6edde52d07b53addc8119b863eafa3e0.ppt
- Количество слайдов: 83
Collaboration Between Acute Care, Primary Care and Home Care Presented by Montefiore Home Care
Learning Objectives • Illustrate need to implement specialized programs • Describe how to develop a program • Illustrate a collaborative approach with primary care and hospital settings • Discuss how these models can be replicated in your agency

Speakers • Angela Schonberg, PT Moderator • Amy Ehrlich, MD Medical Director, MHC • Wojciech Rymarowicz, PT Director of Rehabilitation Services • Roberta Duke, RN Program Manager, Heart Failure • Janice Korenblatt, LCSW Director of Social Work • Mirnova Ceide, MD Geriatric Psychiatry
Montefiore Health System Amy Ehrlich, MD Medical Director, MHC Associate Chief, Division of Geriatrics Montefiore Medical Center
The Bronx Ixtayul. blogs. com Van Cortlandt Lake. Photo: Daniel Avila Courtesy, NYC Parks & Recreation
The Bronx Thesurrealestate. org
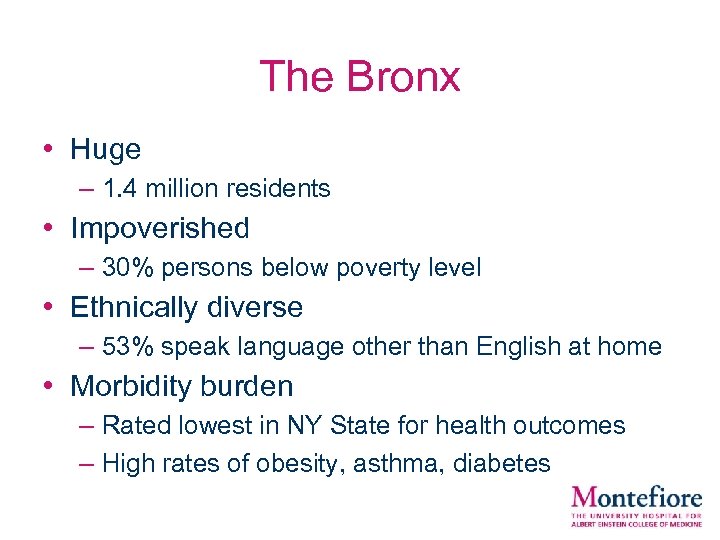
The Bronx • Huge – 1. 4 million residents • Impoverished – 30% persons below poverty level • Ethnically diverse – 53% speak language other than English at home • Morbidity burden – Rated lowest in NY State for health outcomes – High rates of obesity, asthma, diabetes
Montefiore Medical Center
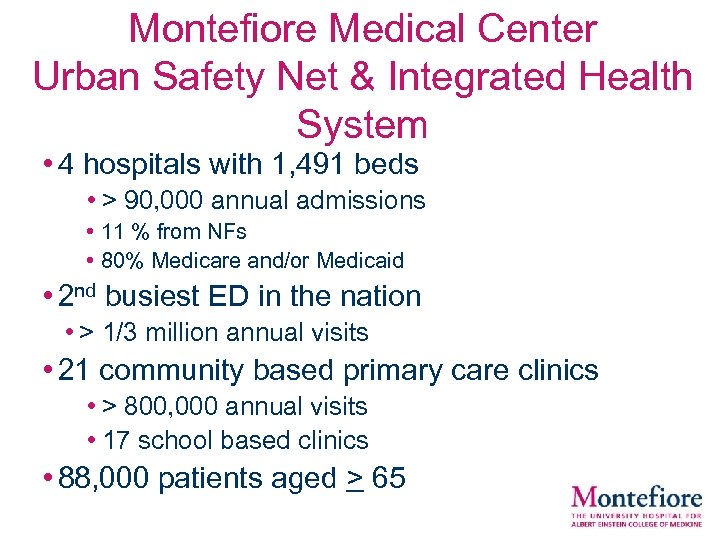
Montefiore Medical Center Urban Safety Net & Integrated Health System • 4 hospitals with 1, 491 beds • > 90, 000 annual admissions • 11 % from NFs • 80% Medicare and/or Medicaid • 2 nd busiest ED in the nation • > 1/3 million annual visits • 21 community based primary care clinics • > 800, 000 annual visits • 17 school based clinics • 88, 000 patients aged > 65
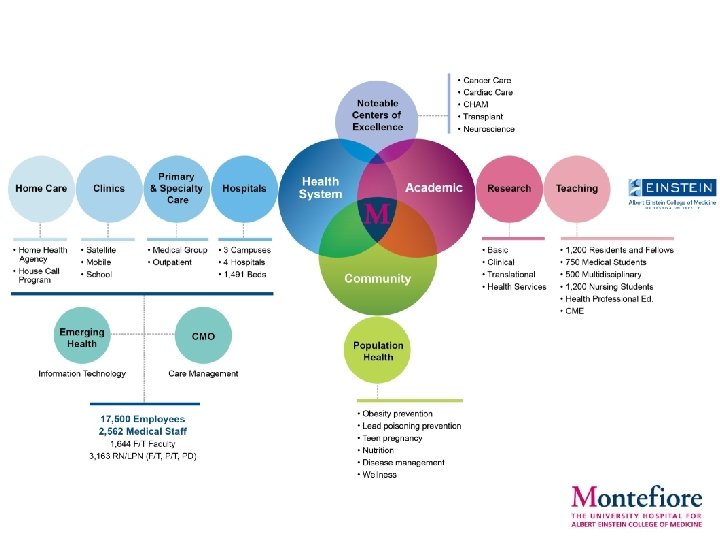

Montefiore’s Care Management Organization (CMO) • Established in 1996 • Wholly-owned subsidiary of Montefiore • Performs care management delegated by health plans • 15 years full risk managed care experience • 94, 000 risk lives (2010) 220, 000 (2013) • Over 1, 900 physicians in the network
Accountable Care Organizations • ACOs: • Groups of physicians, hospitals and other providers who accept responsibility for the quality and cost of care for a population • Triple Aim: • Better care for individuals • Better health for populations • Reduced expenditures
Accountable Care Organizations • Quality Performance • Pay for performance • Rewards for higher quality • Penalties for poor quality • Shared cost savings • Denied if quality performance is low • Dropped from the ACO • Financial risk if poor quality and/or inefficiency
Pioneer ACO Program • Center for Medicare and Medicaid Services (CMS) initiative designed for organizations with experience managing populations • Serves Medicare fee-for-service beneficiaries • Start January 2012 - last 3 -5 years • Quality scoring across multiple domains • Potential shared savings with substantial financial risk and gain
Quality Evaluations • 33 quality metrics in 4 domains: • Patient/Caregiver experience • Care Coordination/Patient Safety • Preventive Health • At-Risk Populations • Performance compared relevant US benchmarks
