2d640a2c9fad3cfec2bfb33d2485b51a.ppt
- Количество слайдов: 24
Collaborative Care: Ongoing Learning and Teaching in a Resident-Faculty Partnership Jennifer Reckrey, MD Joanna Dognin, Psy. D
Objectives Understand the importance of ongoing collaboration between residents and behavioral science faculty 2. Learn a new collaborative teaching model that takes advantage of behavioral scientist expertise while remaining resident-driven 3. Review characteristics of good collaborative experiences 1.
“Ms. Sanders”: Hospital Admission (June) 42 y/o white female with deep scars on her face and arms, recently moved to New York to escape domestic violence in California, no established medical care despite severe asthma and debilitating chronic pain. Admitted to the family medicine service for an asthma exacerbation, but also described severe depression and suicidal ideation.
“Ms. Sanders”: Hospital Admission (June) Psychiatry consulted in the hospital, but her responded to their questions were guarded. Instructed to follow-up in psych clinic after discharge. Given hospital discharge appointment in our primary care clinic.
In Clinic 4 Weeks Later (July) Chief Complaint: asthma and debilitating pain Psychiatric History: many psych hospitalizations and failed medication trials, multiple suicide attempts from a young age, cutting behaviors, history of drug abuse, history of physical and sexual abuse Chaotic life: lack of stable housing since moving from California, history of domestic violence, unstable interpersonal relationships No psych providers accepted her insurance
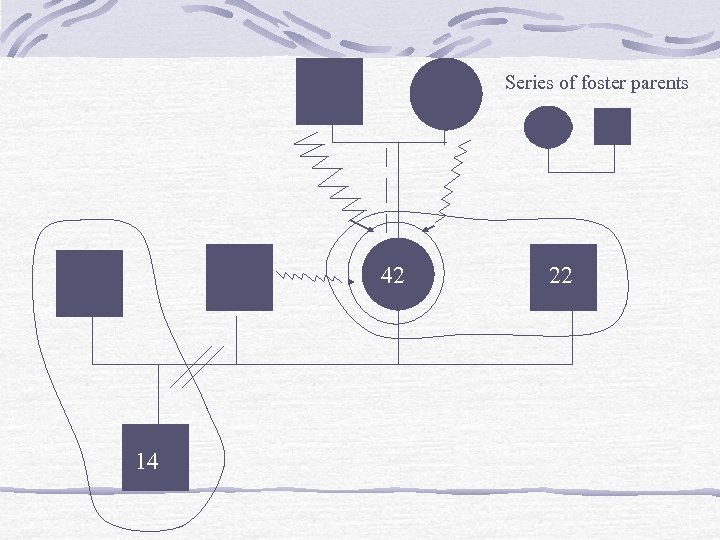
Series of foster parents 42 14 22
Current Clinical Presentation Sad angry Crying, low energy, not leaving house, irritable Increased cutting behaviors Hearing voices: “shut up”, “you’re worthless” Seeing ghosts at night and “the devil shaking his fist at me” Regularly thinks about death and suicide but doesn’t want to die and has no plan
Barriers to Care Poor insurance with very limited mental health coverage. So many concrete service needs: Housing, food, medications, work, money So many physical needs: Asthma, muscle spasms So many mental health needs: Chronic suicidality, poor impulse control Mixed messages
What Happened Next… Talked with medical preceptor: Not actively suicidal, asked SW to further evaluate cutting & to facilitate psych referral. I contracted with the patient for safety and made agreement about outpatient follow up plan. Then I brought in the social worker: Though Ms. Sanders didn’t want to die, she said she was cutting to “bleed out. ” The social worker felt obligated to send her to the psych ER for full evaluation of suicidality. And then patient left against medical advice.
Processing the Aftermath Thinking about it afterwards, I felt like I failed and irreparably damaged our relationship. Confusion between words and actions But talking about feelings helped A safe space to unpack feelings of confusion and frustration Understanding why it was such a difficult case helped.
