c3a68d12816333f9ddc30f5bb17faa33.ppt
- Количество слайдов: 51
Co. Ba. Sys: Il punto di vista del medico Dr. Giovanni Guaraldi

HIV-1

Lo sviluppo dell’ AIDS Viral Load = Velocità del treno CD 4+ = Distanza dal baratro Modificata da Coffin J 1996
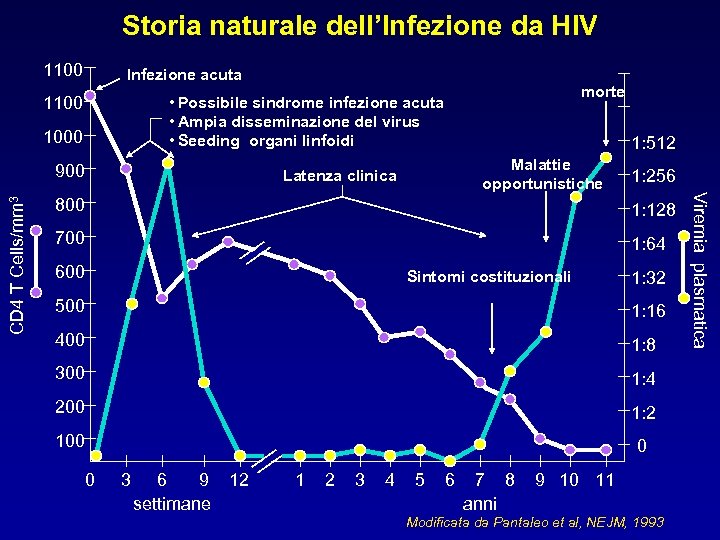
Storia naturale dell’Infezione da HIV 1100 Infezione acuta 1100 1000 900 1: 512 Malattie opportunistiche Latenza clinica 1: 256 800 1: 128 700 1: 64 600 Sintomi costituzionali 1: 32 500 1: 16 400 1: 8 300 1: 4 200 1: 2 100 0 0 3 6 9 settimane 12 1 2 3 4 5 6 7 8 anni 9 10 11 Modificata da Pantaleo et al, NEJM, 1993 Viremia plasmatica CD 4 T Cells/mm 3 morte • Possibile sindrome infezione acuta • Ampia disseminazione del virus • Seeding organi linfoidi

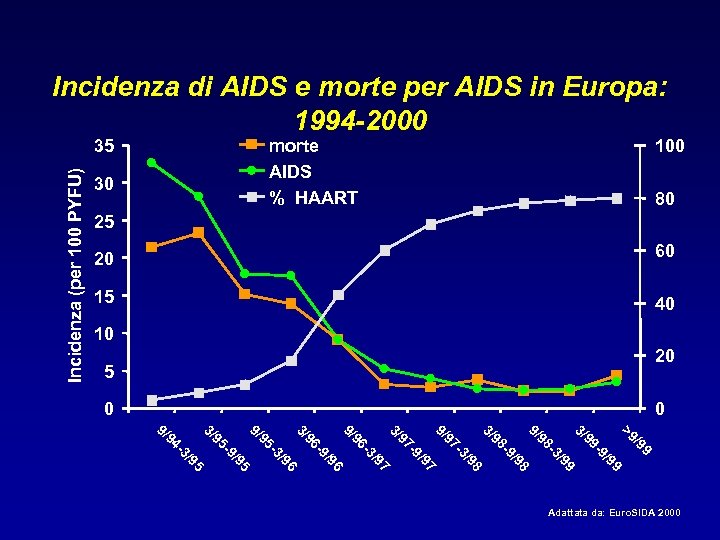
Incidenza di AIDS e morte per AIDS in Europa: 1994 -2000 Incidenza (per 100 PYFU) 35 morte AIDS % HAART 30 100 80 25 20 60 15 40 10 20 5 0 0 9 /9 99 / -9 99 >9 3/ 99 / -3 98 98 / -9 98 9/ 3/ 98 / -3 97 97 / -9 97 / -3 96 97 9/ 3/ 9/ 96 96 / -9 96 3/ / -3 95 9/ 95 / -9 95 95 / -3 94 3/ 9/ Adattata da: Euro. SIDA 2000
Time to act: global apathy towards HIV/AIDS is a crime against humanity
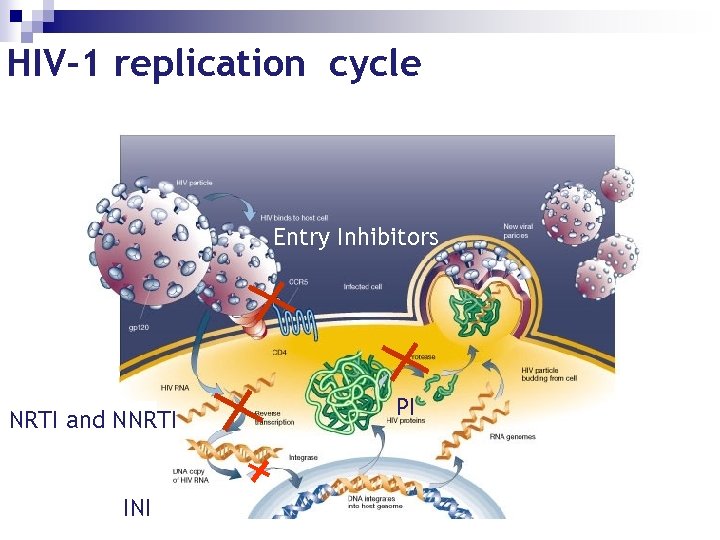
HIV-1 replication cycle Entry Inhibitors NRTI and NNRTI INI PI
