a126ef2ade4a81f7dd74b8187a33b903.ppt
- Количество слайдов: 69
 Compartment syndrome and fasciotomy Supparerk Prichayudh, M. D.
Compartment syndrome and fasciotomy Supparerk Prichayudh, M. D.
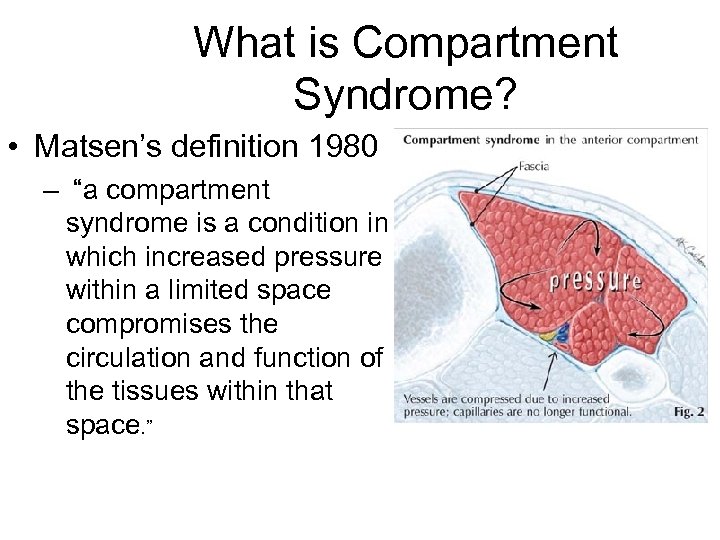 What is Compartment Syndrome? • Matsen’s definition 1980 – “a compartment syndrome is a condition in which increased pressure within a limited space compromises the circulation and function of the tissues within that space. ”
What is Compartment Syndrome? • Matsen’s definition 1980 – “a compartment syndrome is a condition in which increased pressure within a limited space compromises the circulation and function of the tissues within that space. ”
 Where can it occur? • Anywhere there is an enclosed space typically restricted by fascia: – Upper Arm – Forearm – Hand – Thigh – Chest – Abdomen • Raised ICP of the brain
Where can it occur? • Anywhere there is an enclosed space typically restricted by fascia: – Upper Arm – Forearm – Hand – Thigh – Chest – Abdomen • Raised ICP of the brain
 Causes of Compartment Syndrome (Primary) • Fracture of the long bones e. g. Tibia • Crush injuries • Burns Eschar • Lithotomy position • Pneumatic tourniquet • High Injury Trauma • Ischemia/Reperfusion • Penetrating injuries
Causes of Compartment Syndrome (Primary) • Fracture of the long bones e. g. Tibia • Crush injuries • Burns Eschar • Lithotomy position • Pneumatic tourniquet • High Injury Trauma • Ischemia/Reperfusion • Penetrating injuries
 Secondary Extremity Compartment Syndrome • Rare, 0. 08 -0. 148% • part of the post-resuscitation SIRS • significant edema and associated compartment syndromes in 2 to 4 injured or non-injured extremities after massive resuscitation. • Mortality rate 35 -70% • should be suspected in any injured patient who presents with profound hypotension, ISS > 25, transfusion of at least 10 units of PRBC • Rx: early detection and early fasciotomy
Secondary Extremity Compartment Syndrome • Rare, 0. 08 -0. 148% • part of the post-resuscitation SIRS • significant edema and associated compartment syndromes in 2 to 4 injured or non-injured extremities after massive resuscitation. • Mortality rate 35 -70% • should be suspected in any injured patient who presents with profound hypotension, ISS > 25, transfusion of at least 10 units of PRBC • Rx: early detection and early fasciotomy
 Pathophysiology Tissue Injury + Tissue Ischemia +Tissue Reperfusion Cellular injury & Tissue swelling ↑ compartment pressure Compartment syndrome
Pathophysiology Tissue Injury + Tissue Ischemia +Tissue Reperfusion Cellular injury & Tissue swelling ↑ compartment pressure Compartment syndrome
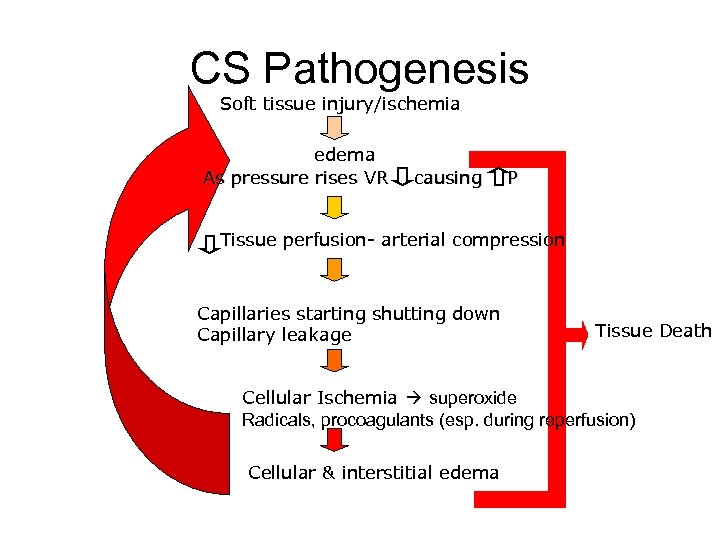 CS Pathogenesis Soft tissue injury/ischemia edema As pressure rises VR causing P Tissue perfusion- arterial compression Capillaries starting shutting down Capillary leakage Tissue Death Cellular Ischemia superoxide Radicals, procoagulants (esp. during reperfusion) Cellular & interstitial edema
CS Pathogenesis Soft tissue injury/ischemia edema As pressure rises VR causing P Tissue perfusion- arterial compression Capillaries starting shutting down Capillary leakage Tissue Death Cellular Ischemia superoxide Radicals, procoagulants (esp. during reperfusion) Cellular & interstitial edema
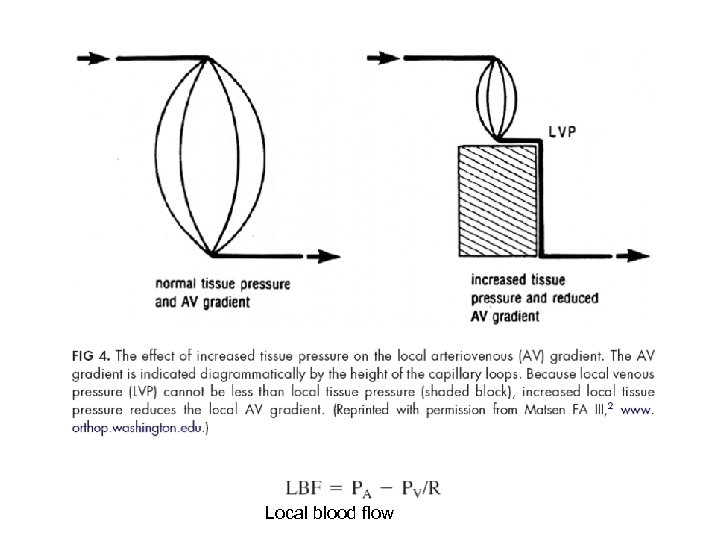 Local blood flow
Local blood flow
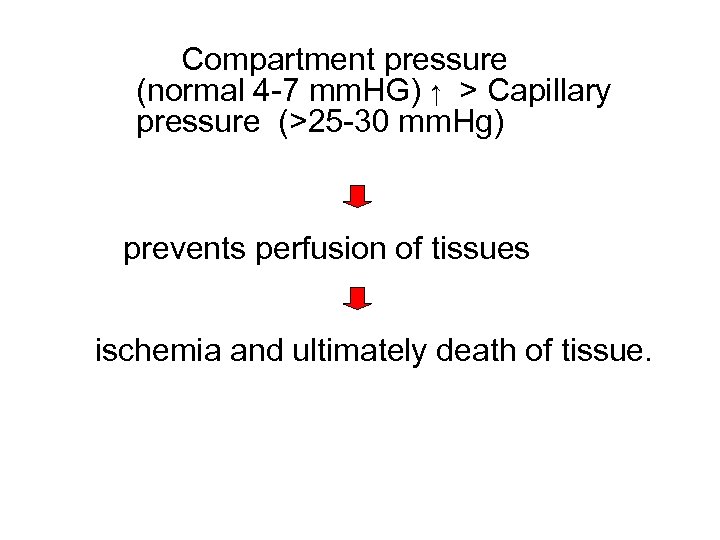 Compartment pressure (normal 4 -7 mm. HG) ↑ > Capillary pressure (>25 -30 mm. Hg) prevents perfusion of tissues ischemia and ultimately death of tissue.
Compartment pressure (normal 4 -7 mm. HG) ↑ > Capillary pressure (>25 -30 mm. Hg) prevents perfusion of tissues ischemia and ultimately death of tissue.
