f1468ee4963f8053ec4b775d0b446545.ppt
- Количество слайдов: 127
CHRONIC OBSTRUCTIVE PULMONARY DISEASE Dr. Sarma RVSN, M. D. , M. Sc (Canada) Consultant in Medicine and Chest, President IMA – Tiruvallur Branch JN Road, Jayanagar, Tiruvallur, TN +91 98940 60593, (4116) 260593 Dr. Sarma@works 1
GOLD GLOBAL INITIATIVE FOR CHRONIC OBSTRUCTIVE LUNG DISEASE NHLBI AND WHO COLLABORATIVE INITIATIVE Dr. Sarma@works 2
WORLD COPD DAY November 19, EVERY YEAR Raising COPD Awareness Worldwide Dr. Sarma@works 3
RELEVANCE 1. COPD is very common 2. COPD is often covert 3. COPD is treatable 4. Culprit is smoking 5. Symptoms + DD Use spirometry 6. GP must know to Dx. Tests, Rx. and refer 7. New advances in Rx. Dr. Sarma@works PURPOSE OF THIS TALK Present the Global strategy for the Diagnosis, Management and Prevention of COPD (updated Nov 2004) BASED ON THE GOLD, NICE NAEPP, CDC, BTS, GUIDELINES 4

DEFINITIONS Dr. Sarma@works 5
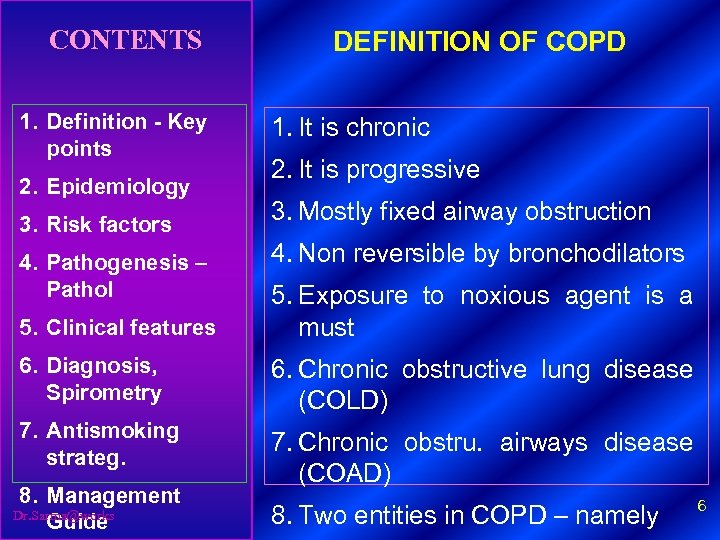
CONTENTS 1. Definition - Key points 2. Epidemiology 3. Risk factors 4. Pathogenesis – Pathol DEFINITION OF COPD 1. It is chronic 2. It is progressive 3. Mostly fixed airway obstruction 4. Non reversible by bronchodilators 5. Clinical features 5. Exposure to noxious agent is a must 6. Diagnosis, Spirometry 6. Chronic obstructive lung disease (COLD) 7. Antismoking strateg. 7. Chronic obstru. airways disease (COAD) 8. Management Dr. Sarma@works Guide 8. Two entities in COPD – namely 6
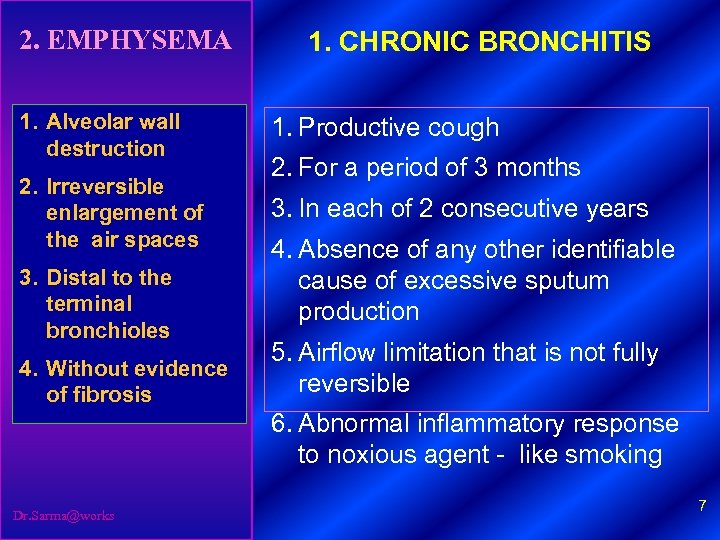
2. EMPHYSEMA 1. Alveolar wall destruction 1. CHRONIC BRONCHITIS 1. Productive cough 2. For a period of 3 months 2. Irreversible enlargement of 3. In each of 2 consecutive years the air spaces 4. Absence of any other identifiable 3. Distal to the cause of excessive sputum terminal production bronchioles 5. Airflow limitation that is not fully 4. Without evidence reversible of fibrosis 6. Abnormal inflammatory response to noxious agent - like smoking Dr. Sarma@works 7
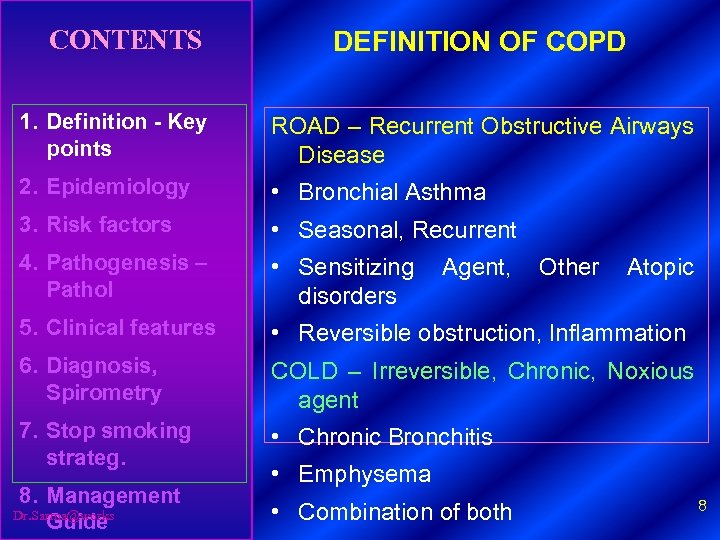
CONTENTS DEFINITION OF COPD 1. Definition - Key points ROAD – Recurrent Obstructive Airways Disease 2. Epidemiology • Bronchial Asthma 3. Risk factors • Seasonal, Recurrent 4. Pathogenesis – Pathol • Sensitizing Agent, Other Atopic disorders 5. Clinical features • Reversible obstruction, Inflammation 6. Diagnosis, Spirometry COLD – Irreversible, Chronic, Noxious agent 7. Stop smoking strateg. • Chronic Bronchitis 8. Management Dr. Sarma@works Guide • Combination of both • Emphysema 8
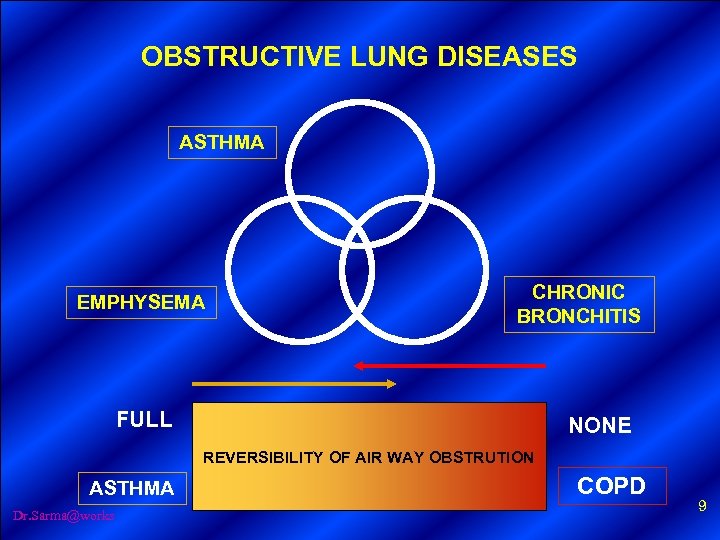
OBSTRUCTIVE LUNG DISEASES ASTHMA EMPHYSEMA CHRONIC BRONCHITIS FULL NONE REVERSIBILITY OF AIR WAY OBSTRUTION ASTHMA Dr. Sarma@works COPD 9
EPIDEMIOLGY OF COPD Dr. Sarma@works 10
CONTENTS 1. Definition - Key points 2. Epidemiology 3. Risk factors 4. Pathogenesis – Pathol 5. Clinical features 6. Diagnosis, Spirometry 7. Stop smoking strateg. 8. Management Dr. Sarma@works Guide KEY POINTS • Underestimated, often covert • It is not diagnosed until clinically overt • By that time it is moderately advanced. • The global burden of COPD will increase • Toll from ↑ tobacco use in alarming 11
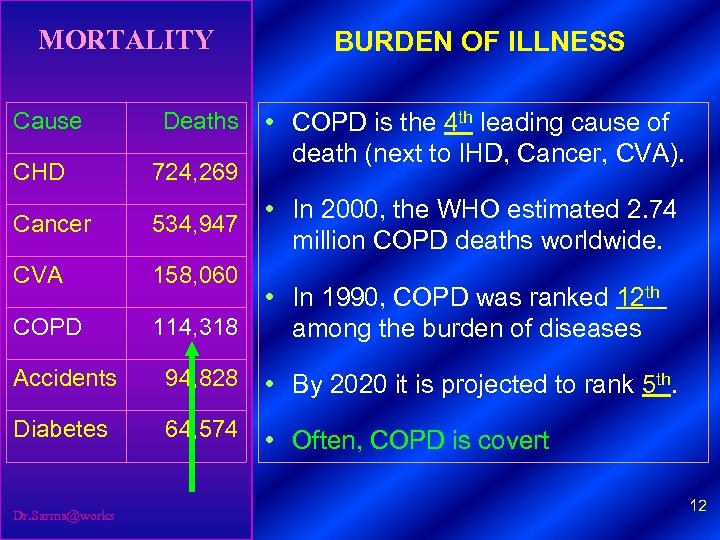
MORTALITY Cause Deaths CHD 724, 269 Cancer 534, 947 CVA BURDEN OF ILLNESS • COPD is the 4 th leading cause of death (next to IHD, Cancer, CVA). 158, 060 COPD • In 2000, the WHO estimated 2. 74 million COPD deaths worldwide. • In 1990, COPD was ranked 12 th 114, 318 among the burden of diseases Accidents 94, 828 • By 2020 it is projected to rank 5 th. Diabetes 64, 574 • Often, COPD is covert Dr. Sarma@works 12
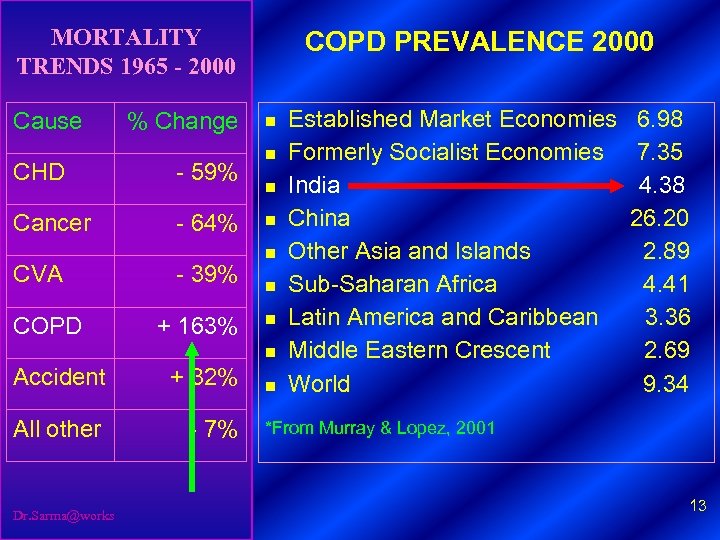
MORTALITY TRENDS 1965 - 2000 Cause % Change CHD - 59% Cancer - 64% CVA COPD - 39% + 163% COPD PREVALENCE 2000 n n n n Accident + 32% All other - 7% Dr. Sarma@works n Established Market Economies 6. 98 Formerly Socialist Economies 7. 35 India 4. 38 China 26. 20 Other Asia and Islands 2. 89 Sub-Saharan Africa 4. 41 Latin America and Caribbean 3. 36 Middle Eastern Crescent 2. 69 World 9. 34 *From Murray & Lopez, 2001 13
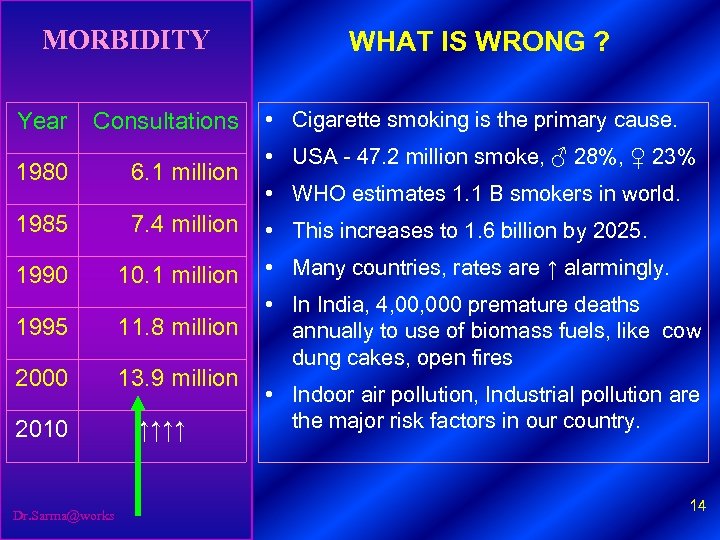
MORBIDITY Year Consultations WHAT IS WRONG ? • Cigarette smoking is the primary cause. • USA - 47. 2 million smoke, ♂ 28%, ♀ 23% 1980 6. 1 million 1985 7. 4 million • This increases to 1. 6 billion by 2025. 1990 10. 1 million • Many countries, rates are ↑ alarmingly. 1995 11. 8 million 2000 13. 9 million • In India, 4, 000 premature deaths annually to use of biomass fuels, like cow dung cakes, open fires 2010 Dr. Sarma@works ↑↑↑↑ • WHO estimates 1. 1 B smokers in world. • Indoor air pollution, Industrial pollution are the major risk factors in our country. 14
SMOKING - THE CULPRIT Dr. Sarma@works 15
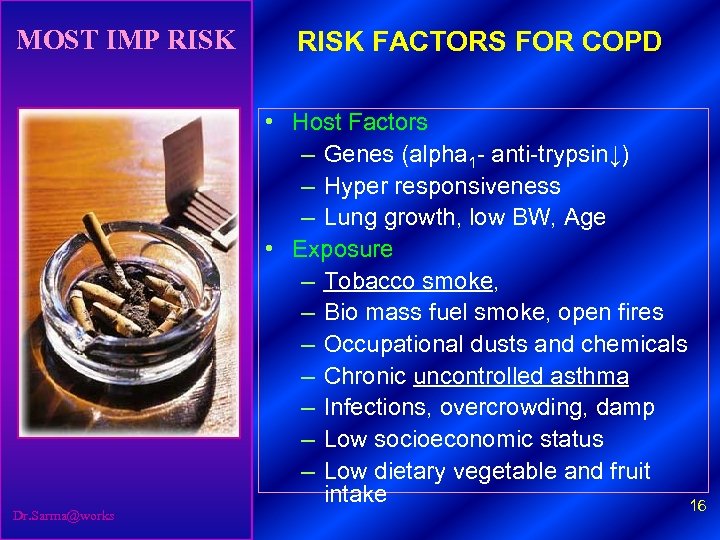
