aec85e2019b84f946893bbf056d711f1.ppt
- Количество слайдов: 96
 Contraception for Women and Couples with HIV
Contraception for Women and Couples with HIV
 Introduction 1. HIV/AIDS epidemic disproportionately affects women 2. Role of family planning in alleviating the burden of HIV 3. Reproductive choices and decisions for clients with HIV 4. ARV therapy basics in the context of family planning 5. Ensuring that services meet the needs of clients with HIV 6. Contraceptive options for women and couples with HIV 7. Family planning counselling for clients with HIV
Introduction 1. HIV/AIDS epidemic disproportionately affects women 2. Role of family planning in alleviating the burden of HIV 3. Reproductive choices and decisions for clients with HIV 4. ARV therapy basics in the context of family planning 5. Ensuring that services meet the needs of clients with HIV 6. Contraceptive options for women and couples with HIV 7. Family planning counselling for clients with HIV
 HIV/AIDS Epidemic Disproportionately Affects Women
HIV/AIDS Epidemic Disproportionately Affects Women
 Burden on Women • In sub-Saharan Africa, women make up 61% of HIV cases. • Proportion of women with HIV is increasing in other regions. Source: UNAIDS and WHO, 2007.
Burden on Women • In sub-Saharan Africa, women make up 61% of HIV cases. • Proportion of women with HIV is increasing in other regions. Source: UNAIDS and WHO, 2007.
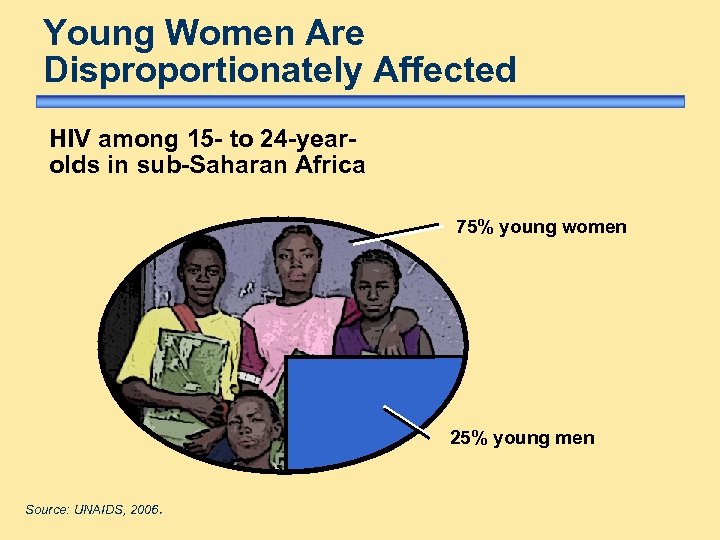 Young Women Are Disproportionately Affected HIV among 15 - to 24 -yearolds in sub-Saharan Africa 75% young women 25% young men Source: UNAIDS, 2006.
Young Women Are Disproportionately Affected HIV among 15 - to 24 -yearolds in sub-Saharan Africa 75% young women 25% young men Source: UNAIDS, 2006.
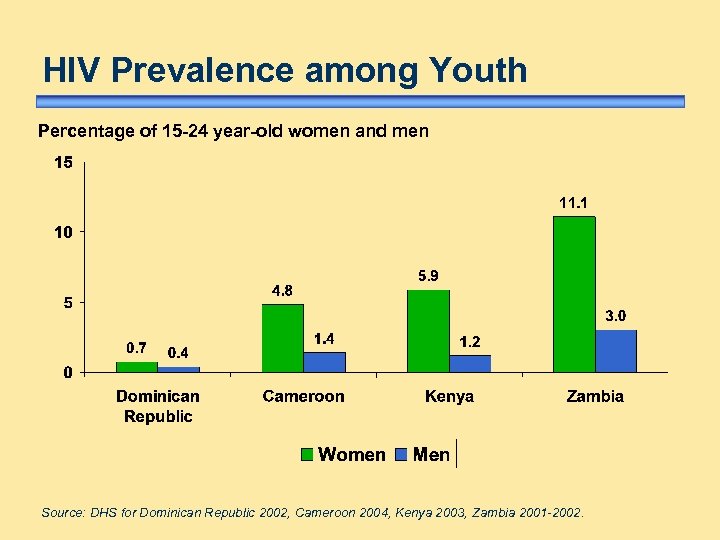 HIV Prevalence among Youth Percentage of 15 -24 year-old women and men Source: DHS for Dominican Republic 2002, Cameroon 2004, Kenya 2003, Zambia 2001 -2002.
HIV Prevalence among Youth Percentage of 15 -24 year-old women and men Source: DHS for Dominican Republic 2002, Cameroon 2004, Kenya 2003, Zambia 2001 -2002.
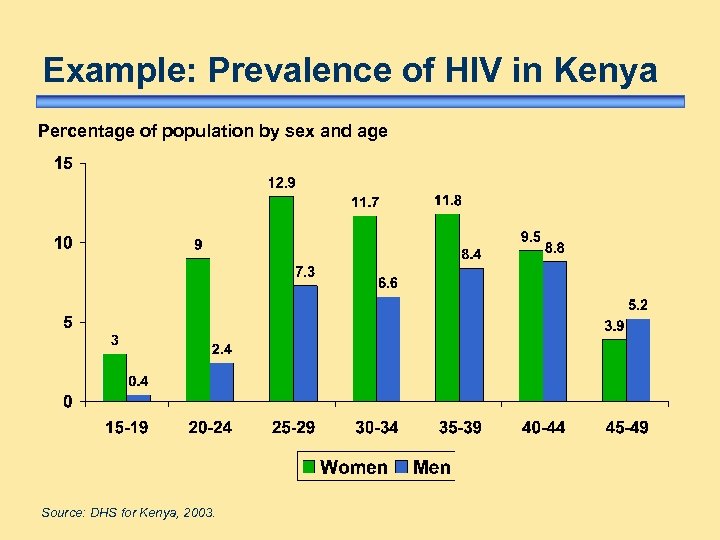 Example: Prevalence of HIV in Kenya Percentage of population by sex and age Source: DHS for Kenya, 2003.
Example: Prevalence of HIV in Kenya Percentage of population by sex and age Source: DHS for Kenya, 2003.
 Pregnant Women Share Burden In many countries of southern Africa, one in three pregnant women are living with HIV. Source: UNAIDS, 2006; UNAIDS, 2006.
Pregnant Women Share Burden In many countries of southern Africa, one in three pregnant women are living with HIV. Source: UNAIDS, 2006; UNAIDS, 2006.
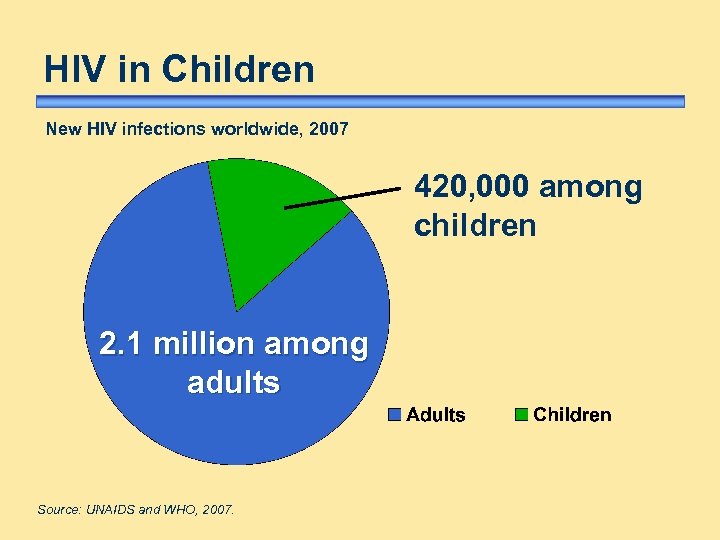 HIV in Children New HIV infections worldwide, 2007 420, 000 among children 2. 1 million among adults Source: UNAIDS and WHO, 2007.
HIV in Children New HIV infections worldwide, 2007 420, 000 among children 2. 1 million among adults Source: UNAIDS and WHO, 2007.
 Children Orphaned by AIDS Consequences: • psychosocial impact • health risks • nutritional deficiencies • economic deprivation • increase in HIV infection risk
Children Orphaned by AIDS Consequences: • psychosocial impact • health risks • nutritional deficiencies • economic deprivation • increase in HIV infection risk
 Why Are Women Vulnerable? Cultural and societal factors • • gender inequities limited opportunities economic dependence on men imbalance in sexual relationships Possible biological factors • large vaginal surface allows more exposure • cervical ectopy may facilitate acquisition Source: UNAIDS, 2006; Moss, 1991.
Why Are Women Vulnerable? Cultural and societal factors • • gender inequities limited opportunities economic dependence on men imbalance in sexual relationships Possible biological factors • large vaginal surface allows more exposure • cervical ectopy may facilitate acquisition Source: UNAIDS, 2006; Moss, 1991.
 Role of Family Planning in Alleviating the Burden of HIV
Role of Family Planning in Alleviating the Burden of HIV
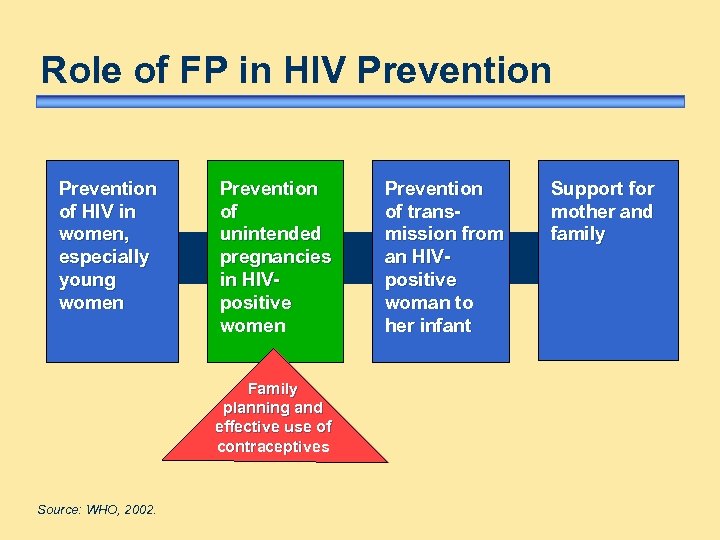 Role of FP in HIV Prevention of HIV in women, especially young women Prevention of unintended pregnancies in HIVpositive women Family planning and effective use of contraceptives Source: WHO, 2002. Prevention of transmission from an HIVpositive woman to her infant Support for mother and family
Role of FP in HIV Prevention of HIV in women, especially young women Prevention of unintended pregnancies in HIVpositive women Family planning and effective use of contraceptives Source: WHO, 2002. Prevention of transmission from an HIVpositive woman to her infant Support for mother and family
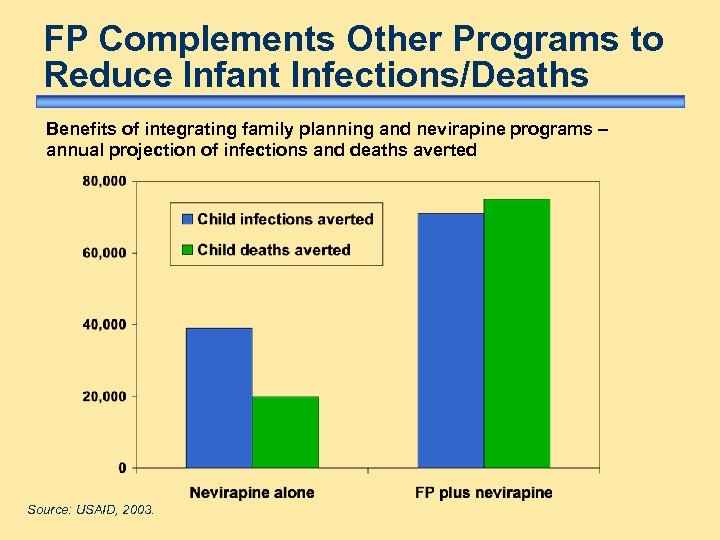 FP Complements Other Programs to Reduce Infant Infections/Deaths Benefits of integrating family planning and nevirapine programs – annual projection of infections and deaths averted Source: USAID, 2003.