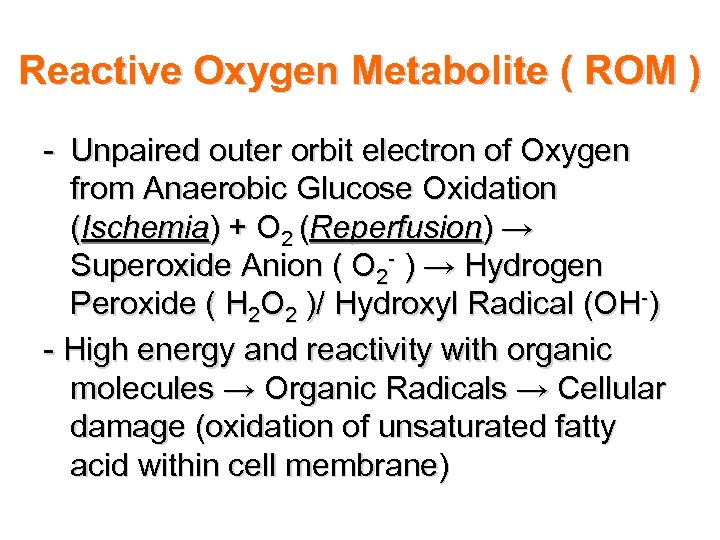 Reactive Oxygen Metabolite ( ROM ) - Unpaired outer orbit electron of Oxygen from Anaerobic Glucose Oxidation (Ischemia) + O 2 (Reperfusion) → Superoxide Anion ( O 2 - ) → Hydrogen Peroxide ( H 2 O 2 )/ Hydroxyl Radical (OH-) - High energy and reactivity with organic molecules → Organic Radicals → Cellular damage (oxidation of unsaturated fatty acid within cell membrane)
Reactive Oxygen Metabolite ( ROM ) - Unpaired outer orbit electron of Oxygen from Anaerobic Glucose Oxidation (Ischemia) + O 2 (Reperfusion) → Superoxide Anion ( O 2 - ) → Hydrogen Peroxide ( H 2 O 2 )/ Hydroxyl Radical (OH-) - High energy and reactivity with organic molecules → Organic Radicals → Cellular damage (oxidation of unsaturated fatty acid within cell membrane)
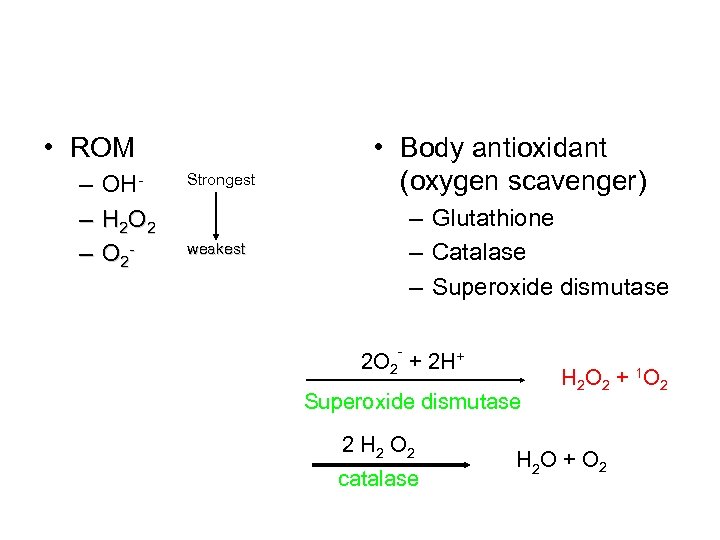 • ROM – OH– H 2 O 2 – O 2 - Strongest • Body antioxidant (oxygen scavenger) – Glutathione – Catalase – Superoxide dismutase weakest - 2 O 2 + 2 H+ Superoxide dismutase 2 H 2 O 2 catalase H 2 O 2 + 1 O 2 H 2 O + O 2
• ROM – OH– H 2 O 2 – O 2 - Strongest • Body antioxidant (oxygen scavenger) – Glutathione – Catalase – Superoxide dismutase weakest - 2 O 2 + 2 H+ Superoxide dismutase 2 H 2 O 2 catalase H 2 O 2 + 1 O 2 H 2 O + O 2
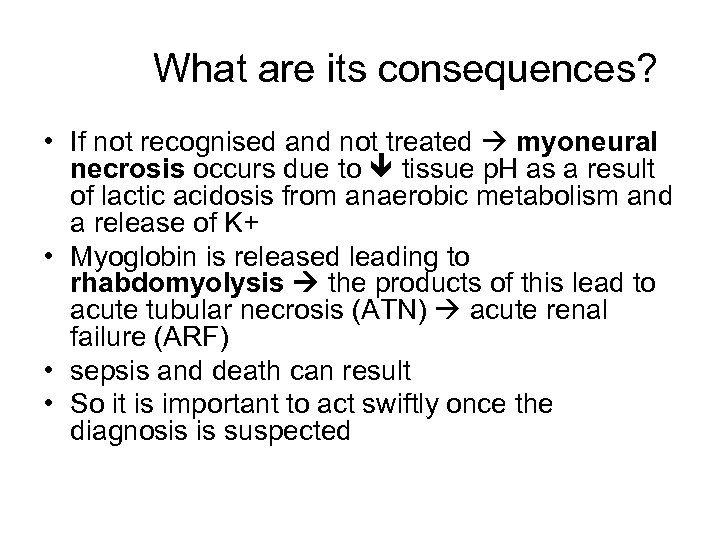 What are its consequences? • If not recognised and not treated myoneural necrosis occurs due to tissue p. H as a result of lactic acidosis from anaerobic metabolism and a release of K+ • Myoglobin is released leading to rhabdomyolysis the products of this lead to acute tubular necrosis (ATN) acute renal failure (ARF) • sepsis and death can result • So it is important to act swiftly once the diagnosis is suspected
What are its consequences? • If not recognised and not treated myoneural necrosis occurs due to tissue p. H as a result of lactic acidosis from anaerobic metabolism and a release of K+ • Myoglobin is released leading to rhabdomyolysis the products of this lead to acute tubular necrosis (ATN) acute renal failure (ARF) • sepsis and death can result • So it is important to act swiftly once the diagnosis is suspected
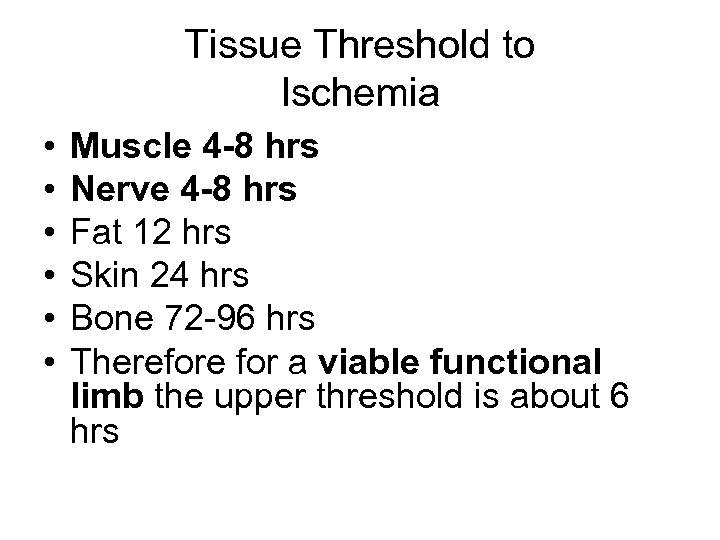 Tissue Threshold to Ischemia • • • Muscle 4 -8 hrs Nerve 4 -8 hrs Fat 12 hrs Skin 24 hrs Bone 72 -96 hrs Therefore for a viable functional limb the upper threshold is about 6 hrs
Tissue Threshold to Ischemia • • • Muscle 4 -8 hrs Nerve 4 -8 hrs Fat 12 hrs Skin 24 hrs Bone 72 -96 hrs Therefore for a viable functional limb the upper threshold is about 6 hrs
 Anatomy
Anatomy
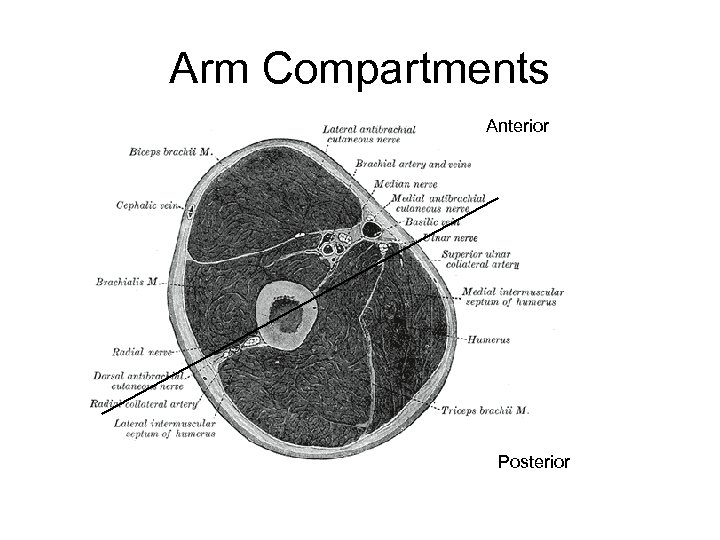 Arm Compartments Anterior Posterior
Arm Compartments Anterior Posterior
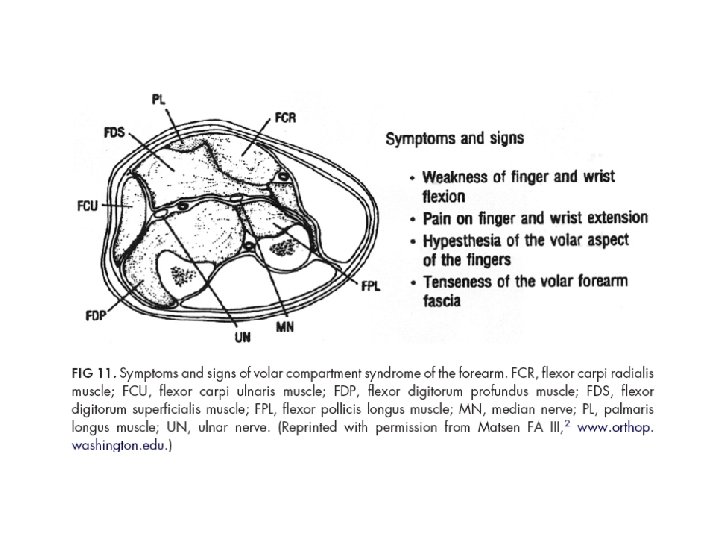
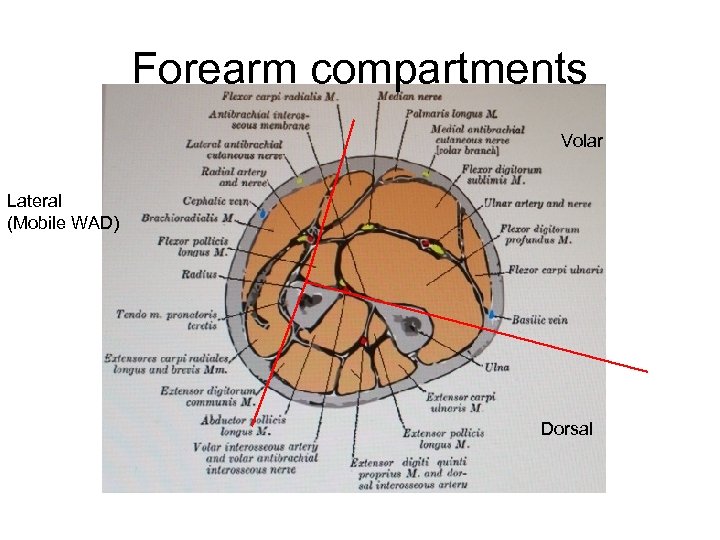 Forearm compartments Volar Lateral (Mobile WAD) Dorsal
Forearm compartments Volar Lateral (Mobile WAD) Dorsal
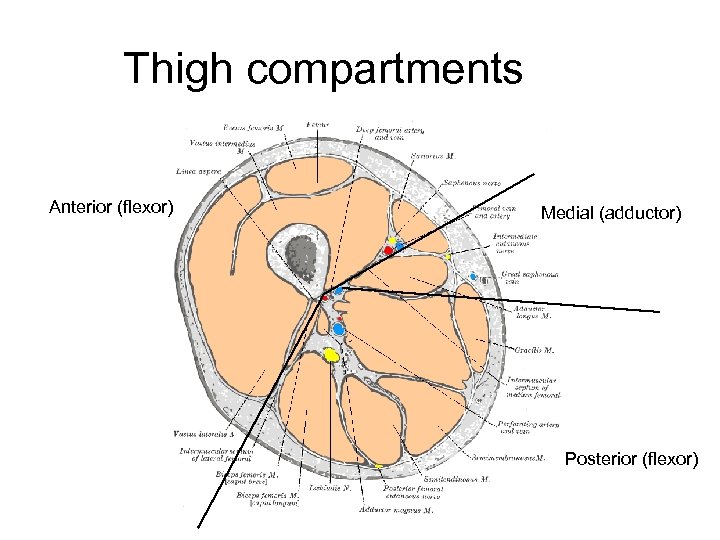 Thigh compartments Anterior (flexor) Medial (adductor) Posterior (flexor)
Thigh compartments Anterior (flexor) Medial (adductor) Posterior (flexor)
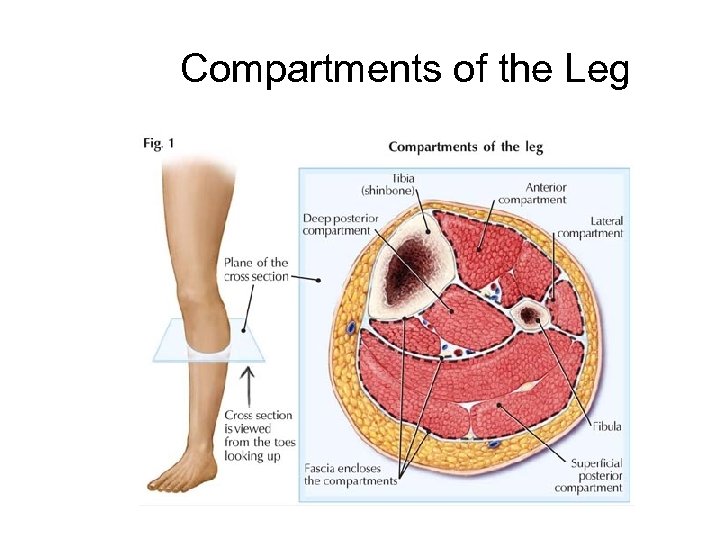 Compartments of the Leg
Compartments of the Leg
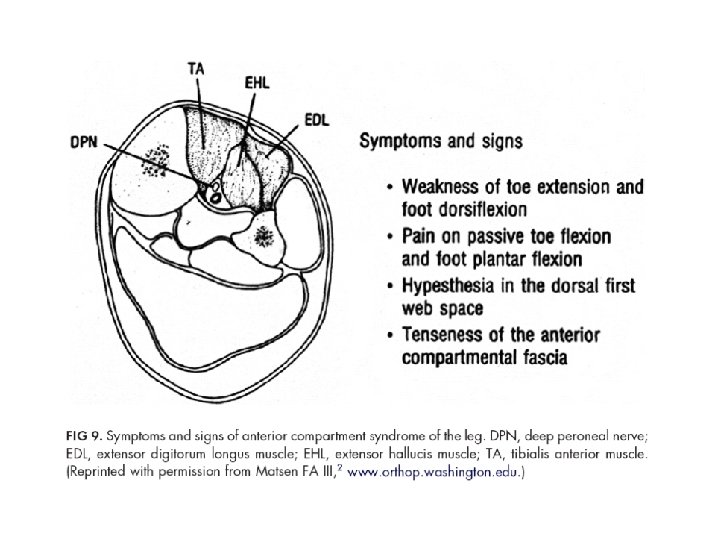
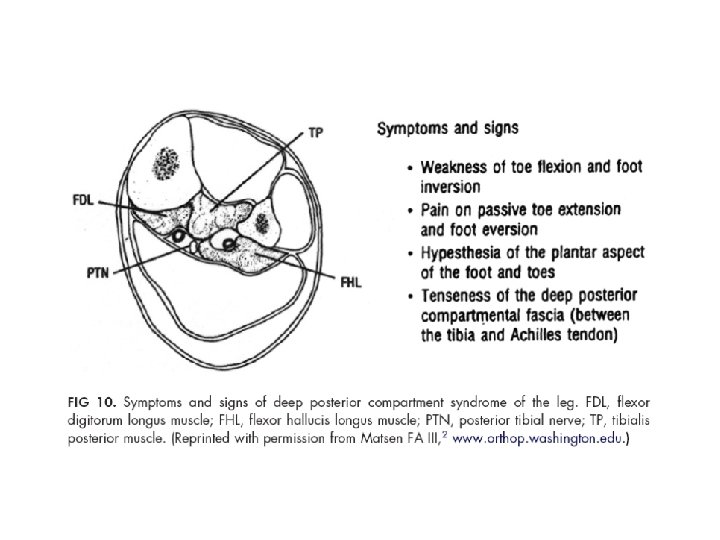
