2a4f5c2c5a2743e5b48bd878499b4016.ppt
- Количество слайдов: 49
 Community partnerships for health related MDG’s Conclusions of The State of the World’s Children 2008 and Systematic Review of the Effectiveness of Community-Based Primary Health Care in Improving Child Health
Community partnerships for health related MDG’s Conclusions of The State of the World’s Children 2008 and Systematic Review of the Effectiveness of Community-Based Primary Health Care in Improving Child Health
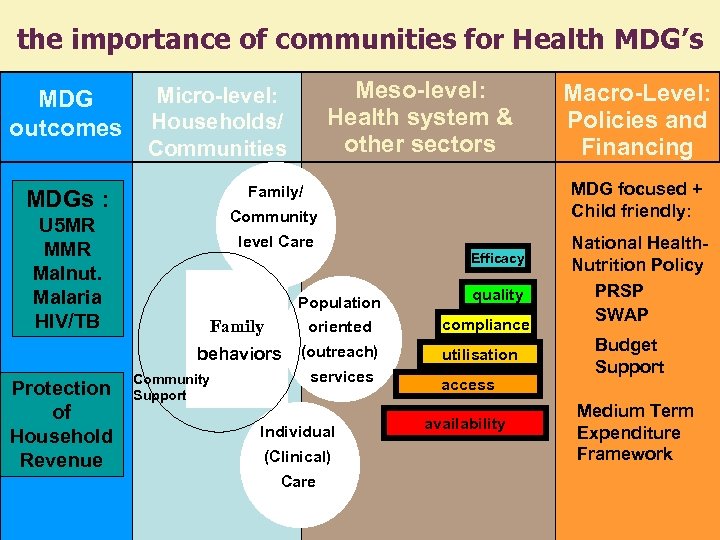 the importance of communities for Health MDG’s MDG outcomes Community level Care Efficacy Population oriented behaviors Protection of Household Revenue Family (outreach) Community Support services Individual (Clinical) Care Macro-Level: Policies and Financing MDG focused + Child friendly: Family/ MDGs : U 5 MR Malnut. Malaria HIV/TB Meso-level: Health system & other sectors Micro-level: Households/ Communities quality compliance utilisation access availability National Health. Nutrition Policy PRSP SWAP Budget Support Medium Term Expenditure Framework
the importance of communities for Health MDG’s MDG outcomes Community level Care Efficacy Population oriented behaviors Protection of Household Revenue Family (outreach) Community Support services Individual (Clinical) Care Macro-Level: Policies and Financing MDG focused + Child friendly: Family/ MDGs : U 5 MR Malnut. Malaria HIV/TB Meso-level: Health system & other sectors Micro-level: Households/ Communities quality compliance utilisation access availability National Health. Nutrition Policy PRSP SWAP Budget Support Medium Term Expenditure Framework
 The Bamako Initiative • Launched by African health Ministers in 1987 • Built on 5 years operations research in Benin (Pahou) and Congo (Kasongo) • Community movement: Community co-managed, cost shared and monitored revitalization of 10. 000 health centers with drug revolving funds • Community Based National Health Systems in Benin, Guinea, Mali, DR Congo, Guinea Bissau • Benin Immmization Coverage from 12% in 1986 to 75 % in 1990 and fully sustained since then • Resiliance demonstrated during Togo, DR Congo, Guinea Bissau and other crisis • Foundation for success of ACSD (10 -20% U 5 MR reduction for $ 500/life saved)
The Bamako Initiative • Launched by African health Ministers in 1987 • Built on 5 years operations research in Benin (Pahou) and Congo (Kasongo) • Community movement: Community co-managed, cost shared and monitored revitalization of 10. 000 health centers with drug revolving funds • Community Based National Health Systems in Benin, Guinea, Mali, DR Congo, Guinea Bissau • Benin Immmization Coverage from 12% in 1986 to 75 % in 1990 and fully sustained since then • Resiliance demonstrated during Togo, DR Congo, Guinea Bissau and other crisis • Foundation for success of ACSD (10 -20% U 5 MR reduction for $ 500/life saved)
 Lessons Learned from a hundred years • Scaling-up will not be achieved through facility-based and outreach services alone: Community Partnerships are central to achieving coverage, creating demand achieving sustainability. • Ensuring a continuum of care by delivering integrated packages of health, nutrition, HIV, water and sanitation interventions will be critical to achieving maximal impact on maternal, newborn and child survival. • Strengthening of ‘health-systems for outcomes’ combines the strength of selective/vertical approaches and comprehensive/horizontal approaches to scaling up evidence-based, high-impact intervention packages and practices, while removing system-wide bottlenecks to health care provision and usage.
Lessons Learned from a hundred years • Scaling-up will not be achieved through facility-based and outreach services alone: Community Partnerships are central to achieving coverage, creating demand achieving sustainability. • Ensuring a continuum of care by delivering integrated packages of health, nutrition, HIV, water and sanitation interventions will be critical to achieving maximal impact on maternal, newborn and child survival. • Strengthening of ‘health-systems for outcomes’ combines the strength of selective/vertical approaches and comprehensive/horizontal approaches to scaling up evidence-based, high-impact intervention packages and practices, while removing system-wide bottlenecks to health care provision and usage.
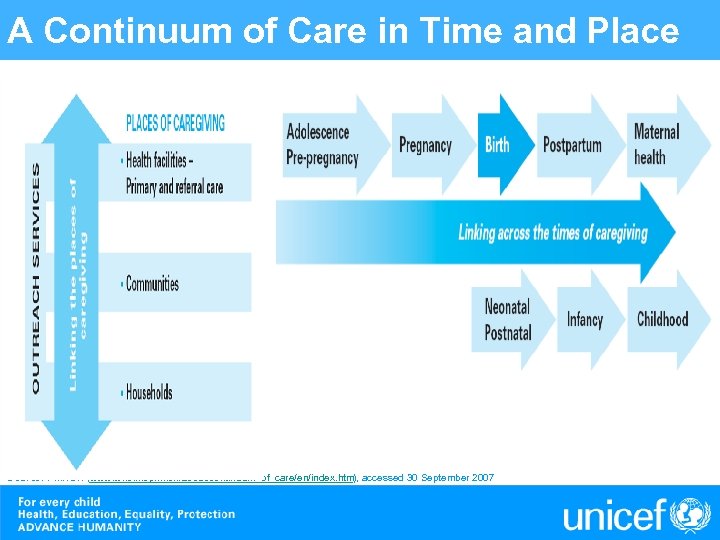 A Continuum of Care in Time and Place Source: PMNCH (www. who. int/pmnch/about/continuum_of_care/en/index. htm), accessed 30 September 2007
A Continuum of Care in Time and Place Source: PMNCH (www. who. int/pmnch/about/continuum_of_care/en/index. htm), accessed 30 September 2007
 Community partnerships in PHC: Ways of enhancing success • • Cohesive, inclusive participation; Support and incentives for workers; Adequate programme supervision and support; Effective referral systems to facility-based care; Intersectoral collaboration; Secure financing; and Integration of community partnerships with district and national health programmes and policies.
Community partnerships in PHC: Ways of enhancing success • • Cohesive, inclusive participation; Support and incentives for workers; Adequate programme supervision and support; Effective referral systems to facility-based care; Intersectoral collaboration; Secure financing; and Integration of community partnerships with district and national health programmes and policies.
