636fd9feba6f9ea410a24fecd564d428.ppt
- Количество слайдов: 64
CHRONIC RENAL FALURE Ebadur Rahman FRCP (Edin), FASN, Specialty Certificate in Nephrology (UK) MRCP (UK), DIM (UK), DNeph (UK), Mmed. Sci. Nephrology (UK). Consultant & clinical tutor Department of Nephrology Riyadh Armed Forces Hospital

CRF/ CKD
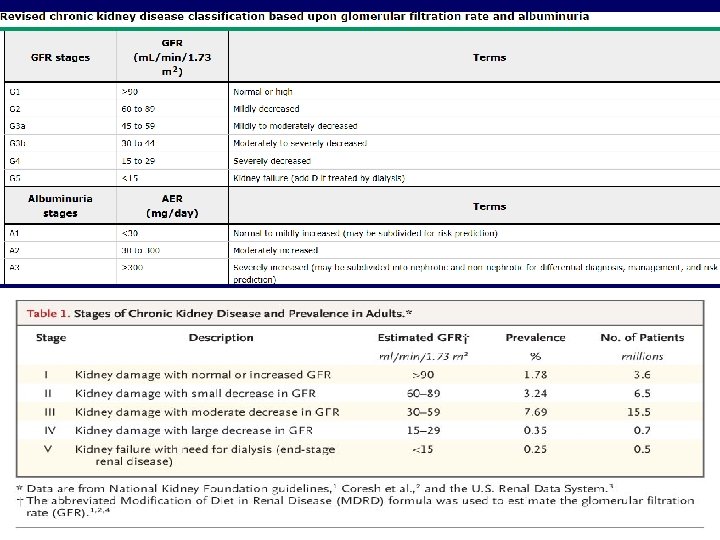
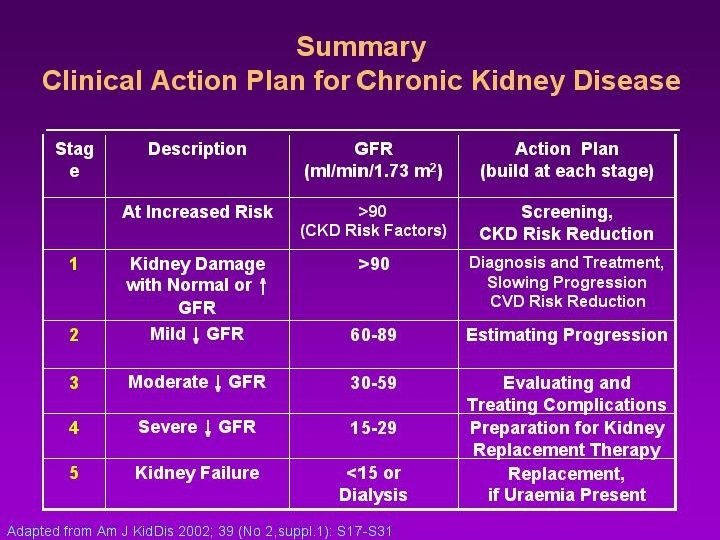
KDIGO DEFINITION • Chronic kidney disease (CKD) is defined – presence of kidney damage (usually detected as urinary albumin excretion of ≥ 30 mg/day, or equivalent) or – decreased kidney function (defined as estimated glomerular filtration rate [e. GFR] <60 m. L/min per 1. 73 m 2) for three or more months, irrespective of the cause.