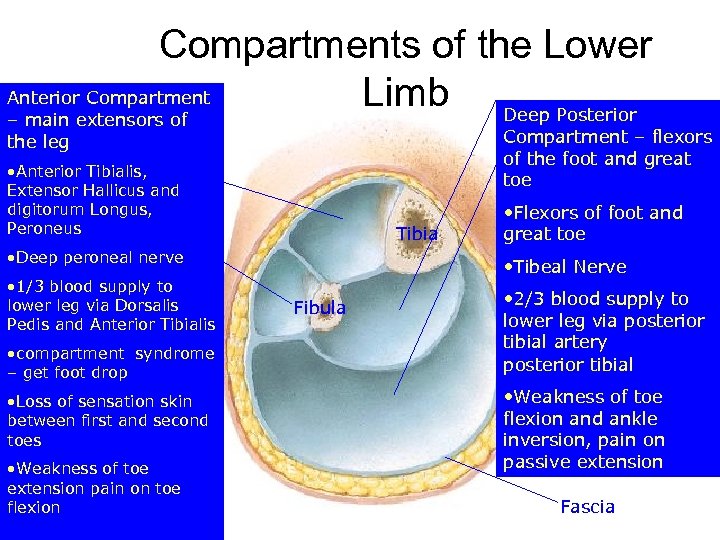 Compartments of the Lower Anterior Compartment Limb Deep Posterior – main extensors of the leg Compartment – flexors Superficial Posterior of the foot and Compartment –great toe superficial flexors • Anterior Tibialis, Lateral Compartment Extensor Hallicus and • Peroneus Longus and digitorum Longus, brevis Peroneus Tibia • Deep peroneal nerve Superficial peroneal nerve • 1/3 blood supply to lower leg via Dorsalis • Plantar flexes foot Pedis and Anterior Tibialis • compartment syndrome – get foot drop • Loss of sensation skin between first and second toes • Weakness of toe extension pain on toe flexion Fibula Flexors of foot • Gastronemius and great toe • Soleus • Tibeal Nerve • Sural & Tibial Nerves • 2/3 blood supply to • Plantar flexors lower leg via posterior tibial artery • Blood supply posterior tibial • Weakness of toe flexion and ankle inversion, pain on passive extension Fascia
Compartments of the Lower Anterior Compartment Limb Deep Posterior – main extensors of the leg Compartment – flexors Superficial Posterior of the foot and Compartment –great toe superficial flexors • Anterior Tibialis, Lateral Compartment Extensor Hallicus and • Peroneus Longus and digitorum Longus, brevis Peroneus Tibia • Deep peroneal nerve Superficial peroneal nerve • 1/3 blood supply to lower leg via Dorsalis • Plantar flexes foot Pedis and Anterior Tibialis • compartment syndrome – get foot drop • Loss of sensation skin between first and second toes • Weakness of toe extension pain on toe flexion Fibula Flexors of foot • Gastronemius and great toe • Soleus • Tibeal Nerve • Sural & Tibial Nerves • 2/3 blood supply to • Plantar flexors lower leg via posterior tibial artery • Blood supply posterior tibial • Weakness of toe flexion and ankle inversion, pain on passive extension Fascia
 • Anterior Compartment is more susceptible to ischemia: • Stronger fascia lower compliance (c= v/ p ) • More slow type 1 muscle fibres – rely on oxidative metabolism. Other compartments have more fast type 2 which can access their increased glycogen stores more via anaerobic metabolism
• Anterior Compartment is more susceptible to ischemia: • Stronger fascia lower compliance (c= v/ p ) • More slow type 1 muscle fibres – rely on oxidative metabolism. Other compartments have more fast type 2 which can access their increased glycogen stores more via anaerobic metabolism
 Diagnosis Clinical Compartment Pressure
Diagnosis Clinical Compartment Pressure
 The 5 components of a physical examination • Inspection (swelling, trauma, skin changes) • Palpation and passive stretch of muscles in the compartments • Evaluation of sensory function • Evaluation of motor function • Evaluation of perfusion
The 5 components of a physical examination • Inspection (swelling, trauma, skin changes) • Palpation and passive stretch of muscles in the compartments • Evaluation of sensory function • Evaluation of motor function • Evaluation of perfusion
 • Nerves are sensitive to diminished oxygen delivery – Sensory change & Weakness Late signs • The presence of palpable pulses at the ankle or wrist in the injured extremity does not rule out the presence of a more proximal compartment syndrome.