 Scaling up community partnerships, a continuum of care, health systems for outcomes • Realign programmes from disease –specific interventions to evidence-based, high-impact, integrated packages to ensure a continuum of care • Make MNCH a central tenet of integrated results based national planning processes for scaling up • Improve the quality and consistency of financing for strengthening health systems • Foster and sustain political commitments, national and international leadership an sustained financing to develop health systems • Create conditions for greater harmonization of global health programmes and partnerships
Scaling up community partnerships, a continuum of care, health systems for outcomes • Realign programmes from disease –specific interventions to evidence-based, high-impact, integrated packages to ensure a continuum of care • Make MNCH a central tenet of integrated results based national planning processes for scaling up • Improve the quality and consistency of financing for strengthening health systems • Foster and sustain political commitments, national and international leadership an sustained financing to develop health systems • Create conditions for greater harmonization of global health programmes and partnerships
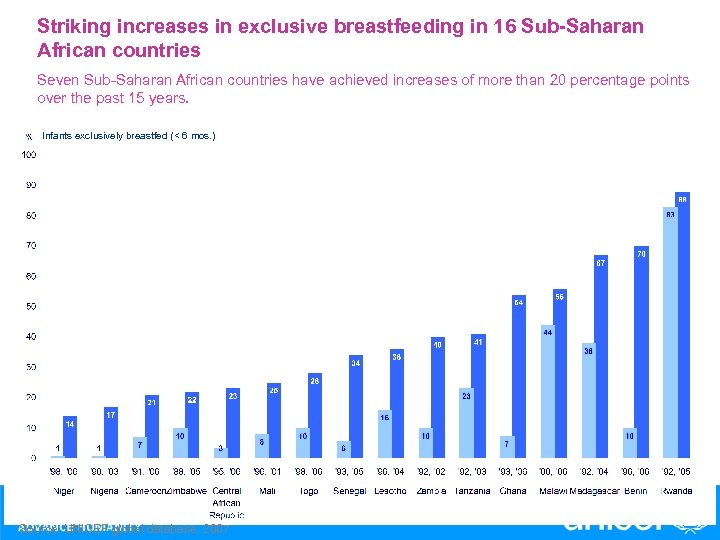 Striking increases in exclusive breastfeeding in 16 Sub-Saharan African countries Seven Sub-Saharan African countries have achieved increases of more than 20 percentage points over the past 15 years. Infants exclusively breastfed (< 6 mos. ) Source: UNICEF global database, 2007
Striking increases in exclusive breastfeeding in 16 Sub-Saharan African countries Seven Sub-Saharan African countries have achieved increases of more than 20 percentage points over the past 15 years. Infants exclusively breastfed (< 6 mos. ) Source: UNICEF global database, 2007
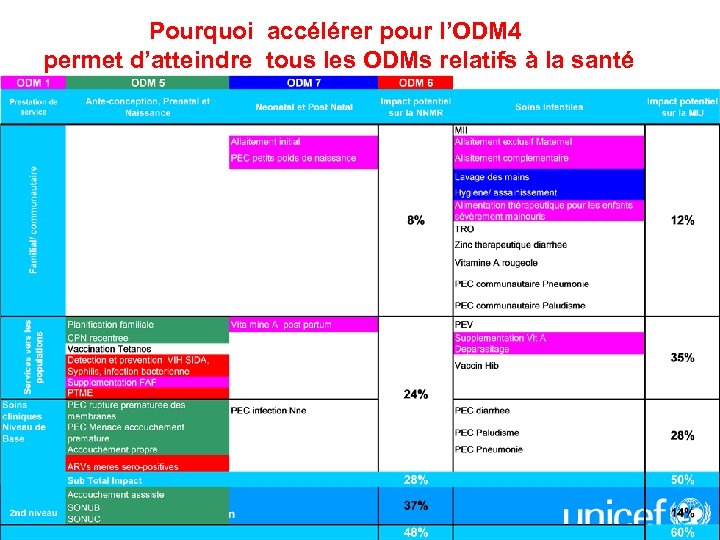 Pourquoi accélérer pour l’ODM 4 permet d’atteindre tous les ODMs relatifs à la santé
Pourquoi accélérer pour l’ODM 4 permet d’atteindre tous les ODMs relatifs à la santé
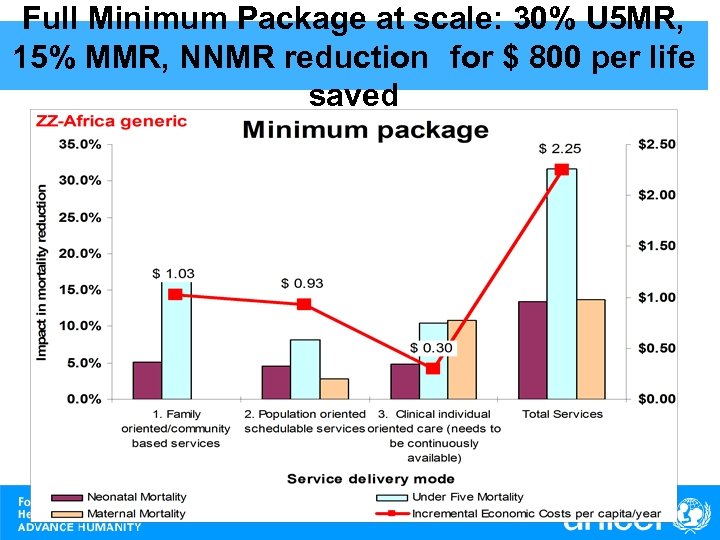 Full Minimum Package at scale: 30% U 5 MR, 15% MMR, NNMR reduction for $ 800 per life saved
Full Minimum Package at scale: 30% U 5 MR, 15% MMR, NNMR reduction for $ 800 per life saved
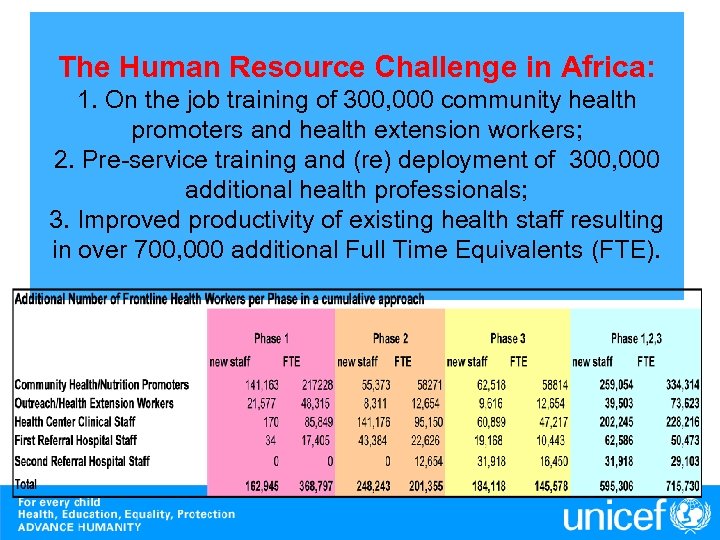 The Human Resource Challenge in Africa: 1. On the job training of 300, 000 community health promoters and health extension workers; 2. Pre-service training and (re) deployment of 300, 000 additional health professionals; 3. Improved productivity of existing health staff resulting in over 700, 000 additional Full Time Equivalents (FTE).
The Human Resource Challenge in Africa: 1. On the job training of 300, 000 community health promoters and health extension workers; 2. Pre-service training and (re) deployment of 300, 000 additional health professionals; 3. Improved productivity of existing health staff resulting in over 700, 000 additional Full Time Equivalents (FTE).
 Systematic Review of the Effectiveness of Community-Based Primary Health Care in Improving Child Health Key Questions • How strong is the evidence that CBPHC can improve child health? • What conditions/program elements must be in place for CBPHC to be effective? • How important are partnerships between communities and health systems? • Does CBPHC promote equity and is it costeffective?
Systematic Review of the Effectiveness of Community-Based Primary Health Care in Improving Child Health Key Questions • How strong is the evidence that CBPHC can improve child health? • What conditions/program elements must be in place for CBPHC to be effective? • How important are partnerships between communities and health systems? • Does CBPHC promote equity and is it costeffective?
 Definition of CBPHC • Activities, interventions, programs that take place in the community outside of health facilities • Includes selective and comprehensive approaches • Includes non-health interventions (e. g. , micro -credit, education, women’s empowerment, societal factors)
Definition of CBPHC • Activities, interventions, programs that take place in the community outside of health facilities • Includes selective and comprehensive approaches • Includes non-health interventions (e. g. , micro -credit, education, women’s empowerment, societal factors)
 Process • Review of available documentation – Peer-reviewed journal articles – Books – Program evaluations – Unpublished reports • Data extraction-2 independent reviewers • Special focus on community context and community partnerships
Process • Review of available documentation – Peer-reviewed journal articles – Books – Program evaluations – Unpublished reports • Data extraction-2 independent reviewers • Special focus on community context and community partnerships
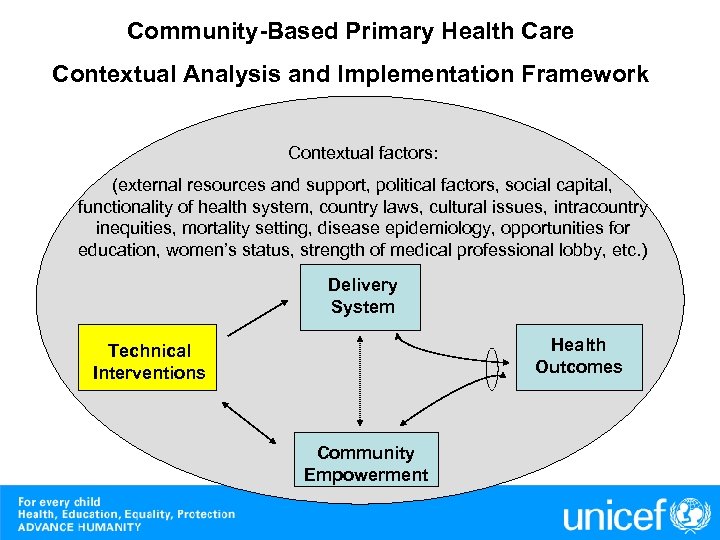 Community-Based Primary Health Care Contextual Analysis and Implementation Framework Contextual factors: (external resources and support, political factors, social capital, functionality of health system, country laws, cultural issues, intracountry inequities, mortality setting, disease epidemiology, opportunities for education, women’s status, strength of medical professional lobby, etc. ) Delivery System Health Outcomes Technical Interventions Community Empowerment