Montefiore’s Pioneer ACO • CMS assigned 23, 000 Medicare Fee-forservice (FFS) beneficiaries • 18% aged < 65 • 59% aged 65 -84 • 23% aged > 85 • Physicians • 70% community-based MDs • 30% Montefiore-employed MDs
Montefiore’s Approach • Identify high risk patients • Analyze CMS claims data • Sentinel events: • ED visits, hospitalizations, dialysis • Develop new initiatives across the network • In-Patient, ED, NFs, ambulatory setting
High Risk ACO Patients • Highest-risk beneficiaries identified (1, 906) • 9% of population = 55% of medical cost • 9% dual eligible • 55% mental health diagnosis • Approximately 70% cared for by voluntary physicians
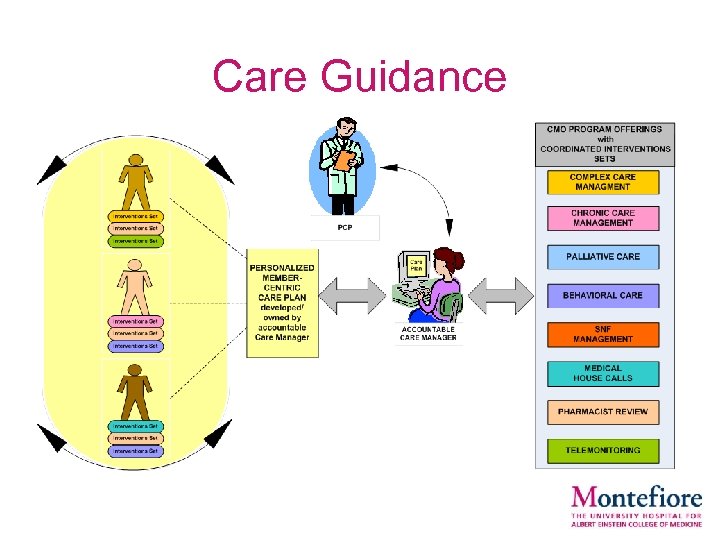
Care Guidance

New Initiatives • Care Guidance (care management) • Emergency Department Case Management • Transition Programs & Post-discharge calls • Nursing Facility (NF) initiatives • Home Care initiatives • Medical Home Visit Program • Integration medical & behavioral care management • Clinical pathways - back pain, heart failure, chest pain • Geriatrics Hospitalist Program • Consultation Services (Geriatrics, Palliative care)
Montefiore Home Care • Established in 1947 as the nation’s first hospital-based home care agency – Created to allow patients the benefits of athome recuperation – It was an innovative concept, referred to as a "hospital without walls" • Certified Home Care Agency accredited by JCAHO
Montefiore Home Care • 11, 573 admissions annually • Average Daily Census: 2, 600 • Skilled visits annually : – Nursing: 113, 012 – Rehabilitation Therapy: 37, 989 – Social Work: 11, 078
Montefiore Home Care Unique Programs • Complex Case – Weekly multidisciplinary rounds – Physicians call-in • Pharmacy consultations – Referrals by clinical staff to Pharm. D • MHC-CMO Joint RN – Collaborate across the network

Montefiore Home Care Disease Specific Programs • • • Elective Joint Replacement Heart Failure Behavioral Health Maternal Child Health Wound Care Palliative Care

Home Care Joint Replacement Rehab Program Presented by Wojciech Rymarowicz MS PT Director of Rehabilitation Service
Home Care Joint Replacement Rehab Program • Primary diagnosis - Osteoarthritis • > 7 million Americans • 2. 3 % of total population live with an artificial joint • 4. 7 million/1. 5% knee • 2. 5 million/0. 8% hip • Age 50 • 4. 6% TKR /2. 3%THR • Age 80 • 10% TKR/6% THR • Women > men American Academy of Orthopedic Surgeons March 2014
Home Care Joint Replacement Rehab Program • Increase Incidence past 10 years < age 64 • TKR > 120% • THR > 73% • Revision TKR > 133% • Revision THR > 27% • Increase related to disproportionate growth in utilization by younger patients and overall population growth • Patients discharged with home health care service • Total Joint Replacements 2000 =19 % 2009 > 41 % American Academy of Orthopedic Surgeons March 2014
Home Care Joint Replacement Rehab Program Implications for new healthcare delivery model • “Baby boom” generation • living to eighth decade and beyond • Medical conditions with greatest impact on the system • degenerative conditions - severe arthritis • afflicting over 15% • estimated to surpass 20% (or 60 million people) by 2020 We need to be ready!!!
