2b3c810ec838c03bd0d24a7f727f364b.ppt
- Количество слайдов: 38
 Common Respiratory Disorders of the Neonate
Common Respiratory Disorders of the Neonate
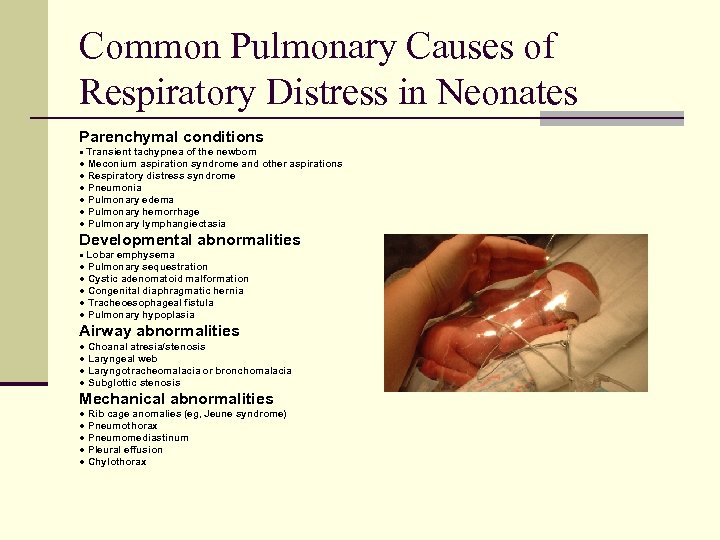 Common Pulmonary Causes of Respiratory Distress in Neonates Parenchymal conditions ● Transient tachypnea of the newborn ● Meconium aspiration syndrome and other aspirations ● Respiratory distress syndrome ● Pneumonia ● Pulmonary edema ● Pulmonary hemorrhage ● Pulmonary lymphangiectasia Developmental abnormalities ● Lobar emphysema ● Pulmonary sequestration ● Cystic adenomatoid malformation ● Congenital diaphragmatic hernia ● Tracheoesophageal fistula ● Pulmonary hypoplasia Airway abnormalities ● Choanal atresia/stenosis ● Laryngeal web ● Laryngotracheomalacia or bronchomalacia ● Subglottic stenosis Mechanical abnormalities ● Rib cage anomalies (eg, Jeune syndrome) ● Pneumothorax ● Pneumomediastinum ● Pleural effusion ● Chylothorax
Common Pulmonary Causes of Respiratory Distress in Neonates Parenchymal conditions ● Transient tachypnea of the newborn ● Meconium aspiration syndrome and other aspirations ● Respiratory distress syndrome ● Pneumonia ● Pulmonary edema ● Pulmonary hemorrhage ● Pulmonary lymphangiectasia Developmental abnormalities ● Lobar emphysema ● Pulmonary sequestration ● Cystic adenomatoid malformation ● Congenital diaphragmatic hernia ● Tracheoesophageal fistula ● Pulmonary hypoplasia Airway abnormalities ● Choanal atresia/stenosis ● Laryngeal web ● Laryngotracheomalacia or bronchomalacia ● Subglottic stenosis Mechanical abnormalities ● Rib cage anomalies (eg, Jeune syndrome) ● Pneumothorax ● Pneumomediastinum ● Pleural effusion ● Chylothorax
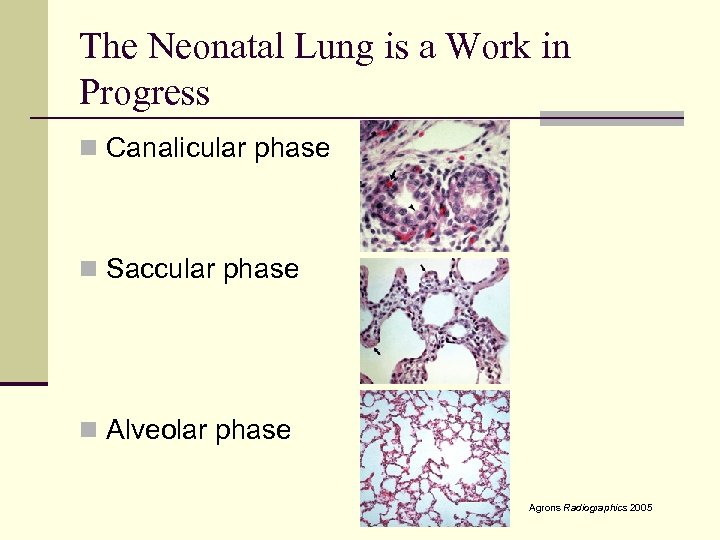 The Neonatal Lung is a Work in Progress n Canalicular phase n Saccular phase n Alveolar phase Agrons Radiographics 2005
