2ffb73bdedaa10788f8ddb27e4357eb2.ppt
- Количество слайдов: 51
 Chronic disease self-management education programs Where should Victoria go? Joanne Jordan BA, BSc, MPH Research Fellow AFV Centre for Rheumatic Diseases The University of Melbourne jjordan@unimelb. edu. au
Chronic disease self-management education programs Where should Victoria go? Joanne Jordan BA, BSc, MPH Research Fellow AFV Centre for Rheumatic Diseases The University of Melbourne jjordan@unimelb. edu. au
 Focus • To determine the value of and potential for the integration of chronic disease selfmanagement education programs into the care continuum • International policy review • Local (Australian centric) policy review • Interviews with key stakeholders, GPs and consumers
Focus • To determine the value of and potential for the integration of chronic disease selfmanagement education programs into the care continuum • International policy review • Local (Australian centric) policy review • Interviews with key stakeholders, GPs and consumers
 Background • Impact of chronic disease in Australia: - >70% of disease burden • Health system geared to acute conditions • Deficiencies in patient care - Lack of education & support for selfmanagement - Lack of ongoing and proactive care
Background • Impact of chronic disease in Australia: - >70% of disease burden • Health system geared to acute conditions • Deficiencies in patient care - Lack of education & support for selfmanagement - Lack of ongoing and proactive care
 Background • Seeking alternative ways to improve treatment quality and patient satisfaction • Policy shift: Medical didactic model Patient centred care Chronic disease self-management has emerged as an important component within the patient centred care approach
Background • Seeking alternative ways to improve treatment quality and patient satisfaction • Policy shift: Medical didactic model Patient centred care Chronic disease self-management has emerged as an important component within the patient centred care approach
 What is self-management? • Consideration of: - the individual with the chronic condition - their family and carers - health professionals - Involves a holistic approach and acknowledging - medical - psycho-social - cultural aspects - Aims to empower individuals
What is self-management? • Consideration of: - the individual with the chronic condition - their family and carers - health professionals - Involves a holistic approach and acknowledging - medical - psycho-social - cultural aspects - Aims to empower individuals
 Putting self-management into context • Self-management is 1 component within chronic disease management • Focus on formal self-management education programs to help assist patients to engage in self-care
Putting self-management into context • Self-management is 1 component within chronic disease management • Focus on formal self-management education programs to help assist patients to engage in self-care
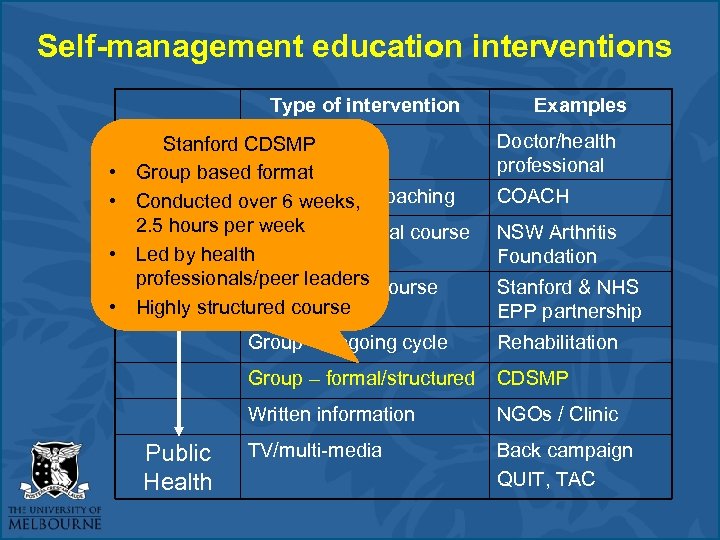 Self-management education interventions Type of intervention Stanford 1: 1 face-to-face Individual CDSMP • Group basedconsultation format 1: 1 6 weeks, • Conducted over telephone coaching 2. 5 hours per week individual course Internet • Led by health professionals/peer leaders course Internet group • Highly structured course Examples Doctor/health professional COACH NSW Arthritis Foundation Stanford & NHS EPP partnership Group – ongoing cycle Group – formal/structured CDSMP Written information Public Health Rehabilitation NGOs / Clinic TV/multi-media Back campaign QUIT, TAC
Self-management education interventions Type of intervention Stanford 1: 1 face-to-face Individual CDSMP • Group basedconsultation format 1: 1 6 weeks, • Conducted over telephone coaching 2. 5 hours per week individual course Internet • Led by health professionals/peer leaders course Internet group • Highly structured course Examples Doctor/health professional COACH NSW Arthritis Foundation Stanford & NHS EPP partnership Group – ongoing cycle Group – formal/structured CDSMP Written information Public Health Rehabilitation NGOs / Clinic TV/multi-media Back campaign QUIT, TAC
