Craniocerebral Injury Jaroslav Plas Dept. of Neurosurgery, 1st

Craniocerebral Injury Jaroslav Plas Dept. of Neurosurgery, 1st Medical Faculty, Charles University Central Military Hospital Prague
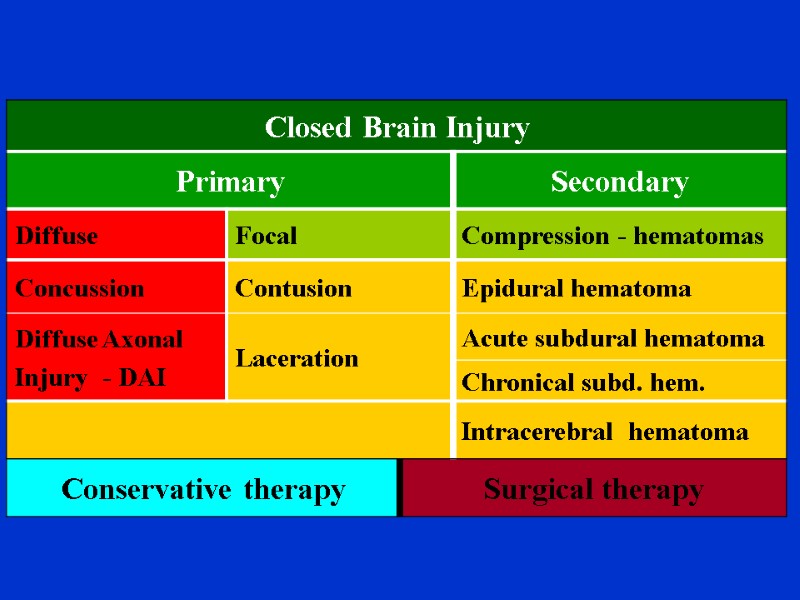
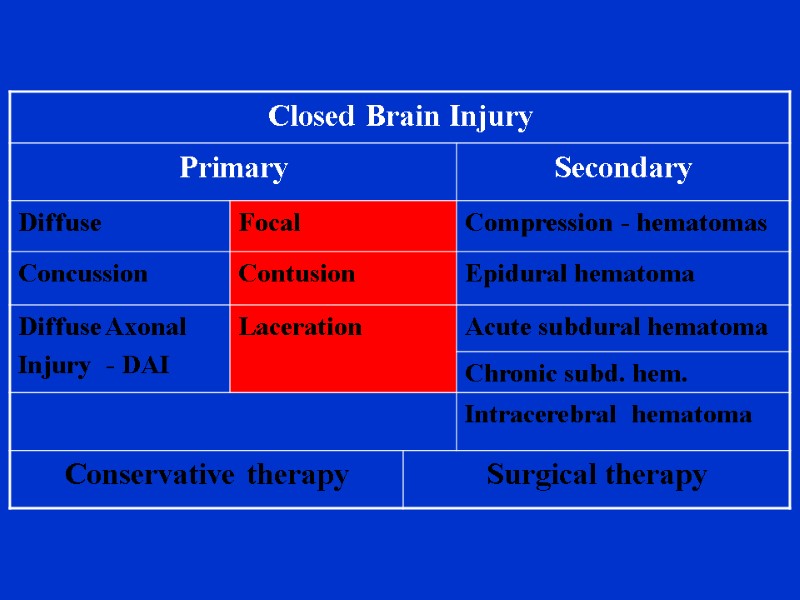
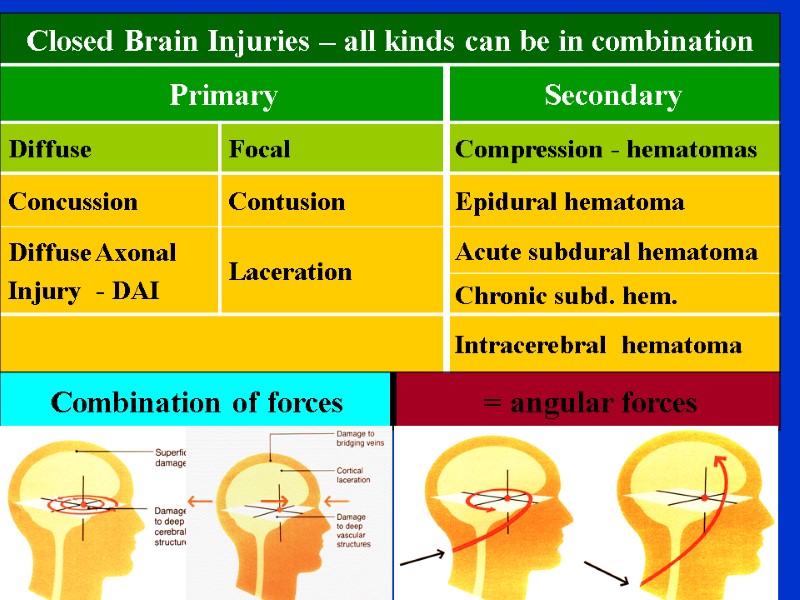
Brain trauma classification possibilities History: Petit, 1773 - concussion, contusion,compression Current concept is based on: consciousness level (disturbance: mild, medium, severe) II. CT finding (focal,diffuse) pathophysiology: (primary or secondary injury)
Classification of brain trauma based on consciousness level severe (GCS: 8 - 3) medium (GCS: 9 - 12) mild (GCS: 13,14) – „mild head injury“ Full consciousness = head trauma, no brain injury (GCS: 15) – „minor head injury
