b7c027ea1c405aab74c3320e912ea5e2.ppt
- Количество слайдов: 38
 Contrast Induced Nephropathy: Predictors, Prevention, and Management Roxana Mehran, MD Columbia University Medical Center Cardiovascular Research Foundation
Contrast Induced Nephropathy: Predictors, Prevention, and Management Roxana Mehran, MD Columbia University Medical Center Cardiovascular Research Foundation
 Disclosures: Research Grant to CRF: Tyco, Guerbert Consultant/ Advisory Board: Flow. Medica
Disclosures: Research Grant to CRF: Tyco, Guerbert Consultant/ Advisory Board: Flow. Medica
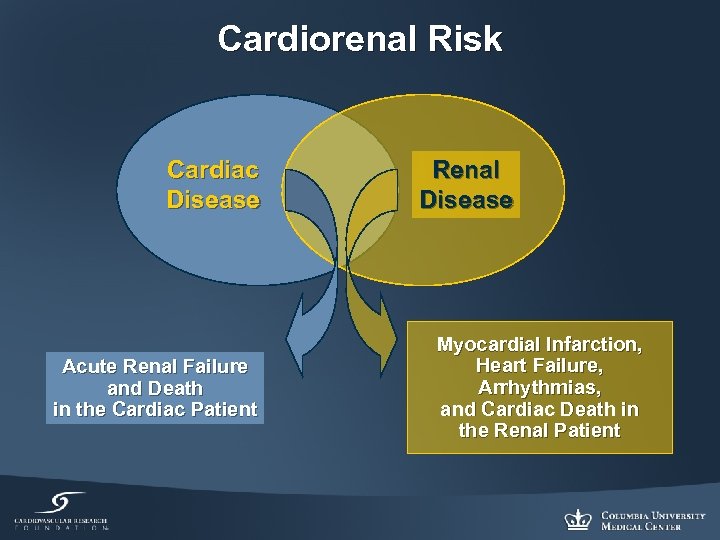 Cardiorenal Risk Cardiac Disease Acute Renal Failure and Death in the Cardiac Patient Renal Disease Myocardial Infarction, Heart Failure, Arrhythmias, and Cardiac Death in the Renal Patient
Cardiorenal Risk Cardiac Disease Acute Renal Failure and Death in the Cardiac Patient Renal Disease Myocardial Infarction, Heart Failure, Arrhythmias, and Cardiac Death in the Renal Patient
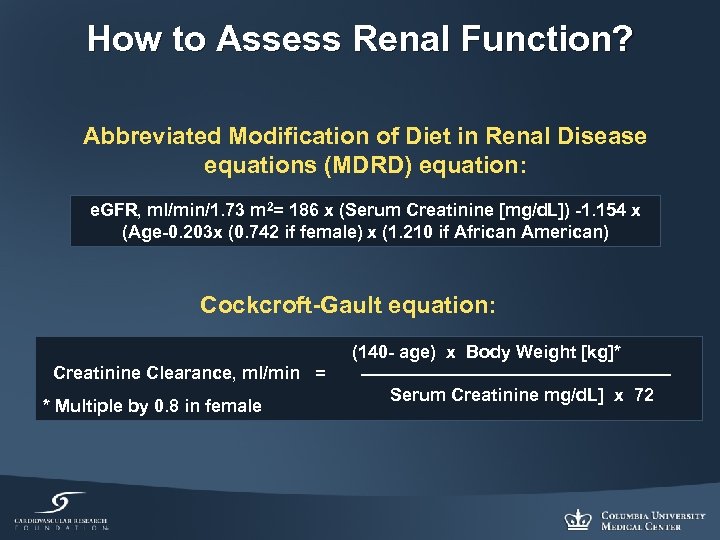 How to Assess Renal Function? Abbreviated Modification of Diet in Renal Disease equations (MDRD) equation: e. GFR, ml/min/1. 73 m 2= 186 x (Serum Creatinine [mg/d. L]) -1. 154 x (Age-0. 203 x (0. 742 if female) x (1. 210 if African American) Cockcroft-Gault equation: (140 - age) x Body Weight [kg]* Creatinine Clearance, ml/min = Serum Creatinine mg/d. L] x 72 * Multiple by 0. 8 in female
How to Assess Renal Function? Abbreviated Modification of Diet in Renal Disease equations (MDRD) equation: e. GFR, ml/min/1. 73 m 2= 186 x (Serum Creatinine [mg/d. L]) -1. 154 x (Age-0. 203 x (0. 742 if female) x (1. 210 if African American) Cockcroft-Gault equation: (140 - age) x Body Weight [kg]* Creatinine Clearance, ml/min = Serum Creatinine mg/d. L] x 72 * Multiple by 0. 8 in female
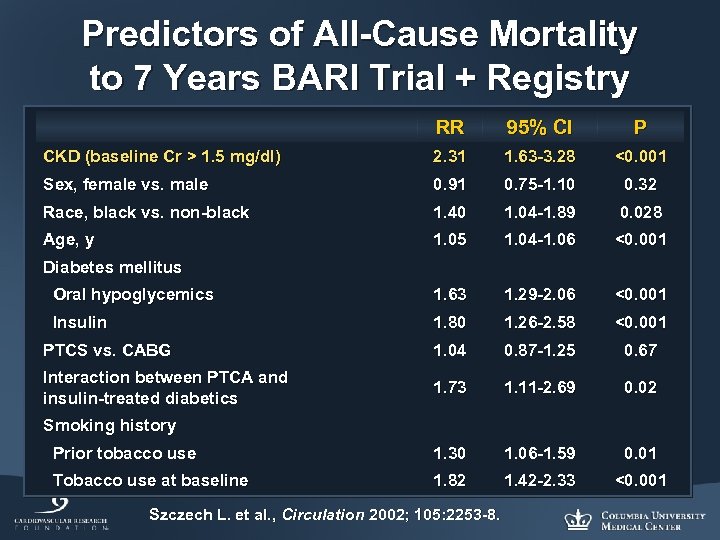 Predictors of All-Cause Mortality to 7 Years BARI Trial + Registry RR 95% CI P CKD (baseline Cr > 1. 5 mg/dl) 2. 31 1. 63 -3. 28 <0. 001 Sex, female vs. male 0. 91 0. 75 -1. 10 0. 32 Race, black vs. non-black 1. 40 1. 04 -1. 89 0. 028 Age, y 1. 05 1. 04 -1. 06 <0. 001 Oral hypoglycemics 1. 63 1. 29 -2. 06 <0. 001 Insulin 1. 80 1. 26 -2. 58 <0. 001 PTCS vs. CABG 1. 04 0. 87 -1. 25 0. 67 Interaction between PTCA and insulin-treated diabetics 1. 73 1. 11 -2. 69 0. 02 Prior tobacco use 1. 30 1. 06 -1. 59 0. 01 Tobacco use at baseline 1. 82 1. 42 -2. 33 <0. 001 Diabetes mellitus Smoking history Szczech L. et al. , Circulation 2002; 105: 2253 -8.
Predictors of All-Cause Mortality to 7 Years BARI Trial + Registry RR 95% CI P CKD (baseline Cr > 1. 5 mg/dl) 2. 31 1. 63 -3. 28 <0. 001 Sex, female vs. male 0. 91 0. 75 -1. 10 0. 32 Race, black vs. non-black 1. 40 1. 04 -1. 89 0. 028 Age, y 1. 05 1. 04 -1. 06 <0. 001 Oral hypoglycemics 1. 63 1. 29 -2. 06 <0. 001 Insulin 1. 80 1. 26 -2. 58 <0. 001 PTCS vs. CABG 1. 04 0. 87 -1. 25 0. 67 Interaction between PTCA and insulin-treated diabetics 1. 73 1. 11 -2. 69 0. 02 Prior tobacco use 1. 30 1. 06 -1. 59 0. 01 Tobacco use at baseline 1. 82 1. 42 -2. 33 <0. 001 Diabetes mellitus Smoking history Szczech L. et al. , Circulation 2002; 105: 2253 -8.