 Policy focus: • National Chronic Disease Strategy (NCDS) - Self-management identified as one of four key action areas - Self-care is important to manage chronic disease and supports need to be implemented at all levels of the health system - Need for programs, initiatives to develop and enhance self-management Self-management education programs
Policy focus: • National Chronic Disease Strategy (NCDS) - Self-management identified as one of four key action areas - Self-care is important to manage chronic disease and supports need to be implemented at all levels of the health system - Need for programs, initiatives to develop and enhance self-management Self-management education programs
 Program focus: • Sharing Health Care Initiative Demonstration Projects - $36. 2 million initiative (2001 -2004) - Explored suitability of chronic condition selfmanagement models within Australian setting
Program focus: • Sharing Health Care Initiative Demonstration Projects - $36. 2 million initiative (2001 -2004) - Explored suitability of chronic condition selfmanagement models within Australian setting
 Policy focus cont… • Australian Better Health Initiative (COAG) • $500 million over 4 years for chronic disease prevention & management - Focus on programs to actively encourage patients to selfmanage their condition • $14. 8 million over 4 years to fund awareness & education self-management of arthritis and osteoporosis
Policy focus cont… • Australian Better Health Initiative (COAG) • $500 million over 4 years for chronic disease prevention & management - Focus on programs to actively encourage patients to selfmanage their condition • $14. 8 million over 4 years to fund awareness & education self-management of arthritis and osteoporosis
 The way forward?
The way forward?
 Integration of CDSMP into the care continuum Lessons to be learnt from: Policy & program trends at the international level
Integration of CDSMP into the care continuum Lessons to be learnt from: Policy & program trends at the international level
 International trends in CDSMP • Focus on generic programs • UK government leader in field • “Expert Patients Programme” • Anglicised version of Stanford CDSMP implemented throughout National Health Service • £ 40 million spent since 2001 • Canada, Germany, Sweden, Denmark • less advanced re: policy and programs
International trends in CDSMP • Focus on generic programs • UK government leader in field • “Expert Patients Programme” • Anglicised version of Stanford CDSMP implemented throughout National Health Service • £ 40 million spent since 2001 • Canada, Germany, Sweden, Denmark • less advanced re: policy and programs
 Self-management policies 1. Stand alone • e. g. Expert Patients Programme (UK) 2. Incorporated as part of a chronic disease management strategy • • generic e. g. British Columbia (Canada) disease specific e. g. USA Arthritis Action Plan 3. Legislation • e. g. Germany • Disease Management Programs
Self-management policies 1. Stand alone • e. g. Expert Patients Programme (UK) 2. Incorporated as part of a chronic disease management strategy • • generic e. g. British Columbia (Canada) disease specific e. g. USA Arthritis Action Plan 3. Legislation • e. g. Germany • Disease Management Programs
 International challenges with the integration of CDSMP • Recruitment of consumers • Engagement with health professionals • Workforce sustainability
International challenges with the integration of CDSMP • Recruitment of consumers • Engagement with health professionals • Workforce sustainability
 Recruitment of consumers 1. Recruitment and retention of a critical mass of individuals has posed challenges • Social marketing - time and resource intensive - reach a small proportion of the target population *concern that some programs might increase health disparities • EPP moving to Community Interest Company - develop, market and deliver new and diverse s-m programs
