4fe845a6588dac665c6699b8a13a30c7.ppt
- Количество слайдов: 59
 CONTRAST NEPHROPATHY MARC J. SCHWEIGER Director Cardiac Catheterization Laboratories, Baystate Medical Center
CONTRAST NEPHROPATHY MARC J. SCHWEIGER Director Cardiac Catheterization Laboratories, Baystate Medical Center
 CONTRAST NEPHROPATHY • • Patients with CRF and those on Dialysis Background Limitations of Studies Prevention – – What is the Appropriate Hydration Regimen? N Acetycysteine Calculating Adjusted Contrast Dose Non Ionic and Isoosmolar Contrast • Recommendations
CONTRAST NEPHROPATHY • • Patients with CRF and those on Dialysis Background Limitations of Studies Prevention – – What is the Appropriate Hydration Regimen? N Acetycysteine Calculating Adjusted Contrast Dose Non Ionic and Isoosmolar Contrast • Recommendations
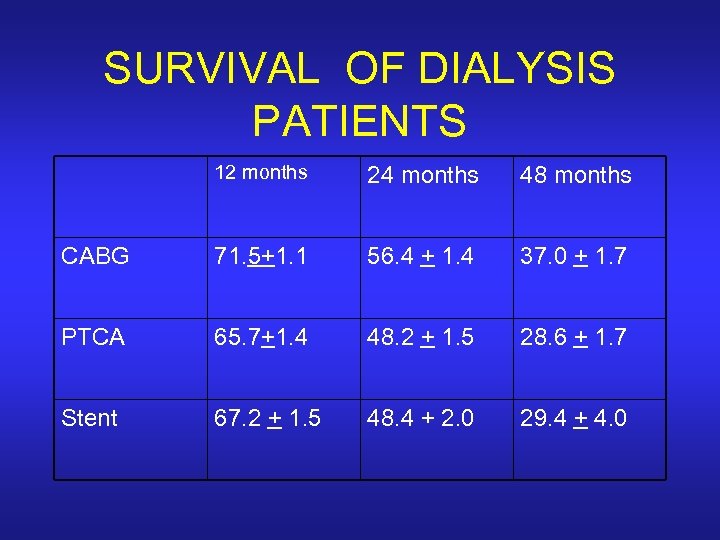 SURVIVAL OF DIALYSIS PATIENTS 12 months 24 months 48 months CABG 71. 5+1. 1 56. 4 + 1. 4 37. 0 + 1. 7 PTCA 65. 7+1. 4 48. 2 + 1. 5 28. 6 + 1. 7 Stent 67. 2 + 1. 5 48. 4 + 2. 0 29. 4 + 4. 0
SURVIVAL OF DIALYSIS PATIENTS 12 months 24 months 48 months CABG 71. 5+1. 1 56. 4 + 1. 4 37. 0 + 1. 7 PTCA 65. 7+1. 4 48. 2 + 1. 5 28. 6 + 1. 7 Stent 67. 2 + 1. 5 48. 4 + 2. 0 29. 4 + 4. 0
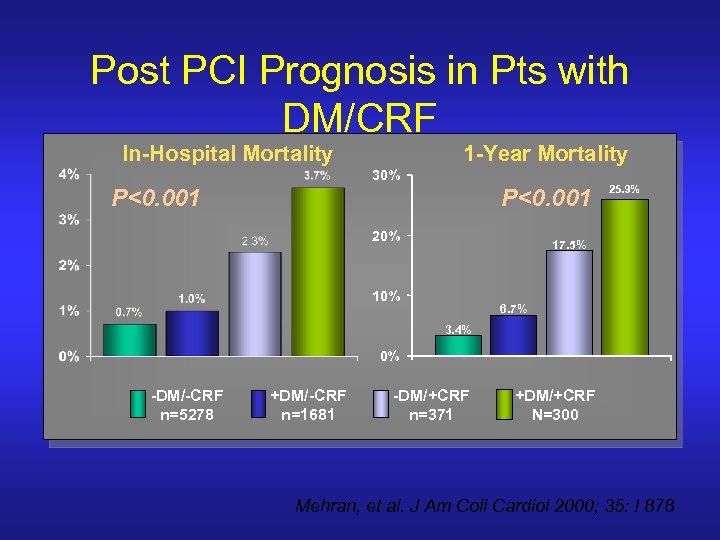 Post PCI Prognosis in Pts with DM/CRF In-Hospital Mortality 1 -Year Mortality 30% P<0. 001 20% 25. 9% 17. 5% 10% 6. 7% 3. 4% 0% -DM/-CRF n=5278 +DM/-CRF n=1681 -DM/+CRF n=371 +DM/+CRF N=300 Mehran, et al. J Am Coll Cardiol 2000; 35: I 878
Post PCI Prognosis in Pts with DM/CRF In-Hospital Mortality 1 -Year Mortality 30% P<0. 001 20% 25. 9% 17. 5% 10% 6. 7% 3. 4% 0% -DM/-CRF n=5278 +DM/-CRF n=1681 -DM/+CRF n=371 +DM/+CRF N=300 Mehran, et al. J Am Coll Cardiol 2000; 35: I 878
 CONTRAST NEPHROPATHY • • Patients with CRF and those on Dialysis Background Limitations of Studies Prevention – – What is the Appropriate Hydration Regimen? N-acetylcysteine Calculating Adjusted Contrast Dose Non Ionic and Isoosmolar Contrast • Recommendations
CONTRAST NEPHROPATHY • • Patients with CRF and those on Dialysis Background Limitations of Studies Prevention – – What is the Appropriate Hydration Regimen? N-acetylcysteine Calculating Adjusted Contrast Dose Non Ionic and Isoosmolar Contrast • Recommendations
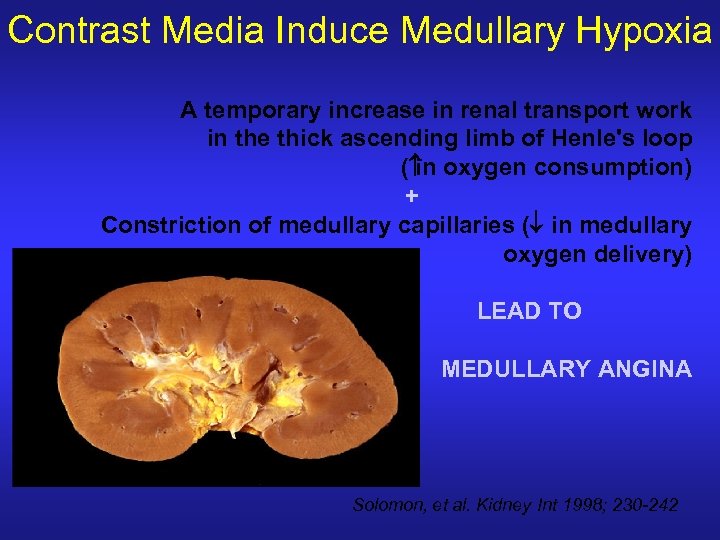 Contrast Media Induce Medullary Hypoxia A temporary increase in renal transport work in the thick ascending limb of Henle's loop ( oxygen consumption) in + Constriction of medullary capillaries (¯ in medullary oxygen delivery) LEAD TO MEDULLARY ANGINA Solomon, et al. Kidney Int 1998; 230 -242
Contrast Media Induce Medullary Hypoxia A temporary increase in renal transport work in the thick ascending limb of Henle's loop ( oxygen consumption) in + Constriction of medullary capillaries (¯ in medullary oxygen delivery) LEAD TO MEDULLARY ANGINA Solomon, et al. Kidney Int 1998; 230 -242
 Post Intervention: Contrast Nephropathy • Contrast nephropathy is the third leading cause of acute renal failure in hospitalized patients (940% incid. in DM with mild to moderate CRI). • Defined as increase in creatinine >0. 5 mgm/dl(or increase of > 25% within 48 hrs. • Related to preexisting renal dysfunction • Diabetes mellitus is additive risk in presence of renal dysfunction • Diabetes mellitus without renal dysfunction – some conflicting data but most likely increased risk Tommaso CL, Cathet Cardiovasc Diag 1994; 31: 316 -321.
Post Intervention: Contrast Nephropathy • Contrast nephropathy is the third leading cause of acute renal failure in hospitalized patients (940% incid. in DM with mild to moderate CRI). • Defined as increase in creatinine >0. 5 mgm/dl(or increase of > 25% within 48 hrs. • Related to preexisting renal dysfunction • Diabetes mellitus is additive risk in presence of renal dysfunction • Diabetes mellitus without renal dysfunction – some conflicting data but most likely increased risk Tommaso CL, Cathet Cardiovasc Diag 1994; 31: 316 -321.