MOST IMP RISK Dr. Sarma@works RISK FACTORS FOR COPD • Host Factors – Genes (alpha 1 - anti-trypsin↓) – Hyper responsiveness – Lung growth, low BW, Age • Exposure – Tobacco smoke, – Bio mass fuel smoke, open fires – Occupational dusts and chemicals – Chronic uncontrolled asthma – Infections, overcrowding, damp – Low socioeconomic status – Low dietary vegetable and fruit intake 16

WOMEN SMOKERS PASSIVE SMOKERS Dr. Sarma@works 17
INTENSE CAUSE FOR CONCERN ? COLLEGE STUDENTS TENDER AGE GROUPS Dr. Sarma@works 18
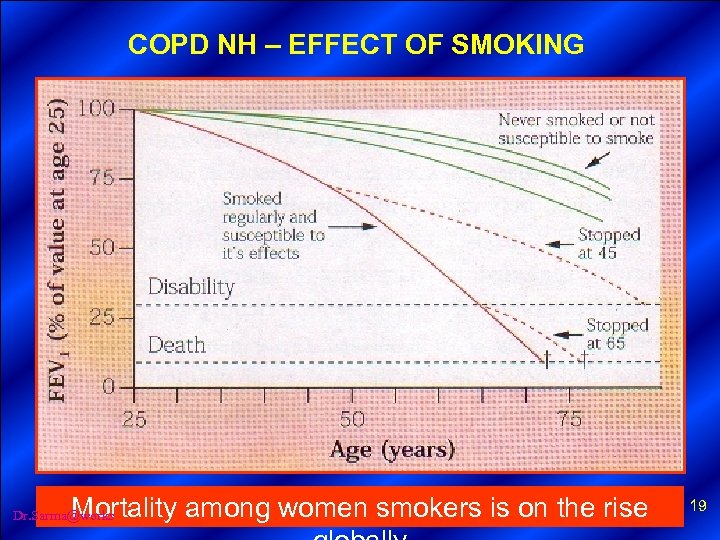
COPD NH – EFFECT OF SMOKING Mortality among women smokers is on the rise Dr. Sarma@works 19
PATHOGENESIS PATOLOGY Dr. Sarma@works AND 20
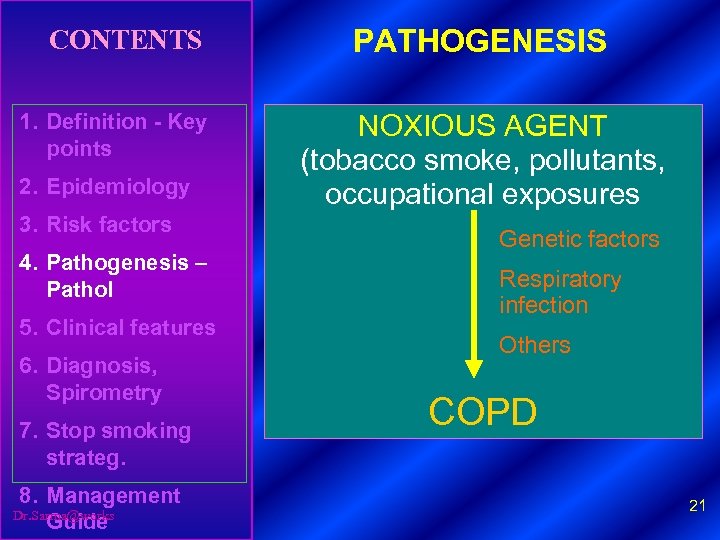
CONTENTS 1. Definition - Key points 2. Epidemiology 3. Risk factors 4. Pathogenesis – Pathol 5. Clinical features 6. Diagnosis, Spirometry 7. Stop smoking strateg. 8. Management Dr. Sarma@works Guide PATHOGENESIS NOXIOUS AGENT (tobacco smoke, pollutants, occupational exposures Genetic factors Respiratory infection Others COPD 21
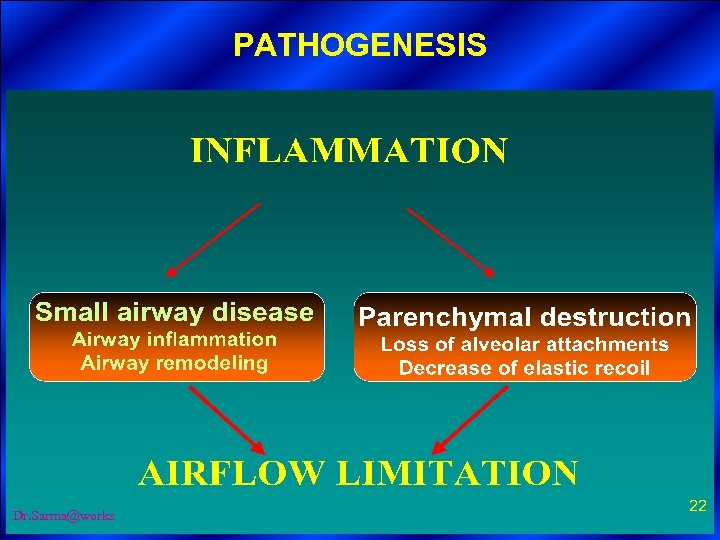
PATHOGENESIS 1. Definition -key points 2. Burden of COPD 3. Classification 4. Risk factors 5. Pathogenesis, 6. Pathophysiology, 7. Management 8. Future research Dr. Sarma@works 22
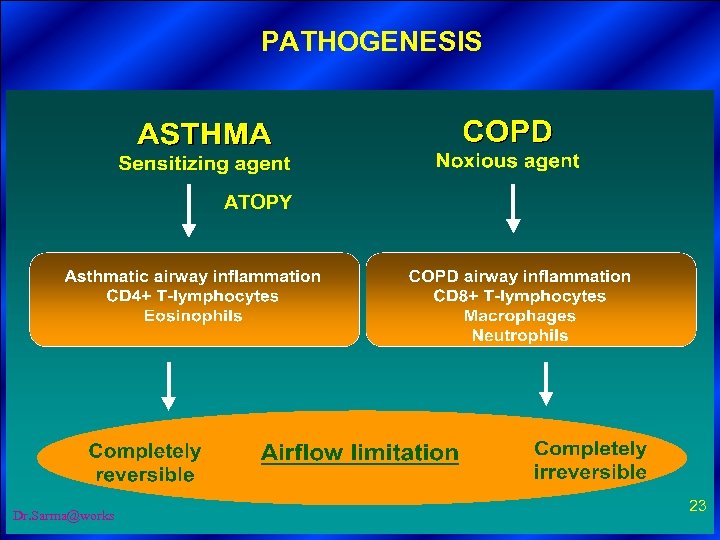
PATHOGENESIS 1. Definition -key points 2. Burden of COPD 3. Classification ATOPY 4. Risk factors 5. Pathogenesis, 6. Pathophysiology, 7. Management 8. Future research Dr. Sarma@works 23
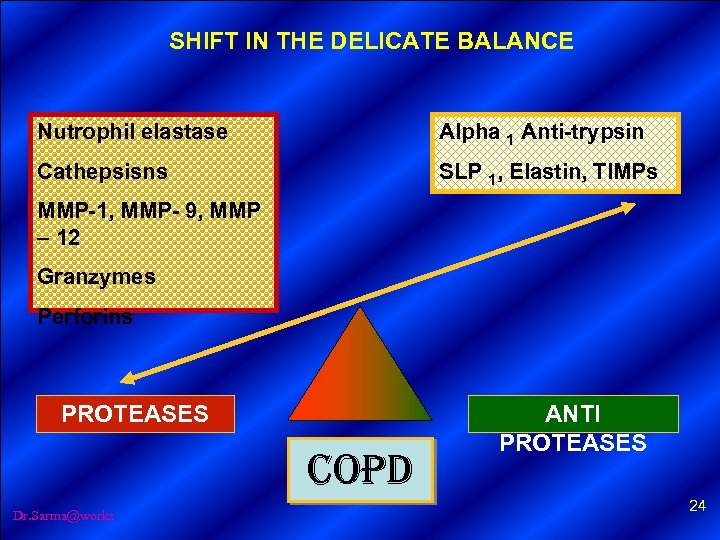
SHIFT IN THE DELICATE BALANCE Nutrophil elastase Alpha 1 Anti-trypsin Cathepsisns SLP 1, Elastin, TIMPs MMP-1, MMP- 9, MMP – 12 Granzymes Perforins PROTEASES COPD Dr. Sarma@works ANTI PROTEASES 24
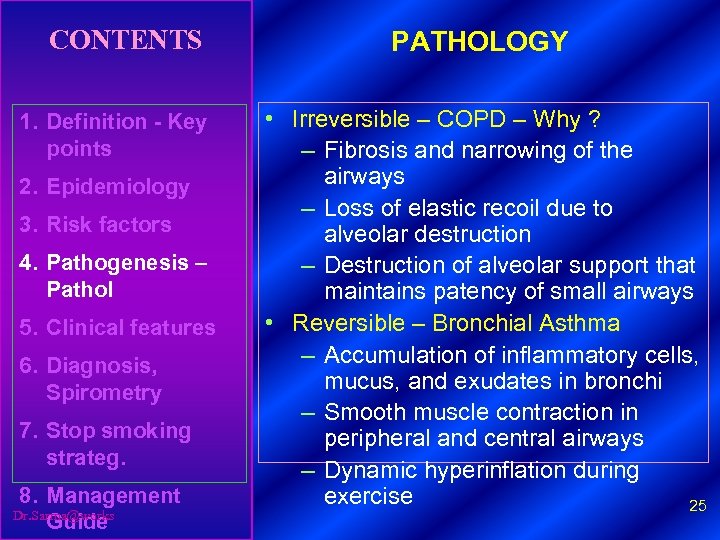
CONTENTS 1. Definition - Key points 2. Epidemiology 3. Risk factors 4. Pathogenesis – Pathol 5. Clinical features 6. Diagnosis, Spirometry 7. Stop smoking strateg. 8. Management Dr. Sarma@works Guide PATHOLOGY • Irreversible – COPD – Why ? – Fibrosis and narrowing of the airways – Loss of elastic recoil due to alveolar destruction – Destruction of alveolar support that maintains patency of small airways • Reversible – Bronchial Asthma – Accumulation of inflammatory cells, mucus, and exudates in bronchi – Smooth muscle contraction in peripheral and central airways – Dynamic hyperinflation during exercise 25
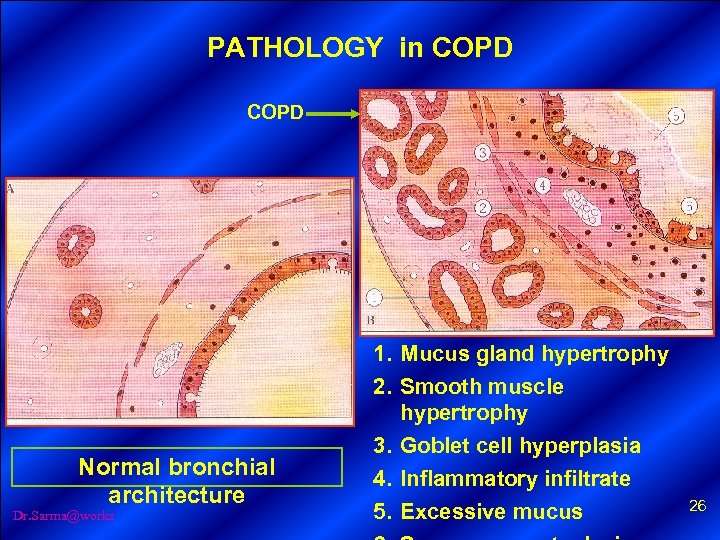
PATHOLOGY in COPD Normal bronchial architecture Dr. Sarma@works 1. Mucus gland hypertrophy 2. Smooth muscle hypertrophy 3. Goblet cell hyperplasia 4. Inflammatory infiltrate 5. Excessive mucus 26
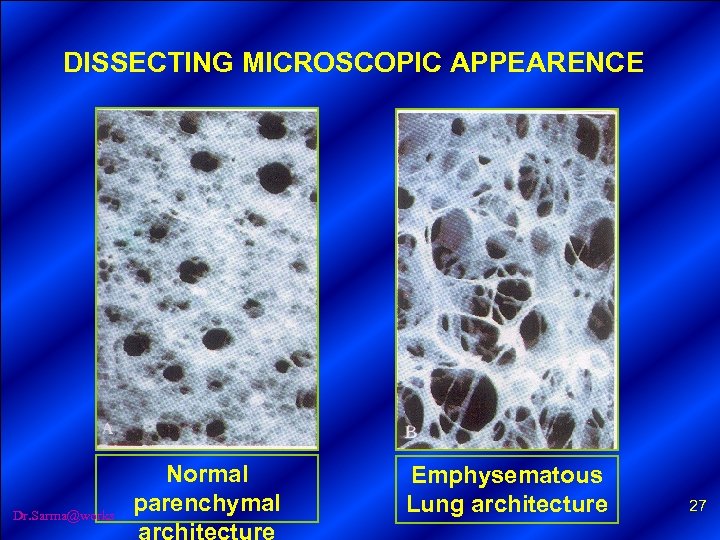
DISSECTING MICROSCOPIC APPEARENCE Dr. Sarma@works Normal parenchymal architecture Emphysematous Lung architecture 27
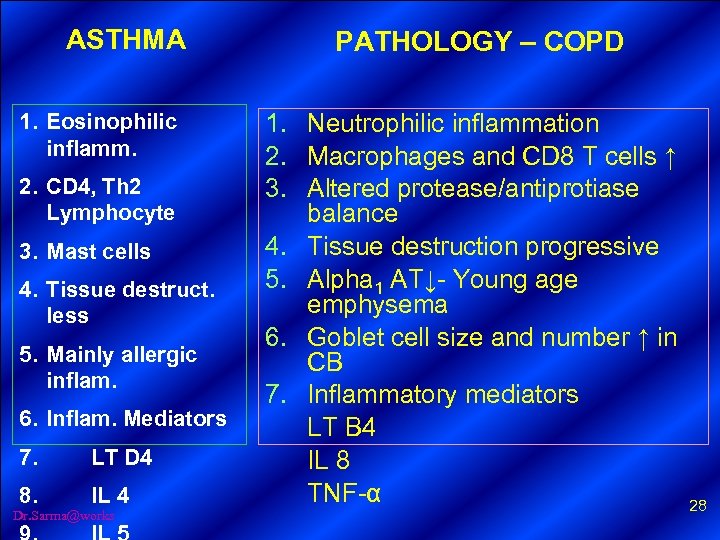
ASTHMA 1. Eosinophilic inflamm. 2. CD 4, Th 2 Lymphocyte 3. Mast cells 4. Tissue destruct. less 5. Mainly allergic inflam. 6. Inflam. Mediators 7. LT D 4 8. IL 4 Dr. Sarma@works PATHOLOGY – COPD 1. Neutrophilic inflammation 2. Macrophages and CD 8 T cells ↑ 3. Altered protease/antiprotiase balance 4. Tissue destruction progressive 5. Alpha 1 AT↓- Young age emphysema 6. Goblet cell size and number ↑ in CB 7. Inflammatory mediators LT B 4 IL 8 TNF-α 28
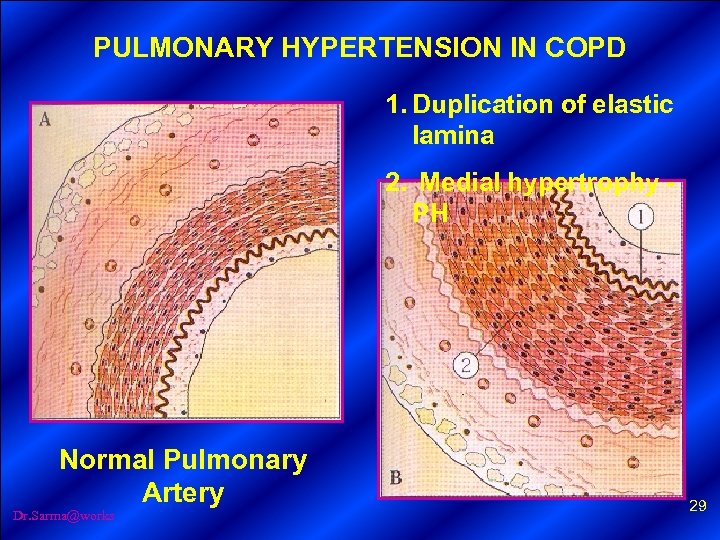
PULMONARY HYPERTENSION IN COPD 1. Duplication of elastic lamina 2. Medial hypertrophy - PH Normal Pulmonary Artery Dr. Sarma@works 29
CLINICAL FEATURES Dr. Sarma@works 30
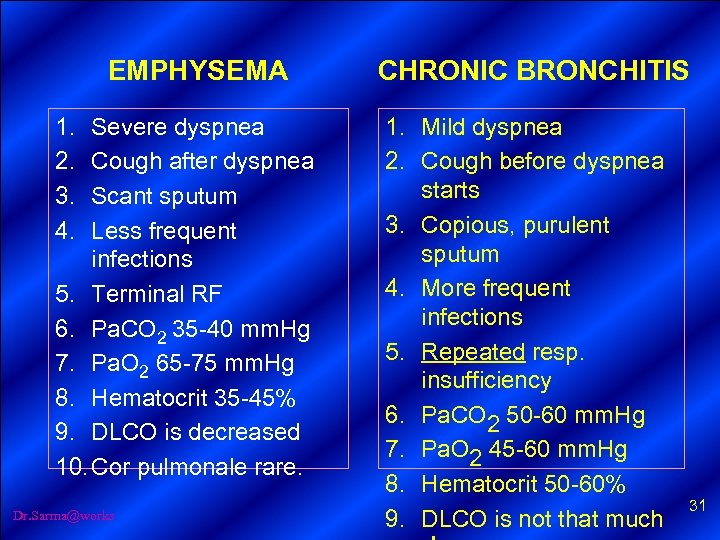
EMPHYSEMA 1. 2. 3. 4. Severe dyspnea Cough after dyspnea Scant sputum Less frequent infections 5. Terminal RF 6. Pa. CO 2 35 -40 mm. Hg 7. Pa. O 2 65 -75 mm. Hg 8. Hematocrit 35 -45% 9. DLCO is decreased 10. Cor pulmonale rare. Dr. Sarma@works CHRONIC BRONCHITIS 1. Mild dyspnea 2. Cough before dyspnea starts 3. Copious, purulent sputum 4. More frequent infections 5. Repeated resp. insufficiency 6. Pa. CO 2 50 -60 mm. Hg 7. Pa. O 2 45 -60 mm. Hg 8. Hematocrit 50 -60% 9. DLCO is not that much 31

EMPHYSEMA CHRONIC BRONCHITIS PINK PUFFER BLUE BLOTTER Dr. Sarma@works 32
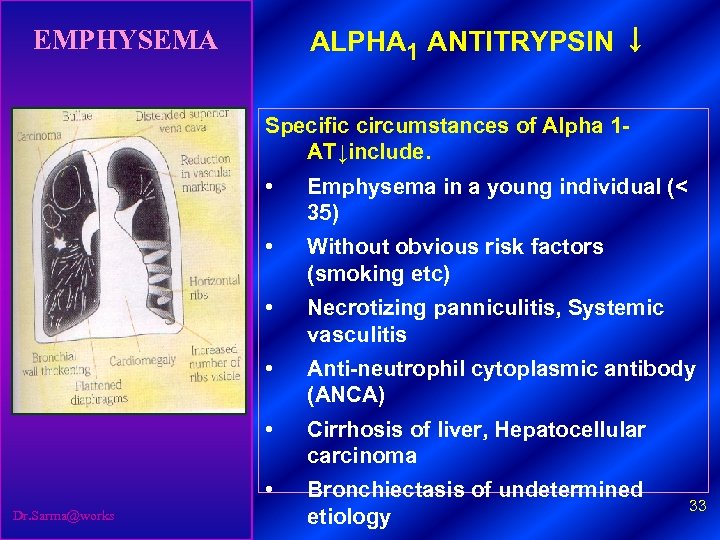
EMPHYSEMA ALPHA 1 ANTITRYPSIN ↓ Specific circumstances of Alpha 1 - AT↓include. • • Without obvious risk factors (smoking etc) • Necrotizing panniculitis, Systemic vasculitis • Anti-neutrophil cytoplasmic antibody (ANCA) • Cirrhosis of liver, Hepatocellular carcinoma • Dr. Sarma@works Emphysema in a young individual (< 35) Bronchiectasis of undetermined etiology 33
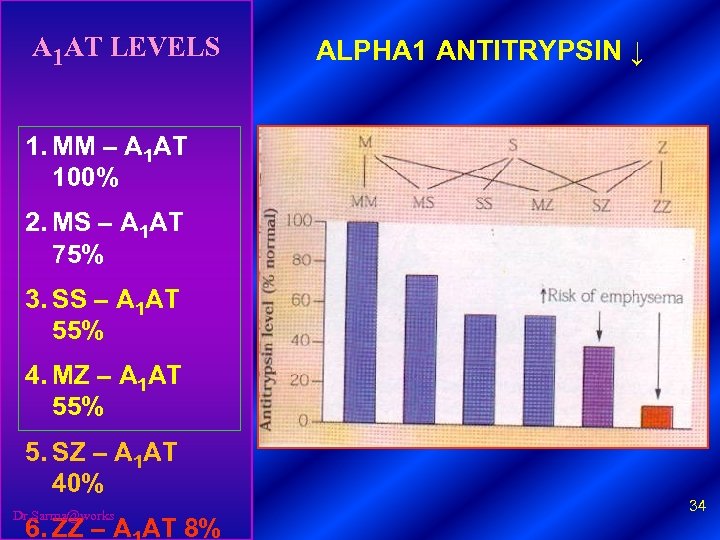
A 1 AT LEVELS ALPHA 1 ANTITRYPSIN ↓ 1. MM – A 1 AT 100% 2. MS – A 1 AT 75% 3. SS – A 1 AT 55% 4. MZ – A 1 AT 55% 5. SZ – A 1 AT 40% Dr. Sarma@works 6. ZZ – A AT 8% 34
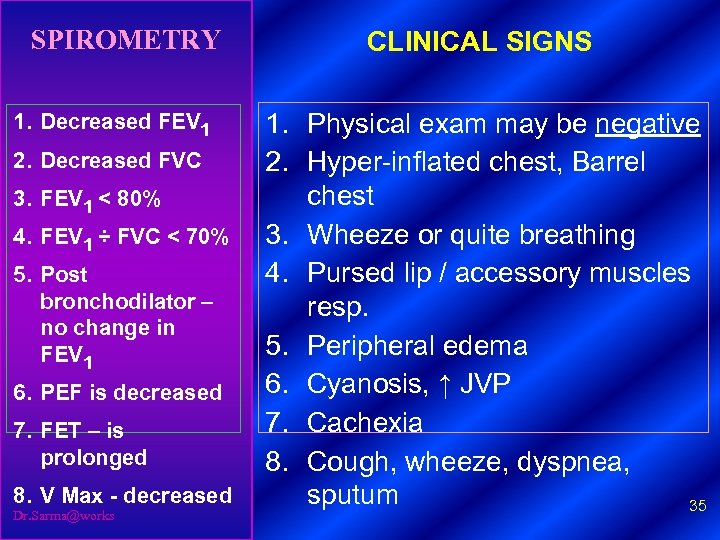
SPIROMETRY 1. Decreased FEV 1 2. Decreased FVC 3. FEV 1 < 80% 4. FEV 1 ÷ FVC < 70% 5. Post bronchodilator – no change in FEV 1 6. PEF is decreased 7. FET – is prolonged 8. V Max - decreased Dr. Sarma@works CLINICAL SIGNS 1. Physical exam may be negative 2. Hyper-inflated chest, Barrel chest 3. Wheeze or quite breathing 4. Pursed lip / accessory muscles resp. 5. Peripheral edema 6. Cyanosis, ↑ JVP 7. Cachexia 8. Cough, wheeze, dyspnea, sputum 35
