e74551a96de696bb9066d0486779ad0b.ppt
- Количество слайдов: 60
 CIMIT ORF Pn. P Program “Plug-and-Play” Medical Device Interoperability Standardization Framework for the Operating Rooms of the Future A multidisciplinary program to standardize communication and control of medical devices to improve patient safety and healthcare efficiency Julian M. Goldman, MD Depts. Of Anesthesia and Biomedical Engineering Massachusetts General Hospital Harvard Medical School
CIMIT ORF Pn. P Program “Plug-and-Play” Medical Device Interoperability Standardization Framework for the Operating Rooms of the Future A multidisciplinary program to standardize communication and control of medical devices to improve patient safety and healthcare efficiency Julian M. Goldman, MD Depts. Of Anesthesia and Biomedical Engineering Massachusetts General Hospital Harvard Medical School
 From This Farnam Operating Amphitheatre, Yale New Haven http: //www. ynhh. org/general/history/oldsur. html
From This Farnam Operating Amphitheatre, Yale New Haven http: //www. ynhh. org/general/history/oldsur. html
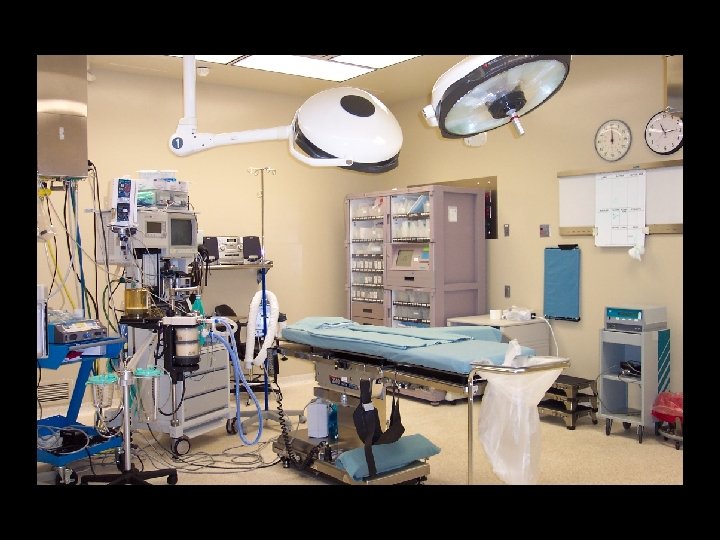
 To This
To This
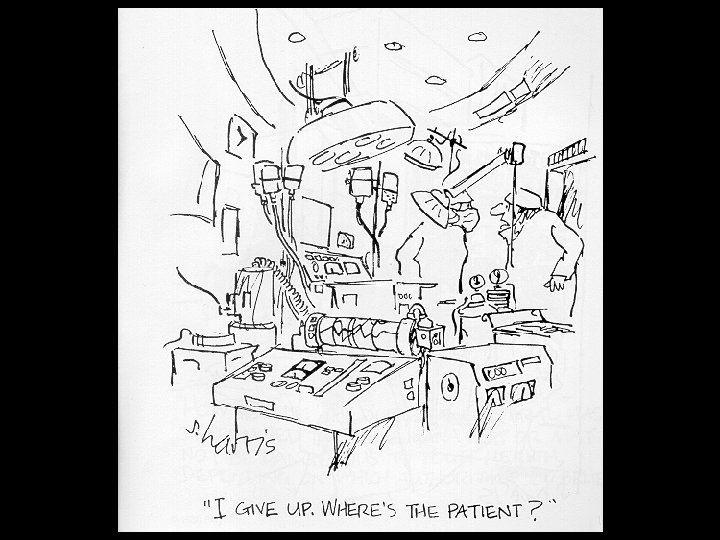
 “minimally invasive surgery” yields “maximally invasive” technology! © 2005 Julian M. Goldman, MD www. orfpnp. org
“minimally invasive surgery” yields “maximally invasive” technology! © 2005 Julian M. Goldman, MD www. orfpnp. org
 What is an “OR of the Future”? l The “Operating Room of the Future” (ORF) is not a specifically configured OR. “ORF” is shorthand for a constellation of emerging innovations in processes and technologies for perioperative care. l The “ORF” may include: l – – – Surgical robots Minimally invasive surgery suites Redesign of the perioperative environment © 2005 Julian M. Goldman, MD www. orfpnp. org
What is an “OR of the Future”? l The “Operating Room of the Future” (ORF) is not a specifically configured OR. “ORF” is shorthand for a constellation of emerging innovations in processes and technologies for perioperative care. l The “ORF” may include: l – – – Surgical robots Minimally invasive surgery suites Redesign of the perioperative environment © 2005 Julian M. Goldman, MD www. orfpnp. org
 The ORF is a “state of mind” © 2005 Julian M. Goldman, MD www. orfpnp. org
The ORF is a “state of mind” © 2005 Julian M. Goldman, MD www. orfpnp. org
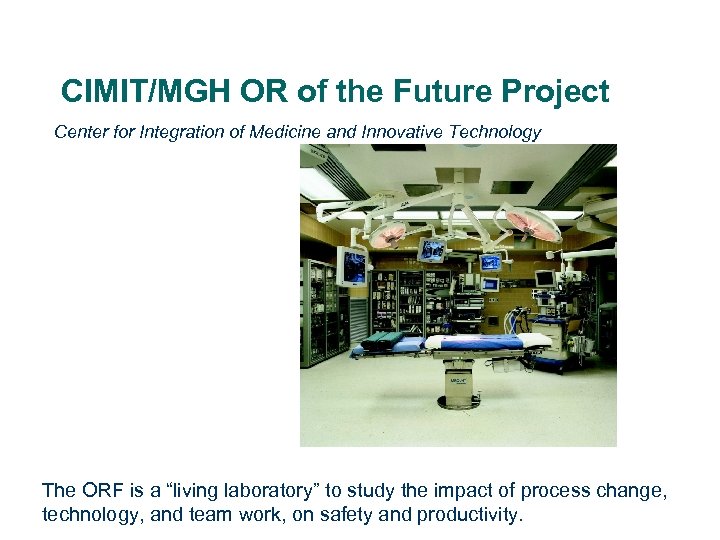 CIMIT/MGH OR of the Future Project Center for Integration of Medicine and Innovative Technology The ORF is a “living laboratory” to study the impact of process change, technology, and team work, on safety and productivity.
CIMIT/MGH OR of the Future Project Center for Integration of Medicine and Innovative Technology The ORF is a “living laboratory” to study the impact of process change, technology, and team work, on safety and productivity.
