Colonic polyps - Waleed Fouad.ppt
- Количество слайдов: 54
Colonic polyps Made by: Islamova Sh. Group: 646 P.
Background n n Polyps are slow-growing overgrowths of the colonic mucosa that carry a small risk (<1%) of becoming malignant. However, because polyps are highly prevalent in the general population (especially with increasing age), they confer an important predisposition to colon cancer and are therefore removed when detected. Patients with isolated polyps are usually asymptomatic. Polyps can occur as part of inherited polyposis syndromes in which their number is greater and the risk for malignant progression is much greater compared to the risk with isolated polyps.
Pathophysiology n n Colonic polyps, or adenomas, are benign epithelial neoplasms that arise from the epithelial cells lining the colon. Polyps are traditionally divided into 4 groups. Hyperplastic polyps. n Adenomas. n Polyposis syndromes. n Miscellaneous. n
Hyperplastic polyps n n Hyperplastic polyps comprise about 90% of all polyps and are totally benign protrusions. They are usually less than 0. 5 cm in diameter. They most commonly occur in the rectosigmoid region during adulthood. The lesions tend to be smaller than adenomas and do not appear to be related to the adenoma-carcinoma sequence.

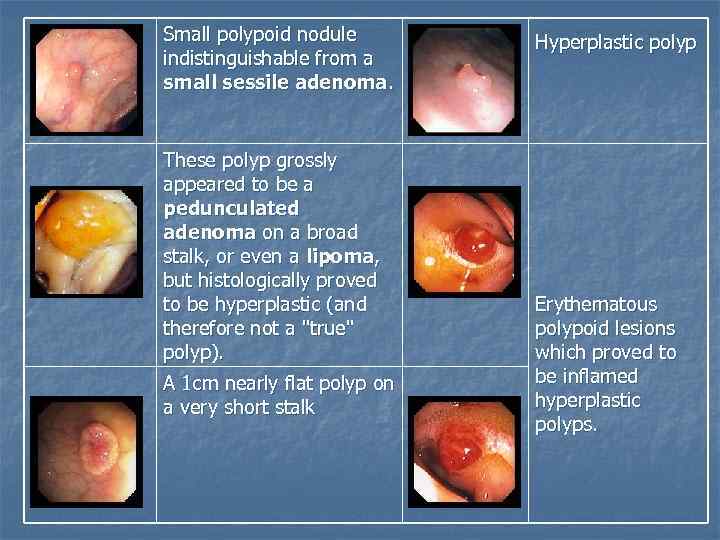
Small polypoid nodule indistinguishable from a small sessile adenoma. These polyp grossly appeared to be a pedunculated adenoma on a broad stalk, or even a lipoma, but histologically proved to be hyperplastic (and therefore not a "true" polyp). A 1 cm nearly flat polyp on a very short stalk Hyperplastic polyp Erythematous polypoid lesions which proved to be inflamed hyperplastic polyps.
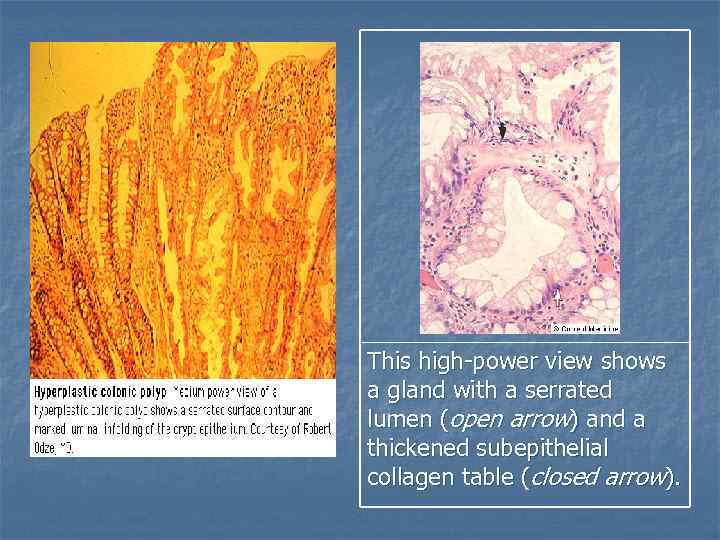
This high-power view shows a gland with a serrated lumen (open arrow) and a thickened subepithelial collagen table (closed arrow).
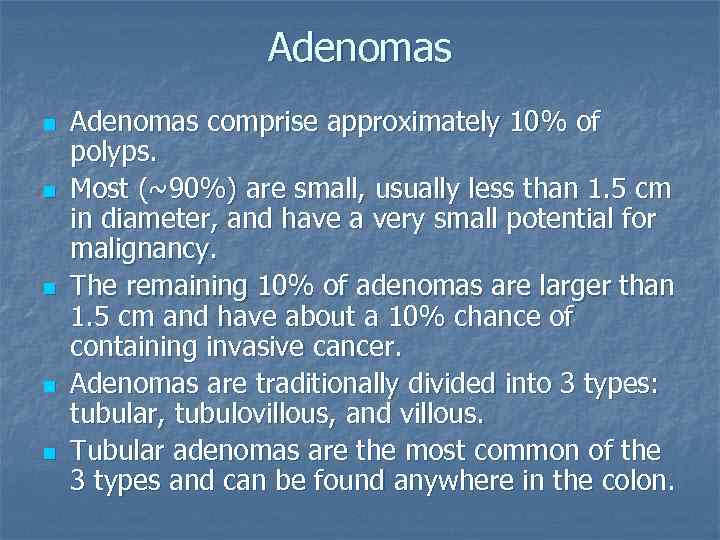
Adenomas n n n Adenomas comprise approximately 10% of polyps. Most (~90%) are small, usually less than 1. 5 cm in diameter, and have a very small potential for malignancy. The remaining 10% of adenomas are larger than 1. 5 cm and have about a 10% chance of containing invasive cancer. Adenomas are traditionally divided into 3 types: tubular, tubulovillous, and villous. Tubular adenomas are the most common of the 3 types and can be found anywhere in the colon.
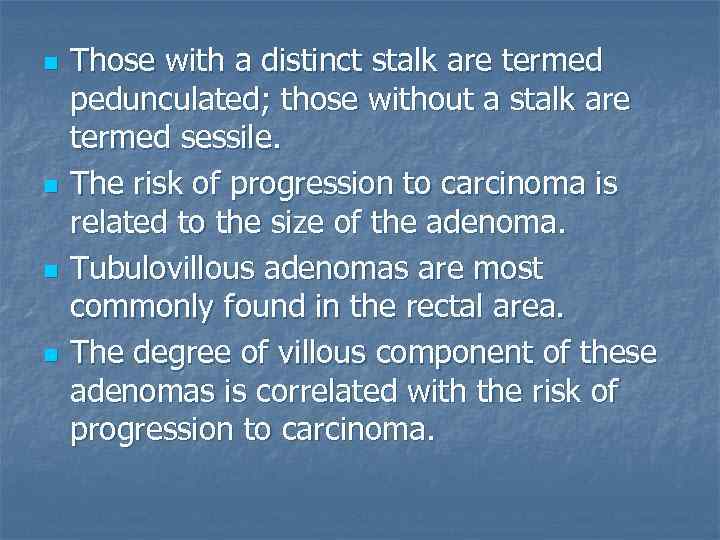
n n Those with a distinct stalk are termed pedunculated; those without a stalk are termed sessile. The risk of progression to carcinoma is related to the size of the adenoma. Tubulovillous adenomas are most commonly found in the rectal area. The degree of villous component of these adenomas is correlated with the risk of progression to carcinoma.
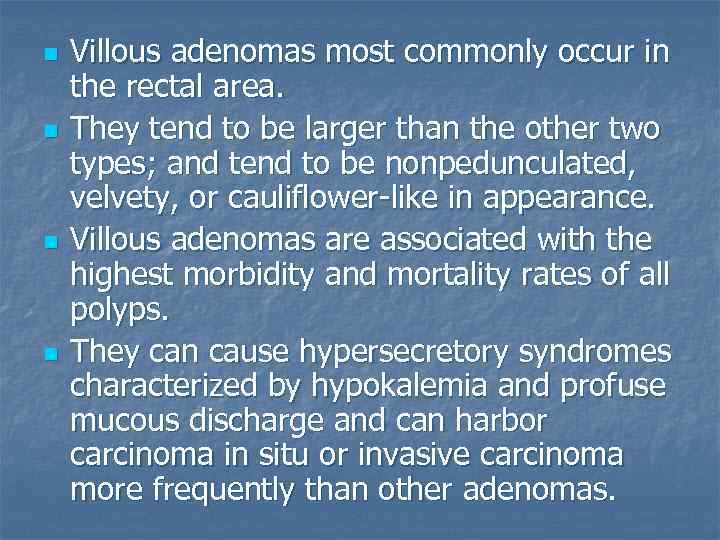
n n Villous adenomas most commonly occur in the rectal area. They tend to be larger than the other two types; and tend to be nonpedunculated, velvety, or cauliflower-like in appearance. Villous adenomas are associated with the highest morbidity and mortality rates of all polyps. They can cause hypersecretory syndromes characterized by hypokalemia and profuse mucous discharge and can harbor carcinoma in situ or invasive carcinoma more frequently than other adenomas.