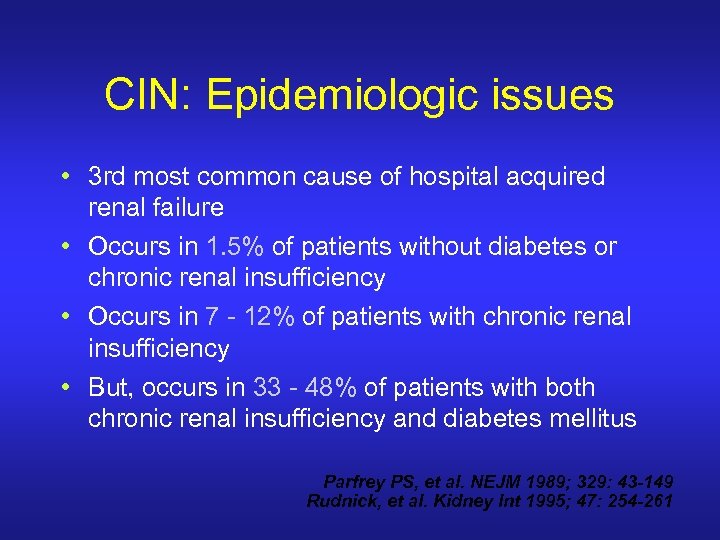 CIN: Epidemiologic issues • 3 rd most common cause of hospital acquired renal failure • Occurs in 1. 5% of patients without diabetes or chronic renal insufficiency • Occurs in 7 - 12% of patients with chronic renal insufficiency • But, occurs in 33 - 48% of patients with both chronic renal insufficiency and diabetes mellitus Parfrey PS, et al. NEJM 1989; 329: 43 -149 Rudnick, et al. Kidney Int 1995; 47: 254 -261
CIN: Epidemiologic issues • 3 rd most common cause of hospital acquired renal failure • Occurs in 1. 5% of patients without diabetes or chronic renal insufficiency • Occurs in 7 - 12% of patients with chronic renal insufficiency • But, occurs in 33 - 48% of patients with both chronic renal insufficiency and diabetes mellitus Parfrey PS, et al. NEJM 1989; 329: 43 -149 Rudnick, et al. Kidney Int 1995; 47: 254 -261
 Incidence & Prognostic Importance of ARF following PCI • Baseline Cr < 2. 0 mg/dl, diabetic patients had higher risk of ARF than nondiabetic pts – Cr < 1. 1(risk 3. 7 % vs 2. 0%, p=0. 05) – Cr 1. 2 -1. 9(risk 4. 5% vs 1. 9%, p<0. 001) • Baseline Cr > 2. 0 mg/dl, risk high regardless of diabetes status – Cr. 2. 0 -2. 9 mg/dl, risk 22. 4% – Cr > 3 mg/dl, risk 30. 6%
Incidence & Prognostic Importance of ARF following PCI • Baseline Cr < 2. 0 mg/dl, diabetic patients had higher risk of ARF than nondiabetic pts – Cr < 1. 1(risk 3. 7 % vs 2. 0%, p=0. 05) – Cr 1. 2 -1. 9(risk 4. 5% vs 1. 9%, p<0. 001) • Baseline Cr > 2. 0 mg/dl, risk high regardless of diabetes status – Cr. 2. 0 -2. 9 mg/dl, risk 22. 4% – Cr > 3 mg/dl, risk 30. 6%
 Prediction of RCN Requiring Dialysis After PCI Mean age = 65, mean contrast volume 250 cc (cath + PCI) N=3695 Independent risk factors: Cr. Cl>>Diabetes>>Contrast Volume Mc. Cullough PA, Am J Med 1997; 103: 386 -375.
Prediction of RCN Requiring Dialysis After PCI Mean age = 65, mean contrast volume 250 cc (cath + PCI) N=3695 Independent risk factors: Cr. Cl>>Diabetes>>Contrast Volume Mc. Cullough PA, Am J Med 1997; 103: 386 -375.
 Incidence of Contrast Induced Renal Dysfunction in Diabetic Patients 54 62 % 213 1022 28 831 Serum Creatinine (mg/dl) Berns A, Kidney International, 1987
Incidence of Contrast Induced Renal Dysfunction in Diabetic Patients 54 62 % 213 1022 28 831 Serum Creatinine (mg/dl) Berns A, Kidney International, 1987
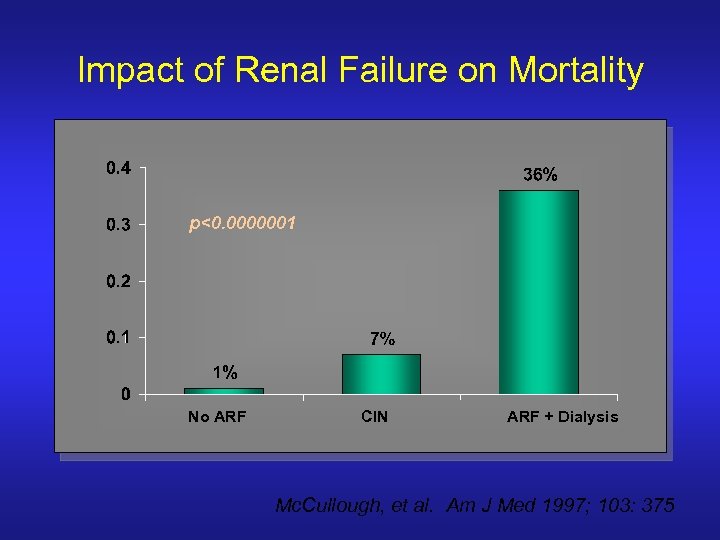 Impact of Renal Failure on Mortality p<0. 0000001 No ARF CIN ARF + Dialysis Mc. Cullough, et al. Am J Med 1997; 103: 375
Impact of Renal Failure on Mortality p<0. 0000001 No ARF CIN ARF + Dialysis Mc. Cullough, et al. Am J Med 1997; 103: 375
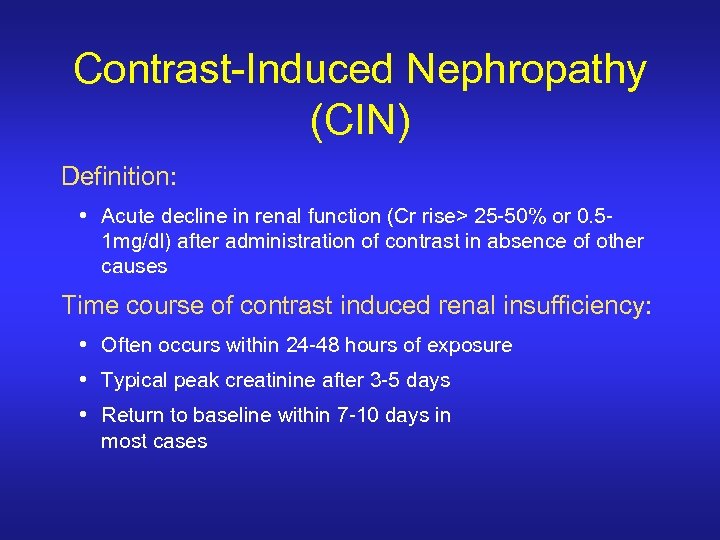 Contrast-Induced Nephropathy (CIN) Definition: • Acute decline in renal function (Cr rise> 25 -50% or 0. 51 mg/dl) after administration of contrast in absence of other causes Time course of contrast induced renal insufficiency: • Often occurs within 24 -48 hours of exposure • Typical peak creatinine after 3 -5 days • Return to baseline within 7 -10 days in most cases
Contrast-Induced Nephropathy (CIN) Definition: • Acute decline in renal function (Cr rise> 25 -50% or 0. 51 mg/dl) after administration of contrast in absence of other causes Time course of contrast induced renal insufficiency: • Often occurs within 24 -48 hours of exposure • Typical peak creatinine after 3 -5 days • Return to baseline within 7 -10 days in most cases
 Risk Factors for CIN Procedure-related Risk Factors Patient-related Risk Factors • • Renal insufficiency Diabetes mellitus with renal insufficiency Multiple myeloma ? Volume depletion Hypotension Low cardiac output Class IV CHF Other nephrotoxins • Multiple contrast media injection within 72 hrs • Intra-arterial injection site • • • High volume of contrast media High osmolality of contrast media High viscosity of contrast media ?
Risk Factors for CIN Procedure-related Risk Factors Patient-related Risk Factors • • Renal insufficiency Diabetes mellitus with renal insufficiency Multiple myeloma ? Volume depletion Hypotension Low cardiac output Class IV CHF Other nephrotoxins • Multiple contrast media injection within 72 hrs • Intra-arterial injection site • • • High volume of contrast media High osmolality of contrast media High viscosity of contrast media ?
