ca552cf4c8df9617b618c8f18817c94f.ppt
- Количество слайдов: 79
 Cost Effectiveness: How Can We Do More With Less? Stephen P. Merry, MD, MPH, DTM&H Assistant Professor of Family Medicine Mayo Clinic, Rochester © 2013 MFMER | slide-1
Cost Effectiveness: How Can We Do More With Less? Stephen P. Merry, MD, MPH, DTM&H Assistant Professor of Family Medicine Mayo Clinic, Rochester © 2013 MFMER | slide-1
 Disclosures • Financial Disclosures • None • Off label drug use • None 2 © 2013 MFMER | slide-2
Disclosures • Financial Disclosures • None • Off label drug use • None 2 © 2013 MFMER | slide-2
 Learning Objectives • Treat chronic diseases in adults and children in resource limited settings in a rational, costeffective way. • Follow an income and country GNP based protocol for hypertension, type 1 and 2 diabetes, hyperlipidemia, and coronary artery disease diagnosis and care. • Design treatment protocols based on guiding principles of cost-effectiveness. 3 © 2013 MFMER | slide-3
Learning Objectives • Treat chronic diseases in adults and children in resource limited settings in a rational, costeffective way. • Follow an income and country GNP based protocol for hypertension, type 1 and 2 diabetes, hyperlipidemia, and coronary artery disease diagnosis and care. • Design treatment protocols based on guiding principles of cost-effectiveness. 3 © 2013 MFMER | slide-3
 Medical Missionaries Behaving Badly • Follow US treatment protocols • “We shouldn’t treat them any differently than we’d want to be treated…” • Treating chronic diseases regardless of benefit or cost • Expensive testing • Expensive monitoring • Expensive meds • Frequent rechecks © 2013 MFMER | slide-4
Medical Missionaries Behaving Badly • Follow US treatment protocols • “We shouldn’t treat them any differently than we’d want to be treated…” • Treating chronic diseases regardless of benefit or cost • Expensive testing • Expensive monitoring • Expensive meds • Frequent rechecks © 2013 MFMER | slide-4
 The Summary Slide Careful consideration of the whole care process from care access to care follow-up including all costs including harms and benefits coupled with compassion Cost effective care 5 © 2013 MFMER | slide-5
The Summary Slide Careful consideration of the whole care process from care access to care follow-up including all costs including harms and benefits coupled with compassion Cost effective care 5 © 2013 MFMER | slide-5
 Disclaimer • I’m a clinician • The following is a patient centric view on cost effectiveness analysis • I’m not an economist © 2013 MFMER | slide-6
Disclaimer • I’m a clinician • The following is a patient centric view on cost effectiveness analysis • I’m not an economist © 2013 MFMER | slide-6
 Cost-Effective Health Care • Caring for people in resource limited setting • Less tests, technology, meds; just the essentials • Less specialists • Less physician driven – lifestyle/public health primary • Avoid futility • Person centered, coordinated, comprehensive care by an accessible primary care provider 7 © 2013 MFMER | slide-7
Cost-Effective Health Care • Caring for people in resource limited setting • Less tests, technology, meds; just the essentials • Less specialists • Less physician driven – lifestyle/public health primary • Avoid futility • Person centered, coordinated, comprehensive care by an accessible primary care provider 7 © 2013 MFMER | slide-7
 Cost Effective Care • Requires analysis of the “care delivery value chain” • Prevention • Testing/Screening • Staging • Delaying progression of disease • Initiation of therapy • Continuous disease management • Management of deterioration Rhatigan et al. Applying the Care Delivery Value Chain: HIV/AIDS Care in Resource Poor Setttings. Harvard Business School working paper, 2009 © 2013 MFMER | slide-8
Cost Effective Care • Requires analysis of the “care delivery value chain” • Prevention • Testing/Screening • Staging • Delaying progression of disease • Initiation of therapy • Continuous disease management • Management of deterioration Rhatigan et al. Applying the Care Delivery Value Chain: HIV/AIDS Care in Resource Poor Setttings. Harvard Business School working paper, 2009 © 2013 MFMER | slide-8
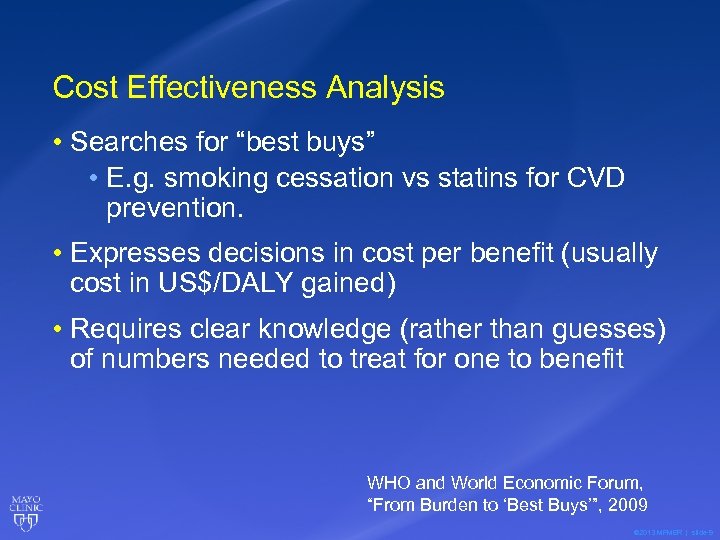 Cost Effectiveness Analysis • Searches for “best buys” • E. g. smoking cessation vs statins for CVD prevention. • Expresses decisions in cost per benefit (usually cost in US$/DALY gained) • Requires clear knowledge (rather than guesses) of numbers needed to treat for one to benefit WHO and World Economic Forum, “From Burden to ‘Best Buys’”, 2009 © 2013 MFMER | slide-9
Cost Effectiveness Analysis • Searches for “best buys” • E. g. smoking cessation vs statins for CVD prevention. • Expresses decisions in cost per benefit (usually cost in US$/DALY gained) • Requires clear knowledge (rather than guesses) of numbers needed to treat for one to benefit WHO and World Economic Forum, “From Burden to ‘Best Buys’”, 2009 © 2013 MFMER | slide-9
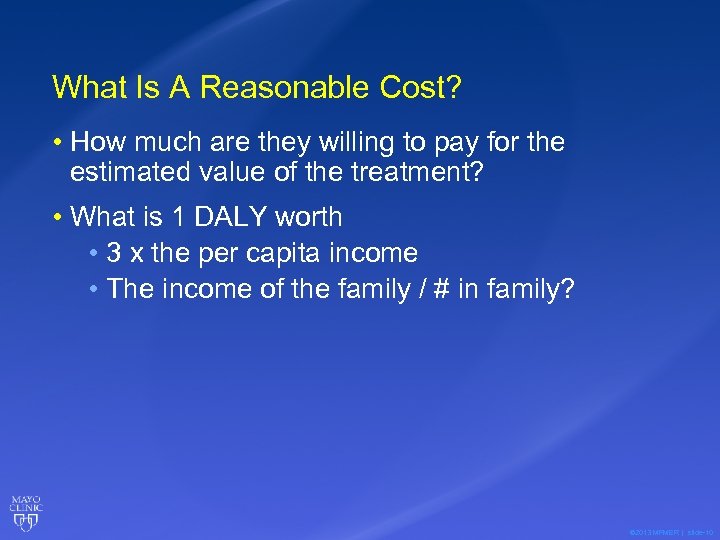 What Is A Reasonable Cost? • How much are they willing to pay for the estimated value of the treatment? • What is 1 DALY worth • 3 x the per capita income • The income of the family / # in family? © 2013 MFMER | slide-10
What Is A Reasonable Cost? • How much are they willing to pay for the estimated value of the treatment? • What is 1 DALY worth • 3 x the per capita income • The income of the family / # in family? © 2013 MFMER | slide-10