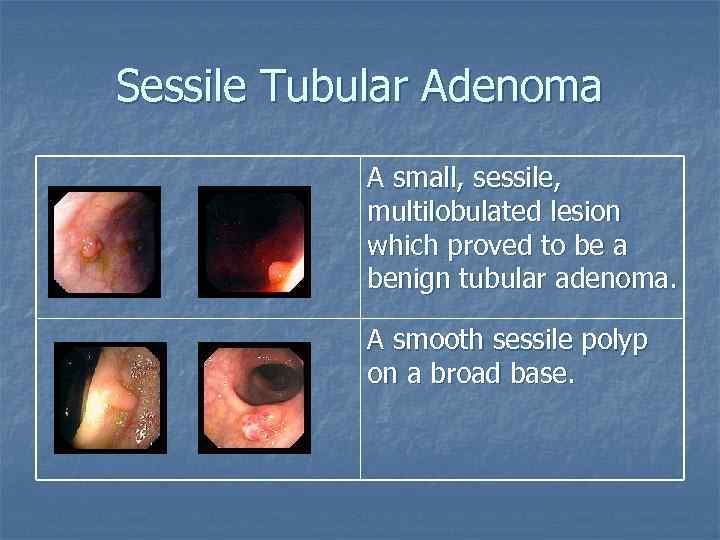
Sessile Tubular Adenoma A small, sessile, multilobulated lesion which proved to be a benign tubular adenoma. A smooth sessile polyp on a broad base.
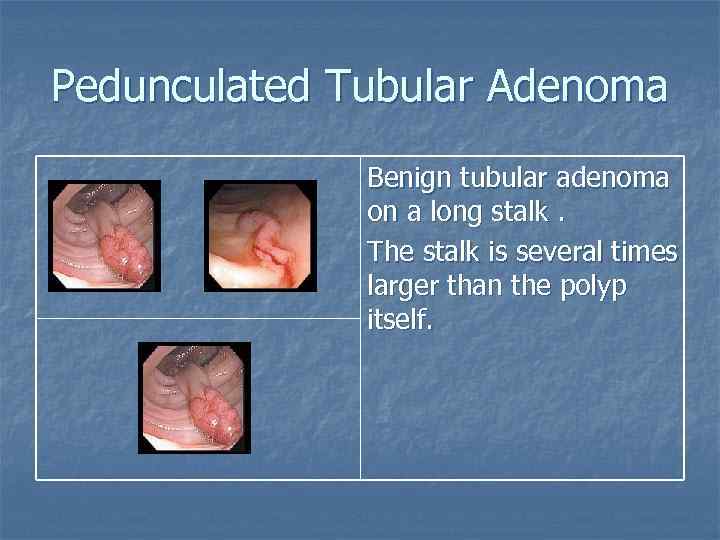
Pedunculated Tubular Adenoma Benign tubular adenoma on a long stalk. The stalk is several times larger than the polyp itself.
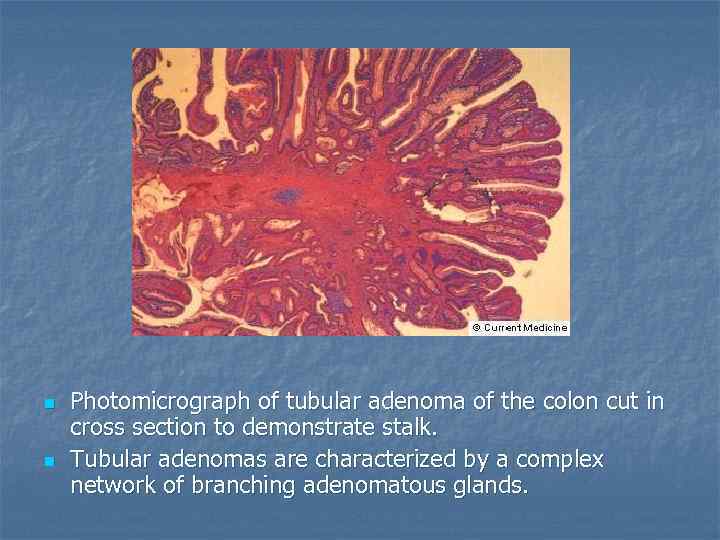
n n Photomicrograph of tubular adenoma of the colon cut in cross section to demonstrate stalk. Tubular adenomas are characterized by a complex network of branching adenomatous glands.
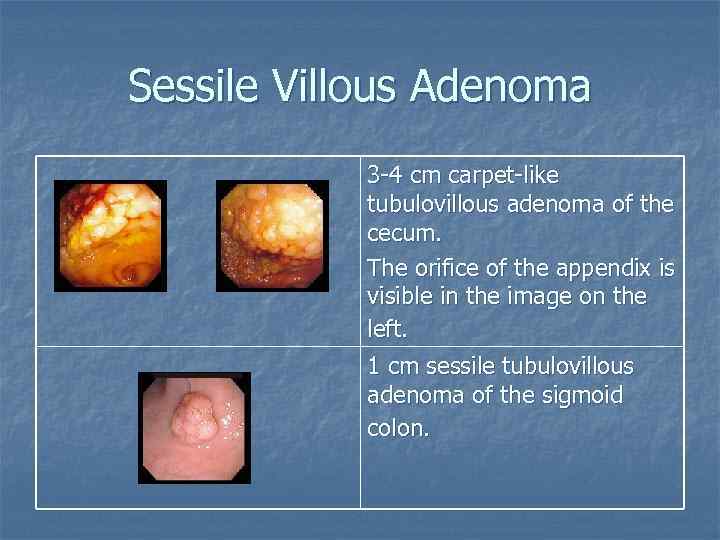
Sessile Villous Adenoma 3 -4 cm carpet-like tubulovillous adenoma of the cecum. The orifice of the appendix is visible in the image on the left. 1 cm sessile tubulovillous adenoma of the sigmoid colon.
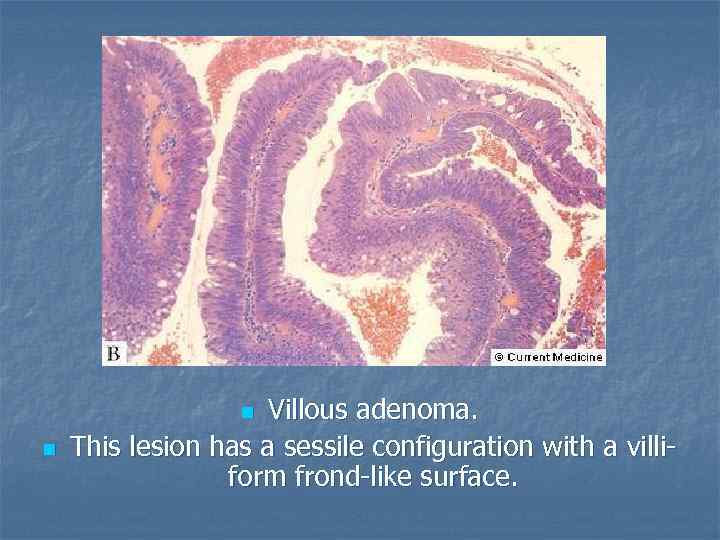
Villous adenoma. This lesion has a sessile configuration with a villiform frond-like surface. n n
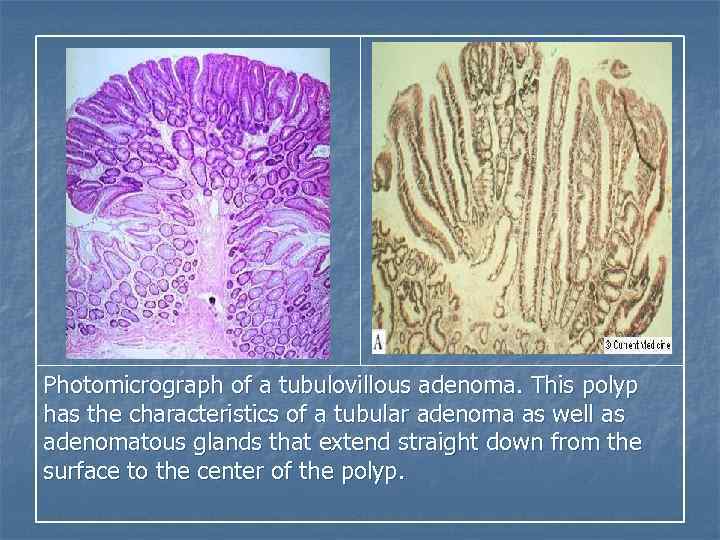
Photomicrograph of a tubulovillous adenoma. This polyp has the characteristics of a tubular adenoma as well as adenomatous glands that extend straight down from the surface to the center of the polyp.