Community-Based Primary Health Care Contextual Analysis and Implementation Framework Contextual factors: (external resources and support, political factors, social capital, functionality of health system, country laws, cultural issues, intracountry inequities, mortality setting, disease epidemiology, opportunities for education, women’s status, strength of medical professional lobby, etc. ) Delivery System Health Outcomes Technical Interventions Community Empowerment
 Technical Interventions Criteria for defining priority effective interventions • Safety demonstrated • Shown to have mortality or nutrition improvement efficacy • Programmatic experience exists • Feasibility of or experience with reaching high coverage
Technical Interventions Criteria for defining priority effective interventions • Safety demonstrated • Shown to have mortality or nutrition improvement efficacy • Programmatic experience exists • Feasibility of or experience with reaching high coverage
 Technical Interventions Priority child survival interventions for scale up • • • Immunizations for mothers and children Vitamin A supplementation Iodine fortification and supplementation when necessary Home-based neonatal care including neonatal sepsis management Clean delivery Hand-washing Household water treatment and safe storage Sanitation ORT and zinc for diarrhea treatment Childhood pneumonia treatment Prevention of mother-to-child transmission of HIV Cotrimoxazole prophylaxis for HIV-infected children
Technical Interventions Priority child survival interventions for scale up • • • Immunizations for mothers and children Vitamin A supplementation Iodine fortification and supplementation when necessary Home-based neonatal care including neonatal sepsis management Clean delivery Hand-washing Household water treatment and safe storage Sanitation ORT and zinc for diarrhea treatment Childhood pneumonia treatment Prevention of mother-to-child transmission of HIV Cotrimoxazole prophylaxis for HIV-infected children
 Technical Interventions Priority child survival interventions for scale up • Insecticide-treated materials and/or indoor residual spraying for malaria • Malaria treatment • Intermittent preventive therapy for malaria for pregnant women • Exclusive breastfeeding promotion for first 6 months • Continued breastfeeding promotion until at least 24 months • Ready to use therapeutic foods for severely malnourished children • Promotion of complementary feeding for children focused on 6 to 23 months • Supplementary feeding for food-insecure families focused on 6 to 23 months
Technical Interventions Priority child survival interventions for scale up • Insecticide-treated materials and/or indoor residual spraying for malaria • Malaria treatment • Intermittent preventive therapy for malaria for pregnant women • Exclusive breastfeeding promotion for first 6 months • Continued breastfeeding promotion until at least 24 months • Ready to use therapeutic foods for severely malnourished children • Promotion of complementary feeding for children focused on 6 to 23 months • Supplementary feeding for food-insecure families focused on 6 to 23 months
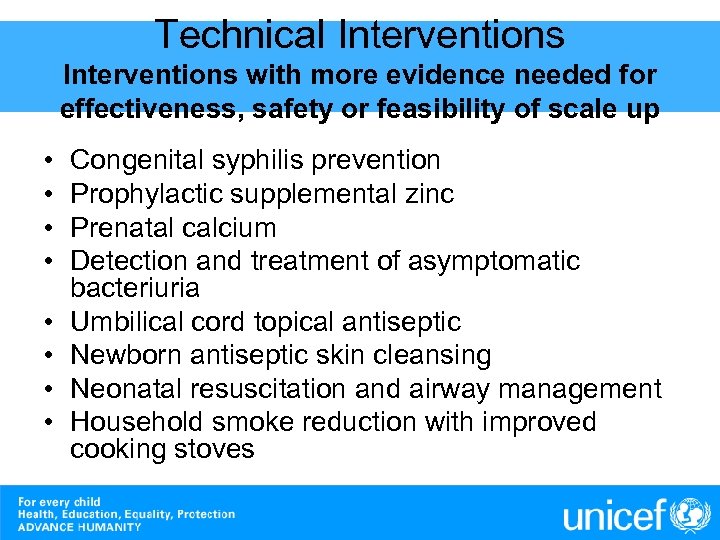 Technical Interventions with more evidence needed for effectiveness, safety or feasibility of scale up • • Congenital syphilis prevention Prophylactic supplemental zinc Prenatal calcium Detection and treatment of asymptomatic bacteriuria Umbilical cord topical antiseptic Newborn antiseptic skin cleansing Neonatal resuscitation and airway management Household smoke reduction with improved cooking stoves
Technical Interventions with more evidence needed for effectiveness, safety or feasibility of scale up • • Congenital syphilis prevention Prophylactic supplemental zinc Prenatal calcium Detection and treatment of asymptomatic bacteriuria Umbilical cord topical antiseptic Newborn antiseptic skin cleansing Neonatal resuscitation and airway management Household smoke reduction with improved cooking stoves
 Technical Interventions with indirect effects on child survival • Family planning • Adult HIV treatment • Maternal mortality reduction
Technical Interventions with indirect effects on child survival • Family planning • Adult HIV treatment • Maternal mortality reduction
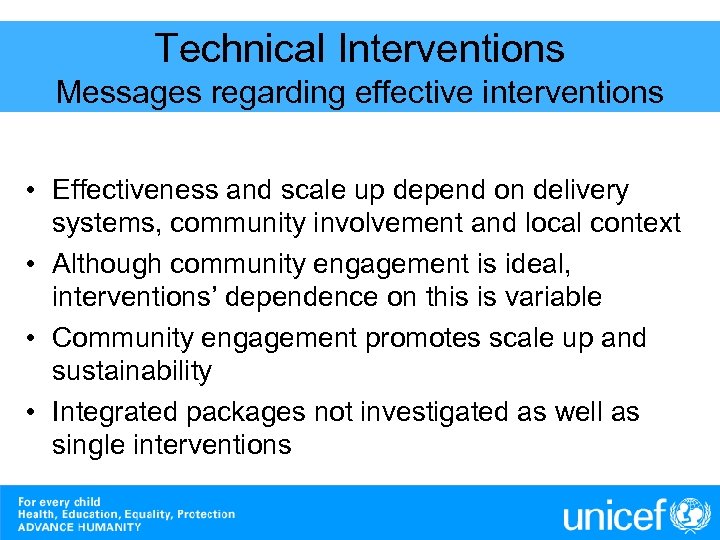 Technical Interventions Messages regarding effective interventions • Effectiveness and scale up depend on delivery systems, community involvement and local context • Although community engagement is ideal, interventions’ dependence on this is variable • Community engagement promotes scale up and sustainability • Integrated packages not investigated as well as single interventions
Technical Interventions Messages regarding effective interventions • Effectiveness and scale up depend on delivery systems, community involvement and local context • Although community engagement is ideal, interventions’ dependence on this is variable • Community engagement promotes scale up and sustainability • Integrated packages not investigated as well as single interventions