FP Complements Other Programs to Reduce Infant Infections/Deaths Benefits of integrating family planning and nevirapine programs – annual projection of infections and deaths averted Source: USAID, 2003.
 Benefits of Providing FP Services For women and couples with HIV: • improves health/well-being of families and communities – spacing/limiting births • prevents unintended pregnancies, thus reducing: – number of infants born HIV-positive – number of future orphans
Benefits of Providing FP Services For women and couples with HIV: • improves health/well-being of families and communities – spacing/limiting births • prevents unintended pregnancies, thus reducing: – number of infants born HIV-positive – number of future orphans
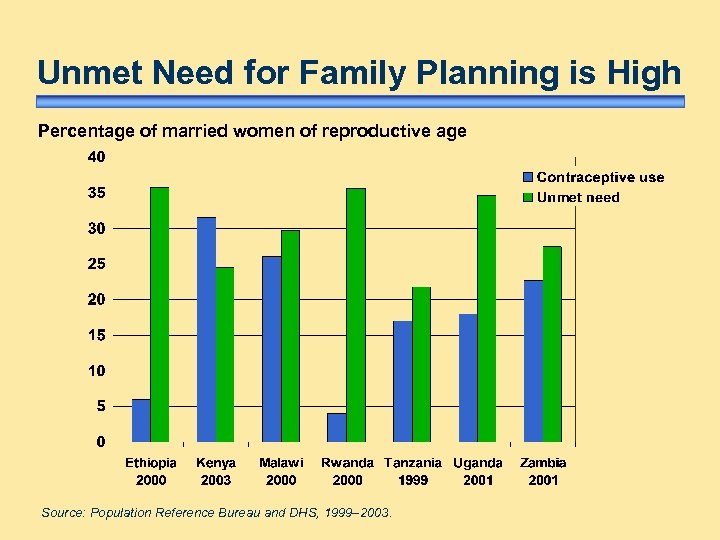 Unmet Need for Family Planning is High Percentage of married women of reproductive age Source: Population Reference Bureau and DHS, 1999– 2003.
Unmet Need for Family Planning is High Percentage of married women of reproductive age Source: Population Reference Bureau and DHS, 1999– 2003.
 Unmet RH Needs of Young Women Evidence: • high STI/HIV rates • unintended pregnancy • mortality/morbidity from unsafe abortion Causes include lack of: • information/education/communication skills • access to adolescent-friendly RH services Source: Ross, 2002.
Unmet RH Needs of Young Women Evidence: • high STI/HIV rates • unintended pregnancy • mortality/morbidity from unsafe abortion Causes include lack of: • information/education/communication skills • access to adolescent-friendly RH services Source: Ross, 2002.
 Reproductive Choices and Decisions for Clients with HIV chi ldb ear ing y anc n reg p contraception
Reproductive Choices and Decisions for Clients with HIV chi ldb ear ing y anc n reg p contraception
 Pregnancy in Women with HIV • Does not accelerate disease • One-third pass HIV to newborn during pregnancy, delivery, and breastfeeding • Possible increased risk of stillbirth and low birth weight Positive developments: • ARV therapy improves health/longevity • PMTCT reduces vertical transmission • Wider availability of support and care services Source: Saada, 2000; Tai, 2007; Brocklehurst, 1998.
Pregnancy in Women with HIV • Does not accelerate disease • One-third pass HIV to newborn during pregnancy, delivery, and breastfeeding • Possible increased risk of stillbirth and low birth weight Positive developments: • ARV therapy improves health/longevity • PMTCT reduces vertical transmission • Wider availability of support and care services Source: Saada, 2000; Tai, 2007; Brocklehurst, 1998.
 Clients with HIV: Reasons to Consider Pregnancy • • Intense desire to have children Pressure to have children Fear that older children may die Concern about infertility Reassured by PMTCT Optimism about ARV Avoid generating suspicions Apprehension about disclosing status Source: Preble, 2003.
Clients with HIV: Reasons to Consider Pregnancy • • Intense desire to have children Pressure to have children Fear that older children may die Concern about infertility Reassured by PMTCT Optimism about ARV Avoid generating suspicions Apprehension about disclosing status Source: Preble, 2003.
 Clients with HIV: Reasons to Avoid Childbearing • Similar concerns to women without HIV: – economic status – desired family size – ideal spacing • Concerns about health and quality of life • Fear of transmitting HIV • Anxiety about leaving orphans • Concerns about limited access to help
Clients with HIV: Reasons to Avoid Childbearing • Similar concerns to women without HIV: – economic status – desired family size – ideal spacing • Concerns about health and quality of life • Fear of transmitting HIV • Anxiety about leaving orphans • Concerns about limited access to help
 Access to Information/Services is Key • Consider reproductive choices • Plan for the future • Avoid unintended pregnancy • Reduce HIV transmission to children • Reduce transmission to partners
Access to Information/Services is Key • Consider reproductive choices • Plan for the future • Avoid unintended pregnancy • Reduce HIV transmission to children • Reduce transmission to partners
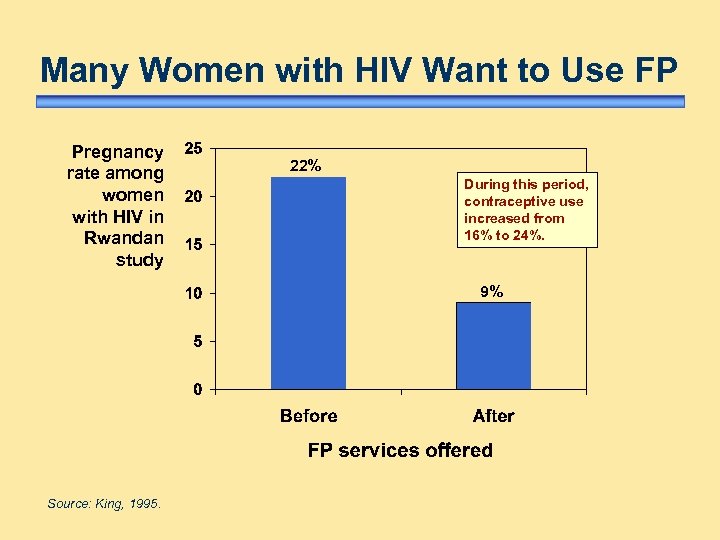 Many Women with HIV Want to Use FP Pregnancy rate among women with HIV in Rwandan study 22% During this period, contraceptive use increased from 16% to 24%. 9% Source: King, 1995.
Many Women with HIV Want to Use FP Pregnancy rate among women with HIV in Rwandan study 22% During this period, contraceptive use increased from 16% to 24%. 9% Source: King, 1995.
 ARV Therapy Basics in the Context of Family Planning
ARV Therapy Basics in the Context of Family Planning
 ARV Therapy Overview • Inhibits replication of the virus • Slows disease progression; improves quality of life • Different drugs attack virus at different stages of replication • Combine three drugs into HAART “cocktail” for best results decrease viral load improve immune function
ARV Therapy Overview • Inhibits replication of the virus • Slows disease progression; improves quality of life • Different drugs attack virus at different stages of replication • Combine three drugs into HAART “cocktail” for best results decrease viral load improve immune function
 Classes of ARV Drugs • NRTIs – Nucleoside reverse transcriptase inhibitors • Nt. RTIs – Nucleotide reverse transcriptase inhibitors • NNRTIs – Non-nucleoside reverse transcriptase inhibitors • PIs – Protease inhibitors • Entry inhibitors (other new classes under development)
Classes of ARV Drugs • NRTIs – Nucleoside reverse transcriptase inhibitors • Nt. RTIs – Nucleotide reverse transcriptase inhibitors • NNRTIs – Non-nucleoside reverse transcriptase inhibitors • PIs – Protease inhibitors • Entry inhibitors (other new classes under development)
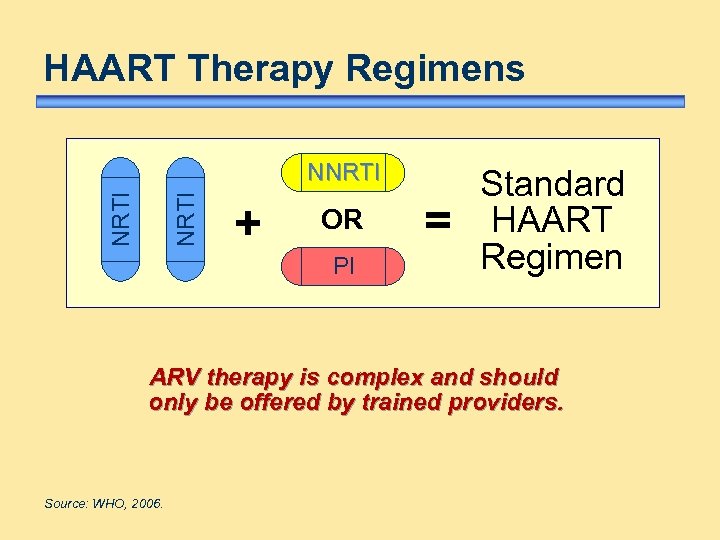 HAART Therapy Regimens NRTI NNRTI + OR PI = Standard HAART Regimen ARV therapy is complex and should only be offered by trained providers. Source: WHO, 2006.
HAART Therapy Regimens NRTI NNRTI + OR PI = Standard HAART Regimen ARV therapy is complex and should only be offered by trained providers. Source: WHO, 2006.
 Use of ARV Drugs for HIV Prophylaxis • Prevent mother-to-child transmission (PMTCT) – drug regimen depends on availability, cost, resistance, possible side effects – reduces vertical transmission by 34% to 50% • Postexposure prophylaxis (PEP) – start as soon as possible; continue 4 weeks – multidrug therapy is more effective • Other uses under study Source: Dabis, 2000; CDC, 2005.
Use of ARV Drugs for HIV Prophylaxis • Prevent mother-to-child transmission (PMTCT) – drug regimen depends on availability, cost, resistance, possible side effects – reduces vertical transmission by 34% to 50% • Postexposure prophylaxis (PEP) – start as soon as possible; continue 4 weeks – multidrug therapy is more effective • Other uses under study Source: Dabis, 2000; CDC, 2005.
