eb73c30fb70ba33a34970b2cfce21f31.ppt
- Количество слайдов: 50
 CONTROLLED HYPOTENSIVE ANAESTHESIA …what is safe ? Dr Hussain Almejadi AL RAZI Hospital
CONTROLLED HYPOTENSIVE ANAESTHESIA …what is safe ? Dr Hussain Almejadi AL RAZI Hospital
 • Definition. • History and evolution. • Physiology. • Blood pressure goal. • Contraindications. • Techniques. • Anaesthetic management. • Our experience in Al RAZI hospital.
• Definition. • History and evolution. • Physiology. • Blood pressure goal. • Contraindications. • Techniques. • Anaesthetic management. • Our experience in Al RAZI hospital.
 • why should we be bothered with hypotensive anaesthesia ? – Decrease blood loss. – Improve operative field. – Decrease duration of surgery.
• why should we be bothered with hypotensive anaesthesia ? – Decrease blood loss. – Improve operative field. – Decrease duration of surgery.
 Decrease in blood loss by 55 % and shorten the operating time by one hour. . Sum DC, Chung PC, Chen WC: Deliberate hypotensive anesthesia with labetalol in reconstructive surgery for scoliosis. Acta Anaesthesiol Sin 1996 Dec; 34(4): 203 -207
Decrease in blood loss by 55 % and shorten the operating time by one hour. . Sum DC, Chung PC, Chen WC: Deliberate hypotensive anesthesia with labetalol in reconstructive surgery for scoliosis. Acta Anaesthesiol Sin 1996 Dec; 34(4): 203 -207
 Significant less blood loss and improving of the surgical field. Precious DS, Splinter W, Bosco D: Induced hypotensive anesthesia for adolescent orthognathic surgery J Oral Maxillofac Surg 1996 Jun; 54(6): 680 -683
Significant less blood loss and improving of the surgical field. Precious DS, Splinter W, Bosco D: Induced hypotensive anesthesia for adolescent orthognathic surgery J Oral Maxillofac Surg 1996 Jun; 54(6): 680 -683
 Intraoperative blood loss is 40% less. Nelson CL, Fontenot HJ: Ten strategies to reduce blood loss in orthopedic surgery Am J Surg 1995, N° 6 A (Suppl. ), 170: 64 -68
Intraoperative blood loss is 40% less. Nelson CL, Fontenot HJ: Ten strategies to reduce blood loss in orthopedic surgery Am J Surg 1995, N° 6 A (Suppl. ), 170: 64 -68
 Deliberate hypotension in orthopedic surgery reduces blood loss, a meta analysis of RCT. CANADAIN JOURNAL OF ANESTHESIA 2007 Mc. Master , Hamilton, Ontario. 17 ARTICLES. CONCLUSION : Deliberate hypotension does reduce blood loss.
Deliberate hypotension in orthopedic surgery reduces blood loss, a meta analysis of RCT. CANADAIN JOURNAL OF ANESTHESIA 2007 Mc. Master , Hamilton, Ontario. 17 ARTICLES. CONCLUSION : Deliberate hypotension does reduce blood loss.
 Definition • It is a State of induced hypotension during anaesthesia to reduce bleeding and improve the surgical field adjusted to the patient’s age , pre-operative blood pressure and past medical history.
Definition • It is a State of induced hypotension during anaesthesia to reduce bleeding and improve the surgical field adjusted to the patient’s age , pre-operative blood pressure and past medical history.
 Definition • Effect VS Safety. • Reduction in systolic blood pressure to 80 -90 mm. Hg. • Decrease in MAP to 50 -60 mm. Hg in normotensive patients. • Reduction in MAP by 30% of the baseline values.
Definition • Effect VS Safety. • Reduction in systolic blood pressure to 80 -90 mm. Hg. • Decrease in MAP to 50 -60 mm. Hg in normotensive patients. • Reduction in MAP by 30% of the baseline values.
 History • • • 1917 Harvey Cushing for neurosurgery. 1943 Kolhstaedt and Page on dogs arterial bleeding. 1946 Gardner arteriotomy. 1948 High spinal. 1951 High epidural. 1951 Enderby ganlion blockade. 1960 Murtagh halothane. 1962 Moraca sodium nitroprusside. 1967 Dimant pacemaker. 1978 Fahmy nitroglycerin. 1981 Zimpfer verapamil. 1982 Fukunaga adenosine.
