8bf59c32de383a01bb6532dc3c4aceaa.ppt
- Количество слайдов: 33
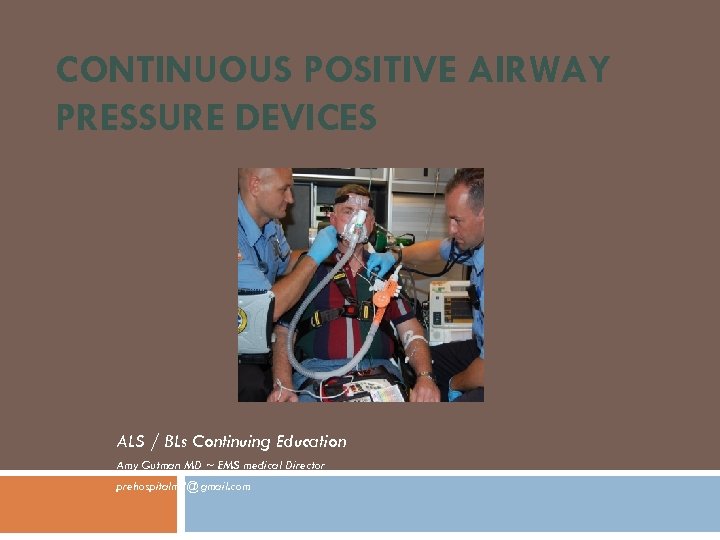
CONTINUOUS POSITIVE AIRWAY PRESSURE DEVICES ALS / BLs Continuing Education Amy Gutman MD ~ EMS medical Director prehospitalmd@gmail. com
Overview CPAP physiology Indications & contraindications EBM literature review OEMS protocol & medical director review
What is CPAP (Continuous Positive Airway Pressure)? High-flow, pressurized & concentrated O 2 delivery system Exhalation port flow restriction device provides positive end expiratory pressure (PEEP) at a set level throughout inspiration & expiration preventing upper airway structures from collapsing &“splinting” open alveoli By placing airway under a constant level of pressure throughout the respiratory cycle, obstructions are "pushed" out of the alveoli Increased intrathoracic pressure reduces preload & afterload, improving left ventricular function Maintains patency of small airways & alveoli Improves gas exchange & reduces work of breathing by moving fluid into vasculature Improves bronchodilator delivery Noninvasive option to support pts through a respiratory crisis, avoid ETI, or buy time until ETI can be performed in a more controlled environment
CPAP vs Bi. PAP CPAP Bi. PAP “Continuous” constant positive pressure throughout respiratory cycle “Bilevels” (2) of positive pressure during different phases of the respiratory cycle When pt breathing in, Inspiratory Positive Airway Pressure (IPAP) exerted When pt breathing out, Expiratory Positive Airway Pressure (EPAP) exerted “Effects of Bi. PAP in patients with COPD” (European Respiratory Journal; 2000 ) Bi. PAP causes higher intrathoracic pressures & reduces myocardial perfusion Bi. PAP causes lower tidal volumes & increases work of breathing (vs CPAP)
