87b17a01c98c0c9ac427ad7440575560.ppt
- Количество слайдов: 46
 Concussion Management and Return to Play 09/10/2010 Cedar Rapids, IA Krishna Prasad Khanal, MBBS, MD
Concussion Management and Return to Play 09/10/2010 Cedar Rapids, IA Krishna Prasad Khanal, MBBS, MD
 Objective n n n Define signs and symptoms of Concussion and sideline evaluation. Management and return to play issues and controversies. Recent Concussion guidelines and consensus statements.
Objective n n n Define signs and symptoms of Concussion and sideline evaluation. Management and return to play issues and controversies. Recent Concussion guidelines and consensus statements.
 Overview n n n Concussions are an important and common injury for athletes. Evaluation, management and RTP decision very challenging. Take home message: must individualize management and RTP decision.
Overview n n n Concussions are an important and common injury for athletes. Evaluation, management and RTP decision very challenging. Take home message: must individualize management and RTP decision.
 Definition n n Vienna Guidelines (Johnston ’ 01) Complex patho-physiological process affecting brain due to traumatic biomechanical forces. Consensus statement on Concussion, Vienna, 2001
Definition n n Vienna Guidelines (Johnston ’ 01) Complex patho-physiological process affecting brain due to traumatic biomechanical forces. Consensus statement on Concussion, Vienna, 2001
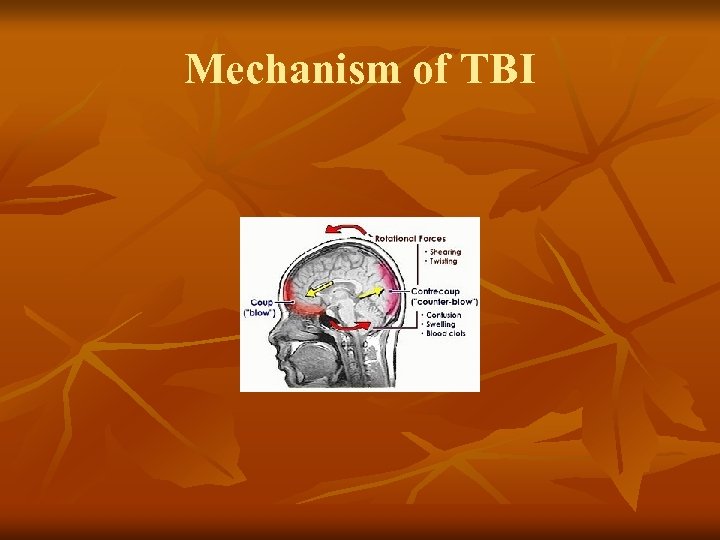 Mechanism of TBI
Mechanism of TBI
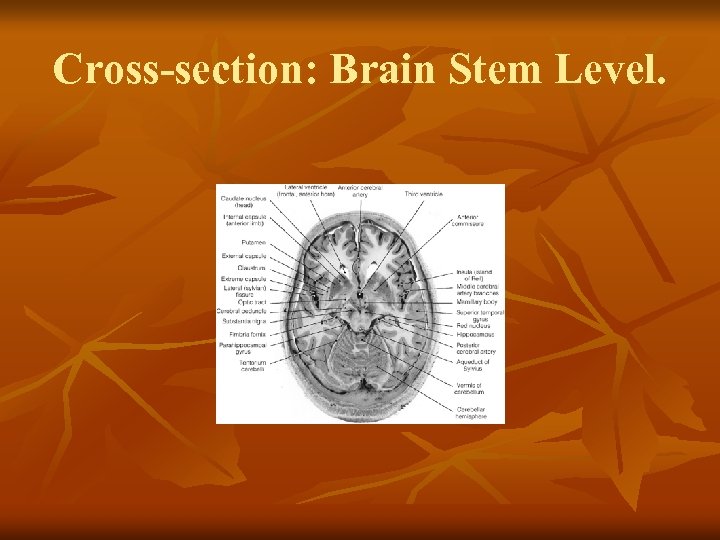 Cross-section: Brain Stem Level.
Cross-section: Brain Stem Level.