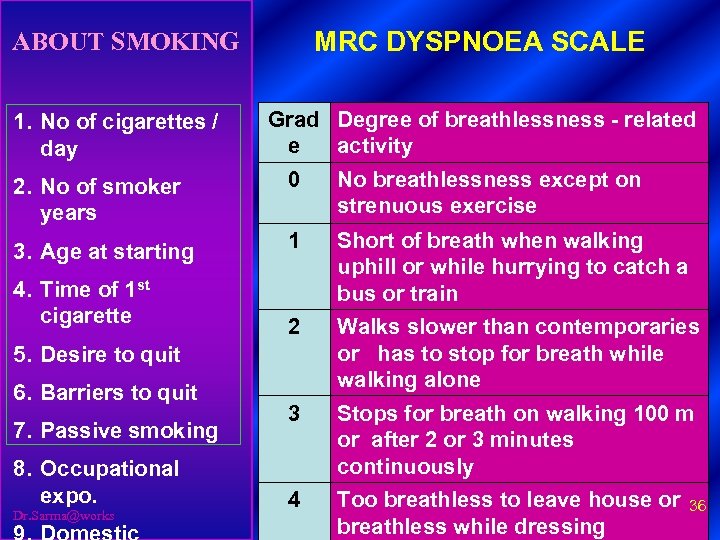
MRC DYSPNOEA SCALE ABOUT SMOKING 1. No of cigarettes / day Grad Degree of breathlessness - related e activity 2. No of smoker years 0 No breathlessness except on strenuous exercise 3. Age at starting 1 Short of breath when walking uphill or while hurrying to catch a bus or train 2 Walks slower than contemporaries or has to stop for breath while walking alone 3 Stops for breath on walking 100 m or after 2 or 3 minutes continuously 4 Too breathless to leave house or 36 breathless while dressing 4. Time of 1 st cigarette 5. Desire to quit 6. Barriers to quit 7. Passive smoking 8. Occupational expo. Dr. Sarma@works
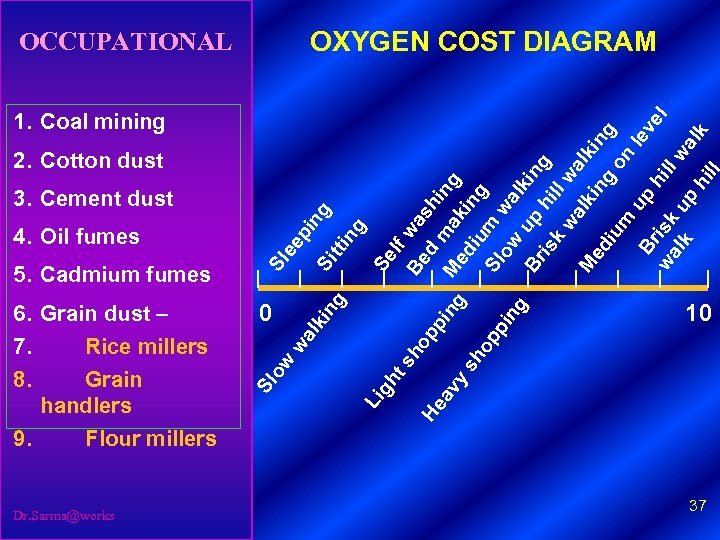
Dr. Sarma@works y sh g ng in pi pp op ho Be w a d sh i M mak n g ed iu ing S l m ow wa l Br u p ki n g h is k i l l wa wa l lk M i n ki n ed g g iu on m le Br u p ve hi is l wa k ll wa lk up lk h ill l f 2. Cotton dust av t s Se ng ng pi 1. Coal mining He gh tti ee 3. Cement dust Li Si ng ki 0 al Sl 6. Grain dust – 7. Rice millers 8. Grain handlers 9. Flour millers w 5. Cadmium fumes ow 4. Oil fumes Sl OCCUPATIONAL OXYGEN COST DIAGRAM 10 37
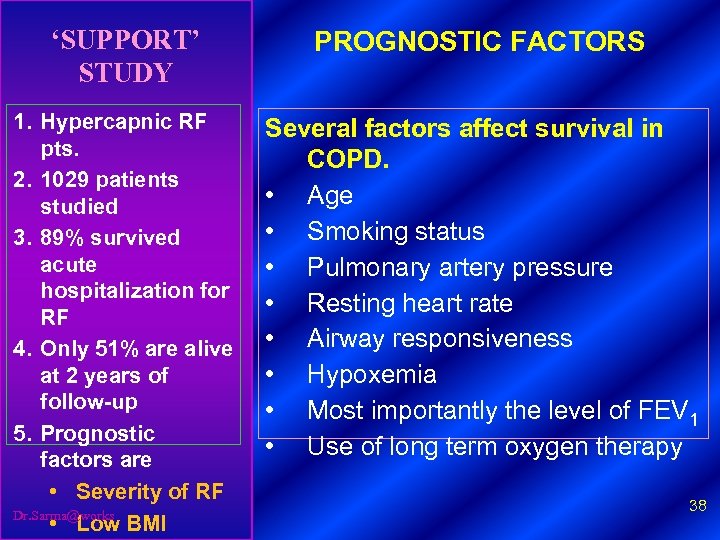
‘SUPPORT’ STUDY PROGNOSTIC FACTORS 1. Hypercapnic RF pts. 2. 1029 patients studied 3. 89% survived acute hospitalization for RF 4. Only 51% are alive at 2 years of follow-up 5. Prognostic factors are • Severity of RF Dr. Sarma@works • Low BMI Several factors affect survival in COPD. • Age • Smoking status • Pulmonary artery pressure • Resting heart rate • Airway responsiveness • Hypoxemia • Most importantly the level of FEV 1 • Use of long term oxygen therapy 38
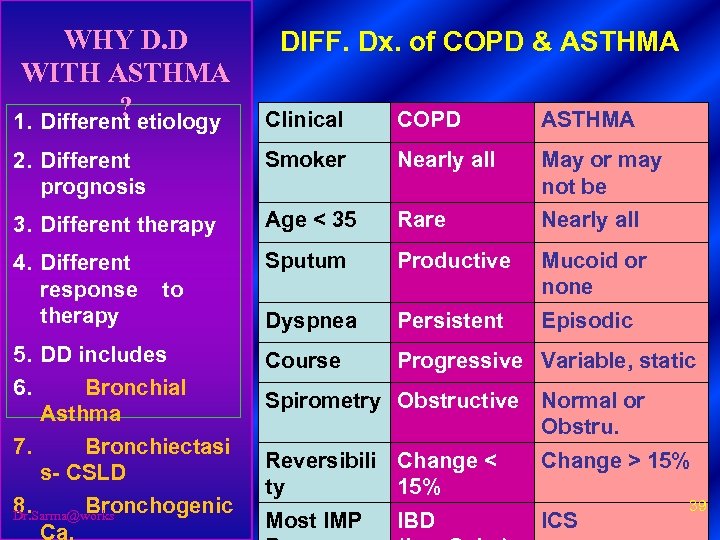
WHY D. D WITH ASTHMA ? 1. Different etiology DIFF. Dx. of COPD & ASTHMA Clinical COPD ASTHMA 2. Different prognosis Smoker Nearly all May or may not be 3. Different therapy Age < 35 Rare Nearly all 4. Different response to therapy Sputum Productive Mucoid or none Dyspnea Persistent Episodic 5. DD includes 6. Bronchial Asthma 7. Bronchiectasi s- CSLD 8. Bronchogenic Dr. Sarma@works Ca. Course Progressive Variable, static Spirometry Obstructive Normal or Obstru. Reversibili Change < ty 15% Change > 15% Most IMP ICS IBD 39

COPD IMAGES Dr. Sarma@works 40
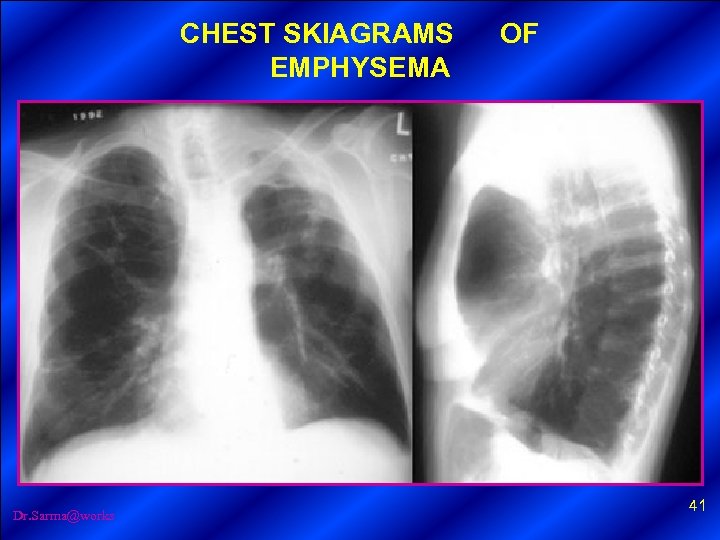
CHEST SKIAGRAMS OF EMPHYSEMA Dr. Sarma@works 41
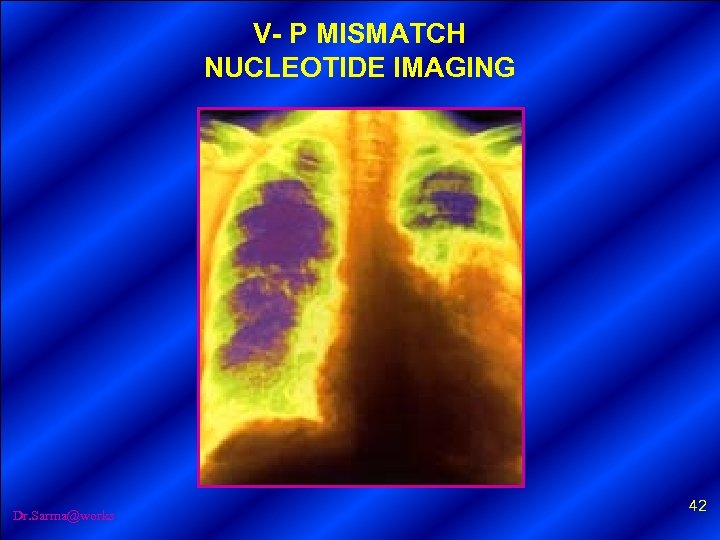
V- P MISMATCH NUCLEOTIDE IMAGING Dr. Sarma@works 42
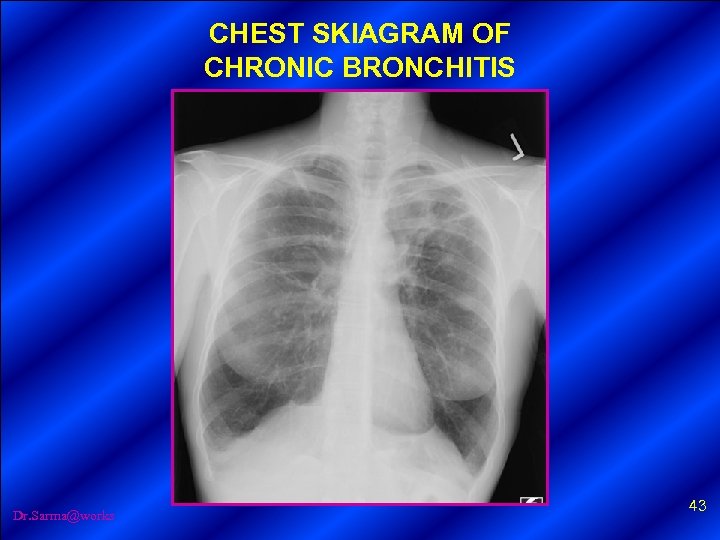
CHEST SKIAGRAM OF CHRONIC BRONCHITIS Dr. Sarma@works 43
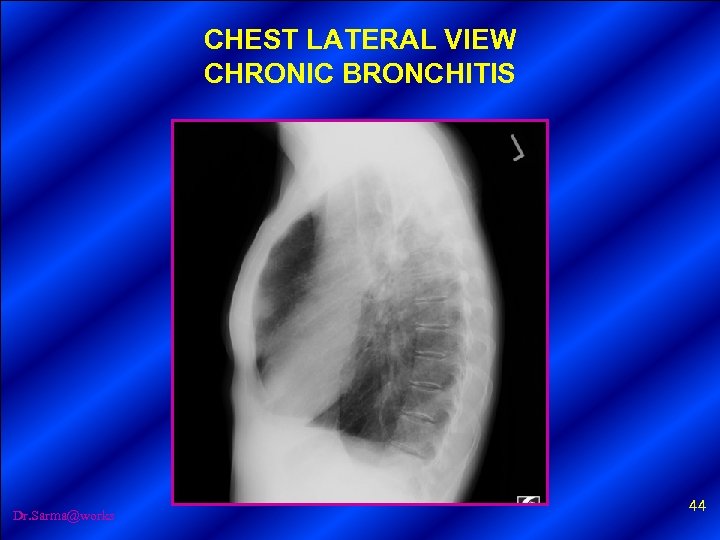
CHEST LATERAL VIEW CHRONIC BRONCHITIS Dr. Sarma@works 44
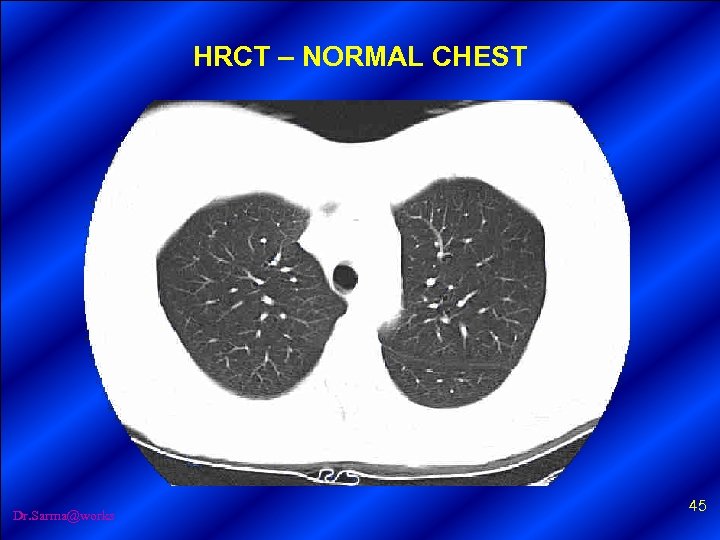
HRCT – NORMAL CHEST Dr. Sarma@works 45
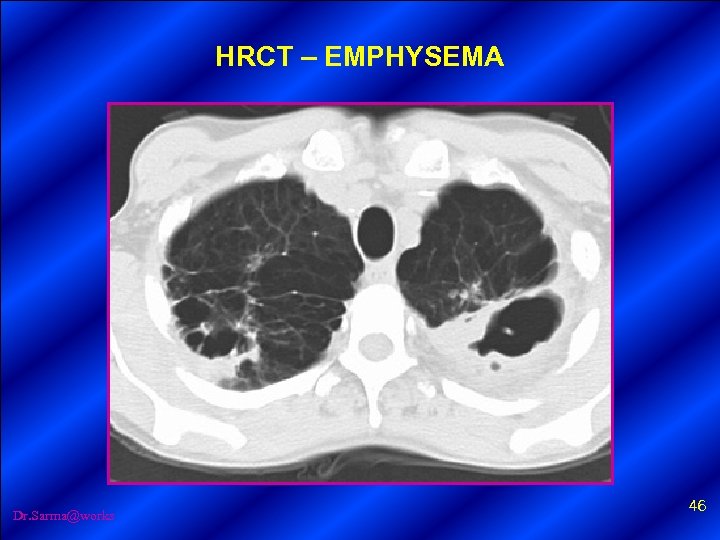
HRCT – EMPHYSEMA Dr. Sarma@works 46
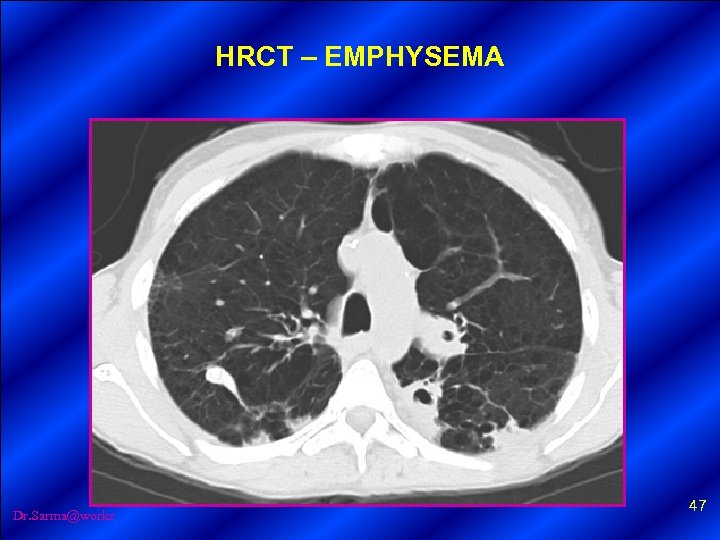
HRCT – EMPHYSEMA Dr. Sarma@works 47
ASSESSMENT OF STABLE COPD Dr. Sarma@works 48
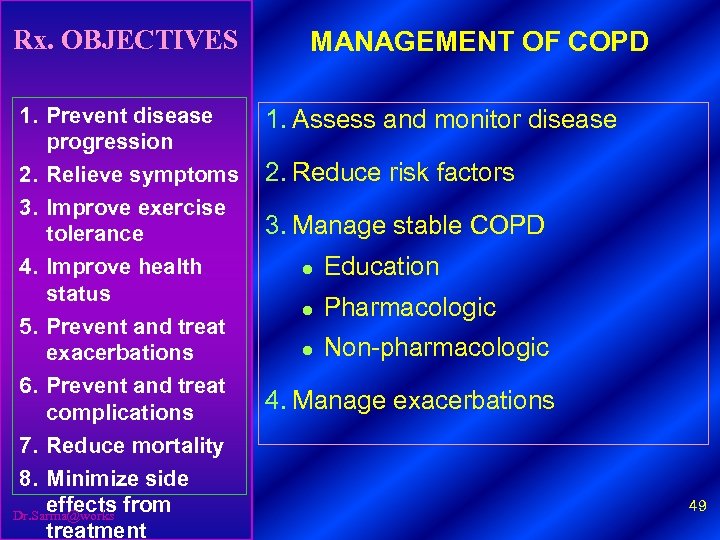
Rx. OBJECTIVES 1. Prevent disease progression 2. Relieve symptoms 3. Improve exercise tolerance 4. Improve health status 5. Prevent and treat exacerbations 6. Prevent and treat complications 7. Reduce mortality 8. Minimize side effects from Dr. Sarma@works treatment MANAGEMENT OF COPD 1. Assess and monitor disease 2. Reduce risk factors 3. Manage stable COPD l Education l Pharmacologic l Non-pharmacologic 4. Manage exacerbations 49
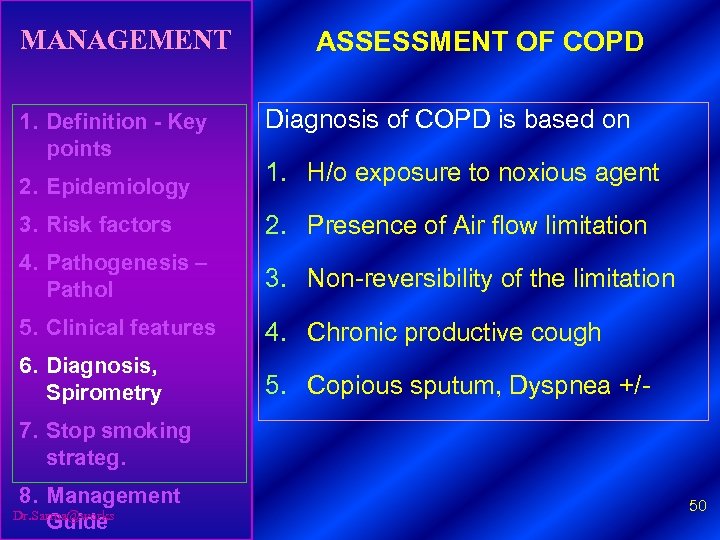
MANAGEMENT 1. Definition - Key points 2. Epidemiology ASSESSMENT OF COPD Diagnosis of COPD is based on 1. H/o exposure to noxious agent 3. Risk factors 2. Presence of Air flow limitation 4. Pathogenesis – Pathol 3. Non-reversibility of the limitation 5. Clinical features 4. Chronic productive cough 6. Diagnosis, Spirometry 5. Copious sputum, Dyspnea +/- 7. Stop smoking strateg. 8. Management Dr. Sarma@works Guide 50
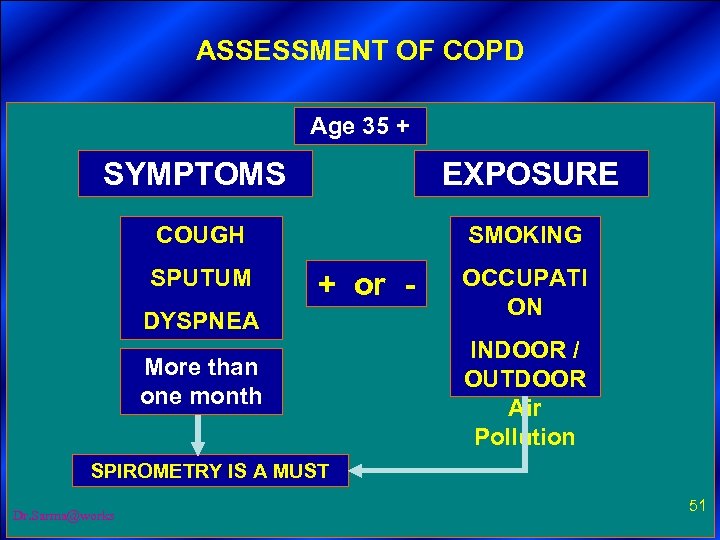
ASSESSMENT OF COPD 1. Assess and monitor disease Age 35 + SYMPTOMS 2. Reduce risk factors EXPOSURE COUGH 3. Manage stable COPD SPUTUM 4. Education DYSPNEA SMOKING + or - 5. Pharmacologic More than one month 6. Nonpharmacologic 7. Manage SPIROMETRY IS A MUST exacerbations Dr. Sarma@works OCCUPATI ON INDOOR / OUTDOOR Air Pollution 51
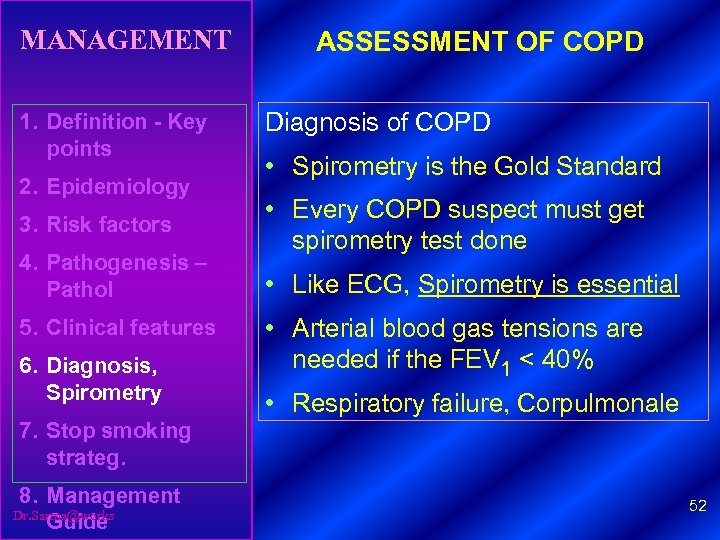
MANAGEMENT 1. Definition - Key points 2. Epidemiology 3. Risk factors 4. Pathogenesis – Pathol 5. Clinical features 6. Diagnosis, Spirometry ASSESSMENT OF COPD Diagnosis of COPD • Spirometry is the Gold Standard • Every COPD suspect must get spirometry test done • Like ECG, Spirometry is essential • Arterial blood gas tensions are needed if the FEV 1 < 40% • Respiratory failure, Corpulmonale 7. Stop smoking strateg. 8. Management Dr. Sarma@works Guide 52
