1820c07748c43b8db3262f5e858a2ab3.ppt
- Количество слайдов: 136
 Colon Disorders and GI Neoplasms Tory Davis PA-C January 2010
Colon Disorders and GI Neoplasms Tory Davis PA-C January 2010
 Colon Disorders Anorectal Disorders Fissure Fistula Hemorrhoid IBS- Irritable Bowel Syndrome Diverticular Disease IBD- Inflammatory Bowel Disease Crohn’s disease Ulcerative Colitis
Colon Disorders Anorectal Disorders Fissure Fistula Hemorrhoid IBS- Irritable Bowel Syndrome Diverticular Disease IBD- Inflammatory Bowel Disease Crohn’s disease Ulcerative Colitis
 GI Neoplasms Esophageal Stomach Colorectal / anorectal Pancreatic Hepatic
GI Neoplasms Esophageal Stomach Colorectal / anorectal Pancreatic Hepatic
 Anal Fissure Acute longitudinal tear or chronic ovoid ulcer in anal epithelium. Located posterior or anterior midline. Pain, severe with defecation Sometimes bleed Often result from laceration with secondary infection. Pain internal sphincter spasm decreased blood supply perpetuating fissure
Anal Fissure Acute longitudinal tear or chronic ovoid ulcer in anal epithelium. Located posterior or anterior midline. Pain, severe with defecation Sometimes bleed Often result from laceration with secondary infection. Pain internal sphincter spasm decreased blood supply perpetuating fissure
 Anal Fissure Tx Reduce local trauma: stool softener, fiber Protect: zinc oxide, glycerin suppository Relieve pain: topical anaesthetic (benzocaine, lidocaine), warm sitz bath Surgical (last choice) - internal sphincterotomy
Anal Fissure Tx Reduce local trauma: stool softener, fiber Protect: zinc oxide, glycerin suppository Relieve pain: topical anaesthetic (benzocaine, lidocaine), warm sitz bath Surgical (last choice) - internal sphincterotomy
 Anorectal Fistula Tube-like tract with one opening in anal tract and other in perianal skin Usually a chronic condition arising from acute perirectal abscess Constant to intermittent drainage of purulent or serosanguinous fluid +/- pain, depends on if infected Exam 1+ openings, +/- palpable cordlike tract. Probe to see depth, direction Tx: Surgical- deroof or seal with fibrin glue
Anorectal Fistula Tube-like tract with one opening in anal tract and other in perianal skin Usually a chronic condition arising from acute perirectal abscess Constant to intermittent drainage of purulent or serosanguinous fluid +/- pain, depends on if infected Exam 1+ openings, +/- palpable cordlike tract. Probe to see depth, direction Tx: Surgical- deroof or seal with fibrin glue
 Hemorrhoids Aka “Piles” Dilated veins of hemorrhoidal plexus in lower rectum Dentate line divides internal from external hemorrhoids Locations: L lateral, R anterior, R posterior zones Often asymptomatic, sometimes itching or protrusion. External: can thrombose. Ow! Internal: often bleed after BM
Hemorrhoids Aka “Piles” Dilated veins of hemorrhoidal plexus in lower rectum Dentate line divides internal from external hemorrhoids Locations: L lateral, R anterior, R posterior zones Often asymptomatic, sometimes itching or protrusion. External: can thrombose. Ow! Internal: often bleed after BM
 Hemorrhoids Internal– graded I- IV I – remain internal II – prolapse with strain, reduce spontaneously III. Require manual reduction after BM IV. Won’t go back
Hemorrhoids Internal– graded I- IV I – remain internal II – prolapse with strain, reduce spontaneously III. Require manual reduction after BM IV. Won’t go back
 Thrombosed Hemorrhoid Results in perianal hematoma Acute onset of exquisite pain Firm blue/purple perianal nodule Tx with sitz baths, analgesics If able in 1 st 24 -48 h, excision gives immediate relief
Thrombosed Hemorrhoid Results in perianal hematoma Acute onset of exquisite pain Firm blue/purple perianal nodule Tx with sitz baths, analgesics If able in 1 st 24 -48 h, excision gives immediate relief
 Tx Non-thrombosed hemorrhoids Symptomatic Sitz baths Witch hazel compress phenylephrine 0. 25% (Preparation H) Anesthetic oint Surgical: photocoag, rubber band ligation, hemorrhoidectomy
Tx Non-thrombosed hemorrhoids Symptomatic Sitz baths Witch hazel compress phenylephrine 0. 25% (Preparation H) Anesthetic oint Surgical: photocoag, rubber band ligation, hemorrhoidectomy
 Irritable Bowel Syndrome
Irritable Bowel Syndrome
 Irritable Bowel Syndrome Poorly understood, but real. Characterized by recurrent upper and lower GI sx, varying abd pain, constipation and/or diarrhea, abd bloating
Irritable Bowel Syndrome Poorly understood, but real. Characterized by recurrent upper and lower GI sx, varying abd pain, constipation and/or diarrhea, abd bloating
 IBS Pathophys No consistent motility abnormality Some pts demonstrate abnl gastrocolic reflex with colonic activity Maybe gastric emptying But even in demonstrated abnormality, sx don’t correlate Excess mucus production even in absence of mucosal injury
IBS Pathophys No consistent motility abnormality Some pts demonstrate abnl gastrocolic reflex with colonic activity Maybe gastric emptying But even in demonstrated abnormality, sx don’t correlate Excess mucus production even in absence of mucosal injury
 More pathophys Hypersensitivity to normal amounts of intraluminal stretch. perception of pain with normal amounts of intestinal gas Can be exacerbated by hormonal fluctuations (incr prostaglandins with menses causes more pain)
More pathophys Hypersensitivity to normal amounts of intraluminal stretch. perception of pain with normal amounts of intestinal gas Can be exacerbated by hormonal fluctuations (incr prostaglandins with menses causes more pain)
 IBS S & S Abdominal pain related to or relieved by defecation Change in stool frequency and/or consistency Mucus in stool Sensation of incomplete evacuation
IBS S & S Abdominal pain related to or relieved by defecation Change in stool frequency and/or consistency Mucus in stool Sensation of incomplete evacuation
 S&S Onset teens or 20 s Irregular, recurrent bouts Sx usually do NOT affect sleep Sx are triggered by stress, also by some foods Varies per patient
S&S Onset teens or 20 s Irregular, recurrent bouts Sx usually do NOT affect sleep Sx are triggered by stress, also by some foods Varies per patient
 Extra-intestinal sx Fibromyalgia Headache Dyspareunia TMJ syndrome Anxiety Depression
Extra-intestinal sx Fibromyalgia Headache Dyspareunia TMJ syndrome Anxiety Depression
 Constipation predominant Constipation alternates with nl BMs Clear-white mucus Colicky or dull constant pain Often relieved by BM Eating may trigger sx Bloating, flatulence, eructation, nausea, dyspepsia, heartburn