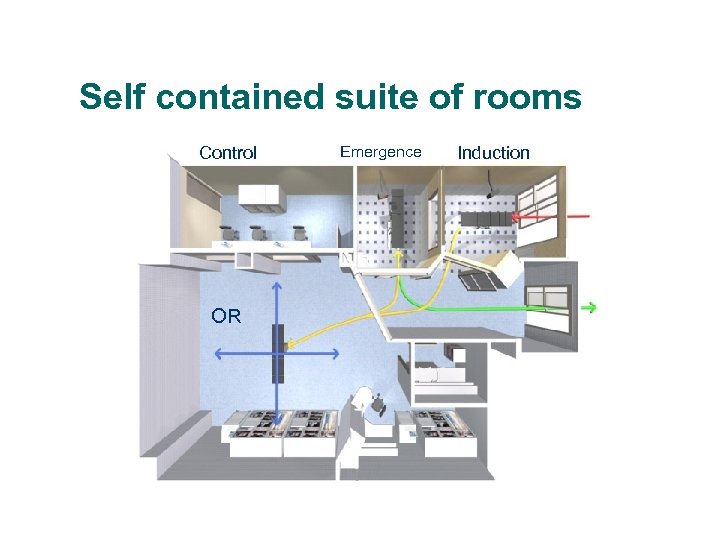 Self contained suite of rooms Control OR Emergence Induction
Self contained suite of rooms Control OR Emergence Induction
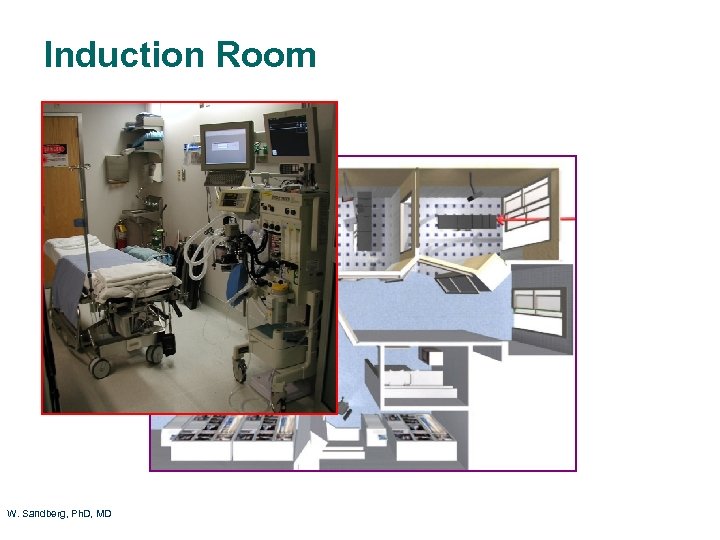 Induction Room W. Sandberg, Ph. D, MD
Induction Room W. Sandberg, Ph. D, MD
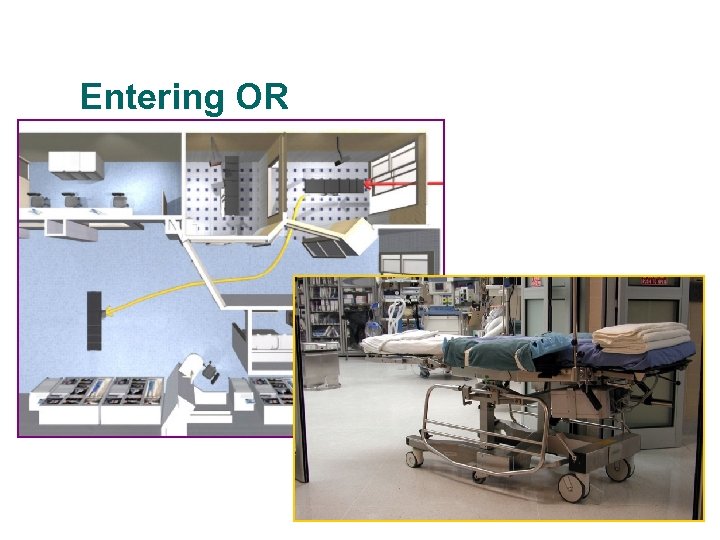 Entering OR
Entering OR
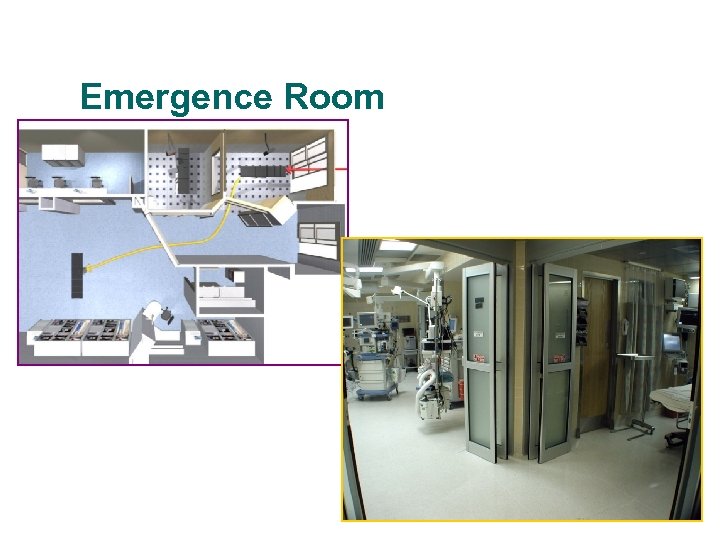 Emergence Room
Emergence Room
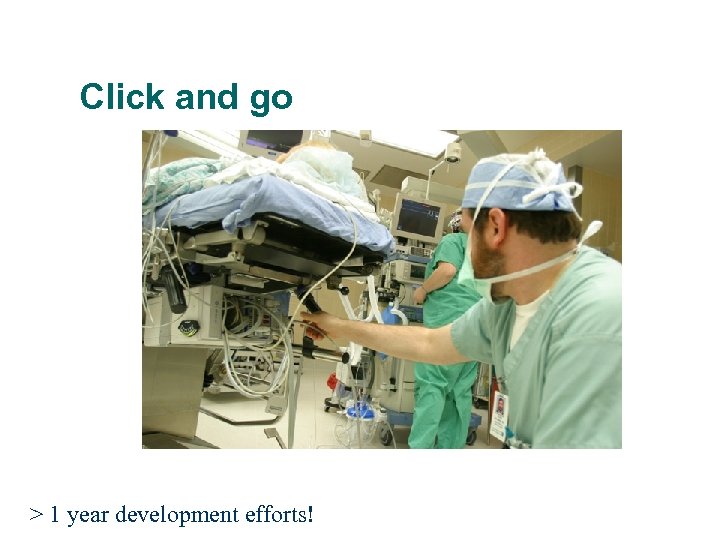 Click and go > 1 year development efforts!
Click and go > 1 year development efforts!