Home Care Joint Replacement Rehab Program PROGRAM GOALS: • • • Increase discharges to home Decrease hospital length of stay Improve pre-operative teaching Achieve functional outcomes Improve patient satisfaction

Home Care Joint Replacement Rehab Program PROGRAM DEVELOPMENT • • • Assess Community - Identify need for specialty program Address Healthcare reform- ACO and bundled payments Partner with Orthopedic Centers or Departments Collaborate with orthopedic surgeons in development of clinical pathways and protocols Establish close relationship with inpatient/outpatient departments /vendors Educate staff including Home Health Aides Implement program Collect and analyze data Present program to payers to facilitate prior HC authorizations Market program
Home Care Joint Replacement Rehab Program HOW DOES IT WORK? • Patients referred by inpatient team for next day admission (SOC) • Patients receive initial visits / RN and PT first day after hospital discharge • Home Health Aide placed as needed • Patients receive daily PT visits /minimum 7 days • Focus on ROM, transfers, and gait training • RN for Medication reconciliation, anticoagulation administration and teaching
Home Care Joint Replacement Rehab Program HOW DOES IT WORK? • Case management role: transition from RN to PT week 1 • Orthopedic Surgeons updated routinely on patient progress • Rehab intervention frequency decreases as patients achieve rehab targets • First post op surgical visit • staples removed (7 -10 days) • prescription for out patient rehab (to avoid delays with appointments) • change in weight bearing status /ambulatory device
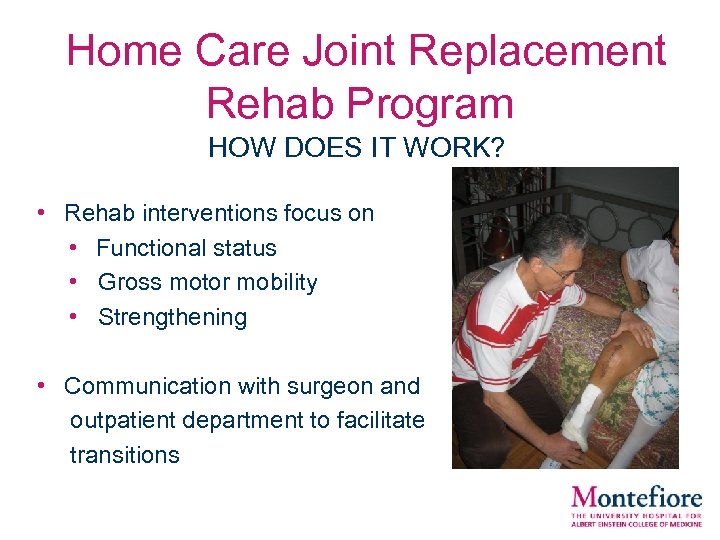
Home Care Joint Replacement Rehab Program HOW DOES IT WORK? • Rehab interventions focus on • Functional status • Gross motor mobility • Strengthening • Communication with surgeon and outpatient department to facilitate transitions
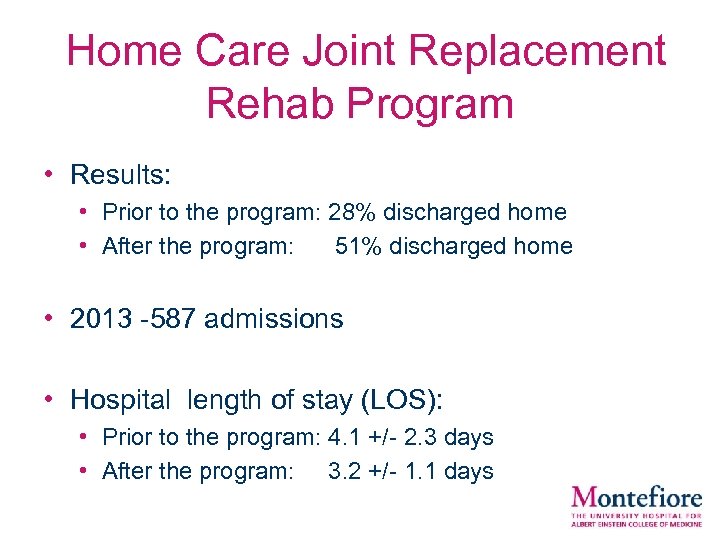
Home Care Joint Replacement Rehab Program • Results: • Prior to the program: 28% discharged home • After the program: 51% discharged home • 2013 -587 admissions • Hospital length of stay (LOS): • Prior to the program: 4. 1 +/- 2. 3 days • After the program: 3. 2 +/- 1. 1 days
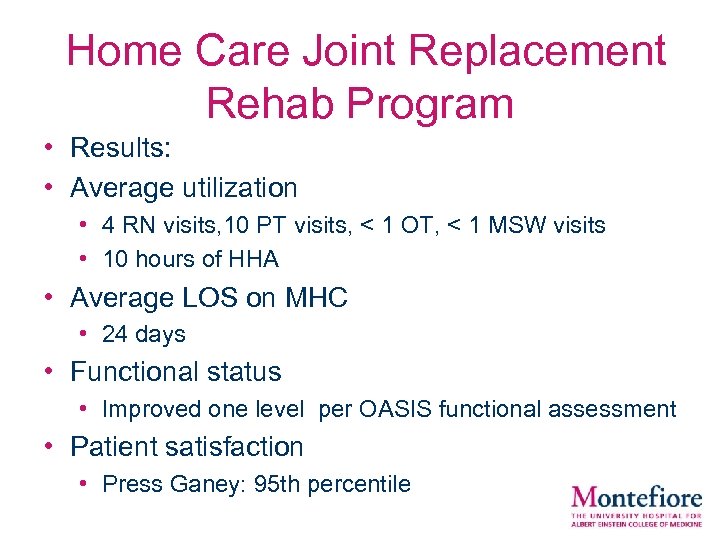
