8f938a93a24b2797243fce98fc618767.ppt
- Количество слайдов: 49
 Cost-effectiveness Analysis Mihail Samnaliev, Ph. D Senior Health Economist Children's Hospital Boston ________ The speaker for this session has reported NO FINANCIAL RELATIONSHIPS with a commercial entity producing healthcarerelated products and/or services 1
Cost-effectiveness Analysis Mihail Samnaliev, Ph. D Senior Health Economist Children's Hospital Boston ________ The speaker for this session has reported NO FINANCIAL RELATIONSHIPS with a commercial entity producing healthcarerelated products and/or services 1
 Outline Definitions, applications Measuring costs Measures of effectiveness: QALYs , other Estimation of health-related quality of life Uncertainty analyses 2
Outline Definitions, applications Measuring costs Measures of effectiveness: QALYs , other Estimation of health-related quality of life Uncertainty analyses 2
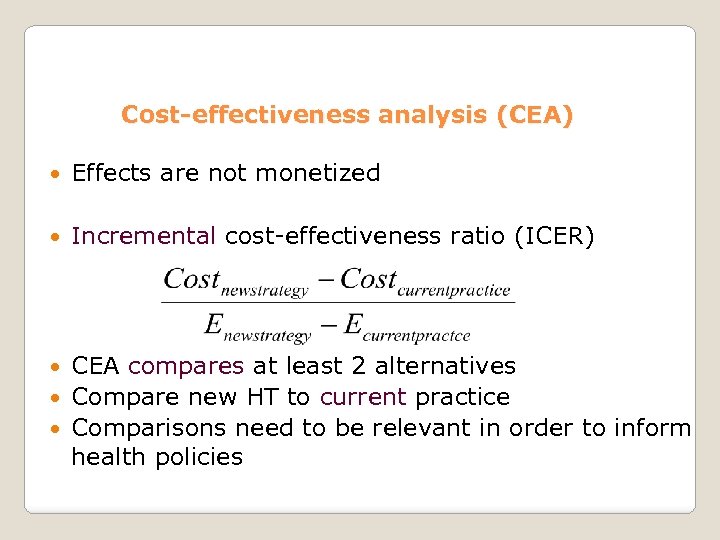 Cost-effectiveness analysis (CEA) Effects are not monetized Incremental cost-effectiveness ratio (ICER) CEA compares at least 2 alternatives Compare new HT to current practice Comparisons need to be relevant in order to inform health policies
Cost-effectiveness analysis (CEA) Effects are not monetized Incremental cost-effectiveness ratio (ICER) CEA compares at least 2 alternatives Compare new HT to current practice Comparisons need to be relevant in order to inform health policies
 Cost-effectiveness of new health technology vs. current practice I Less effective & more costly II More effective & more costly (dominated) III IV Less effective &less costly More effective &less costly (dominant) 4
Cost-effectiveness of new health technology vs. current practice I Less effective & more costly II More effective & more costly (dominated) III IV Less effective &less costly More effective &less costly (dominant) 4
 When is an intervention cost-effective? 1. If it is both less expensive and more effective Often would not present ICER, but differences in costs and effectiveness only OR 2. If it is more expensive (than alternatives) but costs < willingness to pay /additional unit of effectiveness Cost-effectiveness does not necessarily mean cost saving 5
When is an intervention cost-effective? 1. If it is both less expensive and more effective Often would not present ICER, but differences in costs and effectiveness only OR 2. If it is more expensive (than alternatives) but costs < willingness to pay /additional unit of effectiveness Cost-effectiveness does not necessarily mean cost saving 5
 Calculating maximum (threshold) WTP per additional life year or QALY 1. The human capital approach ◦ Easy to implement ◦ Based on one’s earnings (economic output) Limitations Underestimates value for persons who are not working Not based on economic theory 6
Calculating maximum (threshold) WTP per additional life year or QALY 1. The human capital approach ◦ Easy to implement ◦ Based on one’s earnings (economic output) Limitations Underestimates value for persons who are not working Not based on economic theory 6
 Calculating WTP per additional life year or QALY 2. Hypothetical valuations + based on economic theory - methodological limitations Example: Ask individuals with persistent asthma about willingness to pay for a medication that reduces symptom days by 1 per week. 7
Calculating WTP per additional life year or QALY 2. Hypothetical valuations + based on economic theory - methodological limitations Example: Ask individuals with persistent asthma about willingness to pay for a medication that reduces symptom days by 1 per week. 7
 Calculating WTP per additional life year or QALY 3. Revealed preferences, e. g. wage differentials between jobs associated with different risk of death Recommendations $50, 000 and $100, 000 /QALY often used in the US WHO thresholds based on GDP/per capita Depends for other measures of effectiveness; WTP threshold may or may not exist Common practice: p [ cost-effective ] at different WTP ◦ Very cost-effective if ICER < GDP /QALY, Cost effective if 1 to 3 times GDP /QALY, Cost-ineffective if > 3 times GDP /QALY 8
Calculating WTP per additional life year or QALY 3. Revealed preferences, e. g. wage differentials between jobs associated with different risk of death Recommendations $50, 000 and $100, 000 /QALY often used in the US WHO thresholds based on GDP/per capita Depends for other measures of effectiveness; WTP threshold may or may not exist Common practice: p [ cost-effective ] at different WTP ◦ Very cost-effective if ICER < GDP /QALY, Cost effective if 1 to 3 times GDP /QALY, Cost-ineffective if > 3 times GDP /QALY 8