 Perioperative patient transport
Perioperative patient transport
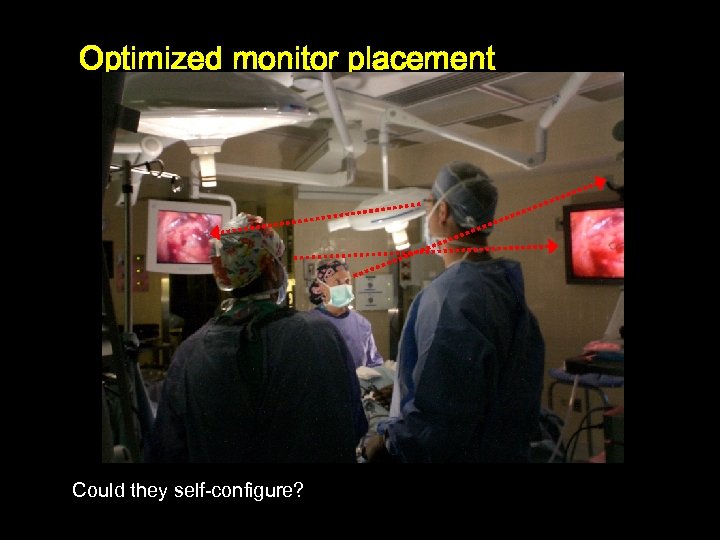 Optimized monitor placement Could they self-configure?
Optimized monitor placement Could they self-configure?
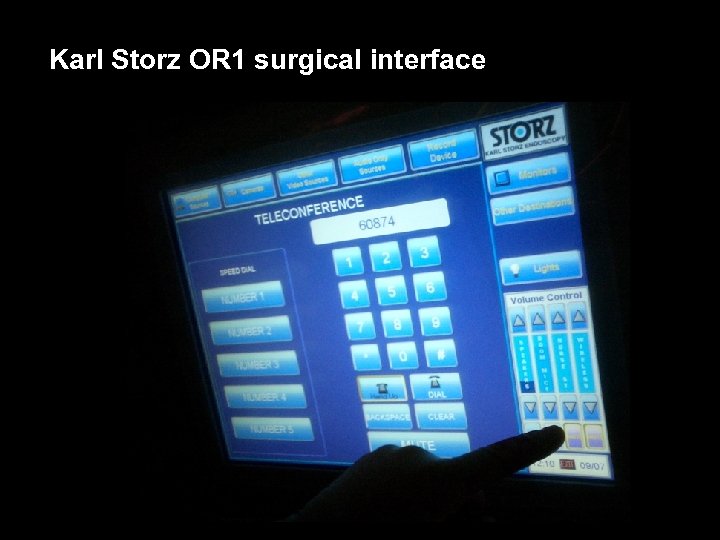 Karl Storz OR 1 surgical interface
Karl Storz OR 1 surgical interface


 Breaking news … © 2005 Julian M. Goldman, MD www. orfpnp. org
Breaking news … © 2005 Julian M. Goldman, MD www. orfpnp. org
 “The President's Plan to Improve Care and Save Lives Through Health IT” 1/27/05 l l l The President is “ …committed to his goal of assuring that most Americans have electronic health records within the next 10 years” “Adopting Uniform Health Information Standards to allow medical information to be stored and easily shared electronically … standards for transmitting Xrays over the Internet; electronic lab results transmitted to physicians …” What’s missing?
“The President's Plan to Improve Care and Save Lives Through Health IT” 1/27/05 l l l The President is “ …committed to his goal of assuring that most Americans have electronic health records within the next 10 years” “Adopting Uniform Health Information Standards to allow medical information to be stored and easily shared electronically … standards for transmitting Xrays over the Internet; electronic lab results transmitted to physicians …” What’s missing?
 © 2005 Julian M. Goldman, MD www. orfpnp. org
© 2005 Julian M. Goldman, MD www. orfpnp. org
 © 2005 Julian M. Goldman, MD www. orfpnp. org
© 2005 Julian M. Goldman, MD www. orfpnp. org

 The “Last Mile” l l l Proposed Health Information Technology innovations address many critical problems in medical record-related data communication Patient and clinician interaction with medical devices is not receiving the same attention Diagnosis and therapy is usually performed with medical devices! © 2005 Julian M. Goldman, MD www. orfpnp. org
The “Last Mile” l l l Proposed Health Information Technology innovations address many critical problems in medical record-related data communication Patient and clinician interaction with medical devices is not receiving the same attention Diagnosis and therapy is usually performed with medical devices! © 2005 Julian M. Goldman, MD www. orfpnp. org
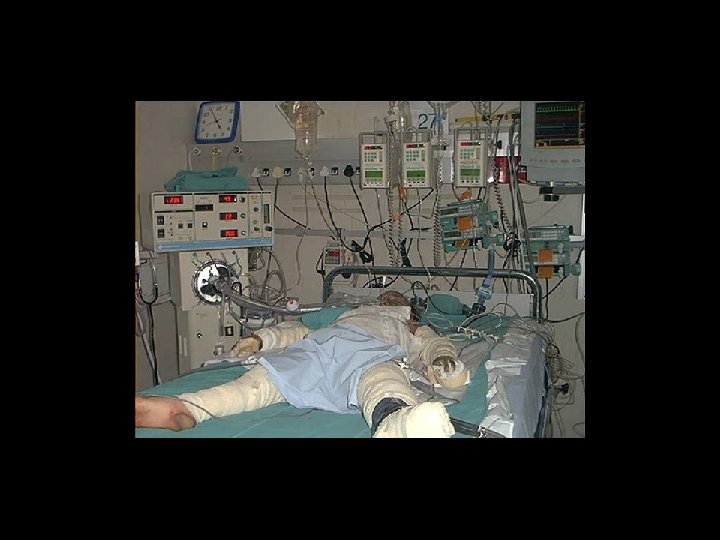
 Problem l l l The OR is a complex and potentially hazardous environment We depend on teamwork and a patchwork of systems to mitigate hazards instead of using automated safety systems (e. g. “interlocks”) Clinicians are not empowered by information technology to achieve complete situational awareness, or to network and control medical devices in the environment – – Absence of smart alarms and automated clinical decision support Absence of technological infrastructure to implement the required solutions © 2005 Julian M. Goldman, MD www. orfpnp. org
Problem l l l The OR is a complex and potentially hazardous environment We depend on teamwork and a patchwork of systems to mitigate hazards instead of using automated safety systems (e. g. “interlocks”) Clinicians are not empowered by information technology to achieve complete situational awareness, or to network and control medical devices in the environment – – Absence of smart alarms and automated clinical decision support Absence of technological infrastructure to implement the required solutions © 2005 Julian M. Goldman, MD www. orfpnp. org
