1f614a814b0f411e487f9c51b6fecd6d.ppt
- Количество слайдов: 38
 City and Hackney Clinical Commissioning Forum Thursday 7 th April 2016 St Joseph’s Hospice
City and Hackney Clinical Commissioning Forum Thursday 7 th April 2016 St Joseph’s Hospice
 Agenda 1. Welcome Haren Patel 2. Safeguarding Audit Haren Patel 3. 5 Year Plan David Maher/Siobhan Harper 4. Clinical Leadership Paul Haigh 5. Quality Premiums Evelina De Angelo Cheong 6. Bilingual Advocacy Siobhan Harper The next Clinical Commissioning Forum will be held on Thursday 5 May 2016, 1. 00 pm in the 1 st Floor Education Centre, St Joseph’s Hospice, Mare Street, Hackney
Agenda 1. Welcome Haren Patel 2. Safeguarding Audit Haren Patel 3. 5 Year Plan David Maher/Siobhan Harper 4. Clinical Leadership Paul Haigh 5. Quality Premiums Evelina De Angelo Cheong 6. Bilingual Advocacy Siobhan Harper The next Clinical Commissioning Forum will be held on Thursday 5 May 2016, 1. 00 pm in the 1 st Floor Education Centre, St Joseph’s Hospice, Mare Street, Hackney
 Safeguarding Children Audit Section 11 of the Children Act 2004 places a statutory duty agencies to ensure that they have in place robust safeguarding arrangements. Oversight of this is placed with the local safeguarding children board. • The CCG will shortly be sending out the Section 11 audits ( on behalf of the CHSCB) to each of the GP practices in City & Hackney. • The audits check the safeguarding arrangements in each practice and are an important component of future CQC inspections. • Two years ago we had a return of 36 audits. This year we hope to be able to say that every practice has returned their audits. • Look out for the email coming soon!
Safeguarding Children Audit Section 11 of the Children Act 2004 places a statutory duty agencies to ensure that they have in place robust safeguarding arrangements. Oversight of this is placed with the local safeguarding children board. • The CCG will shortly be sending out the Section 11 audits ( on behalf of the CHSCB) to each of the GP practices in City & Hackney. • The audits check the safeguarding arrangements in each practice and are an important component of future CQC inspections. • Two years ago we had a return of 36 audits. This year we hope to be able to say that every practice has returned their audits. • Look out for the email coming soon!
 TAKING OUR WORK FORWARD & STP April 2016
TAKING OUR WORK FORWARD & STP April 2016
 CONTEXT • Further guidance on STPs has now been issued – v high level • base case/issues to submit in April • What going to do about them end of June • Whilst the planning footprint is NEL – and an umbrella NEL submission will be made – we are using the guidance to develop our local plan to support our devolution and integration plans • The NEL submission will highlight the key NEL-wide priorities and where these are best transacted at NEL level and where local • Success of NEL plan is critical for accessing money • As C&H we will also have our own priorities and we plan to synthesise these 2 plans by middle of April
CONTEXT • Further guidance on STPs has now been issued – v high level • base case/issues to submit in April • What going to do about them end of June • Whilst the planning footprint is NEL – and an umbrella NEL submission will be made – we are using the guidance to develop our local plan to support our devolution and integration plans • The NEL submission will highlight the key NEL-wide priorities and where these are best transacted at NEL level and where local • Success of NEL plan is critical for accessing money • As C&H we will also have our own priorities and we plan to synthesise these 2 plans by middle of April
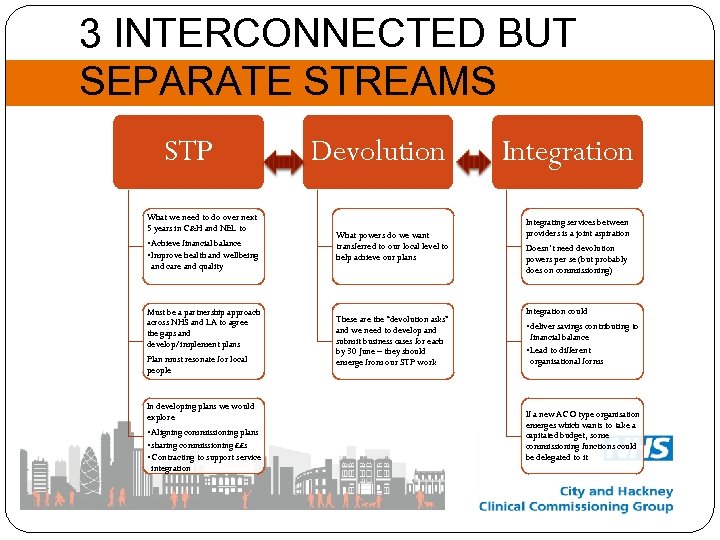 3 INTERCONNECTED BUT SEPARATE STREAMS STP Devolution Integration What we need to do over next 5 years in C&H and NEL to • Achieve financial balance • Improve health and wellbeing and care and quality What powers do we want transferred to our local level to help achieve our plans Integrating services between providers is a joint aspiration Doesn’t need devolution powers per se (but probably does on commissioning) Must be a partnership approach across NHS and LA to agree the gaps and develop/implement plans Plan must resonate for local people These are the “devolution asks” and we need to develop and submit business cases for each by 30 June – they should emerge from our STP work Integration could • deliver savings contributing to financial balance • Lead to different organisational forms In developing plans we would explore • Aligning commissioning plans • sharing commissioning ££s • Contracting to support service integration If a new ACO type organisation emerges which wants to take a capitated budget, some commissioning functions could be delegated to it