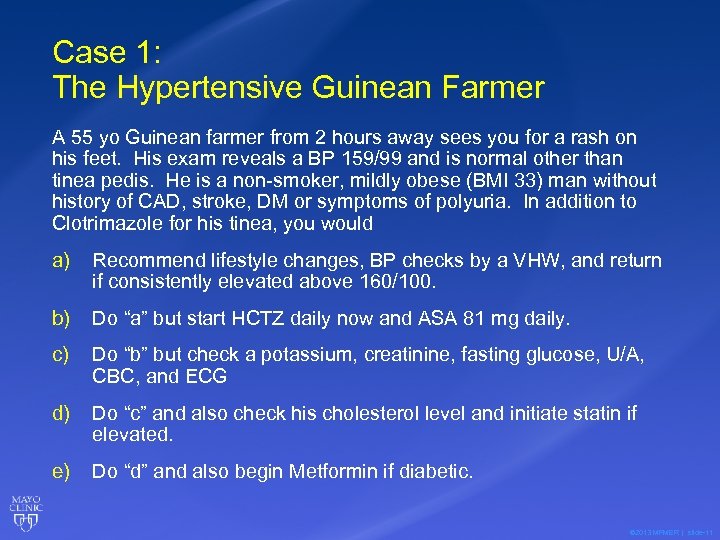 Case 1: The Hypertensive Guinean Farmer A 55 yo Guinean farmer from 2 hours away sees you for a rash on his feet. His exam reveals a BP 159/99 and is normal other than tinea pedis. He is a non-smoker, mildly obese (BMI 33) man without history of CAD, stroke, DM or symptoms of polyuria. In addition to Clotrimazole for his tinea, you would a) Recommend lifestyle changes, BP checks by a VHW, and return if consistently elevated above 160/100. b) Do “a” but start HCTZ daily now and ASA 81 mg daily. c) Do “b” but check a potassium, creatinine, fasting glucose, U/A, CBC, and ECG d) Do “c” and also check his cholesterol level and initiate statin if elevated. e) Do “d” and also begin Metformin if diabetic. © 2013 MFMER | slide-11
Case 1: The Hypertensive Guinean Farmer A 55 yo Guinean farmer from 2 hours away sees you for a rash on his feet. His exam reveals a BP 159/99 and is normal other than tinea pedis. He is a non-smoker, mildly obese (BMI 33) man without history of CAD, stroke, DM or symptoms of polyuria. In addition to Clotrimazole for his tinea, you would a) Recommend lifestyle changes, BP checks by a VHW, and return if consistently elevated above 160/100. b) Do “a” but start HCTZ daily now and ASA 81 mg daily. c) Do “b” but check a potassium, creatinine, fasting glucose, U/A, CBC, and ECG d) Do “c” and also check his cholesterol level and initiate statin if elevated. e) Do “d” and also begin Metformin if diabetic. © 2013 MFMER | slide-11
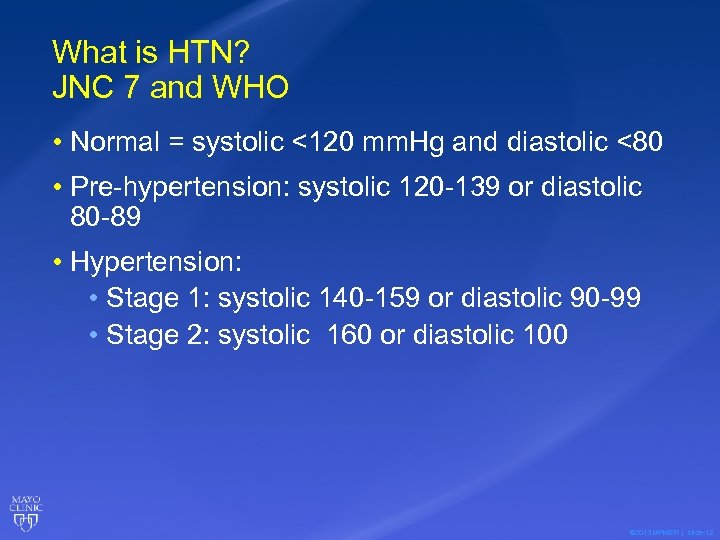 What is HTN? JNC 7 and WHO • Normal = systolic <120 mm. Hg and diastolic <80 • Pre-hypertension: systolic 120 -139 or diastolic 80 -89 • Hypertension: • Stage 1: systolic 140 -159 or diastolic 90 -99 • Stage 2: systolic 160 or diastolic 100 © 2013 MFMER | slide-12
What is HTN? JNC 7 and WHO • Normal = systolic <120 mm. Hg and diastolic <80 • Pre-hypertension: systolic 120 -139 or diastolic 80 -89 • Hypertension: • Stage 1: systolic 140 -159 or diastolic 90 -99 • Stage 2: systolic 160 or diastolic 100 © 2013 MFMER | slide-12
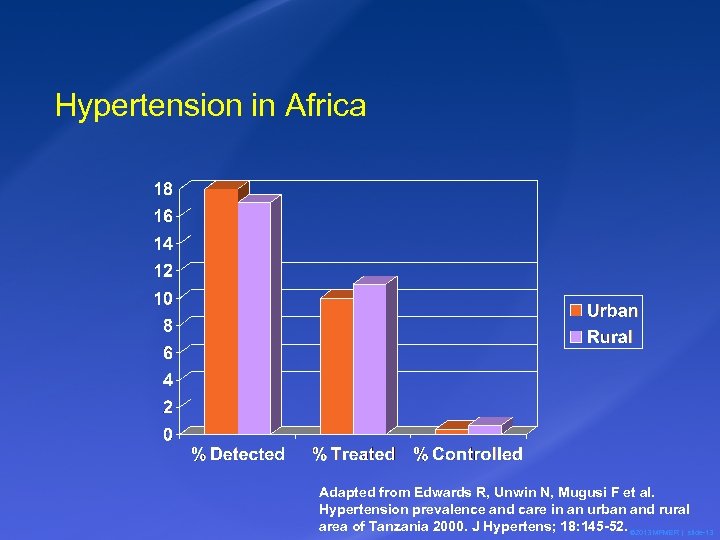 Hypertension in Africa Adapted from Edwards R, Unwin N, Mugusi F et al. Hypertension prevalence and care in an urban and rural area of Tanzania 2000. J Hypertens; 18: 145 -52. © 2013 MFMER | slide-13
Hypertension in Africa Adapted from Edwards R, Unwin N, Mugusi F et al. Hypertension prevalence and care in an urban and rural area of Tanzania 2000. J Hypertens; 18: 145 -52. © 2013 MFMER | slide-13
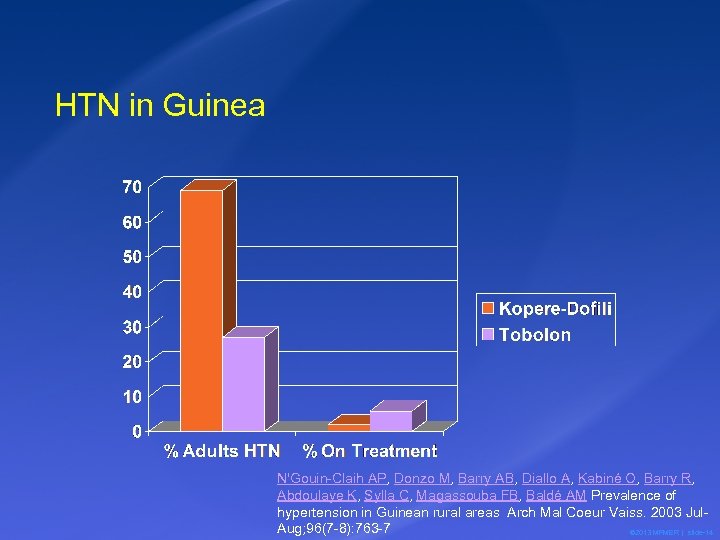 HTN in Guinea N'Gouin-Claih AP, Donzo M, Barry AB, Diallo A, Kabiné O, Barry R, Abdoulaye K, Sylla C, Magassouba FB, Baldé AM Prevalence of hypertension in Guinean rural areas Arch Mal Coeur Vaiss. 2003 Jul. Aug; 96(7 -8): 763 -7 © 2013 MFMER | slide-14
HTN in Guinea N'Gouin-Claih AP, Donzo M, Barry AB, Diallo A, Kabiné O, Barry R, Abdoulaye K, Sylla C, Magassouba FB, Baldé AM Prevalence of hypertension in Guinean rural areas Arch Mal Coeur Vaiss. 2003 Jul. Aug; 96(7 -8): 763 -7 © 2013 MFMER | slide-14
 Should we treat mild HTN? • > 140/90 even if no risk factors? • NNT for 1 year = 700 to prevent 1 MI or stroke related death (mild HTN). • If cost of Rx = US$50/year, is the Guinean farmer REALLY consenting to US $35, 000 to save ? 10 years life (WHO suggests max cost should be 3 x per capita GNP or about $1300 for Guinea)? • Paternalism vs. shared decision making. © 2013 MFMER | slide-15
Should we treat mild HTN? • > 140/90 even if no risk factors? • NNT for 1 year = 700 to prevent 1 MI or stroke related death (mild HTN). • If cost of Rx = US$50/year, is the Guinean farmer REALLY consenting to US $35, 000 to save ? 10 years life (WHO suggests max cost should be 3 x per capita GNP or about $1300 for Guinea)? • Paternalism vs. shared decision making. © 2013 MFMER | slide-15
 Initial Evaluation of HTN • Labs • Dip U/A; maybe other if history, exam or urinalysis suggests need and can afford. • Creatinine • K+ • (ECG) • (Lipids) • (Fasting blood sugar) © 2013 MFMER | slide-18
Initial Evaluation of HTN • Labs • Dip U/A; maybe other if history, exam or urinalysis suggests need and can afford. • Creatinine • K+ • (ECG) • (Lipids) • (Fasting blood sugar) © 2013 MFMER | slide-18
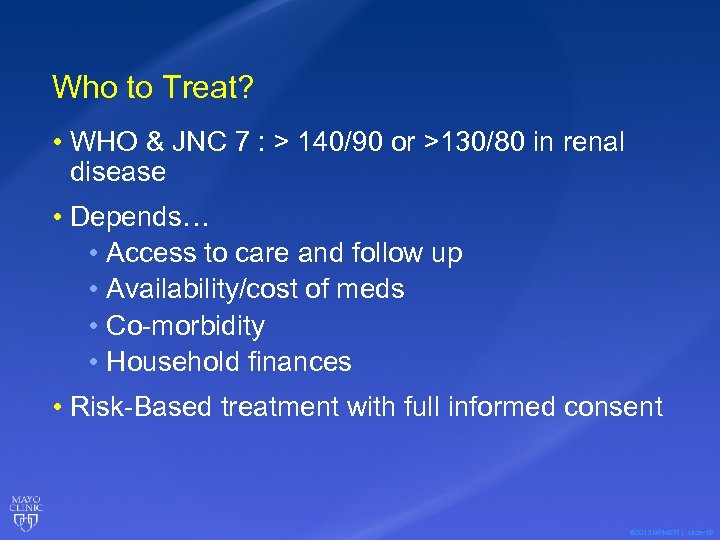 Who to Treat? • WHO & JNC 7 : > 140/90 or >130/80 in renal disease • Depends… • Access to care and follow up • Availability/cost of meds • Co-morbidity • Household finances • Risk-Based treatment with full informed consent © 2013 MFMER | slide-19
Who to Treat? • WHO & JNC 7 : > 140/90 or >130/80 in renal disease • Depends… • Access to care and follow up • Availability/cost of meds • Co-morbidity • Household finances • Risk-Based treatment with full informed consent © 2013 MFMER | slide-19
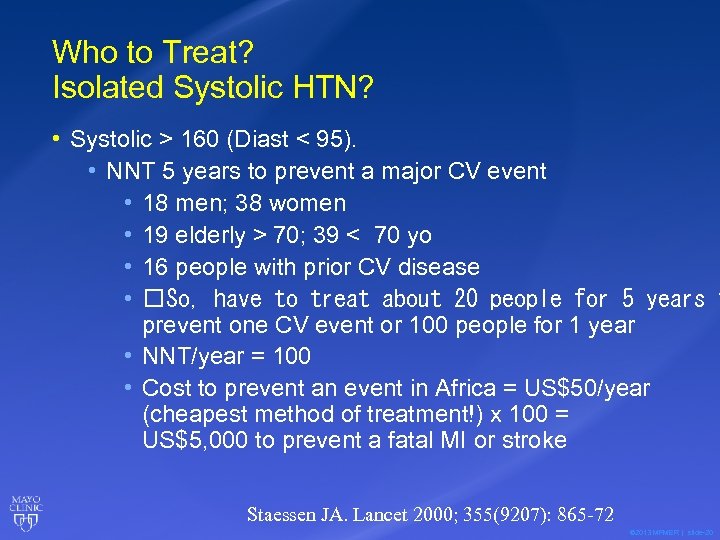 Who to Treat? Isolated Systolic HTN? • Systolic > 160 (Diast < 95). • NNT 5 years to prevent a major CV event • 18 men; 38 women • 19 elderly > 70; 39 < 70 yo • 16 people with prior CV disease • So, have to treat about 20 people for 5 years t prevent one CV event or 100 people for 1 year • NNT/year = 100 • Cost to prevent an event in Africa = US$50/year (cheapest method of treatment!) x 100 = US$5, 000 to prevent a fatal MI or stroke Staessen JA. Lancet 2000; 355(9207): 865 -72 © 2013 MFMER | slide-20