 Safety Interlock Safety interlock at 100° F (38° C). © 2005 Julian M. Goldman, MD www. orfpnp. org
Safety Interlock Safety interlock at 100° F (38° C). © 2005 Julian M. Goldman, MD www. orfpnp. org
 Interlocks l l l Motels Individual devices Generally, NOT across medical device systems © 2005 Julian M. Goldman, MD www. orfpnp. org
Interlocks l l l Motels Individual devices Generally, NOT across medical device systems © 2005 Julian M. Goldman, MD www. orfpnp. org
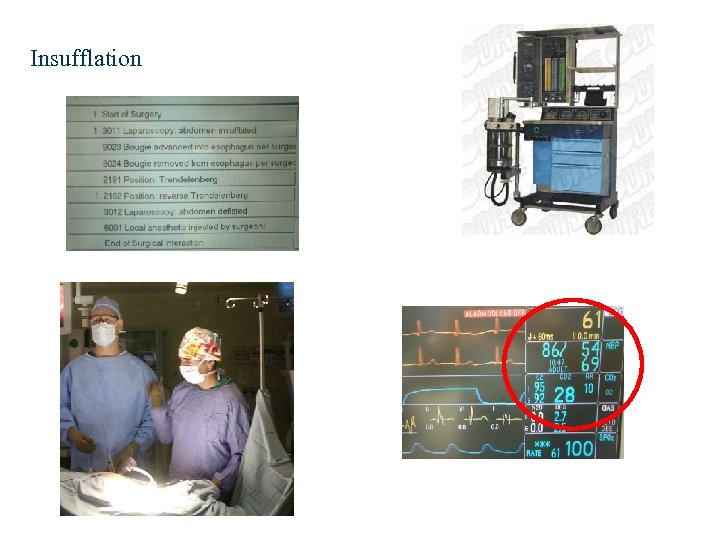 Insufflation
Insufflation
 Benefit of medical device interoperability: Synchronization Ventilation During Intraoperative Cholangiography
Benefit of medical device interoperability: Synchronization Ventilation During Intraoperative Cholangiography
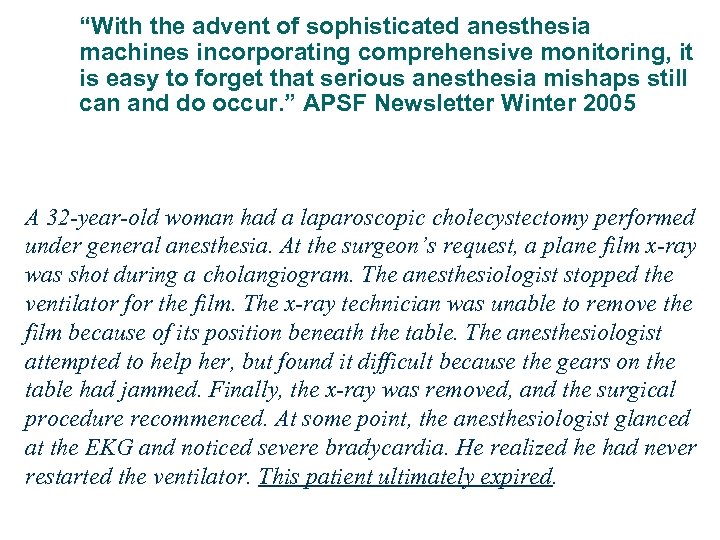 “With the advent of sophisticated anesthesia machines incorporating comprehensive monitoring, it is easy to forget that serious anesthesia mishaps still can and do occur. ” APSF Newsletter Winter 2005 A 32 -year-old woman had a laparoscopic cholecystectomy performed under general anesthesia. At the surgeon’s request, a plane film x-ray was shot during a cholangiogram. The anesthesiologist stopped the ventilator for the film. The x-ray technician was unable to remove the film because of its position beneath the table. The anesthesiologist attempted to help her, but found it difficult because the gears on the table had jammed. Finally, the x-ray was removed, and the surgical procedure recommenced. At some point, the anesthesiologist glanced at the EKG and noticed severe bradycardia. He realized he had never restarted the ventilator. This patient ultimately expired.
“With the advent of sophisticated anesthesia machines incorporating comprehensive monitoring, it is easy to forget that serious anesthesia mishaps still can and do occur. ” APSF Newsletter Winter 2005 A 32 -year-old woman had a laparoscopic cholecystectomy performed under general anesthesia. At the surgeon’s request, a plane film x-ray was shot during a cholangiogram. The anesthesiologist stopped the ventilator for the film. The x-ray technician was unable to remove the film because of its position beneath the table. The anesthesiologist attempted to help her, but found it difficult because the gears on the table had jammed. Finally, the x-ray was removed, and the surgical procedure recommenced. At some point, the anesthesiologist glanced at the EKG and noticed severe bradycardia. He realized he had never restarted the ventilator. This patient ultimately expired.
 Interoperability: Remote Control BP is low -> Stop Infusion
Interoperability: Remote Control BP is low -> Stop Infusion
 Why is interoperability so difficult to implement? l l The OR is a clinical, non-engineered, environment ORF Pn. P problem space is at the nexus of hardware, software, and networking technologies Prior efforts failed to achieve interoperability Poorly-defined safety and business models © 2005 Julian M. Goldman, MD www. orfpnp. org
Why is interoperability so difficult to implement? l l The OR is a clinical, non-engineered, environment ORF Pn. P problem space is at the nexus of hardware, software, and networking technologies Prior efforts failed to achieve interoperability Poorly-defined safety and business models © 2005 Julian M. Goldman, MD www. orfpnp. org