Home Care Joint Replacement Rehab Program • Results: • Average utilization • 4 RN visits, 10 PT visits, < 1 OT, < 1 MSW visits • 10 hours of HHA • Average LOS on MHC • 24 days • Functional status • Improved one level per OASIS functional assessment • Patient satisfaction • Press Ganey: 95 th percentile
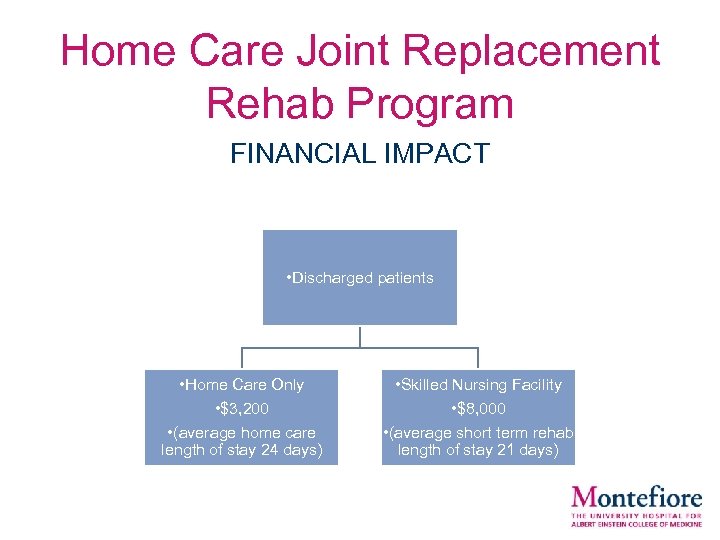
Home Care Joint Replacement Rehab Program FINANCIAL IMPACT • Discharged patients • Home Care Only • $3, 200 • (average home care length of stay 24 days) • Skilled Nursing Facility • $8, 000 • (average short term rehab length of stay 21 days)

Home Care Joint Replacement Rehab Program CHALLENGES • • • Authorizations vs service delivery Change in patient perception Pain management Staffing-weekend coverage Patients concerns/anxiety Physician “buy in”

Home Care Joint Replacement Rehab Program FUTURE • Shorter Acute care LOS • Bundled payments and managed care • Ambulatory procedures • Younger and more active population • Other treatment options • platelet rich plasma (PRP) • stem cells
Montefiore Homecare Heart Failure Program Presented by Roberta Duke RN Program Manager
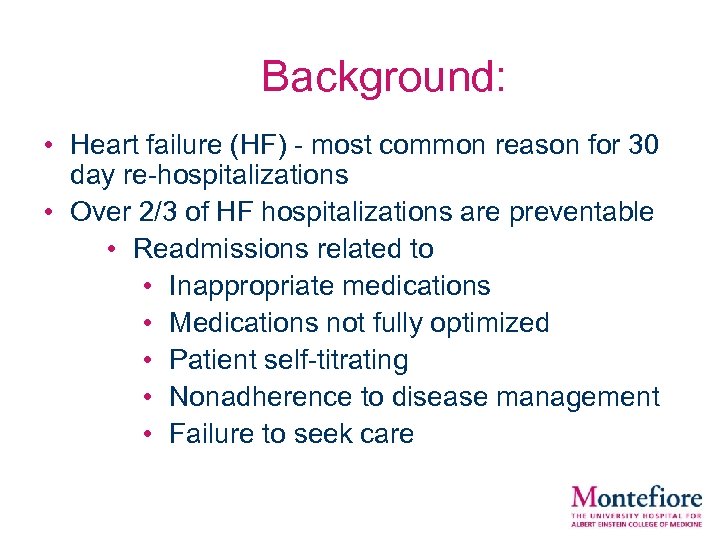
• Background: Heart failure (HF) - most common reason for 30 day re-hospitalizations • Over 2/3 of HF hospitalizations are preventable • Readmissions related to • Inappropriate medications • Medications not fully optimized • Patient self-titrating • Nonadherence to disease management • Failure to seek care
Program Goals: • Provide nursing interventions utilizing evidence based practice • Educate patients and caregivers • Foster adherence to disease management • Transition patients to caring for themselves • Reduce avoidable re-hospitalizations • Collaborate with network on bundled payments • Improve patient satisfaction
Program Development: Collaboration • Collaboration across Montefiore Network – Heart Failure specialty teams • Ileana Pina, MD-Vice Chair Cardiology • Director: N-He. FT (National Heart Failure Training Program) – “Brown Bag Clinics” • Pharmacist lead program for medication reconciliation at time of discharge – CMO HF team – Acute cardiology units
Program Development: Clinician Education • Specialized clinician training – RNs: • Clinical Rotations: – HF clinics, Brown Bag Clinics, Inpatient HF rounds – CMO HF team: Telephonic management • American Association for Heart Failure Nurses (AAHFN) • National Heart Failure Training Program (N-He. FT) • Self-learning module: – Pathophysiology – Pharmacology – Evidence-based practices.
