a3d1eaf4bbec6f74a6c25905debcc685.ppt
- Количество слайдов: 82
 Coronary Heart Disease (CHD) • Leading cause of death in U. S. • Narrowing coronary arteries – Atherosclerosis
Coronary Heart Disease (CHD) • Leading cause of death in U. S. • Narrowing coronary arteries – Atherosclerosis
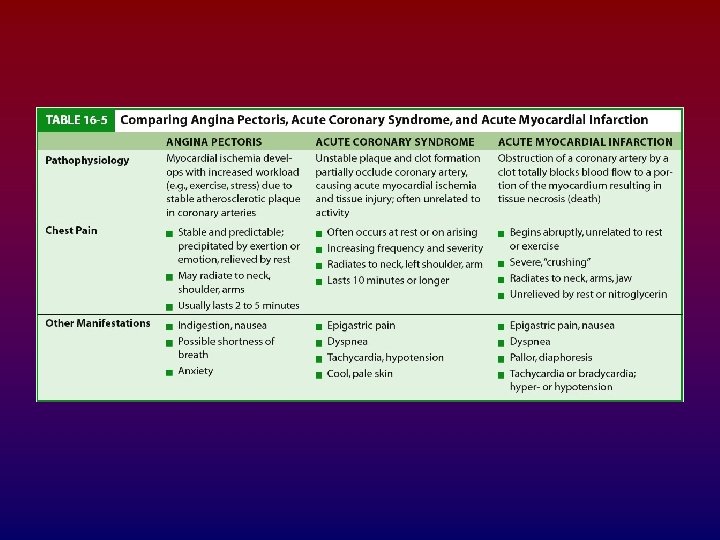
 Angina Pectoris Pathophysiology • • • Obstructed coronary artery Increased myocardial oxygen demand Lactic acid release Leads to pain Three types – Stable – Unstable – Prinzmetal’s: is a syndrome typically consisting of angina (cardiac chest pain) at rest that occurs in cycles. It is caused by vasospasm, a narrowing of the coronary arteries caused by contraction of the smooth muscle tissue in the vessel walls rather than directly by atherosclerosis
Angina Pectoris Pathophysiology • • • Obstructed coronary artery Increased myocardial oxygen demand Lactic acid release Leads to pain Three types – Stable – Unstable – Prinzmetal’s: is a syndrome typically consisting of angina (cardiac chest pain) at rest that occurs in cycles. It is caused by vasospasm, a narrowing of the coronary arteries caused by contraction of the smooth muscle tissue in the vessel walls rather than directly by atherosclerosis
 Angina Pectoris Manifestations • • • Chest pain Radiates Onset with exercise, etc. Relieved by rest, nitroglycerin (NTG) SOB, pallor, fear
Angina Pectoris Manifestations • • • Chest pain Radiates Onset with exercise, etc. Relieved by rest, nitroglycerin (NTG) SOB, pallor, fear
 Acute Coronary Syndrome • Condition that includes: – Unstable angina – Acute myocardial ischemia with or without muscle damage • Associated with coronary artery stenosis and atherosclerotic plaque
Acute Coronary Syndrome • Condition that includes: – Unstable angina – Acute myocardial ischemia with or without muscle damage • Associated with coronary artery stenosis and atherosclerotic plaque
 Acute Myocardial Infarction (AMI) • Pathophysiology – Occluded coronary artery stops blood flow to part of cardiac muscle – Cellular death – Tissue necrosis – Description—heart area affected – Classification
Acute Myocardial Infarction (AMI) • Pathophysiology – Occluded coronary artery stops blood flow to part of cardiac muscle – Cellular death – Tissue necrosis – Description—heart area affected – Classification
 AMI Manifestations • • Chest pain Radiates to shoulder, neck, jaw, arms Lasts longer than 15– 20 minutes Not relieved with NTG Sense of impending doom SOB Diaphoresis Nausea and vomiting
AMI Manifestations • • Chest pain Radiates to shoulder, neck, jaw, arms Lasts longer than 15– 20 minutes Not relieved with NTG Sense of impending doom SOB Diaphoresis Nausea and vomiting
 AMI Manifestations (continued) • Manifestations in women and elderly – May be atypical – Upper abdominal pain – No chest pain but other symptoms
AMI Manifestations (continued) • Manifestations in women and elderly – May be atypical – Upper abdominal pain – No chest pain but other symptoms
 AMI Complications • Related to size and location of infarct • Dysrhythmias • Pump failure – Cardiogenic shock • Pericarditis
AMI Complications • Related to size and location of infarct • Dysrhythmias • Pump failure – Cardiogenic shock • Pericarditis
 Cardiac Dysrhythmias • Pathophysiology – Due to altered formation of impulses or altered conduction of the impulse through the heart – Ectopic beats – Heart block – Reentry phenomenon – Classified to the site of impulse formation or the site and degree of conduction block
Cardiac Dysrhythmias • Pathophysiology – Due to altered formation of impulses or altered conduction of the impulse through the heart – Ectopic beats – Heart block – Reentry phenomenon – Classified to the site of impulse formation or the site and degree of conduction block
 Types of Cardiac Dysrhythmias (continued) • • PVCs Ventricular tachycardia Ventricular fibrillation AV conduction blocks – First degree – Second degree – Third degree
Types of Cardiac Dysrhythmias (continued) • • PVCs Ventricular tachycardia Ventricular fibrillation AV conduction blocks – First degree – Second degree – Third degree
 Types of Cardiac Dysrhythmias • • Supraventricular Sinus tachycardia Sinus bradycardia PAC Atrial flutter Atrial fibrillation Junctional Ventricular dysrhythmias
Types of Cardiac Dysrhythmias • • Supraventricular Sinus tachycardia Sinus bradycardia PAC Atrial flutter Atrial fibrillation Junctional Ventricular dysrhythmias
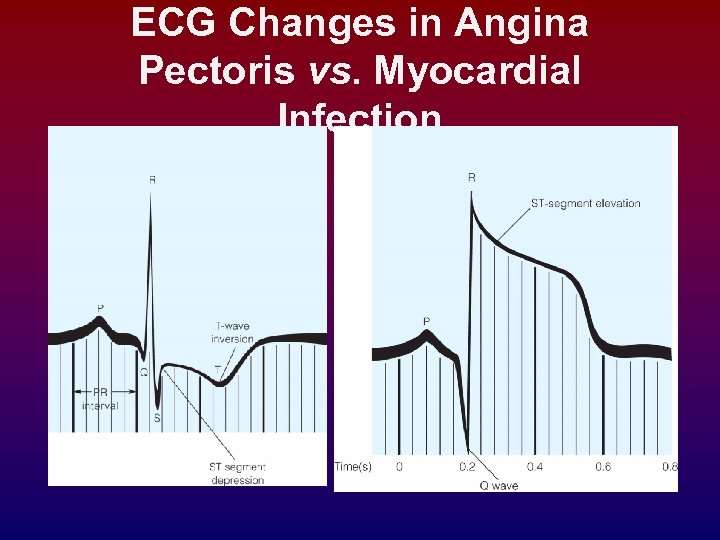 ECG Changes in Angina Pectoris vs. Myocardial Infection