3 INTERCONNECTED BUT SEPARATE STREAMS STP Devolution Integration What we need to do over next 5 years in C&H and NEL to • Achieve financial balance • Improve health and wellbeing and care and quality What powers do we want transferred to our local level to help achieve our plans Integrating services between providers is a joint aspiration Doesn’t need devolution powers per se (but probably does on commissioning) Must be a partnership approach across NHS and LA to agree the gaps and develop/implement plans Plan must resonate for local people These are the “devolution asks” and we need to develop and submit business cases for each by 30 June – they should emerge from our STP work Integration could • deliver savings contributing to financial balance • Lead to different organisational forms In developing plans we would explore • Aligning commissioning plans • sharing commissioning ££s • Contracting to support service integration If a new ACO type organisation emerges which wants to take a capitated budget, some commissioning functions could be delegated to it
 SERVICE INTEGRATION • • • We already have alliance contracts for One Hackney and some mental health services (contracts based on outcomes which all providers in the alliance work together to achieve) We are holding a workshop to understand what an ACO is – April 19 Building on One Hackney there are 2 areas where providers want to start to explore further service integration • Integrating “community/out of hospital” teams across NHS and Social services to keep people in the community (including the role of Community Nurses) • Developing a single point of access for managing crises • These 2 workstreams will be taken forward via the ICPB • From these: • There are likely to be issues for all of the enabler workstreams • There may be devolution asks. • There may be savings/new organisational forms/different contracts • Addressing both of these will support our 5 year plan
SERVICE INTEGRATION • • • We already have alliance contracts for One Hackney and some mental health services (contracts based on outcomes which all providers in the alliance work together to achieve) We are holding a workshop to understand what an ACO is – April 19 Building on One Hackney there are 2 areas where providers want to start to explore further service integration • Integrating “community/out of hospital” teams across NHS and Social services to keep people in the community (including the role of Community Nurses) • Developing a single point of access for managing crises • These 2 workstreams will be taken forward via the ICPB • From these: • There are likely to be issues for all of the enabler workstreams • There may be devolution asks. • There may be savings/new organisational forms/different contracts • Addressing both of these will support our 5 year plan
 • Whilst the previous slide outlines 2 initial areas of focus, other “STP” workstreams will contunue to identify Opportunities for joint commissioning • Opportunities for joint provision/further service integration This will be an iterative process which can be overseen by the Transformation Board and which the individual organisations will need to respond to •
• Whilst the previous slide outlines 2 initial areas of focus, other “STP” workstreams will contunue to identify Opportunities for joint commissioning • Opportunities for joint provision/further service integration This will be an iterative process which can be overseen by the Transformation Board and which the individual organisations will need to respond to •
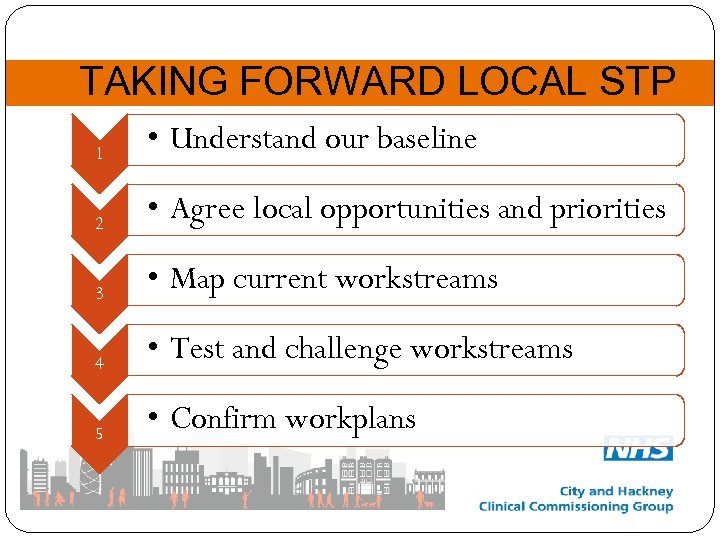 TAKING FORWARD LOCAL STP 1 • Understand our baseline 2 • Agree local opportunities and priorities 3 • Map current workstreams 4 • Test and challenge workstreams 5 • Confirm workplans
TAKING FORWARD LOCAL STP 1 • Understand our baseline 2 • Agree local opportunities and priorities 3 • Map current workstreams 4 • Test and challenge workstreams 5 • Confirm workplans
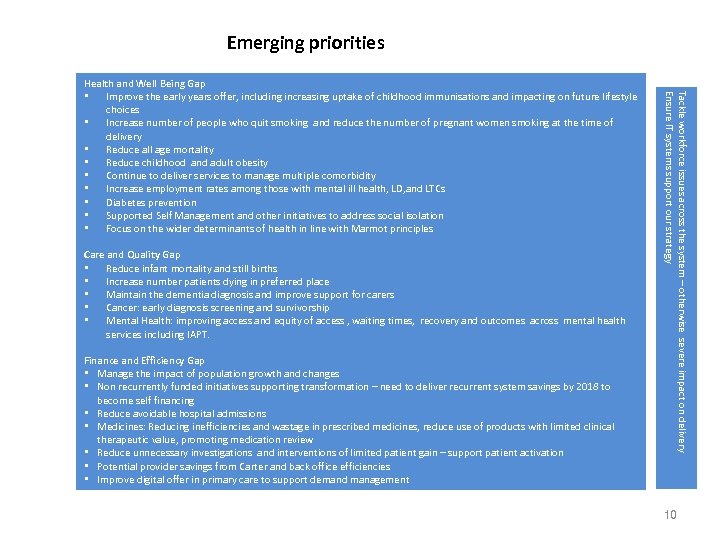 Emerging priorities Care and Quality Gap • Reduce infant mortality and still births • Increase number patients dying in preferred place • Maintain the dementia diagnosis and improve support for carers • Cancer: early diagnosis screening and survivorship • Mental Health: improving access and equity of access , waiting times, recovery and outcomes across mental health services including IAPT. Finance and Efficiency Gap • Manage the impact of population growth and changes • Non recurrently funded initiatives supporting transformation – need to deliver recurrent system savings by 2018 to become self financing • Reduce avoidable hospital admissions • Medicines: Reducing inefficiencies and wastage in prescribed medicines, reduce use of products with limited clinical therapeutic value, promoting medication review • Reduce