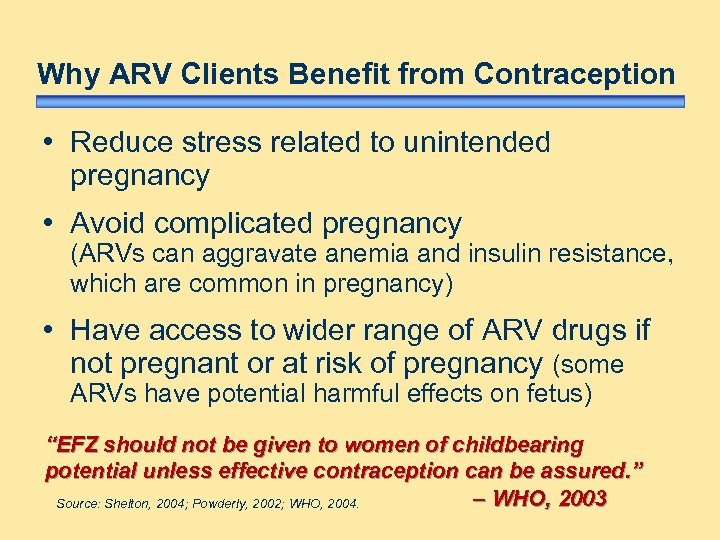 Why ARV Clients Benefit from Contraception • Reduce stress related to unintended pregnancy • Avoid complicated pregnancy (ARVs can aggravate anemia and insulin resistance, which are common in pregnancy) • Have access to wider range of ARV drugs if not pregnant or at risk of pregnancy (some ARVs have potential harmful effects on fetus) “EFZ should not be given to women of childbearing potential unless effective contraception can be assured. ” – WHO, 2003 Source: Shelton, 2004; Powderly, 2002; WHO, 2004.
Why ARV Clients Benefit from Contraception • Reduce stress related to unintended pregnancy • Avoid complicated pregnancy (ARVs can aggravate anemia and insulin resistance, which are common in pregnancy) • Have access to wider range of ARV drugs if not pregnant or at risk of pregnancy (some ARVs have potential harmful effects on fetus) “EFZ should not be given to women of childbearing potential unless effective contraception can be assured. ” – WHO, 2003 Source: Shelton, 2004; Powderly, 2002; WHO, 2004.
 Ensuring That Services Meet the Needs of Clients with HIV
Ensuring That Services Meet the Needs of Clients with HIV
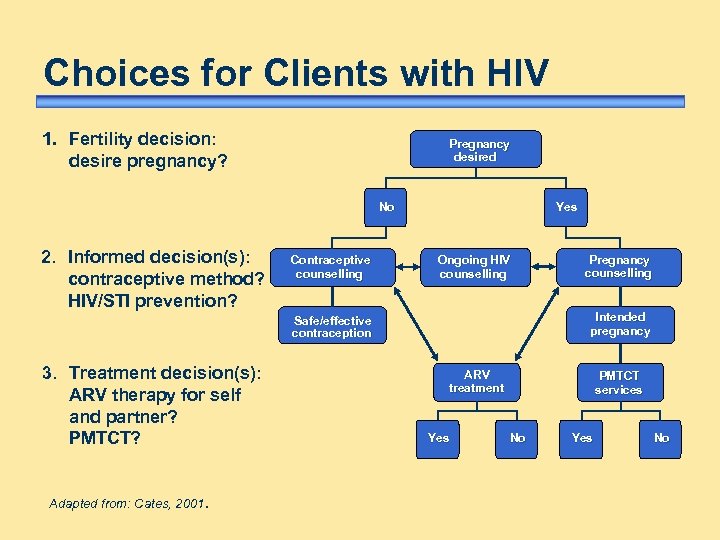 Choices for Clients with HIV 1. Fertility decision: desire pregnancy? Pregnancy desired No 2. Informed decision(s): contraceptive method? HIV/STI prevention? Contraceptive counselling Yes Ongoing HIV counselling Intended pregnancy Safe/effective contraception 3. Treatment decision(s): ARV therapy for self and partner? PMTCT? Adapted from: Cates, 2001. Pregnancy counselling ARV treatment Yes PMTCT services No Yes No
Choices for Clients with HIV 1. Fertility decision: desire pregnancy? Pregnancy desired No 2. Informed decision(s): contraceptive method? HIV/STI prevention? Contraceptive counselling Yes Ongoing HIV counselling Intended pregnancy Safe/effective contraception 3. Treatment decision(s): ARV therapy for self and partner? PMTCT? Adapted from: Cates, 2001. Pregnancy counselling ARV treatment Yes PMTCT services No Yes No
 Clients’ Family Planning Rights All individuals and couples have the right to: • access information and services • a variety of methods from which to choose • make an informed, voluntary choice of contraceptive method • receive their method of choice Clients should be supported in exercising their reproductive rights, regardless of their HIV status.
Clients’ Family Planning Rights All individuals and couples have the right to: • access information and services • a variety of methods from which to choose • make an informed, voluntary choice of contraceptive method • receive their method of choice Clients should be supported in exercising their reproductive rights, regardless of their HIV status.
 Ensuring Informed Choice Effective counsellors: • listen carefully • empathize with client • help clients make their own decisions • are not influenced by personal biases • provide accurate information
Ensuring Informed Choice Effective counsellors: • listen carefully • empathize with client • help clients make their own decisions • are not influenced by personal biases • provide accurate information
 Why Integrate HIV and FP Services Clients seeking HIV-related services AND Clients seeking FP services Share common needs and concerns: • are often sexually active and fertile • are at risk of HIV infection or might be HIV-positive • need to know their HIV status • need access to contraceptives
Why Integrate HIV and FP Services Clients seeking HIV-related services AND Clients seeking FP services Share common needs and concerns: • are often sexually active and fertile • are at risk of HIV infection or might be HIV-positive • need to know their HIV status • need access to contraceptives
 Why Integrate HIV and FP Services continued. . . Creates programmatic synergies including: • more attractive to potential clients – increases access to wider range of services – helps overcome HIV stigma • opportunities for follow-up and support for drug or method adherence
Why Integrate HIV and FP Services continued. . . Creates programmatic synergies including: • more attractive to potential clients – increases access to wider range of services – helps overcome HIV stigma • opportunities for follow-up and support for drug or method adherence
 Benefits of Involving Men • Encourages partner counselling, testing, and disclosure • Helps women act on prevention messages • Helps couples make informed decisions on reproductive health goals and prevention strategies • Improves client satisfaction and adoption, continuation, and successful method use Integrated RH services can provide a valuable opportunity to involve men in a meaningful way.
Benefits of Involving Men • Encourages partner counselling, testing, and disclosure • Helps women act on prevention messages • Helps couples make informed decisions on reproductive health goals and prevention strategies • Improves client satisfaction and adoption, continuation, and successful method use Integrated RH services can provide a valuable opportunity to involve men in a meaningful way.
 Contraceptive Options for Women and Couples with HIV
Contraceptive Options for Women and Couples with HIV
 Factors Affecting Sexual and Reproductive Decisions • Health/well-being of self, partner, children • Access to ARV therapy • Fears related to disclosing HIV status (rejection, violence, financial loss) • Knowledge about contraceptives (including cultural myths and misconceptions) • Stigma regarding condom use • Gender issues/partner opposition
Factors Affecting Sexual and Reproductive Decisions • Health/well-being of self, partner, children • Access to ARV therapy • Fears related to disclosing HIV status (rejection, violence, financial loss) • Knowledge about contraceptives (including cultural myths and misconceptions) • Stigma regarding condom use • Gender issues/partner opposition
 Factors Affecting Method Choice Women with HIV may consider: • safety and effectiveness of the method • duration of protection desired • possible side effects • ease of use • cost and access to resupply • effect on breastfeeding (if postpartum)
Factors Affecting Method Choice Women with HIV may consider: • safety and effectiveness of the method • duration of protection desired • possible side effects • ease of use • cost and access to resupply • effect on breastfeeding (if postpartum)
 Factors Affecting Method Choice continued. . . • how it may interact with other medications, including ARVs • whether it provides protection from STI/HIV transmission and acquisition • whether partner involvement or negotiation are required
Factors Affecting Method Choice continued. . . • how it may interact with other medications, including ARVs • whether it provides protection from STI/HIV transmission and acquisition • whether partner involvement or negotiation are required
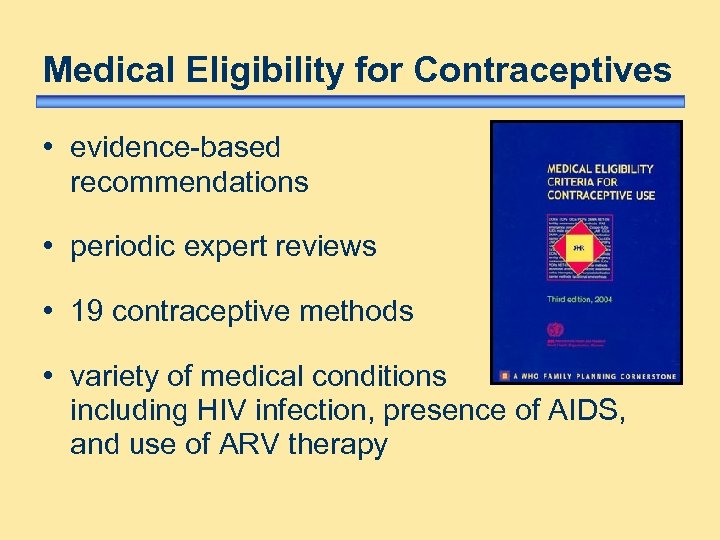 Medical Eligibility for Contraceptives • evidence-based recommendations • periodic expert reviews • 19 contraceptive methods • variety of medical conditions including HIV infection, presence of AIDS, and use of ARV therapy
Medical Eligibility for Contraceptives • evidence-based recommendations • periodic expert reviews • 19 contraceptive methods • variety of medical conditions including HIV infection, presence of AIDS, and use of ARV therapy
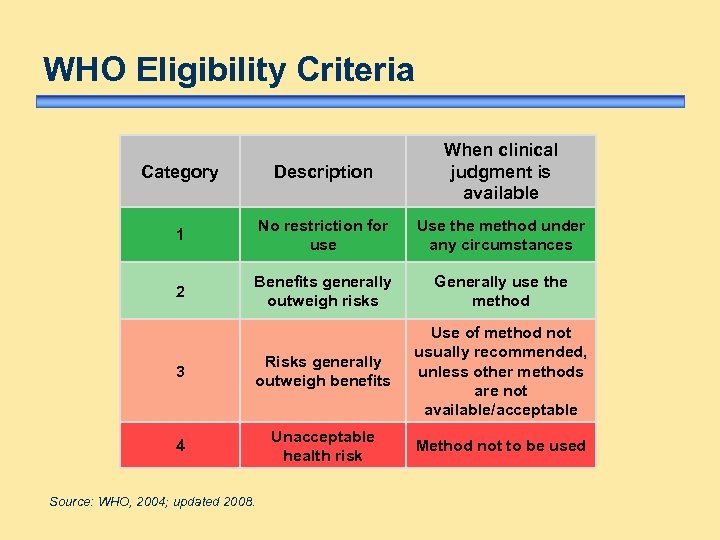 WHO Eligibility Criteria Category Description When clinical judgment is available 1 No restriction for use Use the method under any circumstances 2 Benefits generally outweigh risks Generally use the method 3 Risks generally outweigh benefits Use of method not usually recommended, unless other methods are not available/acceptable 4 Unacceptable health risk Method not to be used Source: WHO, 2004; updated 2008.
WHO Eligibility Criteria Category Description When clinical judgment is available 1 No restriction for use Use the method under any circumstances 2 Benefits generally outweigh risks Generally use the method 3 Risks generally outweigh benefits Use of method not usually recommended, unless other methods are not available/acceptable 4 Unacceptable health risk Method not to be used Source: WHO, 2004; updated 2008.