• Nerves are sensitive to diminished oxygen delivery – Sensory change & Weakness Late signs • The presence of palpable pulses at the ankle or wrist in the injured extremity does not rule out the presence of a more proximal compartment syndrome.
 CS with high pressure tapering of major arteries and temporary occlusion of collateral arteries (rare) Crush injury of forearm Before fasciotomy After fasciotomy
CS with high pressure tapering of major arteries and temporary occlusion of collateral arteries (rare) Crush injury of forearm Before fasciotomy After fasciotomy
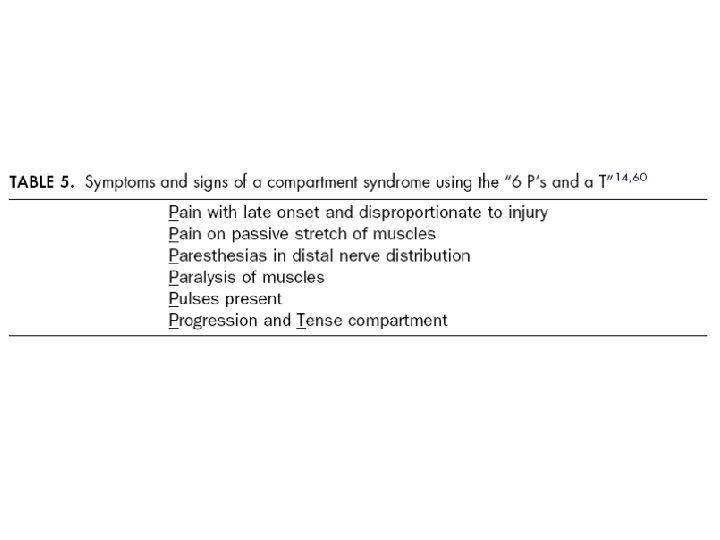
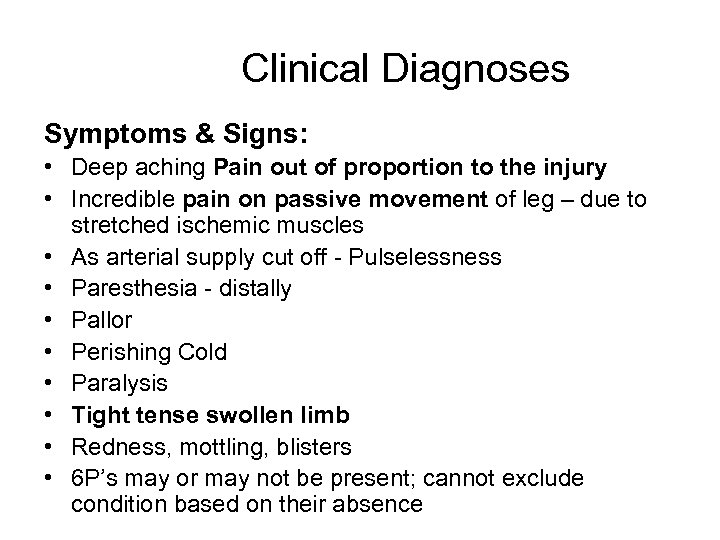 Clinical Diagnoses Symptoms & Signs: • Deep aching Pain out of proportion to the injury • Incredible pain on passive movement of leg – due to stretched ischemic muscles • As arterial supply cut off - Pulselessness • Paresthesia - distally • Pallor • Perishing Cold • Paralysis • Tight tense swollen limb • Redness, mottling, blisters • 6 P’s may or may not be present; cannot exclude condition based on their absence
Clinical Diagnoses Symptoms & Signs: • Deep aching Pain out of proportion to the injury • Incredible pain on passive movement of leg – due to stretched ischemic muscles • As arterial supply cut off - Pulselessness • Paresthesia - distally • Pallor • Perishing Cold • Paralysis • Tight tense swollen limb • Redness, mottling, blisters • 6 P’s may or may not be present; cannot exclude condition based on their absence
 Compartment Pressures • (1) when a comprehensive history and physical examination cannot be performed in the preoperative or postoperative period. • (2) when there are no or few “high risk” criteria in a patient with a moderately severe injury to an extremity • (3) when there is concern about performing an unnecessary fasciotomy (ie, conversion of closed to open fracture).
Compartment Pressures • (1) when a comprehensive history and physical examination cannot be performed in the preoperative or postoperative period. • (2) when there are no or few “high risk” criteria in a patient with a moderately severe injury to an extremity • (3) when there is concern about performing an unnecessary fasciotomy (ie, conversion of closed to open fracture).
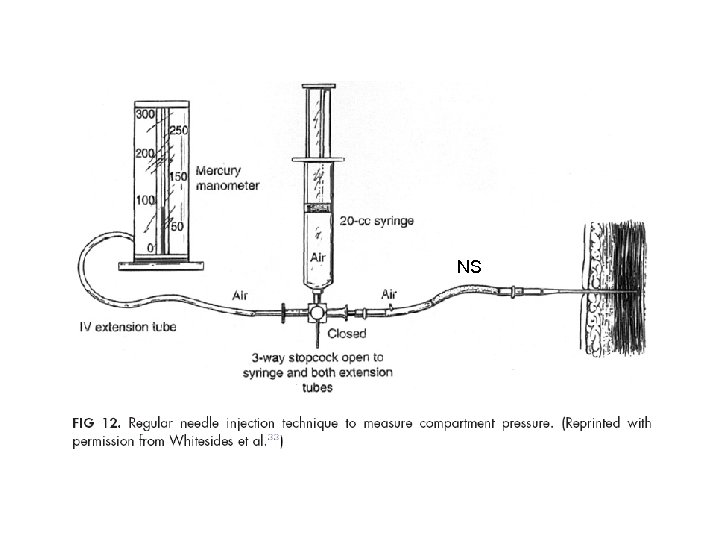 NS
NS
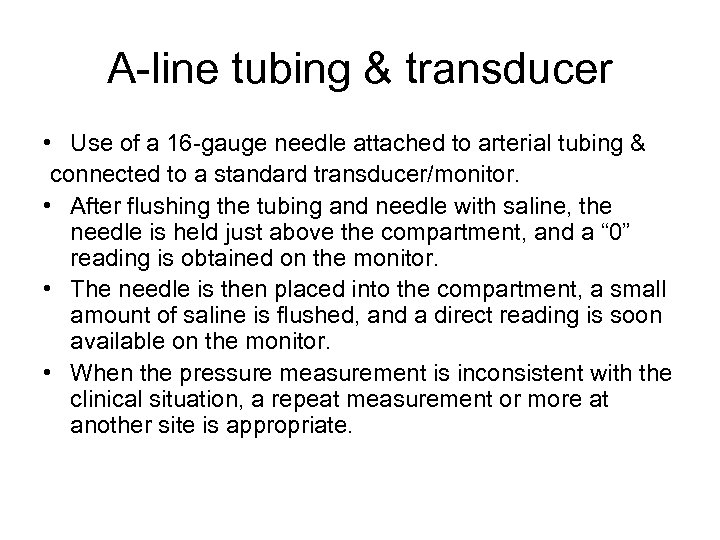 A-line tubing & transducer • Use of a 16 -gauge needle attached to arterial tubing & connected to a standard transducer/monitor. • After flushing the tubing and needle with saline, the needle is held just above the compartment, and a “ 0” reading is obtained on the monitor. • The needle is then placed into the compartment, a small amount of saline is flushed, and a direct reading is soon available on the monitor. • When the pressure measurement is inconsistent with the clinical situation, a repeat measurement or more at another site is appropriate.