Constipation predominant Constipation alternates with nl BMs Clear-white mucus Colicky or dull constant pain Often relieved by BM Eating may trigger sx Bloating, flatulence, eructation, nausea, dyspepsia, heartburn
 Diarrhea predominant Diarrhea immediately after eating, especially after rapid eating Pain, bloating, rectal urgency Incontinence happens
Diarrhea predominant Diarrhea immediately after eating, especially after rapid eating Pain, bloating, rectal urgency Incontinence happens
 Differential Diagnosis Lactose intolerance Diverticular dz Drug induced Drug abuse Biliary tract dz Bacterial enteritis Parasites Early IBD Ischemic colitis, esp if age > 60 Hypothyroid Malabsorption syndromes
Differential Diagnosis Lactose intolerance Diverticular dz Drug induced Drug abuse Biliary tract dz Bacterial enteritis Parasites Early IBD Ischemic colitis, esp if age > 60 Hypothyroid Malabsorption syndromes
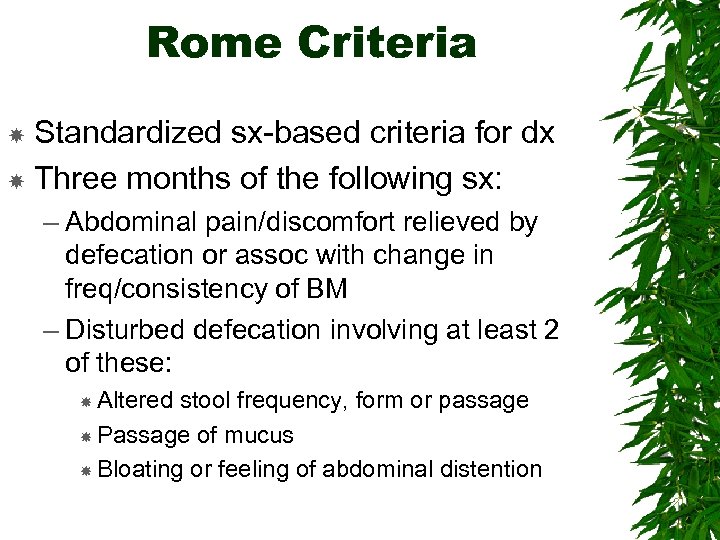 Rome Criteria Standardized sx-based criteria for dx Three months of the following sx: – Abdominal pain/discomfort relieved by defecation or assoc with change in freq/consistency of BM – Disturbed defecation involving at least 2 of these: Altered stool frequency, form or passage Passage of mucus Bloating or feeling of abdominal distention
Rome Criteria Standardized sx-based criteria for dx Three months of the following sx: – Abdominal pain/discomfort relieved by defecation or assoc with change in freq/consistency of BM – Disturbed defecation involving at least 2 of these: Altered stool frequency, form or passage Passage of mucus Bloating or feeling of abdominal distention
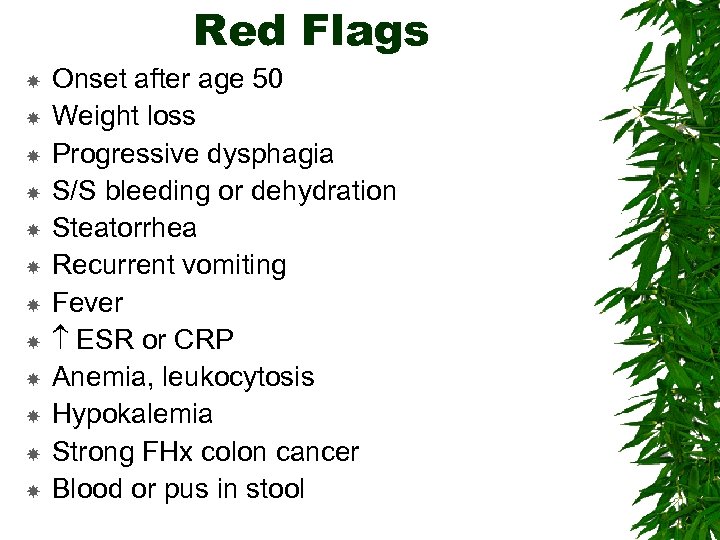 Red Flags Onset after age 50 Weight loss Progressive dysphagia S/S bleeding or dehydration Steatorrhea Recurrent vomiting Fever ESR or CRP Anemia, leukocytosis Hypokalemia Strong FHx colon cancer Blood or pus in stool
Red Flags Onset after age 50 Weight loss Progressive dysphagia S/S bleeding or dehydration Steatorrhea Recurrent vomiting Fever ESR or CRP Anemia, leukocytosis Hypokalemia Strong FHx colon cancer Blood or pus in stool
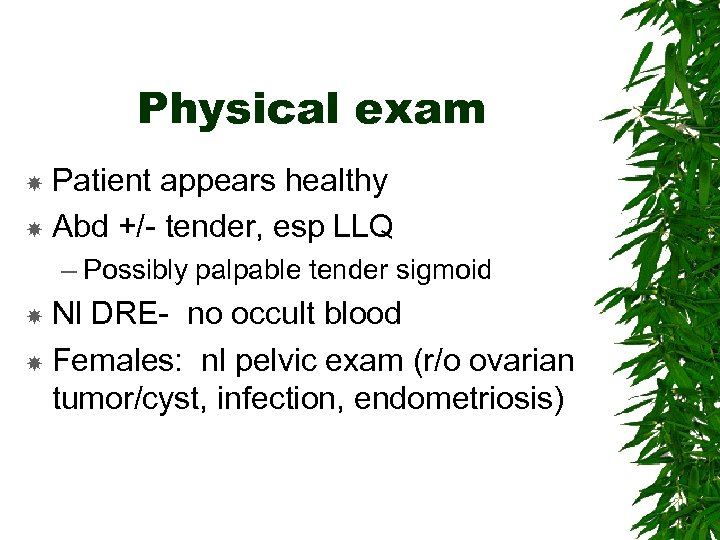 Physical exam Patient appears healthy Abd +/- tender, esp LLQ – Possibly palpable tender sigmoid Nl DRE- no occult blood Females: nl pelvic exam (r/o ovarian tumor/cyst, infection, endometriosis)
Physical exam Patient appears healthy Abd +/- tender, esp LLQ – Possibly palpable tender sigmoid Nl DRE- no occult blood Females: nl pelvic exam (r/o ovarian tumor/cyst, infection, endometriosis)
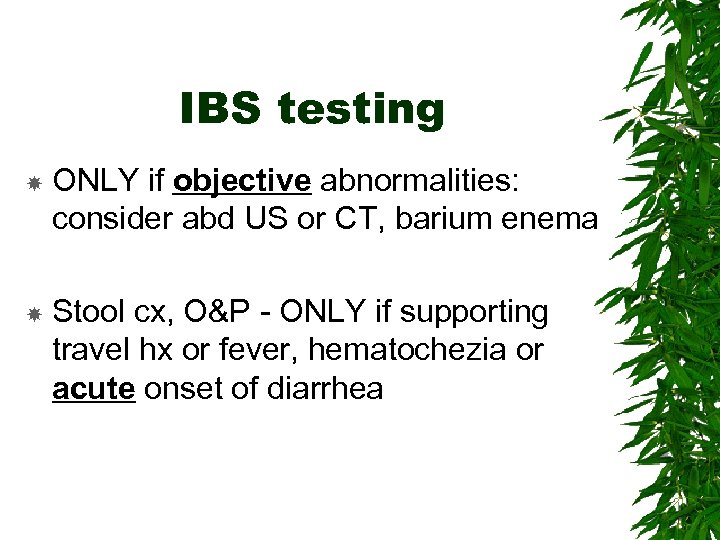 IBS testing ONLY if objective abnormalities: consider abd US or CT, barium enema Stool cx, O&P - ONLY if supporting travel hx or fever, hematochezia or acute onset of diarrhea
IBS testing ONLY if objective abnormalities: consider abd US or CT, barium enema Stool cx, O&P - ONLY if supporting travel hx or fever, hematochezia or acute onset of diarrhea
 IBS tx Sympathetic understanding, patience, explain condition and address fears Diet: – Normal, moderate sized meals eaten slowly. gas-producing food. Consider lactose – Eliminate sorbitol, mannitol in pts with diarrhea – Dietary fiber to bulk up and soften stool, but start low, go slow or you’ll worsen sx ID stressors, mood d/o, or anxiety and address them
IBS tx Sympathetic understanding, patience, explain condition and address fears Diet: – Normal, moderate sized meals eaten slowly. gas-producing food. Consider lactose – Eliminate sorbitol, mannitol in pts with diarrhea – Dietary fiber to bulk up and soften stool, but start low, go slow or you’ll worsen sx ID stressors, mood d/o, or anxiety and address them
 IBS Drugs Anticholinergics to reduce spasm Serotonin receptor modulators
IBS Drugs Anticholinergics to reduce spasm Serotonin receptor modulators
 IBS Drugs Loperamide (Immodium) for diarrhea TCAs for bloating, constipation, abd pain – Down-regulates spinal cord and cortical afferent pathways from intestine Peppermint- relaxes smooth muscle spasm. Significant improvement in clinical studies. Ginger- digestive aid Aloe vera for constipation Fennel – reduces bloating.
IBS Drugs Loperamide (Immodium) for diarrhea TCAs for bloating, constipation, abd pain – Down-regulates spinal cord and cortical afferent pathways from intestine Peppermint- relaxes smooth muscle spasm. Significant improvement in clinical studies. Ginger- digestive aid Aloe vera for constipation Fennel – reduces bloating.
 Inflammatory Bowel Disease Crohn’s Disease Ulcerative Colitis
Inflammatory Bowel Disease Crohn’s Disease Ulcerative Colitis
 IBD 2 distinct disease entities – Only about 10% are “indeterminate colitis” Usually fairly easy to differentiate Both – Cause bloody diarrhea – Are characterized by chronic, relapsing and remitting inflammation of various sites of the GI tract – Have inflammation from cell-mediated immune response in GI mucosa
IBD 2 distinct disease entities – Only about 10% are “indeterminate colitis” Usually fairly easy to differentiate Both – Cause bloody diarrhea – Are characterized by chronic, relapsing and remitting inflammation of various sites of the GI tract – Have inflammation from cell-mediated immune response in GI mucosa
 IBD Epi Gender equal, all ages, but peak incidence ages 14 -24 – UC has 2 nd peak 50 -70 Most common in people of N. European or Anglo-Saxon origin. 1 st degree relatives 4 -20 x increased risk Smoking increases Crohn’s risk, but decreases risk of ulcerative colitis
IBD Epi Gender equal, all ages, but peak incidence ages 14 -24 – UC has 2 nd peak 50 -70 Most common in people of N. European or Anglo-Saxon origin. 1 st degree relatives 4 -20 x increased risk Smoking increases Crohn’s risk, but decreases risk of ulcerative colitis
 IBD Extra-Intestinal Manifestations Common to BOTH Crohn’s and UC 1. Disorders which parallel IBD flares – Peripheral arthritis, episcleritis, aphthous stomatitis, erythema nodosum 2. Disorders probably resulting from IBD but appear independent of flares – Ankylosing spondylitis, sacroiliitis, uveitis, primary sclerosing cholangitis. Can appear years before IBD sx, and should prompt eval for IBD!
IBD Extra-Intestinal Manifestations Common to BOTH Crohn’s and UC 1. Disorders which parallel IBD flares – Peripheral arthritis, episcleritis, aphthous stomatitis, erythema nodosum 2. Disorders probably resulting from IBD but appear independent of flares – Ankylosing spondylitis, sacroiliitis, uveitis, primary sclerosing cholangitis. Can appear years before IBD sx, and should prompt eval for IBD!
