87c5465b207bfd665eb265fe9177caf4.ppt
- Количество слайдов: 12
 CMS-Minnesota Federal State Partnership to Align Administrative Functions for Improvements in Medicare Medicaid Beneficiary Experience Pamela Parker, MPA Special Needs Purchasing Minnesota Department of Human Services Pam. parker@state. mn. us 651 -431 -2512
CMS-Minnesota Federal State Partnership to Align Administrative Functions for Improvements in Medicare Medicaid Beneficiary Experience Pamela Parker, MPA Special Needs Purchasing Minnesota Department of Human Services Pam. parker@state. mn. us 651 -431 -2512
 Medicaid Managed Care in Minnesota • Medicaid managed care since 1985 including dual seniors (700, 000 total enrollment) • 1995: First approved state Medicare/Medicaid demonstration (MSHO) • 2005 -2006: Expanded MSHO Medicare/Medicaid MLTSS program statewide through contracts with 8 D-SNPs • 90% (49, 000) Medicaid seniors enrolled in MLTSS (programs enroll all settings and levels of care) under two options: – Minnesota Senior. Care Plus (MSC+): 13, 000 enrollees (coordinates Medicare, enrollment mandatory) – Minnesota Senior Health Options (MSHO): 36, 000 enrollees (integrates Medicare, enrollment voluntary) 2
Medicaid Managed Care in Minnesota • Medicaid managed care since 1985 including dual seniors (700, 000 total enrollment) • 1995: First approved state Medicare/Medicaid demonstration (MSHO) • 2005 -2006: Expanded MSHO Medicare/Medicaid MLTSS program statewide through contracts with 8 D-SNPs • 90% (49, 000) Medicaid seniors enrolled in MLTSS (programs enroll all settings and levels of care) under two options: – Minnesota Senior. Care Plus (MSC+): 13, 000 enrollees (coordinates Medicare, enrollment mandatory) – Minnesota Senior Health Options (MSHO): 36, 000 enrollees (integrates Medicare, enrollment voluntary) 2
 Minnesota: Why Not FAD? • One of the 15 Original Demo States, not limited to FAD options • Extensive stakeholder involvement • Submitted FAD proposal (with caveats), withdrew with CMS support • After analysis, FAD was not the best option: – MSHO operating for almost 18 years, already reduced utilization – MN had already rebalanced MLTSS system, savings expanded community based services – Actuarial analysis showed reduced revenues under FAD, generally low benchmark state, plans all must buy down Part D, need rural “floor” to operate – Potential disruptions to enrollee care coordination and access to already meager additional benefits – Most savings would go to CMS, State might not capture legislatively expected Medicaid savings under future initiatives 3 – Many FAD features already similar to current operations, others
Minnesota: Why Not FAD? • One of the 15 Original Demo States, not limited to FAD options • Extensive stakeholder involvement • Submitted FAD proposal (with caveats), withdrew with CMS support • After analysis, FAD was not the best option: – MSHO operating for almost 18 years, already reduced utilization – MN had already rebalanced MLTSS system, savings expanded community based services – Actuarial analysis showed reduced revenues under FAD, generally low benchmark state, plans all must buy down Part D, need rural “floor” to operate – Potential disruptions to enrollee care coordination and access to already meager additional benefits – Most savings would go to CMS, State might not capture legislatively expected Medicaid savings under future initiatives 3 – Many FAD features already similar to current operations, others