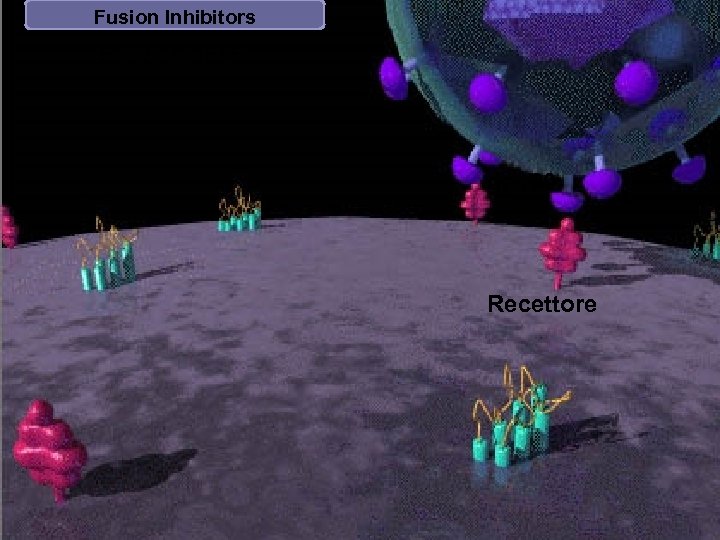
Fusion Inhibitors Enfuvirtide (ENF) gp 120 Recettore
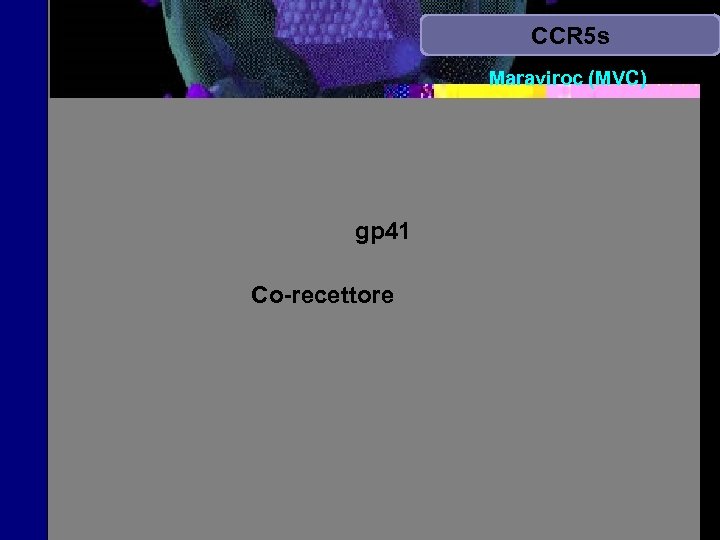
CCR 5 s Maraviroc (MVC) gp 41 Co-recettore
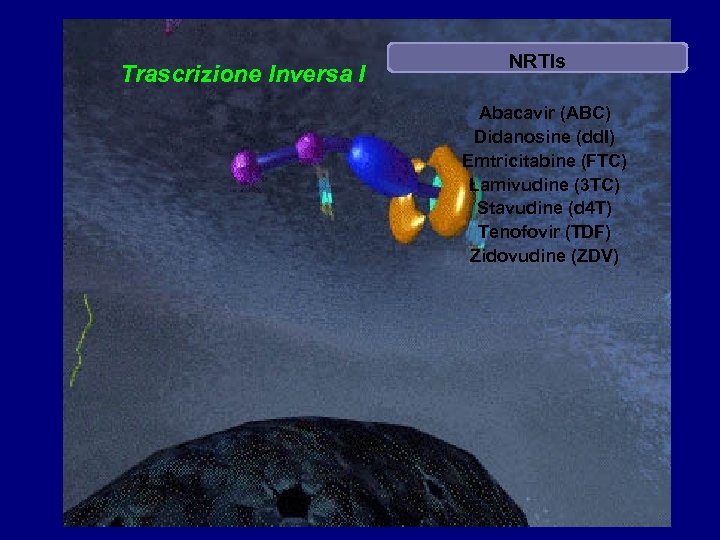
Trascrizione Inversa I NRTIs Abacavir (ABC) Didanosine (dd. I) Emtricitabine (FTC) Lamivudine (3 TC) Stavudine (d 4 T) Tenofovir (TDF) Zidovudine (ZDV)

Trascrizione Inversa II NNRTIs Efavirenz (EFV) Nevirapine (NVP) Etravirine (ETV)
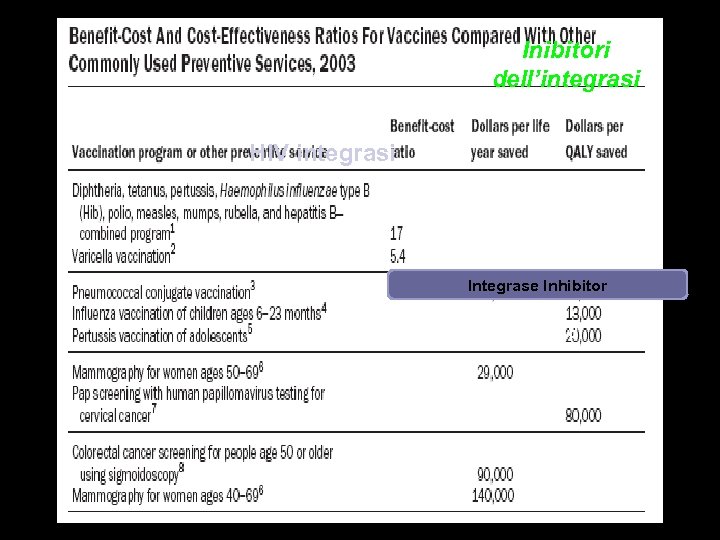
Inibitori dell’integrasi HIV integrasi Integrase Inhibitor MK-0518
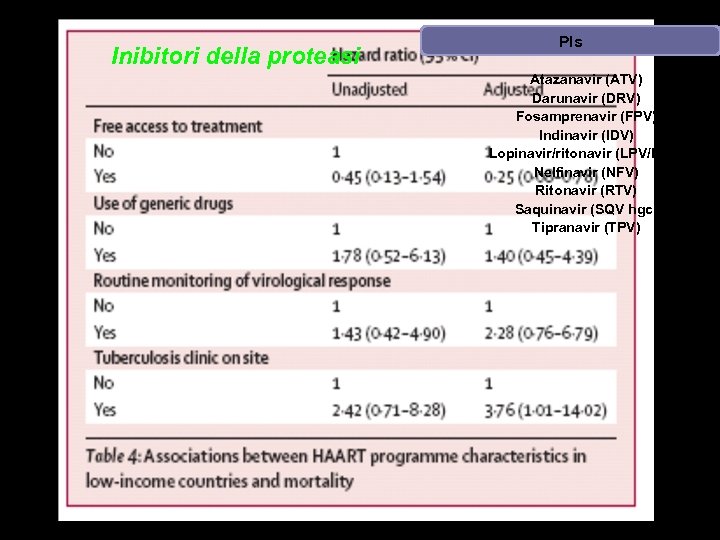
Inibitori della proteasi PIs Atazanavir (ATV) Darunavir (DRV) Fosamprenavir (FPV) Indinavir (IDV) Lopinavir/ritonavir (LPV/RTV) Nelfinavir (NFV) Ritonavir (RTV) Saquinavir (SQV hgc) Tipranavir (TPV)
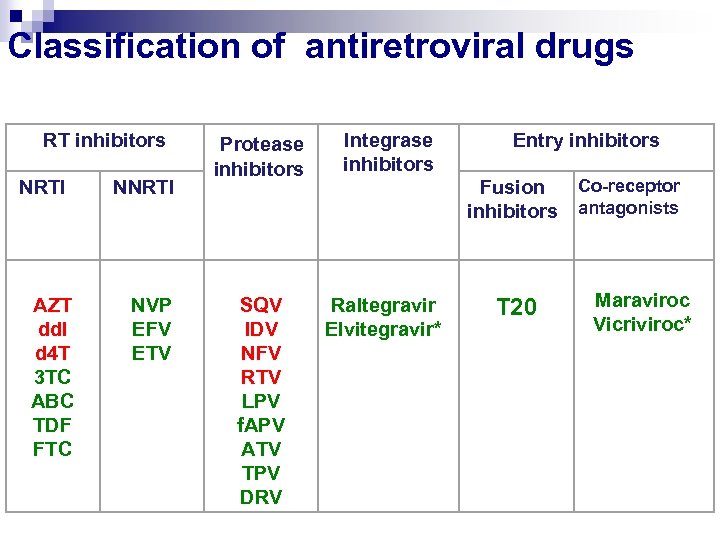
Classification of antiretroviral drugs RT inhibitors NRTI NNRTI Protease inhibitors Integrase inhibitors Entry inhibitors Fusion inhibitors AZT dd. I d 4 T 3 TC ABC TDF FTC NVP EFV ETV SQV IDV NFV RTV LPV f. APV ATV TPV DRV Raltegravir Elvitegravir* T 20 Co-receptor antagonists Maraviroc Vicriviroc*
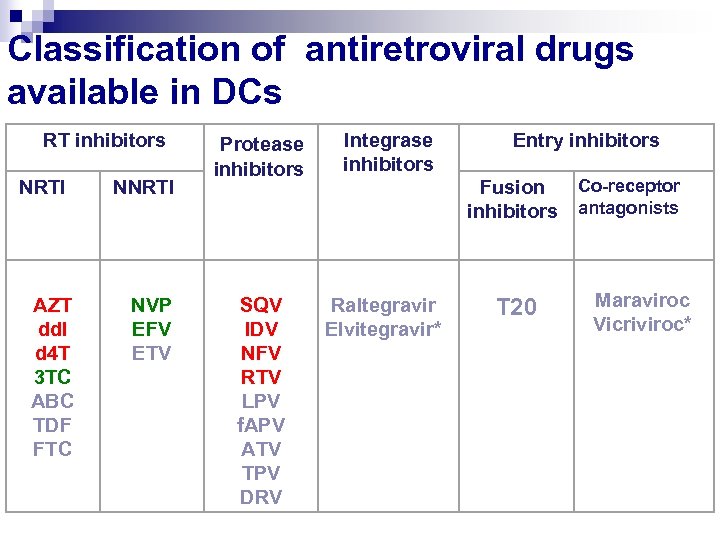
