 Chronic gastritis
Chronic gastritis
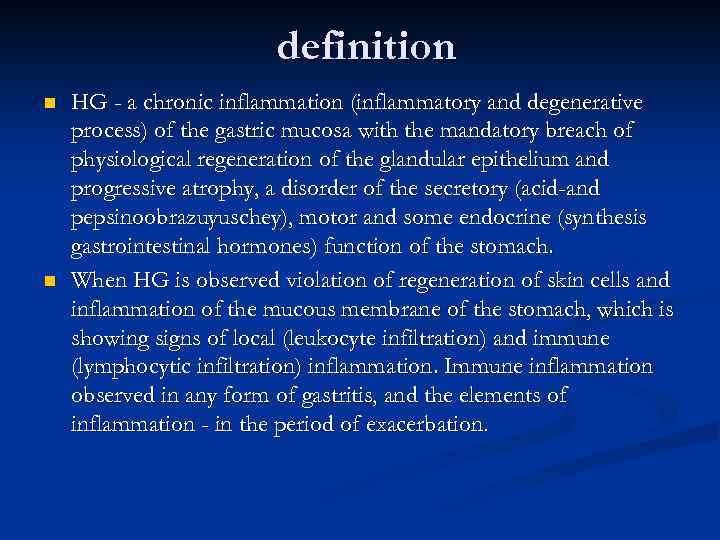 definition n n HG - a chronic inflammation (inflammatory and degenerative process) of the gastric mucosa with the mandatory breach of physiological regeneration of the glandular epithelium and progressive atrophy, a disorder of the secretory (acid-and pepsinoobrazuyuschey), motor and some endocrine (synthesis gastrointestinal hormones) function of the stomach. When HG is observed violation of regeneration of skin cells and inflammation of the mucous membrane of the stomach, which is showing signs of local (leukocyte infiltration) and immune (lymphocytic infiltration) inflammation. Immune inflammation observed in any form of gastritis, and the elements of inflammation - in the period of exacerbation.
definition n n HG - a chronic inflammation (inflammatory and degenerative process) of the gastric mucosa with the mandatory breach of physiological regeneration of the glandular epithelium and progressive atrophy, a disorder of the secretory (acid-and pepsinoobrazuyuschey), motor and some endocrine (synthesis gastrointestinal hormones) function of the stomach. When HG is observed violation of regeneration of skin cells and inflammation of the mucous membrane of the stomach, which is showing signs of local (leukocyte infiltration) and immune (lymphocytic infiltration) inflammation. Immune inflammation observed in any form of gastritis, and the elements of inflammation - in the period of exacerbation.
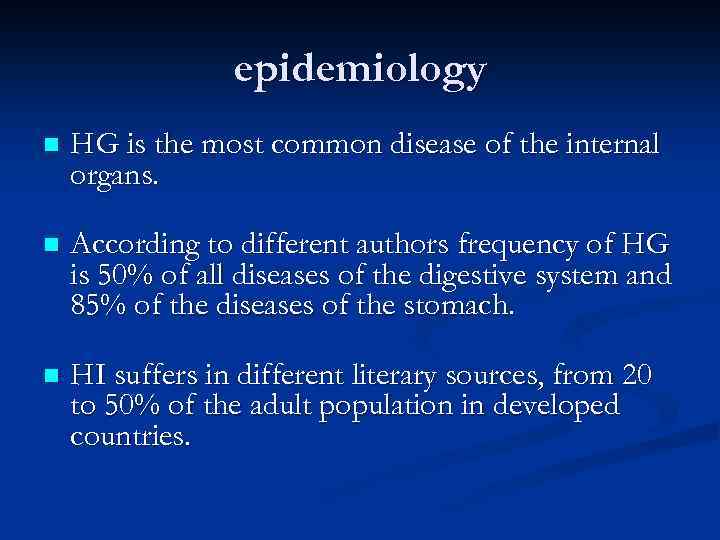 epidemiology n HG is the most common disease of the internal organs. n According to different authors frequency of HG is 50% of all diseases of the digestive system and 85% of the diseases of the stomach. n HI suffers in different literary sources, from 20 to 50% of the adult population in developed countries.
epidemiology n HG is the most common disease of the internal organs. n According to different authors frequency of HG is 50% of all diseases of the digestive system and 85% of the diseases of the stomach. n HI suffers in different literary sources, from 20 to 50% of the adult population in developed countries.
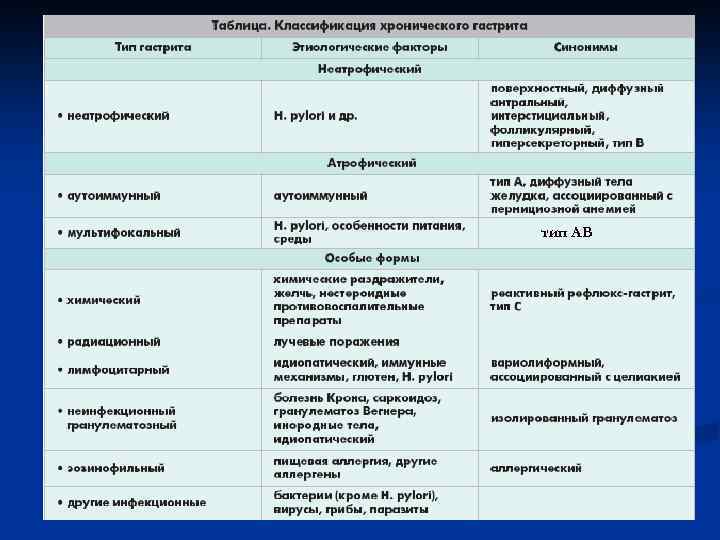 тип АВ
тип АВ
 Continued classification of HG It is also necessary to specify the state of gastric secretion: increased stored (normal) or secretory failure (moderate and severe, including achlorhydria). n HG Phase traditional flow reflects the reference to exacerbation or remission process. n
Continued classification of HG It is also necessary to specify the state of gastric secretion: increased stored (normal) or secretory failure (moderate and severe, including achlorhydria). n HG Phase traditional flow reflects the reference to exacerbation or remission process. n
 Examples of formulations diagnosis Chronic gastritis, gastric antrum (chronic antral gastritis) helicobacterial with increased secretion (or normal secretory function) in the acute phase (discontinuous exacerbation or remission). q Chronic gastritis, gastric body (chronic fundic gastritis) autoimmune with moderate (or severe) secretory failure in the acute phase (discontinuous exacerbation or remission). q Chronic helicobacterial mixed pangastritis normal secretory function (or moderate secretory deficiency) in the acute phase (discontinuous exacerbation or remission). q
Examples of formulations diagnosis Chronic gastritis, gastric antrum (chronic antral gastritis) helicobacterial with increased secretion (or normal secretory function) in the acute phase (discontinuous exacerbation or remission). q Chronic gastritis, gastric body (chronic fundic gastritis) autoimmune with moderate (or severe) secretory failure in the acute phase (discontinuous exacerbation or remission). q Chronic helicobacterial mixed pangastritis normal secretory function (or moderate secretory deficiency) in the acute phase (discontinuous exacerbation or remission). q
 The etiology of HG n Autoantibodies to parietal cells (fundic HG); n The infection of the gastric mucosa “Helicobacter pylori”; n The damaging effect of doudenalnogo contents (bile acids, lizolitsetina) on gastric mucosa at its reflux.
The etiology of HG n Autoantibodies to parietal cells (fundic HG); n The infection of the gastric mucosa “Helicobacter pylori”; n The damaging effect of doudenalnogo contents (bile acids, lizolitsetina) on gastric mucosa at its reflux.