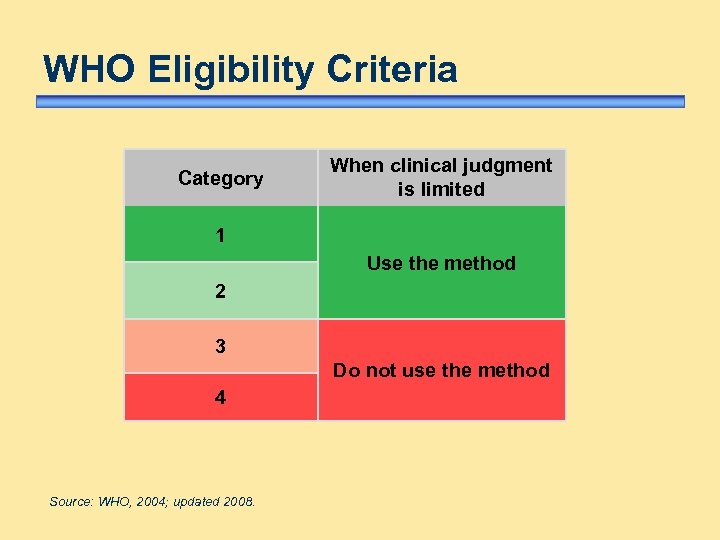 WHO Eligibility Criteria Category When clinical judgment is limited 1 Use the method 2 3 Do not use the method 4 Source: WHO, 2004; updated 2008.
WHO Eligibility Criteria Category When clinical judgment is limited 1 Use the method 2 3 Do not use the method 4 Source: WHO, 2004; updated 2008.
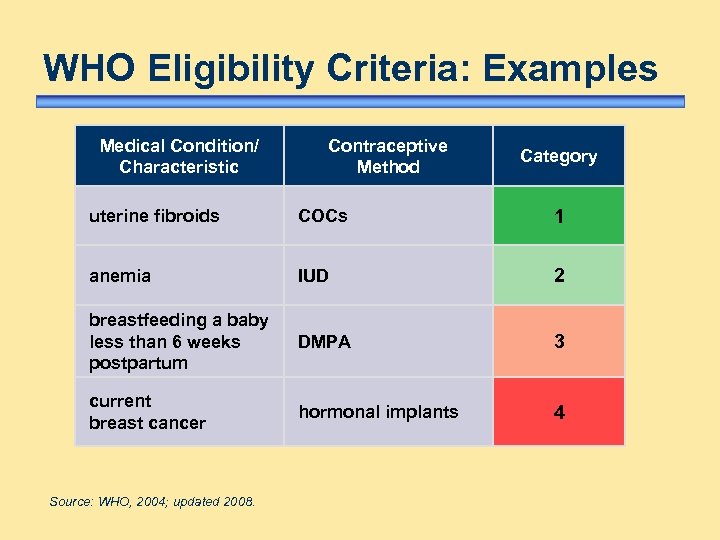 WHO Eligibility Criteria: Examples Medical Condition/ Characteristic Contraceptive Method Category uterine fibroids COCs 1 anemia IUD 2 breastfeeding a baby less than 6 weeks postpartum DMPA 3 current breast cancer hormonal implants 4 Source: WHO, 2004; updated 2008.
WHO Eligibility Criteria: Examples Medical Condition/ Characteristic Contraceptive Method Category uterine fibroids COCs 1 anemia IUD 2 breastfeeding a baby less than 6 weeks postpartum DMPA 3 current breast cancer hormonal implants 4 Source: WHO, 2004; updated 2008.
 Contraceptive Method Options • • barrier methods oral contraceptive pills injectables implants intrauterine device (IUD) female and male sterilization lactational amenorrhoea method (LAM) fertility awareness-based methods Couples with HIV have a wide range of methods from which to choose.
Contraceptive Method Options • • barrier methods oral contraceptive pills injectables implants intrauterine device (IUD) female and male sterilization lactational amenorrhoea method (LAM) fertility awareness-based methods Couples with HIV have a wide range of methods from which to choose.
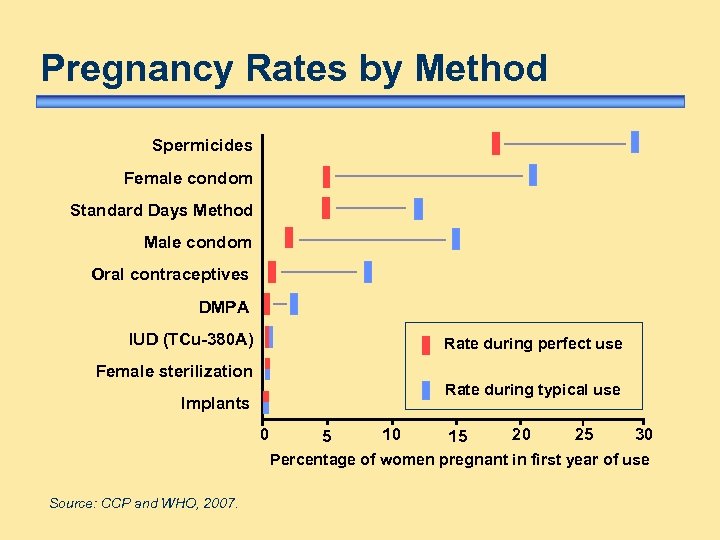 Pregnancy Rates by Method Spermicides Female condom Standard Days Method Male condom Oral contraceptives DMPA IUD (TCu-380 A) Rate during perfect use Female sterilization Rate during typical use Implants 0 5 10 15 20 25 30 Percentage of women pregnant in first year of use Source: CCP and WHO, 2007.
Pregnancy Rates by Method Spermicides Female condom Standard Days Method Male condom Oral contraceptives DMPA IUD (TCu-380 A) Rate during perfect use Female sterilization Rate during typical use Implants 0 5 10 15 20 25 30 Percentage of women pregnant in first year of use Source: CCP and WHO, 2007.
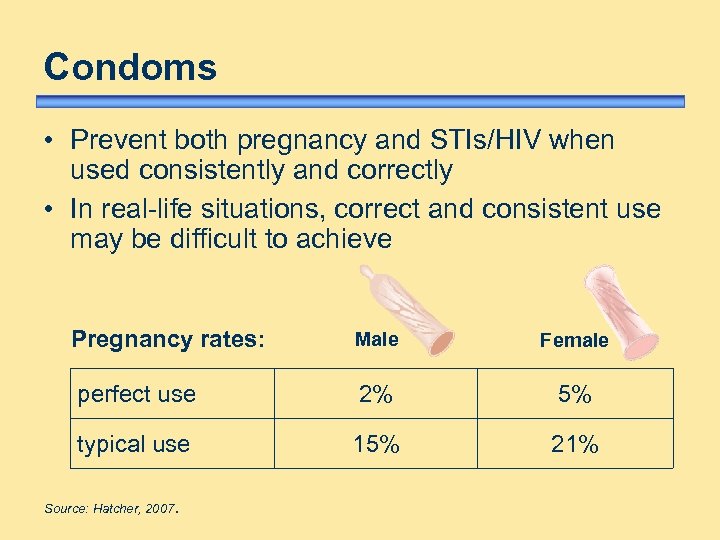 Condoms • Prevent both pregnancy and STIs/HIV when used consistently and correctly • In real-life situations, correct and consistent use may be difficult to achieve Pregnancy rates: Male Female perfect use 2% 5% typical use 15% 21% Source: Hatcher, 2007.
Condoms • Prevent both pregnancy and STIs/HIV when used consistently and correctly • In real-life situations, correct and consistent use may be difficult to achieve Pregnancy rates: Male Female perfect use 2% 5% typical use 15% 21% Source: Hatcher, 2007.
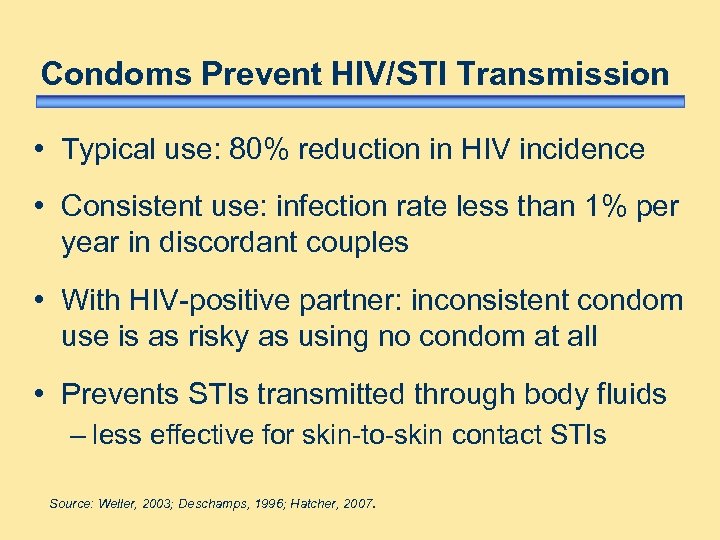 Condoms Prevent HIV/STI Transmission • Typical use: 80% reduction in HIV incidence • Consistent use: infection rate less than 1% per year in discordant couples • With HIV-positive partner: inconsistent condom use is as risky as using no condom at all • Prevents STIs transmitted through body fluids – less effective for skin-to-skin contact STIs Source: Weller, 2003; Deschamps, 1996; Hatcher, 2007.
Condoms Prevent HIV/STI Transmission • Typical use: 80% reduction in HIV incidence • Consistent use: infection rate less than 1% per year in discordant couples • With HIV-positive partner: inconsistent condom use is as risky as using no condom at all • Prevents STIs transmitted through body fluids – less effective for skin-to-skin contact STIs Source: Weller, 2003; Deschamps, 1996; Hatcher, 2007.
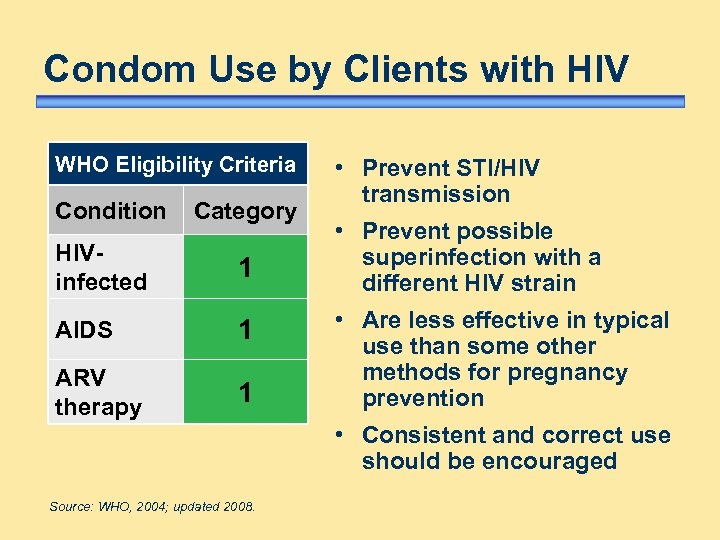 Condom Use by Clients with HIV WHO Eligibility Criteria Condition Category HIVinfected 1 AIDS 1 ARV therapy 1 • Prevent STI/HIV transmission • Prevent possible superinfection with a different HIV strain • Are less effective in typical use than some other methods for pregnancy prevention • Consistent and correct use should be encouraged Source: WHO, 2004; updated 2008.
Condom Use by Clients with HIV WHO Eligibility Criteria Condition Category HIVinfected 1 AIDS 1 ARV therapy 1 • Prevent STI/HIV transmission • Prevent possible superinfection with a different HIV strain • Are less effective in typical use than some other methods for pregnancy prevention • Consistent and correct use should be encouraged Source: WHO, 2004; updated 2008.
 Why Encourage Dual Method Use condoms to protect against STIs/HIV plus another method for increased protection against pregnancy. Reduces: • risk of unintended pregnancy • transmission of HIV between partners • risk of acquiring or transmitting other STIs Dual method use requires ongoing support and encouragement by providers.
Why Encourage Dual Method Use condoms to protect against STIs/HIV plus another method for increased protection against pregnancy. Reduces: • risk of unintended pregnancy • transmission of HIV between partners • risk of acquiring or transmitting other STIs Dual method use requires ongoing support and encouragement by providers.
