a73d6ec29bd3cbc2b4afacd593cad651.ppt
- Количество слайдов: 30
Clinical Laboratory Improvement Amendments of 1988 ( CLIA ’ 88 ) n Federal regulations which govern test results that are used to assess a patient’s condition or make a clinical decision about the patient n CLIA’ 88 classifies tests depending upon complexity as: high, moderate, provider-performed microscopy, or waived n A CLIA Certificate of Waiver is required for labs performing only waived testing
Waived Tests Waived tests include test systems cleared by the FDA for home use and those tests approved for waiver under CLIA criteria. CLIA requires that waived tests must be simple and have a low risk for erroneous results. This does not mean that waived tests are completely error-proof. They should be performed correctly
Testing Oversight n CLIA does not specify requirements for directors of laboratories with a Certificate of Waiver ( some states require a physician ) n The person whose name appears on the CLIA Certificate as the Medical Director is responsible for testing oversight and decision making.
Medical Director or Designee Responsibilities n Ensure appropriate preparation prior to testing, i. e. patient ID, collection and handling n Identify staff responsible for performing and supervising testing. n Ensure staff are trained in each test they perform, aspects of safety, and QC prior to reporting test results n Ensure periodic evaluation of competency Especially important since no specific degree or certification is required and turnover rates are high
Medical Director or Designee Responsibilities: n Establish written policies and procedures for waived testing n Make decisions on how the test results are used and when follow up testing is required n Approve policies before a test is put in place n Review and approve policies every 3 years or more often if changes are made
Importance of Getting it Right! Consider this: n Waived tests are used to adjust medication doses, i. e. anticoagulant therapy n Pregnancy test prior to undergoing radiology tests n Glucose monitoring in diabetic patients
Importance of Preanalytical Processes n Preanalytical errors are the main cause of laboratory errors n Why? Human factor Difficult to detect and correct
Focus on Prevention! n Standardize processes & understand variables, i. e. : Two patient identifiers Use dedicated staff for collection Correct order of draw Methods to prevent hemolysis
Two Patient Identifiers n Two patient identifiers are used when collecting blood or other samples for clinical testing n Two patient identifiers are used when providing other treatments or procedures n The patient’s physical location is not used as an identifier n Containers used for blood and other specimens are labeled in the presence of the patient Ref: Joint Commission, camlab, 2007