 Exogenous risk factors for HG • nutritional - the food " in suhomyatku " abuse of spicy and fried foods , lack of protein and vitamins in the diet , the use of food additives, food jetlag , etc. • psycho-emotional factor - stress, depression • Environmental factors : the state of the atmosphere , the presence of nitrates in food, poor quality of drinking water ? • drugs - NSAIDs , corticosteroids , etc. • bad habits - smoking, alcohol • parasitic infections (especially giardiasis ) • food allergy? • the poor state of dentition • hormonal dysfunction
Exogenous risk factors for HG • nutritional - the food " in suhomyatku " abuse of spicy and fried foods , lack of protein and vitamins in the diet , the use of food additives, food jetlag , etc. • psycho-emotional factor - stress, depression • Environmental factors : the state of the atmosphere , the presence of nitrates in food, poor quality of drinking water ? • drugs - NSAIDs , corticosteroids , etc. • bad habits - smoking, alcohol • parasitic infections (especially giardiasis ) • food allergy? • the poor state of dentition • hormonal dysfunction
 The pathogenesis of autoimmune HG n In the pathogenesis of autoimmune HG occupy the central place of genetically determined autoimmune reaction in the formation of autoantibodies to the parietal cells and leading to severe atrophy of the glands of the mucosa of the gastric fundus. Since it is in the fundal the great bulk of the parietal ( parietal ) cells that produce hydrochloric acid and biermerin, HG of this type is characterized by early onset of acid deficiency until ahilii (in combination with a high level gastrinemii) and B 12 -deficiency anemia.
The pathogenesis of autoimmune HG n In the pathogenesis of autoimmune HG occupy the central place of genetically determined autoimmune reaction in the formation of autoantibodies to the parietal cells and leading to severe atrophy of the glands of the mucosa of the gastric fundus. Since it is in the fundal the great bulk of the parietal ( parietal ) cells that produce hydrochloric acid and biermerin, HG of this type is characterized by early onset of acid deficiency until ahilii (in combination with a high level gastrinemii) and B 12 -deficiency anemia.
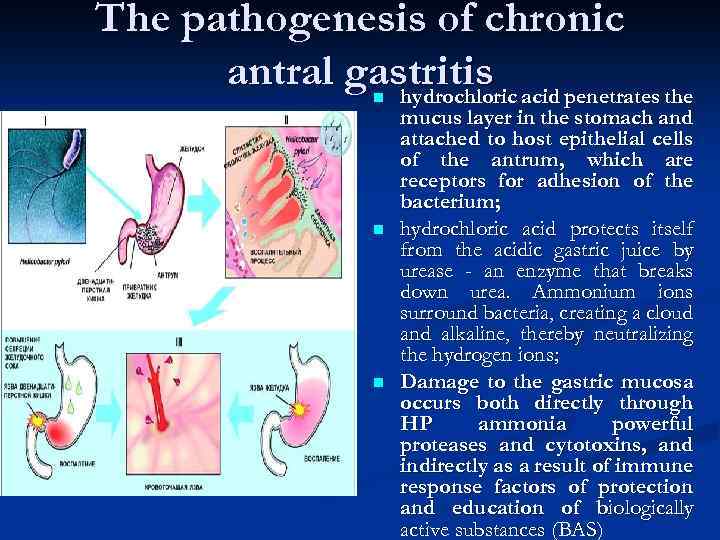 The pathogenesis of chronic antral gastritis acid penetrates the hydrochloric n n n mucus layer in the stomach and attached to host epithelial cells of the antrum, which are receptors for adhesion of the bacterium; hydrochloric acid protects itself from the acidic gastric juice by urease - an enzyme that breaks down urea. Ammonium ions surround bacteria, creating a cloud and alkaline, thereby neutralizing the hydrogen ions; Damage to the gastric mucosa occurs both directly through HP ammonia powerful proteases and cytotoxins, and indirectly as a result of immune response factors of protection and education of biologically active substances (BAS)
The pathogenesis of chronic antral gastritis acid penetrates the hydrochloric n n n mucus layer in the stomach and attached to host epithelial cells of the antrum, which are receptors for adhesion of the bacterium; hydrochloric acid protects itself from the acidic gastric juice by urease - an enzyme that breaks down urea. Ammonium ions surround bacteria, creating a cloud and alkaline, thereby neutralizing the hydrogen ions; Damage to the gastric mucosa occurs both directly through HP ammonia powerful proteases and cytotoxins, and indirectly as a result of immune response factors of protection and education of biologically active substances (BAS)
 continuation With this type of HG release two options: n n 1) involvement in the duodenum to the formation gastroduodenita. For this form of HG is characterized by a motley palette of secretory disorders (including increased secretory activity). This is due to different degrees and the depth of mucosal lesions in fundal and with dysregulation of gastric secretion by the death of cells that produce gastrin in antrum; 2) distribution of inflammatory changes in the proximal direction with a gradual transition to the so-called chronic mixed pangastritis, which is more common in older patients, many years of suffering from chronic antral gastritis. This form of HG occurs with gradually increasing atrophy of the glands and secretory failure.
continuation With this type of HG release two options: n n 1) involvement in the duodenum to the formation gastroduodenita. For this form of HG is characterized by a motley palette of secretory disorders (including increased secretory activity). This is due to different degrees and the depth of mucosal lesions in fundal and with dysregulation of gastric secretion by the death of cells that produce gastrin in antrum; 2) distribution of inflammatory changes in the proximal direction with a gradual transition to the so-called chronic mixed pangastritis, which is more common in older patients, many years of suffering from chronic antral gastritis. This form of HG occurs with gradually increasing atrophy of the glands and secretory failure.
 The pathogenesis of the chemical? (Chemical-induced) HG n It is divided into reflux gastritis and gastric medication form. n When duodenal reflux into the lumen of the stomach contents of the intestines are constantly thrown together with bile, which is rich in lysolecithin and bile acids have a toxic (membranoliticheskoe) effects on epithelial cells. n Medication form is associated with prolonged exposure to drugs or occupational exposures. With this type of HG is always amazed antrum, and then the proximal stomach.
The pathogenesis of the chemical? (Chemical-induced) HG n It is divided into reflux gastritis and gastric medication form. n When duodenal reflux into the lumen of the stomach contents of the intestines are constantly thrown together with bile, which is rich in lysolecithin and bile acids have a toxic (membranoliticheskoe) effects on epithelial cells. n Medication form is associated with prolonged exposure to drugs or occupational exposures. With this type of HG is always amazed antrum, and then the proximal stomach.
 The pathogenesis of specific forms of HG n Granulomatous gastritis characterized by small granules in the lamina propria of the gastric mucosa against the surface or atrophic gastritis. Most often it is about Crohn's disease, sarcoidosis, Wegener's disease gastric localization. A similar picture can give parasites or foreign bodies of the stomach. n Lymphocytic gastritis occurs against autoimmune chronic gastritis, gastric body (pangastrita chronic or mixed), and is characterized by numerous intraepithelial lymphocytes are found among epithelial cell surface (100 epithelial cells 30 and a fixed lymphocytes, normally they are not defined). The pathogenesis of this form of gastritis is not clear until the end. It is believed that this particular immune response to HP in which the gastric mucosa is not detected.