 Counselling about Dual Method Users of other methods may be less likely to use condoms. Encourage clients to consider: • limitations of a single-method approach • their individual risk of pregnancy • whether partners have HIV or other STIs • the negative consequences that may result Source: Diaz, 1995.
Counselling about Dual Method Users of other methods may be less likely to use condoms. Encourage clients to consider: • limitations of a single-method approach • their individual risk of pregnancy • whether partners have HIV or other STIs • the negative consequences that may result Source: Diaz, 1995.
 Counselling about Dual Method Use continued. . . Teach clients: • to negotiate condom use • how to use condoms • importance of using condoms consistently and correctly with all partners Encourage dual method use for all clients with HIV who wish to protect themselves.
Counselling about Dual Method Use continued. . . Teach clients: • to negotiate condom use • how to use condoms • importance of using condoms consistently and correctly with all partners Encourage dual method use for all clients with HIV who wish to protect themselves.
 Hormonal Contraceptives • • Combined oral contraceptive pills (COCs) Progestin-only oral contraceptive pills (POPs) Injectables (Depo-Provera/DMPA) Implants (Norplant, Jadelle, Implanon)
Hormonal Contraceptives • • Combined oral contraceptive pills (COCs) Progestin-only oral contraceptive pills (POPs) Injectables (Depo-Provera/DMPA) Implants (Norplant, Jadelle, Implanon)
 Hormonal Methods: Appropriate for Women with HIV • Very effective • Easy to use • Suitable for short- or long-term use • Reversible • Non-contraceptive health benefits • Serious complications extremely rare
Hormonal Methods: Appropriate for Women with HIV • Very effective • Easy to use • Suitable for short- or long-term use • Reversible • Non-contraceptive health benefits • Serious complications extremely rare
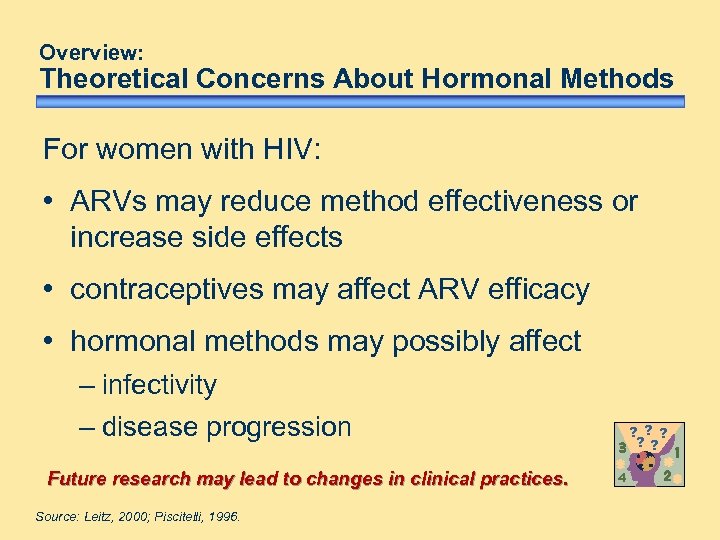 Overview: Theoretical Concerns About Hormonal Methods For women with HIV: • ARVs may reduce method effectiveness or increase side effects • contraceptives may affect ARV efficacy • hormonal methods may possibly affect – infectivity – disease progression Future research may lead to changes in clinical practices. Source: Leitz, 2000; Piscitelli, 1996. ? ? ? 4
Overview: Theoretical Concerns About Hormonal Methods For women with HIV: • ARVs may reduce method effectiveness or increase side effects • contraceptives may affect ARV efficacy • hormonal methods may possibly affect – infectivity – disease progression Future research may lead to changes in clinical practices. Source: Leitz, 2000; Piscitelli, 1996. ? ? ? 4
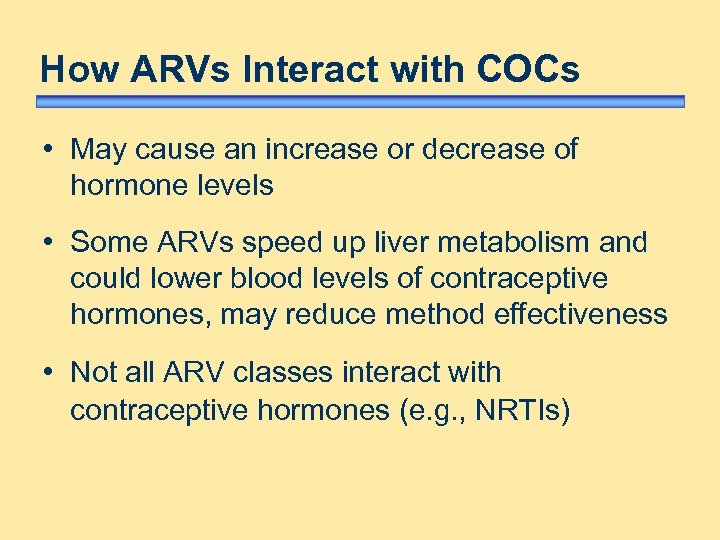 How ARVs Interact with COCs • May cause an increase or decrease of hormone levels • Some ARVs speed up liver metabolism and could lower blood levels of contraceptive hormones, may reduce method effectiveness • Not all ARV classes interact with contraceptive hormones (e. g. , NRTIs)
How ARVs Interact with COCs • May cause an increase or decrease of hormone levels • Some ARVs speed up liver metabolism and could lower blood levels of contraceptive hormones, may reduce method effectiveness • Not all ARV classes interact with contraceptive hormones (e. g. , NRTIs)
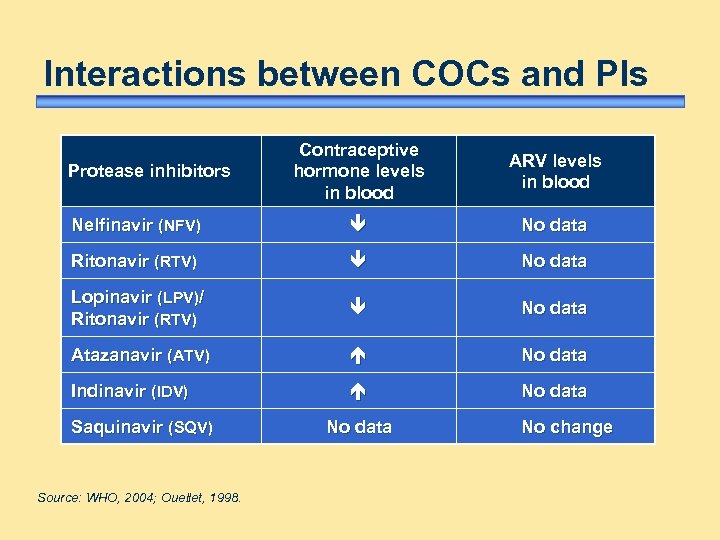 Interactions between COCs and PIs Contraceptive hormone levels in blood ARV levels in blood Nelfinavir (NFV) No data Ritonavir (RTV) No data Lopinavir (LPV)/ Ritonavir (RTV) No data Atazanavir (ATV) No data Indinavir (IDV) No data Protease inhibitors Saquinavir (SQV) Source: WHO, 2004; Ouellet, 1998. No data No change
Interactions between COCs and PIs Contraceptive hormone levels in blood ARV levels in blood Nelfinavir (NFV) No data Ritonavir (RTV) No data Lopinavir (LPV)/ Ritonavir (RTV) No data Atazanavir (ATV) No data Indinavir (IDV) No data Protease inhibitors Saquinavir (SQV) Source: WHO, 2004; Ouellet, 1998. No data No change
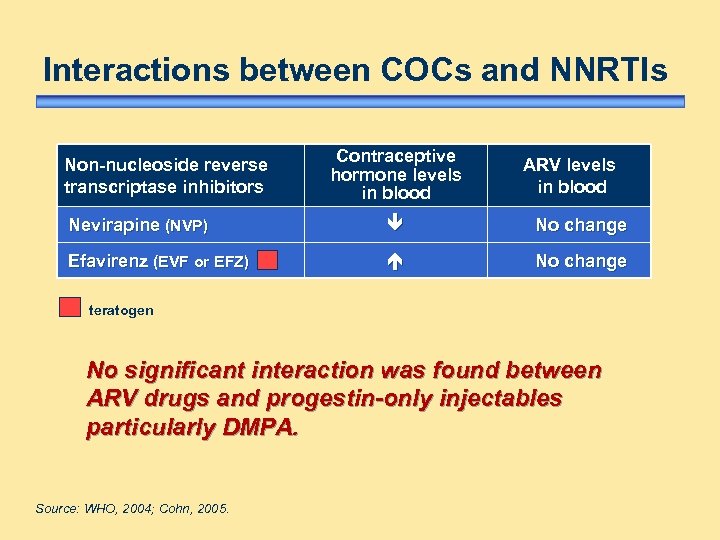 Interactions between COCs and NNRTIs Non-nucleoside reverse transcriptase inhibitors Contraceptive hormone levels in blood ARV levels in blood Nevirapine (NVP) No change Efavirenz (EVF or EFZ) No change teratogen No significant interaction was found between ARV drugs and progestin-only injectables particularly DMPA. Source: WHO, 2004; Cohn, 2005.
Interactions between COCs and NNRTIs Non-nucleoside reverse transcriptase inhibitors Contraceptive hormone levels in blood ARV levels in blood Nevirapine (NVP) No change Efavirenz (EVF or EFZ) No change teratogen No significant interaction was found between ARV drugs and progestin-only injectables particularly DMPA. Source: WHO, 2004; Cohn, 2005.
 Clinical Significance of COC/ARV Interaction Is Unknown • Studies examining clinical outcomes are needed (i. e. , pregnancy rates, ovulation indicators) • No data on interaction between ARVs and hormonal contraceptives other than COCs and DMPA • Ritonavir-boosted protease inhibitors reduce contraceptive hormone blood levels considerably – not generally recommended for women on oral contraceptives or combined injectables – not part of first-line ARV regimens ? ? ? 4
Clinical Significance of COC/ARV Interaction Is Unknown • Studies examining clinical outcomes are needed (i. e. , pregnancy rates, ovulation indicators) • No data on interaction between ARVs and hormonal contraceptives other than COCs and DMPA • Ritonavir-boosted protease inhibitors reduce contraceptive hormone blood levels considerably – not generally recommended for women on oral contraceptives or combined injectables – not part of first-line ARV regimens ? ? ? 4
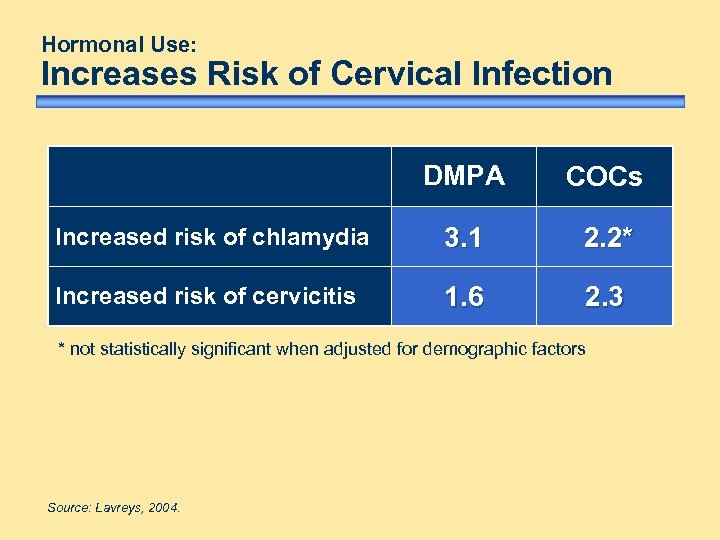 Hormonal Use: Increases Risk of Cervical Infection DMPA COCs Increased risk of chlamydia 3. 1 2. 2* Increased risk of cervicitis 1. 6 2. 3 * not statistically significant when adjusted for demographic factors Source: Lavreys, 2004.
