e28d4b7d448e6ba4f25adb4c157282f5.ppt
- Количество слайдов: 83
CNS Infections Mazin Barry, MD, FRCPC, FACP, DTM&H Assistant Professor and Consultant Division of Infectious Diseases King Saud University

Meningitis
Learning Objectives • Be familiar with clinical presentation of disease • Appreciate different causative organisms • Approach to management • Utilization of antimicrobial therapy • How to prevent disease • Role of Steroids • Case discussion
Variable causes and outcome • Acute Benign Forms of Viral Meningoencephalitis • Rapidly Fatal Bacterial Meningitis with Local Progressive mental deterioration and death • Different etiological organisms • Time of starting appropriate therapy
Definitions • Meningitis – inflammation of the meninges • Encephalitis – infection of the brain parenchyma • Meningoencephalitis – inflammation of brain + meninges • Aseptic meningitis – inflammation of meninges with sterile CSF • Meninges?

Meninges • Meningitis: inflammation of the pia mater and the arachnoid mater, with suppuration of the cerebrospinal fluid

CAUSES OF MENINGITIS INFECTIOUS Viral NON-INFECTIOUS Aseptic Meningitis Bacteria Malignancy Mycobacterial Sarcoid Brucella behcet disease Fungal SLE
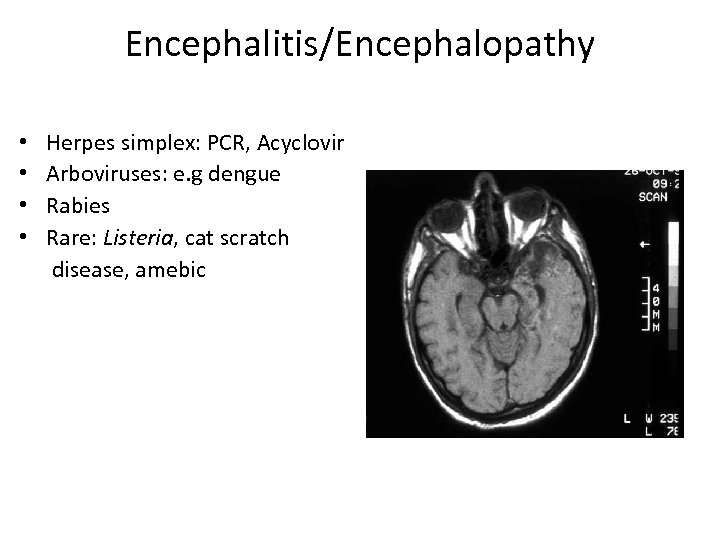
Encephalitis/Encephalopathy • • Herpes simplex: PCR, Acyclovir Arboviruses: e. g dengue Rabies Rare: Listeria, cat scratch disease, amebic
Aseptic Meningitis CSF: pleocytosis 100 s, Norm G &P, Neg Culture Enteroviruses: most common cause 80% HSV-2, and other viruses HIV Partial Rx Bacteria Drugs: MTZ, TMP-SMX, NSAIDs, carbamazapine, IVIG • Rare: leptospirosis • • •

Symptoms of Bacterial Meningitis • High grade sudden fever • Severe Headache • Altered level consciousness, irritability, photophobia • Vomiting • Seizures • Stiff neck • Bulging fontanel in infants
Signs • Vital signs: Fever • Nuchal rigidity • Kerning's sign: while patient is lying supine, with the hip and knee flexed to 90 degrees pain limits passive extension of the knee • Brudzinski's sign: flexion of the neck causes involuntary flexion of the knee and hip • Papilledema • Neurological defecit • Don’t forget source of infection: ears, sinsuses, chest. . etc • Petechiae, ecchymosis

Signs • Absence of all 3 signs of the classic triad of fever, neck stiffness, and an altered mental status virtually eliminates a diagnosis of meningitis • Changes in mental status are more common in bacterial than viral meningitis • Kernig and Brudzinski signs have low sensitivity but high specificity
Most useful Sign • Jolt accentuation maneuver: ask patient to rapidly rotate his or head horizontally: Headache worsens • Sensitivity of 100%, specificity of 54%, positive likelihood ratio of 2. 2, and negative likelihood ratio of 0 for the diagnosis of meningitis JAMA July 1999 Does this adult patient have acute meningitis?