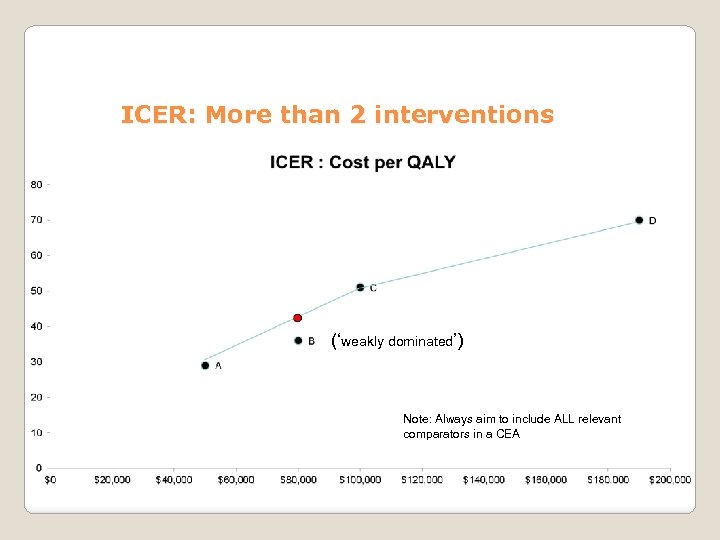 ICER: More than 2 interventions (‘weakly dominated’) Note: Always aim to include ALL relevant comparators in a CEA
ICER: More than 2 interventions (‘weakly dominated’) Note: Always aim to include ALL relevant comparators in a CEA
 CEA applications UK: cost/QALY considered by NHS in reimbursement decisions Not mandatory in most other countries; with varying degree of impact on decision makers Cost/QALY not used for federal reimbursement decisions in the US ; sometimes used by private payers; impacts reimbursement decisions more indirectly; widely used in research
CEA applications UK: cost/QALY considered by NHS in reimbursement decisions Not mandatory in most other countries; with varying degree of impact on decision makers Cost/QALY not used for federal reimbursement decisions in the US ; sometimes used by private payers; impacts reimbursement decisions more indirectly; widely used in research
 Example Blood cancer drug Adcetris (Brentuximab vedotin) approved by the FDA in 2011 Effective compared to no treatment A course of treatment can exceed $100, 000 Q: Decision makers (e. g. a payer): Reimburse or are public health gains expected to be higher if resources are invested elsewhere ? ◦ If no alternative/rare condition, CEA may have much less impact on decision making ◦ If many alternatives already used, CEA more relevant
Example Blood cancer drug Adcetris (Brentuximab vedotin) approved by the FDA in 2011 Effective compared to no treatment A course of treatment can exceed $100, 000 Q: Decision makers (e. g. a payer): Reimburse or are public health gains expected to be higher if resources are invested elsewhere ? ◦ If no alternative/rare condition, CEA may have much less impact on decision making ◦ If many alternatives already used, CEA more relevant
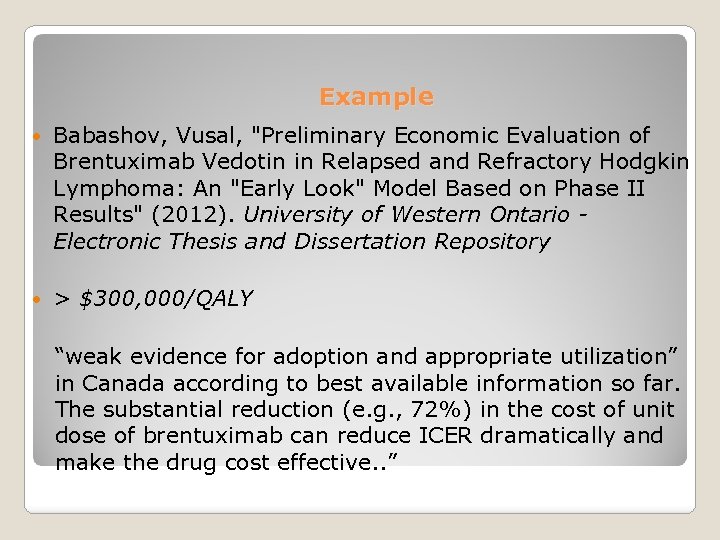 Example Babashov, Vusal, "Preliminary Economic Evaluation of Brentuximab Vedotin in Relapsed and Refractory Hodgkin Lymphoma: An "Early Look" Model Based on Phase II Results" (2012). University of Western Ontario Electronic Thesis and Dissertation Repository > $300, 000/QALY “weak evidence for adoption and appropriate utilization” in Canada according to best available information so far. The substantial reduction (e. g. , 72%) in the cost of unit dose of brentuximab can reduce ICER dramatically and make the drug cost effective. . ”
Example Babashov, Vusal, "Preliminary Economic Evaluation of Brentuximab Vedotin in Relapsed and Refractory Hodgkin Lymphoma: An "Early Look" Model Based on Phase II Results" (2012). University of Western Ontario Electronic Thesis and Dissertation Repository > $300, 000/QALY “weak evidence for adoption and appropriate utilization” in Canada according to best available information so far. The substantial reduction (e. g. , 72%) in the cost of unit dose of brentuximab can reduce ICER dramatically and make the drug cost effective. . ”
 Example 2. How existing CEA can be used (but are not) by policy makers to improve public health outcomes Intervention Cost per (qualityadjusted) life year Extended buprenorphine-naloxone Tx for opioiddependent youth (Polsky et al. 2010 Addiction) $25, 049 Screening every 5 years, vs. a one-time screening program for HIV (Sanders et al. 2005 NEJM) $57, 138 Airline security (paying for air marshals on planes) > $4 million 1 (Stewart and Mueller 2008) ($180 million / life saved) Own calculation More cost-effective interventions buy more QALY-s / each additional dollar 1 13
Example 2. How existing CEA can be used (but are not) by policy makers to improve public health outcomes Intervention Cost per (qualityadjusted) life year Extended buprenorphine-naloxone Tx for opioiddependent youth (Polsky et al. 2010 Addiction) $25, 049 Screening every 5 years, vs. a one-time screening program for HIV (Sanders et al. 2005 NEJM) $57, 138 Airline security (paying for air marshals on planes) > $4 million 1 (Stewart and Mueller 2008) ($180 million / life saved) Own calculation More cost-effective interventions buy more QALY-s / each additional dollar 1 13
 Outline Definitions, applications Measuring costs Measures of effectiveness: QALYs , other Estimation of health-related quality of life Uncertainty analyses and presentation of results CEA in clinical trials 14