ECG Changes in Angina Pectoris vs. Myocardial Infection
 Congestive Heart Failure Dr Ibraheem Bashayreh, RN, Ph. D 04/11/2009 15
Congestive Heart Failure Dr Ibraheem Bashayreh, RN, Ph. D 04/11/2009 15
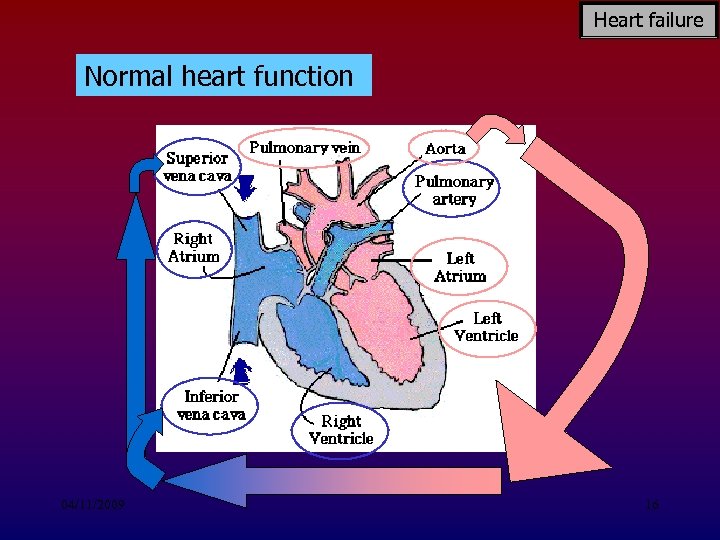 Heart failure Normal heart function 04/11/2009 16
Heart failure Normal heart function 04/11/2009 16
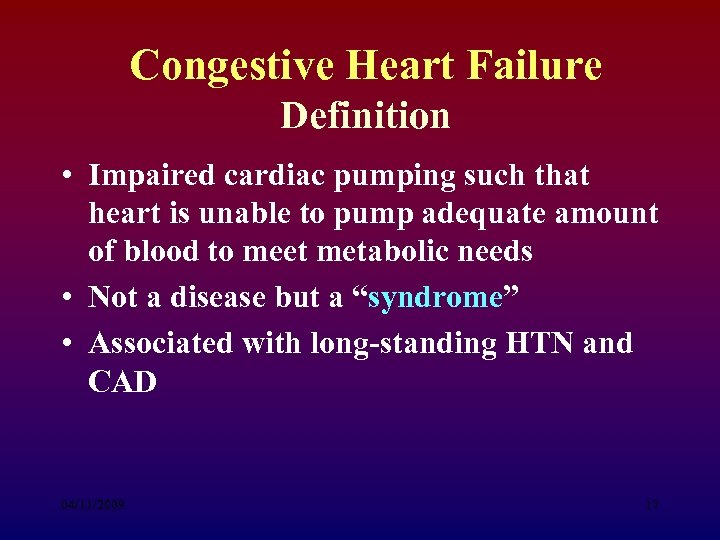 Congestive Heart Failure Definition • Impaired cardiac pumping such that heart is unable to pump adequate amount of blood to meet metabolic needs • Not a disease but a “syndrome” • Associated with long-standing HTN and CAD 04/11/2009 17
Congestive Heart Failure Definition • Impaired cardiac pumping such that heart is unable to pump adequate amount of blood to meet metabolic needs • Not a disease but a “syndrome” • Associated with long-standing HTN and CAD 04/11/2009 17
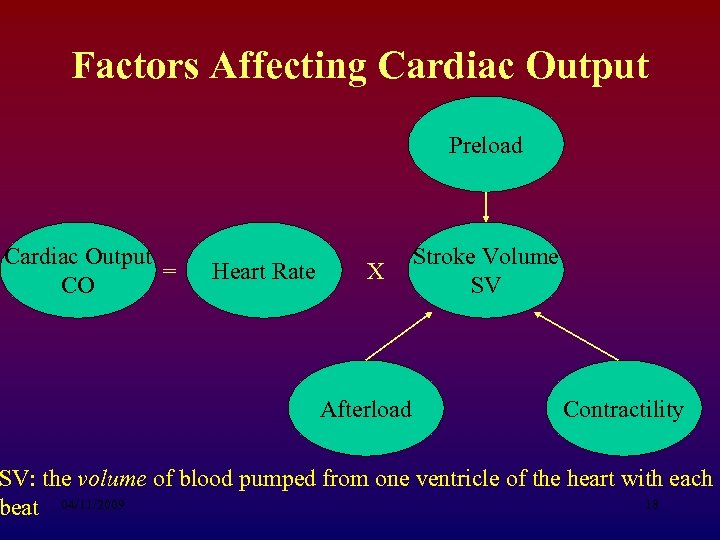 Factors Affecting Cardiac Output Preload Cardiac Output = CO Heart Rate X Afterload Stroke Volume SV Contractility SV: the volume of blood pumped from one ventricle of the heart with each 18 beat 04/11/2009
Factors Affecting Cardiac Output Preload Cardiac Output = CO Heart Rate X Afterload Stroke Volume SV Contractility SV: the volume of blood pumped from one ventricle of the heart with each 18 beat 04/11/2009
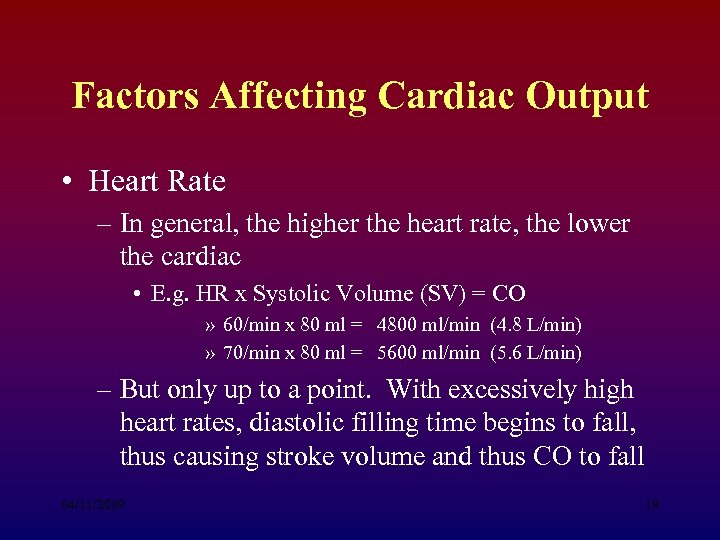 Factors Affecting Cardiac Output • Heart Rate – In general, the higher the heart rate, the lower the cardiac • E. g. HR x Systolic Volume (SV) = CO » 60/min x 80 ml = 4800 ml/min (4. 8 L/min) » 70/min x 80 ml = 5600 ml/min (5. 6 L/min) – But only up to a point. With excessively high heart rates, diastolic filling time begins to fall, thus causing stroke volume and thus CO to fall 04/11/2009 19
Factors Affecting Cardiac Output • Heart Rate – In general, the higher the heart rate, the lower the cardiac • E. g. HR x Systolic Volume (SV) = CO » 60/min x 80 ml = 4800 ml/min (4. 8 L/min) » 70/min x 80 ml = 5600 ml/min (5. 6 L/min) – But only up to a point. With excessively high heart rates, diastolic filling time begins to fall, thus causing stroke volume and thus CO to fall 04/11/2009 19
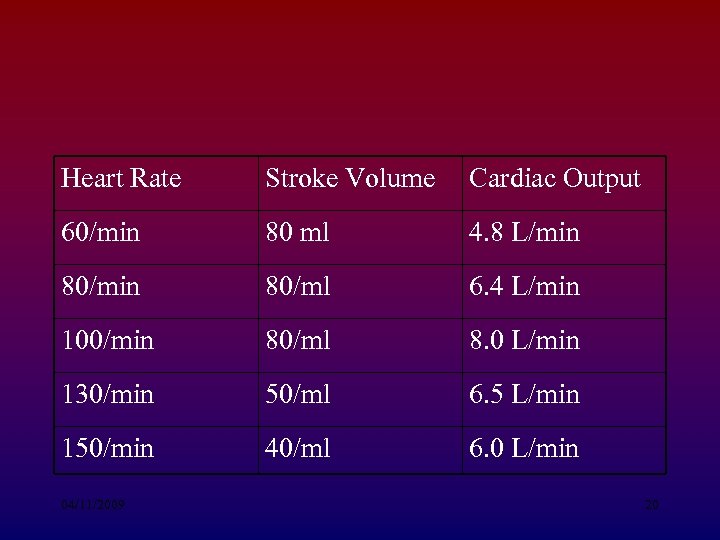 Heart Rate Stroke Volume Cardiac Output 60/min 80 ml 4. 8 L/min 80/ml 6. 4 L/min 100/min 80/ml 8. 0 L/min 130/min 50/ml 6. 5 L/min 150/min 40/ml 6. 0 L/min 04/11/2009 20
Heart Rate Stroke Volume Cardiac Output 60/min 80 ml 4. 8 L/min 80/ml 6. 4 L/min 100/min 80/ml 8. 0 L/min 130/min 50/ml 6. 5 L/min 150/min 40/ml 6. 0 L/min 04/11/2009 20
 Factors Affecting Cardiac Output • Preload – The volume of blood/amount of fiber stretch in the ventricles at the end of diastole (i. e. , before the next contraction) 04/11/2009 21
Factors Affecting Cardiac Output • Preload – The volume of blood/amount of fiber stretch in the ventricles at the end of diastole (i. e. , before the next contraction) 04/11/2009 21
 Factors Affecting Cardiac Output • Preload increases with: • Fluid volume increases • Vasoconstriction (“squeezes” blood from vascular system into heart) • Preload decreases with • Fluid volume losses • Vasodilation (able to “hold” more blood, therefore less returning toheart) 04/11/2009 22
Factors Affecting Cardiac Output • Preload increases with: • Fluid volume increases • Vasoconstriction (“squeezes” blood from vascular system into heart) • Preload decreases with • Fluid volume losses • Vasodilation (able to “hold” more blood, therefore less returning toheart) 04/11/2009 22
 Factors Affecting Cardiac Output • Starling’s Law – Describes the relationship between preload and cardiac output – The greater the heart muscle fibers are stretched (b/c of increases in volume), the greater their subsequent force of contraction – but only up to a point. Beyond that point, fibers get over-stretched and the force of contraction is reduced • Excessive preload = excessive stretch → reduced contraction → reduced SV/CO 04/11/2009 23
Factors Affecting Cardiac Output • Starling’s Law – Describes the relationship between preload and cardiac output – The greater the heart muscle fibers are stretched (b/c of increases in volume), the greater their subsequent force of contraction – but only up to a point. Beyond that point, fibers get over-stretched and the force of contraction is reduced • Excessive preload = excessive stretch → reduced contraction → reduced SV/CO 04/11/2009 23