A-line tubing & transducer • Use of a 16 -gauge needle attached to arterial tubing & connected to a standard transducer/monitor. • After flushing the tubing and needle with saline, the needle is held just above the compartment, and a “ 0” reading is obtained on the monitor. • The needle is then placed into the compartment, a small amount of saline is flushed, and a direct reading is soon available on the monitor. • When the pressure measurement is inconsistent with the clinical situation, a repeat measurement or more at another site is appropriate.
 Near-Infrared Spectroscopy (NIR) • measures wavelengths of hemoglobin and oxyhemoglobin, but not carboxyhemoglobin or myogloblin, and calculates an St. O 2 or saturation of tissue oxygenation. • tissue oxygen saturation can be used for early detection of ischemia and/or neuromuscular dysfunction in patients with a compartment syndrome in an extremity.
Near-Infrared Spectroscopy (NIR) • measures wavelengths of hemoglobin and oxyhemoglobin, but not carboxyhemoglobin or myogloblin, and calculates an St. O 2 or saturation of tissue oxygenation. • tissue oxygen saturation can be used for early detection of ischemia and/or neuromuscular dysfunction in patients with a compartment syndrome in an extremity.
 Treatment 1. Prevention and treatment of reperfusion injury 2. Non operative treatment 3. Fasciotomy
Treatment 1. Prevention and treatment of reperfusion injury 2. Non operative treatment 3. Fasciotomy
 1. Reperfusion Injury - Ischemic phase; Cellular Hypoxia → ↓Energy → ↑Potential to produce ROM( anaerobic glucose metabolism) - Reperfusion phase ( After revascularization, fasciotomy ); O 2→ ↑ROM → Tissue destruction, Rhabdomyolysis (↑ CPK) return of toxic metabolites to systemic circulation (ROM, K+, Bacteria, myoglobin, etc) Hyperkalemia, sepsis, myoglobinuria, ATN, MOF
1. Reperfusion Injury - Ischemic phase; Cellular Hypoxia → ↓Energy → ↑Potential to produce ROM( anaerobic glucose metabolism) - Reperfusion phase ( After revascularization, fasciotomy ); O 2→ ↑ROM → Tissue destruction, Rhabdomyolysis (↑ CPK) return of toxic metabolites to systemic circulation (ROM, K+, Bacteria, myoglobin, etc) Hyperkalemia, sepsis, myoglobinuria, ATN, MOF
 Rx reperfusion injury - 1. Prevention - Decrease ischemic time - Never reperfuse dead limb !!! - 2. Rx hyperkalemia - 3. Prevent RF Prevent myoglobin precipitation in renal tubules - Hydration, promote urine flow > 100 cc/hr, alkalinize urine - 4. Mannitol promote diuresis, antioxidant - 0. 25 -2 g/kg/dose over 4 hours, total < 200 g/d - C/I hypovolemic, anuric patients - 5. antioxidant (vitamin C, E, selenium) - 6. Dialysis if indicated
Rx reperfusion injury - 1. Prevention - Decrease ischemic time - Never reperfuse dead limb !!! - 2. Rx hyperkalemia - 3. Prevent RF Prevent myoglobin precipitation in renal tubules - Hydration, promote urine flow > 100 cc/hr, alkalinize urine - 4. Mannitol promote diuresis, antioxidant - 0. 25 -2 g/kg/dose over 4 hours, total < 200 g/d - C/I hypovolemic, anuric patients - 5. antioxidant (vitamin C, E, selenium) - 6. Dialysis if indicated
 2. Non operative treatment • • (rarely used, in stable patients with good limb function & perfusion) Observation Position of the Extremity Hyperbaric Oxygen Mannitol
2. Non operative treatment • • (rarely used, in stable patients with good limb function & perfusion) Observation Position of the Extremity Hyperbaric Oxygen Mannitol
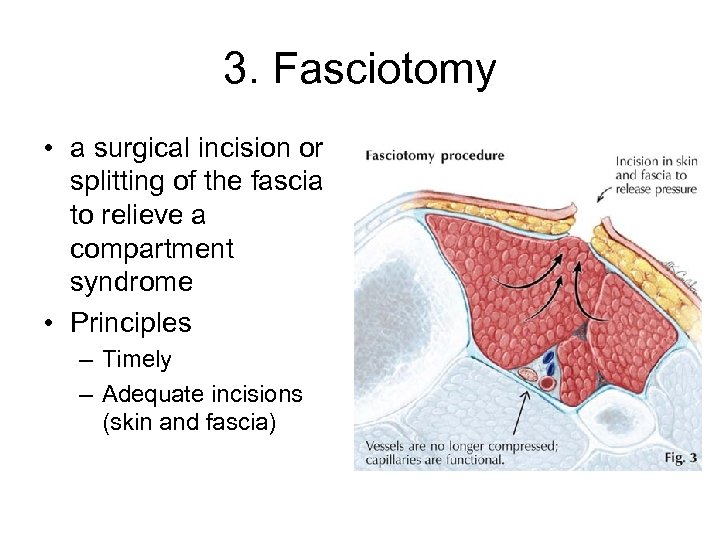 3. Fasciotomy • a surgical incision or splitting of the fascia to relieve a compartment syndrome • Principles – Timely – Adequate incisions (skin and fascia)
3. Fasciotomy • a surgical incision or splitting of the fascia to relieve a compartment syndrome • Principles – Timely – Adequate incisions (skin and fascia)
 Indications for Fasciotomy • • S & S of compartment syndrome compartment pressure > 30 - 35 mm. Hg ∆P (DBP-CP) < 30 mm. Hg Prophylactic – – any popliteal artery injury any combined arterial and venous injury prolonged extremity ischemia > 4 -6 h vascular injury associated with shock; crush injuries; combined skeletal and vascular extremity trauma; and the ligation of a major extremity vein or artery.
Indications for Fasciotomy • • S & S of compartment syndrome compartment pressure > 30 - 35 mm. Hg ∆P (DBP-CP) < 30 mm. Hg Prophylactic – – any popliteal artery injury any combined arterial and venous injury prolonged extremity ischemia > 4 -6 h vascular injury associated with shock; crush injuries; combined skeletal and vascular extremity trauma; and the ligation of a major extremity vein or artery.
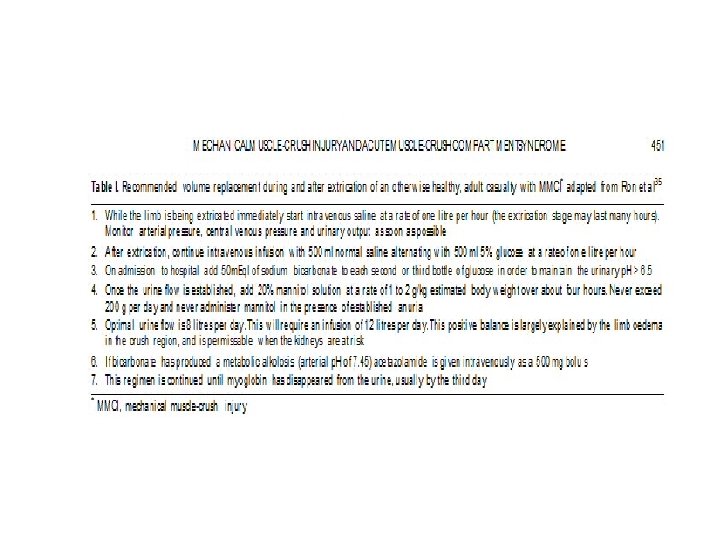
 Reis, et al. Israel J Bone Joint Surg 2005 • Fasciotomy is contraindicated for these reasons: – 1) A fasciotomy for MMCI does not improve outcome (muscle is already dead). – 2) It does increase infection, bleeding and amputation rates. – 3) The fasciotomies and subsequent debridements required consume scarce OR resources that could be better used on others • Only indication for fasciotomy Absence of distal pulse without major arterial injury/ hypotension • Rx conservative, fluid resuscitation
Reis, et al. Israel J Bone Joint Surg 2005 • Fasciotomy is contraindicated for these reasons: – 1) A fasciotomy for MMCI does not improve outcome (muscle is already dead). – 2) It does increase infection, bleeding and amputation rates. – 3) The fasciotomies and subsequent debridements required consume scarce OR resources that could be better used on others • Only indication for fasciotomy Absence of distal pulse without major arterial injury/ hypotension • Rx conservative, fluid resuscitation
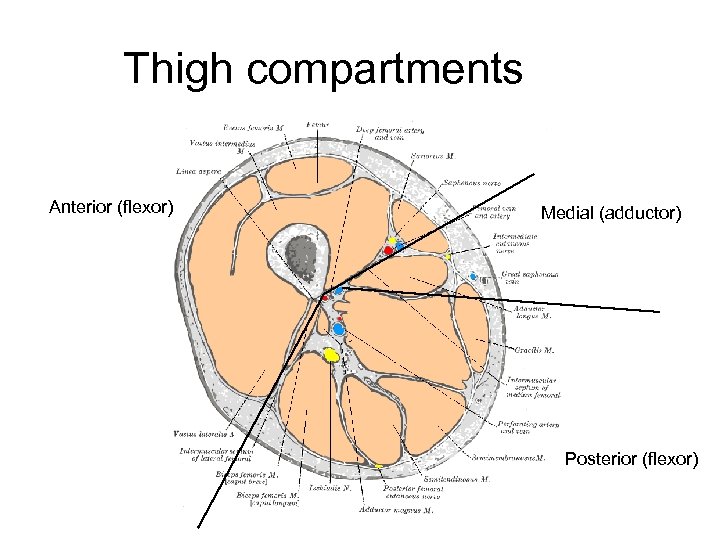 Thigh compartments Anterior (flexor) Medial (adductor) Posterior (flexor)
Thigh compartments Anterior (flexor) Medial (adductor) Posterior (flexor)
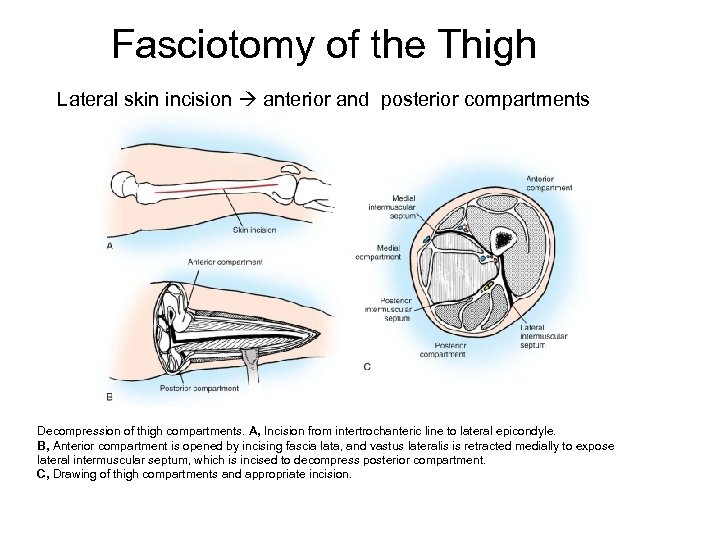 Fasciotomy of the Thigh Lateral skin incision anterior and posterior compartments Decompression of thigh compartments. A, Incision from intertrochanteric line to lateral epicondyle. B, Anterior compartment is opened by incising fascia lata, and vastus lateralis is retracted medially to expose lateral intermuscular septum, which is incised to decompress posterior compartment. C, Drawing of thigh compartments and appropriate incision.
