6e2505a3b4154a82a4f40ec18c283c19.ppt
- Количество слайдов: 51
 Communication, Relationship, and Efficiency in Teams: Educational strategies and tools: Larry Mauksch, M. Ed Senior Lecturer Department of Family Medicine University of Washington
Communication, Relationship, and Efficiency in Teams: Educational strategies and tools: Larry Mauksch, M. Ed Senior Lecturer Department of Family Medicine University of Washington
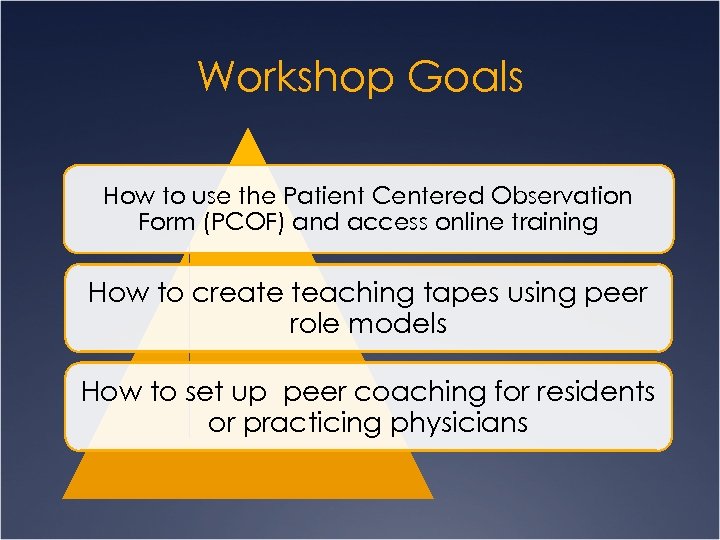 Workshop Goals How to use the Patient Centered Observation Form (PCOF) and access online training How to create teaching tapes using peer role models How to set up peer coaching for residents or practicing physicians
Workshop Goals How to use the Patient Centered Observation Form (PCOF) and access online training How to create teaching tapes using peer role models How to set up peer coaching for residents or practicing physicians
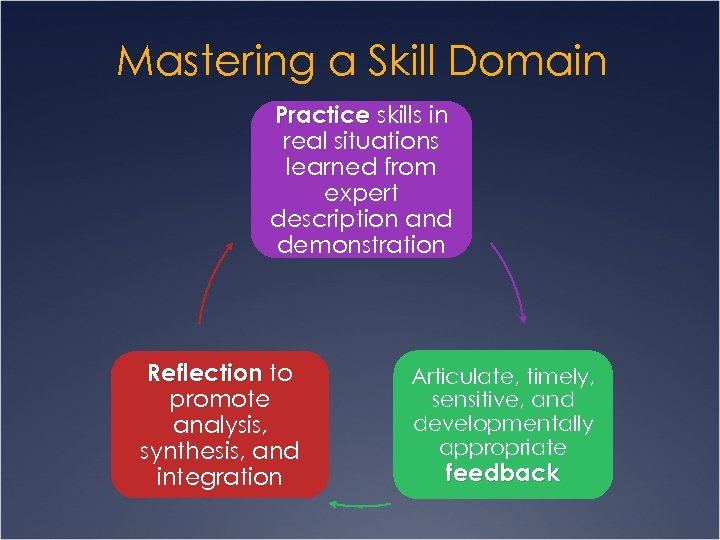 Mastering a Skill Domain Practice skills in real situations learned from expert description and demonstration Reflection to promote analysis, synthesis, and integration Articulate, timely, sensitive, and developmentally appropriate feedback
Mastering a Skill Domain Practice skills in real situations learned from expert description and demonstration Reflection to promote analysis, synthesis, and integration Articulate, timely, sensitive, and developmentally appropriate feedback
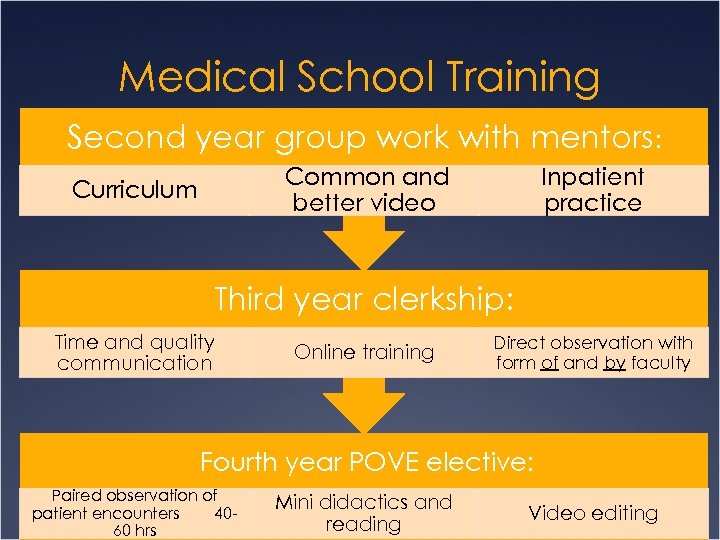 Medical School Training Second year group work with mentors: Common and better video Curriculum Inpatient practice Third year clerkship: Time and quality communication Online training Direct observation with form of and by faculty Fourth year POVE elective: Paired observation of patient encounters 4060 hrs Mini didactics and reading Video editing
Medical School Training Second year group work with mentors: Common and better video Curriculum Inpatient practice Third year clerkship: Time and quality communication Online training Direct observation with form of and by faculty Fourth year POVE elective: Paired observation of patient encounters 4060 hrs Mini didactics and reading Video editing
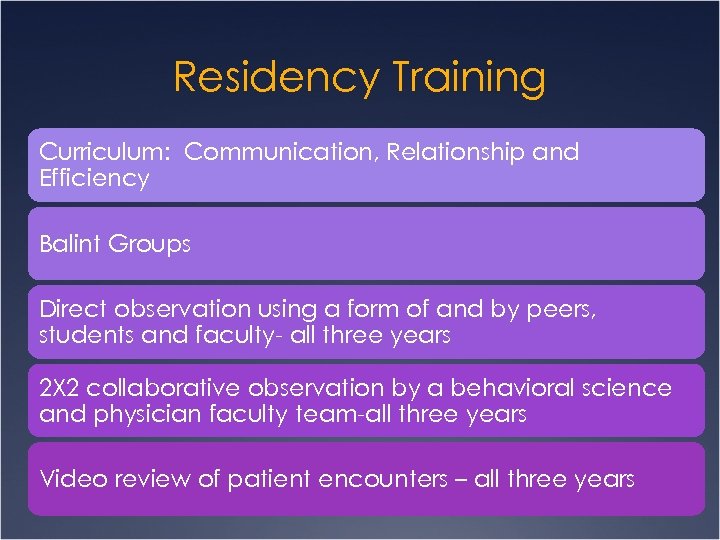 Residency Training Curriculum: Communication, Relationship and Efficiency Balint Groups Direct observation using a form of and by peers, students and faculty- all three years 2 X 2 collaborative observation by a behavioral science and physician faculty team-all three years Video review of patient encounters – all three years
Residency Training Curriculum: Communication, Relationship and Efficiency Balint Groups Direct observation using a form of and by peers, students and faculty- all three years 2 X 2 collaborative observation by a behavioral science and physician faculty team-all three years Video review of patient encounters – all three years
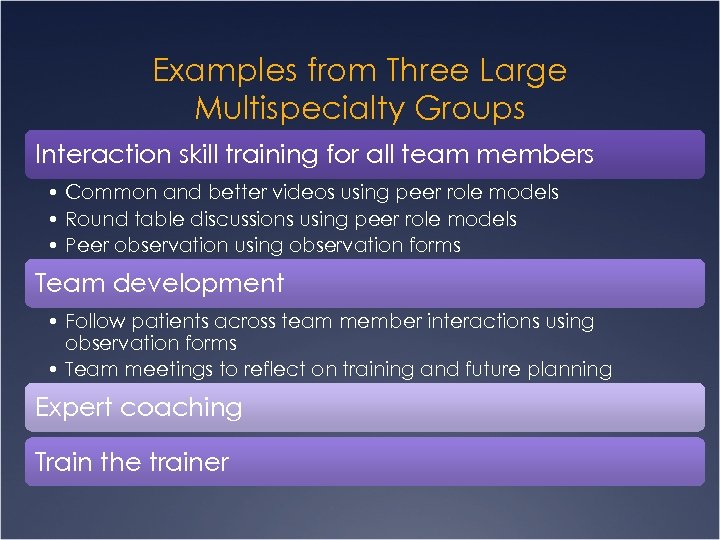 Examples from Three Large Multispecialty Groups Interaction skill training for all team members • Common and better videos using peer role models • Round table discussions using peer role models • Peer observation using observation forms Team development • Follow patients across team member interactions using observation forms • Team meetings to reflect on training and future planning Expert coaching Train the trainer
Examples from Three Large Multispecialty Groups Interaction skill training for all team members • Common and better videos using peer role models • Round table discussions using peer role models • Peer observation using observation forms Team development • Follow patients across team member interactions using observation forms • Team meetings to reflect on training and future planning Expert coaching Train the trainer
 Training Skill differentiation precedes skill integration
Training Skill differentiation precedes skill integration
 Skills That Help Manage Time and Improve Quality
Skills That Help Manage Time and Improve Quality
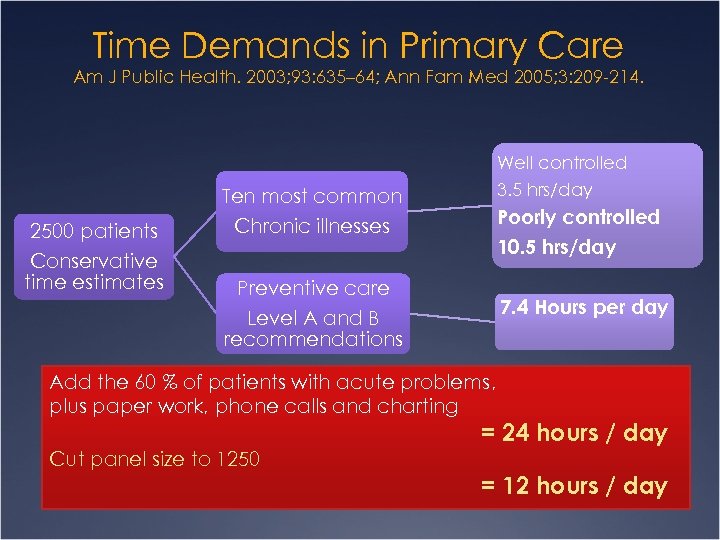 Time Demands in Primary Care Am J Public Health. 2003; 93: 635– 64; Ann Fam Med 2005; 3: 209 -214. Well controlled 2500 patients Conservative time estimates 3. 5 hrs/day Ten most common Chronic illnesses Poorly controlled 10. 5 hrs/day Preventive care Level A and B recommendations 7. 4 Hours per day Add the 60 % of patients with acute problems, plus paper work, phone calls and charting = 24 hours / day Cut panel size to 1250 = 12 hours / day