Who to Treat? Isolated Systolic HTN? • Systolic > 160 (Diast < 95). • NNT 5 years to prevent a major CV event • 18 men; 38 women • 19 elderly > 70; 39 < 70 yo • 16 people with prior CV disease • So, have to treat about 20 people for 5 years t prevent one CV event or 100 people for 1 year • NNT/year = 100 • Cost to prevent an event in Africa = US$50/year (cheapest method of treatment!) x 100 = US$5, 000 to prevent a fatal MI or stroke Staessen JA. Lancet 2000; 355(9207): 865 -72 © 2013 MFMER | slide-20
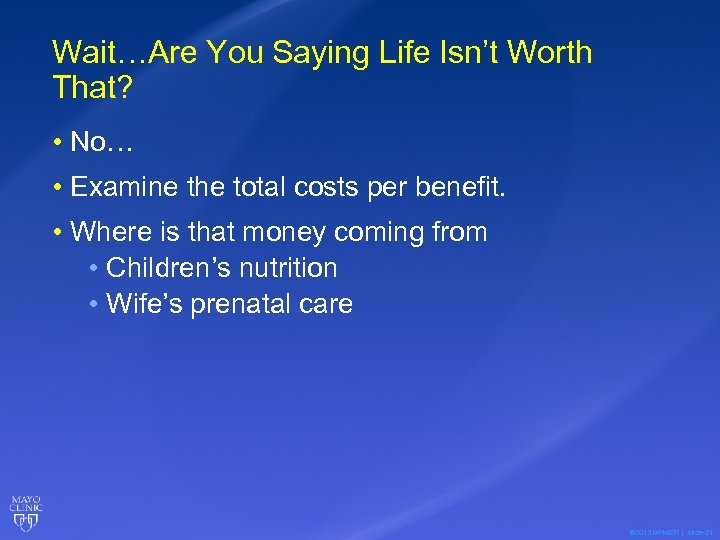 Wait…Are You Saying Life Isn’t Worth That? • No… • Examine the total costs per benefit. • Where is that money coming from • Children’s nutrition • Wife’s prenatal care © 2013 MFMER | slide-21
Wait…Are You Saying Life Isn’t Worth That? • No… • Examine the total costs per benefit. • Where is that money coming from • Children’s nutrition • Wife’s prenatal care © 2013 MFMER | slide-21
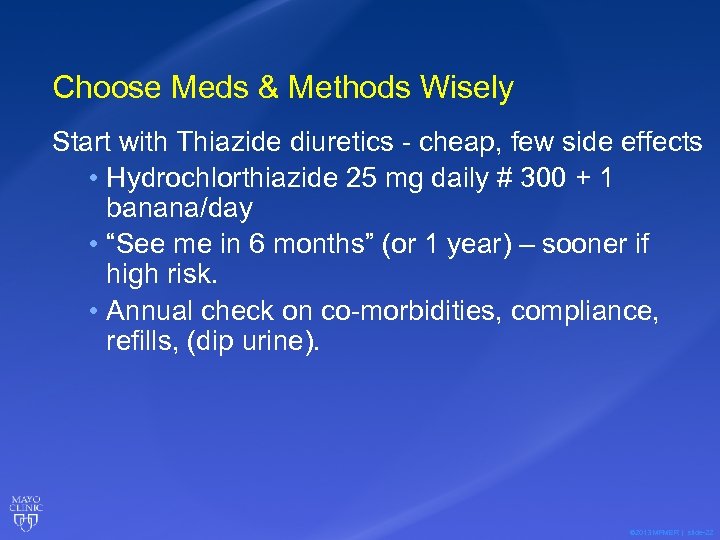 Choose Meds & Methods Wisely Start with Thiazide diuretics - cheap, few side effects • Hydrochlorthiazide 25 mg daily # 300 + 1 banana/day • “See me in 6 months” (or 1 year) – sooner if high risk. • Annual check on co-morbidities, compliance, refills, (dip urine). © 2013 MFMER | slide-22
Choose Meds & Methods Wisely Start with Thiazide diuretics - cheap, few side effects • Hydrochlorthiazide 25 mg daily # 300 + 1 banana/day • “See me in 6 months” (or 1 year) – sooner if high risk. • Annual check on co-morbidities, compliance, refills, (dip urine). © 2013 MFMER | slide-22
 © 2013 MFMER | slide-23
© 2013 MFMER | slide-23
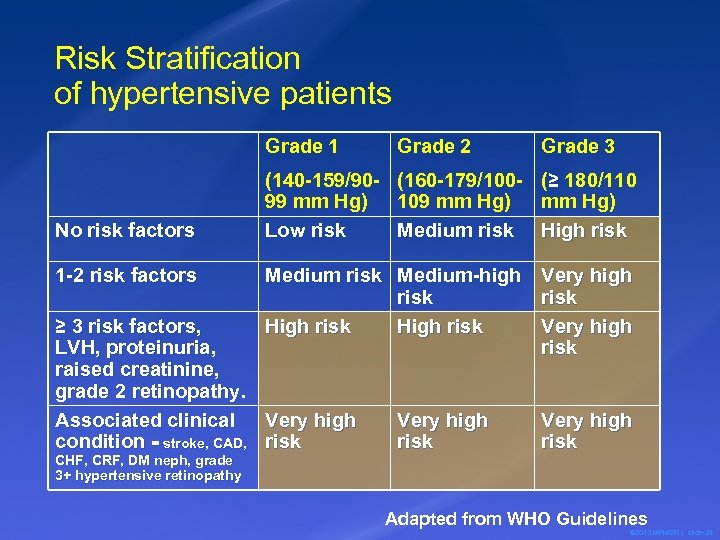 Risk Stratification of hypertensive patients Grade 1 No risk factors 1 -2 risk factors Grade 3 (140 -159/90 - (160 -179/100 - (≥ 180/110 99 mm Hg) 109 mm Hg) Low risk Medium risk High risk Medium-high risk High risk ≥ 3 risk factors, LVH, proteinuria, raised creatinine, grade 2 retinopathy. Associated clinical Very high condition = stroke, CAD, risk CHF, CRF, DM neph, grade 3+ hypertensive retinopathy Grade 2 Very high risk Adapted from WHO Guidelines © 2013 MFMER | slide-24
Risk Stratification of hypertensive patients Grade 1 No risk factors 1 -2 risk factors Grade 3 (140 -159/90 - (160 -179/100 - (≥ 180/110 99 mm Hg) 109 mm Hg) Low risk Medium risk High risk Medium-high risk High risk ≥ 3 risk factors, LVH, proteinuria, raised creatinine, grade 2 retinopathy. Associated clinical Very high condition = stroke, CAD, risk CHF, CRF, DM neph, grade 3+ hypertensive retinopathy Grade 2 Very high risk Adapted from WHO Guidelines © 2013 MFMER | slide-24
 The Big Idea: • Patients/Families/Countries with more resources should be treated at earlier stages with fewer co-morbidities. • If the Guinean Farmer is paying out of pocket, mild hypertension should not probably be treated. © 2013 MFMER | slide-25
The Big Idea: • Patients/Families/Countries with more resources should be treated at earlier stages with fewer co-morbidities. • If the Guinean Farmer is paying out of pocket, mild hypertension should not probably be treated. © 2013 MFMER | slide-25
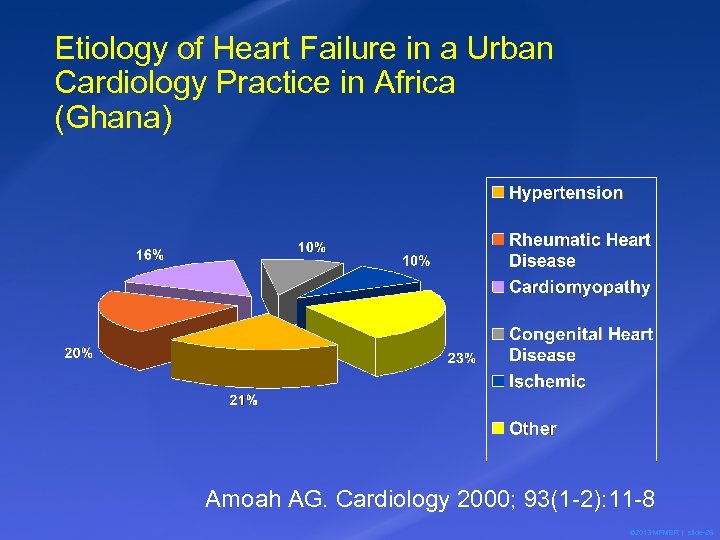 Etiology of Heart Failure in a Urban Cardiology Practice in Africa (Ghana) Amoah AG. Cardiology 2000; 93(1 -2): 11 -8 © 2013 MFMER | slide-26
Etiology of Heart Failure in a Urban Cardiology Practice in Africa (Ghana) Amoah AG. Cardiology 2000; 93(1 -2): 11 -8 © 2013 MFMER | slide-26
 How should we treat mild HTN or low risk patients? • Depends… “Shared Decision Making” • Diet • Low salt • High fruits and vegetables • Weight loss • Less alcohol • Exercise © 2013 MFMER | slide-27
How should we treat mild HTN or low risk patients? • Depends… “Shared Decision Making” • Diet • Low salt • High fruits and vegetables • Weight loss • Less alcohol • Exercise © 2013 MFMER | slide-27
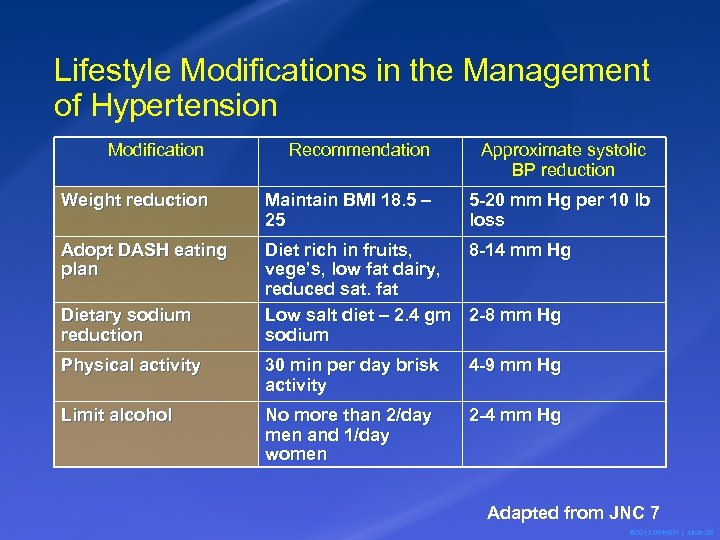 Lifestyle Modifications in the Management of Hypertension Modification Recommendation Approximate systolic BP reduction Weight reduction Maintain BMI 18. 5 – 25 5 -20 mm Hg per 10 lb loss Adopt DASH eating plan Diet rich in fruits, 8 -14 mm Hg vege’s, low fat dairy, reduced sat. fat Low salt diet – 2. 4 gm 2 -8 mm Hg sodium Dietary sodium reduction Physical activity 30 min per day brisk activity 4 -9 mm Hg Limit alcohol No more than 2/day men and 1/day women 2 -4 mm Hg Adapted from JNC 7 © 2013 MFMER | slide-28
Lifestyle Modifications in the Management of Hypertension Modification Recommendation Approximate systolic BP reduction Weight reduction Maintain BMI 18. 5 – 25 5 -20 mm Hg per 10 lb loss Adopt DASH eating plan Diet rich in fruits, 8 -14 mm Hg vege’s, low fat dairy, reduced sat. fat Low salt diet – 2. 4 gm 2 -8 mm Hg sodium Dietary sodium reduction Physical activity 30 min per day brisk activity 4 -9 mm Hg Limit alcohol No more than 2/day men and 1/day women 2 -4 mm Hg Adapted from JNC 7 © 2013 MFMER | slide-28
 Patient Education - HTN • HTN requires lifelong treatment • HTN increases the risk of many diseases – stroke, heart attack, etc. • HTN treatment won’t make you feel much better but it’s good for you. • Lifestyle mod is AS IMPORTANT as medicine. • You need to take your medicine daily. © 2013 MFMER | slide-29
Patient Education - HTN • HTN requires lifelong treatment • HTN increases the risk of many diseases – stroke, heart attack, etc. • HTN treatment won’t make you feel much better but it’s good for you. • Lifestyle mod is AS IMPORTANT as medicine. • You need to take your medicine daily. © 2013 MFMER | slide-29
 Choose Meds Wisely • Goal • Cheap • Convenient • Effective risk reduction • No side effects © 2013 MFMER | slide-30
Choose Meds Wisely • Goal • Cheap • Convenient • Effective risk reduction • No side effects © 2013 MFMER | slide-30