Complications Hydrocephalus Seizures SIADH Subdural effusions & empyema Septic sinus or cortical vein thrombosis Arterial ischemia / infarction (inflammatory vasculitis) CN Palsies (esp deafness) Septic shock / multi-organ failure from bacteremia (esp meningococcus & pneumococcus) • Risk of adrenal hemorrhage with hypo-adrenalism (Waterhouse-Friderichsen syndrome) • •
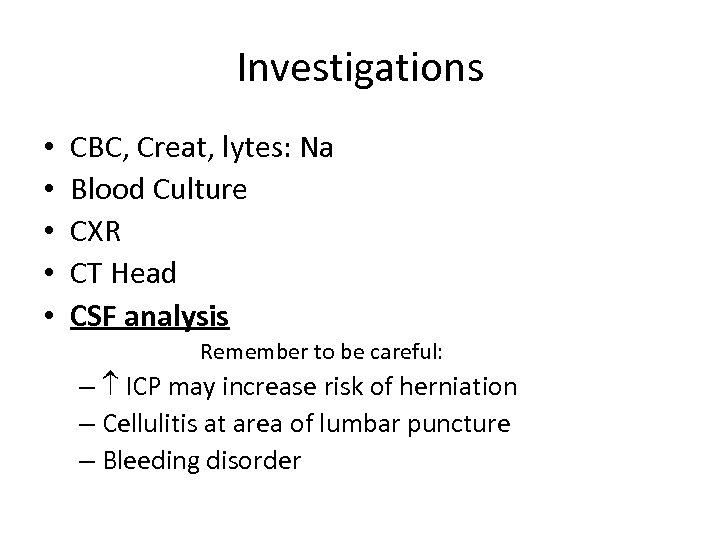
Investigations • • • CBC, Creat, lytes: Na Blood Culture CXR CT Head CSF analysis Remember to be careful: – ICP may increase risk of herniation – Cellulitis at area of lumbar puncture – Bleeding disorder
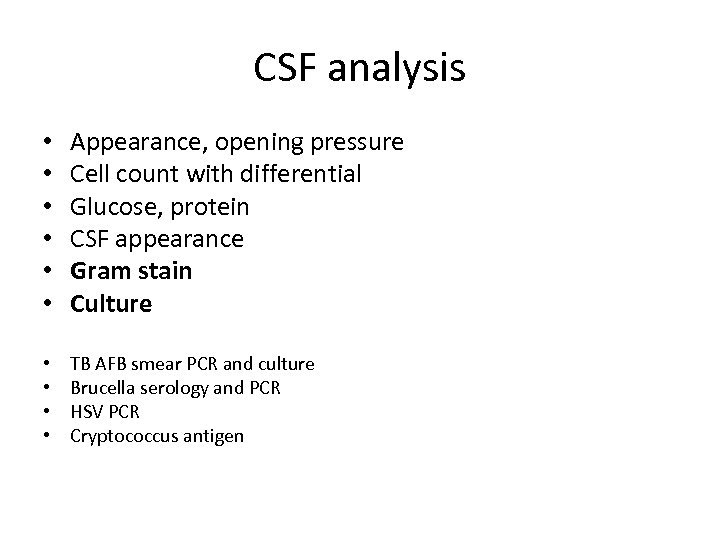
CSF analysis • • • Appearance, opening pressure Cell count with differential Glucose, protein CSF appearance Gram stain Culture • • TB AFB smear PCR and culture Brucella serology and PCR HSV PCR Cryptococcus antigen
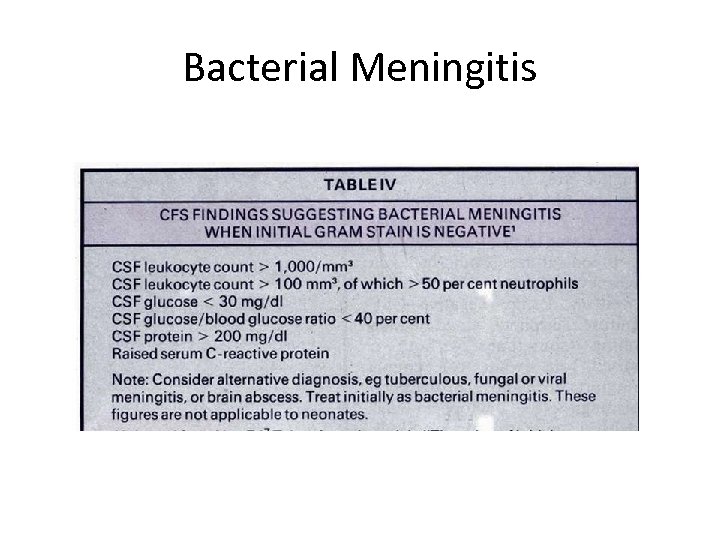
Bacterial Meningitis