The Neonatal Lung is a Work in Progress n Canalicular phase n Saccular phase n Alveolar phase Agrons Radiographics 2005
 Respiratory Distress Syndrome (Hyaline Membrane Disease) n Definition? n 1960 – clinical definition describing respiratory distress and a hyaline membrane lining dilated terminal airspaces n 2006 – clinical definition describing respiratory distress and x-ray findings n There is no “test” for RDS
Respiratory Distress Syndrome (Hyaline Membrane Disease) n Definition? n 1960 – clinical definition describing respiratory distress and a hyaline membrane lining dilated terminal airspaces n 2006 – clinical definition describing respiratory distress and x-ray findings n There is no “test” for RDS
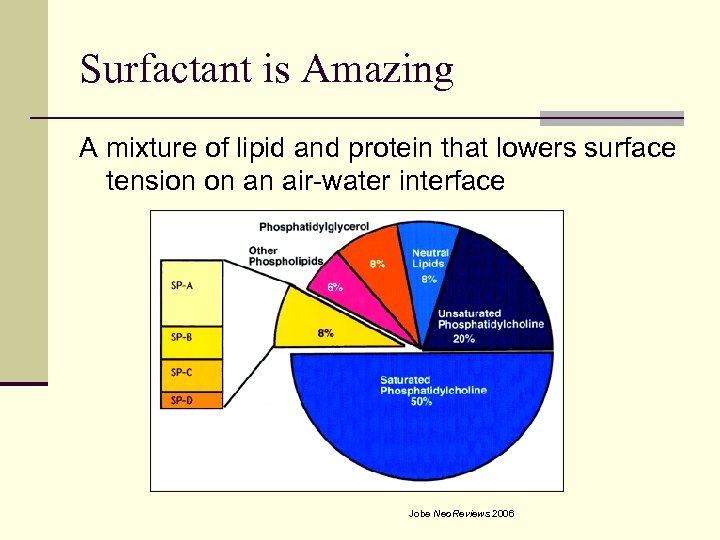 Surfactant is Amazing A mixture of lipid and protein that lowers surface tension on an air-water interface Jobe Neo. Reviews 2006
Surfactant is Amazing A mixture of lipid and protein that lowers surface tension on an air-water interface Jobe Neo. Reviews 2006
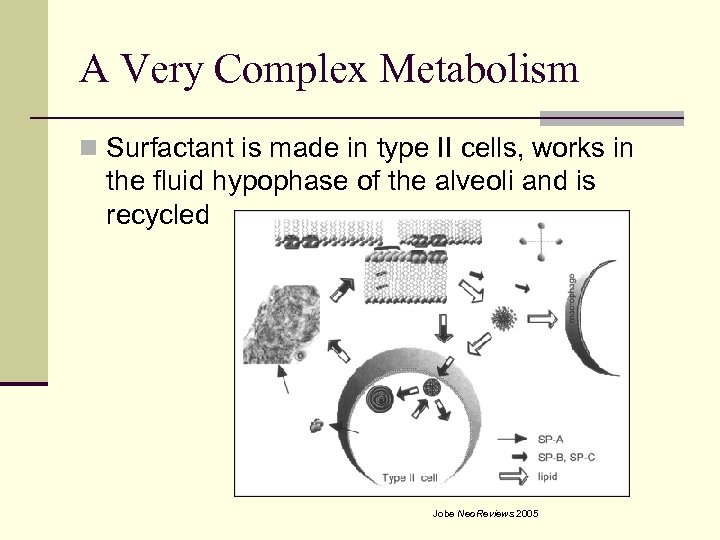 A Very Complex Metabolism n Surfactant is made in type II cells, works in the fluid hypophase of the alveoli and is recycled Jobe Neo. Reviews 2005
A Very Complex Metabolism n Surfactant is made in type II cells, works in the fluid hypophase of the alveoli and is recycled Jobe Neo. Reviews 2005
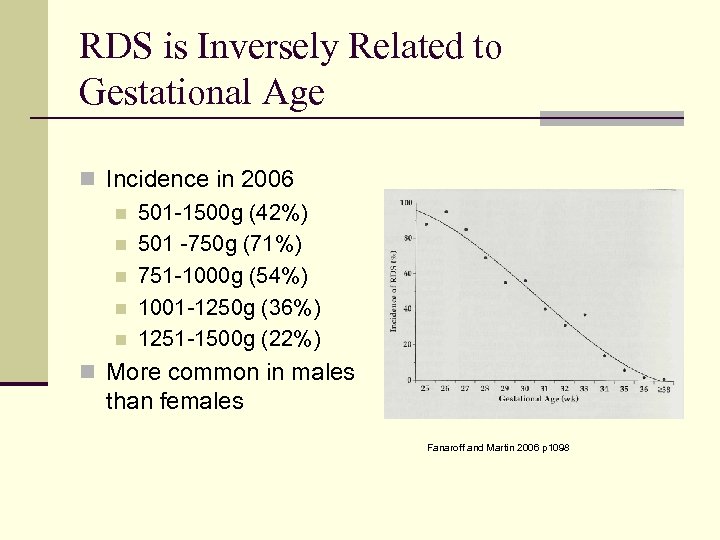 RDS is Inversely Related to Gestational Age n Incidence in 2006 n 501 -1500 g (42%) n 501 -750 g (71%) n 751 -1000 g (54%) n 1001 -1250 g (36%) n 1251 -1500 g (22%) n More common in males than females Fanaroff and Martin 2006 p 1098
