b0f5a5be29b7903467a79dc6779347db.ppt
- Количество слайдов: 35
Common & Uncommon BPSD Behavioral &Psychological Symptoms of Dementia
Definition & Classification of BPSD § So many different classification § No agreed definition of individual behavioural or psychological symptoms § Especially no consensus classification or definition of each BPSD
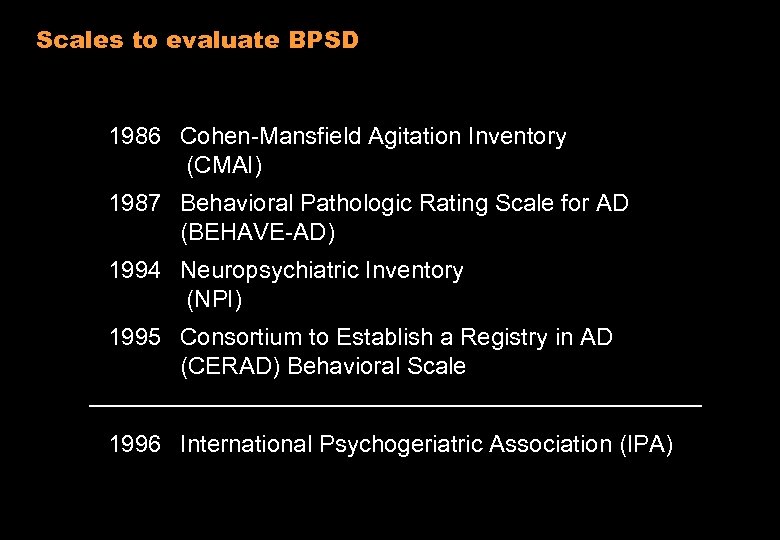
Scales to evaluate BPSD 1986 Cohen-Mansfield Agitation Inventory (CMAI) 1987 Behavioral Pathologic Rating Scale for AD (BEHAVE-AD) 1994 Neuropsychiatric Inventory (NPI) 1995 Consortium to Establish a Registry in AD (CERAD) Behavioral Scale 1996 International Psychogeriatric Association (IPA)
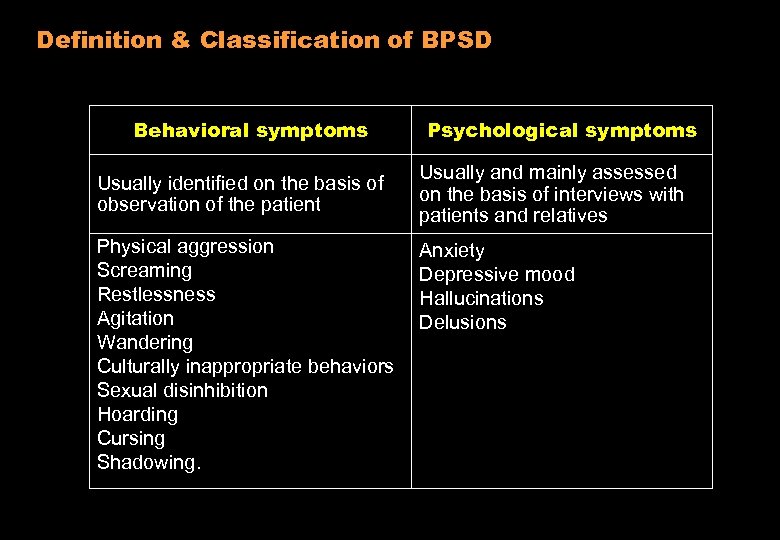
Definition & Classification of BPSD Behavioral symptoms Usually identified on the basis of observation of the patient Physical aggression Screaming Restlessness Agitation Wandering Culturally inappropriate behaviors Sexual disinhibition Hoarding Cursing Shadowing. Psychological symptoms Usually and mainly assessed on the basis of interviews with patients and relatives Anxiety Depressive mood Hallucinations Delusions
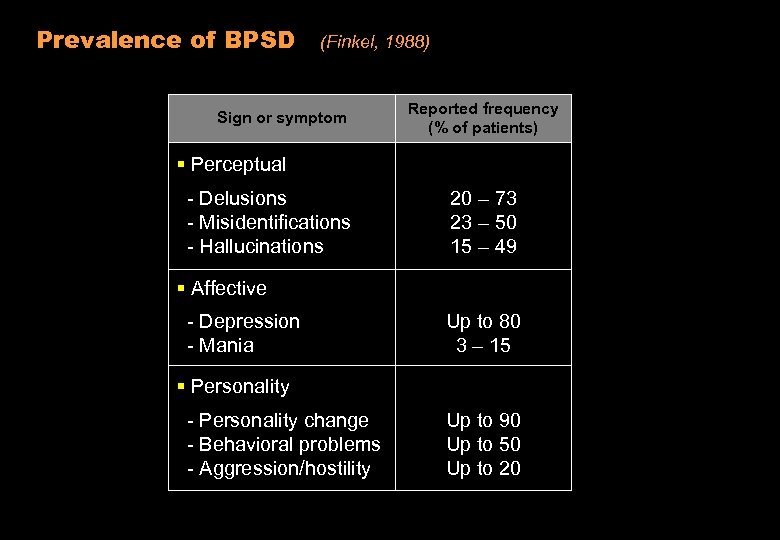