Methods to prevent hemolysis n Appropriate needle bore n Remove the tourniquet as soon as possible n Allow alcohol to dry n Avoid vigorous mixing or shaking n Avoid prolonged contact of serum or plasma with cells
Staff Training and Periodic Competencies n Staff identified by name or job description n Staff trained for each test they are authorized to perform including performance of quality control n Staff trained on the use of each instrument operation, calibration and maintenance
Waived Policy Highlights POLICY: n Waivered laboratory procedures (as defined by the Clinical Laboratory Improvement Amendment of 1988) may be performed by certified personnel with the guidance and assistance of the Medical Director of the lab or designee or may be performed by RMAs, Certified Phlebotomists who have been authorized to perform the tests
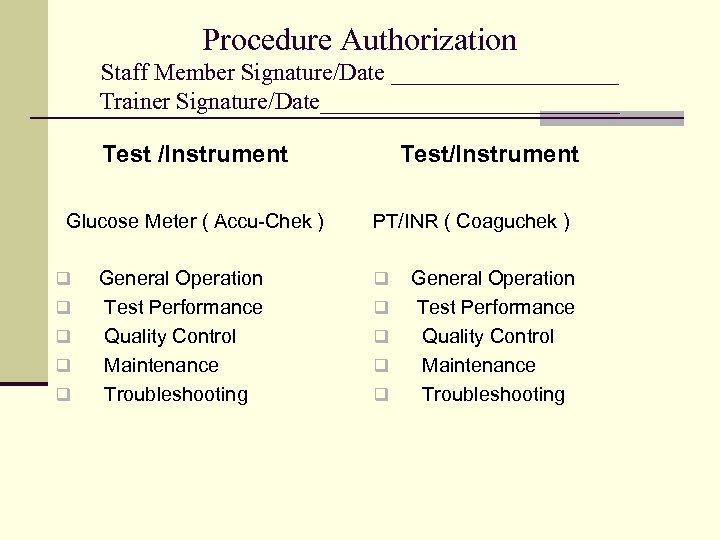
Procedure Authorization Staff Member Signature/Date __________ Trainer Signature/Date_____________ Test /Instrument Test/Instrument Glucose Meter ( Accu-Chek ) PT/INR ( Coaguchek ) q General Operation q Test Performance q Quality Control q Maintenance q Troubleshooting
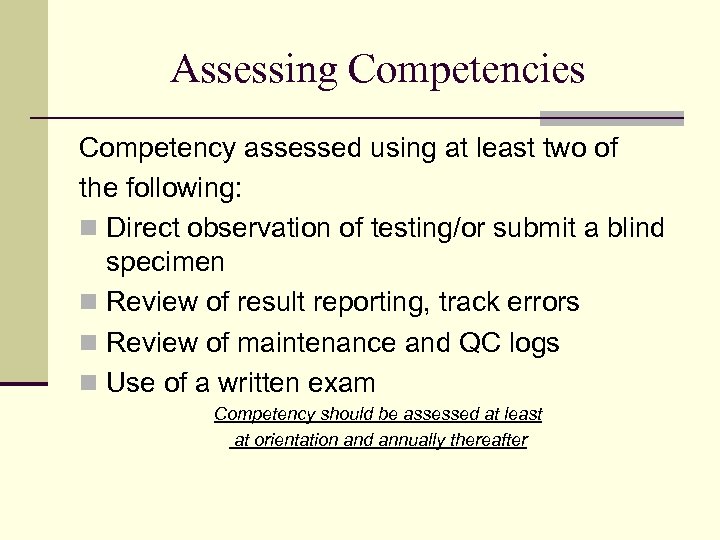
Assessing Competencies Competency assessed using at least two of the following: n Direct observation of testing/or submit a blind specimen n Review of result reporting, track errors n Review of maintenance and QC logs n Use of a written exam Competency should be assessed at least at orientation and annually thereafter
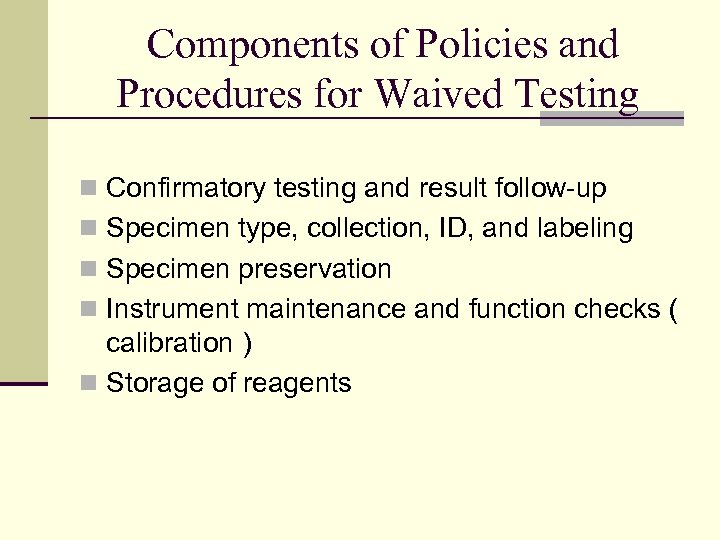
Components of Policies and Procedures for Waived Testing n Confirmatory testing and result follow-up n Specimen type, collection, ID, and labeling n Specimen preservation n Instrument maintenance and function checks ( calibration ) n Storage of reagents
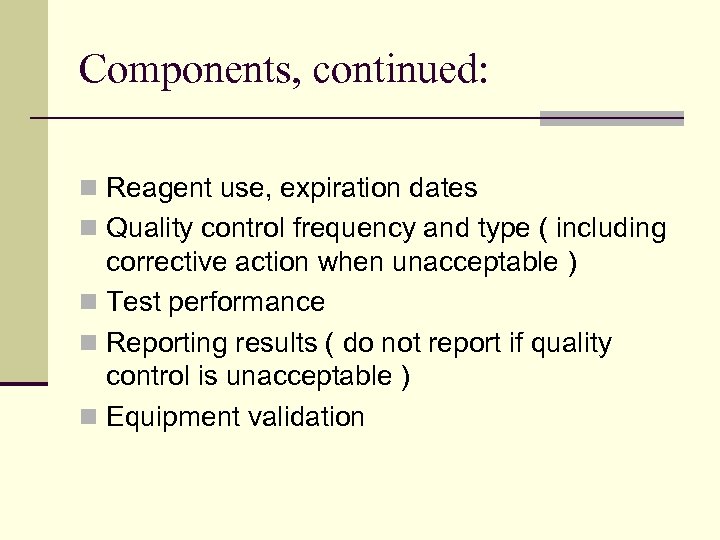
Components, continued: n Reagent use, expiration dates n Quality control frequency and type ( including corrective action when unacceptable ) n Test performance n Reporting results ( do not report if quality control is unacceptable ) n Equipment validation
Waived Policy Highlights n PROCEDURES: n A. Bedside Glucose Accu-Chek Advantage PURPOSE: This policy establishes guidelines for the performance of accurate bedside glucose testing used in clinical decision making such as the rapid evaluation of patients with suspected hypo-or hyperglycemia, the determination of appropriate insulin doses or infusion rates, and assessing the effectiveness of treatment regimens. This method is not used for the diagnosis of diabetes mellitus. These guidelines follow recommendations defined by certain regulatory agencies as dictated by principles of good laboratory practice.