RDS is Inversely Related to Gestational Age n Incidence in 2006 n 501 -1500 g (42%) n 501 -750 g (71%) n 751 -1000 g (54%) n 1001 -1250 g (36%) n 1251 -1500 g (22%) n More common in males than females Fanaroff and Martin 2006 p 1098
 Surfactant Maturation Can Be Accelerated n Corticosteroids n TRH n Inflammation n Heroin
Surfactant Maturation Can Be Accelerated n Corticosteroids n TRH n Inflammation n Heroin
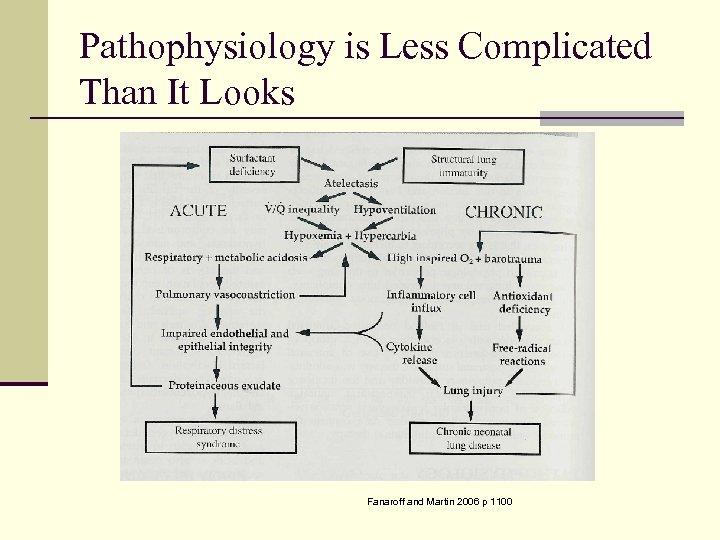 Pathophysiology is Less Complicated Than It Looks Fanaroff and Martin 2006 p 1100
Pathophysiology is Less Complicated Than It Looks Fanaroff and Martin 2006 p 1100
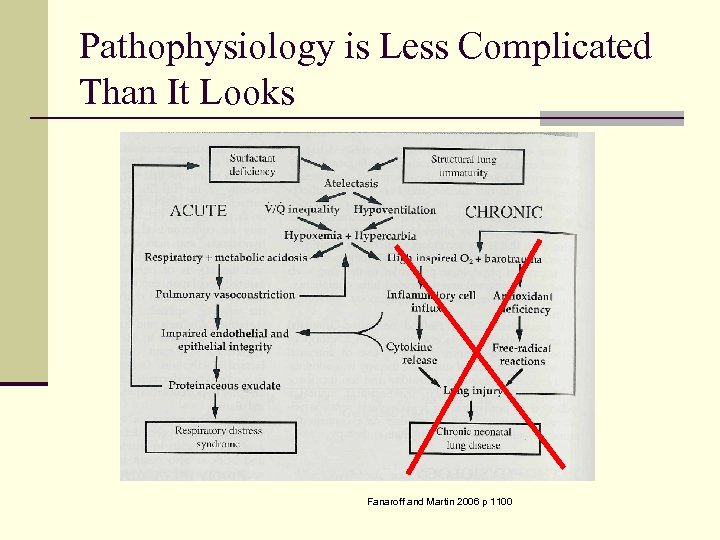 Pathophysiology is Less Complicated Than It Looks Fanaroff and Martin 2006 p 1100
Pathophysiology is Less Complicated Than It Looks Fanaroff and Martin 2006 p 1100
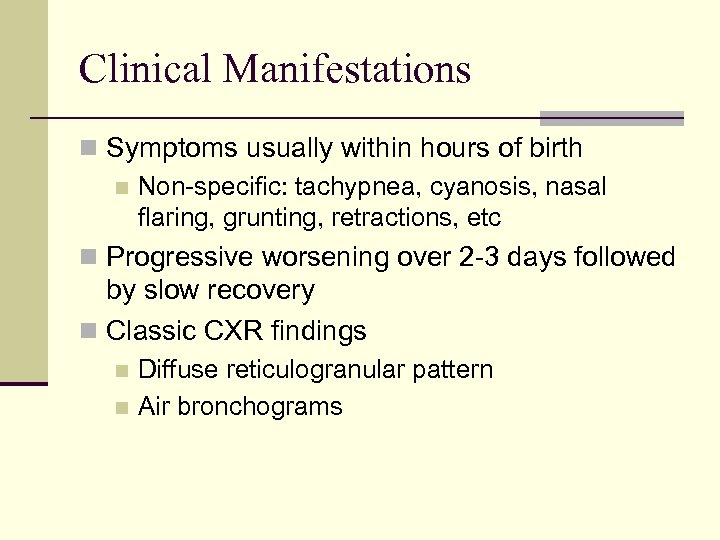 Clinical Manifestations n Symptoms usually within hours of birth n Non-specific: tachypnea, cyanosis, nasal flaring, grunting, retractions, etc n Progressive worsening over 2 -3 days followed by slow recovery n Classic CXR findings Diffuse reticulogranular pattern n Air bronchograms n
Clinical Manifestations n Symptoms usually within hours of birth n Non-specific: tachypnea, cyanosis, nasal flaring, grunting, retractions, etc n Progressive worsening over 2 -3 days followed by slow recovery n Classic CXR findings Diffuse reticulogranular pattern n Air bronchograms n
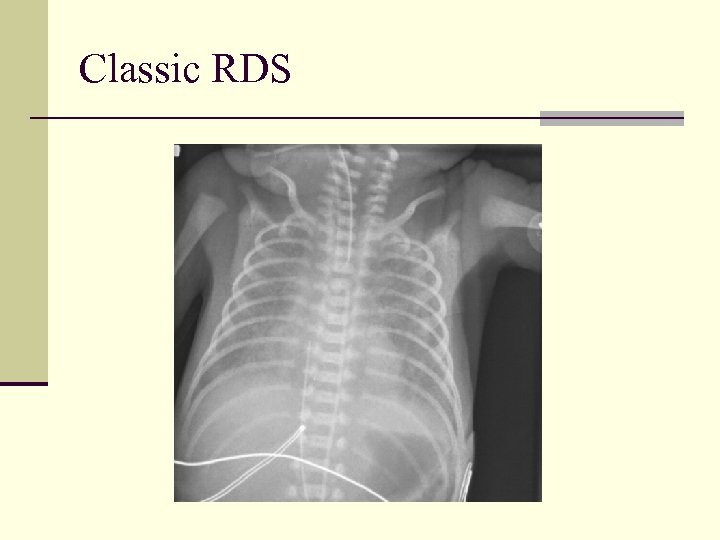 Classic RDS
Classic RDS
 Management 1960 s Style n Supplemental oxygen n High humidity n Antimicrobials n Rocking chair devices n Sternal fixation
Management 1960 s Style n Supplemental oxygen n High humidity n Antimicrobials n Rocking chair devices n Sternal fixation
 Management 2007 Style n Supplemental oxygen and respiratory support n Attention to thermoregulation n Antibiotics n IV fluids n Exogenous surfactant