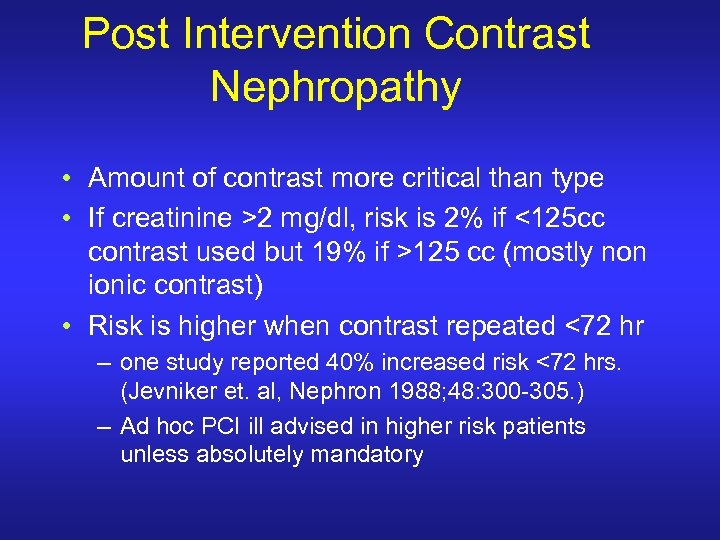 Post Intervention Contrast Nephropathy • Amount of contrast more critical than type • If creatinine >2 mg/dl, risk is 2% if <125 cc contrast used but 19% if >125 cc (mostly non ionic contrast) • Risk is higher when contrast repeated <72 hr – one study reported 40% increased risk <72 hrs. (Jevniker et. al, Nephron 1988; 48: 300 -305. ) – Ad hoc PCI ill advised in higher risk patients unless absolutely mandatory
Post Intervention Contrast Nephropathy • Amount of contrast more critical than type • If creatinine >2 mg/dl, risk is 2% if <125 cc contrast used but 19% if >125 cc (mostly non ionic contrast) • Risk is higher when contrast repeated <72 hr – one study reported 40% increased risk <72 hrs. (Jevniker et. al, Nephron 1988; 48: 300 -305. ) – Ad hoc PCI ill advised in higher risk patients unless absolutely mandatory
 Post Intervention Contrast Nephropathy • Post intervention management – if patient high risk (creatinine >2 mg/dl, esp if diabetic; repeat contrast <72 hrs; large volume of contrast, etc. ) check creatinine/BUN next day – if low risk but large volume used, check labs • Treatment – hydrate – creatinine back to baseline 2 -7 days – dialysis rarely necessary
Post Intervention Contrast Nephropathy • Post intervention management – if patient high risk (creatinine >2 mg/dl, esp if diabetic; repeat contrast <72 hrs; large volume of contrast, etc. ) check creatinine/BUN next day – if low risk but large volume used, check labs • Treatment – hydrate – creatinine back to baseline 2 -7 days – dialysis rarely necessary
 Incidence & Prognostic Importance of Acute Renal Failure Following PCI • Mayo Clinic Retrospective Analysis • Circulation. 105, 2259 -2264, 2002 • • N=7586 ARF defined as increase in Cr >0. 5 mg/dl Incidence 3. 3% Incidence related to baseline serum Cr & presence of diabetes
Incidence & Prognostic Importance of Acute Renal Failure Following PCI • Mayo Clinic Retrospective Analysis • Circulation. 105, 2259 -2264, 2002 • • N=7586 ARF defined as increase in Cr >0. 5 mg/dl Incidence 3. 3% Incidence related to baseline serum Cr & presence of diabetes
 Multivariate Predictors of ARF • + Predictors: Baseline Cr. , MI w/in proceeding 24 h, diabetes, age, history of CHF, peripheral vascular disease, volume (O. R. 1. 12 for each 100 cc increase, 95% CI 1. 02 – 1. 23, p=0. 02) • Negative Predictors: Successful Procedure, RCA PCI
Multivariate Predictors of ARF • + Predictors: Baseline Cr. , MI w/in proceeding 24 h, diabetes, age, history of CHF, peripheral vascular disease, volume (O. R. 1. 12 for each 100 cc increase, 95% CI 1. 02 – 1. 23, p=0. 02) • Negative Predictors: Successful Procedure, RCA PCI
 Long Term Prognostic Implications of ARF after PCI (Hospital Survivors) • 6890 non ARF patients: mortality at 6 months, 1 year and 5 years 2. 3%, 3. 7%, 14. 5%. • 185 ARF patients: 9. 8%, 12. 1%, 44. 6%(p<0. 0001) • Non ARF patients – risk of MI: 2. 7%, 3. 8%, 10. 5% • ARF patients- risk of MI: 4. 3%, 7%, 10. 5%(p=0. 003)
Long Term Prognostic Implications of ARF after PCI (Hospital Survivors) • 6890 non ARF patients: mortality at 6 months, 1 year and 5 years 2. 3%, 3. 7%, 14. 5%. • 185 ARF patients: 9. 8%, 12. 1%, 44. 6%(p<0. 0001) • Non ARF patients – risk of MI: 2. 7%, 3. 8%, 10. 5% • ARF patients- risk of MI: 4. 3%, 7%, 10. 5%(p=0. 003)
 ARF – Clinical Outcomes • Diminished Procedural Success(72. 8% vs 94%, p<0. 0001) • Increased Q wave MI(3. 9% vs. 0. 9%, p<0. 0001) • In hospital mortality 22% vs 1. 4%(p<0. 0001) • Multivariate Predictors of in hospital mortality: Shock, ARF (not baseline Cr)
ARF – Clinical Outcomes • Diminished Procedural Success(72. 8% vs 94%, p<0. 0001) • Increased Q wave MI(3. 9% vs. 0. 9%, p<0. 0001) • In hospital mortality 22% vs 1. 4%(p<0. 0001) • Multivariate Predictors of in hospital mortality: Shock, ARF (not baseline Cr)
 Prognostic Implications of Further Renal Function Deterioration following PCI in patient with pre-existing CRF • 439 pts with baseline serum cr. > 1. 8 • All well hydrated, all received non ionic dye • 161 pts(37%) had increase in serum cr > 25% or required dialysis and 278(63%) did not • JACC, 2000; 36: 1542 -8
Prognostic Implications of Further Renal Function Deterioration following PCI in patient with pre-existing CRF • 439 pts with baseline serum cr. > 1. 8 • All well hydrated, all received non ionic dye • 161 pts(37%) had increase in serum cr > 25% or required dialysis and 278(63%) did not • JACC, 2000; 36: 1542 -8
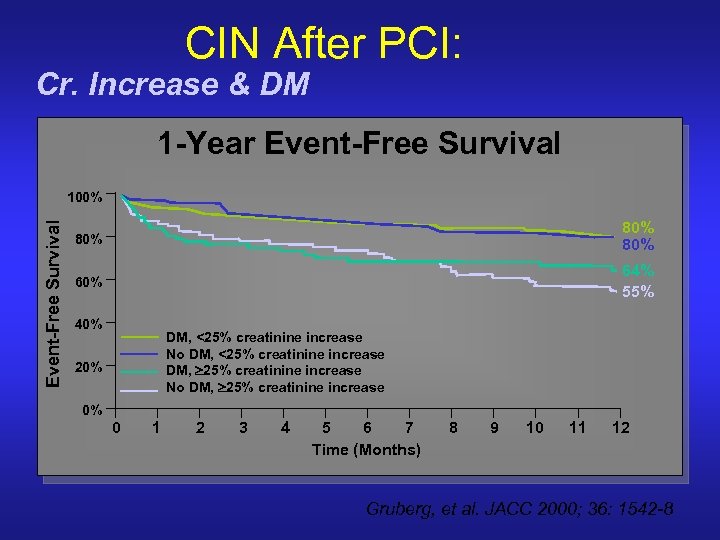 CIN After PCI: Cr. Increase & DM 1 -Year Event-Free Survival 100% 80% 80% 64% 55% 40% DM, <25% creatinine increase No DM, <25% creatinine increase DM, ³ 25% creatinine increase No DM, ³ 25% creatinine increase 20% 0% 0 1 2 3 4 5 6 7 Time (Months) 8 9 10 11 12 Gruberg, et al. JACC 2000; 36: 1542 -8