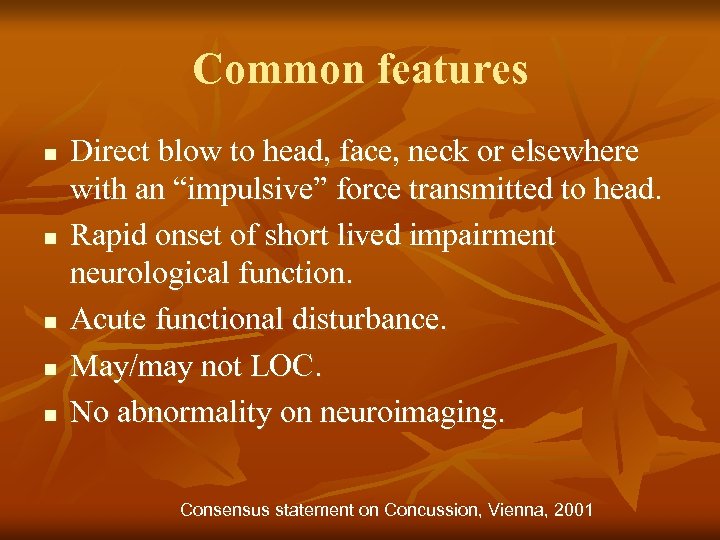 Common features n n n Direct blow to head, face, neck or elsewhere with an “impulsive” force transmitted to head. Rapid onset of short lived impairment neurological function. Acute functional disturbance. May/may not LOC. No abnormality on neuroimaging. Consensus statement on Concussion, Vienna, 2001
Common features n n n Direct blow to head, face, neck or elsewhere with an “impulsive” force transmitted to head. Rapid onset of short lived impairment neurological function. Acute functional disturbance. May/may not LOC. No abnormality on neuroimaging. Consensus statement on Concussion, Vienna, 2001
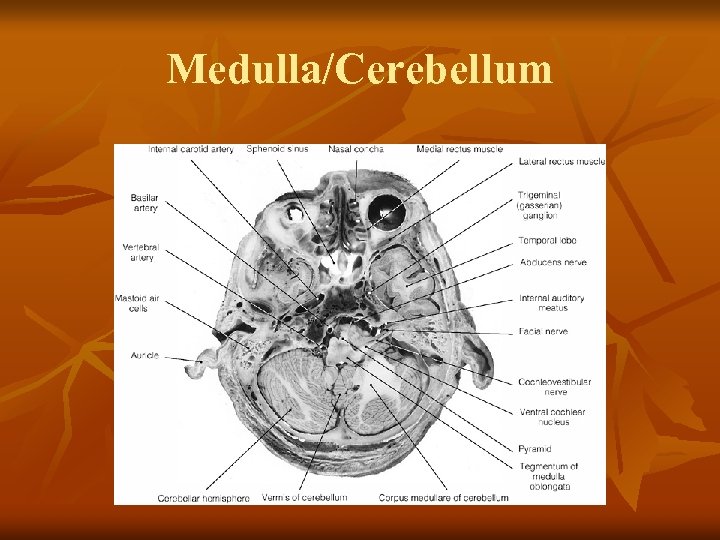 Medulla/Cerebellum
Medulla/Cerebellum
 Pathophysiology n n n Neurochemical and neurometabolic changes Increase in glucose and oxidative metabolism. Increase in demand/Decrease in cerebral blood flow. J. Athl Train. 2001 Jul-Sep; 36(3): 228 -235
Pathophysiology n n n Neurochemical and neurometabolic changes Increase in glucose and oxidative metabolism. Increase in demand/Decrease in cerebral blood flow. J. Athl Train. 2001 Jul-Sep; 36(3): 228 -235
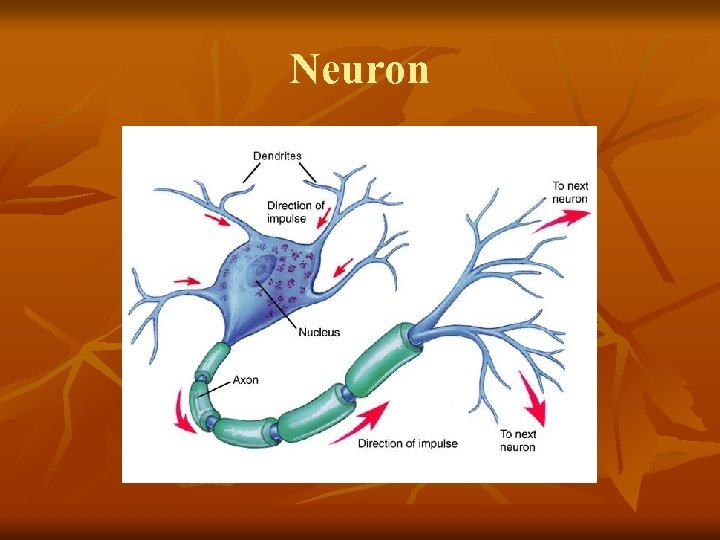 Neuron
Neuron
 Genetics n n Jordan ’ 97; found Apo. E E 4 assoc w/ increased severity of c. TBI in high exposure boxers. College athletes w APOE promoter G-219 T TT genotype may be at an increased risk for having a h/o concussions. Terrell Clin. J Sports Med ’ 08
Genetics n n Jordan ’ 97; found Apo. E E 4 assoc w/ increased severity of c. TBI in high exposure boxers. College athletes w APOE promoter G-219 T TT genotype may be at an increased risk for having a h/o concussions. Terrell Clin. J Sports Med ’ 08
 Epidemiology n n n Increase in diagnosis rate. National High School Federation Data; 20082009: over all total 2. 20 injuries/10, 000 athlete exposures. CDC estimates 1. 1 million persons with TBIs were treated and released from the US hospital ED each year and additional 235, 000 were hospitalized for those injuries. Highest rate among 10 -14 yrs age group. Non-fatal TBI from sports and recreational activities-US, 2001 -2005.