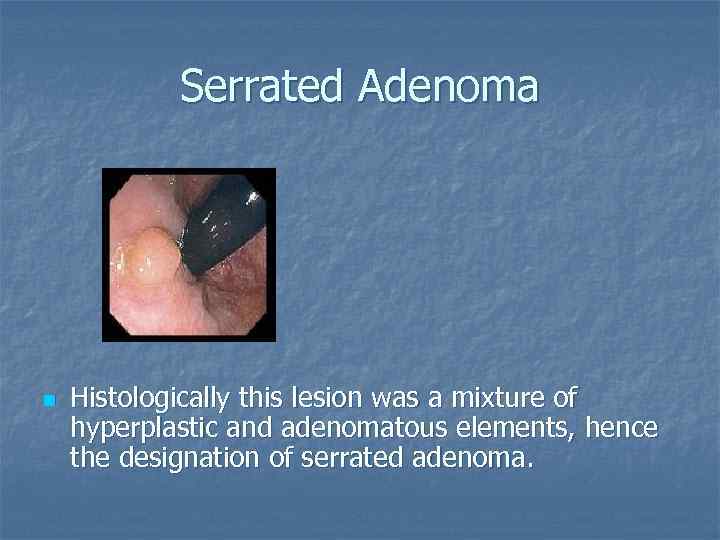
Serrated Adenoma n Histologically this lesion was a mixture of hyperplastic and adenomatous elements, hence the designation of serrated adenoma.
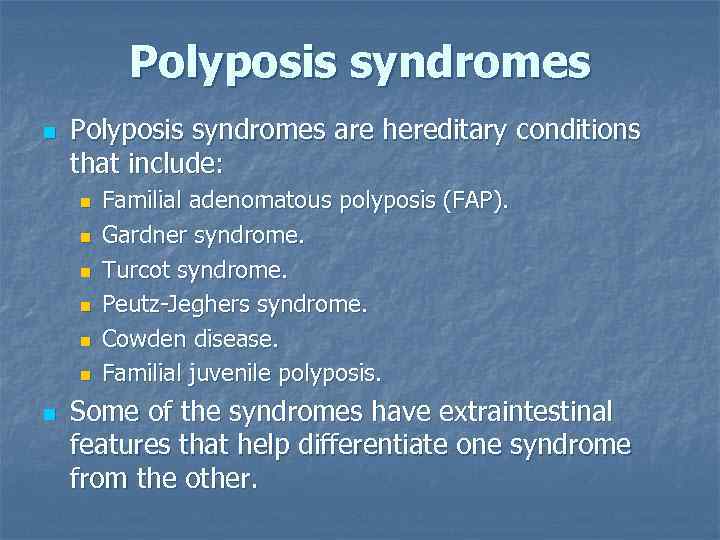
Polyposis syndromes n Polyposis syndromes are hereditary conditions that include: n n n n Familial adenomatous polyposis (FAP). Gardner syndrome. Turcot syndrome. Peutz-Jeghers syndrome. Cowden disease. Familial juvenile polyposis. Some of the syndromes have extraintestinal features that help differentiate one syndrome from the other.
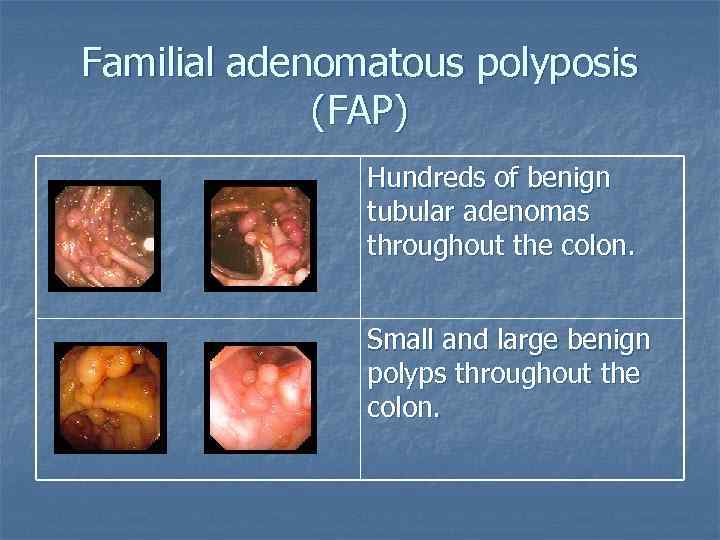
Familial adenomatous polyposis (FAP) Hundreds of benign tubular adenomas throughout the colon. Small and large benign polyps throughout the colon.
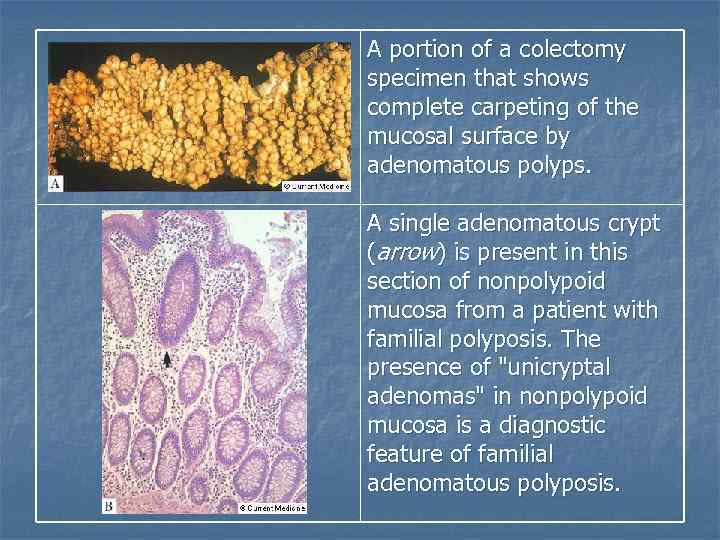
A portion of a colectomy specimen that shows complete carpeting of the mucosal surface by adenomatous polyps. A single adenomatous crypt (arrow) is present in this section of nonpolypoid mucosa from a patient with familial polyposis. The presence of "unicryptal adenomas" in nonpolypoid mucosa is a diagnostic feature of familial adenomatous polyposis.
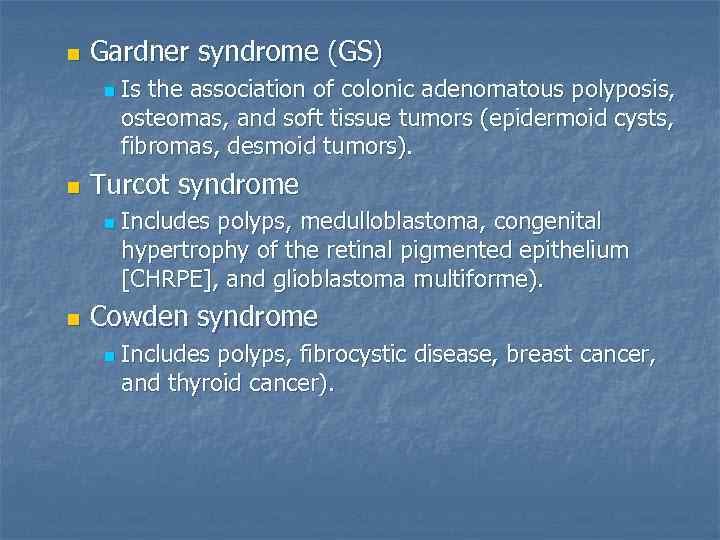
n Gardner syndrome (GS) n n Turcot syndrome n n Is the association of colonic adenomatous polyposis, osteomas, and soft tissue tumors (epidermoid cysts, fibromas, desmoid tumors). Includes polyps, medulloblastoma, congenital hypertrophy of the retinal pigmented epithelium [CHRPE], and glioblastoma multiforme). Cowden syndrome n Includes polyps, fibrocystic disease, breast cancer, and thyroid cancer).
