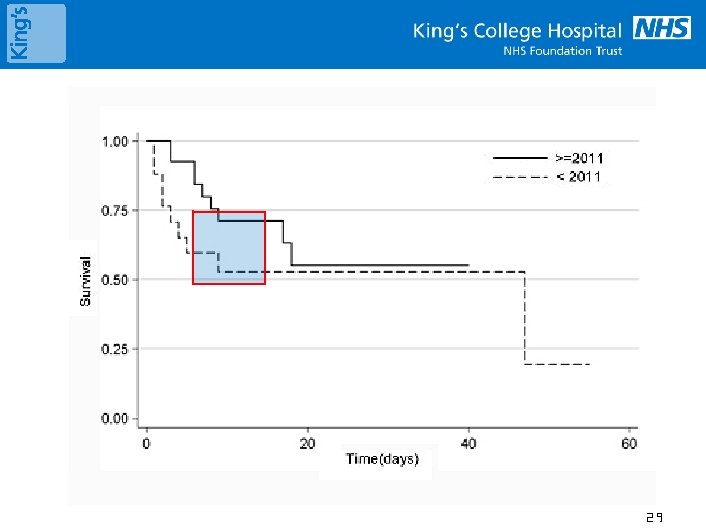 29
29
 30
30
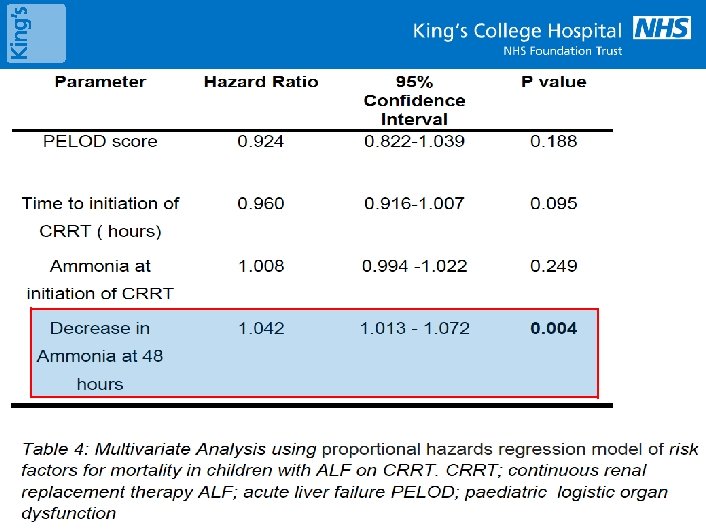
 Conclusions Early implementation of high intensity CRRT which reduces ammonia within 48 hours may provide an increased window for either spontaneous regeneration of liver to take place or for the emergency liver transplant to become available probably by : improving haemodynamics, decreasing ammonia and brain swelling
Conclusions Early implementation of high intensity CRRT which reduces ammonia within 48 hours may provide an increased window for either spontaneous regeneration of liver to take place or for the emergency liver transplant to become available probably by : improving haemodynamics, decreasing ammonia and brain swelling
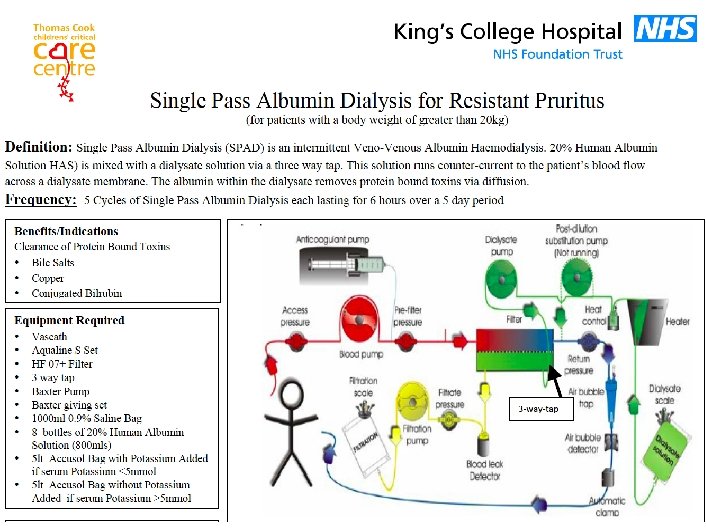
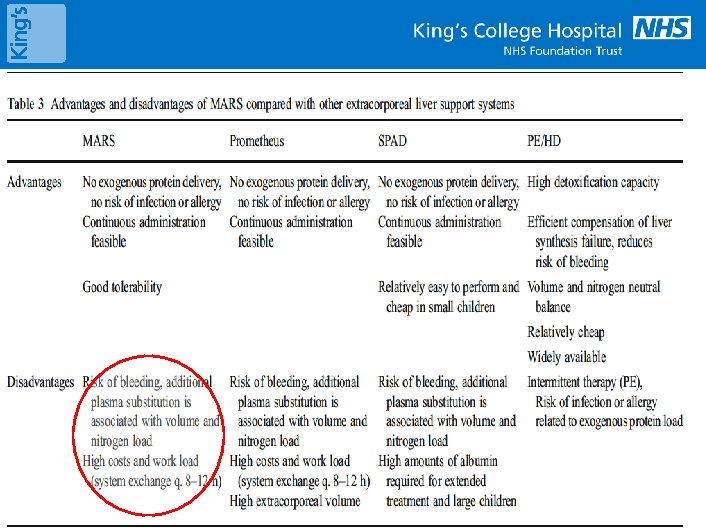
 CRRT modalities and Liver Assist Devices • CRRT – CVVH, CVVHDF – no evidence which is better • TPE – Therapeutic Plasma Exchange • TPE plus CVVH/HD • MARS • SPAD – Single Pass Albumin Dialysis 32
CRRT modalities and Liver Assist Devices • CRRT – CVVH, CVVHDF – no evidence which is better • TPE – Therapeutic Plasma Exchange • TPE plus CVVH/HD • MARS • SPAD – Single Pass Albumin Dialysis 32
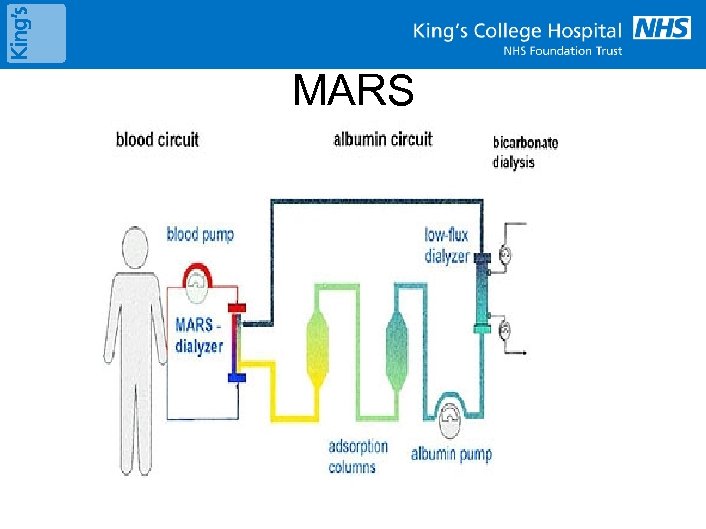 MARS