Bacterial Pathogens Neonates • Group B Streptococci 49%, E coli, enterococci, Klebsiella, Enterobacter, Samonella, Serratia, Listeria Older infants and children – Neisseria meningitidis, S. pneumoniae, M. tuberculosis, H. influenzae
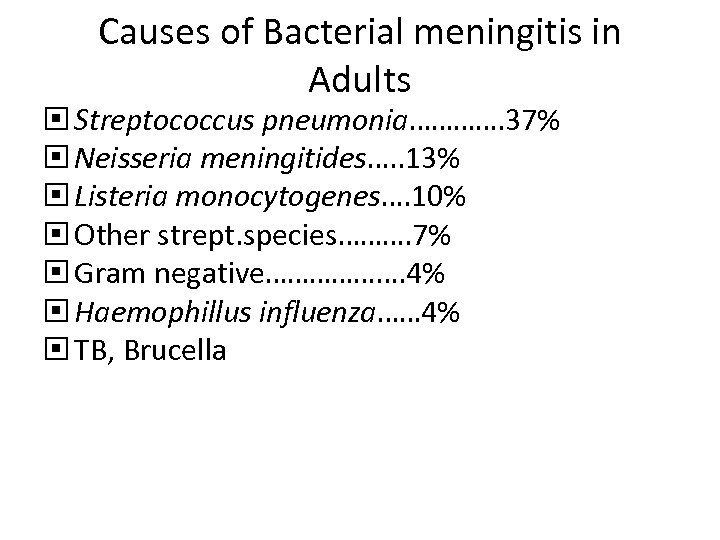
Causes of Bacterial meningitis in Adults Streptococcus pneumonia…………. 37% Neisseria meningitides…. . 13% Listeria monocytogenes…. 10% Other strept. species………. 7% Gram negative………………. 4% Haemophillus influenza…… 4% TB, Brucella

Keep in mind • Global emergence and prevalence of Penicillin- Resistant Streptococcus pneumonia • Dramatic Reduction in invasive Hemophillus influenza disease secondary to use of conjugate Haemophillus Type Bvaccine. • Group B – Streptococci: previously in neonate, now emerging as disease of elderly

Bacterial Meningitis - Empiric Treatment (Gram stain Neg) • Remember MENINGEAL DOSES • Ceftriaxone 2 gm IV Q 12 h – High CSF levels • Vancomycin 500 -750 mg IV Q 6 h (highly penicillin resistant pneumococcus) • Dexamethasone (0. 15 mg/kg IV Q 6 h) for 2 -4 days : 1 st dose 15 -20 min prior to or concomitant with 1 st dose Abx to block TNF production • Ampicillin (for Listeria)
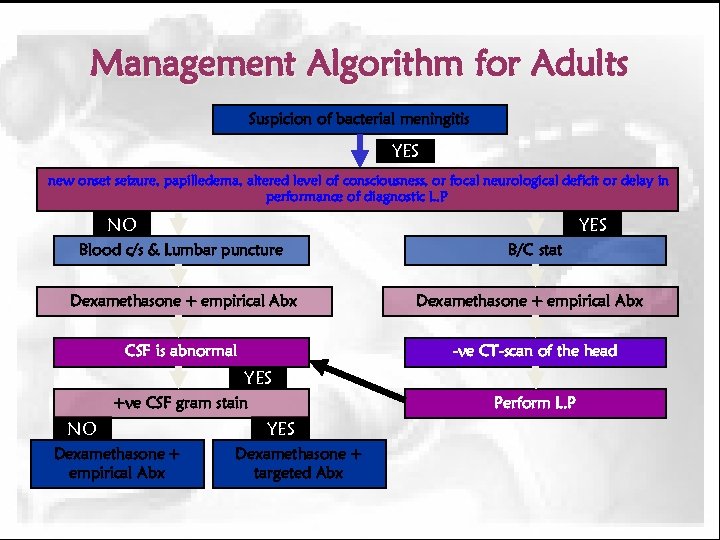
Management Algorithm for Adults Suspicion of bacterial meningitis YES new onset seizure, papilledema, altered level of consciousness, or focal neurological deficit or delay in performance of diagnostic L. P NO YES Blood c/s & Lumbar puncture Dexamethasone + empirical Abx CSF is abnormal B/C stat Dexamethasone + empirical Abx -ve CT-scan of the head YES +ve CSF gram stain NO Dexamethasone + empirical Abx Perform L. P YES Dexamethasone + targeted Abx

Case-1 • 34 years old man returning from Hajj • Fever, severe headache, neck stiffness, vomiting for two days • Found confuzed by family: ER • Temp 38. 4, HR 110, BP 100/70 • Obtunded, Nuchal rigidity, Kerning’s and brudzinski’s signs • Petechiae