Management 2007 Style n Supplemental oxygen and respiratory support n Attention to thermoregulation n Antibiotics n IV fluids n Exogenous surfactant
 Exogenous Surfactant n There is no question that it works n Decreases mortality from RDS n +/- decrease in BPD n Surfactant works best when: n Administered shortly after birth n Given rapidly n Followed by distending pressure
Exogenous Surfactant n There is no question that it works n Decreases mortality from RDS n +/- decrease in BPD n Surfactant works best when: n Administered shortly after birth n Given rapidly n Followed by distending pressure
 Other Surfactant Fun Facts n Components are recycled and “improved” like natural surfactant n May need additional doses n Optimal ventilator strategies following administration are more a matter of opinion than science
Other Surfactant Fun Facts n Components are recycled and “improved” like natural surfactant n May need additional doses n Optimal ventilator strategies following administration are more a matter of opinion than science
 Respiratory Support n Goals are to: n Survive the acute phase of the disease n Minimize side effects n Minimize chance of chronic lung disease n Lots of opinion, but no consensus n Conventional ventilation n n Pressure volume n. CPAP n HFV n
Respiratory Support n Goals are to: n Survive the acute phase of the disease n Minimize side effects n Minimize chance of chronic lung disease n Lots of opinion, but no consensus n Conventional ventilation n n Pressure volume n. CPAP n HFV n
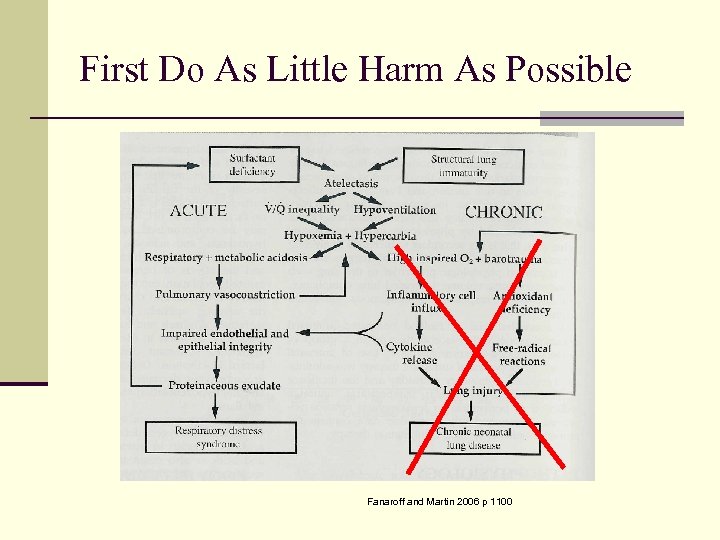 First Do As Little Harm As Possible Fanaroff and Martin 2006 p 1100
First Do As Little Harm As Possible Fanaroff and Martin 2006 p 1100