Time Demands in Primary Care Am J Public Health. 2003; 93: 635– 64; Ann Fam Med 2005; 3: 209 -214. Well controlled 2500 patients Conservative time estimates 3. 5 hrs/day Ten most common Chronic illnesses Poorly controlled 10. 5 hrs/day Preventive care Level A and B recommendations 7. 4 Hours per day Add the 60 % of patients with acute problems, plus paper work, phone calls and charting = 24 hours / day Cut panel size to 1250 = 12 hours / day
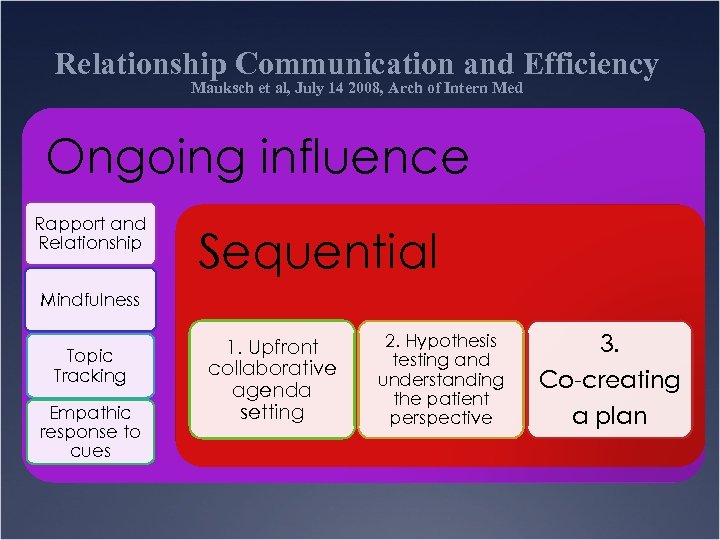 Relationship Communication and Efficiency Mauksch et al, July 14 2008, Arch of Intern Med Ongoing influence Rapport and Relationship Sequential Mindfulness Topic Tracking Empathic response to cues 1. Upfront collaborative agenda setting 2. Hypothesis testing and understanding the patient perspective 3. Co-creating a plan
Relationship Communication and Efficiency Mauksch et al, July 14 2008, Arch of Intern Med Ongoing influence Rapport and Relationship Sequential Mindfulness Topic Tracking Empathic response to cues 1. Upfront collaborative agenda setting 2. Hypothesis testing and understanding the patient perspective 3. Co-creating a plan
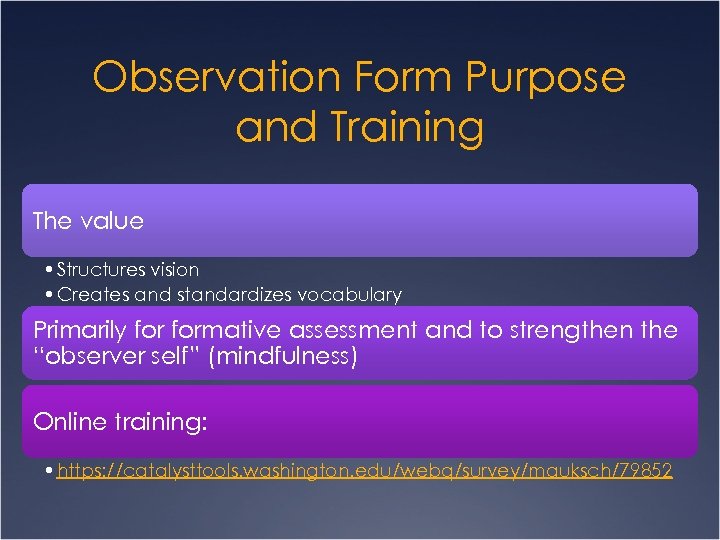 Observation Form Purpose and Training The value • Structures vision • Creates and standardizes vocabulary Primarily formative assessment and to strengthen the “observer self” (mindfulness) Online training: • https: //catalysttools. washington. edu/webq/survey/mauksch/79852
Observation Form Purpose and Training The value • Structures vision • Creates and standardizes vocabulary Primarily formative assessment and to strengthen the “observer self” (mindfulness) Online training: • https: //catalysttools. washington. edu/webq/survey/mauksch/79852
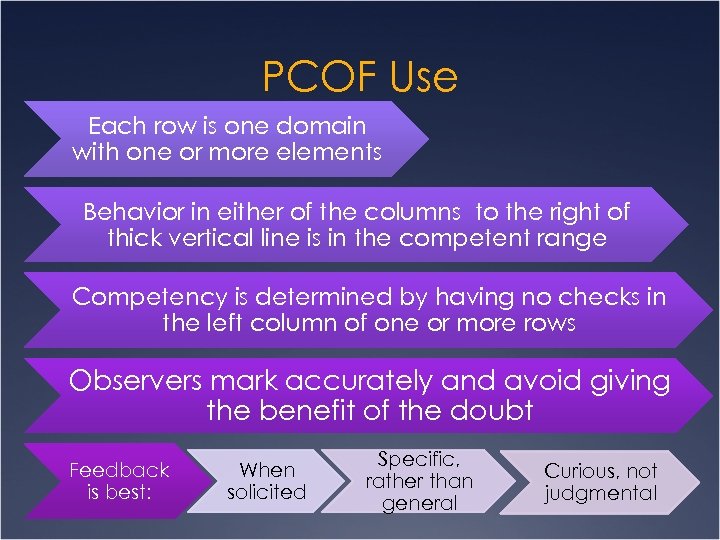 PCOF Use Each row is one domain with one or more elements Behavior in either of the columns to the right of thick vertical line is in the competent range Competency is determined by having no checks in the left column of one or more rows Observers mark accurately and avoid giving the benefit of the doubt Feedback is best: When solicited Specific, rather than general Curious, not judgmental
PCOF Use Each row is one domain with one or more elements Behavior in either of the columns to the right of thick vertical line is in the competent range Competency is determined by having no checks in the left column of one or more rows Observers mark accurately and avoid giving the benefit of the doubt Feedback is best: When solicited Specific, rather than general Curious, not judgmental
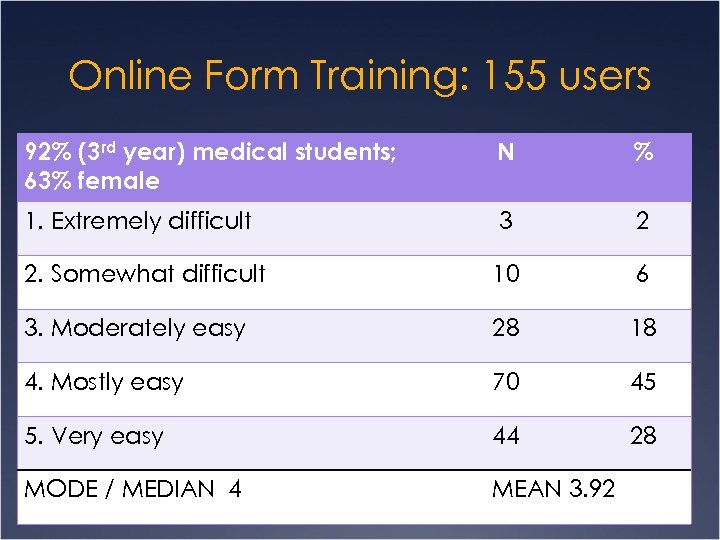 Online Form Training: 155 users 92% (3 rd year) medical students; 63% female N % 1. Extremely difficult 3 2 2. Somewhat difficult 10 6 3. Moderately easy 28 18 4. Mostly easy 70 45 5. Very easy 44 28 MODE / MEDIAN 4 MEAN 3. 92
Online Form Training: 155 users 92% (3 rd year) medical students; 63% female N % 1. Extremely difficult 3 2 2. Somewhat difficult 10 6 3. Moderately easy 28 18 4. Mostly easy 70 45 5. Very easy 44 28 MODE / MEDIAN 4 MEAN 3. 92
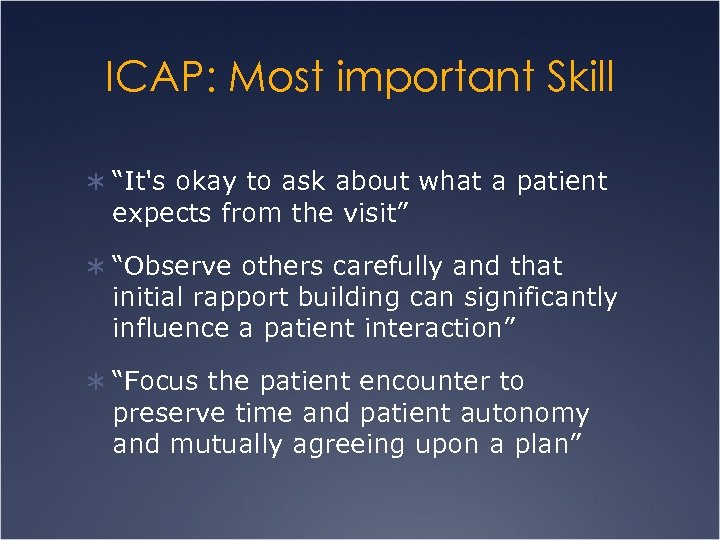 ICAP: Most important Skill Ü “It's okay to ask about what a patient expects from the visit” Ü “Observe others carefully and that initial rapport building can significantly influence a patient interaction” Ü “Focus the patient encounter to preserve time and patient autonomy and mutually agreeing upon a plan”
ICAP: Most important Skill Ü “It's okay to ask about what a patient expects from the visit” Ü “Observe others carefully and that initial rapport building can significantly influence a patient interaction” Ü “Focus the patient encounter to preserve time and patient autonomy and mutually agreeing upon a plan”
 ICAP-Concepts or skills you are confused about? Ü None or nothing 25 Ü “in the co-creating part, what to be flexible about” Ü “Balance between psychosocial part and efficiency” Ü “aren’t there times when some skills are more appropriate? ” Ü “I think I need more practice with organization”
ICAP-Concepts or skills you are confused about? Ü None or nothing 25 Ü “in the co-creating part, what to be flexible about” Ü “Balance between psychosocial part and efficiency” Ü “aren’t there times when some skills are more appropriate? ” Ü “I think I need more practice with organization”