Functions of Kidneys • • Fluid Balance Electrolyte Balanace---Na—K----H Acid base Balance Excretion of waste products of Metabolism and Drugs • Hormonal Secretion Epo—Renin—Active Vit D---D 3
Toxic Metabolites • • • Urea Guanidino Compounds Creatine Creatinine Urates Peptides
Normal GFR — The glomerular filtration rate (GFR) is equal to the sum of the filtration rates in all of the functioning nephrons _The glomeruli, filter approximately 180 liters per day (125 m. L/min) of plasma. The normal value for GFR depends upon age, sex, and body size, and is approximately 130 and 120 m. L/min/1. 73 m 2 for men and women, respectively
• Measure • Estimate
• Measurement of GFR — GFR cannot be measured directly the best method for determining GFR is measurement of the urinary clearance of an ideal filtration marker. Using a filtration marker (x), the equation to calculate the clearance of x (Cx) is: Equation : Cx = (Ux x V)/P x

The gold standard of exogenous filtration markers is inulin • alternative filtration markers – radioactive or nonradioactive iothalamate, iohexol, DTPA, or EDTA
• The most common equations used in the United States are the Cockcroft-Gault and the Modification of Diet in Renal Disease (MDRD) study equations • using the Cockcroft-Gault equation will result in a 10 to 40 percent overestimate of creatinine clearance • The MDRD study equation - standardized to creatinine reference materials measured using gold standard techniques • The CKD-EPI equation