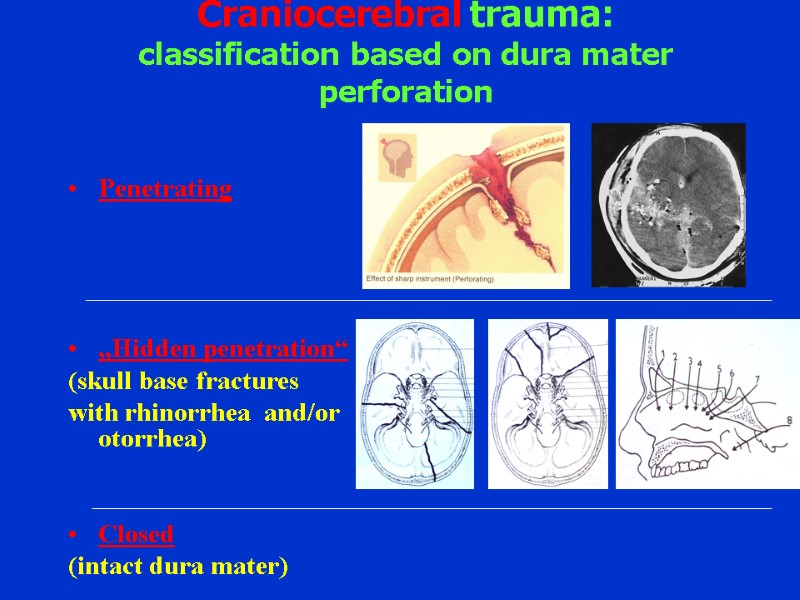
Craniocerebral trauma: classification based on dura mater perforation Penetrating „Hidden penetration“ (skull base fractures with rhinorrhea and/or otorrhea) Closed (intact dura mater)
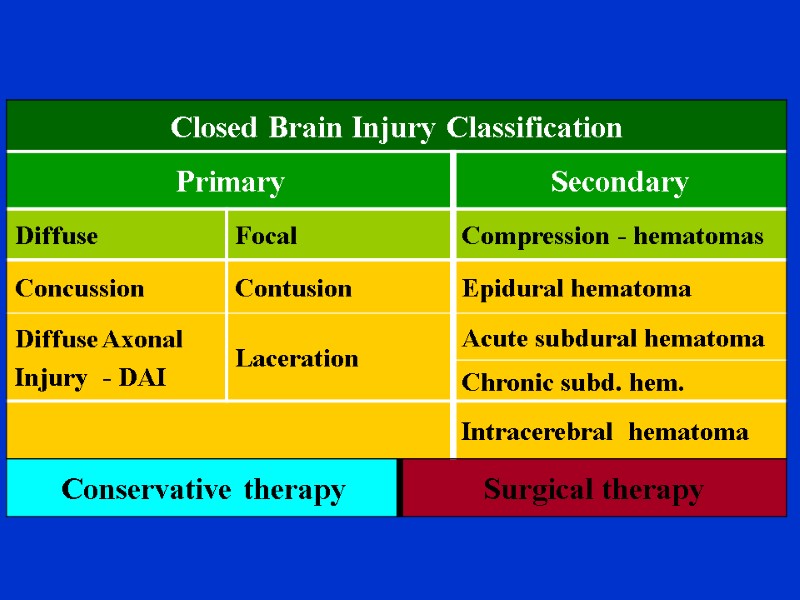
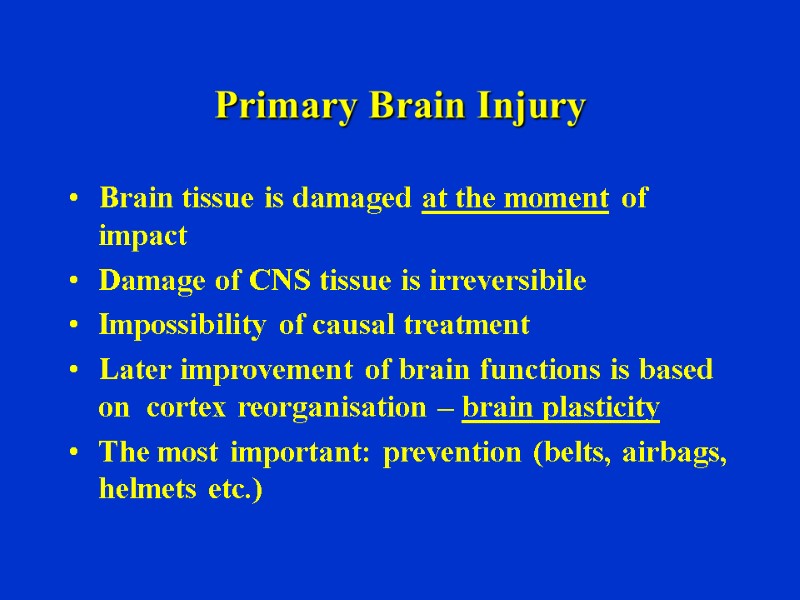
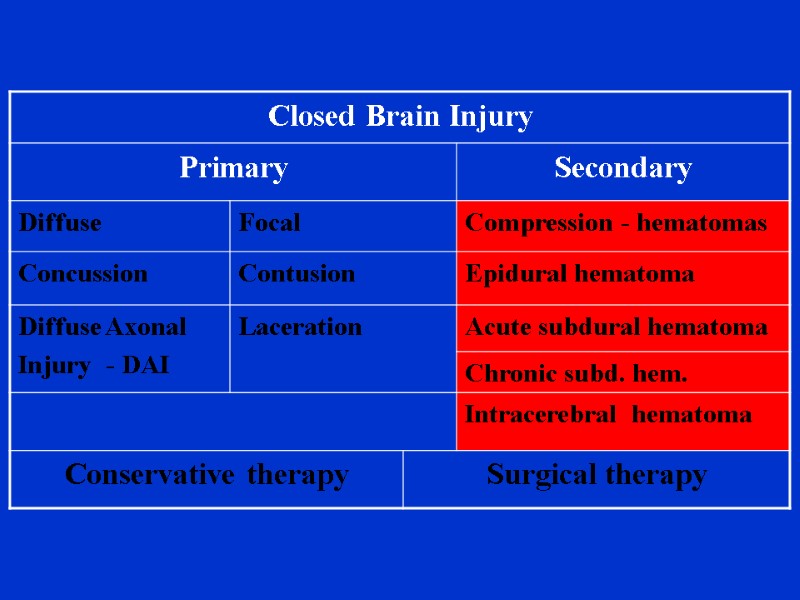
Primary Brain Injury Brain tissue is damaged at the moment of impact Damage of CNS tissue is irreversibile Impossibility of causal treatment Later improvement of brain functions is based on cortex reorganisation – brain plasticity The most important: prevention (belts, airbags, helmets etc.)