Waived Policy Highlights n Negative Result: Only one (1) pink colored line appears in the control region. No apparent pink colored line is visible in the test region. A negative result indicated that there is no Strep A antigen in the swab sample or the Strep A antigen concentration is below the detection level. A negative result should be cultured to confirm the absence of Strep A infection.
Waived Policy Highlights/Result Follow up Critical Values and Unusual Results: n Any glucose value <40 mg/d. L or >400 mg/d. L should be repeated. Repeat results exceeding these limits are designated as Critical Values and should be reported as soon as practical to the physician or physician extender n If at any time results of bedside glucose testing, regardless of whether they are critical values, are inconsistent with the patient’s status, notify the physician or physician extender for instructions.
Quality Control n Quality Control checks are performed at the frequency and number of levels recommended by the manufacturer n If the manufacturer doesn’t recommend the frequency and number, the medical director, designee or organization must define
Documentation of Quality Control n Controls may be documented on a quality control log or located in the patient’s clinical record n Often internal quality controls are documented in the patient’s clinical record, while external is documented on a log along with reagent lot #s, open dates and expiration dates
Waived Policy Highlights Quality Control: Accu-Chek Comfort Curve glucose controls, low and high levels are used for quality control as follows: Frequency: Run both levels of controls (low and high) with the first run of the day. Also, both levels of controls should be run: n Each time a new vial of test strips is opened. n When a vial of test strips has been left opened. n If the Advantage Meter has been dropped. n Whenever the patient’s result contradicts the patient’s condition. n When batteries are replaced.
Waived Policy Highlights Validation of Controls: n Log control results along with other required information on the Quality Control Log. If control test results are not within expected limits, the following steps are recommended: n Confirm that the Hemo. Cue Microcuvettes are within the expiration date shown on the label. n Retest with new controls. n Log the invalid control results and the repeat results on the Quality Control Log along with the corrective action used. § Special Note: If these steps do not correct the problem, call Northern Hospital Laboratory for assistance or contact Hemo. Cue Technical Services by calling 1 -800 -426 -7256. DO NOT REPORT PATIENT TEST RESULTS!