unnecessary investigations and interventions of limited patient gain – support patient activation • Potential provider savings from Carter and back office efficiencies • Improve digital offer in primary care to support demand management Tackle workforce issues across the system – otherwise severe impact on delivery Ensure IT systems support our strategy Health and Well Being Gap • Improve the early years offer, including increasing uptake of childhood immunisations and impacting on future lifestyle choices • Increase number of people who quit smoking and reduce the number of pregnant women smoking at the time of delivery • Reduce all age mortality • Reduce childhood and adult obesity • Continue to deliver services to manage multiple comorbidity • Increase employment rates among those with mental ill health, LD, and LTCs • Diabetes prevention • Supported Self Management and other initiatives to address social isolation • Focus on the wider determinants of health in line with Marmot principles 10
Emerging priorities Care and Quality Gap • Reduce infant mortality and still births • Increase number patients dying in preferred place • Maintain the dementia diagnosis and improve support for carers • Cancer: early diagnosis screening and survivorship • Mental Health: improving access and equity of access , waiting times, recovery and outcomes across mental health services including IAPT. Finance and Efficiency Gap • Manage the impact of population growth and changes • Non recurrently funded initiatives supporting transformation – need to deliver recurrent system savings by 2018 to become self financing • Reduce avoidable hospital admissions • Medicines: Reducing inefficiencies and wastage in prescribed medicines, reduce use of products with limited clinical therapeutic value, promoting medication review • Reduce unnecessary investigations and interventions of limited patient gain – support patient activation • Potential provider savings from Carter and back office efficiencies • Improve digital offer in primary care to support demand management Tackle workforce issues across the system – otherwise severe impact on delivery Ensure IT systems support our strategy Health and Well Being Gap • Improve the early years offer, including increasing uptake of childhood immunisations and impacting on future lifestyle choices • Increase number of people who quit smoking and reduce the number of pregnant women smoking at the time of delivery • Reduce all age mortality • Reduce childhood and adult obesity • Continue to deliver services to manage multiple comorbidity • Increase employment rates among those with mental ill health, LD, and LTCs • Diabetes prevention • Supported Self Management and other initiatives to address social isolation • Focus on the wider determinants of health in line with Marmot principles 10
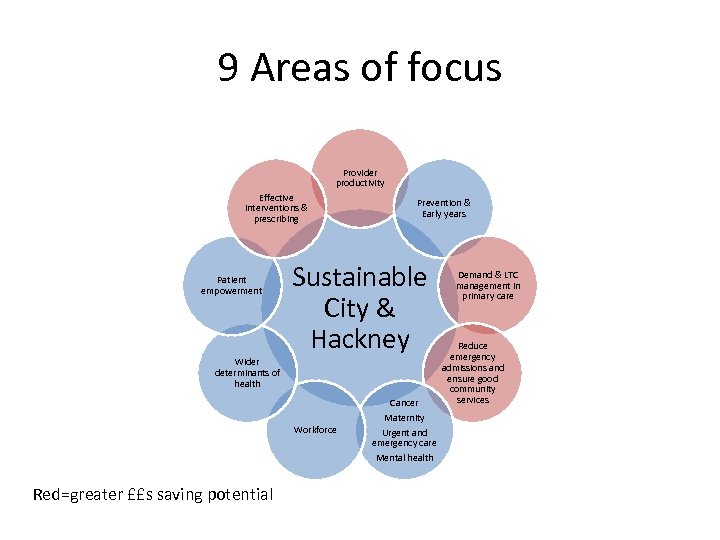 9 Areas of focus Provider productivity Effective interventions & prescribing Patient empowerment Wider determinants of health Prevention & Early years Sustainable City & Hackney Cancer Workforce Red=greater ££s saving potential Maternity Urgent and emergency care Mental health Demand & LTC management in primary care Reduce emergency admissions and ensure good community services
9 Areas of focus Provider productivity Effective interventions & prescribing Patient empowerment Wider determinants of health Prevention & Early years Sustainable City & Hackney Cancer Workforce Red=greater ££s saving potential Maternity Urgent and emergency care Mental health Demand & LTC management in primary care Reduce emergency admissions and ensure good community services
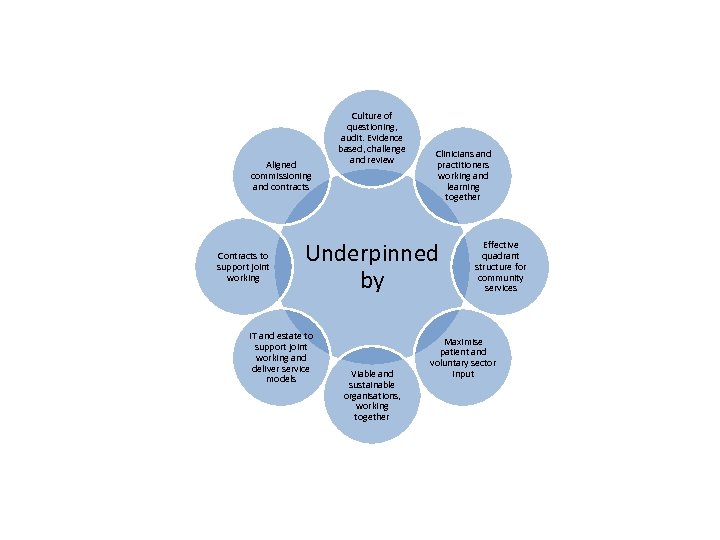 Aligned commissioning and contracts Contracts to support joint working Culture of questioning, audit. Evidence based, challenge and review Clinicians and practitioners working and learning together Underpinned by IT and estate to support joint working and deliver service models Viable and sustainable organisations, working together Effective quadrant structure for community services Maximise patient and voluntary sector input
Aligned commissioning and contracts Contracts to support joint working Culture of questioning, audit. Evidence based, challenge and review Clinicians and practitioners working and learning together Underpinned by IT and estate to support joint working and deliver service models Viable and sustainable organisations, working together Effective quadrant structure for community services Maximise patient and voluntary sector input
 WHATS IN PLACE • • • Invite feedback on priorities CCG & LBH map all current initiatives against the priorities Undertake an analysis of • • • Is there a trajectory to achieve improvements over 5 years Are there any emerging devo asks Are we clear about system financial savings Are plans joined up Ensure City dimension where appropriate