Why Didn’t This Collaboration Work? Different role definitions Lack of relationship history between clinicians Power inequities Attending and social worker and resident Crisis mode vs. teaching mode Comfort with risk (and legal responsibility) Patient factors and experiences working with borderline patients
So Now What? Several 1: 1 meetings (resident, faculty) Continued to process the case and perceived therapeutic disruption, discussed follow-up plans with patient Discussed gray areas in assessing suicidal risk and intervening Focus on clinical reasoning skills and effective collaboration Decided would be a relevant topic for resident teaching AND that we wanted to demonstrate a collaborative model by co-teaching it
Teaching Together (August) Different from typical psychosocial teaching Usually either 1 hr. resident presentation (with supervision of faculty) or 1 hr. faculty didactic We combined 2 back-to-back slots and co-taught the topic Presented suicide facts, personal and societal reactions to suicide Discussed 3 different clinical presentations of suicidal behavior (depressed, schizophrenic, borderline pts) & discussed clinical reasoning & interventions
Teaching Together (August) Why I liked it (Resident): Resident driven but really got into subtleties of difficult concepts like chronic suicidal thoughts and borderline personality disorder Why I liked it (Faculty): Clinically and personally relevant to resident and allowed faculty to effectively utilize mental health expertise
Feedback About Teaching Very interactive seminar with lively discussion 12 residents and faculty filled out evaluations 10 rated presentation “Excellent” 2 rated it “Very good” One faculty member later commented it was best co-teaching seminar he had seen Resident suggested implementing similar coteaching in all psychosocial didactics Clearly, collaborative model was viewed as beneficial to audience
Moving Forward (October) How do we translate academic presentation to the clinical world? Scheduled a joint faculty-resident pt session Resident perspective: sharing burden but not giving away responsibility, seeing interaction modeled, defining roles Faculty perspective: adding mental health expertise while respecting resident’s perspective and previous history with patient
Therapy Session (October) Faculty scheduled pt for individual therapy session Missed appointment followed by intake “Lifetime of pain”, described childhood abuse, feelings of rage/violence towards anyone who sees her vulnerability Intimidating comments towards therapists (“Used to beat up people who I told my feelings to”)
Understanding Therapy Session Help-rejecting behaviors Next appointment: showed up many hours late demanding to be seen Patient/personality barriers to care Need for chaos Continual mixed messages Left therapist VM messages marked “urgent” but then angry when I reached out (“why are you bothering me? ”) Addition of Post Traumatic Stress Disorder diagnosis
Collaboration Continued (January – Present) Many missed visits (PCP and MH) Urgent phone calls & d/c’ed numbers (MH) Psychosocial precepting at all medical visits Key visit: Pain medication request Integrated preceptors feedback despite initial reservation. Found voice in talking to pt Finally… psychiatry involved (in-house) Now a new collaboration
Resident Perspective What I learned (and couldn’t have learned otherwise) Planning ahead and setting an agenda Managing time in the visit Setting limits for our relationship Understanding my own limitations
Faculty Perspective What I learned/ taught (and couldn’t have done otherwise) Clinically: Benefits of having collaborative approach with such a challenging therapy patient (therapy less lonely) Teaching: Need for resident learner to be an active participant in their own learning plan, and how this learning can be translated to multiple settings (clinical care, didactic seminar, conference presentation)
So What Makes a Good Collaborative Relationship? Clear understanding of roles Everybody having their own voice (not a mouthpiece) Negotiation of goals Making difficult decisions together (psych admission? Pain meds? ) Respecting each other’s previous relationship with the patient, and expertise Longitudinal relationship—letting relationship change and shift over time
Advantages of a Collaborative Model Increase credibility and trust Partners in care rather than consultants Feel like equal player vs. guest Positive relationship from collaborative care case carries over into other patient care, precepting moments Both parties feel more empowered and respected Less avoidance of complicated case
Thank you!
2d640a2c9fad3cfec2bfb33d2485b51a.ppt