CPAP O 2 Delivery Prehospital CPAP devices powered by O 2 source delivering >50 psi Some have a fixed flow rate, while others can be adjusted Fixed either 35% or 100% but actual O 2 concentration less depending on leaks and minute ventilation Variable rate increases chance of inadequate oxygen supply The percentage of oxygen delivered (Fi. O 2) usually starts at 30% & can be increased depending on pt needs At 28 -30% Fi. O 2 , a full tank should last approximately: D cylinder E cylinder M cylinder = = = 28 minutes 40 -50 minutes 4 hours
Indications Increased work of breathing limits ability to remove CO 2 Rising CO 2 levels cause narcotic like brain effect (“CO 2 Narcosis”) Fatigue & high CO 2 lead to further lowering of ventilation rate & respiratory failure
Contraindications Need for emergent ETI Hypotension Cannot follow commands Aspiration risk Upper GI bleed / vomiting Recent facial trauma Tracheostomy Chest trauma / suspected pneumothorax Claustrophobic (make an attempt)
Side Effects Anxiety (most common) As CPAP increases intra-thoracic pressure & gastric distention, there is a risk of hypotension & PTX Abruptly stopping treatment can result in decompensation & need for ETI Give hospital advance notice
COPD Lungs lose elastic recoil from scarred alveoli & bronchioles scar Hypercarbic (ventilation issue) Traditional therapies involve brochodilators (requires adequate ventilation) Difficult to ETI prehospitally without RSI Bronchioles collapse during exhalation leading to alveolar air trapping “Pursed lip” breathing increases “auto-PEEP” COPD pts requiring ETI have worse outcomes than if managed conservatively