History • • • 1917 Harvey Cushing for neurosurgery. 1943 Kolhstaedt and Page on dogs arterial bleeding. 1946 Gardner arteriotomy. 1948 High spinal. 1951 High epidural. 1951 Enderby ganlion blockade. 1960 Murtagh halothane. 1962 Moraca sodium nitroprusside. 1967 Dimant pacemaker. 1978 Fahmy nitroglycerin. 1981 Zimpfer verapamil. 1982 Fukunaga adenosine.
 Physiology • Cerebral circulation. • Coronary circulation. • Renal circulation.
Physiology • Cerebral circulation. • Coronary circulation. • Renal circulation.
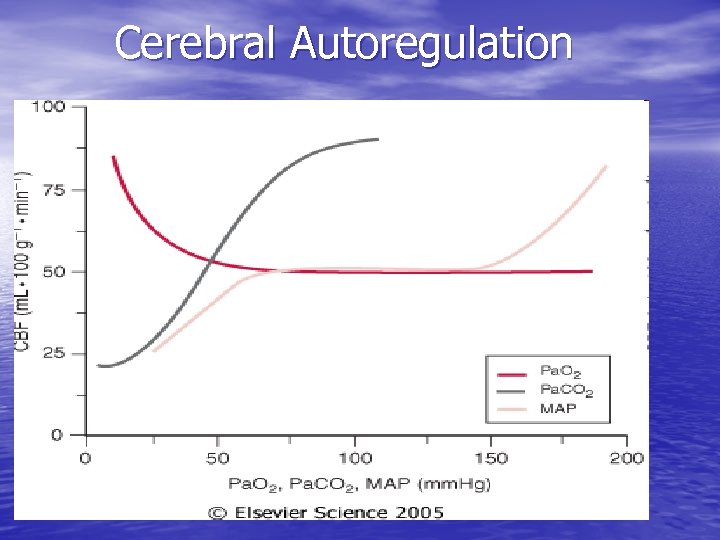 Cerebral Autoregulation
Cerebral Autoregulation
 Cerebral Circulation • Pa. CO 2. • Pa. O 2. • Temperature. • Volatile agents. • Vasodilators.
Cerebral Circulation • Pa. CO 2. • Pa. O 2. • Temperature. • Volatile agents. • Vasodilators.
 Coronary Circulation • Dependent on aortic diastolic blood pressure. • Myocardium extracts most of the oxygen delivered. • Circulation is autoregulated.
Coronary Circulation • Dependent on aortic diastolic blood pressure. • Myocardium extracts most of the oxygen delivered. • Circulation is autoregulated.
 Renal Circulation • Autoregulation over the range 80 -180 mm. Hg ( Miles and Venton 1954 ) • MAP less than 75 mm. Hg leads to decrease in GFR ( Larson et al, 1974 ) • Opioids and inhalational agents stimulate ADH release (Stunn 1974 )
Renal Circulation • Autoregulation over the range 80 -180 mm. Hg ( Miles and Venton 1954 ) • MAP less than 75 mm. Hg leads to decrease in GFR ( Larson et al, 1974 ) • Opioids and inhalational agents stimulate ADH release (Stunn 1974 )
 Respiratory System • Increase in blood flow to the dependent areas. • Vasodilators inhibits hypoxic pulmonary vasoconstriction. • Pa. CO 2 and Et. CO 2 gradient increase.
Respiratory System • Increase in blood flow to the dependent areas. • Vasodilators inhibits hypoxic pulmonary vasoconstriction. • Pa. CO 2 and Et. CO 2 gradient increase.
 Blood Pressure Goal • Reduce blood loss. • Improve the surgical field.
Blood Pressure Goal • Reduce blood loss. • Improve the surgical field.
 Contraindications • Anaethetist factors. • Patients factors.
Contraindications • Anaethetist factors. • Patients factors.
 Anaesthetist factors • Lack of understanding of the technique. • Lack of technical experience. • Inability to monitor the patient adequately.
Anaesthetist factors • Lack of understanding of the technique. • Lack of technical experience. • Inability to monitor the patient adequately.