Outline Definitions, applications Measuring costs Measures of effectiveness: QALYs , other Estimation of health-related quality of life Uncertainty analyses and presentation of results CEA in clinical trials 14
 Measurement of costs Opportunity costs (economic costs): the forgone value of the best alternative use of the same resources used for the intervention In theory , reflected in competitive market prices Expressing in $ allows within/cross sector comparisons Perspective: societal, payer, provider 15
Measurement of costs Opportunity costs (economic costs): the forgone value of the best alternative use of the same resources used for the intervention In theory , reflected in competitive market prices Expressing in $ allows within/cross sector comparisons Perspective: societal, payer, provider 15
 Measurement of costs Focus on resources expected to change as a result of the intervention Often go a step further and focus on major cost drivers Exclude protocol-driven costs (not incurred otherwise) Use local costs (whenever possible), at the level of decision making Use costs from the perspective of the decision maker (e. g. , societal, payer, provider) Aim to capture all costs over entire analytic timeframe Note: there is often a great deal of variability around cost estimates (theoretical and empirical reasons), much larger than clinical outcomes 16
Measurement of costs Focus on resources expected to change as a result of the intervention Often go a step further and focus on major cost drivers Exclude protocol-driven costs (not incurred otherwise) Use local costs (whenever possible), at the level of decision making Use costs from the perspective of the decision maker (e. g. , societal, payer, provider) Aim to capture all costs over entire analytic timeframe Note: there is often a great deal of variability around cost estimates (theoretical and empirical reasons), much larger than clinical outcomes 16
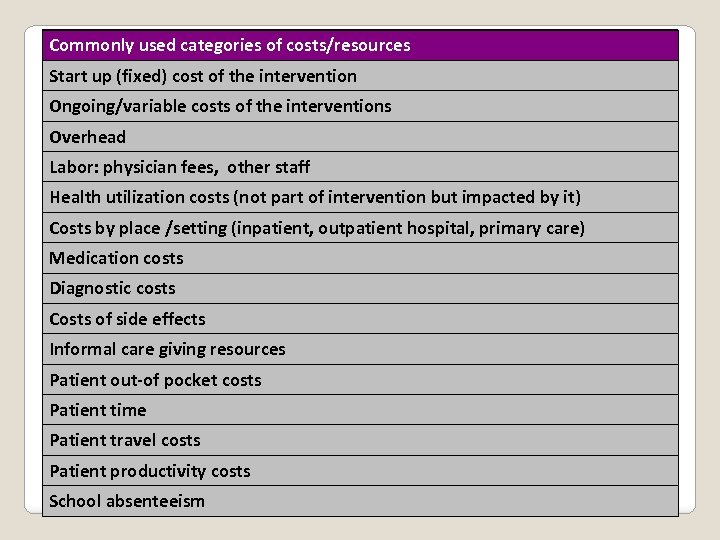 Commonly used categories of costs/resources Start up (fixed) cost of the intervention Ongoing/variable costs of the interventions Overhead Labor: physician fees, other staff Health utilization costs (not part of intervention but impacted by it) Costs by place /setting (inpatient, outpatient hospital, primary care) Medication costs Diagnostic costs Costs of side effects Informal care giving resources Patient out-of pocket costs Patient time Patient travel costs Patient productivity costs School absenteeism
Commonly used categories of costs/resources Start up (fixed) cost of the intervention Ongoing/variable costs of the interventions Overhead Labor: physician fees, other staff Health utilization costs (not part of intervention but impacted by it) Costs by place /setting (inpatient, outpatient hospital, primary care) Medication costs Diagnostic costs Costs of side effects Informal care giving resources Patient out-of pocket costs Patient time Patient travel costs Patient productivity costs School absenteeism
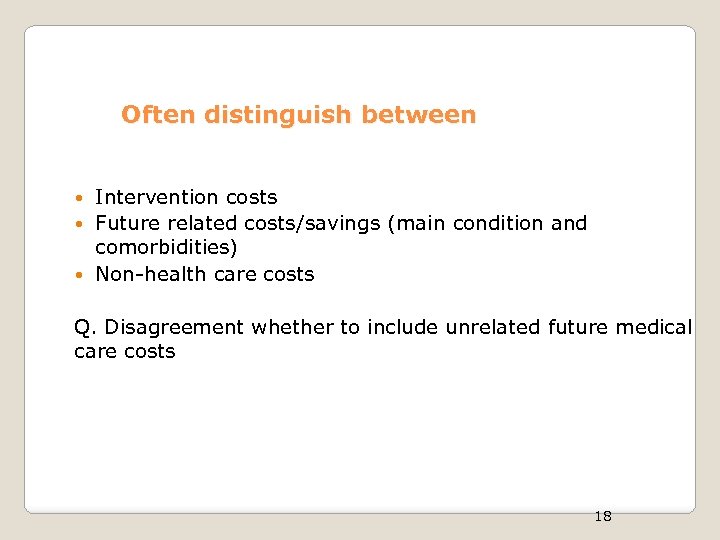 Often distinguish between Intervention costs Future related costs/savings (main condition and comorbidities) Non-health care costs Q. Disagreement whether to include unrelated future medical care costs 18
Often distinguish between Intervention costs Future related costs/savings (main condition and comorbidities) Non-health care costs Q. Disagreement whether to include unrelated future medical care costs 18
 Outline Definitions, applications Measuring costs Measures of effectiveness: QALYs , other Estimation of health-related quality of life Uncertainty analyses and presentation of results Issues specific to pediatric populations CEA in clinical trials Incorporating CEA into grant proposals Review of a CEA (if time permits/leave for 3 rd lecture) 19
Outline Definitions, applications Measuring costs Measures of effectiveness: QALYs , other Estimation of health-related quality of life Uncertainty analyses and presentation of results Issues specific to pediatric populations CEA in clinical trials Incorporating CEA into grant proposals Review of a CEA (if time permits/leave for 3 rd lecture) 19
 II Measures of effectiveness: QALYs Quality-adjusted life years (QALYs) ◦ The recommended measure in CEA ◦ Allows comparisons across interventions ◦ Comprehensive: combines life expectancy & health-related Qo. L (HRQL) Treatment can result in ◦ Better HRQL ◦ Increased life expectancy ◦ Both 20