 Second Rx: Choose Meds Wisely • All meds ~ same benefit in large studies (ALLHAT). • Start with Thiazide diuretics - cheap, few side effects, superior in CHD prevention • CCB’s work best in Africans © 2013 MFMER | slide-31
Second Rx: Choose Meds Wisely • All meds ~ same benefit in large studies (ALLHAT). • Start with Thiazide diuretics - cheap, few side effects, superior in CHD prevention • CCB’s work best in Africans © 2013 MFMER | slide-31
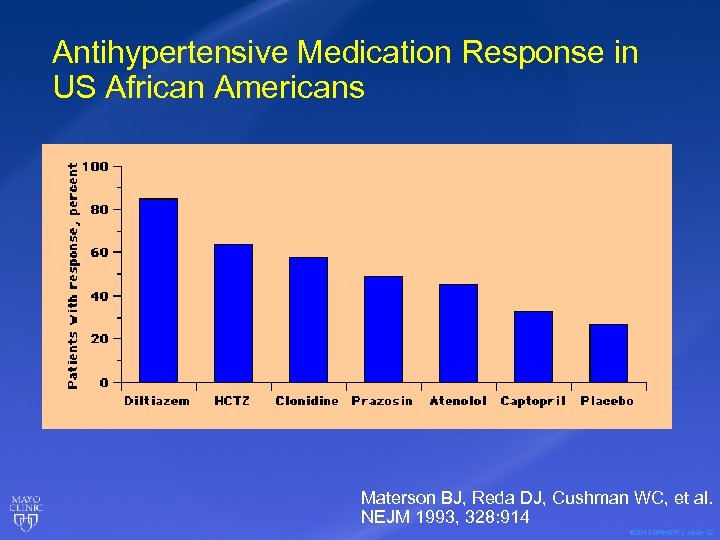 Antihypertensive Medication Response in US African Americans Materson BJ, Reda DJ, Cushman WC, et al. NEJM 1993, 328: 914 © 2013 MFMER | slide-32
Antihypertensive Medication Response in US African Americans Materson BJ, Reda DJ, Cushman WC, et al. NEJM 1993, 328: 914 © 2013 MFMER | slide-32
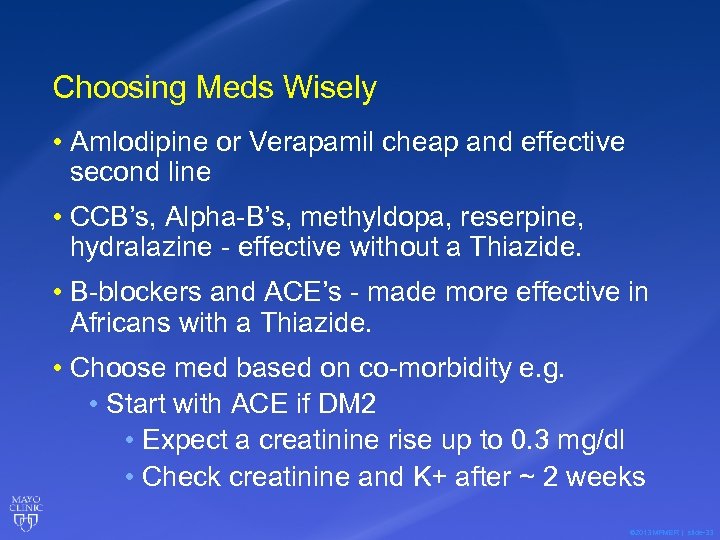 Choosing Meds Wisely • Amlodipine or Verapamil cheap and effective second line • CCB’s, Alpha-B’s, methyldopa, reserpine, hydralazine - effective without a Thiazide. • B-blockers and ACE’s - made more effective in Africans with a Thiazide. • Choose med based on co-morbidity e. g. • Start with ACE if DM 2 • Expect a creatinine rise up to 0. 3 mg/dl • Check creatinine and K+ after ~ 2 weeks © 2013 MFMER | slide-33
Choosing Meds Wisely • Amlodipine or Verapamil cheap and effective second line • CCB’s, Alpha-B’s, methyldopa, reserpine, hydralazine - effective without a Thiazide. • B-blockers and ACE’s - made more effective in Africans with a Thiazide. • Choose med based on co-morbidity e. g. • Start with ACE if DM 2 • Expect a creatinine rise up to 0. 3 mg/dl • Check creatinine and K+ after ~ 2 weeks © 2013 MFMER | slide-33
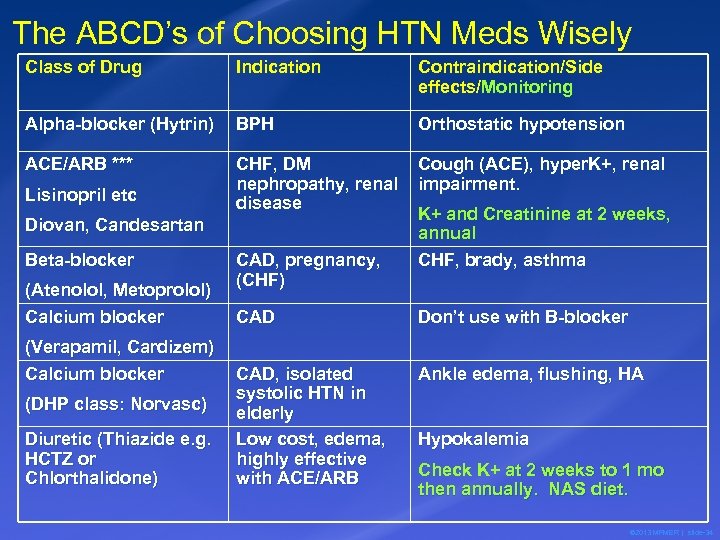 The ABCD’s of Choosing HTN Meds Wisely Class of Drug Indication Contraindication/Side effects/Monitoring Alpha-blocker (Hytrin) BPH Orthostatic hypotension ACE/ARB *** CHF, DM nephropathy, renal disease Cough (ACE), hyper. K+, renal impairment. Lisinopril etc Diovan, Candesartan Beta-blocker (Atenolol, Metoprolol) Calcium blocker (Verapamil, Cardizem) Calcium blocker (DHP class: Norvasc) Diuretic (Thiazide e. g. HCTZ or Chlorthalidone) CAD, pregnancy, (CHF) K+ and Creatinine at 2 weeks, annual CHF, brady, asthma CAD Don’t use with B-blocker CAD, isolated systolic HTN in elderly Low cost, edema, highly effective with ACE/ARB Ankle edema, flushing, HA Hypokalemia Check K+ at 2 weeks to 1 mo then annually. NAS diet. © 2013 MFMER | slide-34
The ABCD’s of Choosing HTN Meds Wisely Class of Drug Indication Contraindication/Side effects/Monitoring Alpha-blocker (Hytrin) BPH Orthostatic hypotension ACE/ARB *** CHF, DM nephropathy, renal disease Cough (ACE), hyper. K+, renal impairment. Lisinopril etc Diovan, Candesartan Beta-blocker (Atenolol, Metoprolol) Calcium blocker (Verapamil, Cardizem) Calcium blocker (DHP class: Norvasc) Diuretic (Thiazide e. g. HCTZ or Chlorthalidone) CAD, pregnancy, (CHF) K+ and Creatinine at 2 weeks, annual CHF, brady, asthma CAD Don’t use with B-blocker CAD, isolated systolic HTN in elderly Low cost, edema, highly effective with ACE/ARB Ankle edema, flushing, HA Hypokalemia Check K+ at 2 weeks to 1 mo then annually. NAS diet. © 2013 MFMER | slide-34
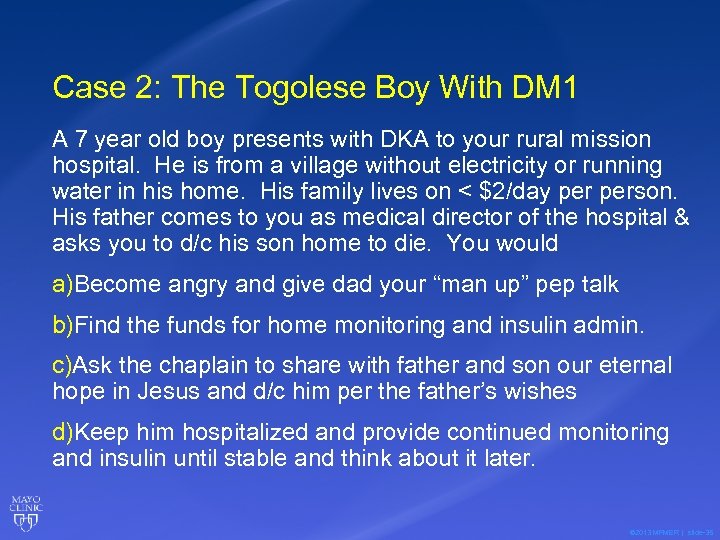 Case 2: The Togolese Boy With DM 1 A 7 year old boy presents with DKA to your rural mission hospital. He is from a village without electricity or running water in his home. His family lives on < $2/day person. His father comes to you as medical director of the hospital & asks you to d/c his son home to die. You would a)Become angry and give dad your “man up” pep talk b)Find the funds for home monitoring and insulin admin. c)Ask the chaplain to share with father and son our eternal hope in Jesus and d/c him per the father’s wishes d)Keep him hospitalized and provide continued monitoring and insulin until stable and think about it later. © 2013 MFMER | slide-35
Case 2: The Togolese Boy With DM 1 A 7 year old boy presents with DKA to your rural mission hospital. He is from a village without electricity or running water in his home. His family lives on < $2/day person. His father comes to you as medical director of the hospital & asks you to d/c his son home to die. You would a)Become angry and give dad your “man up” pep talk b)Find the funds for home monitoring and insulin admin. c)Ask the chaplain to share with father and son our eternal hope in Jesus and d/c him per the father’s wishes d)Keep him hospitalized and provide continued monitoring and insulin until stable and think about it later. © 2013 MFMER | slide-35
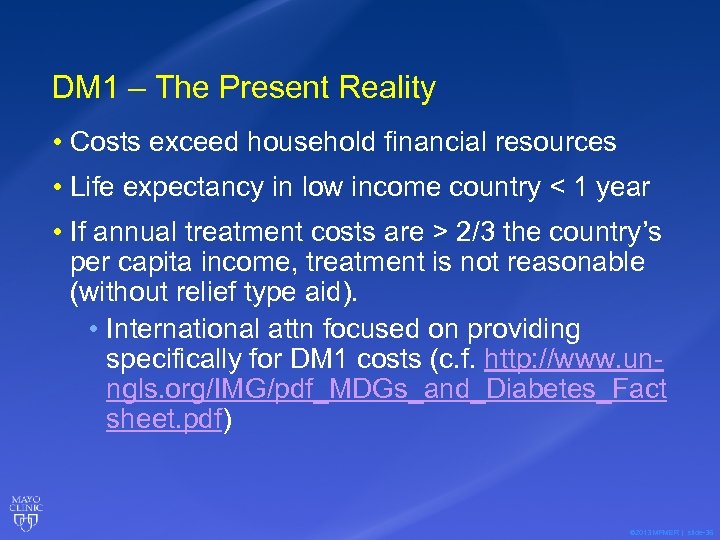 DM 1 – The Present Reality • Costs exceed household financial resources • Life expectancy in low income country < 1 year • If annual treatment costs are > 2/3 the country’s per capita income, treatment is not reasonable (without relief type aid). • International attn focused on providing specifically for DM 1 costs (c. f. http: //www. unngls. org/IMG/pdf_MDGs_and_Diabetes_Fact sheet. pdf) © 2013 MFMER | slide-36
DM 1 – The Present Reality • Costs exceed household financial resources • Life expectancy in low income country < 1 year • If annual treatment costs are > 2/3 the country’s per capita income, treatment is not reasonable (without relief type aid). • International attn focused on providing specifically for DM 1 costs (c. f. http: //www. unngls. org/IMG/pdf_MDGs_and_Diabetes_Fact sheet. pdf) © 2013 MFMER | slide-36
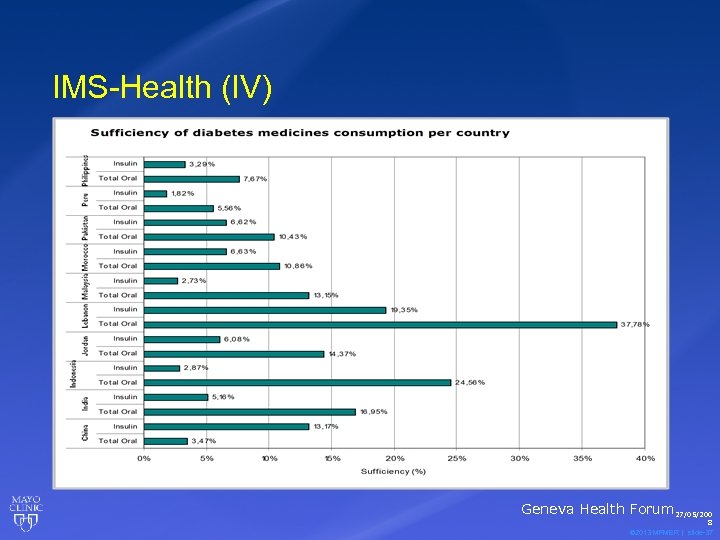 IMS-Health (IV) Geneva Health Forum 27/05/200 8 © 2013 MFMER | slide-37