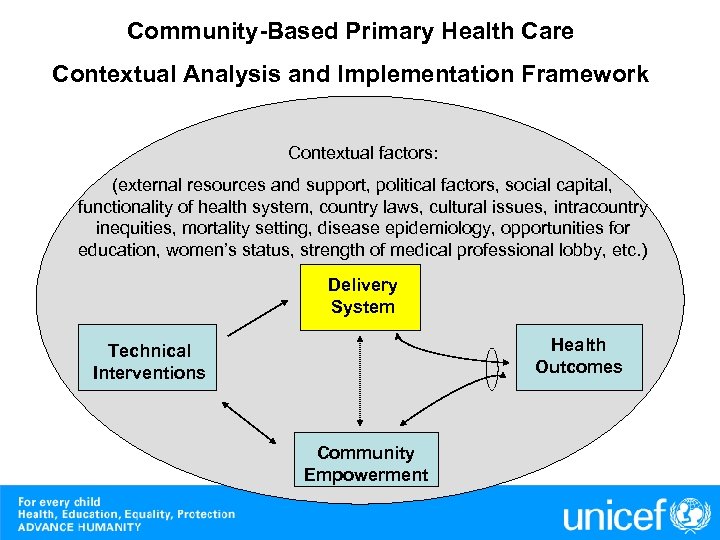 Community-Based Primary Health Care Contextual Analysis and Implementation Framework Contextual factors: (external resources and support, political factors, social capital, functionality of health system, country laws, cultural issues, intracountry inequities, mortality setting, disease epidemiology, opportunities for education, women’s status, strength of medical professional lobby, etc. ) Delivery System Health Outcomes Technical Interventions Community Empowerment
Community-Based Primary Health Care Contextual Analysis and Implementation Framework Contextual factors: (external resources and support, political factors, social capital, functionality of health system, country laws, cultural issues, intracountry inequities, mortality setting, disease epidemiology, opportunities for education, women’s status, strength of medical professional lobby, etc. ) Delivery System Health Outcomes Technical Interventions Community Empowerment
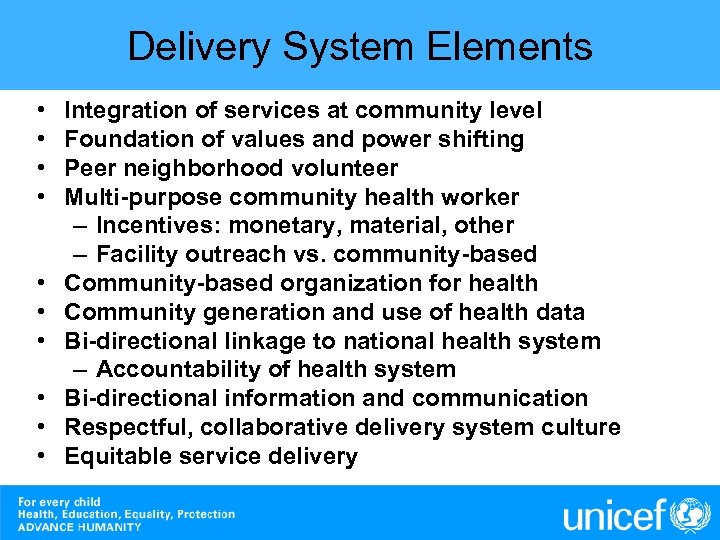 Delivery System Elements • • • Integration of services at community level Foundation of values and power shifting Peer neighborhood volunteer Multi-purpose community health worker – Incentives: monetary, material, other – Facility outreach vs. community-based Community-based organization for health Community generation and use of health data Bi-directional linkage to national health system – Accountability of health system Bi-directional information and communication Respectful, collaborative delivery system culture Equitable service delivery
Delivery System Elements • • • Integration of services at community level Foundation of values and power shifting Peer neighborhood volunteer Multi-purpose community health worker – Incentives: monetary, material, other – Facility outreach vs. community-based Community-based organization for health Community generation and use of health data Bi-directional linkage to national health system – Accountability of health system Bi-directional information and communication Respectful, collaborative delivery system culture Equitable service delivery
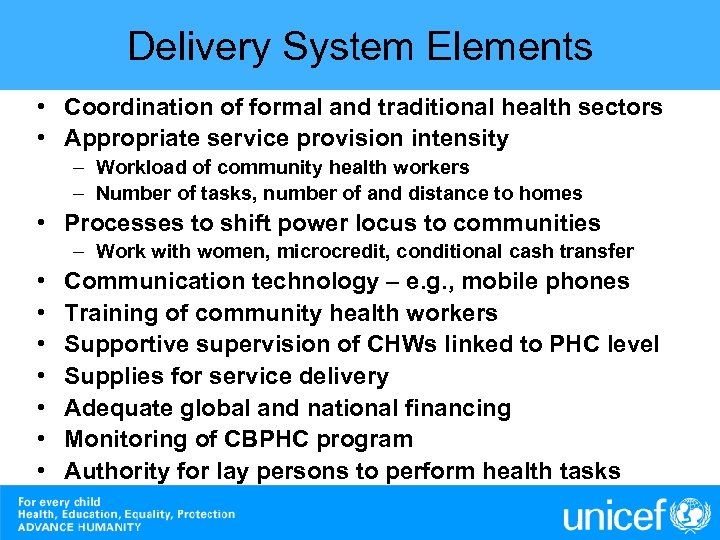 Delivery System Elements • Coordination of formal and traditional health sectors • Appropriate service provision intensity – Workload of community health workers – Number of tasks, number of and distance to homes • Processes to shift power locus to communities – Work with women, microcredit, conditional cash transfer • • Communication technology – e. g. , mobile phones Training of community health workers Supportive supervision of CHWs linked to PHC level Supplies for service delivery Adequate global and national financing Monitoring of CBPHC program Authority for lay persons to perform health tasks
Delivery System Elements • Coordination of formal and traditional health sectors • Appropriate service provision intensity – Workload of community health workers – Number of tasks, number of and distance to homes • Processes to shift power locus to communities – Work with women, microcredit, conditional cash transfer • • Communication technology – e. g. , mobile phones Training of community health workers Supportive supervision of CHWs linked to PHC level Supplies for service delivery Adequate global and national financing Monitoring of CBPHC program Authority for lay persons to perform health tasks
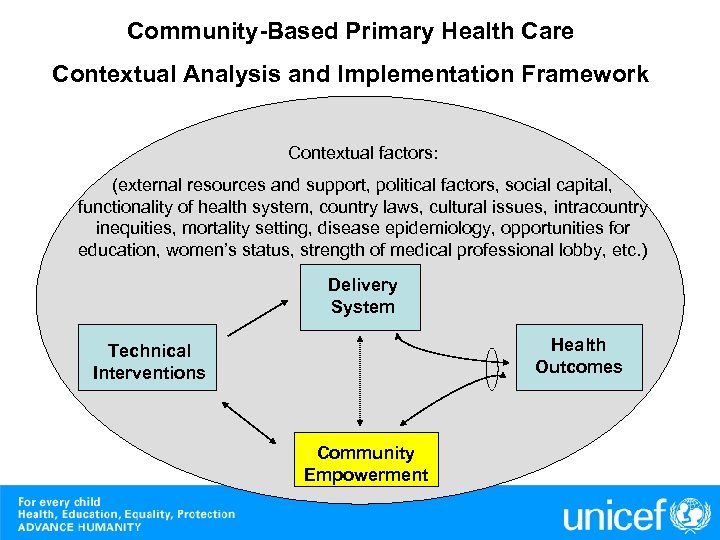 Community-Based Primary Health Care Contextual Analysis and Implementation Framework Contextual factors: (external resources and support, political factors, social capital, functionality of health system, country laws, cultural issues, intracountry inequities, mortality setting, disease epidemiology, opportunities for education, women’s status, strength of medical professional lobby, etc. ) Delivery System Health Outcomes Technical Interventions Community Empowerment
Community-Based Primary Health Care Contextual Analysis and Implementation Framework Contextual factors: (external resources and support, political factors, social capital, functionality of health system, country laws, cultural issues, intracountry inequities, mortality setting, disease epidemiology, opportunities for education, women’s status, strength of medical professional lobby, etc. ) Delivery System Health Outcomes Technical Interventions Community Empowerment
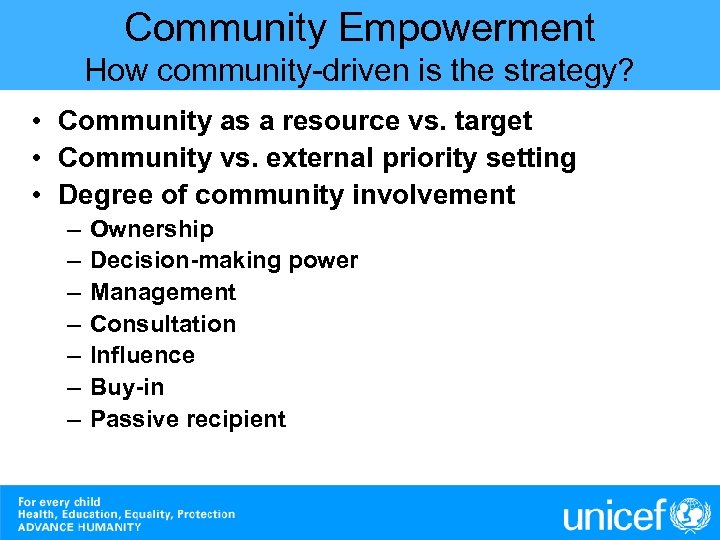 Community Empowerment How community-driven is the strategy? • Community as a resource vs. target • Community vs. external priority setting • Degree of community involvement – – – – Ownership Decision-making power Management Consultation Influence Buy-in Passive recipient
Community Empowerment How community-driven is the strategy? • Community as a resource vs. target • Community vs. external priority setting • Degree of community involvement – – – – Ownership Decision-making power Management Consultation Influence Buy-in Passive recipient