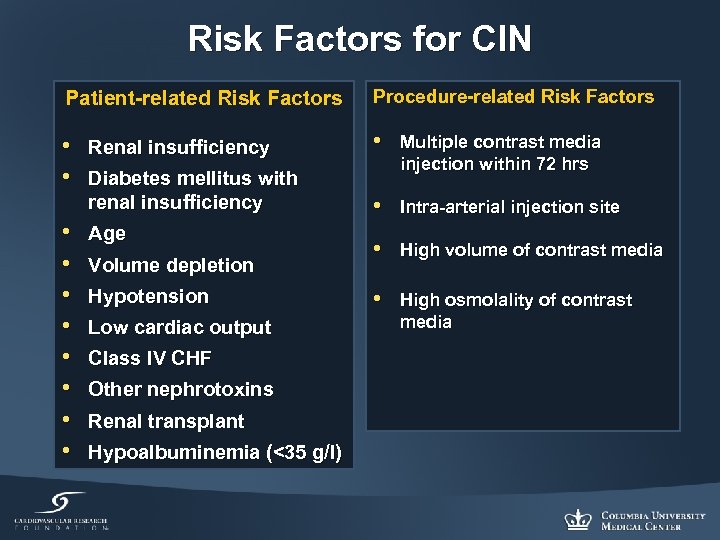 Risk Factors for CIN Patient-related Risk Factors Procedure-related Risk Factors • • Renal insufficiency • Diabetes mellitus with renal insufficiency • • Age Volume depletion Hypotension Low cardiac output Class IV CHF Other nephrotoxins Renal transplant Hypoalbuminemia (<35 g/l) Multiple contrast media injection within 72 hrs • Intra-arterial injection site • High volume of contrast media • High osmolality of contrast media
Risk Factors for CIN Patient-related Risk Factors Procedure-related Risk Factors • • Renal insufficiency • Diabetes mellitus with renal insufficiency • • Age Volume depletion Hypotension Low cardiac output Class IV CHF Other nephrotoxins Renal transplant Hypoalbuminemia (<35 g/l) Multiple contrast media injection within 72 hrs • Intra-arterial injection site • High volume of contrast media • High osmolality of contrast media
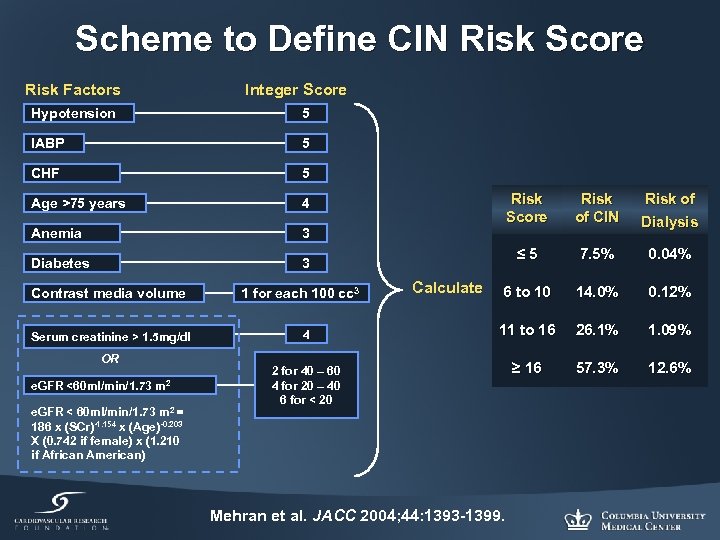 Scheme to Define CIN Risk Score Risk Factors Integer Score Hypotension 5 IABP 5 CHF 5 Age >75 years 4 Anemia 3 Diabetes 3 Contrast media volume Serum creatinine > 1. 5 mg/dl OR e. GFR <60 ml/min/1. 73 m 2 e. GFR < 60 ml/min/1. 73 m 2 = 186 x (SCr)-1. 154 x (Age)-0. 203 X (0. 742 if female) x (1. 210 if African American) 1 for each 100 cc 3 4 Risk Score Dialysis ≤ 5 Calculate Risk of CIN 7. 5% 0. 04% 6 to 10 14. 0% 0. 12% 11 to 16 26. 1% 1. 09% ≥ 16 57. 3% 12. 6% 2 for 40 – 60 4 for 20 – 40 6 for < 20 Mehran et al. JACC 2004; 44: 1393 -1399. Risk of
Scheme to Define CIN Risk Score Risk Factors Integer Score Hypotension 5 IABP 5 CHF 5 Age >75 years 4 Anemia 3 Diabetes 3 Contrast media volume Serum creatinine > 1. 5 mg/dl OR e. GFR <60 ml/min/1. 73 m 2 e. GFR < 60 ml/min/1. 73 m 2 = 186 x (SCr)-1. 154 x (Age)-0. 203 X (0. 742 if female) x (1. 210 if African American) 1 for each 100 cc 3 4 Risk Score Dialysis ≤ 5 Calculate Risk of CIN 7. 5% 0. 04% 6 to 10 14. 0% 0. 12% 11 to 16 26. 1% 1. 09% ≥ 16 57. 3% 12. 6% 2 for 40 – 60 4 for 20 – 40 6 for < 20 Mehran et al. JACC 2004; 44: 1393 -1399. Risk of
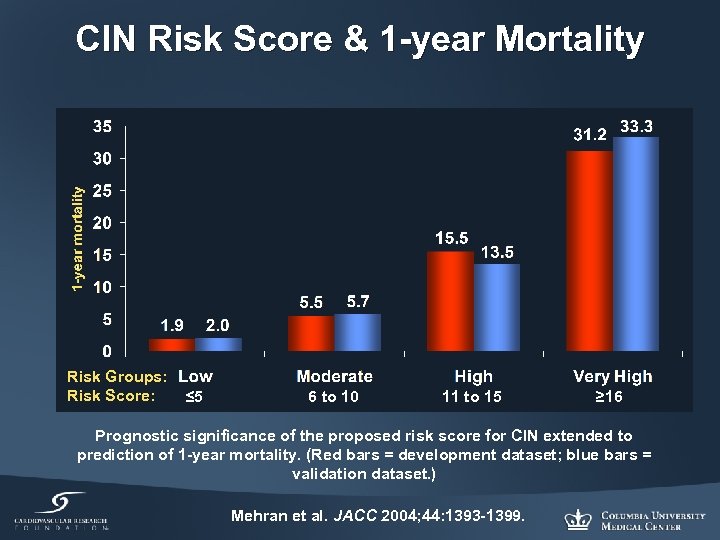 CIN Risk Score & 1 -year Mortality Risk Groups: Risk Score: ≤ 5 6 to 10 11 to 15 ≥ 16 Prognostic significance of the proposed risk score for CIN extended to prediction of 1 -year mortality. (Red bars = development dataset; blue bars = validation dataset. ) Mehran et al. JACC 2004; 44: 1393 -1399.
CIN Risk Score & 1 -year Mortality Risk Groups: Risk Score: ≤ 5 6 to 10 11 to 15 ≥ 16 Prognostic significance of the proposed risk score for CIN extended to prediction of 1 -year mortality. (Red bars = development dataset; blue bars = validation dataset. ) Mehran et al. JACC 2004; 44: 1393 -1399.