Prevalence of BPSD (Finkel, 1988) Sign or symptom Reported frequency (% of patients) § Perceptual - Delusions - Misidentifications - Hallucinations 20 – 73 23 – 50 15 – 49 § Affective - Depression - Mania Up to 80 3 – 15 § Personality - Personality change - Behavioral problems - Aggression/hostility Up to 90 Up to 50 Up to 20
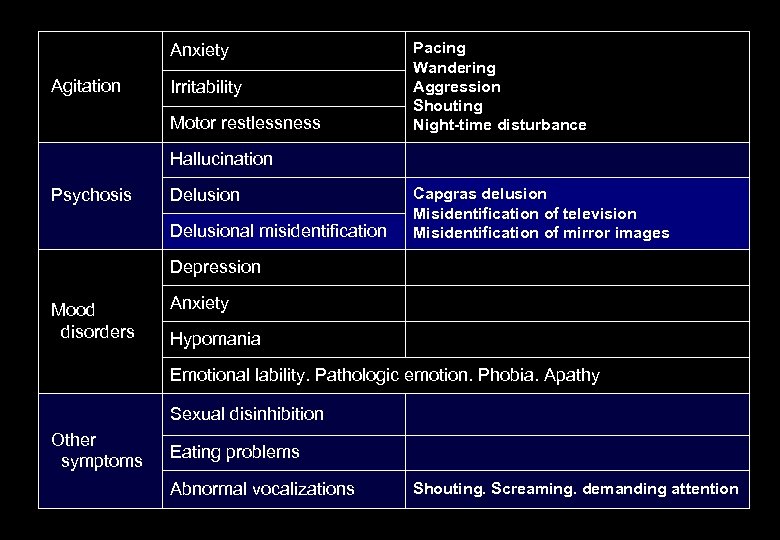
Anxiety Agitation Irritability Motor restlessness Pacing Wandering Aggression Shouting Night-time disturbance Hallucination Psychosis Delusional misidentification Capgras delusion Misidentification of television Misidentification of mirror images Depression Mood disorders Anxiety Hypomania Emotional lability. Pathologic emotion. Phobia. Apathy Sexual disinhibition Other symptoms Eating problems Abnormal vocalizations Shouting. Screaming. demanding attention
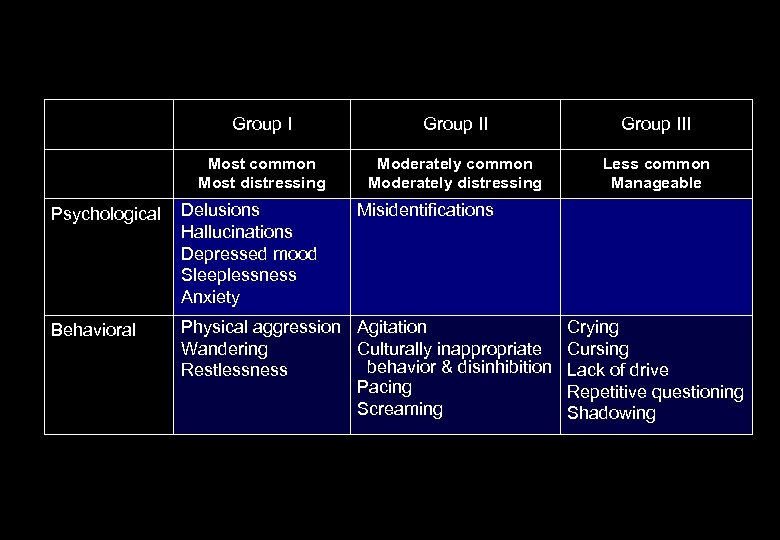
Group III Most common Most distressing Moderately common Moderately distressing Less common Manageable Psychological Delusions Hallucinations Depressed mood Sleeplessness Anxiety Misidentifications Behavioral Physical aggression Agitation Wandering Culturally inappropriate behavior & disinhibition Restlessness Pacing Screaming Crying Cursing Lack of drive Repetitive questioning Shadowing
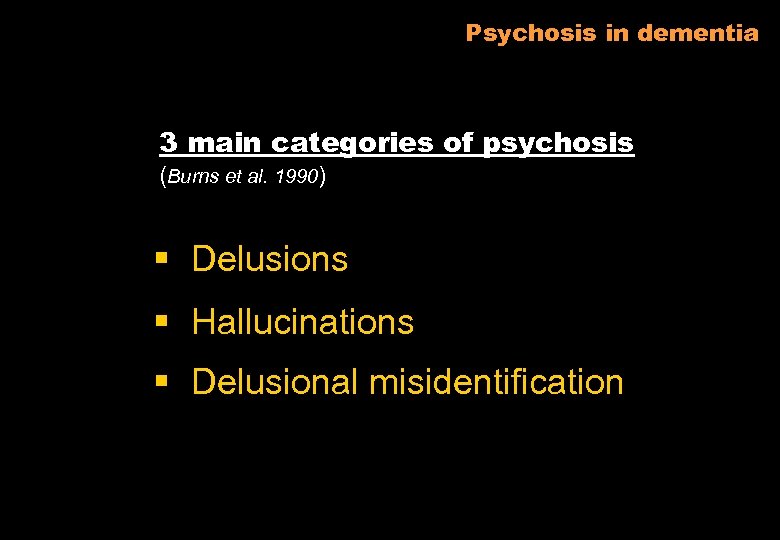
Psychosis in dementia 3 main categories of psychosis (Burns et al. 1990) § Delusions § Hallucinations § Delusional misidentification
