383656e45bca1ecc081ce94d74b5df26.ppt
- Количество слайдов: 22
 CL-1 Parkinson’s Disease Dementia (PDD) A Clinical Perspective Howard Feldman, MDCM, FRCP (C) Professor and Head Division of Neurology Director-Clinic for Alzheimer Disease and Related Dementias University of British Columbia Vancouver, British Columbia, Canada
CL-1 Parkinson’s Disease Dementia (PDD) A Clinical Perspective Howard Feldman, MDCM, FRCP (C) Professor and Head Division of Neurology Director-Clinic for Alzheimer Disease and Related Dementias University of British Columbia Vancouver, British Columbia, Canada
 CL-2 Overview of Parkinson’s Disease Dementia u Clinical presentation and definition of PDD u Disease burden and need for treatment u Diagnostic differentiation from other dementia syndromes and diagnostic criteria u Identification and diagnosis in routine clinical practice
CL-2 Overview of Parkinson’s Disease Dementia u Clinical presentation and definition of PDD u Disease burden and need for treatment u Diagnostic differentiation from other dementia syndromes and diagnostic criteria u Identification and diagnosis in routine clinical practice
 CL-3 Case Presentation u 63 -yr old male, retired bus driver u 10 -yr history of PD (fulfilling UK Brain Bank Criteria) u Initial presentation: R sided resting tremor, rigidity and bradykinesia u Motor symptoms initially improved with l-dopa 300 mg/day u Wearing-off dyskinesia and motor fluctuations after a number of years of L- dopa treatment u Dopamine agonist (bromocriptine) and entacapone initiated u 8 yr into illness gradual cognitive decline and recurrent visual hallucinations (animals and children in the house)
CL-3 Case Presentation u 63 -yr old male, retired bus driver u 10 -yr history of PD (fulfilling UK Brain Bank Criteria) u Initial presentation: R sided resting tremor, rigidity and bradykinesia u Motor symptoms initially improved with l-dopa 300 mg/day u Wearing-off dyskinesia and motor fluctuations after a number of years of L- dopa treatment u Dopamine agonist (bromocriptine) and entacapone initiated u 8 yr into illness gradual cognitive decline and recurrent visual hallucinations (animals and children in the house)
 CL-4 Case Presentation u Behaviorally less motivated, excessive daytime sleepiness, inattentive and forgetful especially for recent events and conversations u Thought process slower, trouble navigating in his own home u Less involved in activities at home, increased assistance needed in ADL u Dopaminergic medication decreased, hallucinations became less frequent, but motor symptoms worsened u Additional hx of sleep disorder elicited – Suggestive REM sleep behavioral disorder 10 yr prior to motor symptom onset