 Preventive Trials
Preventive Trials
 Hydration
Hydration
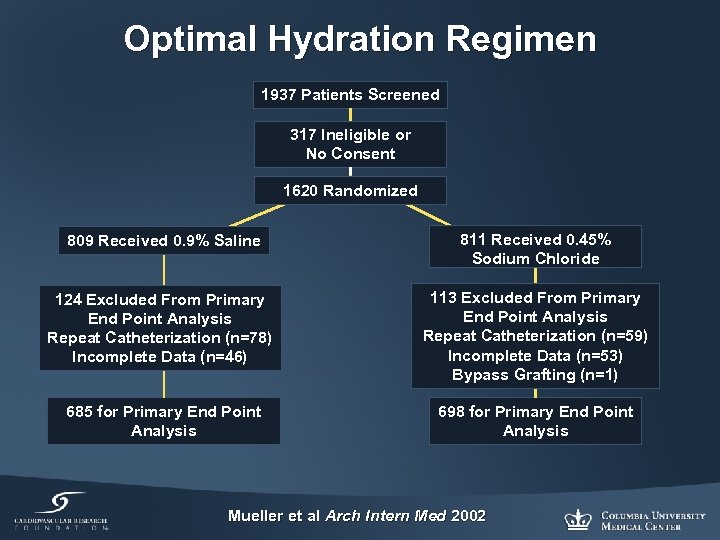 Optimal Hydration Regimen 1937 Patients Screened 317 Ineligible or No Consent 1620 Randomized 809 Received 0. 9% Saline 811 Received 0. 45% Sodium Chloride 124 Excluded From Primary End Point Analysis Repeat Catheterization (n=78) Incomplete Data (n=46) 113 Excluded From Primary End Point Analysis Repeat Catheterization (n=59) Incomplete Data (n=53) Bypass Grafting (n=1) 685 for Primary End Point Analysis 698 for Primary End Point Analysis Mueller et al Arch Intern Med 2002
Optimal Hydration Regimen 1937 Patients Screened 317 Ineligible or No Consent 1620 Randomized 809 Received 0. 9% Saline 811 Received 0. 45% Sodium Chloride 124 Excluded From Primary End Point Analysis Repeat Catheterization (n=78) Incomplete Data (n=46) 113 Excluded From Primary End Point Analysis Repeat Catheterization (n=59) Incomplete Data (n=53) Bypass Grafting (n=1) 685 for Primary End Point Analysis 698 for Primary End Point Analysis Mueller et al Arch Intern Med 2002
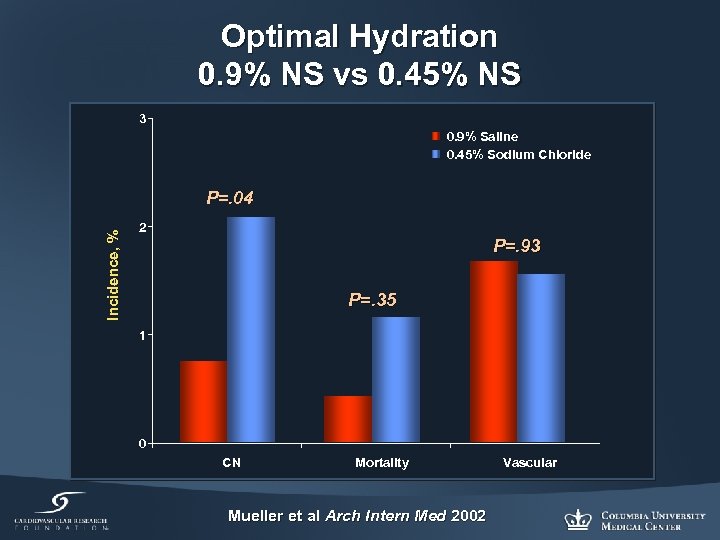 Optimal Hydration 0. 9% NS vs 0. 45% NS 3 0. 9% Saline 0. 45% Sodium Chloride Incidence, % P=. 04 2 P=. 93 P=. 35 1 0 CN Mortality Mueller et al Arch Intern Med 2002 Vascular
Optimal Hydration 0. 9% NS vs 0. 45% NS 3 0. 9% Saline 0. 45% Sodium Chloride Incidence, % P=. 04 2 P=. 93 P=. 35 1 0 CN Mortality Mueller et al Arch Intern Med 2002 Vascular
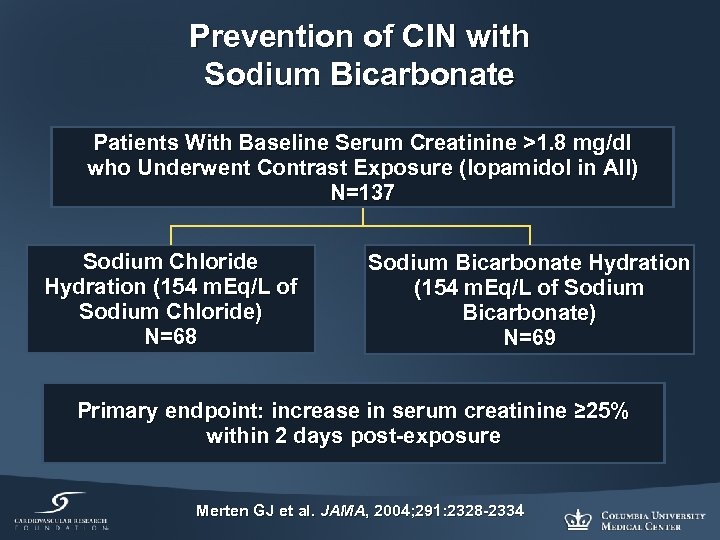 Prevention of CIN with Sodium Bicarbonate Patients With Baseline Serum Creatinine >1. 8 mg/dl who Underwent Contrast Exposure (Iopamidol in All) N=137 Sodium Chloride Hydration (154 m. Eq/L of Sodium Chloride) N=68 Sodium Bicarbonate Hydration (154 m. Eq/L of Sodium Bicarbonate) N=69 Primary endpoint: increase in serum creatinine ≥ 25% within 2 days post-exposure Merten GJ et al. JAMA, 2004; 291: 2328 -2334
Prevention of CIN with Sodium Bicarbonate Patients With Baseline Serum Creatinine >1. 8 mg/dl who Underwent Contrast Exposure (Iopamidol in All) N=137 Sodium Chloride Hydration (154 m. Eq/L of Sodium Chloride) N=68 Sodium Bicarbonate Hydration (154 m. Eq/L of Sodium Bicarbonate) N=69 Primary endpoint: increase in serum creatinine ≥ 25% within 2 days post-exposure Merten GJ et al. JAMA, 2004; 291: 2328 -2334
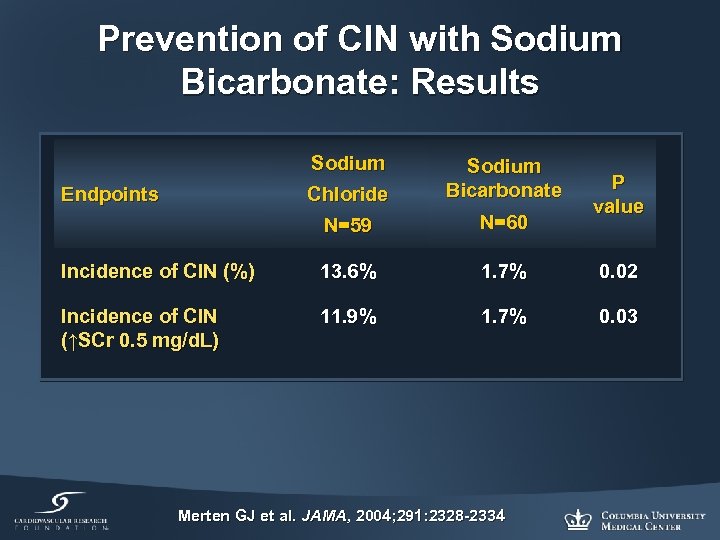 Prevention of CIN with Sodium Bicarbonate: Results Sodium Chloride Sodium Bicarbonate N=59 N=60 Incidence of CIN (%) 13. 6% 1. 7% 0. 02 Incidence of CIN (↑SCr 0. 5 mg/d. L) 11. 9% 1. 7% 0. 03 Endpoints Merten GJ et al. JAMA, 2004; 291: 2328 -2334 P value
Prevention of CIN with Sodium Bicarbonate: Results Sodium Chloride Sodium Bicarbonate N=59 N=60 Incidence of CIN (%) 13. 6% 1. 7% 0. 02 Incidence of CIN (↑SCr 0. 5 mg/d. L) 11. 9% 1. 7% 0. 03 Endpoints Merten GJ et al. JAMA, 2004; 291: 2328 -2334 P value
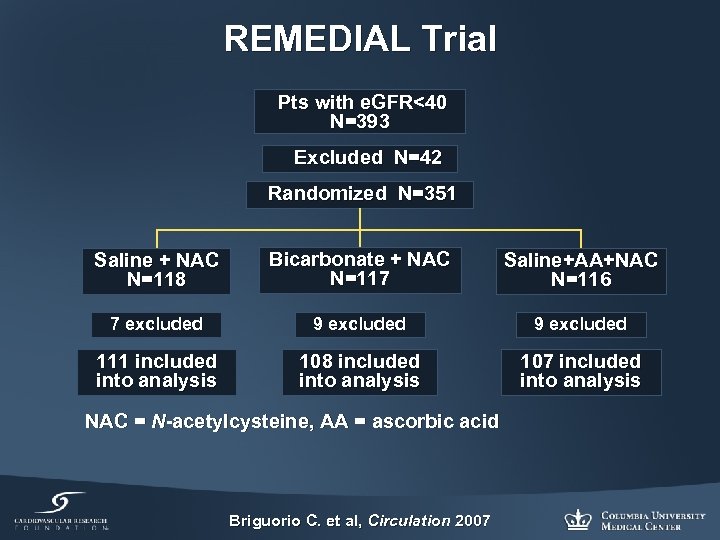 REMEDIAL Trial Pts with e. GFR<40 N=393 Excluded N=42 Randomized N=351 Saline + NAC N=118 Bicarbonate + NAC N=117 Saline+AA+NAC N=116 7 excluded 9 excluded 111 included into analysis 108 included into analysis 107 included into analysis NAC = N-acetylcysteine, AA = ascorbic acid Briguorio C. et al, Circulation 2007
REMEDIAL Trial Pts with e. GFR<40 N=393 Excluded N=42 Randomized N=351 Saline + NAC N=118 Bicarbonate + NAC N=117 Saline+AA+NAC N=116 7 excluded 9 excluded 111 included into analysis 108 included into analysis 107 included into analysis NAC = N-acetylcysteine, AA = ascorbic acid Briguorio C. et al, Circulation 2007