CIN After PCI: Cr. Increase & DM 1 -Year Event-Free Survival 100% 80% 80% 64% 55% 40% DM, <25% creatinine increase No DM, <25% creatinine increase DM, ³ 25% creatinine increase No DM, ³ 25% creatinine increase 20% 0% 0 1 2 3 4 5 6 7 Time (Months) 8 9 10 11 12 Gruberg, et al. JACC 2000; 36: 1542 -8
 % S. Creatinine Increase & 1 -Year Mortality CIN After PCI: Cumulative 1 -Year Mortality 37% 15% n= 16. 5% 18% n= n= 33. 5% n= n= % Increase in Serum Creatinine Significant increase in mortality noted when Cr. increase ³ 25% (p<0. 0001) Gruberg, et al. JACC 2000; 36: 1542 -8
% S. Creatinine Increase & 1 -Year Mortality CIN After PCI: Cumulative 1 -Year Mortality 37% 15% n= 16. 5% 18% n= n= 33. 5% n= n= % Increase in Serum Creatinine Significant increase in mortality noted when Cr. increase ³ 25% (p<0. 0001) Gruberg, et al. JACC 2000; 36: 1542 -8
 Consequences of Acute Renal Failure • After adjustment for comorbid risk factors, ARF independently increases risk of death 1 • Estimated cost of therapy $128, 000 per episode 2 (if dialysis initiated) 1 Levy, et al, JAMA, 1996, 275: 14892 Hamel, et al, Annals of Internal Medicine, 1997, 195 -202
Consequences of Acute Renal Failure • After adjustment for comorbid risk factors, ARF independently increases risk of death 1 • Estimated cost of therapy $128, 000 per episode 2 (if dialysis initiated) 1 Levy, et al, JAMA, 1996, 275: 14892 Hamel, et al, Annals of Internal Medicine, 1997, 195 -202
 Summary of Risk and Impact of RCN • Renal insufficiency is independently associated with all causes of mortality and cardiovascular mortality • Baseline renal insufficiency, diabetes, and dehydration predispose patients to contrast-induced renal failure • Once contrast-induced renal failure occurs, it is associated with a markedly higher in-hospital and long-term mortality following PCI • Diabetes and CRF have additive adverse effects on long-term prognosis after PCI • RCN dramatically increases hospital costs by increasing length of stay and need for dialysis
Summary of Risk and Impact of RCN • Renal insufficiency is independently associated with all causes of mortality and cardiovascular mortality • Baseline renal insufficiency, diabetes, and dehydration predispose patients to contrast-induced renal failure • Once contrast-induced renal failure occurs, it is associated with a markedly higher in-hospital and long-term mortality following PCI • Diabetes and CRF have additive adverse effects on long-term prognosis after PCI • RCN dramatically increases hospital costs by increasing length of stay and need for dialysis
 Limitations of CIN Studies • Small numbers – not megatrials that cardiologists are used to • Varying treatments used – Differing hydration regiments • Varying definitions – Outcomes vary by definitions • Serum Cr- not Creatinine Clearance
Limitations of CIN Studies • Small numbers – not megatrials that cardiologists are used to • Varying treatments used – Differing hydration regiments • Varying definitions – Outcomes vary by definitions • Serum Cr- not Creatinine Clearance
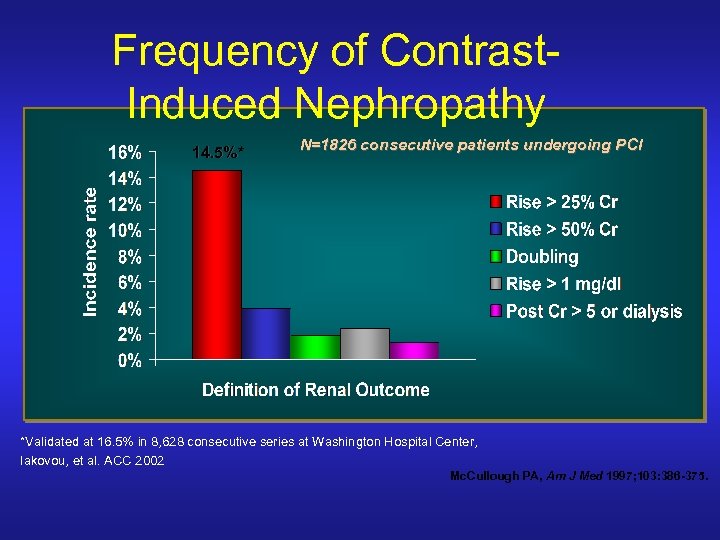 Frequency of Contrast. Induced Nephropathy 14. 5%* N=1826 consecutive patients undergoing PCI *Validated at 16. 5% in 8, 628 consecutive series at Washington Hospital Center, Iakovou, et al. ACC 2002 Mc. Cullough PA, Am J Med 1997; 103: 386 -375.
Frequency of Contrast. Induced Nephropathy 14. 5%* N=1826 consecutive patients undergoing PCI *Validated at 16. 5% in 8, 628 consecutive series at Washington Hospital Center, Iakovou, et al. ACC 2002 Mc. Cullough PA, Am J Med 1997; 103: 386 -375.
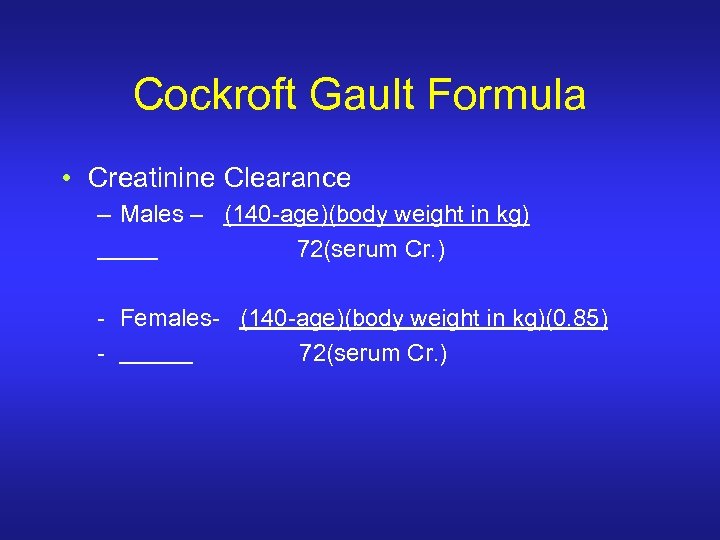 Cockroft Gault Formula • Creatinine Clearance – Males – (140 -age)(body weight in kg) 72(serum Cr. ) - Females- (140 -age)(body weight in kg)(0. 85) 72(serum Cr. )
Cockroft Gault Formula • Creatinine Clearance – Males – (140 -age)(body weight in kg) 72(serum Cr. ) - Females- (140 -age)(body weight in kg)(0. 85) 72(serum Cr. )
 CONTRAST NEPHROPATHY • • Patients with CRF and those on Dialysis Background Limitations of Studies Prevention – – What is the Appropriate Hydration Regimen? N-acetylcysteine (Mucomyst) Calculating Adjusted Contrast Dose Non Ionic and Isoosmolar Contrast • Recommendations
CONTRAST NEPHROPATHY • • Patients with CRF and those on Dialysis Background Limitations of Studies Prevention – – What is the Appropriate Hydration Regimen? N-acetylcysteine (Mucomyst) Calculating Adjusted Contrast Dose Non Ionic and Isoosmolar Contrast • Recommendations
 Post Intervention Contrast Nephropathy • Failed agents for prevention/mitigation of contrast-induced nephropathy – – – Calcium channel antagonists adenosine antagonists dopamine mannitol furosemide endothelin-receptor antagonists
Post Intervention Contrast Nephropathy • Failed agents for prevention/mitigation of contrast-induced nephropathy – – – Calcium channel antagonists adenosine antagonists dopamine mannitol furosemide endothelin-receptor antagonists