CL-4 Case Presentation u Behaviorally less motivated, excessive daytime sleepiness, inattentive and forgetful especially for recent events and conversations u Thought process slower, trouble navigating in his own home u Less involved in activities at home, increased assistance needed in ADL u Dopaminergic medication decreased, hallucinations became less frequent, but motor symptoms worsened u Additional hx of sleep disorder elicited – Suggestive REM sleep behavioral disorder 10 yr prior to motor symptom onset
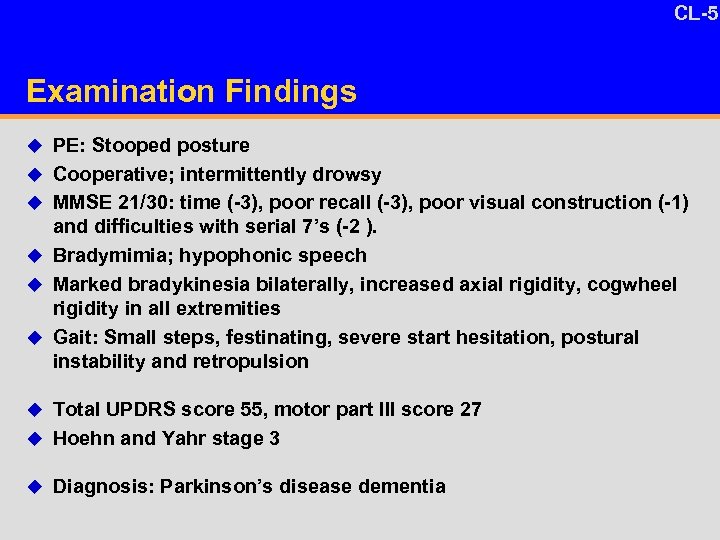 CL-5 Examination Findings u PE: Stooped posture u Cooperative; intermittently drowsy u MMSE 21/30: time (-3), poor recall (-3), poor visual construction (-1) and difficulties with serial 7’s (-2 ). u Bradymimia; hypophonic speech u Marked bradykinesia bilaterally, increased axial rigidity, cogwheel rigidity in all extremities u Gait: Small steps, festinating, severe start hesitation, postural instability and retropulsion u Total UPDRS score 55, motor part III score 27 u Hoehn and Yahr stage 3 u Diagnosis: Parkinson’s disease dementia
CL-5 Examination Findings u PE: Stooped posture u Cooperative; intermittently drowsy u MMSE 21/30: time (-3), poor recall (-3), poor visual construction (-1) and difficulties with serial 7’s (-2 ). u Bradymimia; hypophonic speech u Marked bradykinesia bilaterally, increased axial rigidity, cogwheel rigidity in all extremities u Gait: Small steps, festinating, severe start hesitation, postural instability and retropulsion u Total UPDRS score 55, motor part III score 27 u Hoehn and Yahr stage 3 u Diagnosis: Parkinson’s disease dementia
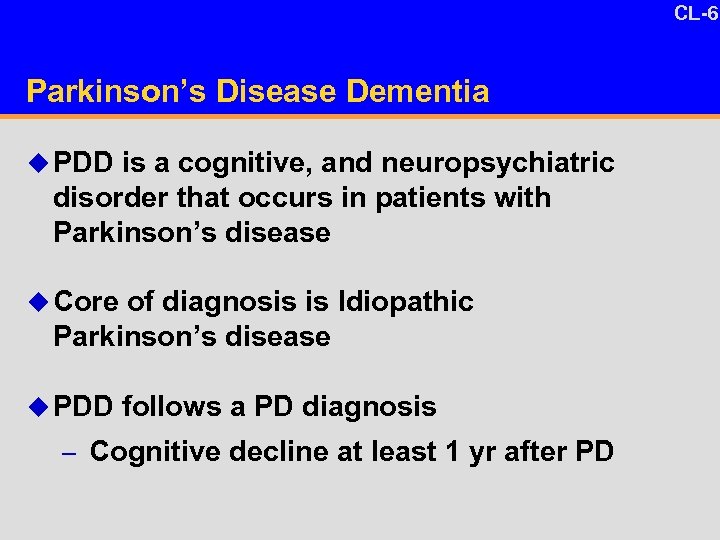 CL-6 10 -4 Parkinson’s Disease Dementia u PDD is a cognitive, and neuropsychiatric disorder that occurs in patients with Parkinson’s disease u Core of diagnosis is Idiopathic Parkinson’s disease u PDD follows a PD diagnosis – Cognitive decline at least 1 yr after PD
CL-6 10 -4 Parkinson’s Disease Dementia u PDD is a cognitive, and neuropsychiatric disorder that occurs in patients with Parkinson’s disease u Core of diagnosis is Idiopathic Parkinson’s disease u PDD follows a PD diagnosis – Cognitive decline at least 1 yr after PD
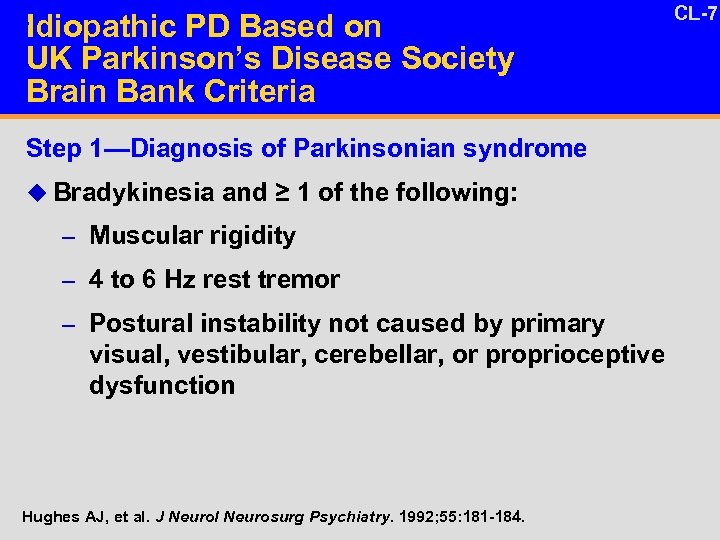 27 Idiopathic PD Based on UK Parkinson’s Disease Society Brain Bank Criteria Protocol_PDD 2311 EXPRESS Sec 9. 5 Appendix 2 DV Step 1—Diagnosis of Parkinsonian syndrome u Bradykinesia and ≥ 1 of the following: – Muscular rigidity – 4 to 6 Hz rest tremor – Postural instability not caused by primary visual, vestibular, cerebellar, or proprioceptive dysfunction Hughes AJ, et al. J Neurol Neurosurg Psychiatry. 1992; 55: 181 -184. CL-7