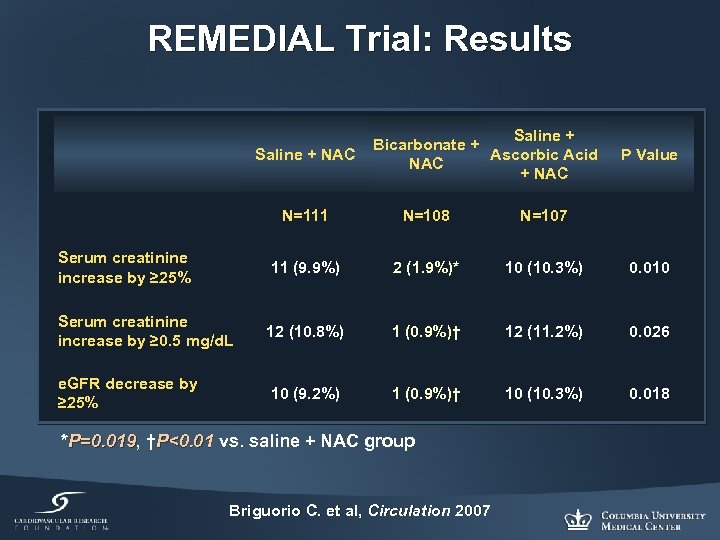 REMEDIAL Trial: Results Saline + Bicarbonate + Ascorbic Acid Saline + NAC P Value N=111 N=108 N=107 Serum creatinine increase by ≥ 25% 11 (9. 9%) 2 (1. 9%)* 10 (10. 3%) 0. 010 Serum creatinine increase by ≥ 0. 5 mg/d. L 12 (10. 8%) 1 (0. 9%)† 12 (11. 2%) 0. 026 e. GFR decrease by ≥ 25% 10 (9. 2%) 1 (0. 9%)† 10 (10. 3%) 0. 018 *P=0. 019, †P<0. 01 vs. saline + NAC group P=0. 019 P<0. 01 Briguorio C. et al, Circulation 2007
REMEDIAL Trial: Results Saline + Bicarbonate + Ascorbic Acid Saline + NAC P Value N=111 N=108 N=107 Serum creatinine increase by ≥ 25% 11 (9. 9%) 2 (1. 9%)* 10 (10. 3%) 0. 010 Serum creatinine increase by ≥ 0. 5 mg/d. L 12 (10. 8%) 1 (0. 9%)† 12 (11. 2%) 0. 026 e. GFR decrease by ≥ 25% 10 (9. 2%) 1 (0. 9%)† 10 (10. 3%) 0. 018 *P=0. 019, †P<0. 01 vs. saline + NAC group P=0. 019 P<0. 01 Briguorio C. et al, Circulation 2007
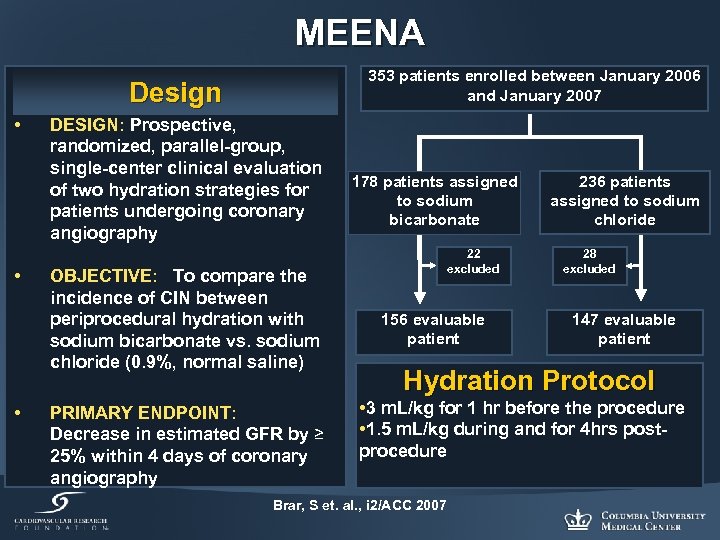 MEENA 353 patients enrolled between January 2006 and January 2007 Design • • • DESIGN: Prospective, randomized, parallel-group, single-center clinical evaluation of two hydration strategies for patients undergoing coronary angiography OBJECTIVE: To compare the incidence of CIN between periprocedural hydration with sodium bicarbonate vs. sodium chloride (0. 9%, normal saline) PRIMARY ENDPOINT: Decrease in estimated GFR by ≥ 25% within 4 days of coronary angiography 178 patients assigned to sodium bicarbonate 22 excluded 156 evaluable patient 236 patients assigned to sodium chloride 28 excluded 147 evaluable patient Hydration Protocol • 3 m. L/kg for 1 hr before the procedure • 1. 5 m. L/kg during and for 4 hrs postprocedure Brar, S et. al. , i 2/ACC 2007
MEENA 353 patients enrolled between January 2006 and January 2007 Design • • • DESIGN: Prospective, randomized, parallel-group, single-center clinical evaluation of two hydration strategies for patients undergoing coronary angiography OBJECTIVE: To compare the incidence of CIN between periprocedural hydration with sodium bicarbonate vs. sodium chloride (0. 9%, normal saline) PRIMARY ENDPOINT: Decrease in estimated GFR by ≥ 25% within 4 days of coronary angiography 178 patients assigned to sodium bicarbonate 22 excluded 156 evaluable patient 236 patients assigned to sodium chloride 28 excluded 147 evaluable patient Hydration Protocol • 3 m. L/kg for 1 hr before the procedure • 1. 5 m. L/kg during and for 4 hrs postprocedure Brar, S et. al. , i 2/ACC 2007
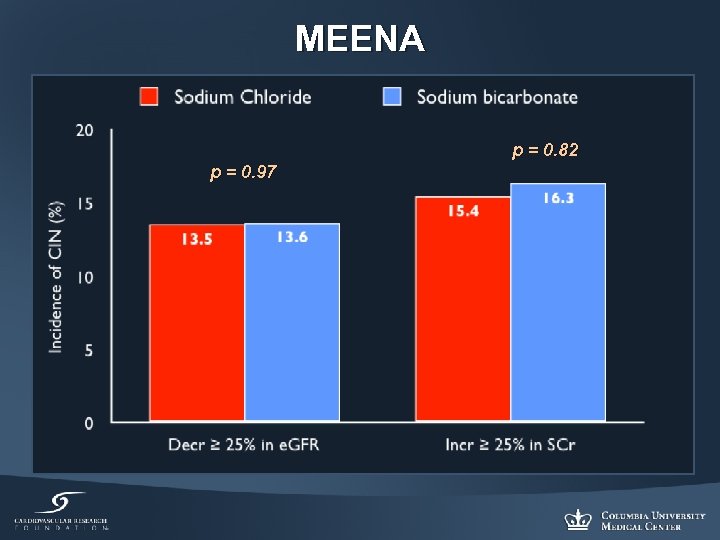 MEENA p = 0. 82 p = 0. 97
MEENA p = 0. 82 p = 0. 97
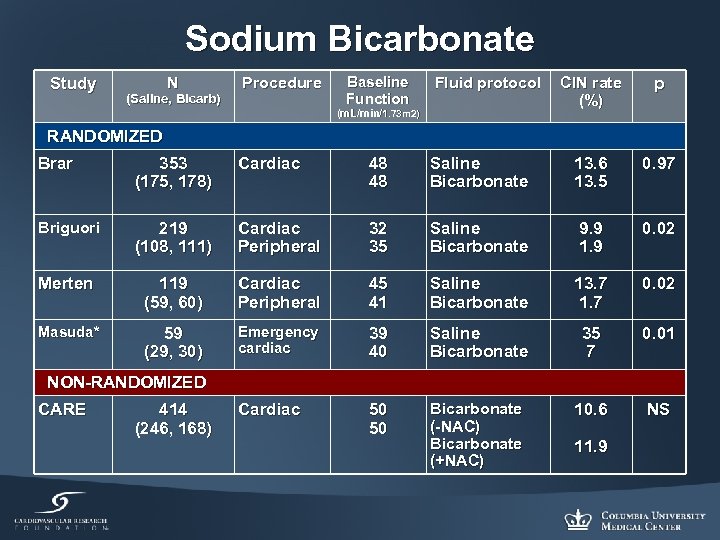 Sodium Bicarbonate Study N (Saline, Bicarb) Procedure Baseline Function Fluid protocol (m. L/min/1. 73 m 2) CIN rate (%) p RANDOMIZED Brar 353 (175, 178) Cardiac 48 48 Saline Bicarbonate 13. 6 13. 5 0. 97 Briguori 219 (108, 111) Cardiac Peripheral 32 35 Saline Bicarbonate 9. 9 1. 9 0. 02 Merten 119 (59, 60) Cardiac Peripheral 45 41 Saline Bicarbonate 13. 7 1. 7 0. 02 Masuda* 59 (29, 30) Emergency cardiac 39 40 Saline Bicarbonate 35 7 0. 01 Cardiac 50 50 Bicarbonate (-NAC) Bicarbonate (+NAC) 10. 6 NS NON-RANDOMIZED CARE 414 (246, 168) 11. 9