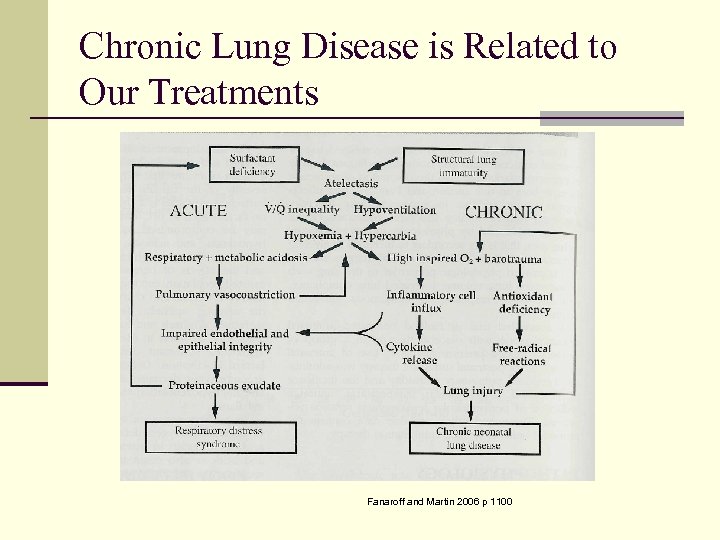 Chronic Lung Disease is Related to Our Treatments Fanaroff and Martin 2006 p 1100
Chronic Lung Disease is Related to Our Treatments Fanaroff and Martin 2006 p 1100
 Ventilator Strategies n Distending pressure n Lower Peak Inspiratory Pressures n Lower Tidal Volumes n Early extubation n Permissive hypercarbia n Permissive hypoxemia
Ventilator Strategies n Distending pressure n Lower Peak Inspiratory Pressures n Lower Tidal Volumes n Early extubation n Permissive hypercarbia n Permissive hypoxemia
 Nasal CPAP? n Some places use it exclusively as their first- line mode of respiratory support n Columbia Univ – 76% success in infants with BW < 1250 g and 50% with BW < 750 g n Requires everyone to buy into the system n Can’t give surfactant unless also intubated n Most places use n. CPAP for less severe symptoms, following extubation or in conjunction with “in-and-out” surfactant
Nasal CPAP? n Some places use it exclusively as their first- line mode of respiratory support n Columbia Univ – 76% success in infants with BW < 1250 g and 50% with BW < 750 g n Requires everyone to buy into the system n Can’t give surfactant unless also intubated n Most places use n. CPAP for less severe symptoms, following extubation or in conjunction with “in-and-out” surfactant
 High Flow Nasal Cannula n Nasal Cannula at atypical flows (< 1 LPM) n Usually 2 -8 LPM in our NICU n Used to provide distending pressure in a similar manner as n. CPAP n Does not appear to be equal to n. CPAP in efficacy n ? Increased respiratory infection rate
High Flow Nasal Cannula n Nasal Cannula at atypical flows (< 1 LPM) n Usually 2 -8 LPM in our NICU n Used to provide distending pressure in a similar manner as n. CPAP n Does not appear to be equal to n. CPAP in efficacy n ? Increased respiratory infection rate