Classification of antiretroviral drugs available in DCs RT inhibitors NRTI NNRTI Protease inhibitors Integrase inhibitors Entry inhibitors Fusion inhibitors AZT dd. I d 4 T 3 TC ABC TDF FTC NVP EFV ETV SQV IDV NFV RTV LPV f. APV ATV TPV DRV Raltegravir Elvitegravir* T 20 Co-receptor antagonists Maraviroc Vicriviroc*
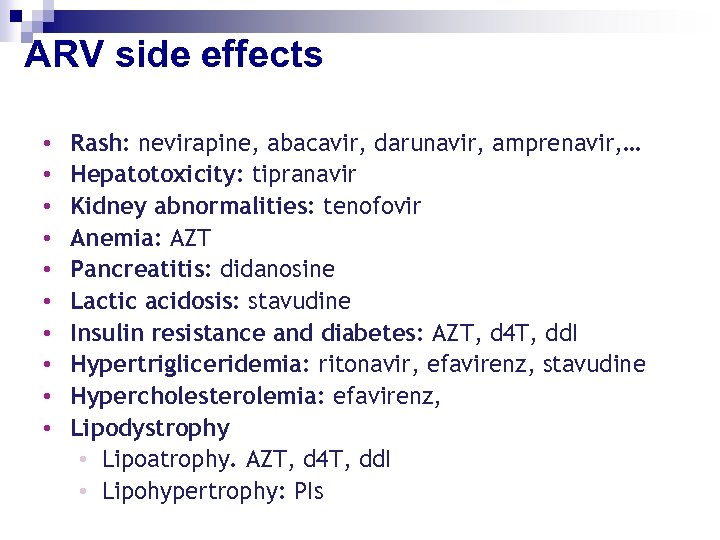
ARV side effects • • • Rash: nevirapine, abacavir, darunavir, amprenavir, … Hepatotoxicity: tipranavir Kidney abnormalities: tenofovir Anemia: AZT Pancreatitis: didanosine Lactic acidosis: stavudine Insulin resistance and diabetes: AZT, d 4 T, dd. I Hypertrigliceridemia: ritonavir, efavirenz, stavudine Hypercholesterolemia: efavirenz, Lipodystrophy • Lipoatrophy. AZT, d 4 T, dd. I • Lipohypertrophy: PIs
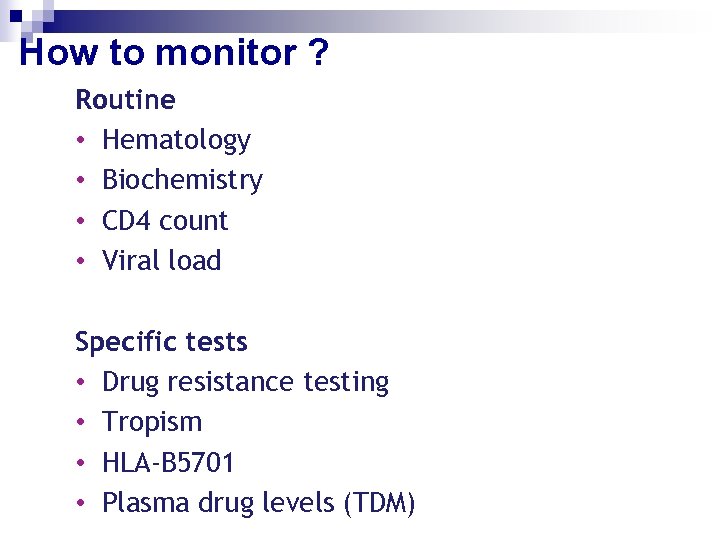
How to monitor ? Routine • Hematology • Biochemistry • CD 4 count • Viral load Specific tests • Drug resistance testing • Tropism • HLA-B 5701 • Plasma drug levels (TDM)
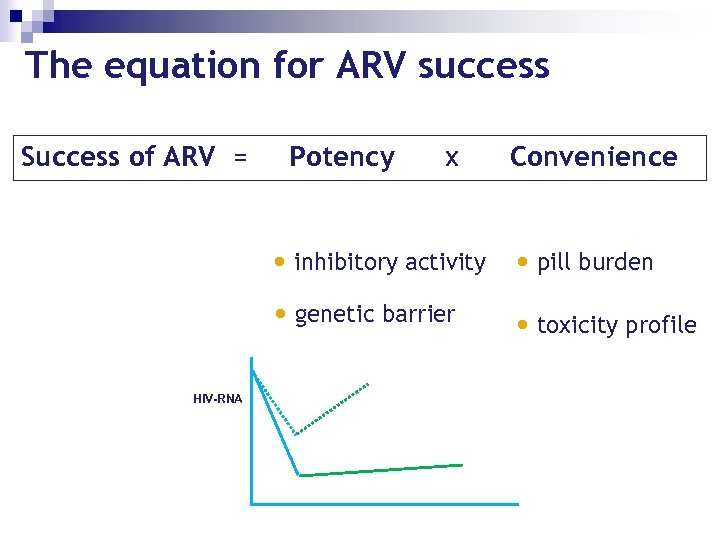
The equation for ARV success Success of ARV = Potency x Convenience • inhibitory activity • pill burden • genetic barrier HIV-RNA • toxicity profile
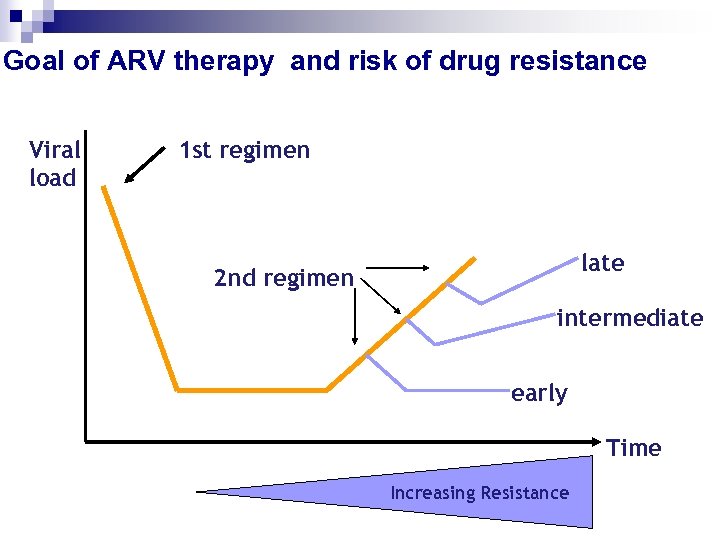
Goal of ARV therapy and risk of drug resistance Viral load 1 st regimen late 2 nd regimen intermediate early Time Increasing Resistance
