11 Ижевск Final.pptx
- Количество слайдов: 67
ЦИТОЛОГИЧЕСКАЯ ДИАГНОСТИКА ЗЛОКАЧЕСТВЕННЫХ НОВООБРАЗОВАНИЙ ЛЕГКИХ КРАВЦОВ В. Г. , К. М. Н, ЧЛЕН МЕЖДУНАРОДНОЙ АКАДЕМИИ ЦИТОЛОГИИ, ЗАВЕДУЮЩИЙ ЦИТОПАТОЛОГИЕЙ МЕДИЦИНСКОГО ЦЕНТРА «МЕИР» , КФАР-САБА, ИЗРАИЛЬ
CYTOLOGICAL DIAGNOSIS OF PULMONARY NEOPLASTIC TUMORS Vladimir Kravtsov MD, Ph. D, MIAC Director of Cytopathology Unit, Meir Medical Center, Kefar-Sava, Israel
Convex-probe EBUS


Bronchoscopy suite
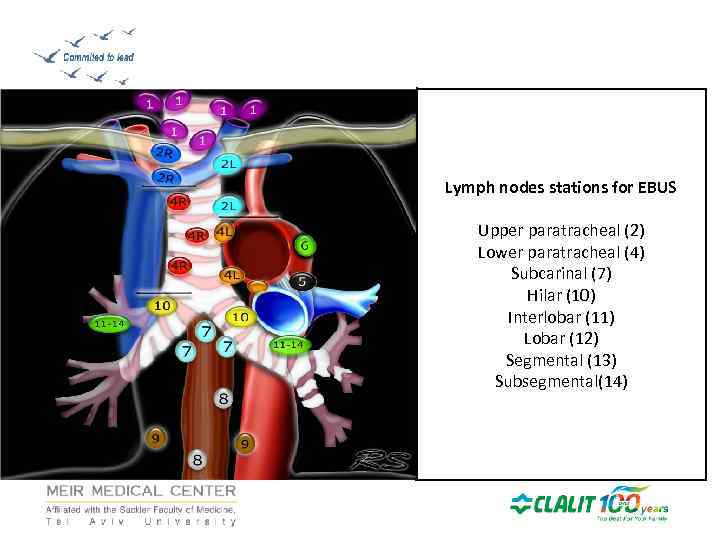
Lymph nodes stations for EBUS Upper paratracheal (2) Lower paratracheal (4) Subcarinal (7) Hilar (10) Interlobar (11) Lobar (12) Segmental (13) Subsegmental(14)
BENEFITS OF ENDOBRONCHIAL US (EBUS) Minimally invasive Outpatient procedure ROSE-Rapid Onsite Evaluation The EBUS is indicated in every case of unexplained mediastinal lymphadenopathy. • Borderline indication in highly suspicion for lymphoma. • Diagnosis and staging of lung cancer • •