II Measures of effectiveness: QALYs Quality-adjusted life years (QALYs) ◦ The recommended measure in CEA ◦ Allows comparisons across interventions ◦ Comprehensive: combines life expectancy & health-related Qo. L (HRQL) Treatment can result in ◦ Better HRQL ◦ Increased life expectancy ◦ Both 20
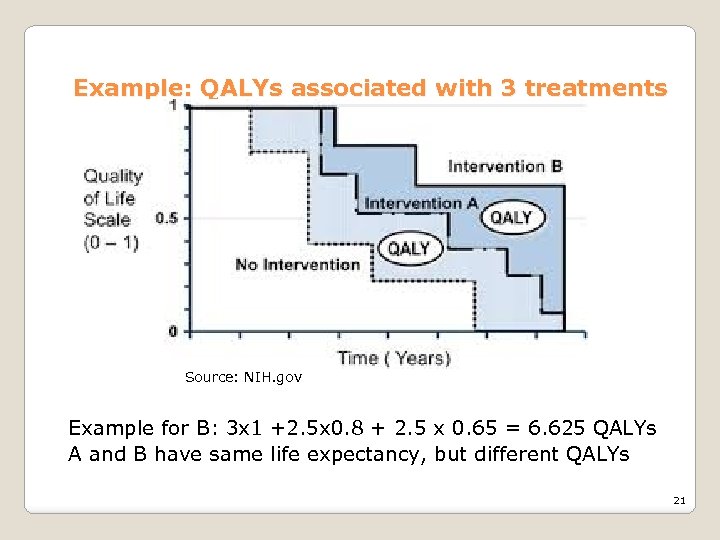 Example: QALYs associated with 3 treatments Source: NIH. gov Example for B: 3 x 1 +2. 5 x 0. 8 + 2. 5 x 0. 65 = 6. 625 QALYs A and B have same life expectancy, but different QALYs 21
Example: QALYs associated with 3 treatments Source: NIH. gov Example for B: 3 x 1 +2. 5 x 0. 8 + 2. 5 x 0. 65 = 6. 625 QALYs A and B have same life expectancy, but different QALYs 21
 Health related quality of life (HRQL) Utility (weights): elicited from patients, based on their preferences Typically measured on a scale 0 to 1, however some instruments allow utility < 0 (worse than death) In contrast, many surveys capture clinical status but are not preference – based. These are not recommended for CEA ◦ For example, 0. 75 scored on Peds. QL does not mean that patients value their health at 0. 75 How do we measure patient preferences /utilities associated with specific health states? 22
Health related quality of life (HRQL) Utility (weights): elicited from patients, based on their preferences Typically measured on a scale 0 to 1, however some instruments allow utility < 0 (worse than death) In contrast, many surveys capture clinical status but are not preference – based. These are not recommended for CEA ◦ For example, 0. 75 scored on Peds. QL does not mean that patients value their health at 0. 75 How do we measure patient preferences /utilities associated with specific health states? 22
 Measuring HRQL Direct methods ◦ Standard Gamble, Time Trade Off, Visual Analogue Scale Preference based surveys ◦ Generic: HUI, EQ-5 D, SF-36, Quality of Well-Being ◦ Disease specific surveys Borrow from published studies 23
Measuring HRQL Direct methods ◦ Standard Gamble, Time Trade Off, Visual Analogue Scale Preference based surveys ◦ Generic: HUI, EQ-5 D, SF-36, Quality of Well-Being ◦ Disease specific surveys Borrow from published studies 23
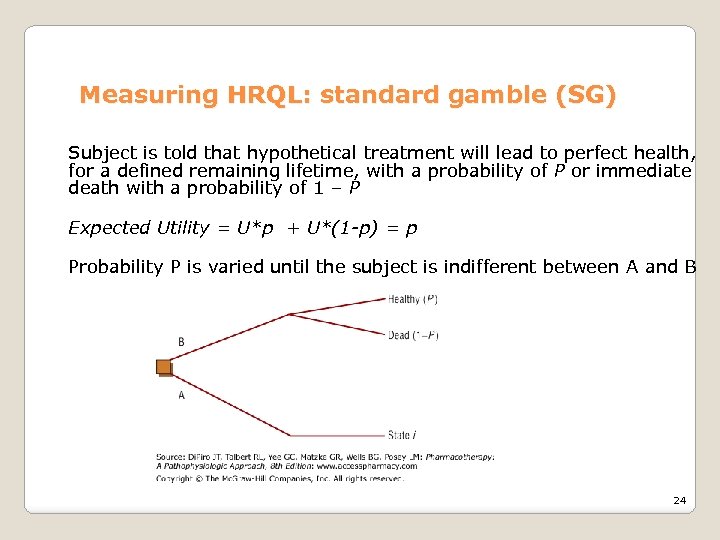 Measuring HRQL: standard gamble (SG) Subject is told that hypothetical treatment will lead to perfect health, for a defined remaining lifetime, with a probability of P or immediate death with a probability of 1 – P Expected Utility = U*p + U*(1 -p) = p Probability P is varied until the subject is indifferent between A and B 24
Measuring HRQL: standard gamble (SG) Subject is told that hypothetical treatment will lead to perfect health, for a defined remaining lifetime, with a probability of P or immediate death with a probability of 1 – P Expected Utility = U*p + U*(1 -p) = p Probability P is varied until the subject is indifferent between A and B 24
 Measuring HRQL: Time trade-off (TTO) Subject is offered 2 alternatives: 1. State i for time t (life expectancy for the individual with the chronic condition) 2. Healthy for time x < t, followed by death Utility for state i= x/t 25
Measuring HRQL: Time trade-off (TTO) Subject is offered 2 alternatives: 1. State i for time t (life expectancy for the individual with the chronic condition) 2. Healthy for time x < t, followed by death Utility for state i= x/t 25
 Measuring HRQL: visual analogue scale (VAS) (Source : Euro. Qol. org) Subject is asked to score their health on a scale from 0 to 100. 26
Measuring HRQL: visual analogue scale (VAS) (Source : Euro. Qol. org) Subject is asked to score their health on a scale from 0 to 100. 26
 Measuring HRQL Direct methods ◦ Standard Gamble, Time Trade Off, Visual Analogue Scale Preference based surveys ◦ Generic: EQ-5 D, HUI, SF-36, Quality of Well-Being ◦ Disease specific Borrow from published studies 27
Measuring HRQL Direct methods ◦ Standard Gamble, Time Trade Off, Visual Analogue Scale Preference based surveys ◦ Generic: EQ-5 D, HUI, SF-36, Quality of Well-Being ◦ Disease specific Borrow from published studies 27
 HUI and EQ-5 D HUI (versions 2 and 3) and Eq-5 D : based on preferences elicited from the general population A representative sample is administered SG /TTO or VAS These are then mapped onto select health states One can then directly use a health classification system and a scoring formula based on the responses from above samples 28
