8b2baf7f7ca70d60bb1017fc4deeedd9.ppt
- Количество слайдов: 81
 Critical Care Nutrition A Case Study of Creating Knowledge and Moving it into Action! Daren K. Heyland Director of Clinical Evaluation Research Unit Queen’s University, Kingston General Hospital Kingston, ON Canada
Critical Care Nutrition A Case Study of Creating Knowledge and Moving it into Action! Daren K. Heyland Director of Clinical Evaluation Research Unit Queen’s University, Kingston General Hospital Kingston, ON Canada
 Learning Objectives • Understand key components of moving ‘knowledge’ into action • List main updates of Canadian Critical Care Nutrition Guidelines
Learning Objectives • Understand key components of moving ‘knowledge’ into action • List main updates of Canadian Critical Care Nutrition Guidelines
 Learning Objectives
Learning Objectives
 Critical Care Nutrition The right nutrient/nutritional strategy The right timing The right patient The right intensity (dose/duration) With the right outcome! www. criticalcarenutrition. com
Critical Care Nutrition The right nutrient/nutritional strategy The right timing The right patient The right intensity (dose/duration) With the right outcome! www. criticalcarenutrition. com

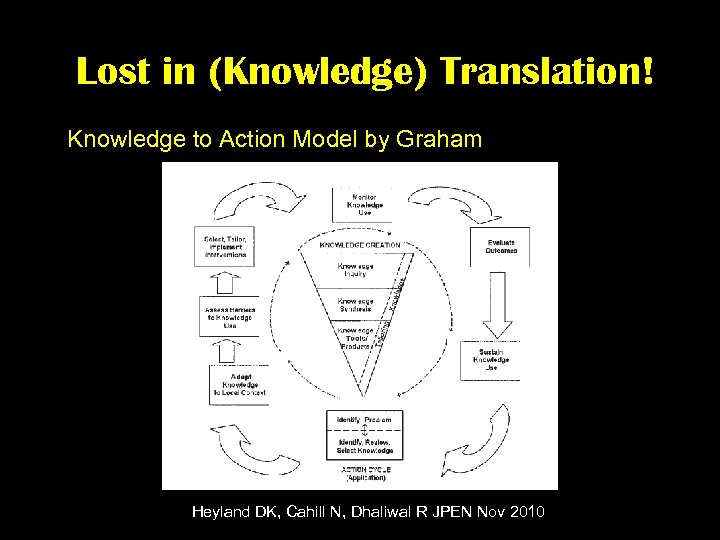 Lost in (Knowledge) Translation! Knowledge to Action Model by Graham Heyland DK, Cahill N, Dhaliwal R JPEN Nov 2010
Lost in (Knowledge) Translation! Knowledge to Action Model by Graham Heyland DK, Cahill N, Dhaliwal R JPEN Nov 2010
 Knowledge Creation
Knowledge Creation
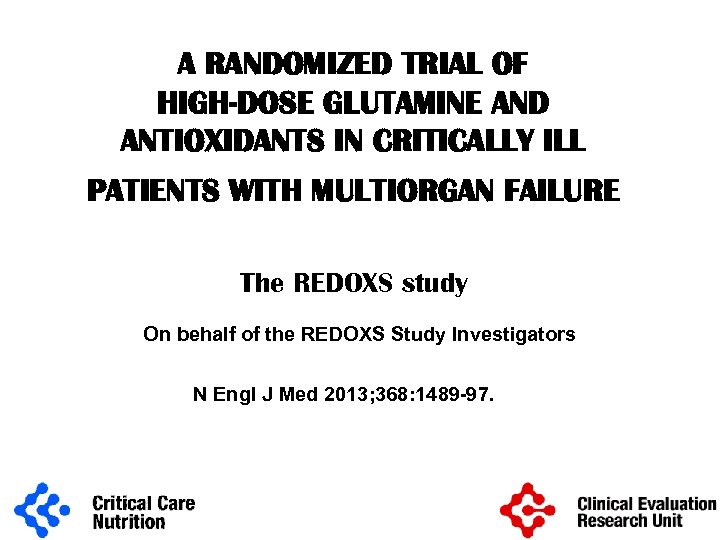 A RANDOMIZED TRIAL OF HIGH-DOSE GLUTAMINE AND ANTIOXIDANTS IN CRITICALLY ILL PATIENTS WITH MULTIORGAN FAILURE The REDOXS study On behalf of the REDOXS Study Investigators N Engl J Med 2013; 368: 1489 -97.
A RANDOMIZED TRIAL OF HIGH-DOSE GLUTAMINE AND ANTIOXIDANTS IN CRITICALLY ILL PATIENTS WITH MULTIORGAN FAILURE The REDOXS study On behalf of the REDOXS Study Investigators N Engl J Med 2013; 368: 1489 -97.
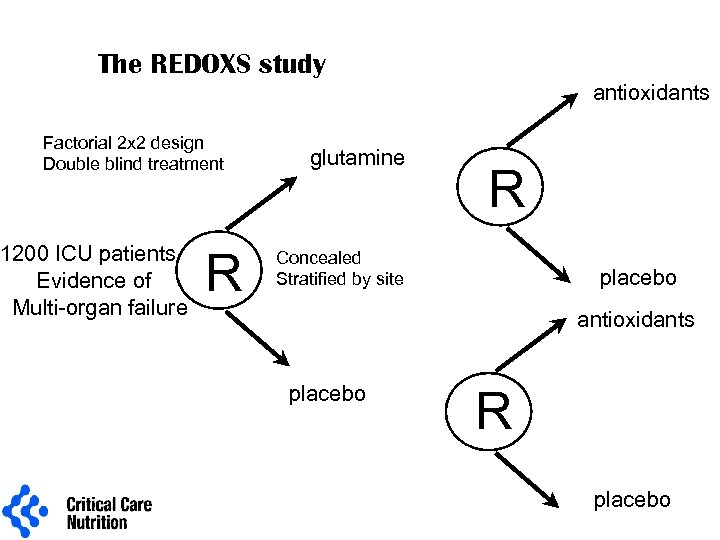 The REDOXS study antioxidants Factorial 2 x 2 design Double blind treatment 1200 ICU patients Evidence of Multi-organ failure R glutamine R Concealed Stratified by site placebo antioxidants placebo R placebo
The REDOXS study antioxidants Factorial 2 x 2 design Double blind treatment 1200 ICU patients Evidence of Multi-organ failure R glutamine R Concealed Stratified by site placebo antioxidants placebo R placebo
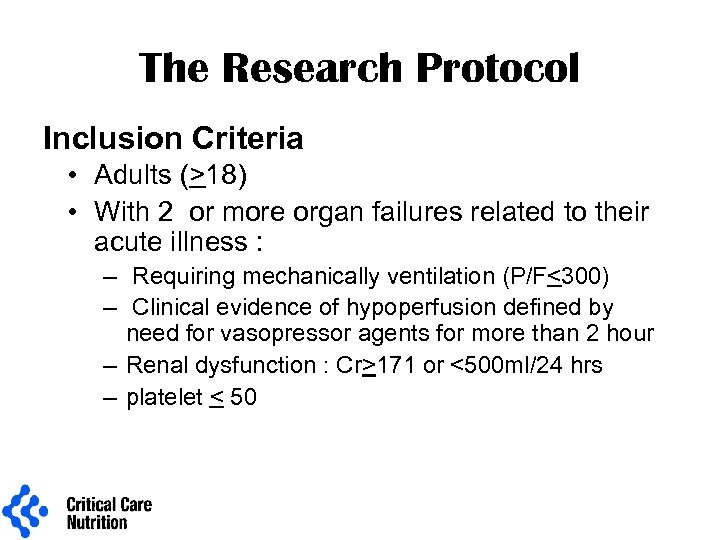 The Research Protocol Inclusion Criteria • Adults (>18) • With 2 or more organ failures related to their acute illness : – Requiring mechanically ventilation (P/F<300) – Clinical evidence of hypoperfusion defined by need for vasopressor agents for more than 2 hour – Renal dysfunction : Cr>171 or <500 ml/24 hrs – platelet < 50
The Research Protocol Inclusion Criteria • Adults (>18) • With 2 or more organ failures related to their acute illness : – Requiring mechanically ventilation (P/F<300) – Clinical evidence of hypoperfusion defined by need for vasopressor agents for more than 2 hour – Renal dysfunction : Cr>171 or <500 ml/24 hrs – platelet < 50
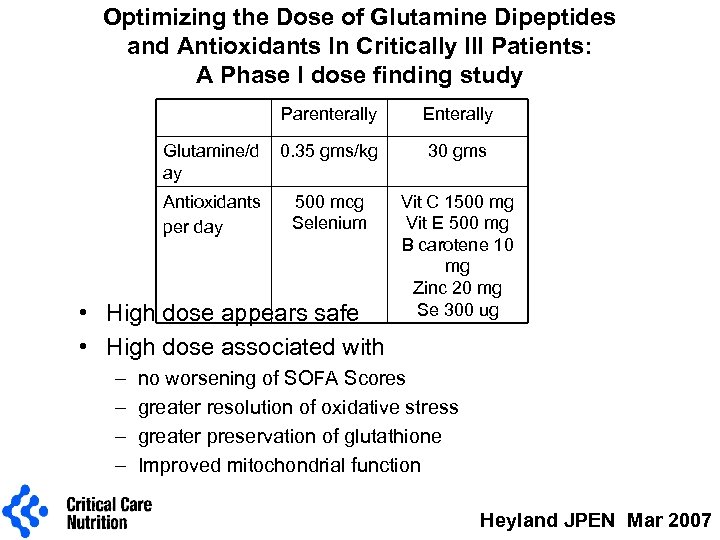 Optimizing the Dose of Glutamine Dipeptides and Antioxidants In Critically Ill Patients: A Phase I dose finding study Parenterally Enterally Glutamine/d ay 0. 35 gms/kg 30 gms Antioxidants per day 500 mcg Selenium Vit C 1500 mg Vit E 500 mg B carotene 10 mg Zinc 20 mg Se 300 ug • High dose appears safe • High dose associated with – – no worsening of SOFA Scores greater resolution of oxidative stress greater preservation of glutathione Improved mitochondrial function Heyland JPEN Mar 2007
Optimizing the Dose of Glutamine Dipeptides and Antioxidants In Critically Ill Patients: A Phase I dose finding study Parenterally Enterally Glutamine/d ay 0. 35 gms/kg 30 gms Antioxidants per day 500 mcg Selenium Vit C 1500 mg Vit E 500 mg B carotene 10 mg Zinc 20 mg Se 300 ug • High dose appears safe • High dose associated with – – no worsening of SOFA Scores greater resolution of oxidative stress greater preservation of glutathione Improved mitochondrial function Heyland JPEN Mar 2007
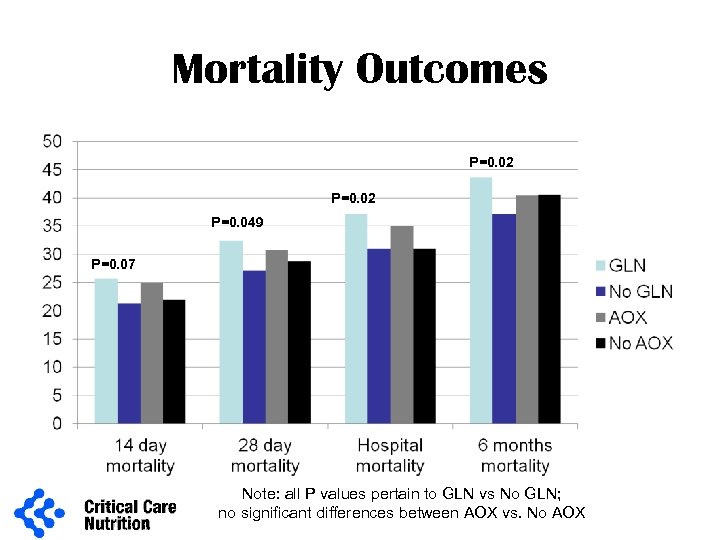 Mortality Outcomes P=0. 02 P=0. 049 P=0. 07 Note: all P values pertain to GLN vs No GLN; no significant differences between AOX vs. No AOX
Mortality Outcomes P=0. 02 P=0. 049 P=0. 07 Note: all P values pertain to GLN vs No GLN; no significant differences between AOX vs. No AOX
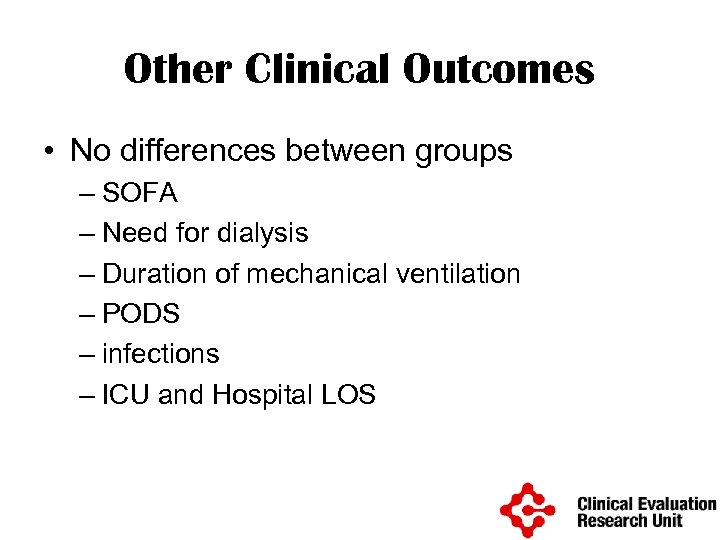 Other Clinical Outcomes • No differences between groups – SOFA – Need for dialysis – Duration of mechanical ventilation – PODS – infections – ICU and Hospital LOS
Other Clinical Outcomes • No differences between groups – SOFA – Need for dialysis – Duration of mechanical ventilation – PODS – infections – ICU and Hospital LOS
 Post-hoc Secondary Analyses
Post-hoc Secondary Analyses