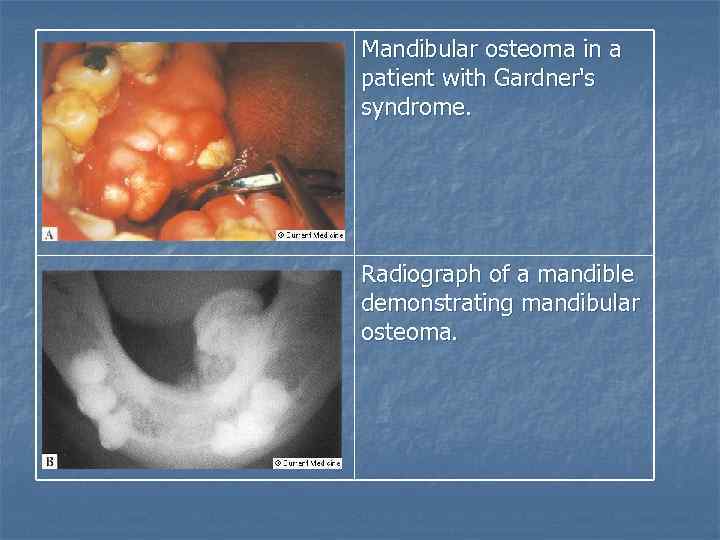
Mandibular osteoma in a patient with Gardner's syndrome. Radiograph of a mandible demonstrating mandibular osteoma.
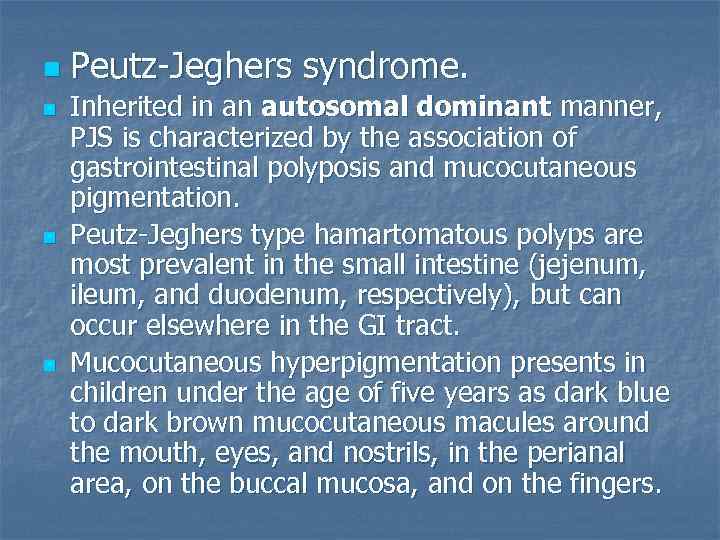
n n Peutz-Jeghers syndrome. Inherited in an autosomal dominant manner, PJS is characterized by the association of gastrointestinal polyposis and mucocutaneous pigmentation. Peutz-Jeghers type hamartomatous polyps are most prevalent in the small intestine (jejenum, ileum, and duodenum, respectively), but can occur elsewhere in the GI tract. Mucocutaneous hyperpigmentation presents in children under the age of five years as dark blue to dark brown mucocutaneous macules around the mouth, eyes, and nostrils, in the perianal area, on the buccal mucosa, and on the fingers.
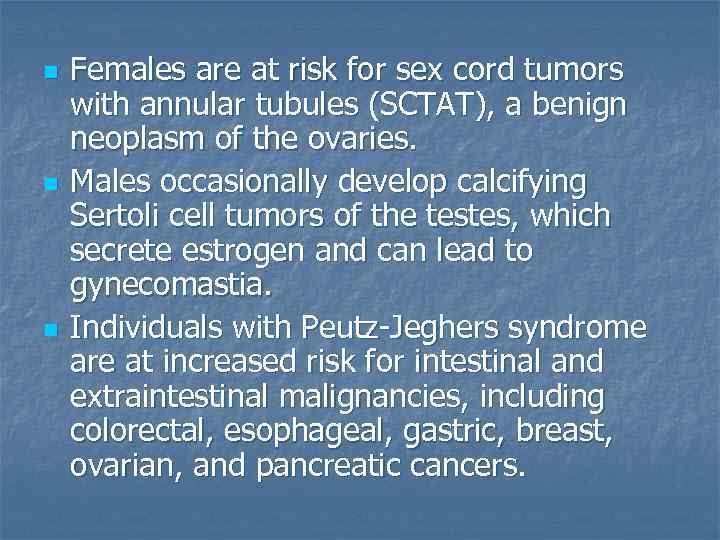
n n n Females are at risk for sex cord tumors with annular tubules (SCTAT), a benign neoplasm of the ovaries. Males occasionally develop calcifying Sertoli cell tumors of the testes, which secrete estrogen and can lead to gynecomastia. Individuals with Peutz-Jeghers syndrome are at increased risk for intestinal and extraintestinal malignancies, including colorectal, esophageal, gastric, breast, ovarian, and pancreatic cancers.
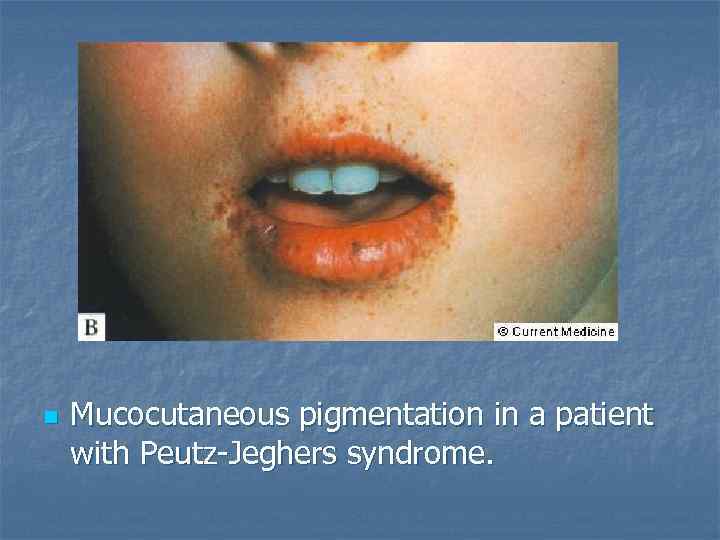
n Mucocutaneous pigmentation in a patient with Peutz-Jeghers syndrome.
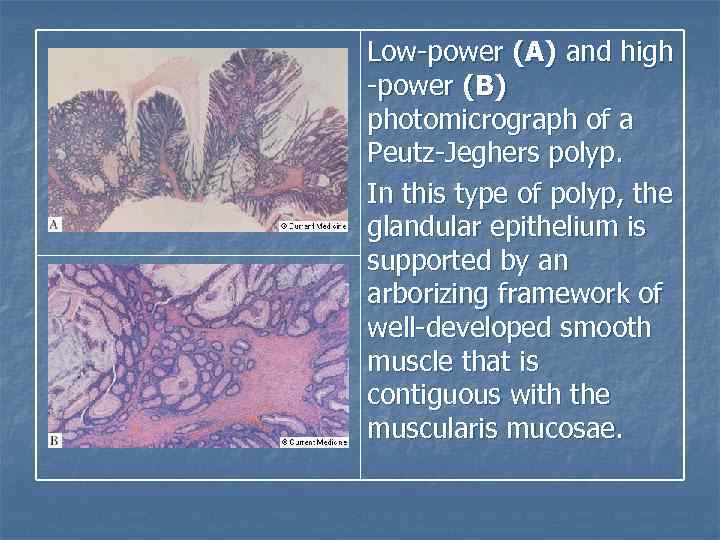
Low-power (A) and high -power (B) photomicrograph of a Peutz-Jeghers polyp. In this type of polyp, the glandular epithelium is supported by an arborizing framework of well-developed smooth muscle that is contiguous with the muscularis mucosae.
Juvenile polyposis syndrome (JPS) n n Juvenile polyposis syndrome (JPS) is characterized by predisposition for hamartomatous polyps in the gastrointestinal (GI) tract, specifically in the stomach, small intestine, colon, and rectum. JPS is diagnosed if any one of the following is present: n n More than five juvenile polyps of the colorectum. OR Multiple juvenile polyps throughout the GI tract. OR Any number of juvenile polyps. and a Family history of juvenile polyps.
n n n The term "juvenile" refers to the type of polyp, not the age of onset of polyps. Most individuals with JPS have some polyps by 20 years of age. Some individuals may only have four or five polyps over their lifetimes, whereas others in the same family may have over a hundred. Most juvenile polyps are benign; however, malignant transformation can occur. Estimates of developing GI cancers in families with JPS range from 9 -50%.