Fasciotomy of the Thigh Lateral skin incision anterior and posterior compartments Decompression of thigh compartments. A, Incision from intertrochanteric line to lateral epicondyle. B, Anterior compartment is opened by incising fascia lata, and vastus lateralis is retracted medially to expose lateral intermuscular septum, which is incised to decompress posterior compartment. C, Drawing of thigh compartments and appropriate incision.
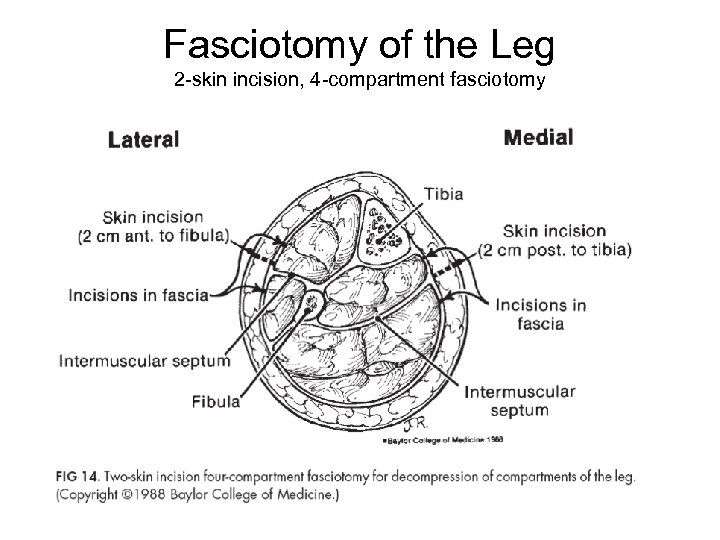 Fasciotomy of the Leg 2 -skin incision, 4 -compartment fasciotomy
Fasciotomy of the Leg 2 -skin incision, 4 -compartment fasciotomy
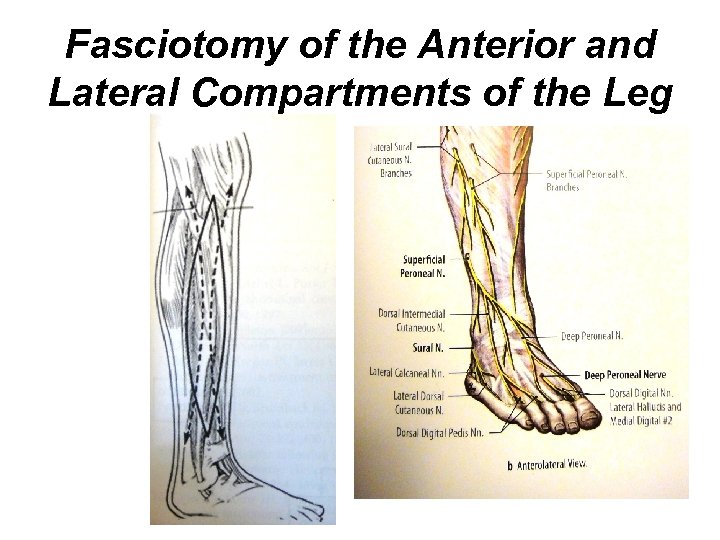 Fasciotomy of the Anterior and Lateral Compartments of the Leg
Fasciotomy of the Anterior and Lateral Compartments of the Leg
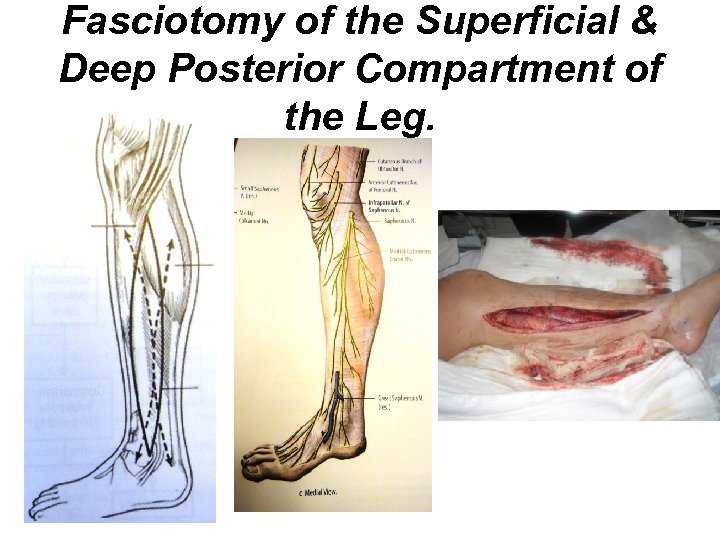 Fasciotomy of the Superficial & Deep Posterior Compartment of the Leg.
Fasciotomy of the Superficial & Deep Posterior Compartment of the Leg.
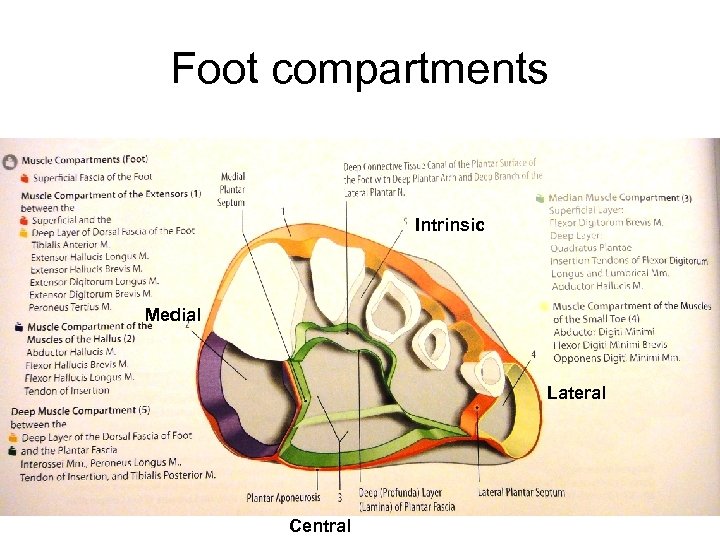 Foot compartments Intrinsic Medial Lateral Central
Foot compartments Intrinsic Medial Lateral Central
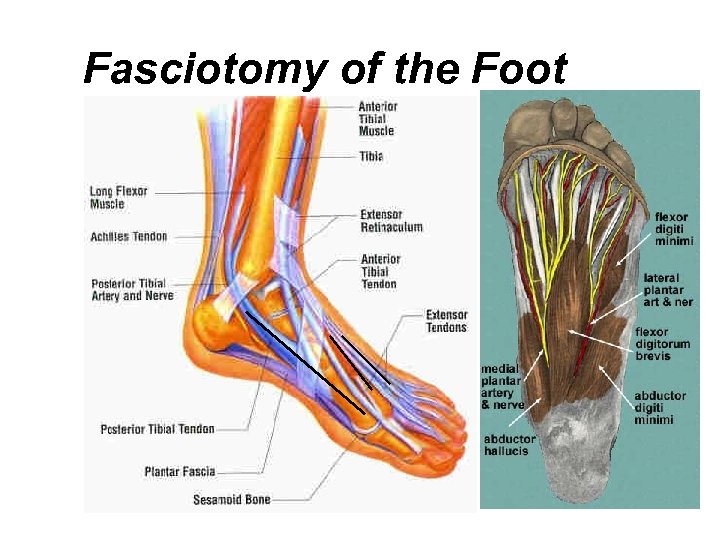 Fasciotomy of the Foot
Fasciotomy of the Foot
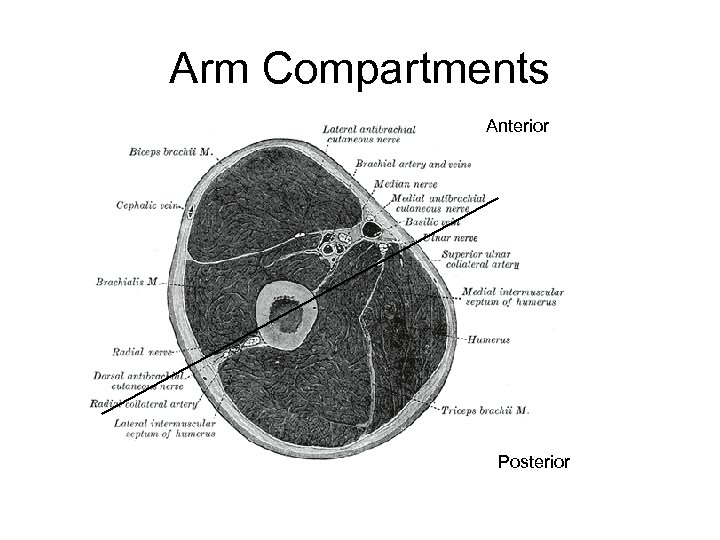 Arm Compartments Anterior Posterior
Arm Compartments Anterior Posterior
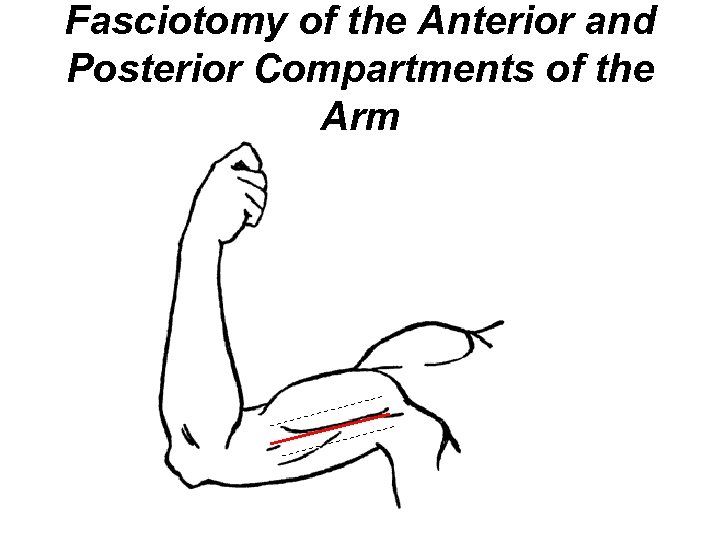 Fasciotomy of the Anterior and Posterior Compartments of the Arm
Fasciotomy of the Anterior and Posterior Compartments of the Arm
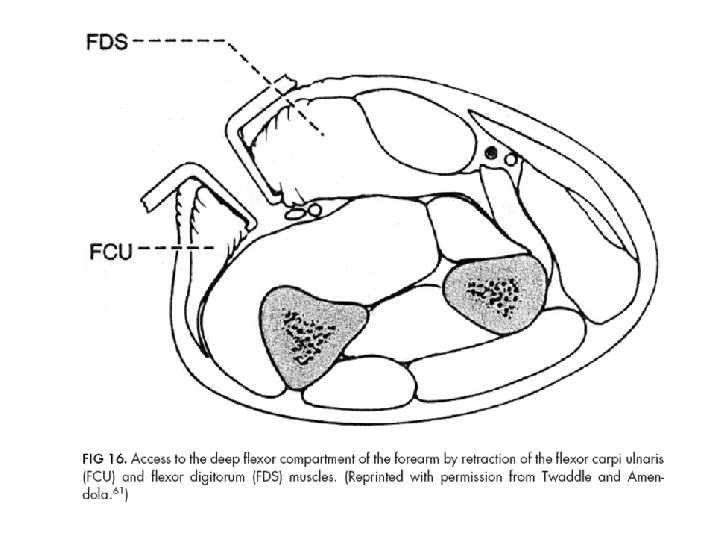
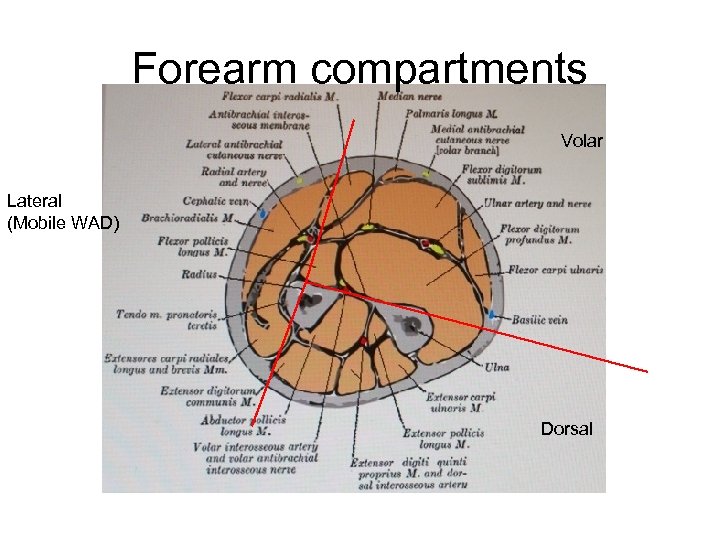 Forearm compartments Volar Lateral (Mobile WAD) Dorsal
