c7c8be0dd42662ee98d5af5e8c06e8e3.ppt
- Количество слайдов: 62
Collaborating Hospice Relationships Martha L. Twaddle MD, FACP, FAAHPM Chief Medical Officer, Midwest Palliative & Hospice Care. Center Associate Professor of Medicine Rush University; School of Medicine Program Director of Palliative Care Rush Medical College Past President, The American Academy of Hospice and Palliative Medicine Steering Committee, The National Consensus Project in Palliative Care www. capc. org
What we’ll cover together… • Using case examples – let’s discuss concepts and opportunities for hospice programs to collaborate with institutions such as hospitals, LTC, ALF, and with other community organizations. www. capc. org
Necessary: • Appreciation of the well established interdisciplinary model within hospice care. • Appreciation of the culture and values of each entity – can be drilled down to specific institutions • Appreciation that together care can be fuller, more effective, robust, and satisfying for all parties. www. capc. org
The Epiphany • Progressive hospices have accepted the challenge of leveraging what we know how to do: interdisciplinary palliative care services (or whatever term you prefer) for a patient population whose needs/preferences extend beyond the boundaries imposed by the Medicare Hospice Benefit. www. capc. org
www. capc. org Scherer
Gertrude • 86 yo widow living independently in small town in central Illinois • Daughter, 53, lives local to the Care. Center and calls looking for “help with my mother. ” • No known terminal diagnosis, no pressing medical issues. • Just a very concerned daughter… www. capc. org
Gertrude • The daughter meets with a Palliative Care Consultant to talk about issues regarding • caring for an aging parent, • the family’s role in Advance Care Planning, • supportive options available in the community. • Daughter moves her mother to the area, into an ALF. Obtains a formal Palliative Care Consultation to see her mother. www. capc. org
Background… • This visit is not covered by insurance – out of pocket consultation expense for the daughter • Scheduled and processed like a patient visit – notes created, can copy family if appropriate. www. capc. org
Gertrude • Over the subsequent year, Gertrude becomes much more frail, afflicted by GI blood loss, recurrent anemia, anorexia, and fatigue. • She declines a medical work-up and consistently preferences that she does not wish to have further hospitalizations. • She falls, and fractures her hip and is hospitalized for emergent repair. www. capc. org
Gertrude • The Palliative Care inpatient service at the local hospital is staffed by the Midwest Care. Center physicians – an inpatient visit is provided to Gertrude. • The PC team helps negotiate the goals of care with the hospital team • The PC team works with her doctors and family to facilitate Gertrude’s transfer to a LTC facility for post-op rehabilitation (skilled care) s/p hip repair. www. capc. org