HUI and EQ-5 D HUI (versions 2 and 3) and Eq-5 D : based on preferences elicited from the general population A representative sample is administered SG /TTO or VAS These are then mapped onto select health states One can then directly use a health classification system and a scoring formula based on the responses from above samples 28
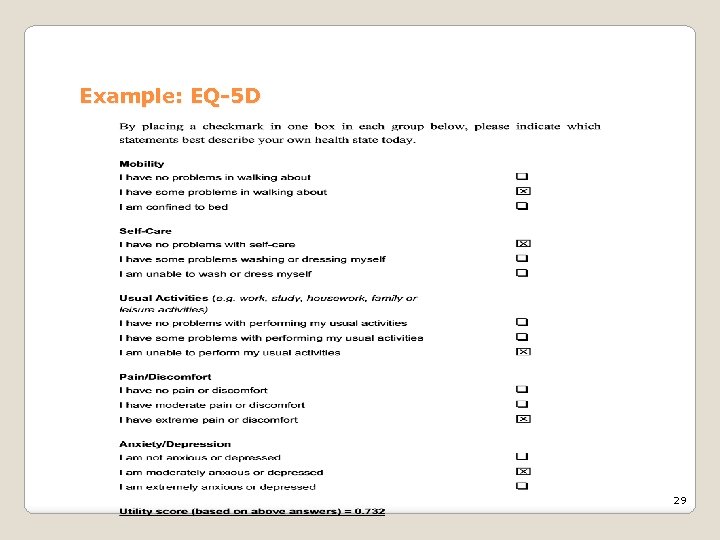 Example: EQ-5 D 29
Example: EQ-5 D 29
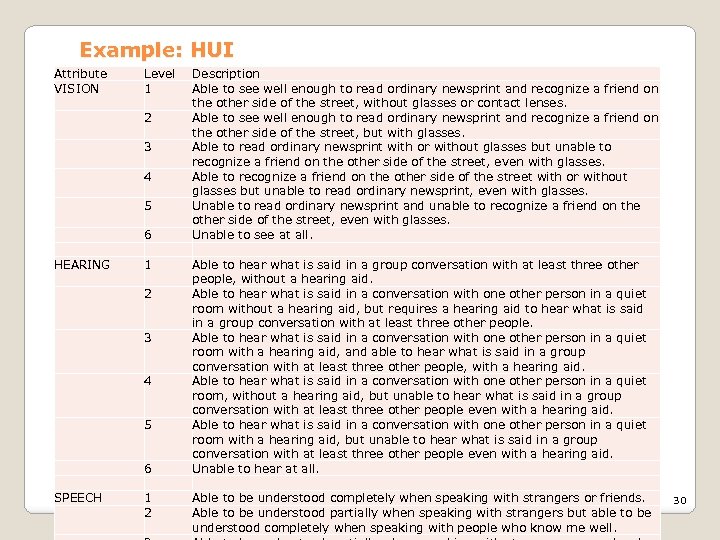 Example: HUI Attribute VISION Level 1 2 3 4 5 HEARING 6 1 2 3 4 5 SPEECH 6 1 2 Description Able to see well enough to read ordinary newsprint and recognize a friend on the other side of the street, without glasses or contact lenses. Able to see well enough to read ordinary newsprint and recognize a friend on the other side of the street, but with glasses. Able to read ordinary newsprint with or without glasses but unable to recognize a friend on the other side of the street, even with glasses. Able to recognize a friend on the other side of the street with or without glasses but unable to read ordinary newsprint, even with glasses. Unable to read ordinary newsprint and unable to recognize a friend on the other side of the street, even with glasses. Unable to see at all. Able to hear what is said in a group conversation with at least three other people, without a hearing aid. Able to hear what is said in a conversation with one other person in a quiet room without a hearing aid, but requires a hearing aid to hear what is said in a group conversation with at least three other people. Able to hear what is said in a conversation with one other person in a quiet room with a hearing aid, and able to hear what is said in a group conversation with at least three other people, with a hearing aid. Able to hear what is said in a conversation with one other person in a quiet room, without a hearing aid, but unable to hear what is said in a group conversation with at least three other people even with a hearing aid. Able to hear what is said in a conversation with one other person in a quiet room with a hearing aid, but unable to hear what is said in a group conversation with at least three other people even with a hearing aid. Unable to hear at all. Able to be understood completely when speaking with strangers or friends. 30 Able to be understood partially when speaking with strangers but able to be understood completely when speaking with people who know me well.
Example: HUI Attribute VISION Level 1 2 3 4 5 HEARING 6 1 2 3 4 5 SPEECH 6 1 2 Description Able to see well enough to read ordinary newsprint and recognize a friend on the other side of the street, without glasses or contact lenses. Able to see well enough to read ordinary newsprint and recognize a friend on the other side of the street, but with glasses. Able to read ordinary newsprint with or without glasses but unable to recognize a friend on the other side of the street, even with glasses. Able to recognize a friend on the other side of the street with or without glasses but unable to read ordinary newsprint, even with glasses. Unable to read ordinary newsprint and unable to recognize a friend on the other side of the street, even with glasses. Unable to see at all. Able to hear what is said in a group conversation with at least three other people, without a hearing aid. Able to hear what is said in a conversation with one other person in a quiet room without a hearing aid, but requires a hearing aid to hear what is said in a group conversation with at least three other people. Able to hear what is said in a conversation with one other person in a quiet room with a hearing aid, and able to hear what is said in a group conversation with at least three other people, with a hearing aid. Able to hear what is said in a conversation with one other person in a quiet room, without a hearing aid, but unable to hear what is said in a group conversation with at least three other people even with a hearing aid. Able to hear what is said in a conversation with one other person in a quiet room with a hearing aid, but unable to hear what is said in a group conversation with at least three other people even with a hearing aid. Unable to hear at all. Able to be understood completely when speaking with strangers or friends. 30 Able to be understood partially when speaking with strangers but able to be understood completely when speaking with people who know me well.