Forearm compartments Volar Lateral (Mobile WAD) Dorsal
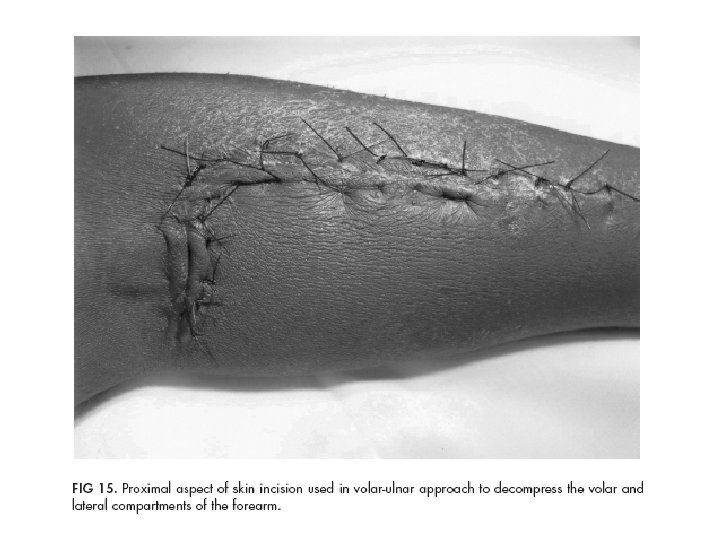
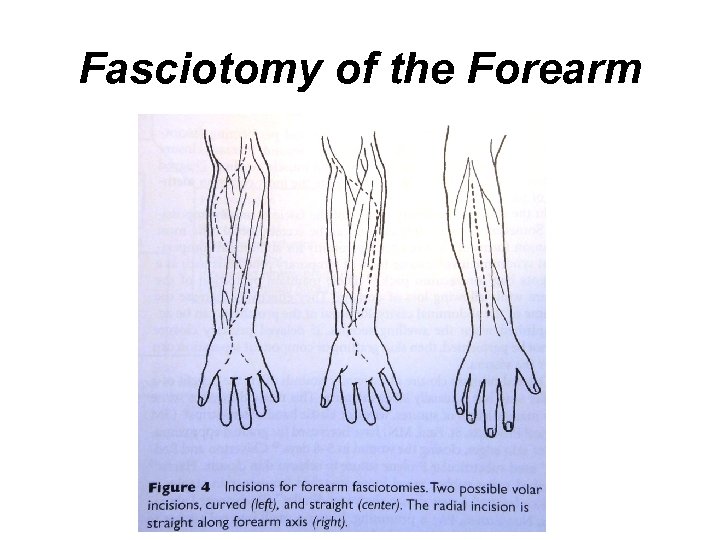 Fasciotomy of the Forearm
Fasciotomy of the Forearm
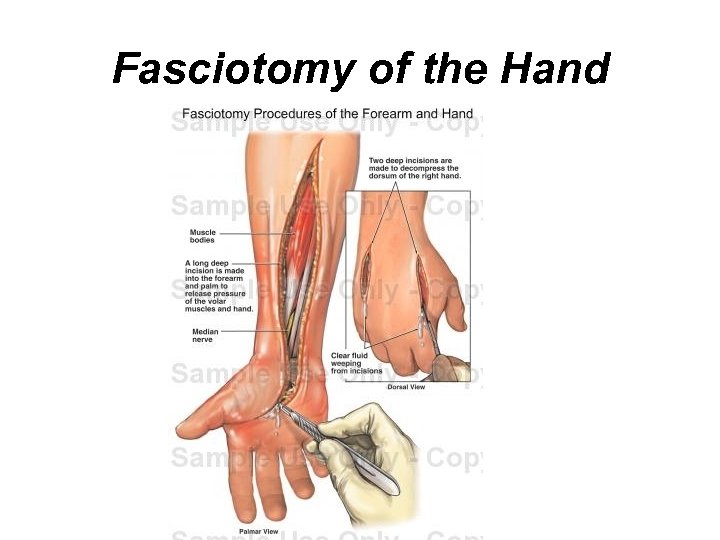 Fasciotomy of the Hand
Fasciotomy of the Hand
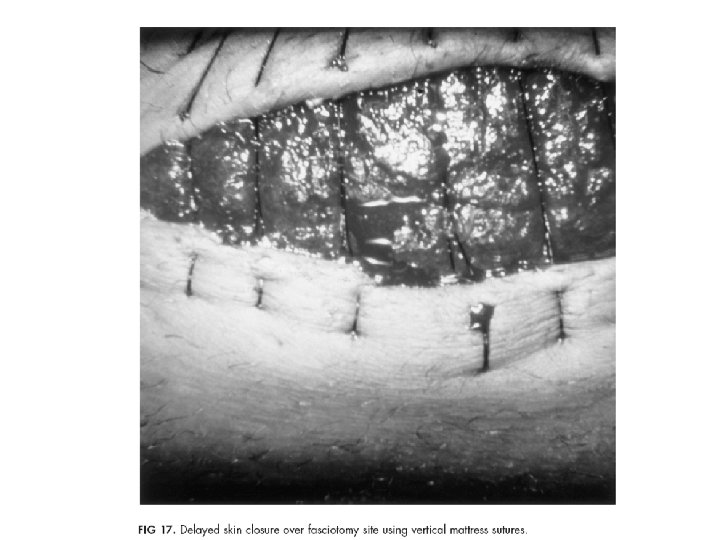
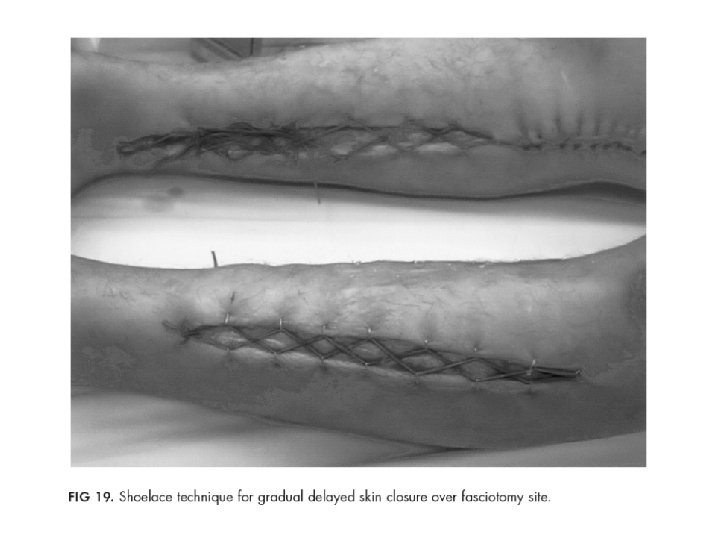
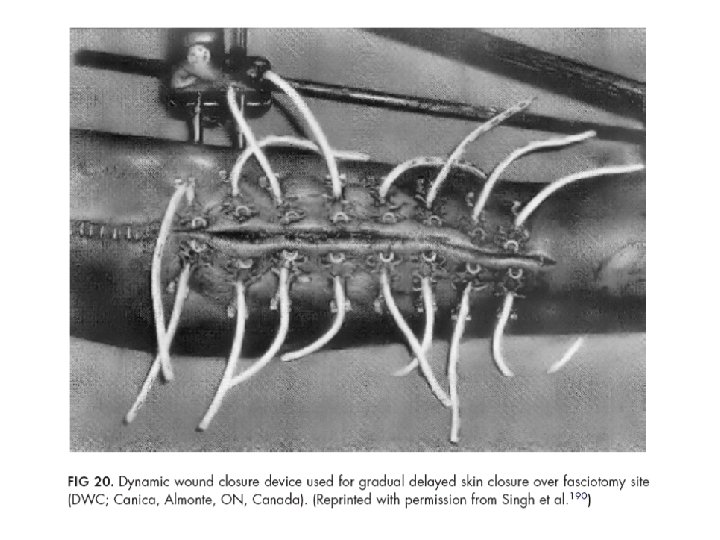
 Closure Techniques • Delayed Primary Closure • Shoelace Technique • Mechanical Devices – STAR (Suture Tension Adjustment Reel) – Dynamic Wound Closure Device (DWC) • Vacuum Assisted Closure • Skin Grafting
Closure Techniques • Delayed Primary Closure • Shoelace Technique • Mechanical Devices – STAR (Suture Tension Adjustment Reel) – Dynamic Wound Closure Device (DWC) • Vacuum Assisted Closure • Skin Grafting

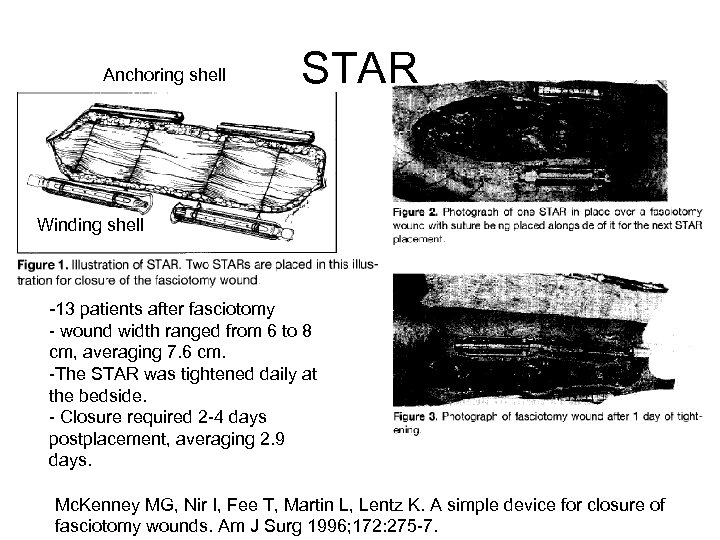 Anchoring shell STAR Winding shell -13 patients after fasciotomy - wound width ranged from 6 to 8 cm, averaging 7. 6 cm. -The STAR was tightened daily at the bedside. - Closure required 2 -4 days postplacement, averaging 2. 9 days. Mc. Kenney MG, Nir I, Fee T, Martin L, Lentz K. A simple device for closure of fasciotomy wounds. Am J Surg 1996; 172: 275 -7.
Anchoring shell STAR Winding shell -13 patients after fasciotomy - wound width ranged from 6 to 8 cm, averaging 7. 6 cm. -The STAR was tightened daily at the bedside. - Closure required 2 -4 days postplacement, averaging 2. 9 days. Mc. Kenney MG, Nir I, Fee T, Martin L, Lentz K. A simple device for closure of fasciotomy wounds. Am J Surg 1996; 172: 275 -7.