27 Idiopathic PD Based on UK Parkinson’s Disease Society Brain Bank Criteria Protocol_PDD 2311 EXPRESS Sec 9. 5 Appendix 2 DV Step 1—Diagnosis of Parkinsonian syndrome u Bradykinesia and ≥ 1 of the following: – Muscular rigidity – 4 to 6 Hz rest tremor – Postural instability not caused by primary visual, vestibular, cerebellar, or proprioceptive dysfunction Hughes AJ, et al. J Neurol Neurosurg Psychiatry. 1992; 55: 181 -184. CL-7
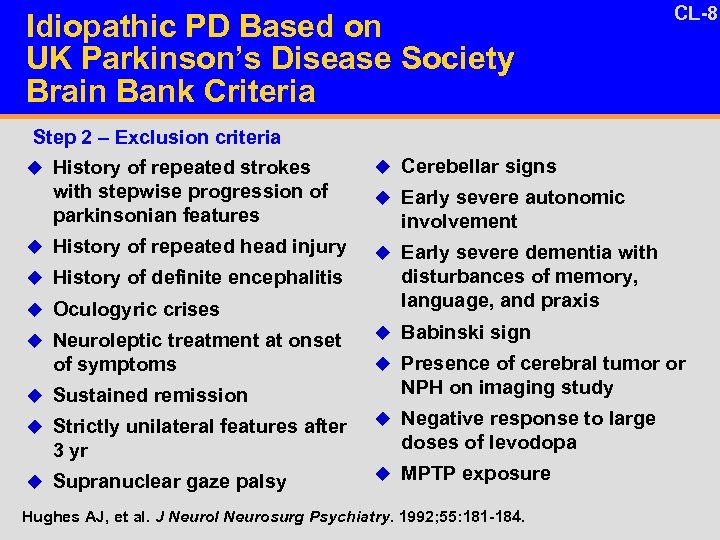 27 Idiopathic PD Based on UK Parkinson’s Disease Society Brain Bank Criteria Protocol_PDD 2311 EXPRESS Sec 9. 5 Appendix 2 DV CL-8 Step 2 – Exclusion criteria u History of repeated strokes with stepwise progression of parkinsonian features u Cerebellar signs u Early severe autonomic involvement u History of repeated head injury u Early severe dementia with u History of definite encephalitis disturbances of memory, language, and praxis u Oculogyric crises u Neuroleptic treatment at onset of symptoms u Sustained remission u Strictly unilateral features after 3 yr u Supranuclear gaze palsy u Babinski sign u Presence of cerebral tumor or NPH on imaging study u Negative response to large doses of levodopa u MPTP exposure Hughes AJ, et al. J Neurol Neurosurg Psychiatry. 1992; 55: 181 -184.
27 Idiopathic PD Based on UK Parkinson’s Disease Society Brain Bank Criteria Protocol_PDD 2311 EXPRESS Sec 9. 5 Appendix 2 DV CL-8 Step 2 – Exclusion criteria u History of repeated strokes with stepwise progression of parkinsonian features u Cerebellar signs u Early severe autonomic involvement u History of repeated head injury u Early severe dementia with u History of definite encephalitis disturbances of memory, language, and praxis u Oculogyric crises u Neuroleptic treatment at onset of symptoms u Sustained remission u Strictly unilateral features after 3 yr u Supranuclear gaze palsy u Babinski sign u Presence of cerebral tumor or NPH on imaging study u Negative response to large doses of levodopa u MPTP exposure Hughes AJ, et al. J Neurol Neurosurg Psychiatry. 1992; 55: 181 -184.
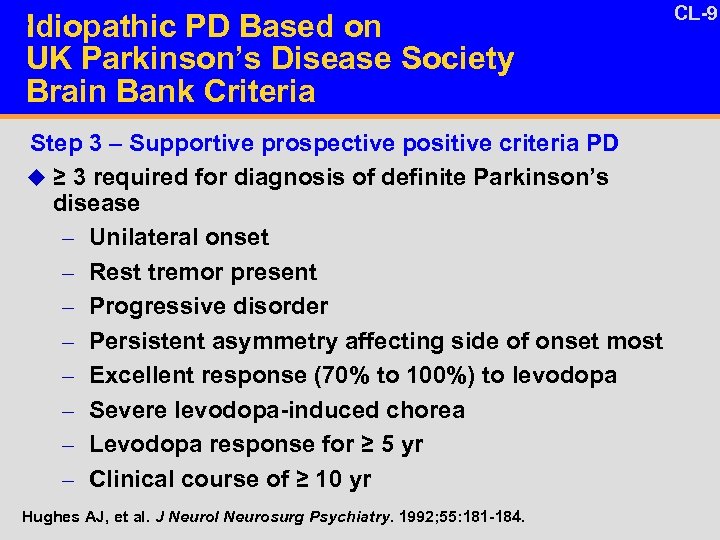 27 Idiopathic PD Based on UK Parkinson’s Disease Society Brain Bank Criteria Protocol_PDD 2311 EXPRESS Sec 9. 5 Appendix 2 DV Step 3 – Supportive prospective positive criteria PD u ≥ 3 required for diagnosis of definite Parkinson’s disease – Unilateral onset – Rest tremor present – Progressive disorder – Persistent asymmetry affecting side of onset most – Excellent response (70% to 100%) to levodopa – Severe levodopa-induced chorea – Levodopa response for ≥ 5 yr – Clinical course of ≥ 10 yr Hughes AJ, et al. J Neurol Neurosurg Psychiatry. 1992; 55: 181 -184. CL-9