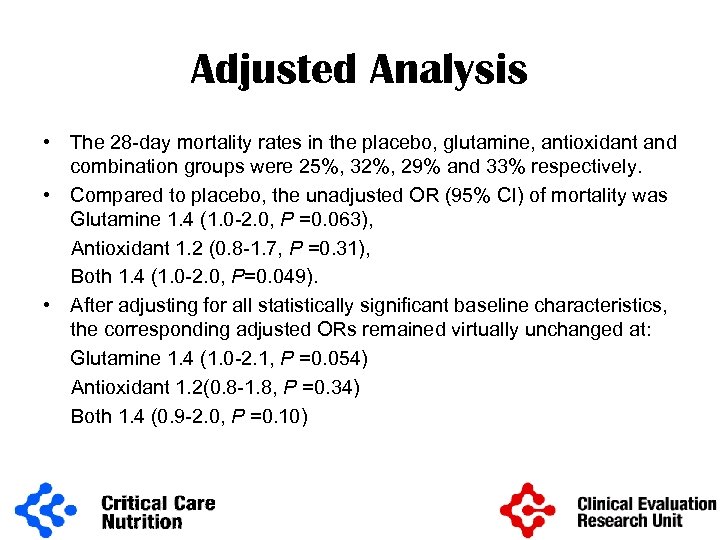 Adjusted Analysis • The 28 -day mortality rates in the placebo, glutamine, antioxidant and combination groups were 25%, 32%, 29% and 33% respectively. • Compared to placebo, the unadjusted OR (95% CI) of mortality was Glutamine 1. 4 (1. 0 -2. 0, P =0. 063), Antioxidant 1. 2 (0. 8 -1. 7, P =0. 31), Both 1. 4 (1. 0 -2. 0, P=0. 049). • After adjusting for all statistically significant baseline characteristics, the corresponding adjusted ORs remained virtually unchanged at: Glutamine 1. 4 (1. 0 -2. 1, P =0. 054) Antioxidant 1. 2(0. 8 -1. 8, P =0. 34) Both 1. 4 (0. 9 -2. 0, P =0. 10)
Adjusted Analysis • The 28 -day mortality rates in the placebo, glutamine, antioxidant and combination groups were 25%, 32%, 29% and 33% respectively. • Compared to placebo, the unadjusted OR (95% CI) of mortality was Glutamine 1. 4 (1. 0 -2. 0, P =0. 063), Antioxidant 1. 2 (0. 8 -1. 7, P =0. 31), Both 1. 4 (1. 0 -2. 0, P=0. 049). • After adjusting for all statistically significant baseline characteristics, the corresponding adjusted ORs remained virtually unchanged at: Glutamine 1. 4 (1. 0 -2. 1, P =0. 054) Antioxidant 1. 2(0. 8 -1. 8, P =0. 34) Both 1. 4 (0. 9 -2. 0, P =0. 10)
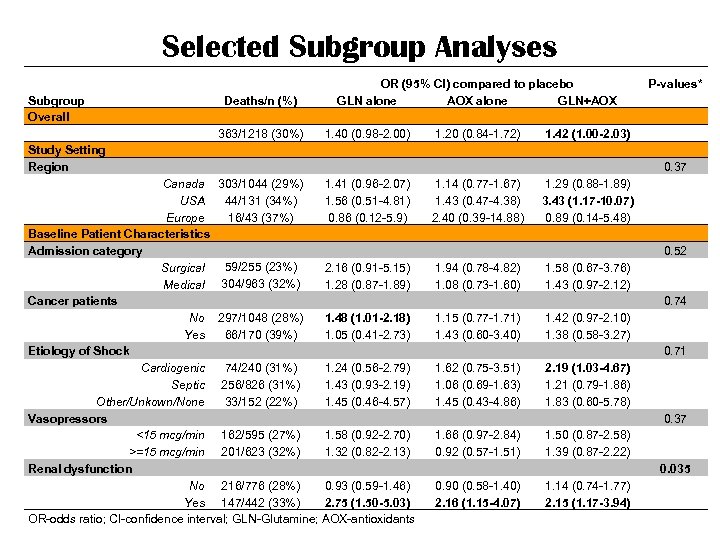 Selected Subgroup Analyses Subgroup Overall Study Setting Region OR (95% CI) compared to placebo GLN alone AOX alone GLN+AOX 1. 40 (0. 98 -2. 00) 1. 20 (0. 84 -1. 72) 1. 42 (1. 00 -2. 03) Canada 1. 41 (0. 96 -2. 07) 1. 14 (0. 77 -1. 67) 1. 29 (0. 88 -1. 89) USA 1. 56 (0. 51 -4. 81) 1. 43 (0. 47 -4. 38) 3. 43 (1. 17 -10. 07) Europe 0. 86 (0. 12 -5. 9) 2. 40 (0. 39 -14. 88) 0. 89 (0. 14 -5. 48) Baseline Patient Characteristics Admission category 59/255 (23%) Surgical 2. 16 (0. 91 -5. 15) 1. 94 (0. 78 -4. 82) 1. 58 (0. 67 -3. 76) Medical 304/963 (32%) 1. 28 (0. 87 -1. 89) 1. 08 (0. 73 -1. 60) 1. 43 (0. 97 -2. 12) Cancer patients No 297/1048 (28%) 1. 48 (1. 01 -2. 18) 1. 15 (0. 77 -1. 71) 1. 42 (0. 97 -2. 10) 66/170 (39%) Yes 1. 05 (0. 41 -2. 73) 1. 43 (0. 60 -3. 40) 1. 38 (0. 58 -3. 27) Etiology of Shock 74/240 (31%) Cardiogenic 1. 24 (0. 56 -2. 79) 1. 62 (0. 75 -3. 51) 2. 19 (1. 03 -4. 67) Septic 256/826 (31%) 1. 43 (0. 93 -2. 19) 1. 06 (0. 69 -1. 63) 1. 21 (0. 79 -1. 86) 33/152 (22%) Other/Unkown/None 1. 45 (0. 46 -4. 57) 1. 45 (0. 43 -4. 86) 1. 83 (0. 60 -5. 78) Vasopressors <15 mcg/min 162/595 (27%) 1. 58 (0. 92 -2. 70) 1. 66 (0. 97 -2. 84) 1. 50 (0. 87 -2. 58) >=15 mcg/min 201/623 (32%) 1. 32 (0. 82 -2. 13) 0. 92 (0. 57 -1. 51) 1. 39 (0. 87 -2. 22) Renal dysfunction No 216/776 (28%) 0. 93 (0. 59 -1. 46) 0. 90 (0. 58 -1. 40) 1. 14 (0. 74 -1. 77) Yes 147/442 (33%) 2. 75 (1. 50 -5. 03) 2. 16 (1. 15 -4. 07) 2. 15 (1. 17 -3. 94) OR-odds ratio; CI-confidence interval; GLN-Glutamine; AOX-antioxidants Deaths/n (%) 363/1218 (30%) 303/1044 (29%) 44/131 (34%) 16/43 (37%) P-values* 0. 37 0. 52 0. 74 0. 71 0. 37 0. 035
Selected Subgroup Analyses Subgroup Overall Study Setting Region OR (95% CI) compared to placebo GLN alone AOX alone GLN+AOX 1. 40 (0. 98 -2. 00) 1. 20 (0. 84 -1. 72) 1. 42 (1. 00 -2. 03) Canada 1. 41 (0. 96 -2. 07) 1. 14 (0. 77 -1. 67) 1. 29 (0. 88 -1. 89) USA 1. 56 (0. 51 -4. 81) 1. 43 (0. 47 -4. 38) 3. 43 (1. 17 -10. 07) Europe 0. 86 (0. 12 -5. 9) 2. 40 (0. 39 -14. 88) 0. 89 (0. 14 -5. 48) Baseline Patient Characteristics Admission category 59/255 (23%) Surgical 2. 16 (0. 91 -5. 15) 1. 94 (0. 78 -4. 82) 1. 58 (0. 67 -3. 76) Medical 304/963 (32%) 1. 28 (0. 87 -1. 89) 1. 08 (0. 73 -1. 60) 1. 43 (0. 97 -2. 12) Cancer patients No 297/1048 (28%) 1. 48 (1. 01 -2. 18) 1. 15 (0. 77 -1. 71) 1. 42 (0. 97 -2. 10) 66/170 (39%) Yes 1. 05 (0. 41 -2. 73) 1. 43 (0. 60 -3. 40) 1. 38 (0. 58 -3. 27) Etiology of Shock 74/240 (31%) Cardiogenic 1. 24 (0. 56 -2. 79) 1. 62 (0. 75 -3. 51) 2. 19 (1. 03 -4. 67) Septic 256/826 (31%) 1. 43 (0. 93 -2. 19) 1. 06 (0. 69 -1. 63) 1. 21 (0. 79 -1. 86) 33/152 (22%) Other/Unkown/None 1. 45 (0. 46 -4. 57) 1. 45 (0. 43 -4. 86) 1. 83 (0. 60 -5. 78) Vasopressors <15 mcg/min 162/595 (27%) 1. 58 (0. 92 -2. 70) 1. 66 (0. 97 -2. 84) 1. 50 (0. 87 -2. 58) >=15 mcg/min 201/623 (32%) 1. 32 (0. 82 -2. 13) 0. 92 (0. 57 -1. 51) 1. 39 (0. 87 -2. 22) Renal dysfunction No 216/776 (28%) 0. 93 (0. 59 -1. 46) 0. 90 (0. 58 -1. 40) 1. 14 (0. 74 -1. 77) Yes 147/442 (33%) 2. 75 (1. 50 -5. 03) 2. 16 (1. 15 -4. 07) 2. 15 (1. 17 -3. 94) OR-odds ratio; CI-confidence interval; GLN-Glutamine; AOX-antioxidants Deaths/n (%) 363/1218 (30%) 303/1044 (29%) 44/131 (34%) 16/43 (37%) P-values* 0. 37 0. 52 0. 74 0. 71 0. 37 0. 035
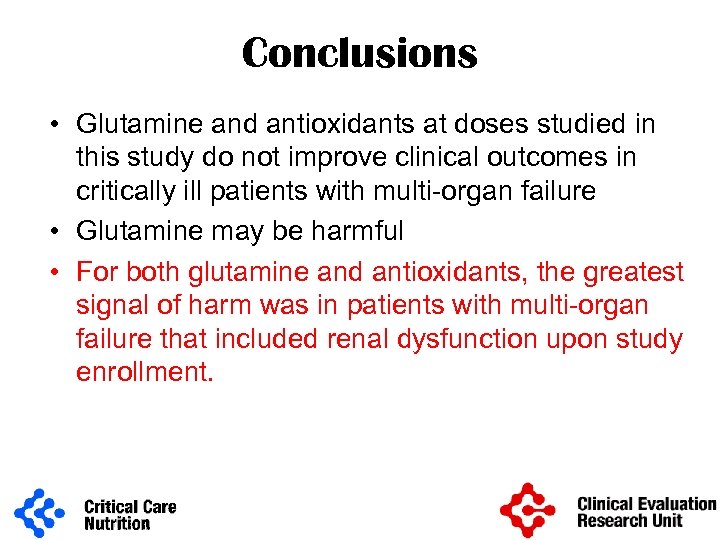 Conclusions • Glutamine and antioxidants at doses studied in this study do not improve clinical outcomes in critically ill patients with multi-organ failure • Glutamine may be harmful • For both glutamine and antioxidants, the greatest signal of harm was in patients with multi-organ failure that included renal dysfunction upon study enrollment.
Conclusions • Glutamine and antioxidants at doses studied in this study do not improve clinical outcomes in critically ill patients with multi-organ failure • Glutamine may be harmful • For both glutamine and antioxidants, the greatest signal of harm was in patients with multi-organ failure that included renal dysfunction upon study enrollment.