Hormonal Use: Increases Risk of Cervical Infection DMPA COCs Increased risk of chlamydia 3. 1 2. 2* Increased risk of cervicitis 1. 6 2. 3 * not statistically significant when adjusted for demographic factors Source: Lavreys, 2004.
 Hormonal Use: May Increase HIV Shedding • HIV shedding may increase risk of HIV transmission to partner • In one study, modest increase in cervical shedding of HIV-infected cells but no free virus • Impact on infectivity is uncertain ? ? ? 4 Source: Wang, 1999; Wang, 2004; John, 2001.
Hormonal Use: May Increase HIV Shedding • HIV shedding may increase risk of HIV transmission to partner • In one study, modest increase in cervical shedding of HIV-infected cells but no free virus • Impact on infectivity is uncertain ? ? ? 4 Source: Wang, 1999; Wang, 2004; John, 2001.
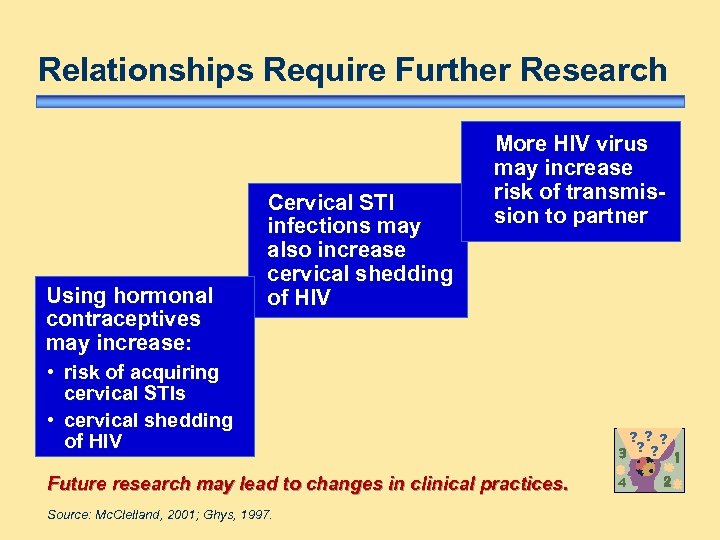 Relationships Require Further Research Using hormonal contraceptives may increase: Cervical STI infections may also increase cervical shedding of HIV More HIV virus may increase risk of transmission to partner • risk of acquiring cervical STIs • cervical shedding of HIV Future research may lead to changes in clinical practices. Source: Mc. Clelland, 2001; Ghys, 1997. ? ? ? 4
Relationships Require Further Research Using hormonal contraceptives may increase: Cervical STI infections may also increase cervical shedding of HIV More HIV virus may increase risk of transmission to partner • risk of acquiring cervical STIs • cervical shedding of HIV Future research may lead to changes in clinical practices. Source: Mc. Clelland, 2001; Ghys, 1997. ? ? ? 4
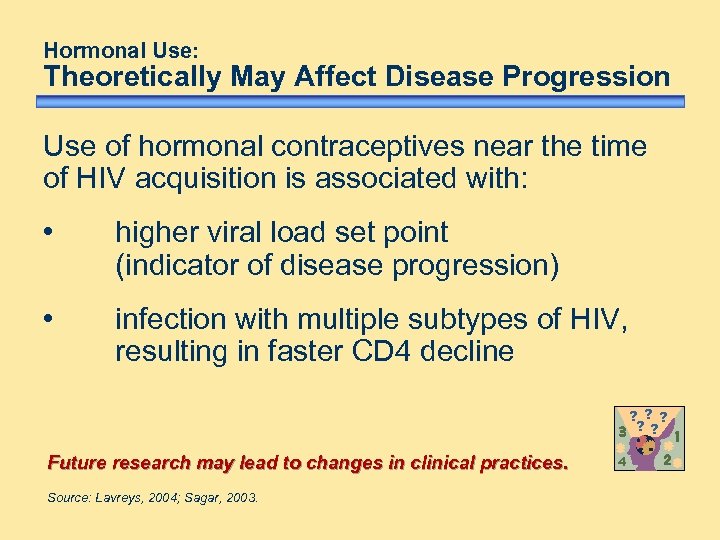 Hormonal Use: Theoretically May Affect Disease Progression Use of hormonal contraceptives near the time of HIV acquisition is associated with: • higher viral load set point (indicator of disease progression) • infection with multiple subtypes of HIV, resulting in faster CD 4 decline ? ? ? Future research may lead to changes in clinical practices. Source: Lavreys, 2004; Sagar, 2003. 4
Hormonal Use: Theoretically May Affect Disease Progression Use of hormonal contraceptives near the time of HIV acquisition is associated with: • higher viral load set point (indicator of disease progression) • infection with multiple subtypes of HIV, resulting in faster CD 4 decline ? ? ? Future research may lead to changes in clinical practices. Source: Lavreys, 2004; Sagar, 2003. 4
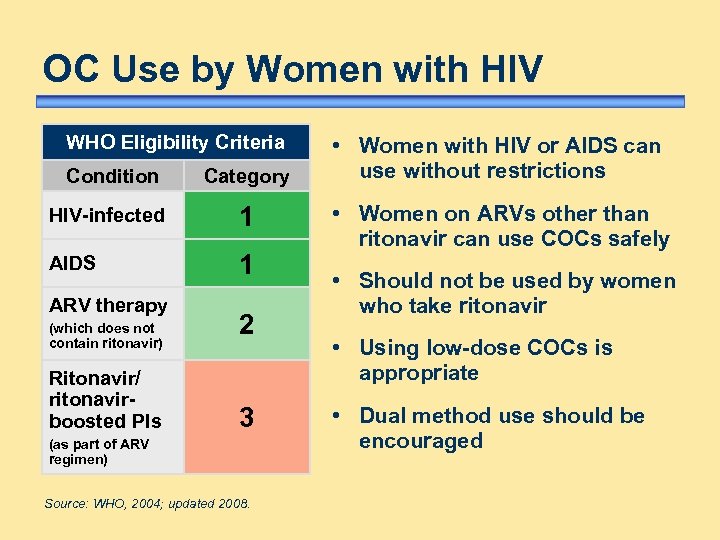 OC Use by Women with HIV WHO Eligibility Criteria Condition Category HIV-infected 1 AIDS 1 ARV therapy (which does not contain ritonavir) Ritonavir/ ritonavirboosted PIs 2 3 (as part of ARV regimen) Source: WHO, 2004; updated 2008. • Women with HIV or AIDS can use without restrictions • Women on ARVs other than ritonavir can use COCs safely • Should not be used by women who take ritonavir • Using low-dose COCs is appropriate • Dual method use should be encouraged
OC Use by Women with HIV WHO Eligibility Criteria Condition Category HIV-infected 1 AIDS 1 ARV therapy (which does not contain ritonavir) Ritonavir/ ritonavirboosted PIs 2 3 (as part of ARV regimen) Source: WHO, 2004; updated 2008. • Women with HIV or AIDS can use without restrictions • Women on ARVs other than ritonavir can use COCs safely • Should not be used by women who take ritonavir • Using low-dose COCs is appropriate • Dual method use should be encouraged
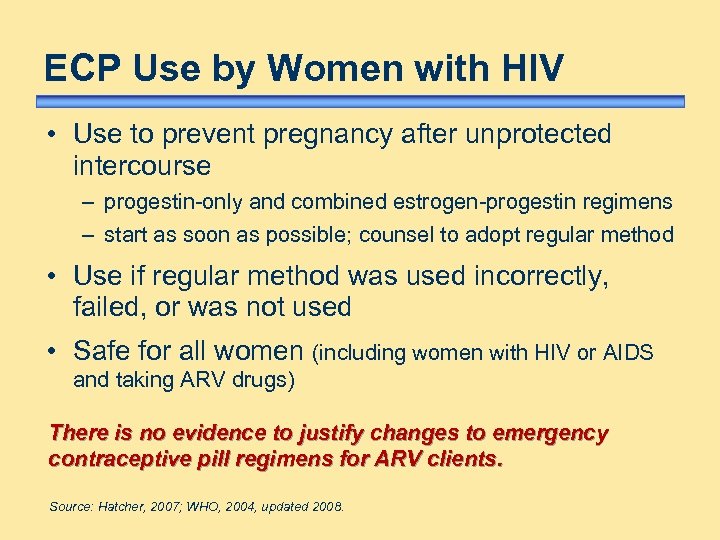 ECP Use by Women with HIV • Use to prevent pregnancy after unprotected intercourse – progestin-only and combined estrogen-progestin regimens – start as soon as possible; counsel to adopt regular method • Use if regular method was used incorrectly, failed, or was not used • Safe for all women (including women with HIV or AIDS and taking ARV drugs) There is no evidence to justify changes to emergency contraceptive pill regimens for ARV clients. Source: Hatcher, 2007; WHO, 2004, updated 2008.
ECP Use by Women with HIV • Use to prevent pregnancy after unprotected intercourse – progestin-only and combined estrogen-progestin regimens – start as soon as possible; counsel to adopt regular method • Use if regular method was used incorrectly, failed, or was not used • Safe for all women (including women with HIV or AIDS and taking ARV drugs) There is no evidence to justify changes to emergency contraceptive pill regimens for ARV clients. Source: Hatcher, 2007; WHO, 2004, updated 2008.
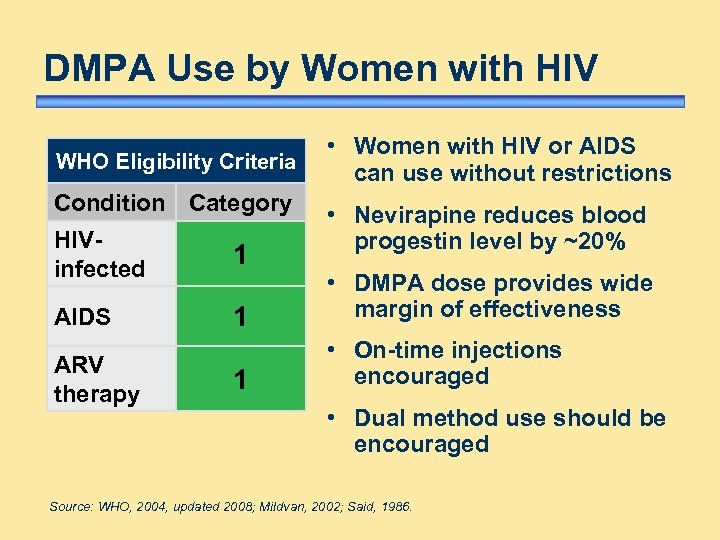 DMPA Use by Women with HIV WHO Eligibility Criteria Condition Category • Women with HIV or AIDS can use without restrictions • Nevirapine reduces blood progestin level by ~20% HIVinfected 1 AIDS 1 • DMPA dose provides wide margin of effectiveness 1 • On-time injections encouraged ARV therapy • Dual method use should be encouraged Source: WHO, 2004, updated 2008; Mildvan, 2002; Said, 1986.