IMS-Health (IV) Geneva Health Forum 27/05/200 8 © 2013 MFMER | slide-37
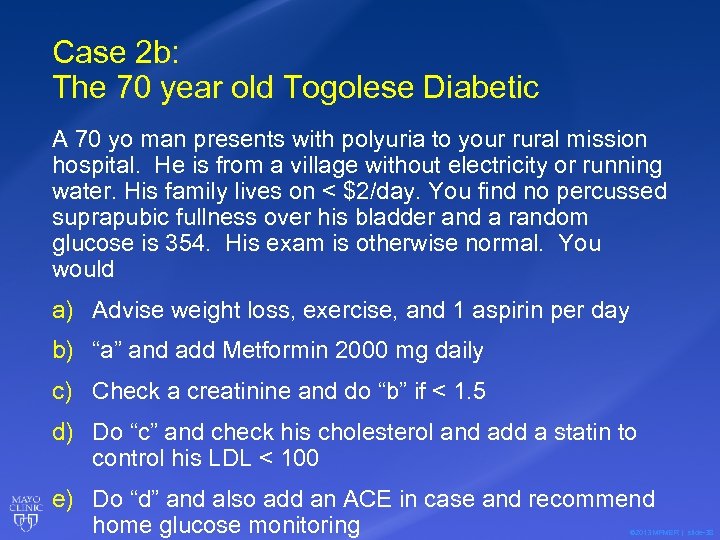 Case 2 b: The 70 year old Togolese Diabetic A 70 yo man presents with polyuria to your rural mission hospital. He is from a village without electricity or running water. His family lives on < $2/day. You find no percussed suprapubic fullness over his bladder and a random glucose is 354. His exam is otherwise normal. You would a) Advise weight loss, exercise, and 1 aspirin per day b) “a” and add Metformin 2000 mg daily c) Check a creatinine and do “b” if < 1. 5 d) Do “c” and check his cholesterol and add a statin to control his LDL < 100 e) Do “d” and also add an ACE in case and recommend home glucose monitoring © 2013 MFMER | slide-38
Case 2 b: The 70 year old Togolese Diabetic A 70 yo man presents with polyuria to your rural mission hospital. He is from a village without electricity or running water. His family lives on < $2/day. You find no percussed suprapubic fullness over his bladder and a random glucose is 354. His exam is otherwise normal. You would a) Advise weight loss, exercise, and 1 aspirin per day b) “a” and add Metformin 2000 mg daily c) Check a creatinine and do “b” if < 1. 5 d) Do “c” and check his cholesterol and add a statin to control his LDL < 100 e) Do “d” and also add an ACE in case and recommend home glucose monitoring © 2013 MFMER | slide-38
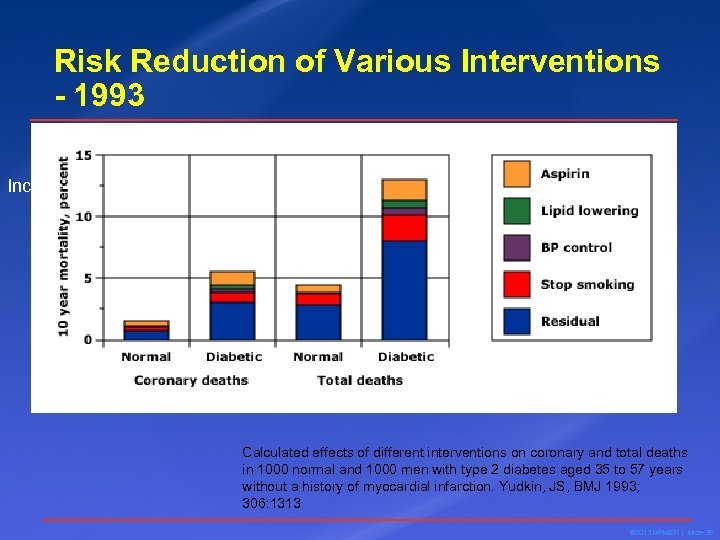 Risk Reduction of Various Interventions - 1993 Increased cardiovascular risk in type 2 diabetes Calculated effects of different interventions on coronary and total deaths in 1000 normal and 1000 men with type 2 diabetes aged 35 to 57 years without a history of myocardial infarction. Yudkin, JS, BMJ 1993; 306: 1313 © 2013 MFMER | slide-39
Risk Reduction of Various Interventions - 1993 Increased cardiovascular risk in type 2 diabetes Calculated effects of different interventions on coronary and total deaths in 1000 normal and 1000 men with type 2 diabetes aged 35 to 57 years without a history of myocardial infarction. Yudkin, JS, BMJ 1993; 306: 1313 © 2013 MFMER | slide-39
 Conclusion Errors… • The residual risk of “MRFIT” is due to high sugars • Lowering sugar will eliminate the risk • We should focus on frequently testing glucose and treating hyperglycemia © 2013 MFMER | slide-40
Conclusion Errors… • The residual risk of “MRFIT” is due to high sugars • Lowering sugar will eliminate the risk • We should focus on frequently testing glucose and treating hyperglycemia © 2013 MFMER | slide-40
 Value of Intensive Glycemic Control 3867 Type 2 DM followed 10 years Conventional Control vs Intensive Control • Diet alone • A 1 C 7. 9% • Diet + Sulfa or Insulin • A 1 C 7% Less weight gain No difference in agent eff. Less hypoglycemia 12% less laser photocoag of retinae No sig difference in deaths Conclusion: Tight control of DM 2 doesn’t affect mortality (or help much). UKPDS 33, Lancet 1998 © 2013 MFMER | slide-41
Value of Intensive Glycemic Control 3867 Type 2 DM followed 10 years Conventional Control vs Intensive Control • Diet alone • A 1 C 7. 9% • Diet + Sulfa or Insulin • A 1 C 7% Less weight gain No difference in agent eff. Less hypoglycemia 12% less laser photocoag of retinae No sig difference in deaths Conclusion: Tight control of DM 2 doesn’t affect mortality (or help much). UKPDS 33, Lancet 1998 © 2013 MFMER | slide-41
 ADVANCE: The End of Tight Control? • 215 centers, 20 countries; U. of Sydney, AU • 11, 140 pts DM 2 randomized to “tight” A 1 C 6. 5% or standard A 1 C to 7. 3%; f/u 5 years • Age > 55, Vascular disease or risk • No difference in CV death, nonfatal MI, stroke. • Less macroalbuminuria (9. 4% vs 10. 9%) • More hypoglycemia (2. 7% vs 1. 5%) The ADVANCE Collaborative Group. INTENSIVE BLOOD GLUCOSE CONTROL AND VASCULAR OUTCOMES IN PATIENTS WITH TYPE 2 DIABETES. N Engl J Med 358(24): 2560, June 12, 2008 © 2013 MFMER | slide-42
ADVANCE: The End of Tight Control? • 215 centers, 20 countries; U. of Sydney, AU • 11, 140 pts DM 2 randomized to “tight” A 1 C 6. 5% or standard A 1 C to 7. 3%; f/u 5 years • Age > 55, Vascular disease or risk • No difference in CV death, nonfatal MI, stroke. • Less macroalbuminuria (9. 4% vs 10. 9%) • More hypoglycemia (2. 7% vs 1. 5%) The ADVANCE Collaborative Group. INTENSIVE BLOOD GLUCOSE CONTROL AND VASCULAR OUTCOMES IN PATIENTS WITH TYPE 2 DIABETES. N Engl J Med 358(24): 2560, June 12, 2008 © 2013 MFMER | slide-42
 ACCORD: The End of Tight Control? • No significant different in MI or stroke • Intensive treatment caused • Increased all-cause mortality 5% vs 4% (P=NS) • More Hypoglycemia 16. 2% vs 5. 1% • More Weight gain > 10 kg 27. 8% vs 14. 1% The Action to Control Cardiovascular Risk in Diabetes (ACCORD) Study Group. The EFFECTS OF INTENSIVE GLUCOSE LOWERING IN TYPE 2 DIABETES. N Engl J Med 358(24): 2545, June 12, 2008 © 2013 MFMER | slide-43
ACCORD: The End of Tight Control? • No significant different in MI or stroke • Intensive treatment caused • Increased all-cause mortality 5% vs 4% (P=NS) • More Hypoglycemia 16. 2% vs 5. 1% • More Weight gain > 10 kg 27. 8% vs 14. 1% The Action to Control Cardiovascular Risk in Diabetes (ACCORD) Study Group. The EFFECTS OF INTENSIVE GLUCOSE LOWERING IN TYPE 2 DIABETES. N Engl J Med 358(24): 2545, June 12, 2008 © 2013 MFMER | slide-43
 The Big Point • Summary of 50 years of type 2 diabetes research: • Glycemic control has little to do with morbidity and mortality • Obesity, inactivity, and other bad behaviors mitigate risk • Correcting the real problems reduce risk. © 2013 MFMER | slide-44