27 Idiopathic PD Based on UK Parkinson’s Disease Society Brain Bank Criteria Protocol_PDD 2311 EXPRESS Sec 9. 5 Appendix 2 DV Step 3 – Supportive prospective positive criteria PD u ≥ 3 required for diagnosis of definite Parkinson’s disease – Unilateral onset – Rest tremor present – Progressive disorder – Persistent asymmetry affecting side of onset most – Excellent response (70% to 100%) to levodopa – Severe levodopa-induced chorea – Levodopa response for ≥ 5 yr – Clinical course of ≥ 10 yr Hughes AJ, et al. J Neurol Neurosurg Psychiatry. 1992; 55: 181 -184. CL-9
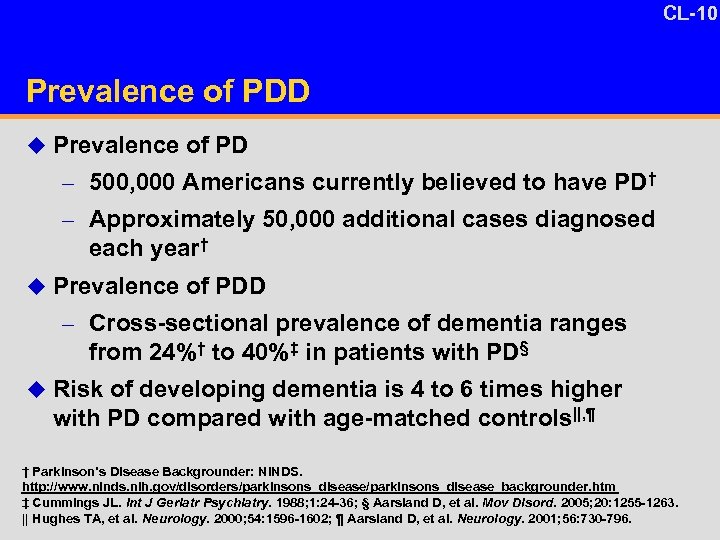 CL-10 13 -6 Prevalence of PDD u Prevalence of PD – 500, 000 Americans currently believed to have PD† – Approximately 50, 000 additional cases diagnosed each year† u Prevalence of PDD – Cross-sectional prevalence of dementia ranges from 24%† to 40%‡ in patients with PD§ u Risk of developing dementia is 4 to 6 times higher with PD compared with age-matched controls||, ¶ † Parkinson’s Disease Backgrounder: NINDS. http: //www. ninds. nih. gov/disorders/parkinsons_disease_backgrounder. htm ‡ Cummings JL. Int J Geriatr Psychiatry. 1988; 1: 24 -36; § Aarsland D, et al. Mov Disord. 2005; 20: 1255 -1263. || Hughes TA, et al. Neurology. 2000; 54: 1596 -1602; ¶ Aarsland D, et al. Neurology. 2001; 56: 730 -796.
CL-10 13 -6 Prevalence of PDD u Prevalence of PD – 500, 000 Americans currently believed to have PD† – Approximately 50, 000 additional cases diagnosed each year† u Prevalence of PDD – Cross-sectional prevalence of dementia ranges from 24%† to 40%‡ in patients with PD§ u Risk of developing dementia is 4 to 6 times higher with PD compared with age-matched controls||, ¶ † Parkinson’s Disease Backgrounder: NINDS. http: //www. ninds. nih. gov/disorders/parkinsons_disease_backgrounder. htm ‡ Cummings JL. Int J Geriatr Psychiatry. 1988; 1: 24 -36; § Aarsland D, et al. Mov Disord. 2005; 20: 1255 -1263. || Hughes TA, et al. Neurology. 2000; 54: 1596 -1602; ¶ Aarsland D, et al. Neurology. 2001; 56: 730 -796.
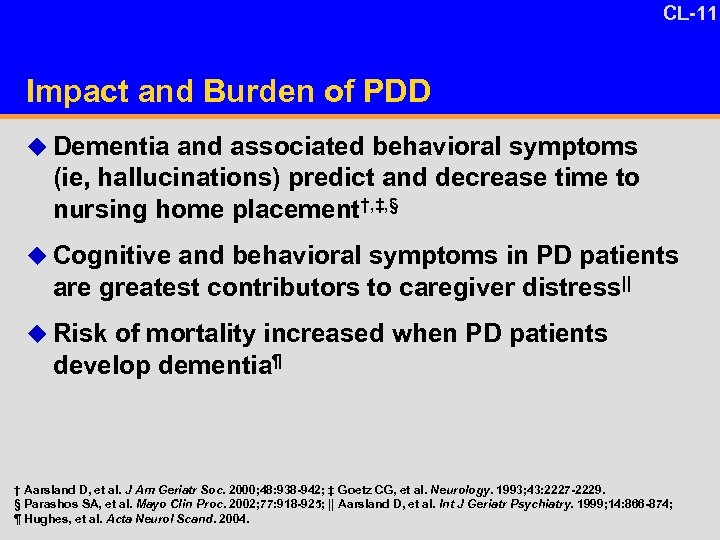 CL-11 15 -10 Impact and Burden of PDD u Dementia and associated behavioral symptoms (ie, hallucinations) predict and decrease time to nursing home placement†, ‡, § u Cognitive and behavioral symptoms in PD patients are greatest contributors to caregiver distress|| u Risk of mortality increased when PD patients develop dementia¶ † Aarsland D, et al. J Am Geriatr Soc. 2000; 48: 938 -942; ‡ Goetz CG, et al. Neurology. 1993; 43: 2227 -2229. § Parashos SA, et al. Mayo Clin Proc. 2002; 77: 918 -925; || Aarsland D, et al. Int J Geriatr Psychiatry. 1999; 14: 866 -874; ¶ Hughes, et al. Acta Neurol Scand. 2004.