Psychosis in dementia Delusions False, unshakable ideas or beliefs that are held with extraordinary conviction and subjective certainty Hallucination Percepts in the absence of a stimulus : Visual > auditory > tactile > olfactory
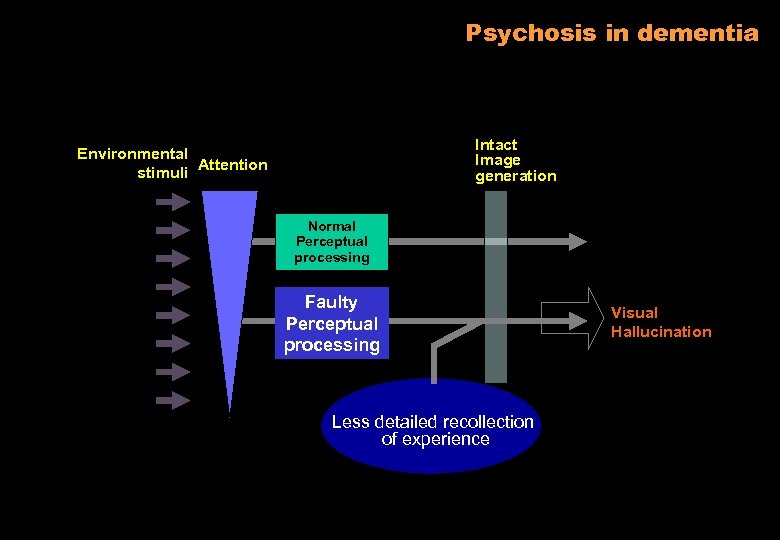
Psychosis in dementia Intact Image generation Environmental stimuli Attention Normal Perceptual processing Faulty Perceptual processing Less detailed recollection of experience Visual Hallucination
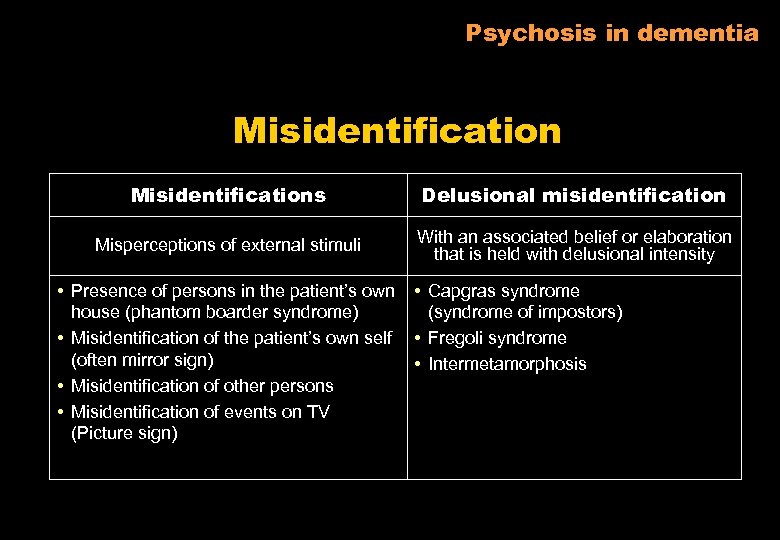
Psychosis in dementia Misidentifications Delusional misidentification Misperceptions of external stimuli With an associated belief or elaboration that is held with delusional intensity • Presence of persons in the patient’s own house (phantom boarder syndrome) • Misidentification of the patient’s own self (often mirror sign) • Misidentification of other persons • Misidentification of events on TV (Picture sign) • Capgras syndrome (syndrome of impostors) • Fregoli syndrome • Intermetamorphosis
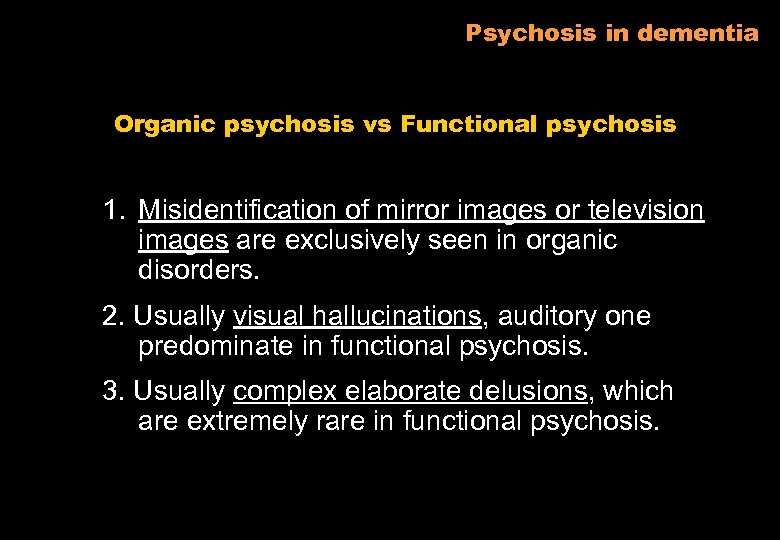
Psychosis in dementia Organic psychosis vs Functional psychosis 1. Misidentification of mirror images or television images are exclusively seen in organic disorders. 2. Usually visual hallucinations, auditory one predominate in functional psychosis. 3. Usually complex elaborate delusions, which are extremely rare in functional psychosis.