Benefits of EBUS • EBUS is performed under moderate sedation or general anesthesia. • Patients recover quickly and can generally go home in the same day. • LN size above 5 mm.
Endoscopic US: Technique • • On site pathologist Conventional smears are prepared Cell blocks Three or more punctures 20 passes Acid fast smear and culture Flow cytometry
Why not Mediastinoscopy? • • • Surgery! Complication rate 1 -2. 6% Mortality 0. 08% Very difficult after the first procedure. No option to reach hillar adenopathy (10, 11, 12 stations).
CASES
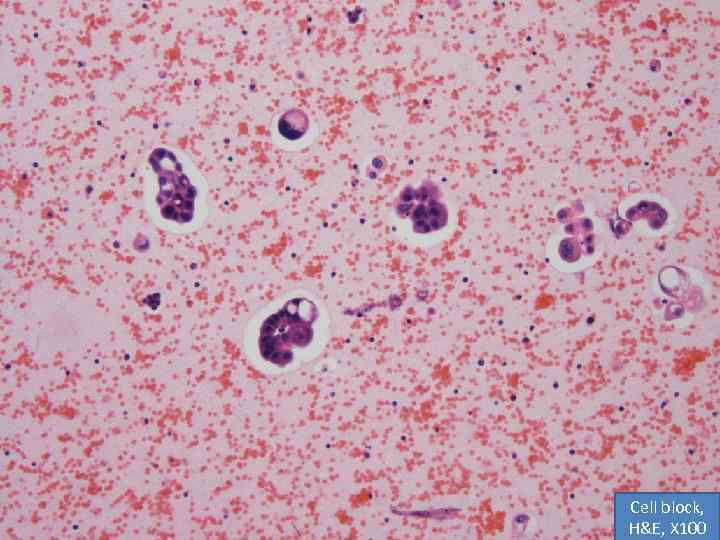
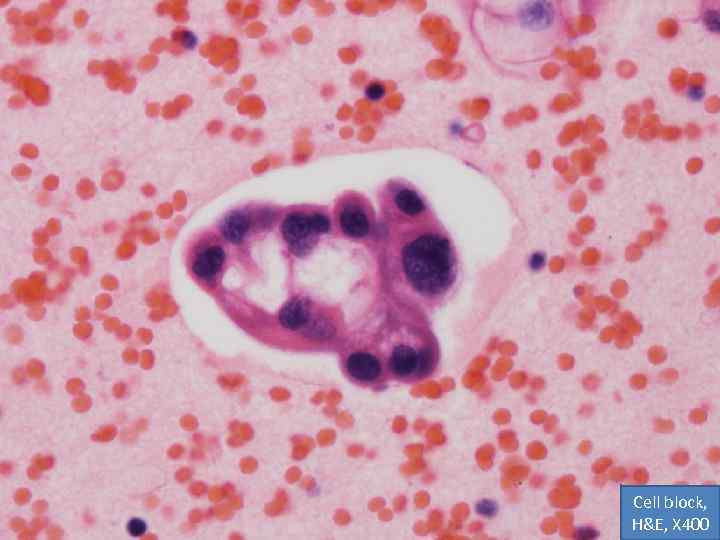
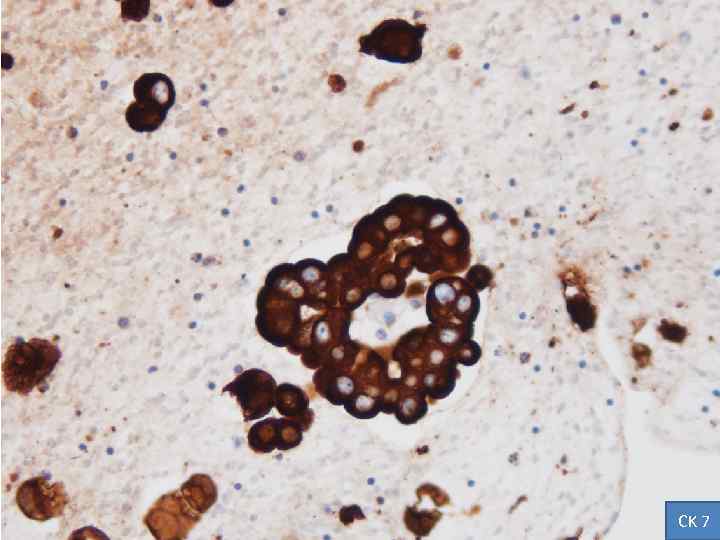
CASE 1 • Male, 65 y. o. • Multiple brain lesions (mts? ) by CT • Mediastinal lymphadenopathy (hilar lymph nodes of Rt. Lung? ) • History of TCC (2010), cystoscopy with biopsy: negative for malignancy (2013) • Clinical diagnosis: secondary neoplasm (SCLC? ) • EBUS: FNA of subcarinal L/N (7)

Cell block, H&E, X 100