DMPA Use by Women with HIV WHO Eligibility Criteria Condition Category • Women with HIV or AIDS can use without restrictions • Nevirapine reduces blood progestin level by ~20% HIVinfected 1 AIDS 1 • DMPA dose provides wide margin of effectiveness 1 • On-time injections encouraged ARV therapy • Dual method use should be encouraged Source: WHO, 2004, updated 2008; Mildvan, 2002; Said, 1986.
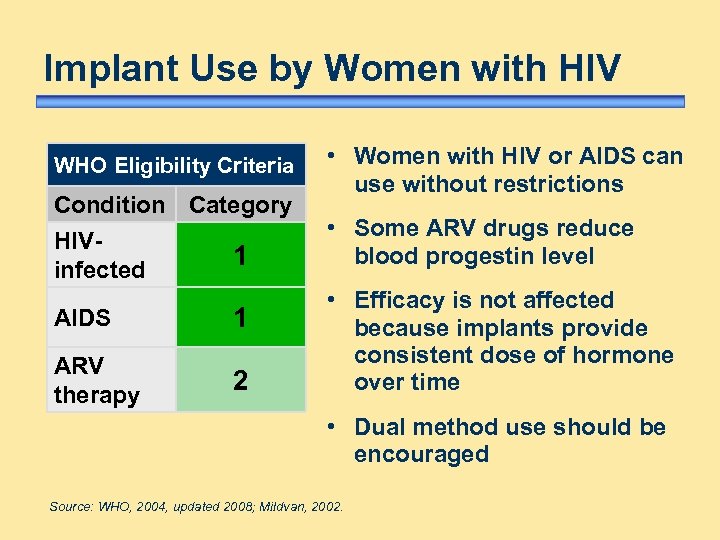 Implant Use by Women with HIV WHO Eligibility Criteria Condition Category HIV 1 infected AIDS 1 ARV therapy 2 • Women with HIV or AIDS can use without restrictions • Some ARV drugs reduce blood progestin level • Efficacy is not affected because implants provide consistent dose of hormone over time • Dual method use should be encouraged Source: WHO, 2004, updated 2008; Mildvan, 2002.
Implant Use by Women with HIV WHO Eligibility Criteria Condition Category HIV 1 infected AIDS 1 ARV therapy 2 • Women with HIV or AIDS can use without restrictions • Some ARV drugs reduce blood progestin level • Efficacy is not affected because implants provide consistent dose of hormone over time • Dual method use should be encouraged Source: WHO, 2004, updated 2008; Mildvan, 2002.
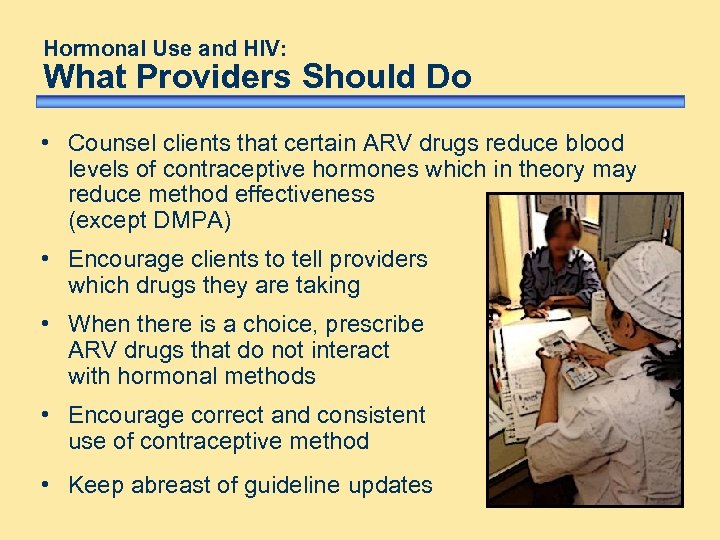 Hormonal Use and HIV: What Providers Should Do • Counsel clients that certain ARV drugs reduce blood levels of contraceptive hormones which in theory may reduce method effectiveness (except DMPA) • Encourage clients to tell providers which drugs they are taking • When there is a choice, prescribe ARV drugs that do not interact with hormonal methods • Encourage correct and consistent use of contraceptive method • Keep abreast of guideline updates
Hormonal Use and HIV: What Providers Should Do • Counsel clients that certain ARV drugs reduce blood levels of contraceptive hormones which in theory may reduce method effectiveness (except DMPA) • Encourage clients to tell providers which drugs they are taking • When there is a choice, prescribe ARV drugs that do not interact with hormonal methods • Encourage correct and consistent use of contraceptive method • Keep abreast of guideline updates
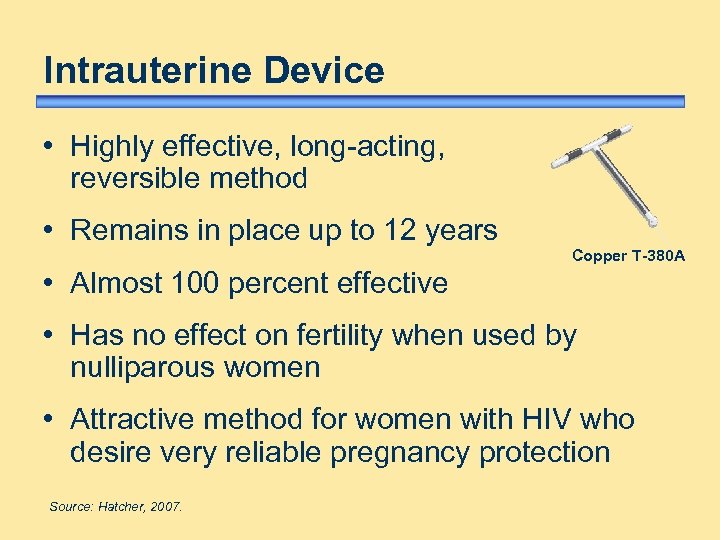 Intrauterine Device • Highly effective, long-acting, reversible method • Remains in place up to 12 years Copper T-380 A • Almost 100 percent effective • Has no effect on fertility when used by nulliparous women • Attractive method for women with HIV who desire very reliable pregnancy protection Source: Hatcher, 2007.
Intrauterine Device • Highly effective, long-acting, reversible method • Remains in place up to 12 years Copper T-380 A • Almost 100 percent effective • Has no effect on fertility when used by nulliparous women • Attractive method for women with HIV who desire very reliable pregnancy protection Source: Hatcher, 2007.
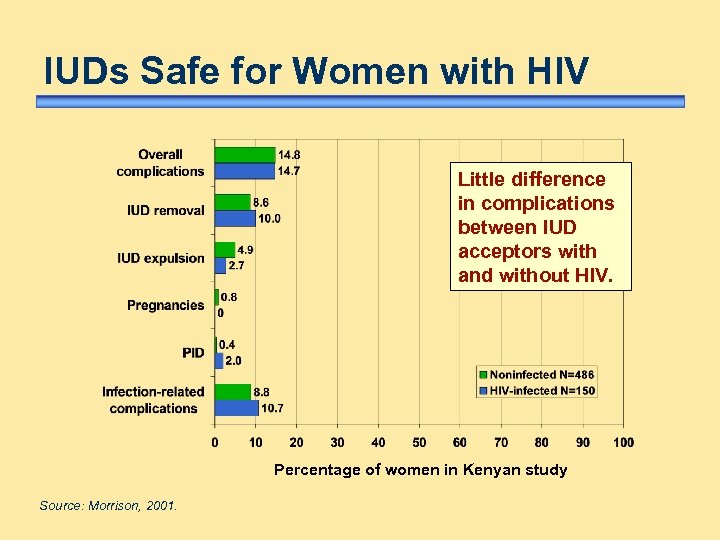 IUDs Safe for Women with HIV Little difference in complications between IUD acceptors with and without HIV. Percentage of women in Kenyan study Source: Morrison, 2001.
IUDs Safe for Women with HIV Little difference in complications between IUD acceptors with and without HIV. Percentage of women in Kenyan study Source: Morrison, 2001.
 IUD Use Does Not Increase HIV Transmission Theoretical concern: • IUD use by women with HIV may increase risk of transmission to partner Research has found: • no post-insertion increase in cervical shedding • no increased risk of partner exposure to higher dose of virus ? ? ? 4 Source: Richardson, 1999.
IUD Use Does Not Increase HIV Transmission Theoretical concern: • IUD use by women with HIV may increase risk of transmission to partner Research has found: • no post-insertion increase in cervical shedding • no increased risk of partner exposure to higher dose of virus ? ? ? 4 Source: Richardson, 1999.
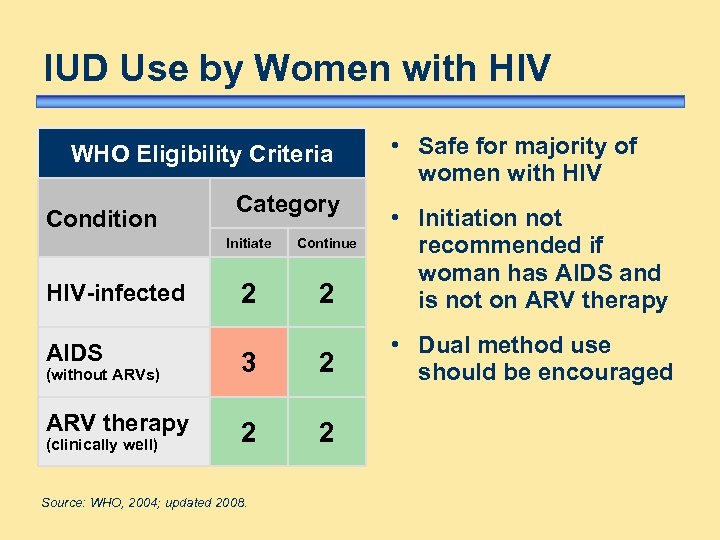 IUD Use by Women with HIV WHO Eligibility Criteria Category • Safe for majority of women with HIV Initiate Condition HIV-infected Continue 2 2 • Initiation not recommended if woman has AIDS and is not on ARV therapy • Dual method use should be encouraged AIDS 3 2 ARV therapy 2 2 (without ARVs) (clinically well) Source: WHO, 2004; updated 2008.
IUD Use by Women with HIV WHO Eligibility Criteria Category • Safe for majority of women with HIV Initiate Condition HIV-infected Continue 2 2 • Initiation not recommended if woman has AIDS and is not on ARV therapy • Dual method use should be encouraged AIDS 3 2 ARV therapy 2 2 (without ARVs) (clinically well) Source: WHO, 2004; updated 2008.
 Spermicides • Provide limited protection with pregnancy rates: – 18% perfect use – 29% typical use • Provide no STI protection • May increase risk of HIV (when used several times per day) Source: Hatcher, 2007; Wilkinson, 2002; WHO, 2002; Van Damme 2002.
Spermicides • Provide limited protection with pregnancy rates: – 18% perfect use – 29% typical use • Provide no STI protection • May increase risk of HIV (when used several times per day) Source: Hatcher, 2007; Wilkinson, 2002; WHO, 2002; Van Damme 2002.
 Diaphragms • Diaphragm used with spermicide – 6% failure rate in perfect use – 16% failure rate in typical use • May offer limited protection from STI/HIV – blocks cervix as entry point for gonorrhoea, chlamydia, and HIV – studies are under way Source: Hatcher, 2007; Moench, 2001; Hu, 2000; Padian, 2007.
Diaphragms • Diaphragm used with spermicide – 6% failure rate in perfect use – 16% failure rate in typical use • May offer limited protection from STI/HIV – blocks cervix as entry point for gonorrhoea, chlamydia, and HIV – studies are under way Source: Hatcher, 2007; Moench, 2001; Hu, 2000; Padian, 2007.