 Community Empowerment Areas requiring community involvement • Leadership • Planning and management • Women • Community management of external resources • Monitoring and evaluation _____________ • • Local context Value system Delivery of services in community Bundle of delivery systems and technical interventions
Community Empowerment Areas requiring community involvement • Leadership • Planning and management • Women • Community management of external resources • Monitoring and evaluation _____________ • • Local context Value system Delivery of services in community Bundle of delivery systems and technical interventions
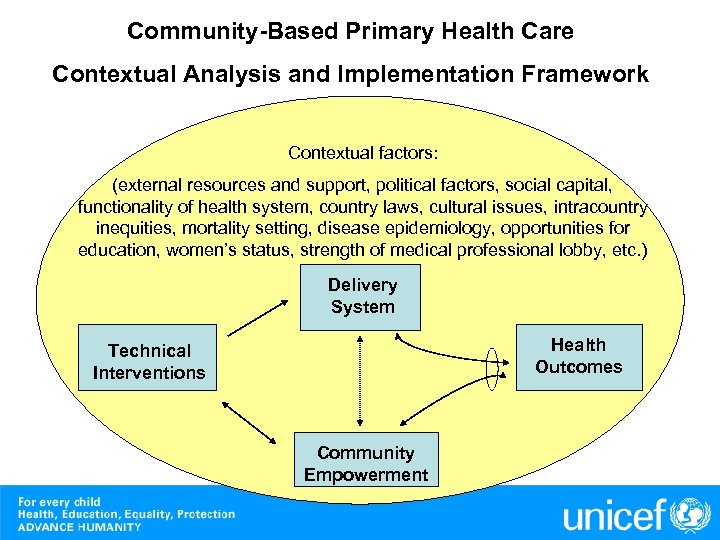 Community-Based Primary Health Care Contextual Analysis and Implementation Framework Contextual factors: (external resources and support, political factors, social capital, functionality of health system, country laws, cultural issues, intracountry inequities, mortality setting, disease epidemiology, opportunities for education, women’s status, strength of medical professional lobby, etc. ) Delivery System Health Outcomes Technical Interventions Community Empowerment
Community-Based Primary Health Care Contextual Analysis and Implementation Framework Contextual factors: (external resources and support, political factors, social capital, functionality of health system, country laws, cultural issues, intracountry inequities, mortality setting, disease epidemiology, opportunities for education, women’s status, strength of medical professional lobby, etc. ) Delivery System Health Outcomes Technical Interventions Community Empowerment
 Key Contextual Factors Ecological Epidemiological Social/Cultural Political Economic Education International funding
Key Contextual Factors Ecological Epidemiological Social/Cultural Political Economic Education International funding
 Recommendations for Implementing CBPHC in Africa 1. 2. 3. 4. 5. 6. “There is no universal solution, but there is a universal process to find appropriate local solutions. ” Carl Taylor Invest in promising CBPHC approaches and field sites, start small, and be willing to help them go to scale within a framework of rigorous evaluation and operations research that demonstrates effectiveness in reducing under-five mortality Look for and support promising young leaders who have a passion for CBPHC or who have the potential for becoming passionate leaders of CBPHC Support opportunities for program leaders to visit and learn from successful experiences – build on success Plan at the outset for long-term sustainability and for the supportive “human” infrastructure required for CBPHC (supervision, training, M&E) Make under-five mortality in defined geographic areas the key outcome indicator and build it into ongoing program operations
Recommendations for Implementing CBPHC in Africa 1. 2. 3. 4. 5. 6. “There is no universal solution, but there is a universal process to find appropriate local solutions. ” Carl Taylor Invest in promising CBPHC approaches and field sites, start small, and be willing to help them go to scale within a framework of rigorous evaluation and operations research that demonstrates effectiveness in reducing under-five mortality Look for and support promising young leaders who have a passion for CBPHC or who have the potential for becoming passionate leaders of CBPHC Support opportunities for program leaders to visit and learn from successful experiences – build on success Plan at the outset for long-term sustainability and for the supportive “human” infrastructure required for CBPHC (supervision, training, M&E) Make under-five mortality in defined geographic areas the key outcome indicator and build it into ongoing program operations
 Next Steps • Forceful statement SOON from the Expert Review Panel to the world (via Lancet? ) – building on the review but moving beyond it • Early completion of the review as originally envisioned • Incorporation of suggestions and recommendation of the Expert Review Panel and others into final report • Broad dissemination of findings
Next Steps • Forceful statement SOON from the Expert Review Panel to the world (via Lancet? ) – building on the review but moving beyond it • Early completion of the review as originally envisioned • Incorporation of suggestions and recommendation of the Expert Review Panel and others into final report • Broad dissemination of findings
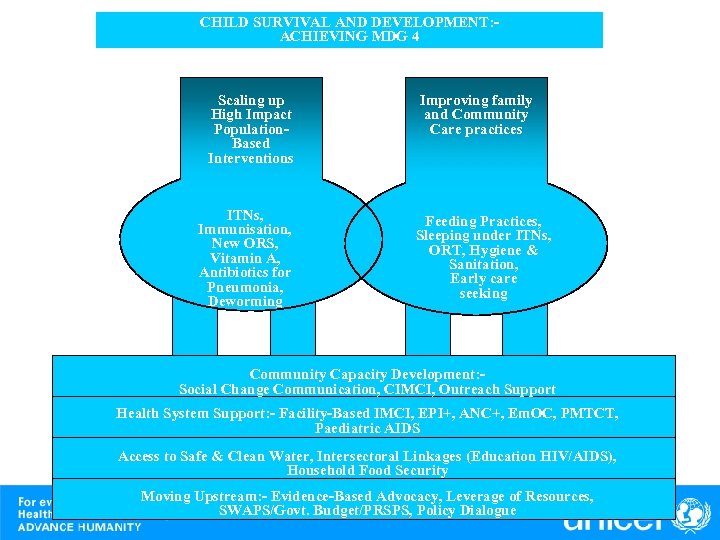 CHILD SURVIVAL AND DEVELOPMENT: ACHIEVING MDG 4 Scaling up High Impact Population. Based Interventions ITNs, Immunisation, New ORS, Vitamin A, Antibiotics for Pneumonia, Deworming Improving family and Community Care practices Feeding Practices, Sleeping under ITNs, ORT, Hygiene & Sanitation, Early care seeking Community Capacity Development: Social Change Communication, CIMCI, Outreach Support Health System Support: - Facility-Based IMCI, EPI+, ANC+, Em. OC, PMTCT, Paediatric AIDS Access to Safe & Clean Water, Intersectoral Linkages (Education HIV/AIDS), Household Food Security Moving Upstream: - Evidence-Based Advocacy, Leverage of Resources, SWAPS/Govt. Budget/PRSPS, Policy Dialogue