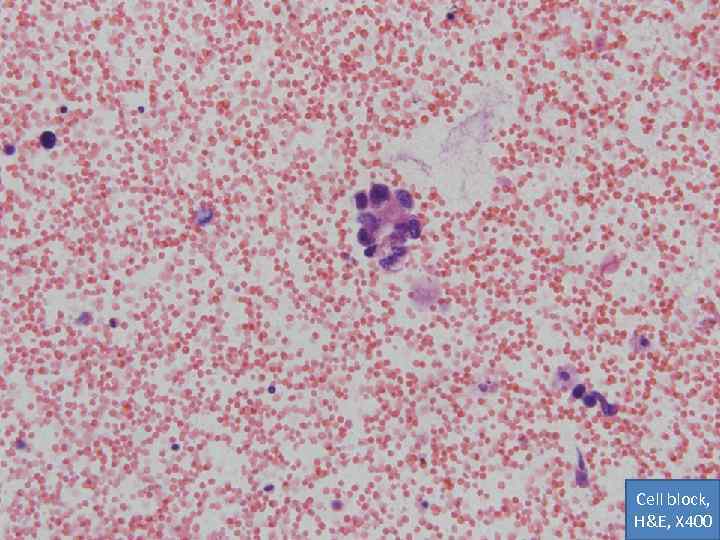
Cell block, H&E, X 400
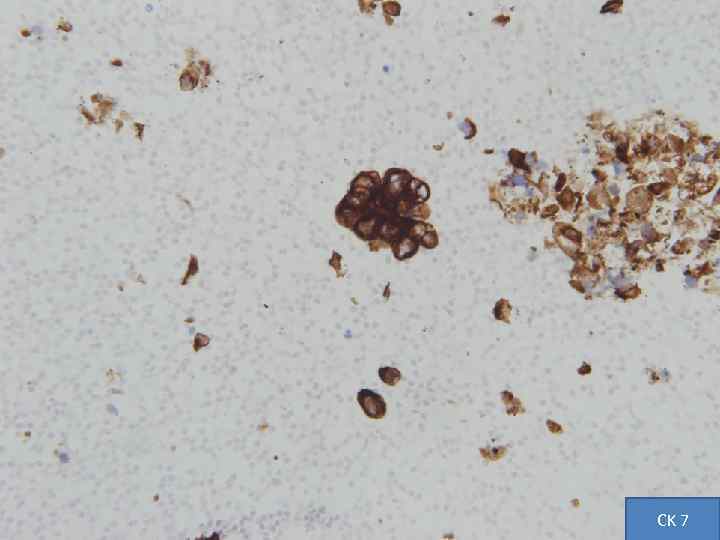
CK 7

TTF-1
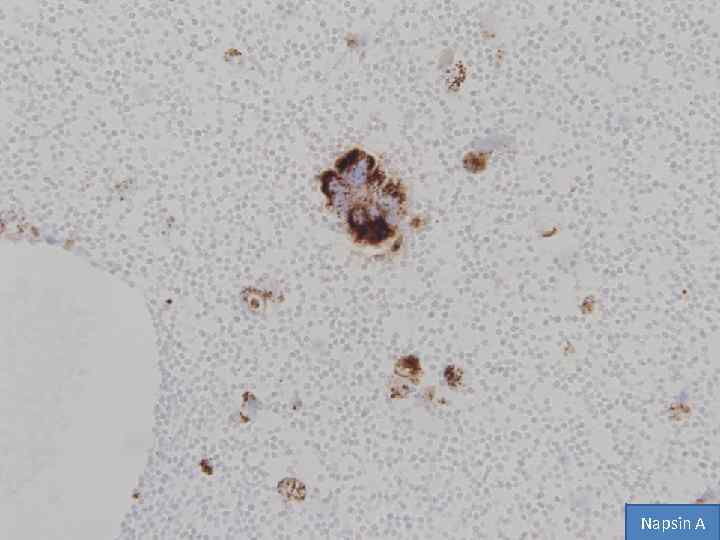
Napsin A
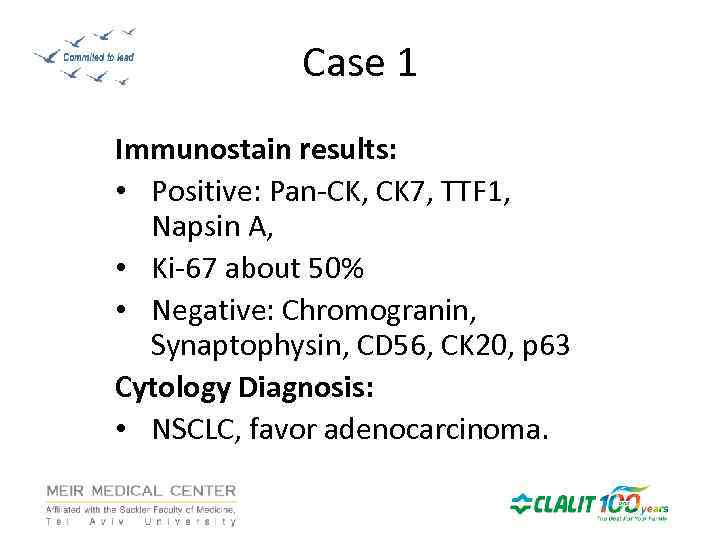
Case 1 Immunostain results: • Positive: Pan-CK, CK 7, TTF 1, Napsin A, • Ki-67 about 50% • Negative: Chromogranin, Synaptophysin, CD 56, CK 20, p 63 Cytology Diagnosis: • NSCLC, favor adenocarcinoma.
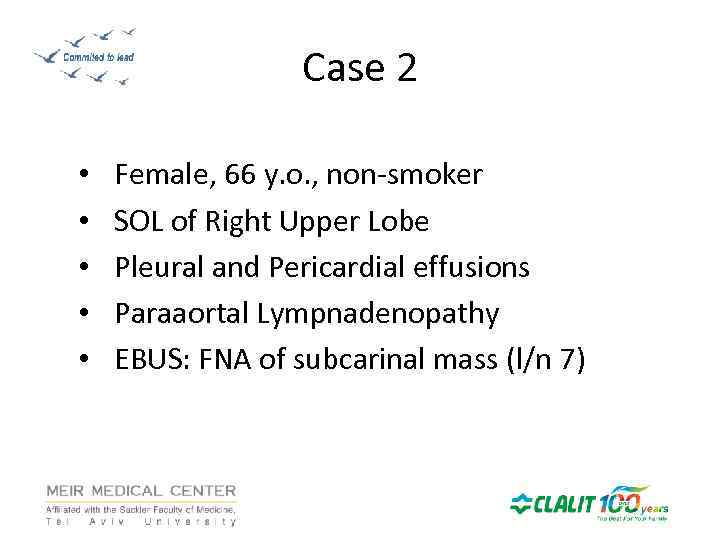
Case 2 • • • Female, 66 y. o. , non-smoker SOL of Right Upper Lobe Pleural and Pericardial effusions Paraaortal Lympnadenopathy EBUS: FNA of subcarinal mass (l/n 7)
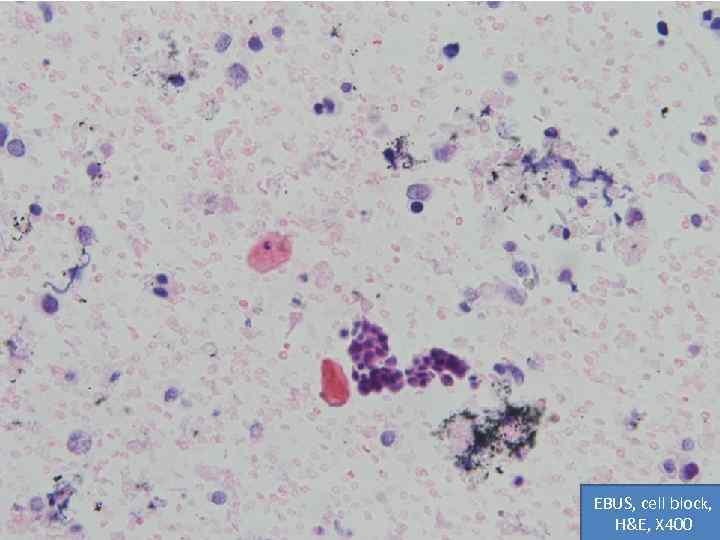
EBUS, cell block, H&E, X 400
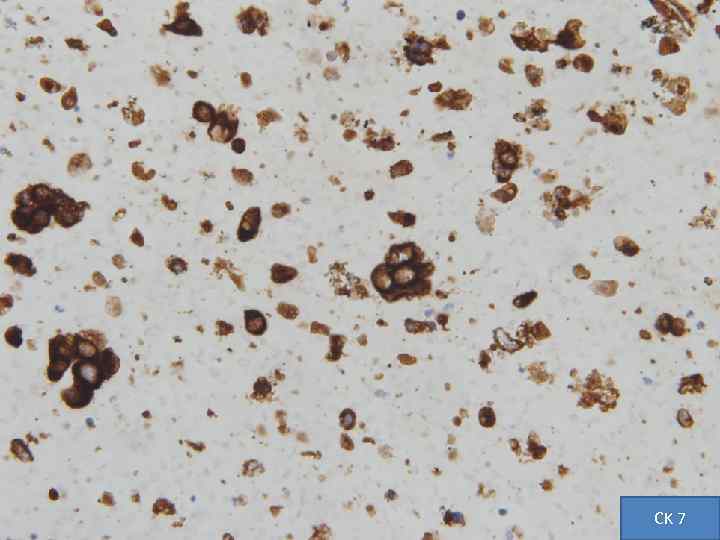
CK 7
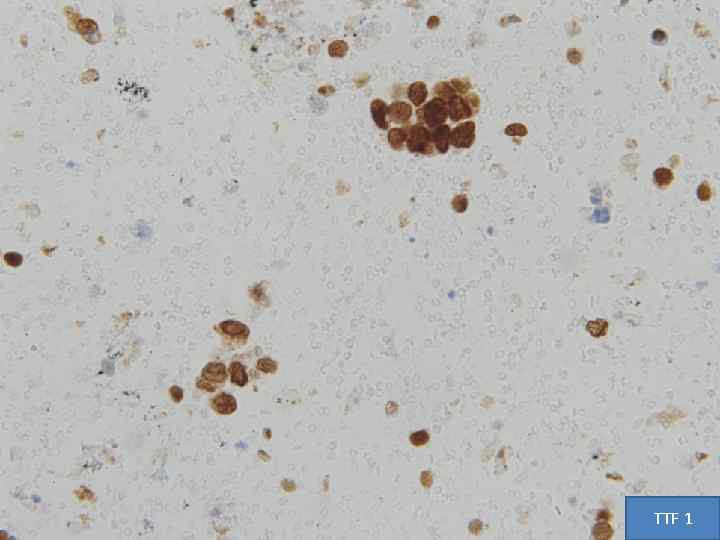
TTF 1
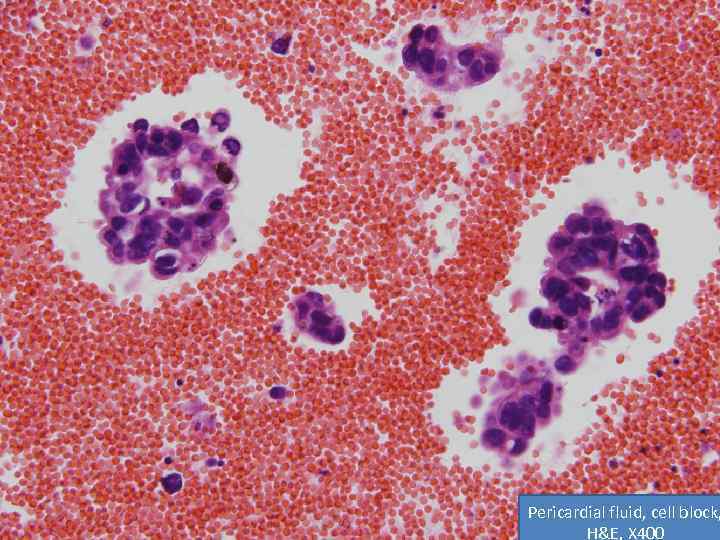
Pericardial fluid, cell block, H&E, X 400
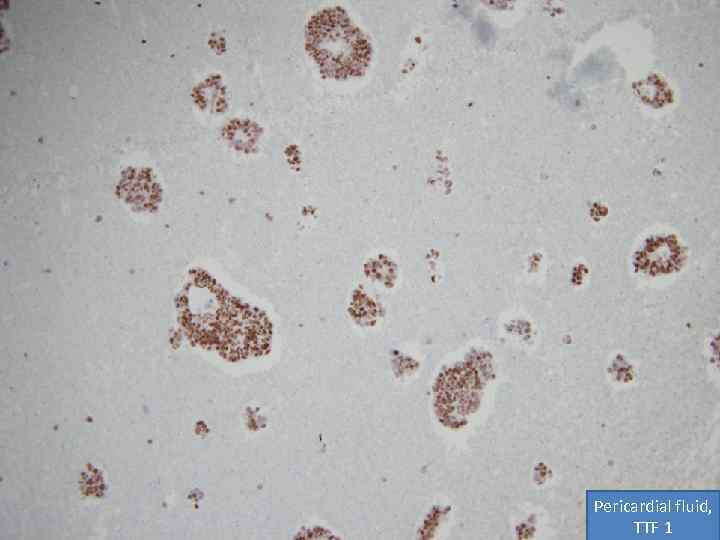
Pericardial fluid, TTF 1
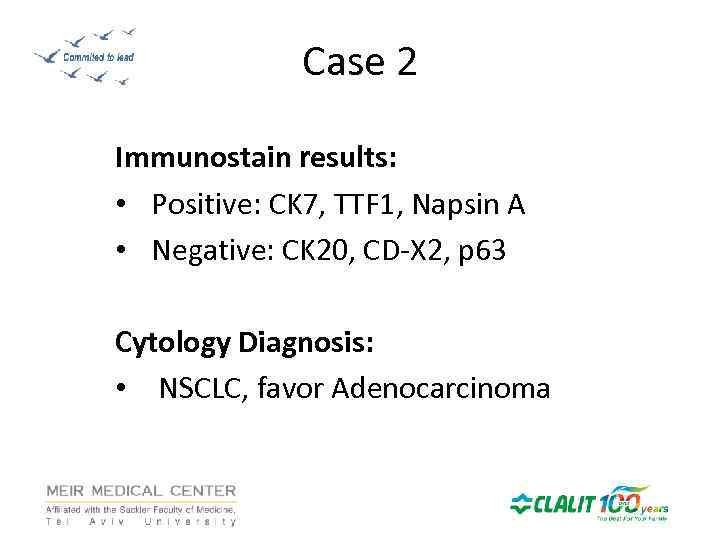
