6c389d166317ab1bc30176687df7d441.ppt
- Количество слайдов: 1
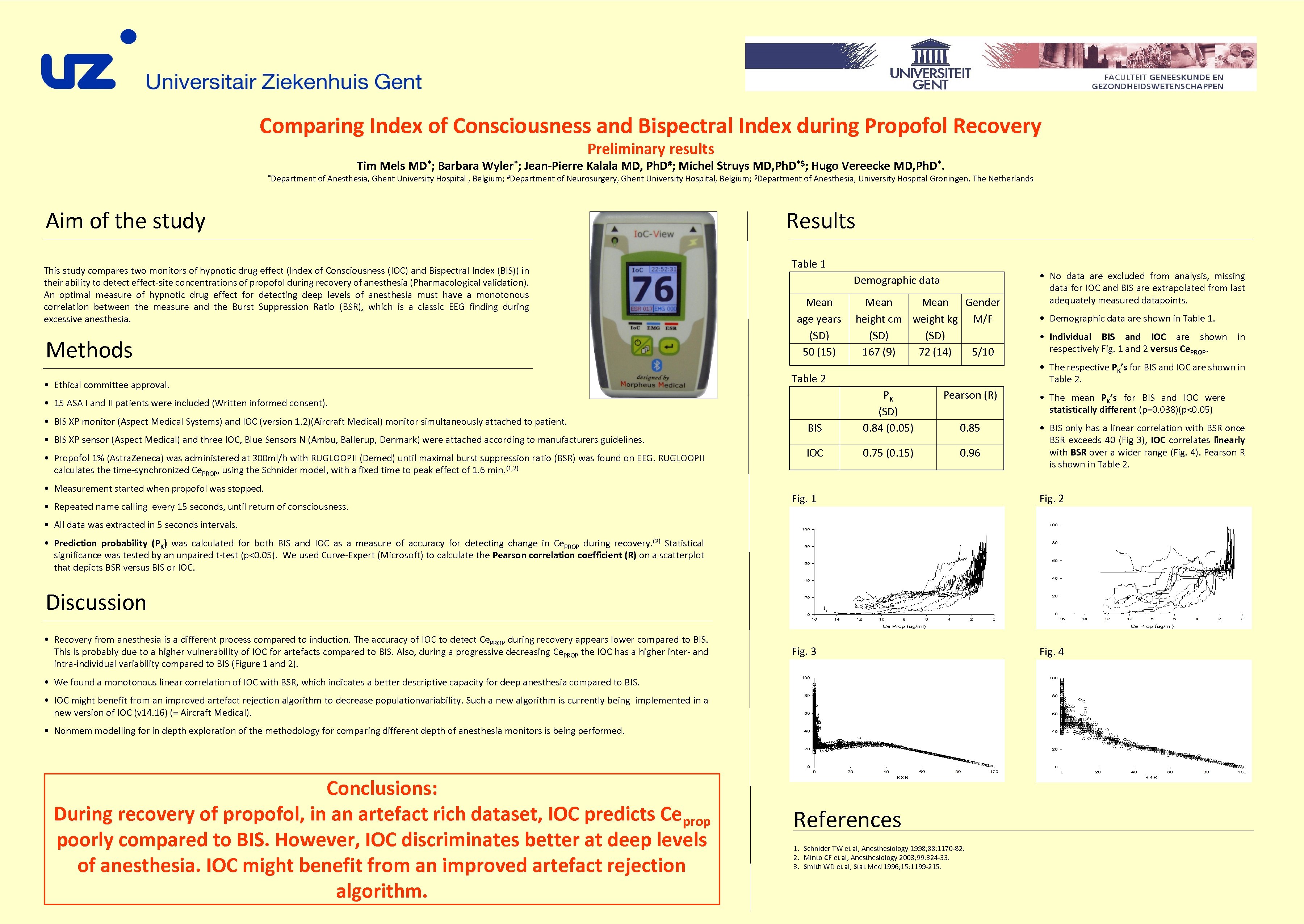
Comparing Index of Consciousness and Bispectral Index during Propofol Recovery Preliminary results *Department Tim Mels MD*; Barbara Wyler*; Jean-Pierre Kalala MD, Ph. D#; Michel Struys MD, Ph. D*$; Hugo Vereecke MD, Ph. D*. of Anesthesia, Ghent University Hospital , Belgium; #Department of Neurosurgery, Ghent University Hospital, Belgium; $Department of Anesthesia, University Hospital Groningen, The Netherlands Aim of the study This study compares two monitors of hypnotic drug effect (Index of Consciousness (IOC) and Bispectral Index (BIS)) in their ability to detect effect-site concentrations of propofol during recovery of anesthesia (Pharmacological validation). An optimal measure of hypnotic drug effect for detecting deep levels of anesthesia must have a monotonous correlation between the measure and the Burst Suppression Ratio (BSR), which is a classic EEG finding during excessive anesthesia. Methods • Ethical committee approval. Results Table 1 Demographic data Mean age years (SD) 50 (15) • BIS XP sensor (Aspect Medical) and three IOC, Blue Sensors N (Ambu, Ballerup, Denmark) were attached according to manufacturers guidelines. • Propofol 1% (Astra. Zeneca) was administered at 300 ml/h with RUGLOOPII (Demed) until maximal burst suppression ratio (BSR) was found on EEG. RUGLOOPII calculates the time-synchronized Ce. PROP, using the Schnider model, with a fixed time to peak effect of 1. 6 min. (1, 2) • Measurement started when propofol was stopped. • Repeated name calling every 15 seconds, until return of consciousness. • Demographic data are shown in Table 1. • Individual BIS and IOC are shown in respectively Fig. 1 and 2 versus Ce. PROP. • The respective PK’s for BIS and IOC are shown in Table 2 Pearson (R) BIS PK (SD) 0. 84 (0. 05) IOC 0. 75 (0. 15) 0. 96 • 15 ASA I and II patients were included (Written informed consent). • BIS XP monitor (Aspect Medical Systems) and IOC (version 1. 2)(Aircraft Medical) monitor simultaneously attached to patient. Mean Gender height cm weight kg M/F (SD) 167 (9) 72 (14) 5/10 • No data are excluded from analysis, missing data for IOC and BIS are extrapolated from last adequately measured datapoints. 