 Patient factors • Cardiac disease. • Diabetes. • Anemia. • Hepatic disease. • Ischaemic cerebrovascular disease. • Renal disease. • Respiratory insufficiency. • Severe systemic hypertension. • Intolerance to drugs used for hypotensive anaesthesia.
Patient factors • Cardiac disease. • Diabetes. • Anemia. • Hepatic disease. • Ischaemic cerebrovascular disease. • Renal disease. • Respiratory insufficiency. • Severe systemic hypertension. • Intolerance to drugs used for hypotensive anaesthesia.
 Absolute contraindications • Known drug allergy. • Inability to monitor the patient adequately. • Unfamiliarity with the technique.
Absolute contraindications • Known drug allergy. • Inability to monitor the patient adequately. • Unfamiliarity with the technique.
 Morbidity and Mortality 1954 little et al – mortality 1 in 291 – morbidity 1 in 31. – Systolic pressure below 80 mm. Hg. 2008 karol et al Anaesthes and Anlgesia. – NO DIFFERENCE.
Morbidity and Mortality 1954 little et al – mortality 1 in 291 – morbidity 1 in 31. – Systolic pressure below 80 mm. Hg. 2008 karol et al Anaesthes and Anlgesia. – NO DIFFERENCE.
 Techniques MAP = CO x SYSTEMIC VASCULAR RESISTANCE
Techniques MAP = CO x SYSTEMIC VASCULAR RESISTANCE
 Decrease cardiac output • Reduce blood volume. • Dilate capacitance vessels. • Decrease cardiac contractility. • Decrease of heart rate.
Decrease cardiac output • Reduce blood volume. • Dilate capacitance vessels. • Decrease cardiac contractility. • Decrease of heart rate.
 Peripheral vascular resistance • Blockade of alpha adrenergic receptors. • Blockade of autonomic ganglion. • Ralaxation of vascular smooth muscle.
Peripheral vascular resistance • Blockade of alpha adrenergic receptors. • Blockade of autonomic ganglion. • Ralaxation of vascular smooth muscle.
 Mechanical manoeuvers • Positioning. • Positive airway pressure. • Spinal anesthesia. • Epidural anesthesia.