MARS
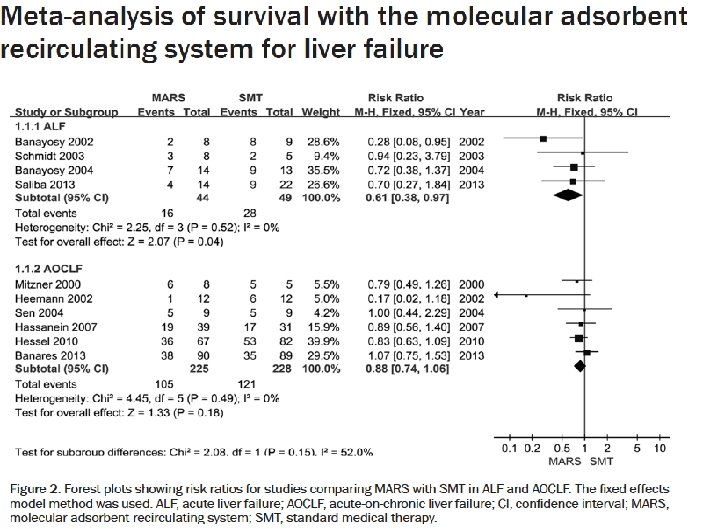
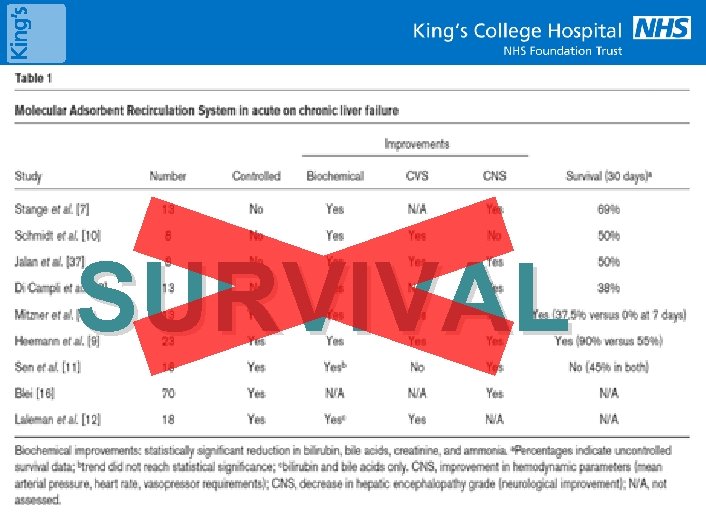 SURVIVAL 34
SURVIVAL 34
 35
35
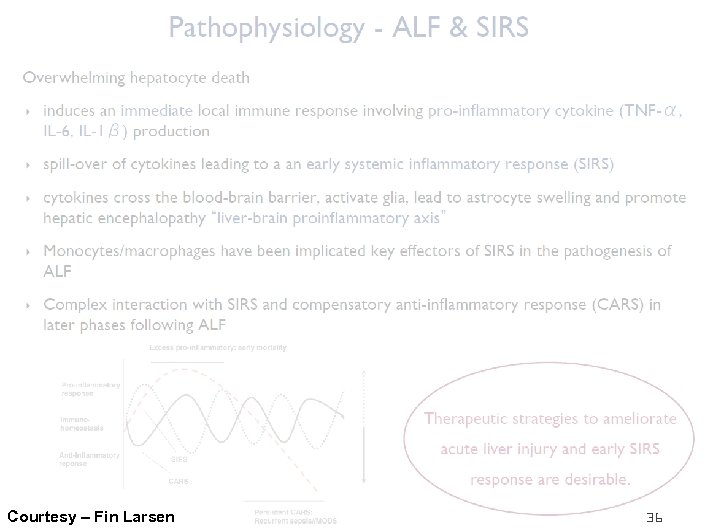 Courtesy – Fin Larsen 36
Courtesy – Fin Larsen 36
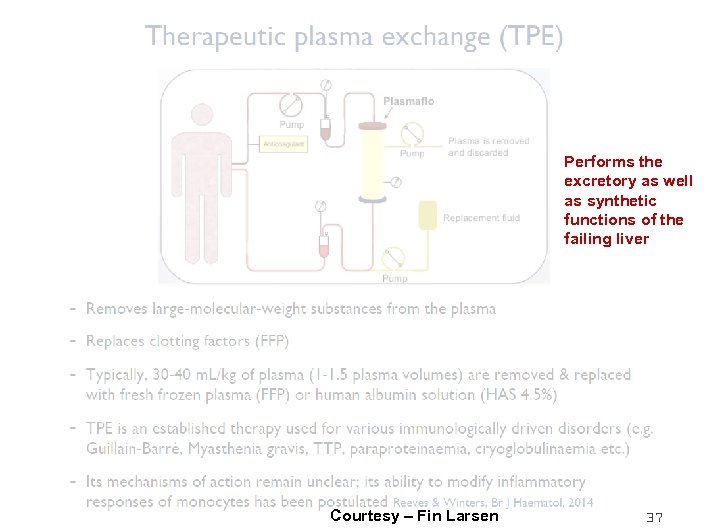 Performs the excretory as well as synthetic functions of the failing liver Courtesy – Fin Larsen 37
Performs the excretory as well as synthetic functions of the failing liver Courtesy – Fin Larsen 37
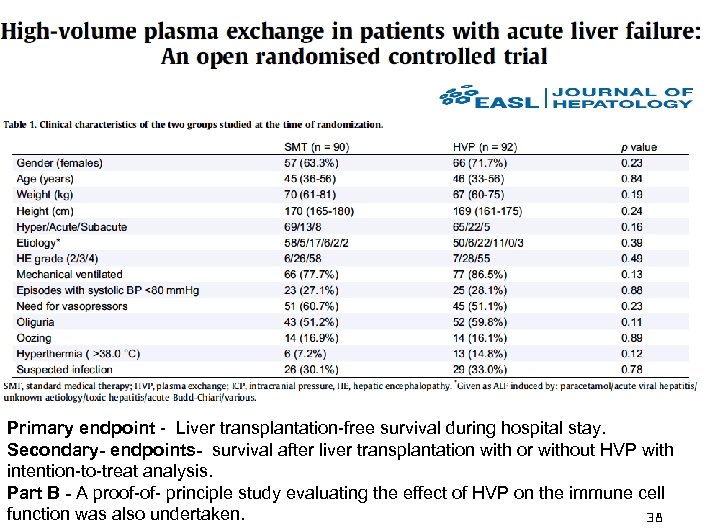 Primary endpoint - Liver transplantation-free survival during hospital stay. Secondary- endpoints- survival after liver transplantation with or without HVP with intention-to-treat analysis. Part B - A proof-of- principle study evaluating the effect of HVP on the immune cell function was also undertaken. 38
Primary endpoint - Liver transplantation-free survival during hospital stay. Secondary- endpoints- survival after liver transplantation with or without HVP with intention-to-treat analysis. Part B - A proof-of- principle study evaluating the effect of HVP on the immune cell function was also undertaken. 38
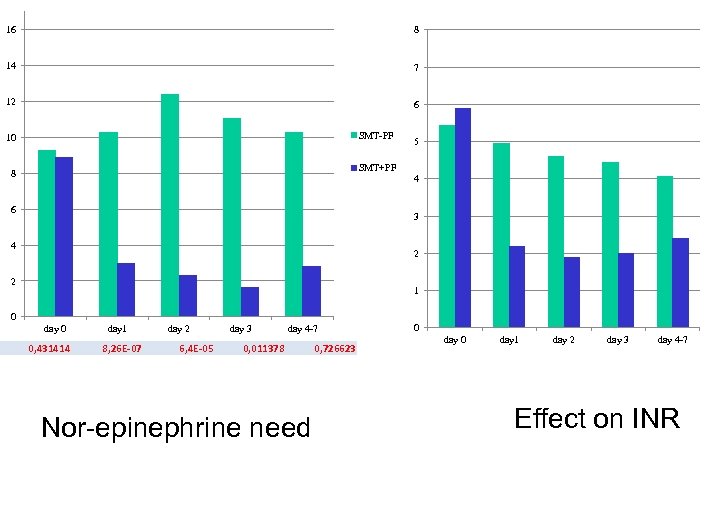 16 8 14 7 12 6 SMT-PF 10 5 SMT+PF 8 4 6 3 4 2 2 1 0 day 0 0, 431414 day 1 8, 26 E-07 day 2 6, 4 E-05 day 3 0, 011378 day 4 -7 0, 726623 Nor-epinephrine need 0 day 1 day 2 day 3 day 4 -7 Effect on INR