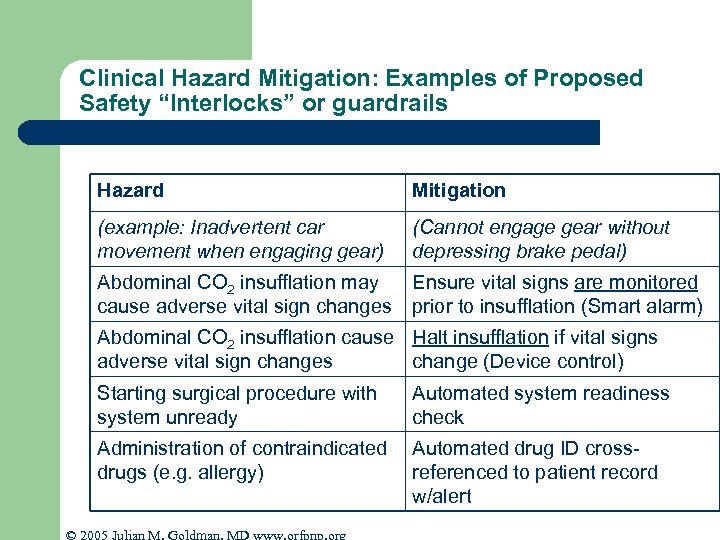 Clinical Hazard Mitigation: Examples of Proposed Safety “Interlocks” or guardrails Hazard Mitigation (example: Inadvertent car movement when engaging gear) (Cannot engage gear without depressing brake pedal) Abdominal CO 2 insufflation may cause adverse vital sign changes Ensure vital signs are monitored prior to insufflation (Smart alarm) Abdominal CO 2 insufflation cause Halt insufflation if vital signs adverse vital sign changes change (Device control) Starting surgical procedure with system unready Automated system readiness check Administration of contraindicated drugs (e. g. allergy) Automated drug ID crossreferenced to patient record w/alert © 2005 Julian M. Goldman, MD www. orfpnp. org
Clinical Hazard Mitigation: Examples of Proposed Safety “Interlocks” or guardrails Hazard Mitigation (example: Inadvertent car movement when engaging gear) (Cannot engage gear without depressing brake pedal) Abdominal CO 2 insufflation may cause adverse vital sign changes Ensure vital signs are monitored prior to insufflation (Smart alarm) Abdominal CO 2 insufflation cause Halt insufflation if vital signs adverse vital sign changes change (Device control) Starting surgical procedure with system unready Automated system readiness check Administration of contraindicated drugs (e. g. allergy) Automated drug ID crossreferenced to patient record w/alert © 2005 Julian M. Goldman, MD www. orfpnp. org
 Smart Alarms & Decision Support l l Require data fusion Contextual information © 2005 Julian M. Goldman, MD www. orfpnp. org
Smart Alarms & Decision Support l l Require data fusion Contextual information © 2005 Julian M. Goldman, MD www. orfpnp. org
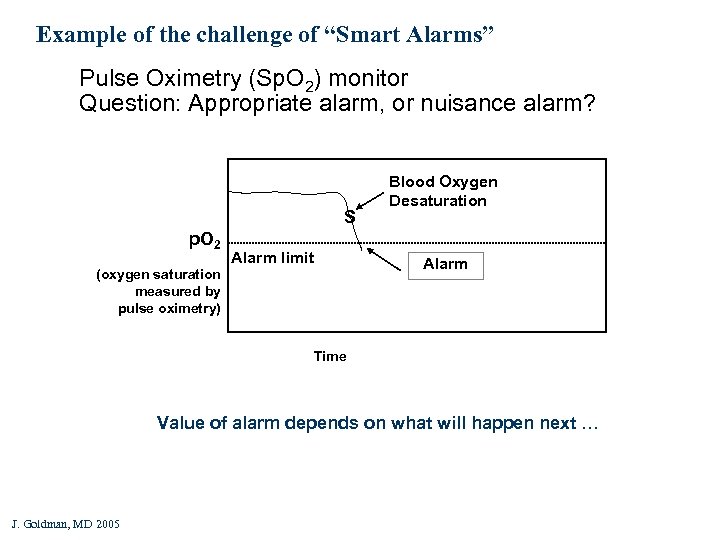 Example of the challenge of “Smart Alarms” Pulse Oximetry (Sp. O 2) monitor Question: Appropriate alarm, or nuisance alarm? S p. O 2 (oxygen saturation measured by pulse oximetry) Alarm limit Blood Oxygen Desaturation Alarm Time Value of alarm depends on what will happen next … J. Goldman, MD 2005
Example of the challenge of “Smart Alarms” Pulse Oximetry (Sp. O 2) monitor Question: Appropriate alarm, or nuisance alarm? S p. O 2 (oxygen saturation measured by pulse oximetry) Alarm limit Blood Oxygen Desaturation Alarm Time Value of alarm depends on what will happen next … J. Goldman, MD 2005
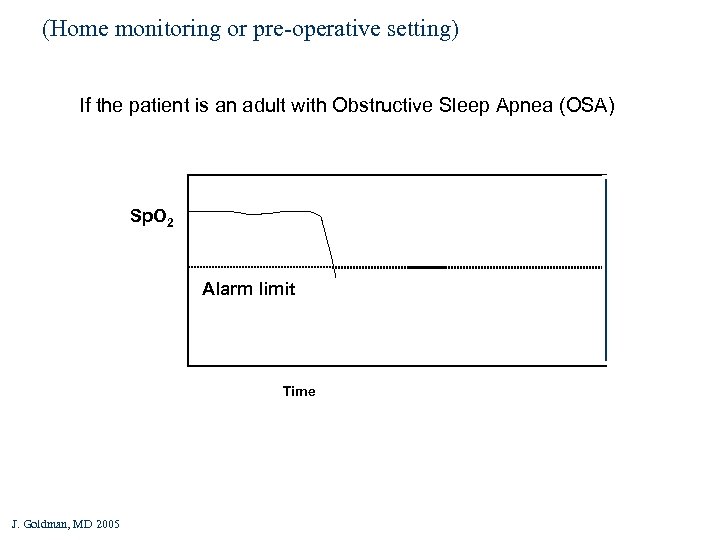 (Home monitoring or pre-operative setting) If the patient is an adult with Obstructive Sleep Apnea (OSA) Self-limiting desaturations Sp. O 2 Alarm limit Time J. Goldman, MD 2005
(Home monitoring or pre-operative setting) If the patient is an adult with Obstructive Sleep Apnea (OSA) Self-limiting desaturations Sp. O 2 Alarm limit Time J. Goldman, MD 2005
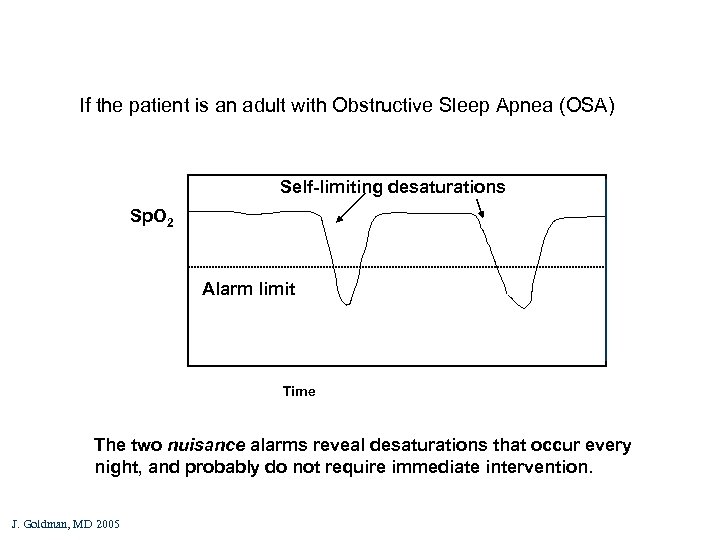 If the patient is an adult with Obstructive Sleep Apnea (OSA) Self-limiting desaturations Sp. O 2 Alarm limit Time The two nuisance alarms reveal desaturations that occur every night, and probably do not require immediate intervention. J. Goldman, MD 2005
If the patient is an adult with Obstructive Sleep Apnea (OSA) Self-limiting desaturations Sp. O 2 Alarm limit Time The two nuisance alarms reveal desaturations that occur every night, and probably do not require immediate intervention. J. Goldman, MD 2005