Epidemiology n n n Increase in diagnosis rate. National High School Federation Data; 20082009: over all total 2. 20 injuries/10, 000 athlete exposures. CDC estimates 1. 1 million persons with TBIs were treated and released from the US hospital ED each year and additional 235, 000 were hospitalized for those injuries. Highest rate among 10 -14 yrs age group. Non-fatal TBI from sports and recreational activities-US, 2001 -2005.
 Concussion Signs/Symptoms n n n Somatic: headache, nausea, vomiting, motor problems, fatigue, dizziness, visual disturbance, phonophobia. Affective: Irritability, depression, emotional lability, sleep disturbance, personality disturbance. Cognitive: Confusion, disorientation, RTA, PTA, LOC, feeling “in a fog”, “Zoned out”, vacant stare, inability to focus, decreased processing speed drowsiness etc. Modified from Herring et al, TPCC ’ 06
Concussion Signs/Symptoms n n n Somatic: headache, nausea, vomiting, motor problems, fatigue, dizziness, visual disturbance, phonophobia. Affective: Irritability, depression, emotional lability, sleep disturbance, personality disturbance. Cognitive: Confusion, disorientation, RTA, PTA, LOC, feeling “in a fog”, “Zoned out”, vacant stare, inability to focus, decreased processing speed drowsiness etc. Modified from Herring et al, TPCC ’ 06
 Complications of Brain Injury n n n Cervical spine injury Skull fracture Intracranial hemorrhage Seizures Post-concussion syndrome Second impact Syndrome
Complications of Brain Injury n n n Cervical spine injury Skull fracture Intracranial hemorrhage Seizures Post-concussion syndrome Second impact Syndrome
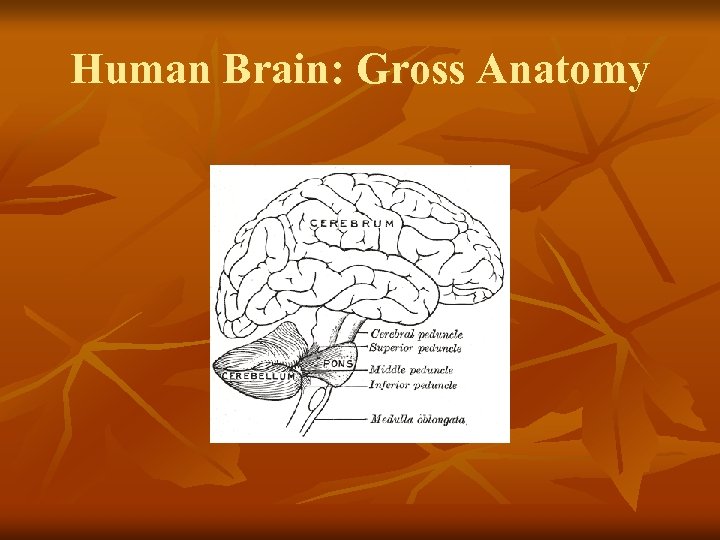 Human Brain: Gross Anatomy
Human Brain: Gross Anatomy
 On-field or Sideline Evaluation n n Medical evaluation: ABCD/R/O structural intracranial lesions. Assessment of concussion using SCAT 2. Monitoring for initial few hrs or send emergently if change in behavior, worsening headache, vomiting, double vision, excessive drowsiness or worsening symptoms. No RTP on day of injury.