CL-11 15 -10 Impact and Burden of PDD u Dementia and associated behavioral symptoms (ie, hallucinations) predict and decrease time to nursing home placement†, ‡, § u Cognitive and behavioral symptoms in PD patients are greatest contributors to caregiver distress|| u Risk of mortality increased when PD patients develop dementia¶ † Aarsland D, et al. J Am Geriatr Soc. 2000; 48: 938 -942; ‡ Goetz CG, et al. Neurology. 1993; 43: 2227 -2229. § Parashos SA, et al. Mayo Clin Proc. 2002; 77: 918 -925; || Aarsland D, et al. Int J Geriatr Psychiatry. 1999; 14: 866 -874; ¶ Hughes, et al. Acta Neurol Scand. 2004.
 CL-12 The Clinical Phenomenology of PDD and Contrast With AD
CL-12 The Clinical Phenomenology of PDD and Contrast With AD
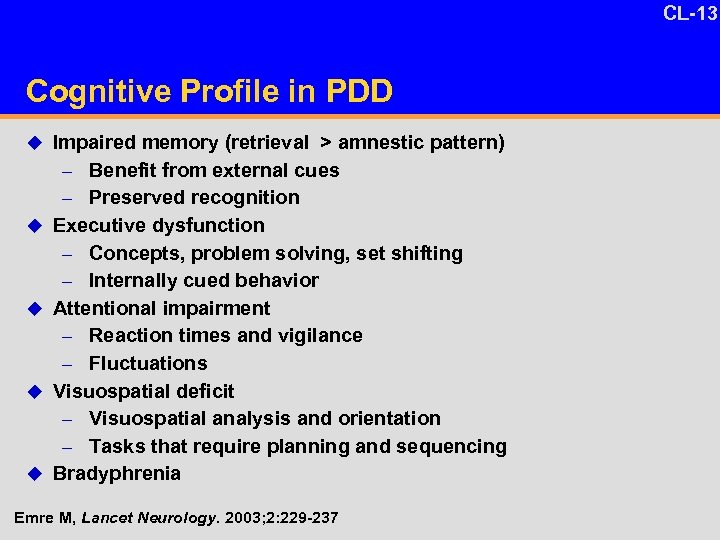 CL-13 Cognitive Profile in PDD u Impaired memory (retrieval > amnestic pattern) Benefit from external cues – Preserved recognition Executive dysfunction – Concepts, problem solving, set shifting – Internally cued behavior Attentional impairment – Reaction times and vigilance – Fluctuations Visuospatial deficit – Visuospatial analysis and orientation – Tasks that require planning and sequencing Bradyphrenia – u u Emre M, Lancet Neurology. 2003; 2: 229 -237
CL-13 Cognitive Profile in PDD u Impaired memory (retrieval > amnestic pattern) Benefit from external cues – Preserved recognition Executive dysfunction – Concepts, problem solving, set shifting – Internally cued behavior Attentional impairment – Reaction times and vigilance – Fluctuations Visuospatial deficit – Visuospatial analysis and orientation – Tasks that require planning and sequencing Bradyphrenia – u u Emre M, Lancet Neurology. 2003; 2: 229 -237
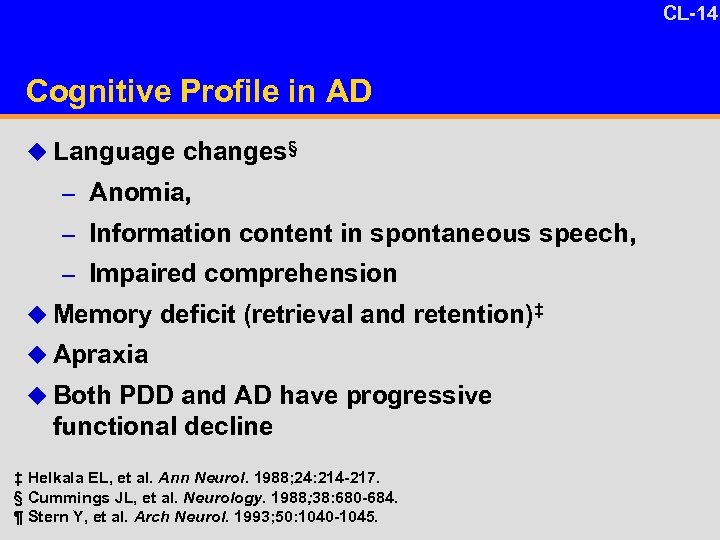 CL-14 Cognitive Profile in AD u Language changes§ – Anomia, – Information content in spontaneous speech, – Impaired comprehension u Memory deficit (retrieval and retention)‡ u Apraxia u Both PDD and AD have progressive functional decline ‡ Helkala EL, et al. Ann Neurol. 1988; 24: 214 -217. § Cummings JL, et al. Neurology. 1988; 38: 680 -684. ¶ Stern Y, et al. Arch Neurol. 1993; 50: 1040 -1045.