0. 85 • The mean PK’s for BIS and IOC were statistically different (p=0. 038)(p<0. 05) • BIS only has a linear correlation with BSR once BSR exceeds 40 (Fig 3), IOC correlates linearly with BSR over a wider range (Fig. 4). Pearson R is shown in Table 2. Fig. 1 Fig. 2 Fig. 3 Fig. 4 • All data was extracted in 5 seconds intervals. • Prediction probability (PK) was calculated for both BIS and IOC as a measure of accuracy for detecting change in Ce. PROP during recovery. (3) Statistical significance was tested by an unpaired t-test (p<0. 05). We used Curve-Expert (Microsoft) to calculate the Pearson correlation coefficient (R) on a scatterplot that depicts BSR versus BIS or IOC. Discussion • Recovery from anesthesia is a different process compared to induction. The accuracy of IOC to detect Ce. PROP during recovery appears lower compared to BIS. This is probably due to a higher vulnerability of IOC for artefacts compared to BIS. Also, during a progressive decreasing Ce. PROP the IOC has a higher inter- and intra-individual variability compared to BIS (Figure 1 and 2). • We found a monotonous linear correlation of IOC with BSR, which indicates a better descriptive capacity for deep anesthesia compared to BIS. • IOC might benefit from an improved artefact rejection algorithm to decrease populationvariability. Such a new algorithm is currently being implemented in a new version of IOC (v 14. 16) (= Aircraft Medical). • Nonmem modelling for in depth exploration of the methodology for comparing different depth of anesthesia monitors is being performed. Conclusions: During recovery of propofol, in an artefact rich dataset, IOC predicts Ce prop poorly compared to BIS. However, IOC discriminates better at deep levels of anesthesia. IOC might benefit from an improved artefact rejection algorithm. BSR References 1. Schnider TW et al, Anesthesiology 1998; 88: 1170 -82. 2. Minto CF et al, Anesthesiology 2003; 99: 324 -33. 3. Smith WD et al, Stat Med 1996; 15: 1199 -215. BSR
6c389d166317ab1bc30176687df7d441.ppt