Background… • The Palliative Care inpatient service is already involved with Gertrude in the outpatient setting – so here does not require a new consultation request, • billed as co-management, • if a group practice – billed as an established patient. • If this was the first meeting – a consult order from the attending physician is preferred – remember the four R’s of consult – Request Render www. capc. org Reason Report
Background… • The patient and family can request Palliative Care as a “second opinion” without a consultation order. • Politically can be “sticky” but may be in patient/family best interest. • Provide reason and report as though a consult www. capc. org
Gertrude • Gertrude cannot achieve the necessary rehab goals in the skilled unit and opts out of “skilled care” into the nursing home room & board. • Guess what!!!? The Midwest Palliative Care. Center physicians “staff” the consult team at this LTC facility and see Gertrude in follow-up. • The team facilitates discussions with Gertrude, her principle physician and family and Gertrude elects to enter hospice care. www. capc. org
Background… • Documentation of choice is necessary. • The patient/family and attending physician choose which agency will be utilized for hospice care – it is not an “automatic” referral to Midwest. • Hospice programs can consider following via their PC consults arm a patient in another hospice program; • requires a contract arrangement with the other hospice. www. capc. org

Midwest is everywhere! How did we get to be that way? ü In 1989 – we had 4 hospice patients ü We practiced B&B hospice ü And defined ourselves by what we “don’t do”…. www. capc. org We asked people to wait! “finish your treatments first…”
The Collegial perspective of our referring physicians… • High association with imminent death • “Consults” were primarily new referrals to hospice • High association with MSO 4 and Ativan www. capc. org
We were the first to ask ourselves…why do we wait? Why is that we wait until death is imminent or, at the very least, obvious, to talk about quality of life and the goals of care? ? ? ! www. capc. org
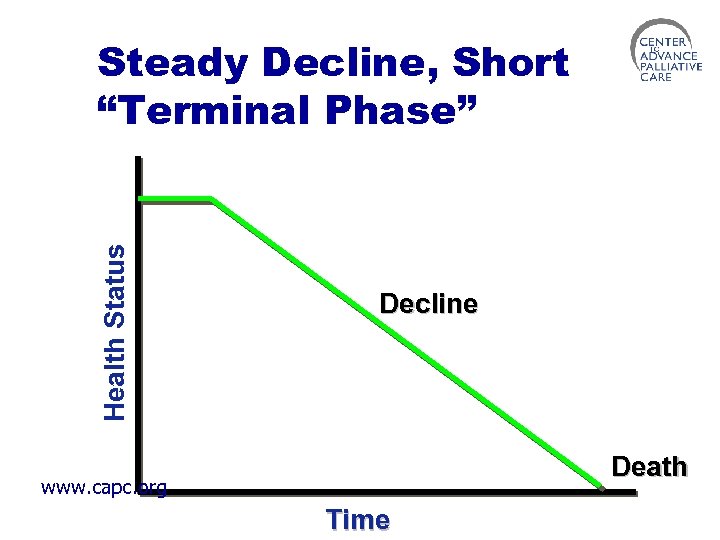
Health Status Steady Decline, Short “Terminal Phase” Decline Death www. capc. org Time
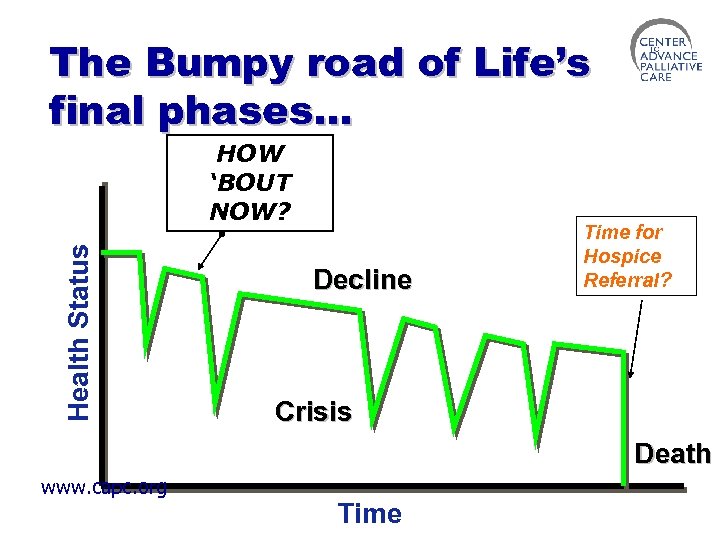
The Bumpy road of Life’s final phases… Health Status HOW ‘BOUT NOW? Decline Time for Hospice Referral? Crisis Death www. capc. org Time
Process changing realizations! The expertise of hospice care is needed, necessary, and vital far upstream to the actual hospice referral. The customer wants our support and expertise, even when they “don’t want hospice” We can tailor our support to meet the needs of patients and families and meet them where they are… www. capc. org
Our awakening spurred our Growth and Activity • 1989 – Community-based not-for-profit Hospice program serving 4 pts • 1995 – Opened our first Hospice IPU and launched a consult service model after the successful Rehab Medicine model • 1998 – launched a home-based Palliative Consult service • 1999 – moved our IPU and expanded our consult service to another (and competitor) hospital system www. capc. org