 Example: HUI VISION Level 2 HEARIN AMBULA DEXTER EMOTIO COGNIT SPEECH G TION ITY N ION 1 1 2 1 PAIN 3 u = 1. 371 (0. 98 * 1. 00 * 0. 93 * 1. 00 * 0. 95 * 1. 00 * 0. 90) - 0. 371 = 0. 70 The scoring formula above is based on the standard gamble utilities measured on the general public Source: HUI ® (http: //www. healthutilities. com/) 31
Example: HUI VISION Level 2 HEARIN AMBULA DEXTER EMOTIO COGNIT SPEECH G TION ITY N ION 1 1 2 1 PAIN 3 u = 1. 371 (0. 98 * 1. 00 * 0. 93 * 1. 00 * 0. 95 * 1. 00 * 0. 90) - 0. 371 = 0. 70 The scoring formula above is based on the standard gamble utilities measured on the general public Source: HUI ® (http: //www. healthutilities. com/) 31
 HRQL : Disease-specific instruments Example: Asthma Quality of Life Questionnaire 32 questions in 4 domains (symptoms, activity limitation, emotional function and environmental stimuli) + More sensitive to changes in health status - My miss other important impacts on health (e. g. associated with comorbidities -Often not scored (but some are mapped onto the generic based instruments) 32
HRQL : Disease-specific instruments Example: Asthma Quality of Life Questionnaire 32 questions in 4 domains (symptoms, activity limitation, emotional function and environmental stimuli) + More sensitive to changes in health status - My miss other important impacts on health (e. g. associated with comorbidities -Often not scored (but some are mapped onto the generic based instruments) 32
 Measuring HRQL Direct methods ◦ Standard Gamble, Time Trade Off, Visual Analogue Scale Preference based surveys ◦ Generic: HUI, EQ-5 D, SF-36, Quality of Well-Being ◦ Disease specific Borrow from published studies 33
Measuring HRQL Direct methods ◦ Standard Gamble, Time Trade Off, Visual Analogue Scale Preference based surveys ◦ Generic: HUI, EQ-5 D, SF-36, Quality of Well-Being ◦ Disease specific Borrow from published studies 33
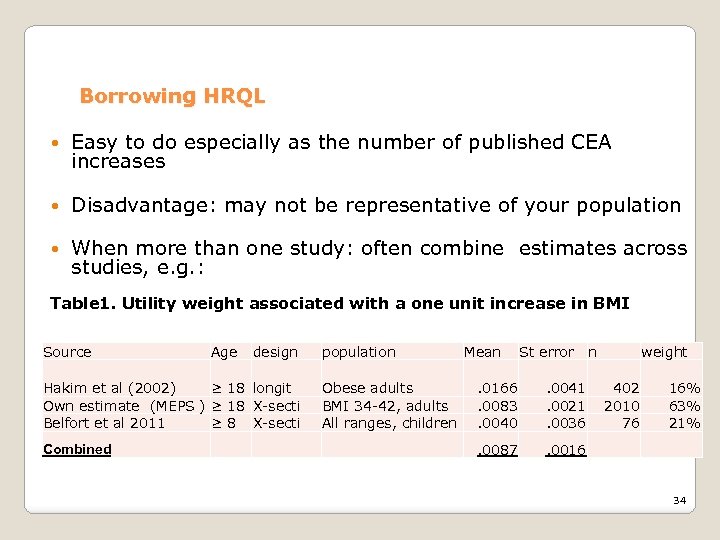 Borrowing HRQL Easy to do especially as the number of published CEA increases Disadvantage: may not be representative of your population When more than one study: often combine estimates across studies, e. g. : Table 1. Utility weight associated with a one unit increase in BMI Source Age design Hakim et al (2002) ≥ 18 longit Own estimate (MEPS ) ≥ 18 X-secti Belfort et al 2011 ≥ 8 X-secti Combined population Obese adults BMI 34 -42, adults All ranges, children Mean St error n . 0166. 0083. 0040 . 0041. 0021. 0036 . 0087 weight 402 2010 76 16% 63% 21% . 0016 34
Borrowing HRQL Easy to do especially as the number of published CEA increases Disadvantage: may not be representative of your population When more than one study: often combine estimates across studies, e. g. : Table 1. Utility weight associated with a one unit increase in BMI Source Age design Hakim et al (2002) ≥ 18 longit Own estimate (MEPS ) ≥ 18 X-secti Belfort et al 2011 ≥ 8 X-secti Combined population Obese adults BMI 34 -42, adults All ranges, children Mean St error n . 0166. 0083. 0040 . 0041. 0021. 0036 . 0087 weight 402 2010 76 16% 63% 21% . 0016 34
 END OF HRQL SECTION 35
END OF HRQL SECTION 35
 Disability –adjusted life years (DALYs) Alternative to QALYs, developed more recently (1993), initially to quantify global burden of disease Often used in studies conducted in developing countries; WHO recommends DALYs for CEA to facilitate comparisons, they don’t reject the validity of QALYs (WHO-CHOICE) IN CEA: $/averted DALYS (rather $/QALYs gained) DALYS = YLL + YLD YLL = years of life lost YLD = years lost to disability 36
Disability –adjusted life years (DALYs) Alternative to QALYs, developed more recently (1993), initially to quantify global burden of disease Often used in studies conducted in developing countries; WHO recommends DALYs for CEA to facilitate comparisons, they don’t reject the validity of QALYs (WHO-CHOICE) IN CEA: $/averted DALYS (rather $/QALYs gained) DALYS = YLL + YLD YLL = years of life lost YLD = years lost to disability 36