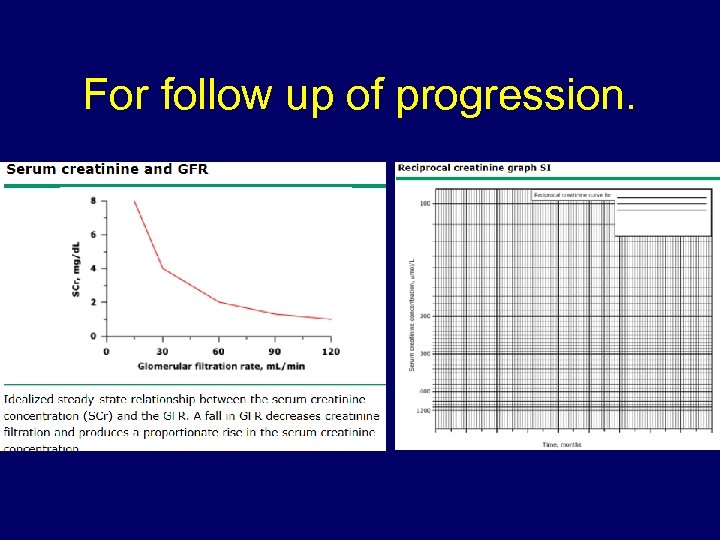
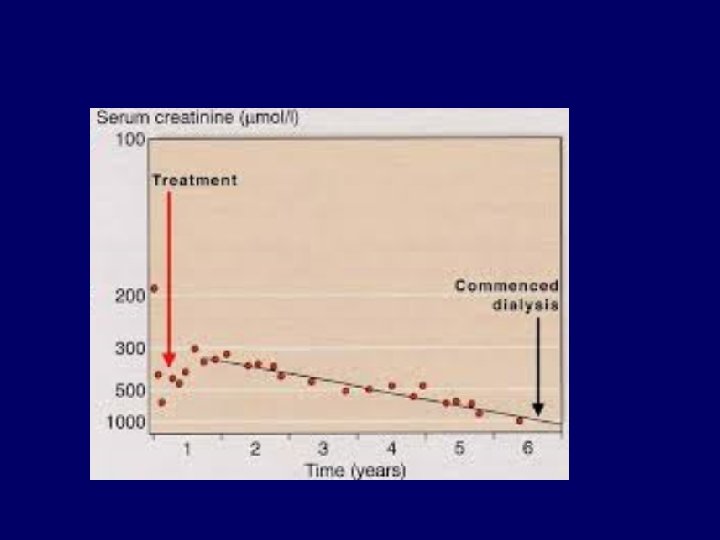
For follow up of progression.
• 54 y lady comes with creatinine 250, urea 12, hgb 9,
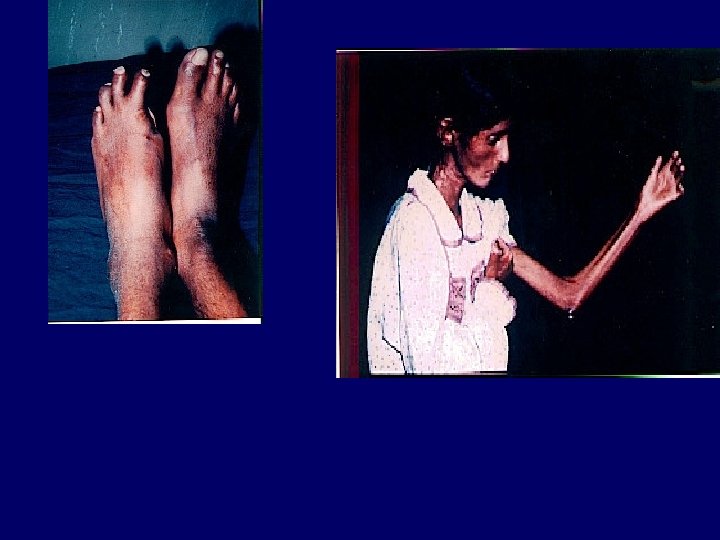
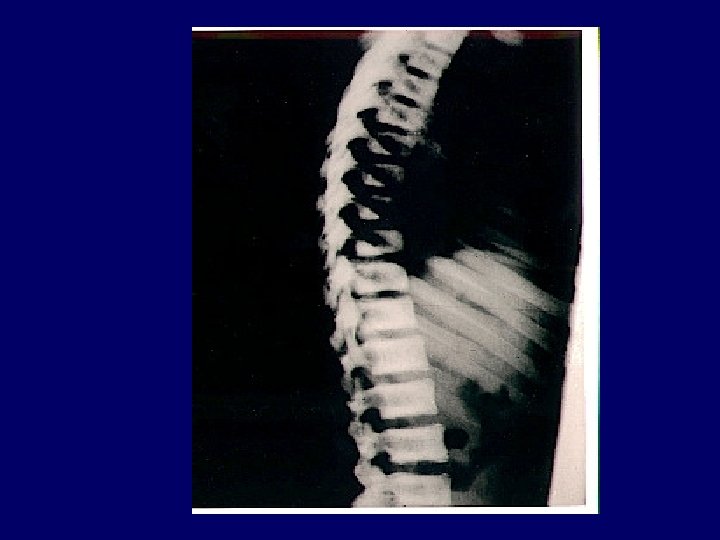
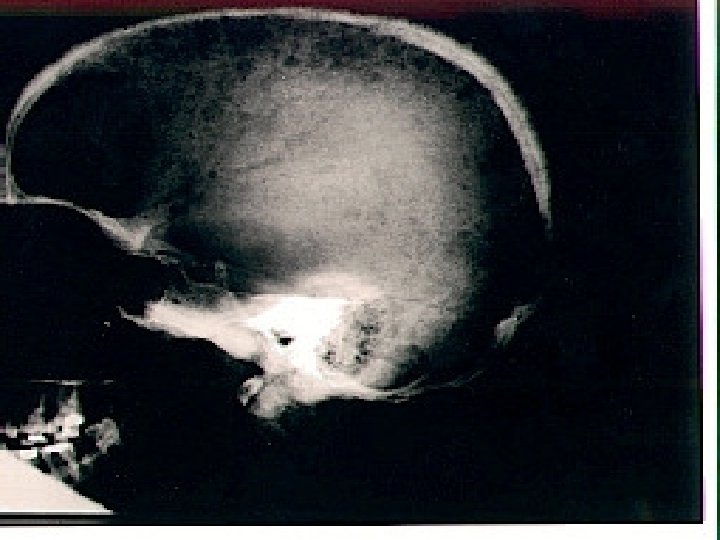
Acute chronic Indicators Of Chronicity ANEMIA BROAD CASTS IN URINE Small Shrunken Kidneys Renal Osteodystrophy Peripheral Neuropathy Skin changes
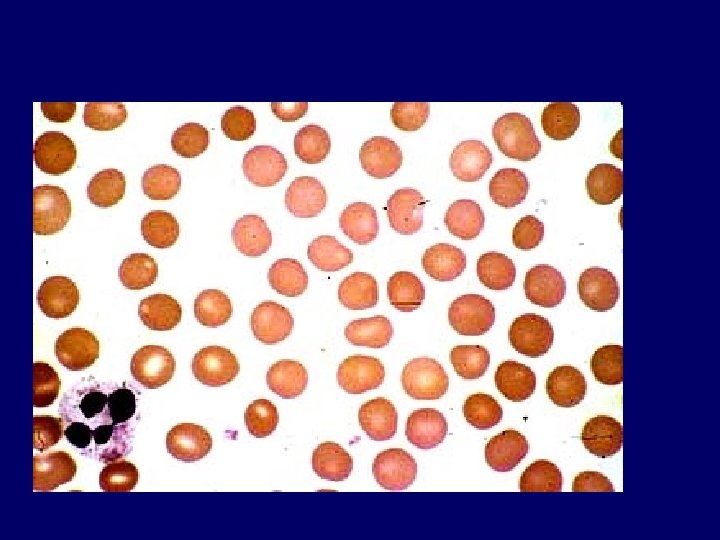
The anemia of chronic kidney disease (CKD) • normocytic and normochromic. • • It is principally due to reduced renal erythropoietin production shortened red cell survival decreased responsiveness to the hormone. Anemia can develop well before the onset of uremic symptoms due to end -stage renal disease (ESRD). • develops when the glomerular filtration rate (GFR) declines to <30 m. L/min, • the anemia of CKD is associated with – decreased cognition and mental acuity, fatigue, and other signs and symptoms. – There also associations with an increased risk of morbidity and mortality, principally due to cardiac disease and stroke
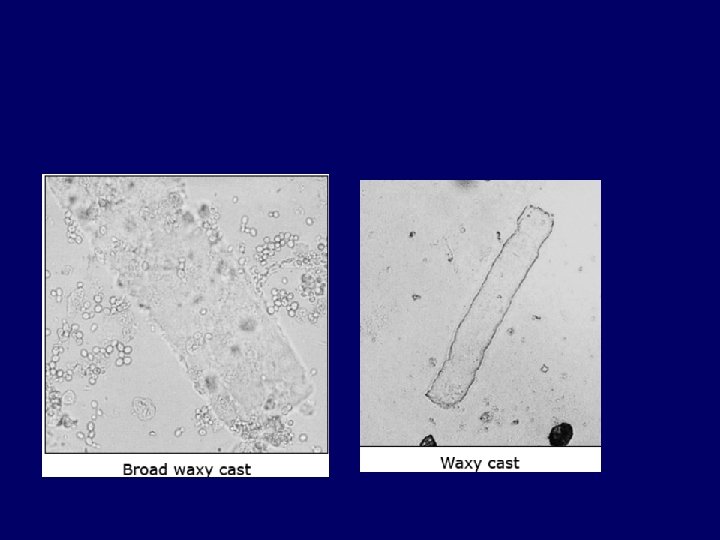

Hyaline casts — Hyaline casts are only slightly more refractile than water and have a transparent, empty appearance (picture 15. Hyaline casts may be observed with small volumes of concentrated urine or with diuretic therapy and are generally nonspecific .