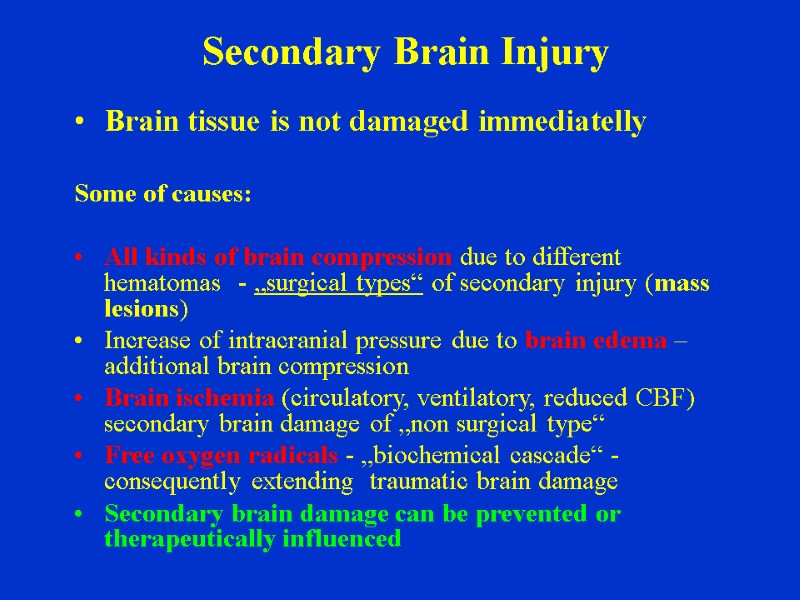
Secondary Brain Injury Brain tissue is not damaged immediatelly Some of causes: All kinds of brain compression due to different hematomas - „surgical types“ of secondary injury (mass lesions) Increase of intracranial pressure due to brain edema –additional brain compression Brain ischemia (circulatory, ventilatory, reduced CBF) secondary brain damage of „non surgical type“ Free oxygen radicals - „biochemical cascade“ -consequently extending traumatic brain damage Secondary brain damage can be prevented or therapeutically influenced
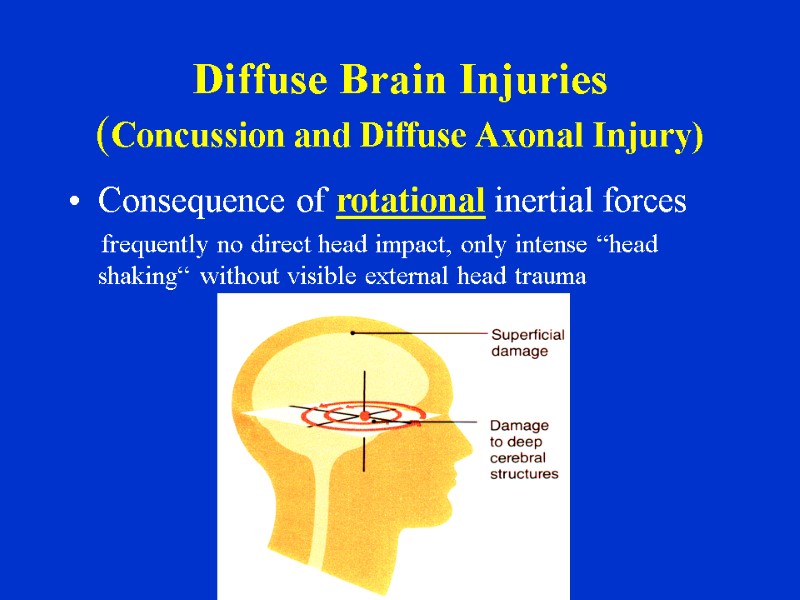
Diffuse Brain Injuries (Concussion and Diffuse Axonal Injury) Consequence of rotational inertial forces frequently no direct head impact, only intense “head shaking“ without visible external head trauma
Brain Concussion Clinical Characteristics Main signs: Consciousness impairment (both qualitative = confussion, or quantitative = uncousniousness). Short lasting (minutes) Amnesia (retrograde, anterograde) – frequently the only sign if lack of objective information on admission Other early signs: nausea, vomiting, dizziness, hypersensitivity to light and/or sounds, decrease of concentration, depression