The Big Point • Summary of 50 years of type 2 diabetes research: • Glycemic control has little to do with morbidity and mortality • Obesity, inactivity, and other bad behaviors mitigate risk • Correcting the real problems reduce risk. © 2013 MFMER | slide-44
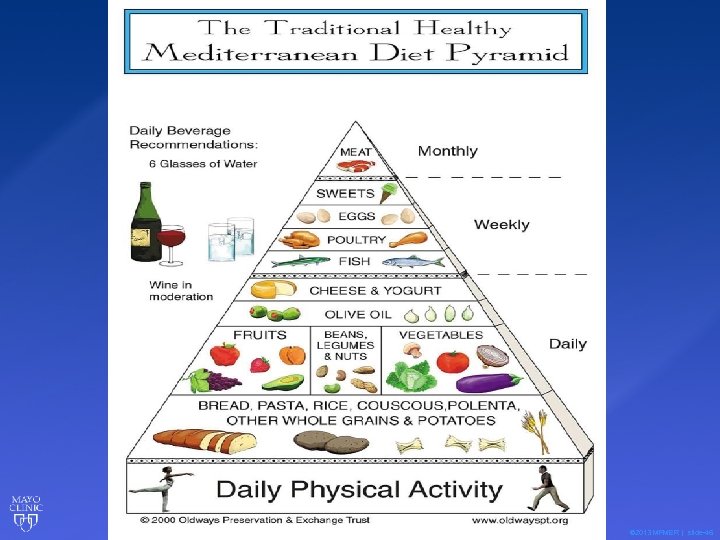
 Rational CV Risk Reduction Method: • Smoking Cessation • Med Diet, weight loss, exercise • ASA • BP normalization • Statin (not lipid lowering) • Glycemic control of minor benefit – use for symptoms unless well resourced. • Self testing wasteful unless on insulin © 2013 MFMER | slide-45
Rational CV Risk Reduction Method: • Smoking Cessation • Med Diet, weight loss, exercise • ASA • BP normalization • Statin (not lipid lowering) • Glycemic control of minor benefit – use for symptoms unless well resourced. • Self testing wasteful unless on insulin © 2013 MFMER | slide-45
 © 2013 MFMER | slide-46
© 2013 MFMER | slide-46
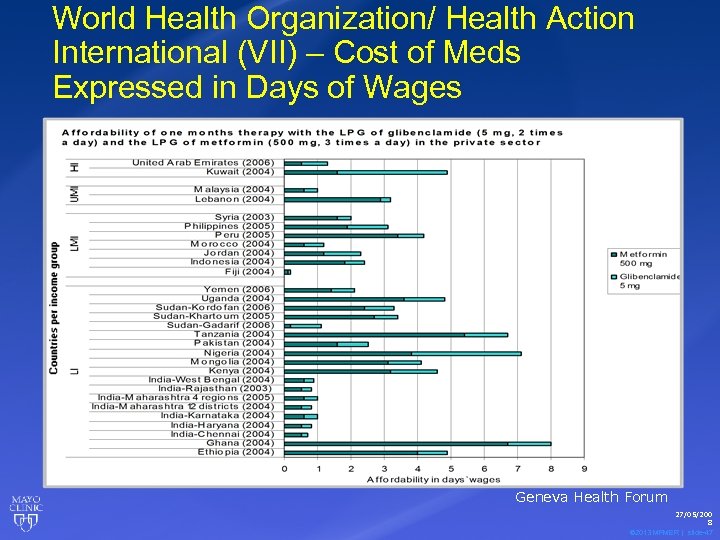 World Health Organization/ Health Action International (VII) – Cost of Meds Expressed in Days of Wages Geneva Health Forum 27/05/200 8 © 2013 MFMER | slide-47
World Health Organization/ Health Action International (VII) – Cost of Meds Expressed in Days of Wages Geneva Health Forum 27/05/200 8 © 2013 MFMER | slide-47
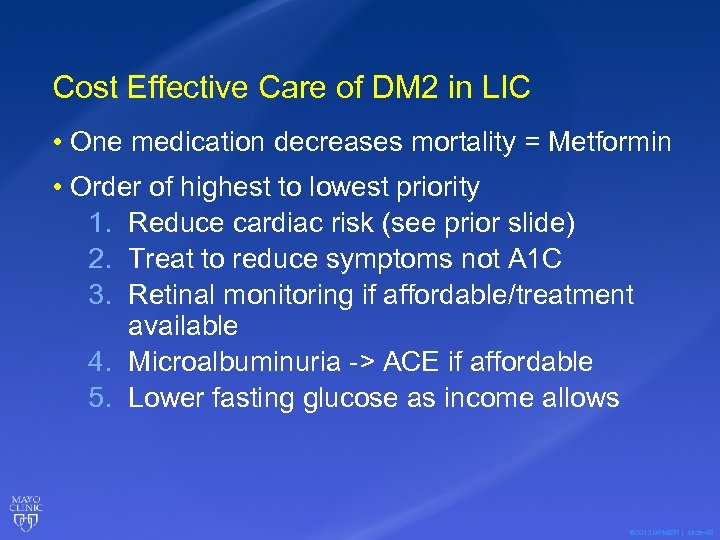 Cost Effective Care of DM 2 in LIC • One medication decreases mortality = Metformin • Order of highest to lowest priority 1. Reduce cardiac risk (see prior slide) 2. Treat to reduce symptoms not A 1 C 3. Retinal monitoring if affordable/treatment available 4. Microalbuminuria -> ACE if affordable 5. Lower fasting glucose as income allows © 2013 MFMER | slide-48
Cost Effective Care of DM 2 in LIC • One medication decreases mortality = Metformin • Order of highest to lowest priority 1. Reduce cardiac risk (see prior slide) 2. Treat to reduce symptoms not A 1 C 3. Retinal monitoring if affordable/treatment available 4. Microalbuminuria -> ACE if affordable 5. Lower fasting glucose as income allows © 2013 MFMER | slide-48
 Case 3: The Pregnant Pakistani Woman A healthy 30 yo G 2 P 1 with an uncomplicated last pregnancy delivered by trained TBA in her home presents for prenatal care to your rural hospital at 12 weeks GA. You would a) Recommend monthly visits increasing to every 2 weeks at term with hospital delivery to be safest b) Recommend she simply again deliver at home with the TBA c) Recommend care at the maternity in town d) Recommend TT 2, iron/folate, insecticide treated bednet use, IPTp, a prenatal visit in each trimester with a midwife or physician and delivery with the midwife. © 2013 MFMER | slide-49
Case 3: The Pregnant Pakistani Woman A healthy 30 yo G 2 P 1 with an uncomplicated last pregnancy delivered by trained TBA in her home presents for prenatal care to your rural hospital at 12 weeks GA. You would a) Recommend monthly visits increasing to every 2 weeks at term with hospital delivery to be safest b) Recommend she simply again deliver at home with the TBA c) Recommend care at the maternity in town d) Recommend TT 2, iron/folate, insecticide treated bednet use, IPTp, a prenatal visit in each trimester with a midwife or physician and delivery with the midwife. © 2013 MFMER | slide-49
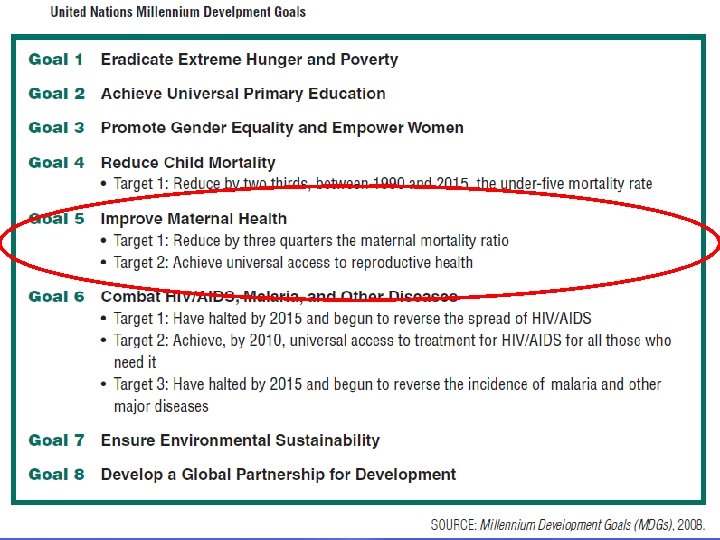 Why Be Involved Institute of Medicine. The U. S. Commitment to Global Health: Recommendations for the New Administration Committee on the U. S. 50 Commitment to Global Health. 2009. © 2013 MFMER | slide-50
Why Be Involved Institute of Medicine. The U. S. Commitment to Global Health: Recommendations for the New Administration Committee on the U. S. 50 Commitment to Global Health. 2009. © 2013 MFMER | slide-50
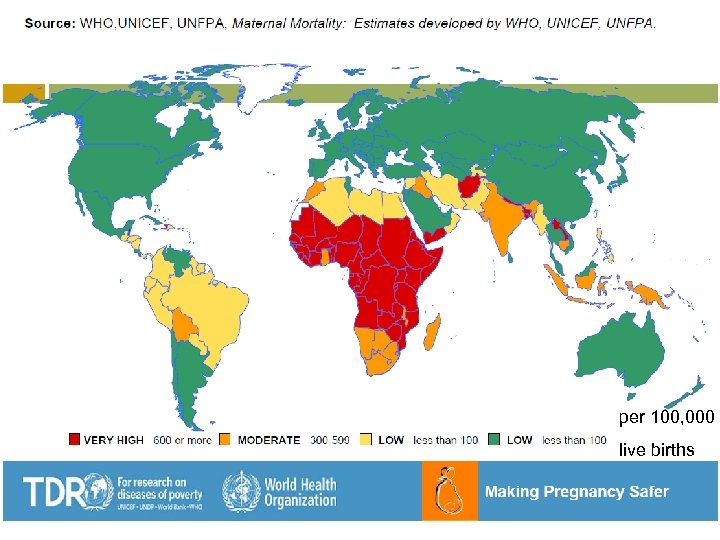 per 100, 000 live births 51 © 2013 MFMER | slide-51
per 100, 000 live births 51 © 2013 MFMER | slide-51
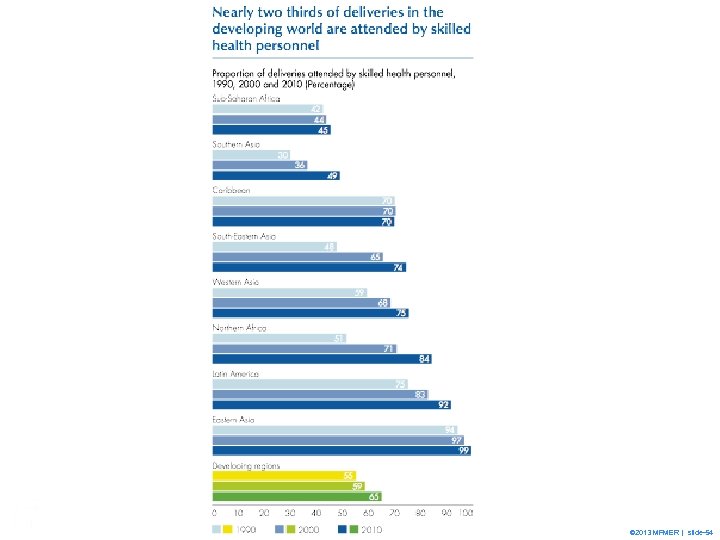
 69 © 2013 MFMER | slide-52
69 © 2013 MFMER | slide-52
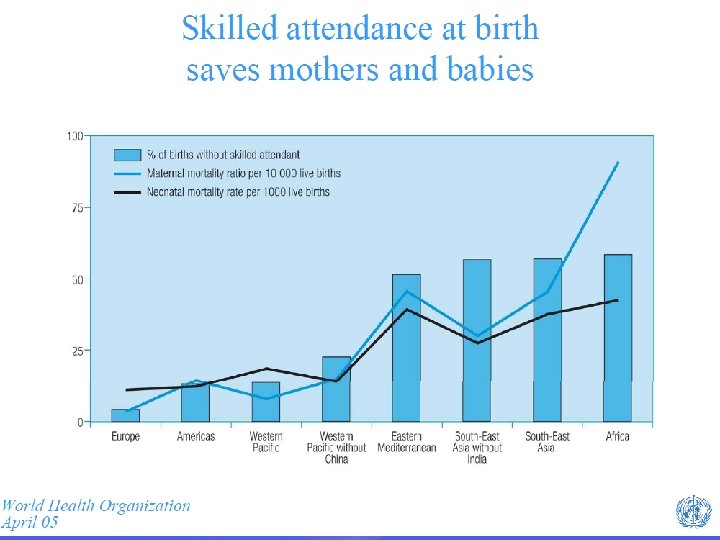
 29 © 2013 MFMER | slide-53
29 © 2013 MFMER | slide-53
 29 © 2013 MFMER | slide-54
29 © 2013 MFMER | slide-54
 55 © 2013 MFMER | slide-55
55 © 2013 MFMER | slide-55
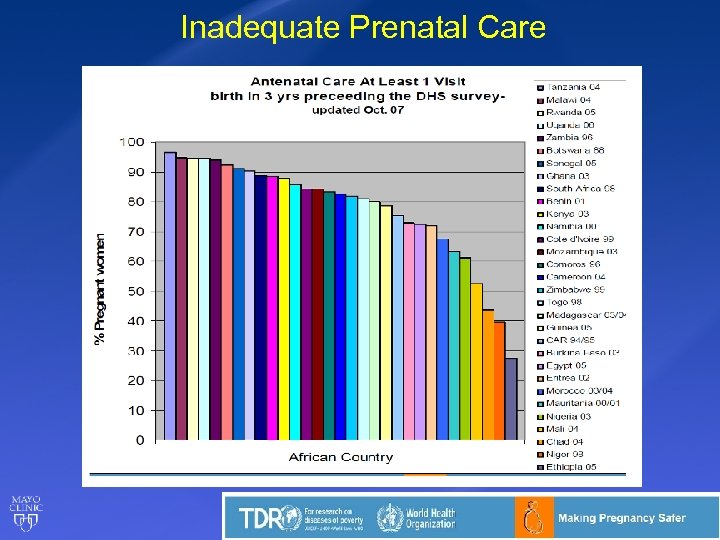 Inadequate Prenatal Care 56 © 2013 MFMER | slide-56
Inadequate Prenatal Care 56 © 2013 MFMER | slide-56
 Prenatal Care ►Requires 1 visit per trimester ►Interventions • Iron/Folate • Fansidar malaria treatment/prophylaxis • IT Bed nets • Tetanus immunization - TT 2 • Advise location of delivery 57 © 2013 MFMER | slide-57
Prenatal Care ►Requires 1 visit per trimester ►Interventions • Iron/Folate • Fansidar malaria treatment/prophylaxis • IT Bed nets • Tetanus immunization - TT 2 • Advise location of delivery 57 © 2013 MFMER | slide-57
 Examining the Care Delivery Value Chain Step By Step © 2013 MFMER | slide-58
Examining the Care Delivery Value Chain Step By Step © 2013 MFMER | slide-58
 Examining the Care Delivery Value Chain • Prevention • Testing/Screening • Staging • Delaying progression of disease • Initiation of therapy • Continuous disease management • Management of deterioration Rhatigan et al. Applying the Care Delivery Value Chain: HIV/AIDS Care in Resource Poor Setttings. Harvard Business School working paper, 2009 © 2013 MFMER | slide-59