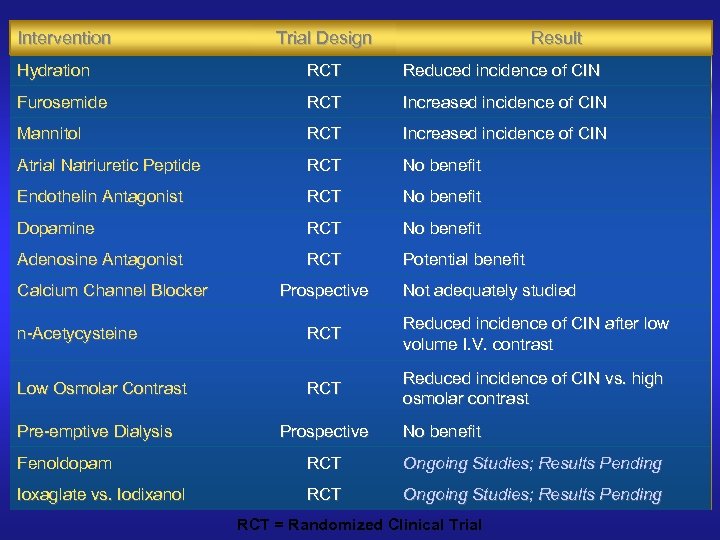 Intervention Trial Design Result Hydration RCT Reduced incidence of CIN Furosemide RCT Increased incidence of CIN Mannitol RCT Increased incidence of CIN Atrial Natriuretic Peptide RCT No benefit Endothelin Antagonist RCT No benefit Dopamine RCT No benefit Adenosine Antagonist RCT Potential benefit Calcium Channel Blocker Prospective Not adequately studied n-Acetycysteine RCT Reduced incidence of CIN after low volume I. V. contrast Low Osmolar Contrast RCT Reduced incidence of CIN vs. high osmolar contrast Pre-emptive Dialysis Prospective No benefit Fenoldopam RCT Ongoing Studies; Results Pending Ioxaglate vs. Iodixanol RCT Ongoing Studies; Results Pending RCT = Randomized Clinical Trial
Intervention Trial Design Result Hydration RCT Reduced incidence of CIN Furosemide RCT Increased incidence of CIN Mannitol RCT Increased incidence of CIN Atrial Natriuretic Peptide RCT No benefit Endothelin Antagonist RCT No benefit Dopamine RCT No benefit Adenosine Antagonist RCT Potential benefit Calcium Channel Blocker Prospective Not adequately studied n-Acetycysteine RCT Reduced incidence of CIN after low volume I. V. contrast Low Osmolar Contrast RCT Reduced incidence of CIN vs. high osmolar contrast Pre-emptive Dialysis Prospective No benefit Fenoldopam RCT Ongoing Studies; Results Pending Ioxaglate vs. Iodixanol RCT Ongoing Studies; Results Pending RCT = Randomized Clinical Trial
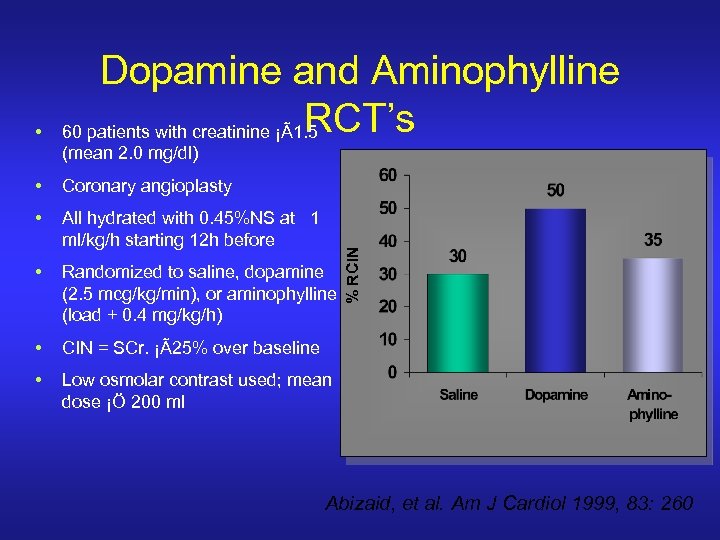 • Dopamine and Aminophylline RCT’s 60 patients with creatinine ¡Ã1. 5 (mean 2. 0 mg/dl) Coronary angioplasty • All hydrated with 0. 45%NS at 1 ml/kg/h starting 12 h before • Randomized to saline, dopamine (2. 5 mcg/kg/min), or aminophylline (load + 0. 4 mg/kg/h) • CIN = SCr. ¡Ã25% over baseline • Low osmolar contrast used; mean dose ¡Ö 200 ml % RCIN • Abizaid, et al. Am J Cardiol 1999, 83: 260
• Dopamine and Aminophylline RCT’s 60 patients with creatinine ¡Ã1. 5 (mean 2. 0 mg/dl) Coronary angioplasty • All hydrated with 0. 45%NS at 1 ml/kg/h starting 12 h before • Randomized to saline, dopamine (2. 5 mcg/kg/min), or aminophylline (load + 0. 4 mg/kg/h) • CIN = SCr. ¡Ã25% over baseline • Low osmolar contrast used; mean dose ¡Ö 200 ml % RCIN • Abizaid, et al. Am J Cardiol 1999, 83: 260
 HYDRATION-Goal: Produce both volume expansion and a large volume of dilute urine • Various protocols in the literature • Should be suited to the clinical situation
HYDRATION-Goal: Produce both volume expansion and a large volume of dilute urine • Various protocols in the literature • Should be suited to the clinical situation
 Prevention of CIN • 78 Pts with CRI (Cr 1. 6 -4. 2 mg/dl) • IV Fluids: 1/2 NS @ 1 ml/kg/hr for 12 hr before & after contrast • Mannitol: 50 g 1 hr before contrast • 60% Furosemide: 80 mg IV 30 min before contrast Non-DM 43% Non-DM % CIN 50% DM 38% 40% 36% 30% 20% 10% 0% 14% 17% 7% Saline + Mannitol Saline + Furosemide Solomon, et al. NEJM 1994; 331: 1416 -1420
Prevention of CIN • 78 Pts with CRI (Cr 1. 6 -4. 2 mg/dl) • IV Fluids: 1/2 NS @ 1 ml/kg/hr for 12 hr before & after contrast • Mannitol: 50 g 1 hr before contrast • 60% Furosemide: 80 mg IV 30 min before contrast Non-DM 43% Non-DM % CIN 50% DM 38% 40% 36% 30% 20% 10% 0% 14% 17% 7% Saline + Mannitol Saline + Furosemide Solomon, et al. NEJM 1994; 331: 1416 -1420
 Comparison of 2 Hydration Regimen in 1620 pts undergoing PCI • Randomly assigned to receive isotonic or half isotonic (with glucose) morning of (elective) or immediately before (emergent) PCI – 1 mg/kg body weight/hr continued until next AM • Increase in serum cr. > 0. 5 defined as contrast mediated nephropathy • Increase in CMR in half isotonic compared with isotonic(2. 0% vs 0. 7%, p=0. 04) – 3 gps benefited most: > 250 cc contrast, women, dm • No difference in cardiac or pvd complications • Archive Intern Med. 2002 162: 329 -336
Comparison of 2 Hydration Regimen in 1620 pts undergoing PCI • Randomly assigned to receive isotonic or half isotonic (with glucose) morning of (elective) or immediately before (emergent) PCI – 1 mg/kg body weight/hr continued until next AM • Increase in serum cr. > 0. 5 defined as contrast mediated nephropathy • Increase in CMR in half isotonic compared with isotonic(2. 0% vs 0. 7%, p=0. 04) – 3 gps benefited most: > 250 cc contrast, women, dm • No difference in cardiac or pvd complications • Archive Intern Med. 2002 162: 329 -336
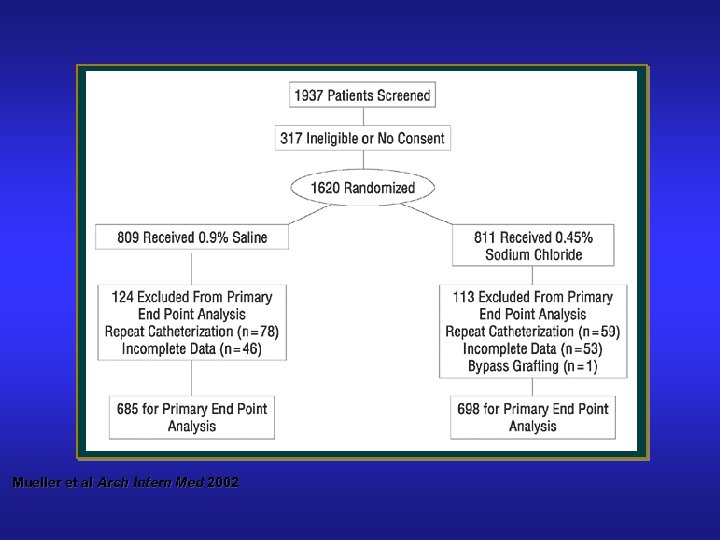 Optimal Hydration Regimen Mueller et al Arch Intern Med 2002
Optimal Hydration Regimen Mueller et al Arch Intern Med 2002
 Optimal Hydration 0. 9 NS vs 0. 45 NS Mueller et al Arch Intern Med 2002
Optimal Hydration 0. 9 NS vs 0. 45 NS Mueller et al Arch Intern Med 2002