ARV therapy is cost-effective in industrialized as well as in resource-limited countries • In a cost effectiveness study in Cote d’Ivore the incremental cost per year of life gained was $1180, for ART and prophylaxis with CD 4 testing. • In a sensitivity analysis based on the lower (25%) and upper (75%) interquartile range survival percentiles, the incremental cost per LYG ranged from $1, 557 to $1, 772 for the group without AIDS and from cost saving to $111 for patients with AIDS. Goldie S NEJM 2006, Egger 2006 22
ARV therapy is cost-effective in vulnerable groups in resource-limited countries • In Uganda ART and cotromoxazole prophylaxis reduced mortality 95% – 93% less estimated rate of orphanood (p<0. 0001) – 81% reduction in mortality in HIV-negative children (p<0. 004) – Having a parent die tripled risk HIV-negative child would die Goldie S NEJM 2006, Egger 2006 23
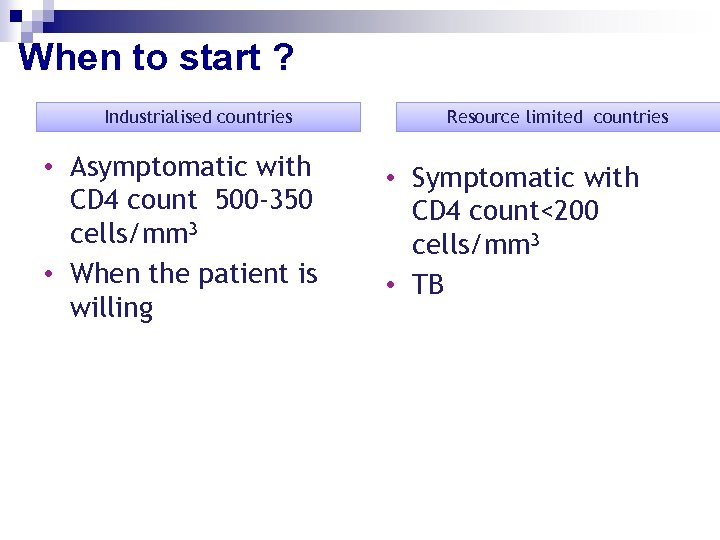
When to start ? Industrialised countries • Asymptomatic with CD 4 count 500 -350 cells/mm 3 • When the patient is willing Resource limited countries • Symptomatic with CD 4 count<200 cells/mm 3 • TB
• Free access to treatment was associated with lower mortality • Higher mortality was seen in programmes that included a TB clinic
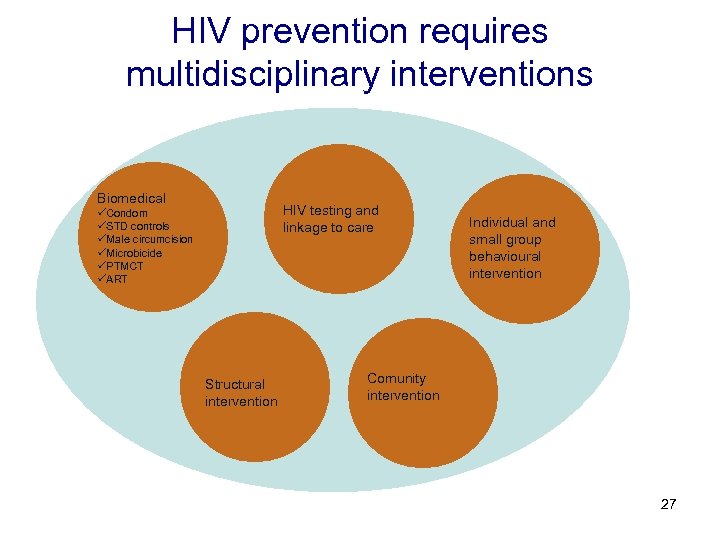