TESTS 1. Definition - Key points 2. Epidemiology 3. Risk factors 4. Pathogenesis – Pathol 5. Clinical features 6. Diagnosis, Spirometry 7. Stop smoking strateg. 8. Management Dr. Sarma@works Guide OTHER INVESTIGATIONS 1. Serial spirometry tests 2. Pulse Oximetry 3. Alpha 1 Anti-trypsin levels 4. TLCO 5. HRCT 6. ECG 7. ECHO 8. Sputum culture 53
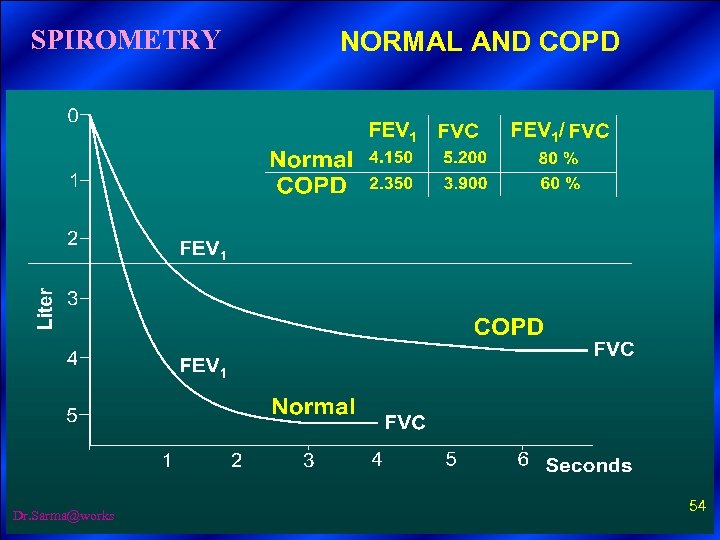
SPIROMETRY Dr. Sarma@works NORMAL AND COPD 54
REVERSIBILITY PROTOCOL 1. Definition - Key points WITH BRONCHODILATOR 1. 2. Epidemiology 3. Risk factors 4. Pathogenesis – Pathol 5. Clinical features 6. Diagnosis, Spirometry 7. Stop smoking strateg. 8. Management Dr. Sarma@works Guide 3. 4. 5. 6. Patient must be clinically stable Patient should avoid Short acting βagonists for 6 hours Long acting βagonists for 12 hours SR Theophylline for 24 hours Baseline spirometry Nebulize Salbuamol 2. 5 mg + Ipatropium 500 mg for 15 minutes with Nacl Wait for 30 minutes Repeat spirometry 55
REVERSIBILITY PROTOCOL WITH STEROIDS 1. Definition - Key points 1. Spirometry before and after steroid 2. Epidemiology 2. Two weeks treatment with 30 mg Prednisolone daily or 3. Risk factors 4. Pathogenesis – Pathol 5. Clinical features 6. Diagnosis, Spirometry 3. Six weeks treatment with 800 mcg to 1000 mcg of inhaled betamethasone/day 4. Results to be interpreted. Look for steroid contraindications 7. Stop smoking strateg. This predicts the COPD group who will benefit 8. Management Dr. Sarma@works Guide from inhaled or systemic steroids 56
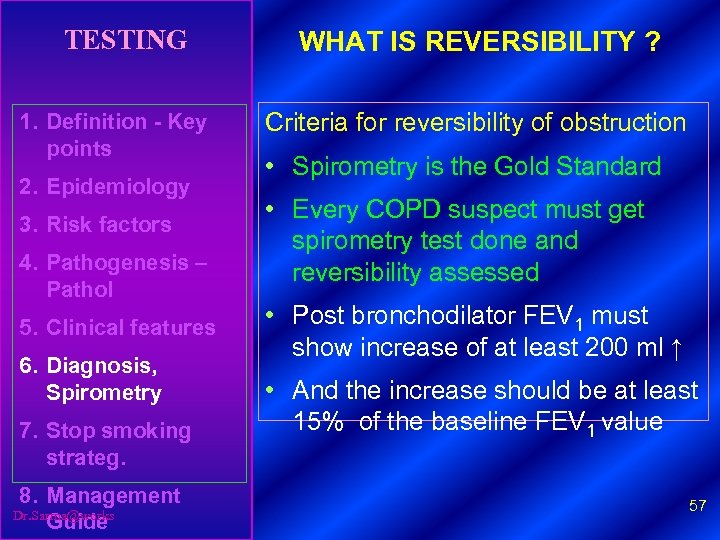
TESTING 1. Definition - Key points 2. Epidemiology 3. Risk factors 4. Pathogenesis – Pathol 5. Clinical features 6. Diagnosis, Spirometry 7. Stop smoking strateg. 8. Management Dr. Sarma@works Guide WHAT IS REVERSIBILITY ? Criteria for reversibility of obstruction • Spirometry is the Gold Standard • Every COPD suspect must get spirometry test done and reversibility assessed • Post bronchodilator FEV 1 must show increase of at least 200 ml ↑ • And the increase should be at least 15% of the baseline FEV 1 value 57
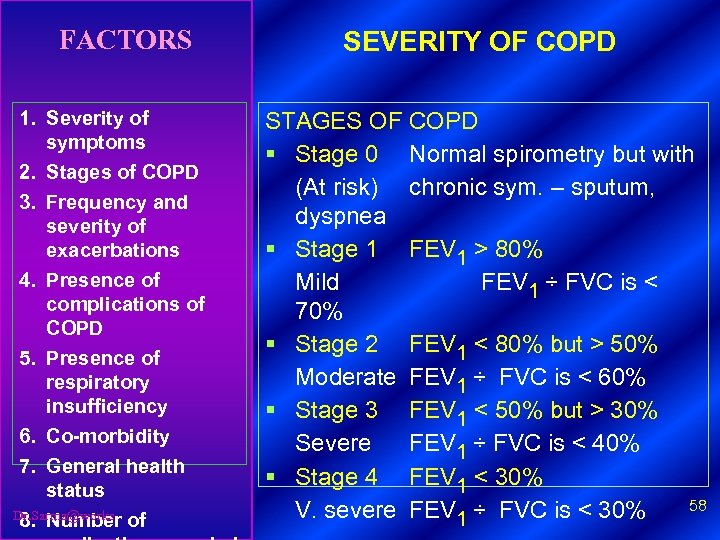
FACTORS 1. Severity of symptoms 2. Stages of COPD 3. Frequency and severity of exacerbations 4. Presence of complications of COPD 5. Presence of respiratory insufficiency 6. Co-morbidity 7. General health status Dr. Sarma@works 8. Number of SEVERITY OF COPD STAGES OF COPD § Stage 0 Normal spirometry but with (At risk) chronic sym. – sputum, dyspnea § Stage 1 FEV 1 > 80% Mild FEV 1 ÷ FVC is < 70% § Stage 2 FEV 1 < 80% but > 50% Moderate FEV 1 ÷ FVC is < 60% § Stage 3 FEV 1 < 50% but > 30% Severe FEV 1 ÷ FVC is < 40% § Stage 4 FEV 1 < 30% 58 V. severe FEV 1 ÷ FVC is < 30%
RISK REDUCTION STRATEGIES Dr. Sarma@works 59
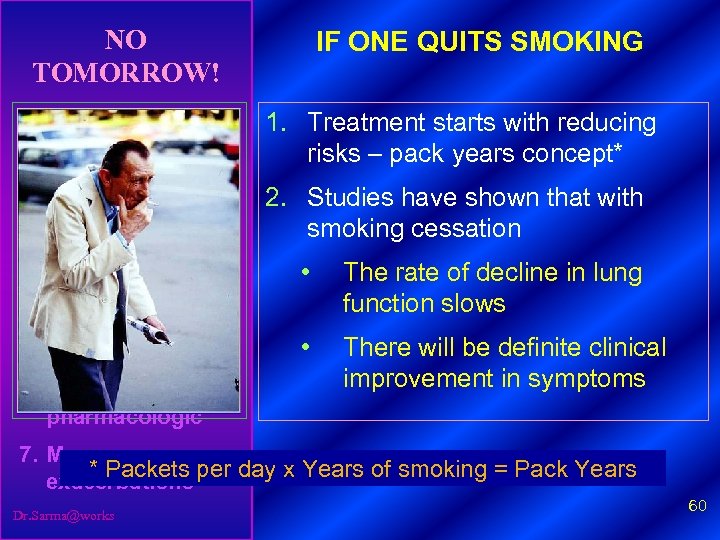
NO TOMORROW! IF ONE QUITS SMOKING 1. Assess and monitor disease 1. Treatment starts with reducing risks – pack years concept* 2. Reduce risk factors 2. Studies have shown that with smoking cessation 3. Manage stable COPD • The rate of decline in lung function slows • There will be definite clinical improvement in symptoms 4. Education 5. Pharmacologic 6. Nonpharmacologic 7. Manage * Packets per day x Years of smoking = Pack Years exacerbations Dr. Sarma@works 60
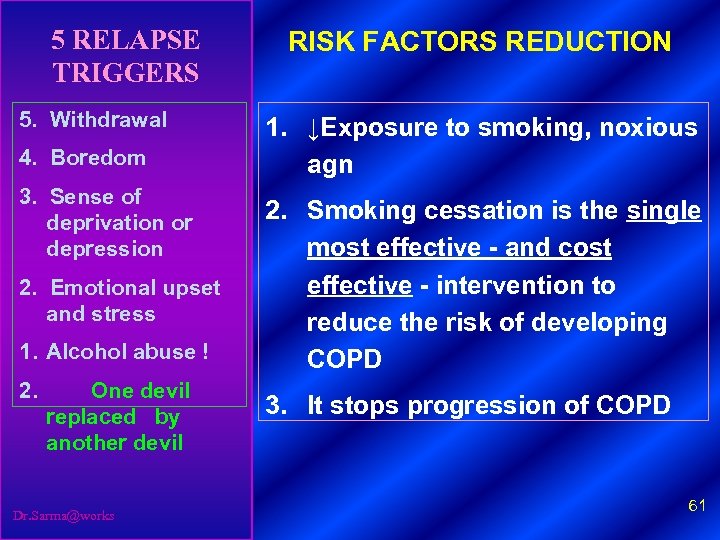
5 RELAPSE TRIGGERS 5. Withdrawal 4. Boredom 3. Sense of deprivation or depression 2. Emotional upset and stress 1. Alcohol abuse ! 2. One devil replaced by another devil Dr. Sarma@works RISK FACTORS REDUCTION 1. ↓Exposure to smoking, noxious agn 2. Smoking cessation is the single most effective - and cost effective - intervention to reduce the risk of developing COPD 3. It stops progression of COPD 61
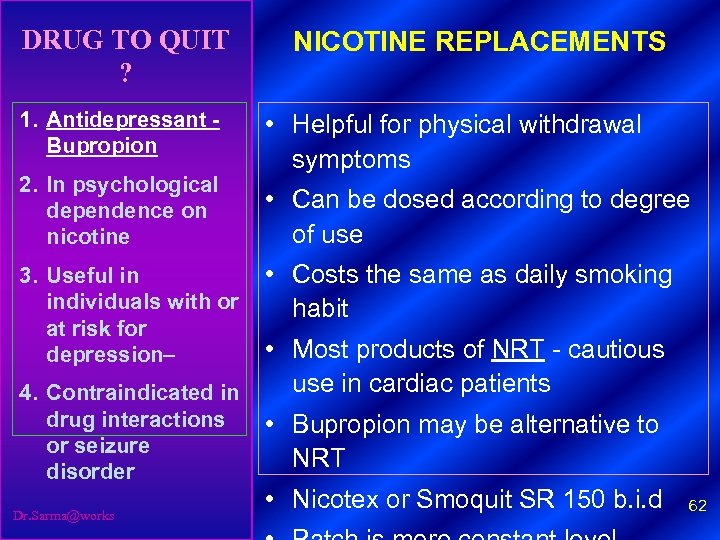
DRUG TO QUIT ? 1. Antidepressant - Bupropion 2. In psychological dependence on nicotine NICOTINE REPLACEMENTS • Helpful for physical withdrawal symptoms • Can be dosed according to degree of use 3. Useful in • Costs the same as daily smoking individuals with or habit at risk for • Most products of NRT - cautious depression– use in cardiac patients 4. Contraindicated in drug interactions • Bupropion may be alternative to or seizure NRT disorder Dr. Sarma@works • Nicotex or Smoquit SR 150 b. i. d 62
COPD MANAGEMENT LATEST GUIDELINES Dr. Sarma@works 63
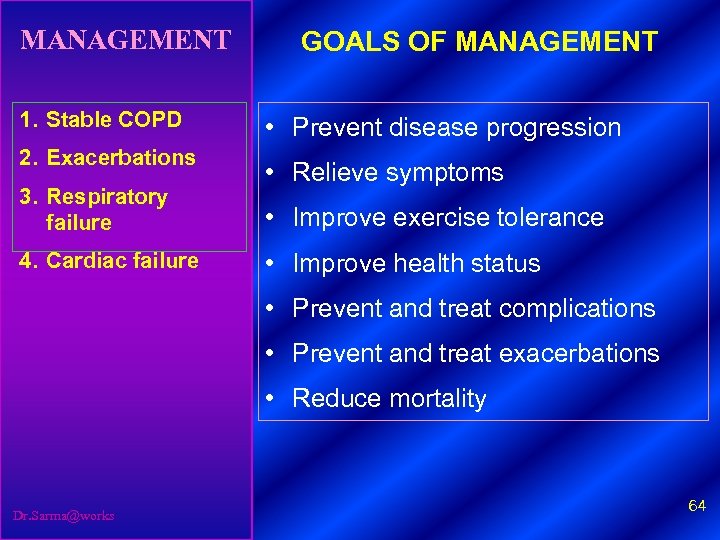
MANAGEMENT 1. Stable COPD 2. Exacerbations 3. Respiratory failure 4. Cardiac failure GOALS OF MANAGEMENT • Prevent disease progression • Relieve symptoms • Improve exercise tolerance • Improve health status • Prevent and treat complications • Prevent and treat exacerbations • Reduce mortality Dr. Sarma@works 64
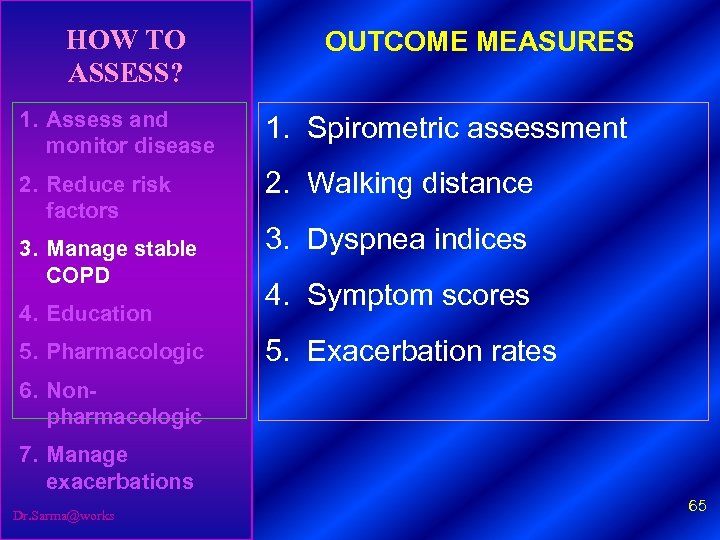
HOW TO ASSESS? OUTCOME MEASURES 1. Assess and monitor disease 1. Spirometric assessment 2. Reduce risk factors 2. Walking distance 3. Manage stable COPD 4. Education 5. Pharmacologic 3. Dyspnea indices 4. Symptom scores 5. Exacerbation rates 6. Nonpharmacologic 7. Manage exacerbations Dr. Sarma@works 65