 Factors Affecting Cardiac Output • Afterload – The resistance against which the ventricle must pump. Excessive afterload = difficult to pump blood → reduced CO/SV – Afterload increased with: • Hypertension • Vasoconstriction – Afterload decreased with: • Vasodilation 04/11/2009 24
Factors Affecting Cardiac Output • Afterload – The resistance against which the ventricle must pump. Excessive afterload = difficult to pump blood → reduced CO/SV – Afterload increased with: • Hypertension • Vasoconstriction – Afterload decreased with: • Vasodilation 04/11/2009 24
 Factors Affecting Cardiac Output • Contractility – Ability of the heart muscle to contract; relates to the strength of contraction. 04/11/2009 25
Factors Affecting Cardiac Output • Contractility – Ability of the heart muscle to contract; relates to the strength of contraction. 04/11/2009 25
 Factors Affecting Cardiac Output • Contractility decreased with: – – infarcted tissue – no contractile strength ischemic tissue – reduced contractile strength. Electrolyte/acid-base imbalance Negative inotropes (medications that decrease contractility, such as beta blockers). • Contractility increased with: – Sympathetic stimulation (effects of epinephrine) – Positive inotropes (medications that increase contractility, such as digoxin, sympathomimmetics) 04/11/2009 26
Factors Affecting Cardiac Output • Contractility decreased with: – – infarcted tissue – no contractile strength ischemic tissue – reduced contractile strength. Electrolyte/acid-base imbalance Negative inotropes (medications that decrease contractility, such as beta blockers). • Contractility increased with: – Sympathetic stimulation (effects of epinephrine) – Positive inotropes (medications that increase contractility, such as digoxin, sympathomimmetics) 04/11/2009 26
 Pathophysiology of CHF • Pump fails → decreased stroke volume /CO. • Compensatory mechanisms kick in to increase CO – SNS stimulation → release of epinephrine/norepinephrine • Increase HR • Increase contractility • Peripheral vasoconstriction (increases afterload) – Myocardial hypertrophy: walls of heart thicken to provide more muscle mass → stronger contractions 04/11/2009 27
Pathophysiology of CHF • Pump fails → decreased stroke volume /CO. • Compensatory mechanisms kick in to increase CO – SNS stimulation → release of epinephrine/norepinephrine • Increase HR • Increase contractility • Peripheral vasoconstriction (increases afterload) – Myocardial hypertrophy: walls of heart thicken to provide more muscle mass → stronger contractions 04/11/2009 27
 Pathophysiology of CHF – Hormonal response: ↓’d renal perfusion interpreted by juxtaglomerular apparatus as hypovolemia. Thus: • Kidneys release renin, which stimulates conversion of antiotensin I → angiotensin II, which causes: – Aldosterone release → Na retention and water retention (via ADH secretion) – Peripheral vasoconstriction 04/11/2009 28
Pathophysiology of CHF – Hormonal response: ↓’d renal perfusion interpreted by juxtaglomerular apparatus as hypovolemia. Thus: • Kidneys release renin, which stimulates conversion of antiotensin I → angiotensin II, which causes: – Aldosterone release → Na retention and water retention (via ADH secretion) – Peripheral vasoconstriction 04/11/2009 28
 Pathophysiology of CHF • Compensatory mechanisms may restore CO to near-normal. • But, if excessive the compensatory mechanisms can worsen heart failure because. . . 04/11/2009 29
Pathophysiology of CHF • Compensatory mechanisms may restore CO to near-normal. • But, if excessive the compensatory mechanisms can worsen heart failure because. . . 04/11/2009 29
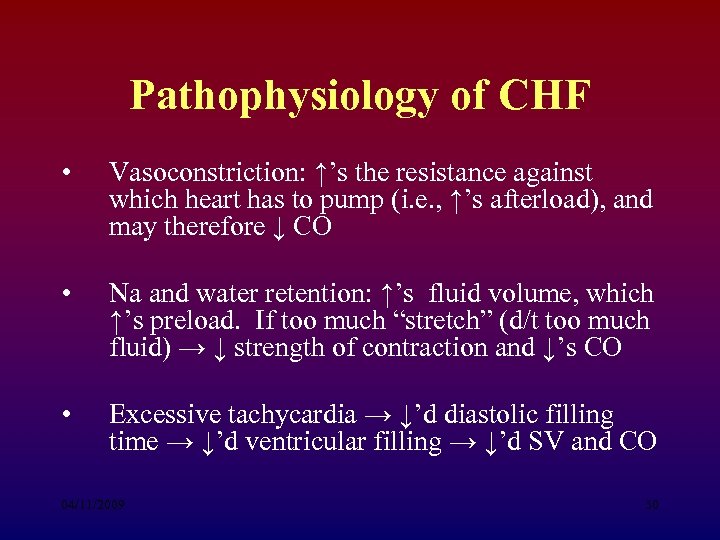 Pathophysiology of CHF • Vasoconstriction: ↑’s the resistance against which heart has to pump (i. e. , ↑’s afterload), and may therefore ↓ CO • Na and water retention: ↑’s fluid volume, which ↑’s preload. If too much “stretch” (d/t too much fluid) → ↓ strength of contraction and ↓’s CO • Excessive tachycardia → ↓’d diastolic filling time → ↓’d ventricular filling → ↓’d SV and CO 04/11/2009 30
Pathophysiology of CHF • Vasoconstriction: ↑’s the resistance against which heart has to pump (i. e. , ↑’s afterload), and may therefore ↓ CO • Na and water retention: ↑’s fluid volume, which ↑’s preload. If too much “stretch” (d/t too much fluid) → ↓ strength of contraction and ↓’s CO • Excessive tachycardia → ↓’d diastolic filling time → ↓’d ventricular filling → ↓’d SV and CO 04/11/2009 30
 Congestive Heart Failure Risk Factors • CAD • Age • HTN • Obesity • Cigarette smoking • Diabetes mellitus • High cholesterol 04/11/2009 • African descent 31