WHATS IN PLACE • • • Invite feedback on priorities CCG & LBH map all current initiatives against the priorities Undertake an analysis of • • • Is there a trajectory to achieve improvements over 5 years Are there any emerging devo asks Are we clear about system financial savings Are plans joined up Ensure City dimension where appropriate
 CHALLENGE • Undertake challenge session(s) across all partners • • • Are we missing opportunities Could we go further Test assumptions re savings and devo asks
CHALLENGE • Undertake challenge session(s) across all partners • • • Are we missing opportunities Could we go further Test assumptions re savings and devo asks
 CONFIRM • • Reconfirm objectives, milestones, leadership arrangements for each workstream and reporting arrangements Need to be clear on • • Enabler issues Devo asks by 30 June Savings – 30 June How we contract for change and improvement across the system
CONFIRM • • Reconfirm objectives, milestones, leadership arrangements for each workstream and reporting arrangements Need to be clear on • • Enabler issues Devo asks by 30 June Savings – 30 June How we contract for change and improvement across the system
 FRAMEWORK • Codesign by patients and clinicians/practitioners with strong leadership arrangements • Self management and information for patients to inform their decisions • Use of email, telephone and other technology • Manage demand as effectively as possible and agree KPIs (eg reduced opd followup) in line with benchmarked best practice • Maintain care in community settings using the quadrant structure of multidisciplinary teams as the delivery model where appropriate • Evidence based and clinically excellent best practice • Upskilling primary care • Minimal handoffs and interfaces between services, reducing waste for patients and clinicians • Integration between practitioners and teams – orientated to patient needs and GPs
FRAMEWORK • Codesign by patients and clinicians/practitioners with strong leadership arrangements • Self management and information for patients to inform their decisions • Use of email, telephone and other technology • Manage demand as effectively as possible and agree KPIs (eg reduced opd followup) in line with benchmarked best practice • Maintain care in community settings using the quadrant structure of multidisciplinary teams as the delivery model where appropriate • Evidence based and clinically excellent best practice • Upskilling primary care • Minimal handoffs and interfaces between services, reducing waste for patients and clinicians • Integration between practitioners and teams – orientated to patient needs and GPs
 END | NOTES
END | NOTES
 CLINICAL LEADERSHIP 2016 MODEL
CLINICAL LEADERSHIP 2016 MODEL
 Role • • • Taking forward the priorities in the 5 year plan Maintaining an eye on performance Pathway development and refresh Consulting with patients and members Taking a leadership role for the system
Role • • • Taking forward the priorities in the 5 year plan Maintaining an eye on performance Pathway development and refresh Consulting with patients and members Taking a leadership role for the system
 • • • Paired with consultant and patient Supported by a salaried doctor from GP Confederation scheme Clear brief and milestones • Support from • • • Pathway Manager Audit at Homerton Programme Board Chair Mentoring for salaried doctor – part of Confed scheme and within Prog Board Development programme
• • • Paired with consultant and patient Supported by a salaried doctor from GP Confederation scheme Clear brief and milestones • Support from • • • Pathway Manager Audit at Homerton Programme Board Chair Mentoring for salaried doctor – part of Confed scheme and within Prog Board Development programme
 Recruitment evening • Thursday 14 April • 1800 • Tomlinson Centre, Queensbridge Road
Recruitment evening • Thursday 14 April • 1800 • Tomlinson Centre, Queensbridge Road
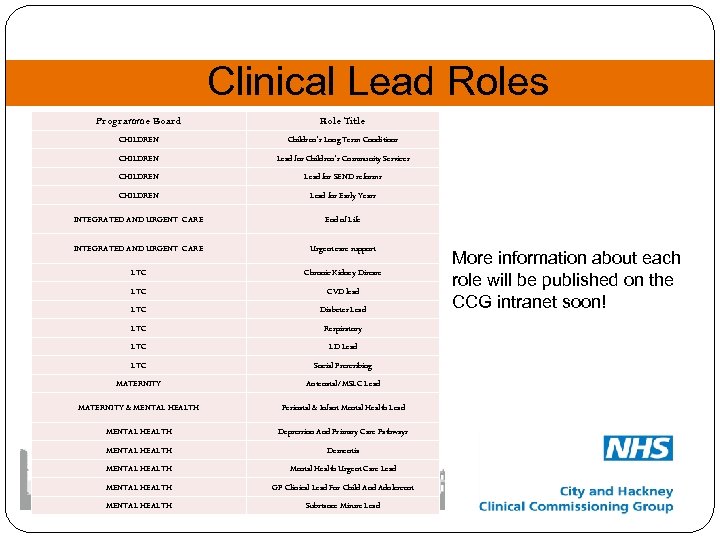 Clinical Lead Roles Programme Board Role Title CHILDREN Children’s Long Term Conditions CHILDREN Lead for Children’s Community Services CHILDREN Lead for SEND reforms CHILDREN Lead for Early Years INTEGRATED AND URGENT CARE End of Life INTEGRATED AND URGENT CARE Urgent care support LTC Chronic Kidney Disease LTC CVD lead LTC Diabetes Lead LTC Respiratory LTC LD Lead LTC Social Prescribing MATERNITY Antenatal/MSLC Lead MATERNITY & MENTAL HEALTH Perinatal & Infant Mental Health Lead MENTAL HEALTH Depression And Primary Care Pathways MENTAL HEALTH Dementia MENTAL HEALTH Mental Health Urgent Care Lead MENTAL HEALTH GP Clinical Lead For Child And Adolescent MENTAL HEALTH Substance Misuse Lead More information about each role will be published on the CCG intranet soon!