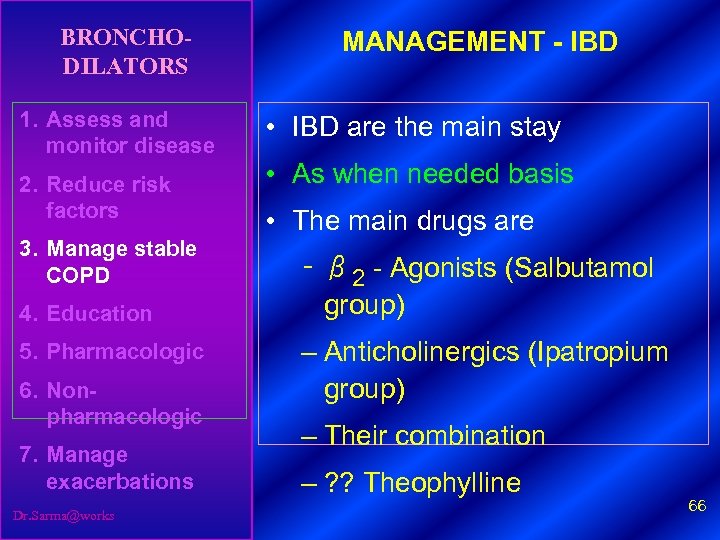
BRONCHODILATORS 1. Assess and monitor disease 2. Reduce risk factors 3. Manage stable COPD 4. Education 5. Pharmacologic 6. Nonpharmacologic 7. Manage exacerbations Dr. Sarma@works MANAGEMENT - IBD • IBD are the main stay • As when needed basis • The main drugs are – β 2 - Agonists (Salbutamol group) – Anticholinergics (Ipatropium group) – Their combination – ? ? Theophylline 66
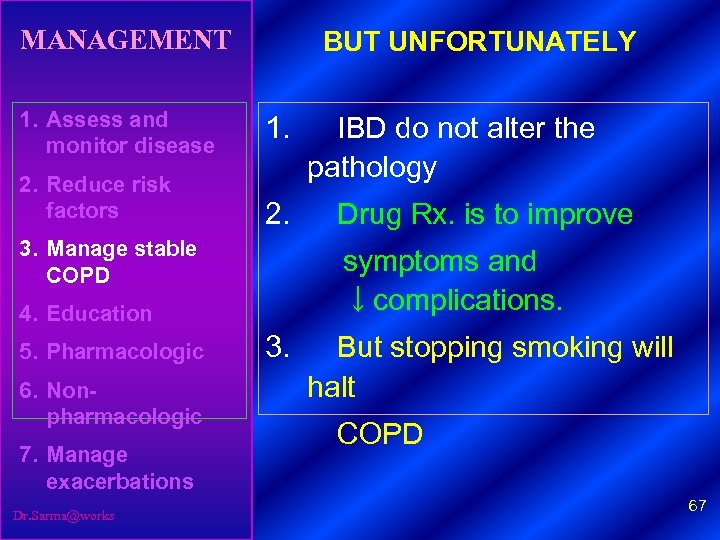
MANAGEMENT 1. Assess and monitor disease 2. Reduce risk factors BUT UNFORTUNATELY 1. 2. 3. Manage stable COPD 6. Nonpharmacologic 7. Manage exacerbations Dr. Sarma@works Drug Rx. is to improve symptoms and ↓complications. 4. Education 5. Pharmacologic IBD do not alter the pathology 3. But stopping smoking will halt COPD 67
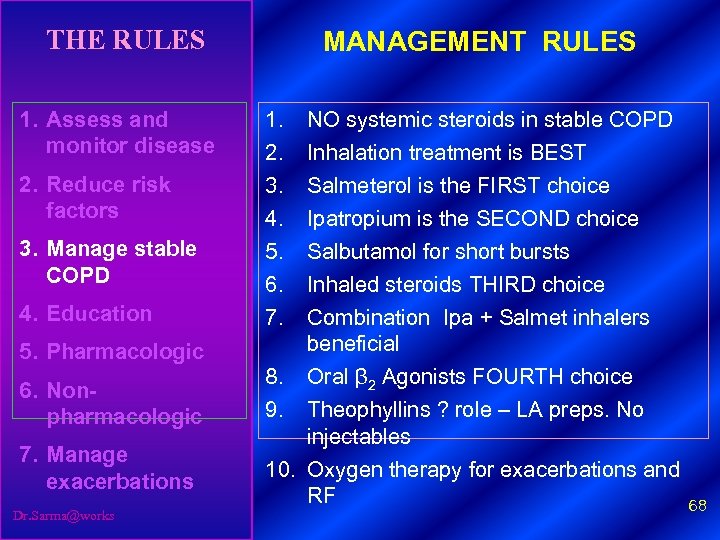
THE RULES 1. Assess and monitor disease 2. Reduce risk factors 3. Manage stable COPD 4. Education 5. Pharmacologic 6. Nonpharmacologic 7. Manage exacerbations Dr. Sarma@works MANAGEMENT RULES 1. 2. 3. 4. 5. 6. 7. NO systemic steroids in stable COPD Inhalation treatment is BEST Salmeterol is the FIRST choice Ipatropium is the SECOND choice Salbutamol for short bursts Inhaled steroids THIRD choice Combination Ipa + Salmet inhalers beneficial 8. Oral β 2 Agonists FOURTH choice 9. Theophyllins ? role – LA preps. No injectables 10. Oxygen therapy for exacerbations and RF 68
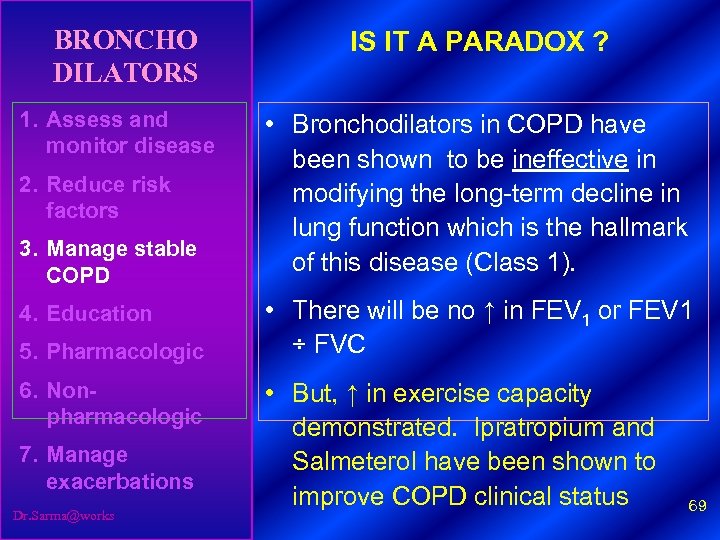
BRONCHO DILATORS IS IT A PARADOX ? 1. Assess and monitor disease • Bronchodilators in COPD have been shown to be ineffective in modifying the long-term decline in lung function which is the hallmark of this disease (Class 1). 2. Reduce risk factors 3. Manage stable COPD 4. Education 5. Pharmacologic 6. Nonpharmacologic 7. Manage exacerbations Dr. Sarma@works • There will be no ↑ in FEV 1 or FEV 1 ÷ FVC • But, ↑ in exercise capacity demonstrated. Ipratropium and Salmeterol have been shown to improve COPD clinical status 69
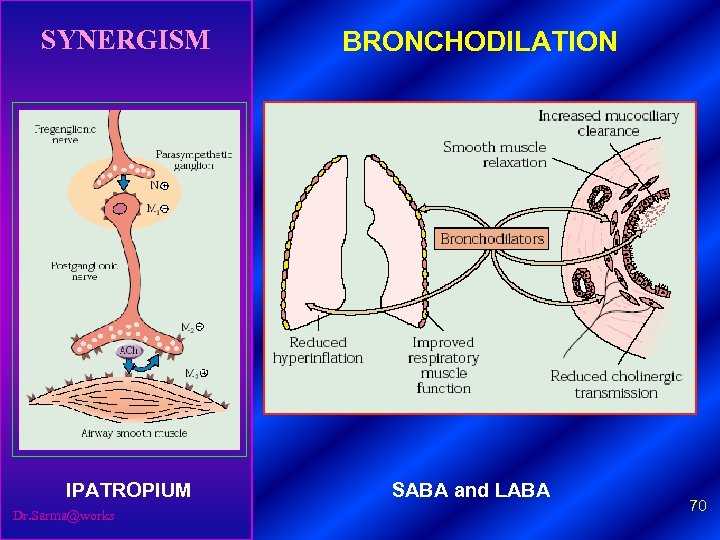
SYNERGISM IPATROPIUM Dr. Sarma@works BRONCHODILATION SABA and LABA 70
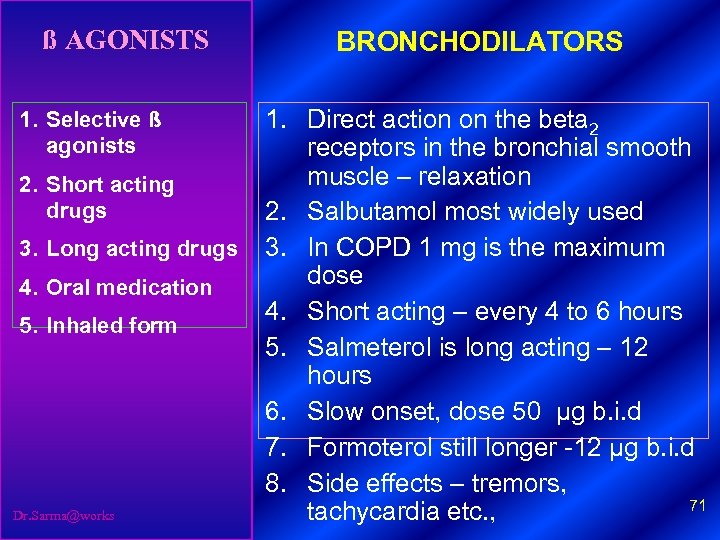
ß AGONISTS 1. Selective ß agonists 2. Short acting drugs 3. Long acting drugs 4. Oral medication 5. Inhaled form Dr. Sarma@works BRONCHODILATORS 1. Direct action on the beta 2 receptors in the bronchial smooth muscle – relaxation 2. Salbutamol most widely used 3. In COPD 1 mg is the maximum dose 4. Short acting – every 4 to 6 hours 5. Salmeterol is long acting – 12 hours 6. Slow onset, dose 50 μg b. i. d 7. Formoterol still longer -12 μg b. i. d 8. Side effects – tremors, 71 tachycardia etc. ,
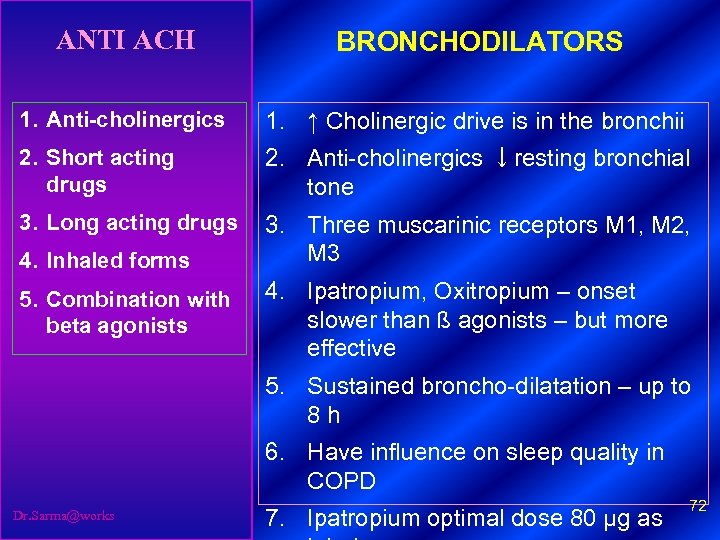
ANTI ACH BRONCHODILATORS 1. Anti-cholinergics 1. ↑ Cholinergic drive is in the bronchii 2. Short acting drugs 2. Anti-cholinergics ↓resting bronchial tone 3. Long acting drugs 3. Three muscarinic receptors M 1, M 2, M 3 4. Inhaled forms 5. Combination with beta agonists 4. Ipatropium, Oxitropium – onset slower than ß agonists – but more effective 5. Sustained broncho-dilatation – up to 8 h 6. Have influence on sleep quality in COPD Dr. Sarma@works 7. Ipatropium optimal dose 80 μg as 72
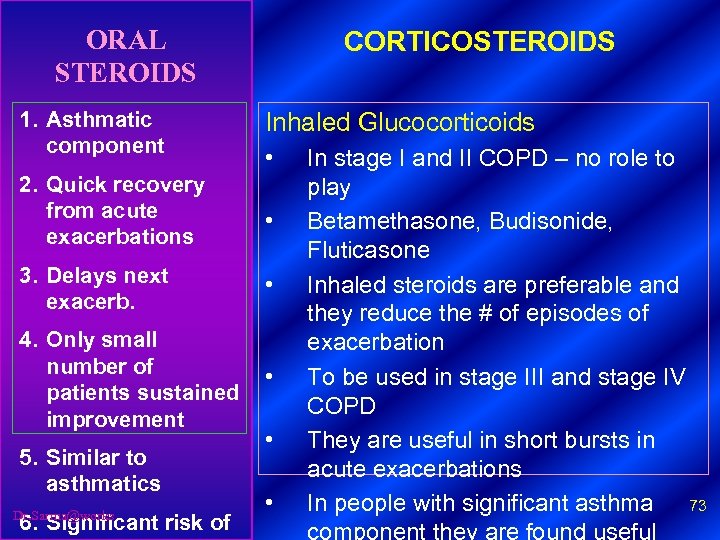
ORAL STEROIDS CORTICOSTEROIDS 1. Asthmatic component Inhaled Glucocorticoids 2. Quick recovery from acute exacerbations • 3. Delays next exacerb. • • 4. Only small number of • patients sustained improvement 5. Similar to asthmatics Dr. Sarma@works 6. Significant risk of • • In stage I and II COPD – no role to play Betamethasone, Budisonide, Fluticasone Inhaled steroids are preferable and they reduce the # of episodes of exacerbation To be used in stage III and stage IV COPD They are useful in short bursts in acute exacerbations In people with significant asthma 73
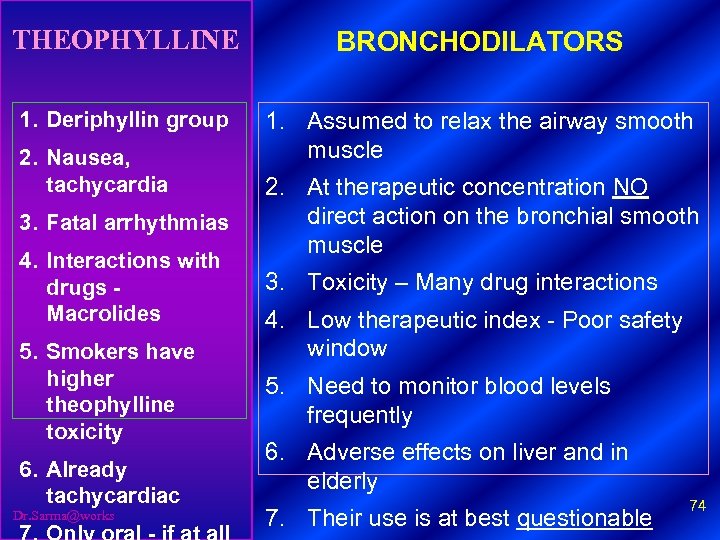
THEOPHYLLINE BRONCHODILATORS 1. Deriphyllin group 1. Assumed to relax the airway smooth muscle 2. Nausea, tachycardia 3. Fatal arrhythmias 4. Interactions with drugs - Macrolides 5. Smokers have higher theophylline toxicity 6. Already tachycardiac Dr. Sarma@works 2. At therapeutic concentration NO direct action on the bronchial smooth muscle 3. Toxicity – Many drug interactions 4. Low therapeutic index - Poor safety window 5. Need to monitor blood levels frequently 6. Adverse effects on liver and in elderly 7. Their use is at best questionable 74
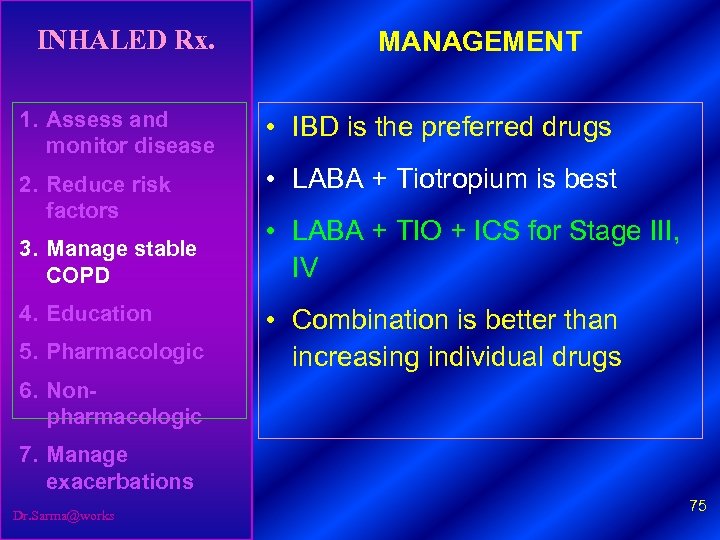
INHALED Rx. MANAGEMENT 1. Assess and monitor disease • IBD is the preferred drugs 2. Reduce risk factors • LABA + Tiotropium is best 3. Manage stable COPD 4. Education 5. Pharmacologic • LABA + TIO + ICS for Stage III, IV • Combination is better than increasing individual drugs 6. Nonpharmacologic 7. Manage exacerbations Dr. Sarma@works 75
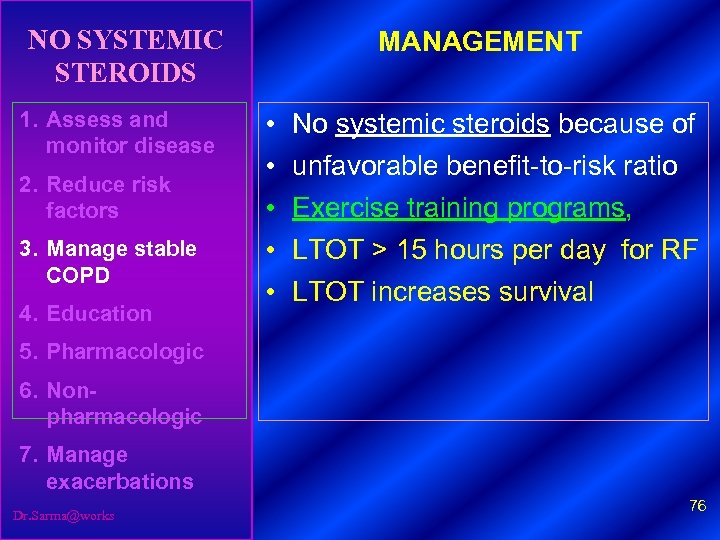