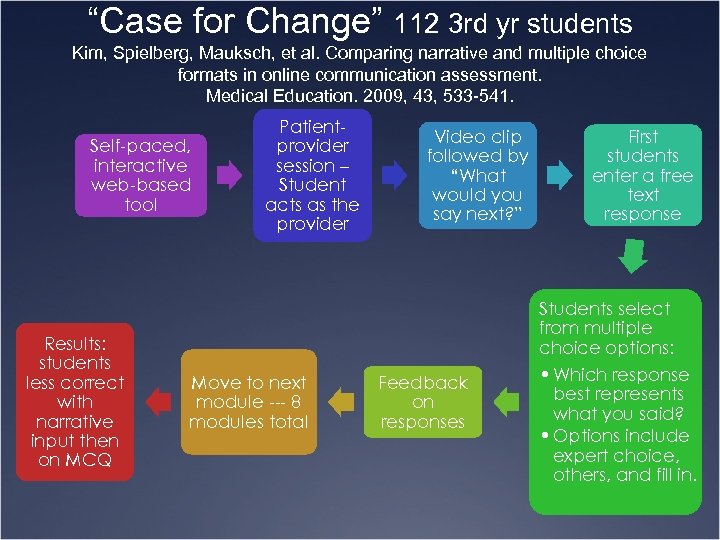 “Case for Change” 112 3 rd yr students Kim, Spielberg, Mauksch, et al. Comparing narrative and multiple choice formats in online communication assessment. Medical Education. 2009, 43, 533 -541. Self-paced, interactive web-based tool Results: students less correct with narrative input then on MCQ Patientprovider session – Student acts as the provider Move to next module --- 8 modules total Video clip followed by “What would you say next? ” Feedback on responses First students enter a free text response Students select from multiple choice options: • Which response best represents what you said? • Options include expert choice, others, and fill in.
“Case for Change” 112 3 rd yr students Kim, Spielberg, Mauksch, et al. Comparing narrative and multiple choice formats in online communication assessment. Medical Education. 2009, 43, 533 -541. Self-paced, interactive web-based tool Results: students less correct with narrative input then on MCQ Patientprovider session – Student acts as the provider Move to next module --- 8 modules total Video clip followed by “What would you say next? ” Feedback on responses First students enter a free text response Students select from multiple choice options: • Which response best represents what you said? • Options include expert choice, others, and fill in.
 Common and Better Video Common Missing core skills • Should not be bad caricature • Better if observer rates it and doesn’t see much to improve Better Re-create the scenario but with core skills • Should be better, but not perfect • Make both videos the same length
Common and Better Video Common Missing core skills • Should not be bad caricature • Better if observer rates it and doesn’t see much to improve Better Re-create the scenario but with core skills • Should be better, but not perfect • Make both videos the same length
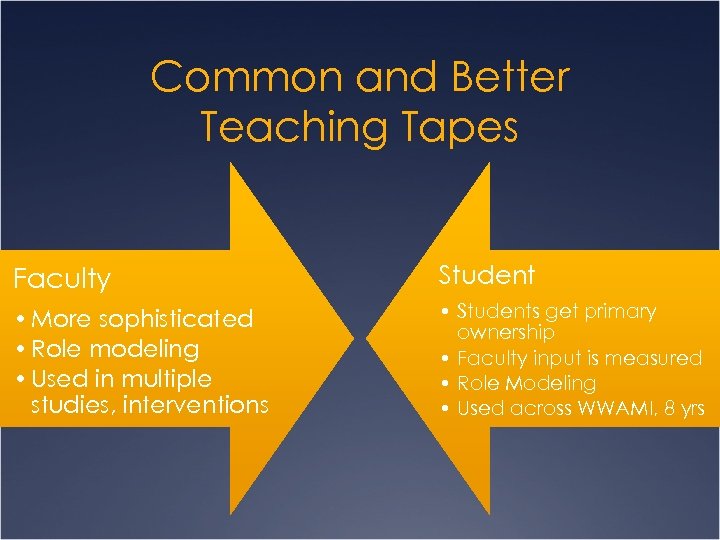 Common and Better Teaching Tapes Faculty Student • More sophisticated • Role modeling • Used in multiple studies, interventions • Students get primary ownership • Faculty input is measured • Role Modeling • Used across WWAMI, 8 yrs
Common and Better Teaching Tapes Faculty Student • More sophisticated • Role modeling • Used in multiple studies, interventions • Students get primary ownership • Faculty input is measured • Role Modeling • Used across WWAMI, 8 yrs
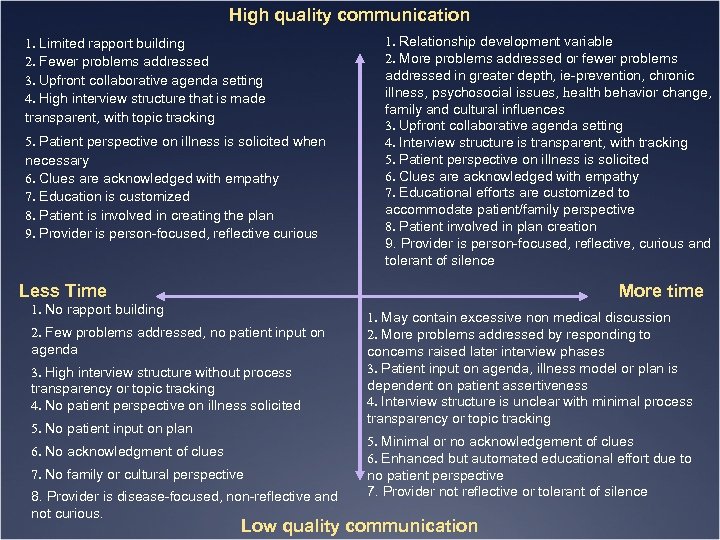 High quality communication 1. Limited rapport building 2. Fewer problems addressed 3. Upfront collaborative agenda setting 4. High interview structure that is made transparent, with topic tracking 5. Patient perspective on illness is solicited when necessary 6. Clues are acknowledged with empathy 7. Education is customized 8. Patient is involved in creating the plan 9. Provider is person-focused, reflective curious 1. Relationship development variable 2. More problems addressed or fewer problems addressed in greater depth, ie-prevention, chronic illness, psychosocial issues, health behavior change, family and cultural influences 3. Upfront collaborative agenda setting 4. Interview structure is transparent, with tracking 5. Patient perspective on illness is solicited 6. Clues are acknowledged with empathy 7. Educational efforts are customized to accommodate patient/family perspective 8. Patient involved in plan creation 9. Provider is person-focused, reflective, curious and tolerant of silence Less Time More time 1. No rapport building 2. Few problems addressed, no patient input on agenda 3. High interview structure without process transparency or topic tracking 4. No patient perspective on illness solicited 5. No patient input on plan 6. No acknowledgment of clues 7. No family or cultural perspective 8. Provider is disease-focused, non-reflective and not curious. 1. May contain excessive non medical discussion 2. More problems addressed by responding to concerns raised later interview phases 3. Patient input on agenda, illness model or plan is dependent on patient assertiveness 4. Interview structure is unclear with minimal process transparency or topic tracking 5. Minimal or no acknowledgement of clues 6. Enhanced but automated educational effort due to no patient perspective 7. Provider not reflective or tolerant of silence Low quality communication