Brain Concussion Pathofysiological principles 1) Temporary depolarisation of huge neurons population without anatomical lesion of brain (in low grade concussion) 2) Microsopic anatomical brain lesions (in higher grades of concussion) = risk of cummulative effect if repeated! Concussion is not always only innocent temporary brain function deterioration „Post-concussion“ syndrome can persists limited time due to above mentioned minimal anatomical damage after high grade concussion Outcome: no permanent neurologial deficit if not repeated
Late Signs of Concussion (post concussion syndrome) Headaches Concentration and alertness problems Memory problems Easily tired Irritability, worsened tolerance of frustration Tinnitus Anxiety Sleep problems
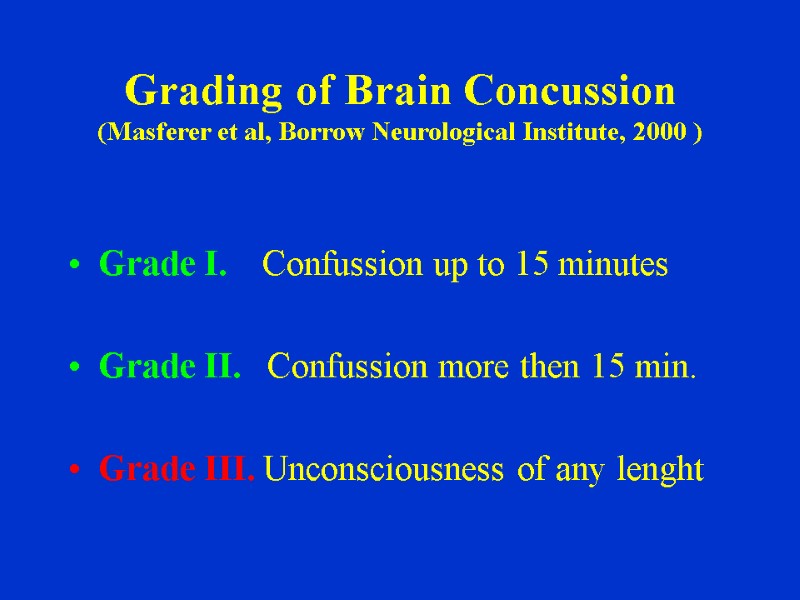
Grading of Brain Concussion (Masferer et al, Borrow Neurological Institute, 2000 ) Grade I. Confussion up to 15 minutes Grade II. Confussion more then 15 min. Grade III. Unconsciousness of any lenght
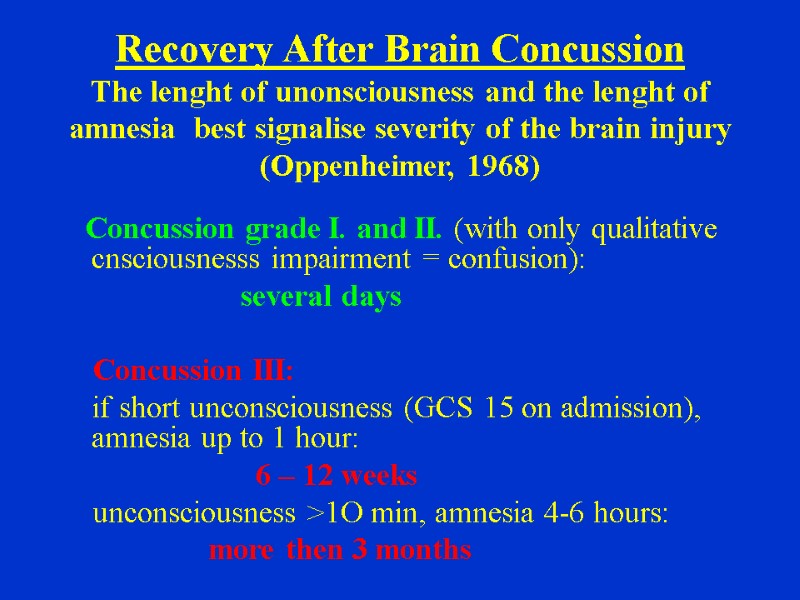
Recovery After Brain Concussion The lenght of unonsciousness and the lenght of amnesia best signalise severity of the brain injury (Oppenheimer, 1968) Concussion grade I. and II. (with only qualitative cnsciousnesss impairment = confusion): several days Concussion III: if short unconsciousness (GCS 15 on admission), amnesia up to 1 hour: 6 – 12 weeks unconsciousness >1O min, amnesia 4-6 hours: more then 3 months
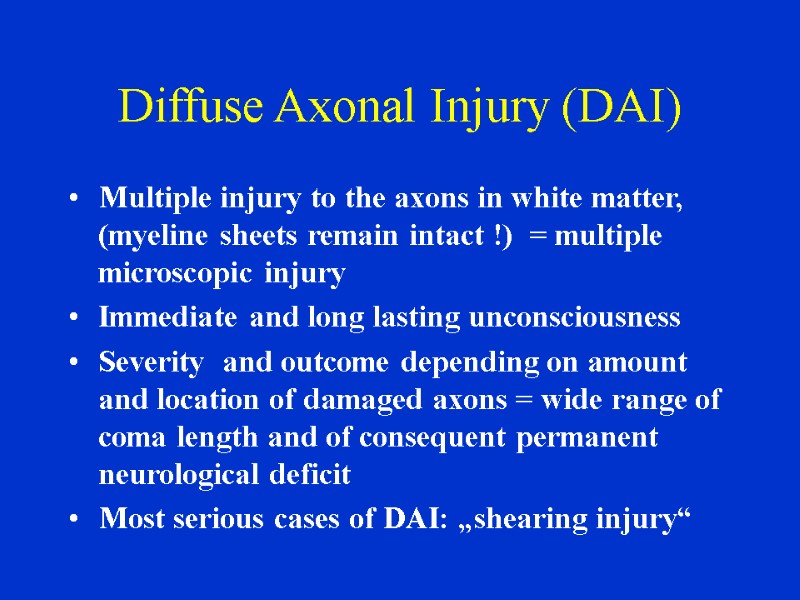