 Other measures of effectiveness When measuring QALYs is not feasible (i. e. HRQL data were not collected during the trial) When the effect of the intervention on QALYs is not easily captured ◦ Short time horizon (e. g. smoking cessation, lower cholesterol) ◦ Instruments not sensitive to changes in health status For conditions for which no (immediate) Tx exists ◦ Cost per additional diagnosis (rather than cost/QALY) Harder to determine whether HT is cost-effective 37
Other measures of effectiveness When measuring QALYs is not feasible (i. e. HRQL data were not collected during the trial) When the effect of the intervention on QALYs is not easily captured ◦ Short time horizon (e. g. smoking cessation, lower cholesterol) ◦ Instruments not sensitive to changes in health status For conditions for which no (immediate) Tx exists ◦ Cost per additional diagnosis (rather than cost/QALY) Harder to determine whether HT is cost-effective 37
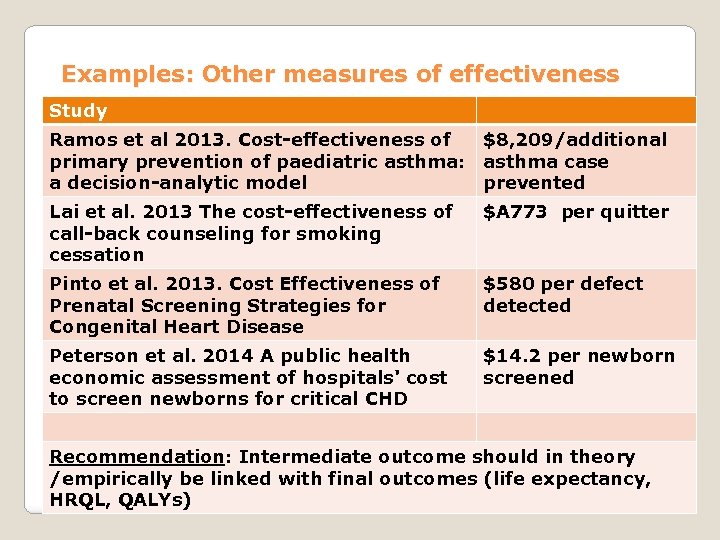 Examples: Other measures of effectiveness Study Ramos et al 2013. Cost-effectiveness of $8, 209/additional primary prevention of paediatric asthma: asthma case a decision-analytic model prevented Lai et al. 2013 The cost-effectiveness of call-back counseling for smoking cessation $A 773 per quitter Pinto et al. 2013. Cost Effectiveness of Prenatal Screening Strategies for Congenital Heart Disease $580 per defect detected Peterson et al. 2014 A public health economic assessment of hospitals' cost to screen newborns for critical CHD $14. 2 per newborn screened Recommendation: Intermediate outcome should in theory /empirically be linked with final outcomes (life expectancy, HRQL, QALYs) 38
Examples: Other measures of effectiveness Study Ramos et al 2013. Cost-effectiveness of $8, 209/additional primary prevention of paediatric asthma: asthma case a decision-analytic model prevented Lai et al. 2013 The cost-effectiveness of call-back counseling for smoking cessation $A 773 per quitter Pinto et al. 2013. Cost Effectiveness of Prenatal Screening Strategies for Congenital Heart Disease $580 per defect detected Peterson et al. 2014 A public health economic assessment of hospitals' cost to screen newborns for critical CHD $14. 2 per newborn screened Recommendation: Intermediate outcome should in theory /empirically be linked with final outcomes (life expectancy, HRQL, QALYs) 38
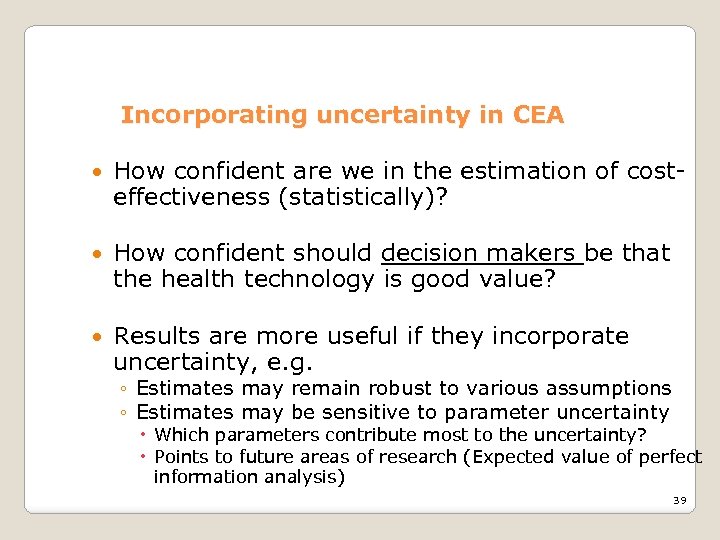 Incorporating uncertainty in CEA How confident are we in the estimation of costeffectiveness (statistically)? How confident should decision makers be that the health technology is good value? Results are more useful if they incorporate uncertainty, e. g. ◦ Estimates may remain robust to various assumptions ◦ Estimates may be sensitive to parameter uncertainty Which parameters contribute most to the uncertainty? Points to future areas of research (Expected value of perfect information analysis) 39
Incorporating uncertainty in CEA How confident are we in the estimation of costeffectiveness (statistically)? How confident should decision makers be that the health technology is good value? Results are more useful if they incorporate uncertainty, e. g. ◦ Estimates may remain robust to various assumptions ◦ Estimates may be sensitive to parameter uncertainty Which parameters contribute most to the uncertainty? Points to future areas of research (Expected value of perfect information analysis) 39
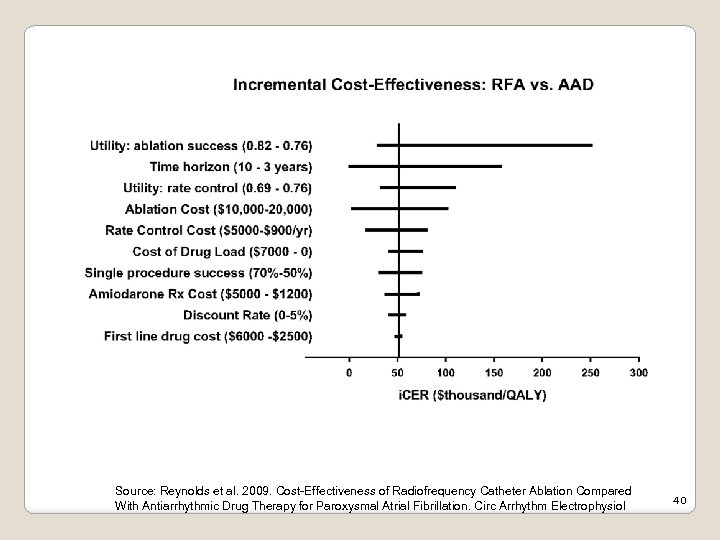 Example 1 -way sensitivity analyses Source: Reynolds et al. 2009. Cost-Effectiveness of Radiofrequency Catheter Ablation Compared With Antiarrhythmic Drug Therapy for Paroxysmal Atrial Fibrillation. Circ Arrhythm Electrophysiol 40
Example 1 -way sensitivity analyses Source: Reynolds et al. 2009. Cost-Effectiveness of Radiofrequency Catheter Ablation Compared With Antiarrhythmic Drug Therapy for Paroxysmal Atrial Fibrillation. Circ Arrhythm Electrophysiol 40
 Incorporating uncertainty in CEA Sensitivity analyses: 1 way, 2 way, …, n-way Probabilistic analyses (Monte Carlo simulations, Bootstrapping). Used to construct: ◦ Confidence intervals ◦ Cost-effectiveness acceptability curves When relying on external data: make sure to record means, standard error and sample size 41
