osteomalacia.pptx
- Количество слайдов: 25
 Clinical manifestations, diagnosis, and treatment of osteomalacia
Clinical manifestations, diagnosis, and treatment of osteomalacia
 Osteomalacia • Osteomalacia is a disorder of bone, characterized by decreased mineralization of newly formed osteoid at sites of bone turnover. • Several different disorders cause osteomalacia via mechanisms that result in – hypocalcemia, – hypophosphatemia, – or direct inhibition of the mineralization process.
Osteomalacia • Osteomalacia is a disorder of bone, characterized by decreased mineralization of newly formed osteoid at sites of bone turnover. • Several different disorders cause osteomalacia via mechanisms that result in – hypocalcemia, – hypophosphatemia, – or direct inhibition of the mineralization process.
 Clinical manifestations • Osteomalacia may be asymptomatic and present radiologically as osteopenia. • It can also produce characteristic symptoms, independently of the underlying cause, including; – diffuse bone and joint pain, – muscle weakness, – muscle spasms, cramps, – a positive Chvostek’s sign, – tingling/numbness, – and difficulty walking.
Clinical manifestations • Osteomalacia may be asymptomatic and present radiologically as osteopenia. • It can also produce characteristic symptoms, independently of the underlying cause, including; – diffuse bone and joint pain, – muscle weakness, – muscle spasms, cramps, – a positive Chvostek’s sign, – tingling/numbness, – and difficulty walking.
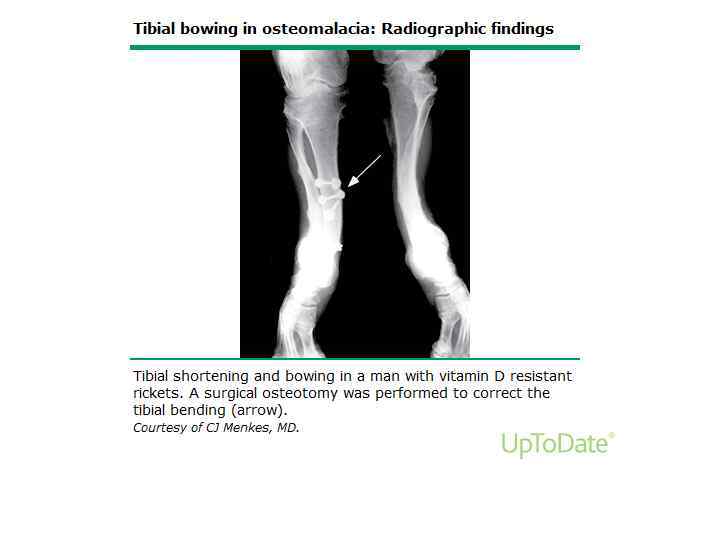
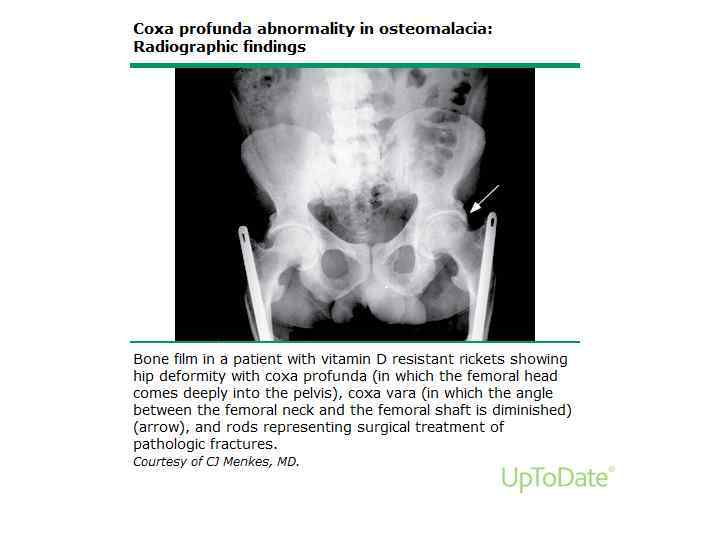
 Clinical manifestations • The pain is characterized as dull and aching and is aggravated by activity and weight bearing. • Fractures may occur with little or no trauma, typically involving the ribs, vertebrae, and long bones. • Abnormal spinal curvature or deformity of the thorax or pelvis appears only in severe osteomalacia of long duration.