NO SYSTEMIC STEROIDS 1. Assess and monitor disease 2. Reduce risk factors 3. Manage stable COPD 4. Education MANAGEMENT • • • No systemic steroids because of unfavorable benefit-to-risk ratio Exercise training programs, LTOT > 15 hours per day for RF LTOT increases survival 5. Pharmacologic 6. Nonpharmacologic 7. Manage exacerbations Dr. Sarma@works 76
MANGEMENT AS PER STAGING Dr. Sarma@works 77
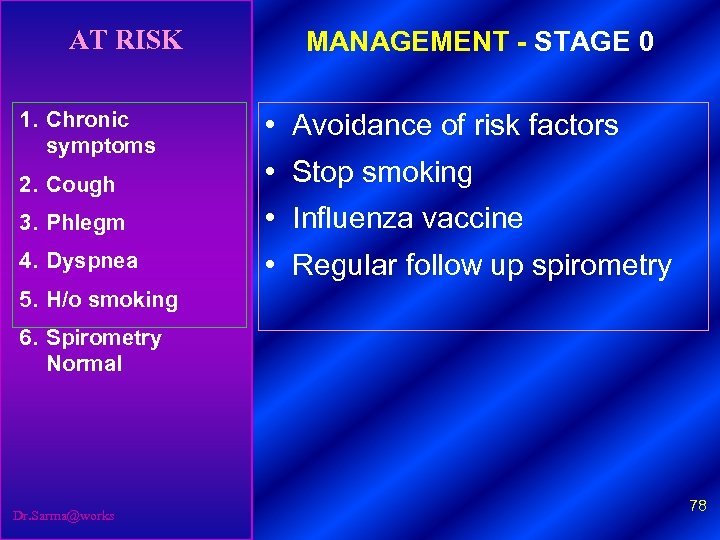
AT RISK 1. Chronic symptoms MANAGEMENT - STAGE 0 • Avoidance of risk factors 2. Cough • Stop smoking 3. Phlegm • Influenza vaccine 4. Dyspnea • Regular follow up spirometry 5. H/o smoking 6. Spirometry Normal Dr. Sarma@works 78
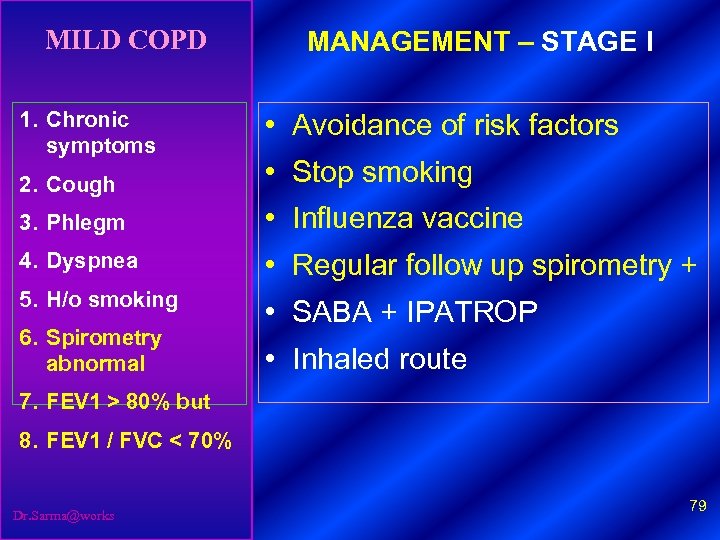
MILD COPD 1. Chronic symptoms MANAGEMENT – STAGE I • Avoidance of risk factors 2. Cough • Stop smoking 3. Phlegm • Influenza vaccine 4. Dyspnea • Regular follow up spirometry + 5. H/o smoking • SABA + IPATROP 6. Spirometry abnormal • Inhaled route 7. FEV 1 > 80% but 8. FEV 1 / FVC < 70% Dr. Sarma@works 79
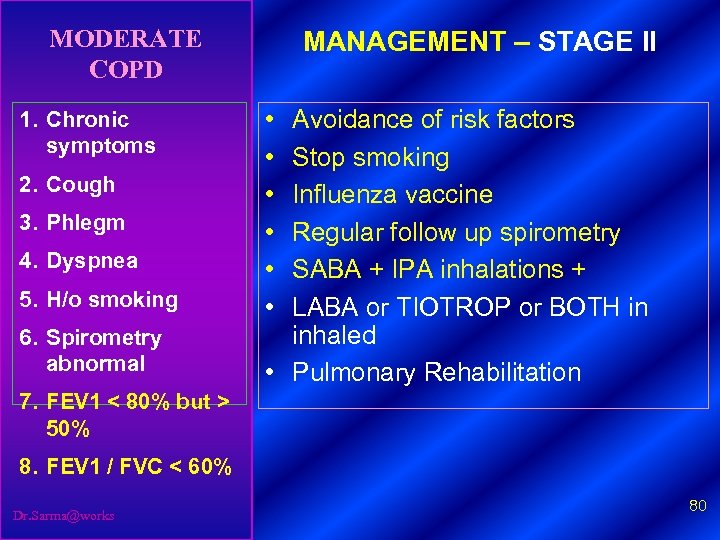
MODERATE COPD 1. Chronic symptoms 2. Cough 3. Phlegm 4. Dyspnea 5. H/o smoking 6. Spirometry abnormal MANAGEMENT – STAGE II • • • Avoidance of risk factors Stop smoking Influenza vaccine Regular follow up spirometry SABA + IPA inhalations + LABA or TIOTROP or BOTH in inhaled • Pulmonary Rehabilitation 7. FEV 1 < 80% but > 50% 8. FEV 1 / FVC < 60% Dr. Sarma@works 80
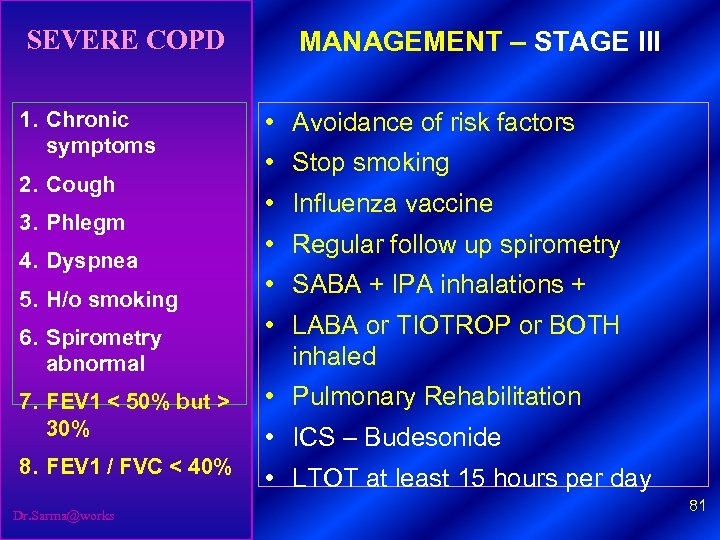
SEVERE COPD 1. Chronic symptoms 2. Cough 3. Phlegm 4. Dyspnea 5. H/o smoking 6. Spirometry abnormal MANAGEMENT – STAGE III • Avoidance of risk factors • Stop smoking • Influenza vaccine • Regular follow up spirometry • SABA + IPA inhalations + • LABA or TIOTROP or BOTH inhaled 7. FEV 1 < 50% but > 30% • Pulmonary Rehabilitation 8. FEV 1 / FVC < 40% • LTOT at least 15 hours per day Dr. Sarma@works • ICS – Budesonide 81
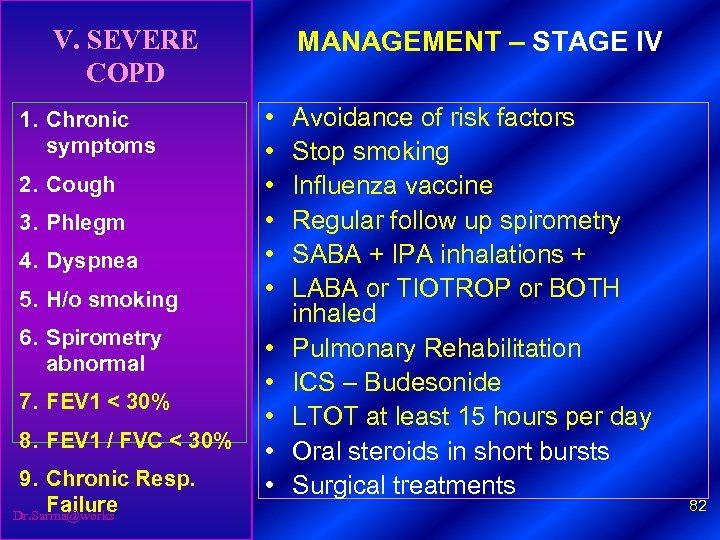
V. SEVERE COPD 1. Chronic symptoms 2. Cough 3. Phlegm 4. Dyspnea 5. H/o smoking 6. Spirometry abnormal 7. FEV 1 < 30% 8. FEV 1 / FVC < 30% 9. Chronic Resp. Failure Dr. Sarma@works MANAGEMENT – STAGE IV • • • Avoidance of risk factors Stop smoking Influenza vaccine Regular follow up spirometry SABA + IPA inhalations + LABA or TIOTROP or BOTH inhaled Pulmonary Rehabilitation ICS – Budesonide LTOT at least 15 hours per day Oral steroids in short bursts Surgical treatments 82

DRUG DELIVERY SYSTEMS - OPTIONS Dr. Sarma@works 83
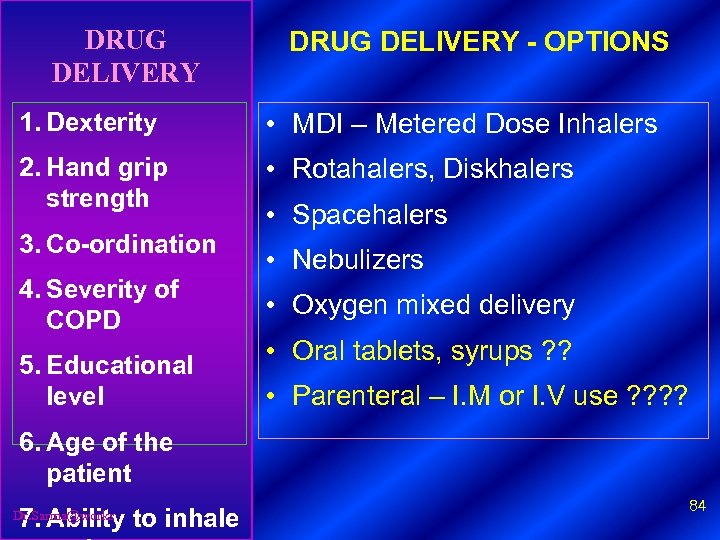
DRUG DELIVERY - OPTIONS 1. Dexterity • MDI – Metered Dose Inhalers 2. Hand grip strength • Rotahalers, Diskhalers 3. Co-ordination 4. Severity of COPD 5. Educational level • Spacehalers • Nebulizers • Oxygen mixed delivery • Oral tablets, syrups ? ? • Parenteral – I. M or I. V use ? ? 6. Age of the patient 7. Ability to inhale Dr. Sarma@works 84
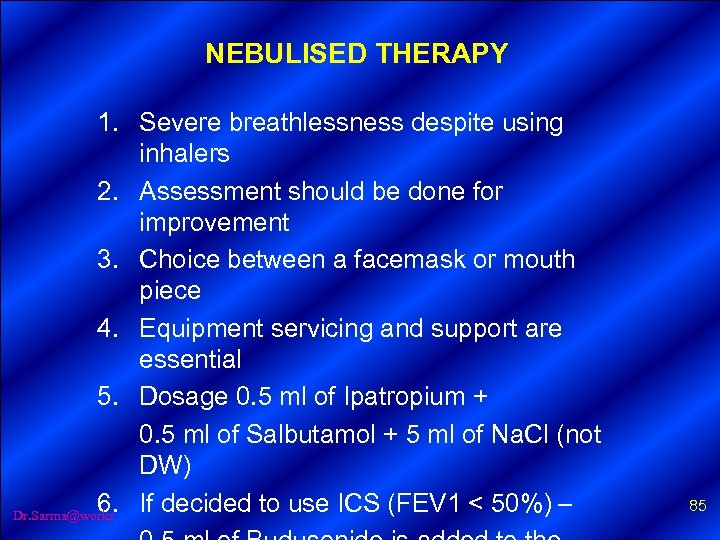
NEBULISED THERAPY 1. Severe breathlessness despite using inhalers 2. Assessment should be done for improvement 3. Choice between a facemask or mouth piece 4. Equipment servicing and support are essential 5. Dosage 0. 5 ml of Ipatropium + 0. 5 ml of Salbutamol + 5 ml of Na. Cl (not DW) 6. If decided to use ICS (FEV 1 < 50%) – Dr. Sarma@works 85
EDUCATION AND REHABILITATION Dr. Sarma@works 86
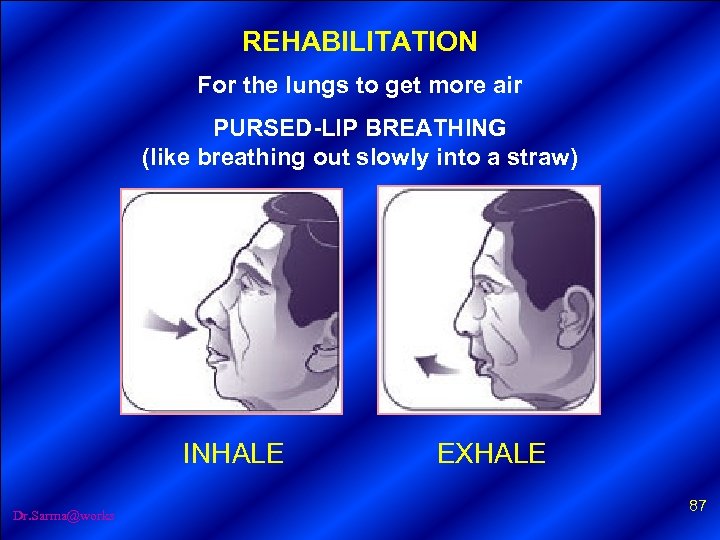
REHABILITATION For the lungs to get more air PURSED-LIP BREATHING (like breathing out slowly into a straw) INHALE Dr. Sarma@works EXHALE 87
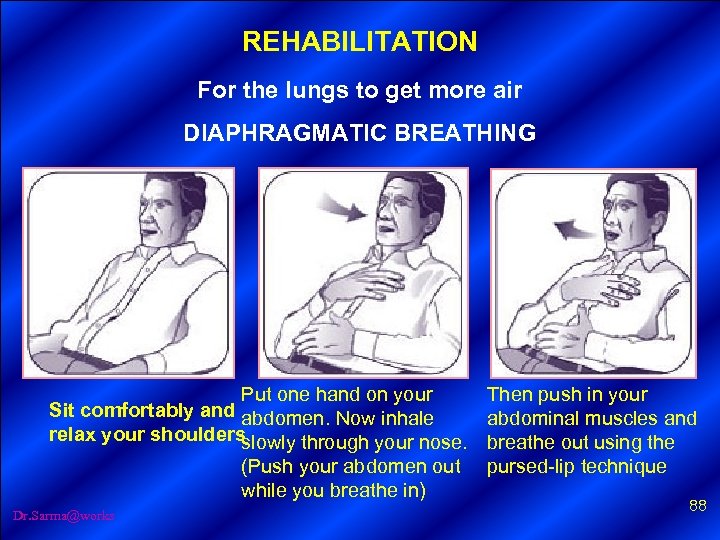
REHABILITATION For the lungs to get more air DIAPHRAGMATIC BREATHING 1. Sit comfortably and relax your shoulders. 2. Put one hand on your abdomen. Now inhale slowly through your nose. (Push your abdomen out while you breathe in) Put one hand on your 3. Then push in your abdominal muscles and breathe out using the pursed-lip technique. (You should feel your Then push in your abdomen go down) abdominal muscles and Sit comfortably and abdomen. Now inhale relax your shoulders Note: slowly through your nose. breathe out using the • Repeat the above maneuver three times and then take a little rest. (Push your abdomen out pursed-lip technique • This exercise can be done many times a day. while you breathe in) Dr. Sarma@works 88
HEALTH EDUCATION – TEAM WORK Dr. Sarma@works 89

EXACERBATIONS RESP. FAILURE Dr. Sarma@works 90
OXIGENERATO R MANAGEMENT – REFERRAL • Diagnosis uncertain • Disproportionate symptoms • Persistent symptoms • Development of lung cancer • Pulmonary rehabilitation • Nebulizer assessment • Oxygen assessment Dr. Sarma@works 91
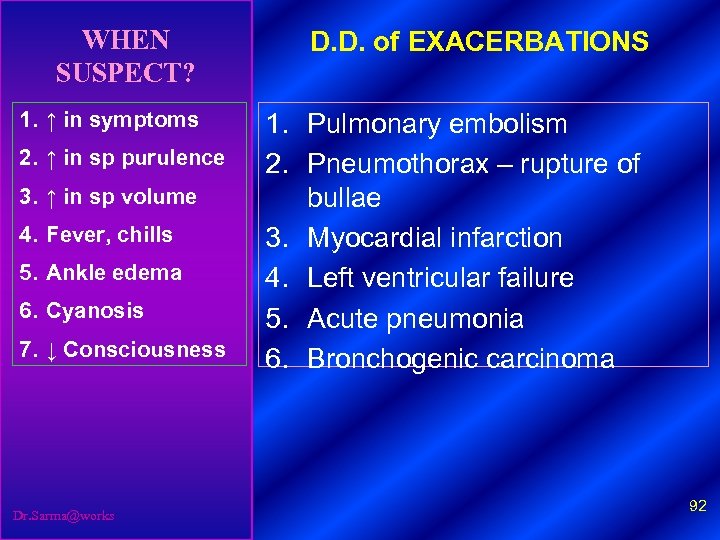
WHEN SUSPECT? D. D. of EXACERBATIONS 1. ↑ in symptoms 1. Pulmonary embolism 2. Pneumothorax – rupture of bullae 3. Myocardial infarction 4. Left ventricular failure 5. Acute pneumonia 6. Bronchogenic carcinoma 2. ↑ in sp purulence 3. ↑ in sp volume 4. Fever, chills 5. Ankle edema 6. Cyanosis 7. ↓ Consciousness Dr. Sarma@works 92
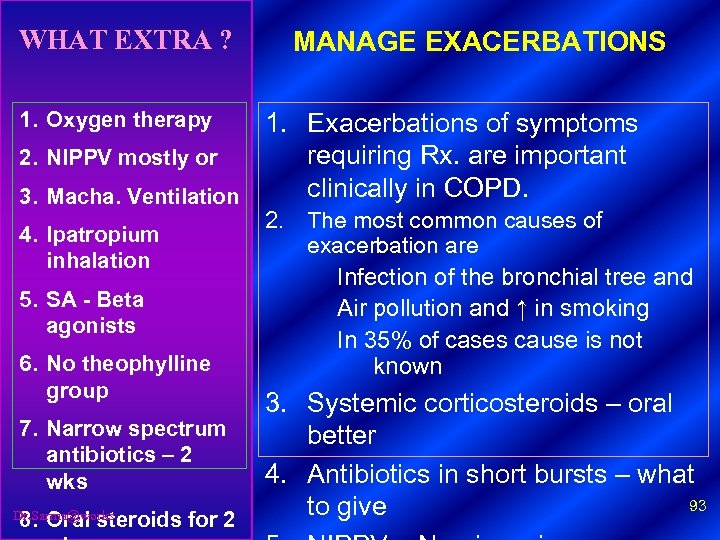