Program Development: Clinician Education – Home Health Aides • Collaboration with vendors to train HHA to recognize signs and symptoms HF: – Clinical signs: » Number of pillows used » Dietary compliance » Weight checks – PT/OT • Clinical monitoring of HF patients
Program Development: Patient/Caregiver Education • Specialized patient/caregiver training – Patient education booklet – Individualized counseling on behavioral modification techniques
Program Development: Clinical Programs • New clinical tools: – Clinical pathways in the EMR – Standards of practice – Telephonic visit template – Compliance measures: • Chart reviews • Observational visits • Telephonic monitoring of patient comprehension and adherence • HF specific reports/tracking • Weekly case conference
Program Development: Clinical Programs • New clinical measurements: – Scales – Abdominal tape measures – Kansas City Cardiomyopathy Questionnaire (KCCQ)
Heart Failure Population Heart Failure population on MHC: 2013: 228 HF active patient • 51% (117/228) have an EF < 40% and/or > 2 hospitalizations in the past 6 month • 75% (88/117) were not followed by a HF physician • 52% (118/228) not on an ACE or ARB
Heart Failure Program: Implementation Patient selection: • EF< 40% and/or > 1 HF hospitalizations in the past 6 months Key Components: • Enhanced clinical monitoring • Nurse visits are front-loaded with telephonic visits performed in between • Education • Collaboration with HF specialists
The Role of Home Care in HF • Homecare offers a unique opportunity to educate patients, families & caregivers • HF trained nurses are the best candidates to identify early signs of de-compensation and with MD collaboration prevent a re-hospitalization • HF trained home health aides(HHA) assist in the plan
Challenges • Coordination of care for patients with complex psycho-social needs • Physician buy-in • Attaining authorizations from HMO • Continuing education for staff
Future Projects: Cardiac Rehabilitation
Behavioral Health Presented by Mirnova Ceide, MD Geriatric Psychiatrist Janice Korenblatt LCSW, Director of Social Work
Embedding Psychiatry into Home Care • < 3% of adults see a mental health professional • 2/3 of PCPs had trouble accessing mental health services • Older adults are less likely to receive follow up mental health care • Major Depression: – 13. 5% of elderly home health care – 6. 5% of older primary care patients
Suicide in the Elderly • Significant increase in the past 10 years. Health experts blame untreated depression. • 16% of all suicide deaths are adults aged > 65 • The National Alliance for the Mentally Ill (NAMI) reports statistics that underscores the lack of depression screening by many primary care physicians: • Adults age > 65 who commit suicide: – 20% saw a doctor the day they die, – 40% the week they die – 70% in the month they die. www. Aplace formom. com 2014, April 14 N. I. H.
Unmet Behavioral Health Needs Lead to … • Noncompliance: noncompliance with plan of care – 3 x more likely • Morbidity: Increases morbidity from chronic medical illnesses – DM twice as likely to have depression – Depressed adults twice as likely to be at risk for OSA – 36% of hospitalized older adults with HF have MDD
Unmet Behavioral Health Needs Lead to… • Hospital Costs: Depression and anxiety increases rehospitalization. – Unplanned hospital 30 day readmission 3 x as likely in elderly with history of depression. – 6 months readmission 3 x as likely in older adults with depressive symptoms. • Mortality: Major Depression associated with increased mortality – 43% increase of risk of all cause death – 2. 6 x risk of CVD death
Integrating Behavioral Health into Home Care • Consult liaison psychiatry: – One time consultations or very limited follow up. • Strategies: – Collaborative model: IMPACT multisite trial • Validated in the elderly • 50% decrease in thoughts of suicide – Colocation: Small scale model in Home Care and Inpatient settings • Most cost effective in capitated or cost sharing systems.