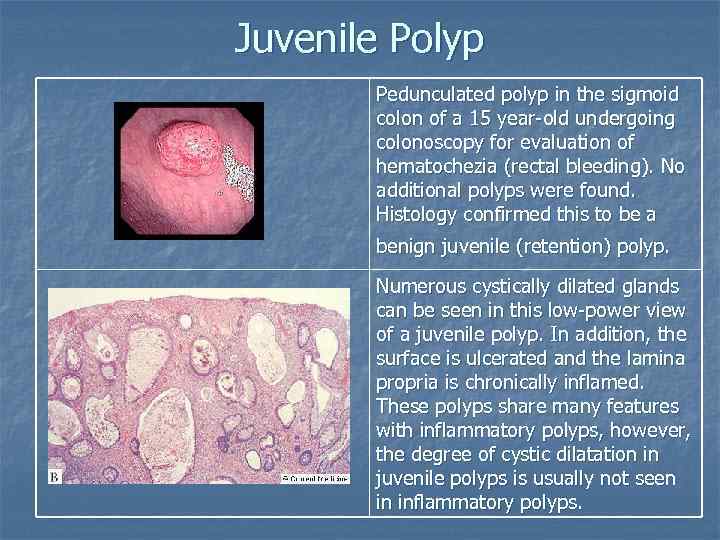
Juvenile Polyp Pedunculated polyp in the sigmoid colon of a 15 year-old undergoing colonoscopy for evaluation of hematochezia (rectal bleeding). No additional polyps were found. Histology confirmed this to be a benign juvenile (retention) polyp. Numerous cystically dilated glands can be seen in this low-power view of a juvenile polyp. In addition, the surface is ulcerated and the lamina propria is chronically inflamed. These polyps share many features with inflammatory polyps, however, the degree of cystic dilatation in juvenile polyps is usually not seen in inflammatory polyps.
Other hereditary syndromes n Hereditary mixed polyposis syndrome Mode of inheritance is unknown. n The syndrome is characterized by atypical juvenile polyps, polyps containing mixed histology, or multiple polyps of more than one histologic type in an individual. n n Neurofibromatosis type 1 (NF 1) n Individuals with NF 1 may exhibit multiple intestinal polypoid neurofibromas or ganglioneuromas in the small bowel, stomach, and colon.
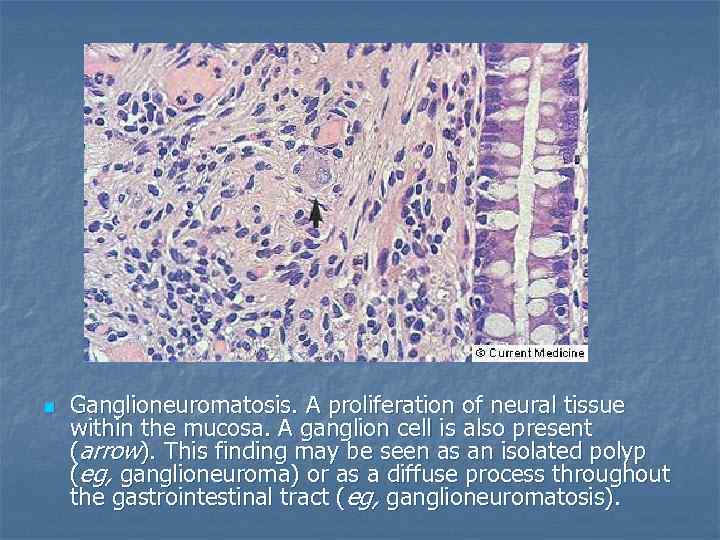
n Ganglioneuromatosis. A proliferation of neural tissue within the mucosa. A ganglion cell is also present (arrow). This finding may be seen as an isolated polyp (eg, ganglioneuroma) or as a diffuse process throughout the gastrointestinal tract (eg, ganglioneuromatosis).
Hereditary non-polyposis colon cancer (HNPCC) n n It is an autosomal dominant colon cancer syndrome with proximal colonic predominance. Few colonic adenomas are present. Other malignancies include cancer of the endometrium, ovary, stomach, small intestine, and urinary tract. It may be difficult to distinguish between HNPCC and attenuated FAP in individuals and families who have few adenomatous colonic polyps.
Acquired syndrome n Cronkite-Canada syndrome n Generalized gastrointestinal hamartomatous polyposis, cutaneous hyperpigmentation, hair loss, and nail atrophy.
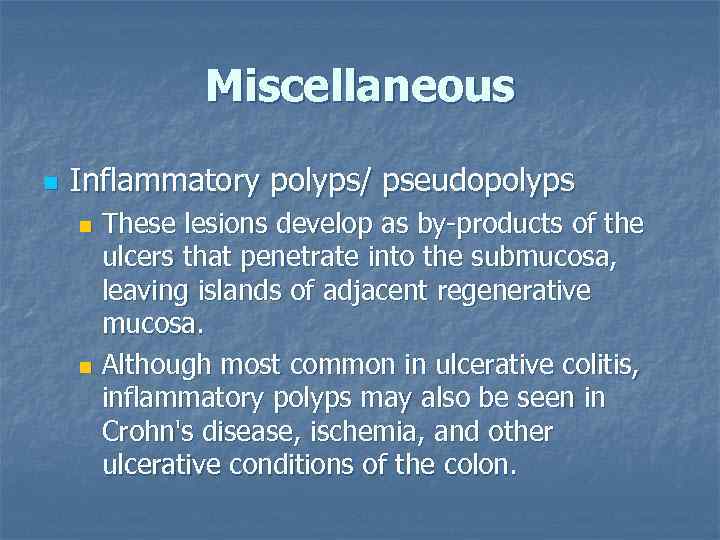
Miscellaneous n Inflammatory polyps/ pseudopolyps These lesions develop as by-products of the ulcers that penetrate into the submucosa, leaving islands of adjacent regenerative mucosa. n Although most common in ulcerative colitis, inflammatory polyps may also be seen in Crohn's disease, ischemia, and other ulcerative conditions of the colon. n
The colonic mucosa shows numerous inflammatory polyps with intervening areas of ulceration. The pseudopolyp has an ulcerated surface lined with granulation tissue. The underlying crypts are distorted and contain regenerative epithelium. The deep lamina propria often contains increased numbers of plasma cells and lymphocytes. Severe ulcerative colitis with pseudopolyps.
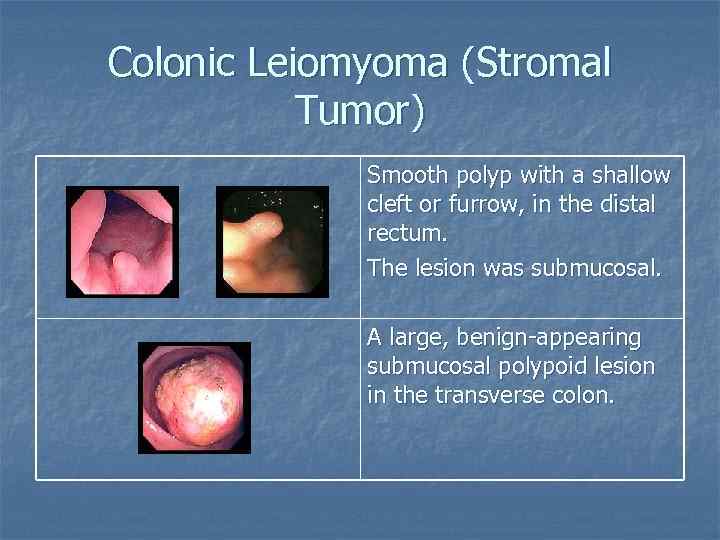
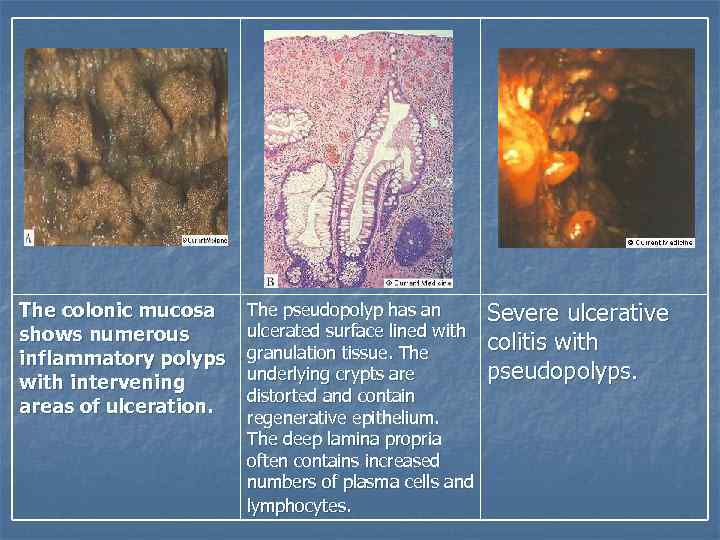
Colonic Leiomyoma (Stromal Tumor) Smooth polyp with a shallow cleft or furrow, in the distal rectum. The lesion was submucosal. A large, benign-appearing submucosal polypoid lesion in the transverse colon.