Diffuse Axonal Injury (DAI) Multiple injury to the axons in white matter, (myeline sheets remain intact !) = multiple microscopic injury Immediate and long lasting unconsciousness Severity and outcome depending on amount and location of damaged axons = wide range of coma length and of consequent permanent neurological deficit Most serious cases of DAI: „shearing injury“
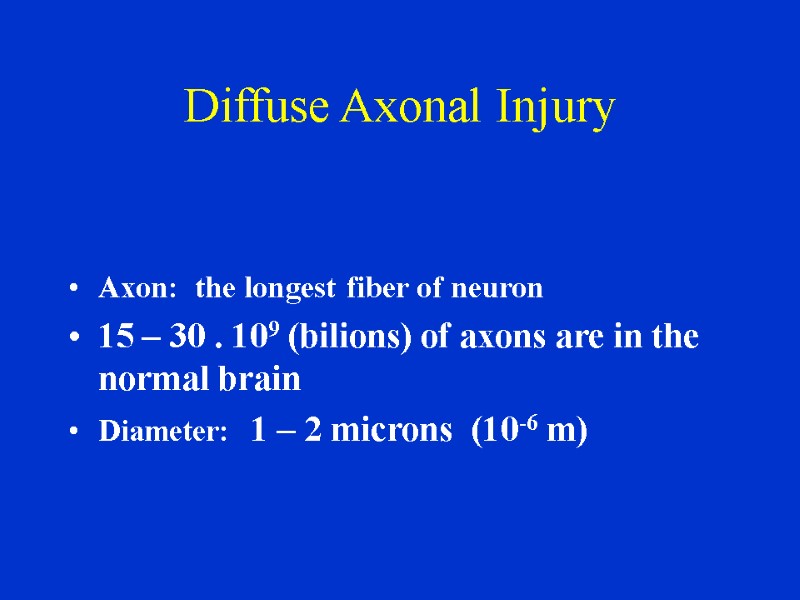
Diffuse Axonal Injury Axon: the longest fiber of neuron 15 – 30 . 109 (bilions) of axons are in the normal brain Diameter: 1 – 2 microns (10-6 m)
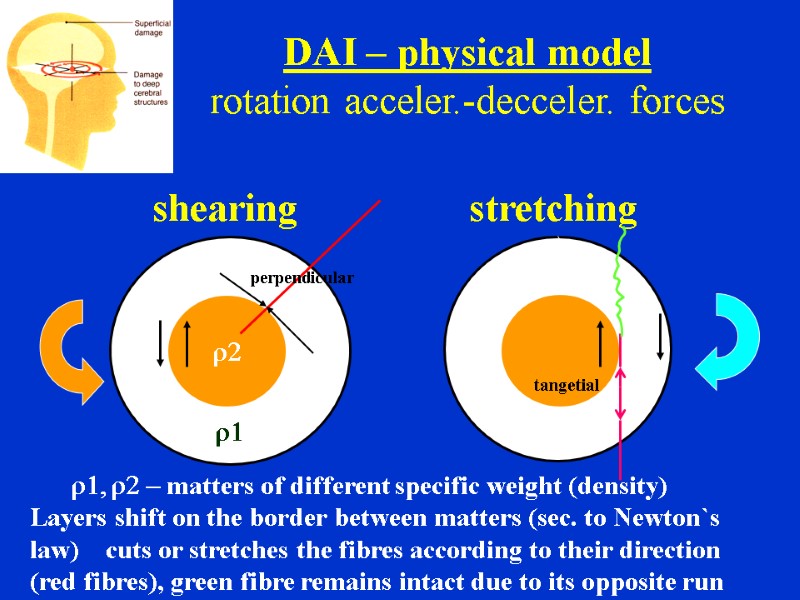
shearing stretching r1 r2 DAI – physical model rotation acceler.-decceler. forces r1, r2 - matters of different specific weight (density) Layers shift on the border between matters (sec. to Newton`s law) cuts or stretches the fibres according to their direction (red fibres), green fibre remains intact due to its opposite run perpendicular tangetial
Relation of Concussion and DAI There is no sharp borderline between high grade concussion and diffuse axonal injury Both these diffuse injury types represent continuous line from grade I. concussion (with only functional - not structural - changes) to the worst type of direct axonal damage in shearing injury
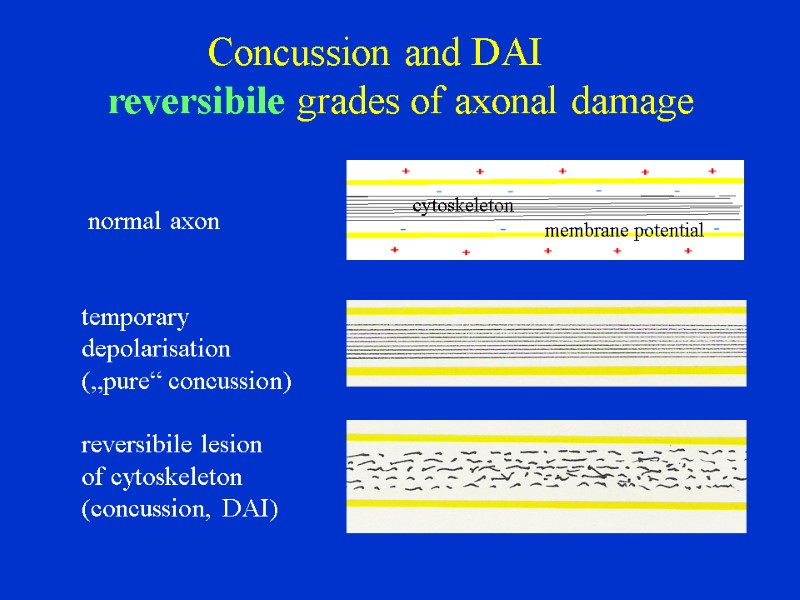
normal axon temporary depolarisation („pure“ concussion) reversibile lesion of cytoskeleton (concussion, DAI) Concussion and DAI reversibile grades of axonal damage cytoskeleton membrane potential
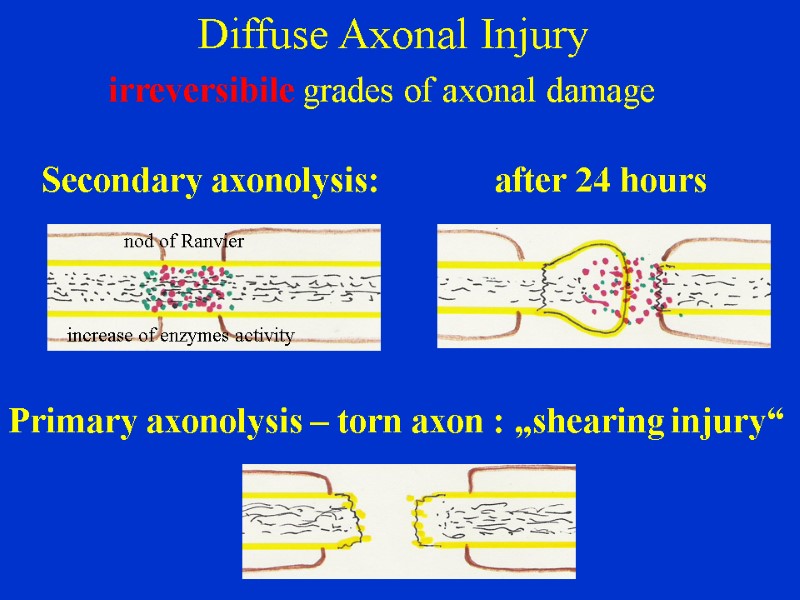