 Challenges Under SNP “World” • No “seat at the table” for States with Medicare to resolve new or ongoing conflicts or to work toward further alignment/efficiencies • Needed clarification of Medicare inclusion in State payment and delivery reforms • No clear authority for many integrated features – Integrated benefit determinations – Integrated provider billing and claims processing – Integrated enrollments (State TPA role) – Need for clarification of integrated member materials – 30 day difference in time allowed for submission for grievance and appeals – Integrated assessments and care coordination – Separate Medicare and Medicaid requirements for QA QIPs/PIPs/CCIPs, etc • Growing number of incidents threatened operational integration, e. g: – Disapproval of all MIPPA contracts in 2012 with no indication to 4 State of CMS clarification/change in policy interpretation
Challenges Under SNP “World” • No “seat at the table” for States with Medicare to resolve new or ongoing conflicts or to work toward further alignment/efficiencies • Needed clarification of Medicare inclusion in State payment and delivery reforms • No clear authority for many integrated features – Integrated benefit determinations – Integrated provider billing and claims processing – Integrated enrollments (State TPA role) – Need for clarification of integrated member materials – 30 day difference in time allowed for submission for grievance and appeals – Integrated assessments and care coordination – Separate Medicare and Medicaid requirements for QA QIPs/PIPs/CCIPs, etc • Growing number of incidents threatened operational integration, e. g: – Disapproval of all MIPPA contracts in 2012 with no indication to 4 State of CMS clarification/change in policy interpretation
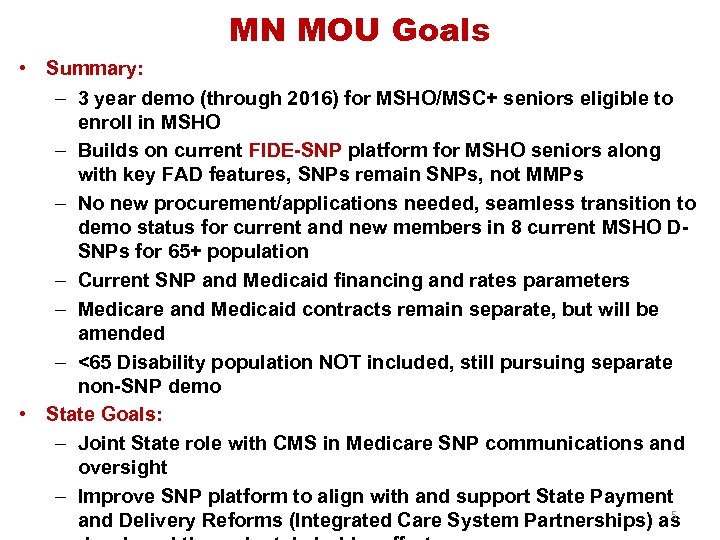 MN MOU Goals • Summary: – 3 year demo (through 2016) for MSHO/MSC+ seniors eligible to enroll in MSHO – Builds on current FIDE-SNP platform for MSHO seniors along with key FAD features, SNPs remain SNPs, not MMPs – No new procurement/applications needed, seamless transition to demo status for current and new members in 8 current MSHO DSNPs for 65+ population – Current SNP and Medicaid financing and rates parameters – Medicare and Medicaid contracts remain separate, but will be amended – <65 Disability population NOT included, still pursuing separate non-SNP demo • State Goals: – Joint State role with CMS in Medicare SNP communications and oversight – Improve SNP platform to align with and support State Payment 5 and Delivery Reforms (Integrated Care System Partnerships) as
MN MOU Goals • Summary: – 3 year demo (through 2016) for MSHO/MSC+ seniors eligible to enroll in MSHO – Builds on current FIDE-SNP platform for MSHO seniors along with key FAD features, SNPs remain SNPs, not MMPs – No new procurement/applications needed, seamless transition to demo status for current and new members in 8 current MSHO DSNPs for 65+ population – Current SNP and Medicaid financing and rates parameters – Medicare and Medicaid contracts remain separate, but will be amended – <65 Disability population NOT included, still pursuing separate non-SNP demo • State Goals: – Joint State role with CMS in Medicare SNP communications and oversight – Improve SNP platform to align with and support State Payment 5 and Delivery Reforms (Integrated Care System Partnerships) as
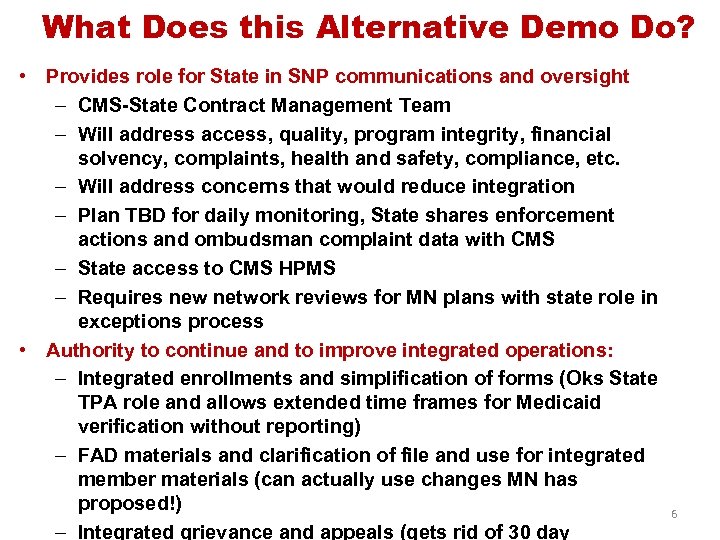 What Does this Alternative Demo Do? • Provides role for State in SNP communications and oversight – CMS-State Contract Management Team – Will address access, quality, program integrity, financial solvency, complaints, health and safety, compliance, etc. – Will address concerns that would reduce integration – Plan TBD for daily monitoring, State shares enforcement actions and ombudsman complaint data with CMS – State access to CMS HPMS – Requires new network reviews for MN plans with state role in exceptions process • Authority to continue and to improve integrated operations: – Integrated enrollments and simplification of forms (Oks State TPA role and allows extended time frames for Medicaid verification without reporting) – FAD materials and clarification of file and use for integrated member materials (can actually use changes MN has proposed!) – Integrated grievance and appeals (gets rid of 30 day 6