Investigations • CSF examination: Opening pressure: 260 mm H 20 & cloudy WBC: 1500/ ml: 96% polymorphs Glucose: 24 mg / dl Protein: 200 mg
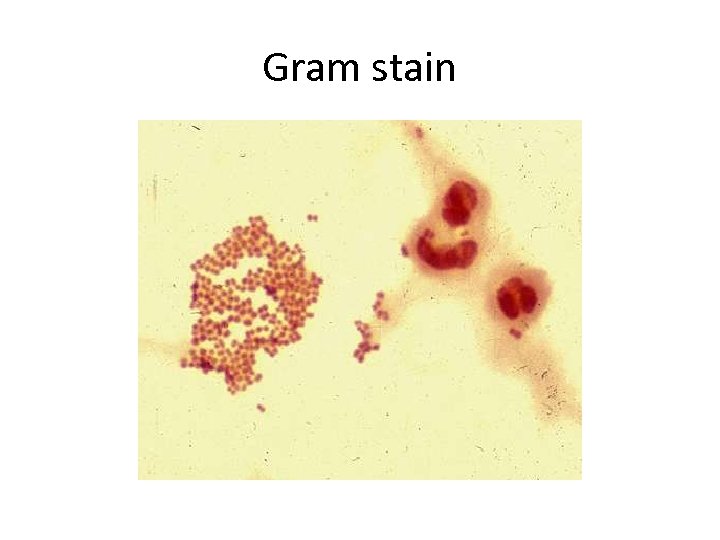
Gram stain


This led to. . • Vaccination: Pre Hajj vaccination in 90’s • serogroups A, C
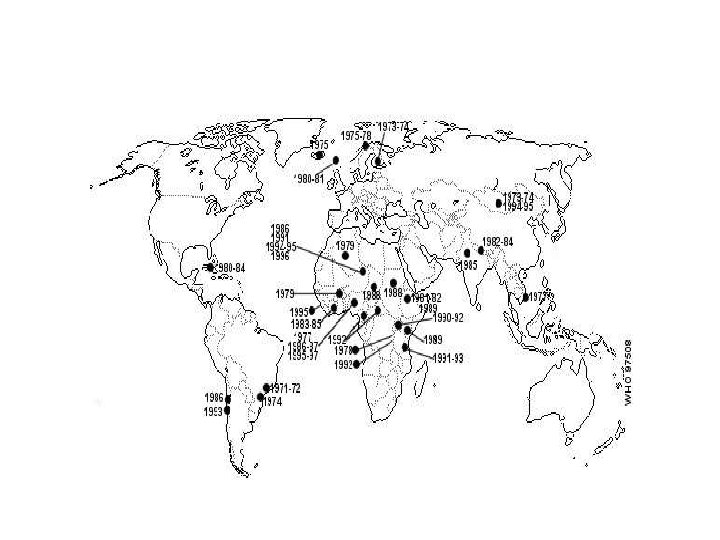
N. meningitidis W 135 & Hajj • In UK alone 2000: 45 cases 8 (18%) deaths • In 2001 34 cases 10 (29%) deaths • Pre hajj: Quadrivalent conjugate meningococcal vaccine: A, C, Y, W 135 (menactra) • Up to 3 years in adult : Does not affect nasopharyngeal carriage and does not provide herd immunity

Meningococcus • Fulminate meningococcemia with purpura: – Overwhelming sepsis, DIC • Meningitis with rash (Petechiae) • Meningitis without rash • Mortality 3 - 10 %





Treatment & Chemoprophylaxis • Droplet Isolation: 48 h post Abx • Treatment: Ceftriaxone or Pen G 7 days • Eradicate nasopharyngeal carriage: house hold contact Health care providers who examined patient closely • Rifampin 600 mg for 2 d or Ciprofloxacin 500 mg once or Ceftriaxone 125 mg I. M once
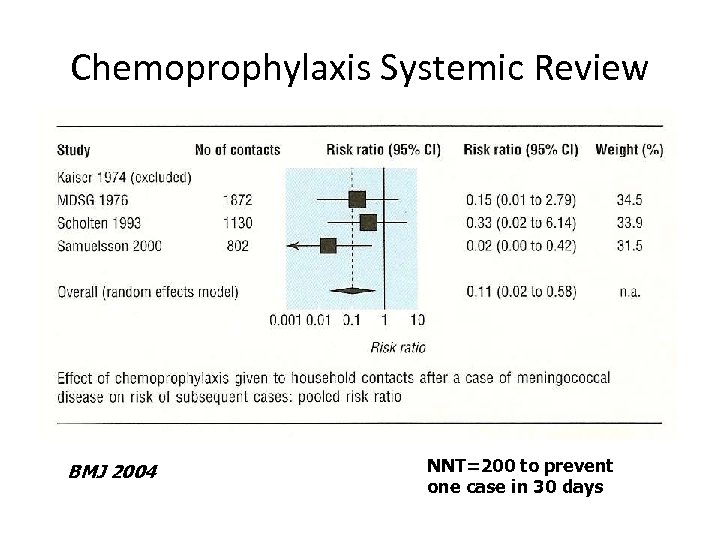
Chemoprophylaxis Systemic Review BMJ 2004 NNT=200 to prevent one case in 30 days