Diffuse Axonal Injury irreversibile grades of axonal damage Secondary axonolysis: after 24 hours Primary axonolysis – torn axon : „shearing injury“ nod of Ranvier increase of enzymes activity
DAI – CT findings Multiple microscopic injury – DAI itself is invisible on CT immediatelly In most serious cases of shearing injury: small clots in white matter, c.callosum, pons = associated small vessels injury = poor prognosis Diffuse brain swelling is frequently acompanying DAI Brain atrophy after appropriate time (2-3 weeks)
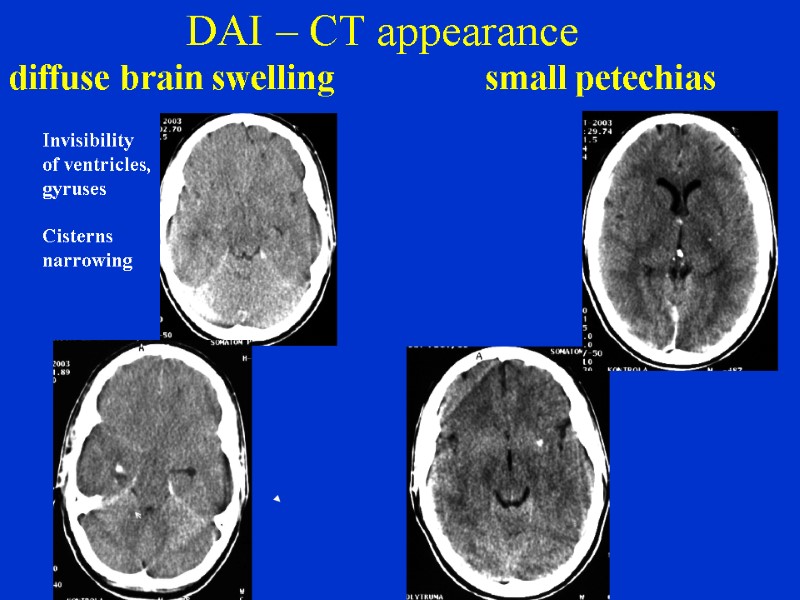
DAI – CT appearance diffuse brain swelling small petechias Invisibility of ventricles, gyruses Cisterns narrowing
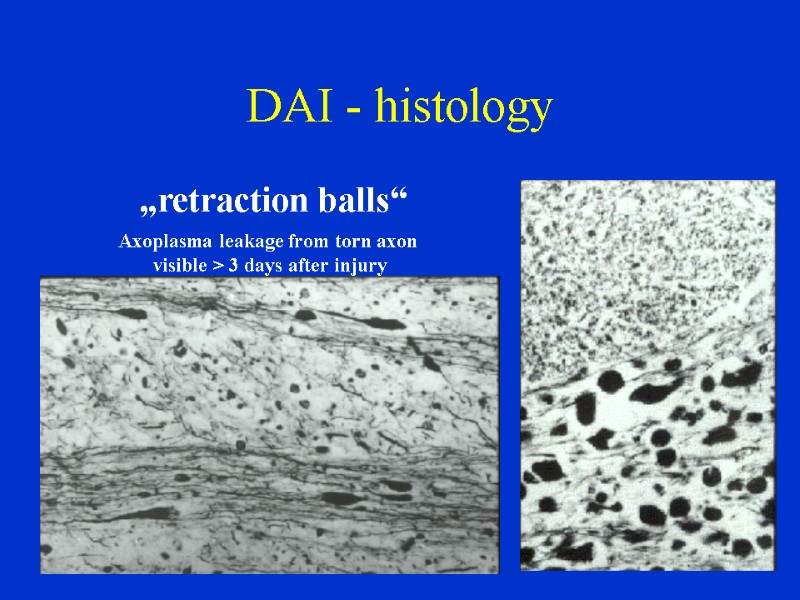
DAI - histology „retraction balls“ Axoplasma leakage from torn axon visible > 3 days after injury
DAI – treatment and outcome No specific treatment: - ICU, art. ventilation - reduction of ICP if raised due to diffuse brain swelling (mannitol, furosemide, barbiturates..) Outcome possibilities: wide spectrum *No focal neurological deficit, good outcome *Focal deficit of different grade and type due to amount and location of damaged axons *Persistent vegetative state *Death
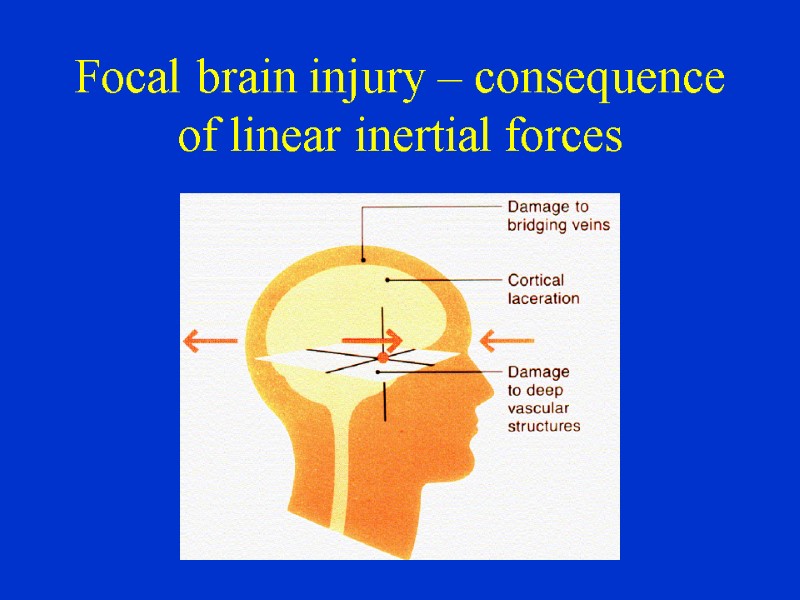
Focal brain injury – consequence of linear inertial forces
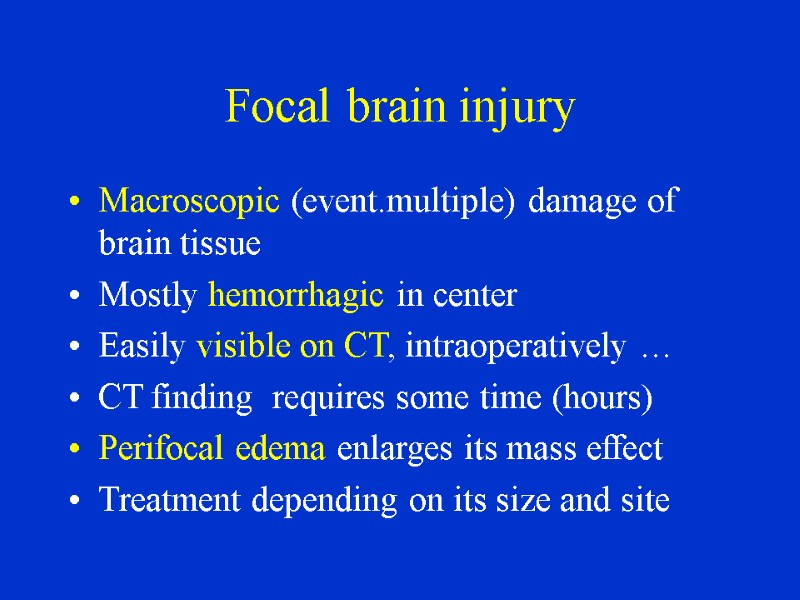