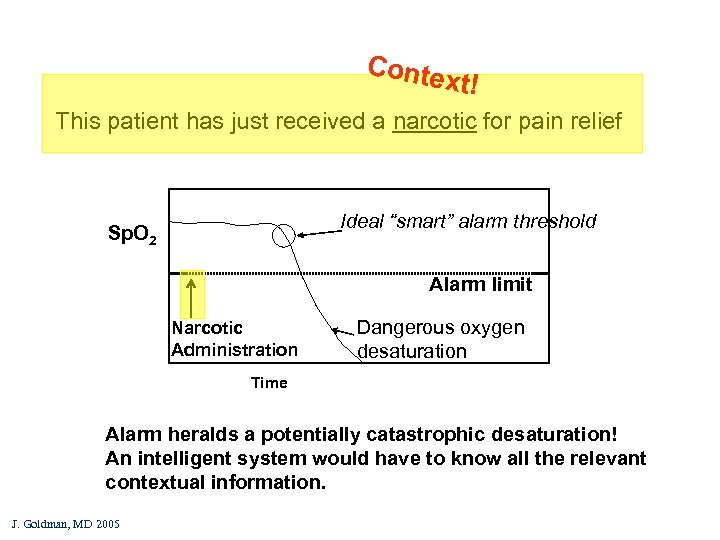 Conte xt! This patient has just received a narcotic for pain relief Ideal “smart” alarm threshold Sp. O 2 Alarm limit Narcotic Administration Dangerous oxygen desaturation Time Alarm heralds a potentially catastrophic desaturation! An intelligent system would have to know all the relevant contextual information. J. Goldman, MD 2005
Conte xt! This patient has just received a narcotic for pain relief Ideal “smart” alarm threshold Sp. O 2 Alarm limit Narcotic Administration Dangerous oxygen desaturation Time Alarm heralds a potentially catastrophic desaturation! An intelligent system would have to know all the relevant contextual information. J. Goldman, MD 2005
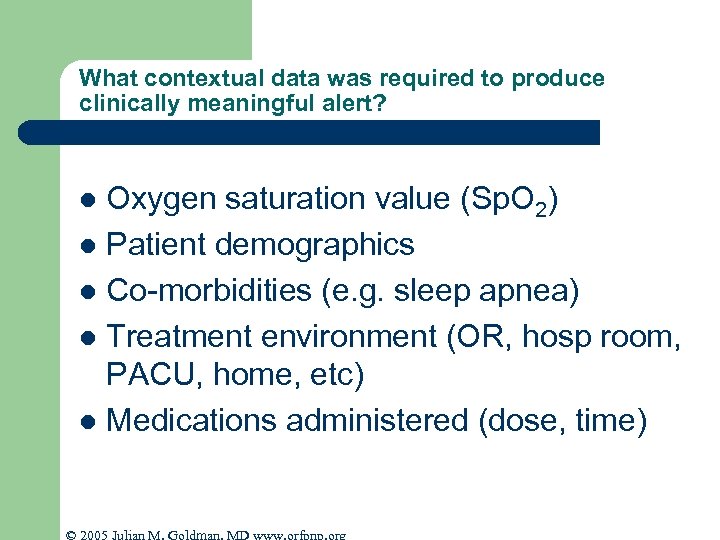 What contextual data was required to produce clinically meaningful alert? Oxygen saturation value (Sp. O 2) l Patient demographics l Co-morbidities (e. g. sleep apnea) l Treatment environment (OR, hosp room, PACU, home, etc) l Medications administered (dose, time) l © 2005 Julian M. Goldman, MD www. orfpnp. org
What contextual data was required to produce clinically meaningful alert? Oxygen saturation value (Sp. O 2) l Patient demographics l Co-morbidities (e. g. sleep apnea) l Treatment environment (OR, hosp room, PACU, home, etc) l Medications administered (dose, time) l © 2005 Julian M. Goldman, MD www. orfpnp. org
 Anesthesia Electronic Medical Record (EMR): Anesthesia Patient Safety Mandate (APSF) l l Vendors deal w/expensive headaches Institutions: same problem Operators: No standardization of data acquisition schemes, data averaging time, etc. No standardized structure to enable decision support systems © 2005 Julian M. Goldman, MD www. orfpnp. org
Anesthesia Electronic Medical Record (EMR): Anesthesia Patient Safety Mandate (APSF) l l Vendors deal w/expensive headaches Institutions: same problem Operators: No standardization of data acquisition schemes, data averaging time, etc. No standardized structure to enable decision support systems © 2005 Julian M. Goldman, MD www. orfpnp. org
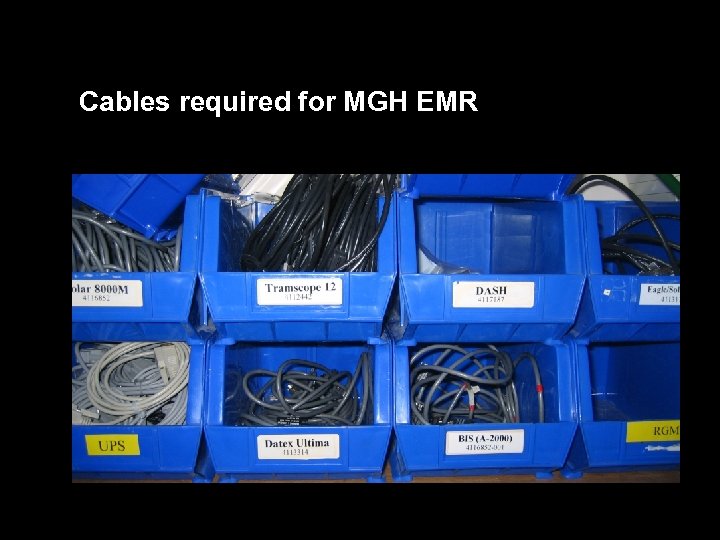 Cables required for MGH EMR
Cables required for MGH EMR
 Future State with ORF Pn. P in place: Comprehensive Data Communication l l l Comprehensive population of the EMR Enhanced clinical situational awareness Decision Support Quality assurance Process improvement Cost analysis © 2005 Julian M. Goldman, MD www. orfpnp. org
Future State with ORF Pn. P in place: Comprehensive Data Communication l l l Comprehensive population of the EMR Enhanced clinical situational awareness Decision Support Quality assurance Process improvement Cost analysis © 2005 Julian M. Goldman, MD www. orfpnp. org
 Future State ORF Pn. P at Work: Device Control l l Device-device control, safety interlocks Remote user actuation of devices – l Bedside control of devices beyond reach, using innovative Human-Device Interfaces “Distributed” medical devices – – distribute CPU, HCI, sensor networks, etc. Physiologic Closed-Loop control Systems l (ISO/IEC JWG 5 and ASTM F 29. 21) © 2005 Julian M. Goldman, MD www. orfpnp. org
Future State ORF Pn. P at Work: Device Control l l Device-device control, safety interlocks Remote user actuation of devices – l Bedside control of devices beyond reach, using innovative Human-Device Interfaces “Distributed” medical devices – – distribute CPU, HCI, sensor networks, etc. Physiologic Closed-Loop control Systems l (ISO/IEC JWG 5 and ASTM F 29. 21) © 2005 Julian M. Goldman, MD www. orfpnp. org