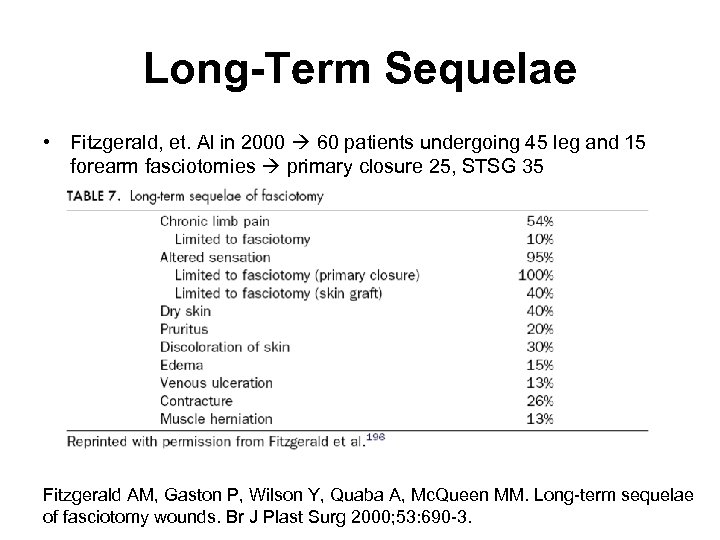 Long-Term Sequelae • Fitzgerald, et. Al in 2000 60 patients undergoing 45 leg and 15 forearm fasciotomies primary closure 25, STSG 35 Fitzgerald AM, Gaston P, Wilson Y, Quaba A, Mc. Queen MM. Long-term sequelae of fasciotomy wounds. Br J Plast Surg 2000; 53: 690 -3.
Long-Term Sequelae • Fitzgerald, et. Al in 2000 60 patients undergoing 45 leg and 15 forearm fasciotomies primary closure 25, STSG 35 Fitzgerald AM, Gaston P, Wilson Y, Quaba A, Mc. Queen MM. Long-term sequelae of fasciotomy wounds. Br J Plast Surg 2000; 53: 690 -3.
 Conclusions: Compartment Syndrome • Early Dx – Pain, Tense, sensory & motor changes – Compartment pressure • Fasciotomy – Clinical of CS – Compartment pressure > 30 -35 mm. Hg – Prophylactic in high risk patients • Prevention and treatment of Reperfusion Injury
Conclusions: Compartment Syndrome • Early Dx – Pain, Tense, sensory & motor changes – Compartment pressure • Fasciotomy – Clinical of CS – Compartment pressure > 30 -35 mm. Hg – Prophylactic in high risk patients • Prevention and treatment of Reperfusion Injury
 References • Dente CJ, Wyrzykowski AD, Feliciano DV. , Fasciotomy. Curr Probl Surg. 2009 Oct; 46(10): 779 -839. • Asensio JA, Trunkey DD, editors. Current therapy of trauma and surgical critical care. Philadelphia: Mosby Elsevier; 2007
References • Dente CJ, Wyrzykowski AD, Feliciano DV. , Fasciotomy. Curr Probl Surg. 2009 Oct; 46(10): 779 -839. • Asensio JA, Trunkey DD, editors. Current therapy of trauma and surgical critical care. Philadelphia: Mosby Elsevier; 2007