The pathogenesis of specific forms of HG n Granulomatous gastritis characterized by small granules in the lamina propria of the gastric mucosa against the surface or atrophic gastritis. Most often it is about Crohn's disease, sarcoidosis, Wegener's disease gastric localization. A similar picture can give parasites or foreign bodies of the stomach. n Lymphocytic gastritis occurs against autoimmune chronic gastritis, gastric body (pangastrita chronic or mixed), and is characterized by numerous intraepithelial lymphocytes are found among epithelial cell surface (100 epithelial cells 30 and a fixed lymphocytes, normally they are not defined). The pathogenesis of this form of gastritis is not clear until the end. It is believed that this particular immune response to HP in which the gastric mucosa is not detected.
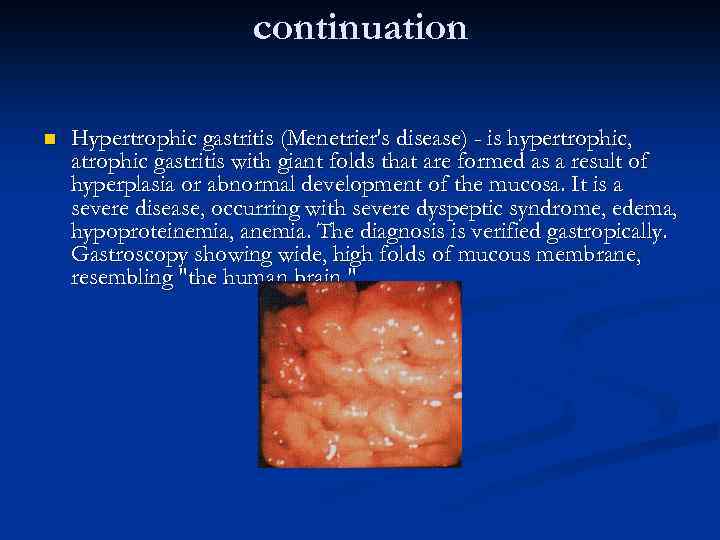 continuation n Hypertrophic gastritis (Menetrier's disease) - is hypertrophic, atrophic gastritis with giant folds that are formed as a result of hyperplasia or abnormal development of the mucosa. It is a severe disease, occurring with severe dyspeptic syndrome, edema, hypoproteinemia, anemia. The diagnosis is verified gastropically. Gastroscopy showing wide, high folds of mucous membrane, resembling "the human brain. "
continuation n Hypertrophic gastritis (Menetrier's disease) - is hypertrophic, atrophic gastritis with giant folds that are formed as a result of hyperplasia or abnormal development of the mucosa. It is a severe disease, occurring with severe dyspeptic syndrome, edema, hypoproteinemia, anemia. The diagnosis is verified gastropically. Gastroscopy showing wide, high folds of mucous membrane, resembling "the human brain. "
 continuation n Eosinophilic gastritis occurs against the surface, or atrophic gastritis, characterized by focal and / or accumulations of diffuse eosinophils in the lamina propria of the mucosa of the stomach. This gastritis is, as a rule, in allergic diseases and allergoses. Often, as a causal factor are the food allergens, or parasites. n Infectious gastritis characterized by focal and / or diffuse clusters of bacteria (gastrospirilly), viruses (cytomegalovirus), fungi (such as Candida) and monocyte reacting them in the lamina propria of the mucosa of the stomach.
continuation n Eosinophilic gastritis occurs against the surface, or atrophic gastritis, characterized by focal and / or accumulations of diffuse eosinophils in the lamina propria of the mucosa of the stomach. This gastritis is, as a rule, in allergic diseases and allergoses. Often, as a causal factor are the food allergens, or parasites. n Infectious gastritis characterized by focal and / or diffuse clusters of bacteria (gastrospirilly), viruses (cytomegalovirus), fungi (such as Candida) and monocyte reacting them in the lamina propria of the mucosa of the stomach.
 clinical manifestations n n Chronic autoimmune gastritis fundic Pain ( dull, aching pain and / or epigastric discomfort , worse or occur after eating small amounts of food especially an irritant effect on the mucous membrane of the stomach , accompanied by a sense of " saturation "); The syndrome of gastric dyspepsia ( severity, and epigastric discomfort after eating, feeling of fullness after taking a very limited amount of food , rotten belching , regurgitation , nausea, bad taste in the mouth in the morning) ; The syndrome of intestinal dyspepsia ( bloating , rumbling and discomfort in the abdomen, especially after taking milk or fatty foods , a tendency to diarrhea , weight loss. Hypochlorhydria In severe diarrhea is the leading complaint , until the development of " ahilicheskih ' diarrhea) ; Symptoms of B 12 deficiency anemia ; Asthenic- neurotic syndrome.
clinical manifestations n n Chronic autoimmune gastritis fundic Pain ( dull, aching pain and / or epigastric discomfort , worse or occur after eating small amounts of food especially an irritant effect on the mucous membrane of the stomach , accompanied by a sense of " saturation "); The syndrome of gastric dyspepsia ( severity, and epigastric discomfort after eating, feeling of fullness after taking a very limited amount of food , rotten belching , regurgitation , nausea, bad taste in the mouth in the morning) ; The syndrome of intestinal dyspepsia ( bloating , rumbling and discomfort in the abdomen, especially after taking milk or fatty foods , a tendency to diarrhea , weight loss. Hypochlorhydria In severe diarrhea is the leading complaint , until the development of " ahilicheskih ' diarrhea) ; Symptoms of B 12 deficiency anemia ; Asthenic- neurotic syndrome.
 clinical manifestations n n On examination revealed pallor of the skin and mucous membranes, dull, brittle hair and nails, bleeding gums, alopecia, weight loss, "varnished" (atrophy of papillae) language, the symptoms of funicular myelosis (sensitivity disorders: paresthesia in the limbs, unsteadiness of gait); n With palpation determined moderate diffuse epigastric tenderness (with associated dysbiosis - also along the large intestine). Chronic autoimmune gastritis fundic
clinical manifestations n n On examination revealed pallor of the skin and mucous membranes, dull, brittle hair and nails, bleeding gums, alopecia, weight loss, "varnished" (atrophy of papillae) language, the symptoms of funicular myelosis (sensitivity disorders: paresthesia in the limbs, unsteadiness of gait); n With palpation determined moderate diffuse epigastric tenderness (with associated dysbiosis - also along the large intestine). Chronic autoimmune gastritis fundic
 clinical manifestations n n Pain syndrome corresponds to the quality and supply , the pain occur on an empty stomach or immediately (15 minutes after the start of the meal ) after eating at stihanii exacerbations are associated with certain types of food ( tapas, smoked products , etc. ) , at the height can be triggered by any product. Irradiation is not typical , maximum palpation pain is in the epigastric region, " the stomach " , the intensity varies. At the young age of the pain can be " yazvennopodobnom " paroxysmal , but the most typical of the average intensity of pain ; n For a typical syndrome of gastric dyspepsia ( occasionally ) heartburn, acid regurgitation , there is a tendency to constipation. Characteristic of bad breath (especially in the morning) ; n There is a tendency Asthenic- neurotic syndrome. Chronic helicobacterial antral gastritis to constipation ;
clinical manifestations n n Pain syndrome corresponds to the quality and supply , the pain occur on an empty stomach or immediately (15 minutes after the start of the meal ) after eating at stihanii exacerbations are associated with certain types of food ( tapas, smoked products , etc. ) , at the height can be triggered by any product. Irradiation is not typical , maximum palpation pain is in the epigastric region, " the stomach " , the intensity varies. At the young age of the pain can be " yazvennopodobnom " paroxysmal , but the most typical of the average intensity of pain ; n For a typical syndrome of gastric dyspepsia ( occasionally ) heartburn, acid regurgitation , there is a tendency to constipation. Characteristic of bad breath (especially in the morning) ; n There is a tendency Asthenic- neurotic syndrome. Chronic helicobacterial antral gastritis to constipation ;
 clinical manifestations n n Pressing nature of pain in the epigastric region; n The main clinical manifestations of the syndrome of gastric dyspepsia are nausea, belching bitter, unpleasant taste in the mouth. Chemical chronic gastritis
clinical manifestations n n Pressing nature of pain in the epigastric region; n The main clinical manifestations of the syndrome of gastric dyspepsia are nausea, belching bitter, unpleasant taste in the mouth. Chemical chronic gastritis
 Diagnosis of chronic gastritis include: Laboratory methods: n Complete blood; n Radioimmunoassay method defined in blood gastrin (norm to 100 ng / l) and pepsinogen 1 (normal 40 -130 mg / l); n Determining the level of uropepsina in urine (normal 38 -96 mg / day); n Immunological method using immunosorbents: AT to parietal cells, antibodies to the enzyme K / Na-ATPase activity in parietal cells, AT to intrinsic factor Castle, AT to HP.