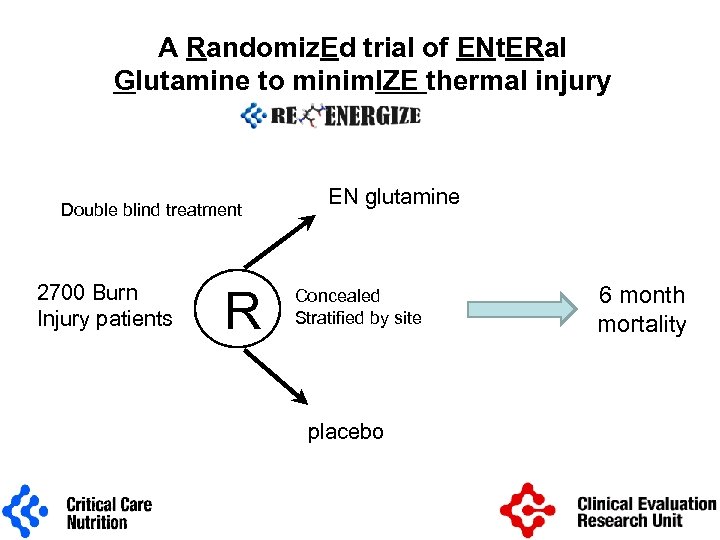 A Randomiz. Ed trial of ENt. ERal Glutamine to minim. IZE thermal injury Double blind treatment 2700 Burn Injury patients R EN glutamine Concealed Stratified by site placebo 6 month mortality
A Randomiz. Ed trial of ENt. ERal Glutamine to minim. IZE thermal injury Double blind treatment 2700 Burn Injury patients R EN glutamine Concealed Stratified by site placebo 6 month mortality
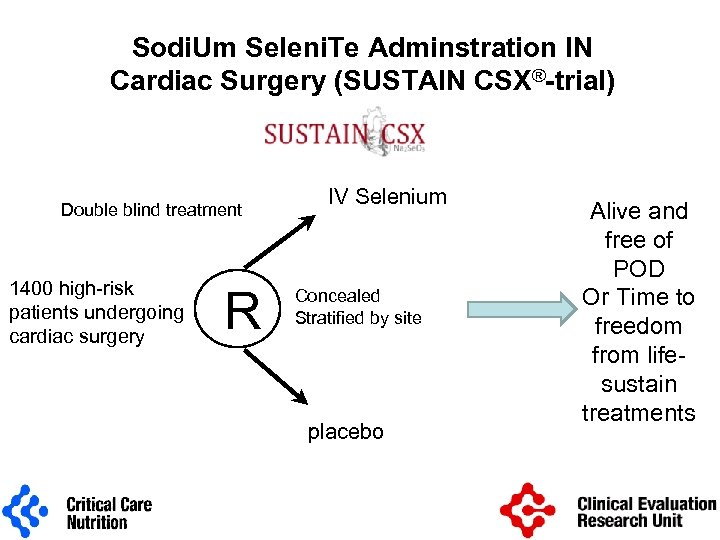 Sodi. Um Seleni. Te Adminstration IN Cardiac Surgery (SUSTAIN CSX®-trial) Double blind treatment 1400 high-risk patients undergoing cardiac surgery R IV Selenium Concealed Stratified by site placebo Alive and free of POD Or Time to freedom from lifesustain treatments
Sodi. Um Seleni. Te Adminstration IN Cardiac Surgery (SUSTAIN CSX®-trial) Double blind treatment 1400 high-risk patients undergoing cardiac surgery R IV Selenium Concealed Stratified by site placebo Alive and free of POD Or Time to freedom from lifesustain treatments
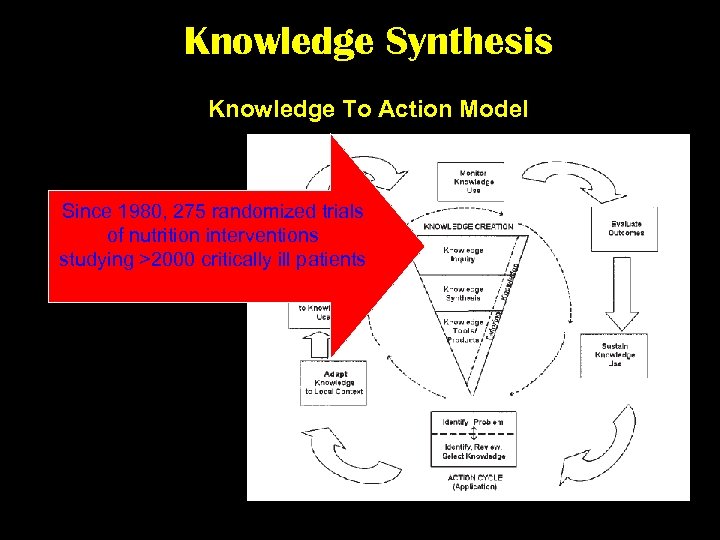 Knowledge Synthesis Knowledge To Action Model Since 1980, 275 randomized trials of nutrition interventions studying >2000 critically ill patients
Knowledge Synthesis Knowledge To Action Model Since 1980, 275 randomized trials of nutrition interventions studying >2000 critically ill patients
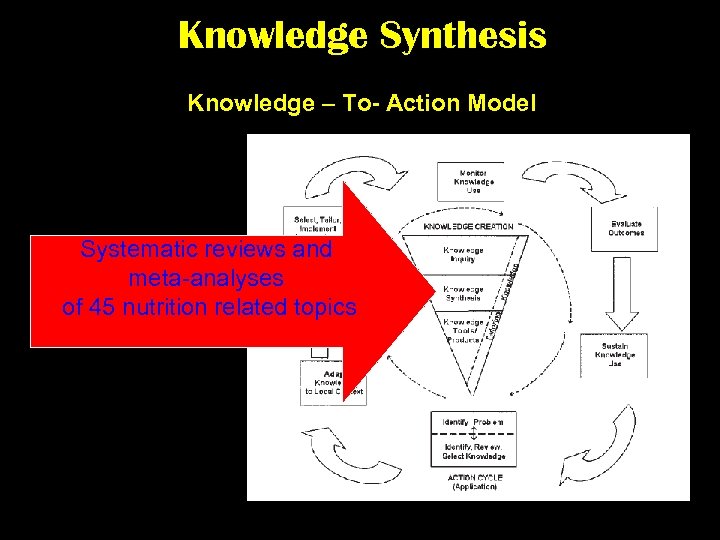 Knowledge Synthesis Knowledge – To- Action Model Systematic reviews and meta-analyses of 45 nutrition related topics
Knowledge Synthesis Knowledge – To- Action Model Systematic reviews and meta-analyses of 45 nutrition related topics
 What does the evidence show about Alternative Lipid Emulsions in the Critically Ill?
What does the evidence show about Alternative Lipid Emulsions in the Critically Ill?
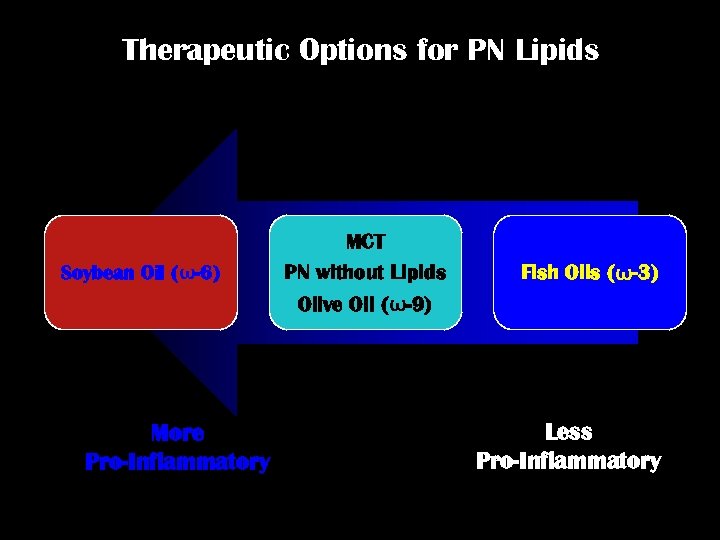 Therapeutic Options for PN Lipids Soybean Oil (ω-6) More Pro-Inflammatory MCT PN without Lipids Olive Oil (ω-9) Fish Oils (ω-3) Less Pro-Inflammatory
Therapeutic Options for PN Lipids Soybean Oil (ω-6) More Pro-Inflammatory MCT PN without Lipids Olive Oil (ω-9) Fish Oils (ω-3) Less Pro-Inflammatory
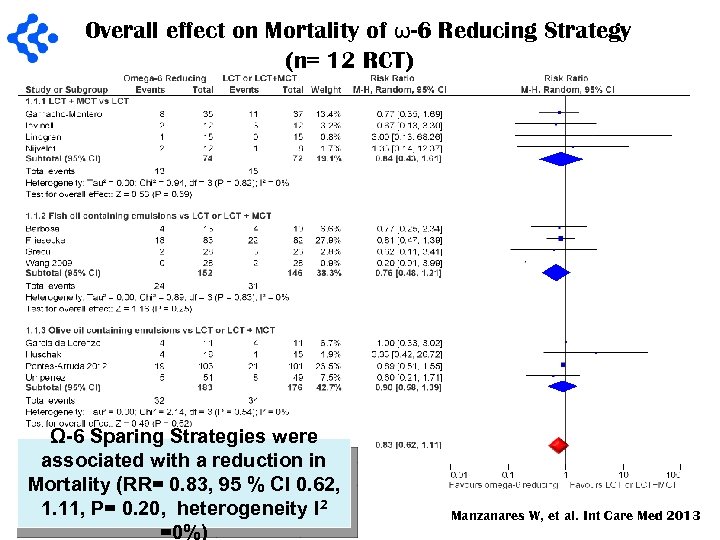 Overall effect on Mortality of ω-6 Reducing Strategy (n= 12 RCT) Ω-6 Sparing Strategies were associated with a reduction in Mortality (RR= 0. 83, 95 % CI 0. 62, 1. 11, P= 0. 20, heterogeneity I 2 =0%) Manzanares W, et al. Int Care Med 2013
Overall effect on Mortality of ω-6 Reducing Strategy (n= 12 RCT) Ω-6 Sparing Strategies were associated with a reduction in Mortality (RR= 0. 83, 95 % CI 0. 62, 1. 11, P= 0. 20, heterogeneity I 2 =0%) Manzanares W, et al. Int Care Med 2013
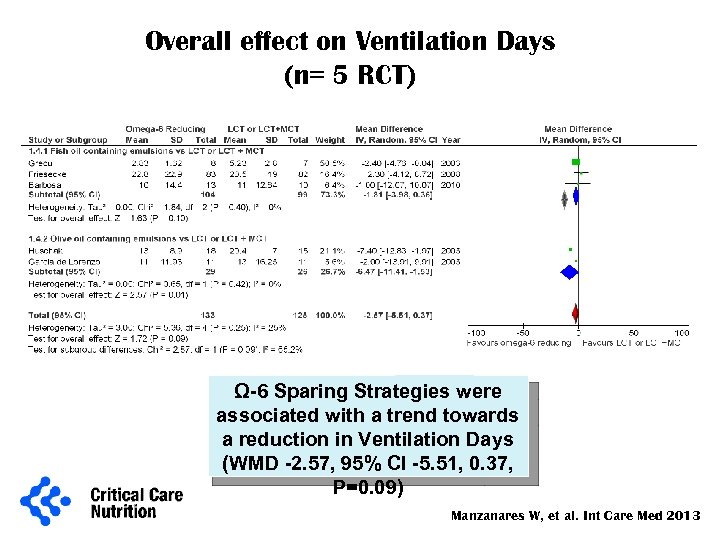 Overall effect on Ventilation Days (n= 5 RCT) Ω-6 Sparing Strategies were associated with a trend towards a reduction in Ventilation Days (WMD -2. 57, 95% CI -5. 51, 0. 37, P=0. 09) Manzanares W, et al. Int Care Med 2013
Overall effect on Ventilation Days (n= 5 RCT) Ω-6 Sparing Strategies were associated with a trend towards a reduction in Ventilation Days (WMD -2. 57, 95% CI -5. 51, 0. 37, P=0. 09) Manzanares W, et al. Int Care Med 2013
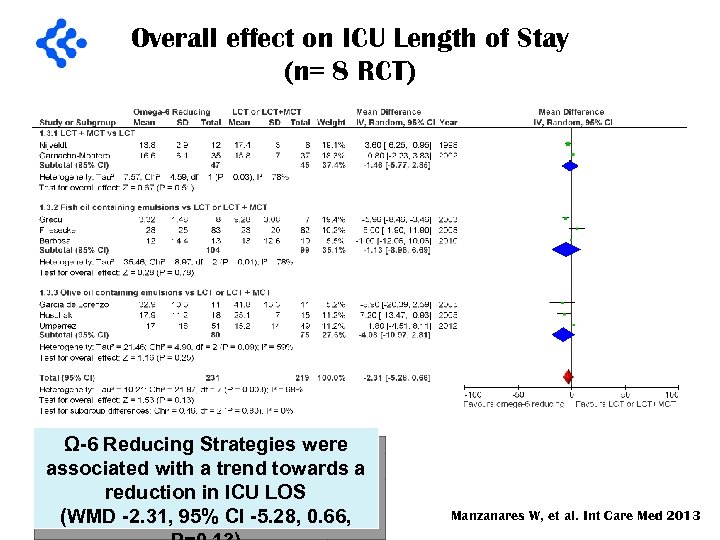 Overall effect on ICU Length of Stay (n= 8 RCT) Ω-6 Reducing Strategies were associated with a trend towards a reduction in ICU LOS (WMD -2. 31, 95% CI -5. 28, 0. 66, Manzanares W, et al. Int Care Med 2013
Overall effect on ICU Length of Stay (n= 8 RCT) Ω-6 Reducing Strategies were associated with a trend towards a reduction in ICU LOS (WMD -2. 31, 95% CI -5. 28, 0. 66, Manzanares W, et al. Int Care Med 2013
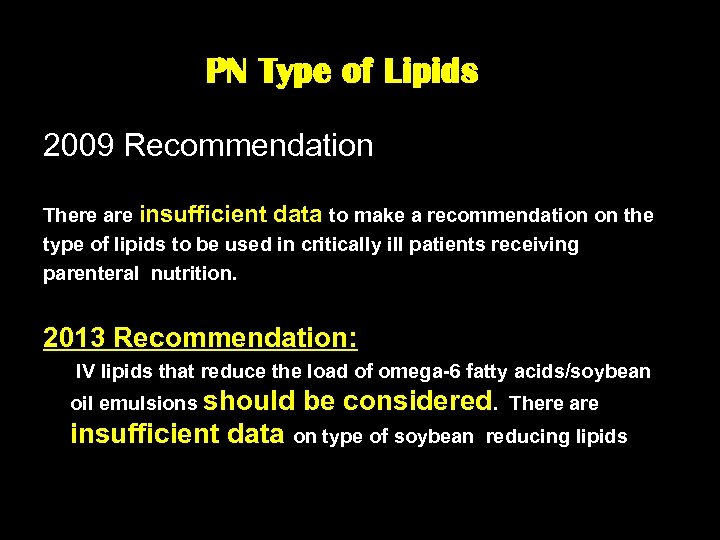 PN Type of Lipids 2009 Recommendation There are insufficient data to make a recommendation on the type of lipids to be used in critically ill patients receiving parenteral nutrition. 2013 Recommendation: IV lipids that reduce the load of omega-6 fatty acids/soybean oil emulsions should be considered. There are insufficient data on type of soybean reducing lipids
PN Type of Lipids 2009 Recommendation There are insufficient data to make a recommendation on the type of lipids to be used in critically ill patients receiving parenteral nutrition. 2013 Recommendation: IV lipids that reduce the load of omega-6 fatty acids/soybean oil emulsions should be considered. There are insufficient data on type of soybean reducing lipids
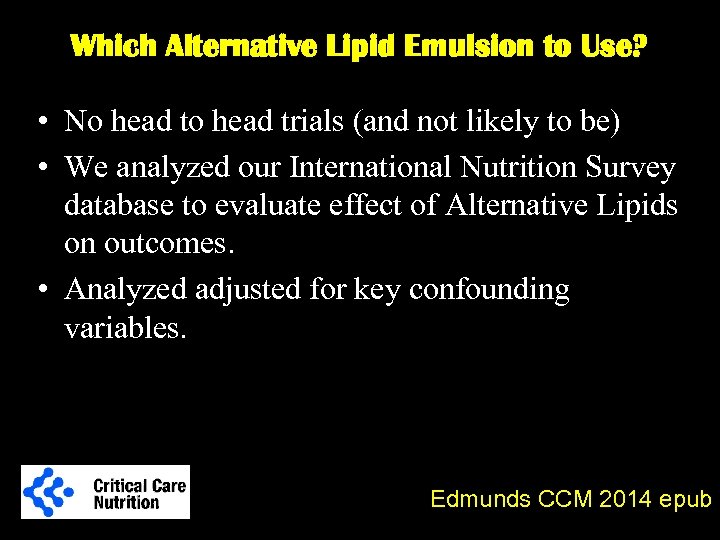 Which Alternative Lipid Emulsion to Use? • No head trials (and not likely to be) • We analyzed our International Nutrition Survey database to evaluate effect of Alternative Lipids on outcomes. • Analyzed adjusted for key confounding variables. Edmunds CCM 2014 epub
Which Alternative Lipid Emulsion to Use? • No head trials (and not likely to be) • We analyzed our International Nutrition Survey database to evaluate effect of Alternative Lipids on outcomes. • Analyzed adjusted for key confounding variables. Edmunds CCM 2014 epub