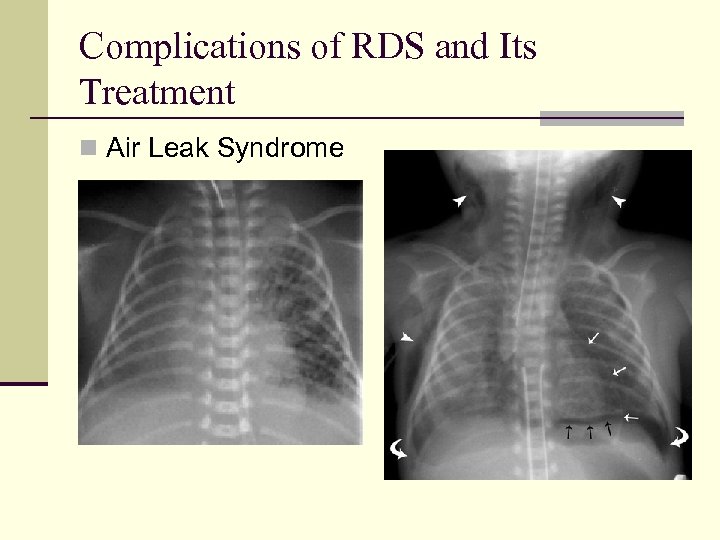 Complications of RDS and Its Treatment n Air Leak Syndrome
Complications of RDS and Its Treatment n Air Leak Syndrome
 More Complications n Airway injury n Subglottic stenosis (1% < 1. 5 kg) n Infection n PDA n IVH n Long-term outcomes n More related to gestational age and BW n Most with normal exercise tolerance
More Complications n Airway injury n Subglottic stenosis (1% < 1. 5 kg) n Infection n PDA n IVH n Long-term outcomes n More related to gestational age and BW n Most with normal exercise tolerance
 BPD, a Most Troubling Complication n It begins with the definition: n Supplemental oxygen at 28 days of life following oxygen/ventilator therapy in the first week of life n Supplemental oxygen at 36 weeks PMA following oxygen/ventilator therapy in the first week of life n NIH consensus conference 2000
BPD, a Most Troubling Complication n It begins with the definition: n Supplemental oxygen at 28 days of life following oxygen/ventilator therapy in the first week of life n Supplemental oxygen at 36 weeks PMA following oxygen/ventilator therapy in the first week of life n NIH consensus conference 2000
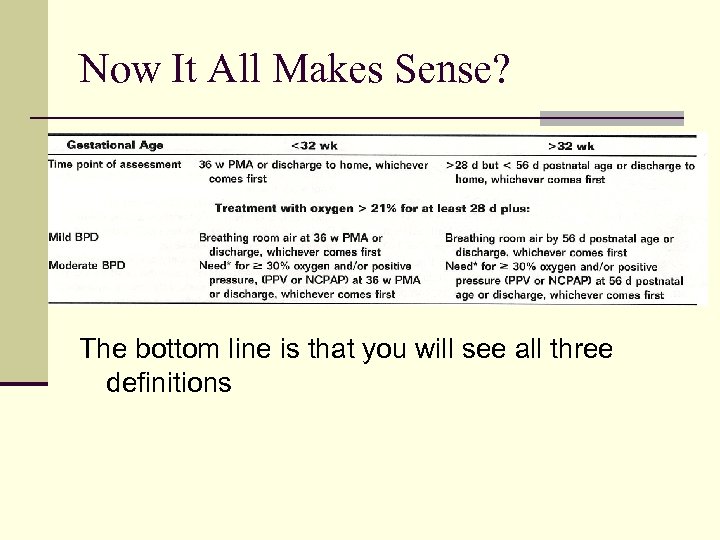 Now It All Makes Sense? The bottom line is that you will see all three definitions
Now It All Makes Sense? The bottom line is that you will see all three definitions
 Pathophysiology of BPD n Lungs are attempting to: n Heal n Grow and develop n Respond to continued insults
Pathophysiology of BPD n Lungs are attempting to: n Heal n Grow and develop n Respond to continued insults
 CLD is Associated With: n Prematurity n Mechanical trauma n Oxygen toxicity n Infection/inflammation n Pulmonary edema n PDA n ? genetics