 IBD Extra-Intestinal Manifestations 3. Consequences of disrupted bowel physiology (primarily seen in severe Crohn’s of small bowel) – Malabsorption (causing B 12 and mineral deficiencies), anemia, clotting disorders, bone demineralization, kidney stones, hydroureter & hydronephrosis (from ureteral compression by inflammatory process) Factors in all 3 categories can increase risk of thromboembolic disease
IBD Extra-Intestinal Manifestations 3. Consequences of disrupted bowel physiology (primarily seen in severe Crohn’s of small bowel) – Malabsorption (causing B 12 and mineral deficiencies), anemia, clotting disorders, bone demineralization, kidney stones, hydroureter & hydronephrosis (from ureteral compression by inflammatory process) Factors in all 3 categories can increase risk of thromboembolic disease
 Crohn’s Disease
Crohn’s Disease
 Crohn’s Disease Chronic transmural inflammatory dz, usually effects distal ileum and RIGHT colon, but can occur anywhere along GI tract Segmental rather than continuous (UC) Not symmetric Can have significant perirectal lesions, but rare rectal bleeding
Crohn’s Disease Chronic transmural inflammatory dz, usually effects distal ileum and RIGHT colon, but can occur anywhere along GI tract Segmental rather than continuous (UC) Not symmetric Can have significant perirectal lesions, but rare rectal bleeding
 Crohn’s pathophys Inflammation of crypts small abscesses & aphthoid ulcers which deep longitudinal and transverse ulcers with mucosal edema Transmural spread of inflam lymphedema, bowel wall thickening Severe inflam muscle hypertrophy, fibrosis, strictures (can cause obstruction)
Crohn’s pathophys Inflammation of crypts small abscesses & aphthoid ulcers which deep longitudinal and transverse ulcers with mucosal edema Transmural spread of inflam lymphedema, bowel wall thickening Severe inflam muscle hypertrophy, fibrosis, strictures (can cause obstruction)
 Crohn’s pathophys Abscesses common, and resulting fistulas can penetrate nearby structures – Bowel loops, bladder (can pee poop), psoas muscle (peritonitis sx), enterocutaneous Granulomas- Pathognomonic. Found in liver, lymph nodes, all layers of bowel wall
Crohn’s pathophys Abscesses common, and resulting fistulas can penetrate nearby structures – Bowel loops, bladder (can pee poop), psoas muscle (peritonitis sx), enterocutaneous Granulomas- Pathognomonic. Found in liver, lymph nodes, all layers of bowel wall
 Crohn’s pathophys Discontinuous affected segments of bowel sharply demarcated from normal areas (“skip areas”) Where is it? – – 35% ileum alone 45% ileum + colon <20% colon alone, usually spares rectum Uncommon in esoph, stomach, duodenum (but can be there)
Crohn’s pathophys Discontinuous affected segments of bowel sharply demarcated from normal areas (“skip areas”) Where is it? – – 35% ileum alone 45% ileum + colon <20% colon alone, usually spares rectum Uncommon in esoph, stomach, duodenum (but can be there)
 Crohn’s S&S Chronic diarrhea w/ abd pain, fever, anorexia, wt loss Tender abdomen with mass or fullness Gross rectal bleeding RARE One third with significant perianal disease: fissures, fistulas, abscesses
Crohn’s S&S Chronic diarrhea w/ abd pain, fever, anorexia, wt loss Tender abdomen with mass or fullness Gross rectal bleeding RARE One third with significant perianal disease: fissures, fistulas, abscesses
 Crohn’s S&S Can present w/ acute abd- looks like appendicitis or obstruction Recurrent disease sx vary- Pain common with simple recurrence and with abscess Severe flare: pt is SICK: marked tenderness, guarding, rebound – Segmental stenosis can bowel obstruction with colicky pain, abd distention, vomiting – Perforation not uncommon. Enterovesicular perf causes pneumaturia. Draining cutaneous fistulas
Crohn’s S&S Can present w/ acute abd- looks like appendicitis or obstruction Recurrent disease sx vary- Pain common with simple recurrence and with abscess Severe flare: pt is SICK: marked tenderness, guarding, rebound – Segmental stenosis can bowel obstruction with colicky pain, abd distention, vomiting – Perforation not uncommon. Enterovesicular perf causes pneumaturia. Draining cutaneous fistulas
 Crohn’s Dx To diagnose, you must first suspect! Suspect in – pt w/ inflam or obstructive sx – pts w/ perianal fistulas – pts w/ unexplained arthritis, fever, anemia, erythema nodosum, – kiddos with growth retardation
Crohn’s Dx To diagnose, you must first suspect! Suspect in – pt w/ inflam or obstructive sx – pts w/ perianal fistulas – pts w/ unexplained arthritis, fever, anemia, erythema nodosum, – kiddos with growth retardation
 Work-up and Dx Pt presents w/ acute abd: – flat & upright plain films, abd CT to find obstruction, abscess, fistula, and to r/o other cause (ie appendicitis) – Consider pelvis U/S for female with predom lower abd/pelvic sx
Work-up and Dx Pt presents w/ acute abd: – flat & upright plain films, abd CT to find obstruction, abscess, fistula, and to r/o other cause (ie appendicitis) – Consider pelvis U/S for female with predom lower abd/pelvic sx
 Work-up and Dx Less acute pres: – GI series with small bowel follow-thru and spot films of terminal ileum – Considered diagnostic if shows stricture, fistulas or separation of bowel loops
Work-up and Dx Less acute pres: – GI series with small bowel follow-thru and spot films of terminal ileum – Considered diagnostic if shows stricture, fistulas or separation of bowel loops
 Work-up and Dx If symptoms predominantly colonic (ie diarrhea) Order barium enema which may show: – Barium reflux into terminal ileum – Irregularity and nodularity of bowel wall – Wall stiffness and thickening – Narrowed lumen Or colonoscopy with bx, sampling for enteric pathogens and visualization of terminal lumen
Work-up and Dx If symptoms predominantly colonic (ie diarrhea) Order barium enema which may show: – Barium reflux into terminal ileum – Irregularity and nodularity of bowel wall – Wall stiffness and thickening – Narrowed lumen Or colonoscopy with bx, sampling for enteric pathogens and visualization of terminal lumen
 Labs CBC to monitor for anemia, leukocytosis CMP to monitor liver function, check for hypoalbuminemia, electrolyte abnormalities ESR, CRP- nonspecific, but useful serially to monitor disease status
Labs CBC to monitor for anemia, leukocytosis CMP to monitor liver function, check for hypoalbuminemia, electrolyte abnormalities ESR, CRP- nonspecific, but useful serially to monitor disease status
 Crohn’s Prognosis Rare cure Intermittent exac/remit Severe dz can be debilitating, severe pain and dysfunction Dz related mortality low, with most caused by GI cancers (small bowel, colon)
Crohn’s Prognosis Rare cure Intermittent exac/remit Severe dz can be debilitating, severe pain and dysfunction Dz related mortality low, with most caused by GI cancers (small bowel, colon)
 Ulcerative Colitis
Ulcerative Colitis
 Ulcerative Colitis Chronic, inflammatory, ulcerative disease arising in colonic mucosa, most often characterized by bloody diarrhea Only in the colon. Continuous, not segmental Symmetric Not perirectal. No abscesses. No fistulas.
Ulcerative Colitis Chronic, inflammatory, ulcerative disease arising in colonic mucosa, most often characterized by bloody diarrhea Only in the colon. Continuous, not segmental Symmetric Not perirectal. No abscesses. No fistulas.