High quality communication 1. Limited rapport building 2. Fewer problems addressed 3. Upfront collaborative agenda setting 4. High interview structure that is made transparent, with topic tracking 5. Patient perspective on illness is solicited when necessary 6. Clues are acknowledged with empathy 7. Education is customized 8. Patient is involved in creating the plan 9. Provider is person-focused, reflective curious 1. Relationship development variable 2. More problems addressed or fewer problems addressed in greater depth, ie-prevention, chronic illness, psychosocial issues, health behavior change, family and cultural influences 3. Upfront collaborative agenda setting 4. Interview structure is transparent, with tracking 5. Patient perspective on illness is solicited 6. Clues are acknowledged with empathy 7. Educational efforts are customized to accommodate patient/family perspective 8. Patient involved in plan creation 9. Provider is person-focused, reflective, curious and tolerant of silence Less Time More time 1. No rapport building 2. Few problems addressed, no patient input on agenda 3. High interview structure without process transparency or topic tracking 4. No patient perspective on illness solicited 5. No patient input on plan 6. No acknowledgment of clues 7. No family or cultural perspective 8. Provider is disease-focused, non-reflective and not curious. 1. May contain excessive non medical discussion 2. More problems addressed by responding to concerns raised later interview phases 3. Patient input on agenda, illness model or plan is dependent on patient assertiveness 4. Interview structure is unclear with minimal process transparency or topic tracking 5. Minimal or no acknowledgement of clues 6. Enhanced but automated educational effort due to no patient perspective 7. Provider not reflective or tolerant of silence Low quality communication
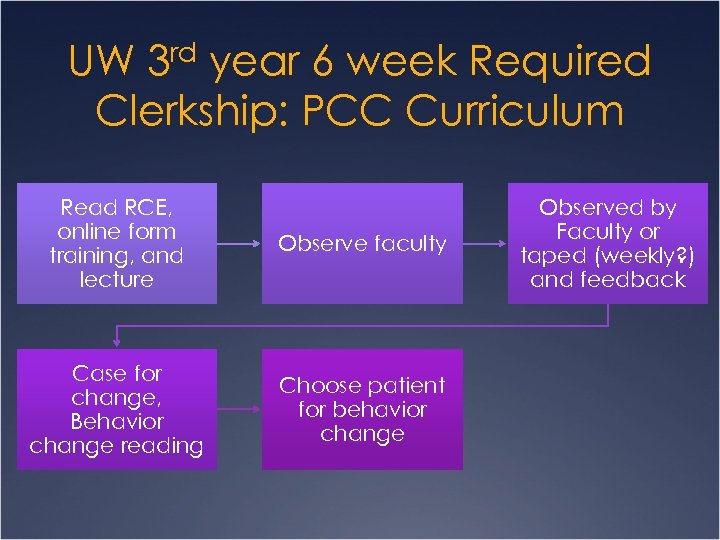 UW 3 rd year 6 week Required Clerkship: PCC Curriculum Read RCE, online form training, and lecture Observe faculty Case for change, Behavior change reading Choose patient for behavior change Observed by Faculty or taped (weekly? ) and feedback
UW 3 rd year 6 week Required Clerkship: PCC Curriculum Read RCE, online form training, and lecture Observe faculty Case for change, Behavior change reading Choose patient for behavior change Observed by Faculty or taped (weekly? ) and feedback
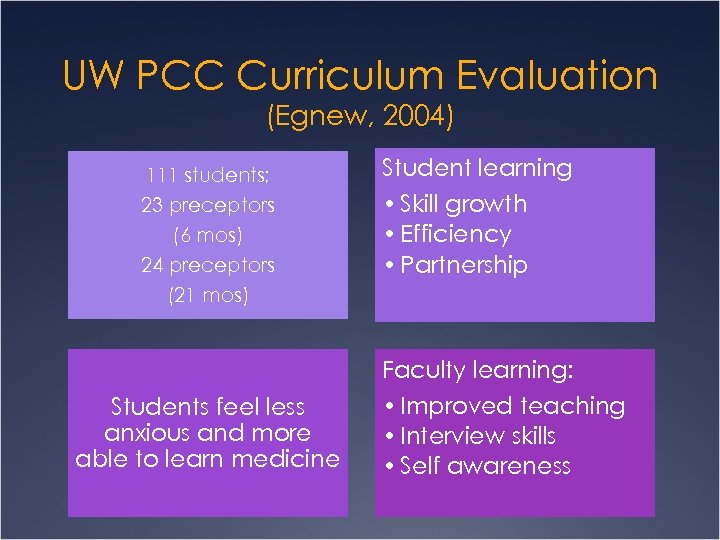 UW PCC Curriculum Evaluation (Egnew, 2004) 111 students; 23 preceptors (6 mos) 24 preceptors (21 mos) Student learning • Skill growth • Efficiency • Partnership Faculty learning: Students feel less anxious and more able to learn medicine • Improved teaching • Interview skills • Self awareness
UW PCC Curriculum Evaluation (Egnew, 2004) 111 students; 23 preceptors (6 mos) 24 preceptors (21 mos) Student learning • Skill growth • Efficiency • Partnership Faculty learning: Students feel less anxious and more able to learn medicine • Improved teaching • Interview skills • Self awareness
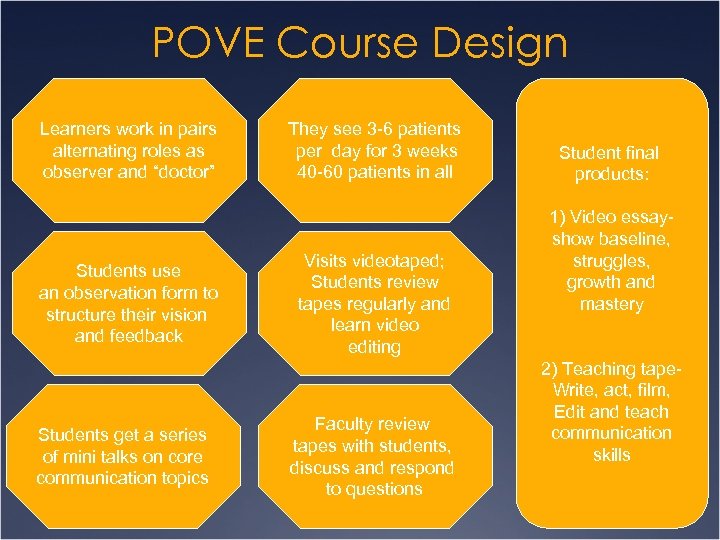 POVE Course Design Learners work in pairs alternating roles as observer and “doctor” Students use an observation form to structure their vision and feedback Students get a series of mini talks on core communication topics They see 3 -6 patients per day for 3 weeks 40 -60 patients in all Visits videotaped; Students review tapes regularly and learn video editing Faculty review tapes with students, discuss and respond to questions Student final products: 1) Video essayshow baseline, struggles, growth and mastery 2) Teaching tape. Write, act, film, Edit and teach communication skills
POVE Course Design Learners work in pairs alternating roles as observer and “doctor” Students use an observation form to structure their vision and feedback Students get a series of mini talks on core communication topics They see 3 -6 patients per day for 3 weeks 40 -60 patients in all Visits videotaped; Students review tapes regularly and learn video editing Faculty review tapes with students, discuss and respond to questions Student final products: 1) Video essayshow baseline, struggles, growth and mastery 2) Teaching tape. Write, act, film, Edit and teach communication skills
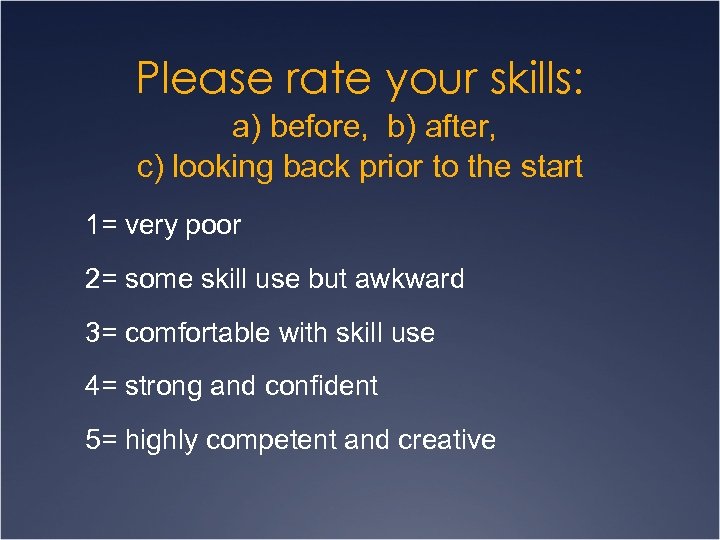 Please rate your skills: a) before, b) after, c) looking back prior to the start 1= very poor 2= some skill use but awkward 3= comfortable with skill use 4= strong and confident 5= highly competent and creative
Please rate your skills: a) before, b) after, c) looking back prior to the start 1= very poor 2= some skill use but awkward 3= comfortable with skill use 4= strong and confident 5= highly competent and creative
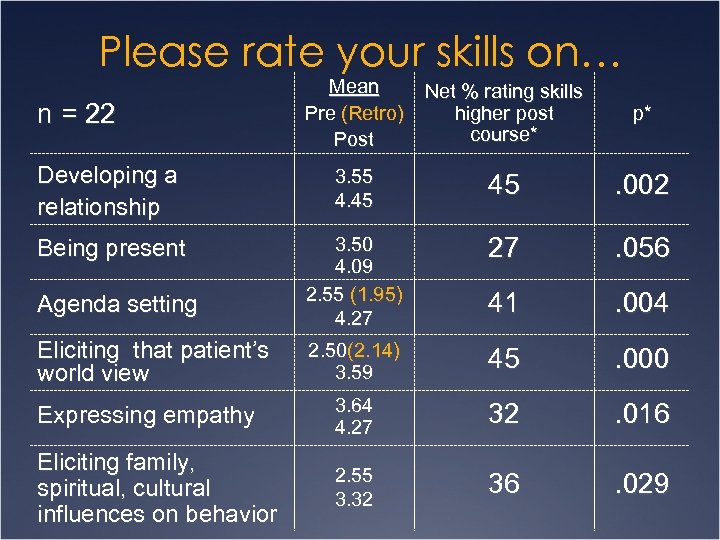 Please rate your skills on… Mean Pre (Retro) Post Net % rating skills higher post course* p* Developing a relationship 3. 55 4. 45 45 . 002 Being present 3. 50 4. 09 2. 55 (1. 95) 4. 27 27 . 056 41 . 004 2. 50(2. 14) 3. 59 45 . 000 Expressing empathy 3. 64 4. 27 32 . 016 Eliciting family, spiritual, cultural influences on behavior 2. 55 3. 32 36 . 029 n = 22 Agenda setting Eliciting that patient’s world view