16 8 14 7 12 6 SMT-PF 10 5 SMT+PF 8 4 6 3 4 2 2 1 0 day 0 0, 431414 day 1 8, 26 E-07 day 2 6, 4 E-05 day 3 0, 011378 day 4 -7 0, 726623 Nor-epinephrine need 0 day 1 day 2 day 3 day 4 -7 Effect on INR
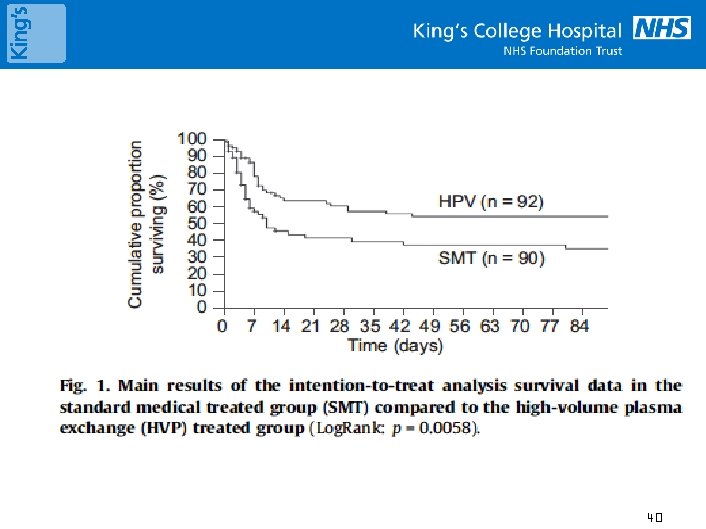 40
40
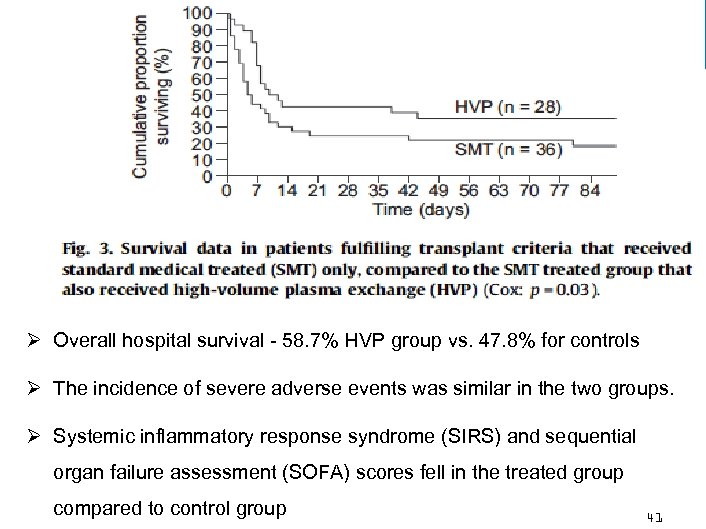 Ø Overall hospital survival - 58. 7% HVP group vs. 47. 8% for controls Ø The incidence of severe adverse events was similar in the two groups. Ø Systemic inflammatory response syndrome (SIRS) and sequential organ failure assessment (SOFA) scores fell in the treated group compared to control group 41
Ø Overall hospital survival - 58. 7% HVP group vs. 47. 8% for controls Ø The incidence of severe adverse events was similar in the two groups. Ø Systemic inflammatory response syndrome (SIRS) and sequential organ failure assessment (SOFA) scores fell in the treated group compared to control group 41
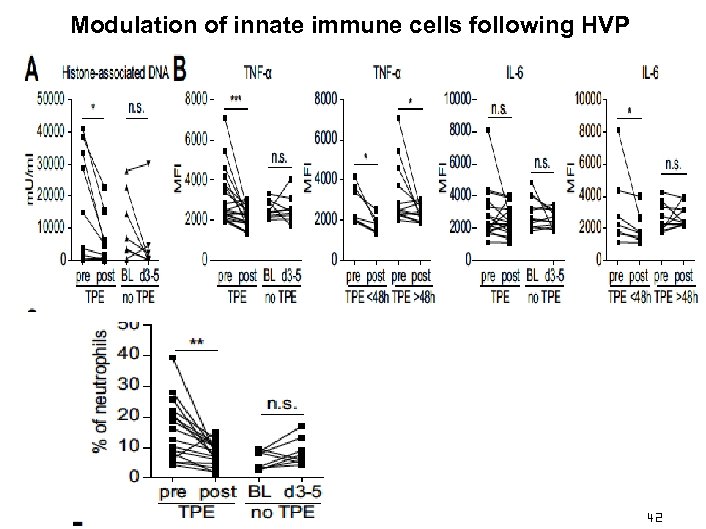 Modulation of innate immune cells following HVP 42
Modulation of innate immune cells following HVP 42