Our awakening spurred our Growth and Activity • 2001 – opened an ambulatory PC consult practice • 2003 – evolved a PC consult service in a LTC facility • 2005 – mourned the death of our first LTC service and grew others • 2005 – leased space in an Oncology practice for PC consults www. capc. org
Our awakening spurred our Growth and Activity • 2006 – we find ourselves increasingly providing specialty services to multiple competing entities. www. capc. org
Behind the scenes of every project: • Understanding the needs and culture of the “customer” • Each institution is unique • Complementing/enhancing their system of care delivery through collaboration • Educating and training “their own” to be a part of our team. www. capc. org
A Model: Our Growth and Activity • Commitment to remain community-based and mission focused • Seek to collaborate and respond to requests to create innovative service models in many different settings • Remain community-based and mission focused • Serving competitive systems in the community! • Tailor our services to meet the needs of each institution – that is “one size does not fit all…” www. capc. org
Hospice Team Transformation • Every consult is an opportunity to identify support needs and answers. • Bring the expertise of the IDT approach, whole person perspective, and experience with prognosis to the acute care and long-term care setting. • Increase advocacy for patients and families and colleagues: “your options are……” • Think outside the box! www. capc. org
Introducing Palliative Care Support early • As a quality initiative for improved symptom control • As a platform for Advance Care planning • As navigators in the complex world of healthcare where medical goals may be discordant with meaningful outcomes • Not just for the sake of the hospice referral – creating robust support systems upstream from “end-of-life” www. capc. org
Our Definition of Palliative Care “Interdisciplinary care that aims to relieve suffering and improve quality of life at any age, at any stage and in any setting, whether the goal is cure or care. ” www. capc. org
Our Target audience • Those with a recent or recurrent diagnosis of a life-threatening illness • Those with chronic illness facing increasing debility, life-limitation, and life change • The frail elderly and their families/caregivers strategizing the “what if. . . ” • The families and caregivers of the above…. www. capc. org
What are the goals of the Palliative Care Team? • Focusing on relief of suffering, promotion of function, clarification of goals of care, and support for patient and family caregivers; aims for best possible quality of life as determined by patient and family • Complementing the healthcare teams in place in whatever setting the patient may be at any one time • Following the patient/family across many settings of care and in/out of many institutions if necessary. www. capc. org
Collaborating Hospice Partnerships • Provide opportunities for hospices and healthcare institutions to fully utilize the strengths and resources of each other to benefit patients & families! www. capc. org