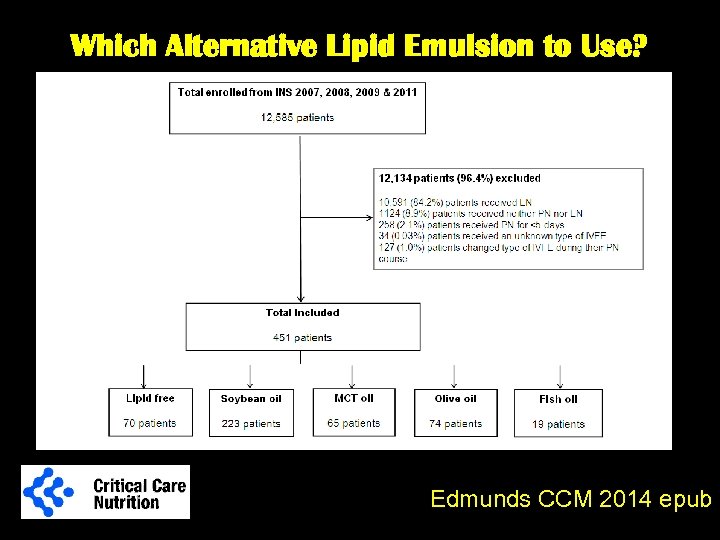 Which Alternative Lipid Emulsion to Use? Edmunds CCM 2014 epub
Which Alternative Lipid Emulsion to Use? Edmunds CCM 2014 epub
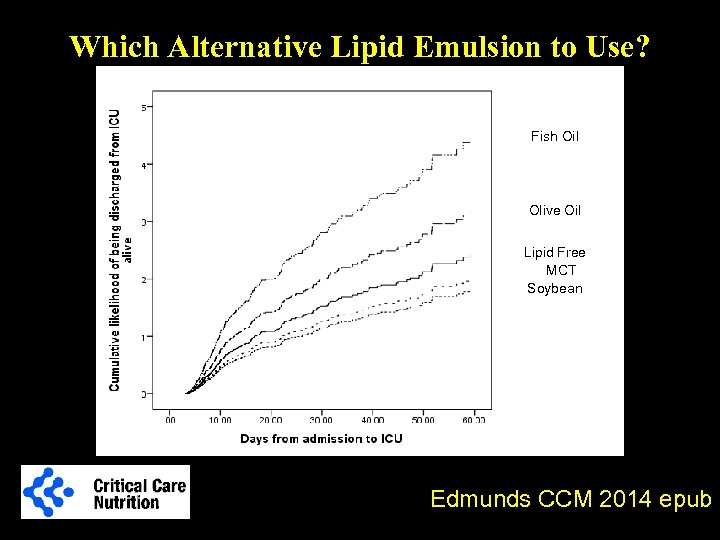 Which Alternative Lipid Emulsion to Use? Fish Oil Olive Oil Lipid Free MCT Soybean Edmunds CCM 2014 epub
Which Alternative Lipid Emulsion to Use? Fish Oil Olive Oil Lipid Free MCT Soybean Edmunds CCM 2014 epub
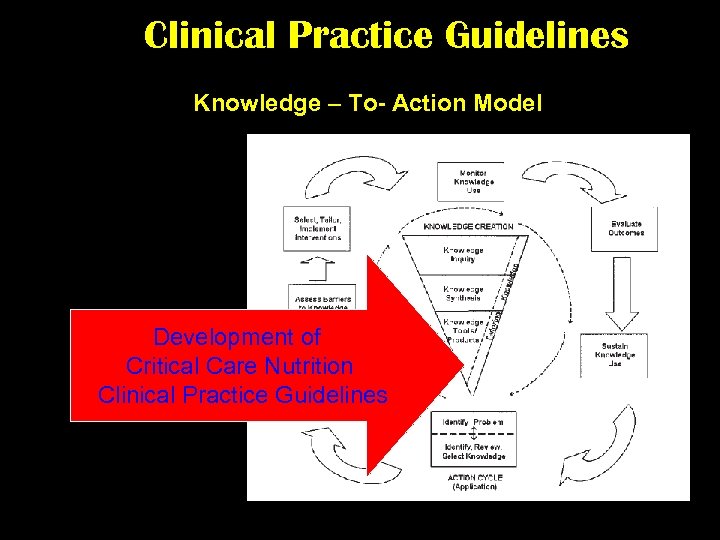 Clinical Practice Guidelines Knowledge – To- Action Model Development of Critical Care Nutrition Clinical Practice Guidelines
Clinical Practice Guidelines Knowledge – To- Action Model Development of Critical Care Nutrition Clinical Practice Guidelines
 Clinical Practice Guidelines for Nutrition § published initially in 2003 § updated 2005, 2007, 2009 and 2013
Clinical Practice Guidelines for Nutrition § published initially in 2003 § updated 2005, 2007, 2009 and 2013
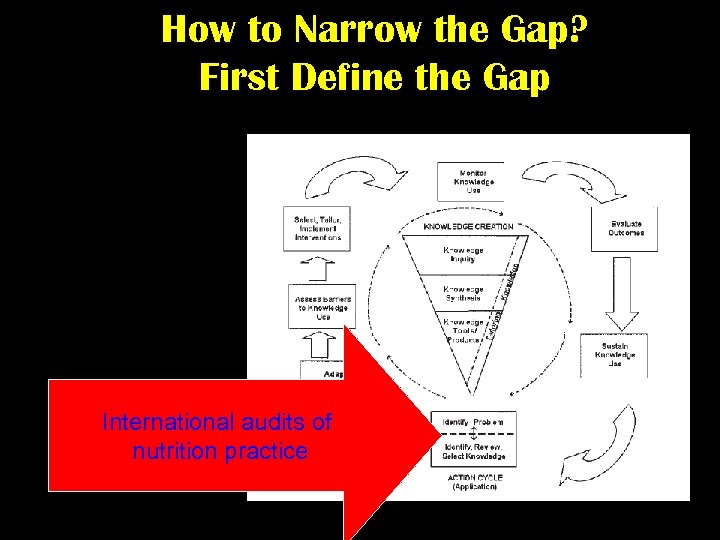 How to Narrow the Gap? First Define the Gap International audits of nutrition practice
How to Narrow the Gap? First Define the Gap International audits of nutrition practice
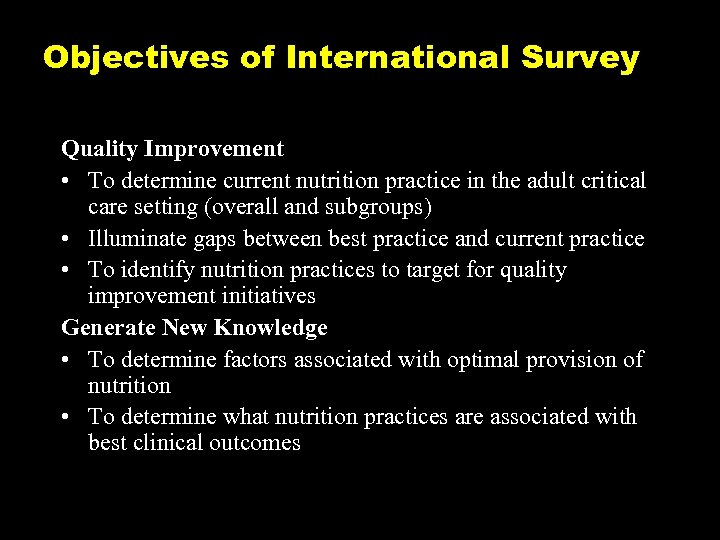 Objectives of International Survey Quality Improvement • To determine current nutrition practice in the adult critical care setting (overall and subgroups) • Illuminate gaps between best practice and current practice • To identify nutrition practices to target for quality improvement initiatives Generate New Knowledge • To determine factors associated with optimal provision of nutrition • To determine what nutrition practices are associated with best clinical outcomes
Objectives of International Survey Quality Improvement • To determine current nutrition practice in the adult critical care setting (overall and subgroups) • Illuminate gaps between best practice and current practice • To identify nutrition practices to target for quality improvement initiatives Generate New Knowledge • To determine factors associated with optimal provision of nutrition • To determine what nutrition practices are associated with best clinical outcomes
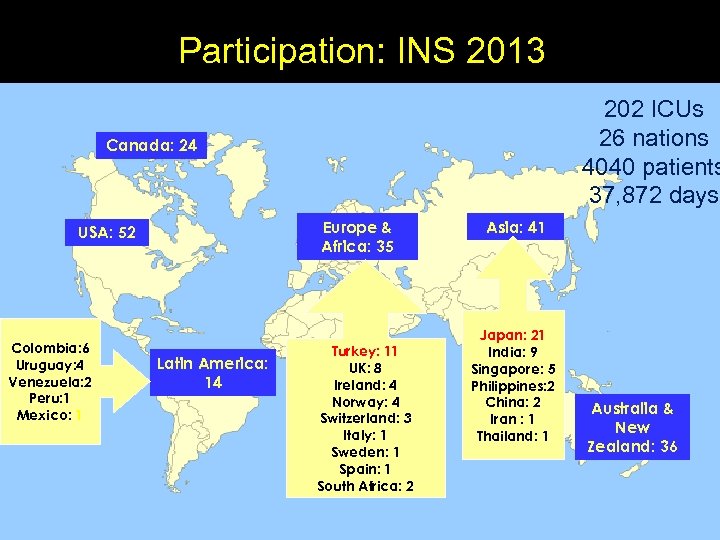 Participation: INS 2013 202 ICUs 26 nations 4040 patients 37, 872 days Canada: 24 Europe & Africa: 35 USA: 52 Colombia: 6 Uruguay: 4 Venezuela: 2 Peru: 1 Mexico: 1 Latin America: 14 Turkey: 11 UK: 8 Ireland: 4 Norway: 4 Switzerland: 3 Italy: 1 Sweden: 1 Spain: 1 South Africa: 2 Asia: 41 Japan: 21 India: 9 Singapore: 5 Philippines: 2 China: 2 Iran : 1 Thailand: 1 Australia & New Zealand: 36
Participation: INS 2013 202 ICUs 26 nations 4040 patients 37, 872 days Canada: 24 Europe & Africa: 35 USA: 52 Colombia: 6 Uruguay: 4 Venezuela: 2 Peru: 1 Mexico: 1 Latin America: 14 Turkey: 11 UK: 8 Ireland: 4 Norway: 4 Switzerland: 3 Italy: 1 Sweden: 1 Spain: 1 South Africa: 2 Asia: 41 Japan: 21 India: 9 Singapore: 5 Philippines: 2 China: 2 Iran : 1 Thailand: 1 Australia & New Zealand: 36
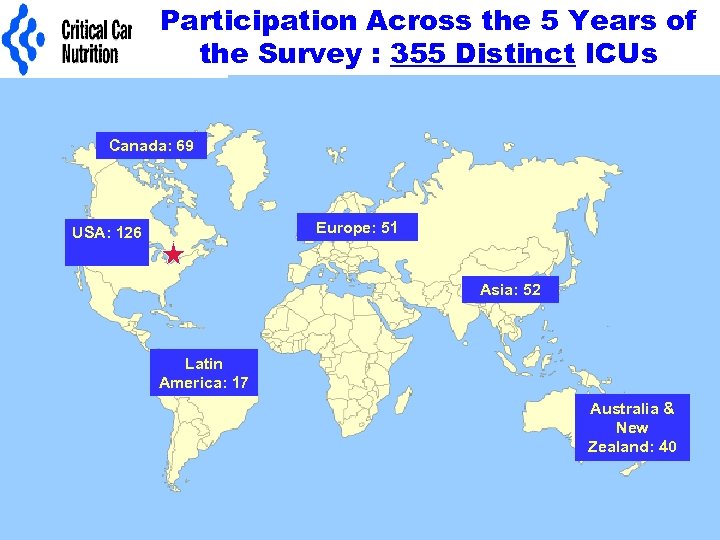 Participation Across the 5 Years of the Survey : 355 Distinct ICUs Canada: 69 Europe: 51 USA: 126 Asia: 52 Latin America: 17 Australia & New Zealand: 40
Participation Across the 5 Years of the Survey : 355 Distinct ICUs Canada: 69 Europe: 51 USA: 126 Asia: 52 Latin America: 17 Australia & New Zealand: 40
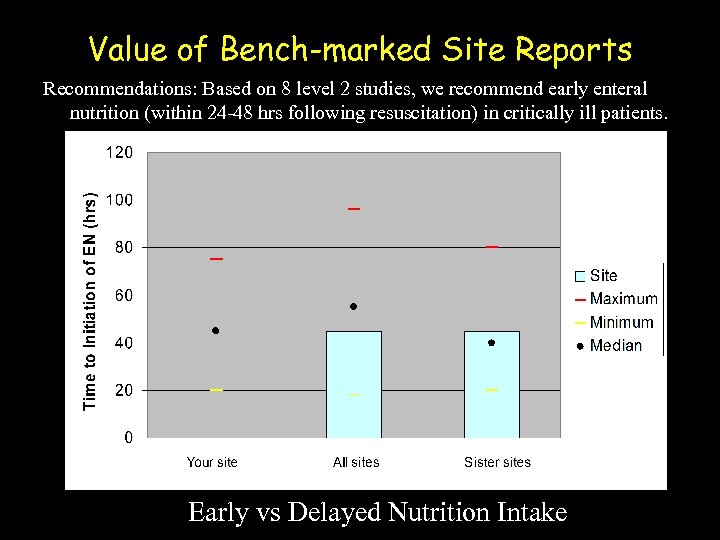 Value of Bench-marked Site Reports Recommendations: Based on 8 level 2 studies, we recommend early enteral nutrition (within 24 -48 hrs following resuscitation) in critically ill patients. Early vs Delayed Nutrition Intake
Value of Bench-marked Site Reports Recommendations: Based on 8 level 2 studies, we recommend early enteral nutrition (within 24 -48 hrs following resuscitation) in critically ill patients. Early vs Delayed Nutrition Intake
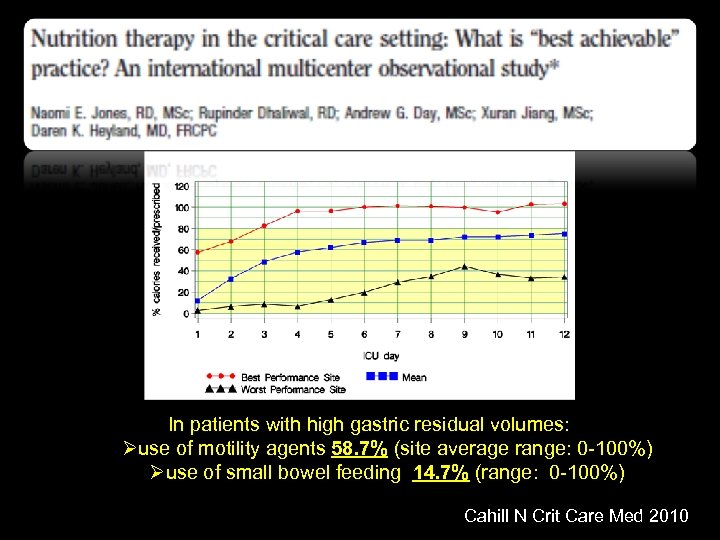 In patients with high gastric residual volumes: Øuse of motility agents 58. 7% (site average range: 0 -100%) Øuse of small bowel feeding 14. 7% (range: 0 -100%) Cahill N Crit Care Med 2010
In patients with high gastric residual volumes: Øuse of motility agents 58. 7% (site average range: 0 -100%) Øuse of small bowel feeding 14. 7% (range: 0 -100%) Cahill N Crit Care Med 2010
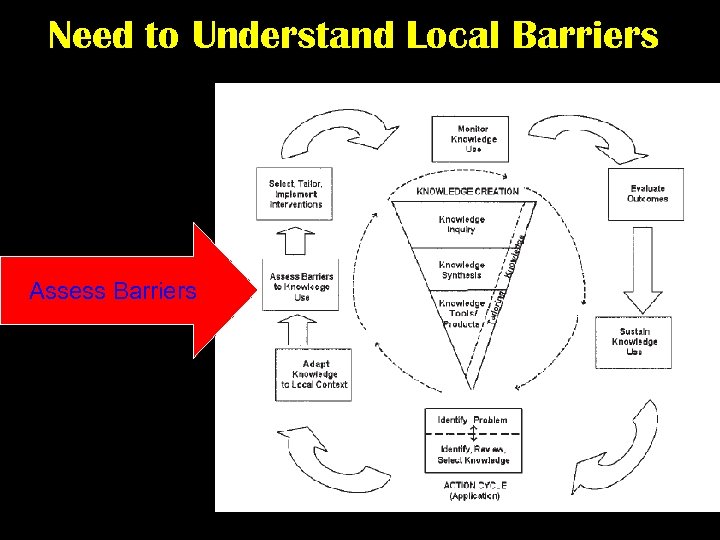 Need to Understand Local Barriers Assess Barriers
Need to Understand Local Barriers Assess Barriers
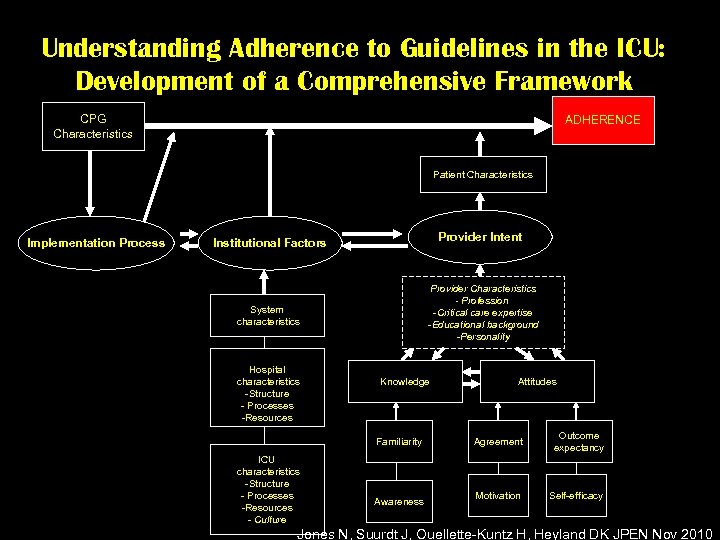 Understanding Adherence to Guidelines in the ICU: Development of a Comprehensive Framework CPG Characteristics ADHERENCE Patient Characteristics Implementation Process Provider Intent Institutional Factors Provider Characteristics - Profession -Critical care expertise -Educational background -Personality System characteristics Hospital characteristics -Structure - Processes -Resources Knowledge Familiarity ICU characteristics -Structure - Processes -Resources - Culture Awareness Attitudes Agreement Outcome expectancy Motivation Self-efficacy Jones N, Suurdt J, Ouellette-Kuntz H, Heyland DK JPEN Nov 2010