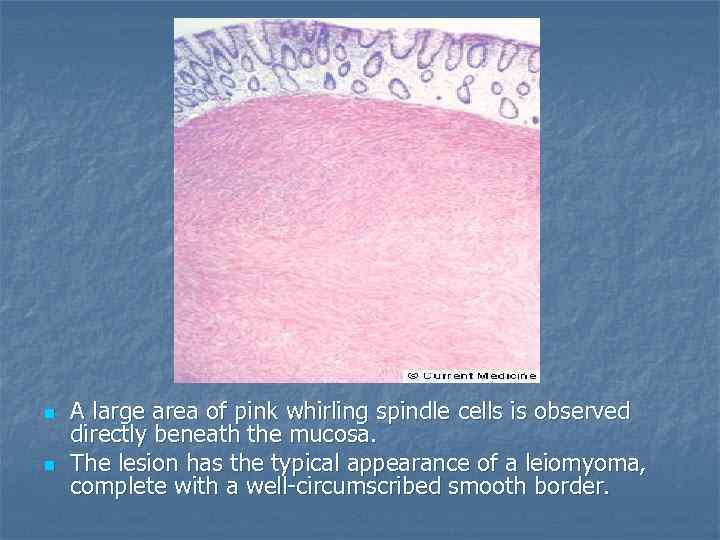
n n A large area of pink whirling spindle cells is observed directly beneath the mucosa. The lesion has the typical appearance of a leiomyoma, complete with a well-circumscribed smooth border.
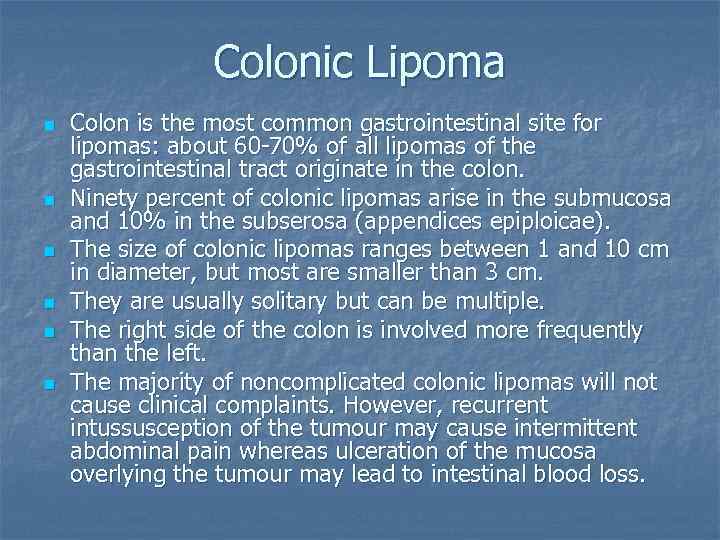
Colonic Lipoma n n n Colon is the most common gastrointestinal site for lipomas: about 60 -70% of all lipomas of the gastrointestinal tract originate in the colon. Ninety percent of colonic lipomas arise in the submucosa and 10% in the subserosa (appendices epiploicae). The size of colonic lipomas ranges between 1 and 10 cm in diameter, but most are smaller than 3 cm. They are usually solitary but can be multiple. The right side of the colon is involved more frequently than the left. The majority of noncomplicated colonic lipomas will not cause clinical complaints. However, recurrent intussusception of the tumour may cause intermittent abdominal pain whereas ulceration of the mucosa overlying the tumour may lead to intestinal blood loss.
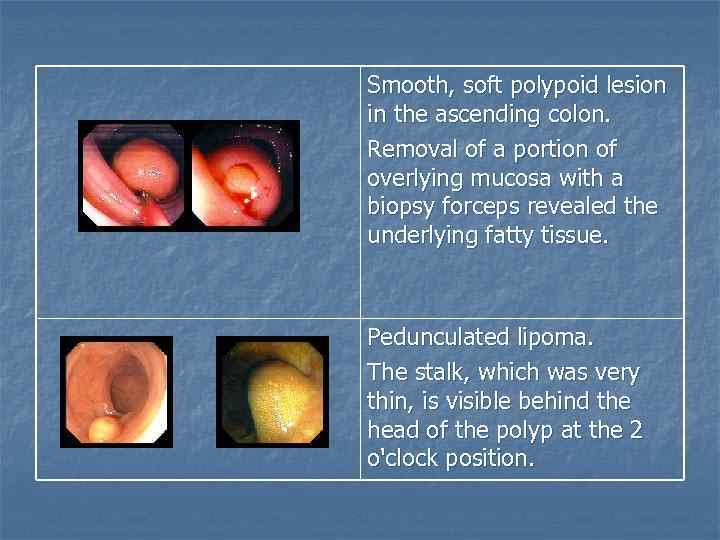
Smooth, soft polypoid lesion in the ascending colon. Removal of a portion of overlying mucosa with a biopsy forceps revealed the underlying fatty tissue. Pedunculated lipoma. The stalk, which was very thin, is visible behind the head of the polyp at the 2 o'clock position.
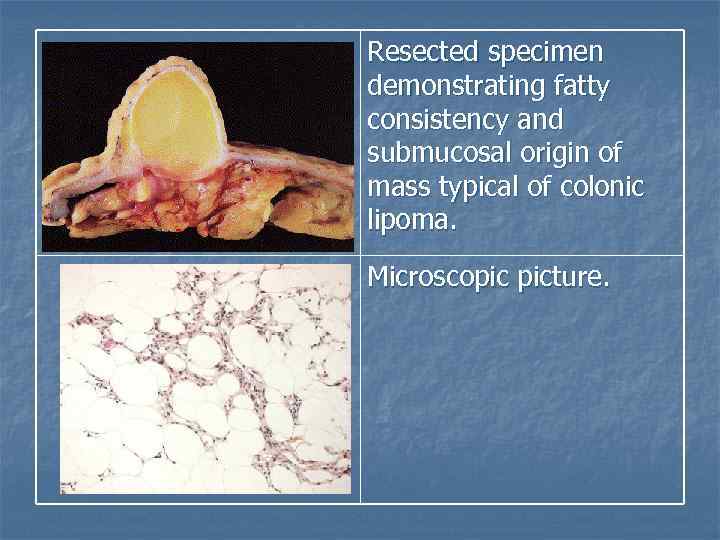
Resected specimen demonstrating fatty consistency and submucosal origin of mass typical of colonic lipoma. Microscopic picture.
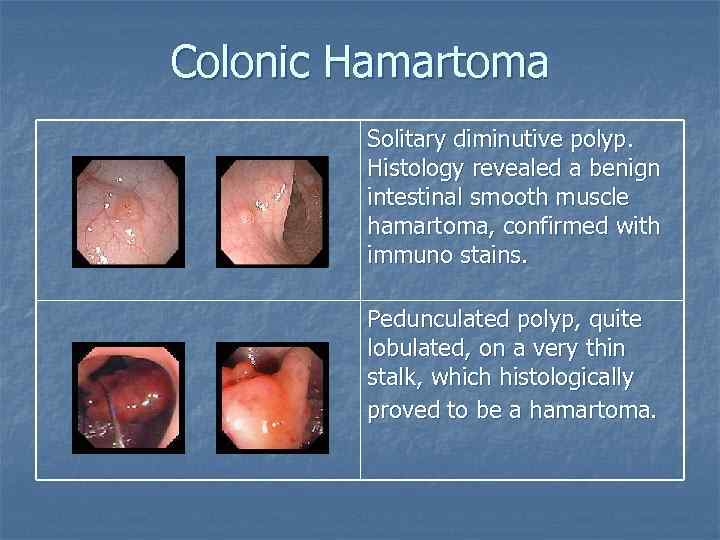
Colonic Hamartoma Solitary diminutive polyp. Histology revealed a benign intestinal smooth muscle hamartoma, confirmed with immuno stains. Pedunculated polyp, quite lobulated, on a very thin stalk, which histologically proved to be a hamartoma.