On-field or Sideline Evaluation n n Medical evaluation: ABCD/R/O structural intracranial lesions. Assessment of concussion using SCAT 2. Monitoring for initial few hrs or send emergently if change in behavior, worsening headache, vomiting, double vision, excessive drowsiness or worsening symptoms. No RTP on day of injury.
 SCAT 2 n n Calculated for athlete>10 yo. Preseason baseline testing can be helpful. Calculated based on symptoms, physical signs, GCS, balance examination, coordination, orientation, immediate memory, concentration, delayed recall scores. No cut off value on SCAT 2 score. Clin J of Sports Medicine, March 2005 -volume 15 -Issue 2 -pp 48 -55 statement.
SCAT 2 n n Calculated for athlete>10 yo. Preseason baseline testing can be helpful. Calculated based on symptoms, physical signs, GCS, balance examination, coordination, orientation, immediate memory, concentration, delayed recall scores. No cut off value on SCAT 2 score. Clin J of Sports Medicine, March 2005 -volume 15 -Issue 2 -pp 48 -55 statement.
 Neuroimaging CT/MRI 1. Prolonged disturbance of conscious state. 2. Focal neurological deficit. 3. Worsening symptoms. n n Role of f. MRI/PET
Neuroimaging CT/MRI 1. Prolonged disturbance of conscious state. 2. Focal neurological deficit. 3. Worsening symptoms. n n Role of f. MRI/PET
 Evaluation in ED or office n n n Comprehensive history, detailed physical examination. Determination of the progression since the time of injury. Determination of the need for emergent neuroimaging.
Evaluation in ED or office n n n Comprehensive history, detailed physical examination. Determination of the progression since the time of injury. Determination of the need for emergent neuroimaging.
 Severity of Injury n n Related to the burden, nature and duration of symptoms. Modifiers (Zurich ’ 09) 1. Age 2. Prior h/o concussion 3. Learning disability 4. Headache/migraine history.
Severity of Injury n n Related to the burden, nature and duration of symptoms. Modifiers (Zurich ’ 09) 1. Age 2. Prior h/o concussion 3. Learning disability 4. Headache/migraine history.
 Objective Balance Assessment n n n Balance error scoring system (BESS) For the assessment of motor domain of neurological functioning. Postural instability: communication between three sensory systems either at central or peripheral level is lost. Clinical J. Sports Med. 2001; 11: 182 -190
Objective Balance Assessment n n n Balance error scoring system (BESS) For the assessment of motor domain of neurological functioning. Postural instability: communication between three sensory systems either at central or peripheral level is lost. Clinical J. Sports Med. 2001; 11: 182 -190
 Neuropsychological testing n n n Evaluate brain behavior relationships. Sensitive in assessment of brain injury. Unique contribution and RTP of concussed athlete. Newer computerized test batteries. Validated testing. Protocols for using NP as part of “concussion plan” evolving. Neurosurgery 2004; 54: 1073 -1078; discussion, 8 -80
Neuropsychological testing n n n Evaluate brain behavior relationships. Sensitive in assessment of brain injury. Unique contribution and RTP of concussed athlete. Newer computerized test batteries. Validated testing. Protocols for using NP as part of “concussion plan” evolving. Neurosurgery 2004; 54: 1073 -1078; discussion, 8 -80
 Concussion Assessment Modalities n n Evoked response potential (ERP) Cortical magnetic stimulation Electroencephalography Biochemical and CSF markers of brain injury. J. Neurotrauma, 2006; 23: 1201 -1210
Concussion Assessment Modalities n n Evoked response potential (ERP) Cortical magnetic stimulation Electroencephalography Biochemical and CSF markers of brain injury. J. Neurotrauma, 2006; 23: 1201 -1210
 Management n n Physical and cognitive rest until symptom resolves and then graded program of exertion prior to medical clearance and RTP. Activities that require concentration and attention may delay recovery. Current Sports Medicine Reports. 2004; 3: 316 -323
Management n n Physical and cognitive rest until symptom resolves and then graded program of exertion prior to medical clearance and RTP. Activities that require concentration and attention may delay recovery. Current Sports Medicine Reports. 2004; 3: 316 -323
 Graduated return to play protocol Rehabilitation stage Functional Exercise 1. No activity Complete rest 2. Light aerobic exercise No resistance 3. Sport specific exercise No head impact 4. Non-contact Progressive resistance 5. Full contact Normal training 6. RTP Normal game play Consensus statement, 3 rd International Conference, Zurich, 2008.