CASE 2 • 26 year old Saudi female presents with fever, cough and headache for the last 3 days. Examination revealed ill – looking woman with sign of consolidation over lower lungs


CASE 2 • Six hours after admission, her headache became worse and rapidly became obstunded. • CSF: WBC: 3000 : 99% PML Sugar: Zero Protein: 260 mg/dl.
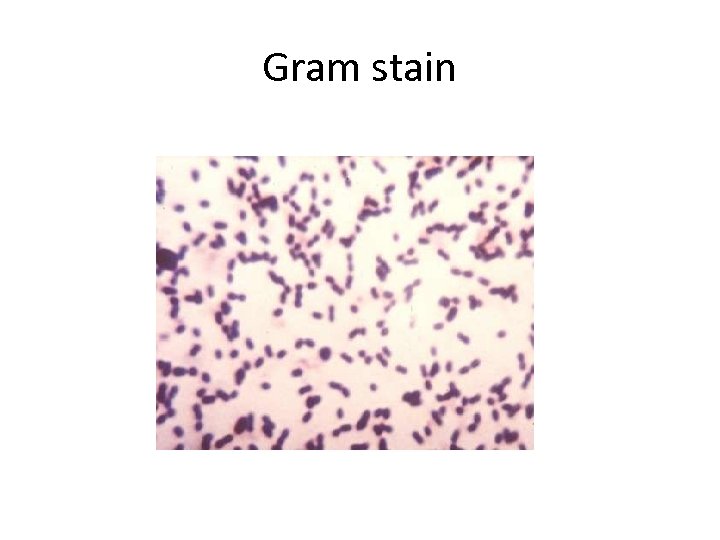
Gram stain
Epidemiological Features of Pneumococcal meningitis • The most common Cause • Highest mortality 20 – 30% • May be associated with other Focus: Pneumonia, Otitis Media, Sinusitis • Head Trauma & CSF Leak • spleenectoy and Sickle cell disease • Global emergence of Penicillin – Resistant

CSF Leak

Treatment & prevention of Pnemococcus meningitis • • • Penicillin G (MIC< 0. 1 mcg/ml) Ceftriaxone 14 days Vancomycin if Highly penicillin resistance (MIC>=2 mcg/ml) Steroids (pre Abx) Vaccination: – Pneumococcal conjugate vaccine (Prevnar 13): Valent conjugate vaccine for children – Pneumococcal polysaccharide vaccine (Pneumovax): 23 purified capsular polysaccharide antigens (serotypes 1, 2, 3, 4, 5, 6 B, 7 F, 8, 9 N, 9 V, 10 A, 11 A, 12 F, 14, 15 B, 17 F, 18 C, 19 A, 19 F, 20, 22 F, 23 F, and 33 F)

Treatment of Pneumococcus meningitis • Steroids (pre 1 st dose Abx) for 4 days • Pen G MIC less than 0. 1 mcg/m. L: Pen G 4 million U Q 4 h or Ampicillin 2 gm IV Q 4 h • Pen G MIC 0. 1 -1: Ceftriaxone 2 gm IV Q 12 h • Pen G Equal to or more than 2: vanco 500750 mg IV Q 6 h and ceftriaxone