Please rate your skills on… Mean Pre (Retro) Post Net % rating skills higher post course* p* Developing a relationship 3. 55 4. 45 45 . 002 Being present 3. 50 4. 09 2. 55 (1. 95) 4. 27 27 . 056 41 . 004 2. 50(2. 14) 3. 59 45 . 000 Expressing empathy 3. 64 4. 27 32 . 016 Eliciting family, spiritual, cultural influences on behavior 2. 55 3. 32 36 . 029 n = 22 Agenda setting Eliciting that patient’s world view
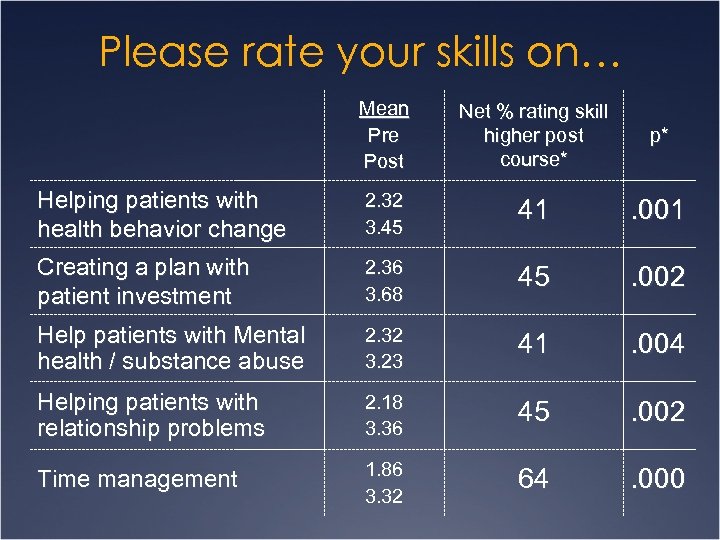 Please rate your skills on… Mean Pre Post Net % rating skill higher post course* p* Helping patients with health behavior change 2. 32 3. 45 41 . 001 Creating a plan with patient investment 2. 36 3. 68 45 . 002 Help patients with Mental health / substance abuse 2. 32 3. 23 41 . 004 Helping patients with relationship problems 2. 18 3. 36 45 . 002 Time management 1. 86 3. 32 64 . 000
Please rate your skills on… Mean Pre Post Net % rating skill higher post course* p* Helping patients with health behavior change 2. 32 3. 45 41 . 001 Creating a plan with patient investment 2. 36 3. 68 45 . 002 Help patients with Mental health / substance abuse 2. 32 3. 23 41 . 004 Helping patients with relationship problems 2. 18 3. 36 45 . 002 Time management 1. 86 3. 32 64 . 000
 Student Feedback: POVE Course Components 1. Detracted from my educational experience 2. Neutral value 3. Mild value 4. Moderate value 5. Strong Value 6. Highest Value
Student Feedback: POVE Course Components 1. Detracted from my educational experience 2. Neutral value 3. Mild value 4. Moderate value 5. Strong Value 6. Highest Value
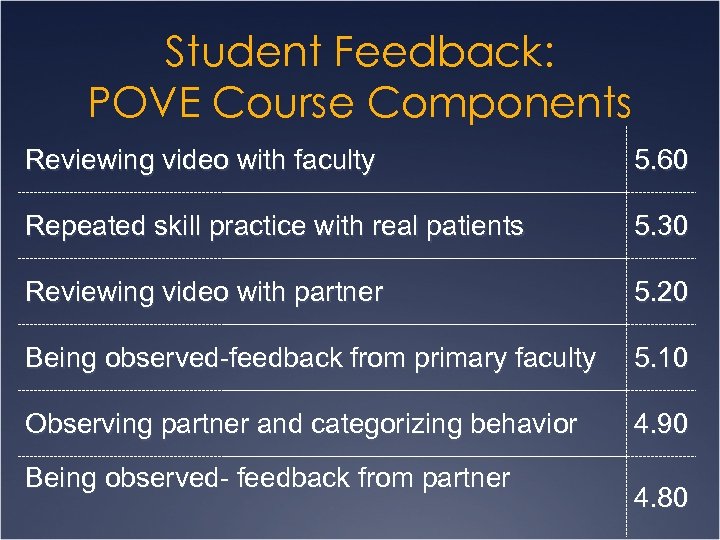 Student Feedback: POVE Course Components Reviewing video with faculty 5. 60 Repeated skill practice with real patients 5. 30 Reviewing video with partner 5. 20 Being observed-feedback from primary faculty 5. 10 Observing partner and categorizing behavior 4. 90 Being observed- feedback from partner 4. 80
Student Feedback: POVE Course Components Reviewing video with faculty 5. 60 Repeated skill practice with real patients 5. 30 Reviewing video with partner 5. 20 Being observed-feedback from primary faculty 5. 10 Observing partner and categorizing behavior 4. 90 Being observed- feedback from partner 4. 80
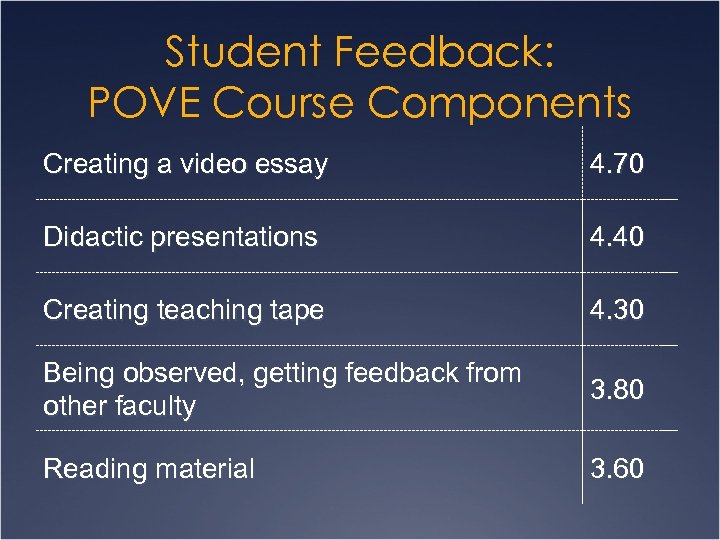 Student Feedback: POVE Course Components Creating a video essay 4. 70 Didactic presentations 4. 40 Creating teaching tape 4. 30 Being observed, getting feedback from other faculty 3. 80 Reading material 3. 60
Student Feedback: POVE Course Components Creating a video essay 4. 70 Didactic presentations 4. 40 Creating teaching tape 4. 30 Being observed, getting feedback from other faculty 3. 80 Reading material 3. 60
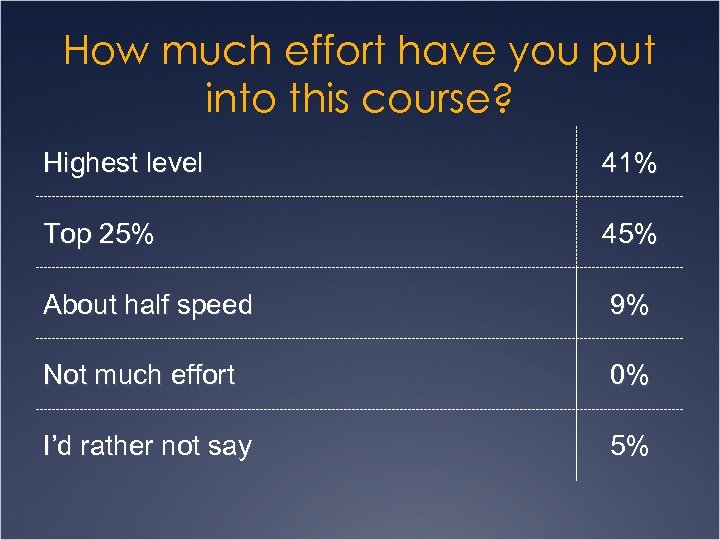 How much effort have you put into this course? Highest level 41% Top 25% 45% About half speed 9% Not much effort 0% I’d rather not say 5%
How much effort have you put into this course? Highest level 41% Top 25% 45% About half speed 9% Not much effort 0% I’d rather not say 5%
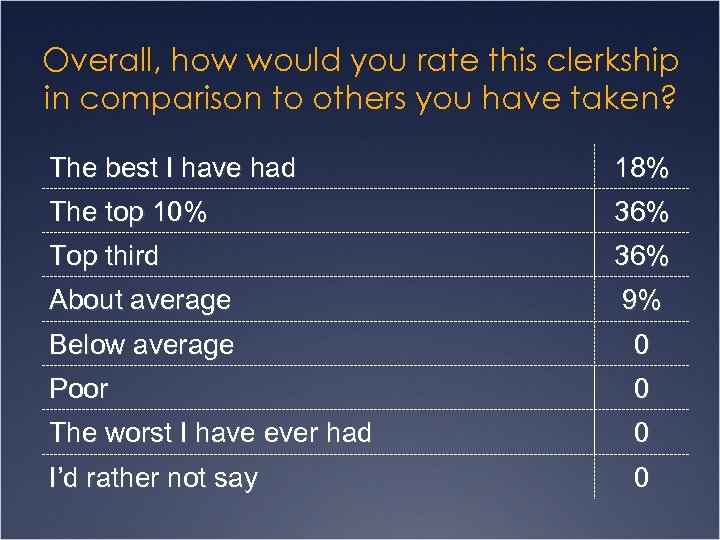 Overall, how would you rate this clerkship in comparison to others you have taken? The best I have had 18% The top 10% 36% Top third 36% About average 9% Below average 0 Poor 0 The worst I have ever had 0 I’d rather not say 0
Overall, how would you rate this clerkship in comparison to others you have taken? The best I have had 18% The top 10% 36% Top third 36% About average 9% Below average 0 Poor 0 The worst I have ever had 0 I’d rather not say 0
 Most rewarding form of teaching Ü Student centered, adult learning, student excitement when feeling a sense of mastery. Ü Close relationships with students Ü Use of educational design- video review Ü Using POVE products to create interest and teach others
Most rewarding form of teaching Ü Student centered, adult learning, student excitement when feeling a sense of mastery. Ü Close relationships with students Ü Use of educational design- video review Ü Using POVE products to create interest and teach others
 Ways to adapt POVE elsewhere Ü Use paired observation with forms with residents and colleagues Ü Self development as teacher and clinician using direct observation Ü Use of video essays and teaching tapes in other educational forums
Ways to adapt POVE elsewhere Ü Use paired observation with forms with residents and colleagues Ü Self development as teacher and clinician using direct observation Ü Use of video essays and teaching tapes in other educational forums