HIV prevention requires multidisciplinary interventions Biomedical HIV testing and linkage to care üCondom üSTD controls üMale circumcision üMicrobicide üPTMCT üART Structural intervention Individual and small group behavioural intervention Comunity intervention 27
• Stigma makes more difficult for members of high-risk groups to access preventive services • Stigma lead HIV-positive women to breast-feed their infants
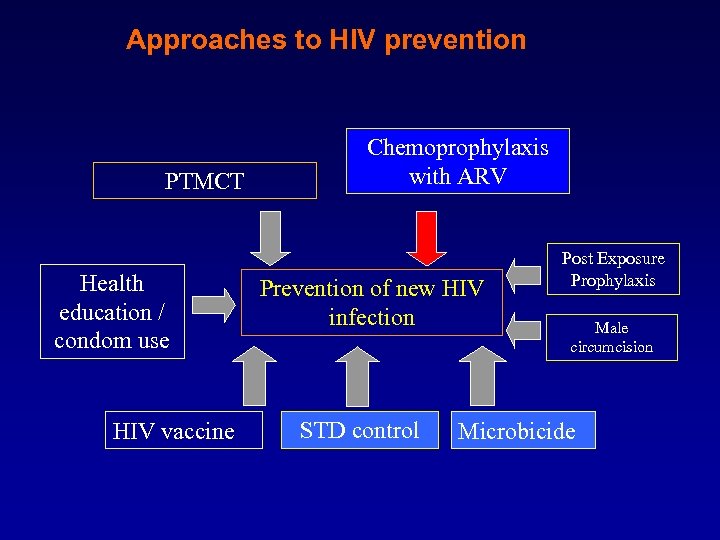
Approaches to HIV prevention PTMCT Health education / condom use HIV vaccine Chemoprophylaxis with ARV Prevention of new HIV infection STD control Post Exposure Prophylaxis Male circumcision Microbicide
HIV Vaccine • In 2007 a huge clinical trial using Merck’s SIV-equivalent gag vaccine failed to show any efficacy. • None of the vaccine products currently in the pipeline stand some reasonable chance of showing efficacy. • We need more discovery research to construct a immunogen to cover the enormous sequence variability of HIV. 30
Condom • Condom use is associated with 80% reduction in transmision • The ethical and moral debate concerning condom blocked any other preventive strategy for many years. – Efficacy change in different population or social context – International political involvement in condom prevention strategy is driven by political issues of international donors. 31