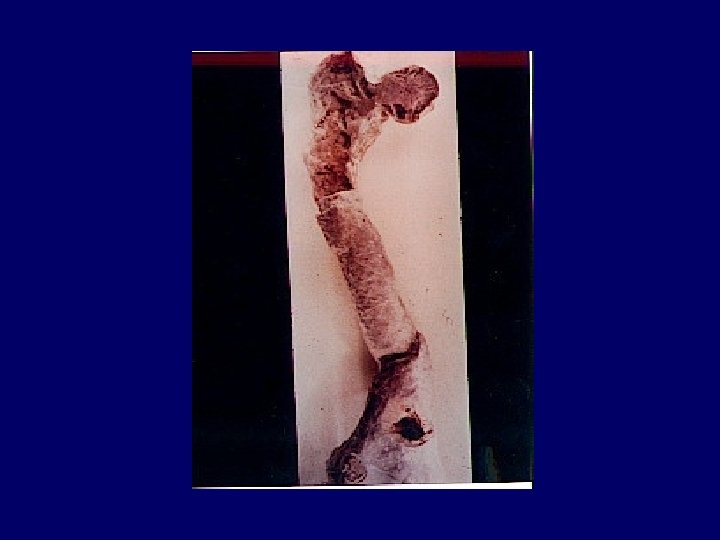
Renal Osteodystrophy • chronic kidney disease-mineral and bone disorder CKD-MBD is defined as a systemic disorder of mineral and bone metabolism due to CKD, manifested by either one or a combination of the following three components: – Abnormalities of calcium, phosphorus, parathyroid hormone (PTH), or vitamin D metabolism – Abnormalities in bone turnover, mineralization, – Extraskeletal calcification
CRF Causes • Hereditary – ADPKD – Alports syndrome – medullary cystic disease of kidneys
Symtomatology 1. 25% loss of Function—few symptoms and few Biochemical abnormalities Proteinuria and HPT 2. Na in CRF Cr Cl=5 -25 mls/min 3. Water---concenreation and dilutional mechanisms 4. K-balance Cr Cl=5 -10 mls/min 5. H—Acid base balance Cr Cl=5 -15 mls/min 6. PO 4 ---Mg—Ca
Symtomatology cont 7 Anemia 8. C. V. S 9. Serositis 10. G. I. Disorders 11. neuromuscular 12. Skeletal—Metastatic Calcification. 13. Skin-14. Immune Response— 15. metabolic TG---16. Hormonal
Hormonal Alterations in Uremia Hormone increased • Prolactin Lactation • Lutinizing hor Gynecomastia • Gastrin Gastritis • Renin Aldosterone HPT • Glucagon Glucose intolerance • Growth Hormone ------------- • Parathormone Osteitis fibrosapruritisothers
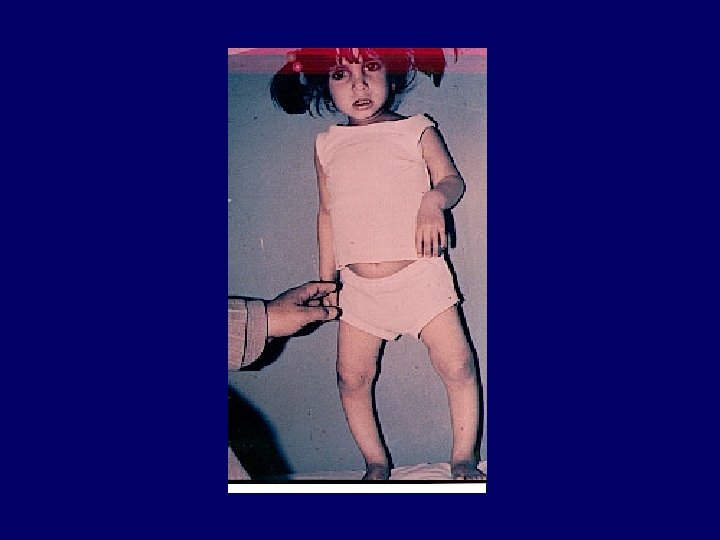
Hormonal Alterations in Uremia • • Hormone decreased 1: 25 -(OH)2 D 3 Osteomalatia ost-fib Erythropoetin Anemia Sometamedin dec linear growth in children • Testosterone Impotence • FSH ?