CLD is Associated With: n Prematurity n Mechanical trauma n Oxygen toxicity n Infection/inflammation n Pulmonary edema n PDA n ? genetics
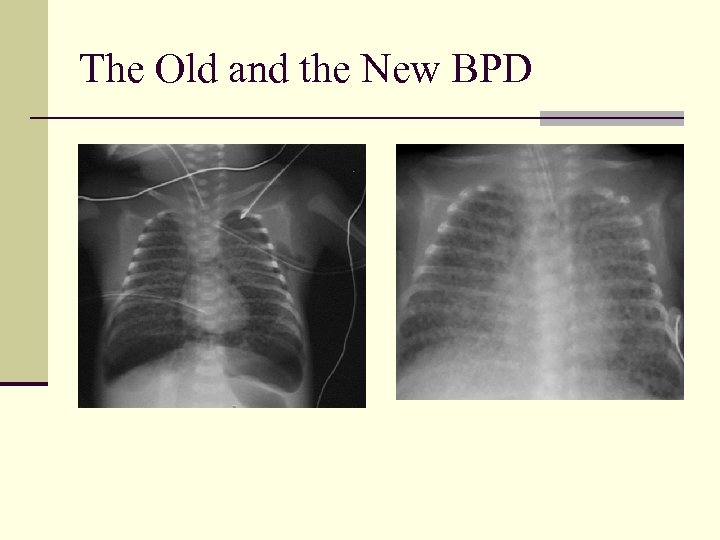 The Old and the New BPD
The Old and the New BPD
 Clinical Features n BPD is a systemic disease n Pulmonary n Respiratory distress n Hypoxemia, hypercarbia n Increased airways resistance n Growth deficiency n Developmental delay n Cardiovascular dysfunction n Systemic hypertension, ventricular hypertrophy n Metabolic derangements n Sodium, calcium, etc
Clinical Features n BPD is a systemic disease n Pulmonary n Respiratory distress n Hypoxemia, hypercarbia n Increased airways resistance n Growth deficiency n Developmental delay n Cardiovascular dysfunction n Systemic hypertension, ventricular hypertrophy n Metabolic derangements n Sodium, calcium, etc
 Management n Minimize further harm n Permissive hypercapnea. etc. n Aggressive nutritional support n Conservative fluid management n Caution with diuretics n +/- bronchodilators n Steroids with caution n Minimize and aggressively treat infections n Developmental care
Management n Minimize further harm n Permissive hypercapnea. etc. n Aggressive nutritional support n Conservative fluid management n Caution with diuretics n +/- bronchodilators n Steroids with caution n Minimize and aggressively treat infections n Developmental care
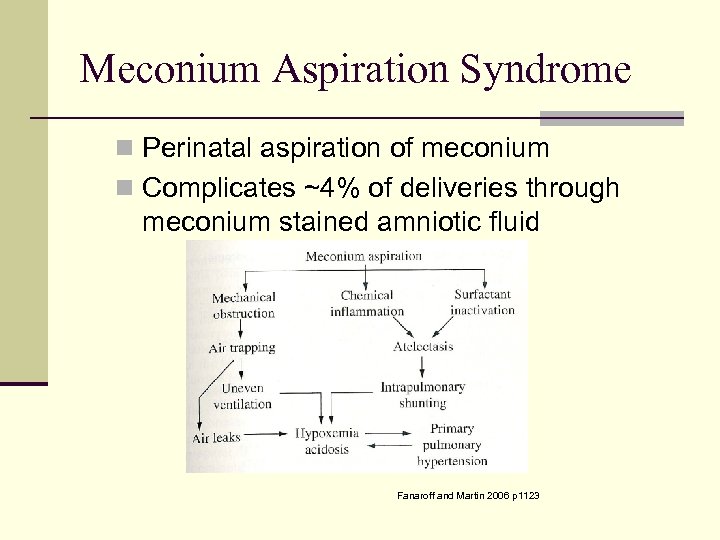 Meconium Aspiration Syndrome n Perinatal aspiration of meconium n Complicates ~4% of deliveries through meconium stained amniotic fluid Fanaroff and Martin 2006 p 1123
Meconium Aspiration Syndrome n Perinatal aspiration of meconium n Complicates ~4% of deliveries through meconium stained amniotic fluid Fanaroff and Martin 2006 p 1123
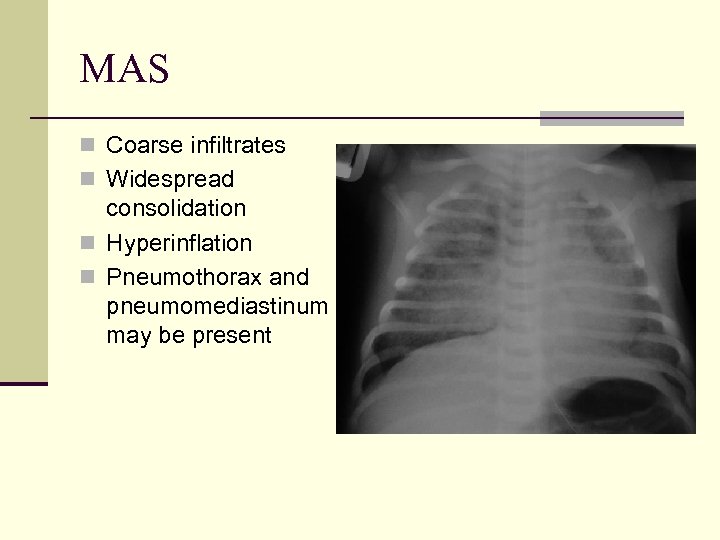 MAS n Coarse infiltrates n Widespread consolidation n Hyperinflation n Pneumothorax and pneumomediastinum may be present