Clinical Lead Roles Programme Board Role Title CHILDREN Children’s Long Term Conditions CHILDREN Lead for Children’s Community Services CHILDREN Lead for SEND reforms CHILDREN Lead for Early Years INTEGRATED AND URGENT CARE End of Life INTEGRATED AND URGENT CARE Urgent care support LTC Chronic Kidney Disease LTC CVD lead LTC Diabetes Lead LTC Respiratory LTC LD Lead LTC Social Prescribing MATERNITY Antenatal/MSLC Lead MATERNITY & MENTAL HEALTH Perinatal & Infant Mental Health Lead MENTAL HEALTH Depression And Primary Care Pathways MENTAL HEALTH Dementia MENTAL HEALTH Mental Health Urgent Care Lead MENTAL HEALTH GP Clinical Lead For Child And Adolescent MENTAL HEALTH Substance Misuse Lead More information about each role will be published on the CCG intranet soon!
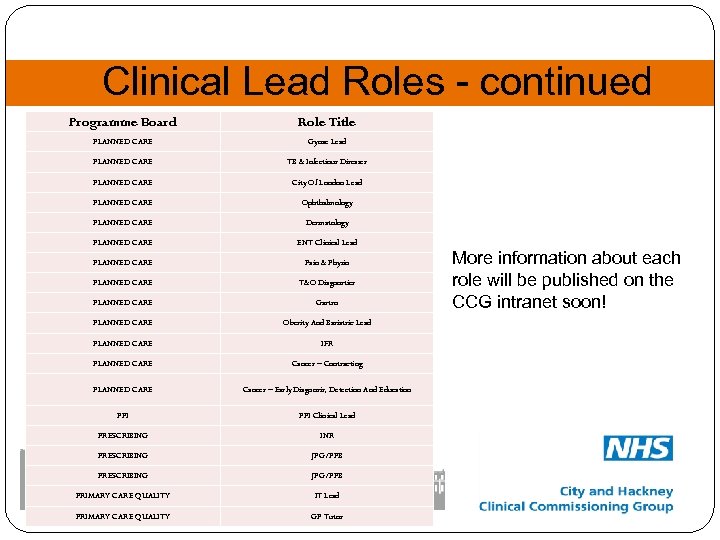 Clinical Lead Roles - continued Programme Board Role Title PLANNED CARE Gynae Lead PLANNED CARE TB & Infectious Diseases PLANNED CARE City Of London Lead PLANNED CARE Ophthalmology PLANNED CARE Dermatology PLANNED CARE ENT Clinical Lead PLANNED CARE Pain & Physio PLANNED CARE T&O Diagnostics PLANNED CARE Gastro PLANNED CARE Obesity And Bariatric Lead PLANNED CARE IFR PLANNED CARE Cancer – Contracting PLANNED CARE Cancer – Early Diagnosis, Detection And Education PPI Clinical Lead PRESCRIBING INR PRESCRIBING JPG/PPB PRIMARY CARE QUALITY IT Lead PRIMARY CARE QUALITY GP Tutor More information about each role will be published on the CCG intranet soon!
Clinical Lead Roles - continued Programme Board Role Title PLANNED CARE Gynae Lead PLANNED CARE TB & Infectious Diseases PLANNED CARE City Of London Lead PLANNED CARE Ophthalmology PLANNED CARE Dermatology PLANNED CARE ENT Clinical Lead PLANNED CARE Pain & Physio PLANNED CARE T&O Diagnostics PLANNED CARE Gastro PLANNED CARE Obesity And Bariatric Lead PLANNED CARE IFR PLANNED CARE Cancer – Contracting PLANNED CARE Cancer – Early Diagnosis, Detection And Education PPI Clinical Lead PRESCRIBING INR PRESCRIBING JPG/PPB PRIMARY CARE QUALITY IT Lead PRIMARY CARE QUALITY GP Tutor More information about each role will be published on the CCG intranet soon!