 UC Pathophysiology Begins in rectum – Can remain localized (ulcerative proctitis), or extend to involve entire colon Inflammation affects mucosa and submucosa only, with sharp border between healthy/diseased tissue
UC Pathophysiology Begins in rectum – Can remain localized (ulcerative proctitis), or extend to involve entire colon Inflammation affects mucosa and submucosa only, with sharp border between healthy/diseased tissue
 More UC patho Fulminant colitis: transmural extension of ulceration (NB this is the only time UC is transmural) ileus & peritonitis Colon loses muscular tone and dilates TOXIC MEGACOLON
More UC patho Fulminant colitis: transmural extension of ulceration (NB this is the only time UC is transmural) ileus & peritonitis Colon loses muscular tone and dilates TOXIC MEGACOLON
 UC- S&S Bloody diarrhea of varied intensity & duration. Asymptomatic periods Insidious onset of attack urge to defecate – Mild low abd cramps – Blood/mucus in stools – Can start s/p infection (ie amebiasis)
UC- S&S Bloody diarrhea of varied intensity & duration. Asymptomatic periods Insidious onset of attack urge to defecate – Mild low abd cramps – Blood/mucus in stools – Can start s/p infection (ie amebiasis)
 UC S&S When ulceration confined to rectosigmoid: – Stool generally normal to hard – Rectal discharges of mucus loaded with RBCs and WBCs accompany or occur between bowel movements. – Systemic sx mild or absent
UC S&S When ulceration confined to rectosigmoid: – Stool generally normal to hard – Rectal discharges of mucus loaded with RBCs and WBCs accompany or occur between bowel movements. – Systemic sx mild or absent
 UC S&S When ulceration extends proximally: – Stools looser, more frequent (>10/day) – Severe cramps, rectal tenesmus – No night respite (diff from IBS or psychogenic diarrhea) – Stools watery, or all blood and pus – Severe: Systemic sx include malaise, fever, anemia, anorexia, and wt loss Can cause hemorrhage requiring transfusion
UC S&S When ulceration extends proximally: – Stools looser, more frequent (>10/day) – Severe cramps, rectal tenesmus – No night respite (diff from IBS or psychogenic diarrhea) – Stools watery, or all blood and pus – Severe: Systemic sx include malaise, fever, anemia, anorexia, and wt loss Can cause hemorrhage requiring transfusion
 UC Diagnosis Typical sx by hx, particular attn to extra -intestinal S&S or hx prev similar attacks Need to distinguish from Crohn’s, other causes of acute colitis (infection, ischemia)
UC Diagnosis Typical sx by hx, particular attn to extra -intestinal S&S or hx prev similar attacks Need to distinguish from Crohn’s, other causes of acute colitis (infection, ischemia)
 UC Testing Labs: same as Crohn’s Stool cx Microscopy of fresh poop for Entamoeba histolitica Recent hosp or abx? Check C. diff toxin stool assay Sigmoidoscopy- permits visualization, but can’t distinguish between Crohn’s and UC
UC Testing Labs: same as Crohn’s Stool cx Microscopy of fresh poop for Entamoeba histolitica Recent hosp or abx? Check C. diff toxin stool assay Sigmoidoscopy- permits visualization, but can’t distinguish between Crohn’s and UC
 W/U fulminant sx Flat and upright abd xray: look for toxic megacolon NO SCOPES (perf risk!) CBC, ESR, lytes, PT/PTT, type and cross Watch closely for progressive peritonitis Serial abdominal films to follow course
W/U fulminant sx Flat and upright abd xray: look for toxic megacolon NO SCOPES (perf risk!) CBC, ESR, lytes, PT/PTT, type and cross Watch closely for progressive peritonitis Serial abdominal films to follow course
 UC Prognosis Usually chronic with remit/relapse – 10% recover completely from initial event – 10% have initial presentation with fulminant colitis; can die Risk of colon cancer – Proportional to duration of sx and amt of colon affected, but NOT to disease activity
UC Prognosis Usually chronic with remit/relapse – 10% recover completely from initial event – 10% have initial presentation with fulminant colitis; can die Risk of colon cancer – Proportional to duration of sx and amt of colon affected, but NOT to disease activity
 Colon Cancer in UC Begins to appear about 7 yr from illness onset in pt w/ extensive disease Cumulative likelihood : – 3% at 15 yrs, 5% at 20 yrs, 9% at 25 yrs Regular colonoscopies after 8 -10 yrs of disease – ANY grade of dysplasia is high risk to progress to cancer, and colectomy is advised
Colon Cancer in UC Begins to appear about 7 yr from illness onset in pt w/ extensive disease Cumulative likelihood : – 3% at 15 yrs, 5% at 20 yrs, 9% at 25 yrs Regular colonoscopies after 8 -10 yrs of disease – ANY grade of dysplasia is high risk to progress to cancer, and colectomy is advised
 IBD Treatment Both Crohn’s and UC
IBD Treatment Both Crohn’s and UC
 5 -aminosalicylic acid (5 -ASA) Blocks production of leukotrienes and prostaglandins Only active intraluminally Sulfasalazine Start low, go slow. Add folate supplement. Check CBC, LFTs serially
5 -aminosalicylic acid (5 -ASA) Blocks production of leukotrienes and prostaglandins Only active intraluminally Sulfasalazine Start low, go slow. Add folate supplement. Check CBC, LFTs serially
 Corticosteroids For acute flares- not ideal for maint Until sx remit (7 -28 days) then taper
Corticosteroids For acute flares- not ideal for maint Until sx remit (7 -28 days) then taper
 Immunomodulating agents- Azathioprine Inhibit T cell function Good & effective long term- may steroid needs. Takes 1 -3 months to reach efficacy Monitor for bone marrow suppression 3 -5% develop high fever or pancreatitis – do NOT retry Rare hepatotoxicity, check LFTs q 6 mo
Immunomodulating agents- Azathioprine Inhibit T cell function Good & effective long term- may steroid needs. Takes 1 -3 months to reach efficacy Monitor for bone marrow suppression 3 -5% develop high fever or pancreatitis – do NOT retry Rare hepatotoxicity, check LFTs q 6 mo
 Immunomodulating agents Methotrexate – – For severe dz not responsive to steroids, failed azathioprine. Cyclosporine- blocks lymphocyte activation – For severe UC unresponsive to steroids, pts who may o/w need colectomy – In Crohn’s, used for refractory fistulas or pyoderma – Reserve use, and don’t use >6 mo. Renal toxicity, seizures, opportunistic infection
Immunomodulating agents Methotrexate – – For severe dz not responsive to steroids, failed azathioprine. Cyclosporine- blocks lymphocyte activation – For severe UC unresponsive to steroids, pts who may o/w need colectomy – In Crohn’s, used for refractory fistulas or pyoderma – Reserve use, and don’t use >6 mo. Renal toxicity, seizures, opportunistic infection
 Anticytokine drugs Infliximab, CDP 571, CDP 870, adalimumab Antibodies against TNF
Anticytokine drugs Infliximab, CDP 571, CDP 870, adalimumab Antibodies against TNF
 ALSO Antibiotics – Useful in Crohn’s, not UC – Help heal fistulas – Metronidazole or Cipro Probiotics Supportive Care
ALSO Antibiotics – Useful in Crohn’s, not UC – Help heal fistulas – Metronidazole or Cipro Probiotics Supportive Care
 Crohn’s Tx General: cramps/diarrhea loperamide (except in acute/severe) Mild: 5 -ASA, abx Moderate: steroids, transition to maint – Obstruction: add NG suction, IV fluids, parenteral nutrition – Usually resolves in few days
Crohn’s Tx General: cramps/diarrhea loperamide (except in acute/severe) Mild: 5 -ASA, abx Moderate: steroids, transition to maint – Obstruction: add NG suction, IV fluids, parenteral nutrition – Usually resolves in few days
 Crohn’s Tx Fulminant/abscess: toxic appearance, fever, persistent vomiting, rebound – IV fluids, abx, surgical or percutaneous drainage – No steroids till infection controlled Fistulas: abx, if no response in 3 -4 weeks, add immunomodulator