 Have you noticed changes in your clinical practice? Ü Yes 11; No 2 Ü Describe the changes Ü Mindfulness Ü Tuned in to residents and students in the moment Ü Reflection Ü Better awareness of skills I tried to implement Ü Communication skills Ü Agenda setting Ü Patient perspective Ü Communication while using an EHR
Have you noticed changes in your clinical practice? Ü Yes 11; No 2 Ü Describe the changes Ü Mindfulness Ü Tuned in to residents and students in the moment Ü Reflection Ü Better awareness of skills I tried to implement Ü Communication skills Ü Agenda setting Ü Patient perspective Ü Communication while using an EHR
 Can the course provide leverage in the bigger system? Ü Medical leaders were influenced through seeing student presentations Ü Caused significant curricular change Ü Elements of POVE can improve existing courses
Can the course provide leverage in the bigger system? Ü Medical leaders were influenced through seeing student presentations Ü Caused significant curricular change Ü Elements of POVE can improve existing courses
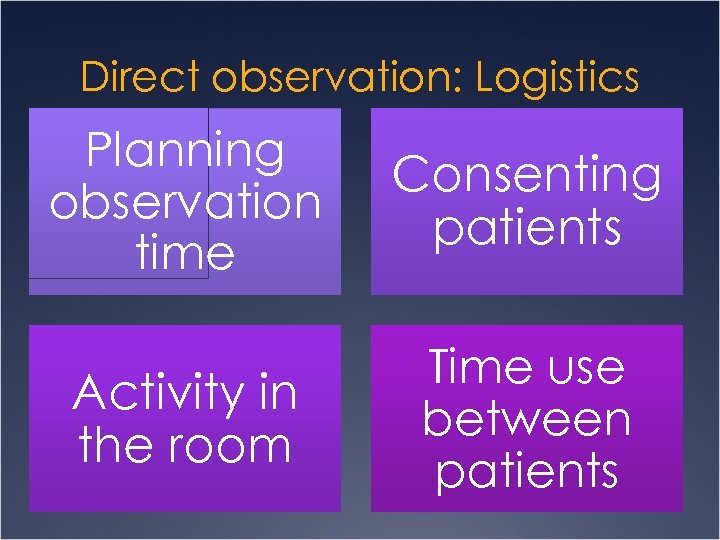 Direct observation: Logistics Planning observation time Consenting patients Activity in the room Time use between patients
Direct observation: Logistics Planning observation time Consenting patients Activity in the room Time use between patients
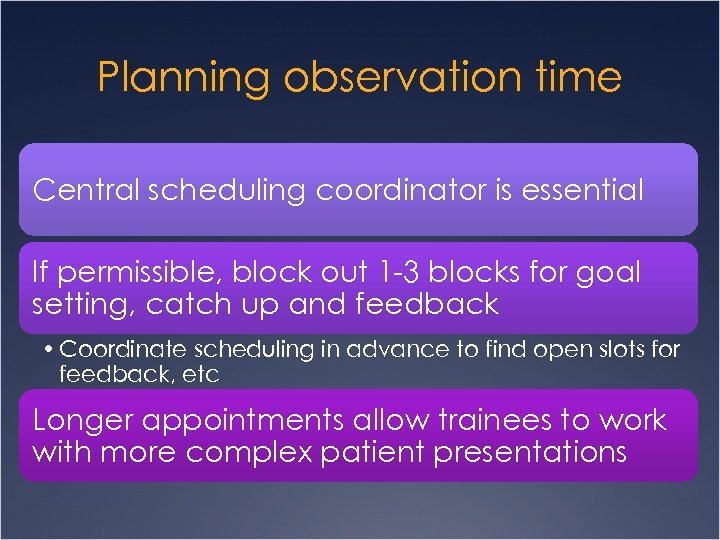 Planning observation time Central scheduling coordinator is essential If permissible, block out 1 -3 blocks for goal setting, catch up and feedback • Coordinate scheduling in advance to find open slots for feedback, etc Longer appointments allow trainees to work with more complex patient presentations
Planning observation time Central scheduling coordinator is essential If permissible, block out 1 -3 blocks for goal setting, catch up and feedback • Coordinate scheduling in advance to find open slots for feedback, etc Longer appointments allow trainees to work with more complex patient presentations
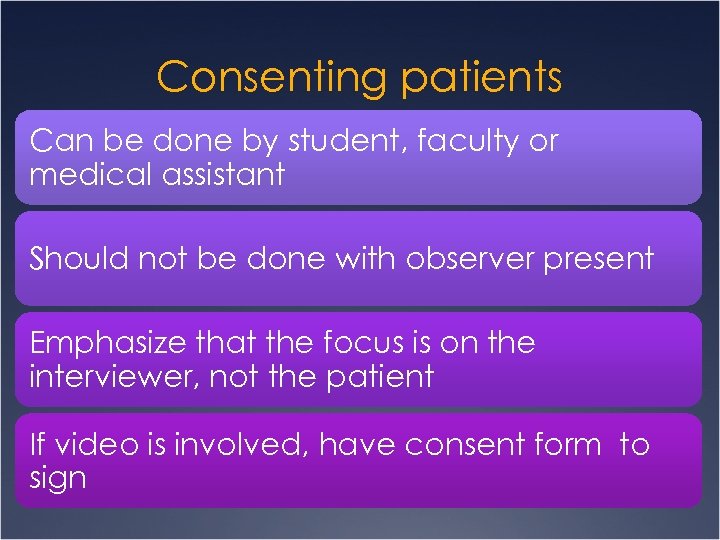 Consenting patients Can be done by student, faculty or medical assistant Should not be done with observer present Emphasize that the focus is on the interviewer, not the patient If video is involved, have consent form to sign
Consenting patients Can be done by student, faculty or medical assistant Should not be done with observer present Emphasize that the focus is on the interviewer, not the patient If video is involved, have consent form to sign
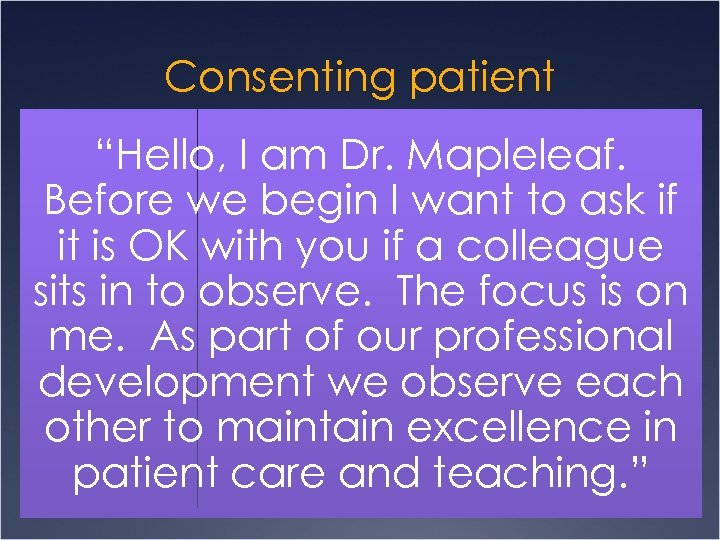 Consenting patient “Hello, I am Dr. Mapleleaf. Before we begin I want to ask if it is OK with you if a colleague sits in to observe. The focus is on me. As part of our professional development we observe each other to maintain excellence in patient care and teaching. ”
Consenting patient “Hello, I am Dr. Mapleleaf. Before we begin I want to ask if it is OK with you if a colleague sits in to observe. The focus is on me. As part of our professional development we observe each other to maintain excellence in patient care and teaching. ”
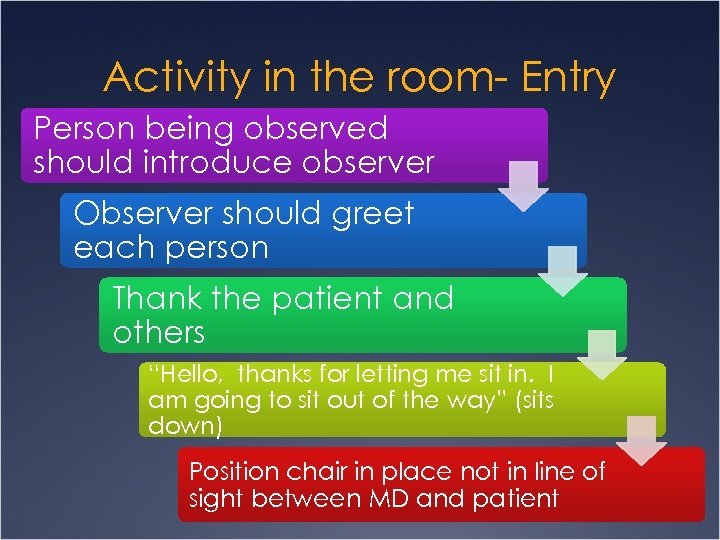 Activity in the room- Entry Person being observed should introduce observer Observer should greet each person Thank the patient and others “Hello, thanks for letting me sit in. I am going to sit out of the way” (sits down) Position chair in place not in line of sight between MD and patient
Activity in the room- Entry Person being observed should introduce observer Observer should greet each person Thank the patient and others “Hello, thanks for letting me sit in. I am going to sit out of the way” (sits down) Position chair in place not in line of sight between MD and patient
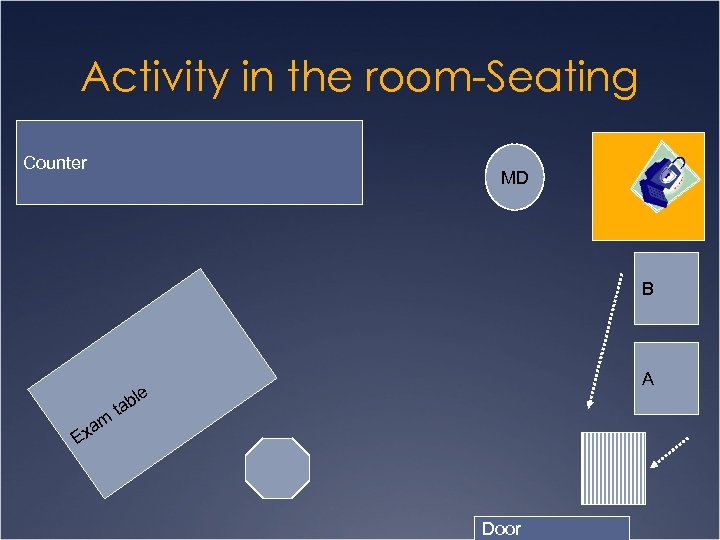 Activity in the room-Seating Counter MD B am ta A ble Ex Door
Activity in the room-Seating Counter MD B am ta A ble Ex Door
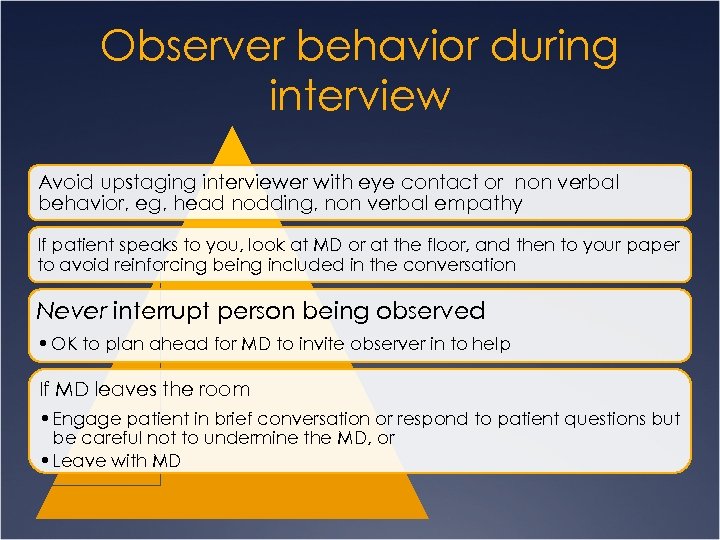 Observer behavior during interview Avoid upstaging interviewer with eye contact or non verbal behavior, eg, head nodding, non verbal empathy If patient speaks to you, look at MD or at the floor, and then to your paper to avoid reinforcing being included in the conversation Never interrupt person being observed • OK to plan ahead for MD to invite observer in to help If MD leaves the room • Engage patient in brief conversation or respond to patient questions but be careful not to undermine the MD, or • Leave with MD