WHAT EXTRA ? 1. Oxygen therapy 2. NIPPV mostly or 3. Macha. Ventilation 4. Ipatropium inhalation 5. SA - Beta agonists 6. No theophylline group 7. Narrow spectrum antibiotics – 2 wks 8. Oral steroids for 2 Dr. Sarma@works MANAGE EXACERBATIONS 1. Exacerbations of symptoms requiring Rx. are important clinically in COPD. 2. The most common causes of exacerbation are Infection of the bronchial tree and Air pollution and ↑ in smoking In 35% of cases cause is not known 3. Systemic corticosteroids – oral better 4. Antibiotics in short bursts – what 93 to give
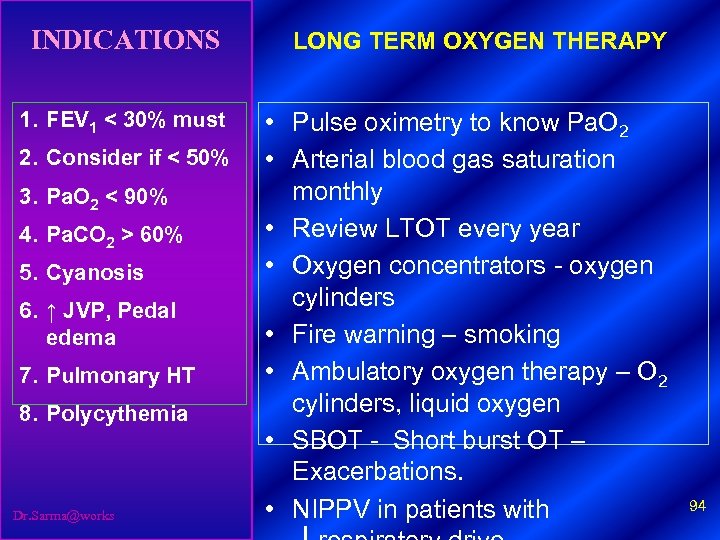
INDICATIONS LONG TERM OXYGEN THERAPY 1. FEV 1 < 30% must • Pulse oximetry to know Pa. O 2 • Arterial blood gas saturation monthly • Review LTOT every year • Oxygen concentrators - oxygen cylinders • Fire warning – smoking • Ambulatory oxygen therapy – O 2 cylinders, liquid oxygen • SBOT - Short burst OT – Exacerbations. • NIPPV in patients with 2. Consider if < 50% 3. Pa. O 2 < 90% 4. Pa. CO 2 > 60% 5. Cyanosis 6. ↑ JVP, Pedal edema 7. Pulmonary HT 8. Polycythemia Dr. Sarma@works 94
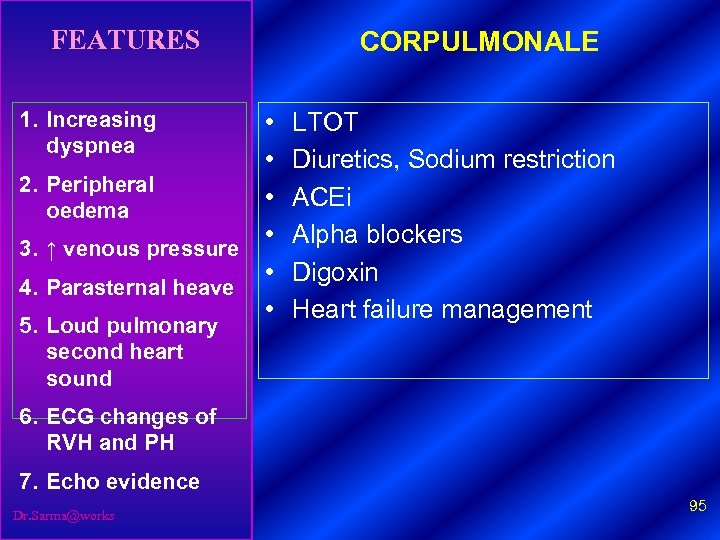
FEATURES 1. Increasing dyspnea • • 2. Peripheral • oedema • 3. ↑ venous pressure • 4. Parasternal heave • 5. Loud pulmonary second heart sound CORPULMONALE LTOT Diuretics, Sodium restriction ACEi Alpha blockers Digoxin Heart failure management 6. ECG changes of RVH and PH 7. Echo evidence Dr. Sarma@works 95
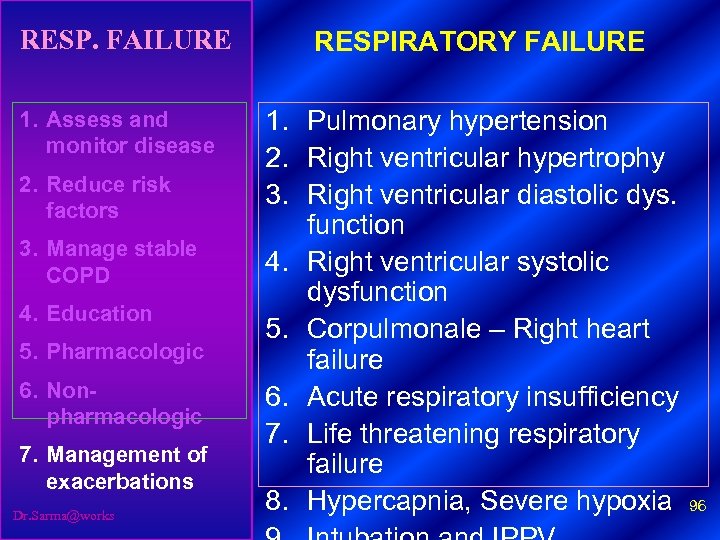
RESP. FAILURE RESPIRATORY FAILURE 1. Assess and monitor disease 1. Pulmonary hypertension 2. Right ventricular hypertrophy 3. Right ventricular diastolic dys. function 4. Right ventricular systolic dysfunction 5. Corpulmonale – Right heart failure 6. Acute respiratory insufficiency 7. Life threatening respiratory failure 8. Hypercapnia, Severe hypoxia 96 2. Reduce risk factors 3. Manage stable COPD 4. Education 5. Pharmacologic 6. Nonpharmacologic 7. Management of exacerbations Dr. Sarma@works
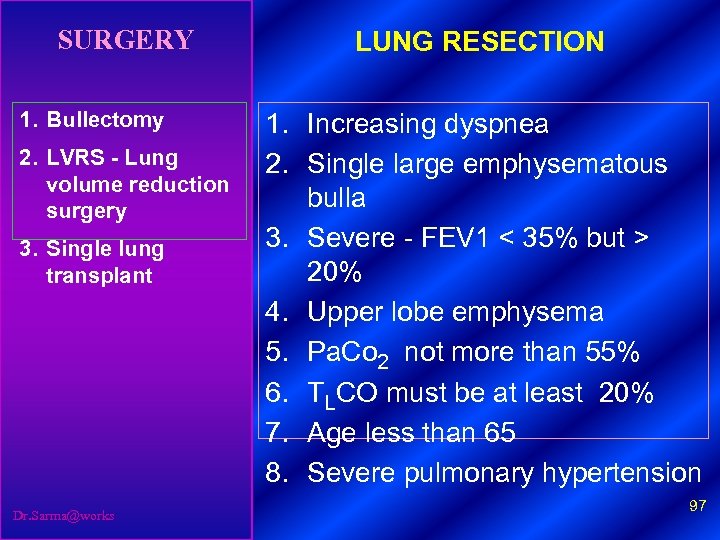
SURGERY 1. Bullectomy 2. LVRS - Lung volume reduction surgery 3. Single lung transplant Dr. Sarma@works LUNG RESECTION 1. Increasing dyspnea 2. Single large emphysematous bulla 3. Severe - FEV 1 < 35% but > 20% 4. Upper lobe emphysema 5. Pa. Co 2 not more than 55% 6. TLCO must be at least 20% 7. Age less than 65 8. Severe pulmonary hypertension 97
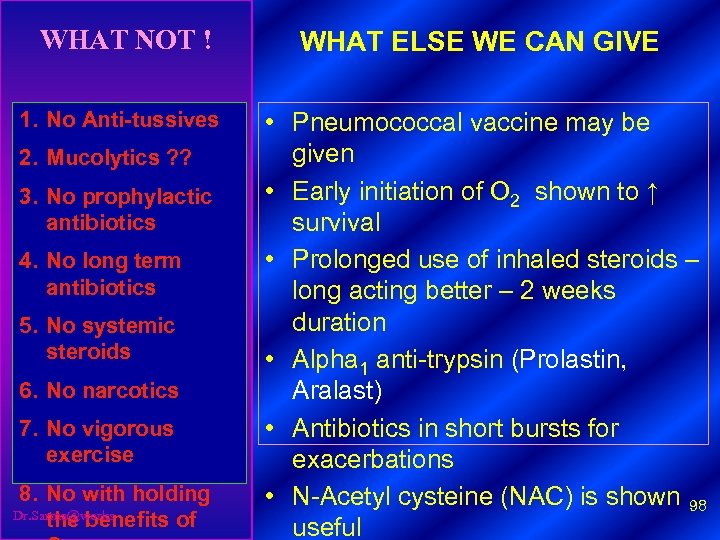
WHAT NOT ! 1. No Anti-tussives 2. Mucolytics ? ? 3. No prophylactic antibiotics 4. No long term antibiotics 5. No systemic steroids 6. No narcotics 7. No vigorous exercise 8. No with holding Dr. Sarma@works the benefits of WHAT ELSE WE CAN GIVE • Pneumococcal vaccine may be given • Early initiation of O 2 shown to ↑ survival • Prolonged use of inhaled steroids – long acting better – 2 weeks duration • Alpha 1 anti-trypsin (Prolastin, Aralast) • Antibiotics in short bursts for exacerbations • N-Acetyl cysteine (NAC) is shown 98 useful

COPD - FUTURE DEVELOPMENTS Dr. Sarma@works 99
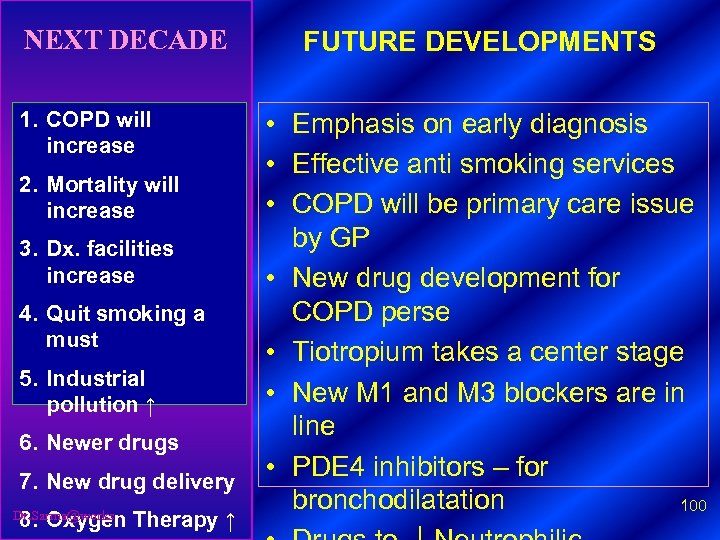
NEXT DECADE 1. COPD will increase 2. Mortality will increase 3. Dx. facilities increase 4. Quit smoking a must 5. Industrial pollution ↑ 6. Newer drugs 7. New drug delivery 8. Oxygen Therapy ↑ Dr. Sarma@works FUTURE DEVELOPMENTS • Emphasis on early diagnosis • Effective anti smoking services • COPD will be primary care issue by GP • New drug development for COPD perse • Tiotropium takes a center stage • New M 1 and M 3 blockers are in line • PDE 4 inhibitors – for bronchodilatation 100
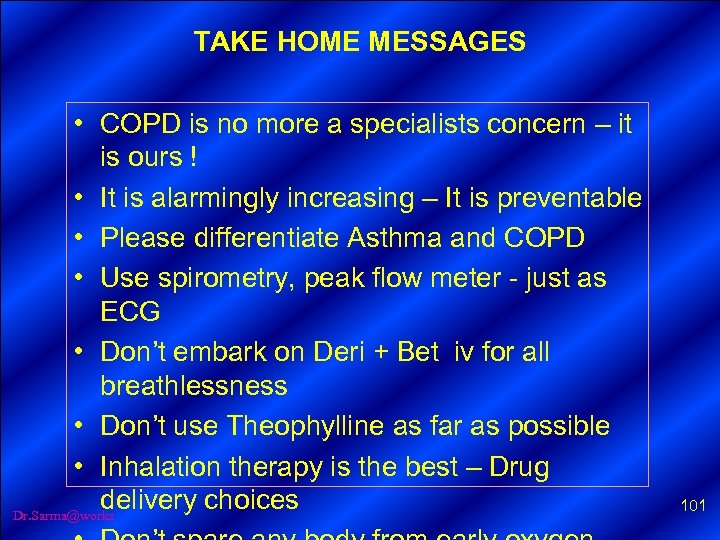
TAKE HOME MESSAGES • COPD is no more a specialists concern – it is ours ! • It is alarmingly increasing – It is preventable • Please differentiate Asthma and COPD • Use spirometry, peak flow meter - just as ECG • Don’t embark on Deri + Bet iv for all breathlessness • Don’t use Theophylline as far as possible • Inhalation therapy is the best – Drug delivery choices Dr. Sarma@works 101
SELF SCREENING Dr. Sarma@works 102
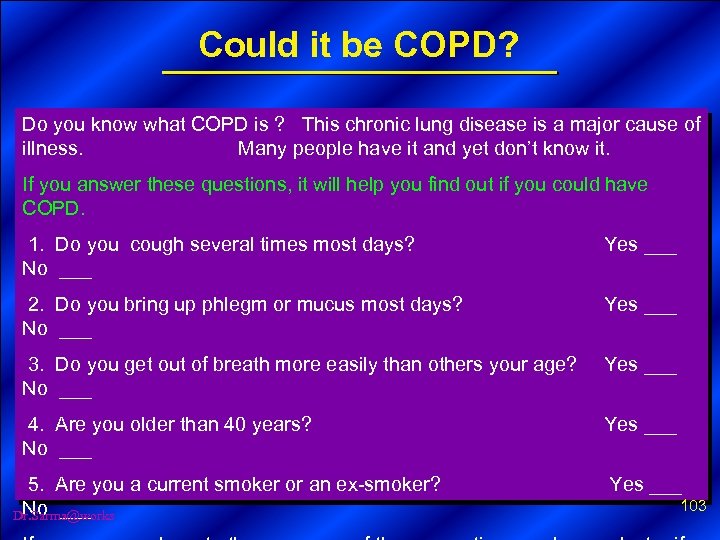
Could it be COPD? Do you know what COPD is ? This chronic lung disease is a major cause of illness. Many people have it and yet don’t know it. If you answer these questions, it will help you find out if you could have COPD. 1. Do you cough several times most days? No ___ Yes ___ 2. Do you bring up phlegm or mucus most days? No ___ Yes ___ 3. Do you get out of breath more easily than others your age? Yes ___ No ___ 4. Are you older than 40 years? No ___ Yes ___ 5. Are you a current smoker or an ex-smoker? Yes ___ 103 No ___ Dr. Sarma@works
ASTHMA V/s COPD Take HOME GUIDE Dr. Sarma@works 104
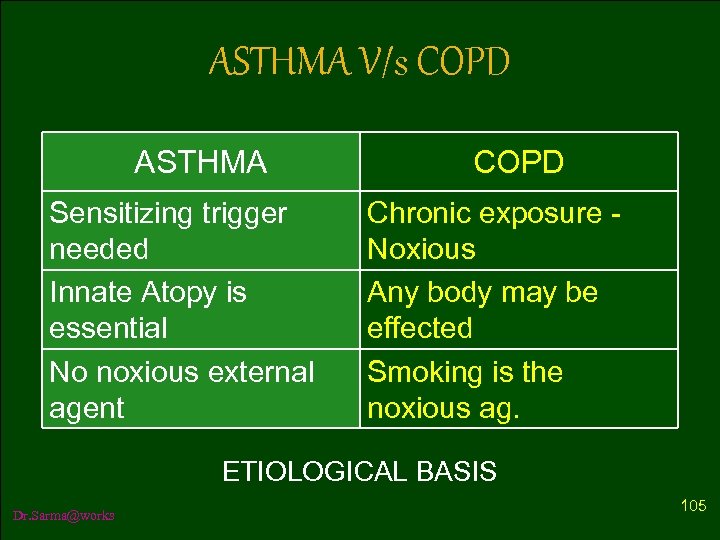
ASTHMA V/s COPD ASTHMA Sensitizing trigger needed Innate Atopy is essential No noxious external agent COPD Chronic exposure Noxious Any body may be effected Smoking is the noxious ag. ETIOLOGICAL BASIS Dr. Sarma@works 105