Focal brain injury Macroscopic (event.multiple) damage of brain tissue Mostly hemorrhagic in center Easily visible on CT, intraoperatively … CT finding requires some time (hours) Perifocal edema enlarges its mass effect Treatment depending on its size and site
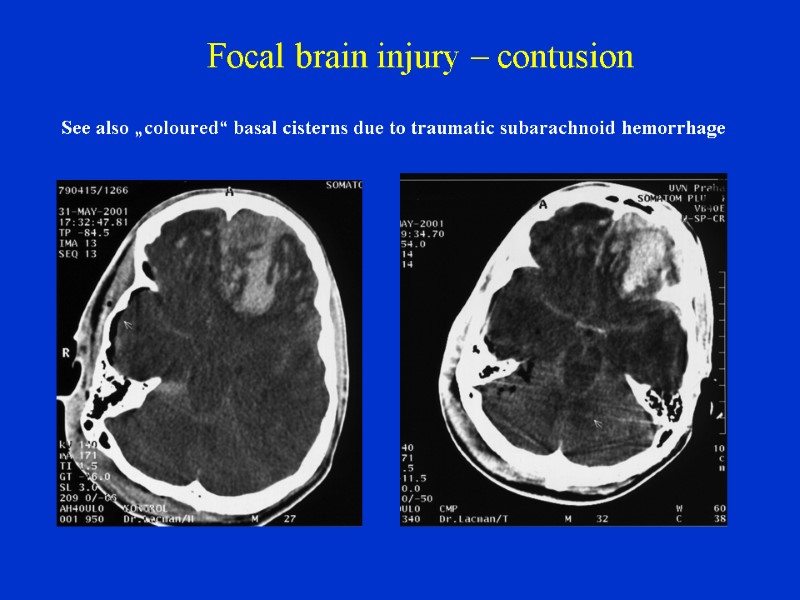
Focal brain injury – contusion See also „coloured“ basal cisterns due to traumatic subarachnoid hemorrhage
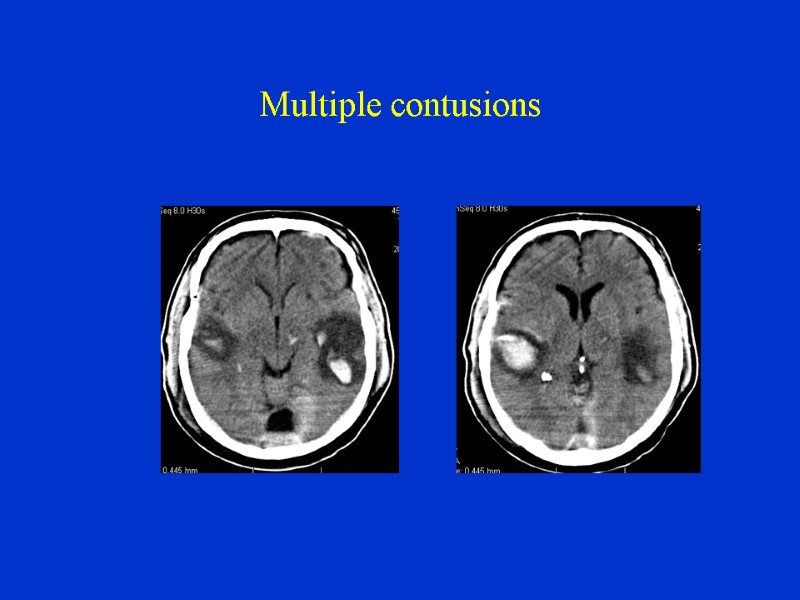
Multiple contusions
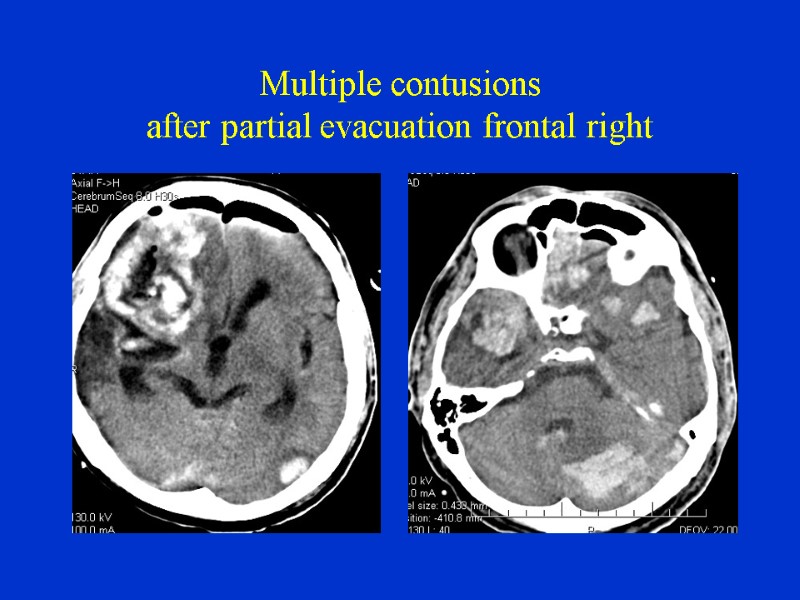
Multiple contusions after partial evacuation frontal right
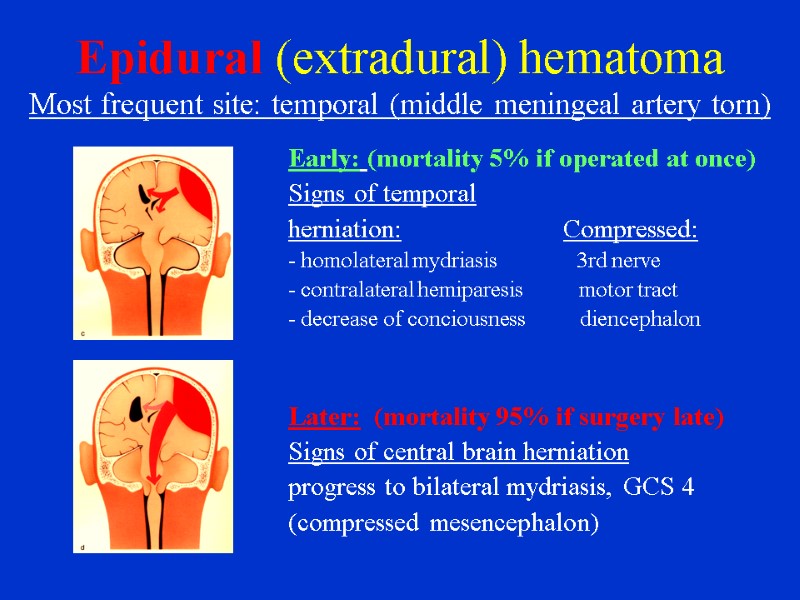
Epidural (extradural) hematoma Most frequent site: temporal (middle meningeal artery torn) Early: (mortality 5% if operated at once) Signs of temporal herniation: Compressed: - homolateral mydriasis 3rd nerve - contralateral hemiparesis motor tract - decrease of conciousness diencephalon Later: (mortality 95% if surgery late) Signs of central brain herniation progress to bilateral mydriasis, GCS 4 (compressed mesencephalon)
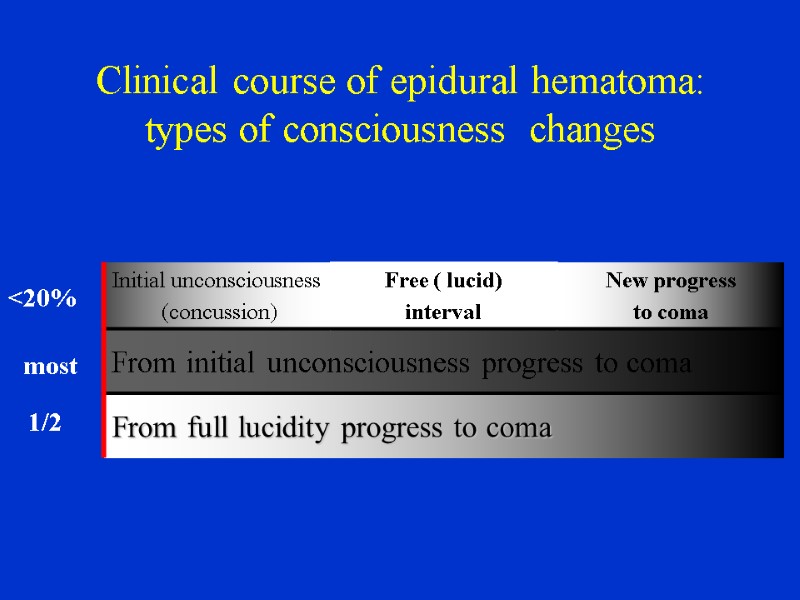
Clinical course of epidural hematoma: types of consciousness changes <20% 1/2 most
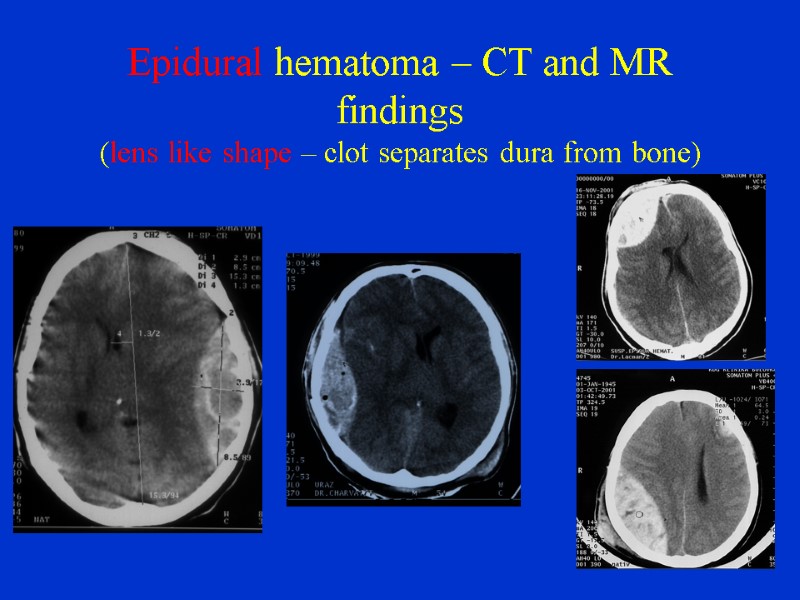
Epidural hematoma – CT and MR findings (lens like shape – clot separates dura from bone)
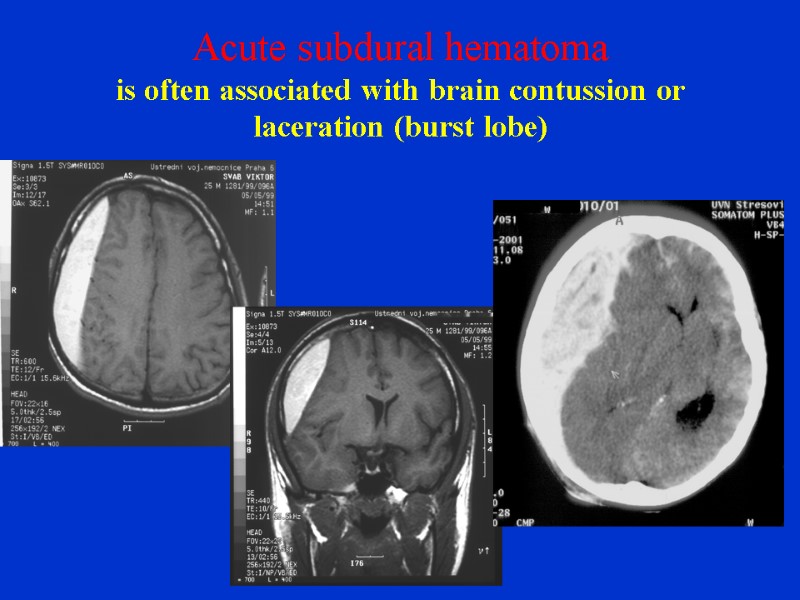
Acute subdural hematoma is often associated with brain contussion or laceration (burst lobe)
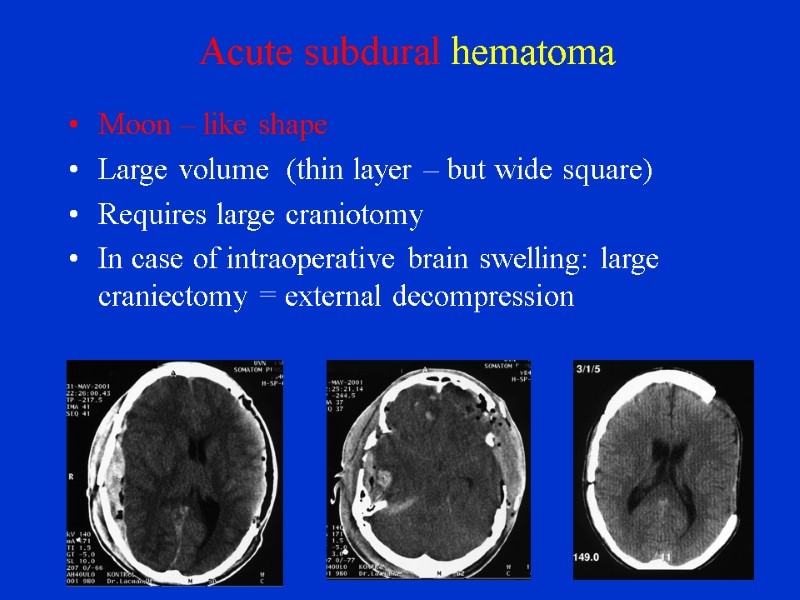