Crohn’s Tx Fulminant/abscess: toxic appearance, fever, persistent vomiting, rebound – IV fluids, abx, surgical or percutaneous drainage – No steroids till infection controlled Fistulas: abx, if no response in 3 -4 weeks, add immunomodulator
 Crohn’s Surgery 70% ultimately will have surgery- but reserve for recurrent obstruction, intractable fistula/abscess Resection ameliorates, does NOT cure – Further surgery required in 50% of cases – Recurrence is likely, even if all disease is removed
Crohn’s Surgery 70% ultimately will have surgery- but reserve for recurrent obstruction, intractable fistula/abscess Resection ameliorates, does NOT cure – Further surgery required in 50% of cases – Recurrence is likely, even if all disease is removed
 UC Tx General – Limit raw fruits and veggies – Try milk-free – Loperamide prn Mild Left Sided disease – 5 ASA enema/suppository (kind of topical tx) – Steroid enema – Maybe oral 5 -ASA
UC Tx General – Limit raw fruits and veggies – Try milk-free – Loperamide prn Mild Left Sided disease – 5 ASA enema/suppository (kind of topical tx) – Steroid enema – Maybe oral 5 -ASA
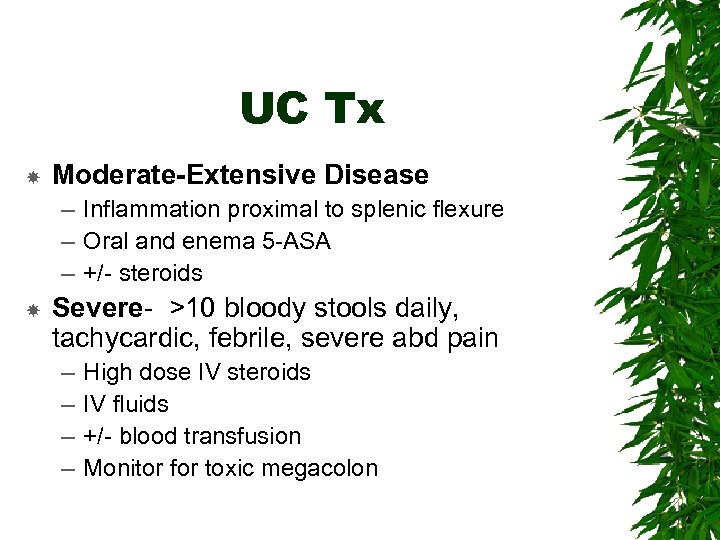 UC Tx Moderate-Extensive Disease – Inflammation proximal to splenic flexure – Oral and enema 5 -ASA – +/- steroids Severe- >10 bloody stools daily, tachycardic, febrile, severe abd pain – – High dose IV steroids IV fluids +/- blood transfusion Monitor for toxic megacolon
UC Tx Moderate-Extensive Disease – Inflammation proximal to splenic flexure – Oral and enema 5 -ASA – +/- steroids Severe- >10 bloody stools daily, tachycardic, febrile, severe abd pain – – High dose IV steroids IV fluids +/- blood transfusion Monitor for toxic megacolon
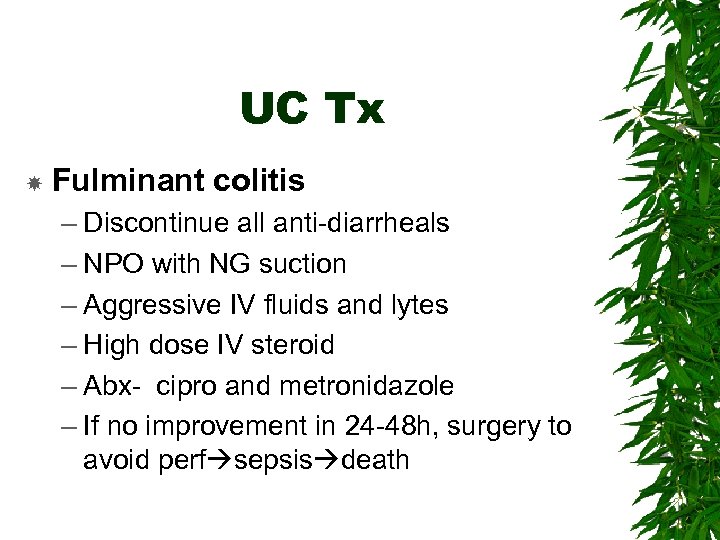 UC Tx Fulminant colitis – Discontinue all anti-diarrheals – NPO with NG suction – Aggressive IV fluids and lytes – High dose IV steroid – Abx- cipro and metronidazole – If no improvement in 24 -48 h, surgery to avoid perf sepsis death
UC Tx Fulminant colitis – Discontinue all anti-diarrheals – NPO with NG suction – Aggressive IV fluids and lytes – High dose IV steroid – Abx- cipro and metronidazole – If no improvement in 24 -48 h, surgery to avoid perf sepsis death
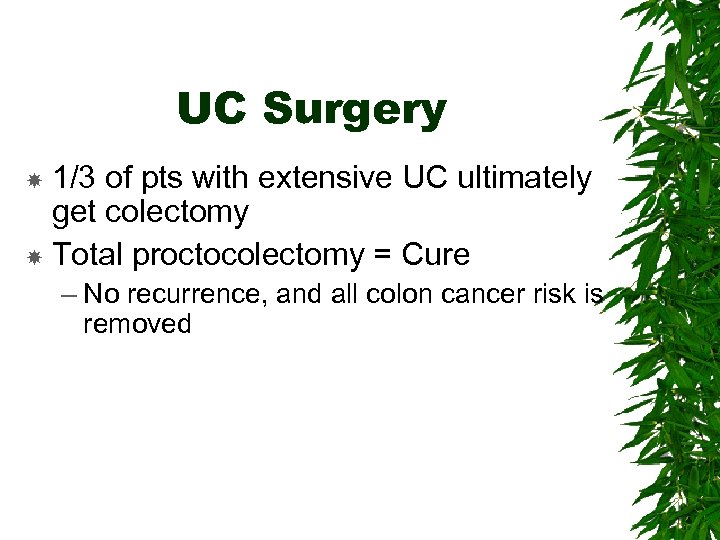 UC Surgery 1/3 of pts with extensive UC ultimately get colectomy Total proctocolectomy = Cure – No recurrence, and all colon cancer risk is removed
UC Surgery 1/3 of pts with extensive UC ultimately get colectomy Total proctocolectomy = Cure – No recurrence, and all colon cancer risk is removed
 Diverticular Disease
Diverticular Disease
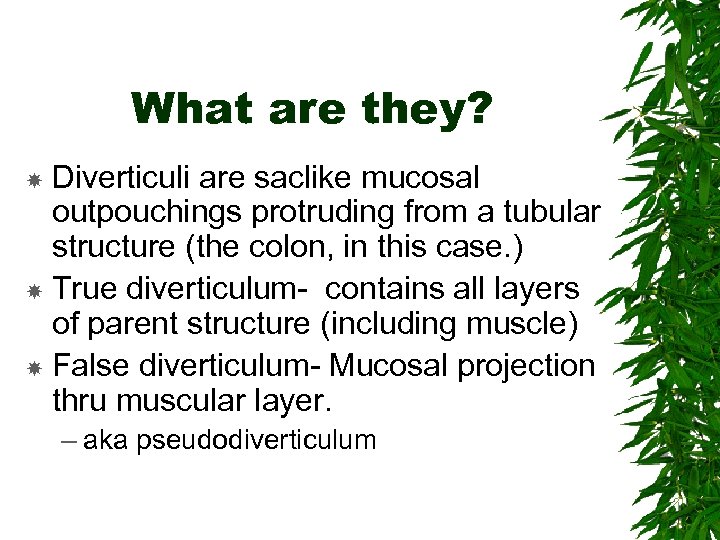 What are they? Diverticuli are saclike mucosal outpouchings protruding from a tubular structure (the colon, in this case. ) True diverticulum- contains all layers of parent structure (including muscle) False diverticulum- Mucosal projection thru muscular layer. – aka pseudodiverticulum
What are they? Diverticuli are saclike mucosal outpouchings protruding from a tubular structure (the colon, in this case. ) True diverticulum- contains all layers of parent structure (including muscle) False diverticulum- Mucosal projection thru muscular layer. – aka pseudodiverticulum
 Diverticulosis Presence of multiple pseudodiverticuli in the colon. Likely result of lifelong low fiber diet Usually asymptomatic, but sometimes inflame or bleed Usually in sigmoid, but can be anywhere in large colon Uncommon under age 40. every 90 yo has them.
Diverticulosis Presence of multiple pseudodiverticuli in the colon. Likely result of lifelong low fiber diet Usually asymptomatic, but sometimes inflame or bleed Usually in sigmoid, but can be anywhere in large colon Uncommon under age 40. every 90 yo has them.
 Why? Increased intraluminal pressure causes mucosal extrusion thru weak points in muscular layer of bowel. Usually next to intramural vasculature – Why? – area of weakness, there is already a hole there
Why? Increased intraluminal pressure causes mucosal extrusion thru weak points in muscular layer of bowel. Usually next to intramural vasculature – Why? – area of weakness, there is already a hole there
 S & S Diverticulosis 70% asymptomatic. Usually incidental finding 15 -25% become inflamed and painful (diverticulitis) 10 -15% painless bleeding. Likely caused by erosion of adjacent vasculature by local trauma (hard stool)
S & S Diverticulosis 70% asymptomatic. Usually incidental finding 15 -25% become inflamed and painful (diverticulitis) 10 -15% painless bleeding. Likely caused by erosion of adjacent vasculature by local trauma (hard stool)
 Diverticulosis Tx Reduce segmental spasm. High fiber diet, supplement with psyllium seed or bran Tx of diverticular bleed: – 75% stop spontaneously but many will bleed enough to require transfusion. Tx of bleeding is surgical. Colonoscopic epi, heat or laser.
Diverticulosis Tx Reduce segmental spasm. High fiber diet, supplement with psyllium seed or bran Tx of diverticular bleed: – 75% stop spontaneously but many will bleed enough to require transfusion. Tx of bleeding is surgical. Colonoscopic epi, heat or laser.
 Diverticulitis Inflammation of a diverticulum Usually in sigmoid Micro or macro perforation releases intestinal bacteria Localized inflammation in 75% Remaining 25% can lead to abscess, free intraperitoneal perforation, bowel obstruction, fistulas to bladder, small bowel, etc
Diverticulitis Inflammation of a diverticulum Usually in sigmoid Micro or macro perforation releases intestinal bacteria Localized inflammation in 75% Remaining 25% can lead to abscess, free intraperitoneal perforation, bowel obstruction, fistulas to bladder, small bowel, etc
 Diverticulitis S & S Abdominal pain LLQ tenderness Fever +/- peritoneal signs If obstructed, n/v, abdominal distention Bleeding is rare Fistula can present as pneumaturia, feculent vaginal discharge, cutaneous or myofascial infection
Diverticulitis S & S Abdominal pain LLQ tenderness Fever +/- peritoneal signs If obstructed, n/v, abdominal distention Bleeding is rare Fistula can present as pneumaturia, feculent vaginal discharge, cutaneous or myofascial infection
 Dx High suspicion in known diverticulosis ABD CT with oral and IV contrast – Need to r/o other causes, like appendicitis, colon CA, ovarian CA – Labs: CBC shows leukocytosis
Dx High suspicion in known diverticulosis ABD CT with oral and IV contrast – Need to r/o other causes, like appendicitis, colon CA, ovarian CA – Labs: CBC shows leukocytosis
 Diverticulitis TX Mild- Rest, liquid diet, oral abx, go home. – cipro 500 mg BID or – amox/clavulanate 500 mg TID PLUS metronidazole 500 mg QID Sx subside quickly. Proceed to low fiber diet for 1 month Barium enema in 2 -4 weeks to eval colon Then back to high fiber diet
Diverticulitis TX Mild- Rest, liquid diet, oral abx, go home. – cipro 500 mg BID or – amox/clavulanate 500 mg TID PLUS metronidazole 500 mg QID Sx subside quickly. Proceed to low fiber diet for 1 month Barium enema in 2 -4 weeks to eval colon Then back to high fiber diet
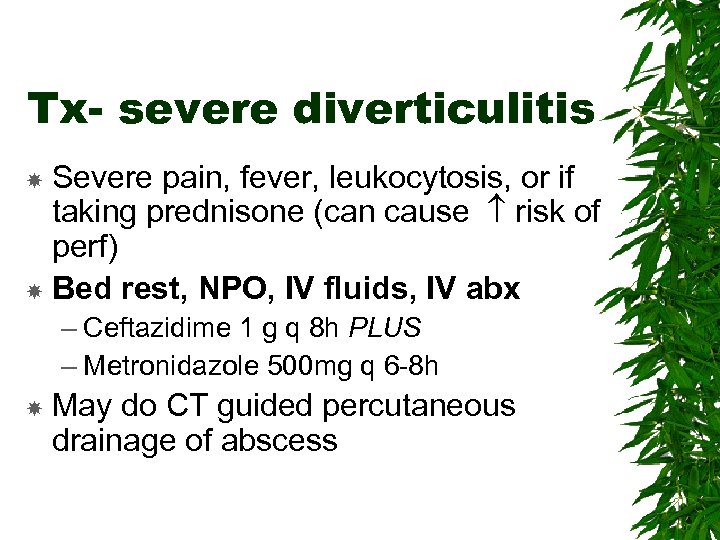 Tx- severe diverticulitis Severe pain, fever, leukocytosis, or if taking prednisone (can cause risk of perf) Bed rest, NPO, IV fluids, IV abx – Ceftazidime 1 g q 8 h PLUS – Metronidazole 500 mg q 6 -8 h May do CT guided percutaneous drainage of abscess
Tx- severe diverticulitis Severe pain, fever, leukocytosis, or if taking prednisone (can cause risk of perf) Bed rest, NPO, IV fluids, IV abx – Ceftazidime 1 g q 8 h PLUS – Metronidazole 500 mg q 6 -8 h May do CT guided percutaneous drainage of abscess
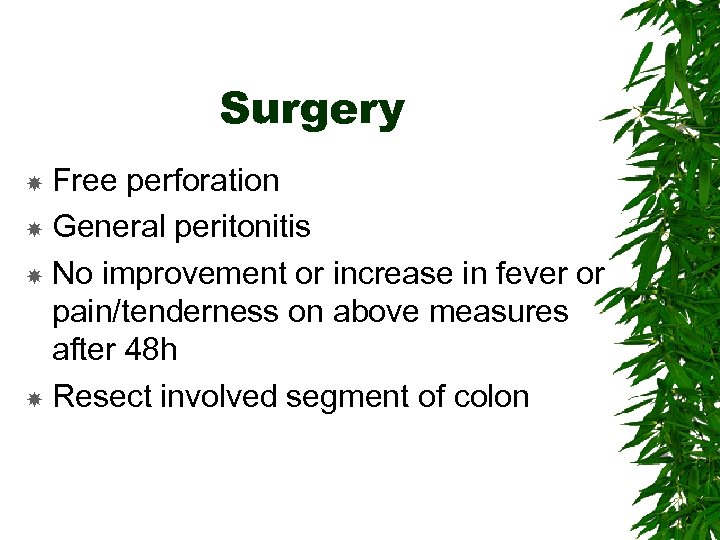 Surgery Free perforation General peritonitis No improvement or increase in fever or pain/tenderness on above measures after 48 h Resect involved segment of colon
Surgery Free perforation General peritonitis No improvement or increase in fever or pain/tenderness on above measures after 48 h Resect involved segment of colon