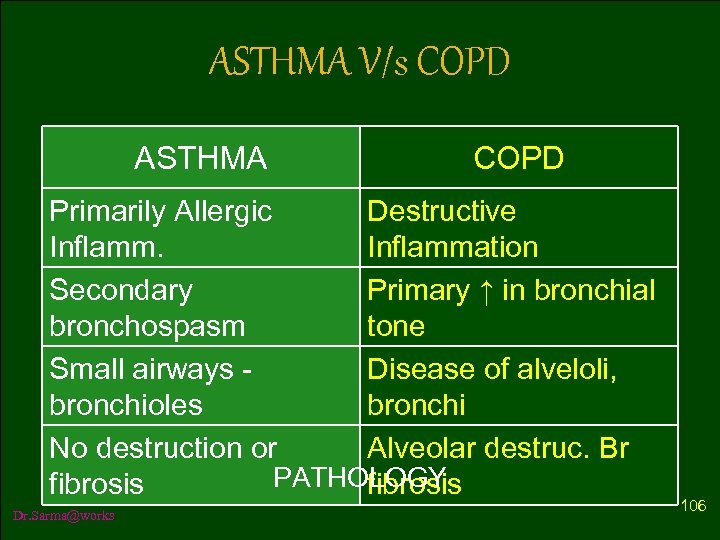
ASTHMA V/s COPD ASTHMA COPD Primarily Allergic Destructive Inflammation Secondary Primary ↑ in bronchial bronchospasm tone Small airways - Disease of alveloli, bronchioles bronchi No destruction or Alveolar destruc. Br PATHOLOGY fibrosis Dr. Sarma@works 106
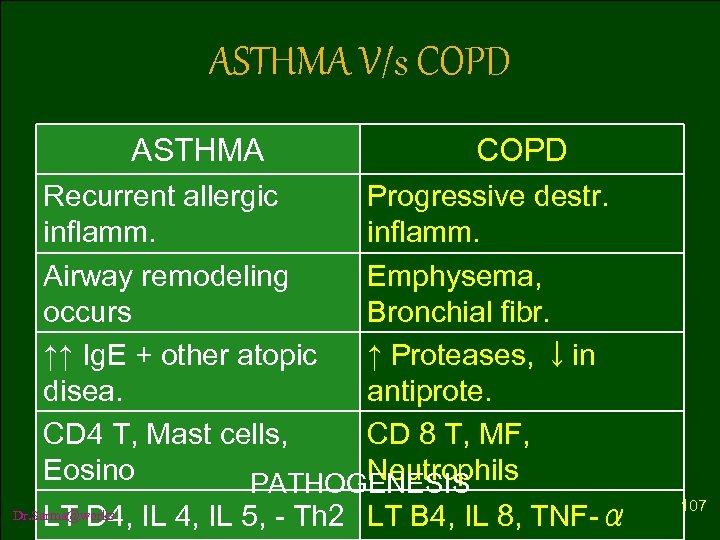
ASTHMA V/s COPD ASTHMA COPD Recurrent allergic Progressive destr. inflamm. Airway remodeling Emphysema, occurs Bronchial fibr. ↑↑ Ig. E + other atopic ↑ Proteases, ↓in disea. antiprote. CD 4 T, Mast cells, CD 8 T, MF, Eosino Neutrophils PATHOGENESIS LT D 4, IL 5, - Th 2 LT B 4, IL 8, TNF-α Dr. Sarma@works 107
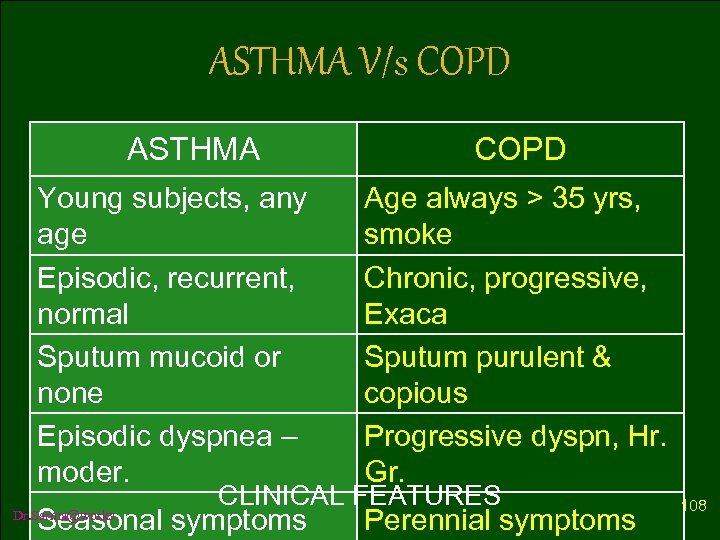
ASTHMA V/s COPD ASTHMA Young subjects, any age Episodic, recurrent, normal Sputum mucoid or none Episodic dyspnea – moder. Age always > 35 yrs, smoke Chronic, progressive, Exaca Sputum purulent & copious Progressive dyspn, Hr. Gr. CLINICAL FEATURES Seasonal symptoms Dr. Sarma@works COPD Perennial symptoms 108
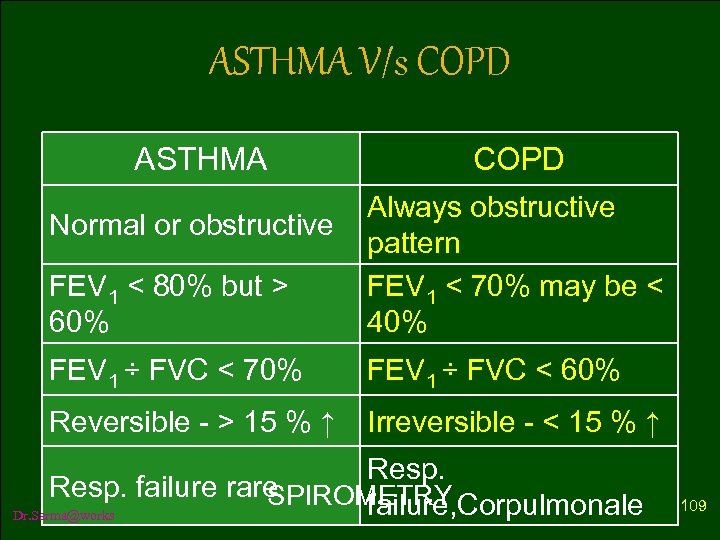
ASTHMA V/s COPD ASTHMA COPD FEV 1 < 80% but > 60% Always obstructive pattern FEV 1 < 70% may be < 40% FEV 1 ÷ FVC < 70% FEV 1 ÷ FVC < 60% Reversible - > 15 % ↑ Irreversible - < 15 % ↑ Normal or obstructive Resp. failure rare SPIROMETRY failure, Corpulmonale Dr. Sarma@works 109
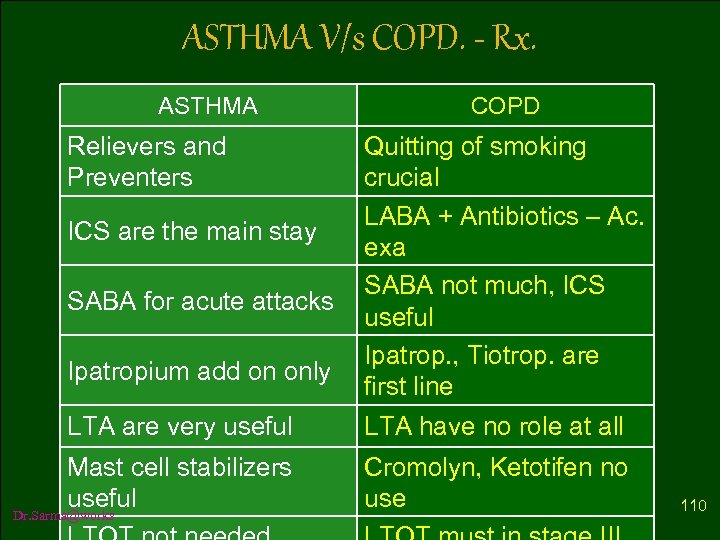
ASTHMA V/s COPD. - Rx. ASTHMA Relievers and Preventers ICS are the main stay SABA for acute attacks Ipatropium add on only LTA are very useful COPD Quitting of smoking crucial LABA + Antibiotics – Ac. exa SABA not much, ICS useful Ipatrop. , Tiotrop. are first line LTA have no role at all Mast cell stabilizers Cromolyn, Ketotifen no Treatment useful use Dr. Sarma@works 110
“The old order changeth yielding place to new; Lest, one good custom should corrupt the world. ” Tennyson Sir Lord, Alfred This is most pertinent today to Asthma and COPD Holm and Harris & NEJM Dr. Sarma@works 111
PREVENT COPD Dr. Sarma@works 112
THE DEADLIEST DEVIL Dr. Sarma@works 113

SURE TO GRAVE Dr. Sarma@works 114
AND FINALLY Tell me what harm smoking does not cause ? ? Dr. Sarma@works 115
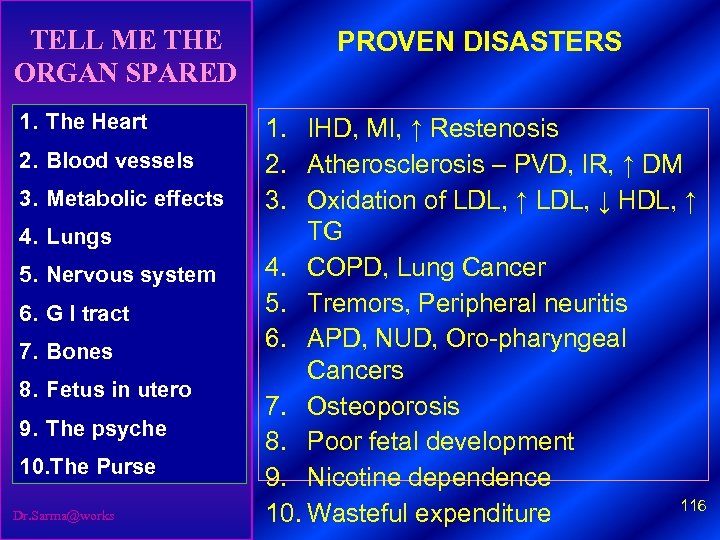
TELL ME THE ORGAN SPARED 1. The Heart 2. Blood vessels 3. Metabolic effects 4. Lungs 5. Nervous system 6. G I tract 7. Bones 8. Fetus in utero 9. The psyche 10. The Purse Dr. Sarma@works PROVEN DISASTERS 1. IHD, MI, ↑ Restenosis 2. Atherosclerosis – PVD, IR, ↑ DM 3. Oxidation of LDL, ↑ LDL, ↓ HDL, ↑ TG 4. COPD, Lung Cancer 5. Tremors, Peripheral neuritis 6. APD, NUD, Oro-pharyngeal Cancers 7. Osteoporosis 8. Poor fetal development 9. Nicotine dependence 116 10. Wasteful expenditure
The Onus here is on us Most of these effects have dose-response relationship. Most of them are reversible if smoking is stopped early. Reducing the # reduces the risk – inverse If we are a smoker, let us quit smoking – set response. an example. Let us motivate every month at least one person to quit. What right we have, to make others passive smokers? Dr. Sarma@works 117
Pledge to stop smoking Dr. Sarma@works 118
WHAT CAN WE DO ? ? Dr. Sarma@works 119
MY SINS IF CARE NOT TO DO THESE – THEN ALL If, in patients I treat, I have • Not controlled his DM • Not evaluated for IHD • Not kept BP to goal • Not controlled lipids • Not advised the obese • Not persuaded a smoker Dr. Sarma@works • Not prevented OS PUNY AS SIN S 120
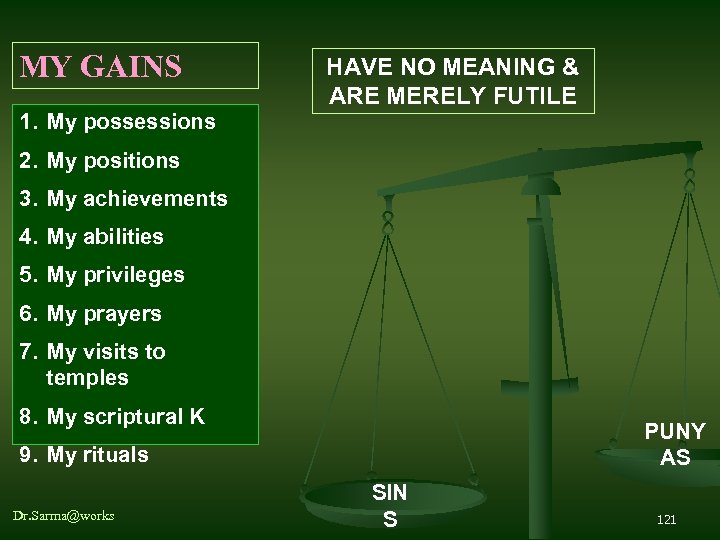
MY GAINS HAVE NO MEANING & ARE MERELY FUTILE 1. My possessions 2. My positions 3. My achievements 4. My abilities 5. My privileges 6. My prayers 7. My visits to temples 8. My scriptural K PUNY AS 9. My rituals Dr. Sarma@works SIN S 121
REMEMBER, WE ARE BLESSED WITH THE OPPORTUNITY Dr. Sarma@works 122
Om Asatho maa sad gamaya Om Tamaso maa jyothir gamaya Om Mrityor maa amritam gamaya Om Sarveshaam swasthir bhavathu Om Sarveshaam shaantir bhavathu Om Shaantihi || Dr. Sarma@works 123
Important Announcement A CD format of today’s presentation is ready 1. COPD, Asthma and basics of spirometry In addition it, also contains 2. ECG workshop presented earlier 3. Guidelines on Hypertension treatment Dr. Sarma@works 124
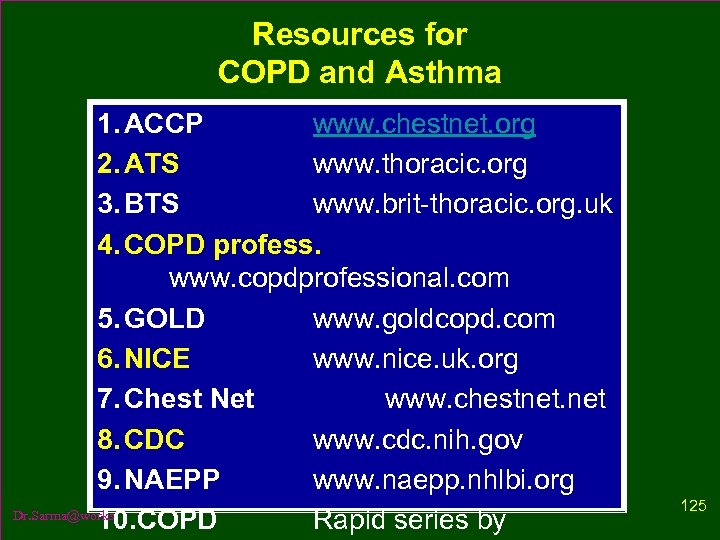
Resources for COPD and Asthma 1. ACCP www. chestnet. org 2. ATS www. thoracic. org 3. BTS www. brit-thoracic. org. uk 4. COPD profess. www. copdprofessional. com 5. GOLD www. goldcopd. com 6. NICE www. nice. uk. org 7. Chest Net www. chestnet. net 8. CDC www. cdc. nih. gov 9. NAEPP www. naepp. nhlbi. org Dr. Sarma@works 10. COPD Rapid series by 125

PLEASE CONTACT US Dr. Sarma RVSN, M. D. , M. Sc (Canada) JN Road, Jayanagar, Tiruvallur, TN +91 98940 60593, (4116) 260593 Dr. Kumaran. M, B. Sc. , M. B. B. S. , 10 North Raja St, Tiruvallur, TN +91 98941 10450, (4116) 260288 WE WILL MEET AGAIN SOON Dr. Sarma@works 126
NANRI, VANAKKAM Dr. Sarma@works 127
f1468ee4963f8053ec4b775d0b446545.ppt