Sodium Bicarbonate Study N (Saline, Bicarb) Procedure Baseline Function Fluid protocol (m. L/min/1. 73 m 2) CIN rate (%) p RANDOMIZED Brar 353 (175, 178) Cardiac 48 48 Saline Bicarbonate 13. 6 13. 5 0. 97 Briguori 219 (108, 111) Cardiac Peripheral 32 35 Saline Bicarbonate 9. 9 1. 9 0. 02 Merten 119 (59, 60) Cardiac Peripheral 45 41 Saline Bicarbonate 13. 7 1. 7 0. 02 Masuda* 59 (29, 30) Emergency cardiac 39 40 Saline Bicarbonate 35 7 0. 01 Cardiac 50 50 Bicarbonate (-NAC) Bicarbonate (+NAC) 10. 6 NS NON-RANDOMIZED CARE 414 (246, 168) 11. 9
 N-ACETYLCYSTEINE (NAC)
N-ACETYLCYSTEINE (NAC)
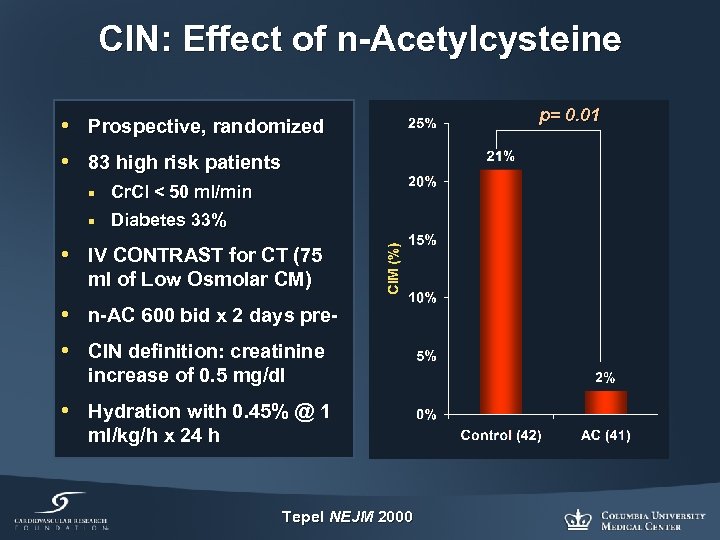 CIN: Effect of n-Acetylcysteine • Prospective, randomized • 83 high risk patients ¡ Cr. Cl < 50 ml/min ¡ Diabetes 33% • IV CONTRAST for CT (75 ml of Low Osmolar CM) • n-AC 600 bid x 2 days pre • CIN definition: creatinine increase of 0. 5 mg/dl • Hydration with 0. 45% @ 1 ml/kg/h x 24 h Tepel NEJM 2000 p= 0. 01
CIN: Effect of n-Acetylcysteine • Prospective, randomized • 83 high risk patients ¡ Cr. Cl < 50 ml/min ¡ Diabetes 33% • IV CONTRAST for CT (75 ml of Low Osmolar CM) • n-AC 600 bid x 2 days pre • CIN definition: creatinine increase of 0. 5 mg/dl • Hydration with 0. 45% @ 1 ml/kg/h x 24 h Tepel NEJM 2000 p= 0. 01
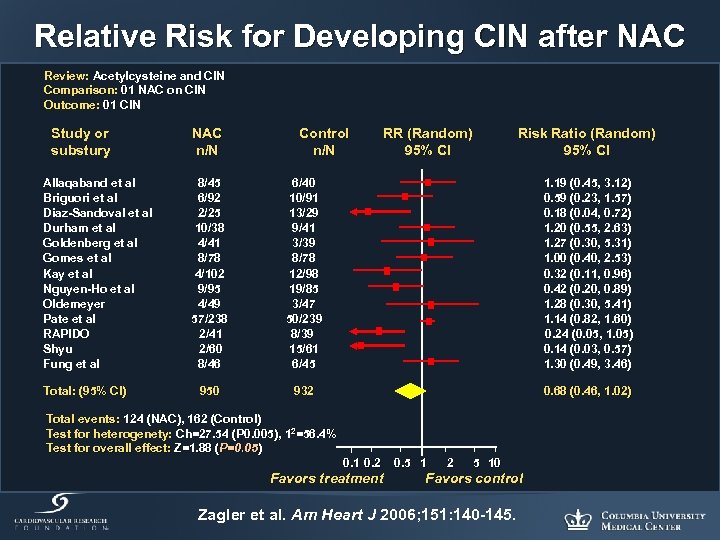 Relative Risk for Developing CIN after NAC Review: Acetylcysteine and CIN Comparison: 01 NAC on CIN Outcome: 01 CIN Study or substury Allaqaband et al Briguori et al Diaz-Sandoval et al Durham et al Goldenberg et al Gomes et al Kay et al Nguyen-Ho et al Oldemeyer Pate et al RAPIDO Shyu Fung et al Total: (95% Cl) NAC n/N Control n/N RR (Random) 95% Cl Risk Ratio (Random) 95% Cl 8/45 6/92 2/25 10/38 4/41 8/78 4/102 9/95 4/49 57/238 2/41 2/60 8/46 6/40 10/91 13/29 9/41 3/39 8/78 12/98 19/85 3/47 50/239 8/39 15/61 6/45 1. 19 (0. 45, 3. 12) 0. 59 (0. 23, 1. 57) 0. 18 (0. 04, 0. 72) 1. 20 (0. 55, 2. 63) 1. 27 (0. 30, 5. 31) 1. 00 (0. 40, 2. 53) 0. 32 (0. 11, 0. 96) 0. 42 (0. 20, 0. 89) 1. 28 (0. 30, 5. 41) 1. 14 (0. 82, 1. 60) 0. 24 (0. 05, 1. 05) 0. 14 (0. 03, 0. 57) 1. 30 (0. 49, 3. 46) 950 932 0. 68 (0. 46, 1. 02) Total events: 124 (NAC), 162 (Control) Test for heterogenety: Ch=27. 54 (P 0. 005), 12=56. 4% Test for heterogenety: Ch=27. 54 (P 0. 005), 1 Test for overall effect: Z=1. 88 (P=0. 05) 0. 1 0. 2 Favors treatment 0. 5 1 2 5 10 Favors control Zagler et al. Am Heart J 2006; 151: 140 -145.
Relative Risk for Developing CIN after NAC Review: Acetylcysteine and CIN Comparison: 01 NAC on CIN Outcome: 01 CIN Study or substury Allaqaband et al Briguori et al Diaz-Sandoval et al Durham et al Goldenberg et al Gomes et al Kay et al Nguyen-Ho et al Oldemeyer Pate et al RAPIDO Shyu Fung et al Total: (95% Cl) NAC n/N Control n/N RR (Random) 95% Cl Risk Ratio (Random) 95% Cl 8/45 6/92 2/25 10/38 4/41 8/78 4/102 9/95 4/49 57/238 2/41 2/60 8/46 6/40 10/91 13/29 9/41 3/39 8/78 12/98 19/85 3/47 50/239 8/39 15/61 6/45 1. 19 (0. 45, 3. 12) 0. 59 (0. 23, 1. 57) 0. 18 (0. 04, 0. 72) 1. 20 (0. 55, 2. 63) 1. 27 (0. 30, 5. 31) 1. 00 (0. 40, 2. 53) 0. 32 (0. 11, 0. 96) 0. 42 (0. 20, 0. 89) 1. 28 (0. 30, 5. 41) 1. 14 (0. 82, 1. 60) 0. 24 (0. 05, 1. 05) 0. 14 (0. 03, 0. 57) 1. 30 (0. 49, 3. 46) 950 932 0. 68 (0. 46, 1. 02) Total events: 124 (NAC), 162 (Control) Test for heterogenety: Ch=27. 54 (P 0. 005), 12=56. 4% Test for heterogenety: Ch=27. 54 (P 0. 005), 1 Test for overall effect: Z=1. 88 (P=0. 05) 0. 1 0. 2 Favors treatment 0. 5 1 2 5 10 Favors control Zagler et al. Am Heart J 2006; 151: 140 -145.