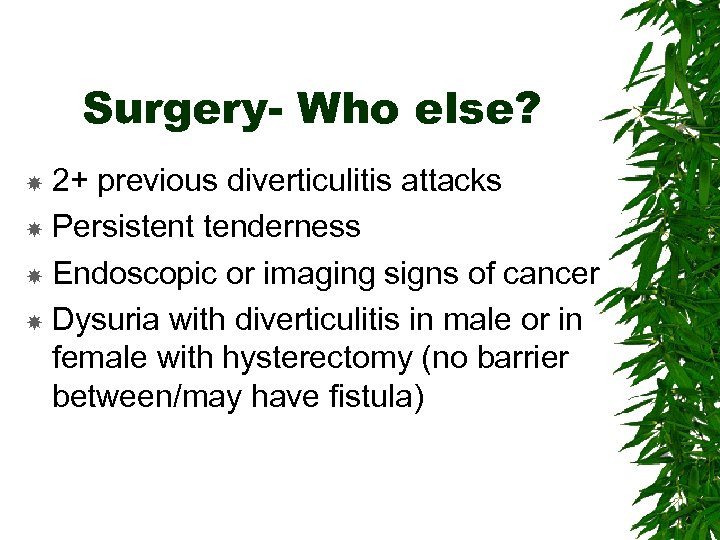 Surgery- Who else? 2+ previous diverticulitis attacks Persistent tenderness Endoscopic or imaging signs of cancer Dysuria with diverticulitis in male or in female with hysterectomy (no barrier between/may have fistula)
Surgery- Who else? 2+ previous diverticulitis attacks Persistent tenderness Endoscopic or imaging signs of cancer Dysuria with diverticulitis in male or in female with hysterectomy (no barrier between/may have fistula)
 GI Neoplasms
GI Neoplasms
 Cancer in the GI Tract Cancer: unregulated cell growth (neoplasm) plus the ability to invade distant tissues (malignancy) Cancer arises usually from rapidly dividing or damaged tissue Entire GI tract susceptible:
Cancer in the GI Tract Cancer: unregulated cell growth (neoplasm) plus the ability to invade distant tissues (malignancy) Cancer arises usually from rapidly dividing or damaged tissue Entire GI tract susceptible:
 Esophageal Cancer 13, 500 cases and 12, 500 deaths overall annually Squamous cell- Most common type Adenocarcinoma- 2 nd most common Other esophageal tumors: spindle cell, verrucous, pseudosarcoma, malignant melanoma – 3% are metastases
Esophageal Cancer 13, 500 cases and 12, 500 deaths overall annually Squamous cell- Most common type Adenocarcinoma- 2 nd most common Other esophageal tumors: spindle cell, verrucous, pseudosarcoma, malignant melanoma – 3% are metastases
 Squamous cell 8 k cases annually In US – 4 -5 x more common in blacks – 2 -3 x more common in males Risk factors: alcohol ingestion, tobacco use (any form), achalasia, HPV infection, ingestion of caustic or hot liquids, irradiation, esophageal webs
Squamous cell 8 k cases annually In US – 4 -5 x more common in blacks – 2 -3 x more common in males Risk factors: alcohol ingestion, tobacco use (any form), achalasia, HPV infection, ingestion of caustic or hot liquids, irradiation, esophageal webs
 Esophageal Adenocarcinoma Usually in distal esoph 4 x more common in whites – >50% of esoph CA in whites Smoking! – But not alcohol Most cases develop from Barrett’s esophagus
Esophageal Adenocarcinoma Usually in distal esoph 4 x more common in whites – >50% of esoph CA in whites Smoking! – But not alcohol Most cases develop from Barrett’s esophagus
 Esoph CA S&S Earliest stages- no sx Dysphagia when lumen <14 mm – Progressive from solids, semisolids, liquids, saliva. – Wt loss- universal, even with good appetite
Esoph CA S&S Earliest stages- no sx Dysphagia when lumen <14 mm – Progressive from solids, semisolids, liquids, saliva. – Wt loss- universal, even with good appetite
 Esoph CA S&S Compression of nerves by mass effect – Recurrent laryngeal hoarseness – Sympathetic Horner’s sign (ptosis, miosis, anhidrosis, enophthalmosis, anisocoria) - usually unilateral – Elsewhere spinal pain, hiccups, paralysis of diaphragm Dyspnea from malignant pleural effusion or pulmonary metastases
Esoph CA S&S Compression of nerves by mass effect – Recurrent laryngeal hoarseness – Sympathetic Horner’s sign (ptosis, miosis, anhidrosis, enophthalmosis, anisocoria) - usually unilateral – Elsewhere spinal pain, hiccups, paralysis of diaphragm Dyspnea from malignant pleural effusion or pulmonary metastases
 Esoph CA Dx If suspicious, endoscopy with bx If confirmed – CT chest/abd to assess spread – Endoscopic U/S to assess depth of tumor and regional node involvement – CBC, lytes, LFTs
Esoph CA Dx If suspicious, endoscopy with bx If confirmed – CT chest/abd to assess spread – Endoscopic U/S to assess depth of tumor and regional node involvement – CBC, lytes, LFTs
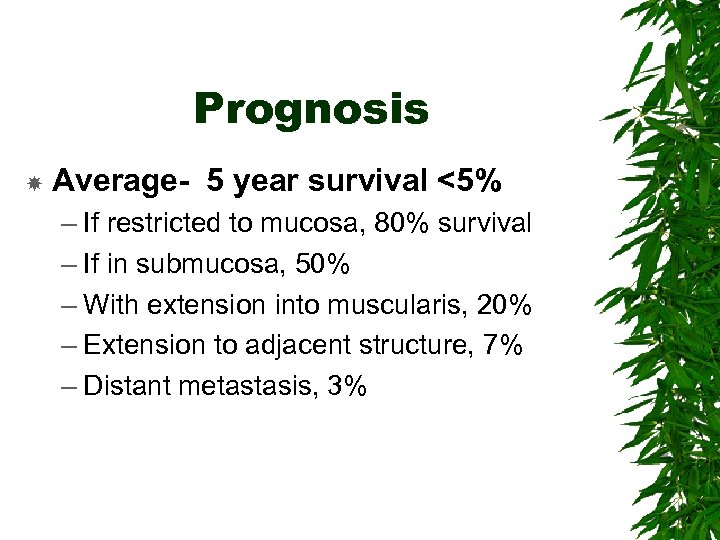 Prognosis Average- 5 year survival <5% – If restricted to mucosa, 80% survival – If in submucosa, 50% – With extension into muscularis, 20% – Extension to adjacent structure, 7% – Distant metastasis, 3%
Prognosis Average- 5 year survival <5% – If restricted to mucosa, 80% survival – If in submucosa, 50% – With extension into muscularis, 20% – Extension to adjacent structure, 7% – Distant metastasis, 3%
 Treatment Stage 0, I, some II- surgical resection only, no benefit to chemo or radiation Stage II, III- Preoperative radiation/chemo to size, then surgery – Surg: en bloc resection of whole tumor with clean margins, all potentially malignant lymph nodes, part of prox stomach to get draining lymphatics, then gastric pull-up with esophogastric anastomsis. – If no surg, both chemo & rad Stage IV- palliation, no surgery
Treatment Stage 0, I, some II- surgical resection only, no benefit to chemo or radiation Stage II, III- Preoperative radiation/chemo to size, then surgery – Surg: en bloc resection of whole tumor with clean margins, all potentially malignant lymph nodes, part of prox stomach to get draining lymphatics, then gastric pull-up with esophogastric anastomsis. – If no surg, both chemo & rad Stage IV- palliation, no surgery
 Palliation & Support Relieve obstruction to allow oral intake – Stent, dilation, radiation, laser coag Nutritional support. Enteral or parenteral supplementation. Consider early surgical/endoscopic placement of feeding tubes to allow feeding when esoph blocked End-of-life decisions made early
Palliation & Support Relieve obstruction to allow oral intake – Stent, dilation, radiation, laser coag Nutritional support. Enteral or parenteral supplementation. Consider early surgical/endoscopic placement of feeding tubes to allow feeding when esoph blocked End-of-life decisions made early
 Gastric Cancer 21 k cases, 12 k deaths 95% gastric adenocarcinoma 2 nd MC cancer worldwide Multifactorial etiology; H. Pylori causative in most cases
Gastric Cancer 21 k cases, 12 k deaths 95% gastric adenocarcinoma 2 nd MC cancer worldwide Multifactorial etiology; H. Pylori causative in most cases
 Types of Gastric Adenocarcinoma Classified by gross appearance 1. Protruding- polypoid. Better prog b/c detected sooner 2. Penetrating- ulcerated tumor 3. Superficial spreading- spreads along mucosa or infiltrates superficially within stomach wall
Types of Gastric Adenocarcinoma Classified by gross appearance 1. Protruding- polypoid. Better prog b/c detected sooner 2. Penetrating- ulcerated tumor 3. Superficial spreading- spreads along mucosa or infiltrates superficially within stomach wall
 Gastric CA S&S Initially nonspecific dyspepsia Later: – Early satiety (gets full really easy) If tumor obstructs peptic outlet or if stomach nondistensible – Dyspepsia If tumor obstructs esoph outlet – Weight loss – Hematemesis, melena with secondary anemia – Sometimes primary sx are from mets (jaundice, bone fracture, ascites)
Gastric CA S&S Initially nonspecific dyspepsia Later: – Early satiety (gets full really easy) If tumor obstructs peptic outlet or if stomach nondistensible – Dyspepsia If tumor obstructs esoph outlet – Weight loss – Hematemesis, melena with secondary anemia – Sometimes primary sx are from mets (jaundice, bone fracture, ascites)
 Physical Exam May be normal, or you may find – Heme positive stool – Epigastric mass – Adenopathy – umbilical, L supraclavicular, L axillary – Hepatomegaly
Physical Exam May be normal, or you may find – Heme positive stool – Epigastric mass – Adenopathy – umbilical, L supraclavicular, L axillary – Hepatomegaly
 Gastric CA Dx Endoscopy with multiple bx and brush cytology CT chest/abd for spread- if CT neg, endoscopic U/S CBC, lytes, LFTs- to assess hydration, anemia, liver mets
Gastric CA Dx Endoscopy with multiple bx and brush cytology CT chest/abd for spread- if CT neg, endoscopic U/S CBC, lytes, LFTs- to assess hydration, anemia, liver mets
 Prognosis Overall 5 year survival 5 -15% In mucosa only 80% In local nodes 20 -40% More widespread, fatal within 1 year