Congestive Heart Failure Risk Factors • CAD • Age • HTN • Obesity • Cigarette smoking • Diabetes mellitus • High cholesterol 04/11/2009 • African descent 31
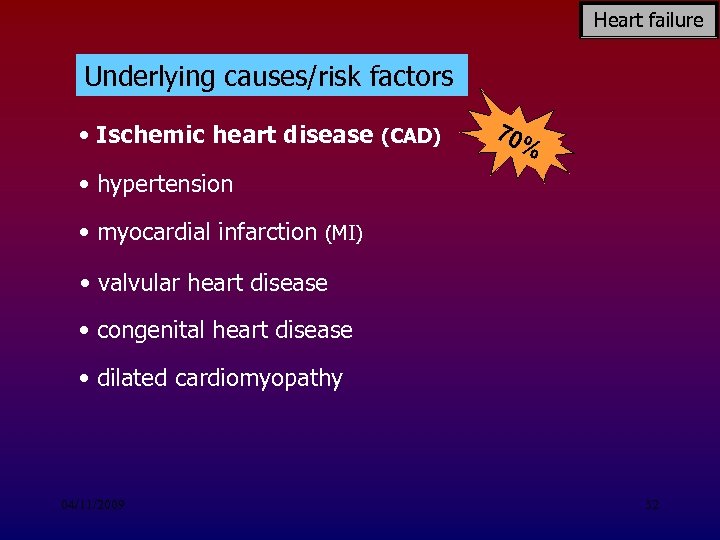 Heart failure Underlying causes/risk factors • Ischemic heart disease (CAD) 70 % • hypertension • myocardial infarction (MI) • valvular heart disease • congenital heart disease • dilated cardiomyopathy 04/11/2009 32
Heart failure Underlying causes/risk factors • Ischemic heart disease (CAD) 70 % • hypertension • myocardial infarction (MI) • valvular heart disease • congenital heart disease • dilated cardiomyopathy 04/11/2009 32
 Congestive Heart Failure Types of Congestive Heart Failure • Left-sided failure – Most common form – Blood backs up through the left atrium into the pulmonary veins • Pulmonary congestion and edema – Eventually leads to biventricular failure 04/11/2009 33
Congestive Heart Failure Types of Congestive Heart Failure • Left-sided failure – Most common form – Blood backs up through the left atrium into the pulmonary veins • Pulmonary congestion and edema – Eventually leads to biventricular failure 04/11/2009 33
 Congestive Heart Failure Types of Congestive Heart Failure • Left-sided failure – Most common cause: • HTN • Cardiomyopathy • Valvular disorders • CAD (myocardial infarction) 04/11/2009 34
Congestive Heart Failure Types of Congestive Heart Failure • Left-sided failure – Most common cause: • HTN • Cardiomyopathy • Valvular disorders • CAD (myocardial infarction) 04/11/2009 34
 Congestive Heart Failure Types of Congestive Heart Failure • Right-sided failure – Results from diseased right ventricle – Blood backs up into right atrium and venous circulation – Causes • LVF • Cor pulmonale: failure of the right side of the heart brought on by long-term high blood pressure in the pulmonary arteries and right ventricle of the heart 04/11/2009 • RV infarction 35
Congestive Heart Failure Types of Congestive Heart Failure • Right-sided failure – Results from diseased right ventricle – Blood backs up into right atrium and venous circulation – Causes • LVF • Cor pulmonale: failure of the right side of the heart brought on by long-term high blood pressure in the pulmonary arteries and right ventricle of the heart 04/11/2009 • RV infarction 35
 Congestive Heart Failure Types of Congestive Heart Failure • Right-sided failure – Venous congestion • Peripheral edema • Hepatomegaly • Splenomegaly • Jugular venous distension 04/11/2009 36
Congestive Heart Failure Types of Congestive Heart Failure • Right-sided failure – Venous congestion • Peripheral edema • Hepatomegaly • Splenomegaly • Jugular venous distension 04/11/2009 36
 Congestive Heart Failure Types of Congestive Heart Failure • Right-sided failure – Primary cause is left-sided failure – Cor pulmonale • RV dilation and hypertrophy caused by pulmonary pathology 04/11/2009 37
Congestive Heart Failure Types of Congestive Heart Failure • Right-sided failure – Primary cause is left-sided failure – Cor pulmonale • RV dilation and hypertrophy caused by pulmonary pathology 04/11/2009 37
 Acute Congestive Heart Failure Clinical Manifestations • Pulmonary edema (what will you hear? ) – Agitation – Pale or cyanotic – Cold, clammy skin – Severe dyspnea – Tachypnea – Pink, frothy sputum 04/11/2009 38
Acute Congestive Heart Failure Clinical Manifestations • Pulmonary edema (what will you hear? ) – Agitation – Pale or cyanotic – Cold, clammy skin – Severe dyspnea – Tachypnea – Pink, frothy sputum 04/11/2009 38
 Chronic Congestive Heart Failure Clinical Manifestations • Fatigue • Dyspnea – Paroxysmal nocturnal dyspnea (PND) • Tachycardia • Edema – (lung, liver, abdomen, legs) • Nocturia 04/11/2009 39
Chronic Congestive Heart Failure Clinical Manifestations • Fatigue • Dyspnea – Paroxysmal nocturnal dyspnea (PND) • Tachycardia • Edema – (lung, liver, abdomen, legs) • Nocturia 04/11/2009 39
 Chronic Congestive Heart Failure Clinical Manifestations • Behavioral changes – Restlessness, confusion, attention span • Chest pain (d/t CO and ↑ myocardial work) • Weight changes (r/t fluid retention) • Skin changes – Dusky appearance 04/11/2009 40
Chronic Congestive Heart Failure Clinical Manifestations • Behavioral changes – Restlessness, confusion, attention span • Chest pain (d/t CO and ↑ myocardial work) • Weight changes (r/t fluid retention) • Skin changes – Dusky appearance 04/11/2009 40