CHILD SURVIVAL AND DEVELOPMENT: ACHIEVING MDG 4 Scaling up High Impact Population. Based Interventions ITNs, Immunisation, New ORS, Vitamin A, Antibiotics for Pneumonia, Deworming Improving family and Community Care practices Feeding Practices, Sleeping under ITNs, ORT, Hygiene & Sanitation, Early care seeking Community Capacity Development: Social Change Communication, CIMCI, Outreach Support Health System Support: - Facility-Based IMCI, EPI+, ANC+, Em. OC, PMTCT, Paediatric AIDS Access to Safe & Clean Water, Intersectoral Linkages (Education HIV/AIDS), Household Food Security Moving Upstream: - Evidence-Based Advocacy, Leverage of Resources, SWAPS/Govt. Budget/PRSPS, Policy Dialogue
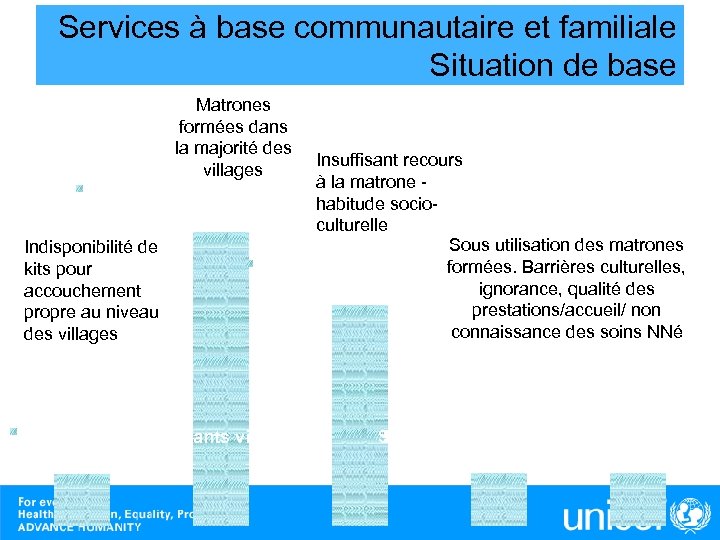 Services à base communautaire et familiale Situation de base Matrones formées dans la majorité des Insuffisant recours villages à la matrone Series 1, Access des matrones F, habitude socio 85. 0% culturelle Sous utilisation des matrones Indisponibilité de formées. Barrières culturelles, Series 1, Acc par matrone, kits pour ignorance, qualité des 63. 9% accouchement prestations/accueil/ non propre au niveau connaissance des soins NNé des villages Series 1, Dispo intrants village, 15. 0% Series 1, Acc par matrones form, + T˚, Series 1, Acc propre + Matrone F 15. 2%
Services à base communautaire et familiale Situation de base Matrones formées dans la majorité des Insuffisant recours villages à la matrone Series 1, Access des matrones F, habitude socio 85. 0% culturelle Sous utilisation des matrones Indisponibilité de formées. Barrières culturelles, Series 1, Acc par matrone, kits pour ignorance, qualité des 63. 9% accouchement prestations/accueil/ non propre au niveau connaissance des soins NNé des villages Series 1, Dispo intrants village, 15. 0% Series 1, Acc par matrones form, + T˚, Series 1, Acc propre + Matrone F 15. 2%
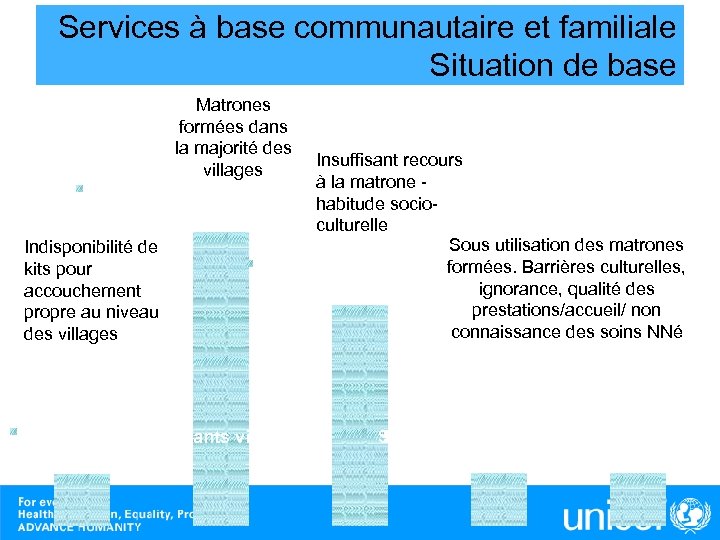 Services à base communautaire et familiale Situation de base Matrones formées dans la majorité des Insuffisant recours villages à la matrone Series 1, Access des matrones F, habitude socio 85. 0% culturelle Sous utilisation des matrones Indisponibilité de formées. Barrières culturelles, Series 1, Acc par matrone, kits pour ignorance, qualité des 63. 9% accouchement prestations/accueil/ non propre au niveau connaissance des soins NNé des villages Series 1, Dispo intrants village, 15. 0% Series 1, Acc par matrones form, + T˚, Series 1, Acc propre + Matrone F 15. 2%
Services à base communautaire et familiale Situation de base Matrones formées dans la majorité des Insuffisant recours villages à la matrone Series 1, Access des matrones F, habitude socio 85. 0% culturelle Sous utilisation des matrones Indisponibilité de formées. Barrières culturelles, Series 1, Acc par matrone, kits pour ignorance, qualité des 63. 9% accouchement prestations/accueil/ non propre au niveau connaissance des soins NNé des villages Series 1, Dispo intrants village, 15. 0% Series 1, Acc par matrones form, + T˚, Series 1, Acc propre + Matrone F 15. 2%
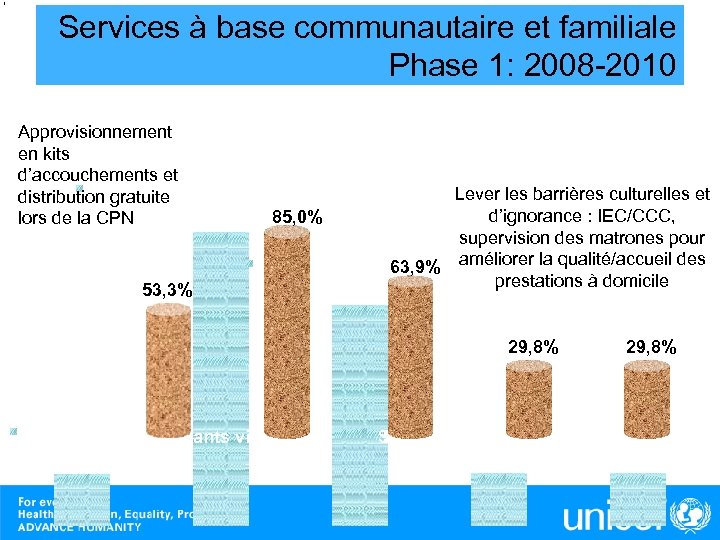 Services à base communautaire et familiale Phase 1: 2008 -2010 Approvisionnement en kits d’accouchements et Series 1, distribution gratuite Access des matrones F, 85. 0% 85, 0% lors de la CPN 53, 3% Lever les barrières culturelles et d’ignorance : IEC/CCC, supervision des matrones pour 63, 9% améliorer la qualité/accueil des Series 1, Acc par matrone, prestations à domicile 63. 9% 29, 8% Series 1, Dispo intrants village, 15. 0% 29, 8% Series 1, Acc par matrones form, + T˚, Series 1, Acc propre + Matrone F 15. 2%
Services à base communautaire et familiale Phase 1: 2008 -2010 Approvisionnement en kits d’accouchements et Series 1, distribution gratuite Access des matrones F, 85. 0% 85, 0% lors de la CPN 53, 3% Lever les barrières culturelles et d’ignorance : IEC/CCC, supervision des matrones pour 63, 9% améliorer la qualité/accueil des Series 1, Acc par matrone, prestations à domicile 63. 9% 29, 8% Series 1, Dispo intrants village, 15. 0% 29, 8% Series 1, Acc par matrones form, + T˚, Series 1, Acc propre + Matrone F 15. 2%
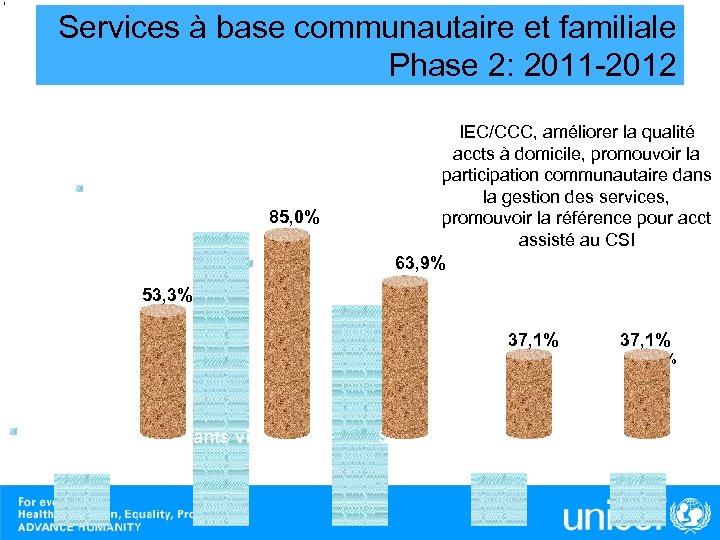 Services à base communautaire et familiale Phase 2: 2011 -2012 IEC/CCC, améliorer la qualité accts à domicile, promouvoir la participation communautaire dans Series 1, Access des matrones F, la gestion des services, 85. 0% 85, 0% promouvoir la référence pour acct assisté au CSI 63, 9% Series 1, Acc par matrone, 53, 3% 63. 9% 37, 1% 29, 8% Series 1, Dispo intrants village, 15. 0% 37, 1% 29, 8% Series 1, Acc par matrones form, + T˚, Series 1, Acc propre + Matrone F 15. 2%
Services à base communautaire et familiale Phase 2: 2011 -2012 IEC/CCC, améliorer la qualité accts à domicile, promouvoir la participation communautaire dans Series 1, Access des matrones F, la gestion des services, 85. 0% 85, 0% promouvoir la référence pour acct assisté au CSI 63, 9% Series 1, Acc par matrone, 53, 3% 63. 9% 37, 1% 29, 8% Series 1, Dispo intrants village, 15. 0% 37, 1% 29, 8% Series 1, Acc par matrones form, + T˚, Series 1, Acc propre + Matrone F 15. 2%