Recruitment of consumers 1. Recruitment and retention of a critical mass of individuals has posed challenges • Social marketing - time and resource intensive - reach a small proportion of the target population *concern that some programs might increase health disparities • EPP moving to Community Interest Company - develop, market and deliver new and diverse s-m programs
 Health professional engagement • Health professionals crucial to the viability of programs • Primary conduits for patients with chronic conditions to enter self-management programs − Gatekeepers to the health system
Health professional engagement • Health professionals crucial to the viability of programs • Primary conduits for patients with chronic conditions to enter self-management programs − Gatekeepers to the health system
 Barriers to health professional engagement • Wariness of new initiatives • Lack of structured and uniform referral mechanism • Uncertainty of benefits to patients • Need for local evidence relating to patient outcomes and sustainability of programs
Barriers to health professional engagement • Wariness of new initiatives • Lack of structured and uniform referral mechanism • Uncertainty of benefits to patients • Need for local evidence relating to patient outcomes and sustainability of programs
 Workforce Sustainability • Complexities with peer led programs − Position of peer leaders and trainers in the health sector − Administration/resources/support
Workforce Sustainability • Complexities with peer led programs − Position of peer leaders and trainers in the health sector − Administration/resources/support
 Summary: Issues at the international level 1. Integration of CDSMP into the health sector is in its infancy 2. Recruitment and retention of a critical mass of individuals (patients and leaders) has posed challenges 3. Programs only reach a small proportion of the target population
Summary: Issues at the international level 1. Integration of CDSMP into the health sector is in its infancy 2. Recruitment and retention of a critical mass of individuals (patients and leaders) has posed challenges 3. Programs only reach a small proportion of the target population
 Summary: Issues at the international level 4. Engagement with health professionals 4. Translation of community programs to the health sector − Workforce issues
Summary: Issues at the international level 4. Engagement with health professionals 4. Translation of community programs to the health sector − Workforce issues
 ext ont yc oca L olic lp
ext ont yc oca L olic lp
 Australia Policy Initiatives • Strong policy direction • National Chronic Disease Strategy • Sharing Health Care Initiative Demonstration Projects • Australian Better Health Initiative
Australia Policy Initiatives • Strong policy direction • National Chronic Disease Strategy • Sharing Health Care Initiative Demonstration Projects • Australian Better Health Initiative
 State policy overview
State policy overview
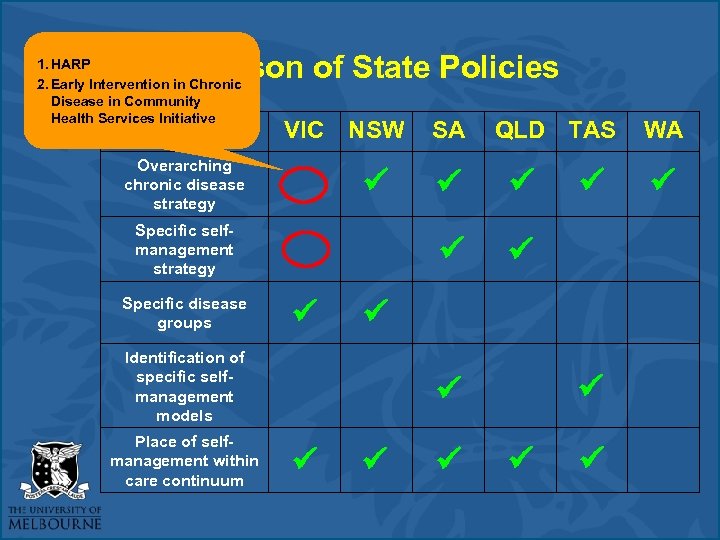 Comparison of State Policies 1. HARP 2. Early Intervention in Chronic Disease in Community Health Services Initiative VIC NSW Overarching chronic disease strategy Identification of specific selfmanagement models Place of selfmanagement within care continuum QLD TAS Specific selfmanagement strategy Specific disease groups SA WA
Comparison of State Policies 1. HARP 2. Early Intervention in Chronic Disease in Community Health Services Initiative VIC NSW Overarching chronic disease strategy Identification of specific selfmanagement models Place of selfmanagement within care continuum QLD TAS Specific selfmanagement strategy Specific disease groups SA WA
 What is the extent of integration of CDSMP within Australia? Short term trials or demonstration projects e. g. Sharing Health Care Initiative
What is the extent of integration of CDSMP within Australia? Short term trials or demonstration projects e. g. Sharing Health Care Initiative
 Sharing Health Care Initiative (SHCI) • 1999 Enhanced Primary Care Package - Shift from acute to primary care • SHCI considered a range of generic CDSM models for integration into wider health care system • 12 demonstration projects (8 focused on for SHCI evaluation)
