5cfcd0b410f35ee642512f5f82c09a2d.ppt
- Количество слайдов: 24
CONTEXT BEFORE IMPLEMENTATION: DECISION MAKERS’ VIEWS OF A PEERLED HEALTHY LIFESTYLE INTERVENTION FOR PEOPLE WITH SERIOUS MENTAL ILLNESS Leopoldo J. Cabassa and Ana Stefancic SIRC 2017 Conference Seattle, WA

2 Acknowledgements • Funding: National Institute of Mental Health: R 01 MH 104574 • Collaborators: Richard Younge, Roberto Lewis-Fernández, Nabila El. Bassel, José Luchsinger, Lauren Gates, Melanie Wall, Lara C. Weinstein, and Lawrence Palinkas • Community Partners: Pathways to • Housing PA, Project HOME, and The Bridge • • Research Assistants: Morgan Dawkins, Sonika Aggarwal, Nathaniel Lu, Kechna Cadet, Talha Alvi, Kristen • Gurdak, Katy Svehaug, Bailey Wier Peer Specialists: Kelli Adams, Yonnie Harris, Lawrence Samuels, Jeff Constantakis Doctoral Students: Lauren Bochicchio, Kathleen O’Hara MSW/MA Students: Adriana Bastardas, Elizabeth Gary, Shirley Capa, Konul Jafarova, Ahmed Alif, Brigid Magdamo, Chelsea Irwin
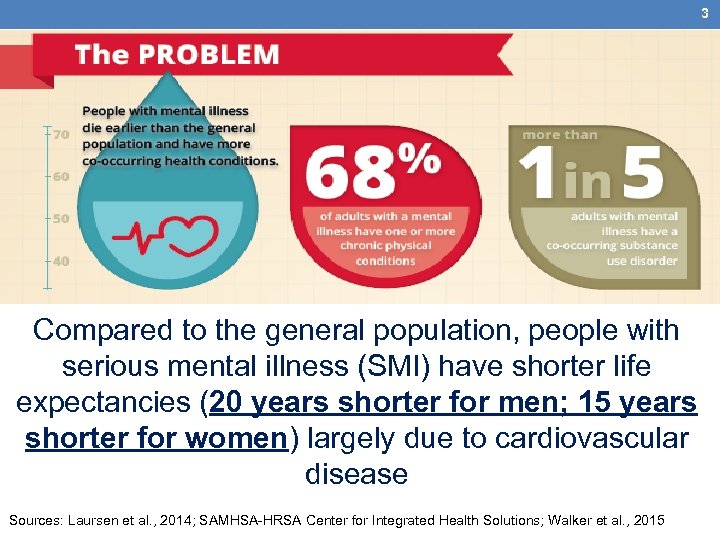
3 Compared to the general population, people with serious mental illness (SMI) have shorter life expectancies (20 years shorter for men; 15 years shorter for women) largely due to cardiovascular disease Sources: Laursen et al. , 2014; SAMHSA-HRSA Center for Integrated Health Solutions; Walker et al. , 2015
4 Supportive Housing • Growing service sector for people with serious mental illness • Provide affordable, community-based housing alongside health, mental health, and social services • Common supportive housing models for people with SMI: • Housing First • Treatment First
5 Why Deliver Health Interventions in Supportive Housing? • Setting for bringing health interventions to “people’s doorsteps” • Many have programs that focus on health, wellness, and recovery • Many employ peer specialists • Clients’ preference for bringing peer-led health interventions into this setting Source: Cabassa et al. , Trials. 2015: 16: 388

6 Modifiable Risk Factors Environment Medical Care Health Behaviors • Unstable housing • Poverty • Food environment • Underuse of services • Poor quality of care • Medication sideeffects • Smoking • Sedentary lifestyle • Unhealthy diets Sources: Allison et al. , 2009; Cabassa et al. , 2014; Newcomer et al. , 2007
7 Peer-Led Group Lifestyle Balance Program (PGLB) Goals • Achieve a healthy balance through: • Healthy eating • Physically activity • Uses behavioral techniques (e. g. , self- monitoring, problem solving) • Delivered by trained peer-specialists • Group Intervention (≈1 hour each, 22 in total) • “To Do” assignment to work on at home • In between session contact to sustain engagement

8 Implementation Gap • Healthy lifestyle interventions are not routinely used in supportive housing • Peer specialists in supportive housing do not commonly deliver health interventions • Stakeholders’ views and perceptions of a peer-led healthy lifestyle program are unknown • Contextual factors that can shape the implementation of peer-led healthy lifestyle interventions in supportive housing have not been studied