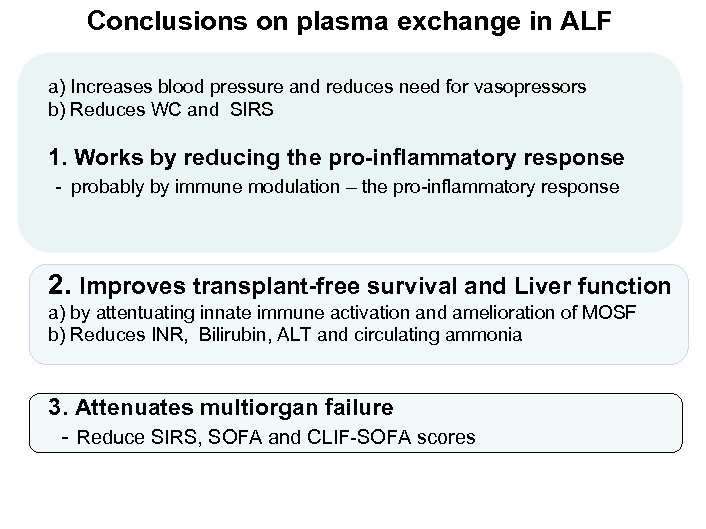 Conclusions on plasma exchange in ALF a) Increases blood pressure and reduces need for vasopressors b) Reduces WC and SIRS 1. Works by reducing the pro-inflammatory response - probably by immune modulation – the pro-inflammatory response 2. Improves transplant-free survival and Liver function a) by attentuating innate immune activation and amelioration of MOSF b) Reduces INR, Bilirubin, ALT and circulating ammonia 3. Attenuates multiorgan failure - Reduce SIRS, SOFA and CLIF-SOFA scores
Conclusions on plasma exchange in ALF a) Increases blood pressure and reduces need for vasopressors b) Reduces WC and SIRS 1. Works by reducing the pro-inflammatory response - probably by immune modulation – the pro-inflammatory response 2. Improves transplant-free survival and Liver function a) by attentuating innate immune activation and amelioration of MOSF b) Reduces INR, Bilirubin, ALT and circulating ammonia 3. Attenuates multiorgan failure - Reduce SIRS, SOFA and CLIF-SOFA scores
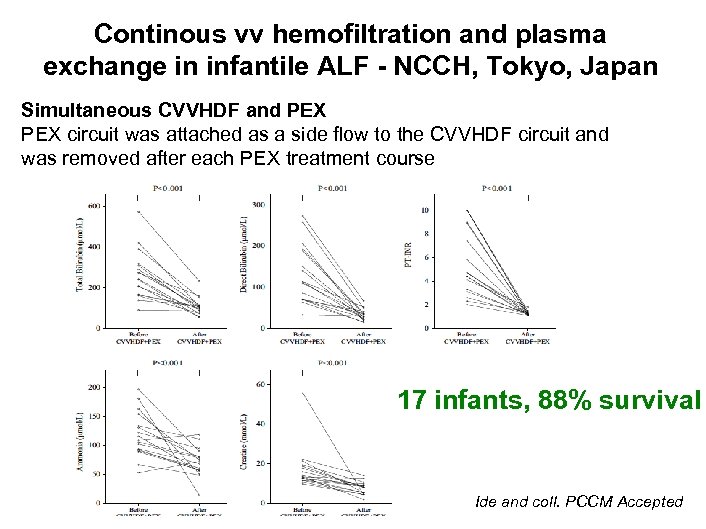 Continous vv hemofiltration and plasma exchange in infantile ALF - NCCH, Tokyo, Japan Simultaneous CVVHDF and PEX circuit was attached as a side flow to the CVVHDF circuit and was removed after each PEX treatment course 17 infants, 88% survival Ide and coll. PCCM Accepted