Our Hospital – Hospice teams • Rush North Shore Medical Center • Evanston Northwestern Healthcare • Evanston Hospital • Glenbrook Hospital • Highland Park Hospital • Lake Forest Hospital • St. Francis Hospital www. capc. org
LTC/ALF Teams • Contracts with over 150 LTC and ALF facilities • Three have robust Palliative Care and Hospice services of 15 to 30 patients • Regular “rounds” provide real time teamwork, education, and enhanced communication • Settings host regular community and staff educational events as well as on-site bereavement support and memorial services www. capc. org
The “Consult” starts the conversations • For any setting – the how of the “consult”… • Patient, physician or family initiated • Any patient, any diagnosis, any age v not driven by prognosis – but by perceived need. • Any location • • Hospital SNF, ALF Community or ambulatory clinic Home www. capc. org
Palliative Care Consult Team A Fluid Interdisciplinary Team Model Hospice and Institution’s staff create the team: • Hospital – ward staff, pharmacist, hospital chaplains and SW + PC practitioners • LTC – ward staff, SW, PT, OT + PC practitioners • ALF – RNs of ALF + PC practitioners, LCSW +/home health • Office setting – our practitioners and LCSWs www. capc. org
Palliative Care Consult Team • In addition to clinical care, goals of: üEducation – disseminating information üDiffusing tensions and intensity v. The blessing of the “second opinion” üSpreading the support for patients and families üSupporting the professional caregivers üAffirming the Art of Caring www. capc. org
Documentation • Your notes say a lot of who you are • Document using the Domains of Quality Palliative Care (National. Consensus. Project. org) www. capc. org
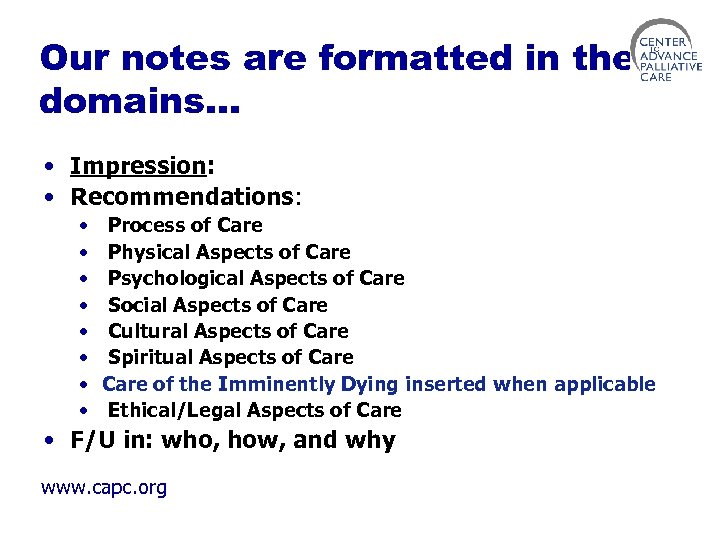
Our notes are formatted in the domains… • Impression: • Recommendations: • • Process of Care Physical Aspects of Care Psychological Aspects of Care Social Aspects of Care Cultural Aspects of Care Spiritual Aspects of Care of the Imminently Dying inserted when applicable Ethical/Legal Aspects of Care • F/U in: who, how, and why www. capc. org
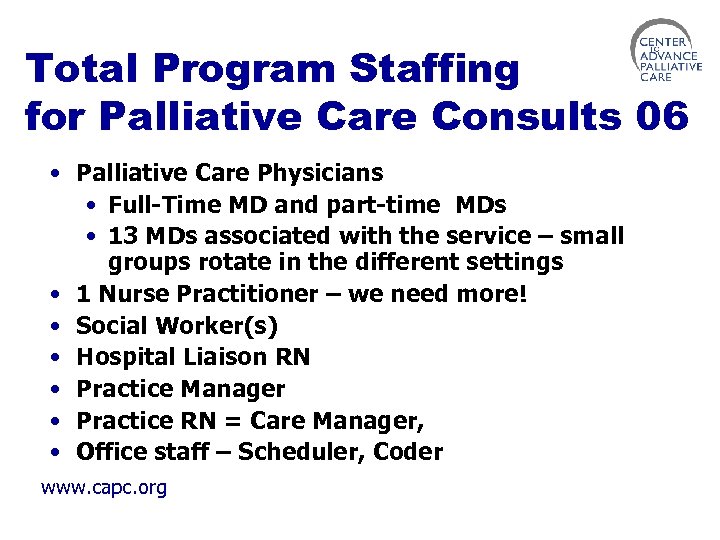
Total Program Staffing for Palliative Care Consults 06 • Palliative Care Physicians • Full-Time MD and part-time MDs • 13 MDs associated with the service – small groups rotate in the different settings • 1 Nurse Practitioner – we need more! • Social Worker(s) • Hospital Liaison RN • Practice Manager • Practice RN = Care Manager, • Office staff – Scheduler, Coder www. capc. org
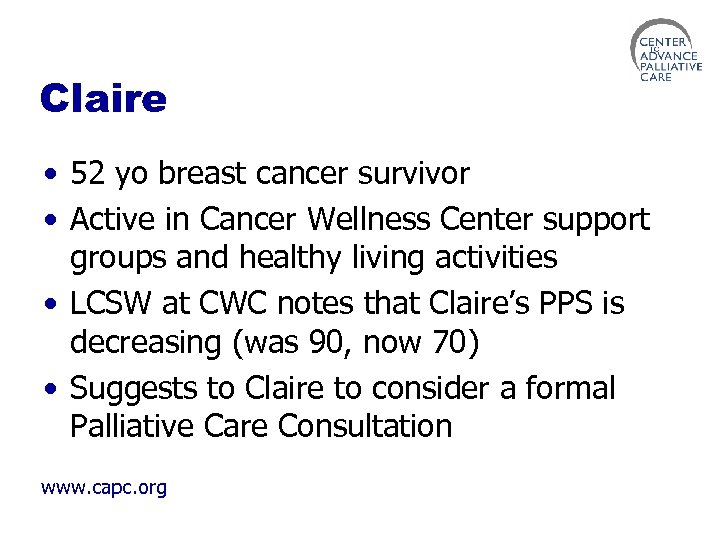
Claire • 52 yo breast cancer survivor • Active in Cancer Wellness Center support groups and healthy living activities • LCSW at CWC notes that Claire’s PPS is decreasing (was 90, now 70) • Suggests to Claire to consider a formal Palliative Care Consultation www. capc. org
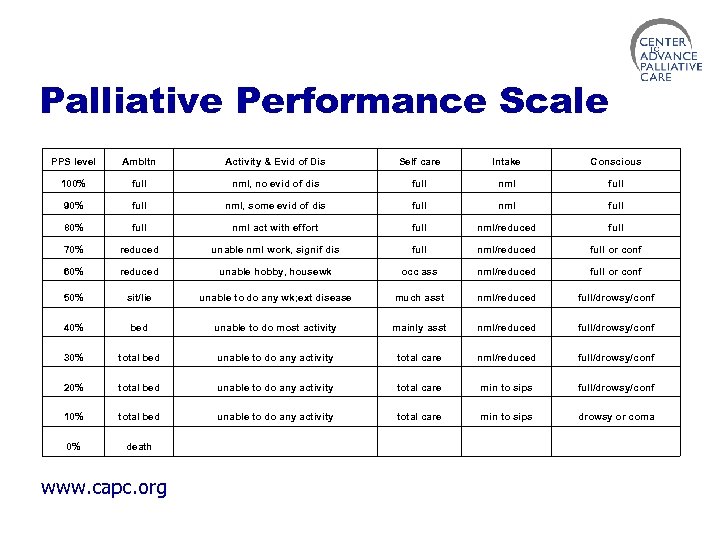