Understanding Adherence to Guidelines in the ICU: Development of a Comprehensive Framework CPG Characteristics ADHERENCE Patient Characteristics Implementation Process Provider Intent Institutional Factors Provider Characteristics - Profession -Critical care expertise -Educational background -Personality System characteristics Hospital characteristics -Structure - Processes -Resources Knowledge Familiarity ICU characteristics -Structure - Processes -Resources - Culture Awareness Attitudes Agreement Outcome expectancy Motivation Self-efficacy Jones N, Suurdt J, Ouellette-Kuntz H, Heyland DK JPEN Nov 2010
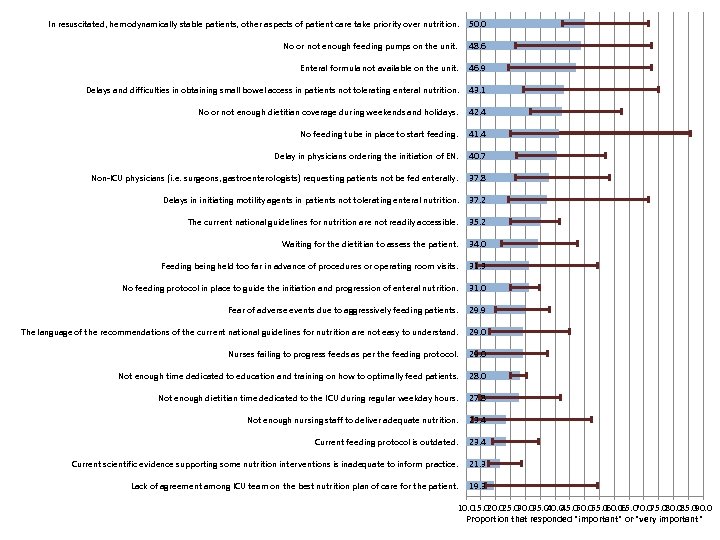 In resuscitated, hemodynamically stable patients, other aspects of patient care take priority over nutrition. 50. 0 No or not enough feeding pumps on the unit. 48. 6 Enteral formula not available on the unit. 46. 9 Delays and difficulties in obtaining small bowel access in patients not tolerating enteral nutrition. 43. 1 No or not enough dietitian coverage during weekends and holidays. 42. 4 No feeding tube in place to start feeding. 41. 4 Delay in physicians ordering the initiation of EN. 40. 7 Non-ICU physicians (i. e. surgeons, gastroenterologists) requesting patients not be fed enterally. 37. 8 Delays in initiating motility agents in patients not tolerating enteral nutrition. 37. 2 The current national guidelines for nutrition are not readily accessible. 35. 2 Waiting for the dietitian to assess the patient. 34. 0 Feeding being held too far in advance of procedures or operating room visits. 31. 3 No feeding protocol in place to guide the initiation and progression of enteral nutrition. 31. 0 Fear of adverse events due to aggressively feeding patients. 29. 9 The language of the recommendations of the current national guidelines for nutrition are not easy to understand. 29. 0 Nurses failing to progress feeds as per the feeding protocol. 29. 0 Not enough time dedicated to education and training on how to optimally feed patients. 28. 0 Not enough dietitian time dedicated to the ICU during regular weekday hours. 27. 8 Not enough nursing staff to deliver adequate nutrition. 23. 4 Current feeding protocol is outdated. 23. 4 Current scientific evidence supporting some nutrition interventions is inadequate to inform practice. 21. 3 Lack of agreement among ICU team on the best nutrition plan of care for the patient. 19. 3 10. 0 20. 0 30. 0 40. 0 50. 0 60. 0 70. 0 80. 0 90. 0 15. 0 25. 0 35. 0 45. 0 55. 0 65. 0 75. 0 85. 0 Proportion that responded "important" or "very important"
In resuscitated, hemodynamically stable patients, other aspects of patient care take priority over nutrition. 50. 0 No or not enough feeding pumps on the unit. 48. 6 Enteral formula not available on the unit. 46. 9 Delays and difficulties in obtaining small bowel access in patients not tolerating enteral nutrition. 43. 1 No or not enough dietitian coverage during weekends and holidays. 42. 4 No feeding tube in place to start feeding. 41. 4 Delay in physicians ordering the initiation of EN. 40. 7 Non-ICU physicians (i. e. surgeons, gastroenterologists) requesting patients not be fed enterally. 37. 8 Delays in initiating motility agents in patients not tolerating enteral nutrition. 37. 2 The current national guidelines for nutrition are not readily accessible. 35. 2 Waiting for the dietitian to assess the patient. 34. 0 Feeding being held too far in advance of procedures or operating room visits. 31. 3 No feeding protocol in place to guide the initiation and progression of enteral nutrition. 31. 0 Fear of adverse events due to aggressively feeding patients. 29. 9 The language of the recommendations of the current national guidelines for nutrition are not easy to understand. 29. 0 Nurses failing to progress feeds as per the feeding protocol. 29. 0 Not enough time dedicated to education and training on how to optimally feed patients. 28. 0 Not enough dietitian time dedicated to the ICU during regular weekday hours. 27. 8 Not enough nursing staff to deliver adequate nutrition. 23. 4 Current feeding protocol is outdated. 23. 4 Current scientific evidence supporting some nutrition interventions is inadequate to inform practice. 21. 3 Lack of agreement among ICU team on the best nutrition plan of care for the patient. 19. 3 10. 0 20. 0 30. 0 40. 0 50. 0 60. 0 70. 0 80. 0 90. 0 15. 0 25. 0 35. 0 45. 0 55. 0 65. 0 75. 0 85. 0 Proportion that responded "important" or "very important"
 Can we do better with our current feeding protocols? The same thinking that got you into this mess won’t get you out of it!
Can we do better with our current feeding protocols? The same thinking that got you into this mess won’t get you out of it!