Clinical manifestations • The pain is characterized as dull and aching and is aggravated by activity and weight bearing. • Fractures may occur with little or no trauma, typically involving the ribs, vertebrae, and long bones. • Abnormal spinal curvature or deformity of the thorax or pelvis appears only in severe osteomalacia of long duration.
 Clinical manifestations • The muscle weakness characteristically is proximal and may be associated with muscle wasting, hypotonia, and discomfort with movement. • There may also be a waddling gait. • It is likely that high levels of parathyroid hormone (PTH) and low levels of phosphate and calcitriol all contribute to the myopathy, since similar findings occur in primary hyperparathyroidism.
Clinical manifestations • The muscle weakness characteristically is proximal and may be associated with muscle wasting, hypotonia, and discomfort with movement. • There may also be a waddling gait. • It is likely that high levels of parathyroid hormone (PTH) and low levels of phosphate and calcitriol all contribute to the myopathy, since similar findings occur in primary hyperparathyroidism.
 Laboratory findings • Alkaline phosphatase elevated in 95 to 100 percent • Serum calcium and phosphorus reduced in 27 to 38 percent • Urinary calcium low in 87 percent • 25 -hydroxyvitamin D (calcidiol) <15 ng/m. L in 100 percent • PTH elevated in 100 percent Basha B and et al, Am J Med. 2000; Bhambri R and et al J Clin Densitom. 2006.
Laboratory findings • Alkaline phosphatase elevated in 95 to 100 percent • Serum calcium and phosphorus reduced in 27 to 38 percent • Urinary calcium low in 87 percent • 25 -hydroxyvitamin D (calcidiol) <15 ng/m. L in 100 percent • PTH elevated in 100 percent Basha B and et al, Am J Med. 2000; Bhambri R and et al J Clin Densitom. 2006.
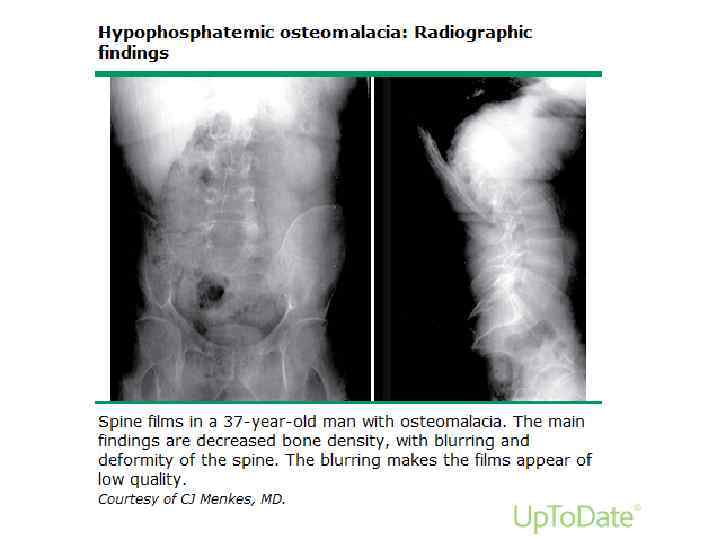
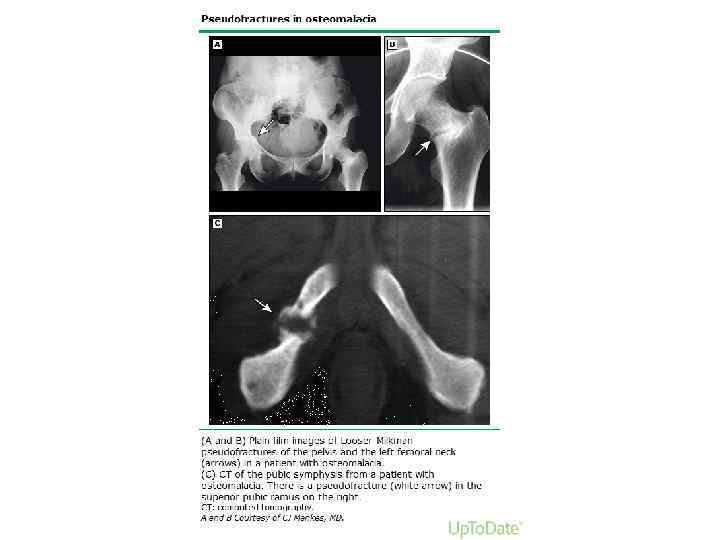
 Radiographic findings • The radiological abnormalities in adults who develop osteomalacia are less striking than those seen in children with rickets. • Reduced bone density with thinning of the cortex is the most common finding but it is very nonspecific. • More specific are changes in vertebral bodies and Looser zones. • Infrequently, radiologic evidence of secondary hyperparathyroidism can be seen (subperiosteal resorption of the phalanges, bone cysts, and resorption of the distal ends of long bones such as the clavicle and humerus).