Prognosis Overall 5 year survival 5 -15% In mucosa only 80% In local nodes 20 -40% More widespread, fatal within 1 year
 Treatment Depends on spread and pt preference Surgery- If ca limited to stomach and local nodes only, gastrectomy with local node removal results in 10 month survival (vs 3 -4 without) Extensive node involvement or mets palliation
Treatment Depends on spread and pt preference Surgery- If ca limited to stomach and local nodes only, gastrectomy with local node removal results in 10 month survival (vs 3 -4 without) Extensive node involvement or mets palliation
 Colorectal Neoplasms
Colorectal Neoplasms
 Polyps Mass of tissue arising from bowel wall, protruding into lumen Pedunculated or sessile Occur in rectum, sigmoid, with decreasing frequency toward cecum Usually no symptoms Concern: malignant transformation in previously benign adenomatous polyp
Polyps Mass of tissue arising from bowel wall, protruding into lumen Pedunculated or sessile Occur in rectum, sigmoid, with decreasing frequency toward cecum Usually no symptoms Concern: malignant transformation in previously benign adenomatous polyp
 Polyp S&S and Dx Usually no sx If any, rectal bleeding Most found incidentally on colonoscopy Tx: snare or electrosurgical bx during colonoscopy – If incomplete removal, laparotomy – If deep invasion into muscularis, eval for colon cancer – Monitor with serial scopes
Polyp S&S and Dx Usually no sx If any, rectal bleeding Most found incidentally on colonoscopy Tx: snare or electrosurgical bx during colonoscopy – If incomplete removal, laparotomy – If deep invasion into muscularis, eval for colon cancer – Monitor with serial scopes
 Colorectal Cancer 130 k cases, 57 k deaths Incidence rises after 40, peaks 60 -75 70% in rectum/sigmoid 95% adenocarcinoma, usually transformation within adenomatous polyp. 80% sporadic, 20% heritable
Colorectal Cancer 130 k cases, 57 k deaths Incidence rises after 40, peaks 60 -75 70% in rectum/sigmoid 95% adenocarcinoma, usually transformation within adenomatous polyp. 80% sporadic, 20% heritable
 Colorectal Ca risk factors Ulcerative colitis Diet – Low fiber -fiber speeds colonic transit, reduces exposure to carcinogens – High in animal protein – High fat Theory: Fats increase anaerobes in colon which convert bile to – High in refined carbs Smoking Genetic factors
Colorectal Ca risk factors Ulcerative colitis Diet – Low fiber -fiber speeds colonic transit, reduces exposure to carcinogens – High in animal protein – High fat Theory: Fats increase anaerobes in colon which convert bile to – High in refined carbs Smoking Genetic factors
 Genetic risk factors: hereditary polyp syndromes (Look-ups) – Polyposis coli (Familial Adenosis Polyposis - FAP) – Hereditary Non-Polyposis Colon CA (HNPCC) – Peutz-Jeghers Syndrome – Familial Juvenile Polyposis Coli – Found during family medical history – Generally warrant more frequent screening
Genetic risk factors: hereditary polyp syndromes (Look-ups) – Polyposis coli (Familial Adenosis Polyposis - FAP) – Hereditary Non-Polyposis Colon CA (HNPCC) – Peutz-Jeghers Syndrome – Familial Juvenile Polyposis Coli – Found during family medical history – Generally warrant more frequent screening
 S&S-depend on location R colon- bleeding (occult or melena) anemia fatigue/weakness – Large lumen, liquid contents, so rare obstruction L colon- Constipation alt with diarrhea or stool freq. Partial or complete obstruction with abd pain can be initial presentation – Smaller lumen, semisolid contents. CA can encircle bowel. Sigmoid or rectal- tenesmus, ribbon stools
S&S-depend on location R colon- bleeding (occult or melena) anemia fatigue/weakness – Large lumen, liquid contents, so rare obstruction L colon- Constipation alt with diarrhea or stool freq. Partial or complete obstruction with abd pain can be initial presentation – Smaller lumen, semisolid contents. CA can encircle bowel. Sigmoid or rectal- tenesmus, ribbon stools
 Screening For Colorectal Cancer Very large part of primary care practices Screening method and frequency based on risk assessment, average or high – Average Risk: No 1 st order relatives with colon CA No prior Hx colon CA or polyps No Hx IBD – High Risk: Yes to any of the above
Screening For Colorectal Cancer Very large part of primary care practices Screening method and frequency based on risk assessment, average or high – Average Risk: No 1 st order relatives with colon CA No prior Hx colon CA or polyps No Hx IBD – High Risk: Yes to any of the above
 Colon CA Screening Modalities: – Fecal Occult Blood Testing (FOBT) – Sigmoidoscopy – Colonoscopy
Colon CA Screening Modalities: – Fecal Occult Blood Testing (FOBT) – Sigmoidoscopy – Colonoscopy
 FOBT alone reduces mortality from colon CA by 33% – Sensitivity single FOBT is 30% – Annual FOBT screen 92% sensitive – 2% of positive FOBT have CA Problems with FOBT: – Misses non-bleeding polyps – Reduces mortality only 30% – Many false positives
FOBT alone reduces mortality from colon CA by 33% – Sensitivity single FOBT is 30% – Annual FOBT screen 92% sensitive – 2% of positive FOBT have CA Problems with FOBT: – Misses non-bleeding polyps – Reduces mortality only 30% – Many false positives
 Sigmoidoscopy reaches 60 cm to splenic flexure – Misses about ½ of colon – Reduces mortality by 60% – Screen every 5 years – If polyps or lesions found must do colonoscopy
Sigmoidoscopy reaches 60 cm to splenic flexure – Misses about ½ of colon – Reduces mortality by 60% – Screen every 5 years – If polyps or lesions found must do colonoscopy
 Colonoscopy most sensitive screen – Finds most polyps – Can remove by bx simultaneously – Requires conscious sedation – Risk of perforation, other hazards – Not usually an office procedure – Prep
Colonoscopy most sensitive screen – Finds most polyps – Can remove by bx simultaneously – Requires conscious sedation – Risk of perforation, other hazards – Not usually an office procedure – Prep
 DCBE Double Contrast Barium Enema – Screens entire colon – No sedation required – Some cramping – Prep required – Must do colonoscopy if lesions found
DCBE Double Contrast Barium Enema – Screens entire colon – No sedation required – Some cramping – Prep required – Must do colonoscopy if lesions found
 Virtual colonoscopy using computerenhanced spiral CT scan – Initial studies in screening populations showed high sensitivity similar to colonoscopy – If lesions found, need colonoscopy anyway – Still must do prep – No bx possible
Virtual colonoscopy using computerenhanced spiral CT scan – Initial studies in screening populations showed high sensitivity similar to colonoscopy – If lesions found, need colonoscopy anyway – Still must do prep – No bx possible
 Capsule Colonoscopy Pill or Capsule Colonoscopy easier on patient – Prep, then swallow pill – Recording sensors attached to abdomen – Results downloaded and reviewed after 6 -8 hours – No manipulation of camera possible – Colonoscopy for biopsy of lesions – Limited data to date, not recommended, yet
Capsule Colonoscopy Pill or Capsule Colonoscopy easier on patient – Prep, then swallow pill – Recording sensors attached to abdomen – Results downloaded and reviewed after 6 -8 hours – No manipulation of camera possible – Colonoscopy for biopsy of lesions – Limited data to date, not recommended, yet
 Average risk Average Risk: screen all pts >50 y. o. Choices: – Offer FOBT or FIT yearly. If positive, then colonoscopy – Offer sigmoidoscopy every 5 years. If positive, then colonoscopy – Offer colonoscopy every 10 years – Offer DCBE every 5 years
Average risk Average Risk: screen all pts >50 y. o. Choices: – Offer FOBT or FIT yearly. If positive, then colonoscopy – Offer sigmoidoscopy every 5 years. If positive, then colonoscopy – Offer colonoscopy every 10 years – Offer DCBE every 5 years