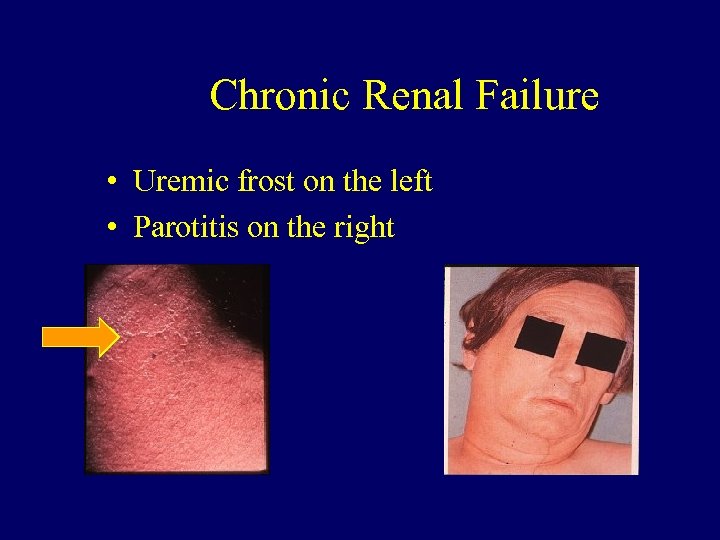
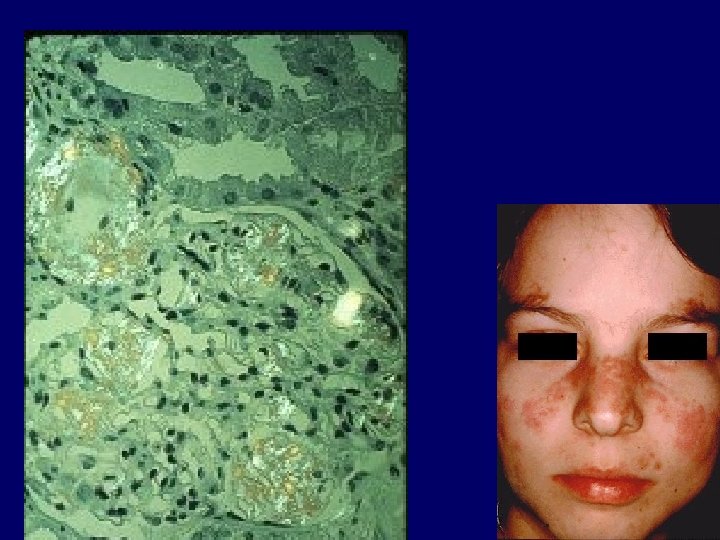
Chronic Renal Failure • Uremic frost on the left • Parotitis on the right

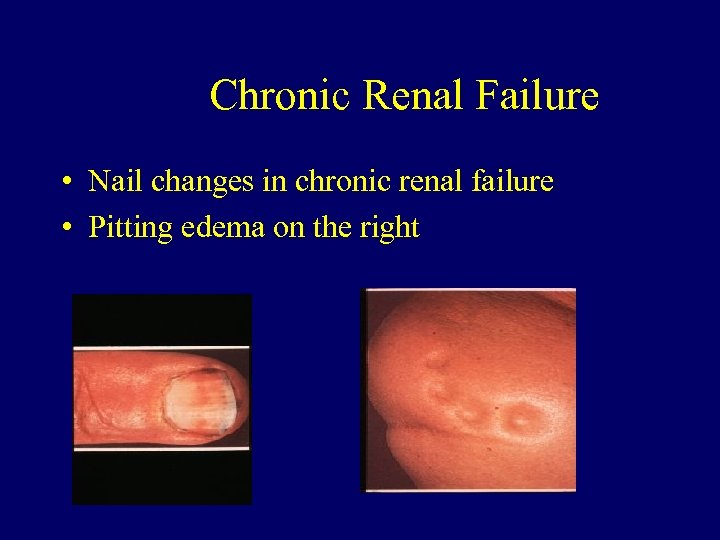
Chronic Renal Failure • Nail changes in chronic renal failure • Pitting edema on the right





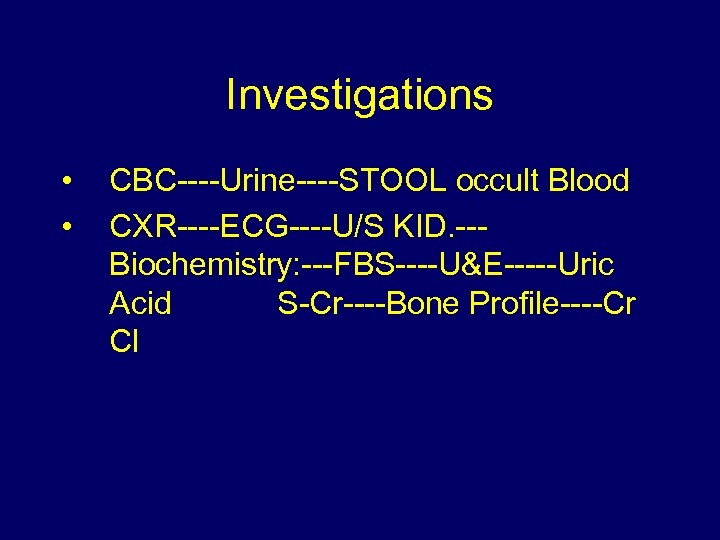
Investigations • • CBC----Urine----STOOL occult Blood CXR----ECG----U/S KID. --Biochemistry: ---FBS----U&E-----Uric Acid S-Cr----Bone Profile----Cr Cl
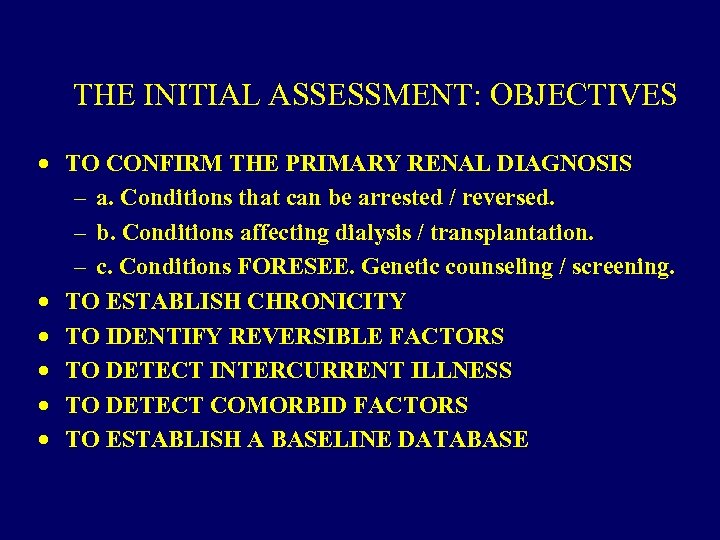
THE INITIAL ASSESSMENT: OBJECTIVES · TO CONFIRM THE PRIMARY RENAL DIAGNOSIS – a. Conditions that can be arrested / reversed. – b. Conditions affecting dialysis / transplantation. – c. Conditions FORESEE. Genetic counseling / screening. · TO ESTABLISH CHRONICITY · TO IDENTIFY REVERSIBLE FACTORS · TO DETECT INTERCURRENT ILLNESS · TO DETECT COMORBID FACTORS · TO ESTABLISH A BASELINE DATABASE