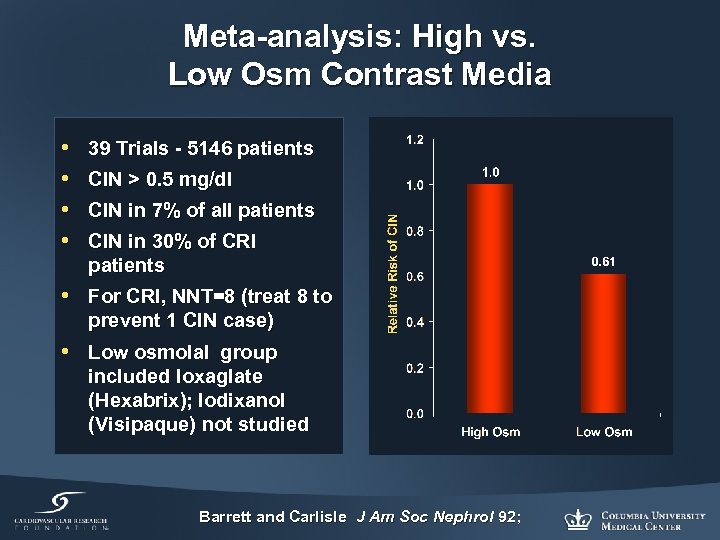 Meta-analysis: High vs. Low Osm Contrast Media • • 39 Trials - 5146 patients CIN > 0. 5 mg/dl CIN in 7% of all patients CIN in 30% of CRI patients • For CRI, NNT=8 (treat 8 to prevent 1 CIN case) • Low osmolal group included Ioxaglate (Hexabrix); Iodixanol (Visipaque) not studied Barrett and Carlisle J Am Soc Nephrol 92;
Meta-analysis: High vs. Low Osm Contrast Media • • 39 Trials - 5146 patients CIN > 0. 5 mg/dl CIN in 7% of all patients CIN in 30% of CRI patients • For CRI, NNT=8 (treat 8 to prevent 1 CIN case) • Low osmolal group included Ioxaglate (Hexabrix); Iodixanol (Visipaque) not studied Barrett and Carlisle J Am Soc Nephrol 92;
 The NEPHRIC Study Nephrotoxicity in High-risk Patients a Double Blind Randomized Multicentre Study of Iso-osmolar and Low-osmolar Non-ionic Contrast Media
The NEPHRIC Study Nephrotoxicity in High-risk Patients a Double Blind Randomized Multicentre Study of Iso-osmolar and Low-osmolar Non-ionic Contrast Media
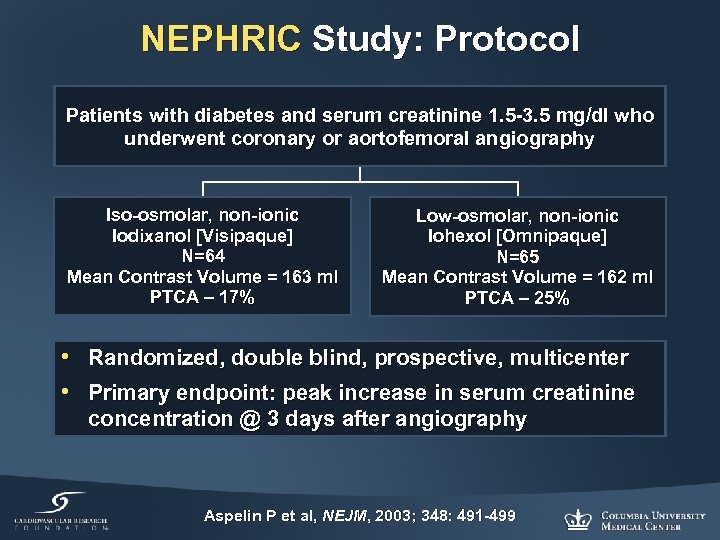 NEPHRIC Study: Protocol Patients with diabetes and serum creatinine 1. 5 -3. 5 mg/dl who underwent coronary or aortofemoral angiography Iso-osmolar, non-ionic Iodixanol [Visipaque] N=64 Mean Contrast Volume = 163 ml PTCA – 17% Low-osmolar, non-ionic Iohexol [Omnipaque] N=65 Mean Contrast Volume = 162 ml PTCA – 25% • Randomized, double blind, prospective, multicenter • Primary endpoint: peak increase in serum creatinine concentration @ 3 days after angiography Aspelin P et al, NEJM, 2003; 348: 491 -499
NEPHRIC Study: Protocol Patients with diabetes and serum creatinine 1. 5 -3. 5 mg/dl who underwent coronary or aortofemoral angiography Iso-osmolar, non-ionic Iodixanol [Visipaque] N=64 Mean Contrast Volume = 163 ml PTCA – 17% Low-osmolar, non-ionic Iohexol [Omnipaque] N=65 Mean Contrast Volume = 162 ml PTCA – 25% • Randomized, double blind, prospective, multicenter • Primary endpoint: peak increase in serum creatinine concentration @ 3 days after angiography Aspelin P et al, NEJM, 2003; 348: 491 -499
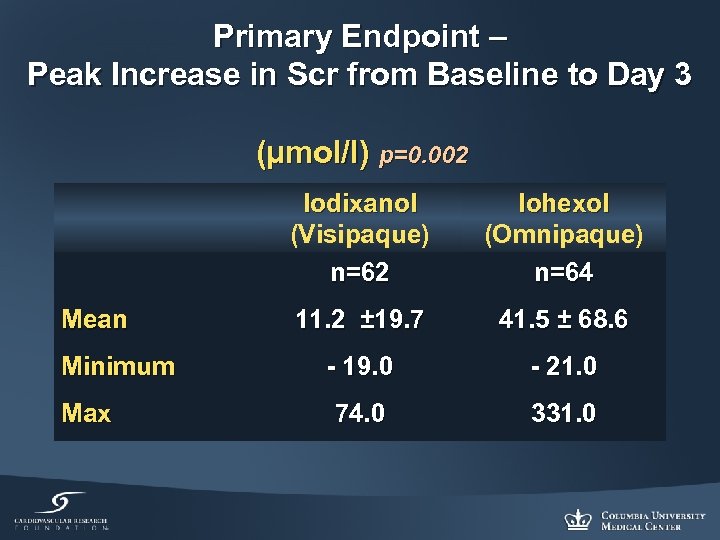 Primary Endpoint – Peak Increase in Scr from Baseline to Day 3 (µmol/l) p=0. 002 Iodixanol (Visipaque) n=62 Mean Minimum Max Iohexol (Omnipaque) n=64 11. 2 ± 19. 7 41. 5 ± 68. 6 - 19. 0 - 21. 0 74. 0 331. 0
Primary Endpoint – Peak Increase in Scr from Baseline to Day 3 (µmol/l) p=0. 002 Iodixanol (Visipaque) n=62 Mean Minimum Max Iohexol (Omnipaque) n=64 11. 2 ± 19. 7 41. 5 ± 68. 6 - 19. 0 - 21. 0 74. 0 331. 0
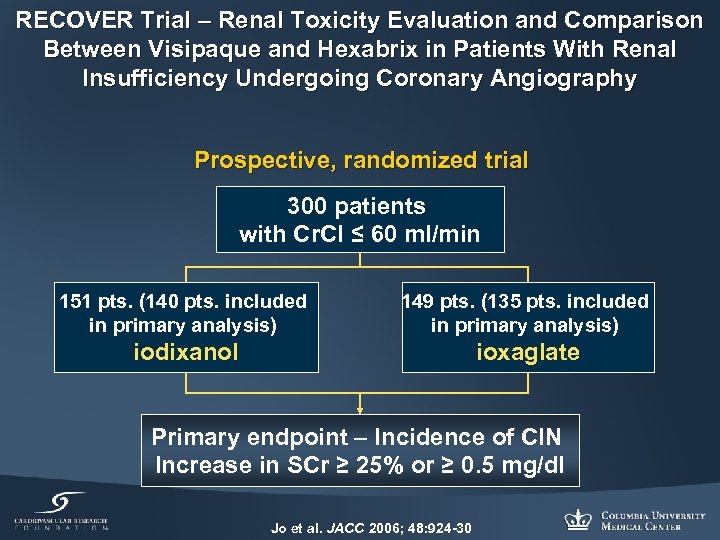 RECOVER Trial – Renal Toxicity Evaluation and Comparison Between Visipaque and Hexabrix in Patients With Renal Insufficiency Undergoing Coronary Angiography Prospective, randomized trial 300 patients with Cr. Cl ≤ 60 ml/min 151 pts. (140 pts. included in primary analysis) 149 pts. (135 pts. included in primary analysis) iodixanol ioxaglate Primary endpoint – Incidence of CIN Increase in SCr ≥ 25% or ≥ 0. 5 mg/dl Jo et al. JACC 2006; 48: 924 -30