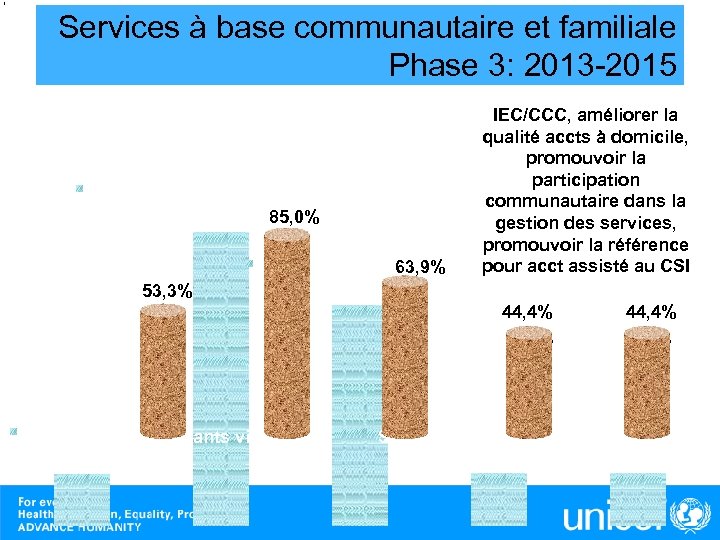 Services à base communautaire et familiale Phase 3: 2013 -2015 IEC/CCC, améliorer la qualité accts à domicile, promouvoir la participation Series 1, Access des matrones F, communautaire dans la 85. 0% 85, 0% gestion des services, promouvoir la référence pour acct assisté au CSI 63, 9% Series 1, Acc par matrone, 63. 9% 53, 3% 44, 4% 37, 1% Series 1, Dispo intrants village, 15. 0% 37, 1% Series 1, Acc par matrones form, + T˚, Series 1, Acc propre + Matrone F 15. 2%
Services à base communautaire et familiale Phase 3: 2013 -2015 IEC/CCC, améliorer la qualité accts à domicile, promouvoir la participation Series 1, Access des matrones F, communautaire dans la 85. 0% 85, 0% gestion des services, promouvoir la référence pour acct assisté au CSI 63, 9% Series 1, Acc par matrone, 63. 9% 53, 3% 44, 4% 37, 1% Series 1, Dispo intrants village, 15. 0% 37, 1% Series 1, Acc par matrones form, + T˚, Series 1, Acc propre + Matrone F 15. 2%
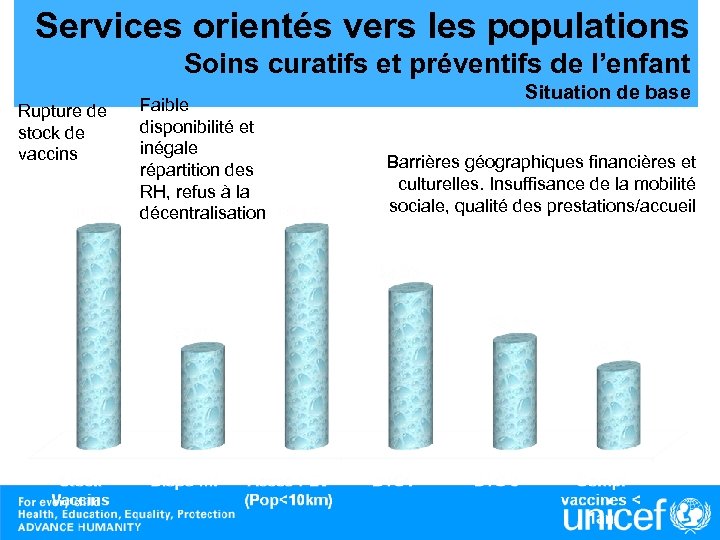 Services orientés vers les populations Soins curatifs et préventifs de l’enfant Rupture de stock de vaccins Faible disponibilité et inégale répartition des RH, refus à la décentralisation Situation de base Barrières géographiques financières et culturelles. Insuffisance de la mobilité sociale, qualité des prestations/accueil
Services orientés vers les populations Soins curatifs et préventifs de l’enfant Rupture de stock de vaccins Faible disponibilité et inégale répartition des RH, refus à la décentralisation Situation de base Barrières géographiques financières et culturelles. Insuffisance de la mobilité sociale, qualité des prestations/accueil
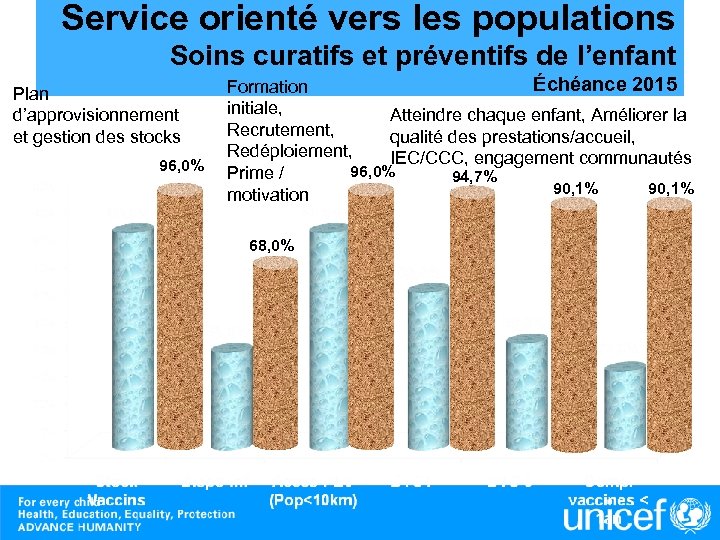 Service orienté vers les populations Soins curatifs et préventifs de l’enfant Plan d’approvisionnement et gestion des stocks 96, 0% Échéance 2015 Formation initiale, Atteindre chaque enfant, Améliorer la Recrutement, qualité des prestations/accueil, Redéploiement, IEC/CCC, engagement communautés 96, 0% Prime / 94, 7% 90, 1% motivation 68, 0%
Service orienté vers les populations Soins curatifs et préventifs de l’enfant Plan d’approvisionnement et gestion des stocks 96, 0% Échéance 2015 Formation initiale, Atteindre chaque enfant, Améliorer la Recrutement, qualité des prestations/accueil, Redéploiement, IEC/CCC, engagement communautés 96, 0% Prime / 94, 7% 90, 1% motivation 68, 0%
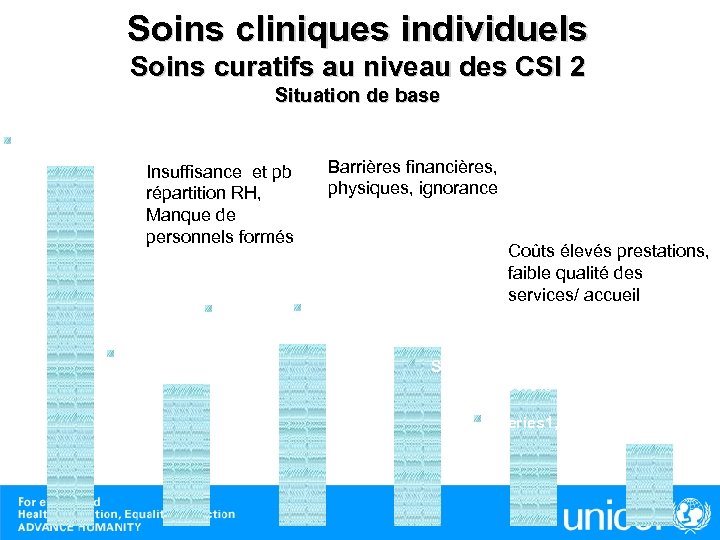 Soins cliniques individuels Soins curatifs au niveau des CSI 2 Situation de base Series 1, Stocks de ME , 95. 0% Insuffisance et pb répartition RH, Manque de personnels formés Barrières financières, physiques, ignorance Coûts élevés prestations, faible qualité des services/ accueil Series 1, 5 km CDS, Fievre soignee ext, 47. 1% 48. 0% Series 1, Infirm. , 37. 3% Series 1, Fievre traite prof, 36. 0% Series 1, Prof forme PCIME, 21. 6%
Soins cliniques individuels Soins curatifs au niveau des CSI 2 Situation de base Series 1, Stocks de ME , 95. 0% Insuffisance et pb répartition RH, Manque de personnels formés Barrières financières, physiques, ignorance Coûts élevés prestations, faible qualité des services/ accueil Series 1, 5 km CDS, Fievre soignee ext, 47. 1% 48. 0% Series 1, Infirm. , 37. 3% Series 1, Fievre traite prof, 36. 0% Series 1, Prof forme PCIME, 21. 6%
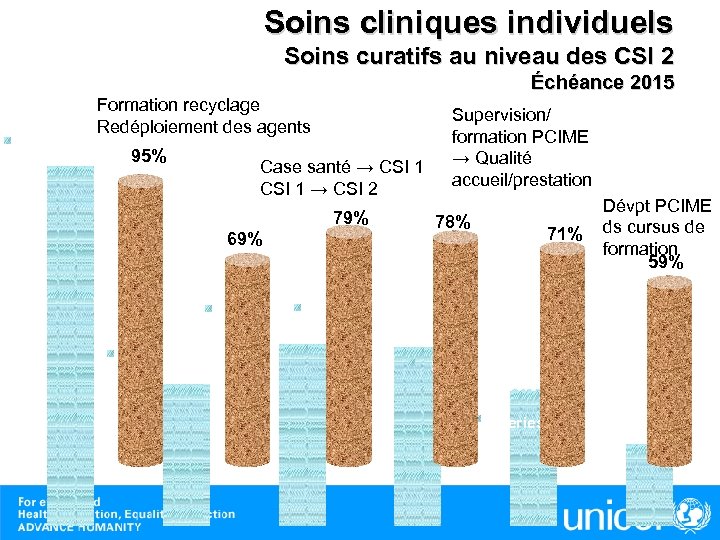 Soins cliniques individuels Soins curatifs au niveau des CSI 2 Échéance 2015 Formation recyclage Redéploiement des agents Series 1, Stocks de ME , 95% 95. 0% Case santé → CSI 1 → CSI 2 79% 69% Supervision/ formation PCIME → Qualité accueil/prestation 78% 71% Dévpt PCIME ds cursus de formation 59% Series 1, 5 km CDS, Fievre soignee ext, 47. 1% 48. 0% Series 1, Infirm. , 37. 3% Series 1, Fievre traite prof, 36. 0% Series 1, Prof forme PCIME, 21. 6%
Soins cliniques individuels Soins curatifs au niveau des CSI 2 Échéance 2015 Formation recyclage Redéploiement des agents Series 1, Stocks de ME , 95% 95. 0% Case santé → CSI 1 → CSI 2 79% 69% Supervision/ formation PCIME → Qualité accueil/prestation 78% 71% Dévpt PCIME ds cursus de formation 59% Series 1, 5 km CDS, Fievre soignee ext, 47. 1% 48. 0% Series 1, Infirm. , 37. 3% Series 1, Fievre traite prof, 36. 0% Series 1, Prof forme PCIME, 21. 6%
 2006: A regional JUMP START: World Press Photo 2005 Scaling up of key health nutrition and WASH evidence based effective interventions
2006: A regional JUMP START: World Press Photo 2005 Scaling up of key health nutrition and WASH evidence based effective interventions
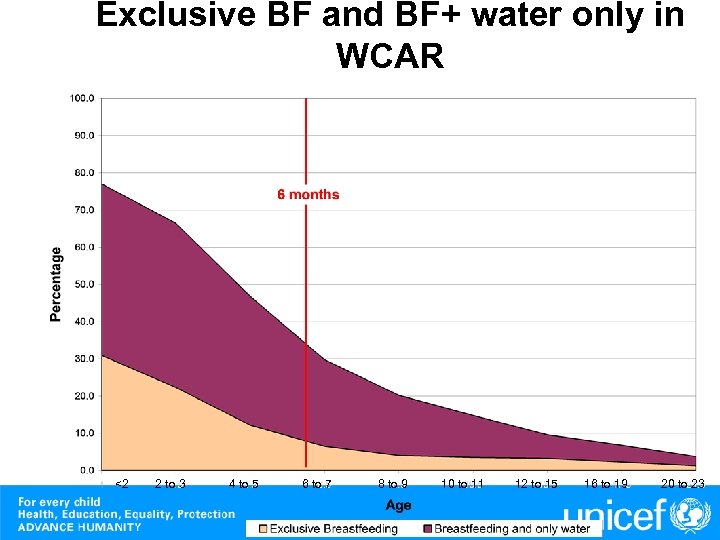 Exclusive BF and BF+ water only in WCAR <2 2 to 3 4 to 5 6 to 7 8 to 9 10 to 11 12 to 15 16 to 19 20 to 23
Exclusive BF and BF+ water only in WCAR <2 2 to 3 4 to 5 6 to 7 8 to 9 10 to 11 12 to 15 16 to 19 20 to 23
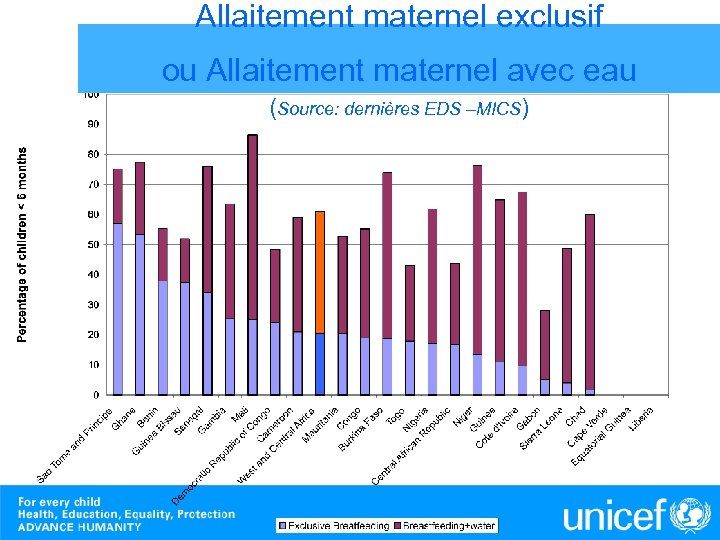 Allaitement maternel exclusif ou Allaitement maternel avec eau (Source: dernières EDS –MICS)
Allaitement maternel exclusif ou Allaitement maternel avec eau (Source: dernières EDS –MICS)