 Congestive Heart Failure Classification • Based on the person’s tolerance to physical activity – Class 1: No limitation of physical activity – Class 2: Slight limitation – Class 3: Marked limitation – Class 4: Inability to carry on any physical activity without discomfort 04/11/2009 41
Congestive Heart Failure Classification • Based on the person’s tolerance to physical activity – Class 1: No limitation of physical activity – Class 2: Slight limitation – Class 3: Marked limitation – Class 4: Inability to carry on any physical activity without discomfort 04/11/2009 41
 Congestive Heart Failure Diagnostic Studies • Primary goal is to determine underlying cause – Physical exam – Chest x-ray – ECG – Hemodynamic assessment 04/11/2009 42
Congestive Heart Failure Diagnostic Studies • Primary goal is to determine underlying cause – Physical exam – Chest x-ray – ECG – Hemodynamic assessment 04/11/2009 42
 Congestive Heart Failure Diagnostic Studies • Primary goal is to determine underlying cause – Echocardiogram (Uses ultrasound to visualize myocardial structures and movement, calculate EF) – Cardiac catheterization 04/11/2009 43
Congestive Heart Failure Diagnostic Studies • Primary goal is to determine underlying cause – Echocardiogram (Uses ultrasound to visualize myocardial structures and movement, calculate EF) – Cardiac catheterization 04/11/2009 43
 Acute Congestive Heart Failure Nursing and Collaborative Management • Primary goal is to improve LV function by: – Decreasing intravascular volume – Decreasing venous return – Decreasing afterload – Improving gas exchange and oxygenation – Improving cardiac function – Reducing anxiety 04/11/2009 44
Acute Congestive Heart Failure Nursing and Collaborative Management • Primary goal is to improve LV function by: – Decreasing intravascular volume – Decreasing venous return – Decreasing afterload – Improving gas exchange and oxygenation – Improving cardiac function – Reducing anxiety 04/11/2009 44
 Acute Congestive Heart Failure Nursing and Collaborative Management • Decreasing intravascular volume – Improves LV function by reducing venous return – Loop diuretic: drug of choice – Reduces preload – High Fowler’s position 04/11/2009 45
Acute Congestive Heart Failure Nursing and Collaborative Management • Decreasing intravascular volume – Improves LV function by reducing venous return – Loop diuretic: drug of choice – Reduces preload – High Fowler’s position 04/11/2009 45
 Acute Congestive Heart Failure Nursing and Collaborative Management • Decreasing afterload – Drug therapy: • vasodilation, Angiotensin-converting enzyme (ACE) inhibitors – Decreases pulmonary congestion 04/11/2009 46
Acute Congestive Heart Failure Nursing and Collaborative Management • Decreasing afterload – Drug therapy: • vasodilation, Angiotensin-converting enzyme (ACE) inhibitors – Decreases pulmonary congestion 04/11/2009 46
 Acute Congestive Heart Failure Nursing and Collaborative Management • Improving cardiac function – Positive inotropes • Improving gas exchange and oxygenation – Administer oxygen, sometimes intubate and ventilate • Reducing anxiety – Morphine 04/11/2009 47
Acute Congestive Heart Failure Nursing and Collaborative Management • Improving cardiac function – Positive inotropes • Improving gas exchange and oxygenation – Administer oxygen, sometimes intubate and ventilate • Reducing anxiety – Morphine 04/11/2009 47
 Chronic Congestive Heart Failure Collaborative Care • Treat underlying cause • Maximize CO • Alleviate symptoms 04/11/2009 48
Chronic Congestive Heart Failure Collaborative Care • Treat underlying cause • Maximize CO • Alleviate symptoms 04/11/2009 48
 Chronic Congestive Heart Failure Collaborative Care • • Oxygen treatment Rest Biventricular pacing Cardiac transplantation 04/11/2009 49
Chronic Congestive Heart Failure Collaborative Care • • Oxygen treatment Rest Biventricular pacing Cardiac transplantation 04/11/2009 49
 Chronic Congestive Heart Failure Drug Therapy • ACE inhibitors • Diuretics • Inotropic drugs : drugs that influence the force of contraction of cardiac muscle • Vasodilators • -Adrenergic blockers 04/11/2009 50
Chronic Congestive Heart Failure Drug Therapy • ACE inhibitors • Diuretics • Inotropic drugs : drugs that influence the force of contraction of cardiac muscle • Vasodilators • -Adrenergic blockers 04/11/2009 50
 Chronic Congestive Heart Failure Nutritional Therapy • Fluid restrictions not commonly prescribed • Sodium restriction – 2 g sodium diet • Daily weights – Same time each day – Wearing same type of clothing 04/11/2009 51