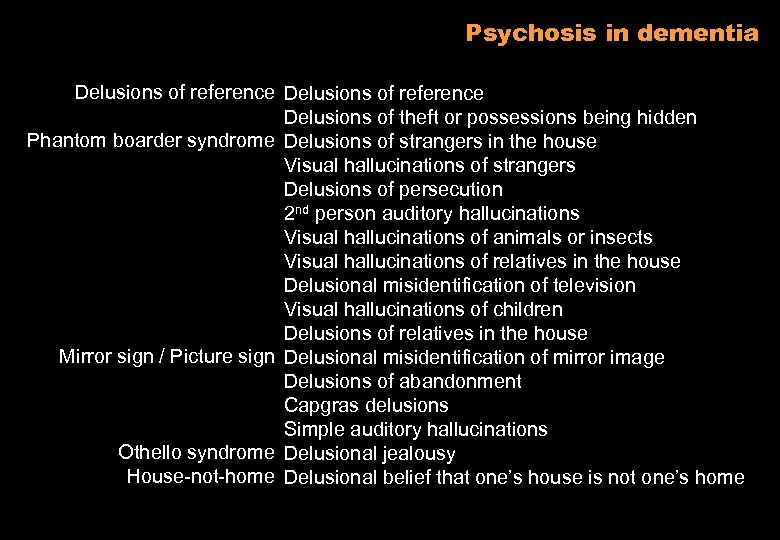
Psychosis in dementia Delusions of reference Delusions of theft or possessions being hidden Phantom boarder syndrome Delusions of strangers in the house Visual hallucinations of strangers Delusions of persecution 2 nd person auditory hallucinations Visual hallucinations of animals or insects Visual hallucinations of relatives in the house Delusional misidentification of television Visual hallucinations of children Delusions of relatives in the house Mirror sign / Picture sign Delusional misidentification of mirror image Delusions of abandonment Capgras delusions Simple auditory hallucinations Othello syndrome Delusional jealousy House-not-home Delusional belief that one’s house is not one’s home
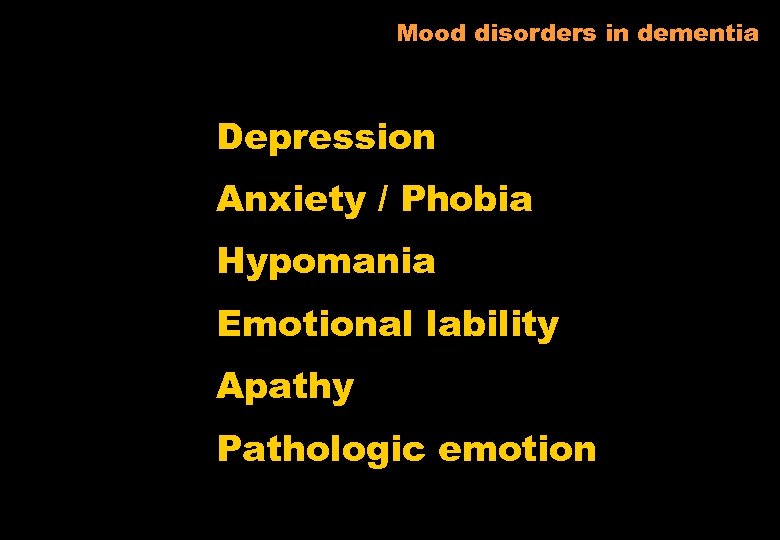
Mood disorders in dementia Depression Anxiety / Phobia Hypomania Emotional lability Apathy Pathologic emotion
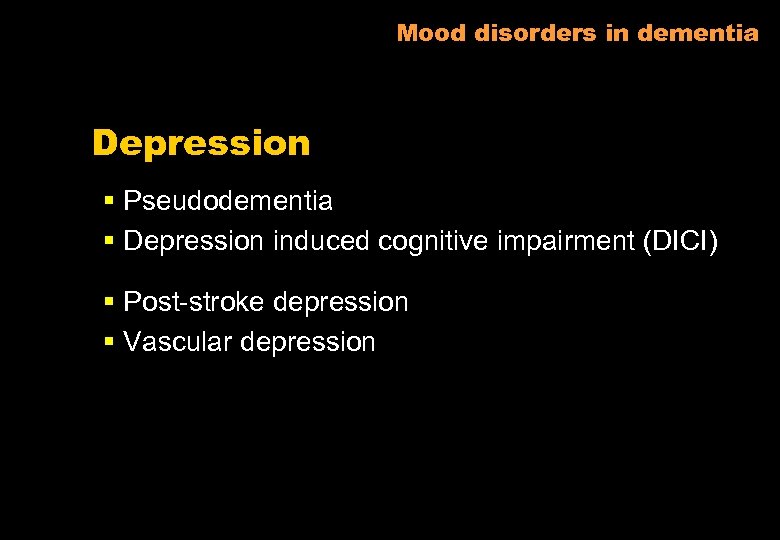
Mood disorders in dementia Depression § Pseudodementia § Depression induced cognitive impairment (DICI) § Post-stroke depression § Vascular depression
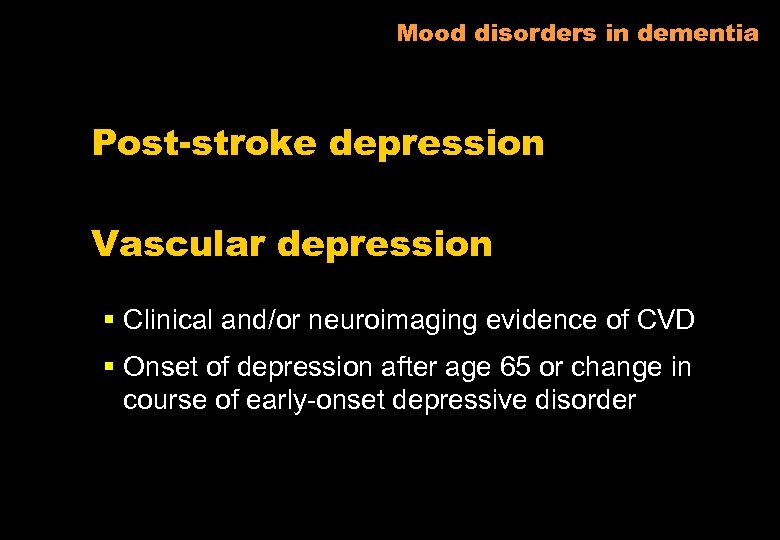
Mood disorders in dementia Post-stroke depression Vascular depression § Clinical and/or neuroimaging evidence of CVD § Onset of depression after age 65 or change in course of early-onset depressive disorder

