9c0cdc7b463c8b23188bc39b2b690d8d.ppt
- Количество слайдов: 51
 Concussions: New Guidelines and What It Means In Today’s Athletic Environment Aaron Bott, MD Dave Schultz, MEd, ATC Sports Medicine Outreach Program Nebraska Sports Concussion Network
Concussions: New Guidelines and What It Means In Today’s Athletic Environment Aaron Bott, MD Dave Schultz, MEd, ATC Sports Medicine Outreach Program Nebraska Sports Concussion Network
 The Concussion Problem • Concussion injury reporting increasing • • dramatically. Substantial changes in concussion management guidelines in past 3 -5 yrs. General void in education and awareness. Disregard for seriousness of “minor” injuries. Lack of consensus on management protocol by healthcare professionals.
The Concussion Problem • Concussion injury reporting increasing • • dramatically. Substantial changes in concussion management guidelines in past 3 -5 yrs. General void in education and awareness. Disregard for seriousness of “minor” injuries. Lack of consensus on management protocol by healthcare professionals.
 The Concussion Problem • Athletes, knowingly & unknowingly, playing with symptoms, leave the brain vulnerable to longterm neurological impairment, serious and catastrophic injury, even death.
The Concussion Problem • Athletes, knowingly & unknowingly, playing with symptoms, leave the brain vulnerable to longterm neurological impairment, serious and catastrophic injury, even death.
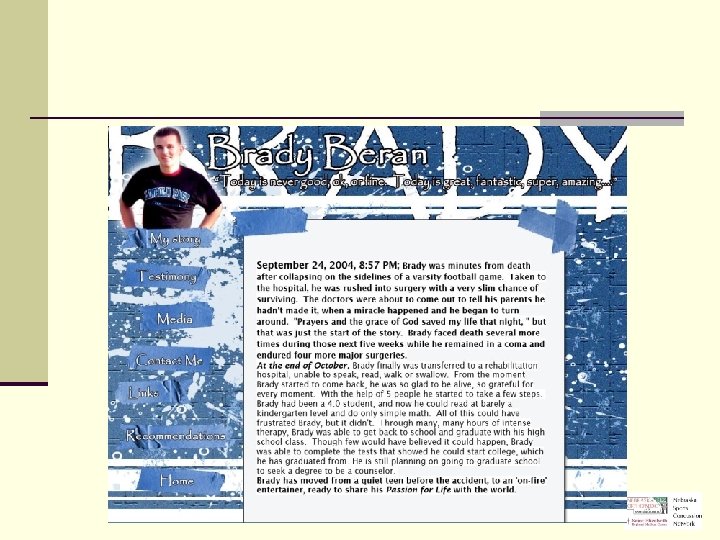
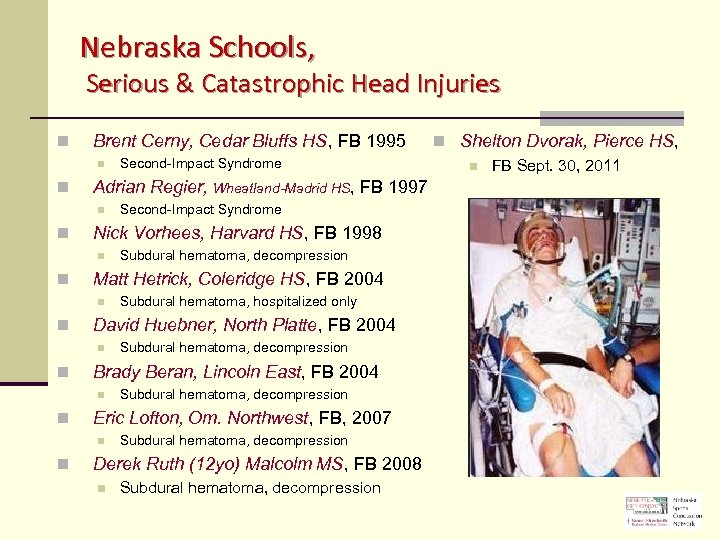 Nebraska Schools, Serious & Catastrophic Head Injuries n Brent Cerny, Cedar Bluffs HS, FB 1995 n n Adrian Regier, Wheatland-Madrid HS, FB 1997 n n Subdural hematoma, decompression Eric Lofton, Om. Northwest, FB, 2007 n n Subdural hematoma, decompression Brady Beran, Lincoln East, FB 2004 n n Subdural hematoma, hospitalized only David Huebner, North Platte, FB 2004 n n Subdural hematoma, decompression Matt Hetrick, Coleridge HS, FB 2004 n n Second-Impact Syndrome Nick Vorhees, Harvard HS, FB 1998 n n Second-Impact Syndrome Subdural hematoma, decompression Derek Ruth (12 yo) Malcolm MS, FB 2008 n Subdural hematoma, decompression n Shelton Dvorak, Pierce HS, n FB Sept. 30, 2011
Nebraska Schools, Serious & Catastrophic Head Injuries n Brent Cerny, Cedar Bluffs HS, FB 1995 n n Adrian Regier, Wheatland-Madrid HS, FB 1997 n n Subdural hematoma, decompression Eric Lofton, Om. Northwest, FB, 2007 n n Subdural hematoma, decompression Brady Beran, Lincoln East, FB 2004 n n Subdural hematoma, hospitalized only David Huebner, North Platte, FB 2004 n n Subdural hematoma, decompression Matt Hetrick, Coleridge HS, FB 2004 n n Second-Impact Syndrome Nick Vorhees, Harvard HS, FB 1998 n n Second-Impact Syndrome Subdural hematoma, decompression Derek Ruth (12 yo) Malcolm MS, FB 2008 n Subdural hematoma, decompression n Shelton Dvorak, Pierce HS, n FB Sept. 30, 2011
 Concussion Scenarios • On-field Injuries (acute) • “Bell-Rung, Dinged” • “Dazed, Shaken Up, Rocked, Lit-Up” • Injuries that are unknown and unreported • Injuries occurring outside team play • MVA, playing on other teams, other mishaps • Accumulative, sub-concussive injuries • Post-Concussion Syndrome (chronic)
Concussion Scenarios • On-field Injuries (acute) • “Bell-Rung, Dinged” • “Dazed, Shaken Up, Rocked, Lit-Up” • Injuries that are unknown and unreported • Injuries occurring outside team play • MVA, playing on other teams, other mishaps • Accumulative, sub-concussive injuries • Post-Concussion Syndrome (chronic)
 Post-Concussion Syndrome • Chronic Headache (migraine) • Sensitivity to Light & Noise • Chronic Fatigue • Balance (vestibular) Problems • Behavioral Changes • Sleep Problems • Cognitive Deficits • Academic Difficulties
Post-Concussion Syndrome • Chronic Headache (migraine) • Sensitivity to Light & Noise • Chronic Fatigue • Balance (vestibular) Problems • Behavioral Changes • Sleep Problems • Cognitive Deficits • Academic Difficulties