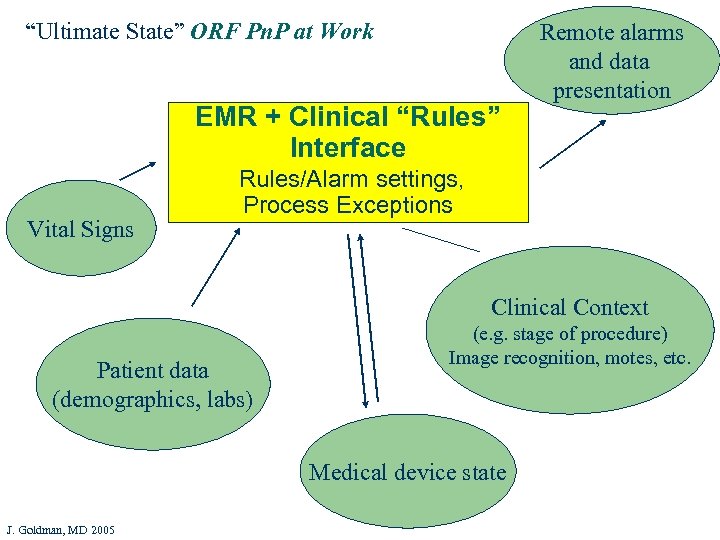 “Ultimate State” ORF Pn. P at Work EMR + Clinical “Rules” Interface Vital Signs Remote alarms and data presentation Rules/Alarm settings, Process Exceptions Clinical Context Patient data (demographics, labs) (e. g. stage of procedure) Image recognition, motes, etc. Medical device state J. Goldman, MD 2005
“Ultimate State” ORF Pn. P at Work EMR + Clinical “Rules” Interface Vital Signs Remote alarms and data presentation Rules/Alarm settings, Process Exceptions Clinical Context Patient data (demographics, labs) (e. g. stage of procedure) Image recognition, motes, etc. Medical device state J. Goldman, MD 2005
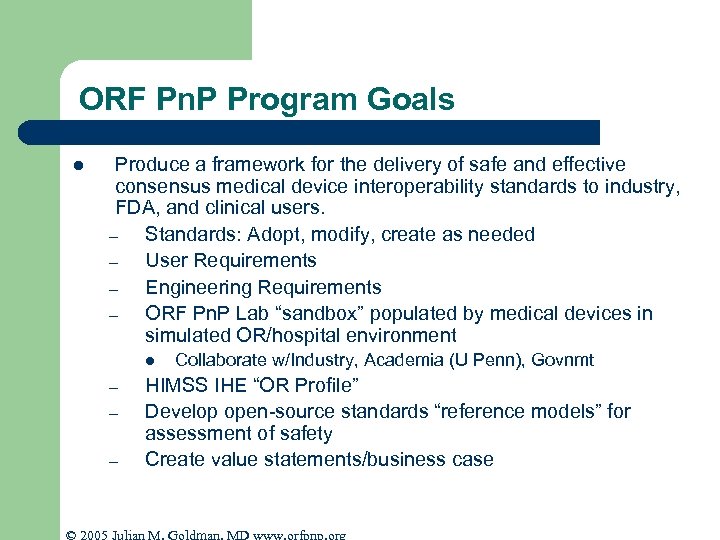 ORF Pn. P Program Goals l Produce a framework for the delivery of safe and effective consensus medical device interoperability standards to industry, FDA, and clinical users. – Standards: Adopt, modify, create as needed – User Requirements – Engineering Requirements – ORF Pn. P Lab “sandbox” populated by medical devices in simulated OR/hospital environment l – – – Collaborate w/Industry, Academia (U Penn), Govnmt HIMSS IHE “OR Profile” Develop open-source standards “reference models” for assessment of safety Create value statements/business case © 2005 Julian M. Goldman, MD www. orfpnp. org
ORF Pn. P Program Goals l Produce a framework for the delivery of safe and effective consensus medical device interoperability standards to industry, FDA, and clinical users. – Standards: Adopt, modify, create as needed – User Requirements – Engineering Requirements – ORF Pn. P Lab “sandbox” populated by medical devices in simulated OR/hospital environment l – – – Collaborate w/Industry, Academia (U Penn), Govnmt HIMSS IHE “OR Profile” Develop open-source standards “reference models” for assessment of safety Create value statements/business case © 2005 Julian M. Goldman, MD www. orfpnp. org
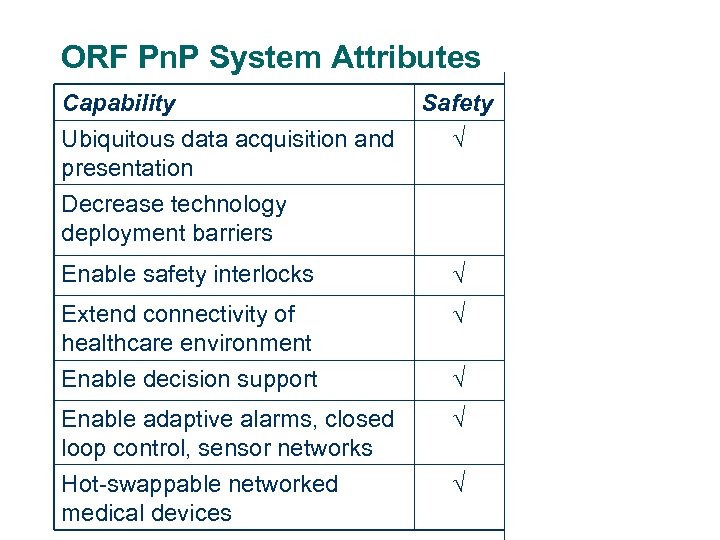 ORF Pn. P System Attributes Capability Ubiquitous data acquisition and presentation Decrease technology deployment barriers Safety Efficiency Enable safety interlocks Extend connectivity of healthcare environment Enable decision support Enable adaptive alarms, closed loop control, sensor networks Hot-swappable networked medical devices
ORF Pn. P System Attributes Capability Ubiquitous data acquisition and presentation Decrease technology deployment barriers Safety Efficiency Enable safety interlocks Extend connectivity of healthcare environment Enable decision support Enable adaptive alarms, closed loop control, sensor networks Hot-swappable networked medical devices
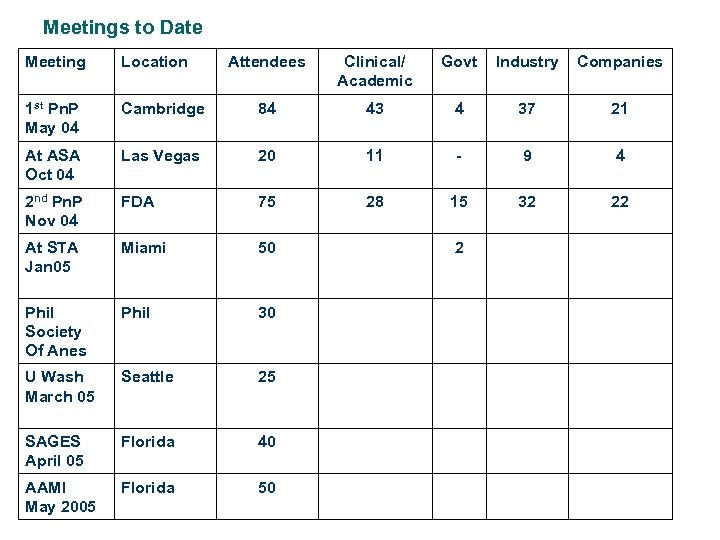 Meetings to Date Meeting Location Attendees Clinical/ Academic Govt Industry Companies 1 st Pn. P May 04 Cambridge 84 43 4 37 21 At ASA Oct 04 Las Vegas 20 11 - 9 4 2 nd Pn. P Nov 04 FDA 75 28 15 32 22 At STA Jan 05 Miami 50 Phil Society Of Anes Phil 30 U Wash March 05 Seattle 25 SAGES April 05 Florida 40 AAMI May 2005 Florida 50 2
Meetings to Date Meeting Location Attendees Clinical/ Academic Govt Industry Companies 1 st Pn. P May 04 Cambridge 84 43 4 37 21 At ASA Oct 04 Las Vegas 20 11 - 9 4 2 nd Pn. P Nov 04 FDA 75 28 15 32 22 At STA Jan 05 Miami 50 Phil Society Of Anes Phil 30 U Wash March 05 Seattle 25 SAGES April 05 Florida 40 AAMI May 2005 Florida 50 2