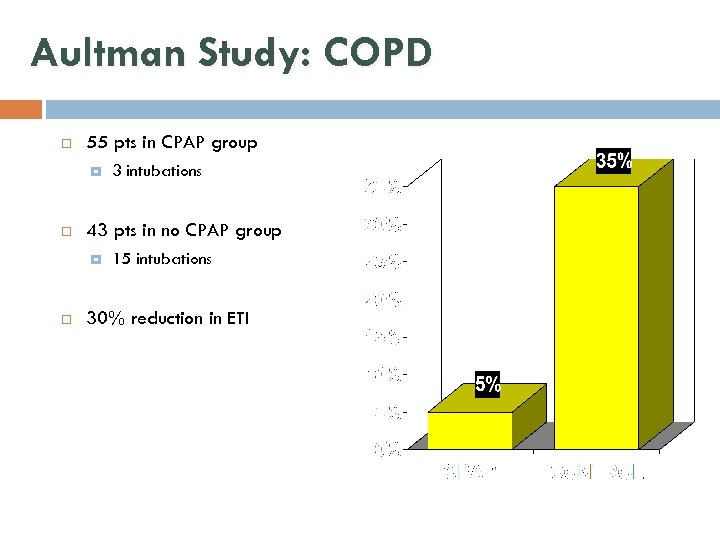
Aultman Study: COPD 55 pts in CPAP group 43 pts in no CPAP group 3 intubations 15 intubations 30% reduction in ETI
Congestive Heart Failure Incidence 1: 100 pt transports >65 yo 25% medicare admissions Increased interstitial fluid interferes with gas exchange / oxygenation Lymphatics remove 10 -20 cc pulmonary fluid/ hr Increased myocardial workload results in higher O 2 demands in pts who often have ischemic heart disease Traditional therapies reduce pre-load & after-load as well as remove interstitial fluid CPAP “pushes” fluid out of alveoli back into the vascular & lymphatic tissues 33% have ETI if no attempts at non-invasive pressure support Intubated pts have 4 X greater mortality of non-intubated pt
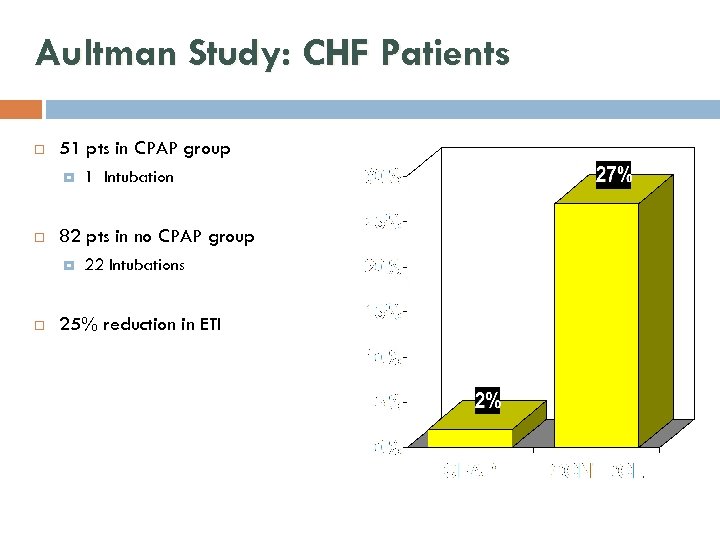
Aultman Study: CHF Patients 51 pts in CPAP group 82 pts in no CPAP group 1 Intubation 22 Intubations 25% reduction in ETI
Asthma Bronchospasm & increased work of breathing Pts cannot physically move air in & out of the lungs due to spasm CPAP delivers aerosolized medications & “splints” open spasming alveoli & bronchioles
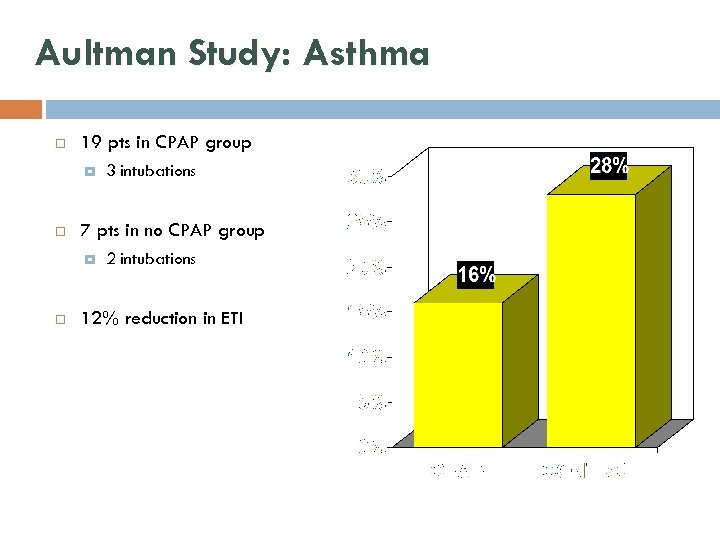
Aultman Study: Asthma 19 pts in CPAP group 7 pts in no CPAP group 3 intubations 2 intubations 12% reduction in ETI
Equipment Easy to use & portable Adjustable to patient’s needs Easily started & discontinued Provide quantifiable & reliable airway pressures Conservative oxygen utilization Limited interference with administration of “traditional” cardio-respiratory therapies