Examining the Care Delivery Value Chain • Prevention • Testing/Screening • Staging • Delaying progression of disease • Initiation of therapy • Continuous disease management • Management of deterioration Rhatigan et al. Applying the Care Delivery Value Chain: HIV/AIDS Care in Resource Poor Setttings. Harvard Business School working paper, 2009 © 2013 MFMER | slide-59
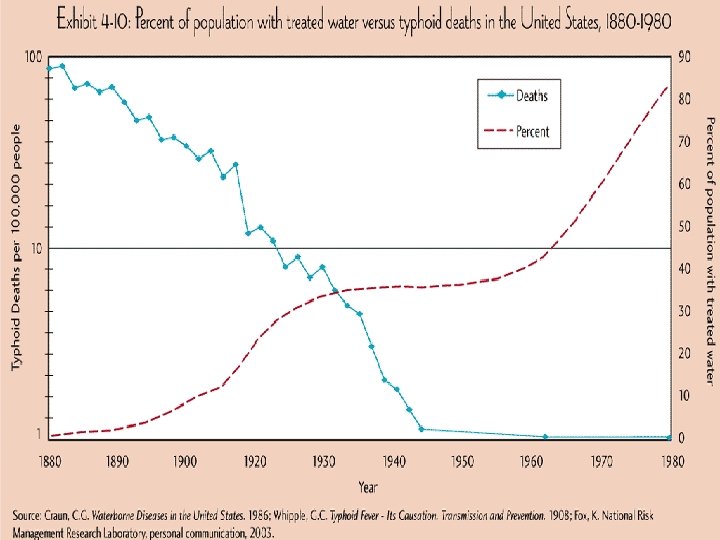
 Cost Effectiveness: Prevention • Lifestyle/public health • Latrines • Hand washing • Clean water (vs pills for NTD’s) • Insecticide treated bed nets • Smoking cessation • Weight loss • Exercise DM 2, HTN • Med Diet 60 © 2013 MFMER | slide-60
Cost Effectiveness: Prevention • Lifestyle/public health • Latrines • Hand washing • Clean water (vs pills for NTD’s) • Insecticide treated bed nets • Smoking cessation • Weight loss • Exercise DM 2, HTN • Med Diet 60 © 2013 MFMER | slide-60
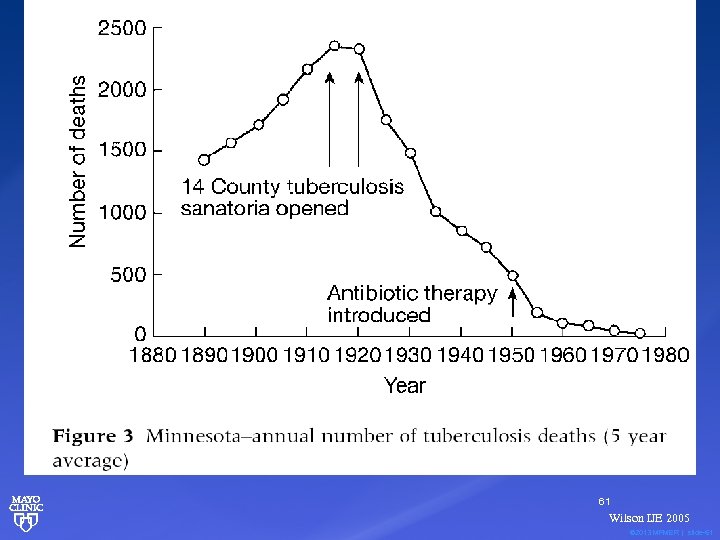 61 Wilson IJE 2005 © 2013 MFMER | slide-61
61 Wilson IJE 2005 © 2013 MFMER | slide-61
 © 2013 MFMER | slide-62
© 2013 MFMER | slide-62
 Cost Effectiveness: Prevention • Lifestyle/public health • Latrines • Hand washing • Clean water (vs pills for NTD’s) • Insecticide treated bed nets • Smoking cessation • Weight loss • Exercise DM 2, HTN • Med Diet • Aspirin CAD 63 © 2013 MFMER | slide-63
Cost Effectiveness: Prevention • Lifestyle/public health • Latrines • Hand washing • Clean water (vs pills for NTD’s) • Insecticide treated bed nets • Smoking cessation • Weight loss • Exercise DM 2, HTN • Med Diet • Aspirin CAD 63 © 2013 MFMER | slide-63
 Cost Effectiveness Diagnosis • Limited labs Choose 1 or 2 • Limited imaging Use rarely • Careful exam Yet efficient • Rare specialists Virtual Consults Textbooks or 64 © 2013 MFMER | slide-64
Cost Effectiveness Diagnosis • Limited labs Choose 1 or 2 • Limited imaging Use rarely • Careful exam Yet efficient • Rare specialists Virtual Consults Textbooks or 64 © 2013 MFMER | slide-64
 Empiric Rx: WHO IMCI (Integrated Management of Childhood Illness) – Syndromic Diagnoses • Cough (and fever) • Increased respiratory rate • ≥ 60 if age < 2 mos. • ≥ 50 if age 2 -12 mos. • ≥ 40 if age 12 mos. to 5 years = Pneumonia • Lower chest retractions • (Hypoxia, crackles, percussed dullness rather than CXR) 65 © 2013 MFMER | slide-65
Empiric Rx: WHO IMCI (Integrated Management of Childhood Illness) – Syndromic Diagnoses • Cough (and fever) • Increased respiratory rate • ≥ 60 if age < 2 mos. • ≥ 50 if age 2 -12 mos. • ≥ 40 if age 12 mos. to 5 years = Pneumonia • Lower chest retractions • (Hypoxia, crackles, percussed dullness rather than CXR) 65 © 2013 MFMER | slide-65
 Cost Effectiveness • Treatment • Lifestyle/public health Sustainable cheap • Essential meds No fru-fru • Efficient treatment of chronic disease • Balance NNTB / NNTH Mental Math • Avoid futility End of life care 66 © 2013 MFMER | slide-66
Cost Effectiveness • Treatment • Lifestyle/public health Sustainable cheap • Essential meds No fru-fru • Efficient treatment of chronic disease • Balance NNTB / NNTH Mental Math • Avoid futility End of life care 66 © 2013 MFMER | slide-66
 Cost Effective Care • Treatment • Lifestyle/public health Sustainable cheap • Essential meds and meds only when essential • No treatment for URI’s, most OM, conjunctivitis, sinusitis, acute bronchitis • I & D not antibiotic for abscess • No expensive junk 67 © 2013 MFMER | slide-67
Cost Effective Care • Treatment • Lifestyle/public health Sustainable cheap • Essential meds and meds only when essential • No treatment for URI’s, most OM, conjunctivitis, sinusitis, acute bronchitis • I & D not antibiotic for abscess • No expensive junk 67 © 2013 MFMER | slide-67
 Cost Effective Care • Treatment • Lifestyle/public health Sustainable cheap • Essential meds No fru-fru • Task Shifting - Increase access and lower costs 68 © 2013 MFMER | slide-68
Cost Effective Care • Treatment • Lifestyle/public health Sustainable cheap • Essential meds No fru-fru • Task Shifting - Increase access and lower costs 68 © 2013 MFMER | slide-68
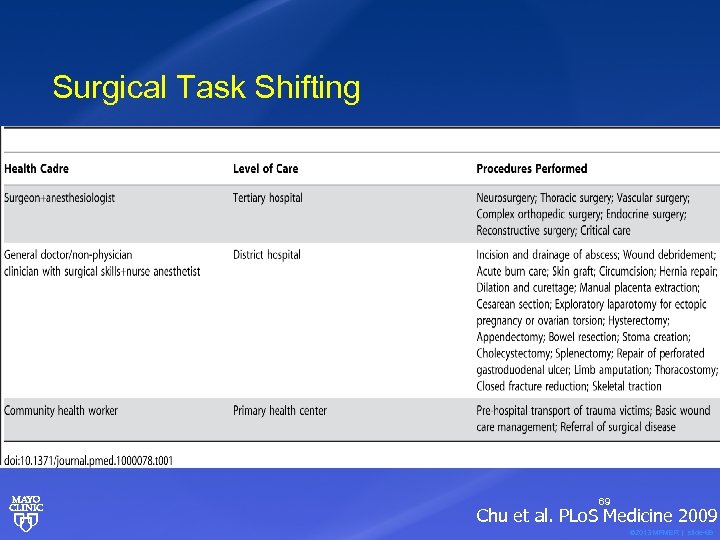 Surgical Task Shifting 69 Chu et al. PLo. S Medicine 2009 © 2013 MFMER | slide-69
Surgical Task Shifting 69 Chu et al. PLo. S Medicine 2009 © 2013 MFMER | slide-69
 Surgical Task Shifting 70 Merry, World J Surg, 2011 © 2013 MFMER | slide-70
Surgical Task Shifting 70 Merry, World J Surg, 2011 © 2013 MFMER | slide-70
 Cost Effective Care • Treatment • Lifestyle/public health Sustainable cheap • Essential meds No fru-fru • Task Shifting Access • Efficient treatment of chronic disease • Pills if treatment saves life for < 3 x per capita GNP (3 x personal income? ) 71 © 2013 MFMER | slide-71
Cost Effective Care • Treatment • Lifestyle/public health Sustainable cheap • Essential meds No fru-fru • Task Shifting Access • Efficient treatment of chronic disease • Pills if treatment saves life for < 3 x per capita GNP (3 x personal income? ) 71 © 2013 MFMER | slide-71
 Cost Effective Care • Treatment • Lifestyle/public health Sustainable cheap • Essential meds No fru-fru • Efficient treatment of chronic disease • Task Shifting Access • Balance NNTB / NNTH Mental Math 72 © 2013 MFMER | slide-72
Cost Effective Care • Treatment • Lifestyle/public health Sustainable cheap • Essential meds No fru-fru • Efficient treatment of chronic disease • Task Shifting Access • Balance NNTB / NNTH Mental Math 72 © 2013 MFMER | slide-72
 Cost Effective Care • Treatment • Lifestyle/public health Sustainable cheap • Essential meds No fru-fru • Efficient treatment of chronic disease • Task Shifting Access • Balance NNTB / NNTH • Avoid futility care Mental Math End of life 73 © 2013 MFMER | slide-73