RECOVER Trial – Renal Toxicity Evaluation and Comparison Between Visipaque and Hexabrix in Patients With Renal Insufficiency Undergoing Coronary Angiography Prospective, randomized trial 300 patients with Cr. Cl ≤ 60 ml/min 151 pts. (140 pts. included in primary analysis) 149 pts. (135 pts. included in primary analysis) iodixanol ioxaglate Primary endpoint – Incidence of CIN Increase in SCr ≥ 25% or ≥ 0. 5 mg/dl Jo et al. JACC 2006; 48: 924 -30
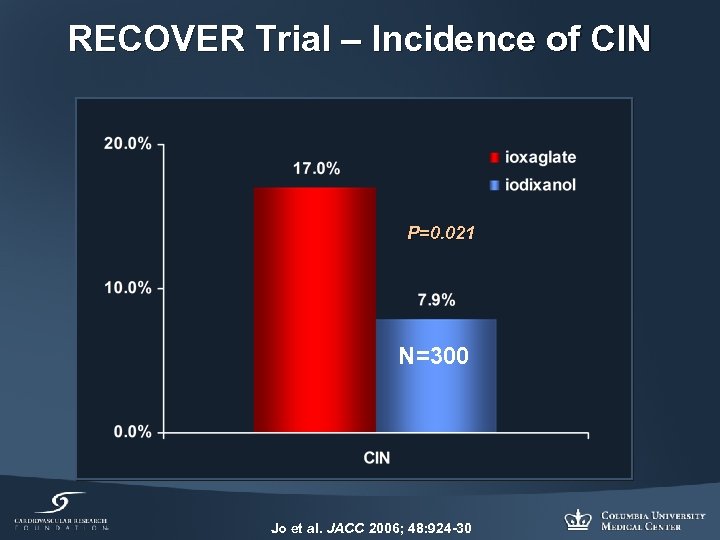 RECOVER Trial – Incidence of CIN P=0. 021 N=300 Jo et al. JACC 2006; 48: 924 -30
RECOVER Trial – Incidence of CIN P=0. 021 N=300 Jo et al. JACC 2006; 48: 924 -30
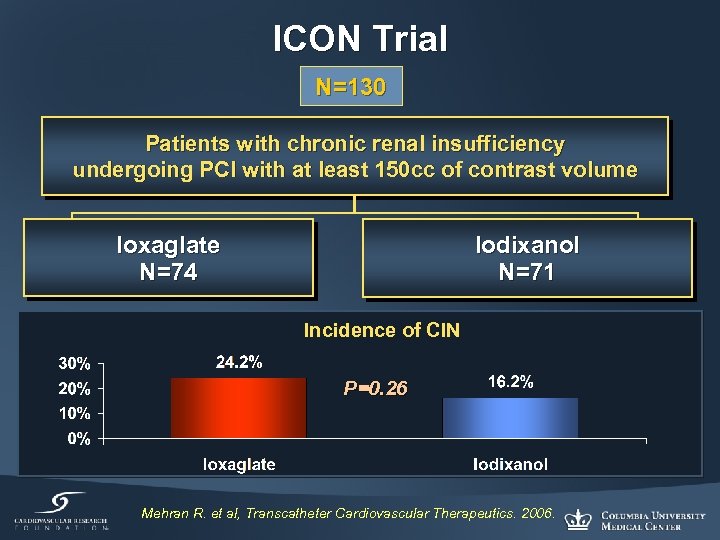 ICON Trial N=130 Patients with chronic renal insufficiency undergoing PCI with at least 150 cc of contrast volume Ioxaglate N=74 Iodixanol N=71 Incidence of CIN P=0. 26 Mehran R. et al, Transcatheter Cardiovascular Therapeutics. 2006.
ICON Trial N=130 Patients with chronic renal insufficiency undergoing PCI with at least 150 cc of contrast volume Ioxaglate N=74 Iodixanol N=71 Incidence of CIN P=0. 26 Mehran R. et al, Transcatheter Cardiovascular Therapeutics. 2006.
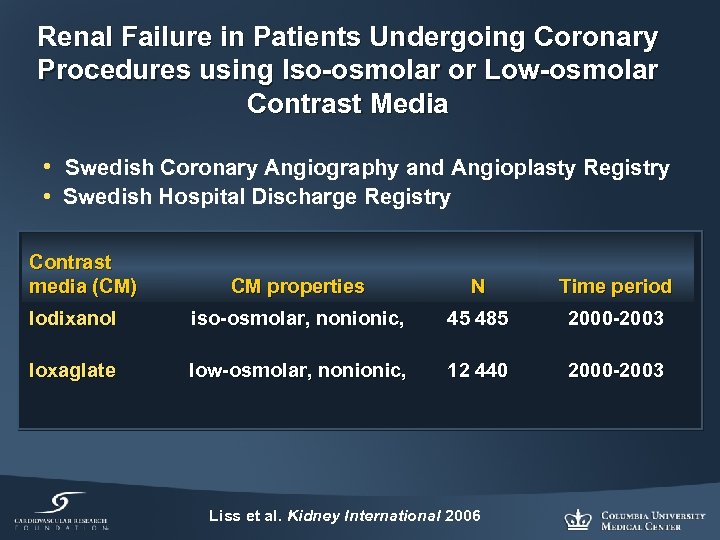 Renal Failure in Patients Undergoing Coronary Procedures using Iso-osmolar or Low-osmolar Contrast Media • Swedish Coronary Angiography and Angioplasty Registry • Swedish Hospital Discharge Registry Contrast media (CM) CM properties N Time period Iodixanol iso-osmolar, nonionic, 45 485 2000 -2003 Ioxaglate low-osmolar, nonionic, 12 440 2000 -2003 Liss et al. Kidney International 2006
Renal Failure in Patients Undergoing Coronary Procedures using Iso-osmolar or Low-osmolar Contrast Media • Swedish Coronary Angiography and Angioplasty Registry • Swedish Hospital Discharge Registry Contrast media (CM) CM properties N Time period Iodixanol iso-osmolar, nonionic, 45 485 2000 -2003 Ioxaglate low-osmolar, nonionic, 12 440 2000 -2003 Liss et al. Kidney International 2006
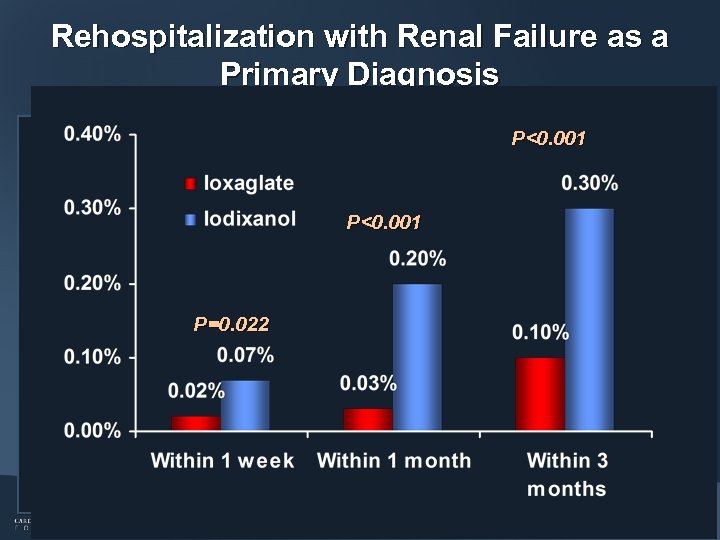 Rehospitalization with Renal Failure as a Primary Diagnosis P<0. 001 P=0. 022 Liss et al. Kidney International 2006
Rehospitalization with Renal Failure as a Primary Diagnosis P<0. 001 P=0. 022 Liss et al. Kidney International 2006
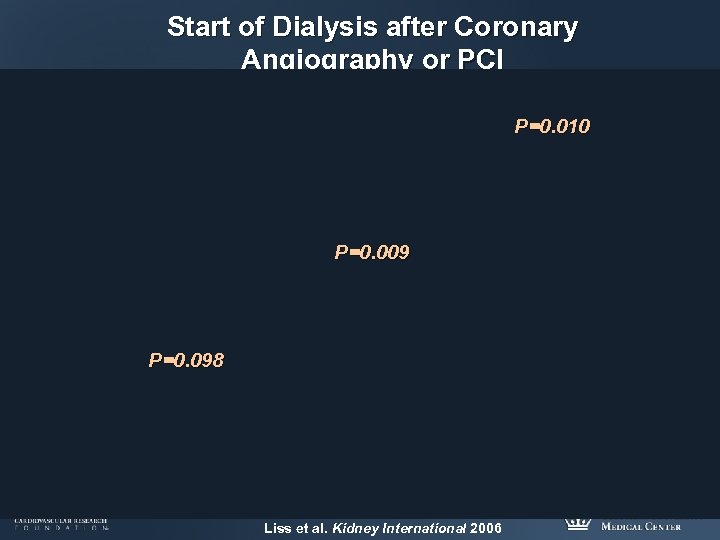 Start of Dialysis after Coronary Angiography or PCI P=0. 010 P=0. 009 P=0. 098 Liss et al. Kidney International 2006
Start of Dialysis after Coronary Angiography or PCI P=0. 010 P=0. 009 P=0. 098 Liss et al. Kidney International 2006
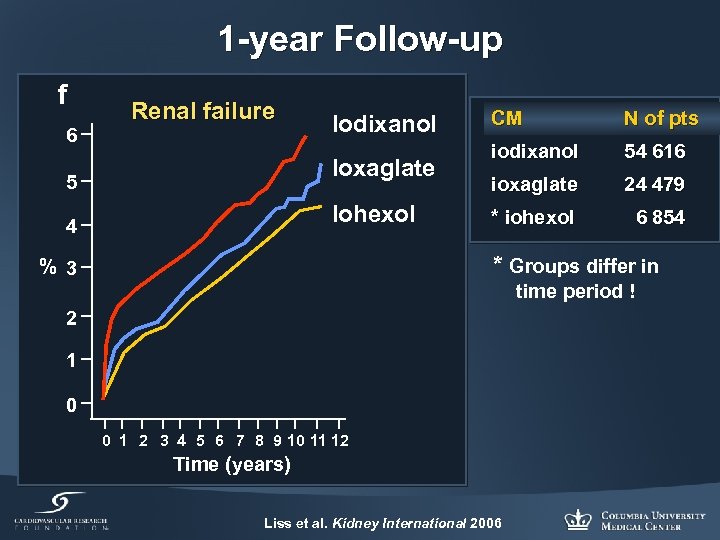 1 -year Follow-up f 6 Renal failure Iodixanol Ioxaglate 5 Iohexol 4 CM N of pts iodixanol 54 616 ioxaglate 24 479 * iohexol 6 854 * Groups differ in % 3 time period ! 2 1 0 0 1 2 3 4 5 6 7 8 9 10 11 12 Time (years) Liss et al. Kidney International 2006
1 -year Follow-up f 6 Renal failure Iodixanol Ioxaglate 5 Iohexol 4 CM N of pts iodixanol 54 616 ioxaglate 24 479 * iohexol 6 854 * Groups differ in % 3 time period ! 2 1 0 0 1 2 3 4 5 6 7 8 9 10 11 12 Time (years) Liss et al. Kidney International 2006