Circumcision • Observational studies indicate that circumcised men have lower levels of HIV • In December 2006 the Data Safety and Monitoring Board stopped two trials assessing the impact of male circumcision on HIV risk carried out in Kisumu, Kenya, and Rakai District, Uganda showing at least a 53% and 51% reduction in risk of acquiring HIV infection, respectively, in comparison with the no intervention arm 32
Circumcision & UNAIDS • Is as an efficacious intervention for HIV prevention • Must be implemented as a public health intervention as part of a comprehensive HIV prevention package • Circumcision for HIV-positive men is not recommended. • Male circumcision should never replace other known methods of HIV prevention 33
Risk for HIV infection is associated with a history of medical injections & blood transfusions Reverse causality? or Iatrogenic trasmission? Receiving prophylactic tetanus immunizations during pregnancy approximately doubled the risk for a woman subsequently having a positive HIV test result in Kenya 34
• Prevention and treatment go hand in hand
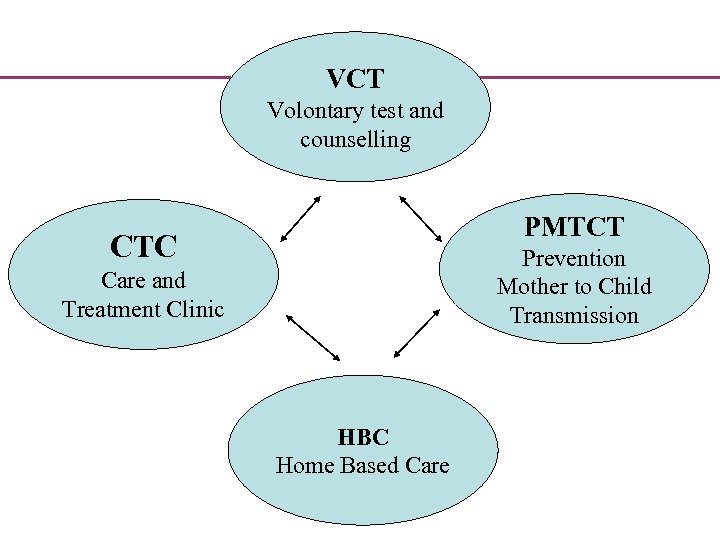