Diagnosis of chronic gastritis include: Laboratory methods: n Complete blood; n Radioimmunoassay method defined in blood gastrin (norm to 100 ng / l) and pepsinogen 1 (normal 40 -130 mg / l); n Determining the level of uropepsina in urine (normal 38 -96 mg / day); n Immunological method using immunosorbents: AT to parietal cells, antibodies to the enzyme K / Na-ATPase activity in parietal cells, AT to intrinsic factor Castle, AT to HP.
 Diagnosis of chronic gastritis include: Instrumental methods: n The endoscopic method (gastroduodenoscopy) with taking diagnostic biopsies; n Morphological study gastrobioptatov; n Determination of acid production: fractional gastric intubation, the types of p. H meters.
Diagnosis of chronic gastritis include: Instrumental methods: n The endoscopic method (gastroduodenoscopy) with taking diagnostic biopsies; n Morphological study gastrobioptatov; n Determination of acid production: fractional gastric intubation, the types of p. H meters.
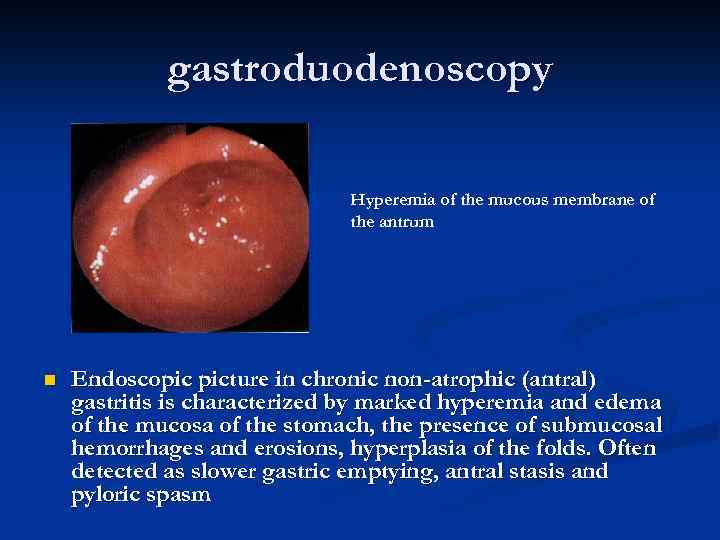 gastroduodenoscopy Hyperemia of the mucous membrane of the antrum n Endoscopic picture in chronic non-atrophic (antral) gastritis is characterized by marked hyperemia and edema of the mucosa of the stomach, the presence of submucosal hemorrhages and erosions, hyperplasia of the folds. Often detected as slower gastric emptying, antral stasis and pyloric spasm
gastroduodenoscopy Hyperemia of the mucous membrane of the antrum n Endoscopic picture in chronic non-atrophic (antral) gastritis is characterized by marked hyperemia and edema of the mucosa of the stomach, the presence of submucosal hemorrhages and erosions, hyperplasia of the folds. Often detected as slower gastric emptying, antral stasis and pyloric spasm
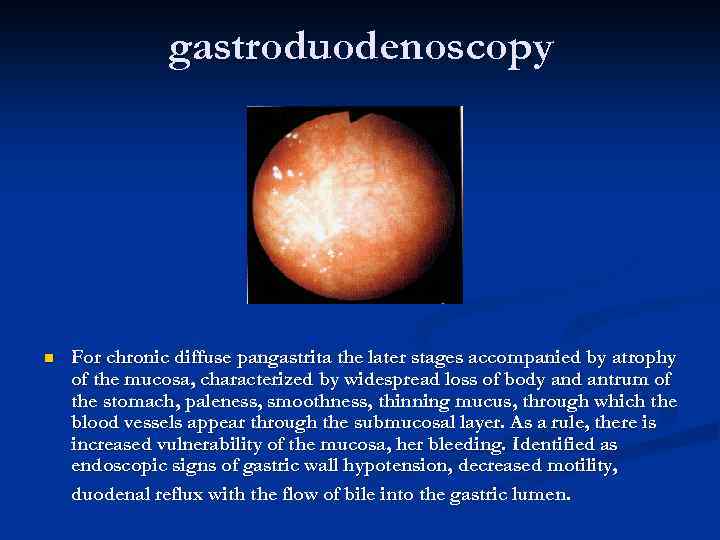 gastroduodenoscopy n For chronic diffuse pangastrita the later stages accompanied by atrophy of the mucosa, characterized by widespread loss of body and antrum of the stomach, paleness, smoothness, thinning mucus, through which the blood vessels appear through the submucosal layer. As a rule, there is increased vulnerability of the mucosa, her bleeding. Identified as endoscopic signs of gastric wall hypotension, decreased motility, duodenal reflux with the flow of bile into the gastric lumen.
gastroduodenoscopy n For chronic diffuse pangastrita the later stages accompanied by atrophy of the mucosa, characterized by widespread loss of body and antrum of the stomach, paleness, smoothness, thinning mucus, through which the blood vessels appear through the submucosal layer. As a rule, there is increased vulnerability of the mucosa, her bleeding. Identified as endoscopic signs of gastric wall hypotension, decreased motility, duodenal reflux with the flow of bile into the gastric lumen.
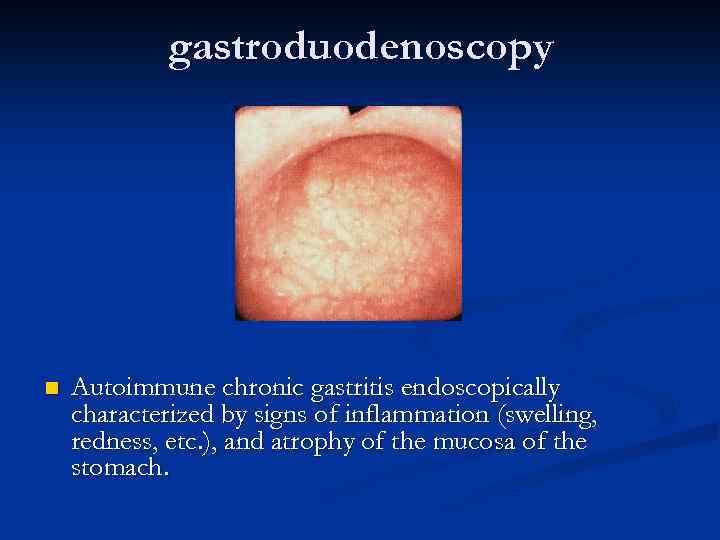 gastroduodenoscopy n Autoimmune chronic gastritis endoscopically characterized by signs of inflammation (swelling, redness, etc. ), and atrophy of the mucosa of the stomach.
gastroduodenoscopy n Autoimmune chronic gastritis endoscopically characterized by signs of inflammation (swelling, redness, etc. ), and atrophy of the mucosa of the stomach.