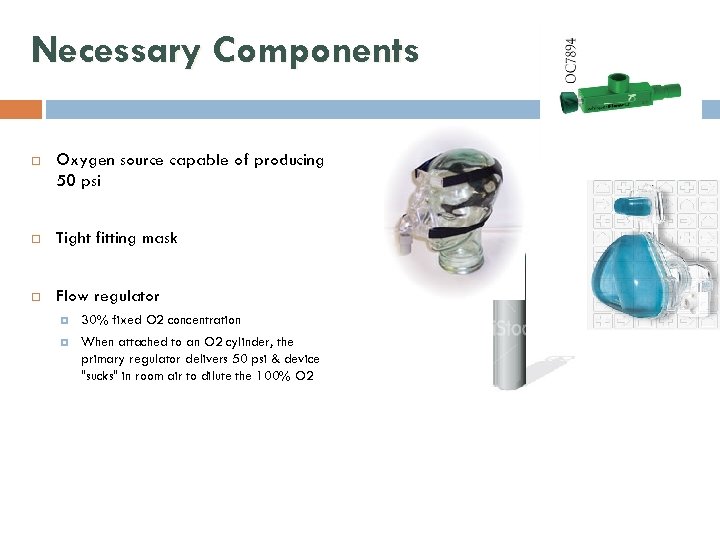
Necessary Components Oxygen source capable of producing 50 psi Tight fitting mask Flow regulator 30% fixed O 2 concentration When attached to an O 2 cylinder, the primary regulator delivers 50 psi & device "sucks" in room air to dilute the 100% O 2
PEEP Valve PEEP valve connected to exhalation port to maintain a constant circuit pressure Each PEEP valve rated at a certain level measured in 2. 5 cm. H 2 O increments Common increments are 5. 0 or 7. 5 cm. H 20
Important Points Continually check for air leaks & pt tolerance Do not break seal to give meds If pt improves, continue CPAP until ED personnel transfer pt to their equipment If pt deteriorates, discontinue CPAP & prepare for ETI Notify destination hospital that CPAP is been used
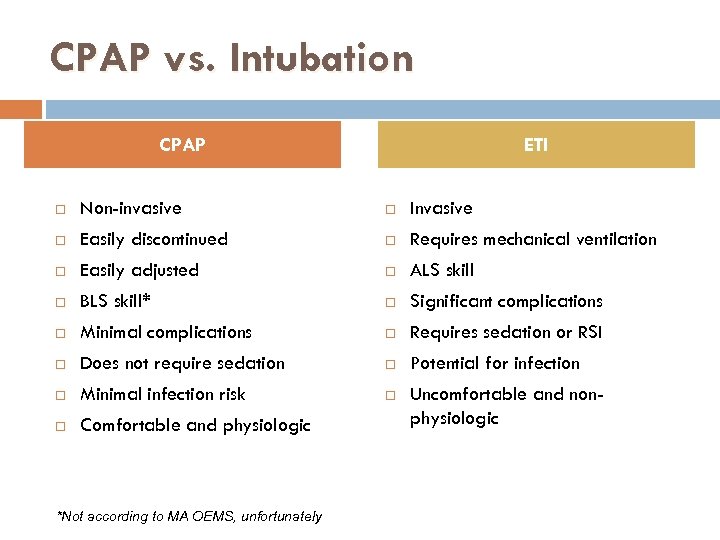
CPAP vs. Intubation CPAP ETI Non-invasive Invasive Easily discontinued Requires mechanical ventilation Easily adjusted ALS skill BLS skill* Significant complications Minimal complications Requires sedation or RSI Does not require sedation Potential for infection Minimal infection risk Comfortable and physiologic Uncomfortable and nonphysiologic *Not according to MA OEMS, unfortunately
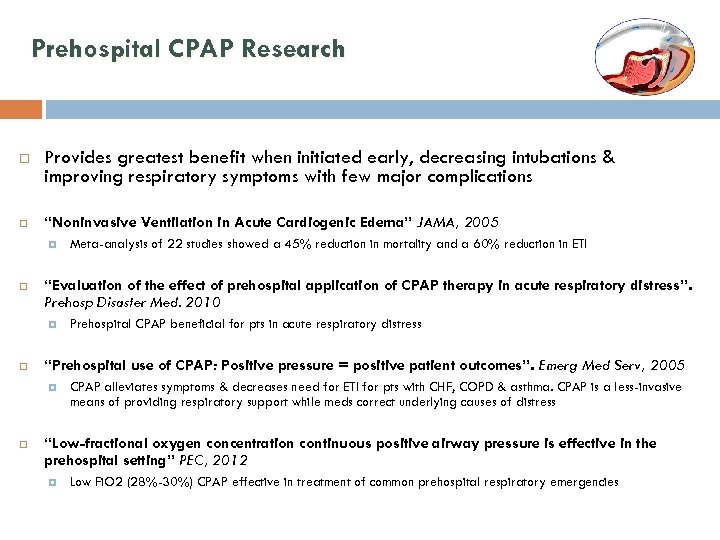
Prehospital CPAP Research Provides greatest benefit when initiated early, decreasing intubations & improving respiratory symptoms with few major complications “Noninvasive Ventilation in Acute Cardiogenic Edema” JAMA, 2005 “Evaluation of the effect of prehospital application of CPAP therapy in acute respiratory distress”. Prehosp Disaster Med. 2010 Prehospital CPAP beneficial for pts in acute respiratory distress “Prehospital use of CPAP: Positive pressure = positive patient outcomes”. Emerg Med Serv, 2005 Meta-analysis of 22 studies showed a 45% reduction in mortality and a 60% reduction in ETI CPAP alleviates symptoms & decreases need for ETI for pts with CHF, COPD & asthma. CPAP is a less-invasive means of providing respiratory support while meds correct underlying causes of distress “Low-fractional oxygen concentration continuous positive airway pressure is effective in the prehospital setting” PEC, 2012 Low Fi. O 2 (28%-30%) CPAP effective in treatment of common prehospital respiratory emergencies
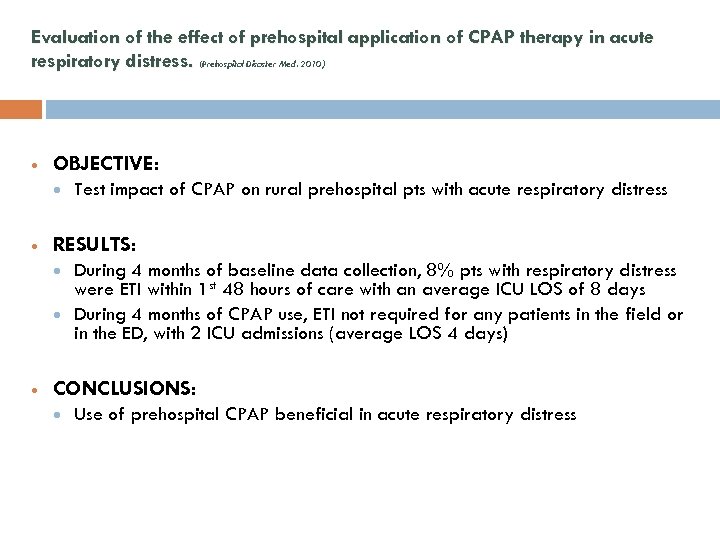
Evaluation of the effect of prehospital application of CPAP therapy in acute respiratory distress. (Prehospital Disaster Med. 2010) OBJECTIVE: RESULTS: Test impact of CPAP on rural prehospital pts with acute respiratory distress During 4 months of baseline data collection, 8% pts with respiratory distress were ETI within 1 st 48 hours of care with an average ICU LOS of 8 days During 4 months of CPAP use, ETI not required for any patients in the field or in the ED, with 2 ICU admissions (average LOS 4 days) CONCLUSIONS: Use of prehospital CPAP beneficial in acute respiratory distress
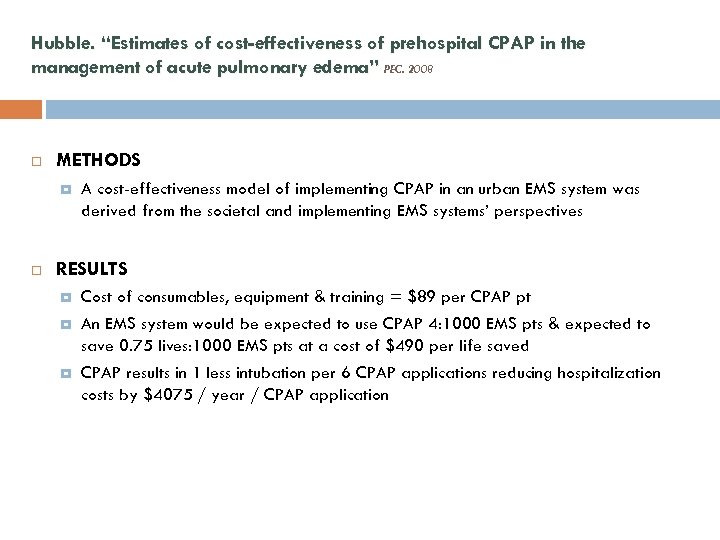
Hubble. “Estimates of cost-effectiveness of prehospital CPAP in the management of acute pulmonary edema” PEC. 2008 METHODS A cost-effectiveness model of implementing CPAP in an urban EMS system was derived from the societal and implementing EMS systems’ perspectives RESULTS Cost of consumables, equipment & training = $89 per CPAP pt An EMS system would be expected to use CPAP 4: 1000 EMS pts & expected to save 0. 75 lives: 1000 EMS pts at a cost of $490 per life saved CPAP results in 1 less intubation per 6 CPAP applications reducing hospitalization costs by $4075 / year / CPAP application