S. Pneumonia Prevention • Pneumococcal conjugate vaccine (PCV) is a vaccine used to protect infants and young children – 13 serotypes of Streptococcus – Prevnar 13® is a vaccine approved for children 6 weeks through 17 years of age for the prevention of invasive disease caused by 13 Streptococcus pneumoniae strains (1, 3, 4, 5, 6 A, 6 B, 7 F, 9 V, 14, 18 C, 19 A, 19 F, and 23 F), and for children 6 weeks through 5 years for the prevention of otitis media caused by 7 of the 13 strains (4, 6 B, 9 V, 14, 18 C, 19 F, and 23 F) Based upon immune responses to the vaccine, Prevnar 13® is also approved for adults 50 years of age and older for the prevention of pneumococcal pneumonia and invasive disease caused by the 13 vaccine strains Prevnar 13® is not 100% effective and will only help protect against the 13 strains included in the vaccine
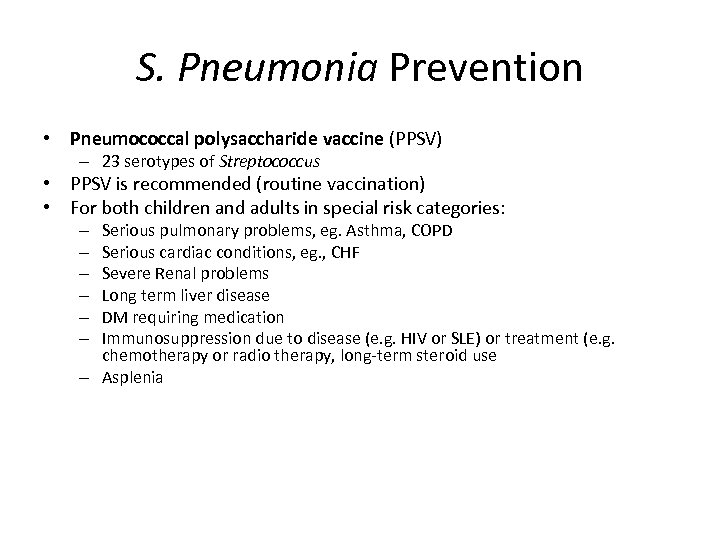
S. Pneumonia Prevention • Pneumococcal polysaccharide vaccine (PPSV) – 23 serotypes of Streptococcus • PPSV is recommended (routine vaccination) • For both children and adults in special risk categories: Serious pulmonary problems, eg. Asthma, COPD Serious cardiac conditions, eg. , CHF Severe Renal problems Long term liver disease DM requiring medication Immunosuppression due to disease (e. g. HIV or SLE) or treatment (e. g. chemotherapy or radio therapy, long-term steroid use – Asplenia – – –

Lancet review 2004

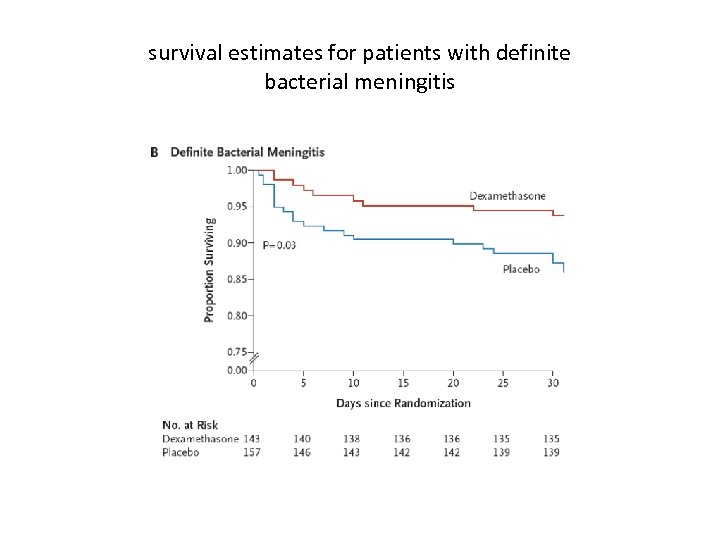
survival estimates for patients with definite bacterial meningitis
Case 3 • 70 year old man with malaise, anorexia loss of weight of 7 kg over 1 month • Underwent Colonoscopy prior to symptoms onset • Watery diarrhea 4 times a day for 1 wk • Fever, chills and headache for 3 days • Double vision for 2 days • Neck stiffness, jolt accentuation, 6 th CN palsy

CSF • Cloudy • WBC: 1000 70% lymphocytes Glucose: 50 mg / dl Protein: 170 mg

Gram Stain

Listeria Monocytogenes • Risk groups: age <1 y or >50 y Alcoholics pregnancy: up to 30% immunocopromised 70 % • Routes of transmission: *mainly food borne *transplacental /vertical *Cross contamination(nursery) *inoculation(skin) farmers *colo/ sigmoidoscopy bacteremia / meningitis ( up to 5% healthy : N flora)

Listeria Monocytogenes Meningitis Treatment • Ampicillin 2 gm IV Q 4 h +/- Gentamicin 2 mg/kg loading dose then 1. 7 mg/kg Q 8 h • 21 day duration • Penicillin allergy patients: TMP-SMX or Meropenem
Case 4 • 56 year old Indian man presented to the infectious disease clinic with low grade fever and night sweats for 6 wks and headache for 4 wks • T: 38. 2 C, speaking well • Opthalmoplegia • Neck stiffnes. . bilateral papillodema