Continous vv hemofiltration and plasma exchange in infantile ALF - NCCH, Tokyo, Japan Simultaneous CVVHDF and PEX circuit was attached as a side flow to the CVVHDF circuit and was removed after each PEX treatment course 17 infants, 88% survival Ide and coll. PCCM Accepted
 45
45
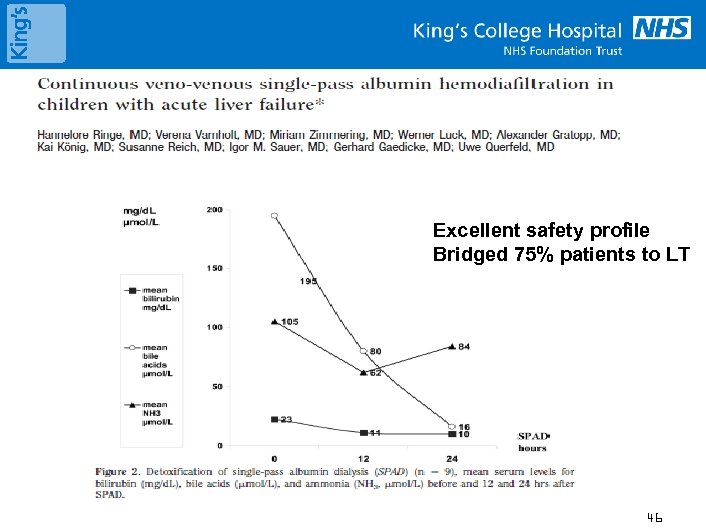 Excellent safety profile Bridged 75% patients to LT 46
Excellent safety profile Bridged 75% patients to LT 46
 47
47
 Role of Tandem therapies • CRRT plus TPE /Plasmapheresis • Combination of therapies – CRRT, TPE, MARS Safety and Efficacy of Tandem Hemodialysis and Plasma Exchange in Children Schaefer, Akos Ujszaszi, Susanne Schaefer, Karl Heinz Heckert, Franz Schaefer, and Claus Peter Schmitt Paglialonga F, Ardissino G, Biasuzzi A, Testa S, Edefonti A. Tandem plasma-exchange and haemodialysis in a paediatric dialysis unit. Pediatric Nephrology March 2012, Volume 27, Issue 3, pp 493– 495 48
Role of Tandem therapies • CRRT plus TPE /Plasmapheresis • Combination of therapies – CRRT, TPE, MARS Safety and Efficacy of Tandem Hemodialysis and Plasma Exchange in Children Schaefer, Akos Ujszaszi, Susanne Schaefer, Karl Heinz Heckert, Franz Schaefer, and Claus Peter Schmitt Paglialonga F, Ardissino G, Biasuzzi A, Testa S, Edefonti A. Tandem plasma-exchange and haemodialysis in a paediatric dialysis unit. Pediatric Nephrology March 2012, Volume 27, Issue 3, pp 493– 495 48