Case 2 Immunostain results: • Positive: CK 7, TTF 1, Napsin A • Negative: CK 20, CD-X 2, p 63 Cytology Diagnosis: • NSCLC, favor Adenocarcinoma
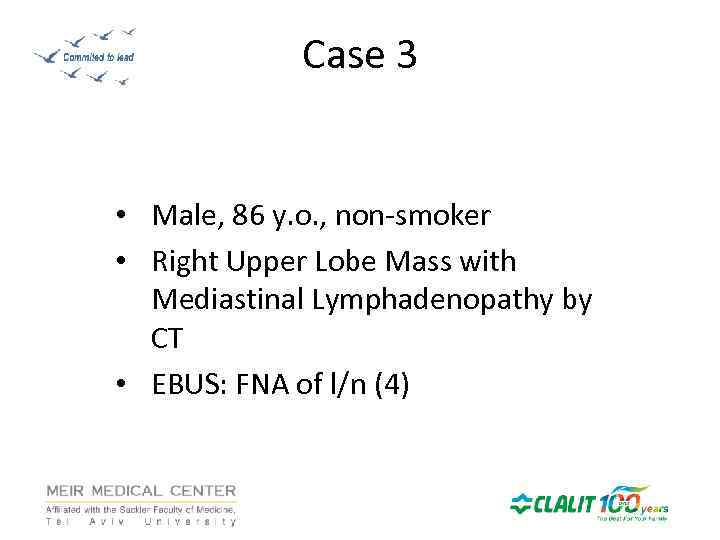
Case 3 • Male, 86 y. o. , non-smoker • Right Upper Lobe Mass with Mediastinal Lymphadenopathy by CT • EBUS: FNA of l/n (4)
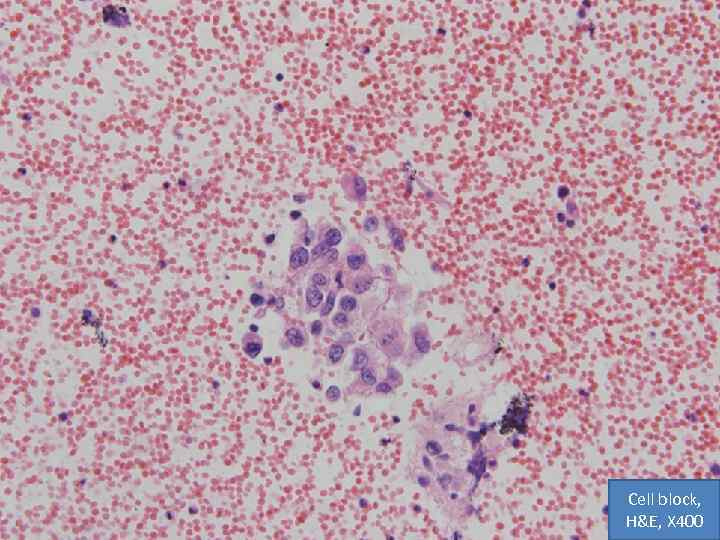
Cell block, H&E, X 400
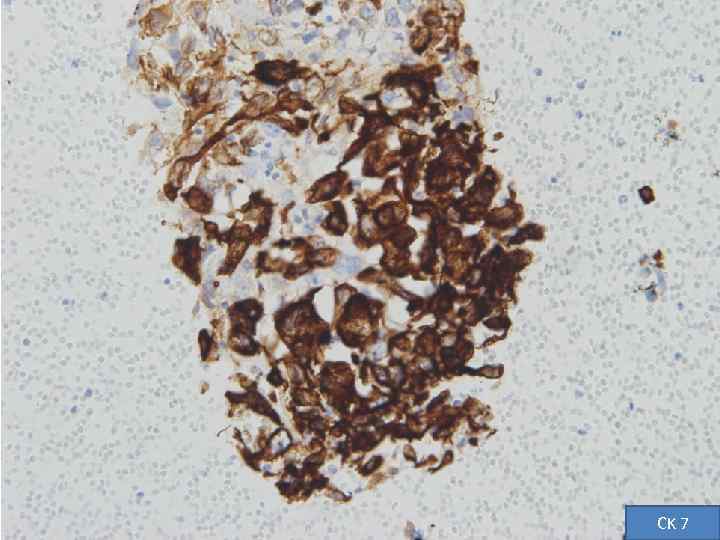
CK 7
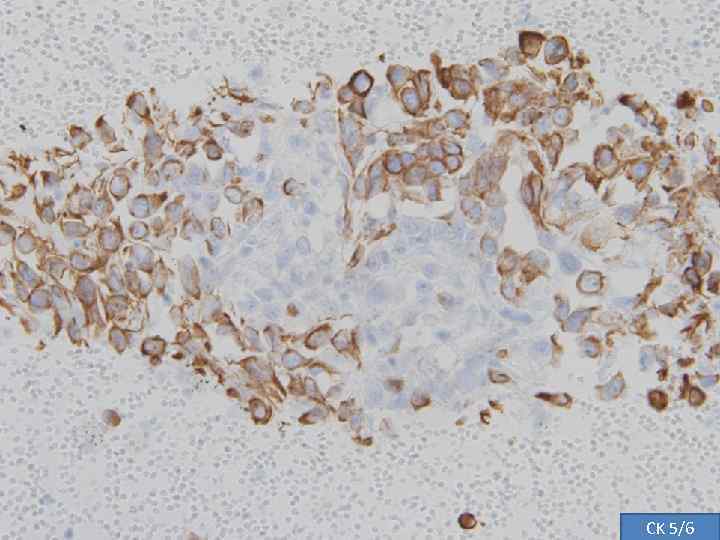
CK 5/6
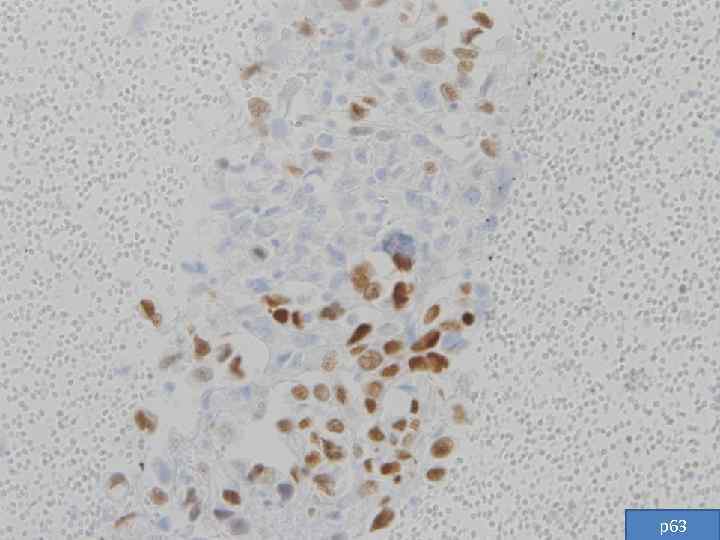
p 63
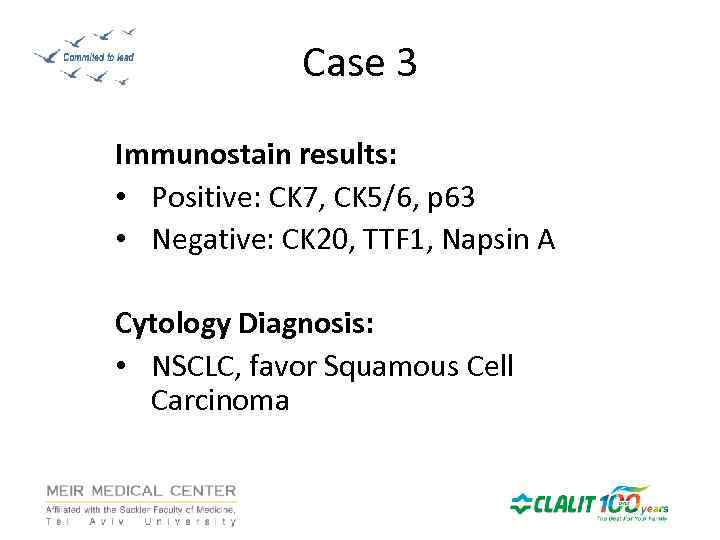
Case 3 Immunostain results: • Positive: CK 7, CK 5/6, p 63 • Negative: CK 20, TTF 1, Napsin A Cytology Diagnosis: • NSCLC, favor Squamous Cell Carcinoma
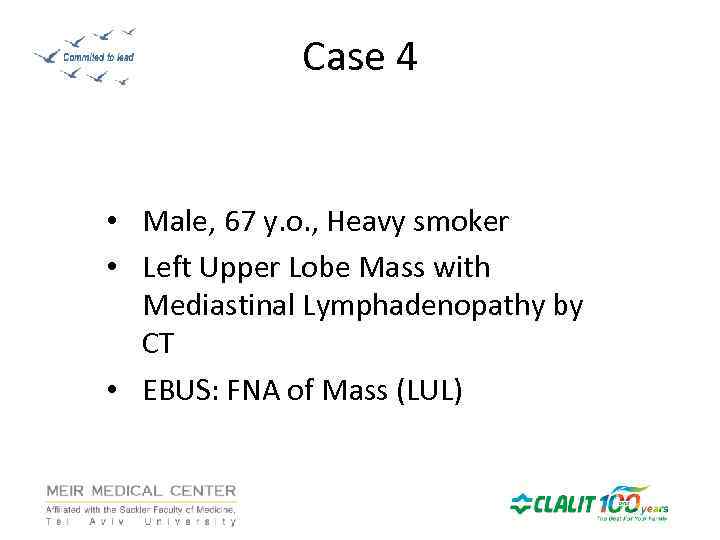
Case 4 • Male, 67 y. o. , Heavy smoker • Left Upper Lobe Mass with Mediastinal Lymphadenopathy by CT • EBUS: FNA of Mass (LUL)
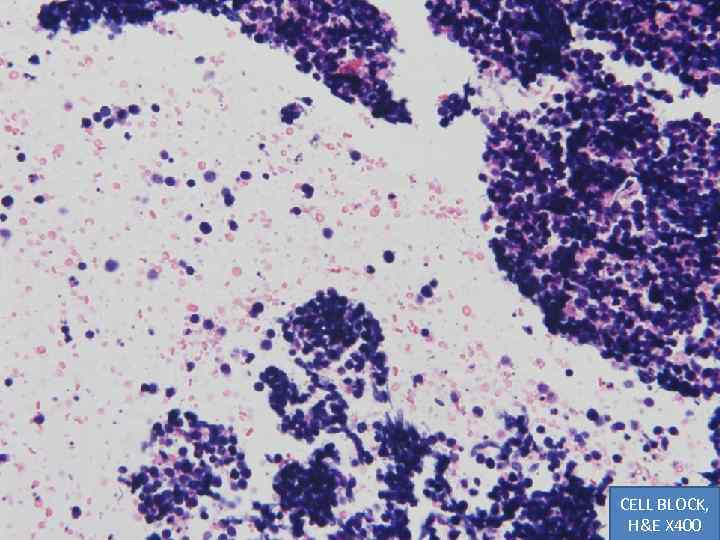
CELL BLOCK, H&E X 400