Model for Geriatric Psychiatry in Home Care Identify and treat the homebound elderly with depression • Model program to integrate psychiatry into Home Care – 2004: Home Care established collaboration with Dept. of Psychiatry at Montefiore. –New York Cornell Westchester provided the training for clinical staff on recognizing symptoms of depression. –Educational program for geriatric psychiatry fellows, residents and medical students
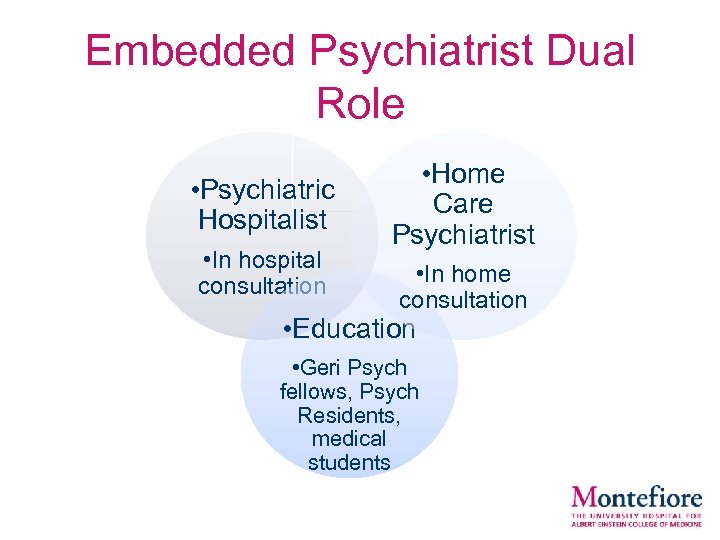
Embedded Psychiatrist Dual Role • Psychiatric Hospitalist • In hospital consultation • Home Care Psychiatrist • In home consultation • Education • Geri Psych fellows, Psych Residents, medical students
Training Program • PHQ 2 and PHQ-9 – Assessment instrument for of both screening and evaluating – They have both been validated in primary care populations. Sensitivity > 80% • Training utilized the Outcome and Assessment Information Set (OASIS) – CMS instrument required of home health agencies for reimbursement – This allowed depression screening and treatment to be captured in the reimbursement for Home Care
Scoring and Screening for Depression • PHQ-2: scores range from 0 - 6 • 86% sensitive and 78% specific for major depression • Score of > 3 requires further evaluation for depression • Referred to Home Care social worker who completes PHQ-9
Reasons for Referrals to Geriatric Psychiatry • • • Depression Anxiety Psychosis Hoarding Dementia with behavioral disturbance Capacity evaluation
Geriatric Psychiatry Home Care Program Goals : – Establish a program to provide care to population that underutilizes mental health services – Improve collaboration with hospital and primary care providers Outcome measures: – Reached men and minorities who underutilize mental health treatment – Timeliness of evaluations – Reached the population for which the institution has taken financial risk – Enhanced collaboration with hospital and primary care