 SUMMARY No Evidence for RRT in Liver patients Should we undertake CRRT in ALF • Yes - and review : population data vs individual care Why ? –Neuro-protection, metabolic disarray, bridge for recovery or transplant When • Earlier - need new markers Mode • CRRT – unstable, TPE coming in fashion !! Access sites • Internal Jugular Dose • No evidence in Paediatrics • High – gaining popularity Anticoagulation - YES • PGI 2 and /or low dose heparin
SUMMARY No Evidence for RRT in Liver patients Should we undertake CRRT in ALF • Yes - and review : population data vs individual care Why ? –Neuro-protection, metabolic disarray, bridge for recovery or transplant When • Earlier - need new markers Mode • CRRT – unstable, TPE coming in fashion !! Access sites • Internal Jugular Dose • No evidence in Paediatrics • High – gaining popularity Anticoagulation - YES • PGI 2 and /or low dose heparin
 Anticoagulation in RRT in liver patients – is it different ? Should CRRT circuits in patients with hepatic failure be anti-coagulated? 50
Anticoagulation in RRT in liver patients – is it different ? Should CRRT circuits in patients with hepatic failure be anti-coagulated? 50
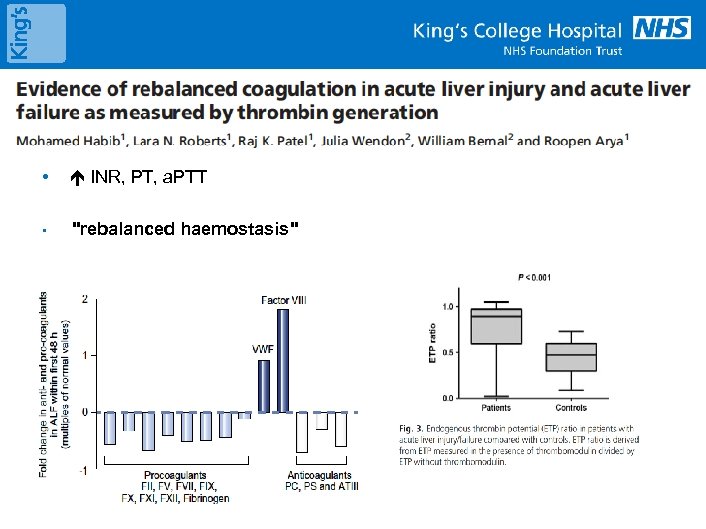 Background : Coagulopathy & Liver Disease • INR, PT, a. PTT • "rebalanced haemostasis"
Background : Coagulopathy & Liver Disease • INR, PT, a. PTT • "rebalanced haemostasis"
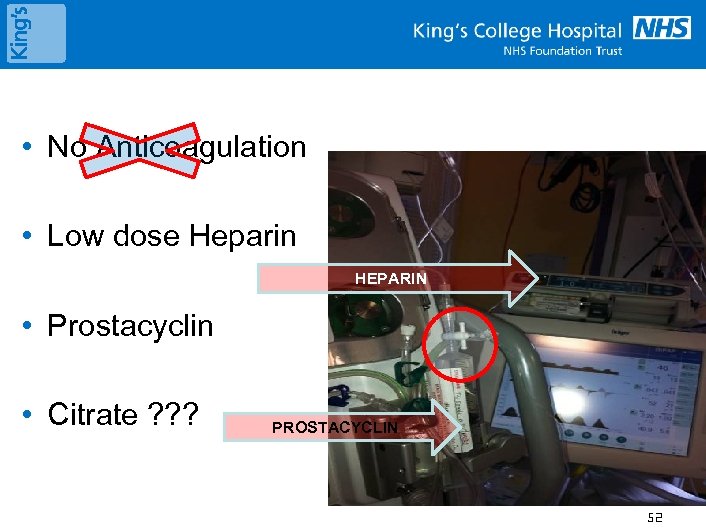 • No Anticoagulation • Low dose Heparin HEPARIN • Prostacyclin • Citrate ? ? ? PROSTACYCLIN 52
• No Anticoagulation • Low dose Heparin HEPARIN • Prostacyclin • Citrate ? ? ? PROSTACYCLIN 52
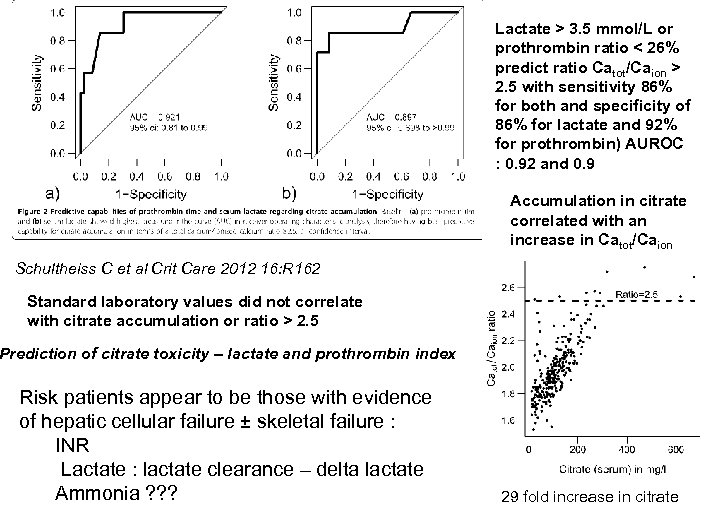 Lactate > 3. 5 mmol/L or prothrombin ratio < 26% predict ratio Catot/Caion > 2. 5 with sensitivity 86% for both and specificity of 86% for lactate and 92% for prothrombin) AUROC : 0. 92 and 0. 9 Accumulation in citrate correlated with an increase in Catot/Caion Schultheiss C et al Crit Care 2012 16: R 162 Standard laboratory values did not correlate with citrate accumulation or ratio > 2. 5 Prediction of citrate toxicity – lactate and prothrombin index Risk patients appear to be those with evidence of hepatic cellular failure ± skeletal failure : INR Lactate : lactate clearance – delta lactate Ammonia ? ? ? 29 fold increase in citrate