Observer behavior during interview Avoid upstaging interviewer with eye contact or non verbal behavior, eg, head nodding, non verbal empathy If patient speaks to you, look at MD or at the floor, and then to your paper to avoid reinforcing being included in the conversation Never interrupt person being observed • OK to plan ahead for MD to invite observer in to help If MD leaves the room • Engage patient in brief conversation or respond to patient questions but be careful not to undermine the MD, or • Leave with MD
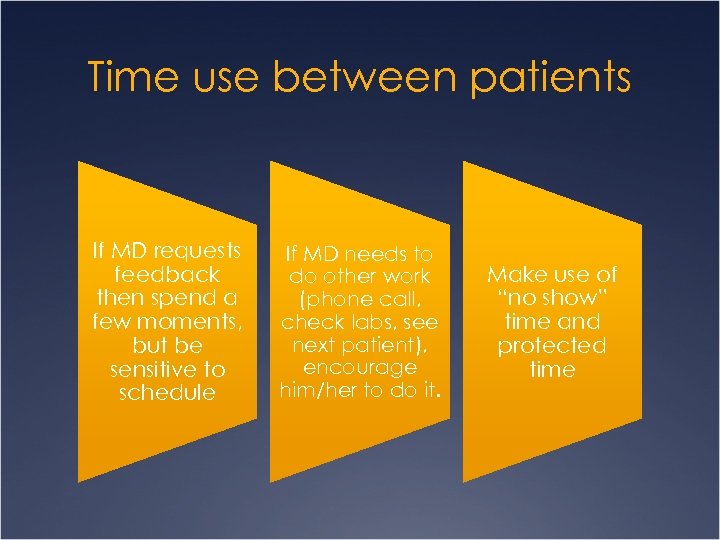 Time use between patients If MD requests feedback then spend a few moments, but be sensitive to schedule If MD needs to do other work (phone call, check labs, see next patient), encourage him/her to do it. Make use of “no show” time and protected time
Time use between patients If MD requests feedback then spend a few moments, but be sensitive to schedule If MD needs to do other work (phone call, check labs, see next patient), encourage him/her to do it. Make use of “no show” time and protected time
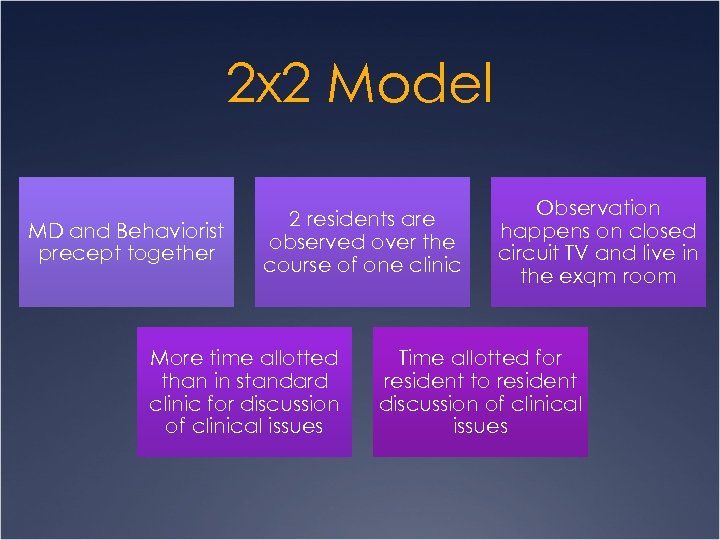 2 x 2 Model MD and Behaviorist precept together 2 residents are observed over the course of one clinic More time allotted than in standard clinic for discussion of clinical issues Observation happens on closed circuit TV and live in the exqm room Time allotted for resident to resident discussion of clinical issues
2 x 2 Model MD and Behaviorist precept together 2 residents are observed over the course of one clinic More time allotted than in standard clinic for discussion of clinical issues Observation happens on closed circuit TV and live in the exqm room Time allotted for resident to resident discussion of clinical issues

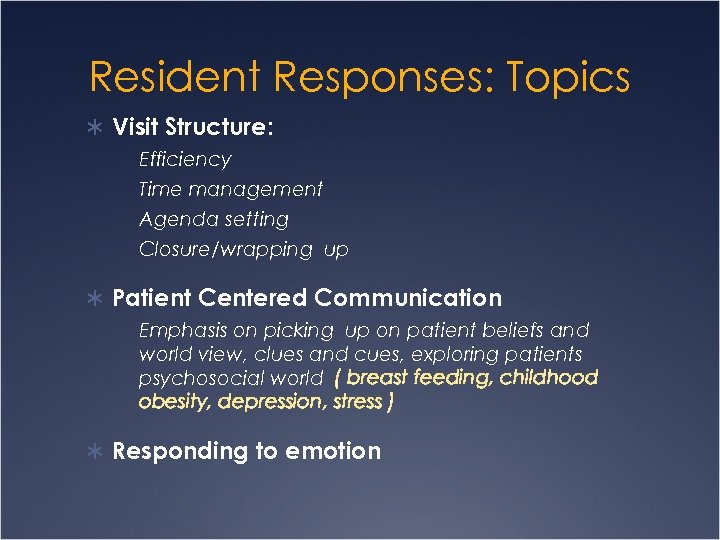 Resident Responses: Topics Ü Visit Structure: Efficiency Time management Agenda setting Closure/wrapping up Ü Patient Centered Communication Emphasis on picking up on patient beliefs and world view, clues and cues, exploring patients psychosocial world ( breast feeding, childhood obesity, depression, stress ) Ü Responding to emotion
Resident Responses: Topics Ü Visit Structure: Efficiency Time management Agenda setting Closure/wrapping up Ü Patient Centered Communication Emphasis on picking up on patient beliefs and world view, clues and cues, exploring patients psychosocial world ( breast feeding, childhood obesity, depression, stress ) Ü Responding to emotion
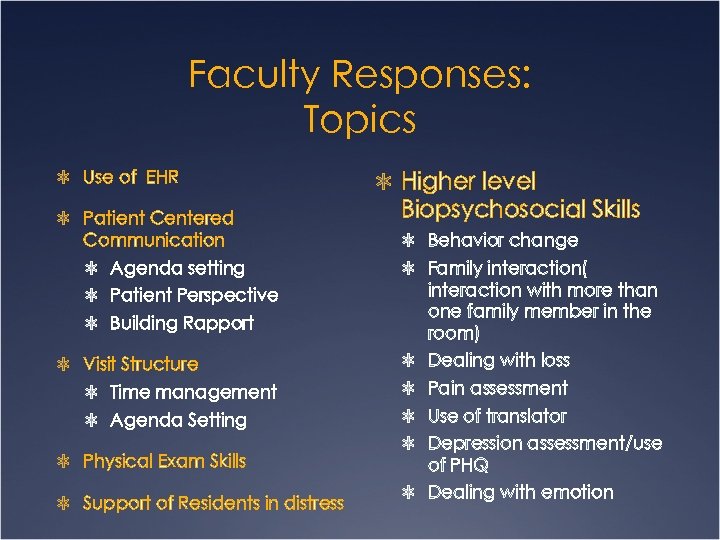 Faculty Responses: Topics Ü Use of EHR Ü Patient Centered Ü Higher level Biopsychosocial Skills Communication Ü Behavior change Ü Agenda setting Ü Family interaction( Ü Patient Perspective Ü Building Rapport Ü Visit Structure interaction with more than one family member in the room) Ü Dealing with loss Ü Time management Ü Pain assessment Ü Agenda Setting Ü Use of translator Ü Physical Exam Skills Ü Support of Residents in distress Ü Depression assessment/use of PHQ Ü Dealing with emotion
Faculty Responses: Topics Ü Use of EHR Ü Patient Centered Ü Higher level Biopsychosocial Skills Communication Ü Behavior change Ü Agenda setting Ü Family interaction( Ü Patient Perspective Ü Building Rapport Ü Visit Structure interaction with more than one family member in the room) Ü Dealing with loss Ü Time management Ü Pain assessment Ü Agenda Setting Ü Use of translator Ü Physical Exam Skills Ü Support of Residents in distress Ü Depression assessment/use of PHQ Ü Dealing with emotion
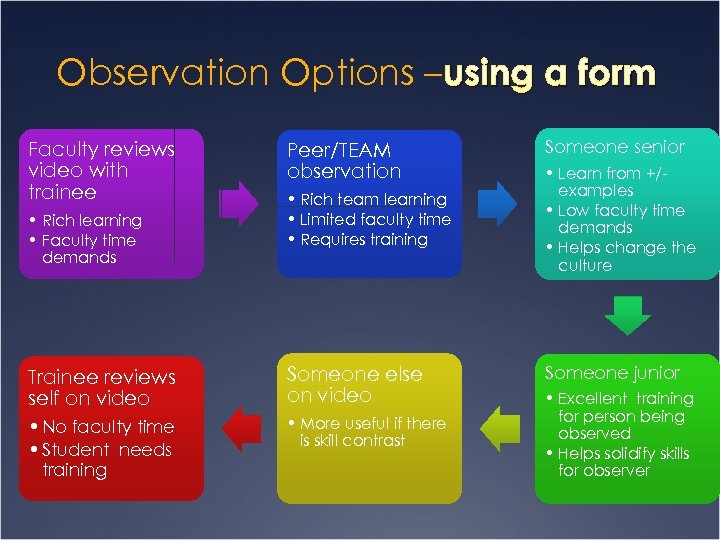 Observation Options – using a form Faculty reviews video with trainee • Rich learning • Faculty time demands Peer/TEAM observation • Rich team learning • Limited faculty time • Requires training Trainee reviews self on video Someone else on video • No faculty time • Student needs training • More useful if there is skill contrast Someone senior • Learn from +/examples • Low faculty time demands • Helps change the culture Someone junior • Excellent training for person being observed • Helps solidify skills for observer
Observation Options – using a form Faculty reviews video with trainee • Rich learning • Faculty time demands Peer/TEAM observation • Rich team learning • Limited faculty time • Requires training Trainee reviews self on video Someone else on video • No faculty time • Student needs training • More useful if there is skill contrast Someone senior • Learn from +/examples • Low faculty time demands • Helps change the culture Someone junior • Excellent training for person being observed • Helps solidify skills for observer