Instrument Maintenance/Calibration n Follow manufacturer’s instructions for instrument maintenance and calibration checks n Instrument maintenance and calibration checks must be documented n Very important! Individual test results can be associated with quality control, reagent lots, instrument records, and calibration checks
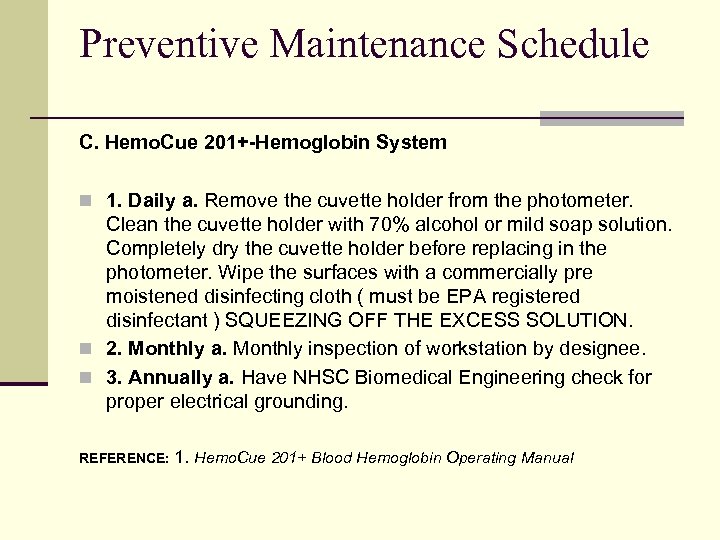
Preventive Maintenance Schedule C. Hemo. Cue 201+-Hemoglobin System n 1. Daily a. Remove the cuvette holder from the photometer. Clean the cuvette holder with 70% alcohol or mild soap solution. Completely dry the cuvette holder before replacing in the photometer. Wipe the surfaces with a commercially pre moistened disinfecting cloth ( must be EPA registered disinfectant ) SQUEEZING OFF THE EXCESS SOLUTION. n 2. Monthly a. Monthly inspection of workstation by designee. n 3. Annually a. Have NHSC Biomedical Engineering check for proper electrical grounding. REFERENCE: 1. Hemo. Cue 201+ Blood Hemoglobin Operating Manual
Result Reporting n Quantitative test result reports in the patient’s clinical record for waived testing are accompanied by reference limits ( normal values ) specific to the test method used and the population served n Reference: Joint Commission Standards for Waived Testing
Hard Copy or EMR n Result on a hard copy: Design the lab result form with reference limits adjacent to the test result n Result in EMR: EMR page for entering lab results may not be formatted to have reference limits adjacent to the test result n If not what? The reference limits must be located elsewhere in the medical record and the result must have a notation directing the reader to that location
Documentation of Critical Values n Very Important to document reporting of critical values, i. e. , Critical value reported to Dr. John Smith at 2: 30 pm on April 15, 2012 by Mary Midkiff
Morbidity and Mortality Weekly Report Indicates Risks n Lack of current manufacturers’ instructions including updates n Failure to follow manufacturers’ instructions including performing quality control n Reporting of incorrect results n Lack of adherence to expiration dates n Inappropriate storage requirements Reference: Morbidity and Mortality Weekly report, November 11, 2005
Morbidity and Mortality , conti. , n Failure to perform test system function checks or calibration checks n Lack of documentation, including quality control and tests performed n Inadequate training n Lack of understanding about good laboratory practices n Reference: Morbidity and Mortality Weekly Report, November 11, 2005
a73d6ec29bd3cbc2b4afacd593cad651.ppt