What Does this Alternative Demo Do? • Provides role for State in SNP communications and oversight – CMS-State Contract Management Team – Will address access, quality, program integrity, financial solvency, complaints, health and safety, compliance, etc. – Will address concerns that would reduce integration – Plan TBD for daily monitoring, State shares enforcement actions and ombudsman complaint data with CMS – State access to CMS HPMS – Requires new network reviews for MN plans with state role in exceptions process • Authority to continue and to improve integrated operations: – Integrated enrollments and simplification of forms (Oks State TPA role and allows extended time frames for Medicaid verification without reporting) – FAD materials and clarification of file and use for integrated member materials (can actually use changes MN has proposed!) – Integrated grievance and appeals (gets rid of 30 day 6
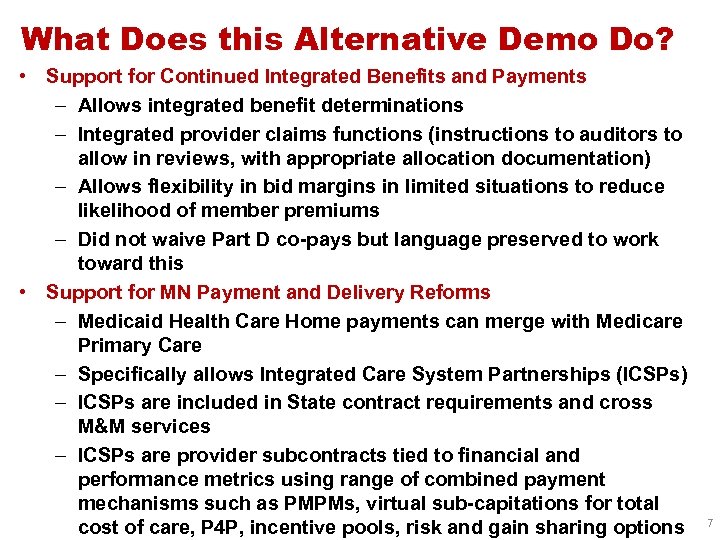 What Does this Alternative Demo Do? • Support for Continued Integrated Benefits and Payments – Allows integrated benefit determinations – Integrated provider claims functions (instructions to auditors to allow in reviews, with appropriate allocation documentation) – Allows flexibility in bid margins in limited situations to reduce likelihood of member premiums – Did not waive Part D co-pays but language preserved to work toward this • Support for MN Payment and Delivery Reforms – Medicaid Health Care Home payments can merge with Medicare Primary Care – Specifically allows Integrated Care System Partnerships (ICSPs) – ICSPs are included in State contract requirements and cross M&M services – ICSPs are provider subcontracts tied to financial and performance metrics using range of combined payment mechanisms such as PMPMs, virtual sub-capitations for total cost of care, P 4 P, incentive pools, risk and gain sharing options 7
What Does this Alternative Demo Do? • Support for Continued Integrated Benefits and Payments – Allows integrated benefit determinations – Integrated provider claims functions (instructions to auditors to allow in reviews, with appropriate allocation documentation) – Allows flexibility in bid margins in limited situations to reduce likelihood of member premiums – Did not waive Part D co-pays but language preserved to work toward this • Support for MN Payment and Delivery Reforms – Medicaid Health Care Home payments can merge with Medicare Primary Care – Specifically allows Integrated Care System Partnerships (ICSPs) – ICSPs are included in State contract requirements and cross M&M services – ICSPs are provider subcontracts tied to financial and performance metrics using range of combined payment mechanisms such as PMPMs, virtual sub-capitations for total cost of care, P 4 P, incentive pools, risk and gain sharing options 7
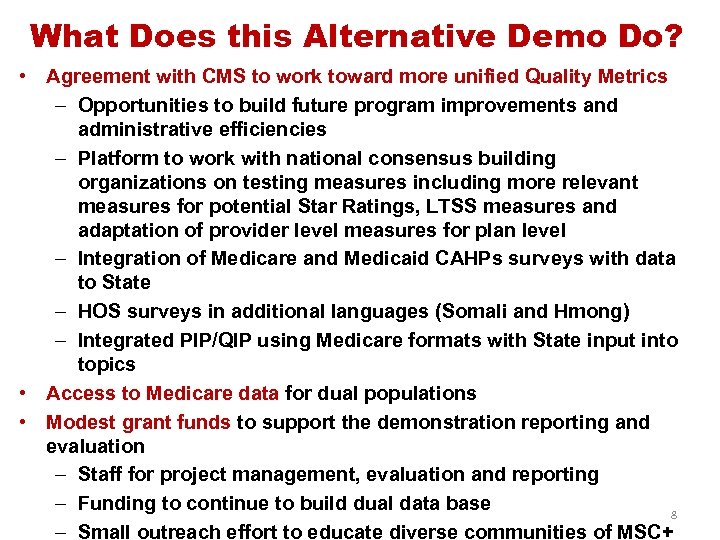 What Does this Alternative Demo Do? • Agreement with CMS to work toward more unified Quality Metrics – Opportunities to build future program improvements and administrative efficiencies – Platform to work with national consensus building organizations on testing measures including more relevant measures for potential Star Ratings, LTSS measures and adaptation of provider level measures for plan level – Integration of Medicare and Medicaid CAHPs surveys with data to State – HOS surveys in additional languages (Somali and Hmong) – Integrated PIP/QIP using Medicare formats with State input into topics • Access to Medicare data for dual populations • Modest grant funds to support the demonstration reporting and evaluation – Staff for project management, evaluation and reporting – Funding to continue to build dual data base 8 – Small outreach effort to educate diverse communities of MSC+