 END | NOTES
END | NOTES
 Quality Premium (QP) 2016/17 Clinical Commissioning Forum April 2016
Quality Premium (QP) 2016/17 Clinical Commissioning Forum April 2016
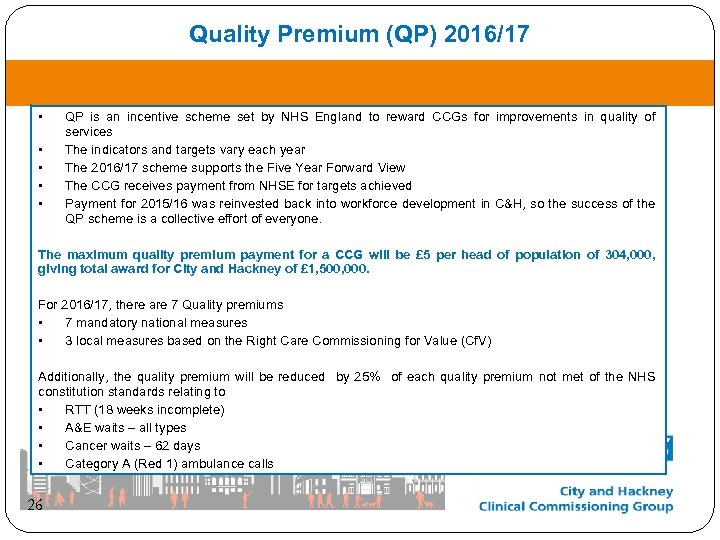 Quality Premium (QP) 2016/17 • • • QP is an incentive scheme set by NHS England to reward CCGs for improvements in quality of services The indicators and targets vary each year The 2016/17 scheme supports the Five Year Forward View The CCG receives payment from NHSE for targets achieved Payment for 2015/16 was reinvested back into workforce development in C&H, so the success of the QP scheme is a collective effort of everyone. The maximum quality premium payment for a CCG will be £ 5 per head of population of 304, 000, giving total award for City and Hackney of £ 1, 500, 000. For 2016/17, there are 7 Quality premiums • 7 mandatory national measures • 3 local measures based on the Right Care Commissioning for Value (Cf. V) Additionally, the quality premium will be reduced by 25% of each quality premium not met of the NHS constitution standards relating to • RTT (18 weeks incomplete) • A&E waits – all types • Cancer waits – 62 days • Category A (Red 1) ambulance calls 26
Quality Premium (QP) 2016/17 • • • QP is an incentive scheme set by NHS England to reward CCGs for improvements in quality of services The indicators and targets vary each year The 2016/17 scheme supports the Five Year Forward View The CCG receives payment from NHSE for targets achieved Payment for 2015/16 was reinvested back into workforce development in C&H, so the success of the QP scheme is a collective effort of everyone. The maximum quality premium payment for a CCG will be £ 5 per head of population of 304, 000, giving total award for City and Hackney of £ 1, 500, 000. For 2016/17, there are 7 Quality premiums • 7 mandatory national measures • 3 local measures based on the Right Care Commissioning for Value (Cf. V) Additionally, the quality premium will be reduced by 25% of each quality premium not met of the NHS constitution standards relating to • RTT (18 weeks incomplete) • A&E waits – all types • Cancer waits – 62 days • Category A (Red 1) ambulance calls 26
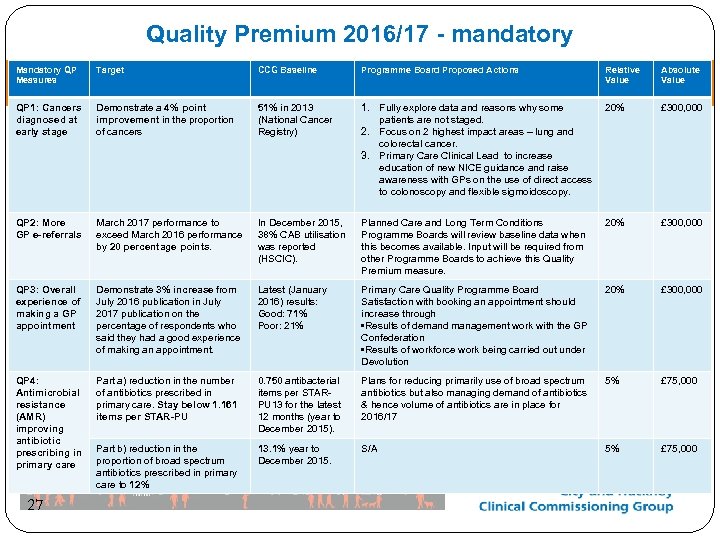 Quality Premium 2016/17 - mandatory Mandatory QP Measures Target CCG Baseline Programme Board Proposed Actions QP 1: Cancers diagnosed at early stage Demonstrate a 4% point improvement in the proportion of cancers 51% in 2013 (National Cancer Registry) 1. Fully explore data and reasons why some 20% patients are not staged. 2. Focus on 2 highest impact areas – lung and colorectal cancer. 3. Primary Care Clinical Lead to increase education of new NICE guidance and raise awareness with GPs on the use of direct access to colonoscopy and flexible sigmoidoscopy. £ 300, 000 QP 2: More GP e-referrals March 2017 performance to exceed March 2016 performance by 20 percentage points. In December 2015, 38% CAB utilisation was reported (HSCIC). Planned Care and Long Term Conditions Programme Boards will review baseline data when this becomes available. Input will be required from other Programme Boards to achieve this Quality Premium measure. 20% £ 300, 000 QP 3: Overall experience of making a GP appointment Demonstrate 3% increase from July 2016 publication in July 2017 publication on the percentage of respondents who said they had a good experience of making an appointment. Latest (January 2016) results: Good: 71% Poor: 21% Primary Care Quality Programme Board Satisfaction with booking an appointment should increase through • Results of demand management work with the GP Confederation • Results of workforce work being carried out under Devolution 20% £ 300, 000 QP 4: Antimicrobial resistance (AMR) improving antibiotic prescribing in primary care Part a) reduction in the number of antibiotics prescribed in primary care. Stay below 1. 161 items per STAR-PU 0. 750 antibacterial items per STARPU 13 for the latest 12 months (year to December 2015). Plans for reducing primarily use of broad spectrum antibiotics but also managing demand of antibiotics & hence volume of antibiotics are in place for 2016/17 5% £ 75, 000 Part b) reduction in the proportion of broad spectrum antibiotics prescribed in primary care to 12% 13. 1% year to December 2015. S/A 5% £ 75, 000 27 Relative Value Absolute Value
Quality Premium 2016/17 - mandatory Mandatory QP Measures Target CCG Baseline Programme Board Proposed Actions QP 1: Cancers diagnosed at early stage Demonstrate a 4% point improvement in the proportion of cancers 51% in 2013 (National Cancer Registry) 1. Fully explore data and reasons why some 20% patients are not staged. 2. Focus on 2 highest impact areas – lung and colorectal cancer. 3. Primary Care Clinical Lead to increase education of new NICE guidance and raise awareness with GPs on the use of direct access to colonoscopy and flexible sigmoidoscopy. £ 300, 000 QP 2: More GP e-referrals March 2017 performance to exceed March 2016 performance by 20 percentage points. In December 2015, 38% CAB utilisation was reported (HSCIC). Planned Care and Long Term Conditions Programme Boards will review baseline data when this becomes available. Input will be required from other Programme Boards to achieve this Quality Premium measure. 