Palliative Performance Scale PPS level Ambltn Activity & Evid of Dis Self care Intake Conscious 100% full nml, no evid of dis full nml full 90% full nml, some evid of dis full nml full 80% full nml act with effort full nml/reduced full 70% reduced unable nml work, signif dis full nml/reduced full or conf 60% reduced unable hobby, housewk occ ass nml/reduced full or conf 50% sit/lie unable to do any wk; ext disease much asst nml/reduced full/drowsy/conf 40% bed unable to do most activity mainly asst nml/reduced full/drowsy/conf 30% total bed unable to do any activity total care nml/reduced full/drowsy/conf 20% total bed unable to do any activity total care min to sips full/drowsy/conf 10% total bed unable to do any activity total care min to sips drowsy or coma 0% death www. capc. org
Claire • Calls Midwest to arrange outpatient visit. • Midwest calls Oncologist for “an order” • Oncologist expresses shock – “She doesn’t need hospice!” • Midwest describes the difference • Claire sees Palliative Care practitioner in office setting www. capc. org
Claire & PCC • Discuss and establish greater clarity around Claire’s goals • Coordinate with CWC (Wellness IDT) to facilitate a plan of care that integrates with community programs for exercise, massage, and individual psychology work • Continue intermittent care for over 2 years, through several treatment courses for the breast cancer • Claire actually enters and leaves hospice care during this 2 year period – gets better during her time in hospice, • Then reenters hospice again approximately 8 weeks before her death. www. capc. org
www. capc. org
Althea • 84 yo widowed lady diagnosed with colon cancer moves in with her son and his family • Enters hospice care given diagnosis and communication of poor prognosis • Hospice home care continues for several months www. capc. org
Althea • Despite diagnosis – Althea is “doing fine” • Her son’s family is not… • Family meeting (many) facilitates transition of Althea to neighborhood nursing home • Althea thrives in the social environment, gains weight, becomes increasingly active • “graduates” from hospice and lives 2 more years!!! • Seen intermittently with PCC in the NH www. capc. org
Opportunities for ongoing care • In the “old days” – a hospice discharge or revocation meant “good-bye for now” • Today we have capacity to continue to support patients/families without the limitations of only one programmatic structure www. capc. org
Challenges within these opportunities • We must think beyond one programmatic structure • We must honor the regulatory milieu of many programmatic structures and how to move correctly effectively between them • We must be overt in our support of patient/family choice www. capc. org
Where do I start? www. capc. org
How to Make it Happen 1. 2. 3. 4. 5. 6. Build on Established Relationships Get sound legal advice Recognize and address internal resistance Use Education as a powerful tool for change Make it easy to bill appropriately for services Anticipate growth www. capc. org
1. Build on Existing Relationships • Leverage the earned credibility hospice programs have established in the community; this is a key resource in developing partner relationships • Assure that hospice physician and nurse leadership have the skills, credibility and visibility to elicit referrals www. capc. org