Mood disorders in dementia Apathy § Relatively common § May be mistaken for those of major depression § Lack of motivation without the dysphoria or vegetative symptoms of depression Hypomania Extreme elevation of mood
Anxiety in dementia § Related to the manifestation of other BPSD or independently • Godot syndrome • Fear of being left alone > phobia
Wandering in dementia Wandering A tendency to move about in either the seemingly aimless or disorientated fashion or in pursuit of an indefinable or unobtainable goal (Snyder et al, 1978, Stokes 1986)
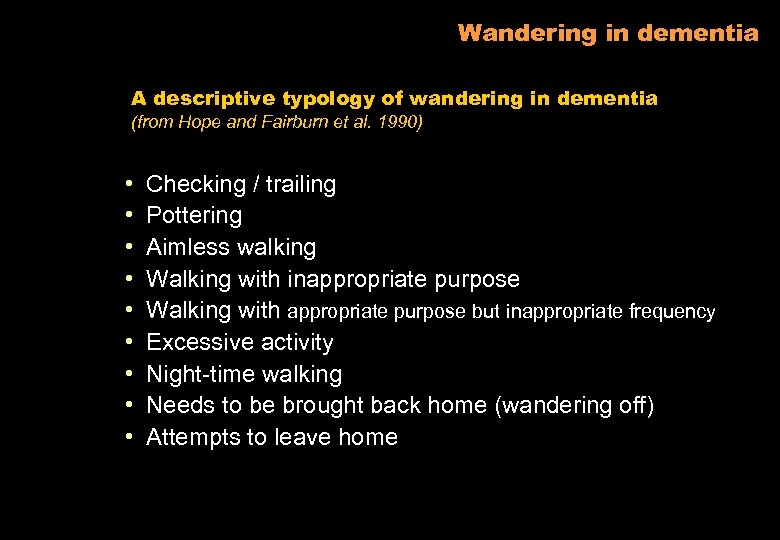
Wandering in dementia A descriptive typology of wandering in dementia (from Hope and Fairburn et al. 1990) • • • Checking / trailing Pottering Aimless walking Walking with inappropriate purpose Walking with appropriate purpose but inappropriate frequency Excessive activity Night-time walking Needs to be brought back home (wandering off) Attempts to leave home
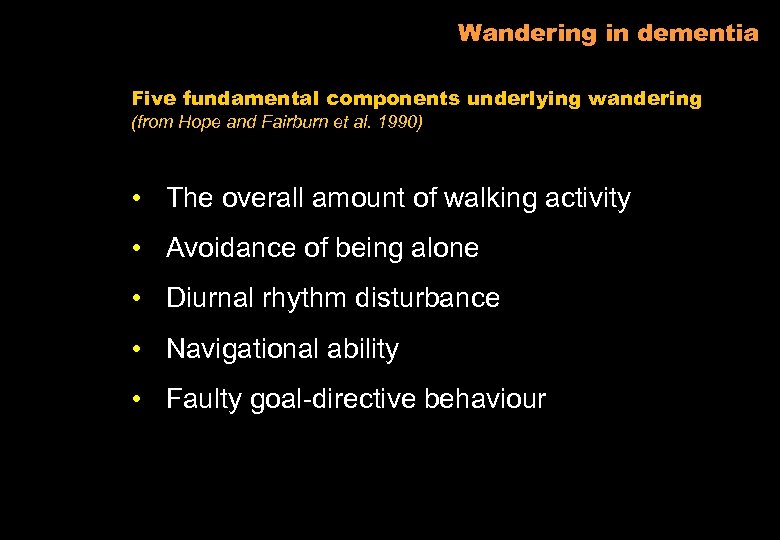
Wandering in dementia Five fundamental components underlying wandering (from Hope and Fairburn et al. 1990) • The overall amount of walking activity • Avoidance of being alone • Diurnal rhythm disturbance • Navigational ability • Faulty goal-directive behaviour
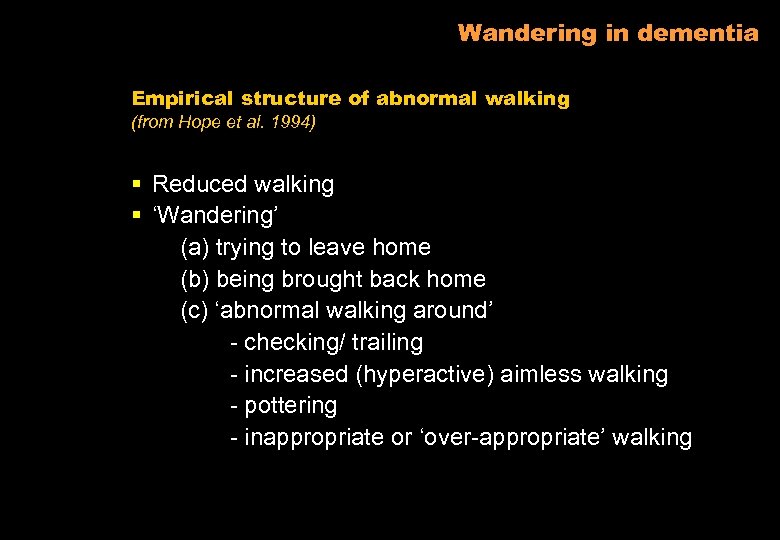
Wandering in dementia Empirical structure of abnormal walking (from Hope et al. 1994) § Reduced walking § ‘Wandering’ (a) trying to leave home (b) being brought back home (c) ‘abnormal walking around’ - checking/ trailing - increased (hyperactive) aimless walking - pottering - inappropriate or ‘over-appropriate’ walking