 The Concussion Problem • Growing evidence of causation for memory impairment, emotional instability, erratic behavior, depression, problems with impulse control, and early onset neuro-degenerative diseases. • • Dementia Chronic Traumatic Encephalopathy (CTE) • Boxers, NFL football players
The Concussion Problem • Growing evidence of causation for memory impairment, emotional instability, erratic behavior, depression, problems with impulse control, and early onset neuro-degenerative diseases. • • Dementia Chronic Traumatic Encephalopathy (CTE) • Boxers, NFL football players
 CTE n CTE, first reported in 1928 and originally referred to as “dementia pugilistica” because it was believed to only affect boxers, is a progressive neurodegenerative disease caused by repetitive trauma to the brain. The use of the terms Traumatic Encephalopathy and CTE were first used in the 1960 s. n The disease is characterized by the build-up of a toxic protein called tau in the form of neurofibrillary tangles (NFTs) and neuropil threads (NTs) throughout the brain. The abnormal protein initially impairs the normal functioning of the brain and eventually kills brain cells. n Early on, CTE sufferers may display clinical symptoms such as memory impairment, emotional instability, erratic behavior, depression and problems with impulse control. However, CTE eventually progresses to full-blown dementia. Although similar to Alzheimer’s disease, CTE is an entirely distinct disease.
CTE n CTE, first reported in 1928 and originally referred to as “dementia pugilistica” because it was believed to only affect boxers, is a progressive neurodegenerative disease caused by repetitive trauma to the brain. The use of the terms Traumatic Encephalopathy and CTE were first used in the 1960 s. n The disease is characterized by the build-up of a toxic protein called tau in the form of neurofibrillary tangles (NFTs) and neuropil threads (NTs) throughout the brain. The abnormal protein initially impairs the normal functioning of the brain and eventually kills brain cells. n Early on, CTE sufferers may display clinical symptoms such as memory impairment, emotional instability, erratic behavior, depression and problems with impulse control. However, CTE eventually progresses to full-blown dementia. Although similar to Alzheimer’s disease, CTE is an entirely distinct disease.
 CTE
CTE
 TAKE HOME Many head related catastrophes do not arise from the blow on the day of the catastrophe – but from an exacerbation of an earlier blow that did not heal. Concussions not only result from a substantial blow or impact to the head, but also result from the accumulative affect of minor blows over time (hours/days/weeks), where such circumstances are much less apparent to the untrained and uniformed.
TAKE HOME Many head related catastrophes do not arise from the blow on the day of the catastrophe – but from an exacerbation of an earlier blow that did not heal. Concussions not only result from a substantial blow or impact to the head, but also result from the accumulative affect of minor blows over time (hours/days/weeks), where such circumstances are much less apparent to the untrained and uniformed.
 LB 260 - Concussion Awareness Act • Interscholastic sports teams, and any youth sports organizations, 19 yo and younger. • 3 Primary Components: • Education, annual basis Education • • Coaches concussion training (online) Athletes/Parents provided concussion information Removal of athlete if “reasonably suspected” of having concussion. Written Clearance for RTP by appropriate licensed healthcare professional, and parent.
LB 260 - Concussion Awareness Act • Interscholastic sports teams, and any youth sports organizations, 19 yo and younger. • 3 Primary Components: • Education, annual basis Education • • Coaches concussion training (online) Athletes/Parents provided concussion information Removal of athlete if “reasonably suspected” of having concussion. Written Clearance for RTP by appropriate licensed healthcare professional, and parent.