Radiographic findings • The radiological abnormalities in adults who develop osteomalacia are less striking than those seen in children with rickets. • Reduced bone density with thinning of the cortex is the most common finding but it is very nonspecific. • More specific are changes in vertebral bodies and Looser zones. • Infrequently, radiologic evidence of secondary hyperparathyroidism can be seen (subperiosteal resorption of the phalanges, bone cysts, and resorption of the distal ends of long bones such as the clavicle and humerus).
 Bone mineral density • Several studies have demonstrated markedly reduced spine, hip, and forearm bone density (as measured by DEXA]) in patients with osteomalacia related to vitamin D deficiency. • However, bone mineral density (BMD) is not required for the diagnosis of osteomalacia, and bone mineral density (DXA) findings are unable to differentiate osteomalacia and osteoporosis.
Bone mineral density • Several studies have demonstrated markedly reduced spine, hip, and forearm bone density (as measured by DEXA]) in patients with osteomalacia related to vitamin D deficiency. • However, bone mineral density (BMD) is not required for the diagnosis of osteomalacia, and bone mineral density (DXA) findings are unable to differentiate osteomalacia and osteoporosis.
 DIAGNOSIS AND EVALUATION • Osteomalacia should be suspected in cases of bone pain associated with; – – – malabsorption, gastric bypass surgery, celiac sprue, chronic hepatic disease, or chronic kidney disease. • The diagnosis is based on a combination of; – clinical features (bone pain, tenderness, fractures, muscle weakness), – laboratory results, – radiologic findings. • Radiographs may be helpful in certain settings (eg, severe bone pain), to distinguish osteomalacia from multiple myeloma or Paget disease of bone.
DIAGNOSIS AND EVALUATION • Osteomalacia should be suspected in cases of bone pain associated with; – – – malabsorption, gastric bypass surgery, celiac sprue, chronic hepatic disease, or chronic kidney disease. • The diagnosis is based on a combination of; – clinical features (bone pain, tenderness, fractures, muscle weakness), – laboratory results, – radiologic findings. • Radiographs may be helpful in certain settings (eg, severe bone pain), to distinguish osteomalacia from multiple myeloma or Paget disease of bone.
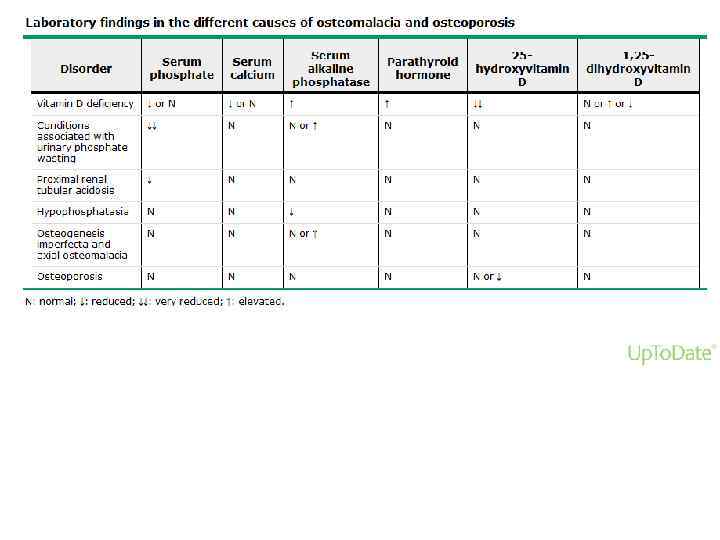
 DIAGNOSIS AND EVALUATION • Laboratory abnormalities in osteomalacia are largely dependent on its cause. • The initial laboratory evaluation should include measurement of serum concentrations of – – – – calcium, phosphate, alkaline phosphatase, 25 -hydroxyvitamin D (25 OHD), parathyroid hormone, electrolytes, blood urea nitrogen (BUN), and creatinine.