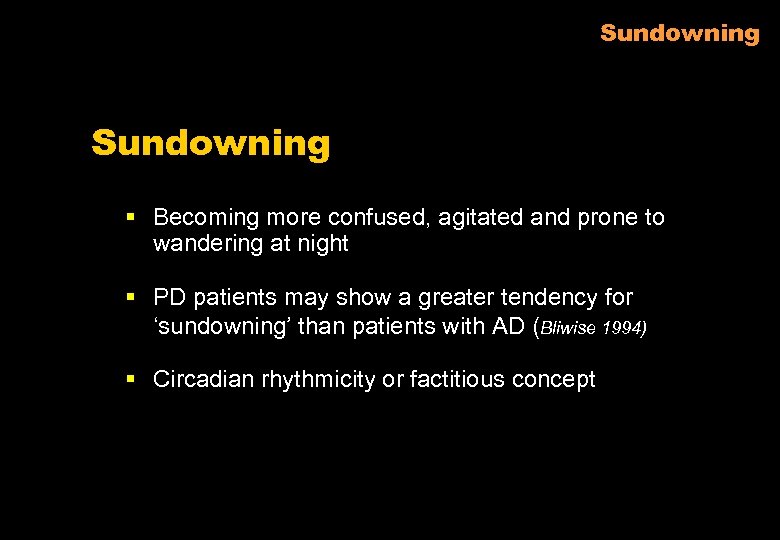
Sundowning § Becoming more confused, agitated and prone to wandering at night § PD patients may show a greater tendency for ‘sundowning’ than patients with AD (Bliwise 1994) § Circadian rhythmicity or factitious concept
Aggression behaviour 3 distinct syndromes of aggressive behaviour § Aggression § Personality change § Agitation
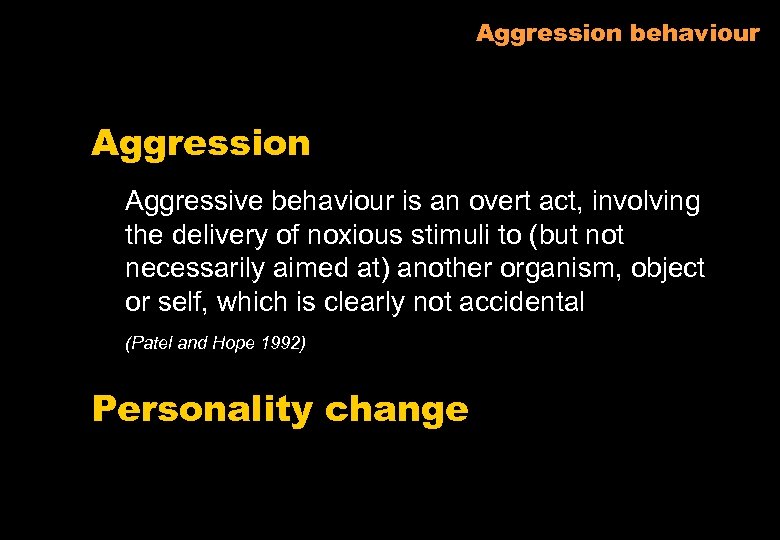
Aggression behaviour Aggression Aggressive behaviour is an overt act, involving the delivery of noxious stimuli to (but not necessarily aimed at) another organism, object or self, which is clearly not accidental (Patel and Hope 1992) Personality change

Aggression behaviour Agitation Inappropriate verbal, vocal or motor activity not explained by needs or confusion per se’ Inappropriateness in three categories 1) the person may be abusive towards self & other 2) appropriate behaviour, but with inappropriate frequency 3) inappropriate according to social standards for a specific situation
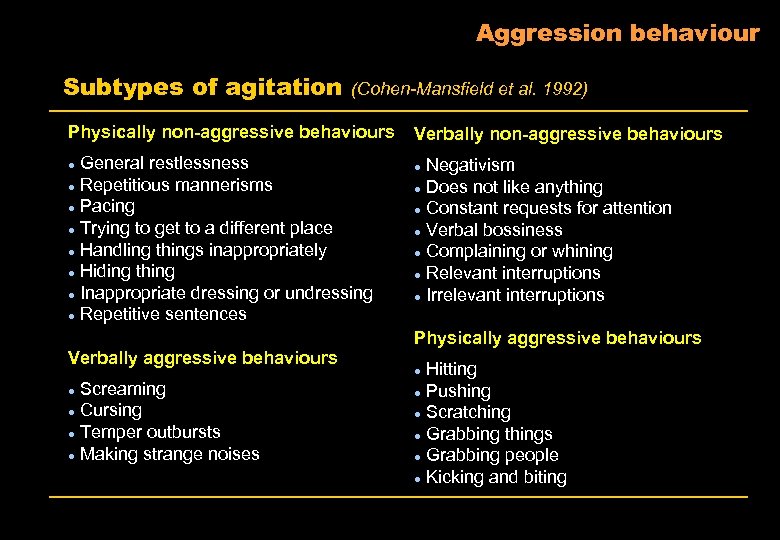