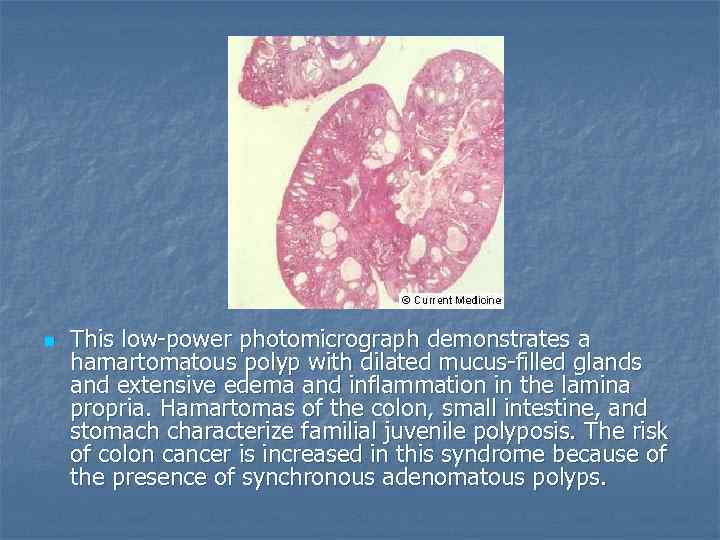
n This low-power photomicrograph demonstrates a hamartomatous polyp with dilated mucus-filled glands and extensive edema and inflammation in the lamina propria. Hamartomas of the colon, small intestine, and stomach characterize familial juvenile polyposis. The risk of colon cancer is increased in this syndrome because of the presence of synchronous adenomatous polyps.
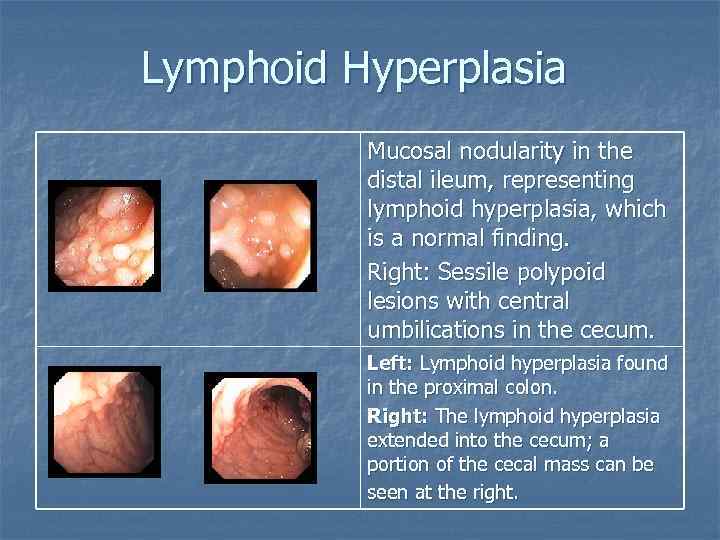
Lymphoid Hyperplasia Mucosal nodularity in the distal ileum, representing lymphoid hyperplasia, which is a normal finding. Right: Sessile polypoid lesions with central umbilications in the cecum. Left: Lymphoid hyperplasia found in the proximal colon. Right: The lymphoid hyperplasia extended into the cecum; a portion of the cecal mass can be seen at the right.
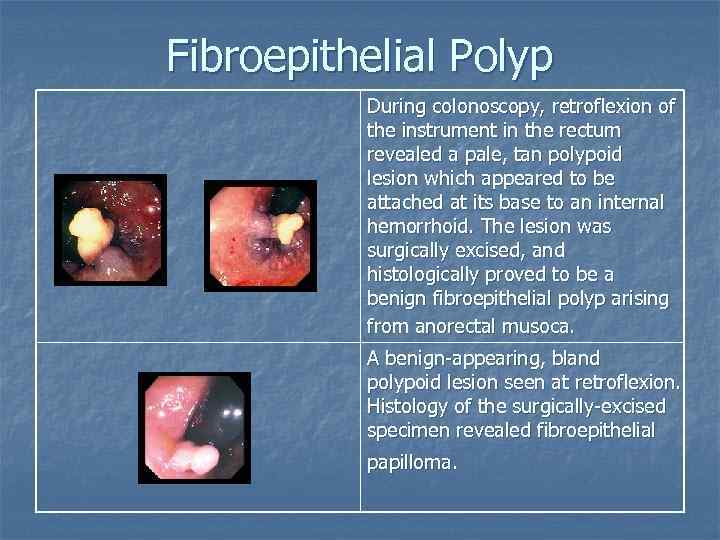
Fibroepithelial Polyp During colonoscopy, retroflexion of the instrument in the rectum revealed a pale, tan polypoid lesion which appeared to be attached at its base to an internal hemorrhoid. The lesion was surgically excised, and histologically proved to be a benign fibroepithelial polyp arising from anorectal musoca. A benign-appearing, bland polypoid lesion seen at retroflexion. Histology of the surgically-excised specimen revealed fibroepithelial papilloma.
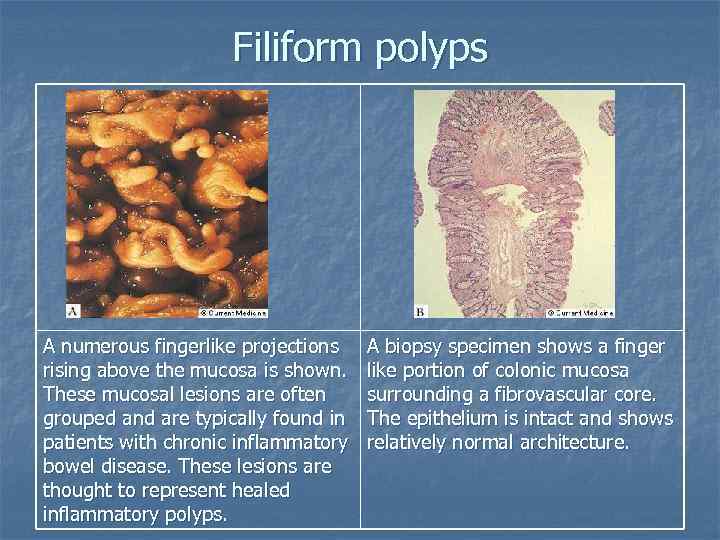
Filiform polyps A numerous fingerlike projections rising above the mucosa is shown. These mucosal lesions are often grouped and are typically found in patients with chronic inflammatory bowel disease. These lesions are thought to represent healed inflammatory polyps. A biopsy specimen shows a finger like portion of colonic mucosa surrounding a fibrovascular core. The epithelium is intact and shows relatively normal architecture.
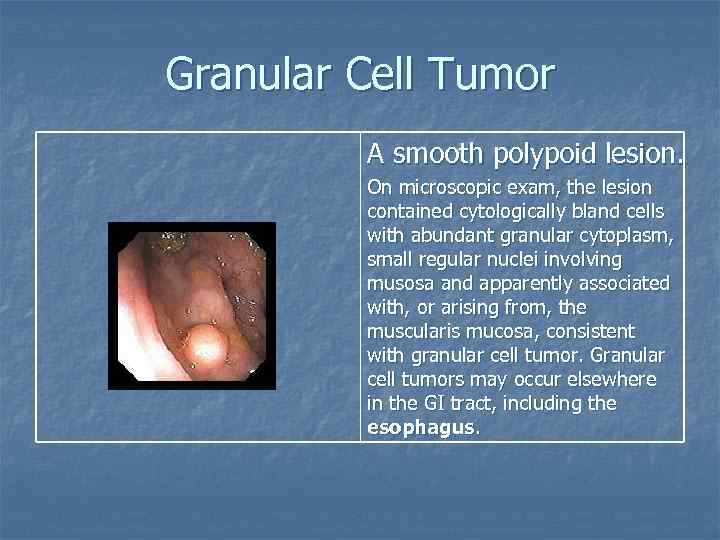
Granular Cell Tumor A smooth polypoid lesion. On microscopic exam, the lesion contained cytologically bland cells with abundant granular cytoplasm, small regular nuclei involving musosa and apparently associated with, or arising from, the muscularis mucosa, consistent with granular cell tumor. Granular cell tumors may occur elsewhere in the GI tract, including the esophagus.
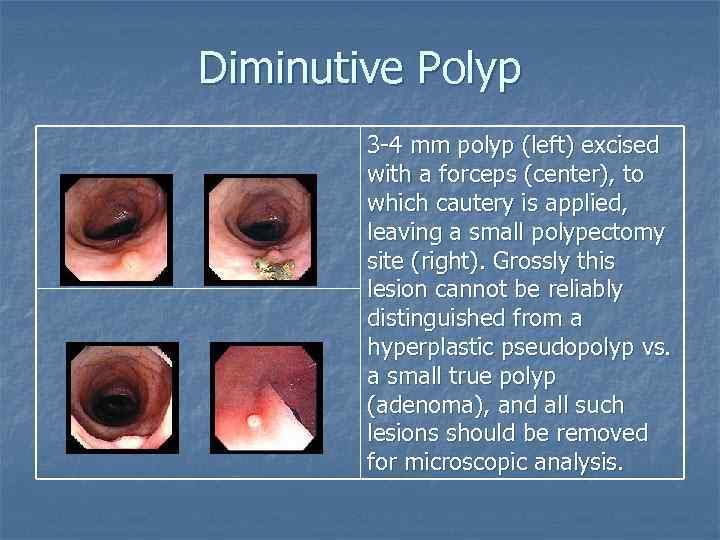
Diminutive Polyp 3 -4 mm polyp (left) excised with a forceps (center), to which cautery is applied, leaving a small polypectomy site (right). Grossly this lesion cannot be reliably distinguished from a hyperplastic pseudopolyp vs. a small true polyp (adenoma), and all such lesions should be removed for microscopic analysis.