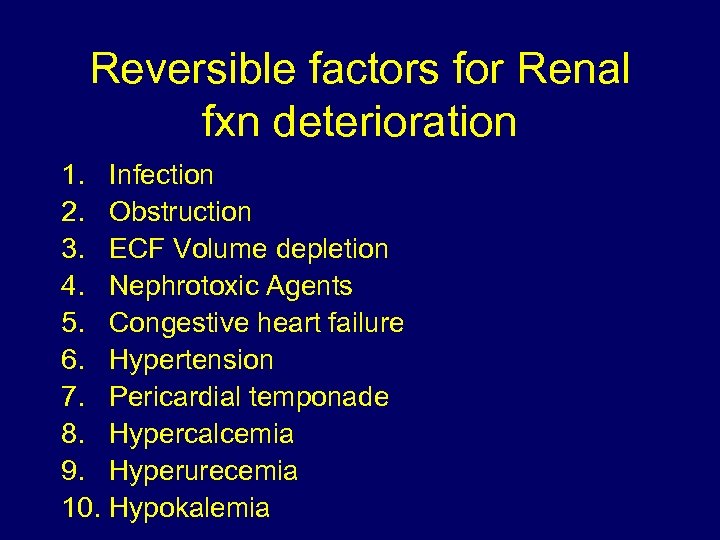
Reversible factors for Renal fxn deterioration 1. Infection 2. Obstruction 3. ECF Volume depletion 4. Nephrotoxic Agents 5. Congestive heart failure 6. Hypertension 7. Pericardial temponade 8. Hypercalcemia 9. Hyperurecemia 10. Hypokalemia
PRINCIPLES MANAGEMENT IN CKD • • CORRECTION OF HYPOCALCEMIA CORRECTION OF ACIDOSIS CORRECTION OF HYPERPHOPHATAEMIA MONITORING PTH LEVELS AND CONTROL OF RENAL OSTEODYSTROPHY
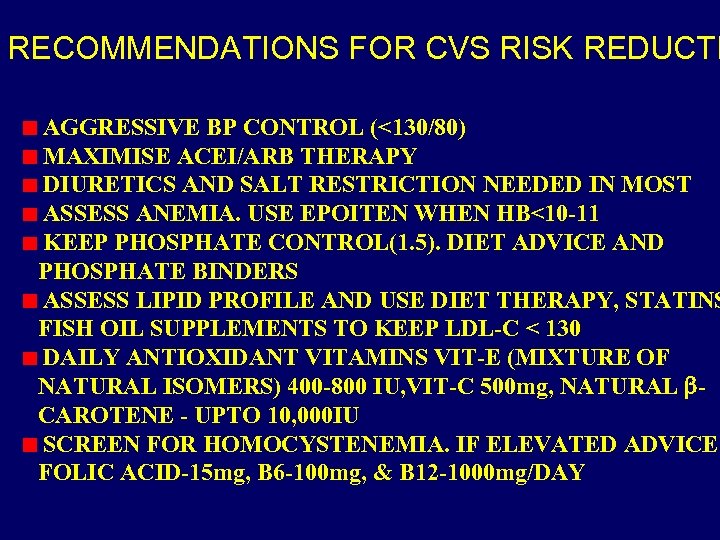
RECOMMENDATIONS FOR CVS RISK REDUCTI AGGRESSIVE BP CONTROL (<130/80) MAXIMISE ACEI/ARB THERAPY DIURETICS AND SALT RESTRICTION NEEDED IN MOST ASSESS ANEMIA. USE EPOITEN WHEN HB<10 -11 KEEP PHOSPHATE CONTROL(1. 5). DIET ADVICE AND PHOSPHATE BINDERS ASSESS LIPID PROFILE AND USE DIET THERAPY, STATINS FISH OIL SUPPLEMENTS TO KEEP LDL-C < 130 DAILY ANTIOXIDANT VITAMINS VIT-E (MIXTURE OF NATURAL ISOMERS) 400 -800 IU, VIT-C 500 mg, NATURAL CAROTENE - UPTO 10, 000 IU SCREEN FOR HOMOCYSTENEMIA. IF ELEVATED ADVICE FOLIC ACID-15 mg, B 6 -100 mg, & B 12 -1000 mg/DAY