20% £ 300, 000 QP 3: Overall experience of making a GP appointment Demonstrate 3% increase from July 2016 publication in July 2017 publication on the percentage of respondents who said they had a good experience of making an appointment. Latest (January 2016) results: Good: 71% Poor: 21% Primary Care Quality Programme Board Satisfaction with booking an appointment should increase through • Results of demand management work with the GP Confederation • Results of workforce work being carried out under Devolution 20% £ 300, 000 QP 4: Antimicrobial resistance (AMR) improving antibiotic prescribing in primary care Part a) reduction in the number of antibiotics prescribed in primary care. Stay below 1. 161 items per STAR-PU 0. 750 antibacterial items per STARPU 13 for the latest 12 months (year to December 2015). Plans for reducing primarily use of broad spectrum antibiotics but also managing demand of antibiotics & hence volume of antibiotics are in place for 2016/17 5% £ 75, 000 Part b) reduction in the proportion of broad spectrum antibiotics prescribed in primary care to 12% 13. 1% year to December 2015. S/A 5% £ 75, 000 27 Relative Value Absolute Value
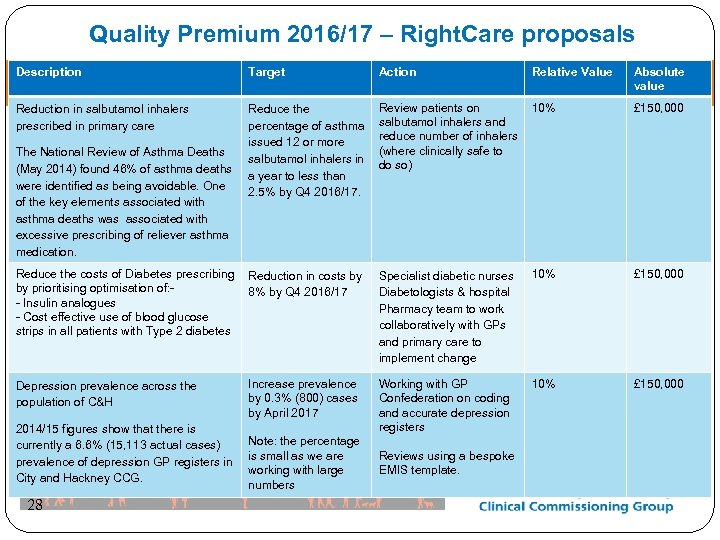 Quality Premium 2016/17 – Right. Care proposals Description Target Action Reduction in salbutamol inhalers prescribed in primary care Reduce the percentage of asthma issued 12 or more salbutamol inhalers in a year to less than 2. 5% by Q 4 2016/17. Review patients on 10% salbutamol inhalers and reduce number of inhalers (where clinically safe to do so) £ 150, 000 Specialist diabetic nurses Diabetologists & hospital Pharmacy team to work collaboratively with GPs and primary care to implement change 10% £ 150, 000 Working with GP Confederation on coding and accurate depression registers 10% £ 150, 000 The National Review of Asthma Deaths (May 2014) found 46% of asthma deaths were identified as being avoidable. One of the key elements associated with asthma deaths was associated with excessive prescribing of reliever asthma medication. Reduce the costs of Diabetes prescribing Reduction in costs by by prioritising optimisation of: 8% by Q 4 2016/17 - Insulin analogues - Cost effective use of blood glucose strips in all patients with Type 2 diabetes Depression prevalence across the population of C&H 2014/15 figures show that there is currently a 6. 6% (15, 113 actual cases) prevalence of depression GP registers in City and Hackney CCG. 28 Increase prevalence by 0. 3% (800) cases by April 2017 Note: the percentage is small as we are working with large numbers Reviews using a bespoke EMIS template. Relative Value Absolute value
Quality Premium 2016/17 – Right. Care proposals Description Target Action Reduction in salbutamol inhalers prescribed in primary care Reduce the percentage of asthma issued 12 or more salbutamol inhalers in a year to less than 2. 5% by Q 4 2016/17. Review patients on 10% salbutamol inhalers and reduce number of inhalers (where clinically safe to do so) £ 150, 000 Specialist diabetic nurses Diabetologists & hospital Pharmacy team to work collaboratively with GPs and primary care to implement change 10% £ 150, 000 Working with GP Confederation on coding and accurate depression registers 10% £ 150, 000 The National Review of Asthma Deaths (May 2014) found 46% of asthma deaths were identified as being avoidable. One of the key elements associated with asthma deaths was associated with excessive prescribing of reliever asthma medication. Reduce the costs of Diabetes prescribing Reduction in costs by by prioritising optimisation of: 8% by Q 4 2016/17 - Insulin analogues - Cost effective use of blood glucose strips in all patients with Type 2 diabetes Depression prevalence across the population of C&H 2014/15 figures show that there is currently a 6. 6% (15, 113 actual cases) prevalence of depression GP registers in City and Hackney CCG. 28 Increase prevalence by 0. 3% (800) cases by April 2017 Note: the percentage is small as we are working with large numbers Reviews using a bespoke EMIS template. Relative Value Absolute value
 Quality Premium 2016/17 Next Steps • Received feedback from CCF • Develop robust plans ready for submission to NHSE with the operating plan on 11. 4. 16 • Sign off from CEC and Governing Body 29
Quality Premium 2016/17 Next Steps • Received feedback from CCF • Develop robust plans ready for submission to NHSE with the operating plan on 11. 4. 16 • Sign off from CEC and Governing Body 29
 END | NOTES
END | NOTES
 Bi-Lingual Advocacy Services Clinical Commissioning Forum April 2016
Bi-Lingual Advocacy Services Clinical Commissioning Forum April 2016
 The Service The service is provided by the Homerton UHFT under the Community Health Services (CHS) contract with the CCG. Contract value £ 860 k The Bi-Lingual Advocacy Service is for Non-English speaking patients and provides: • Face to Face Interpreting Services to community and primary care services • Telephone Interpreting Services to community and primary care services • Advocacy is part of the general offer and in simple terms provides support to patients in assessing choices and making decisions in addition to the interpreting 32
The Service The service is provided by the Homerton UHFT under the Community Health Services (CHS) contract with the CCG. Contract value £ 860 k The Bi-Lingual Advocacy Service is for Non-English speaking patients and provides: • Face to Face Interpreting Services to community and primary care services • Telephone Interpreting Services to community and primary care services • Advocacy is part of the general offer and in simple terms provides support to patients in assessing choices and making decisions in addition to the interpreting 32