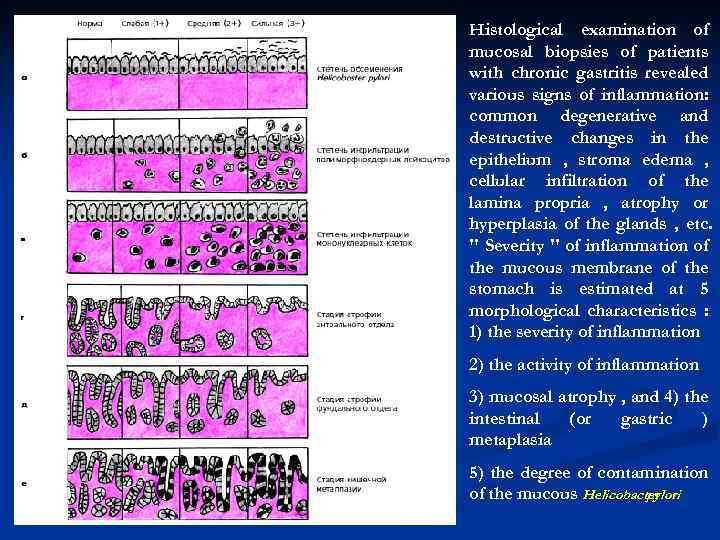 Histological examination of mucosal biopsies of patients with chronic gastritis revealed various signs of inflammation: common degenerative and destructive changes in the epithelium , stroma edema , cellular infiltration of the lamina propria , atrophy or hyperplasia of the glands , etc. " Severity " of inflammation of the mucous membrane of the stomach is estimated at 5 morphological characteristics : 1) the severity of inflammation 2) the activity of inflammation 3) mucosal atrophy , and 4) the intestinal (or gastric ) metaplasia 5) the degree of contamination of the mucous Helicobacter pylori
Histological examination of mucosal biopsies of patients with chronic gastritis revealed various signs of inflammation: common degenerative and destructive changes in the epithelium , stroma edema , cellular infiltration of the lamina propria , atrophy or hyperplasia of the glands , etc. " Severity " of inflammation of the mucous membrane of the stomach is estimated at 5 morphological characteristics : 1) the severity of inflammation 2) the activity of inflammation 3) mucosal atrophy , and 4) the intestinal (or gastric ) metaplasia 5) the degree of contamination of the mucous Helicobacter pylori
 Methods for detection of Helicobacter pylori (HP) infection Cytological research method n Material for cytological smears are the biopsies obtained during endoscopy of the sections of the antral mucosa of the stomach or duodenum with the most severe morphological changes ( redness , swelling , etc. ). Smears were dried and stained with Romanovsky Giemsa , or by Papengeymu metanolazureozinovoy mixture. n Microscopy of stained smears can detect the presence of HP and roughly estimate the number of microorganisms. There are three degrees of contamination of the mucous membranes : n 1. weak ( + ) - up to 20 microbial cells in the field of view ; 2. moderate ( + + ) - from 20 to 40 microbial cells in the field of view ; 3. high ( + + + ) - more than 40 microbes in sight. n n
Methods for detection of Helicobacter pylori (HP) infection Cytological research method n Material for cytological smears are the biopsies obtained during endoscopy of the sections of the antral mucosa of the stomach or duodenum with the most severe morphological changes ( redness , swelling , etc. ). Smears were dried and stained with Romanovsky Giemsa , or by Papengeymu metanolazureozinovoy mixture. n Microscopy of stained smears can detect the presence of HP and roughly estimate the number of microorganisms. There are three degrees of contamination of the mucous membranes : n 1. weak ( + ) - up to 20 microbial cells in the field of view ; 2. moderate ( + + ) - from 20 to 40 microbial cells in the field of view ; 3. high ( + + + ) - more than 40 microbes in sight. n n
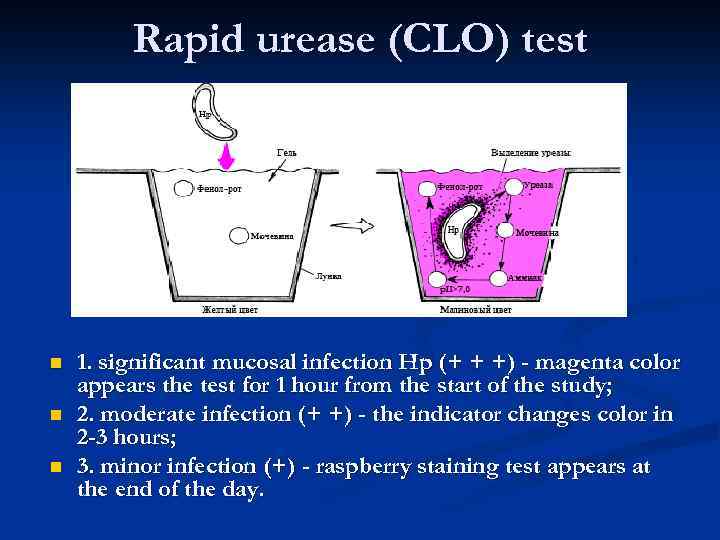 Rapid urease (CLO) test n n n 1. significant mucosal infection Hp (+ + +) - magenta color appears the test for 1 hour from the start of the study; 2. moderate infection (+ +) - the indicator changes color in 2 -3 hours; 3. minor infection (+) - raspberry staining test appears at the end of the day.
Rapid urease (CLO) test n n n 1. significant mucosal infection Hp (+ + +) - magenta color appears the test for 1 hour from the start of the study; 2. moderate infection (+ +) - the indicator changes color in 2 -3 hours; 3. minor infection (+) - raspberry staining test appears at the end of the day.
 microbiological method n The most specific method is cultivating bacteria H. pylori in microaerophilic conditions for special environments with the definition of urease, catalase and oxidase activity of the colonies. Because of the high cost and complexity of bacteriological method is rarely used mainly for evaluation of drug sensitivity of H. pylori resistance of standard treatment.
microbiological method n The most specific method is cultivating bacteria H. pylori in microaerophilic conditions for special environments with the definition of urease, catalase and oxidase activity of the colonies. Because of the high cost and complexity of bacteriological method is rarely used mainly for evaluation of drug sensitivity of H. pylori resistance of standard treatment.
 antibody method n Based on the identification of patients infected with HP -specific antibodies which can be detected in serum after 3 -4 weeks after infection. Sufficiently high antibody titer is maintained even in the period of clinical remission of the disease. A negative test is after successful antibiotic treatment , allowing you to use the method to monitor the effectiveness of this therapy. n For the detection of specific antibodies using various techniques , in particular, an enzyme immunoassay method (ELISA) with determination of antibody Ig. G and Ig. A classes in serum.
antibody method n Based on the identification of patients infected with HP -specific antibodies which can be detected in serum after 3 -4 weeks after infection. Sufficiently high antibody titer is maintained even in the period of clinical remission of the disease. A negative test is after successful antibiotic treatment , allowing you to use the method to monitor the effectiveness of this therapy. n For the detection of specific antibodies using various techniques , in particular, an enzyme immunoassay method (ELISA) with determination of antibody Ig. G and Ig. A classes in serum.