CL-14 Cognitive Profile in AD u Language changes§ – Anomia, – Information content in spontaneous speech, – Impaired comprehension u Memory deficit (retrieval and retention)‡ u Apraxia u Both PDD and AD have progressive functional decline ‡ Helkala EL, et al. Ann Neurol. 1988; 24: 214 -217. § Cummings JL, et al. Neurology. 1988; 38: 680 -684. ¶ Stern Y, et al. Arch Neurol. 1993; 50: 1040 -1045.
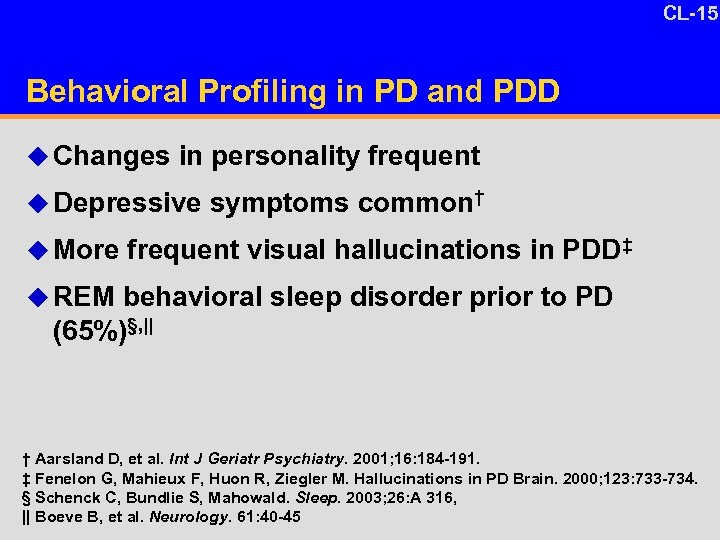 CL-15 Behavioral Profiling in PD and PDD u Changes in personality frequent u Depressive symptoms common† u More frequent visual hallucinations in PDD‡ u REM behavioral sleep disorder prior to PD (65%)§, || † Aarsland D, et al. Int J Geriatr Psychiatry. 2001; 16: 184 -191. ‡ Fenelon G, Mahieux F, Huon R, Ziegler M. Hallucinations in PD Brain. 2000; 123: 733 -734. § Schenck C, Bundlie S, Mahowald. Sleep. 2003; 26: A 316, || Boeve B, et al. Neurology. 61: 40 -45
CL-15 Behavioral Profiling in PD and PDD u Changes in personality frequent u Depressive symptoms common† u More frequent visual hallucinations in PDD‡ u REM behavioral sleep disorder prior to PD (65%)§, || † Aarsland D, et al. Int J Geriatr Psychiatry. 2001; 16: 184 -191. ‡ Fenelon G, Mahieux F, Huon R, Ziegler M. Hallucinations in PD Brain. 2000; 123: 733 -734. § Schenck C, Bundlie S, Mahowald. Sleep. 2003; 26: A 316, || Boeve B, et al. Neurology. 61: 40 -45
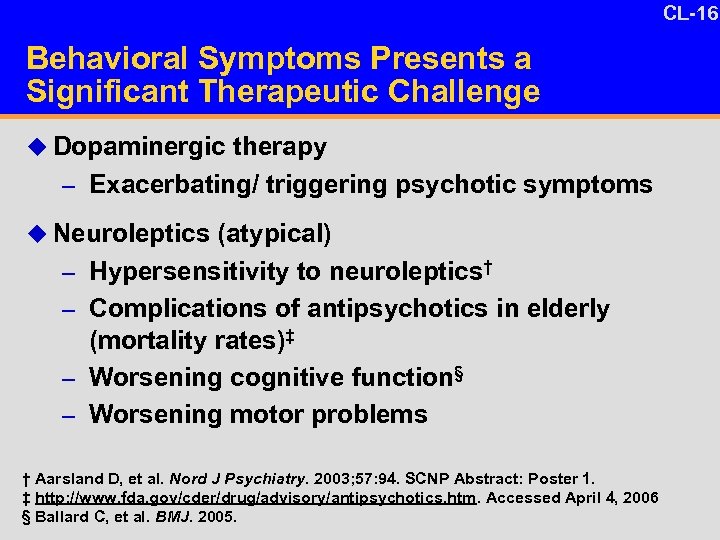 CL-16 Behavioral Symptoms Presents a Significant Therapeutic Challenge u Dopaminergic therapy – Exacerbating/ triggering psychotic symptoms u Neuroleptics (atypical) – Hypersensitivity to neuroleptics† – Complications of antipsychotics in elderly (mortality rates)‡ – Worsening cognitive function§ – Worsening motor problems † Aarsland D, et al. Nord J Psychiatry. 2003; 57: 94. SCNP Abstract: Poster 1. ‡ http: //www. fda. gov/cder/drug/advisory/antipsychotics. htm. Accessed April 4, 2006 § Ballard C, et al. BMJ. 2005.