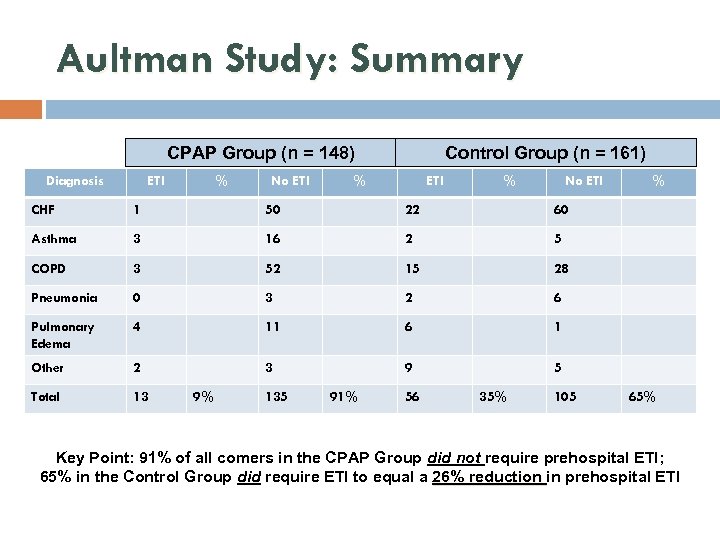
Aultman Study: Summary CPAP Group (n = 148) Diagnosis ETI % No ETI Control Group (n = 161) % ETI % No ETI CHF 1 50 22 60 Asthma 3 16 2 5 COPD 3 52 15 28 Pneumonia 0 3 2 6 Pulmonary Edema 4 11 6 1 Other 2 3 9 5 Total 13 % 9% 135 91% 56 35% 105 65% Key Point: 91% of all comers in the CPAP Group did not require prehospital ETI; 65% in the Control Group did require ETI to equal a 26% reduction in prehospital ETI
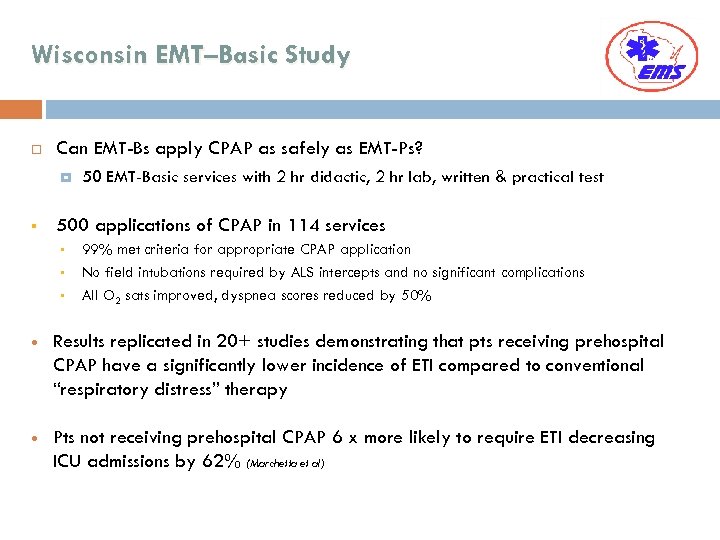
Wisconsin EMT–Basic Study Can EMT-Bs apply CPAP as safely as EMT-Ps? § 500 applications of CPAP in 114 services § § § 50 EMT-Basic services with 2 hr didactic, 2 hr lab, written & practical test 99% met criteria for appropriate CPAP application No field intubations required by ALS intercepts and no significant complications All O 2 sats improved, dyspnea scores reduced by 50% Results replicated in 20+ studies demonstrating that pts receiving prehospital CPAP have a significantly lower incidence of ETI compared to conventional “respiratory distress” therapy Pts not receiving prehospital CPAP 6 x more likely to require ETI decreasing ICU admissions by 62% (Marchetta et al)
Points to Consider How good is your current therapy for respiratory distress? Aggressive use of bronchodilators? Aggressive nitrates for CHF? Prehospital & ED intubation rate? Do you have active medical oversight? Advanced airway management is considered a sentinel event ALS or BOTH?