 Non-invasive urea breath test A solution of urea labeled with 14 C (a radioactive isotope - the source of the radioactive load) or 13 C in orange juice is taken by mouth. Cleavage urea influenced H. pylori urease evaluated after 30 minutes by the presence of a labeled carbon dioxide exhaled gas. n It has close to 100% specificity and sensitivity. n
Non-invasive urea breath test A solution of urea labeled with 14 C (a radioactive isotope - the source of the radioactive load) or 13 C in orange juice is taken by mouth. Cleavage urea influenced H. pylori urease evaluated after 30 minutes by the presence of a labeled carbon dioxide exhaled gas. n It has close to 100% specificity and sensitivity. n
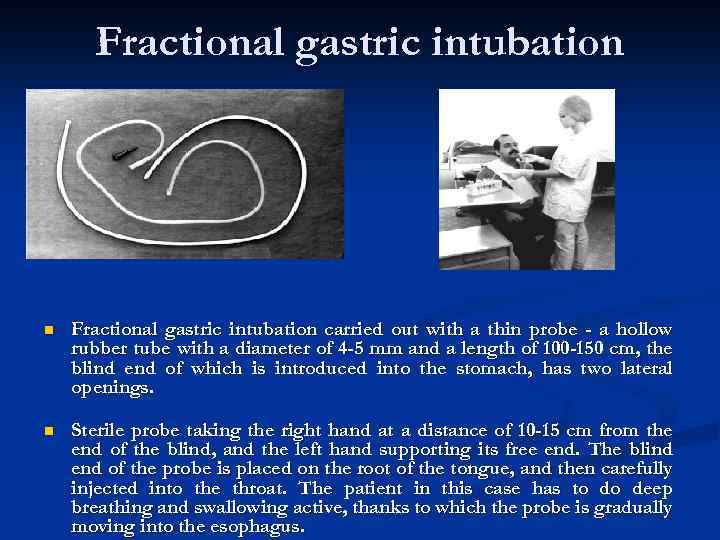 Fractional gastric intubation n Fractional gastric intubation carried out with a thin probe - a hollow rubber tube with a diameter of 4 -5 mm and a length of 100 -150 cm, the blind end of which is introduced into the stomach, has two lateral openings. n Sterile probe taking the right hand at a distance of 10 -15 cm from the end of the blind, and the left hand supporting its free end. The blind end of the probe is placed on the root of the tongue, and then carefully injected into the throat. The patient in this case has to do deep breathing and swallowing active, thanks to which the probe is gradually moving into the esophagus.
Fractional gastric intubation n Fractional gastric intubation carried out with a thin probe - a hollow rubber tube with a diameter of 4 -5 mm and a length of 100 -150 cm, the blind end of which is introduced into the stomach, has two lateral openings. n Sterile probe taking the right hand at a distance of 10 -15 cm from the end of the blind, and the left hand supporting its free end. The blind end of the probe is placed on the root of the tongue, and then carefully injected into the throat. The patient in this case has to do deep breathing and swallowing active, thanks to which the probe is gradually moving into the esophagus.
 continuation We study the amount of gastric juice; n The color and odor of the gastric juice; n Impurities; n Determine the acidity of gastric juice. allocate: 1. normoatsidnoe state (normoaciditas); 2. giperatsidnom state (hyperaciditas); 3. hypoacid state (hypoaciditas); 4. anatsidny state (anaciditas). n
continuation We study the amount of gastric juice; n The color and odor of the gastric juice; n Impurities; n Determine the acidity of gastric juice. allocate: 1. normoatsidnoe state (normoaciditas); 2. giperatsidnom state (hyperaciditas); 3. hypoacid state (hypoaciditas); 4. anatsidny state (anaciditas). n
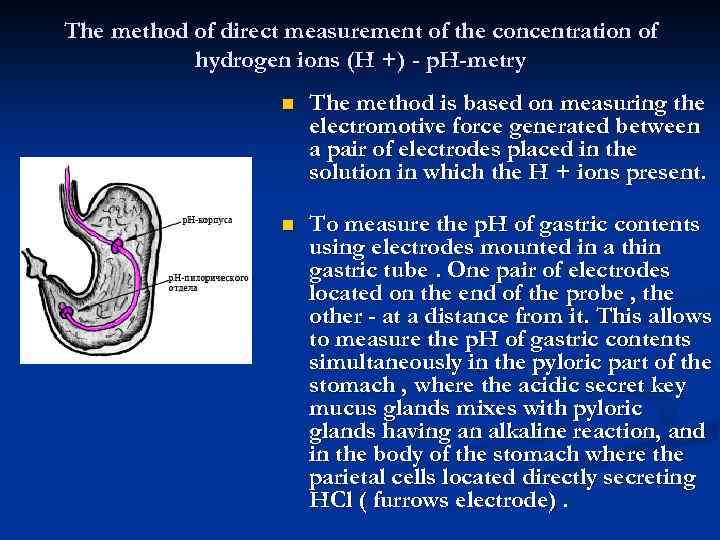 The method of direct measurement of the concentration of hydrogen ions (H +) - p. H-metry n The method is based on measuring the electromotive force generated between a pair of electrodes placed in the solution in which the H + ions present. n To measure the p. H of gastric contents using electrodes mounted in a thin gastric tube. One pair of electrodes located on the end of the probe , the other - at a distance from it. This allows to measure the p. H of gastric contents simultaneously in the pyloric part of the stomach , where the acidic secret key mucus glands mixes with pyloric glands having an alkaline reaction, and in the body of the stomach where the parietal cells located directly secreting HCl ( furrows electrode).
The method of direct measurement of the concentration of hydrogen ions (H +) - p. H-metry n The method is based on measuring the electromotive force generated between a pair of electrodes placed in the solution in which the H + ions present. n To measure the p. H of gastric contents using electrodes mounted in a thin gastric tube. One pair of electrodes located on the end of the probe , the other - at a distance from it. This allows to measure the p. H of gastric contents simultaneously in the pyloric part of the stomach , where the acidic secret key mucus glands mixes with pyloric glands having an alkaline reaction, and in the body of the stomach where the parietal cells located directly secreting HCl ( furrows electrode).
 continuation n To evaluate gastric acid-function often uses three p. H measured hull electrode disposed in the stomach: n 1. p. H-body on an empty stomach; n 2. p. H in the body basal secretory phase; n 3. p. H-body during the phase-stimulated gastric secretion. n As stimulants used secretion stimuli act directly on the receptors of the stomach (pentagastrin, histamine), and / or preferably on the centers of the vagus nerve (insulin).
continuation n To evaluate gastric acid-function often uses three p. H measured hull electrode disposed in the stomach: n 1. p. H-body on an empty stomach; n 2. p. H in the body basal secretory phase; n 3. p. H-body during the phase-stimulated gastric secretion. n As stimulants used secretion stimuli act directly on the receptors of the stomach (pentagastrin, histamine), and / or preferably on the centers of the vagus nerve (insulin).
 differential Diagnosis n Scope of differential diagnostic search when symptoms of gastritis covers gastric cancer, polyps , ulcers. The problem of differences in these diseases are usually there to perform a benchmarking study fibrogastrocopy with biopsy , and in cases of suspected endophytic tumor growth - X-ray with contrast barium sulfate. The distinction between chronic gastritis and pathology of the hepatobiliary system and the pancreas is performed using ultrasound of the abdomen. It must be remembered that the presence of h. CG does not exclude the existence of other problems at the level of the digestive system that requires clarification of cause- effect relationships and the corresponding adjustment of therapy.