 CIN: Effect of N-acetylcysteine • Prospective, randomized • 83 high risk patients – Cr. Cl < 50 ml/min – Diabetes 33% 20% CIN (%) • IV Contrast for CT (75 ml of Low Osmolar CM) • n-AC 600 bid x 2 days pre • CIN definition: creatinine increase of 0. 5 mg/dl • Hydration with 0. 45% @ 1 ml/kg/h x 24 h p= 0. 01 25% 21% 15% 10% 5% 2% 0% Control (42) AC (41) Tepel, et al. NEJM 2000; 343: 180 -184
CIN: Effect of N-acetylcysteine • Prospective, randomized • 83 high risk patients – Cr. Cl < 50 ml/min – Diabetes 33% 20% CIN (%) • IV Contrast for CT (75 ml of Low Osmolar CM) • n-AC 600 bid x 2 days pre • CIN definition: creatinine increase of 0. 5 mg/dl • Hydration with 0. 45% @ 1 ml/kg/h x 24 h p= 0. 01 25% 21% 15% 10% 5% 2% 0% Control (42) AC (41) Tepel, et al. NEJM 2000; 343: 180 -184
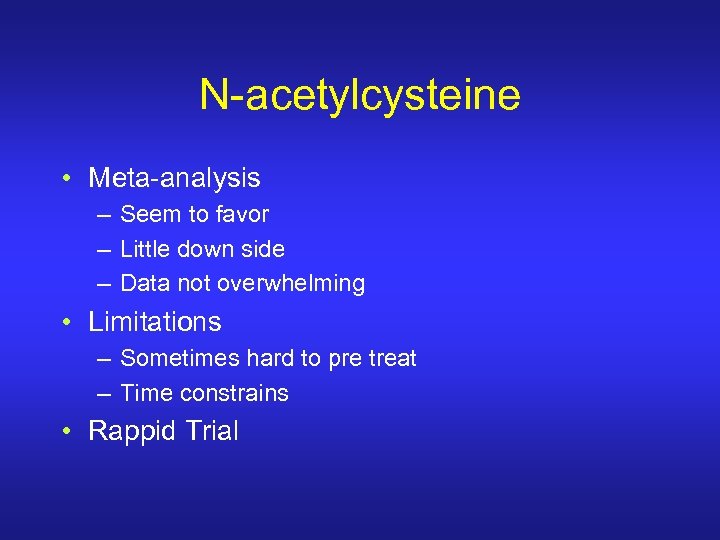 N-acetylcysteine • Meta-analysis – Seem to favor – Little down side – Data not overwhelming • Limitations – Sometimes hard to pre treat – Time constrains • Rappid Trial
N-acetylcysteine • Meta-analysis – Seem to favor – Little down side – Data not overwhelming • Limitations – Sometimes hard to pre treat – Time constrains • Rappid Trial
 Rappid Trial • N=80 • All Cr Clearance < 50 ml/min or serum Cr > 1. 36 mg/dl • Randomized to IV NAC(150 mg/kg in 500 cc NS over 30 min. pre procedure , then 50 mg/kg in 500 cc over 4 hours) or IV hydration(1 cc/kg/hr ) 12 hours pre and post • All received Visapaque
Rappid Trial • N=80 • All Cr Clearance < 50 ml/min or serum Cr > 1. 36 mg/dl • Randomized to IV NAC(150 mg/kg in 500 cc NS over 30 min. pre procedure , then 50 mg/kg in 500 cc over 4 hours) or IV hydration(1 cc/kg/hr ) 12 hours pre and post • All received Visapaque
 Rappid Results • CIN in 2% of NAC vs 21% of hydration pts (p=0. 45) • Mean Serum Cr fell in NAC group (p=0. 02) and was unchanged in hydration group • 3 pts had NAC discontinued after bolus because of flushing, itching, and or rash
Rappid Results • CIN in 2% of NAC vs 21% of hydration pts (p=0. 45) • Mean Serum Cr fell in NAC group (p=0. 02) and was unchanged in hydration group • 3 pts had NAC discontinued after bolus because of flushing, itching, and or rash
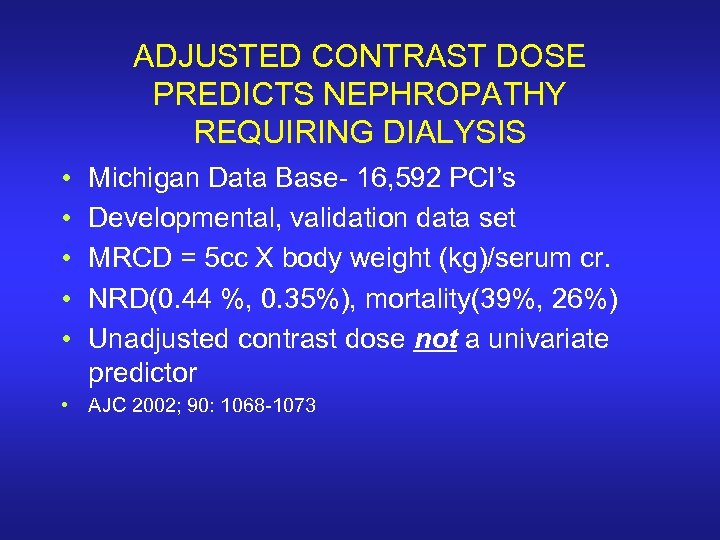 ADJUSTED CONTRAST DOSE PREDICTS NEPHROPATHY REQUIRING DIALYSIS • • • Michigan Data Base- 16, 592 PCI’s Developmental, validation data set MRCD = 5 cc X body weight (kg)/serum cr. NRD(0. 44 %, 0. 35%), mortality(39%, 26%) Unadjusted contrast dose not a univariate predictor • AJC 2002; 90: 1068 -1073
ADJUSTED CONTRAST DOSE PREDICTS NEPHROPATHY REQUIRING DIALYSIS • • • Michigan Data Base- 16, 592 PCI’s Developmental, validation data set MRCD = 5 cc X body weight (kg)/serum cr. NRD(0. 44 %, 0. 35%), mortality(39%, 26%) Unadjusted contrast dose not a univariate predictor • AJC 2002; 90: 1068 -1073
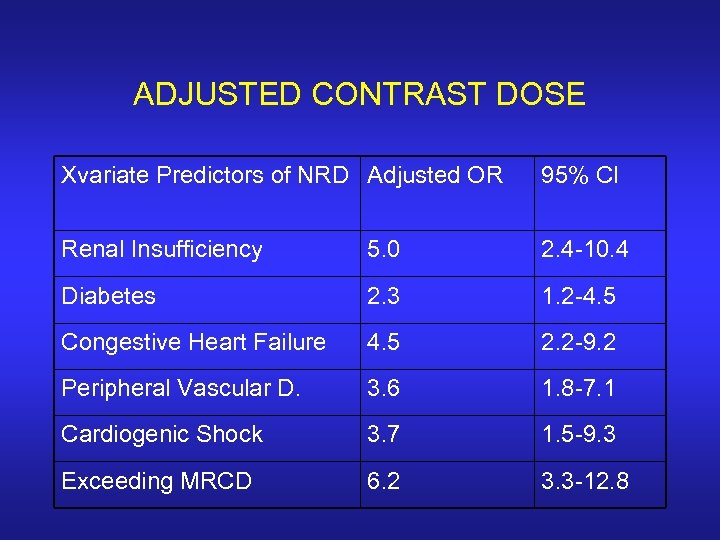 ADJUSTED CONTRAST DOSE Xvariate Predictors of NRD Adjusted OR 95% CI Renal Insufficiency 5. 0 2. 4 -10. 4 Diabetes 2. 3 1. 2 -4. 5 Congestive Heart Failure 4. 5 2. 2 -9. 2 Peripheral Vascular D. 3. 6 1. 8 -7. 1 Cardiogenic Shock 3. 7 1. 5 -9. 3 Exceeding MRCD 6. 2 3. 3 -12. 8
ADJUSTED CONTRAST DOSE Xvariate Predictors of NRD Adjusted OR 95% CI Renal Insufficiency 5. 0 2. 4 -10. 4 Diabetes 2. 3 1. 2 -4. 5 Congestive Heart Failure 4. 5 2. 2 -9. 2 Peripheral Vascular D. 3. 6 1. 8 -7. 1 Cardiogenic Shock 3. 7 1. 5 -9. 3 Exceeding MRCD 6. 2 3. 3 -12. 8
 ADJUSTED CONTRAST DOSE • Progressive increased incidence of nephropathy related dialysis with increasing number of risk factors • Among risk factors, contrast dose is potentially modifiable • Once MRCD exceeded, there was a progressive exponential increase in NRD – 2. 4% NRD if MRCD exceeded, 0. 18% if not – 1 -1. 5 MRCD- 1% NRD, 1. 5 -2 – 3. 5%, 2 -3 – 7%, >3 - 8%
ADJUSTED CONTRAST DOSE • Progressive increased incidence of nephropathy related dialysis with increasing number of risk factors • Among risk factors, contrast dose is potentially modifiable • Once MRCD exceeded, there was a progressive exponential increase in NRD – 2. 4% NRD if MRCD exceeded, 0. 18% if not – 1 -1. 5 MRCD- 1% NRD, 1. 5 -2 – 3. 5%, 2 -3 – 7%, >3 - 8%
 CONTRAST NEPHROPATHY • Patients on Dialysis • Background of Problem • Newer Data – – Prognosis and Incidence – All Comers Prognosis and Incidence – Pre-existing Renal d. Calculating Adjusted Contrast Dose Non Ionic and Isoosmolar Contrast • Recommendations
CONTRAST NEPHROPATHY • Patients on Dialysis • Background of Problem • Newer Data – – Prognosis and Incidence – All Comers Prognosis and Incidence – Pre-existing Renal d. Calculating Adjusted Contrast Dose Non Ionic and Isoosmolar Contrast • Recommendations
 Effects of Ionic vs Non Ionic Contrast on Renal Function post angiography-Gomes et al: Radiology 1989
Effects of Ionic vs Non Ionic Contrast on Renal Function post angiography-Gomes et al: Radiology 1989