MAS n Coarse infiltrates n Widespread consolidation n Hyperinflation n Pneumothorax and pneumomediastinum may be present
 Management of MAS n Prevention n Supportive respiratory therapy n ? Higher p. O 2 n Normal p. CO 2 n Nitric oxide and other PPHN therapies n Antibiotics n surfactant
Management of MAS n Prevention n Supportive respiratory therapy n ? Higher p. O 2 n Normal p. CO 2 n Nitric oxide and other PPHN therapies n Antibiotics n surfactant
 Transient Tachypnea n Described in the 1960 s n Later called RDS Type 2 n Delayed clearance of pulmonary fluid n More common in: n Late preterm n C/S birth n Perinatal depression n Maternal diabetes n Diagnosis of exclusion
Transient Tachypnea n Described in the 1960 s n Later called RDS Type 2 n Delayed clearance of pulmonary fluid n More common in: n Late preterm n C/S birth n Perinatal depression n Maternal diabetes n Diagnosis of exclusion
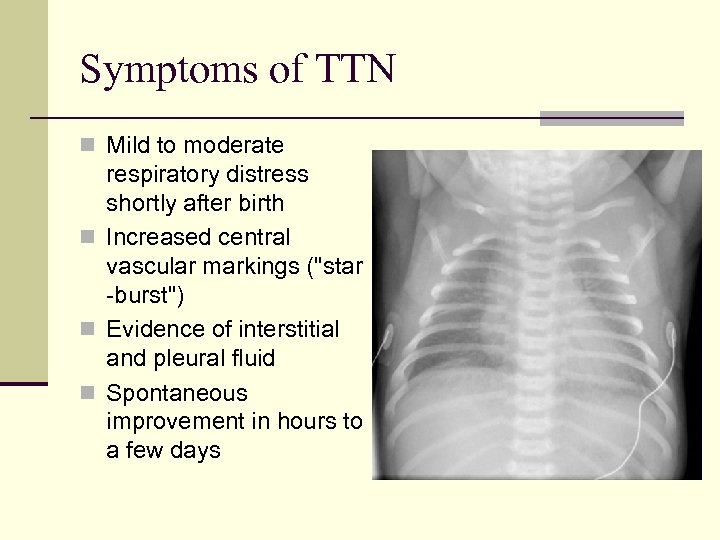 Symptoms of TTN n Mild to moderate respiratory distress shortly after birth n Increased central vascular markings ("star -burst") n Evidence of interstitial and pleural fluid n Spontaneous improvement in hours to a few days
Symptoms of TTN n Mild to moderate respiratory distress shortly after birth n Increased central vascular markings ("star -burst") n Evidence of interstitial and pleural fluid n Spontaneous improvement in hours to a few days
 Other Aspiration Syndromes n Babies can aspirate blood and amniotic fluid n No specific diagnostic test n May mimic TTN or MAS n Management is the same
Other Aspiration Syndromes n Babies can aspirate blood and amniotic fluid n No specific diagnostic test n May mimic TTN or MAS n Management is the same