Lactate > 3. 5 mmol/L or prothrombin ratio < 26% predict ratio Catot/Caion > 2. 5 with sensitivity 86% for both and specificity of 86% for lactate and 92% for prothrombin) AUROC : 0. 92 and 0. 9 Accumulation in citrate correlated with an increase in Catot/Caion Schultheiss C et al Crit Care 2012 16: R 162 Standard laboratory values did not correlate with citrate accumulation or ratio > 2. 5 Prediction of citrate toxicity – lactate and prothrombin index Risk patients appear to be those with evidence of hepatic cellular failure ± skeletal failure : INR Lactate : lactate clearance – delta lactate Ammonia ? ? ? 29 fold increase in citrate
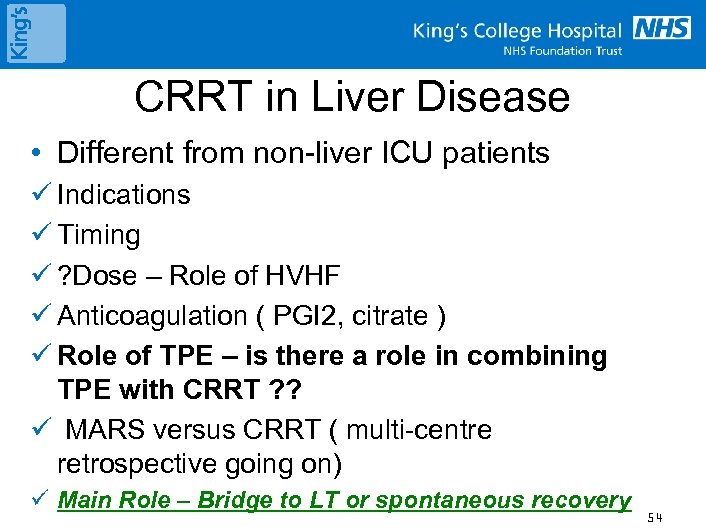 CRRT in Liver Disease • Different from non-liver ICU patients ü Indications ü Timing ü ? Dose – Role of HVHF ü Anticoagulation ( PGI 2, citrate ) ü Role of TPE – is there a role in combining TPE with CRRT ? ? ü MARS versus CRRT ( multi-centre retrospective going on) ü Main Role – Bridge to LT or spontaneous recovery 54
CRRT in Liver Disease • Different from non-liver ICU patients ü Indications ü Timing ü ? Dose – Role of HVHF ü Anticoagulation ( PGI 2, citrate ) ü Role of TPE – is there a role in combining TPE with CRRT ? ? ü MARS versus CRRT ( multi-centre retrospective going on) ü Main Role – Bridge to LT or spontaneous recovery 54