Aggression behaviour Subtypes of agitation (Cohen-Mansfield et al. 1992) Physically non-aggressive behaviours General restlessness l Repetitious mannerisms l Pacing l Trying to get to a different place l Handling things inappropriately l Hiding thing l Inappropriate dressing or undressing l Repetitive sentences l Verbally aggressive behaviours Screaming l Cursing l Temper outbursts l Making strange noises l Verbally non-aggressive behaviours Negativism l Does not like anything l Constant requests for attention l Verbal bossiness l Complaining or whining l Relevant interruptions l Irrelevant interruptions l Physically aggressive behaviours Hitting l Pushing l Scratching l Grabbing things l Grabbing people l Kicking and biting l
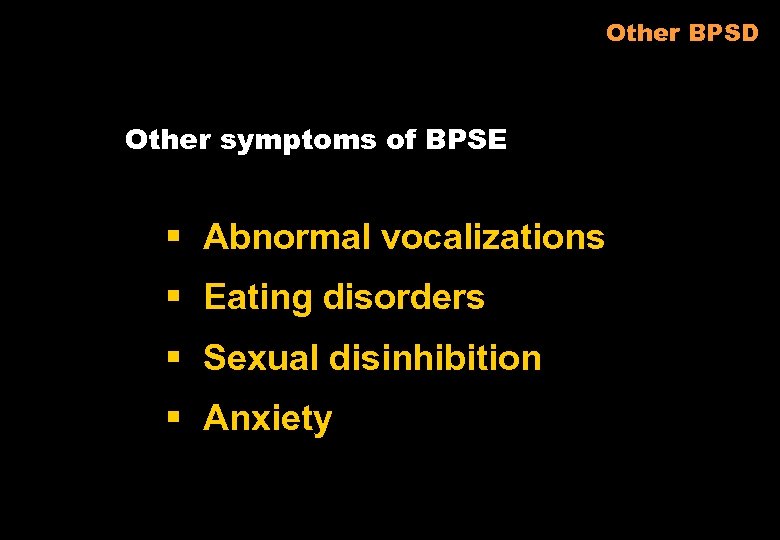
Other BPSD Other symptoms of BPSE § Abnormal vocalizations § Eating disorders § Sexual disinhibition § Anxiety
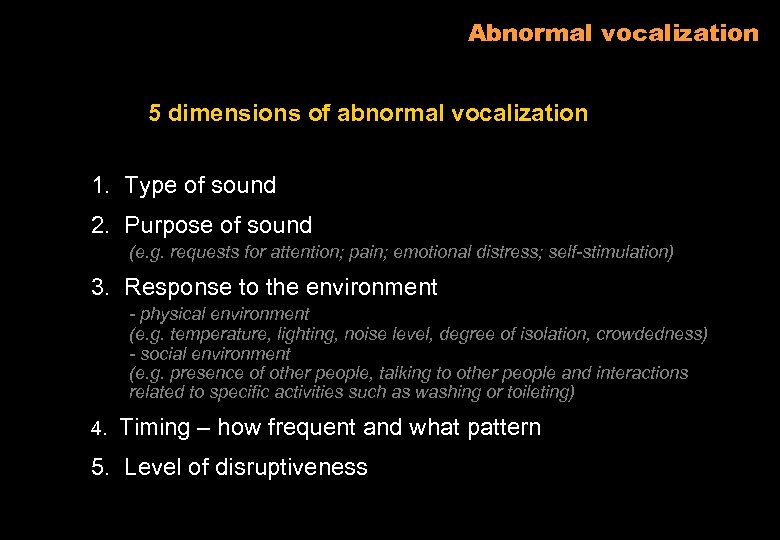
Abnormal vocalization 5 dimensions of abnormal vocalization 1. Type of sound 2. Purpose of sound (e. g. requests for attention; pain; emotional distress; self-stimulation) 3. Response to the environment - physical environment (e. g. temperature, lighting, noise level, degree of isolation, crowdedness) - social environment (e. g. presence of other people, talking to other people and interactions related to specific activities such as washing or toileting) 4. Timing – how frequent and what pattern 5. Level of disruptiveness
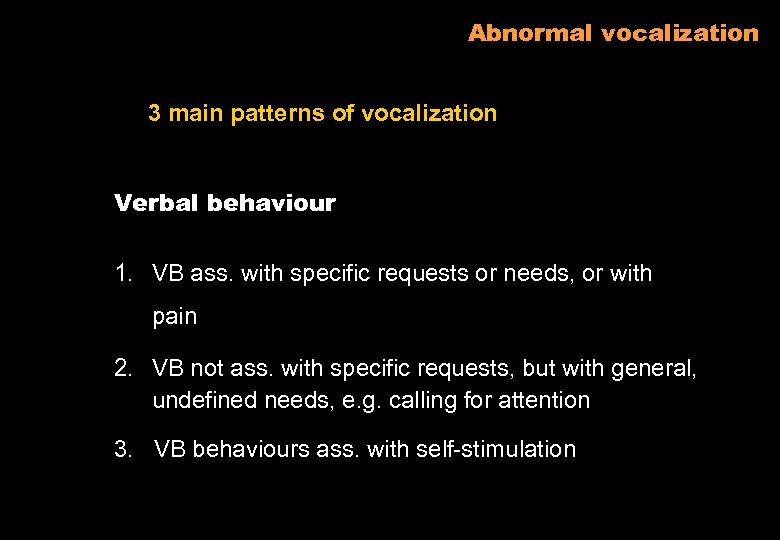