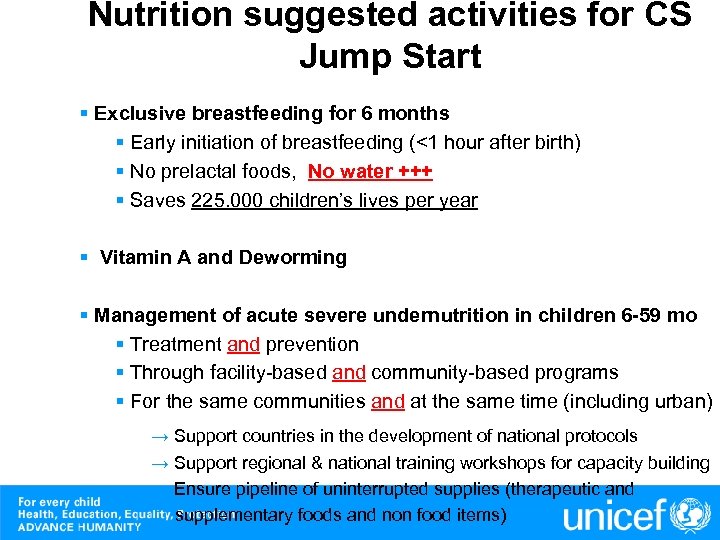 Nutrition suggested activities for CS Jump Start § Exclusive breastfeeding for 6 months § Early initiation of breastfeeding (<1 hour after birth) § No prelactal foods, No water +++ § Saves 225. 000 children’s lives per year § Vitamin A and Deworming § Management of acute severe undernutrition in children 6 -59 mo § Treatment and prevention § Through facility-based and community-based programs § For the same communities and at the same time (including urban) → Support countries in the development of national protocols → Support regional & national training workshops for capacity building → Ensure pipeline of uninterrupted supplies (therapeutic and supplementary foods and non food items)
Nutrition suggested activities for CS Jump Start § Exclusive breastfeeding for 6 months § Early initiation of breastfeeding (<1 hour after birth) § No prelactal foods, No water +++ § Saves 225. 000 children’s lives per year § Vitamin A and Deworming § Management of acute severe undernutrition in children 6 -59 mo § Treatment and prevention § Through facility-based and community-based programs § For the same communities and at the same time (including urban) → Support countries in the development of national protocols → Support regional & national training workshops for capacity building → Ensure pipeline of uninterrupted supplies (therapeutic and supplementary foods and non food items)
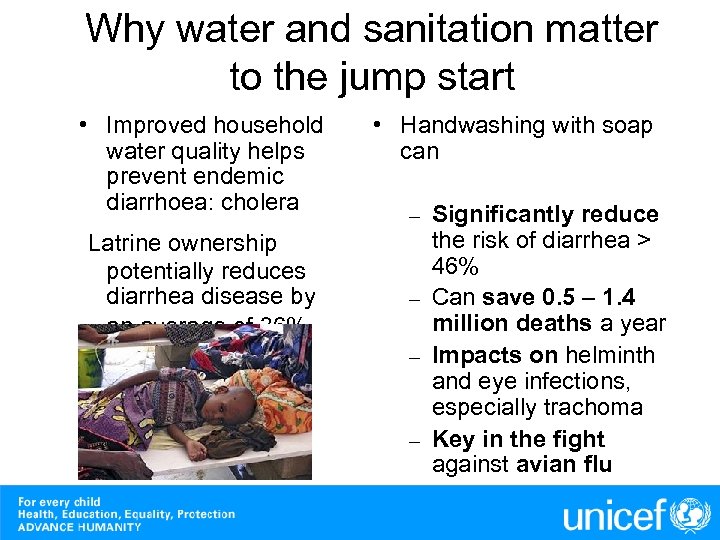 Why water and sanitation matter to the jump start • Improved household water quality helps prevent endemic diarrhoea: cholera Latrine ownership potentially reduces diarrhea disease by an average of 36% • Handwashing with soap can Significantly reduce the risk of diarrhea > 46% – Can save 0. 5 – 1. 4 million deaths a year – Impacts on helminth and eye infections, especially trachoma – Key in the fight against avian flu –
Why water and sanitation matter to the jump start • Improved household water quality helps prevent endemic diarrhoea: cholera Latrine ownership potentially reduces diarrhea disease by an average of 36% • Handwashing with soap can Significantly reduce the risk of diarrhea > 46% – Can save 0. 5 – 1. 4 million deaths a year – Impacts on helminth and eye infections, especially trachoma – Key in the fight against avian flu –
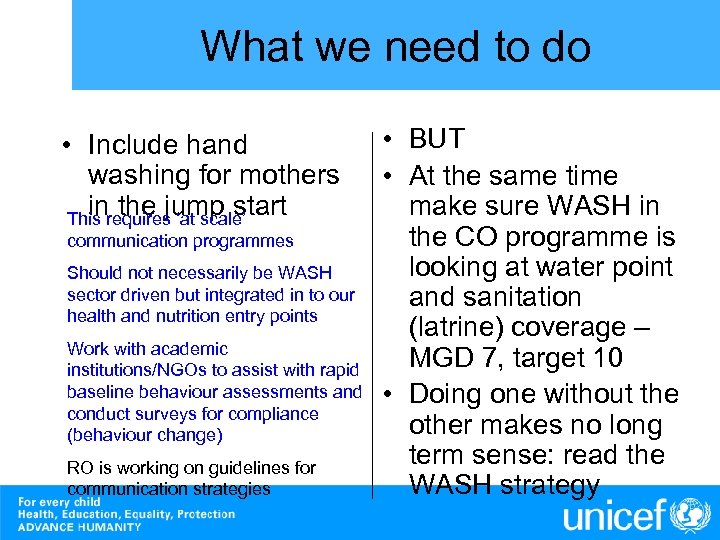 What we need to do • Include hand washing for mothers in the jump start This requires ‘at scale’ communication programmes Should not necessarily be WASH sector driven but integrated in to our health and nutrition entry points Work with academic institutions/NGOs to assist with rapid baseline behaviour assessments and conduct surveys for compliance (behaviour change) RO is working on guidelines for communication strategies • BUT • At the same time make sure WASH in the CO programme is looking at water point and sanitation (latrine) coverage – MGD 7, target 10 • Doing one without the other makes no long term sense: read the WASH strategy
What we need to do • Include hand washing for mothers in the jump start This requires ‘at scale’ communication programmes Should not necessarily be WASH sector driven but integrated in to our health and nutrition entry points Work with academic institutions/NGOs to assist with rapid baseline behaviour assessments and conduct surveys for compliance (behaviour change) RO is working on guidelines for communication strategies • BUT • At the same time make sure WASH in the CO programme is looking at water point and sanitation (latrine) coverage – MGD 7, target 10 • Doing one without the other makes no long term sense: read the WASH strategy
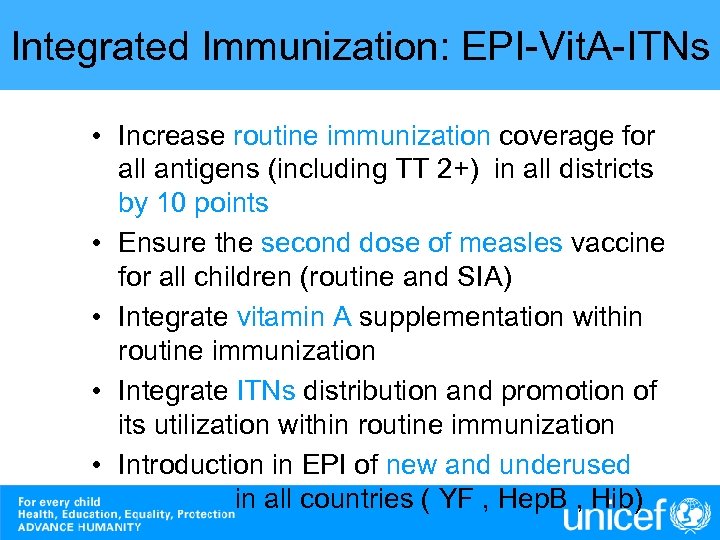 Integrated Immunization: EPI-Vit. A-ITNs • Increase routine immunization coverage for all antigens (including TT 2+) in all districts by 10 points • Ensure the second dose of measles vaccine for all children (routine and SIA) • Integrate vitamin A supplementation within routine immunization • Integrate ITNs distribution and promotion of its utilization within routine immunization • Introduction in EPI of new and underused vaccines in all countries ( YF , Hep. B , Hib)
Integrated Immunization: EPI-Vit. A-ITNs • Increase routine immunization coverage for all antigens (including TT 2+) in all districts by 10 points • Ensure the second dose of measles vaccine for all children (routine and SIA) • Integrate vitamin A supplementation within routine immunization • Integrate ITNs distribution and promotion of its utilization within routine immunization • Introduction in EPI of new and underused vaccines in all countries ( YF , Hep. B , Hib)
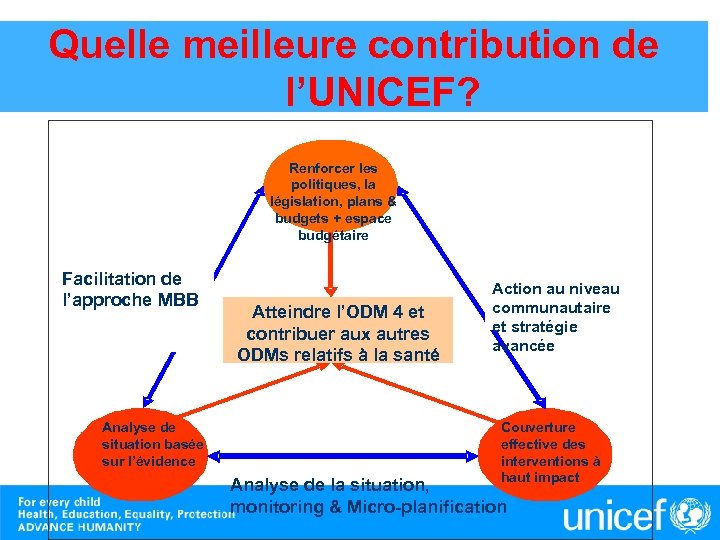 Quelle meilleure contribution de l’UNICEF? Renforcer les politiques, la législation, plans & budgets + espace budgétaire Facilitation de l’approche MBB Analyse de situation basée sur l’évidence Atteindre l’ODM 4 et contribuer aux autres ODMs relatifs à la santé Action au niveau communautaire et stratégie avancée Couverture effective des interventions à haut impact Analyse de la situation, monitoring & Micro-planification
Quelle meilleure contribution de l’UNICEF? Renforcer les politiques, la législation, plans & budgets + espace budgétaire Facilitation de l’approche MBB Analyse de situation basée sur l’évidence Atteindre l’ODM 4 et contribuer aux autres ODMs relatifs à la santé Action au niveau communautaire et stratégie avancée Couverture effective des interventions à haut impact Analyse de la situation, monitoring & Micro-planification