Graduated return to play protocol Rehabilitation stage Functional Exercise 1. No activity Complete rest 2. Light aerobic exercise No resistance 3. Sport specific exercise No head impact 4. Non-contact Progressive resistance 5. Full contact Normal training 6. RTP Normal game play Consensus statement, 3 rd International Conference, Zurich, 2008.
 Same day RTP n n Young(<18 yo) athlete should be treated more conservatively. Done on adult athletes with good team physician experience and sufficient resources.
Same day RTP n n Young(<18 yo) athlete should be treated more conservatively. Done on adult athletes with good team physician experience and sufficient resources.
 Pharmacology n n n Management of sleep disturbance, anxiety Management of headache, vomiting, dizziness During RTP, the concussed athlete should not only be symptom free but also should not be taking any medications that may mask or modify the symptoms of concussion.
Pharmacology n n n Management of sleep disturbance, anxiety Management of headache, vomiting, dizziness During RTP, the concussed athlete should not only be symptom free but also should not be taking any medications that may mask or modify the symptoms of concussion.
 Pre-participation Concussion Evaluation n Comprehensive structured history. Modification and optimization of protective behavior. Educating high risk athlete.
Pre-participation Concussion Evaluation n Comprehensive structured history. Modification and optimization of protective behavior. Educating high risk athlete.
 Modifying Factors in Concussion Management n n n May need additional management considerations. Symptoms, signs, sequelae, temporal, threshold. Age, co and premorbidities, medication, behavior, type of sports. Consensus statement 3 rd International Conference, Zurich, Nov. 2008.
Modifying Factors in Concussion Management n n n May need additional management considerations. Symptoms, signs, sequelae, temporal, threshold. Age, co and premorbidities, medication, behavior, type of sports. Consensus statement 3 rd International Conference, Zurich, Nov. 2008.
 Significance of LOC/Amnesia n n LOC>1 min duration may modify management and predictor of the outcome. RTA poorly reflective of injury severity. Neurology, 1973; 23: 196 -197
Significance of LOC/Amnesia n n LOC>1 min duration may modify management and predictor of the outcome. RTA poorly reflective of injury severity. Neurology, 1973; 23: 196 -197
 Depression n Common diagnosis Long term consequence Should be part of comprehensive history/patient and care taker education. Injury. 2008; 39: 604 -611
Depression n Common diagnosis Long term consequence Should be part of comprehensive history/patient and care taker education. Injury. 2008; 39: 604 -611
 Child and Adolescent Athlete n n n Role of both patient and parent input as well as teacher and school input when appropriate. * Developmentally sensitive cognitive test. ** Role of trained neuro-psychologist more important to interpret assessment data. *** Complete symptom free before RTP. Limitation of cognitive stressors. *Clinic Pediatric(Phila). 2008; 47: 106 -113 **J. Athl Train. 2008; 43: 456 -463 ***Br J Sports Med. 2004; 38: 657
Child and Adolescent Athlete n n n Role of both patient and parent input as well as teacher and school input when appropriate. * Developmentally sensitive cognitive test. ** Role of trained neuro-psychologist more important to interpret assessment data. *** Complete symptom free before RTP. Limitation of cognitive stressors. *Clinic Pediatric(Phila). 2008; 47: 106 -113 **J. Athl Train. 2008; 43: 456 -463 ***Br J Sports Med. 2004; 38: 657
 Elite vs. non-Elite Athlete n All athletes regardless of level of participation should be managed using same treatment and RTP paradigm.
Elite vs. non-Elite Athlete n All athletes regardless of level of participation should be managed using same treatment and RTP paradigm.
 Chronic Traumatic Brain Injury n Repeated sports concussion and late life cognitive impairment.
Chronic Traumatic Brain Injury n Repeated sports concussion and late life cognitive impairment.