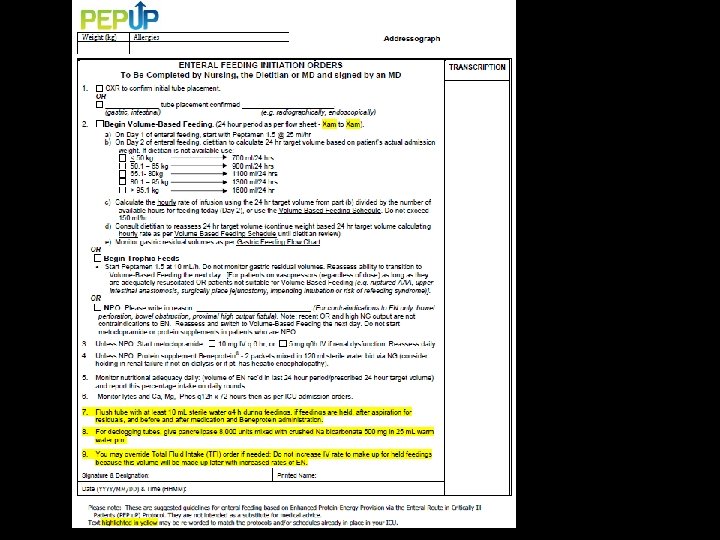
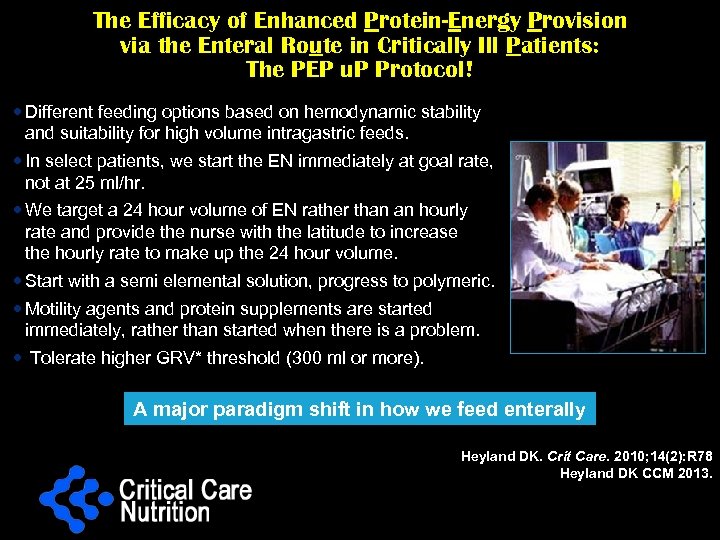 The Efficacy of Enhanced Protein-Energy Provision via the Enteral Route in Critically Ill Patients: The PEP u. P Protocol! Different feeding options based on hemodynamic stability and suitability for high volume intragastric feeds. In select patients, we start the EN immediately at goal rate, not at 25 ml/hr. We target a 24 hour volume of EN rather than an hourly rate and provide the nurse with the latitude to increase the hourly rate to make up the 24 hour volume. Start with a semi elemental solution, progress to polymeric. Motility agents and protein supplements are started immediately, rather than started when there is a problem. Tolerate higher GRV* threshold (300 ml or more). A major paradigm shift in how we feed enterally * GRV: gastric residual volume Heyland DK. Crit Care. 2010; 14(2): R 78 Heyland DK CCM 2013.
The Efficacy of Enhanced Protein-Energy Provision via the Enteral Route in Critically Ill Patients: The PEP u. P Protocol! Different feeding options based on hemodynamic stability and suitability for high volume intragastric feeds. In select patients, we start the EN immediately at goal rate, not at 25 ml/hr. We target a 24 hour volume of EN rather than an hourly rate and provide the nurse with the latitude to increase the hourly rate to make up the 24 hour volume. Start with a semi elemental solution, progress to polymeric. Motility agents and protein supplements are started immediately, rather than started when there is a problem. Tolerate higher GRV* threshold (300 ml or more). A major paradigm shift in how we feed enterally * GRV: gastric residual volume Heyland DK. Crit Care. 2010; 14(2): R 78 Heyland DK CCM 2013.
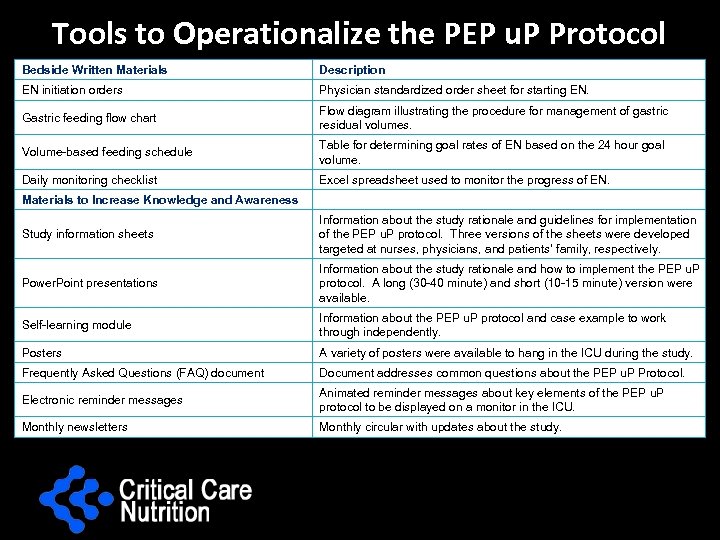 Tools to Operationalize the PEP u. P Protocol Bedside Written Materials Description EN initiation orders Physician standardized order sheet for starting EN. Gastric feeding flow chart Flow diagram illustrating the procedure for management of gastric residual volumes. Volume-based feeding schedule Table for determining goal rates of EN based on the 24 hour goal volume. Daily monitoring checklist Excel spreadsheet used to monitor the progress of EN. Materials to Increase Knowledge and Awareness Study information sheets Information about the study rationale and guidelines for implementation of the PEP u. P protocol. Three versions of the sheets were developed targeted at nurses, physicians, and patients’ family, respectively. Power. Point presentations Information about the study rationale and how to implement the PEP u. P protocol. A long (30 -40 minute) and short (10 -15 minute) version were available. Self-learning module Information about the PEP u. P protocol and case example to work through independently. Posters A variety of posters were available to hang in the ICU during the study. Frequently Asked Questions (FAQ) document Document addresses common questions about the PEP u. P Protocol. Electronic reminder messages Animated reminder messages about key elements of the PEP u. P protocol to be displayed on a monitor in the ICU. Monthly newsletters Monthly circular with updates about the study.
Tools to Operationalize the PEP u. P Protocol Bedside Written Materials Description EN initiation orders Physician standardized order sheet for starting EN. Gastric feeding flow chart Flow diagram illustrating the procedure for management of gastric residual volumes. Volume-based feeding schedule Table for determining goal rates of EN based on the 24 hour goal volume. Daily monitoring checklist Excel spreadsheet used to monitor the progress of EN. Materials to Increase Knowledge and Awareness Study information sheets Information about the study rationale and guidelines for implementation of the PEP u. P protocol. Three versions of the sheets were developed targeted at nurses, physicians, and patients’ family, respectively. Power. Point presentations Information about the study rationale and how to implement the PEP u. P protocol. A long (30 -40 minute) and short (10 -15 minute) version were available. Self-learning module Information about the PEP u. P protocol and case example to work through independently. Posters A variety of posters were available to hang in the ICU during the study. Frequently Asked Questions (FAQ) document Document addresses common questions about the PEP u. P Protocol. Electronic reminder messages Animated reminder messages about key elements of the PEP u. P protocol to be displayed on a monitor in the ICU. Monthly newsletters Monthly circular with updates about the study.
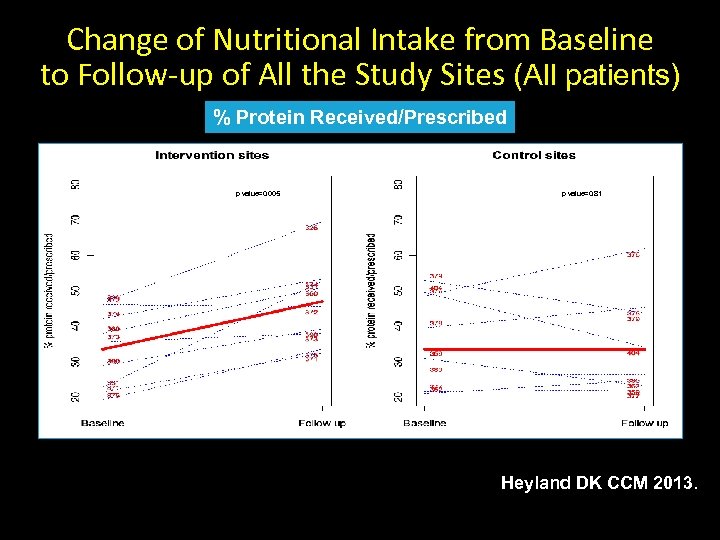 Change of Nutritional Intake from Baseline to Follow-up of All the Study Sites (All patients) % Protein Received/Prescribed p value=0. 005 p value=0. 81 Heyland DK CCM 2013.
Change of Nutritional Intake from Baseline to Follow-up of All the Study Sites (All patients) % Protein Received/Prescribed p value=0. 005 p value=0. 81 Heyland DK CCM 2013.
 Results of the Canadian PEP u. P Collaborative • 8 ICUs implemented PEP u. P protocol through Fall of 2012 -Spring 2013 • Compared to 16 ICUs (concurrent control group) • All evaluated their nutrition performance in the context of INS 2013 Heyland JPEN 2014 (in submission)
Results of the Canadian PEP u. P Collaborative • 8 ICUs implemented PEP u. P protocol through Fall of 2012 -Spring 2013 • Compared to 16 ICUs (concurrent control group) • All evaluated their nutrition performance in the context of INS 2013 Heyland JPEN 2014 (in submission)
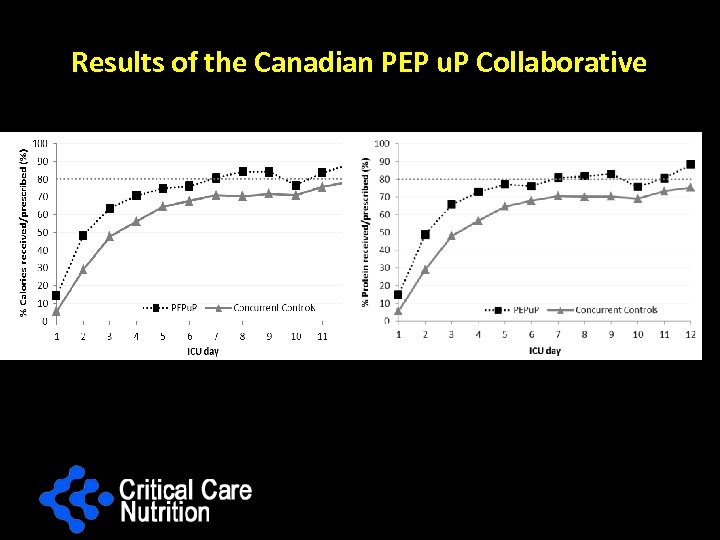 Results of the Canadian PEP u. P Collaborative
Results of the Canadian PEP u. P Collaborative
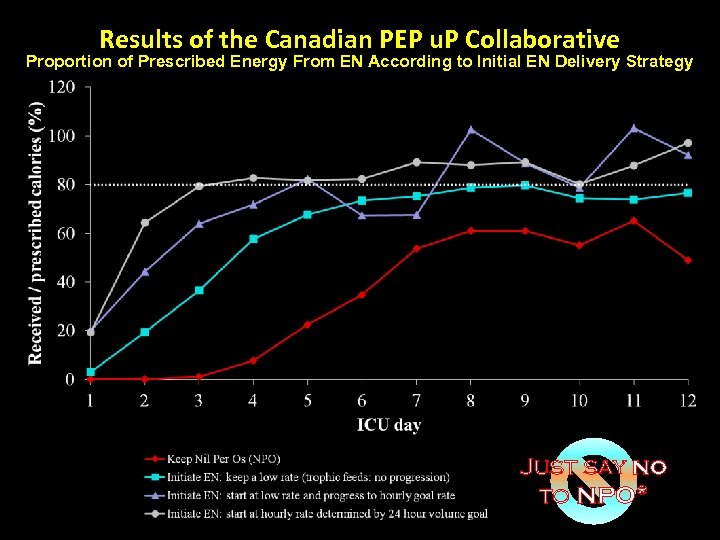 Results of the Canadian PEP u. P Collaborative Proportion of Prescribed Energy From EN According to Initial EN Delivery Strategy Just say no to NPO*
Results of the Canadian PEP u. P Collaborative Proportion of Prescribed Energy From EN According to Initial EN Delivery Strategy Just say no to NPO*
 New Collaborative: PEP UP US? • Want to add a slide here re: this?
New Collaborative: PEP UP US? • Want to add a slide here re: this?