 High-Risk Patient Screening For High Risk pts begin to screen age 40 1 st order relative screen every 3 -5 years Genetic syndromes- more frequent screening. Likely will be followed by specialist
High-Risk Patient Screening For High Risk pts begin to screen age 40 1 st order relative screen every 3 -5 years Genetic syndromes- more frequent screening. Likely will be followed by specialist
 Screening For Colorectal Cancer Overall screening efforts very poor – And liability very high… 65% of all cases found when symptomatic, not at screening
Screening For Colorectal Cancer Overall screening efforts very poor – And liability very high… 65% of all cases found when symptomatic, not at screening
 Prognosis 10 year survival – CA limited to mucosa 90% – Extension thru bowel wall 70 -80% – With positive nodes 30 -50% – With metastases <20%
Prognosis 10 year survival – CA limited to mucosa 90% – Extension thru bowel wall 70 -80% – With positive nodes 30 -50% – With metastases <20%
 Colorectal Cancer Tx Surgical- wide resection of tumor, plus regional lymph drainage with reanastomosis Adjuvant chemo survival by 10 -30% If no surgical cure option, consider palliative surgery, or tumor debulking measures (lessen obstructive sx)
Colorectal Cancer Tx Surgical- wide resection of tumor, plus regional lymph drainage with reanastomosis Adjuvant chemo survival by 10 -30% If no surgical cure option, consider palliative surgery, or tumor debulking measures (lessen obstructive sx)
 Follow-up Colonoscopy q year x 5 yrs, then q 3 yrs H&P, CBC, LFTs q 3 months x 3 yrs, then q 6 months x 2 yr
Follow-up Colonoscopy q year x 5 yrs, then q 3 yrs H&P, CBC, LFTs q 3 months x 3 yrs, then q 6 months x 2 yr
 Small Intestine Tumors Less than 5% all GI cancers Many benign tumors: adenomas, leiomyomas, lipomas, angiomas Increased risk malignancy with Crohn’s Dz, celiac disease – Adenocarcinoma, lymphoma Presentation: recurrent cramping abd pain, periodic small bowel obstruction (SBO), intussusception, chronic bleeds
Small Intestine Tumors Less than 5% all GI cancers Many benign tumors: adenomas, leiomyomas, lipomas, angiomas Increased risk malignancy with Crohn’s Dz, celiac disease – Adenocarcinoma, lymphoma Presentation: recurrent cramping abd pain, periodic small bowel obstruction (SBO), intussusception, chronic bleeds
 Small Intestine Tumors Diagnose with CT and DCBE – Usually out of reach of colonoscope or EGD Exploratory laparotomy for biopsy Stage as colon cancer Treat with surgical resection, +/radiation or chemo for debulking
Small Intestine Tumors Diagnose with CT and DCBE – Usually out of reach of colonoscope or EGD Exploratory laparotomy for biopsy Stage as colon cancer Treat with surgical resection, +/radiation or chemo for debulking
 Anorectal cancer Usually adenocarcinoma Mets to lymphatics of rectum and inguinal nodes Risk factors: HPV, chronic fistulas, irradiation, receptive anal intercourse, Screening with Pap/HPV testing Tx: wide local excision, chemo and rad
Anorectal cancer Usually adenocarcinoma Mets to lymphatics of rectum and inguinal nodes Risk factors: HPV, chronic fistulas, irradiation, receptive anal intercourse, Screening with Pap/HPV testing Tx: wide local excision, chemo and rad
 Pancreatic Cancer 30, 500 cases, 29, 000 deaths Most are exocrine tumors, primarily ductal adenocarcinoma 80% found in head of pancreas Mean age 55, 2 x more common in males Risk: smoking, chronic pancreatitis, longstanding DM, some heredity
Pancreatic Cancer 30, 500 cases, 29, 000 deaths Most are exocrine tumors, primarily ductal adenocarcinoma 80% found in head of pancreas Mean age 55, 2 x more common in males Risk: smoking, chronic pancreatitis, longstanding DM, some heredity
 Pancreatic Cancer Usually no symptoms until lesion too advanced to resect Symptoms non-specific, with large DDx – Weight loss, pain, anorexia, fatigue, dyspepsia, reflux, jaundice – Severe upper abd pain, radiates to back, relieved by forward lean or fetal position – Obstructive jaundice and resulting pruritis in 80 -90%
Pancreatic Cancer Usually no symptoms until lesion too advanced to resect Symptoms non-specific, with large DDx – Weight loss, pain, anorexia, fatigue, dyspepsia, reflux, jaundice – Severe upper abd pain, radiates to back, relieved by forward lean or fetal position – Obstructive jaundice and resulting pruritis in 80 -90%
 S&S Palpable mass, ascites in 20% Left supraclavicular lymphadenopathy (Virchow's node) 90% have locally advanced dz w/ retroperitoneal structure involvement, regional lymph spread, or mets at time of pres
S&S Palpable mass, ascites in 20% Left supraclavicular lymphadenopathy (Virchow's node) 90% have locally advanced dz w/ retroperitoneal structure involvement, regional lymph spread, or mets at time of pres
 Diagnosing Pancreatic Cancer U/S initially to show ducts, stones, masses CT better defines tumor, and vascular involvement MRI great for vasculature Biopsy: transcutaneous, ERCP, guided fineneedle aspiration
Diagnosing Pancreatic Cancer U/S initially to show ducts, stones, masses CT better defines tumor, and vascular involvement MRI great for vasculature Biopsy: transcutaneous, ERCP, guided fineneedle aspiration
 Prognosis/tx Overall, <2% survival 80 -90% unresectable (mets or invasion of major blood vessels) If resectable- Whipple procedure (pancreaticoduodenectomy) with adjuvant chemo+ rad 40% 2 yr and 25% 5 yr survival if node negative
Prognosis/tx Overall, <2% survival 80 -90% unresectable (mets or invasion of major blood vessels) If resectable- Whipple procedure (pancreaticoduodenectomy) with adjuvant chemo+ rad 40% 2 yr and 25% 5 yr survival if node negative
 Treatment Appropriate end-of-life care: managing death, hospice care, etc Sx Control! PAIN- opioids (without concern for addiction as barrier to effective pain control)
Treatment Appropriate end-of-life care: managing death, hospice care, etc Sx Control! PAIN- opioids (without concern for addiction as barrier to effective pain control)
 Hepatic cancer Liver is common place for metastasis for many primary cancers, esp from GI tract, breast, lung, pancreas. – Mets more common than primary hepatocellular carcinoma Primary cancer 14 k deaths annually in US Primary liver cancer more common in pts with cirrhosis, common in areas with prevalent Hep B & C infections – Risk 100 fold in chronic hep B carriers
Hepatic cancer Liver is common place for metastasis for many primary cancers, esp from GI tract, breast, lung, pancreas. – Mets more common than primary hepatocellular carcinoma Primary cancer 14 k deaths annually in US Primary liver cancer more common in pts with cirrhosis, common in areas with prevalent Hep B & C infections – Risk 100 fold in chronic hep B carriers
 Liver Ca S&S Initially nonspecific: abd pain, fever PE may show RUQ mass, or BIG, hard, tender liver Hepatic bruits with pleuritic pain Late: jaundice, hepatic encephalopathy
Liver Ca S&S Initially nonspecific: abd pain, fever PE may show RUQ mass, or BIG, hard, tender liver Hepatic bruits with pleuritic pain Late: jaundice, hepatic encephalopathy
 Primary Liver Cancer Dx with – imaging: U/S, MRI or abd CT w/ contrast – Labs: AFP – Liver bx for definitive dx Overall 2 year survival <5% – IF tumor is <2 cm and localized to one lobe, can try resection or transplant. Chemo/rad NO help.
Primary Liver Cancer Dx with – imaging: U/S, MRI or abd CT w/ contrast – Labs: AFP – Liver bx for definitive dx Overall 2 year survival <5% – IF tumor is <2 cm and localized to one lobe, can try resection or transplant. Chemo/rad NO help.
 Hepatic Ca Prevention Hep B vaccination Prevent cirrhosis Screen pts with cirrhosis for CA – AFP and liver U/S q 6 -12 mo
Hepatic Ca Prevention Hep B vaccination Prevent cirrhosis Screen pts with cirrhosis for CA – AFP and liver U/S q 6 -12 mo