DIAGNOSIS AND EVALUATION • Laboratory abnormalities in osteomalacia are largely dependent on its cause. • The initial laboratory evaluation should include measurement of serum concentrations of – – – – calcium, phosphate, alkaline phosphatase, 25 -hydroxyvitamin D (25 OHD), parathyroid hormone, electrolytes, blood urea nitrogen (BUN), and creatinine.
 Bone biopsy • Bone biopsy with tetracycline labeling is the most accurate way to diagnose osteomalacia. • However, it is infrequently performed clinically because it is invasive and because the diagnosis can usually be made from a combination of clinical and laboratory findings.
Bone biopsy • Bone biopsy with tetracycline labeling is the most accurate way to diagnose osteomalacia. • However, it is infrequently performed clinically because it is invasive and because the diagnosis can usually be made from a combination of clinical and laboratory findings.
 DIFFERENTIAL DIAGNOSIS • Other causes of bone fractures, bone pain, and reduced bone mineral density (BMD) include; – osteoporosis, – malignancy, – Paget’s disease, – and hyperparathyroidism. • Most of these diagnoses can be distinguished from osteomalacia by the clinical history, physical examination, and a combination of laboratory and radiologic studies.
DIFFERENTIAL DIAGNOSIS • Other causes of bone fractures, bone pain, and reduced bone mineral density (BMD) include; – osteoporosis, – malignancy, – Paget’s disease, – and hyperparathyroidism. • Most of these diagnoses can be distinguished from osteomalacia by the clinical history, physical examination, and a combination of laboratory and radiologic studies.
 TREATMENT • The treatment of osteomalacia should be directed at reversal of the underlying disorder, if possible, and correction of – hypophosphatemia, – hypocalcemia, – and vitamin D deficiency.
TREATMENT • The treatment of osteomalacia should be directed at reversal of the underlying disorder, if possible, and correction of – hypophosphatemia, – hypocalcemia, – and vitamin D deficiency.
 Vitamin D deficiency • Vitamin D supplementation in patients who are deficient in this hormone leads to a dramatic improvement in muscle strength and bone tenderness within weeks. • Bone density may improve within three to six months. • Vitamin D, rather than its metabolites, is used when possible since the cost is modest. • Vitamin D metabolites are required when there is abnormal vitamin D metabolism (liver or renal disease).
Vitamin D deficiency • Vitamin D supplementation in patients who are deficient in this hormone leads to a dramatic improvement in muscle strength and bone tenderness within weeks. • Bone density may improve within three to six months. • Vitamin D, rather than its metabolites, is used when possible since the cost is modest. • Vitamin D metabolites are required when there is abnormal vitamin D metabolism (liver or renal disease).
 Vitamin D deficiency • The serum calcium concentration and urinary calcium excretion are monitored, initially after one month and three months, and then less frequently (every 6 to 12 months), until 24 -hour urinary calcium excretion is normal. • The serum calcium concentration is monitored to permit early detection of hypercalcemia from excessive dosing. • Serum 25 -hydroxyvitamin D should be measured approximately three to four months after initiating therapy. • The dose should be adjusted to prevent hypercalciuria or hypercalcemia. • In most cases, serum calcium and phosphate are normal after a few weeks of treatment, but alkaline phosphatase remains elevated for several months. • Healing of osteomalacia is considered to have occurred when there are increases in urinary calcium excretion and bone density. • Healing may take many months to a year and varies with the degree and duration of the deficiency.
Vitamin D deficiency • The serum calcium concentration and urinary calcium excretion are monitored, initially after one month and three months, and then less frequently (every 6 to 12 months), until 24 -hour urinary calcium excretion is normal. • The serum calcium concentration is monitored to permit early detection of hypercalcemia from excessive dosing. • Serum 25 -hydroxyvitamin D should be measured approximately three to four months after initiating therapy. • The dose should be adjusted to prevent hypercalciuria or hypercalcemia. • In most cases, serum calcium and phosphate are normal after a few weeks of treatment, but alkaline phosphatase remains elevated for several months. • Healing of osteomalacia is considered to have occurred when there are increases in urinary calcium excretion and bone density. • Healing may take many months to a year and varies with the degree and duration of the deficiency.