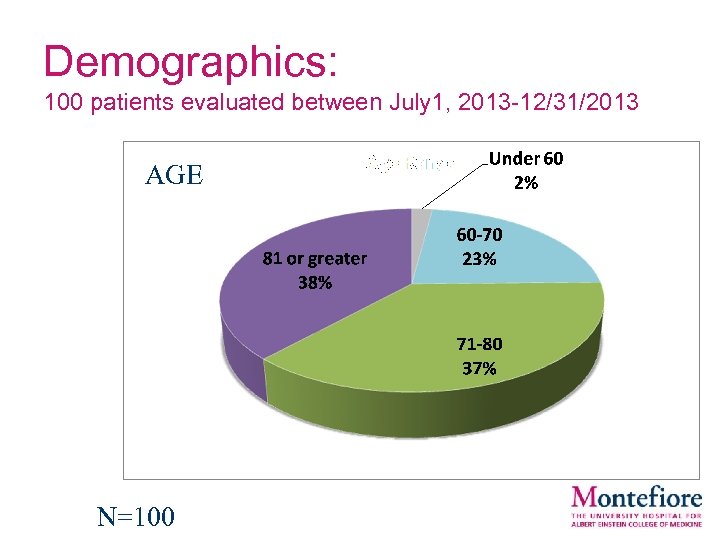
Demographics: 100 patients evaluated between July 1, 2013 -12/31/2013 AGE N=100
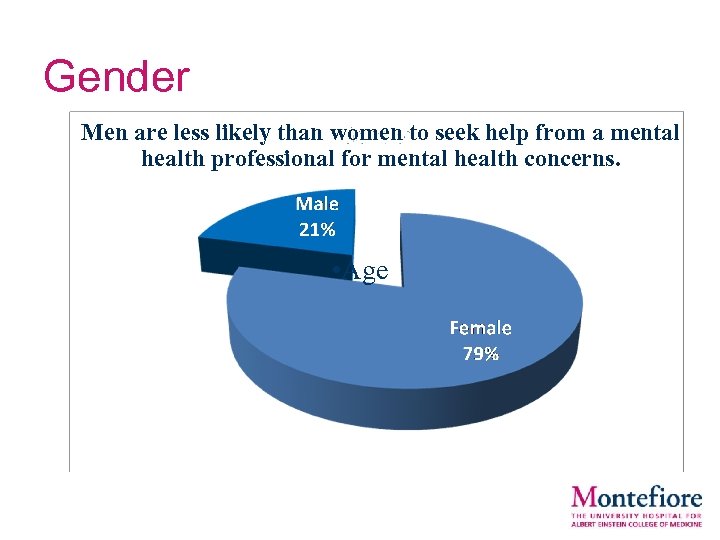
Gender Men are less likely than women to seek help from a mental health professional for mental health concerns. • N=100 • Age
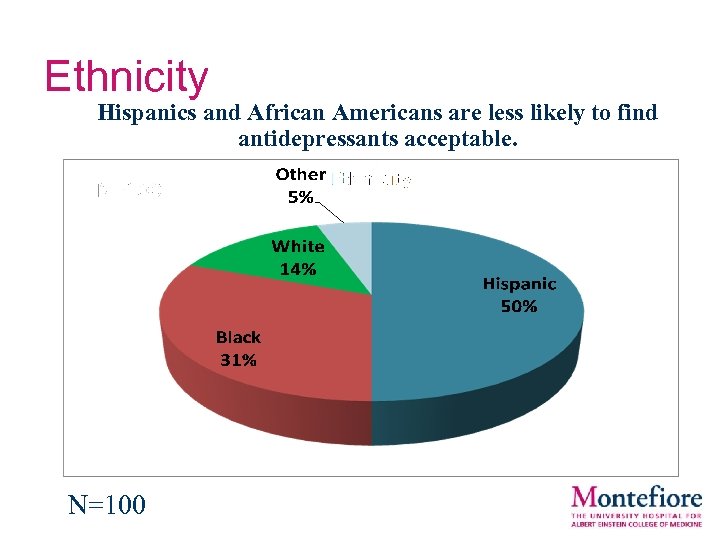
Ethnicity Hispanics and African Americans are less likely to find antidepressants acceptable. N=100
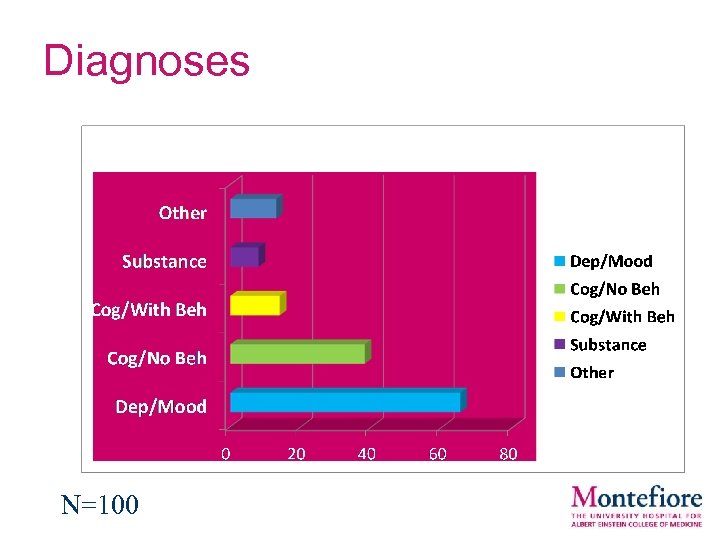
Diagnoses N=100
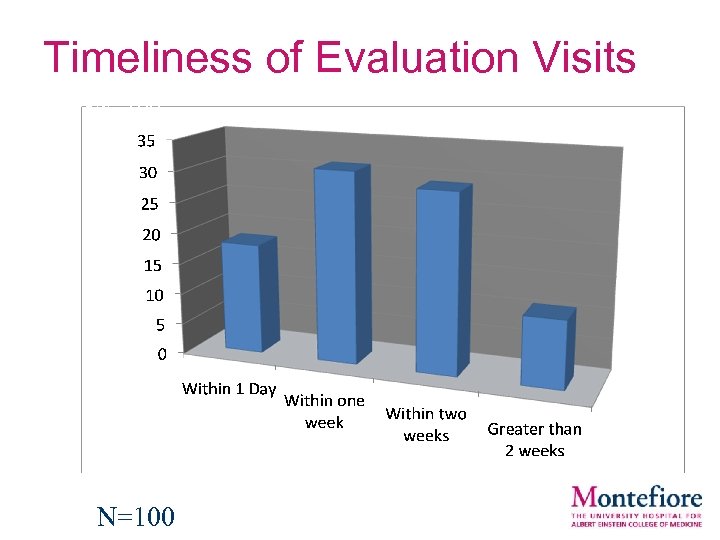
Timeliness of Evaluation Visits • N=100
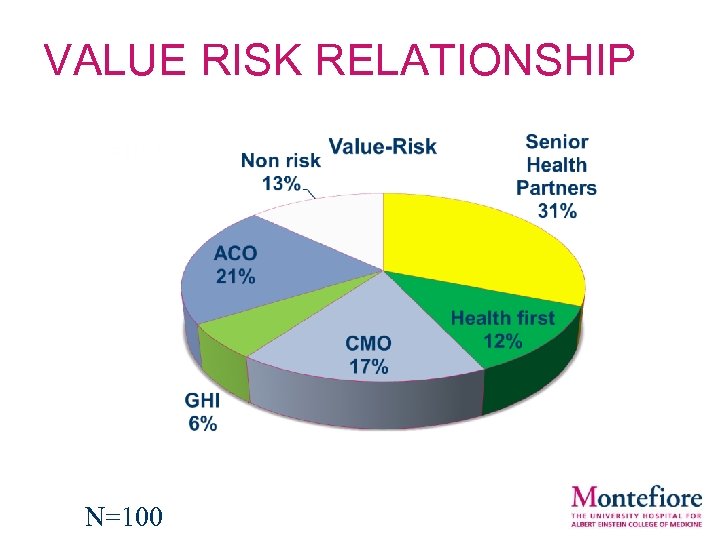
VALUE RISK RELATIONSHIP N=100

Treatment Options • Medications – Depression/Anxiety: Selective Serotonin Reuptake Inhibitors (SSRI’s) are most commonly prescribed or Serotonin Norepinephrine Reuptake Inhibitors and other drug classes. – Dementia with Psychosis/Behavioral Disturbance: Antipsychotics-atypical or typical. • Psychological Interventions – Counseling provided by home care social workers – Out patient mental health providers for continued care • Adult Day Program/ Senior Centers – Pts with Medicaid are eligible for day programs. – Minimizes agitation, improves depression, improves sleep.
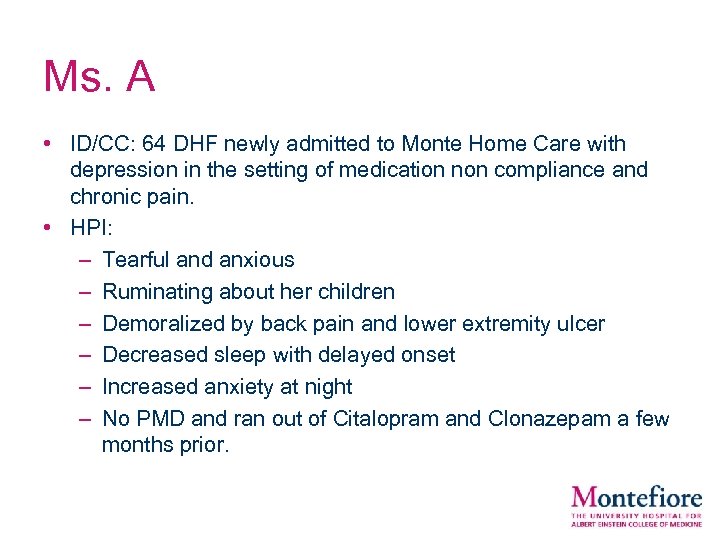
Ms. A • ID/CC: 64 DHF newly admitted to Monte Home Care with depression in the setting of medication non compliance and chronic pain. • HPI: – Tearful and anxious – Ruminating about her children – Demoralized by back pain and lower extremity ulcer – Decreased sleep with delayed onset – Increased anxiety at night – No PMD and ran out of Citalopram and Clonazepam a few months prior.