CL-16 Behavioral Symptoms Presents a Significant Therapeutic Challenge u Dopaminergic therapy – Exacerbating/ triggering psychotic symptoms u Neuroleptics (atypical) – Hypersensitivity to neuroleptics† – Complications of antipsychotics in elderly (mortality rates)‡ – Worsening cognitive function§ – Worsening motor problems † Aarsland D, et al. Nord J Psychiatry. 2003; 57: 94. SCNP Abstract: Poster 1. ‡ http: //www. fda. gov/cder/drug/advisory/antipsychotics. htm. Accessed April 4, 2006 § Ballard C, et al. BMJ. 2005.
 CL-17 Diagnosing PDD The DSM criteria
CL-17 Diagnosing PDD The DSM criteria
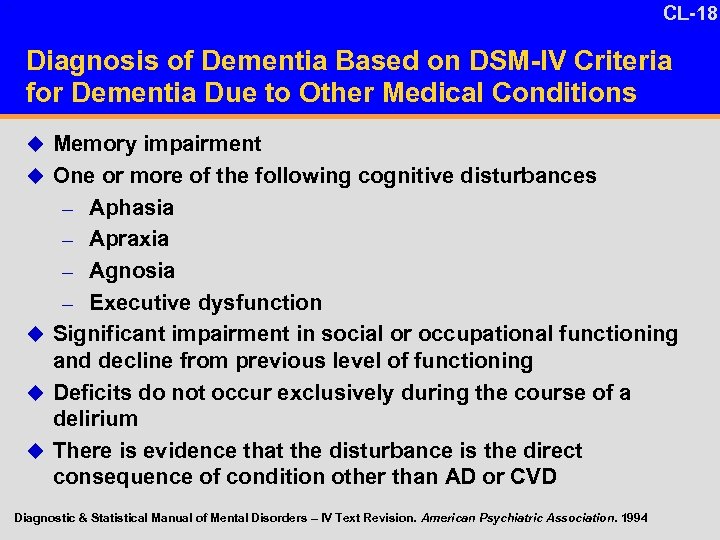 CL-18 1 Diagnosis of Dementia Based on DSM-IV Criteria for Dementia Due to Other Medical Conditions u Memory impairment u One or more of the following cognitive disturbances – Aphasia – Apraxia – Agnosia – Executive dysfunction u Significant impairment in social or occupational functioning and decline from previous level of functioning u Deficits do not occur exclusively during the course of a delirium u There is evidence that the disturbance is the direct consequence of condition other than AD or CVD Diagnostic & Statistical Manual of Mental Disorders – IV Text Revision. American Psychiatric Association. 1994
CL-18 1 Diagnosis of Dementia Based on DSM-IV Criteria for Dementia Due to Other Medical Conditions u Memory impairment u One or more of the following cognitive disturbances – Aphasia – Apraxia – Agnosia – Executive dysfunction u Significant impairment in social or occupational functioning and decline from previous level of functioning u Deficits do not occur exclusively during the course of a delirium u There is evidence that the disturbance is the direct consequence of condition other than AD or CVD Diagnostic & Statistical Manual of Mental Disorders – IV Text Revision. American Psychiatric Association. 1994
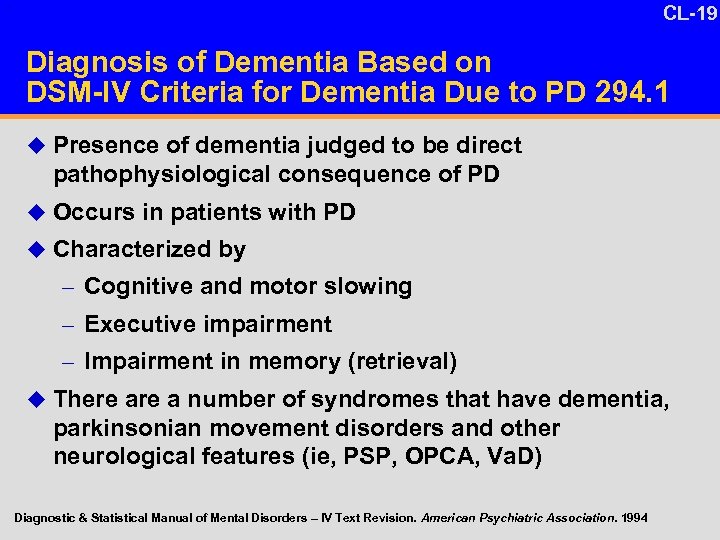 CL-19 1 Diagnosis of Dementia Based on DSM-IV Criteria for Dementia Due to PD 294. 1 u Presence of dementia judged to be direct pathophysiological consequence of PD u Occurs in patients with PD u Characterized by – Cognitive and motor slowing – Executive impairment – Impairment in memory (retrieval) u There a number of syndromes that have dementia, parkinsonian movement disorders and other neurological features (ie, PSP, OPCA, Va. D) Diagnostic & Statistical Manual of Mental Disorders – IV Text Revision. American Psychiatric Association. 1994
CL-19 1 Diagnosis of Dementia Based on DSM-IV Criteria for Dementia Due to PD 294. 1 u Presence of dementia judged to be direct pathophysiological consequence of PD u Occurs in patients with PD u Characterized by – Cognitive and motor slowing – Executive impairment – Impairment in memory (retrieval) u There a number of syndromes that have dementia, parkinsonian movement disorders and other neurological features (ie, PSP, OPCA, Va. D) Diagnostic & Statistical Manual of Mental Disorders – IV Text Revision. American Psychiatric Association. 1994