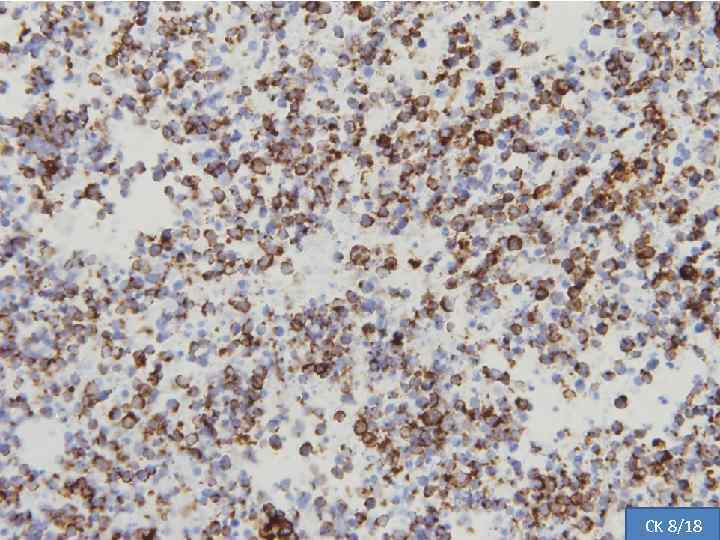
CK 8/18
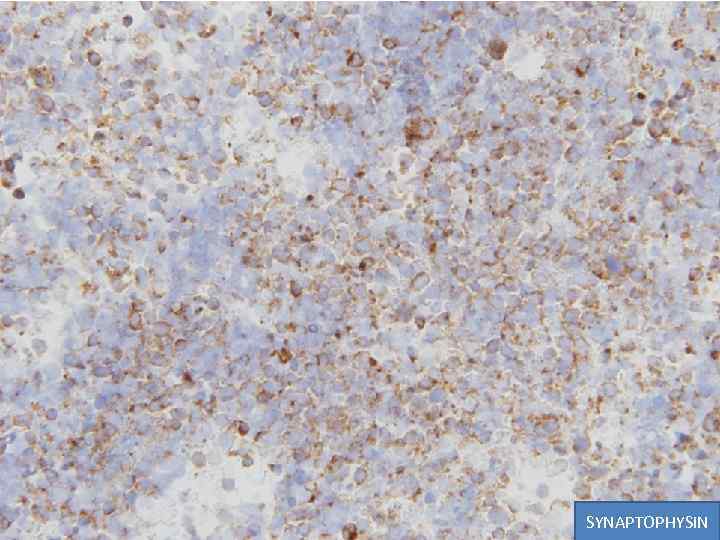
SYNAPTOPHYSIN
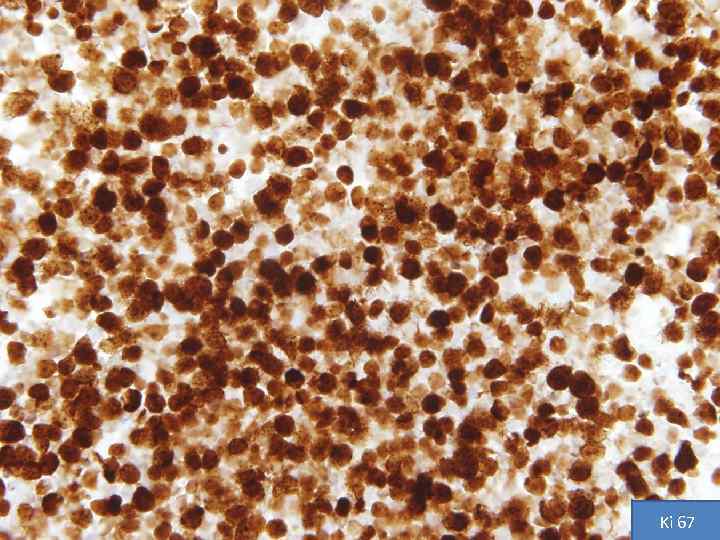
Ki 67
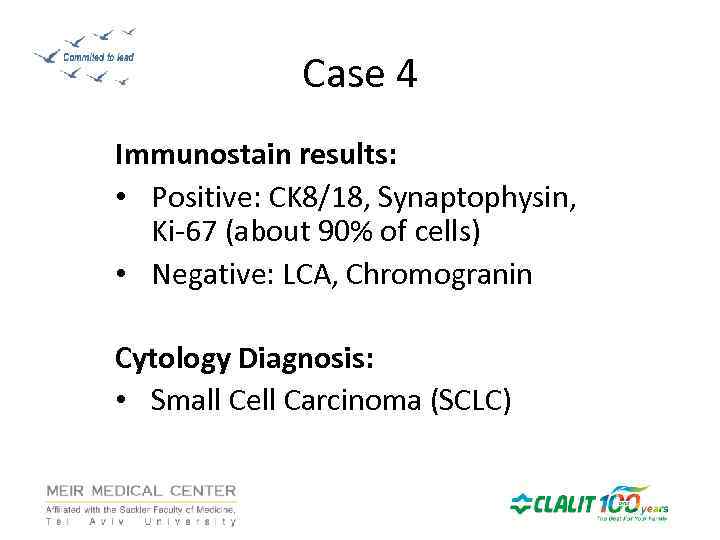
Case 4 Immunostain results: • Positive: CK 8/18, Synaptophysin, Ki-67 (about 90% of cells) • Negative: LCA, Chromogranin Cytology Diagnosis: • Small Cell Carcinoma (SCLC)
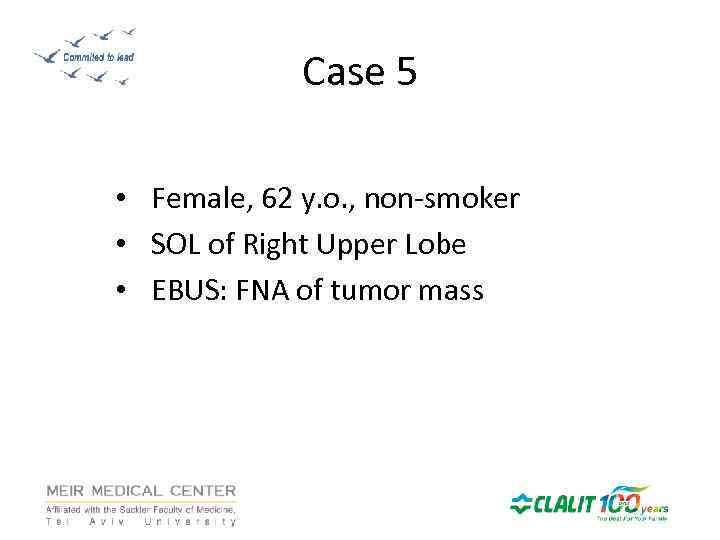
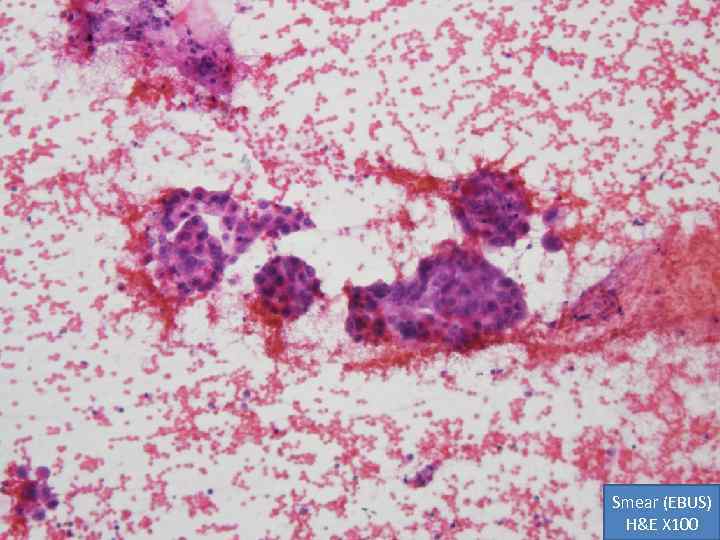
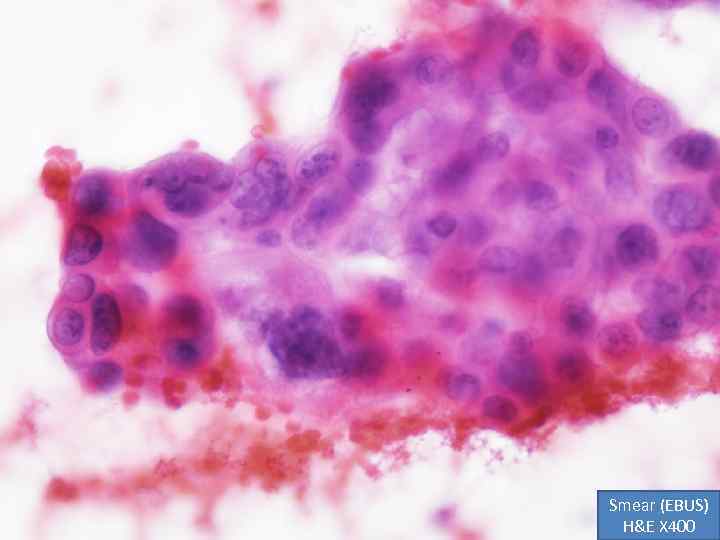
Case 5 • Female, 62 y. o. , non-smoker • SOL of Right Upper Lobe • EBUS: FNA of tumor mass
Smear (EBUS) H&E X 100
Smear (EBUS) H&E X 400
Cell block, H&E, X 100
Cell block, H&E, X 400
CK 7

CA 125
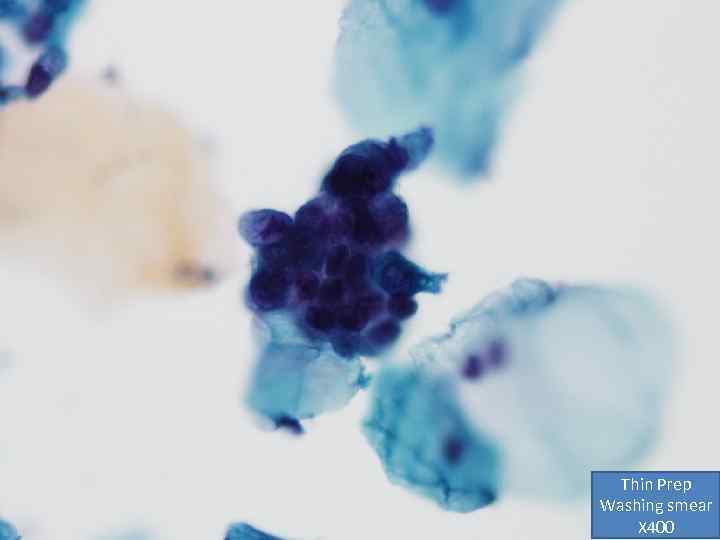
Thin Prep Washing smear X 400
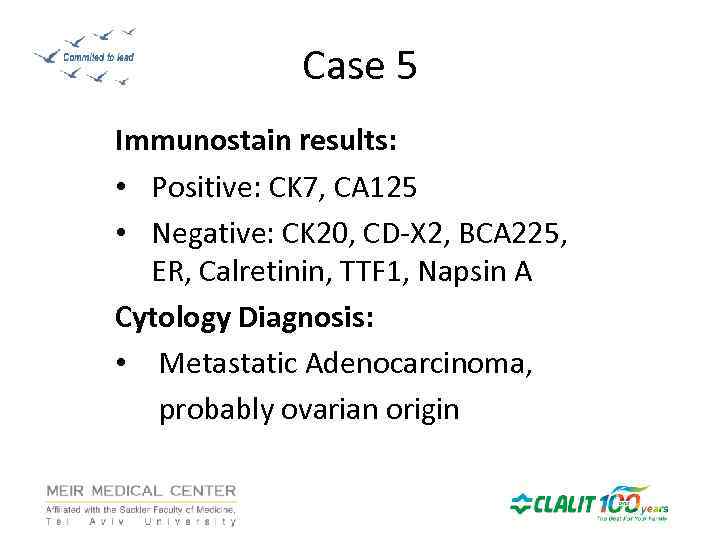
Case 5 Immunostain results: • Positive: CK 7, CA 125 • Negative: CK 20, CD-X 2, BCA 225, ER, Calretinin, TTF 1, Napsin A Cytology Diagnosis: • Metastatic Adenocarcinoma, probably ovarian origin