 Appropriate Licensed Healthcare Provider • Physician: MD/DO, PA-C, APRN Neuropsychologist Athletic Trainer Or, qualified individual able to provide healthcare services where doing so falls within one’s scope of practice and state licensure, AND trained in the evaluation and management of traumatic brain injuries among a pediatric population. LB 260, July 2012
Appropriate Licensed Healthcare Provider • Physician: MD/DO, PA-C, APRN Neuropsychologist Athletic Trainer Or, qualified individual able to provide healthcare services where doing so falls within one’s scope of practice and state licensure, AND trained in the evaluation and management of traumatic brain injuries among a pediatric population. LB 260, July 2012
 CONCUSSIONS Definition A complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces. 1. Direct blow to the head region; impulsive force transmitted to the head. 2. Rapid onset of short-lived neurological impairment that resolve spontaneously. 3. Acutely, symptoms largely reflect a functional disturbance, rather than structural injury. 4. Symptoms may or may not involve LOC, where resolution follows a sequential course, where some of which may be prolonged. 5. No abnormality in standard structural neuro-imaging studies. Consensus Statement on Concussions in Sport: The 3 rd International Conference on Concussion in Sport held in Zurich, P Mc. Crory, W Meeuwisse, K Johnston, J Dvorak, M Aubry, M Molloy & R Cantu, Br. J. Sports Med. 2009; 43; i 76 -i 84, doi: 10. 1136/bjsm. 2009. 058248
CONCUSSIONS Definition A complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces. 1. Direct blow to the head region; impulsive force transmitted to the head. 2. Rapid onset of short-lived neurological impairment that resolve spontaneously. 3. Acutely, symptoms largely reflect a functional disturbance, rather than structural injury. 4. Symptoms may or may not involve LOC, where resolution follows a sequential course, where some of which may be prolonged. 5. No abnormality in standard structural neuro-imaging studies. Consensus Statement on Concussions in Sport: The 3 rd International Conference on Concussion in Sport held in Zurich, P Mc. Crory, W Meeuwisse, K Johnston, J Dvorak, M Aubry, M Molloy & R Cantu, Br. J. Sports Med. 2009; 43; i 76 -i 84, doi: 10. 1136/bjsm. 2009. 058248
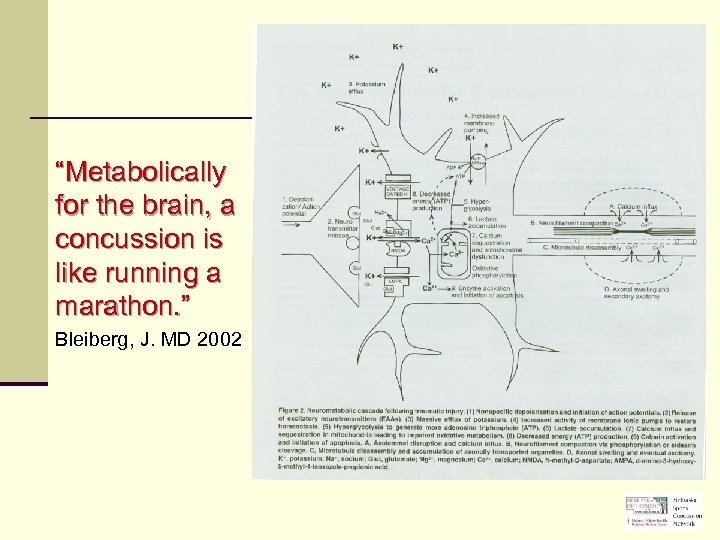 “Metabolically for the brain, a concussion is like running a marathon. ” Bleiberg, J. MD 2002
“Metabolically for the brain, a concussion is like running a marathon. ” Bleiberg, J. MD 2002
 CONCUSSIONS Neurometabolic Cascade n Indiscriminate release of neurotransmitters n Unchecked ionic fluxes n n K+ efflux huge Ca+ influx n n mitochondrial oxidation activates cell death mechanisms n Neuronal depolarization n Glucose metabolism n cellular energy crisis n cerebral blood flow State of Post. Concussive Vulnerability
CONCUSSIONS Neurometabolic Cascade n Indiscriminate release of neurotransmitters n Unchecked ionic fluxes n n K+ efflux huge Ca+ influx n n mitochondrial oxidation activates cell death mechanisms n Neuronal depolarization n Glucose metabolism n cellular energy crisis n cerebral blood flow State of Post. Concussive Vulnerability
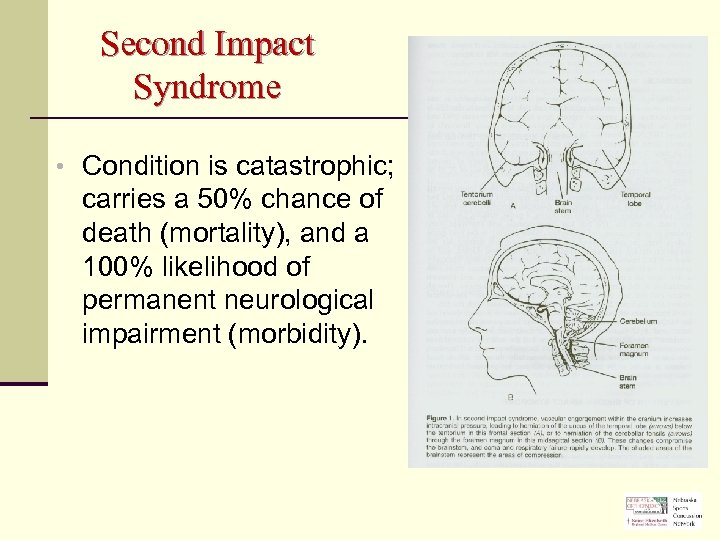 Second Impact Syndrome • Condition is catastrophic; carries a 50% chance of death (mortality), and a 100% likelihood of permanent neurological impairment (morbidity).
Second Impact Syndrome • Condition is catastrophic; carries a 50% chance of death (mortality), and a 100% likelihood of permanent neurological impairment (morbidity).