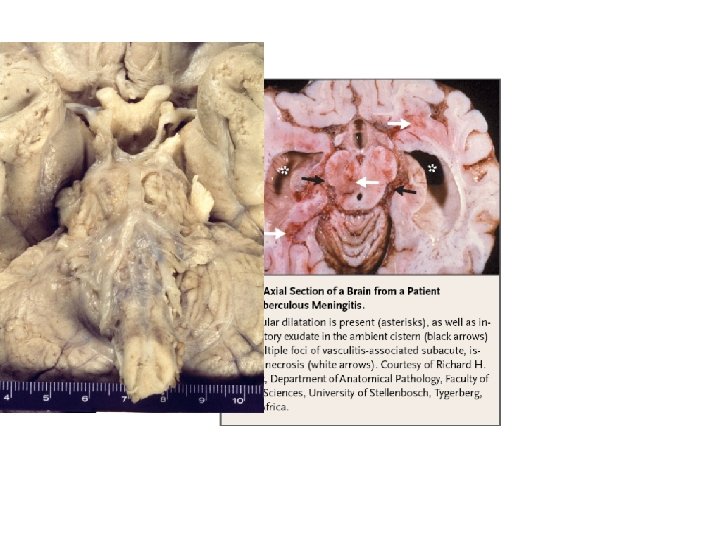
LABORATORY RESULTS. . • CSF: xanthocromic wbc 340 L: 85 % protein 1. 5 g sugar 25 mg
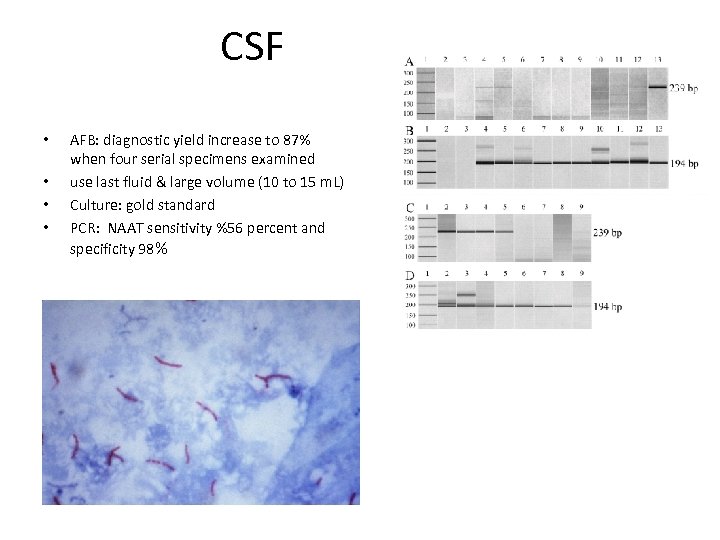
CSF • • AFB: diagnostic yield increase to 87% when four serial specimens examined use last fluid & large volume (10 to 15 m. L) Culture: gold standard PCR: NAAT sensitivity %56 percent and specificity 98%

www. aic. cuhk. edu. hk/web 8/TB-meningitis. htm

Antibiotic Chemotherapy CSF concentrations: • INH, Pyrazinamidine, pass freely into the CSF • Rif has 10% the concentration as in Plasma • Streptomycin or ethionamide do not pass BBB in absence of inflammation. *Supplemental Pyrodoxine with INH Therapy

Dexamethasone in TB meningitis • 545 pt were randomly assigned to groups that received either dexamethasone (274 pt) or placebo (271 pt) • Dexamethasone was started as soon as possible after the start of antituberculosis treatment