differential Diagnosis n Scope of differential diagnostic search when symptoms of gastritis covers gastric cancer, polyps , ulcers. The problem of differences in these diseases are usually there to perform a benchmarking study fibrogastrocopy with biopsy , and in cases of suspected endophytic tumor growth - X-ray with contrast barium sulfate. The distinction between chronic gastritis and pathology of the hepatobiliary system and the pancreas is performed using ultrasound of the abdomen. It must be remembered that the presence of h. CG does not exclude the existence of other problems at the level of the digestive system that requires clarification of cause- effect relationships and the corresponding adjustment of therapy.
 treatment 1. diet: fraction (5 - 6 times a day) diet ; 2. absolutely contraindicated in chocolate, coffee , carbonated drinks, alcohol ; 3. excludes canned food, concentrates (including a series of " just add water " ) and surrogates of any products , spices, herbs , and products "Fast food", food , provoking unrest (milk , sour cream , grape , black bread and etc. ) , smoked , fatty and fried foods , pastry products ; 4. the cardinal rule : "Do not eat something from which hurts " - that is, exception idiosyncrasy of the product. Fractional , 5 -6 -single meal you can use it " antacid " effect ; to the exclusion of smoking, which disrupts the blood supply of the stomach ( in the first place , the lesser curvature ). 5.
treatment 1. diet: fraction (5 - 6 times a day) diet ; 2. absolutely contraindicated in chocolate, coffee , carbonated drinks, alcohol ; 3. excludes canned food, concentrates (including a series of " just add water " ) and surrogates of any products , spices, herbs , and products "Fast food", food , provoking unrest (milk , sour cream , grape , black bread and etc. ) , smoked , fatty and fried foods , pastry products ; 4. the cardinal rule : "Do not eat something from which hurts " - that is, exception idiosyncrasy of the product. Fractional , 5 -6 -single meal you can use it " antacid " effect ; to the exclusion of smoking, which disrupts the blood supply of the stomach ( in the first place , the lesser curvature ). 5.
 The principles of treatment of autoimmune HG I. Replacement therapy to compensate for digestion (and B 12 deficiency) against atrophy comprising: 1. Appointment of dilute hydrochloric acid / 20 -40 drops to a glass of water through a straw while eating / oral agents and / atsidin pepsin, Pepcid /. 2. Purpose of enzyme preparations ( Creon , pantsitrat ). 3. Assigning resources that enhance microcirculation and protein synthesis and repair processes : preparations of nicotinic acid / nicotinamide, nikoshpan , komplamin , Teonikol 1 table. X 3 times a day / metiluratsil / 0. 5 x 3 times a day / solkoseril / 2 ml 1 -2 times a day / m /. 4. Appointment of vitamins B and C inside and injections and B 12 injections.
The principles of treatment of autoimmune HG I. Replacement therapy to compensate for digestion (and B 12 deficiency) against atrophy comprising: 1. Appointment of dilute hydrochloric acid / 20 -40 drops to a glass of water through a straw while eating / oral agents and / atsidin pepsin, Pepcid /. 2. Purpose of enzyme preparations ( Creon , pantsitrat ). 3. Assigning resources that enhance microcirculation and protein synthesis and repair processes : preparations of nicotinic acid / nicotinamide, nikoshpan , komplamin , Teonikol 1 table. X 3 times a day / metiluratsil / 0. 5 x 3 times a day / solkoseril / 2 ml 1 -2 times a day / m /. 4. Appointment of vitamins B and C inside and injections and B 12 injections.
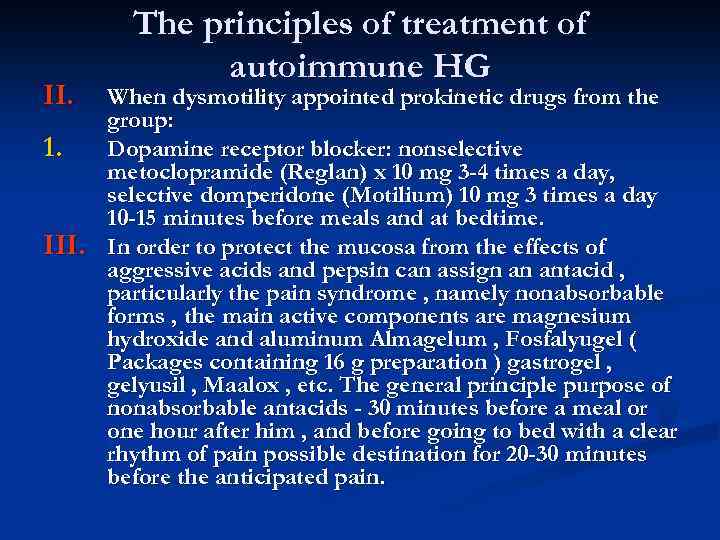 II. 1. III. The principles of treatment of autoimmune HG When dysmotility appointed prokinetic drugs from the group: Dopamine receptor blocker: nonselective metoclopramide (Reglan) x 10 mg 3 -4 times a day, selective domperidone (Motilium) 10 mg 3 times a day 10 -15 minutes before meals and at bedtime. In order to protect the mucosa from the effects of aggressive acids and pepsin can assign an antacid , particularly the pain syndrome , namely nonabsorbable forms , the main active components are magnesium hydroxide and aluminum Almagelum , Fosfalyugel ( Packages containing 16 g preparation ) gastrogel , gelyusil , Maalox , etc. The general principle purpose of nonabsorbable antacids - 30 minutes before a meal or one hour after him , and before going to bed with a clear rhythm of pain possible destination for 20 -30 minutes before the anticipated pain.
II. 1. III. The principles of treatment of autoimmune HG When dysmotility appointed prokinetic drugs from the group: Dopamine receptor blocker: nonselective metoclopramide (Reglan) x 10 mg 3 -4 times a day, selective domperidone (Motilium) 10 mg 3 times a day 10 -15 minutes before meals and at bedtime. In order to protect the mucosa from the effects of aggressive acids and pepsin can assign an antacid , particularly the pain syndrome , namely nonabsorbable forms , the main active components are magnesium hydroxide and aluminum Almagelum , Fosfalyugel ( Packages containing 16 g preparation ) gastrogel , gelyusil , Maalox , etc. The general principle purpose of nonabsorbable antacids - 30 minutes before a meal or one hour after him , and before going to bed with a clear rhythm of pain possible destination for 20 -30 minutes before the anticipated pain.