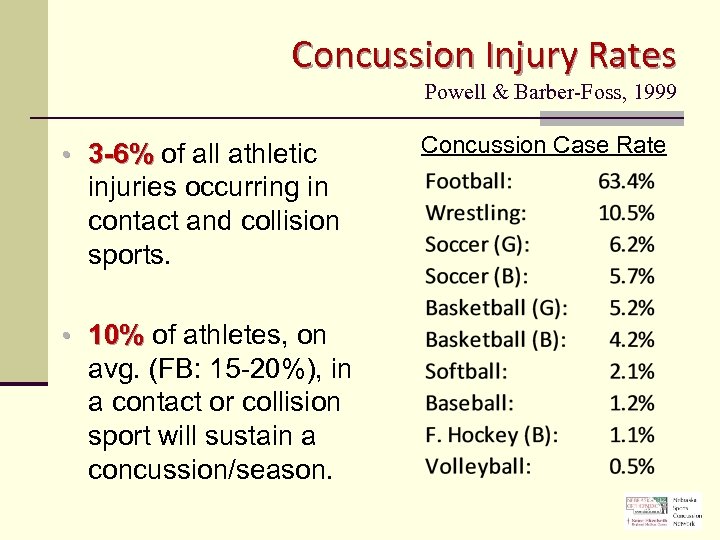 Concussion Injury Rates Powell & Barber-Foss, 1999 • 3 -6% of all athletic injuries occurring in contact and collision sports. • 10% of athletes, on avg. (FB: 15 -20%), in a contact or collision sport will sustain a concussion/season. Concussion Case Rate
Concussion Injury Rates Powell & Barber-Foss, 1999 • 3 -6% of all athletic injuries occurring in contact and collision sports. • 10% of athletes, on avg. (FB: 15 -20%), in a contact or collision sport will sustain a concussion/season. Concussion Case Rate
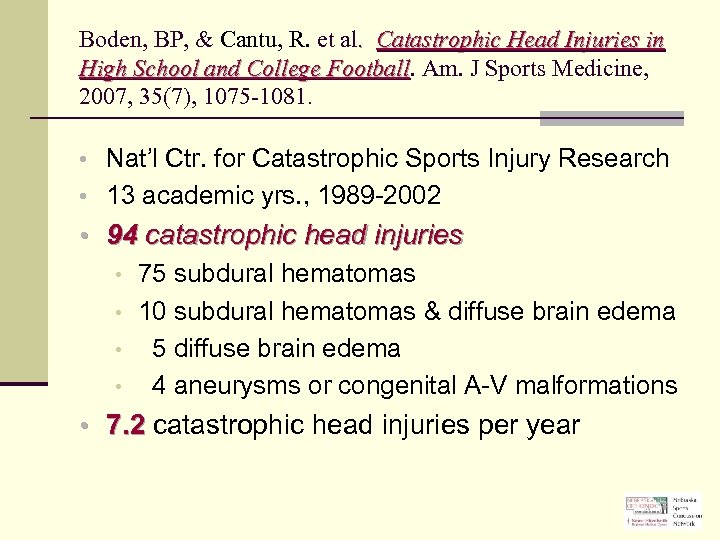 Boden, BP, & Cantu, R. et al. Catastrophic Head Injuries in High School and College Football. Am. J Sports Medicine, Football 2007, 35(7), 1075 -1081. • Nat’l Ctr. for Catastrophic Sports Injury Research • 13 academic yrs. , 1989 -2002 • 94 catastrophic head injuries • 75 subdural hematomas • 10 subdural hematomas & diffuse brain edema • 5 diffuse brain edema • 4 aneurysms or congenital A-V malformations • 7. 2 catastrophic head injuries per year
Boden, BP, & Cantu, R. et al. Catastrophic Head Injuries in High School and College Football. Am. J Sports Medicine, Football 2007, 35(7), 1075 -1081. • Nat’l Ctr. for Catastrophic Sports Injury Research • 13 academic yrs. , 1989 -2002 • 94 catastrophic head injuries • 75 subdural hematomas • 10 subdural hematomas & diffuse brain edema • 5 diffuse brain edema • 4 aneurysms or congenital A-V malformations • 7. 2 catastrophic head injuries per year
 CONCUSSIONS Symptoms • Subtleties of “Symptoms” are not easily identifiable, but are at the core of proper concussion management. • Greater concern for length of time symptoms are present, more so than which ones, or how many – but all 3 remain important to proper assessment & diagnosis of concussion.
CONCUSSIONS Symptoms • Subtleties of “Symptoms” are not easily identifiable, but are at the core of proper concussion management. • Greater concern for length of time symptoms are present, more so than which ones, or how many – but all 3 remain important to proper assessment & diagnosis of concussion.
 CONCUSSIONS Hallmark Signs • Loss of consciousness • Confusion • Disoriented • Unsteady
CONCUSSIONS Hallmark Signs • Loss of consciousness • Confusion • Disoriented • Unsteady
 Severity Grading Scales
Severity Grading Scales
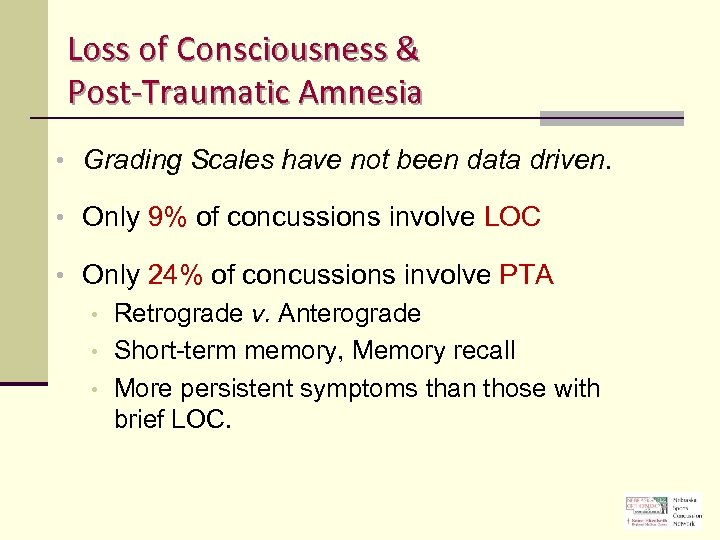 Loss of Consciousness & Post-Traumatic Amnesia • Grading Scales have not been data driven. • Only 9% of concussions involve LOC • Only 24% of concussions involve PTA • Retrograde v. Anterograde • Short-term memory, Memory recall • More persistent symptoms than those with brief LOC.
Loss of Consciousness & Post-Traumatic Amnesia • Grading Scales have not been data driven. • Only 9% of concussions involve LOC • Only 24% of concussions involve PTA • Retrograde v. Anterograde • Short-term memory, Memory recall • More persistent symptoms than those with brief LOC.