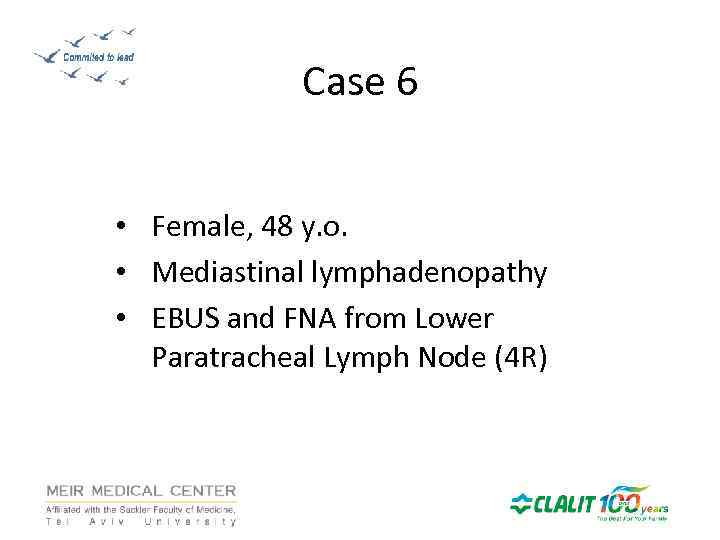
Case 6 • Female, 48 y. o. • Mediastinal lymphadenopathy • EBUS and FNA from Lower Paratracheal Lymph Node (4 R)
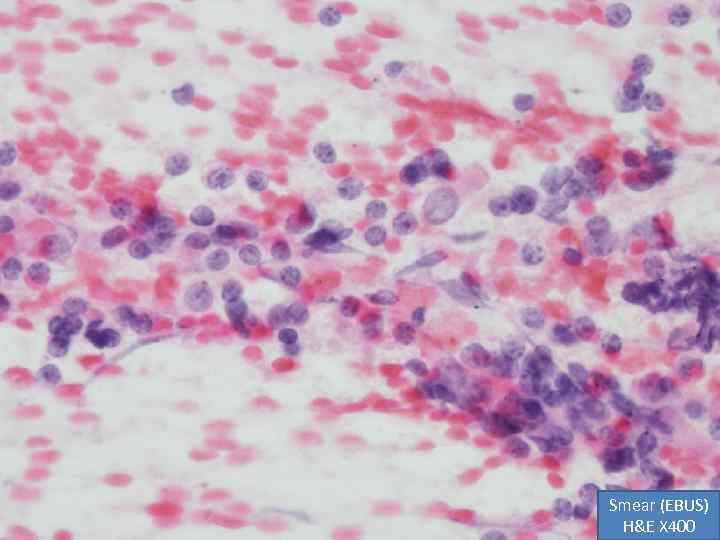
Smear (EBUS) H&E X 400
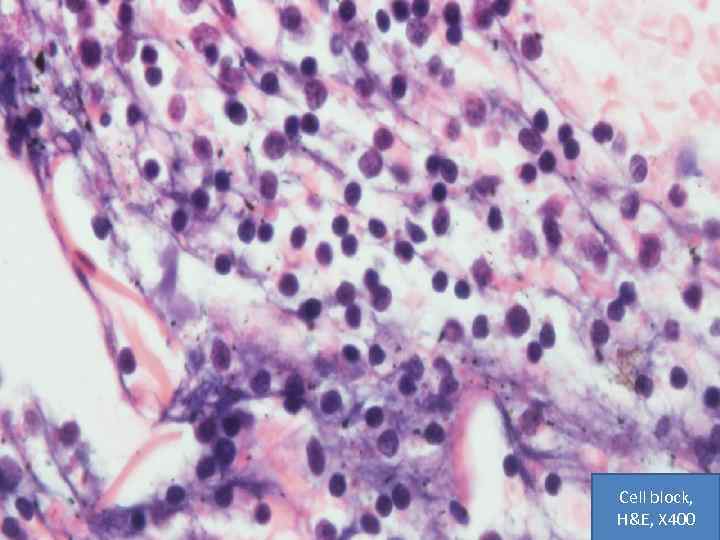
Cell block, H&E, X 400
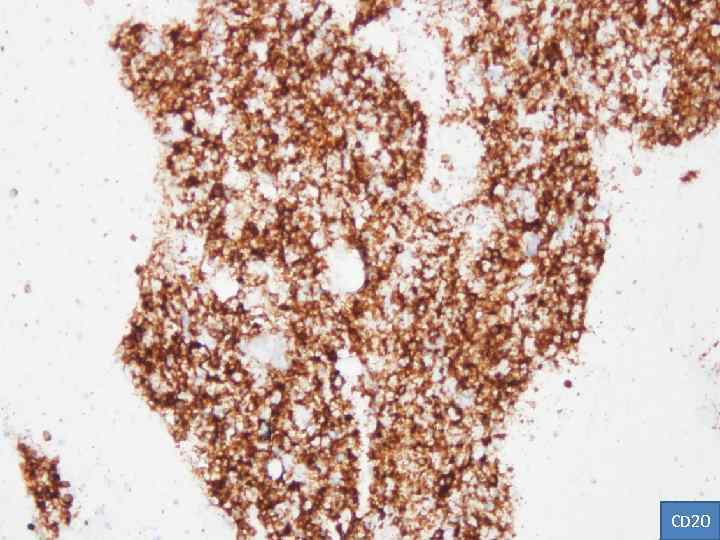
CD 20
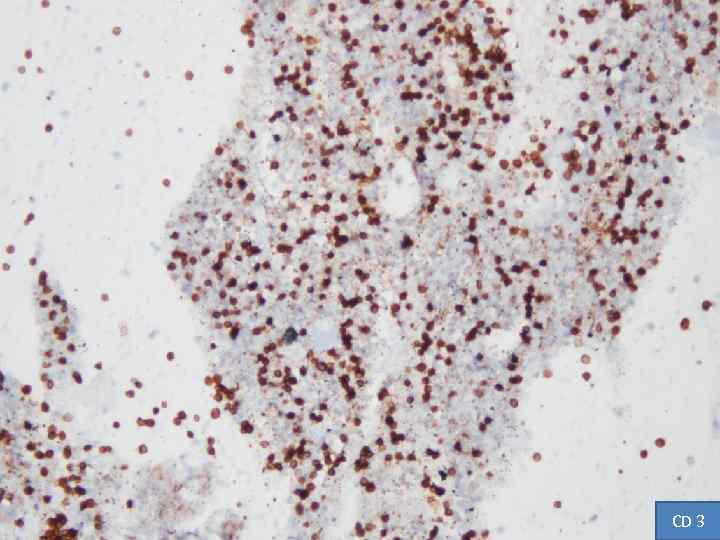
CD 3
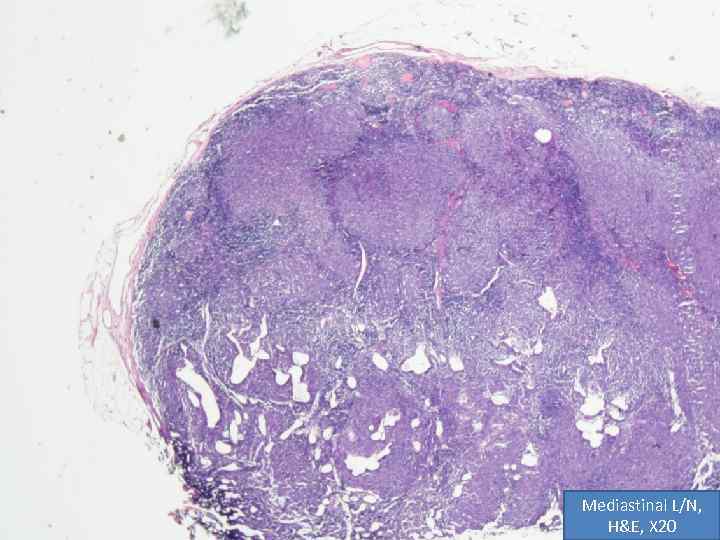
Mediastinal L/N, H&E, X 20
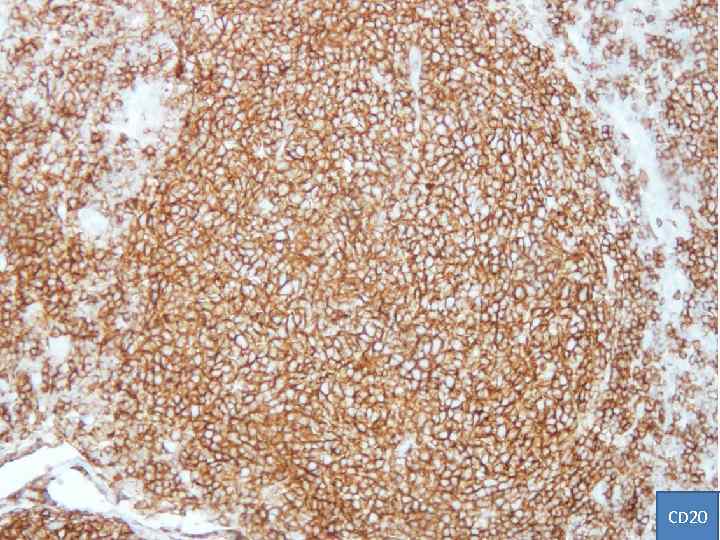
CD 20
Case 6 Immunostain results: • Positive: CD 20 and CD 3 Cytology Diagnosis: • Lymphoproliferative Disorder Pathology Diagnosis: • Follicular lymphoma, Low grade
Case 7 • Male, 76 y. o. • Mediastinal lymphadenopathy • EBUS and FNA from Subcarinal Lymph Node (7)
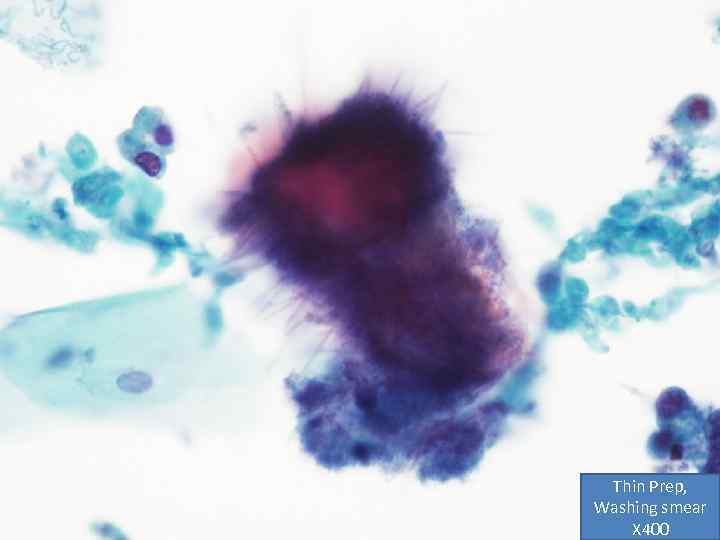
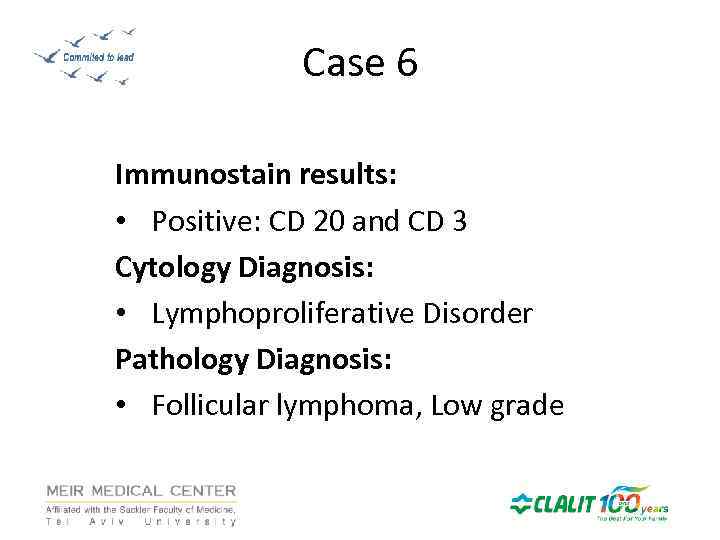
Thin Prep, Washing smear X 400
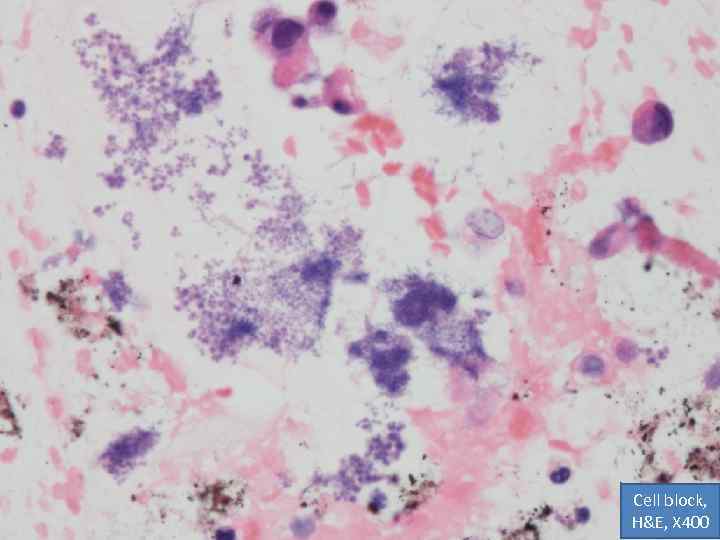