Mechanical manoeuvers • Positioning. • Positive airway pressure. • Spinal anesthesia. • Epidural anesthesia.
 Pharmacologic technique • Ideal agent - Ease of administration - Predictable & dose-dependent effect - Rapid onset/offset - Quick elimination without the production of toxic metabolites - Minimal effects on blood flow to vital organs
Pharmacologic technique • Ideal agent - Ease of administration - Predictable & dose-dependent effect - Rapid onset/offset - Quick elimination without the production of toxic metabolites - Minimal effects on blood flow to vital organs
 Inhalational anesthetics negative inotropic effect vasodilation Advantage Disadvantage • Provides surgical • Decreases CO • Cerebral vasodilation • • • anesthesia Rapid onset/offset Easy to titrate Cerebral protection
Inhalational anesthetics negative inotropic effect vasodilation Advantage Disadvantage • Provides surgical • Decreases CO • Cerebral vasodilation • • • anesthesia Rapid onset/offset Easy to titrate Cerebral protection
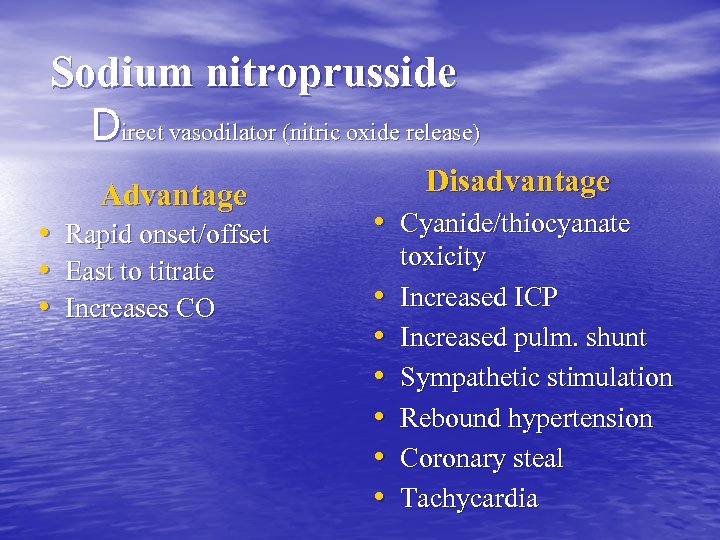 Sodium nitroprusside Direct vasodilator (nitric oxide release) Advantage • Rapid onset/offset • East to titrate • Increases CO Disadvantage • Cyanide/thiocyanate toxicity • Increased ICP • Increased pulm. shunt • Sympathetic stimulation • Rebound hypertension • Coronary steal • Tachycardia
Sodium nitroprusside Direct vasodilator (nitric oxide release) Advantage • Rapid onset/offset • East to titrate • Increases CO Disadvantage • Cyanide/thiocyanate toxicity • Increased ICP • Increased pulm. shunt • Sympathetic stimulation • Rebound hypertension • Coronary steal • Tachycardia
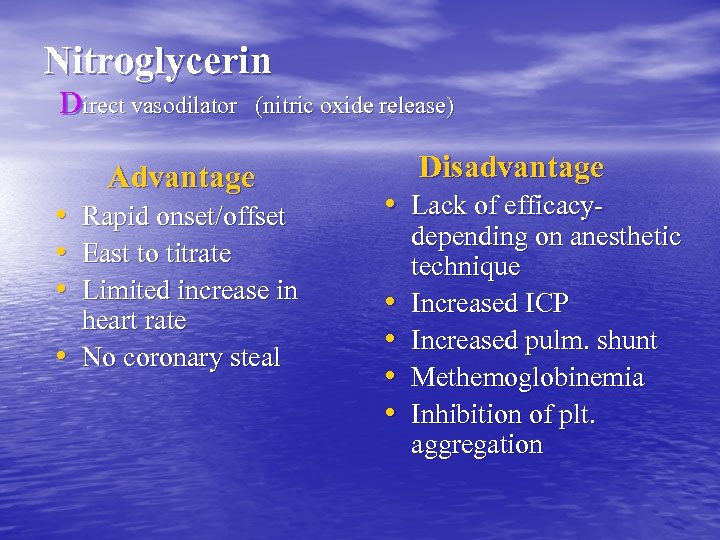 Nitroglycerin Direct vasodilator (nitric oxide release) Advantage • Rapid onset/offset • East to titrate • Limited increase in heart rate • No coronary steal Disadvantage • Lack of efficacydepending on anesthetic technique • Increased ICP • Increased pulm. shunt • Methemoglobinemia • Inhibition of plt. aggregation