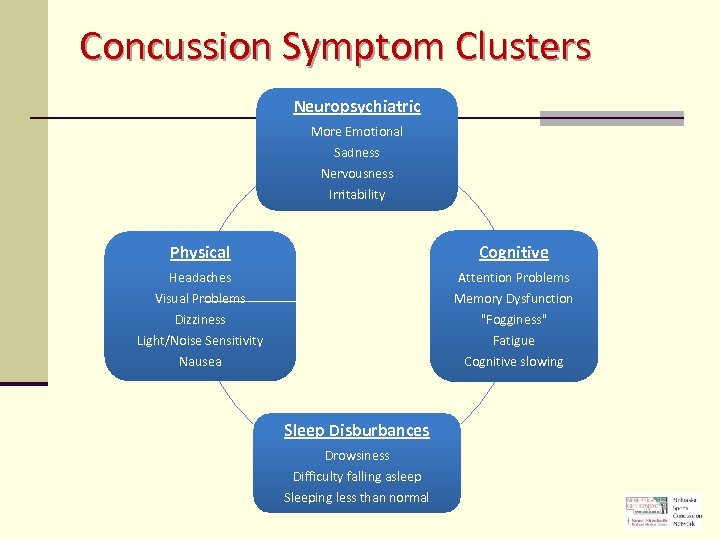 Concussion Symptom Clusters Neuropsychiatric More Emotional Sadness Nervousness Irritability Physical Cognitive Headaches Attention Problems Visual Problems Dizziness Light/Noise Sensitivity Nausea Memory Dysfunction "Fogginess" Fatigue Cognitive slowing Sleep Disburbances Drowsiness Difficulty falling asleep Sleeping less than normal
Concussion Symptom Clusters Neuropsychiatric More Emotional Sadness Nervousness Irritability Physical Cognitive Headaches Attention Problems Visual Problems Dizziness Light/Noise Sensitivity Nausea Memory Dysfunction "Fogginess" Fatigue Cognitive slowing Sleep Disburbances Drowsiness Difficulty falling asleep Sleeping less than normal
![CONCUSSIONS Symptoms – Reported by Athlete [50%] • Prior History (risk factor) • Feeling CONCUSSIONS Symptoms – Reported by Athlete [50%] • Prior History (risk factor) • Feeling](https://present5.com/presentation/9c0cdc7b463c8b23188bc39b2b690d8d/image-26.jpg) CONCUSSIONS Symptoms – Reported by Athlete [50%] • Prior History (risk factor) • Feeling like in a “fog” • Headache • Difficulty • Nausea • Balance Problem/ • Dizziness • Fatigue • Drowsiness • Blurred vision • • • concentrating Difficulty remembering Sensitivity to light Sensitivity to noise Feeling slowed down
CONCUSSIONS Symptoms – Reported by Athlete [50%] • Prior History (risk factor) • Feeling like in a “fog” • Headache • Difficulty • Nausea • Balance Problem/ • Dizziness • Fatigue • Drowsiness • Blurred vision • • • concentrating Difficulty remembering Sensitivity to light Sensitivity to noise Feeling slowed down
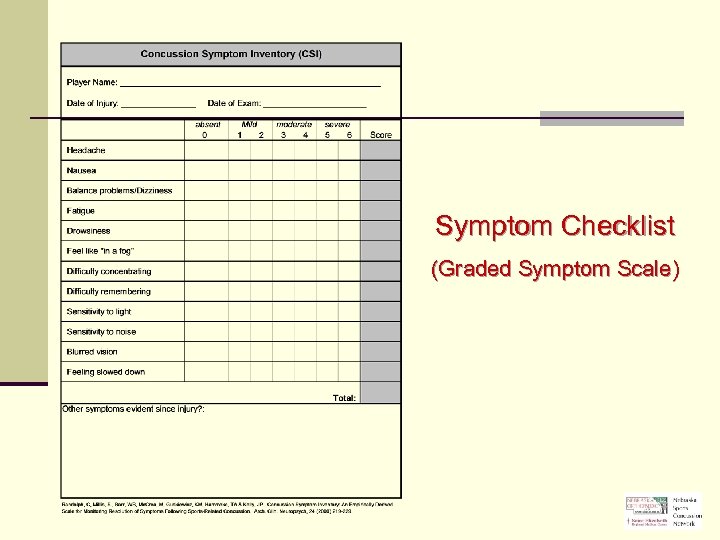 Symptom Checklist (Graded Symptom Scale)
Symptom Checklist (Graded Symptom Scale)
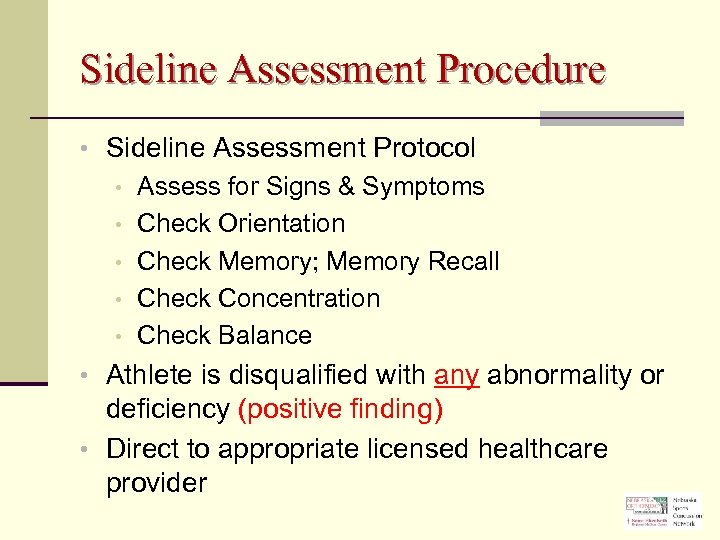 Sideline Assessment Procedure • Sideline Assessment Protocol • Assess for Signs & Symptoms • Check Orientation • Check Memory; Memory Recall • Check Concentration • Check Balance • Athlete is disqualified with any abnormality or deficiency (positive finding) • Direct to appropriate licensed healthcare provider
Sideline Assessment Procedure • Sideline Assessment Protocol • Assess for Signs & Symptoms • Check Orientation • Check Memory; Memory Recall • Check Concentration • Check Balance • Athlete is disqualified with any abnormality or deficiency (positive finding) • Direct to appropriate licensed healthcare provider
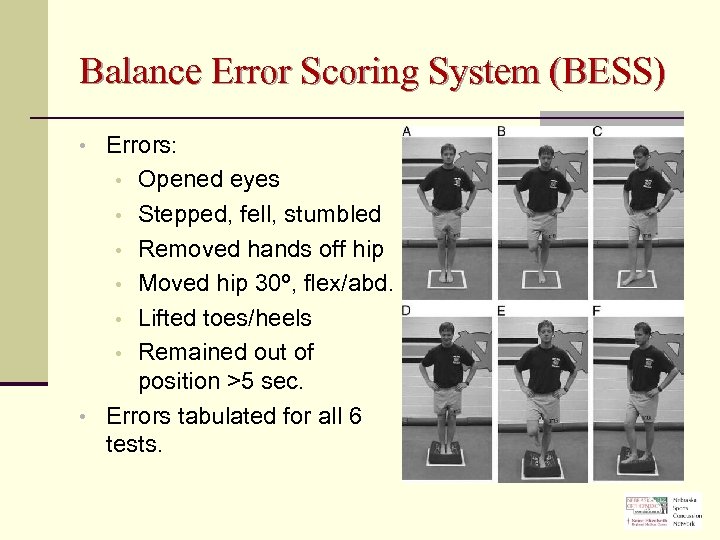 Balance Error Scoring System (BESS) • Errors: Opened eyes • Stepped, fell, stumbled • Removed hands off hip • Moved hip 30º, flex/abd. • Lifted toes/heels • Remained out of position >5 sec. • Errors tabulated for all 6 tests. •
Balance Error Scoring System (BESS) • Errors: Opened eyes • Stepped, fell, stumbled • Removed hands off hip • Moved hip 30º, flex/abd. • Lifted toes/heels • Remained out of position >5 sec. • Errors tabulated for all 6 tests. •
 CONCUSSIONS No universal agreement on Grading Scales or Management Protocol. Unanimous agreement that an athlete with post-concussion symptoms does not return to play contact/collision sports.