 Spermicide/Diaphragm: Use By Women with HIV • Use not recommended • Spermicides alone or used with a diaphragm may increase the risk of HIV transmission • If a woman desires reliable pregnancy protection, encourage consideration of other methods • Encourage dual method use Source: WHO, 2004, updated 2008; Gottlieb, 2004.
Spermicide/Diaphragm: Use By Women with HIV • Use not recommended • Spermicides alone or used with a diaphragm may increase the risk of HIV transmission • If a woman desires reliable pregnancy protection, encourage consideration of other methods • Encourage dual method use Source: WHO, 2004, updated 2008; Gottlieb, 2004.
 Surgical Sterilization • Good for couples who want no more children Female • Safe, simple surgical procedure • Considered permanent • Very effective; pregnancy rates: – Female: 0. 5% after one year, increasing to 1. 85% over ten years – Male: 0. 1% - 0. 15% (possibly higher) Source: Hatcher, 2007. Mal e
Surgical Sterilization • Good for couples who want no more children Female • Safe, simple surgical procedure • Considered permanent • Very effective; pregnancy rates: – Female: 0. 5% after one year, increasing to 1. 85% over ten years – Male: 0. 1% - 0. 15% (possibly higher) Source: Hatcher, 2007. Mal e
 Sterilization Use by Clients with HIV • No medical reasons to deny sterilization to clients with HIV • Procedure may be delayed in event of acute HIV-related infection • Encourage condom use to prevent STI/HIV transmission Source: WHO, 2004; updated 2008.
Sterilization Use by Clients with HIV • No medical reasons to deny sterilization to clients with HIV • Procedure may be delayed in event of acute HIV-related infection • Encourage condom use to prevent STI/HIV transmission Source: WHO, 2004; updated 2008.
 Lactational Amenorrhoea Method • Temporary contraceptive option • Used by postpartum women who: – are less than six months postpartum – are fully or nearly fully breastfeeding – have no menses • Safe, convenient, effective Source: Hatcher, 2007.
Lactational Amenorrhoea Method • Temporary contraceptive option • Used by postpartum women who: – are less than six months postpartum – are fully or nearly fully breastfeeding – have no menses • Safe, convenient, effective Source: Hatcher, 2007.
 LAM Use by Women with HIV • Advise that children can become infected – risk of acquisition through breast milk ~16% • Exclusive breastfeeding during first six months may reduce risk of acquisition by infant (compared to mixed feeding) • Exclusive use of formula or other substitutes eliminates risk of transmission through breast milk (often not possible) Source: Nduati, 2000; De Cock, 2000; WHO, 2006.
LAM Use by Women with HIV • Advise that children can become infected – risk of acquisition through breast milk ~16% • Exclusive breastfeeding during first six months may reduce risk of acquisition by infant (compared to mixed feeding) • Exclusive use of formula or other substitutes eliminates risk of transmission through breast milk (often not possible) Source: Nduati, 2000; De Cock, 2000; WHO, 2006.
 Fertility Awareness-based Methods • Identify fertile days of the menstrual cycle – observe fertility signs (symptothermal method, cervical mucus method) – monitor cycle days (calendar method, standard days method) • Abstinence or barrier methods should be used during the fertile time • Pregnancy rate: – perfect use 1% to 9% – typical use 12 to 25% Source: CCP and WHO, 2007.
Fertility Awareness-based Methods • Identify fertile days of the menstrual cycle – observe fertility signs (symptothermal method, cervical mucus method) – monitor cycle days (calendar method, standard days method) • Abstinence or barrier methods should be used during the fertile time • Pregnancy rate: – perfect use 1% to 9% – typical use 12 to 25% Source: CCP and WHO, 2007.
 FAB Methods Use by Women with HIV Women who are HIV-positive with or without AIDS and those on ARV therapy: • can use without restrictions (calendar and standard days methods rely on regular menstrual cycles) • should be encouraged to use condoms If the client does not want more children, other methods that are less client-dependent should be considered. Source: WHO, 2004; updated 2008.
FAB Methods Use by Women with HIV Women who are HIV-positive with or without AIDS and those on ARV therapy: • can use without restrictions (calendar and standard days methods rely on regular menstrual cycles) • should be encouraged to use condoms If the client does not want more children, other methods that are less client-dependent should be considered. Source: WHO, 2004; updated 2008.
 Summary of Contraceptive Choices • Use two methods concurrently (condoms plus another contraceptive method) • Use one method and understand its limitations (prevent pregnancy versus prevent transmission) – effective pregnancy prevention but no STI/HIV protection – condoms protect from STIs/HIV but typically less effective preventing pregnancy than some other methods • Use no method and abstain from sexual intercourse
Summary of Contraceptive Choices • Use two methods concurrently (condoms plus another contraceptive method) • Use one method and understand its limitations (prevent pregnancy versus prevent transmission) – effective pregnancy prevention but no STI/HIV protection – condoms protect from STIs/HIV but typically less effective preventing pregnancy than some other methods • Use no method and abstain from sexual intercourse
 Family Planning Counselling for Clients with HIV
Family Planning Counselling for Clients with HIV
 Essential Counselling Skills • Be sensitive to circumstances of women and couples with HIV • Respect clients’ rights • Ensure that all women, regardless of HIV status, are free to make informed choices about pregnancy and contraception • Assure privacy and confidentiality
Essential Counselling Skills • Be sensitive to circumstances of women and couples with HIV • Respect clients’ rights • Ensure that all women, regardless of HIV status, are free to make informed choices about pregnancy and contraception • Assure privacy and confidentiality
 Essential Counselling Skills continued. . . • Help clients consider how HIV affects individual circumstances and needs • Tailor counselling session to needs of client • Facilitate partner involvement and offer partner counselling • Provide comprehensive, factual, unbiased information • Support client’s FP decisions, even if you disagree Avoid any type of coercion. Source: Chervenak, 1996.
Essential Counselling Skills continued. . . • Help clients consider how HIV affects individual circumstances and needs • Tailor counselling session to needs of client • Facilitate partner involvement and offer partner counselling • Provide comprehensive, factual, unbiased information • Support client’s FP decisions, even if you disagree Avoid any type of coercion. Source: Chervenak, 1996.
 Counselling about Pregnancy Providers should discuss: • pregnancy does not accelerate HIV disease • condom use to prevent STI/HIV transmission between partners • risks/rates of mother-to-child transmission • ARV drugs reduce transmission at delivery Source: Mc. Intyre, 1998; Bessinger, 1998; European Collaborative Study and the Swiss HIV Pregnancy Cohort, 1997; Vimercati, 2000; Gray, 2005; Working Group on Mother-to-Infant Transmission of HIV, 1995; Dabis, 2000.
Counselling about Pregnancy Providers should discuss: • pregnancy does not accelerate HIV disease • condom use to prevent STI/HIV transmission between partners • risks/rates of mother-to-child transmission • ARV drugs reduce transmission at delivery Source: Mc. Intyre, 1998; Bessinger, 1998; European Collaborative Study and the Swiss HIV Pregnancy Cohort, 1997; Vimercati, 2000; Gray, 2005; Working Group on Mother-to-Infant Transmission of HIV, 1995; Dabis, 2000.
 Counselling about Pregnancy continued. . . • Malaria during pregnancy may increase risk of – HIV transmission to infant – miscarriage • Artificial feeding or exclusive breastfeeding reduces postpartum transmission • Implications of rearing a child with HIV • Availability of family support • Location/logistics of care and treatment Source: ter Kuile, 2004; WHO Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality, 2000.
Counselling about Pregnancy continued. . . • Malaria during pregnancy may increase risk of – HIV transmission to infant – miscarriage • Artificial feeding or exclusive breastfeeding reduces postpartum transmission • Implications of rearing a child with HIV • Availability of family support • Location/logistics of care and treatment Source: ter Kuile, 2004; WHO Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality, 2000.
 Counselling about Contraception Providers should discuss: • characteristics of contraceptive methods • possible side effects and complications • method effectiveness and ability to use correctly • implications/drug interactions for women with HIV who choose hormonal contraception and: – are on ARV therapy – are taking rifampicin or rifabutin (co-infection with TB)
Counselling about Contraception Providers should discuss: • characteristics of contraceptive methods • possible side effects and complications • method effectiveness and ability to use correctly • implications/drug interactions for women with HIV who choose hormonal contraception and: – are on ARV therapy – are taking rifampicin or rifabutin (co-infection with TB)
 Counselling about Contraception continued. . . • limitations of methods in preventing pregnancy and STI/HIV transmission • advantages of dual protection, including dual method use • partner’s willingness to use condoms, condom negotiation strategies • when to return and where to access services
Counselling about Contraception continued. . . • limitations of methods in preventing pregnancy and STI/HIV transmission • advantages of dual protection, including dual method use • partner’s willingness to use condoms, condom negotiation strategies • when to return and where to access services
 ARVs and Hormonal Contraception For women using ARV drugs and hormonal contraception, providers should discuss: • importance of taking pills on schedule • in implications of late reinjection (particularly • possibility of using condoms to provide additional protection from pregnancy the case of NET-EN) (in case hormonal contraceptive effectiveness is compromised by ARVs)
ARVs and Hormonal Contraception For women using ARV drugs and hormonal contraception, providers should discuss: • importance of taking pills on schedule • in implications of late reinjection (particularly • possibility of using condoms to provide additional protection from pregnancy the case of NET-EN) (in case hormonal contraceptive effectiveness is compromised by ARVs)
 Additional Counselling Topics • Importance of knowing partner’s HIV status – encourage partner testing if status is unknown – discuss health implications/prevention strategies for discordant/concordant couples • Considerations in disclosing HIV status – risk of abandonment – violence – loss of financial support
Additional Counselling Topics • Importance of knowing partner’s HIV status – encourage partner testing if status is unknown – discuss health implications/prevention strategies for discordant/concordant couples • Considerations in disclosing HIV status – risk of abandonment – violence – loss of financial support
 Additional Counselling Topics continued. . . • Offer referrals to other RH services as needed: – STI management/treatment – postpartum, postabortion, antenatal care – HIV care and treatment • Discuss available support systems: – family – community – social – legal – nutritional – child health
Additional Counselling Topics continued. . . • Offer referrals to other RH services as needed: – STI management/treatment – postpartum, postabortion, antenatal care – HIV care and treatment • Discuss available support systems: – family – community – social – legal – nutritional – child health
 Program Requirements To address contraceptive needs of clients with HIV, programs should: • ensure providers have necessary skills • ensure availability of FP commodities/supplies • provide adequate counselling and storage facilities • ensure supervision/management support • have referral system in place
Program Requirements To address contraceptive needs of clients with HIV, programs should: • ensure providers have necessary skills • ensure availability of FP commodities/supplies • provide adequate counselling and storage facilities • ensure supervision/management support • have referral system in place
 Role of Contraceptive Services Contraceptive services can: • be sources of information and methods • assist with preventing HIV transmission • help clients consider effect of HIV on family health • assist clients to make informed RH choices
Role of Contraceptive Services Contraceptive services can: • be sources of information and methods • assist with preventing HIV transmission • help clients consider effect of HIV on family health • assist clients to make informed RH choices
 Conclusion With very limited exceptions, almost any method of contraception can be used by clients with HIV.
Conclusion With very limited exceptions, almost any method of contraception can be used by clients with HIV.
 Produced by Family Health International in collaboration with the ACQUIRE Project. Financial support provided by the United States Agency for International Development, Regional Economic Development Services Office for East and Southern Africa (REDSO/ESA).
Produced by Family Health International in collaboration with the ACQUIRE Project. Financial support provided by the United States Agency for International Development, Regional Economic Development Services Office for East and Southern Africa (REDSO/ESA).