Nitroglycerin Direct vasodilator (nitric oxide release) Advantage • Rapid onset/offset • East to titrate • Limited increase in heart rate • No coronary steal Disadvantage • Lack of efficacydepending on anesthetic technique • Increased ICP • Increased pulm. shunt • Methemoglobinemia • Inhibition of plt. aggregation
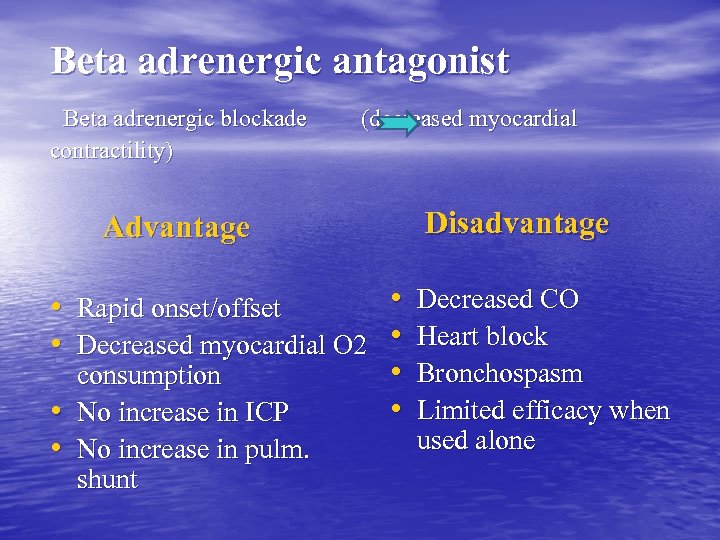 Beta adrenergic antagonist Beta adrenergic blockade (decreased myocardial contractility) Advantage Disadvantage • Decreased CO • Rapid onset/offset • Decreased myocardial O 2 • Heart block • Bronchospasm consumption • Limited efficacy when • No increase in ICP used alone • No increase in pulm. shunt
Beta adrenergic antagonist Beta adrenergic blockade (decreased myocardial contractility) Advantage Disadvantage • Decreased CO • Rapid onset/offset • Decreased myocardial O 2 • Heart block • Bronchospasm consumption • Limited efficacy when • No increase in ICP used alone • No increase in pulm. shunt
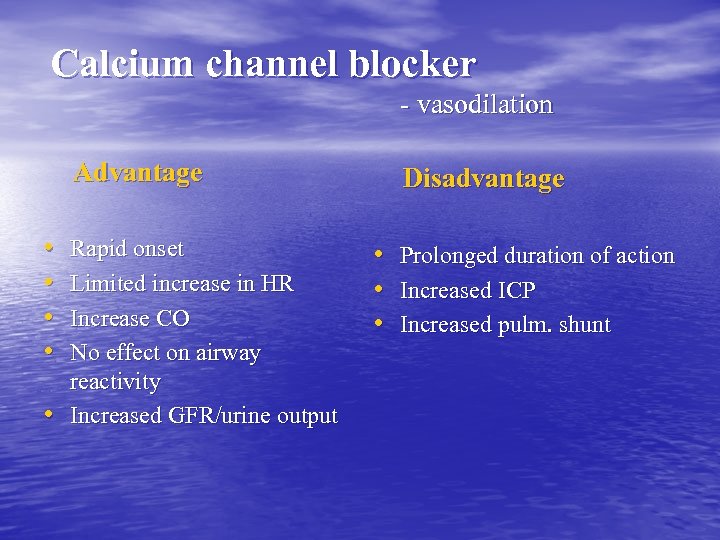 Calcium channel blocker - vasodilation Advantage • • • Rapid onset Limited increase in HR Increase CO No effect on airway reactivity Increased GFR/urine output Disadvantage • • • Prolonged duration of action Increased ICP Increased pulm. shunt
Calcium channel blocker - vasodilation Advantage • • • Rapid onset Limited increase in HR Increase CO No effect on airway reactivity Increased GFR/urine output Disadvantage • • • Prolonged duration of action Increased ICP Increased pulm. shunt
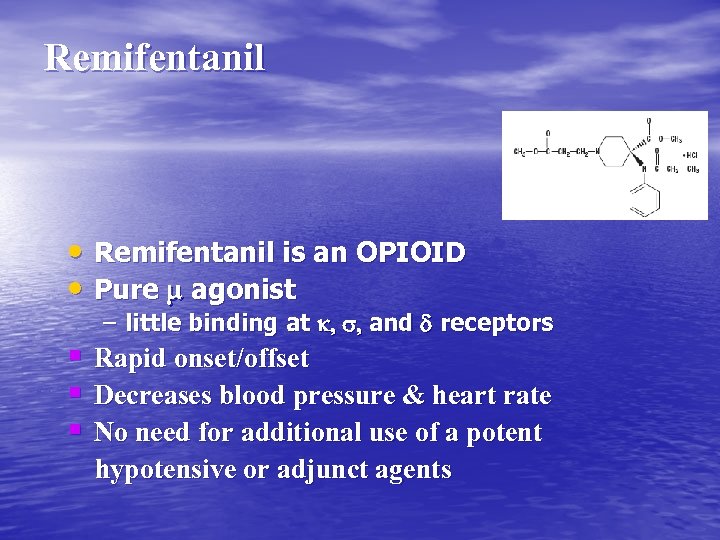 Remifentanil • Remifentanil is an OPIOID • Pure m agonist – little binding at k, s, and d receptors § Rapid onset/offset § Decreases blood pressure & heart rate § No need for additional use of a potent hypotensive or adjunct agents
Remifentanil • Remifentanil is an OPIOID • Pure m agonist – little binding at k, s, and d receptors § Rapid onset/offset § Decreases blood pressure & heart rate § No need for additional use of a potent hypotensive or adjunct agents