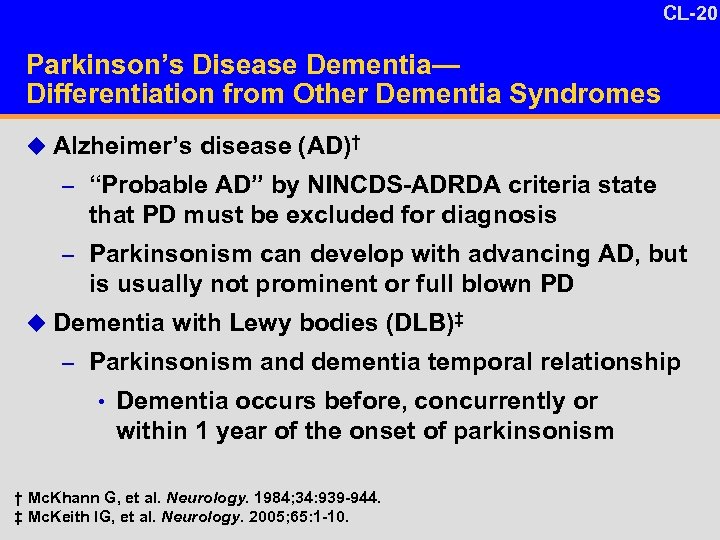 CL-20 10 -4 Parkinson’s Disease Dementia— Differentiation from Other Dementia Syndromes u Alzheimer’s disease (AD)† – “Probable AD” by NINCDS-ADRDA criteria state that PD must be excluded for diagnosis – Parkinsonism can develop with advancing AD, but is usually not prominent or full blown PD u Dementia with Lewy bodies (DLB)‡ – Parkinsonism and dementia temporal relationship • Dementia occurs before, concurrently or within 1 year of the onset of parkinsonism † Mc. Khann G, et al. Neurology. 1984; 34: 939 -944. ‡ Mc. Keith IG, et al. Neurology. 2005; 65: 1 -10.
CL-20 10 -4 Parkinson’s Disease Dementia— Differentiation from Other Dementia Syndromes u Alzheimer’s disease (AD)† – “Probable AD” by NINCDS-ADRDA criteria state that PD must be excluded for diagnosis – Parkinsonism can develop with advancing AD, but is usually not prominent or full blown PD u Dementia with Lewy bodies (DLB)‡ – Parkinsonism and dementia temporal relationship • Dementia occurs before, concurrently or within 1 year of the onset of parkinsonism † Mc. Khann G, et al. Neurology. 1984; 34: 939 -944. ‡ Mc. Keith IG, et al. Neurology. 2005; 65: 1 -10.
 CL-21 PDD Can be Diagnosed in Routine Clinical Practice u DSM criteria for dementia due to other medical conditions can be applied by physicians for diagnosis in routine clinical practice u These criteria do not require specific psychometric test scores u The temporal relationship between the onset of the dementia and the diagnosis of PD can be obtained from patient history (at least 1 year) † Mc. Keith I, et al. Neurology. 2005; 65: 1863 -1872.
CL-21 PDD Can be Diagnosed in Routine Clinical Practice u DSM criteria for dementia due to other medical conditions can be applied by physicians for diagnosis in routine clinical practice u These criteria do not require specific psychometric test scores u The temporal relationship between the onset of the dementia and the diagnosis of PD can be obtained from patient history (at least 1 year) † Mc. Keith I, et al. Neurology. 2005; 65: 1863 -1872.
 CL-22 Conclusion u PDD is a clinical disease with a unique progression – Begins with Parkinson’s disease – Motor signs present for years before onset of dementia – Dementia syndrome characterized by memory, executive, attentional, and functional deficits – Prominent neuropsychiatric symptoms with psychotic features u PDD can be identified and diagnosed in usual settings of care u Need for effective treatments – There are no currently approved treatment options
CL-22 Conclusion u PDD is a clinical disease with a unique progression – Begins with Parkinson’s disease – Motor signs present for years before onset of dementia – Dementia syndrome characterized by memory, executive, attentional, and functional deficits – Prominent neuropsychiatric symptoms with psychotic features u PDD can be identified and diagnosed in usual settings of care u Need for effective treatments – There are no currently approved treatment options