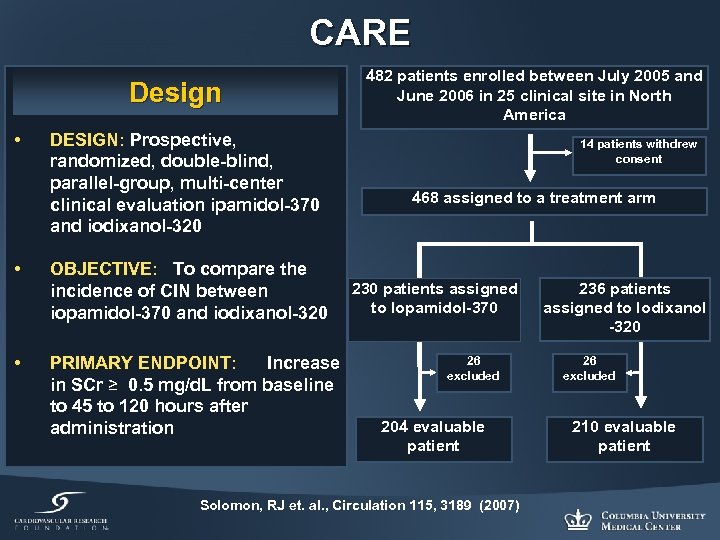 CARE Design • DESIGN: Prospective, randomized, double-blind, parallel-group, multi-center clinical evaluation ipamidol-370 and iodixanol-320 • OBJECTIVE: To compare the incidence of CIN between iopamidol-370 and iodixanol-320 • PRIMARY ENDPOINT: Increase in SCr ≥ 0. 5 mg/d. L from baseline to 45 to 120 hours after administration 482 patients enrolled between July 2005 and June 2006 in 25 clinical site in North America 14 patients withdrew consent 468 assigned to a treatment arm 230 patients assigned to Iopamidol-370 26 excluded 204 evaluable patient Solomon, RJ et. al. , Circulation 115, 3189 (2007) 236 patients assigned to Iodixanol -320 26 excluded 210 evaluable patient
CARE Design • DESIGN: Prospective, randomized, double-blind, parallel-group, multi-center clinical evaluation ipamidol-370 and iodixanol-320 • OBJECTIVE: To compare the incidence of CIN between iopamidol-370 and iodixanol-320 • PRIMARY ENDPOINT: Increase in SCr ≥ 0. 5 mg/d. L from baseline to 45 to 120 hours after administration 482 patients enrolled between July 2005 and June 2006 in 25 clinical site in North America 14 patients withdrew consent 468 assigned to a treatment arm 230 patients assigned to Iopamidol-370 26 excluded 204 evaluable patient Solomon, RJ et. al. , Circulation 115, 3189 (2007) 236 patients assigned to Iodixanol -320 26 excluded 210 evaluable patient
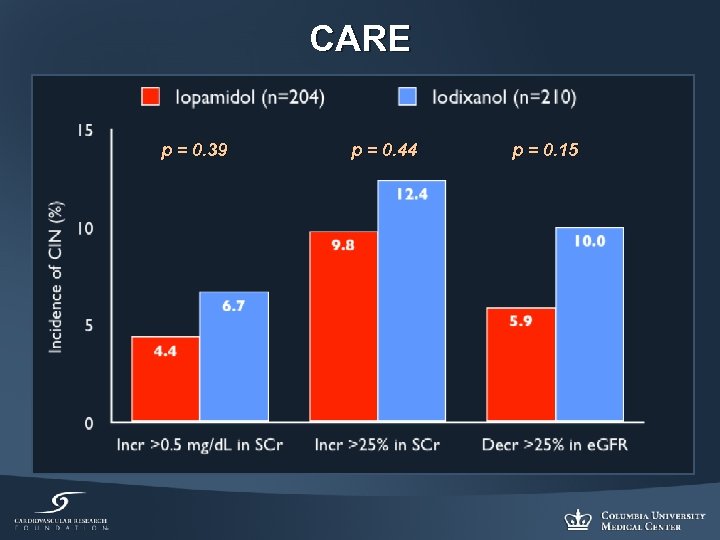 CARE p = 0. 39 p = 0. 44 p = 0. 15
CARE p = 0. 39 p = 0. 44 p = 0. 15
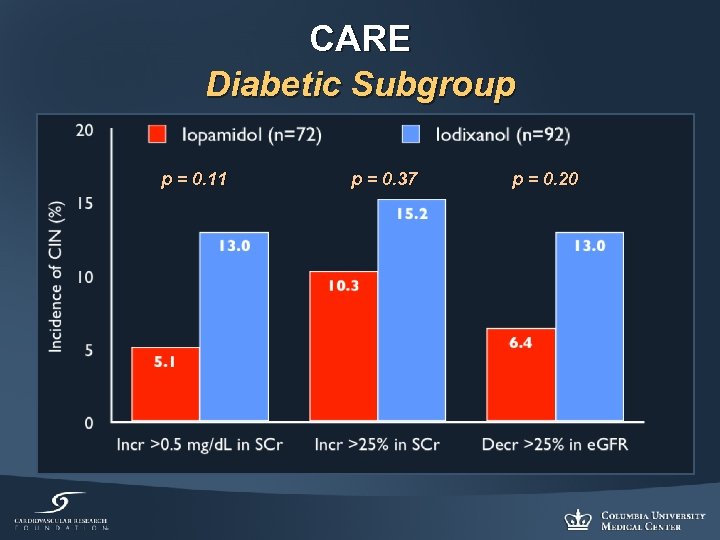 CARE Diabetic Subgroup p = 0. 11 p = 0. 37 p = 0. 20
CARE Diabetic Subgroup p = 0. 11 p = 0. 37 p = 0. 20
 Conclusions (1) • CRI is one of the most important independent predictors of poor outcome post PCI • CIN remains a frequent source of acute renal failure and is associated with increased morbidity and mortality, and higher resource utilization • Several factors predispose patients to CIN • Preventive measures pre procedure, as well as careful post procedure management should be routine in all patients
Conclusions (1) • CRI is one of the most important independent predictors of poor outcome post PCI • CIN remains a frequent source of acute renal failure and is associated with increased morbidity and mortality, and higher resource utilization • Several factors predispose patients to CIN • Preventive measures pre procedure, as well as careful post procedure management should be routine in all patients
 Conclusions (2) • • • Hydration pre-PCI (12 hours recommended) D/C nephrotoxic drugs (NSAIDS, antibiotics, etc) Role of n-acetylcysteine is disputable No Role for IV Fenoldopam Sodium bicarbonate may be useful, but need more definitive data • Limit contrast agent volume • Low-osmolar agents are better than high-osmolar ¡ Within non-ionic contrast, the data are contradictory • Role of local drug delivery for prevention of CIN requires further investigation • Role of Cooling Therapy is being examined: COOL CIN Study
Conclusions (2) • • • Hydration pre-PCI (12 hours recommended) D/C nephrotoxic drugs (NSAIDS, antibiotics, etc) Role of n-acetylcysteine is disputable No Role for IV Fenoldopam Sodium bicarbonate may be useful, but need more definitive data • Limit contrast agent volume • Low-osmolar agents are better than high-osmolar ¡ Within non-ionic contrast, the data are contradictory • Role of local drug delivery for prevention of CIN requires further investigation • Role of Cooling Therapy is being examined: COOL CIN Study