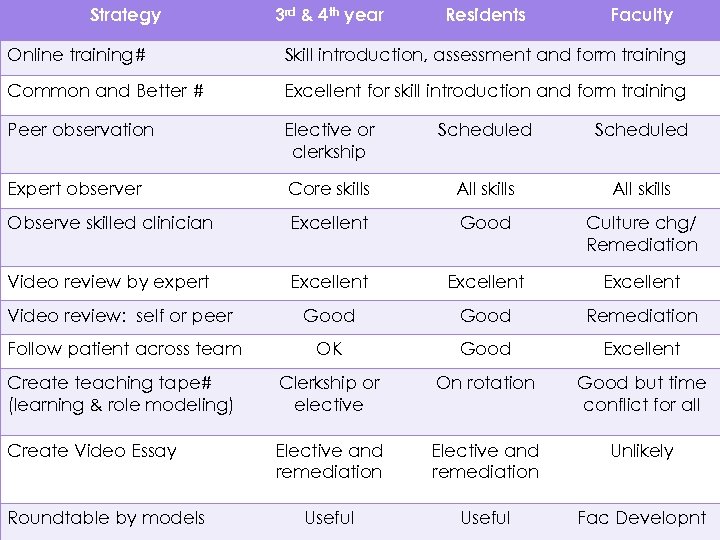 Strategy 3 rd & 4 th year Residents Faculty Online training# Skill introduction, assessment and form training Common and Better # Excellent for skill introduction and form training Peer observation Elective or clerkship Scheduled Expert observer Core skills All skills Observe skilled clinician Excellent Good Culture chg/ Remediation Video review by expert Excellent Video review: self or peer Good Remediation Follow patient across team OK Good Excellent Create teaching tape# (learning & role modeling) Clerkship or elective On rotation Good but time conflict for all Create Video Essay Elective and remediation Unlikely Useful Fac Developnt Roundtable by models
Strategy 3 rd & 4 th year Residents Faculty Online training# Skill introduction, assessment and form training Common and Better # Excellent for skill introduction and form training Peer observation Elective or clerkship Scheduled Expert observer Core skills All skills Observe skilled clinician Excellent Good Culture chg/ Remediation Video review by expert Excellent Video review: self or peer Good Remediation Follow patient across team OK Good Excellent Create teaching tape# (learning & role modeling) Clerkship or elective On rotation Good but time conflict for all Create Video Essay Elective and remediation Unlikely Useful Fac Developnt Roundtable by models
 Collaborative Precepting 2 x 2 For residencies Culture change Time for resident reflection MD Precepting broader and easier • Decreased patient volume
Collaborative Precepting 2 x 2 For residencies Culture change Time for resident reflection MD Precepting broader and easier • Decreased patient volume
 Bibliography Arnold RW, Losh DP, Mauksch LB, et al. Lexicon creation to promote faculty development in medical communication. Patient Educ Couns 2009; 74: 179 -83. Egnew TR, Mauksch LB, Greer T, Farber SJ. Integrating communication training into a required family medicine clerkship. Acad Med 2004; 79: 737 -43. Epstein RM, Mauksch L, Carroll J, Jaen CR. Have you really addressed your patient's concerns? Fam Pract Manag 2008; 15: 35 -40. Kim S, Spielberg F, Mauksch L, et al. Comparing narrative and multiple-choice formats in online communication skill assessment. Med Educ 2009; 43: 533 -41. Losh DP, Mauksch LB, Arnold RW, et al. Teaching inpatient communication skills to medical students: an innovative strategy. Acad Med 2005; 80: 118 -24.
Bibliography Arnold RW, Losh DP, Mauksch LB, et al. Lexicon creation to promote faculty development in medical communication. Patient Educ Couns 2009; 74: 179 -83. Egnew TR, Mauksch LB, Greer T, Farber SJ. Integrating communication training into a required family medicine clerkship. Acad Med 2004; 79: 737 -43. Epstein RM, Mauksch L, Carroll J, Jaen CR. Have you really addressed your patient's concerns? Fam Pract Manag 2008; 15: 35 -40. Kim S, Spielberg F, Mauksch L, et al. Comparing narrative and multiple-choice formats in online communication skill assessment. Med Educ 2009; 43: 533 -41. Losh DP, Mauksch LB, Arnold RW, et al. Teaching inpatient communication skills to medical students: an innovative strategy. Acad Med 2005; 80: 118 -24.
 Bibliography Continued Mauksch LB, Dugdale DC, Dodson S, Epstein R. Relationship, Communication, and Efficiency in the Medical Encounter: Creating a Clinical Model From a Literature Review. Arch Intern Med 2008; 168: 1387 -95. Mauksch LB, Hillenburg L, Robins L. The established focus protocol: training for collaborative agenda setting and time management in the medical interview. Families, Systems and Health 2001; 19: 147 -57. Schirmer JM, Mauksch L, Lang F, et al. Assessing communication competence: a review of current tools. Fam Med 2005; 37: 18492. *Weissmann, P. , Branch, W. Gracey, et al. Role Modeling Humanistic Behavior: Learning bedside manner from the experts. Academic Medicine, 2006, 81, 661 -667
Bibliography Continued Mauksch LB, Dugdale DC, Dodson S, Epstein R. Relationship, Communication, and Efficiency in the Medical Encounter: Creating a Clinical Model From a Literature Review. Arch Intern Med 2008; 168: 1387 -95. Mauksch LB, Hillenburg L, Robins L. The established focus protocol: training for collaborative agenda setting and time management in the medical interview. Families, Systems and Health 2001; 19: 147 -57. Schirmer JM, Mauksch L, Lang F, et al. Assessing communication competence: a review of current tools. Fam Med 2005; 37: 18492. *Weissmann, P. , Branch, W. Gracey, et al. Role Modeling Humanistic Behavior: Learning bedside manner from the experts. Academic Medicine, 2006, 81, 661 -667