1. • • • Build on Existing Relationships (continued) Focus on helping referral sources with THEIR patients Deliver quality services in a timely manner Document Outcomes to create a record of accomplishment - to serve as benchmarks for peer assessment - to create a baseline for quality assurance initiatives - to justify funding support - www. capc. org
2. Get Sound Legal Advice • Be aware that each State has its own unique set of legal and regulatory requirements e. g. see all State list of corporate practice of medicine laws (tool) • There alternative organizational structures within which professional health care services can be rendered e. g. see Raffa legal opinion (tool) • Health Care Attorneys are specialists – you need one. www. capc. org
2. Get Sound Legal Advice (continued) • Use contracts to define who will provide what services and how - e. g. MD and RN’s to Consult Sx - e. g. leased space for a Hospice IPU • Use contracts to define how services get reimbused - e. g. XRT - e. g. invasive pain management - e. g. dietary and housekeeping for IPU www. capc. org
2. Get Sound Legal Advice (continued) • Make sure contracts are REGULARLY reviewed and updated www. capc. org
3. Recognize the Barrier of Internal Resistance • While hospitals and hospices are both in the business of healthcare, providers and administrators from each setting bring different skills and perceptions to the table • Creating a climate of collaboration takes time: it is a process and not an event • For early initiatives, involve individuals from each setting who can focus on the desired outcomes and who are amenable to change. www. capc. org
4. Use Education as a Powerful tool for change • Integrate with or join the faculty at are teaching institutions • Develop formal curriculum for the disciplines of medicine, nursing, social work etc and open your doors to students • Provide regular educational sessions in institutional settings via Grand Rounds, Noon Conference, Specialty rounds, Inservices, etc. www. capc. org
5. Bill for Services • Understand that Part B billing is very different than billing for Medicare Hospice services • Determine if your organization can/should assume Part B billing or if that function is to be subcontracted (a “make” or “buy” decision) • Make it easy for physicians and nurse practitioners to bill (see tool); • Provide coding information (Charles) • Bill from the beginning – do not delay this aspect of the work • Track the financial data – for business reasons and to justify new, on-going and/or enhanced funding support www. capc. org
6. Anticipate Growth • Assume several different utilization projections and use them to test different staffing scenarios • Identify and monitor referral data patterns • Create staffing flexibility by developing position descriptions identifying cross-program and/or cross-provider functions - e. g. liaison nurse (see position description) • Identify or develop access to per diem services - e. g. PCCHNS Private Care, Inc. www. capc. org
Where has this journey taken us? www. capc. org
“You must be the change you wish to see in the world” MK Gandhi www. capc. org

Mtwaddle@carecenter. org www. capc. org
c7c8be0dd42662ee98d5af5e8c06e8e3.ppt