Dexamethasone in TB meningitis • Grad I: GCS 15 no focal deficit, Grade II: GCS 1114 or A deficit, Grade III GCS <10 • Grade I • Patients with grade I disease received two weeks of intravenous therapy • 0. 3 mg per kilogram per day for week 1 • 0. 2 mg per kilogram per day for week 2 • 4 weeks of oral therapy (0. 1 mg per kilogram per day for week 3, then a total of 3 mg per day, decreasing by 1 mg each week)
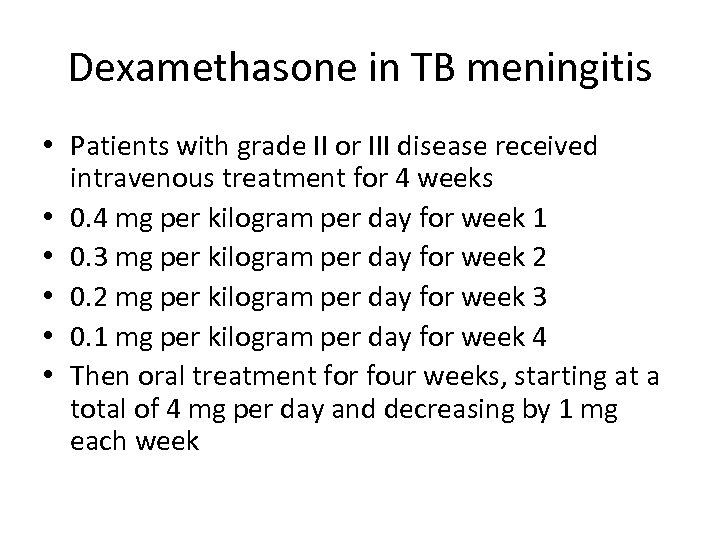
Dexamethasone in TB meningitis • Patients with grade II or III disease received intravenous treatment for 4 weeks • 0. 4 mg per kilogram per day for week 1 • 0. 3 mg per kilogram per day for week 2 • 0. 2 mg per kilogram per day for week 3 • 0. 1 mg per kilogram per day for week 4 • Then oral treatment for four weeks, starting at a total of 4 mg per day and decreasing by 1 mg each week


Steroids in TB meningitis • Treatment with dexamethasone is associated with a reduced risk of death (relative risk, 0. 69; 95% CI, 0. 52 to 0. 92; P=0. 01)

Case 5 • 30 yo Saudi sheep herder with 3 weeks headache blurred vision • Looks uncomfortable, Temp 38. 1 • Jolt accentuation present
Case 5 • • • CSF pleocytosis 105 mostly lymphocytes Blood culture grew Brucella sp Brucella titre 1: 320 Brucella PCR in CSF poistive Treatement: Doxycycline, Rifampin, TMP-SMX
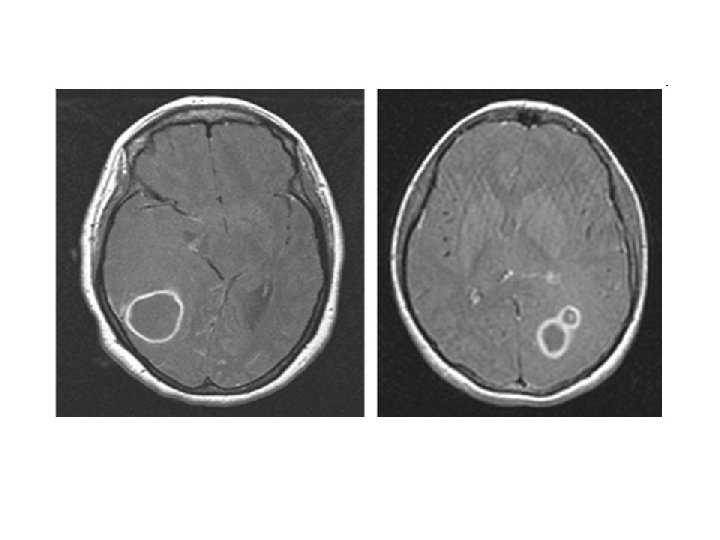
Case 6 • 32 HIV poistive gentleman with 3 weeks history of forgetfulness change in personality • Presents with generalized seizure to ER • After ABC and stabilization CT done

Case 6 • • CD 4: 77, VL 1 340 324 Toxoplasma Ig. G poitive Brain Bx: Toxplasma Gondii Pyrimethamine + sulfadiazine + folinic acid
Case 7 • • 46 gentleman with fever for 1 week Headache for 3 days Prosthetic AVR 6 years ago Fever 39. 1, Stiff neck
Case 7 • • Blood Culture: staphylococcus Aureus TEE: vegetation aortic valve Drainage of brain abscess: MSSA Treatment: Cloxacillin, flagyl

Brain Abscess • Organisms: – Streptococci (60 -70%), Bacteroides (20 -40%), Enterobacteriacea (25 -33%), S. Aureus (10 -15%), S. Milleri. – Rare: Nocardia, Listeria • CT brain: If abscess more than 2. 5 cm then surgical drainage. And if patient neurologically unstable or decrease LOC drain regardless of size • Antimicrobials: empirically Ceftriaxone with metronidazole, otherwise according to susceptability • Duration untill response by nueroimaging
Subdural Empyema • In adults 60 -90% are extension of: – Sinusitis – Otitis media • Surgical emergency: must drain • Abx same as brain abscess
Case 4 • Treatment: Doxycycline, Rifampin, TMP-SMX • Many weeks till CSF parameters normalize
e28d4b7d448e6ba4f25adb4c157282f5.ppt