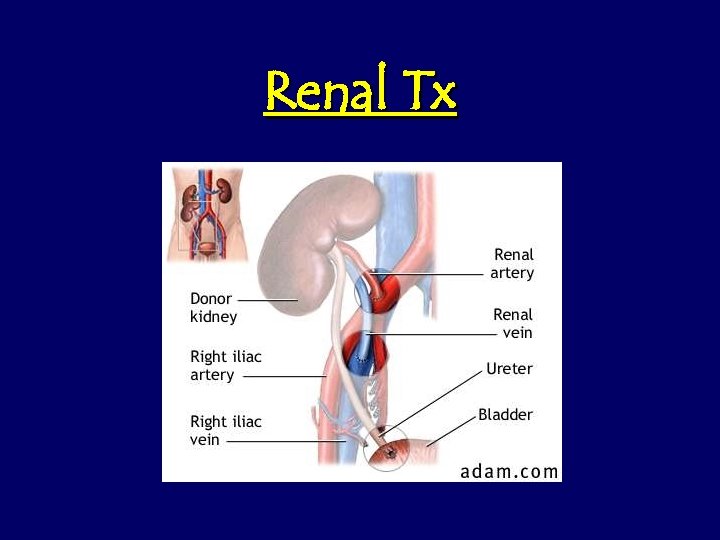
Renal Tx
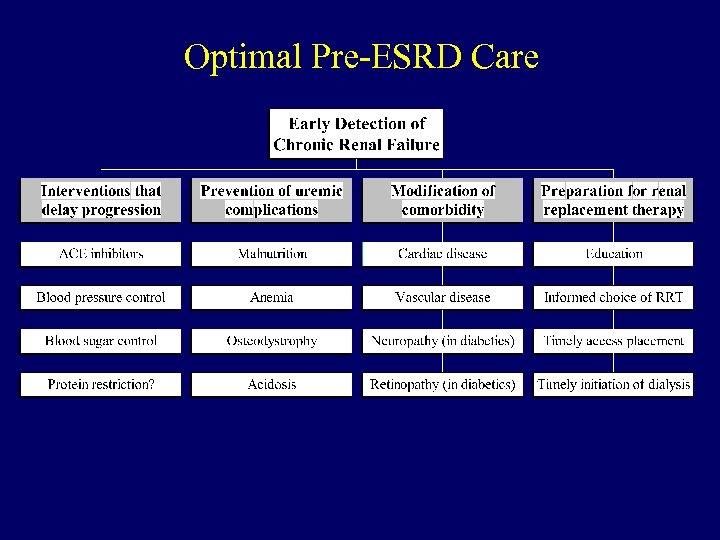
Optimal Pre-ESRD Care
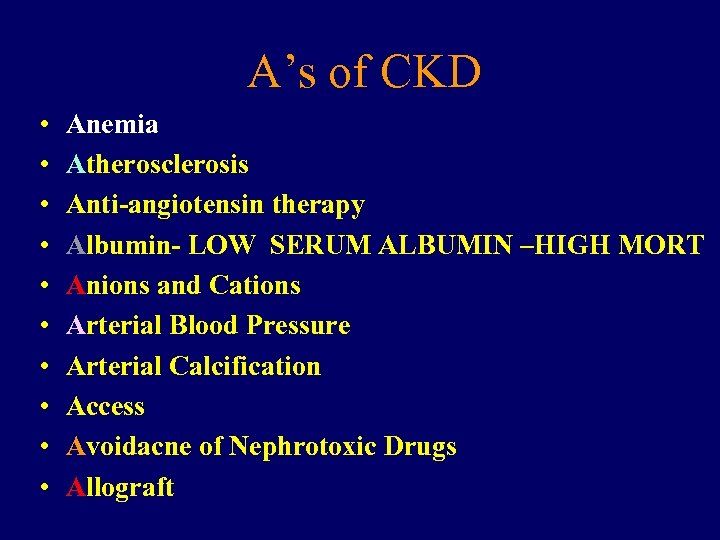
A’s of CKD • • • Anemia Atherosclerosis Anti-angiotensin therapy Albumin- LOW SERUM ALBUMIN –HIGH MORT Anions and Cations Arterial Blood Pressure Arterial Calcification Access Avoidacne of Nephrotoxic Drugs Allograft
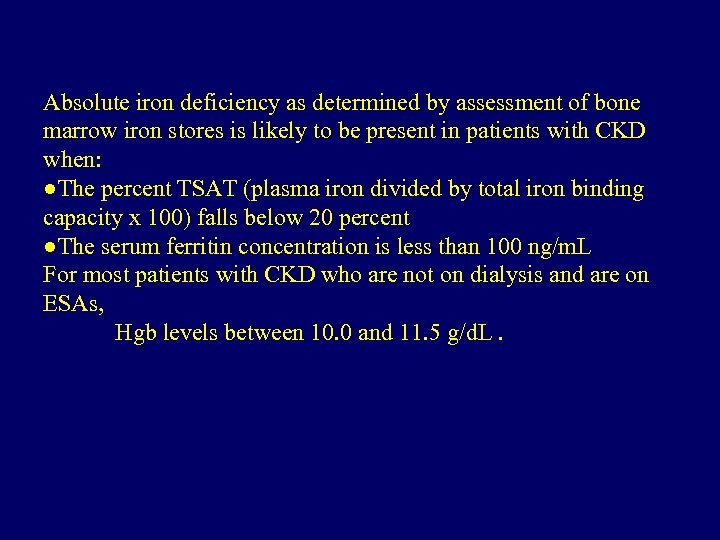
Absolute iron deficiency as determined by assessment of bone marrow iron stores is likely to be present in patients with CKD when: ●The percent TSAT (plasma iron divided by total iron binding capacity x 100) falls below 20 percent ●The serum ferritin concentration is less than 100 ng/m. L For most patients with CKD who are not on dialysis and are on ESAs, Hgb levels between 10. 0 and 11. 5 g/d. L.
Management • • patients with proteinuric (defined as protein excretion above 500 to 1000 mg/day) nondiabetic CKD – renin-angiotensin system (RAS) inhibitor as first-line therapy for the treatment of hypertension – In hypertensive patients with nonproteinuric nondiabetic CKD who have edema, - a diuretic as first-line therapy ( patients with proteinuric nondiabetic CKD, we suggest a proteinuria goal of less than 1000 mg/day In patients with proteinuric nondiabetic CKD, we recommend a blood pressure goal of less than 130/80 mm. Hg rather than 140/90 mm. Hg In patients with nonproteinuric nondiabetic CKD, we recommend a blood pressure goal of at least less than 140/90 mm. Hg In patients with established atherosclerotic cardiovascular disease, outcomes are better when the systolic pressure is lowered to below 130 to 135 mm. Hg. In most patients with nondiabetic CKD, donot use combination therapy with ACE inhibitors and ARBs
636fd9feba6f9ea410a24fecd564d428.ppt