Chronic Congestive Heart Failure Nutritional Therapy • Fluid restrictions not commonly prescribed • Sodium restriction – 2 g sodium diet • Daily weights – Same time each day – Wearing same type of clothing 04/11/2009 51
 Chronic Congestive Heart Failure Nursing Management Nursing Assessment • • Past health history Medications Functional health problems Cold, diaphoretic skin 04/11/2009 52
Chronic Congestive Heart Failure Nursing Management Nursing Assessment • • Past health history Medications Functional health problems Cold, diaphoretic skin 04/11/2009 52
 Chronic Congestive Heart Failure Nursing Management Nursing Assessment • • • Tachypnea Tachycardia Crackles Abdominal distension Restlessness 04/11/2009 53
Chronic Congestive Heart Failure Nursing Management Nursing Assessment • • • Tachypnea Tachycardia Crackles Abdominal distension Restlessness 04/11/2009 53
 Chronic Congestive Heart Failure Nursing Management Nursing Diagnoses • • • Activity intolerance Excess fluid volume Disturbed sleep pattern Impaired gas exchange Anxiety 04/11/2009 54
Chronic Congestive Heart Failure Nursing Management Nursing Diagnoses • • • Activity intolerance Excess fluid volume Disturbed sleep pattern Impaired gas exchange Anxiety 04/11/2009 54
 Chronic Congestive Heart Failure Nursing Management Planning • Overall goals: – Peripheral edema – Shortness of breath – Exercise tolerance – Drug compliance – No complications 04/11/2009 55
Chronic Congestive Heart Failure Nursing Management Planning • Overall goals: – Peripheral edema – Shortness of breath – Exercise tolerance – Drug compliance – No complications 04/11/2009 55
 Chronic Congestive Heart Failure Nursing Management Nursing Implementation • Acute intervention – Establishment of quality of life goals – Symptom management – Conservation of physical/emotional energy – Support systems are essential 04/11/2009 56
Chronic Congestive Heart Failure Nursing Management Nursing Implementation • Acute intervention – Establishment of quality of life goals – Symptom management – Conservation of physical/emotional energy – Support systems are essential 04/11/2009 56
 What is Blood Pressure? • The force of blood against the wall of the arteries. • Systolic- as the heart beats • Diastolic - as the heart relaxes • Written as systolic over diastolic. • Normal Blood pressure is less than 130 mm Hg systolic and less than 85 mm Hg diastolic. 04/11/2009 57
What is Blood Pressure? • The force of blood against the wall of the arteries. • Systolic- as the heart beats • Diastolic - as the heart relaxes • Written as systolic over diastolic. • Normal Blood pressure is less than 130 mm Hg systolic and less than 85 mm Hg diastolic. 04/11/2009 57
 High Blood Pressure • A consistent blood pressure of 140/90 mm Hg or higher is considered high blood pressure. • It increases chance for heart disease, kidney disease, and for having a stroke. • 1 out of 4 Americans have High Bp. • Has no warning signs or symptoms. 04/11/2009 58
High Blood Pressure • A consistent blood pressure of 140/90 mm Hg or higher is considered high blood pressure. • It increases chance for heart disease, kidney disease, and for having a stroke. • 1 out of 4 Americans have High Bp. • Has no warning signs or symptoms. 04/11/2009 58
 Why is High Blood Pressure Important? • • Makes the Heart work too hard. Makes the walls of arteries hard. Increases risk for heart disease and stroke. Can cause heart failure, kidney disease, and blindness. 04/11/2009 59
Why is High Blood Pressure Important? • • Makes the Heart work too hard. Makes the walls of arteries hard. Increases risk for heart disease and stroke. Can cause heart failure, kidney disease, and blindness. 04/11/2009 59
 How Does It Effect the Body? The Brain • High blood pressure is the most important risk factor for stroke. • Can cause a break in a weakened blood vessel which then bleeds in the brain. 04/11/2009 60
How Does It Effect the Body? The Brain • High blood pressure is the most important risk factor for stroke. • Can cause a break in a weakened blood vessel which then bleeds in the brain. 04/11/2009 60
 The Heart • High Blood Pressure is a major risk factor for heart attack. • Is the number one risk factor for Congestive Heart Failure. 04/11/2009 61
The Heart • High Blood Pressure is a major risk factor for heart attack. • Is the number one risk factor for Congestive Heart Failure. 04/11/2009 61