CONCUSSIONS No universal agreement on Grading Scales or Management Protocol. Unanimous agreement that an athlete with post-concussion symptoms does not return to play contact/collision sports.
 Know who you’re dealing with Type A - Warrior n “…they’ll have to drag me off the field before I stop playing – I’M FINE!!!” Type B – Drama Queen n “My mom and dad made me go out. I hate playing… I’m looking for a way out… make it look like I have a concussion”.
Know who you’re dealing with Type A - Warrior n “…they’ll have to drag me off the field before I stop playing – I’M FINE!!!” Type B – Drama Queen n “My mom and dad made me go out. I hate playing… I’m looking for a way out… make it look like I have a concussion”.
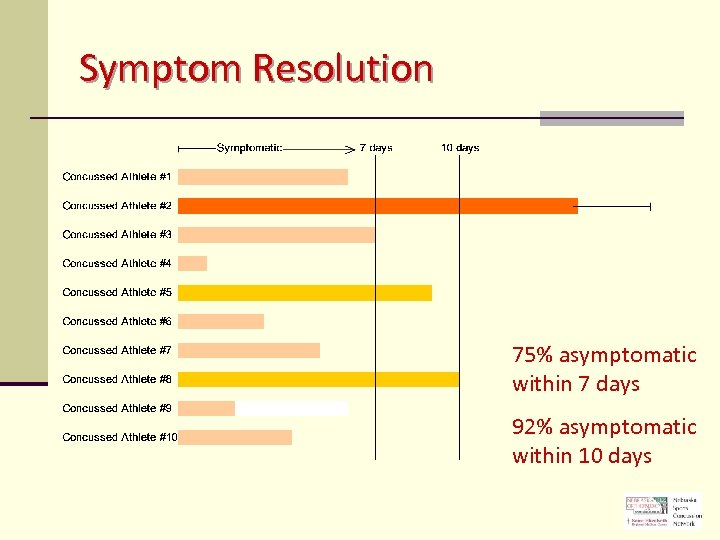 Symptom Resolution 75% asymptomatic within 7 days 92% asymptomatic within 10 days
Symptom Resolution 75% asymptomatic within 7 days 92% asymptomatic within 10 days
 Symptoms vs. Neurocognitive Function • Management & Return to Play (RTP) decisions placing greater emphasis on brain function and the value of Neurocognitive Testing. • Generally, Symptoms tend to resolve before Neurocognitive Brain Function.
Symptoms vs. Neurocognitive Function • Management & Return to Play (RTP) decisions placing greater emphasis on brain function and the value of Neurocognitive Testing. • Generally, Symptoms tend to resolve before Neurocognitive Brain Function.
 (Neuro)Cognitive Function • Concentration • Memory • Short-term • Delayed Recall • Reaction Time • Attention Span • Processing Speed
(Neuro)Cognitive Function • Concentration • Memory • Short-term • Delayed Recall • Reaction Time • Attention Span • Processing Speed
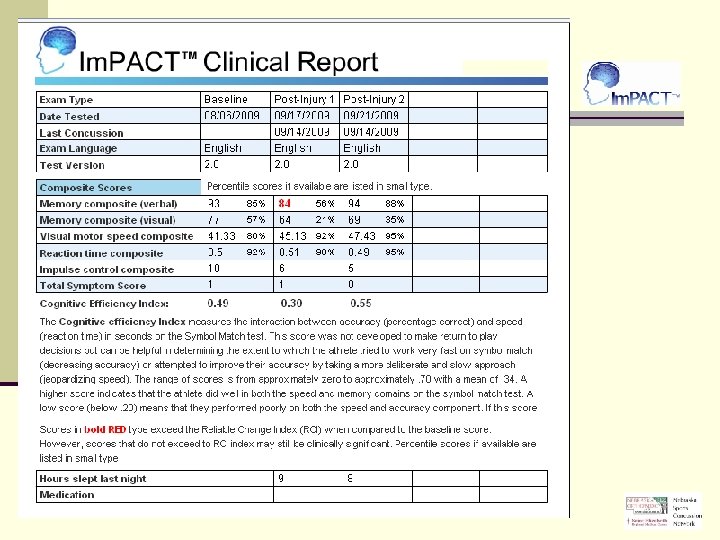
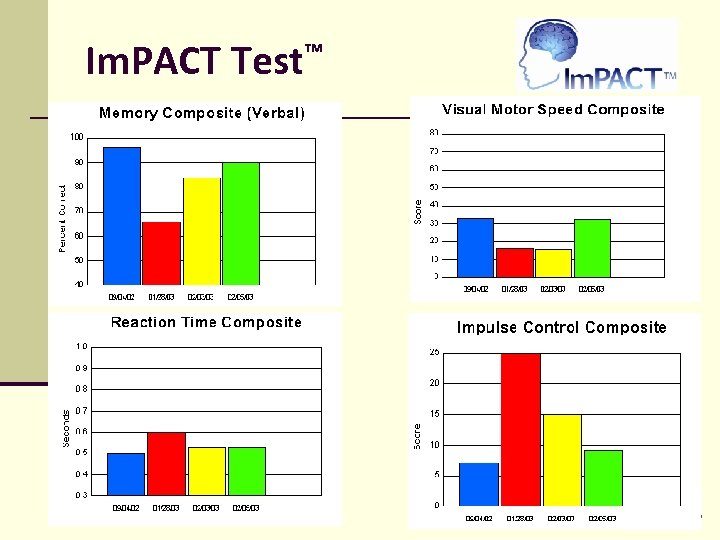
 Neurocognitive Testing • Computerized application (on-line) • Evaluation of multiple aspects of brain function: • Memory, Attention, Processing Speed, Reaction Time, Concentration • “Snapshot” of brain function. • Pre-Injury v. Post-Injury Test Comparison • Valid, objective, more consistent, safer concussion management and RTP decisions.