 Incidence of CIN (Cr. Increase >1 mg/dl) in pts with preexisting renal disease: Ionic High Osmolar vs Ionic Low Osmolar Contrast. Rudrick MR et al: Kidney International: 1995 N Non Ionic Cr. > 1. 5 mg/dl 296 4% 7% Cr. > 1. 5 mg/dl + doabetes mellitus 213 12% 21% Cr. < 1. 5 mg/dl 359 0 0 Cr. < 1. 5 mg/dl + Diabetes mellitus total 315 1% 1% 1183 3% 7%(p<0. 002)
Incidence of CIN (Cr. Increase >1 mg/dl) in pts with preexisting renal disease: Ionic High Osmolar vs Ionic Low Osmolar Contrast. Rudrick MR et al: Kidney International: 1995 N Non Ionic Cr. > 1. 5 mg/dl 296 4% 7% Cr. > 1. 5 mg/dl + doabetes mellitus 213 12% 21% Cr. < 1. 5 mg/dl 359 0 0 Cr. < 1. 5 mg/dl + Diabetes mellitus total 315 1% 1% 1183 3% 7%(p<0. 002)
 META ANALYSIS High vs. Low Osmolar Contrast Media 39 Trials - 5146 patients CIN > 0. 5 mg/dl CIN in 7% of all patients CIN in 30% of CRI patients • For CRI, NNT=8 (treat 8 to prevent 1 CIN case) • Low osmolar group including Ioxaglate (Hexabrix) superior to High osmolar group; Iodixanol (Visipaque) not studied 1. 2 1 Relative Risk of CIN • • 1. 0 0. 8 0. 61 0. 6 0. 4 0. 2 0 High Osm Low Osm Barrett, et al. Radiology 1993; 188: 171 -178
META ANALYSIS High vs. Low Osmolar Contrast Media 39 Trials - 5146 patients CIN > 0. 5 mg/dl CIN in 7% of all patients CIN in 30% of CRI patients • For CRI, NNT=8 (treat 8 to prevent 1 CIN case) • Low osmolar group including Ioxaglate (Hexabrix) superior to High osmolar group; Iodixanol (Visipaque) not studied 1. 2 1 Relative Risk of CIN • • 1. 0 0. 8 0. 61 0. 6 0. 4 0. 2 0 High Osm Low Osm Barrett, et al. Radiology 1993; 188: 171 -178
 ISOOSMOLAR VS LOW OSMOLAR CONTRAST • 129 high risk patient (diabetes, serum cr. >1. 5<3. 5 • Iodixanol(visapaque)-320 mg iodine/dl, 290 m. Osm/kg water vs. Iohexol(omnipaque)- 350 mg iodine/dl, 780 m. Osm/kg water • All patients well hydrated • Average contrast 166 cc • NEJM: 2/6/03
ISOOSMOLAR VS LOW OSMOLAR CONTRAST • 129 high risk patient (diabetes, serum cr. >1. 5<3. 5 • Iodixanol(visapaque)-320 mg iodine/dl, 290 m. Osm/kg water vs. Iohexol(omnipaque)- 350 mg iodine/dl, 780 m. Osm/kg water • All patients well hydrated • Average contrast 166 cc • NEJM: 2/6/03
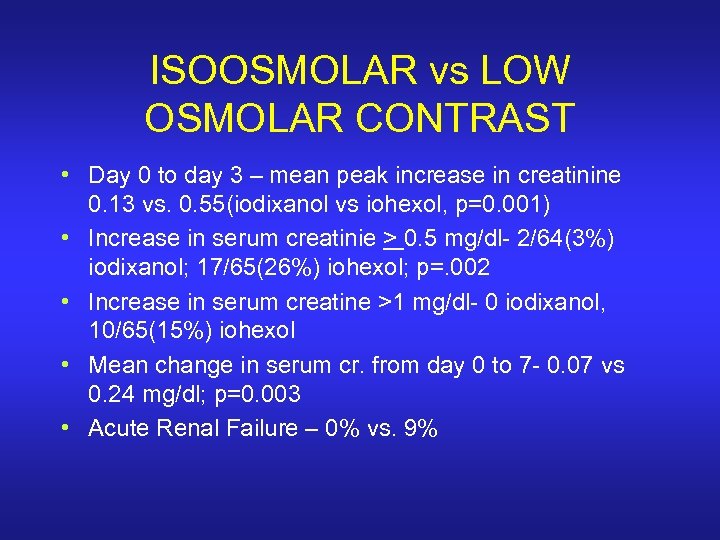 ISOOSMOLAR vs LOW OSMOLAR CONTRAST • Day 0 to day 3 – mean peak increase in creatinine 0. 13 vs. 0. 55(iodixanol vs iohexol, p=0. 001) • Increase in serum creatinie > 0. 5 mg/dl- 2/64(3%) iodixanol; 17/65(26%) iohexol; p=. 002 • Increase in serum creatine >1 mg/dl- 0 iodixanol, 10/65(15%) iohexol • Mean change in serum cr. from day 0 to 7 - 0. 07 vs 0. 24 mg/dl; p=0. 003 • Acute Renal Failure – 0% vs. 9%
ISOOSMOLAR vs LOW OSMOLAR CONTRAST • Day 0 to day 3 – mean peak increase in creatinine 0. 13 vs. 0. 55(iodixanol vs iohexol, p=0. 001) • Increase in serum creatinie > 0. 5 mg/dl- 2/64(3%) iodixanol; 17/65(26%) iohexol; p=. 002 • Increase in serum creatine >1 mg/dl- 0 iodixanol, 10/65(15%) iohexol • Mean change in serum cr. from day 0 to 7 - 0. 07 vs 0. 24 mg/dl; p=0. 003 • Acute Renal Failure – 0% vs. 9%
 VALOR Trial • US Prospective Double Blind Randomized Trial – up to 60 Sites • Patients with CRI (Defined as Cr >1. 5 mg/d. L in women and 1. 7 mg/d. L in men) • Creatinine Measured to 72 hours post procedure or until peak occurs • 2 Groups: – Iodixanol and N-acetylcysteine – LOCM and N-acetylcysteine
VALOR Trial • US Prospective Double Blind Randomized Trial – up to 60 Sites • Patients with CRI (Defined as Cr >1. 5 mg/d. L in women and 1. 7 mg/d. L in men) • Creatinine Measured to 72 hours post procedure or until peak occurs • 2 Groups: – Iodixanol and N-acetylcysteine – LOCM and N-acetylcysteine
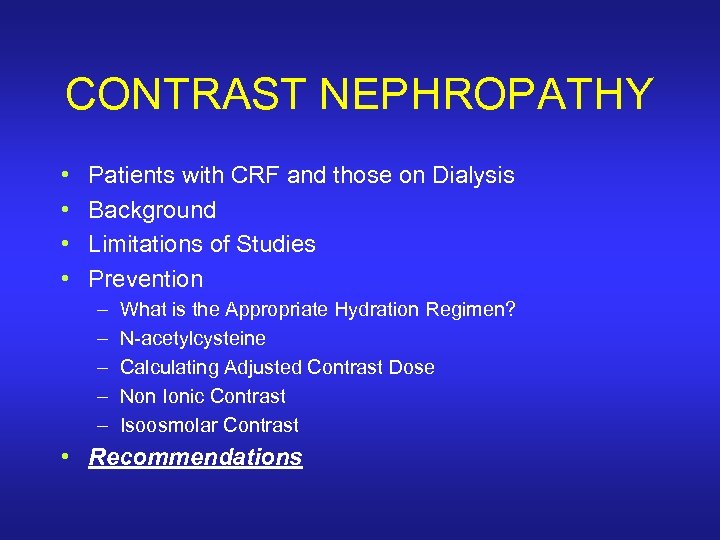 CONTRAST NEPHROPATHY • • Patients with CRF and those on Dialysis Background Limitations of Studies Prevention – – – What is the Appropriate Hydration Regimen? N-acetylcysteine Calculating Adjusted Contrast Dose Non Ionic Contrast Isoosmolar Contrast • Recommendations
CONTRAST NEPHROPATHY • • Patients with CRF and those on Dialysis Background Limitations of Studies Prevention – – – What is the Appropriate Hydration Regimen? N-acetylcysteine Calculating Adjusted Contrast Dose Non Ionic Contrast Isoosmolar Contrast • Recommendations
 PROPOSED GUIDELINES FOR HIGH RISK PATIENTS • • Aggressive Hydration Determine MRCD( 5 cc x weight(kg)/serum Cr. Avoid exceeding( mix contrast, LV gram) Consider staged procedure Non Ionic Contrast Isoosmolar Contrast(? need more data) N-acetylcysteine
PROPOSED GUIDELINES FOR HIGH RISK PATIENTS • • Aggressive Hydration Determine MRCD( 5 cc x weight(kg)/serum Cr. Avoid exceeding( mix contrast, LV gram) Consider staged procedure Non Ionic Contrast Isoosmolar Contrast(? need more data) N-acetylcysteine