9 Study Questions • How do directors and program managers in supportive housing view a peer-led healthy lifestyle intervention before its implementation? • What contextual factors are thought to shape the implementation of this intervention in supportive housing agencies?
10 Methods • Sample: Directors and project managers from 3 supportive housing agencies (1 housing first and 2 treatment first) • Method: Semi-structured qualitative interviews • Vignette presentation of our peer-led healthy lifestyle intervention • Rank-ordering exercise of top three facilitators, barriers, and intervention characteristics • Analytical Strategy: • Directed content analysis informed by our conceptual approach: • Diffusion of Innovations: “Perceptions count” • Consolidated Framework of Implementation Research: “Context matters”
11 Participant Characteristics (N = 12) • Agency Directors: 3 Program Managers: 9 • Average years working in organization: • 5. 2 (sd = 4. 8) • Age: 46. 9 (sd = 12. 3) • Female: 75% • Ethnicity/Race • Non-Hispanic White: 83. 3% • African Americans: 8. 3% • Hispanic: 8. 3% • Average years working with people with SMI: • 16. 4 (sd = 9. 6) • Average years working in supportive housing: • 14. 6 (sd = 10. 7)
12 WHAT ARE DIRECTORS AND PROGRAM MANAGERS VIEWS OF PGLB?
13 Views of PGLB • Viewed as a “great idea”; “much needed program”; “a big need with the folks we serve” • Perceived benefits: • Peer-run: “I think that's awesome” • Focus on “wellness”, “the nutritional and physical aspects” of the intervention. • “Spillover. . . on their other goals and their sense of self-efficacy in other parts of their lives” • “It can have a cultural shift toward more health integration [in the organization] • Key concerns: • “Mostly logistic. . office space. . ” • “How do we make sure. . . people stay engaged” • “Clash with what people are already doing [other services]”
14 What Intervention Characteristics Were Most Valued for Supporting PGLB Implementation? 1. Relative advantage: “shows that an intervention work” 2. Compatibility to clients: “meets the needs of the population” 3. Trialability: “pilot funds to try out intervention for limited time” • Cost: “if it can get reimbursed, it’s always a perk” • Complexity: “easily delivered by peer specialists” • Training: “training program and manual and having an online community. . . would be invaluable”
15 WHAT FACTORS COULD SHAPE THE IMPLEMENTATION OF PGLB IN SUPPORTIVE HOUSING AGENCIES?
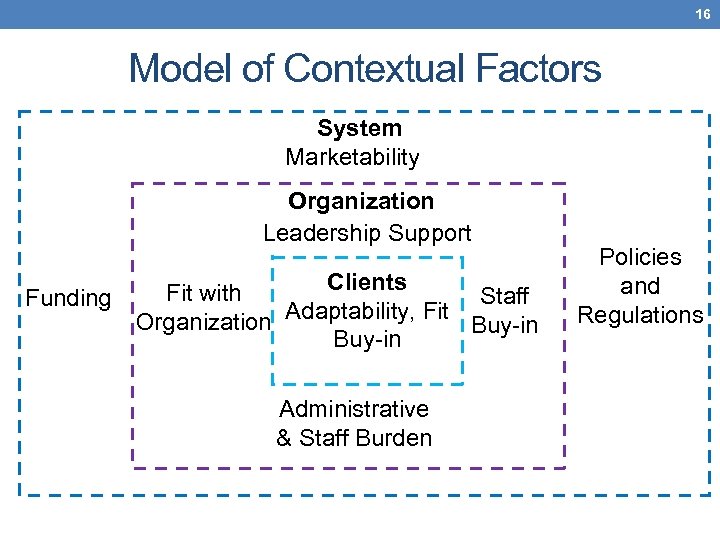
16 Model of Contextual Factors System Marketability Organization Leadership Support Funding Clients Fit with Staff Adaptability, Fit Organization Buy-in Administrative & Staff Burden Policies and Regulations
17 System-Level Factors • Revolved around the organization’s capacity to manage risks and benefits • Focus on: • Funding: “If it’s reimbursable it’s gonna be a go” • Managing external regulations: “Ridiculous amounts of reporting and oversight and demands from a funder” • Marketability: “Staying competitive with other agencies”
18 Organization-Level Factors • Revolved around themes of leadership support, ensuring compatibility with organization’s mission and addressing staff buy-in and administrative burden • Focus on: • Leadership: “[If] leadership wasn’t behind it. . . it wouldn’t come up off the ground” • Fit: “Match GLB with philosophy and mission of our agency is definitely a facilitator” • Staff buy-in: “[Without] most respected and creative staff on board. . . then it’s not going to roll out. ” • Administrative and staff burden: “Staff can only take so much more both in terms of workload and time and administrative burden. ”
19 Client-Level Factors • Revolved around making sure the intervention addresses clients’ needs and sustains their interest and support • Focus on: • Adaptability: “Adapting - so basically the PGLB being able to meet the need of where our folks are” • Fit: “Most importantly has to meet the needs of the population. That is the number 1 priority for the program” • Buy-in: “Usually not being able to sustain something has to do with the clients losing interest. ”
20 Discussion • PGLB viewed as a valuable intervention • Decision makers focused on the benefits, fit, cost and importance of piloting the intervention • Interplay of funding concerns, external regulations, leadership support, fit with organization’s mission, concerns about administrative burdens, and staff and clients’ buy-in were viewed as critical for implementation
21 Lessons for Implementation Strategies • Disseminate information focusing on relative advantage, fit, and cost • Pilot funds to build experience and infrastructure • Financial planning to address cost concerns • Management supports to enhance organizations’ capacity to address financial, regulations, and administrative issues. • Combination of collaborative planning, provider training, and restructuring needed to ensure compatibility and buy-in
22 Limitations • Small sample of agencies • Supportive housing agencies engaged in health integration efforts (early adopters) • Only examined directors and program managers perspectives
23 Conclusions • Examining context before implementation can help: • Identify barriers and facilitators • Shape the selection and development of implementation strategies • Future work is needed to develop contextually- grounded implementation strategies to help deploy health interventions that can reduce health disparities among people with SMI.
24 Thank You // Gracias Leopoldo J. Cabassa, M. S. W. , Ph. D. Associate Professor George Warren Brown School of Social Work Washington University in St. Louis ljcabassa@wustl. edu
5cfcd0b410f35ee642512f5f82c09a2d.ppt