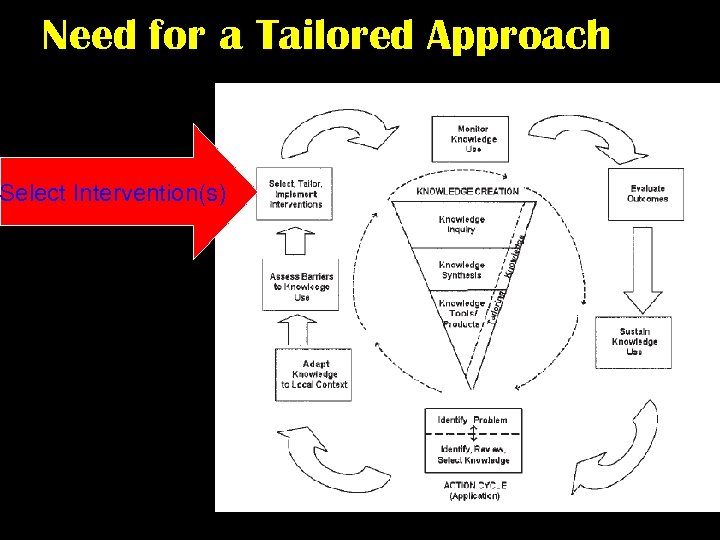 Need for a Tailored Approach Select Intervention(s)
Need for a Tailored Approach Select Intervention(s)
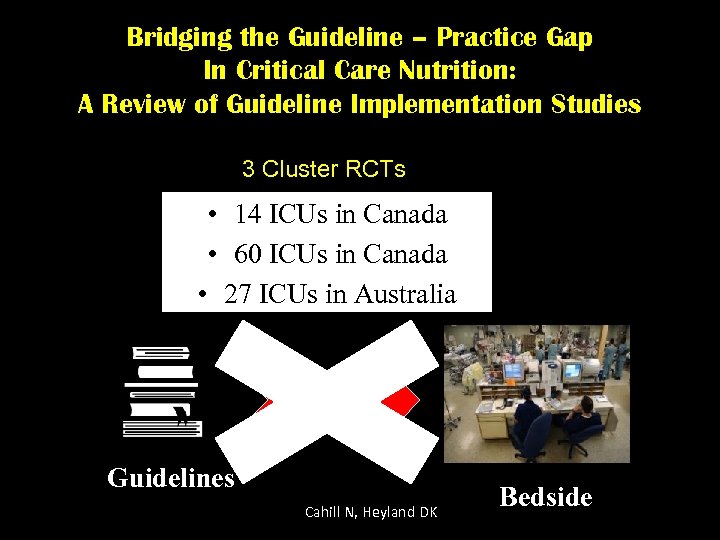 Bridging the Guideline – Practice Gap In Critical Care Nutrition: A Review of Guideline Implementation Studies 3 Cluster RCTs • 14 ICUs in Canada • 60 ICUs in Canada • 27 ICUs in Australia Guidelines Cahill N, Heyland DK Bedside
Bridging the Guideline – Practice Gap In Critical Care Nutrition: A Review of Guideline Implementation Studies 3 Cluster RCTs • 14 ICUs in Canada • 60 ICUs in Canada • 27 ICUs in Australia Guidelines Cahill N, Heyland DK Bedside
 Practice Changing Interventions ØProtocolize/automate care ØImprove organizational culture ØDevelop local opinion leaders ØAudit and feedback with bench-marked site reports ØAssess barriers and have interactive workshops with small group problem solving ØImplement strategies with rapid cycle change (PDSA) ØEducational reminders (checklists, manuals, posters, pocket cards) ØOne on one academic detailing
Practice Changing Interventions ØProtocolize/automate care ØImprove organizational culture ØDevelop local opinion leaders ØAudit and feedback with bench-marked site reports ØAssess barriers and have interactive workshops with small group problem solving ØImplement strategies with rapid cycle change (PDSA) ØEducational reminders (checklists, manuals, posters, pocket cards) ØOne on one academic detailing
 What works best at your site? (barriers and enablers will vary site to site) What is already working well at your site? (strengths and weakness are different across sites)
What works best at your site? (barriers and enablers will vary site to site) What is already working well at your site? (strengths and weakness are different across sites)
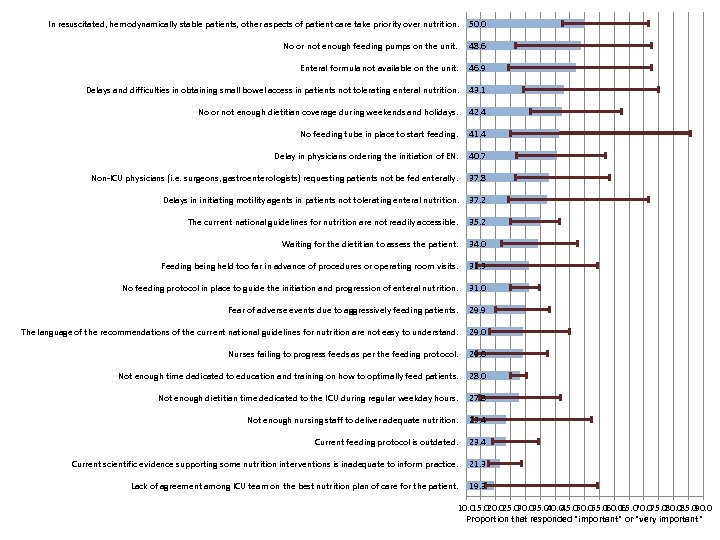 In resuscitated, hemodynamically stable patients, other aspects of patient care take priority over nutrition. 50. 0 No or not enough feeding pumps on the unit. 48. 6 Enteral formula not available on the unit. 46. 9 Delays and difficulties in obtaining small bowel access in patients not tolerating enteral nutrition. 43. 1 No or not enough dietitian coverage during weekends and holidays. 42. 4 No feeding tube in place to start feeding. 41. 4 Delay in physicians ordering the initiation of EN. 40. 7 Non-ICU physicians (i. e. surgeons, gastroenterologists) requesting patients not be fed enterally. 37. 8 Delays in initiating motility agents in patients not tolerating enteral nutrition. 37. 2 The current national guidelines for nutrition are not readily accessible. 35. 2 Waiting for the dietitian to assess the patient. 34. 0 Feeding being held too far in advance of procedures or operating room visits. 31. 3 No feeding protocol in place to guide the initiation and progression of enteral nutrition. 31. 0 Fear of adverse events due to aggressively feeding patients. 29. 9 The language of the recommendations of the current national guidelines for nutrition are not easy to understand. 29. 0 Nurses failing to progress feeds as per the feeding protocol. 29. 0 Not enough time dedicated to education and training on how to optimally feed patients. 28. 0 Not enough dietitian time dedicated to the ICU during regular weekday hours. 27. 8 Not enough nursing staff to deliver adequate nutrition. 23. 4 Current feeding protocol is outdated. 23. 4 Current scientific evidence supporting some nutrition interventions is inadequate to inform practice. 21. 3 Lack of agreement among ICU team on the best nutrition plan of care for the patient. 19. 3 10. 0 20. 0 30. 0 40. 0 50. 0 60. 0 70. 0 80. 0 90. 0 15. 0 25. 0 35. 0 45. 0 55. 0 65. 0 75. 0 85. 0 Proportion that responded "important" or "very important"
In resuscitated, hemodynamically stable patients, other aspects of patient care take priority over nutrition. 50. 0 No or not enough feeding pumps on the unit. 48. 6 Enteral formula not available on the unit. 46. 9 Delays and difficulties in obtaining small bowel access in patients not tolerating enteral nutrition. 43. 1 No or not enough dietitian coverage during weekends and holidays. 42. 4 No feeding tube in place to start feeding. 41. 4 Delay in physicians ordering the initiation of EN. 40. 7 Non-ICU physicians (i. e. surgeons, gastroenterologists) requesting patients not be fed enterally. 37. 8 Delays in initiating motility agents in patients not tolerating enteral nutrition. 37. 2 The current national guidelines for nutrition are not readily accessible. 35. 2 Waiting for the dietitian to assess the patient. 34. 0 Feeding being held too far in advance of procedures or operating room visits. 31. 3 No feeding protocol in place to guide the initiation and progression of enteral nutrition. 31. 0 Fear of adverse events due to aggressively feeding patients. 29. 9 The language of the recommendations of the current national guidelines for nutrition are not easy to understand. 29. 0 Nurses failing to progress feeds as per the feeding protocol. 29. 0 Not enough time dedicated to education and training on how to optimally feed patients. 28. 0 Not enough dietitian time dedicated to the ICU during regular weekday hours. 27. 8 Not enough nursing staff to deliver adequate nutrition. 23. 4 Current feeding protocol is outdated. 23. 4 Current scientific evidence supporting some nutrition interventions is inadequate to inform practice. 21. 3 Lack of agreement among ICU team on the best nutrition plan of care for the patient. 19. 3 10. 0 20. 0 30. 0 40. 0 50. 0 60. 0 70. 0 80. 0 90. 0 15. 0 25. 0 35. 0 45. 0 55. 0 65. 0 75. 0 85. 0 Proportion that responded "important" or "very important"
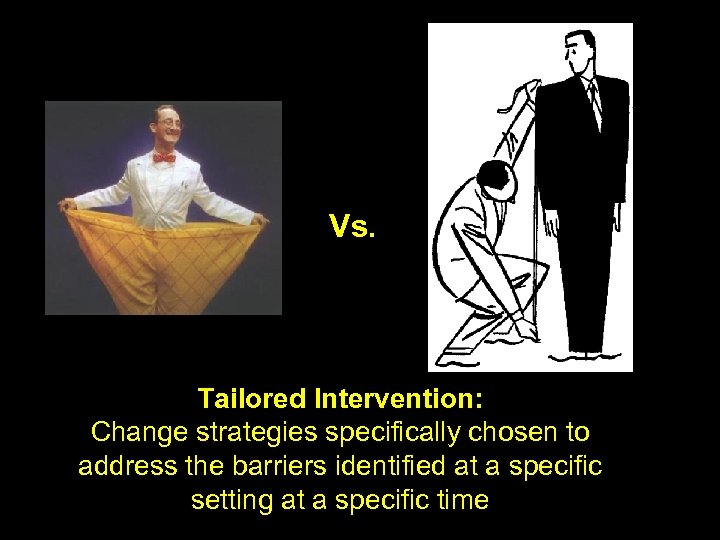 Vs. Tailored Intervention: Change strategies specifically chosen to address the barriers identified at a specific setting at a specific time
Vs. Tailored Intervention: Change strategies specifically chosen to address the barriers identified at a specific setting at a specific time
 Systematic Review of Tailored Interventions • • 26 studies of tailored interventions Pooled OR 1. 52 (95% CI 1. 27 -1. 82), p=0. 001 Variation in methodology None in clinical nutrition Baker et al Cochrane Database Syst Rev 2010
Systematic Review of Tailored Interventions • • 26 studies of tailored interventions Pooled OR 1. 52 (95% CI 1. 27 -1. 82), p=0. 001 Variation in methodology None in clinical nutrition Baker et al Cochrane Database Syst Rev 2010
 PERFormance Enhancement of the Canadian nutrition guidelines through a Tailored Implementation Strategy: The PERFECTIS Study Hypothesis Barriers are inversely related to nutrition performance and tailoring change strategies to overcome barriers to change will reduce the presence of these barriers and lead to improvements in nutrition practice.
PERFormance Enhancement of the Canadian nutrition guidelines through a Tailored Implementation Strategy: The PERFECTIS Study Hypothesis Barriers are inversely related to nutrition performance and tailoring change strategies to overcome barriers to change will reduce the presence of these barriers and lead to improvements in nutrition practice.