Neurocognitive Testing • Computerized application (on-line) • Evaluation of multiple aspects of brain function: • Memory, Attention, Processing Speed, Reaction Time, Concentration • “Snapshot” of brain function. • Pre-Injury v. Post-Injury Test Comparison • Valid, objective, more consistent, safer concussion management and RTP decisions.
 Neurocognitive Testing Baseline Testing • Preseason testing under normal conditions prior to injury. • Testing conducted online in computer labs at schools by school staff. • Testing completed in ~25 minutes; multiple users to be tested at same time. • Baseline data saved on secure server and accessed if an athlete sustains a head injury requiring post-injury testing.
Neurocognitive Testing Baseline Testing • Preseason testing under normal conditions prior to injury. • Testing conducted online in computer labs at schools by school staff. • Testing completed in ~25 minutes; multiple users to be tested at same time. • Baseline data saved on secure server and accessed if an athlete sustains a head injury requiring post-injury testing.
 Neurocognitive Testing Post-Injury Testing • If an athlete sustains a concussion, they are tested again, 24 -72 hrs. s/p injury, or upon being asymptomatic. • Post-injury testing is conducted by a trained physician, Neuropsych. , or school’s ATC. • Post-injury test data are compared to preinjury baseline data. • Once post-injury test scores return to baseline (normal), athlete may RTP*.
Neurocognitive Testing Post-Injury Testing • If an athlete sustains a concussion, they are tested again, 24 -72 hrs. s/p injury, or upon being asymptomatic. • Post-injury testing is conducted by a trained physician, Neuropsych. , or school’s ATC. • Post-injury test data are compared to preinjury baseline data. • Once post-injury test scores return to baseline (normal), athlete may RTP*.
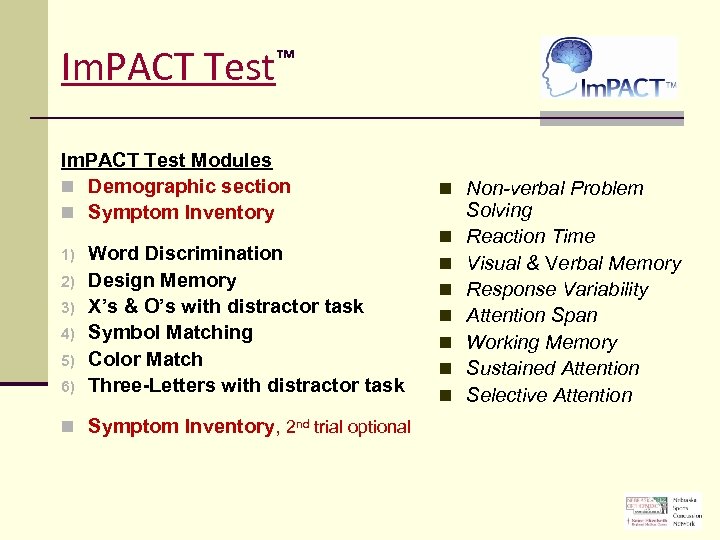 Im. PACT ™ Test Im. PACT Test Modules n Demographic section n Symptom Inventory 1) 2) 3) 4) 5) 6) Word Discrimination Design Memory X’s & O’s with distractor task Symbol Matching Color Match Three-Letters with distractor task n Symptom Inventory, 2 nd trial optional n Non-verbal Problem n n n n Solving Reaction Time Visual & Verbal Memory Response Variability Attention Span Working Memory Sustained Attention Selective Attention
Im. PACT ™ Test Im. PACT Test Modules n Demographic section n Symptom Inventory 1) 2) 3) 4) 5) 6) Word Discrimination Design Memory X’s & O’s with distractor task Symbol Matching Color Match Three-Letters with distractor task n Symptom Inventory, 2 nd trial optional n Non-verbal Problem n n n n Solving Reaction Time Visual & Verbal Memory Response Variability Attention Span Working Memory Sustained Attention Selective Attention
 Im. PACT Test™
Im. PACT Test™
 Return to Play Criteria • • Symptom-Free at Rest Symptom-free with Cognitive/Physical Exertion Stepwise RTP Progression Normal Neurocognitive Data
Return to Play Criteria • • Symptom-Free at Rest Symptom-free with Cognitive/Physical Exertion Stepwise RTP Progression Normal Neurocognitive Data
 Stepwise Return to Play Progression 1. Complete Rest while symptomatic • Physical & Cognitive Rest 2. Begin light, aerobic activity (15 -20 min. ) • Bike, Walk, Swim; no wt. lifting 3. Sport/Position conditioning drills (30 -45 min. ) 4. Non-Contact practice (physician authorization) 5. Full, unrestricted practice 6. Competition
Stepwise Return to Play Progression 1. Complete Rest while symptomatic • Physical & Cognitive Rest 2. Begin light, aerobic activity (15 -20 min. ) • Bike, Walk, Swim; no wt. lifting 3. Sport/Position conditioning drills (30 -45 min. ) 4. Non-Contact practice (physician authorization) 5. Full, unrestricted practice 6. Competition
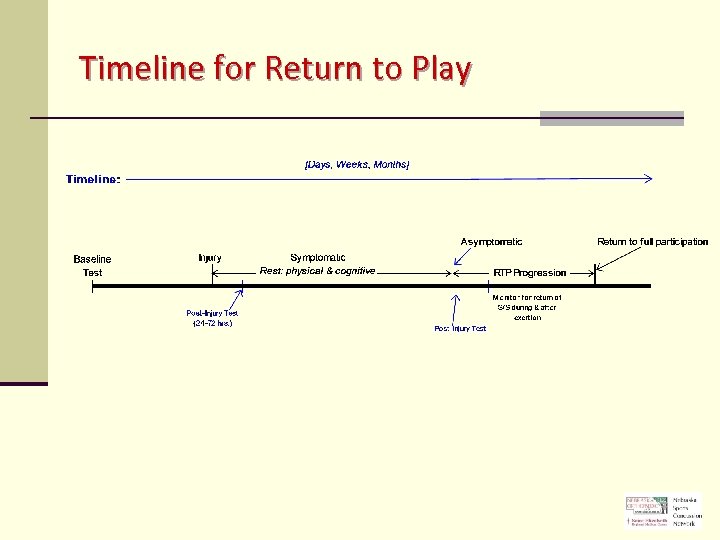 Timeline for Return to Play
Timeline for Return to Play