 Vitamin D deficiency • In addition to vitamin D supplementation, all patients should maintain a calcium intake of at least 1000 mg per day, since inadequate intake of calcium may contribute to the development of osteomalacia. • There is no standard dosing regimen for treating vitamin D deficiency. • One common approach is to treat nutritional deficiency (25 OHD <20 ng/m. L [50 nmol/L]) with 50, 000 international units (units) of vitamin D 2 or D 3 orally once per week for six to eight weeks, and then 800 units of vitamin D 3 daily thereafter.
Vitamin D deficiency • In addition to vitamin D supplementation, all patients should maintain a calcium intake of at least 1000 mg per day, since inadequate intake of calcium may contribute to the development of osteomalacia. • There is no standard dosing regimen for treating vitamin D deficiency. • One common approach is to treat nutritional deficiency (25 OHD <20 ng/m. L [50 nmol/L]) with 50, 000 international units (units) of vitamin D 2 or D 3 orally once per week for six to eight weeks, and then 800 units of vitamin D 3 daily thereafter.
 Vitamin D deficiency • In malabsorptive states; 10, 000 to 50, 000 units daily may be necessary to replete as in patients with gastric bypass or malabsorption. • In liver disease, the vitamin D metabolite, calcidiol (25 -hydroxyvitamin D), should be used because it does not require hepatic 25 hydroxylation. • The dose in this situation is 50 to 200 micrograms/day.
Vitamin D deficiency • In malabsorptive states; 10, 000 to 50, 000 units daily may be necessary to replete as in patients with gastric bypass or malabsorption. • In liver disease, the vitamin D metabolite, calcidiol (25 -hydroxyvitamin D), should be used because it does not require hepatic 25 hydroxylation. • The dose in this situation is 50 to 200 micrograms/day.
 Vitamin D deficiency • Calcitriol (1, 25 -dihydroxyvitamin D) is a vitamin D metabolite available in capsules of 0. 25 and 0. 5 micrograms. • It has a rapid onset of action and the half-life is only six hours. • It is associated with a fairly high incidence of hypercalcemia and patients should be followed carefully. • It is most useful in those with decreased synthesis of calcitriol, as occurs in chronic renal failure or in type 1 vitamin D-dependent rickets
Vitamin D deficiency • Calcitriol (1, 25 -dihydroxyvitamin D) is a vitamin D metabolite available in capsules of 0. 25 and 0. 5 micrograms. • It has a rapid onset of action and the half-life is only six hours. • It is associated with a fairly high incidence of hypercalcemia and patients should be followed carefully. • It is most useful in those with decreased synthesis of calcitriol, as occurs in chronic renal failure or in type 1 vitamin D-dependent rickets
 Other Causes • Hereditary hypophosphatemic rickets is treated with a combination of phosphate supplementation and calcitriol. • Tumor-induced osteomalacia is treated similarly until the causative tumor can be removed, or indefinitely if tumor removal is not possible. • In renal insufficiency, both oral and intravenous calcitriol can be used. • Osteomalacia of renal tubular acidosis is treated initially with 5000 to 10, 000 units per day of vitamin D. The acidosis is corrected with sodium and/or potassium citrate. Once the bone heals, supraphysiologic doses of vitamin D (above 800 units/day) should not be necessary. • For hypophosphatasia or the rare skeletal disorders of defective bone matrix (axial osteomalacia and fibrogenesis imperfecta), there are no established therapies.
Other Causes • Hereditary hypophosphatemic rickets is treated with a combination of phosphate supplementation and calcitriol. • Tumor-induced osteomalacia is treated similarly until the causative tumor can be removed, or indefinitely if tumor removal is not possible. • In renal insufficiency, both oral and intravenous calcitriol can be used. • Osteomalacia of renal tubular acidosis is treated initially with 5000 to 10, 000 units per day of vitamin D. The acidosis is corrected with sodium and/or potassium citrate. Once the bone heals, supraphysiologic doses of vitamin D (above 800 units/day) should not be necessary. • For hypophosphatasia or the rare skeletal disorders of defective bone matrix (axial osteomalacia and fibrogenesis imperfecta), there are no established therapies.