OEMS 3. 4 Bronchospasm / Respiratory Distress Assessment & Treatment Priorities Scene safety, BSI Maintain open airway, assist ventilations prn, administer oxygen as needed Check hemodynamic stability, symptoms, LOC, ABCs, vitals, monitor / ECG Obtain OPQRST & SAMPLE Determine level of respiratory distress Mild: Slight wheezing. mild cough, able to move air without difficulty Severe: Poor air movement, dyspnea, use of accessory muscles, tachypnea, tachycardia. M ay present without wheezes Rapid transport w/ wo ALS. Do not allow pt to exert themselves in a position of comfort or appropriate to treatment(s) required
OEMS 3. 4 Bronchospasm / Respiratory Distress BLS Procedures Activate ALS intercept but initiate rapid transport w / wo ALS Mild Distress: Encourage &/or assist pt to self-administer their prescribed inhaler if indicated Continually reassess vitals Contact Medical Control to: Repeat a 2 nd MDI dose if required & if maximum dose not reached Assist in using MDI Use MDI if not specifically been prescribed for patient
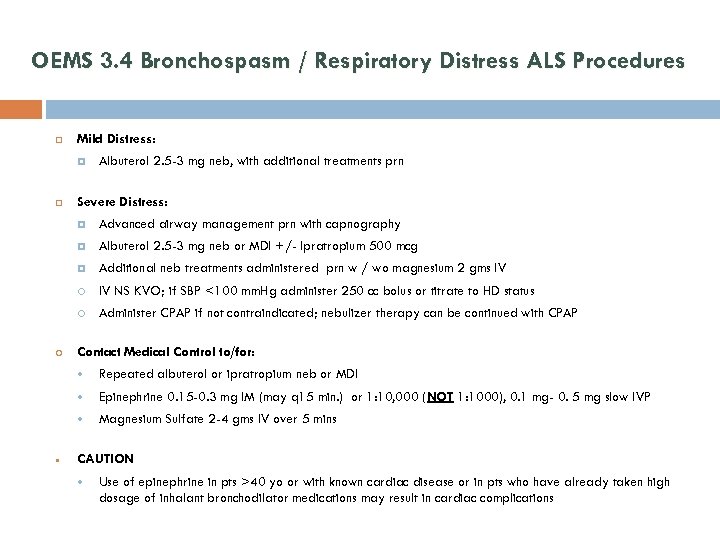
OEMS 3. 4 Bronchospasm / Respiratory Distress ALS Procedures Mild Distress: Albuterol 2. 5 -3 mg neb, with additional treatments prn Severe Distress: Albuterol 2. 5 -3 mg neb or MDI +/- Ipratropium 500 mcg Additional neb treatments administered prn w / wo magnesium 2 gms IV IV NS KVO; if SBP <100 mm. Hg administer 250 cc bolus or titrate to HD status Advanced airway management prn with capnography Administer CPAP if not contraindicated; nebulizer therapy can be continued with CPAP Contact Medical Control to/for: Epinephrine 0. 15 -0. 3 mg IM (may q 15 min. ) or 1: 10, 000 (NOT 1: 1000), 0. 1 mg- 0. 5 mg slow IVP Repeated albuterol or ipratropium neb or MDI Magnesium Sulfate 2 -4 gms IV over 5 mins CAUTION Use of epinephrine in pts >40 yo or with known cardiac disease or in pts who have already taken high dosage of inhalant bronchodilator medications may result in cardiac complications