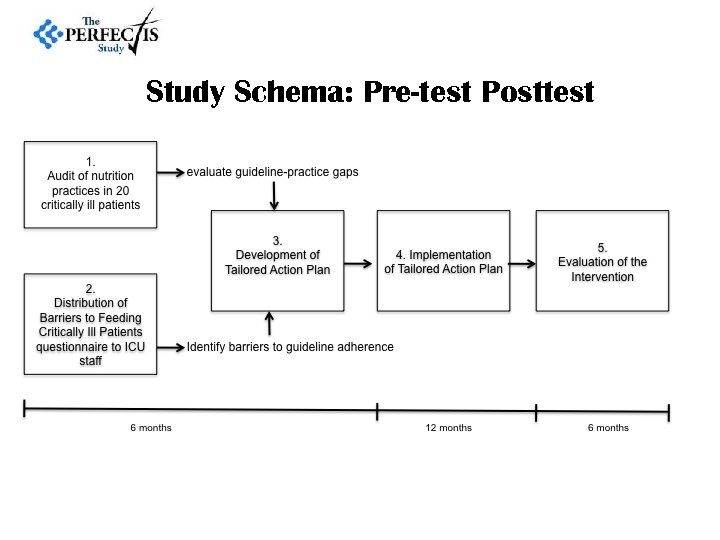 Study Schema: Pre-test Posttest
Study Schema: Pre-test Posttest
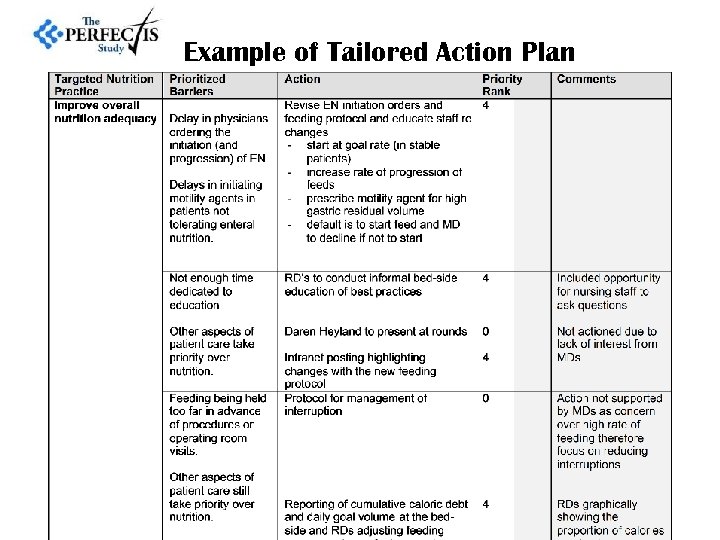 Example of Tailored Action Plan
Example of Tailored Action Plan
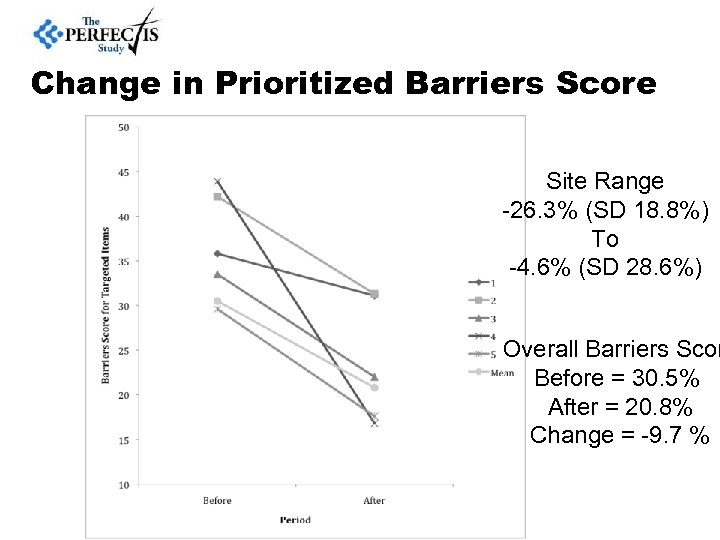 Change in Prioritized Barriers Score Site Range -26. 3% (SD 18. 8%) To -4. 6% (SD 28. 6%) Overall Barriers Scor Before = 30. 5% After = 20. 8% Change = -9. 7 %
Change in Prioritized Barriers Score Site Range -26. 3% (SD 18. 8%) To -4. 6% (SD 28. 6%) Overall Barriers Scor Before = 30. 5% After = 20. 8% Change = -9. 7 %
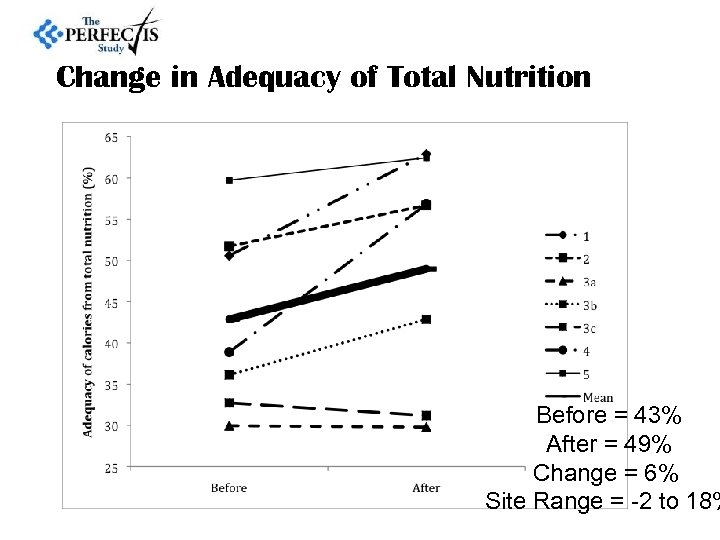 Change in Adequacy of Total Nutrition Before = 43% After = 49% Change = 6% Site Range = -2 to 18%
Change in Adequacy of Total Nutrition Before = 43% After = 49% Change = 6% Site Range = -2 to 18%
 OPTimal nutrition by Informing and Capacitating family members of best practices: The OPTICs feasibility study Investigators Andrea Marshall, RN, MN, Ph. D Daren Heyland, MD, FRCPC, MSc Naomi Cahill, RD, Ph. D candidate Rupinder Dhaliwal, RD
OPTimal nutrition by Informing and Capacitating family members of best practices: The OPTICs feasibility study Investigators Andrea Marshall, RN, MN, Ph. D Daren Heyland, MD, FRCPC, MSc Naomi Cahill, RD, Ph. D candidate Rupinder Dhaliwal, RD
 Gap exists: best practice & current practice • Evidence-based nutrition guidelines are inconsistently implemented • Large scale, multi-faceted interventions have failed to improve nutrition practices & have not improved nutritional adequacy for the critically ill • Engaging family members to act as advocates for nutrition may be a promising strategy to narrow the gap between best practice & current practice both in the ICU and post ICU
Gap exists: best practice & current practice • Evidence-based nutrition guidelines are inconsistently implemented • Large scale, multi-faceted interventions have failed to improve nutrition practices & have not improved nutritional adequacy for the critically ill • Engaging family members to act as advocates for nutrition may be a promising strategy to narrow the gap between best practice & current practice both in the ICU and post ICU
 Objectives: Definitive study Hypothesis Educating families about the importance of nutrition and having them advocate for better nutrition for their loved one in the ICU will result in better nutrition delivery during critical illness and in the recovery phase
Objectives: Definitive study Hypothesis Educating families about the importance of nutrition and having them advocate for better nutrition for their loved one in the ICU will result in better nutrition delivery during critical illness and in the recovery phase
 Evidence for Family Advocacy • Literature supports family-centered care 1, 2, 3, 4 • Families and ICU staff are very supportive of family involvement in patient care. Most patients are also favourable of family involvement in their care 1 1. Garrouste-Orgeas M, Willems V, Timsit JF, Diaw F, Brochon S, Vesin A, et al. Opinions of families, staff, and patients about family participation in care in intensive care units. J Crit Care. 2010; 25(4): 634 -40. 2. Cypress BS. The lived ICU experience of nurses, patients and family members: a phenomenological study with Merleau-Pontian perspective. Intensive Crit Care Nurs. 2011; 27(5): 273 -80 3. Kinsala EL. The Very Important Partner program: integrating family and friends into the health care experience. Prog Cardiovasc Nurs. 1999; 14(3): 103 -10. 4. Mitchell M, Chaboyer W, Burmeister E, Foster M. Positive effects of a nursing intervention on family-centered care in adult critical care. Am J Crit Care. 2009; 18(6): 543 -52; quiz 53.
Evidence for Family Advocacy • Literature supports family-centered care 1, 2, 3, 4 • Families and ICU staff are very supportive of family involvement in patient care. Most patients are also favourable of family involvement in their care 1 1. Garrouste-Orgeas M, Willems V, Timsit JF, Diaw F, Brochon S, Vesin A, et al. Opinions of families, staff, and patients about family participation in care in intensive care units. J Crit Care. 2010; 25(4): 634 -40. 2. Cypress BS. The lived ICU experience of nurses, patients and family members: a phenomenological study with Merleau-Pontian perspective. Intensive Crit Care Nurs. 2011; 27(5): 273 -80 3. Kinsala EL. The Very Important Partner program: integrating family and friends into the health care experience. Prog Cardiovasc Nurs. 1999; 14(3): 103 -10. 4. Mitchell M, Chaboyer W, Burmeister E, Foster M. Positive effects of a nursing intervention on family-centered care in adult critical care. Am J Crit Care. 2009; 18(6): 543 -52; quiz 53.
 Objectives: Feasibility Study Primary aim: Evaluate the feasibility and acceptability of an intervention designed to educate family members about the importance of adequate nutrition in ICU and during recovery from critical illness
Objectives: Feasibility Study Primary aim: Evaluate the feasibility and acceptability of an intervention designed to educate family members about the importance of adequate nutrition in ICU and during recovery from critical illness
 Intervention: Family education session & patient nutrition history Education session and booklet • Information about nutrition therapy • Nutrition therapy risks, side effects • Initiating oral feeds following EN or PN • How family members can be advocates for the best nutrition practices Nutrition history (Family member) • Weight loss history • Past diets, food intolerances/allergies, GI problems • Chewing/swallowing difficulties • Eating patterns • Food preferences
Intervention: Family education session & patient nutrition history Education session and booklet • Information about nutrition therapy • Nutrition therapy risks, side effects • Initiating oral feeds following EN or PN • How family members can be advocates for the best nutrition practices Nutrition history (Family member) • Weight loss history • Past diets, food intolerances/allergies, GI problems • Chewing/swallowing difficulties • Eating patterns • Food preferences
 Creating a Culture of Clinical Excellence in Critical Care Nutrition: The ‘Best of the Best’ Award Heyland JPEN 2010: in press
Creating a Culture of Clinical Excellence in Critical Care Nutrition: The ‘Best of the Best’ Award Heyland JPEN 2010: in press
 Recognition and Reward Recognition a powerful motivator of human performance
Recognition and Reward Recognition a powerful motivator of human performance
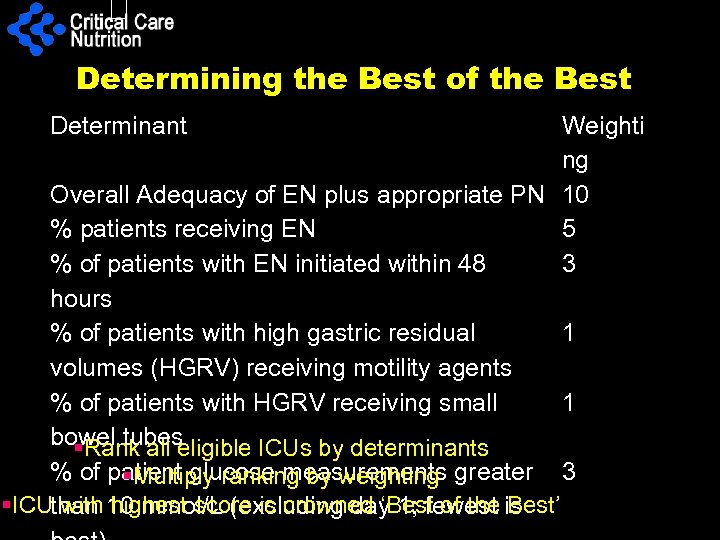 Determining the Best of the Best Determinant Weighti ng Overall Adequacy of EN plus appropriate PN 10 % patients receiving EN 5 % of patients with EN initiated within 48 3 hours % of patients with high gastric residual 1 volumes (HGRV) receiving motility agents % of patients with HGRV receiving small 1 bowel tubes §Rank all eligible ICUs by determinants % of patient glucose measurements greater 3 §Multiply ranking by weighting §ICU with highest score is crowned ‘Best of the Best’ than 10 mmol/L (excluding day 1; fewest is
Determining the Best of the Best Determinant Weighti ng Overall Adequacy of EN plus appropriate PN 10 % patients receiving EN 5 % of patients with EN initiated within 48 3 hours % of patients with high gastric residual 1 volumes (HGRV) receiving motility agents % of patients with HGRV receiving small 1 bowel tubes §Rank all eligible ICUs by determinants % of patient glucose measurements greater 3 §Multiply ranking by weighting §ICU with highest score is crowned ‘Best of the Best’ than 10 mmol/L (excluding day 1; fewest is
 2008 Best of the Best Top 3 ICUs 1. Department of Critical Care Medicine, Auckland City Hospital, Auckland, New Zealand 2. Kingston General Hospital, Kingston, Canada 3. Regional Hospital A. Cardarelli, Italy Top 3
2008 Best of the Best Top 3 ICUs 1. Department of Critical Care Medicine, Auckland City Hospital, Auckland, New Zealand 2. Kingston General Hospital, Kingston, Canada 3. Regional Hospital A. Cardarelli, Italy Top 3
 Best of the Best 2011 The Team at the Alfred Hospital ICU, Melbourne, Australia
Best of the Best 2011 The Team at the Alfred Hospital ICU, Melbourne, Australia
 2013 Best of the Best TOP 3 Sites 1. Kingston General Hospital, Kidd 2 ICU Canada 2. Hospital General de Medellín, luz Castro de Gutiérrez Unidad de cuidados intensivos , Colombia 3. The Ministry of Health Ankara, Numune Research and Training Hospital Turkey Top 3
2013 Best of the Best TOP 3 Sites 1. Kingston General Hospital, Kidd 2 ICU Canada 2. Hospital General de Medellín, luz Castro de Gutiérrez Unidad de cuidados intensivos , Colombia 3. The Ministry of Health Ankara, Numune Research and Training Hospital Turkey Top 3
 Kingston General Hospital
Kingston General Hospital
 Hospital General de Medellín Colombia
Hospital General de Medellín Colombia
 The Ministry of Health Ankara Turkey
The Ministry of Health Ankara Turkey
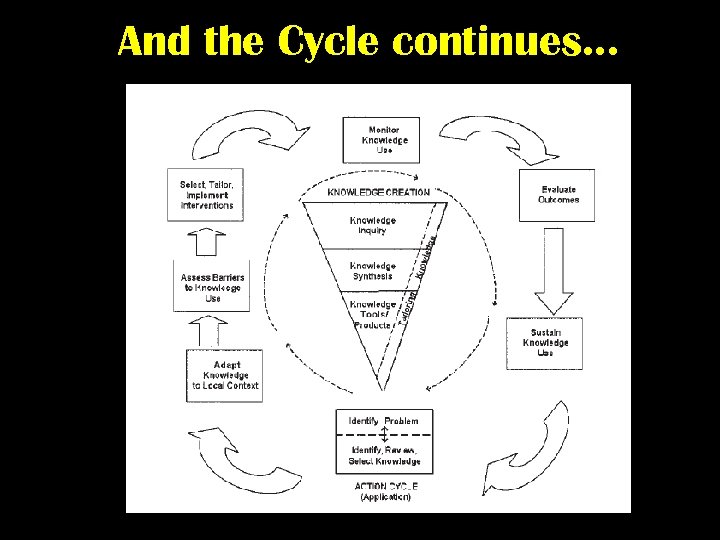 And the Cycle continues. . .
And the Cycle continues. . .
 More (and Earlier) is Better! If you feed them (better!) They will leave (sooner!)
More (and Earlier) is Better! If you feed them (better!) They will leave (sooner!)