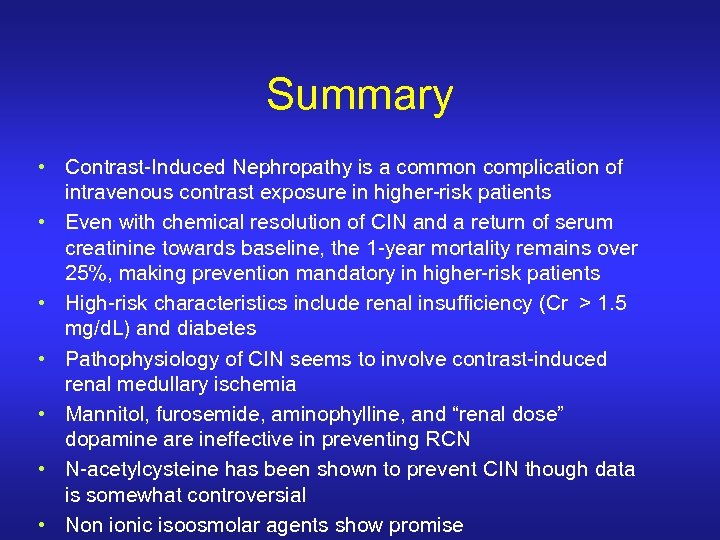 Summary • Contrast-Induced Nephropathy is a common complication of intravenous contrast exposure in higher-risk patients • Even with chemical resolution of CIN and a return of serum creatinine towards baseline, the 1 -year mortality remains over 25%, making prevention mandatory in higher-risk patients • High-risk characteristics include renal insufficiency (Cr > 1. 5 mg/d. L) and diabetes • Pathophysiology of CIN seems to involve contrast-induced renal medullary ischemia • Mannitol, furosemide, aminophylline, and “renal dose” dopamine are ineffective in preventing RCN • N-acetylcysteine has been shown to prevent CIN though data is somewhat controversial • Non ionic isoosmolar agents show promise
Summary • Contrast-Induced Nephropathy is a common complication of intravenous contrast exposure in higher-risk patients • Even with chemical resolution of CIN and a return of serum creatinine towards baseline, the 1 -year mortality remains over 25%, making prevention mandatory in higher-risk patients • High-risk characteristics include renal insufficiency (Cr > 1. 5 mg/d. L) and diabetes • Pathophysiology of CIN seems to involve contrast-induced renal medullary ischemia • Mannitol, furosemide, aminophylline, and “renal dose” dopamine are ineffective in preventing RCN • N-acetylcysteine has been shown to prevent CIN though data is somewhat controversial • Non ionic isoosmolar agents show promise
 Summary of Risk and Impact of CIN • Renal insufficiency is independently associated with all causes of mortality and cardiovascular mortality • Baseline renal insufficiency, diabetes, and dehydration predispose patients to contrast-induced renal failure • Once contrast-induced renal failure occurs, it is associated with a markedly higher in-hospital and long-term mortality following PCI • Diabetes and CRF have additive adverse effects on long-term prognosis after PCI • CIN dramatically increases hospital costs by increasing length of stay and need for dialysis
Summary of Risk and Impact of CIN • Renal insufficiency is independently associated with all causes of mortality and cardiovascular mortality • Baseline renal insufficiency, diabetes, and dehydration predispose patients to contrast-induced renal failure • Once contrast-induced renal failure occurs, it is associated with a markedly higher in-hospital and long-term mortality following PCI • Diabetes and CRF have additive adverse effects on long-term prognosis after PCI • CIN dramatically increases hospital costs by increasing length of stay and need for dialysis
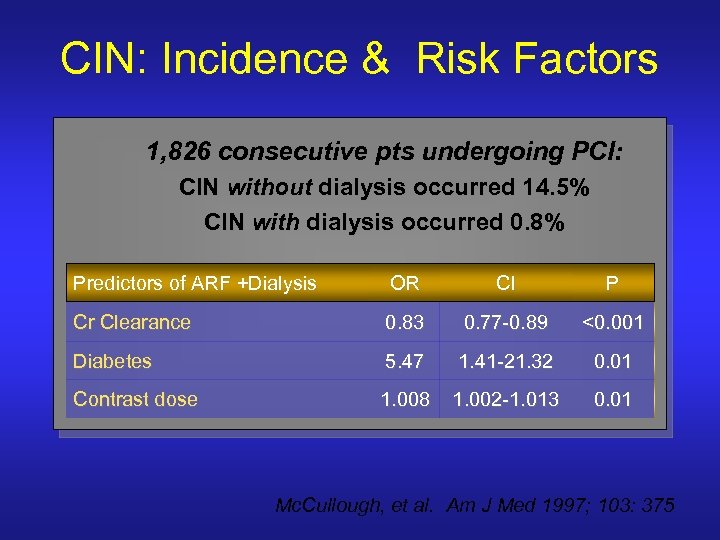 CIN: Incidence & Risk Factors 1, 826 consecutive pts undergoing PCI: CIN without dialysis occurred 14. 5% CIN with dialysis occurred 0. 8% Predictors of ARF +Dialysis OR CI P Cr Clearance 0. 83 0. 77 -0. 89 <0. 001 Diabetes 5. 47 1. 41 -21. 32 0. 01 Contrast dose 1. 008 1. 002 -1. 013 0. 01 Mc. Cullough, et al. Am J Med 1997; 103: 375
CIN: Incidence & Risk Factors 1, 826 consecutive pts undergoing PCI: CIN without dialysis occurred 14. 5% CIN with dialysis occurred 0. 8% Predictors of ARF +Dialysis OR CI P Cr Clearance 0. 83 0. 77 -0. 89 <0. 001 Diabetes 5. 47 1. 41 -21. 32 0. 01 Contrast dose 1. 008 1. 002 -1. 013 0. 01 Mc. Cullough, et al. Am J Med 1997; 103: 375
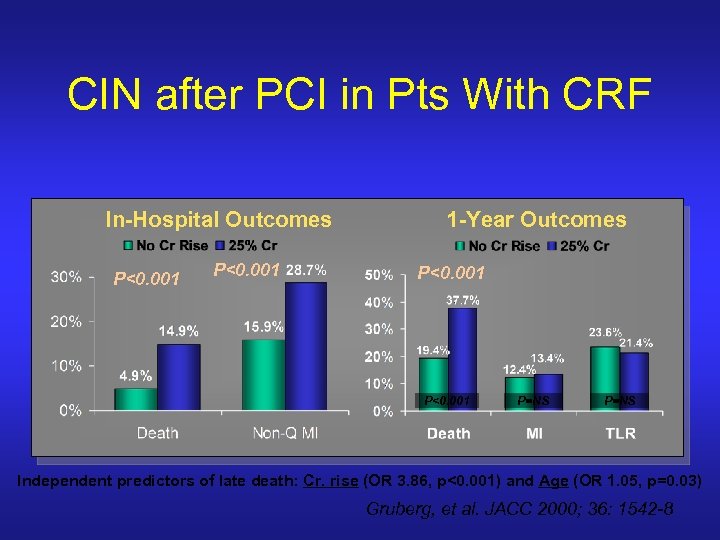 CIN after PCI in Pts With CRF In-Hospital Outcomes P<0. 001 1 -Year Outcomes P<0. 001 P=NS Independent predictors of late death: Cr. rise (OR 3. 86, p<0. 001) and Age (OR 1. 05, p=0. 03) Gruberg, et al. JACC 2000; 36: 1542 -8
CIN after PCI in Pts With CRF In-Hospital Outcomes P<0. 001 1 -Year Outcomes P<0. 001 P=NS Independent predictors of late death: Cr. rise (OR 3. 86, p<0. 001) and Age (OR 1. 05, p=0. 03) Gruberg, et al. JACC 2000; 36: 1542 -8
 Fenoldopam for Prevention of Contrast Nephropathy • Not currently FDA approved for this indication • Peripheral dopamine-1 receptor agonist • Proposed mechanism of renal protection: – vasodilatation of efferent and afferent arterioles – maintains or increases glomerular filtration rate – promotes natriuresis and diuresis
Fenoldopam for Prevention of Contrast Nephropathy • Not currently FDA approved for this indication • Peripheral dopamine-1 receptor agonist • Proposed mechanism of renal protection: – vasodilatation of efferent and afferent arterioles – maintains or increases glomerular filtration rate – promotes natriuresis and diuresis
 Renal Function Deterioration with Pre Existing Renal D • Independent Predictors: LVEF, Contrast Volume(not creatinine) • In hospital. Mortality 14. 9% vs. 4. 9%, 1 year 37. 7% vs. 19. 4% • 31% required dialysis – in hospital mortality 22. 6%, 1 year 45. 2%(35. 4% for those with renal deterioration not requiring dialysis)
Renal Function Deterioration with Pre Existing Renal D • Independent Predictors: LVEF, Contrast Volume(not creatinine) • In hospital. Mortality 14. 9% vs. 4. 9%, 1 year 37. 7% vs. 19. 4% • 31% required dialysis – in hospital mortality 22. 6%, 1 year 45. 2%(35. 4% for those with renal deterioration not requiring dialysis)