Cost Effective Care • Treatment • Lifestyle/public health Sustainable cheap • Essential meds No fru-fru • Efficient treatment of chronic disease • Task Shifting Access • Balance NNTB / NNTH • Avoid futility care Mental Math End of life 73 © 2013 MFMER | slide-73
 Cost Effective Care • Treatment • Avoid futility - intensive care of terminal patients • Helping patients/families accept death and place their trust in Jesus • Learning to die well – hospice, chaplains, pastors, community 74 © 2013 MFMER | slide-74
Cost Effective Care • Treatment • Avoid futility - intensive care of terminal patients • Helping patients/families accept death and place their trust in Jesus • Learning to die well – hospice, chaplains, pastors, community 74 © 2013 MFMER | slide-74
 Cost Effective Care • Treatment • Lifestyle/public health • Essential meds • Efficient treatment of chronic disease • Task Shifting • Balance NNTB / NNTH • Avoid futility 75 © 2013 MFMER | slide-75
Cost Effective Care • Treatment • Lifestyle/public health • Essential meds • Efficient treatment of chronic disease • Task Shifting • Balance NNTB / NNTH • Avoid futility 75 © 2013 MFMER | slide-75
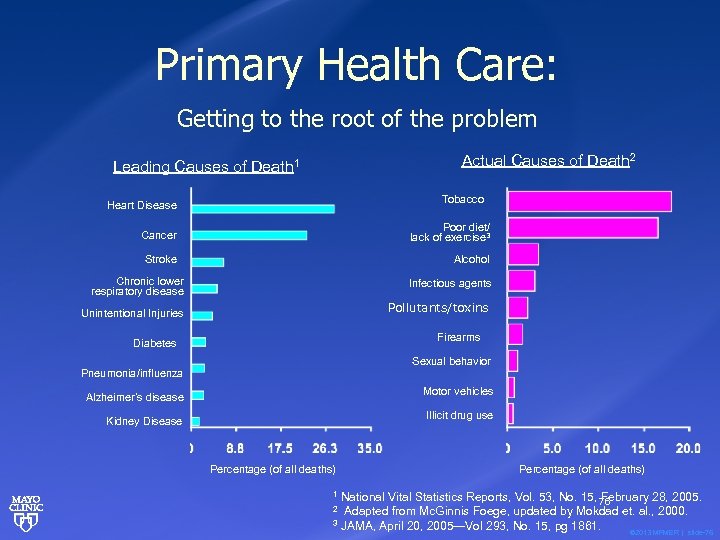 Primary Health Care: Getting to the root of the problem Actual Causes of Death 2 Leading Causes of Death 1 Tobacco Heart Disease Cancer Poor diet/ lack of exercise 3 Stroke Alcohol Chronic lower respiratory disease Infectious agents Pollutants/toxins Unintentional Injuries Firearms Diabetes Sexual behavior Pneumonia/influenza Motor vehicles Alzheimer’s disease Illicit drug use Kidney Disease Percentage (of all deaths) 1 National Vital Statistics Reports, Vol. 53, No. 15, February 28, 2005. 76 2 Adapted from Mc. Ginnis Foege, updated by Mokdad et. al. , 2000. 3 JAMA, April 20, 2005—Vol 293, No. 15, pg 1861. © 2013 MFMER | slide-76
Primary Health Care: Getting to the root of the problem Actual Causes of Death 2 Leading Causes of Death 1 Tobacco Heart Disease Cancer Poor diet/ lack of exercise 3 Stroke Alcohol Chronic lower respiratory disease Infectious agents Pollutants/toxins Unintentional Injuries Firearms Diabetes Sexual behavior Pneumonia/influenza Motor vehicles Alzheimer’s disease Illicit drug use Kidney Disease Percentage (of all deaths) 1 National Vital Statistics Reports, Vol. 53, No. 15, February 28, 2005. 76 2 Adapted from Mc. Ginnis Foege, updated by Mokdad et. al. , 2000. 3 JAMA, April 20, 2005—Vol 293, No. 15, pg 1861. © 2013 MFMER | slide-76
 Case 4: The Anginal African Farmer You’re seeing a 55 yo African small business owner who presents with angina. He smokes a few cigarettes per day, eats a reasonable diet though high salt. Exam shows a BMI of 33, BP 160/105, otherwise normal exam. In order of most to least importance, which of the following would you do? a)Advise weight loss b)Control HTN with a B-blocker c)Smoking cessation d)Lipid lowering to LDL < 70 e)Advise he exercise daily © 2013 MFMER | slide-77
Case 4: The Anginal African Farmer You’re seeing a 55 yo African small business owner who presents with angina. He smokes a few cigarettes per day, eats a reasonable diet though high salt. Exam shows a BMI of 33, BP 160/105, otherwise normal exam. In order of most to least importance, which of the following would you do? a)Advise weight loss b)Control HTN with a B-blocker c)Smoking cessation d)Lipid lowering to LDL < 70 e)Advise he exercise daily © 2013 MFMER | slide-77
 Closing Thoughts • Academic cost effectiveness analysis depends on presuppositions about benefits and harms. • Docs in Cost Effective Care folder • HIV/AIDS meningitis care – Boulware et al • NCD’s in Asia BMJ and book chapter NCD’s • Best Buys • MDG’s and Diabetes – Interest group driven • Harvard Business School paper © 2013 MFMER | slide-78
Closing Thoughts • Academic cost effectiveness analysis depends on presuppositions about benefits and harms. • Docs in Cost Effective Care folder • HIV/AIDS meningitis care – Boulware et al • NCD’s in Asia BMJ and book chapter NCD’s • Best Buys • MDG’s and Diabetes – Interest group driven • Harvard Business School paper © 2013 MFMER | slide-78
 Medical Missionaries Behaving Well • Follow country MOH treatment protocols • Focus on prevention • Treat patients intelligently with regard to absolute benefits and all costs and the patient’s financial resources. © 2013 MFMER | slide-79
Medical Missionaries Behaving Well • Follow country MOH treatment protocols • Focus on prevention • Treat patients intelligently with regard to absolute benefits and all costs and the patient’s financial resources. © 2013 MFMER | slide-79
 Learning Objectives • Treat chronic diseases in adults and children in resource limited settings in a rational, costeffective way. • Follow an income and country GNP based protocol for hypertension, type 1 and 2 diabetes, hyperlipidemia, and coronary artery disease diagnosis and care. • Design treatment protocols based on guiding principles of cost-effectiveness. 80 © 2013 MFMER | slide-80
Learning Objectives • Treat chronic diseases in adults and children in resource limited settings in a rational, costeffective way. • Follow an income and country GNP based protocol for hypertension, type 1 and 2 diabetes, hyperlipidemia, and coronary artery disease diagnosis and care. • Design treatment protocols based on guiding principles of cost-effectiveness. 80 © 2013 MFMER | slide-80
 Questions & Discussion © 2013 MFMER | slide-81
Questions & Discussion © 2013 MFMER | slide-81