 Directions for WGs on high-level clinical requirements l l l The proposed standards could permit seamless connectivity of medical devices to allow data communication and control of medical devices. The unique challenge of this project is that we are striving to develop an infrastructure for innovation. Therefore, it is important to define the high-level general system requirements without getting bogged down in the details of technical specifications. Manufacturers/designers need to know what we need the system to do, so that they can determine how to best provide the desired functionality. © 2005 Julian M. Goldman, MD www. orfpnp. org
Directions for WGs on high-level clinical requirements l l l The proposed standards could permit seamless connectivity of medical devices to allow data communication and control of medical devices. The unique challenge of this project is that we are striving to develop an infrastructure for innovation. Therefore, it is important to define the high-level general system requirements without getting bogged down in the details of technical specifications. Manufacturers/designers need to know what we need the system to do, so that they can determine how to best provide the desired functionality. © 2005 Julian M. Goldman, MD www. orfpnp. org
 l l l Think of examples of connectivity that could a) solve current clinical problems, b) improve safety or efficiency, or c) enable innovative clinical systems of the future. Assume that there are no technical, economic, legal, or regulatory obstacles to deploying a comprehensive ORF Pn. P system. What clinical challenges exist today that could be solved by the proposed system? Which obstacles to safety, efficiency, and teamwork could be reduced or eliminated by the proposed system? How would this approach affect the practice environment, both clinically and from a business perspective? What risks may be introduced by a Pn. P system, and how could they be mitigated?
l l l Think of examples of connectivity that could a) solve current clinical problems, b) improve safety or efficiency, or c) enable innovative clinical systems of the future. Assume that there are no technical, economic, legal, or regulatory obstacles to deploying a comprehensive ORF Pn. P system. What clinical challenges exist today that could be solved by the proposed system? Which obstacles to safety, efficiency, and teamwork could be reduced or eliminated by the proposed system? How would this approach affect the practice environment, both clinically and from a business perspective? What risks may be introduced by a Pn. P system, and how could they be mitigated?
 www. ORFPn. P. org For information about the OR of the Future project: www. CIMIT. org
www. ORFPn. P. org For information about the OR of the Future project: www. CIMIT. org
 AAMI BI&T May/June 2005
AAMI BI&T May/June 2005
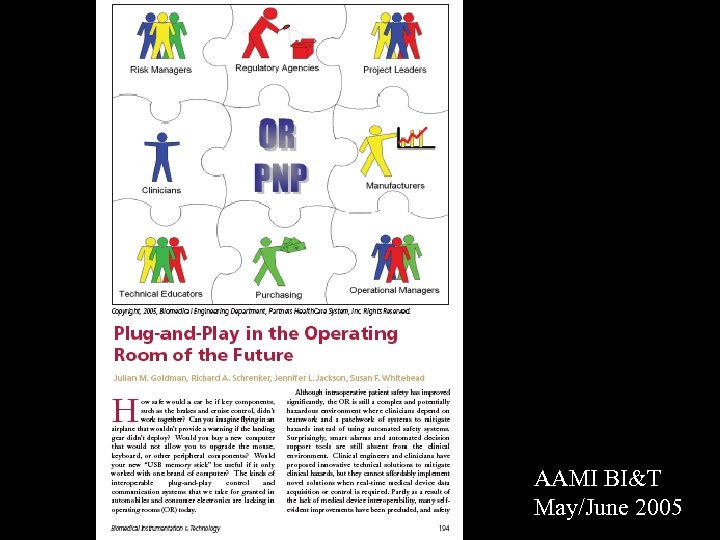 AAMI BI&T May/June 2005
AAMI BI&T May/June 2005
 Next ORF Pn. P Meeting June Monday June 6 – Tuesday June 7 Cambridge, Massachusetts (Next week!) © 2005 Julian M. Goldman, MD www. orfpnp. org
Next ORF Pn. P Meeting June Monday June 6 – Tuesday June 7 Cambridge, Massachusetts (Next week!) © 2005 Julian M. Goldman, MD www. orfpnp. org
 Thank you © 2005 Julian M. Goldman, MD www. orfpnp. org
Thank you © 2005 Julian M. Goldman, MD www. orfpnp. org