 Vienna Guidelines n n n Modern definition of concussion. Concept of NP testing as “cornerstone” of evaluation. No RTP on same day. Medical evaluation for all concussions. Progression from no activity to game play with six stages; 24 hrs for each stage. Aubrey ’ 02
Vienna Guidelines n n n Modern definition of concussion. Concept of NP testing as “cornerstone” of evaluation. No RTP on same day. Medical evaluation for all concussions. Progression from no activity to game play with six stages; 24 hrs for each stage. Aubrey ’ 02
 Prague Guidelines n n n SCAT No same day RTP. Simple vs. complex concussion. Use of NP only for complex concussion. Same stepwise progression. Mc. Crory ’ 05
Prague Guidelines n n n SCAT No same day RTP. Simple vs. complex concussion. Use of NP only for complex concussion. Same stepwise progression. Mc. Crory ’ 05
 Team Physician Consensus Conference* n n Symptomatic athlete should not return to play. Same day RTP controversial. Safest course of action: hold an athlete. Consider additional factors in RTP: 1. Severity of injury. 2. Previous injury (no, severity, proximity). 3. Significant injury to minor blow. 4. Age, sport, learning disabilities. Herring et al, ’ 05, ’ 06 *Collaboration of ACSM, AMSSM, AOSSM, AAOS, AAFP,
Team Physician Consensus Conference* n n Symptomatic athlete should not return to play. Same day RTP controversial. Safest course of action: hold an athlete. Consider additional factors in RTP: 1. Severity of injury. 2. Previous injury (no, severity, proximity). 3. Significant injury to minor blow. 4. Age, sport, learning disabilities. Herring et al, ’ 05, ’ 06 *Collaboration of ACSM, AMSSM, AOSSM, AAOS, AAFP,
 Zurich Consensus Statement n n n Simple vs. complex eliminated. Individualized RTP. Differentiation of elite vs. non-elite. Modifiers Same day RTP in very specific situations for adult athlete.
Zurich Consensus Statement n n n Simple vs. complex eliminated. Individualized RTP. Differentiation of elite vs. non-elite. Modifiers Same day RTP in very specific situations for adult athlete.
 Return to play: Controversies n n n Same day RTP Rate of progression. Role of NP; what tests, timeline of testing, who interprets test.
Return to play: Controversies n n n Same day RTP Rate of progression. Role of NP; what tests, timeline of testing, who interprets test.
 Injury Prevention Helmets and mouth guards 1. Helmeted sports similar to non-helmeted sports re: injury incidence. 2. No helmet in any sports prevents concussion. 3. Mouth guards do not prevent concussion; prevent dental injury. n BMJ. 2005; 330: 281 -283
Injury Prevention Helmets and mouth guards 1. Helmeted sports similar to non-helmeted sports re: injury incidence. 2. No helmet in any sports prevents concussion. 3. Mouth guards do not prevent concussion; prevent dental injury. n BMJ. 2005; 330: 281 -283
 Rule Change n n Rule enforcement may be a critical aspect of modifying injury risk. Role of referees.
Rule Change n n Rule enforcement may be a critical aspect of modifying injury risk. Role of referees.
 Risk Compensation n Paradoxical increase in injury rates due to behavioral change. Clin J Sports Med. 2004; 14: 193 -196.
Risk Compensation n Paradoxical increase in injury rates due to behavioral change. Clin J Sports Med. 2004; 14: 193 -196.
 Aggression vs. Violence n n Address violence that may increase concussion risk. Respect and support fair play. Arch Pediatric Adolesc Med. 2000; 154: 11 -15
Aggression vs. Violence n n Address violence that may increase concussion risk. Respect and support fair play. Arch Pediatric Adolesc Med. 2000; 154: 11 -15
 Future Directions n n n n n How many is too many? Gender effects on injury risk, severity and outcome. Genetics and other factors. Pediatric injury and management paradigms. Rehabilitation strategies (e. g. Exercise therapy). Novel imaging modality: role of f. MRI/DTI. Long term outcomes like depression/suicide. On field injury severity outcomes. Concussion surveillance. Protective factors.
Future Directions n n n n n How many is too many? Gender effects on injury risk, severity and outcome. Genetics and other factors. Pediatric injury and management paradigms. Rehabilitation strategies (e. g. Exercise therapy). Novel imaging modality: role of f. MRI/DTI. Long term outcomes like depression/suicide. On field injury severity outcomes. Concussion surveillance. Protective factors.
 Thank You
Thank You