 Take Home • FAR/coach’s role is to “RECOGNIZE” potential for head injury. • If any S/S are noted, FAR/coach removes athlete. “The End – period. ” Out of coach’s or player’s hands. • Coaches should never render their own decision for RTP involving a concussed athlete or one suspected of having a concussion, without written authorization from appropriate licensed healthcare professional.
Take Home • FAR/coach’s role is to “RECOGNIZE” potential for head injury. • If any S/S are noted, FAR/coach removes athlete. “The End – period. ” Out of coach’s or player’s hands. • Coaches should never render their own decision for RTP involving a concussed athlete or one suspected of having a concussion, without written authorization from appropriate licensed healthcare professional.
 Return to Play • Schools/Athletic Training Staff retain the responsibility to disqualify any athlete’s RTP in the presence of note from anyone that clears an athlete that remains symptomatic. 1. Symptom-Free, during exertion. 2. Neurocognitive Test scores return to normal. 3. Athlete completes RTP Progression before resuming play.
Return to Play • Schools/Athletic Training Staff retain the responsibility to disqualify any athlete’s RTP in the presence of note from anyone that clears an athlete that remains symptomatic. 1. Symptom-Free, during exertion. 2. Neurocognitive Test scores return to normal. 3. Athlete completes RTP Progression before resuming play.
 Nebraska Sports Concussion Network • Nebraska Orthopaedic & Sports Medicine, PC • Saint Elizabeth Regional Medical Center • Medical Director, Daniel Tomes, MD • 100+ Credentialed Im. PACT Consultants • Regional Sponsors & Medical Communities • 80+ High School Athletic Programs • 9, 000+ tests since July 2010
Nebraska Sports Concussion Network • Nebraska Orthopaedic & Sports Medicine, PC • Saint Elizabeth Regional Medical Center • Medical Director, Daniel Tomes, MD • 100+ Credentialed Im. PACT Consultants • Regional Sponsors & Medical Communities • 80+ High School Athletic Programs • 9, 000+ tests since July 2010
 Im. PACT Demo Test www. impacttestonline. com/impactdemo Customer ID: KJZB 2 X 8 FHG (case sensitive)
Im. PACT Demo Test www. impacttestonline. com/impactdemo Customer ID: KJZB 2 X 8 FHG (case sensitive)
 Resources • Nebraska Sports Concussion Network • http: //www. Neb. Sports. Concussion. org/ • Im. PACT Testing Services • http: //www. impacttest. com/
Resources • Nebraska Sports Concussion Network • http: //www. Neb. Sports. Concussion. org/ • Im. PACT Testing Services • http: //www. impacttest. com/
 In Review • • • Recognize that a concussion has occurred. If concussion occurred, stop participation, refer to appropriate healthcare provider Symptom resolution varies widely. While symptomatic, remain at rest, both physically and cognitively. RTP timeframe can not be established in earliest stages of recovery. RTP occurs after all criteria have been met.
In Review • • • Recognize that a concussion has occurred. If concussion occurred, stop participation, refer to appropriate healthcare provider Symptom resolution varies widely. While symptomatic, remain at rest, both physically and cognitively. RTP timeframe can not be established in earliest stages of recovery. RTP occurs after all criteria have been met.
 Questions Patrick E. Clare, MD Ronald O. Schwab, MD Donald J. Walla, MD Thomas. M. Heiser, MD Daniel R. Ripa, MD David J. Clare, MD James W. Gallentine, MD Steven J. Volin, MD Justin D. Harris, MD Scott A. Swanson, MD Daniel B. Cullan II, MD Aaron M. Bott, MD Joseph Mulka, MD
Questions Patrick E. Clare, MD Ronald O. Schwab, MD Donald J. Walla, MD Thomas. M. Heiser, MD Daniel R. Ripa, MD David J. Clare, MD James W. Gallentine, MD Steven J. Volin, MD Justin D. Harris, MD Scott A. Swanson, MD Daniel B. Cullan II, MD Aaron M. Bott, MD Joseph Mulka, MD
 THANK YOU
THANK YOU