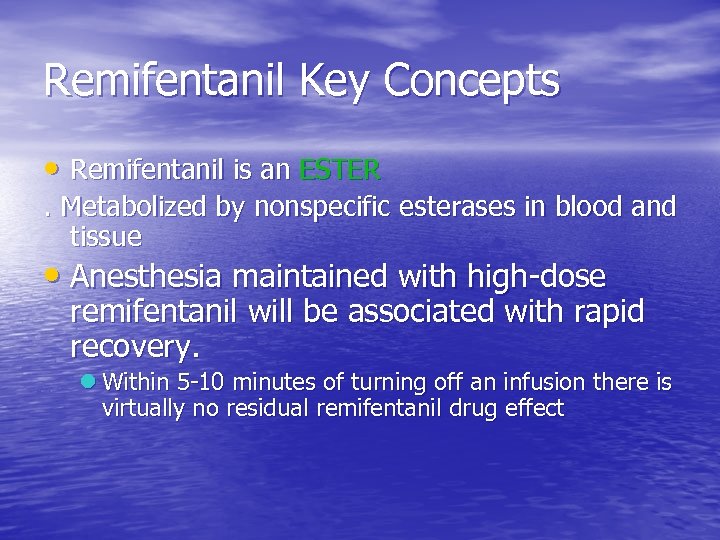 Remifentanil Key Concepts • Remifentanil is an ESTER. Metabolized by nonspecific esterases in blood and tissue • Anesthesia maintained with high-dose remifentanil will be associated with rapid recovery. l Within 5 -10 minutes of turning off an infusion there is virtually no residual remifentanil drug effect
Remifentanil Key Concepts • Remifentanil is an ESTER. Metabolized by nonspecific esterases in blood and tissue • Anesthesia maintained with high-dose remifentanil will be associated with rapid recovery. l Within 5 -10 minutes of turning off an infusion there is virtually no residual remifentanil drug effect
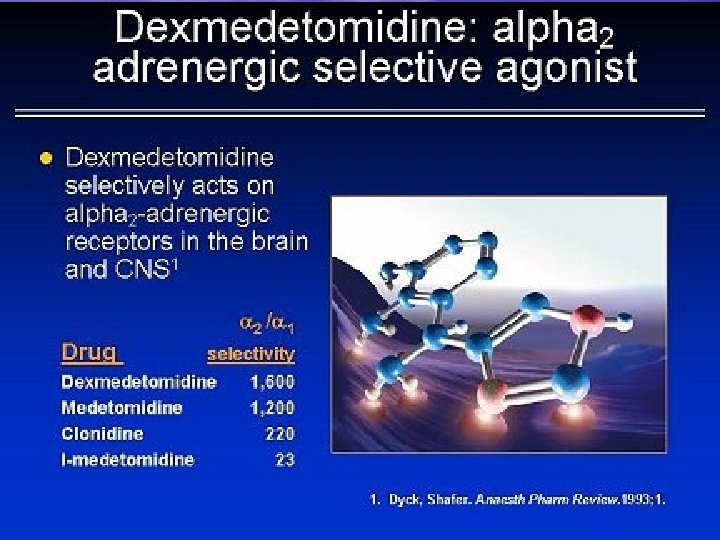
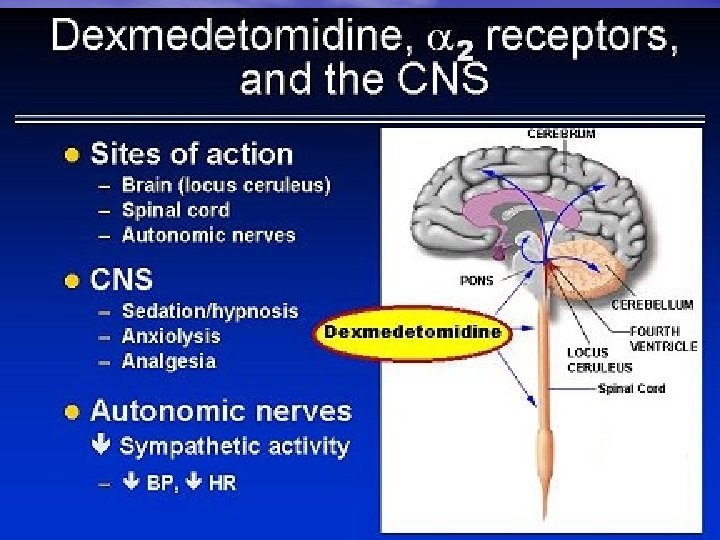
 Dosing and Administration • Dex. should be administered using a controlled • • • infusion device. Dex. dosing should be individualized and titrated to the desired clinical effect For adult patients Dex. is generally initiated with a infusion of 1 mcg/kg over 10 minutes, followed by a maintenance infusion of 0. 2 to 0. 7 mcg/kg/hr It is not necessary to discontinue Dex. prior to extubation
Dosing and Administration • Dex. should be administered using a controlled • • • infusion device. Dex. dosing should be individualized and titrated to the desired clinical effect For adult patients Dex. is generally initiated with a infusion of 1 mcg/kg over 10 minutes, followed by a maintenance infusion of 0. 2 to 0. 7 mcg/kg/hr It is not necessary to discontinue Dex. prior to extubation
 • Comparison between dexmedetomidine and remifentanil for controlled hypotension during tympanoplasty. • CONCLUSIONS: Infusion of dexmedetomidine, at the doses used in this study, was less effective than remifentanil in achieving controlled hypotension, good surgical field exposure condition and surgeons' satisfaction during tympanoplasty. 2008 -05, Eur J Anaesthesiol. , 25(5): 369 -74. Epub 2008 Feb 25.