What Does this Alternative Demo Do? • Agreement with CMS to work toward more unified Quality Metrics – Opportunities to build future program improvements and administrative efficiencies – Platform to work with national consensus building organizations on testing measures including more relevant measures for potential Star Ratings, LTSS measures and adaptation of provider level measures for plan level – Integration of Medicare and Medicaid CAHPs surveys with data to State – HOS surveys in additional languages (Somali and Hmong) – Integrated PIP/QIP using Medicare formats with State input into topics • Access to Medicare data for dual populations • Modest grant funds to support the demonstration reporting and evaluation – Staff for project management, evaluation and reporting – Funding to continue to build dual data base 8 – Small outreach effort to educate diverse communities of MSC+
 Measurement Challenges • Multiple layers of overlapping but unaligned measures and approaches by many levels of government and research entities leads to inefficiency and lack of focus, who is in charge? • Good work by NCQA and NQF and SCAN and Commonwealth on initiatives that outline issues and recommendations for integrated programs, MLTSS and people with dual eligiblity, but proposed new measures will add even more complexity and may miss current timelines for SNPS and demos! • Overwhelming numbers of measures and extremely high expectations in short time frames for both SNPs and demos • Many current measures and accepted benchmarks are being brought over from regular Medicare Advantage or Commercial HEDIS and are not appropriate for, or exclude old-old and younger disabled or those with multiple complex conditions • There are gaps in other measures that may be needed but don’t exist or are in development (e. g. care coordination, primary care communications) • States lack resources for measurement development, but
Measurement Challenges • Multiple layers of overlapping but unaligned measures and approaches by many levels of government and research entities leads to inefficiency and lack of focus, who is in charge? • Good work by NCQA and NQF and SCAN and Commonwealth on initiatives that outline issues and recommendations for integrated programs, MLTSS and people with dual eligiblity, but proposed new measures will add even more complexity and may miss current timelines for SNPS and demos! • Overwhelming numbers of measures and extremely high expectations in short time frames for both SNPs and demos • Many current measures and accepted benchmarks are being brought over from regular Medicare Advantage or Commercial HEDIS and are not appropriate for, or exclude old-old and younger disabled or those with multiple complex conditions • There are gaps in other measures that may be needed but don’t exist or are in development (e. g. care coordination, primary care communications) • States lack resources for measurement development, but
 Measurement Challenges • Medicare data access for States is better but still highly complex and problematic • Dual populations include many smaller subpopulations with highly variable care trajectories, difficult to measure and assign benchmarks/expectations • Clinician experts point out that use of inappropriate benchmarks could be extremely harmful to those with complex co-morbid conditions • Sophisticated risk adjustment is needed for appropriate comparisons but not widely used for many measurement comparisons • Multiple levels of providers with overlapping responsibility make it difficult to assign accountability (PCP, Specialists, Rehab, S/NFs, Residential vs SNP level? ) • SNPs serving duals should not be compared to regular Medicare Advantage serving a very different population • How to balance new burdens vs new opportunity to shape 10 process?