 Issues The service has always offered face to face advocacy using its own staff and regular bank staff supported by telephone translation but over the years the demand range of languages has increased in excess of in house staff and bank resourcing and this has led to rationing of face to face and more reliance on telephone translation services e. g. language line. However, rationing hasn’t fixed the issue of increasing demand the service feels that without increased resources that their future offer to GPs and primary care should be telephone interpreting and face to face advocacy has to be withdrawn. Apart from BSL there may be scope for some specific criteria to exceptions where face to face may still be provided. 33
Issues The service has always offered face to face advocacy using its own staff and regular bank staff supported by telephone translation but over the years the demand range of languages has increased in excess of in house staff and bank resourcing and this has led to rationing of face to face and more reliance on telephone translation services e. g. language line. However, rationing hasn’t fixed the issue of increasing demand the service feels that without increased resources that their future offer to GPs and primary care should be telephone interpreting and face to face advocacy has to be withdrawn. Apart from BSL there may be scope for some specific criteria to exceptions where face to face may still be provided. 33
 Inequalities The current model risks promoting health inequalities as the model of in house bi lingual advocacy can only accommodate certain community languages and also may by default scope out patients who may benefit from advocacy but do not have a language need i. e. English speaking patients. There is a wide variance in utilisation of advocacy across general practice – Some practices do not use at all! Several practices have access to advocacy via subcontracts with Derman and the Hackney Chinese Community service who provide the service with set sessions – these may not reflect need Some languages get the full advocacy service but where there is no existing in house staff or regular bank staff to cover these are contracted out to interpreting services. BSL provision is not provided in house and access is variable. • • • 34
Inequalities The current model risks promoting health inequalities as the model of in house bi lingual advocacy can only accommodate certain community languages and also may by default scope out patients who may benefit from advocacy but do not have a language need i. e. English speaking patients. There is a wide variance in utilisation of advocacy across general practice – Some practices do not use at all! Several practices have access to advocacy via subcontracts with Derman and the Hackney Chinese Community service who provide the service with set sessions – these may not reflect need Some languages get the full advocacy service but where there is no existing in house staff or regular bank staff to cover these are contracted out to interpreting services. BSL provision is not provided in house and access is variable. • • • 34
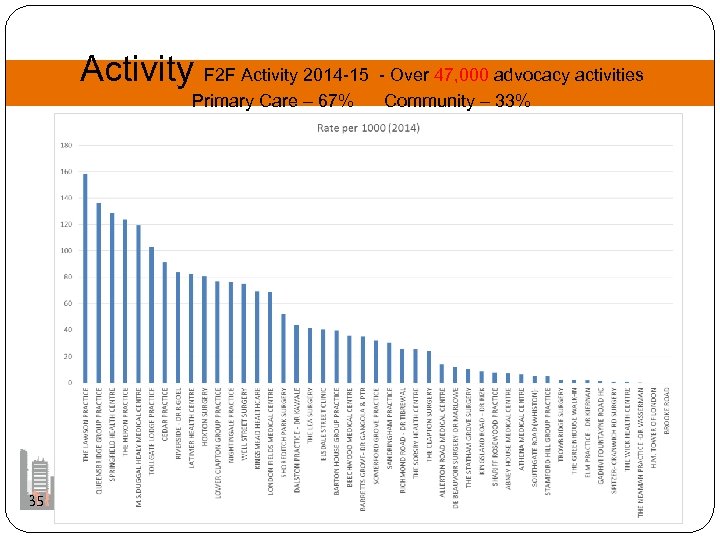 Activity F 2 F Activity 2014 -15 - Over 47, 000 advocacy activities Primary Care – 67% Community – 33% 35
Activity F 2 F Activity 2014 -15 - Over 47, 000 advocacy activities Primary Care – 67% Community – 33% 35
 What do we need to commission? • The current bi-lingual advocacy model is not financially sustainable but will changes such as increasing telephone interpreting, reducing in-house advocacy, adapting criteria address sustainability? • The service doesn’t separate advocacy (associated with all patients with mental or physical impairment rather than language/culture) Is this fair to other groups that we don’t commission advocacy for? Should we be commissioning language services and advocacy separately? • Inequalities need to be addressed - we need a service that is fair to all and meets need and not demand. • Some practices either don’t use or use very little face to face interpretation – Why and is there something that can be learned and shared? • Many other London CCG areas rely entirely on telephone interpreting for GP practices - Is there a need for F 2 F or is it a preference? 36
What do we need to commission? • The current bi-lingual advocacy model is not financially sustainable but will changes such as increasing telephone interpreting, reducing in-house advocacy, adapting criteria address sustainability? • The service doesn’t separate advocacy (associated with all patients with mental or physical impairment rather than language/culture) Is this fair to other groups that we don’t commission advocacy for? Should we be commissioning language services and advocacy separately? • Inequalities need to be addressed - we need a service that is fair to all and meets need and not demand. • Some practices either don’t use or use very little face to face interpretation – Why and is there something that can be learned and shared? • Many other London CCG areas rely entirely on telephone interpreting for GP practices - Is there a need for F 2 F or is it a preference? 36
 Plan • Re-specify service specification with the involvement of all stakeholders including voluntary sector • Get broad agreement on service model • Benchmark service costs with other models 37
Plan • Re-specify service specification with the involvement of all stakeholders including voluntary sector • Get broad agreement on service model • Benchmark service costs with other models 37
 END | NOTES
END | NOTES