 The Kidneys • Kidneys act as filters to rid the body of wastes. • High blood pressure can narrow and thicken the blood vessels. • Waste builds up in the blood, can result in kidney damage. 04/11/2009 62
The Kidneys • Kidneys act as filters to rid the body of wastes. • High blood pressure can narrow and thicken the blood vessels. • Waste builds up in the blood, can result in kidney damage. 04/11/2009 62
 The Eyes • Can eventually cause blood vessels to break and bleed in the eye. • Can result in blurred vision or even blindness. 04/11/2009 63
The Eyes • Can eventually cause blood vessels to break and bleed in the eye. • Can result in blurred vision or even blindness. 04/11/2009 63
 The Arteries • Causes arteries to harden. • This in turn causes the kidneys and heart to work harder. • Contributes to a number of problems. 04/11/2009 64
The Arteries • Causes arteries to harden. • This in turn causes the kidneys and heart to work harder. • Contributes to a number of problems. 04/11/2009 64
 What causes High Blood Pressure? • • Causes vary Narrowing of the arteries Greater than normal volume of blood Heart beating faster or more forcefully than it should • Another medical problem • The exact cause is not known. 04/11/2009 65
What causes High Blood Pressure? • • Causes vary Narrowing of the arteries Greater than normal volume of blood Heart beating faster or more forcefully than it should • Another medical problem • The exact cause is not known. 04/11/2009 65
 Who can develop High Blood Pressure? • Anyone, but it is more common in: • African Americans- get it earlier and more often then Caucasians. • As we get older. 60% of Americans over 60 have hypertension. • Overweight, family history • High normal bp: 135 -139/85 -89 mm Hg. 04/11/2009 66
Who can develop High Blood Pressure? • Anyone, but it is more common in: • African Americans- get it earlier and more often then Caucasians. • As we get older. 60% of Americans over 60 have hypertension. • Overweight, family history • High normal bp: 135 -139/85 -89 mm Hg. 04/11/2009 66
 Detection • Dr. ’s will diagnose a person with 2 or more readings of 140/90 mm Hg or higher taken on more than one occasion. • White-Coat Hypertension • Measured using a spygmomameter. 04/11/2009 67
Detection • Dr. ’s will diagnose a person with 2 or more readings of 140/90 mm Hg or higher taken on more than one occasion. • White-Coat Hypertension • Measured using a spygmomameter. 04/11/2009 67
 Tips for Having your blood pressure taken. • Don’t drink coffee or smoke cigarettes for 30 minutes before. • Before test sit for five minutes with back supported and feet flat on the ground. Test your arm on a table even with your heart. • Wear short sleeves so your arm is exposed. 04/11/2009 68
Tips for Having your blood pressure taken. • Don’t drink coffee or smoke cigarettes for 30 minutes before. • Before test sit for five minutes with back supported and feet flat on the ground. Test your arm on a table even with your heart. • Wear short sleeves so your arm is exposed. 04/11/2009 68
 Tips for having blood pressure taken. • Go to the bathroom before test. A full bladder can affect bp reading. • Get 2 readings and average the two of them. • Ask the Dr. or nurse to tell you the result in numbers. 04/11/2009 69
Tips for having blood pressure taken. • Go to the bathroom before test. A full bladder can affect bp reading. • Get 2 readings and average the two of them. • Ask the Dr. or nurse to tell you the result in numbers. 04/11/2009 69
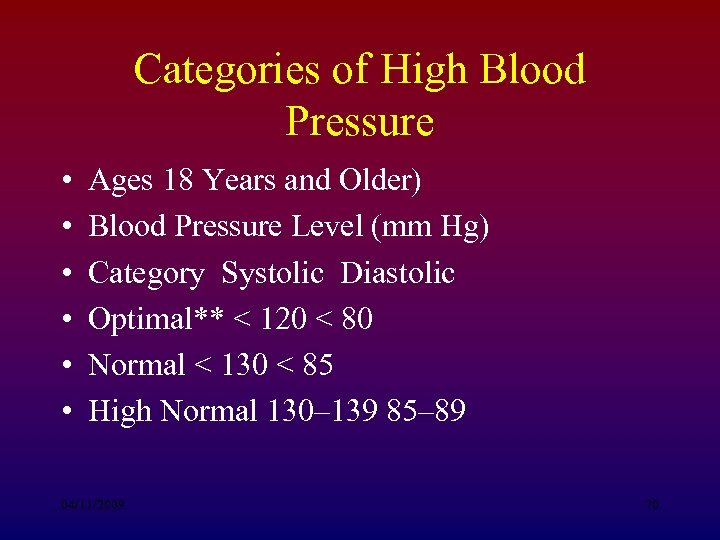 Categories of High Blood Pressure • • • Ages 18 Years and Older) Blood Pressure Level (mm Hg) Category Systolic Diastolic Optimal** < 120 < 80 Normal < 130 < 85 High Normal 130– 139 85– 89 04/11/2009 70
Categories of High Blood Pressure • • • Ages 18 Years and Older) Blood Pressure Level (mm Hg) Category Systolic Diastolic Optimal** < 120 < 80 Normal < 130 < 85 High Normal 130– 139 85– 89 04/11/2009 70
 Categories of High Blood Pressure • • • 04/11/2009 Stage 1 Stage 2 Stage 3 140– 159 /90– 99 160– 179 /100– 109 180 /110 71
Categories of High Blood Pressure • • • 04/11/2009 Stage 1 Stage 2 Stage 3 140– 159 /90– 99 160– 179 /100– 109 180 /110 71
 Preventing Hypertension Adopt a healthy lifestyle by: • • • Following a healthy eating pattern. Maintaining a healthy weight. Being Physically Active. Limiting Alcohol. Quitting Smoking. 04/11/2009 72
Preventing Hypertension Adopt a healthy lifestyle by: • • • Following a healthy eating pattern. Maintaining a healthy weight. Being Physically Active. Limiting Alcohol. Quitting Smoking. 04/11/2009 72