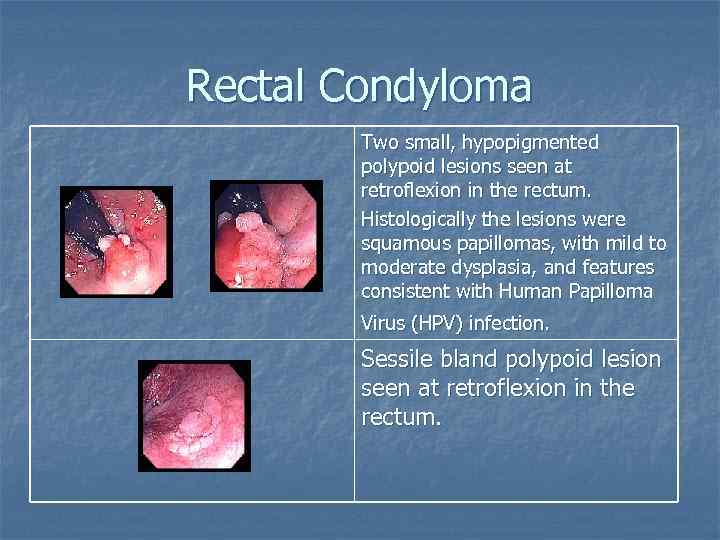
Rectal Condyloma Two small, hypopigmented polypoid lesions seen at retroflexion in the rectum. Histologically the lesions were squamous papillomas, with mild to moderate dysplasia, and features consistent with Human Papilloma Virus (HPV) infection. Sessile bland polypoid lesion seen at retroflexion in the rectum.
Lymphomatous polyposis n n Occurrence of primary extranodal lymphomas in the gastrointestinal tract. Two types include: Multiple lymphomatous polyposis. n Mediterranean-type lymphoma. n
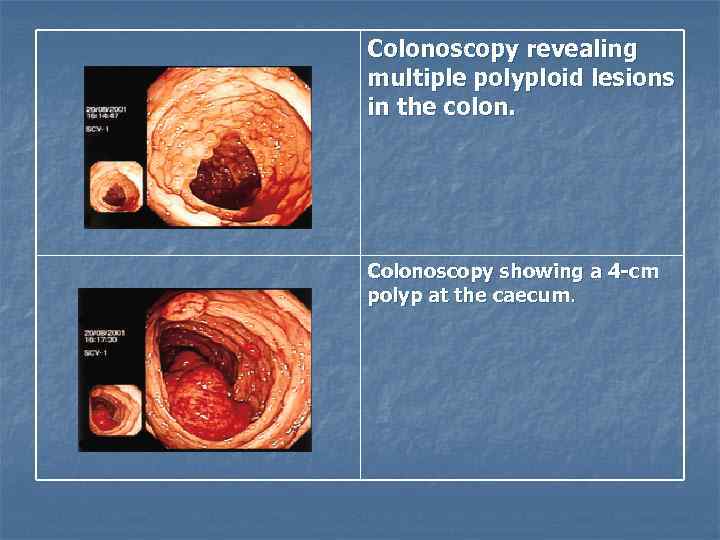
Colonoscopy revealing multiple polyploid lesions in the colon. Colonoscopy showing a 4 -cm polyp at the caecum.
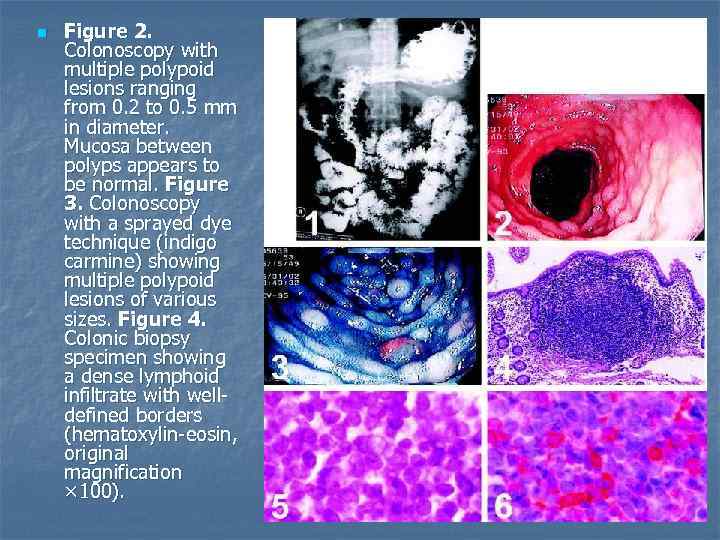
n Figure 2. Colonoscopy with multiple polypoid lesions ranging from 0. 2 to 0. 5 mm in diameter. Mucosa between polyps appears to be normal. Figure 3. Colonoscopy with a sprayed dye technique (indigo carmine) showing multiple polypoid lesions of various sizes. Figure 4. Colonic biopsy specimen showing a dense lymphoid infiltrate with welldefined borders (hematoxylin-eosin, original magnification × 100).
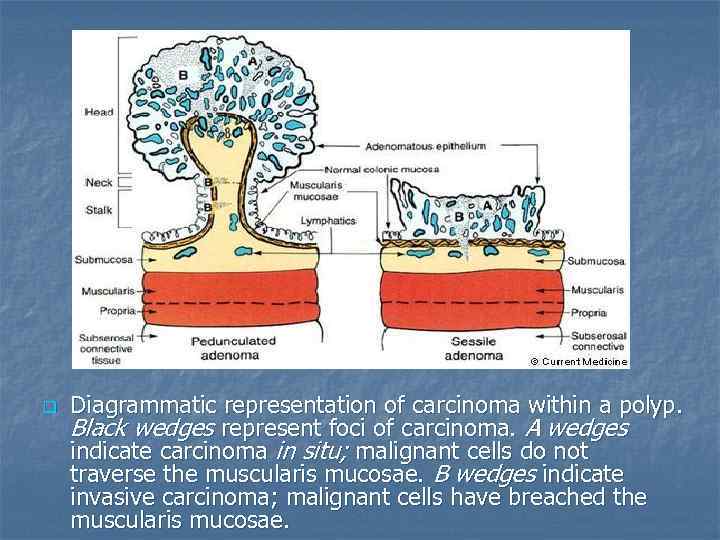
q Diagrammatic representation of carcinoma within a polyp. Black wedges represent foci of carcinoma. A wedges indicate carcinoma in situ; malignant cells do not traverse the muscularis mucosae. B wedges indicate invasive carcinoma; malignant cells have breached the muscularis mucosae.
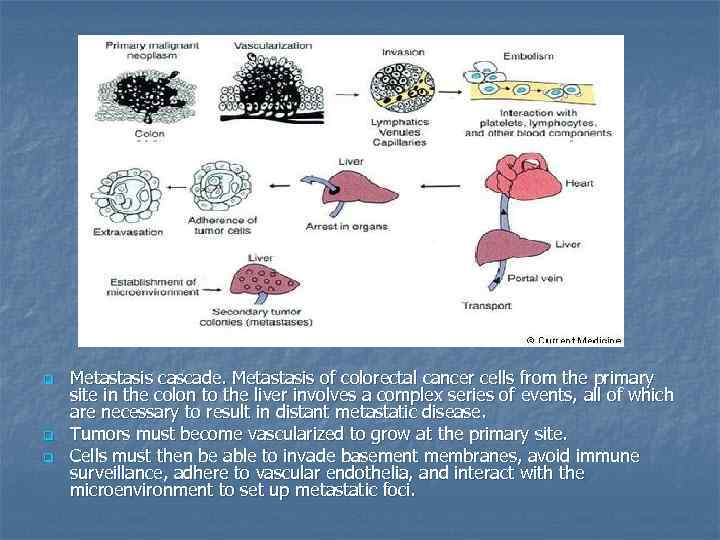
q q q Metastasis cascade. Metastasis of colorectal cancer cells from the primary site in the colon to the liver involves a complex series of events, all of which are necessary to result in distant metastatic disease. Tumors must become vascularized to grow at the primary site. Cells must then be able to invade basement membranes, avoid immune surveillance, adhere to vascular endothelia, and interact with the microenvironment to set up metastatic foci.
Thank you
Colonic polyps - Waleed Fouad.ppt