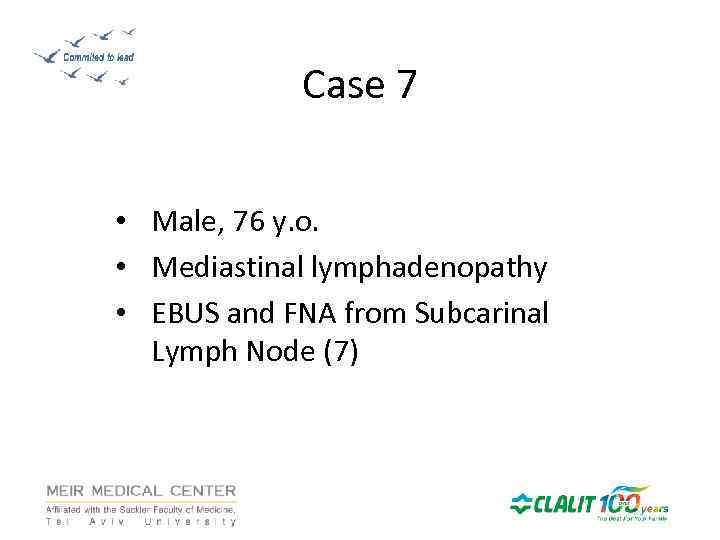
Cell block, H&E, X 400
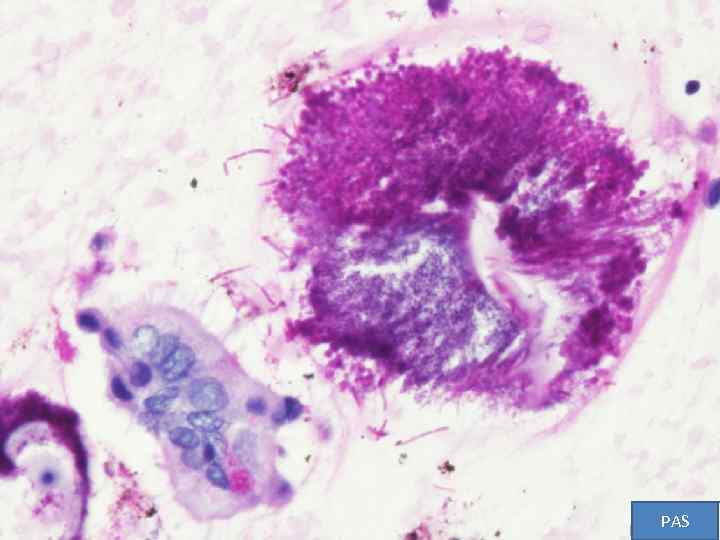
PAS
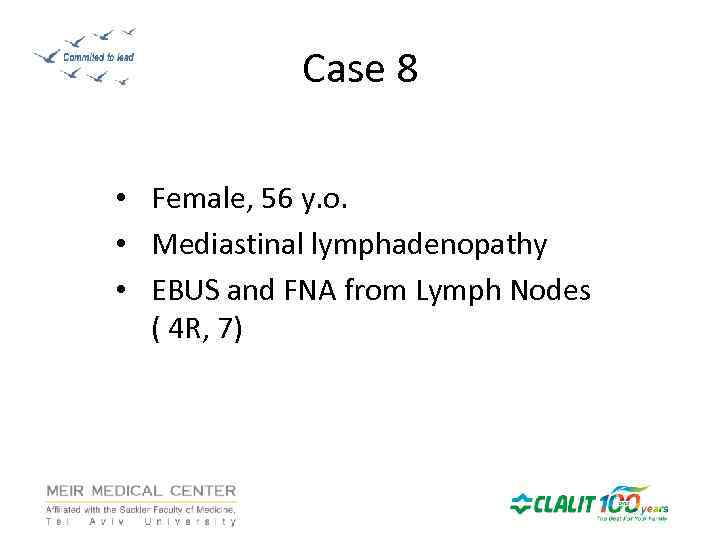
Case 8 • Female, 56 y. o. • Mediastinal lymphadenopathy • EBUS and FNA from Lymph Nodes ( 4 R, 7)
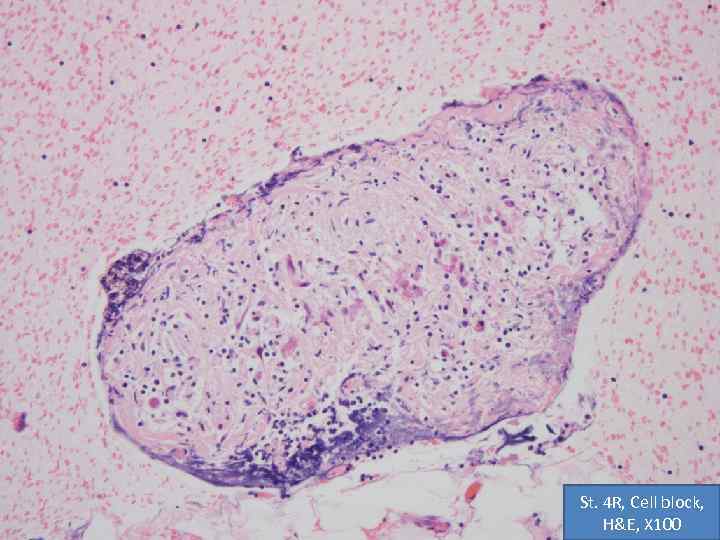
St. 4 R, Cell block, H&E, X 100

St. 4 R, Cell block, H&E, X 100
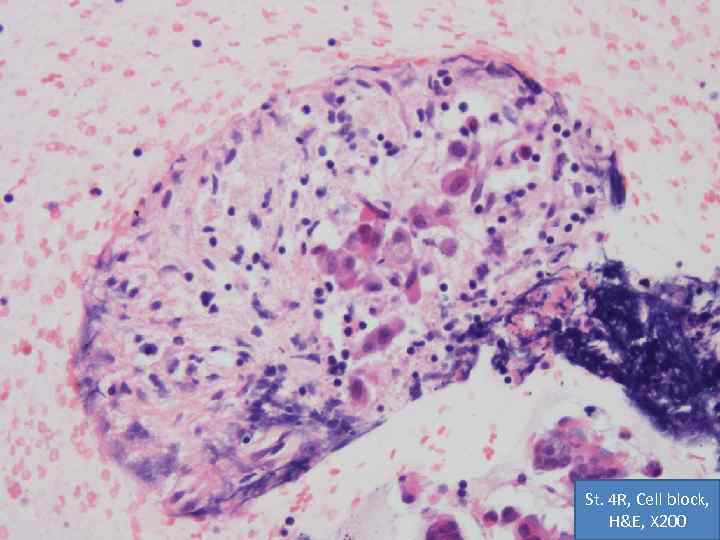
St. 4 R, Cell block, H&E, X 200
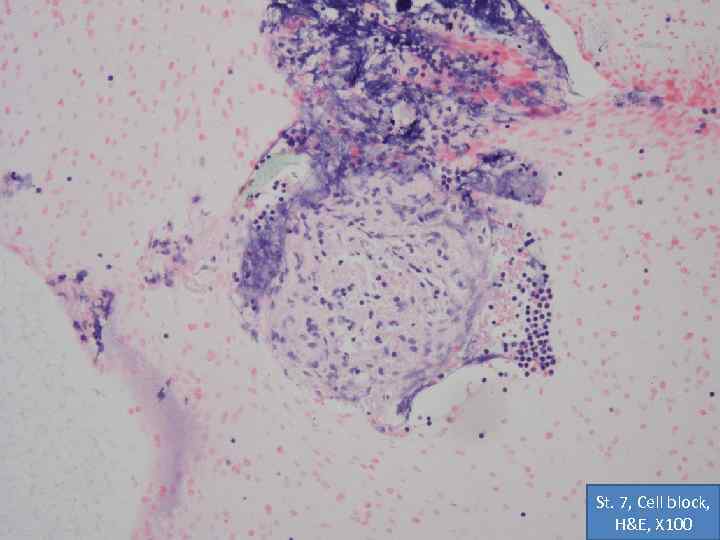
St. 7, Cell block, H&E, X 100
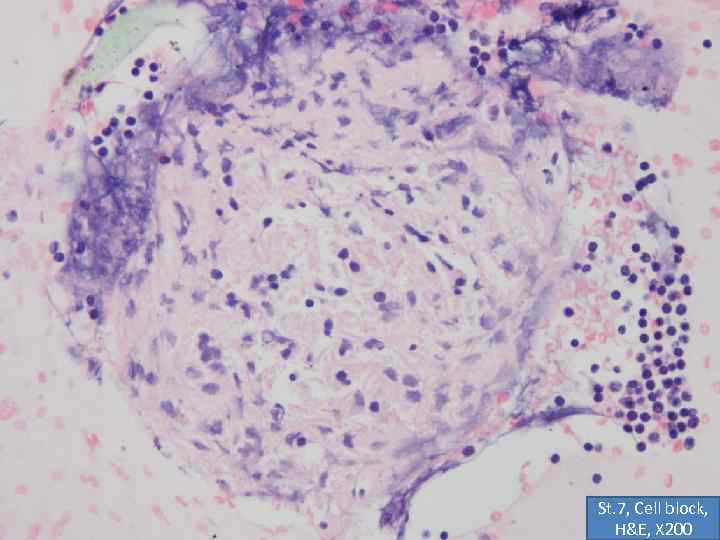
St. 7, Cell block, H&E, X 200
Case 8 Cytology Diagnosis: • Non-necrotizing epitheliod granulomas, consistent with sarcoidosis.
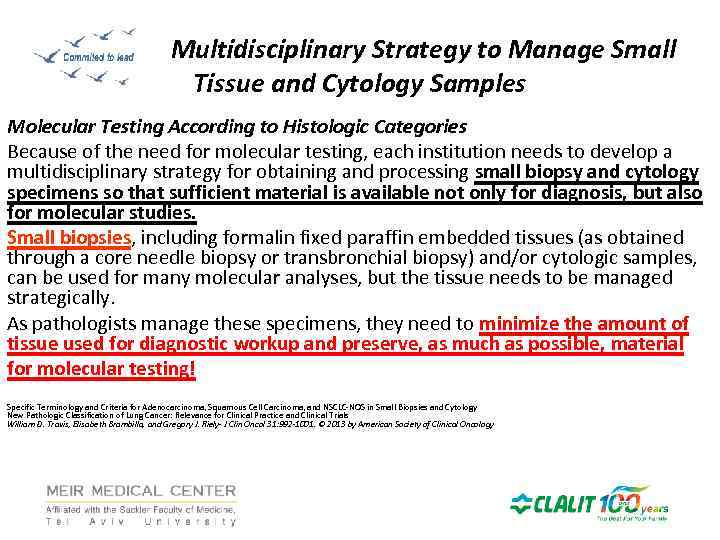
Multidisciplinary Strategy to Manage Small Tissue and Cytology Samples Molecular Testing According to Histologic Categories Because of the need for molecular testing, each institution needs to develop a multidisciplinary strategy for obtaining and processing small biopsy and cytology specimens so that sufficient material is available not only for diagnosis, but also for molecular studies. Small biopsies, including formalin fixed paraffin embedded tissues (as obtained through a core needle biopsy or transbronchial biopsy) and/or cytologic samples, can be used for many molecular analyses, but the tissue needs to be managed strategically. As pathologists manage these specimens, they need to minimize the amount of tissue used for diagnostic workup and preserve, as much as possible, material for molecular testing! Specific Terminology and Criteria for Adenocarcinoma, Squamous Cell Carcinoma, and NSCLC-NOS in Small Biopsies and Cytology New Pathologic Classification of Lung Cancer: Relevance for Clinical Practice and Clinical Trials William D. Travis, Elisabeth Brambilla, and Gregory J. Riely- J Clin Oncol 31: 992 -1001. © 2013 by American Society of Clinical Oncology

THANKS / СПАСИБО
11 Ижевск Final.pptx