Incorporating uncertainty in CEA Sensitivity analyses: 1 way, 2 way, …, n-way Probabilistic analyses (Monte Carlo simulations, Bootstrapping). Used to construct: ◦ Confidence intervals ◦ Cost-effectiveness acceptability curves When relying on external data: make sure to record means, standard error and sample size 41
 Incorporating uncertainty: ICER estimates 100 k/QALY I II 42
Incorporating uncertainty: ICER estimates 100 k/QALY I II 42
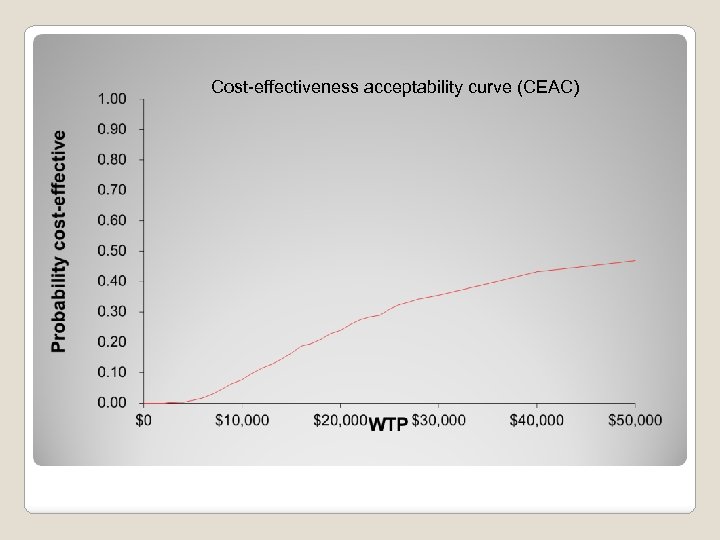 Cost-effectiveness acceptability curve (CEAC)
Cost-effectiveness acceptability curve (CEAC)
 Alternative representation of the ICER (Δ Cost / Δ E) ICER can be converted to Net Monetary Benefit (NMB) at given Willingness to pay (WTP): NMB = WTP*Effectiveness – Cost Example: Δ Cost =$80 k, Δ E= 2 QALYs, WTP = 50 k ◦ ICER = $40, 000 ◦ NMB = $20, 000 + NMB is linear, always defined; + More intuitive to decision makers than ICER 44
Alternative representation of the ICER (Δ Cost / Δ E) ICER can be converted to Net Monetary Benefit (NMB) at given Willingness to pay (WTP): NMB = WTP*Effectiveness – Cost Example: Δ Cost =$80 k, Δ E= 2 QALYs, WTP = 50 k ◦ ICER = $40, 000 ◦ NMB = $20, 000 + NMB is linear, always defined; + More intuitive to decision makers than ICER 44
 CEA in clinical trials 45
CEA in clinical trials 45
 CEA in clinical trials: Advantages Efficiency Internal validity Timeliness (Ramsey et al, ISPOR 2010) Able to collect HRQL directly from the sample, as opposed to borrowing from other studies 46
CEA in clinical trials: Advantages Efficiency Internal validity Timeliness (Ramsey et al, ISPOR 2010) Able to collect HRQL directly from the sample, as opposed to borrowing from other studies 46
 CEA in clinical trials : limitations Effectiveness vs. efficacy Use intent-to-treat approach Length of follow up Cost and benefits may occur beyond the trial duration Conduct within trial analysis as well as beyond (if needed) Study (usually powered for clinical outcomes) may be underpowered for economic outcomes 47
CEA in clinical trials : limitations Effectiveness vs. efficacy Use intent-to-treat approach Length of follow up Cost and benefits may occur beyond the trial duration Conduct within trial analysis as well as beyond (if needed) Study (usually powered for clinical outcomes) may be underpowered for economic outcomes 47
 Incorporating CEA in grant proposals Always limited by space ◦ Why is CEA important to include? ◦ List all cost categories that will be included ◦ Intervention /program costs vs. other costs ◦ How would costs be aggregated, e. g. total per patient ◦ Measures of effectiveness ◦ If QALYs: describe how HRQL will be measured ◦ Calculation of ICER ; statistical analyses; missing data ◦ Sensitivity analyses: 1 -way, 2 -way, PSA ◦ How would results be used by policy makers 48
Incorporating CEA in grant proposals Always limited by space ◦ Why is CEA important to include? ◦ List all cost categories that will be included ◦ Intervention /program costs vs. other costs ◦ How would costs be aggregated, e. g. total per patient ◦ Measures of effectiveness ◦ If QALYs: describe how HRQL will be measured ◦ Calculation of ICER ; statistical analyses; missing data ◦ Sensitivity analyses: 1 -way, 2 -way, PSA ◦ How would results be used by policy makers 48
 Criticisms of CEA l ICER not always intuitive /easy to understand by decision makers l Requires a threshold ICER (e. g. $100 k / QALY) l Methodological challenges l Equity considerations: cost-effectiveness can depend on age, gender, disability, etc. l Equity (or other considerations may be more important than economic efficiency) 49
Criticisms of CEA l ICER not always intuitive /easy to understand by decision makers l Requires a threshold ICER (e. g. $100 k / QALY) l Methodological challenges l Equity considerations: cost-effectiveness can depend on age, gender, disability, etc. l Equity (or other considerations may be more important than economic efficiency) 49