 DASH diet • • • Dietary Approaches to Stop Hypertension. Was an 11 week trial. Differences from the food pyramid: an increase of 1 daily serving of veggies. and increase of 1 -2 servings of fruit. inclusion of 4 -5 servings of nuts, seeds, and beans. 04/11/2009 73
DASH diet • • • Dietary Approaches to Stop Hypertension. Was an 11 week trial. Differences from the food pyramid: an increase of 1 daily serving of veggies. and increase of 1 -2 servings of fruit. inclusion of 4 -5 servings of nuts, seeds, and beans. 04/11/2009 73
 Tips for Reducing Sodium • Buy fresh, plain frozen or canned “no added salt” veggies. • Use fresh poultry, lean meat, and fish. • Use herbs, spices, and salt-free seasonings at the table and while cooking. • Choose convenience foods low in salt. • Rinse canned foods to reduce sodium. 04/11/2009 74
Tips for Reducing Sodium • Buy fresh, plain frozen or canned “no added salt” veggies. • Use fresh poultry, lean meat, and fish. • Use herbs, spices, and salt-free seasonings at the table and while cooking. • Choose convenience foods low in salt. • Rinse canned foods to reduce sodium. 04/11/2009 74
 Maintain Healthy Weight • Blood pressure rises as weight rises. • Obesity is also a risk factor for heart disease. • Even a 10# weight loss can reduce blood pressure. 04/11/2009 75
Maintain Healthy Weight • Blood pressure rises as weight rises. • Obesity is also a risk factor for heart disease. • Even a 10# weight loss can reduce blood pressure. 04/11/2009 75
 Be Physically Active • Helps lower blood pressure and lose/ maintain weight. • 30 minutes of moderate level activity on most days of week. Can even break it up into 10 minute sessions. • Use stairs instead of elevator, get off bus 2 stops early, Park your car at the far end of the lot and walk! 04/11/2009 76
Be Physically Active • Helps lower blood pressure and lose/ maintain weight. • 30 minutes of moderate level activity on most days of week. Can even break it up into 10 minute sessions. • Use stairs instead of elevator, get off bus 2 stops early, Park your car at the far end of the lot and walk! 04/11/2009 76
 Limit Alcohol Intake Alcohol raises blood pressure and can harm liver, brain, and heart 04/11/2009 77
Limit Alcohol Intake Alcohol raises blood pressure and can harm liver, brain, and heart 04/11/2009 77
 Quit Smoking • Injures blood vessel walls • Speeds up process of hardening of the arteries. 04/11/2009 78
Quit Smoking • Injures blood vessel walls • Speeds up process of hardening of the arteries. 04/11/2009 78
 Other Treatment • If Lifestyle Modification is not working, blood pressure medication may be needed, there are several types: • Diuretics-work on the kidney to remove access water and fluid from body to lower bp. • Beta blockers-reduce impulses to the heart and blood vessels. 04/11/2009 79
Other Treatment • If Lifestyle Modification is not working, blood pressure medication may be needed, there are several types: • Diuretics-work on the kidney to remove access water and fluid from body to lower bp. • Beta blockers-reduce impulses to the heart and blood vessels. 04/11/2009 79
 Other Treatment • ACE inhibitors- cause blood vessels to relax and blood to flow freely. • Angiotensin antagonists- work the same as ACE inhibitors. • Calcium Channel Blockers- causes the blood vessel to relax and widen. • Alpha Blocker- blocks an impulse to the heart causing blood to flow more freely. 04/11/2009 80
Other Treatment • ACE inhibitors- cause blood vessels to relax and blood to flow freely. • Angiotensin antagonists- work the same as ACE inhibitors. • Calcium Channel Blockers- causes the blood vessel to relax and widen. • Alpha Blocker- blocks an impulse to the heart causing blood to flow more freely. 04/11/2009 80
 Other Treatment • Alpha-beta blockers- work the same as beta blockers, also slow the heart down. • Nervous system inhibitors- slow nerve impulses to the heart. • Vasodilators- cause blood vessel to widen, allowing blood to flow more freely. 04/11/2009 81
Other Treatment • Alpha-beta blockers- work the same as beta blockers, also slow the heart down. • Nervous system inhibitors- slow nerve impulses to the heart. • Vasodilators- cause blood vessel to widen, allowing blood to flow more freely. 04/11/2009 81
 Conclusion • Hypertension is a very controllable disease, with drastic consequences if left uncontrolled. 04/11/2009 82
Conclusion • Hypertension is a very controllable disease, with drastic consequences if left uncontrolled. 04/11/2009 82