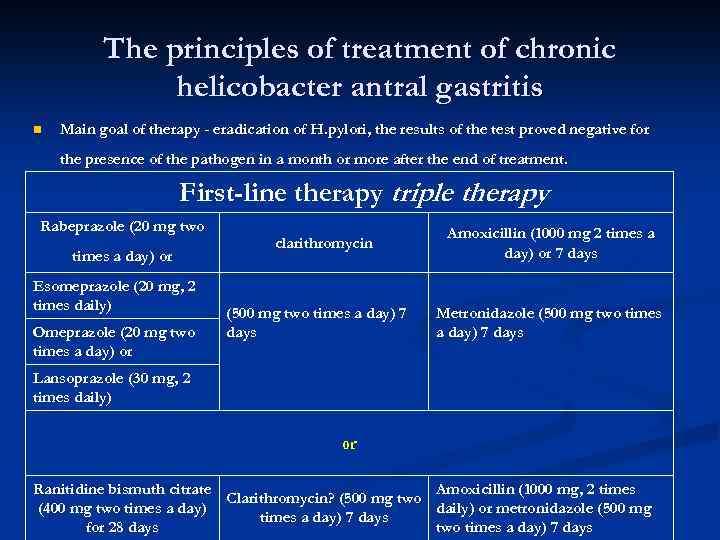 The principles of treatment of chronic helicobacter antral gastritis n Main goal of therapy - eradication of H. pylori, the results of the test proved negative for the presence of the pathogen in a month or more after the end of treatment. First-line therapy triple therapy Rabeprazole (20 mg two times a day) or Esomeprazole (20 mg, 2 times daily) Omeprazole (20 mg two times a day) or Lansoprazole (30 mg, 2 times daily) clarithromycin (500 mg two times a day) 7 days Amoxicillin (1000 mg 2 times a day) or 7 days Metronidazole (500 mg two times a day) 7 days or Ranitidine bismuth citrate Amoxicillin (1000 mg, 2 times Clarithromycin? (500 mg two (400 mg two times a day) daily) or metronidazole (500 mg times a day) 7 days for 28 days two times a day) 7 days
The principles of treatment of chronic helicobacter antral gastritis n Main goal of therapy - eradication of H. pylori, the results of the test proved negative for the presence of the pathogen in a month or more after the end of treatment. First-line therapy triple therapy Rabeprazole (20 mg two times a day) or Esomeprazole (20 mg, 2 times daily) Omeprazole (20 mg two times a day) or Lansoprazole (30 mg, 2 times daily) clarithromycin (500 mg two times a day) 7 days Amoxicillin (1000 mg 2 times a day) or 7 days Metronidazole (500 mg two times a day) 7 days or Ranitidine bismuth citrate Amoxicillin (1000 mg, 2 times Clarithromycin? (500 mg two (400 mg two times a day) daily) or metronidazole (500 mg times a day) 7 days for 28 days two times a day) 7 days
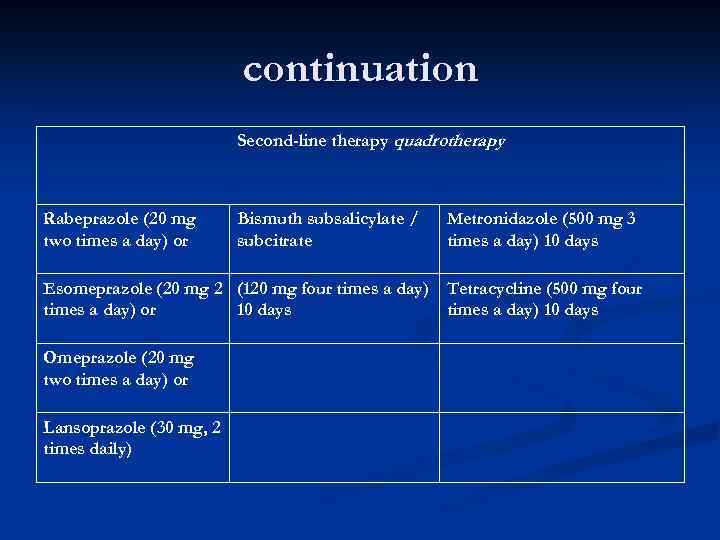 continuation Second-line therapy quadrotherapy Rabeprazole (20 mg two times a day) or Bismuth subsalicylate / subcitrate Metronidazole (500 mg 3 times a day) 10 days Esomeprazole (20 mg 2 (120 mg four times a day) Tetracycline (500 mg four times a day) or 10 days times a day) 10 days Lansoprazole (30 mg, 2 times daily) Omeprazole (20 mg two times a day) or
continuation Second-line therapy quadrotherapy Rabeprazole (20 mg two times a day) or Bismuth subsalicylate / subcitrate Metronidazole (500 mg 3 times a day) 10 days Esomeprazole (20 mg 2 (120 mg four times a day) Tetracycline (500 mg four times a day) or 10 days times a day) 10 days Lansoprazole (30 mg, 2 times daily) Omeprazole (20 mg two times a day) or
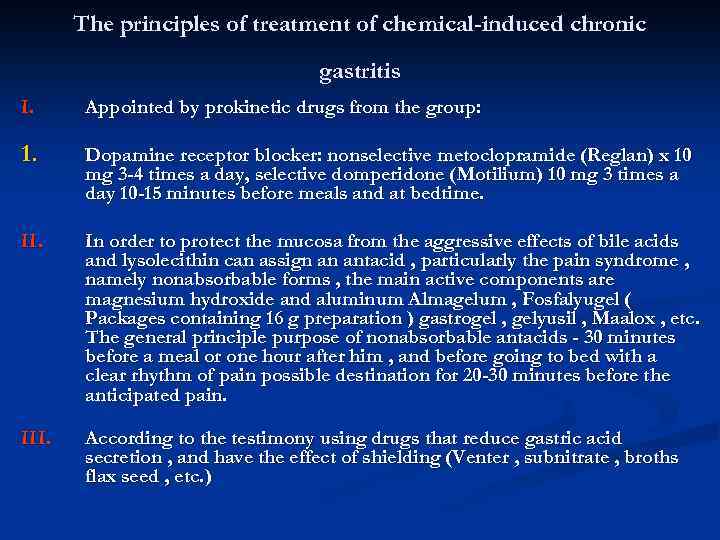 The principles of treatment of chemical-induced chronic gastritis I. Appointed by prokinetic drugs from the group: 1. Dopamine receptor blocker: nonselective metoclopramide (Reglan) x 10 mg 3 -4 times a day, selective domperidone (Motilium) 10 mg 3 times a day 10 -15 minutes before meals and at bedtime. II. In order to protect the mucosa from the aggressive effects of bile acids and lysolecithin can assign an antacid , particularly the pain syndrome , namely nonabsorbable forms , the main active components are magnesium hydroxide and aluminum Almagelum , Fosfalyugel ( Packages containing 16 g preparation ) gastrogel , gelyusil , Maalox , etc. The general principle purpose of nonabsorbable antacids - 30 minutes before a meal or one hour after him , and before going to bed with a clear rhythm of pain possible destination for 20 -30 minutes before the anticipated pain. III. According to the testimony using drugs that reduce gastric acid secretion , and have the effect of shielding (Venter , subnitrate , broths flax seed , etc. )
The principles of treatment of chemical-induced chronic gastritis I. Appointed by prokinetic drugs from the group: 1. Dopamine receptor blocker: nonselective metoclopramide (Reglan) x 10 mg 3 -4 times a day, selective domperidone (Motilium) 10 mg 3 times a day 10 -15 minutes before meals and at bedtime. II. In order to protect the mucosa from the aggressive effects of bile acids and lysolecithin can assign an antacid , particularly the pain syndrome , namely nonabsorbable forms , the main active components are magnesium hydroxide and aluminum Almagelum , Fosfalyugel ( Packages containing 16 g preparation ) gastrogel , gelyusil , Maalox , etc. The general principle purpose of nonabsorbable antacids - 30 minutes before a meal or one hour after him , and before going to bed with a clear rhythm of pain possible destination for 20 -30 minutes before the anticipated pain. III. According to the testimony using drugs that reduce gastric acid secretion , and have the effect of shielding (Venter , subnitrate , broths flax seed , etc. )
 clinical examination Examinations of patients are held 1 -2 times a year and, if necessary supplemented by gastroscopy and biopsy
clinical examination Examinations of patients are held 1 -2 times a year and, if necessary supplemented by gastroscopy and biopsy
 forecast HG did not significantly affect the length and quality of life of patients. There might be a spontaneous remission of the disease. The prognosis worsens with hypertrophic gastritis in patients with autoimmune HG and mixed helicobacter pangastritom because of the increased risk in these cases of gastric cancer.
forecast HG did not significantly affect the length and quality of life of patients. There might be a spontaneous remission of the disease. The prognosis worsens with hypertrophic gastritis in patients with autoimmune HG and mixed helicobacter pangastritom because of the increased risk in these cases of gastric cancer.
 Thank you for Attention!
Thank you for Attention!