Abnormal vocalization 3 main patterns of vocalization Verbal behaviour 1. VB ass. with specific requests or needs, or with pain 2. VB not ass. with specific requests, but with general, undefined needs, e. g. calling for attention 3. VB behaviours ass. with self-stimulation
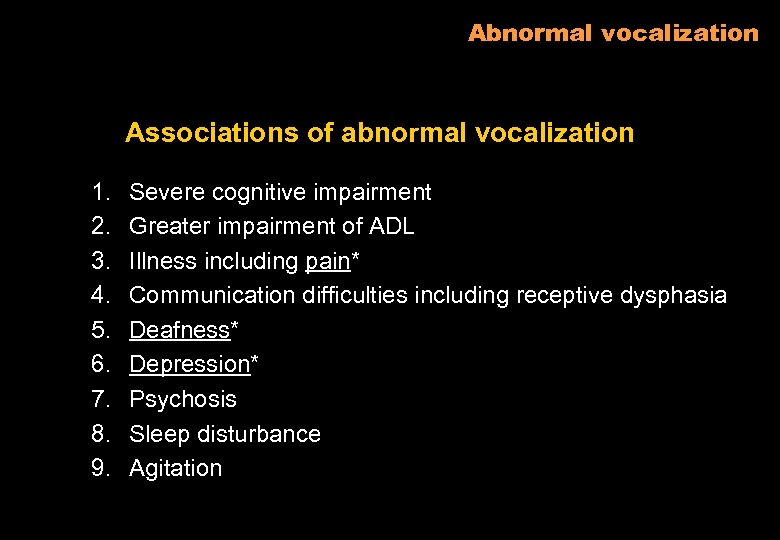
Abnormal vocalization Associations of abnormal vocalization 1. 2. 3. 4. 5. 6. 7. 8. 9. Severe cognitive impairment Greater impairment of ADL Illness including pain* Communication difficulties including receptive dysphasia Deafness* Depression* Psychosis Sleep disturbance Agitation
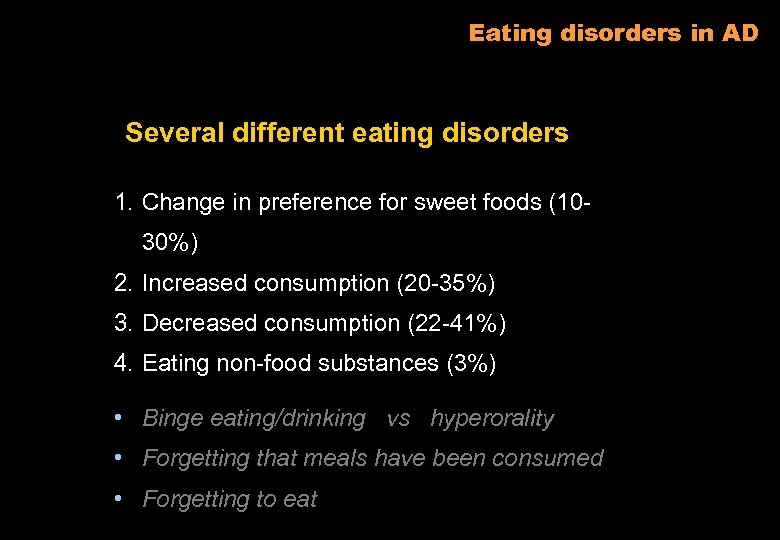
Eating disorders in AD Several different eating disorders 1. Change in preference for sweet foods (1030%) 2. Increased consumption (20 -35%) 3. Decreased consumption (22 -41%) 4. Eating non-food substances (3%) • Binge eating/drinking vs hyperorality • Forgetting that meals have been consumed • Forgetting to eat
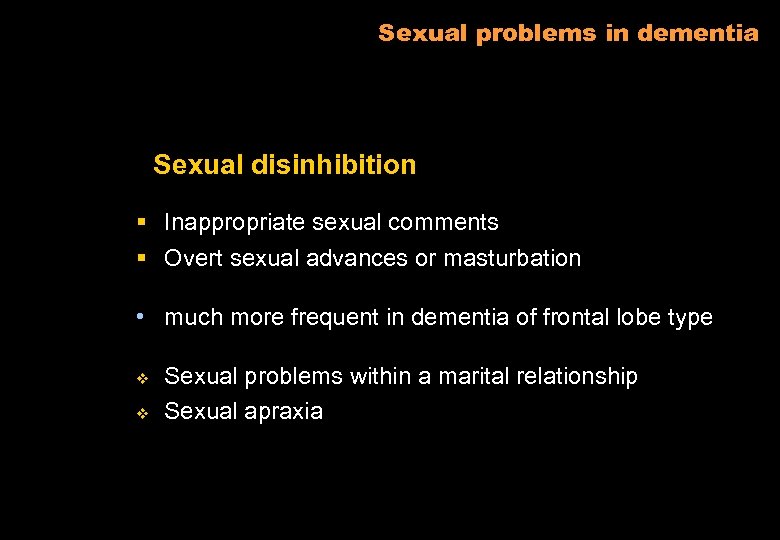
Sexual problems in dementia Sexual disinhibition § Inappropriate sexual comments § Overt sexual advances or masturbation • much more frequent in dementia of frontal lobe type v v Sexual problems within a marital relationship Sexual apraxia
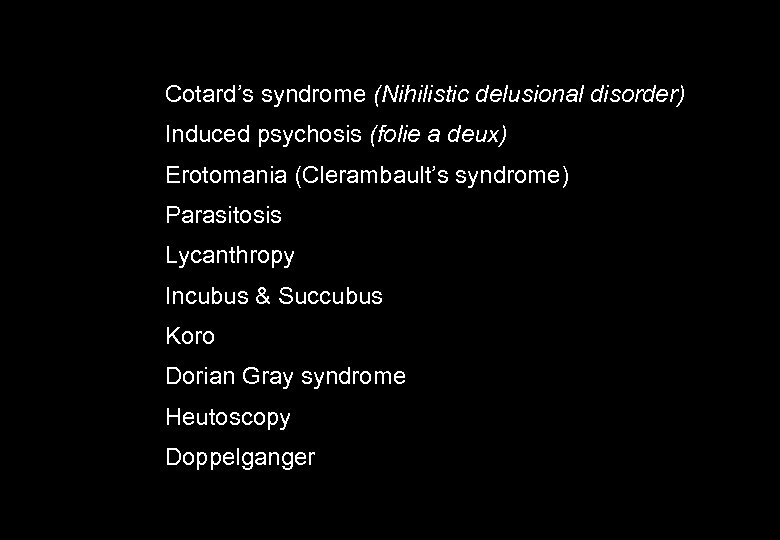
Cotard’s syndrome (Nihilistic delusional disorder) Induced psychosis (folie a deux) Erotomania (Clerambault’s syndrome) Parasitosis Lycanthropy Incubus & Succubus Koro Dorian Gray syndrome Heutoscopy Doppelganger

b0f5a5be29b7903467a79dc6779347db.ppt