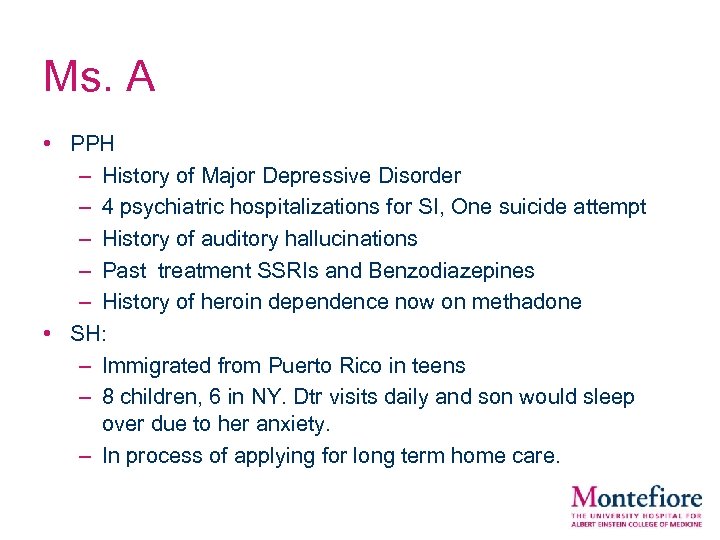
Ms. A • PPH – History of Major Depressive Disorder – 4 psychiatric hospitalizations for SI, One suicide attempt – History of auditory hallucinations – Past treatment SSRIs and Benzodiazepines – History of heroin dependence now on methadone • SH: – Immigrated from Puerto Rico in teens – 8 children, 6 in NY. Dtr visits daily and son would sleep over due to her anxiety. – In process of applying for long term home care.
Ms. A • PMH – DM, CHF, Asthma, left lower extremity ulcer • MSE – Anxious appearing Hispanic woman – Psychomotor agitated – Depressed mood – No SI, no hallucinations or delusions. – MMSE 25/30
Ms. A • A/P – Diagnoses: MDD, Unspecified Anxiety disorder, Opioid use disorder on maintenance – Restarted on Clonazepam and started on Duloxetine. • Follow up – She was later admitted to the hospital for increased left foot pain, suicidality and reported her daughter was abusive. – Upon consultation was able to speak with primary team and explained that there has been no previous reports or signs of abuse in the home. – Pt later rescinded her accusation and SI and was quite happy with daughter and son. She was started on Duloxetine which she has not been taking and was discharged home. – Upon follow up home visit was doing well.
Ms. B • ID/CC: 90 DHF with h/o anxiety seen for gradual decline in memory and paranoia • HPI: – Per son, pt getting more suspicious about neighbors and daughter in law. – Barricading herself in house. – Stopped taking medications. – Thought people were stealing her clothes and trying to get her apartment. (Complicated scenario related to her ex husband).
Ms. B • PPH – H/o panic attacks – Recently diagnosed with Dementia • SH: – Lives alone with HHA for 3 hrs when she allowed HHA to come. – Daughter in law primary caregiver because son lived in Florida. – No power of attorney (POA) • PMH – Vit D deficiency – Glaucoma – Pre diabetic
Ms. B • MSE: – Thin, temporal wasting; Home untidy, Pigeons kept in a laundry basket with a broom to weigh it down. – Bedroom windows covered in cardboard and lots of clutter. – Barricade near door – Lots of Meals on Wheels entrees in freezer with chair against fridge to keep it closed. – Forgetful, poor attention, rapid speech, tangential – Persecutory delusions – MMSE 12/30
Ms. B • A/P: – Dementia with behavioral disturbance – SW very involved in case. APS was called and declined case. – Pt found not to have capacity. – Risperidone started for delusions. • Follow up: – Pt refused meds from daughter in law and son had to return from Florida to care for her. – He felt unable to get POA or take her to NH. – Joint visit with RN: EMS called, ER informed, Pt went calmly. – Pt placed in NH from ER.
Conclusion: Triple Aim • Accountable Care Organization: Triple Aim – Better care for individuals – Better health for populations – Reduced expenditures • Better care for individuals – Demonstrated the benefits of a colocation model of mental health integration in order to: • Identify high risk patients • Provide timely evaluation and care • Increase access to mental health care
Conclusion: Triple Aim • Better health for populations: – engage hard to reach populations (i. e. men and minorities) • Reduced expenditures – Transition to appropriate settings (i. e. Hospice, SNF, Adult Day) – Collaborate with primary care, hospital and community agencies
Adapting the Model • Partnering with department of psychiatry or mental health providers – Training site for learners • Forging relationship with community agencies • Aligning with recent CMS payment and policy updates – Bundled payments – Value Based Purchasing – Shared cost models

QUESTIONS
6edde52d07b53addc8119b863eafa3e0.ppt