Measurement Challenges • Medicare data access for States is better but still highly complex and problematic • Dual populations include many smaller subpopulations with highly variable care trajectories, difficult to measure and assign benchmarks/expectations • Clinician experts point out that use of inappropriate benchmarks could be extremely harmful to those with complex co-morbid conditions • Sophisticated risk adjustment is needed for appropriate comparisons but not widely used for many measurement comparisons • Multiple levels of providers with overlapping responsibility make it difficult to assign accountability (PCP, Specialists, Rehab, S/NFs, Residential vs SNP level? ) • SNPs serving duals should not be compared to regular Medicare Advantage serving a very different population • How to balance new burdens vs new opportunity to shape 10 process?
 Some Recommendations • Bring together CMS/national leaders/stakeholders or appoint a single entity to develop consensus on a “measurement work plan” across Medicare and Medicaid at all levels (legislation may be required) • Clarify and simplify sets of meaningful measures for Medicare-Medicaid, special needs and complex populations • Focus on reasonable do-able numbers of measures and scope thinking of both plan and provider levels • Clarify level of application of measures • Un-duplicate measures and approaches • Recommend subsets of measures to fit subpopulations • Develop blue prints for appropriate use of risk adjustment • Leave room for State level needs and initiatives • Layering on more measures is not the answer,
Some Recommendations • Bring together CMS/national leaders/stakeholders or appoint a single entity to develop consensus on a “measurement work plan” across Medicare and Medicaid at all levels (legislation may be required) • Clarify and simplify sets of meaningful measures for Medicare-Medicaid, special needs and complex populations • Focus on reasonable do-able numbers of measures and scope thinking of both plan and provider levels • Clarify level of application of measures • Un-duplicate measures and approaches • Recommend subsets of measures to fit subpopulations • Develop blue prints for appropriate use of risk adjustment • Leave room for State level needs and initiatives • Layering on more measures is not the answer,
 Summary • Use MN experience and MOU to explore pathways toward continued CMS/SNP/State collaboration and coordination • MOU is consistent with Med. PAC recommendations to extend D-SNP authority for integrated D-SNPs • MOU is consistent with NAMD recommendations to improve coordination between States and D-SNPs • Use integrated platform with SNP partners to further payment and delivery reform at provider levels across Medicare, Medicaid, primary, acute, behavioral health and long term services and supports • Also can be testing ground for different measurement strategies • Much yet to work out with CMS work plans and processes, phased approach to implementing some features (especially around measurement) • Important to be part of the demo process, v. s. on outside caught in no-man’s land • Leftovers: 12 – Keep working on the 365 day issue and the waiver of Part D co-
Summary • Use MN experience and MOU to explore pathways toward continued CMS/SNP/State collaboration and coordination • MOU is consistent with Med. PAC recommendations to extend D-SNP authority for integrated D-SNPs • MOU is consistent with NAMD recommendations to improve coordination between States and D-SNPs • Use integrated platform with SNP partners to further payment and delivery reform at provider levels across Medicare, Medicaid, primary, acute, behavioral health and long term services and supports • Also can be testing ground for different measurement strategies • Much yet to work out with CMS work plans and processes, phased approach to implementing some features (especially around measurement) • Important to be part of the demo process, v. s. on outside caught in no-man’s land • Leftovers: 12 – Keep working on the 365 day issue and the waiver of Part D co-