• Comparison between dexmedetomidine and remifentanil for controlled hypotension during tympanoplasty. • CONCLUSIONS: Infusion of dexmedetomidine, at the doses used in this study, was less effective than remifentanil in achieving controlled hypotension, good surgical field exposure condition and surgeons' satisfaction during tympanoplasty. 2008 -05, Eur J Anaesthesiol. , 25(5): 369 -74. Epub 2008 Feb 25.
 Preoperative management • Thorough knowledge by the anaesthetist. • Proper patient evaluation and selection. • HB of 10 g/dl. • Arterial blood gas analysis sampling. • Good level of anxiolytics , analgesics. • Vagolytic drugs should be avoided.
Preoperative management • Thorough knowledge by the anaesthetist. • Proper patient evaluation and selection. • HB of 10 g/dl. • Arterial blood gas analysis sampling. • Good level of anxiolytics , analgesics. • Vagolytic drugs should be avoided.
 Intraoperative management • Stress free induction. • Nasal intubation ? . • Enough peripheral venous access. • Pressure points.
Intraoperative management • Stress free induction. • Nasal intubation ? . • Enough peripheral venous access. • Pressure points.
 Monitoring • Invasive blood pressure. • ECG V 5 lead with ST segment analysis. • Central venous pressure. • Urine output. • Temperature. • Blood loss.
Monitoring • Invasive blood pressure. • ECG V 5 lead with ST segment analysis. • Central venous pressure. • Urine output. • Temperature. • Blood loss.
 Fluid therapy • Deficit replacement. • Maintenance. • Blood loss.
Fluid therapy • Deficit replacement. • Maintenance. • Blood loss.
 • Induced hypotension should start at the time of mucosal incision. • Only to the level needed to reduce bleeding. • Only during specific surgical phase.
• Induced hypotension should start at the time of mucosal incision. • Only to the level needed to reduce bleeding. • Only during specific surgical phase.
 Postoperative management • Rebound hypertension. • Reactionary hemorrhage.
Postoperative management • Rebound hypertension. • Reactionary hemorrhage.
 Our experience in AL RAZI hospital • Strong points. • Area of improvement.
Our experience in AL RAZI hospital • Strong points. • Area of improvement.
 Strong points • One OT is allocated for hypotensive anaesthesia/TIVA. • Propofol – remifentenyl. • Invasive monitoring is a must.
Strong points • One OT is allocated for hypotensive anaesthesia/TIVA. • Propofol – remifentenyl. • Invasive monitoring is a must.
 Area of improvement • Patients selection. • Reduction in blood transfusion.
Area of improvement • Patients selection. • Reduction in blood transfusion.
 Future studies • Prospective. • Control of age and physical status. • Bigger sample size. • Type of surgery. • Controlled studies. • Same technique. • Doppler technique.
Future studies • Prospective. • Control of age and physical status. • Bigger sample size. • Type of surgery. • Controlled studies. • Same technique. • Doppler technique.

 THANK YOU
THANK YOU