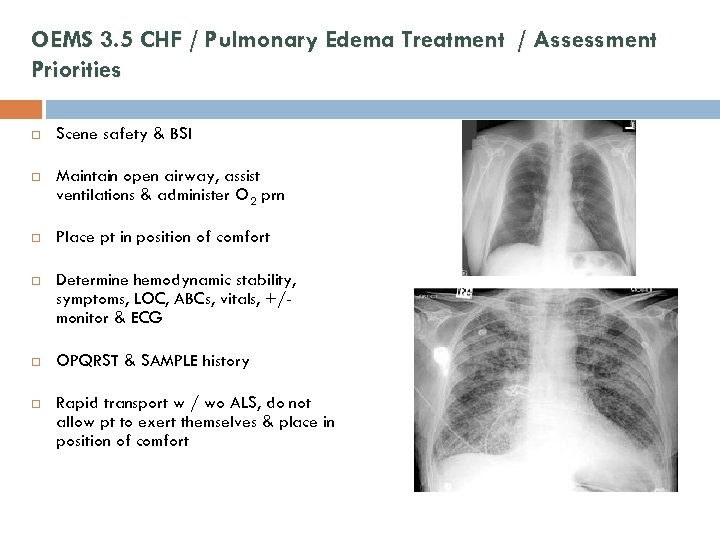
OEMS 3. 5 CHF / Pulmonary Edema Treatment / Assessment Priorities Scene safety & BSI Maintain open airway, assist ventilations & administer O 2 prn Place pt in position of comfort Determine hemodynamic stability, symptoms, LOC, ABCs, vitals, +/monitor & ECG OPQRST & SAMPLE history Rapid transport w / wo ALS, do not allow pt to exert themselves & place in position of comfort
OEMS 3. 5 CHF / Pulmonary Edema BLS Procedures Activate ALS intercept if necessary & available Rapid transport, w / wo ALS Notify receiving hospital
OEMS 3. 5 CHF / Pulmonary Edema ALS Procedures Advanced airway management w/ capnography if indicated IV NS KVO en route to the hospital If SBP < 100 mm. Hg administer 250 cc bolus or titrate to HD status NTG SL or spray if SBP > 100 mm. Hg; may repeat q 5 mins x 2 If pt has taken a PDE 5 - inhibitor (i. e. Viagra) do not administered without a medical control order Contact Medical Control if SBP <100 mm. Hg Contact Medical Control for / if: Nitropaste 1 inch to anterior chest wall Furosemide 20 -40 mg IVP or 40 -80 mg IVP if patient already on diuretics Dopamine 2 - 20 mcg/kg/min To facilitate ETI Medical Control may order Midazolam 2. 5 mg IN or slow IVP. Repeat prn to a total dose of 5 mg
Summary CPAP alleviates respiratory symptoms & decreases need for ETI for pts with respiratory distress Safe, portable & easy to apply Does not replace ETI, but a less-invasive means of providing respiratory support while meds work to correct the underlying cause of respiratory distress Best results with rapid & aggressive use Use your medical control!
References Keith Wesley MD. Wisconsin State EMS Medical Director Mark Marchetta RN, BS, NREMT-P; Mark Resanovich, EMT-P. Aultman Health Foundation (Canton, Ohio) OEMS website and MA State Prehospital Treatment Protocol Brady & Mosby Textbooks “Respiratory Distress” Also see references cited throughout presentation
8bf59c32de383a01bb6532dc3c4aceaa.ppt