VCT Volontary test and counselling PMTCT CTC Prevention Mother to Child Transmission Care and Treatment Clinic HBC Home Based Care
VCT- Il test HIV Capillus Determine
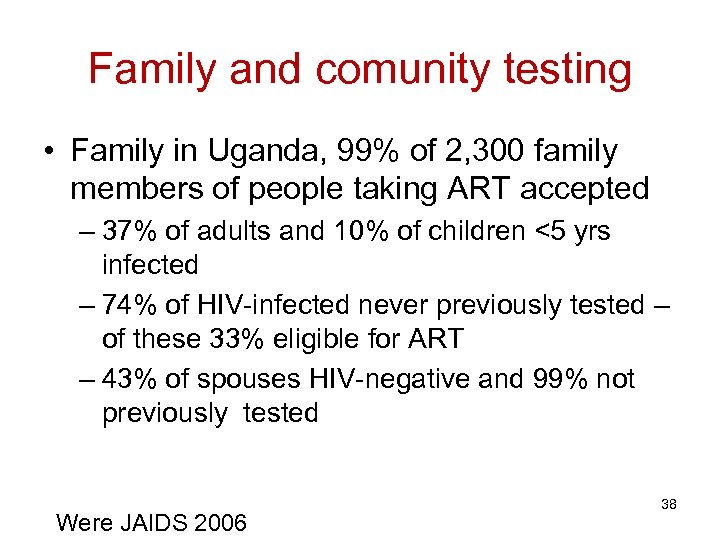
Family and comunity testing • Family in Uganda, 99% of 2, 300 family members of people taking ART accepted – 37% of adults and 10% of children <5 yrs infected – 74% of HIV-infected never previously tested – of these 33% eligible for ART – 43% of spouses HIV-negative and 99% not previously tested Were JAIDS 2006 38

PMCTC!?

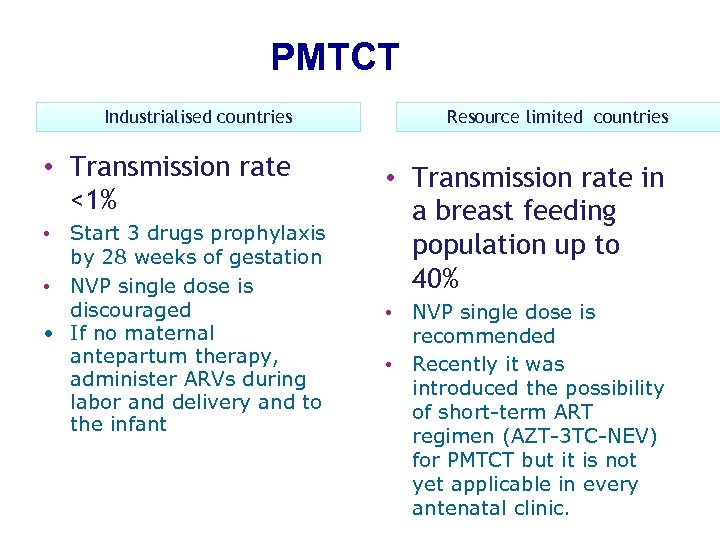
PMTCT Industrialised countries • Transmission rate <1% • Start 3 drugs prophylaxis by 28 weeks of gestation • NVP single dose is discouraged • If no maternal antepartum therapy, administer ARVs during labor and delivery and to the infant Resource limited countries • Transmission rate in a breast feeding population up to 40% • NVP single dose is recommended • Recently it was introduced the possibility of short-term ART regimen (AZT-3 TC-NEV) for PMTCT but it is not yet applicable in every antenatal clinic.
PMCTC • National guidelines for PMCTC in Tanzania suggest use of Nevirapina single-dose at labour • Recently it was introduced the possibility of short-term ART regimen (AZT-3 TC-NEV) for PMTCT but it is not yet applicable in every antenatal clinic.