Acute subdural hematoma Moon – like shape Large volume (thin layer – but wide square) Requires large craniotomy In case of intraoperative brain swelling: large craniectomy = external decompression
Acute subdural hematoma clinical appearence More severe condition from the beginning (in comparison with extradural bleeding) Usually without lucid interval, immediate unconsciousness progressing to coma Signs of temporal brain herniation: homolateral mydriasis, contralateral hemiparesis, coma Worse outcome due to association with primary brain injury and rapid ICP elevation
Chronic subdural hematoma Patients with brain atrophy Source of bleeding: bridging veins, coagulation disorders No unconsciousness - minor trauma („forgotten head hit“), no immediate signs Enlargement due to repeated bleeding from capsule vessels Long latency of symptoms: > 20 days (weeks, month) Signs: dementia, paresis, dysfasia, drowsiness Treatment: burr hole, evacuation, lavage, drainage
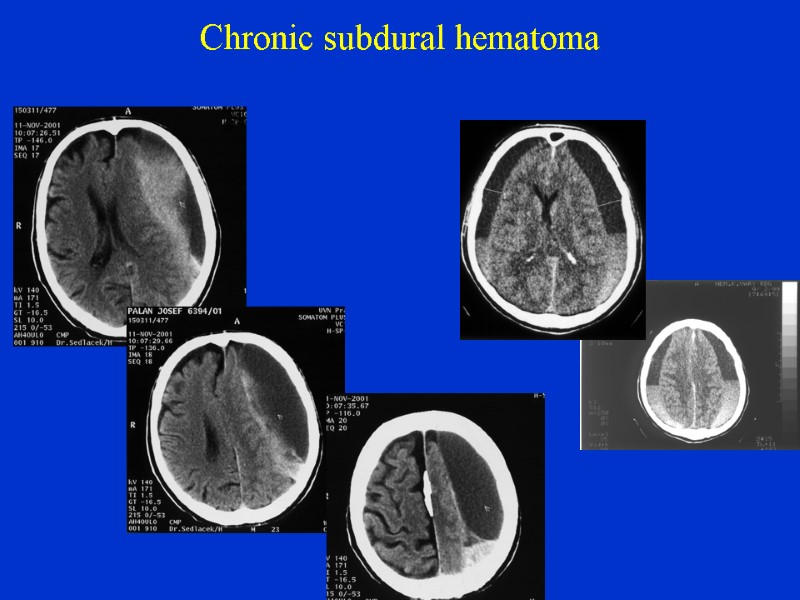
Chronic subdural hematoma
Traumatic intracerebral hematoma Relation to contusion: continous line from „pure contusion“ to „pure hematoma“ Treatment: surgery in case of mass effect – like in cases of large contussions
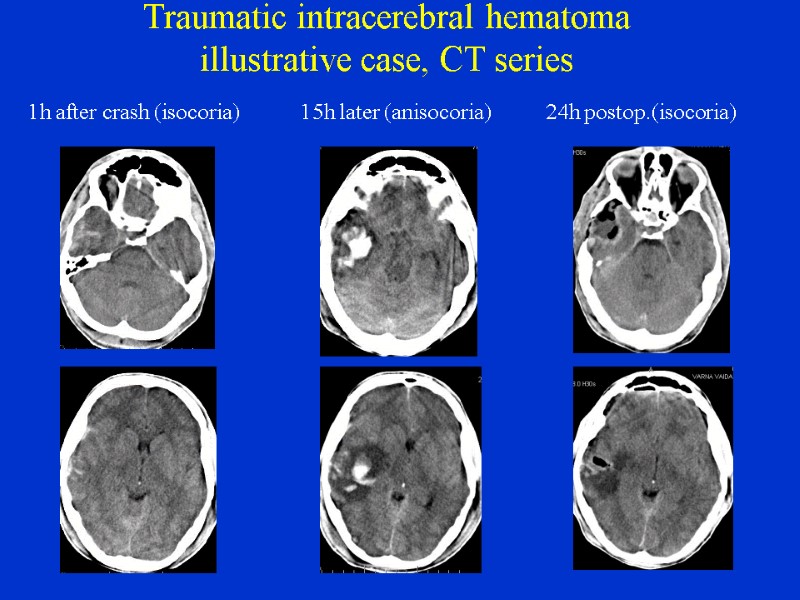
Traumatic intracerebral hematoma illustrative case, CT series 1h after crash (isocoria) 15h later (anisocoria) 24h postop.(isocoria)
14878-brain_trauma_2.ppt
- Количество слайдов: 42