CTC Usokami - Iringa (Tanzania)
Servizi offerti • • • informazione test HIV e counselling esami ematologici visite mediche distribuzione di farmaci per le infezioni opportunistiche distribuzioni di farmaci antiretrovirali distribuzione del supporto alimentare sostegno economico per il trasporto dai villaggi di residenza visita domiciliare
Scale-up of HIV/AIDS care ART delivery models • Health systems that are already struggling • Individualized medical with an absolute model vs public health shortage of qualified model health staff • “vertical” vs “horzontal” programs 45
“Task shifting” and comunity care • Physician shortage – In US 1 phy per 0. 6 PLWA – In Malawi 1 phy per 7, 400 PLWA • Programs have incorporated peripheral clinics staffed by clinical officers and nurses; mobile support teams; community members and home based care 46
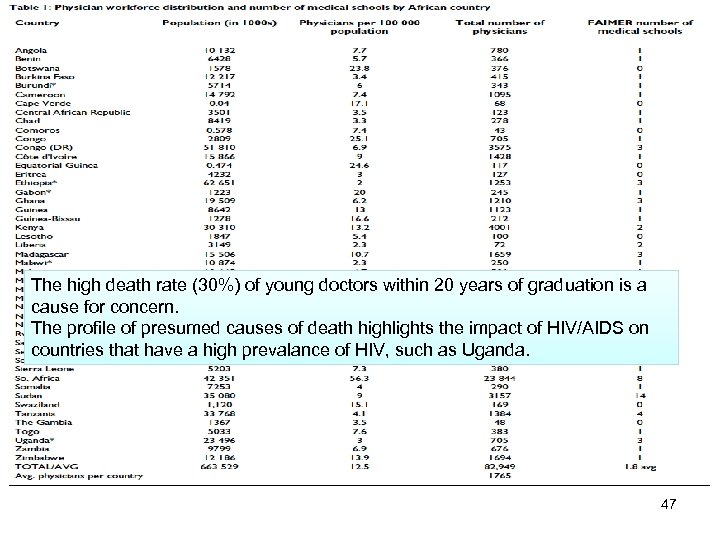
The high death rate (30%) of young doctors within 20 years of graduation is a cause for concern. The profile of presumed causes of death highlights the impact of HIV/AIDS on countries that have a high prevalance of HIV, such as Uganda. 47
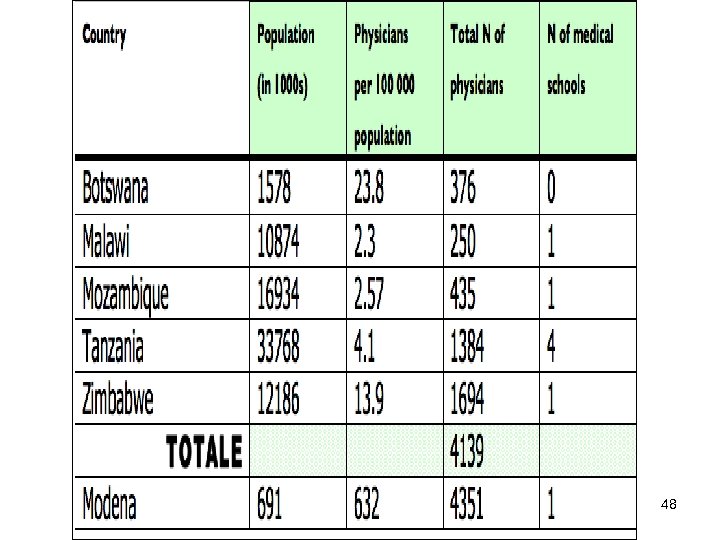
48

49
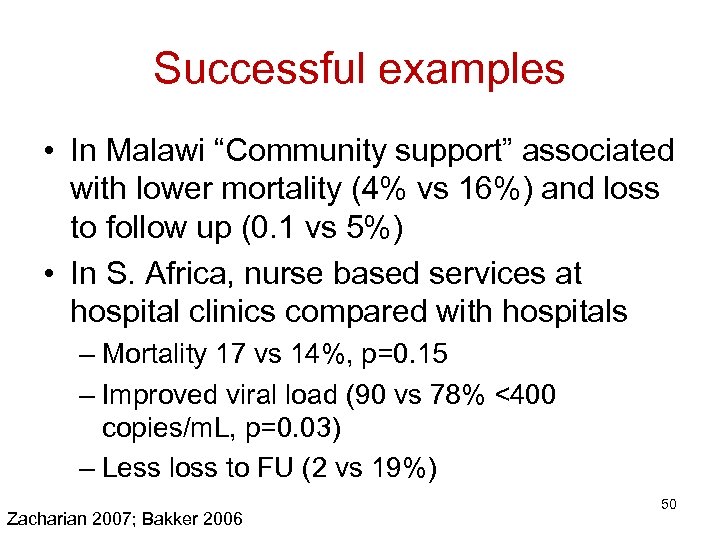
Successful examples • In Malawi “Community support” associated with lower mortality (4% vs 16%) and loss to follow up (0. 1 vs 5%) • In S. Africa, nurse based services at hospital clinics compared with hospitals – Mortality 17 vs 14%, p=0. 15 – Improved viral load (90 vs 78% <400 copies/m. L, p=0. 03) – Less loss to FU (2 vs 19%) Zacharian 2007; Bakker 2006 50
Examples of HIV/AIDS activities, including ART, held by community participation • Management of opportunistic infections • Recognition and referral of individuals with ‘risk signs’ to community nurses or hospital • Adherence counselling • Counselling on drug reactions and early referral • Defaulter tracing • Nutritional support • Community mobilization centers and community farms • Vocational training and income generation activities for HIV/AIDS orphans • Pre-school activities for HIV/AIDS orphans <5 years • Information, education and communication /behavior change • interventions 51
c3a68d12816333f9ddc30f5bb17faa33.ppt