Sharing Health Care Initiative (SHCI) • 1999 Enhanced Primary Care Package - Shift from acute to primary care • SHCI considered a range of generic CDSM models for integration into wider health care system • 12 demonstration projects (8 focused on for SHCI evaluation)
 Sharing Health Care Initiative (SHCI) • Evaluation (DHA) − A lot enthusiasm: contribution − GP engagement limited • Inability to capitalise on MBS / EPC items relating to chronic disease to assist with referral process • Social marketing strategies predominant
Sharing Health Care Initiative (SHCI) • Evaluation (DHA) − A lot enthusiasm: contribution − GP engagement limited • Inability to capitalise on MBS / EPC items relating to chronic disease to assist with referral process • Social marketing strategies predominant
 SHCI Evaluation: Barriers & Enablers • Barriers to patient participation - dissemination of information transport ill health too busy/disinterested • Successful strategies • targeted specific groups and • modified content/delivery to suit needs e. g. CALD
SHCI Evaluation: Barriers & Enablers • Barriers to patient participation - dissemination of information transport ill health too busy/disinterested • Successful strategies • targeted specific groups and • modified content/delivery to suit needs e. g. CALD
 Integration themes – international & local 1. Profile of self-management needs to be raised within health sector 2. Engagement of health professional is essential 3. Structured referral pathways and networks across the care continuum are required 4. Programs need to be flexible in both content and delivery
Integration themes – international & local 1. Profile of self-management needs to be raised within health sector 2. Engagement of health professional is essential 3. Structured referral pathways and networks across the care continuum are required 4. Programs need to be flexible in both content and delivery
 To integrate or not to integrate? • Self-management has the potential to make a profound contribution to health and wellbeing across the care continuum • However it is currently unknown if programs are meeting the needs of consumers & health professionals in terms of: • content, • accessibility, and • reach
To integrate or not to integrate? • Self-management has the potential to make a profound contribution to health and wellbeing across the care continuum • However it is currently unknown if programs are meeting the needs of consumers & health professionals in terms of: • content, • accessibility, and • reach
 Feedback at the grassroots level Consultation with Victorian GPs & Consumers
Feedback at the grassroots level Consultation with Victorian GPs & Consumers
 Qualitative study • Methods - Interviews : 17 GPs and 43 consumers - Purposeful sampling employed - Consumers : GPs, Rheumatologists and existing research database - GPs recruited via 3 Div of General Practices (Northern, Dandenong & South Gippsland)
Qualitative study • Methods - Interviews : 17 GPs and 43 consumers - Purposeful sampling employed - Consumers : GPs, Rheumatologists and existing research database - GPs recruited via 3 Div of General Practices (Northern, Dandenong & South Gippsland)
 Common Barriers (GPs & Consumers) “GPs need to know how beneficial or valuable these programs are so they are able to assess whether this could potentially benefit patients” • Lack of general awareness and knowledge “Lack of knowledge by health professionals, if it was advertised in GP surgeries, hospitals, specialists telling people about it … just make people aware of these programs …” • Consumer perceptions that health professionals should advertise or spread information
Common Barriers (GPs & Consumers) “GPs need to know how beneficial or valuable these programs are so they are able to assess whether this could potentially benefit patients” • Lack of general awareness and knowledge “Lack of knowledge by health professionals, if it was advertised in GP surgeries, hospitals, specialists telling people about it … just make people aware of these programs …” • Consumer perceptions that health professionals should advertise or spread information
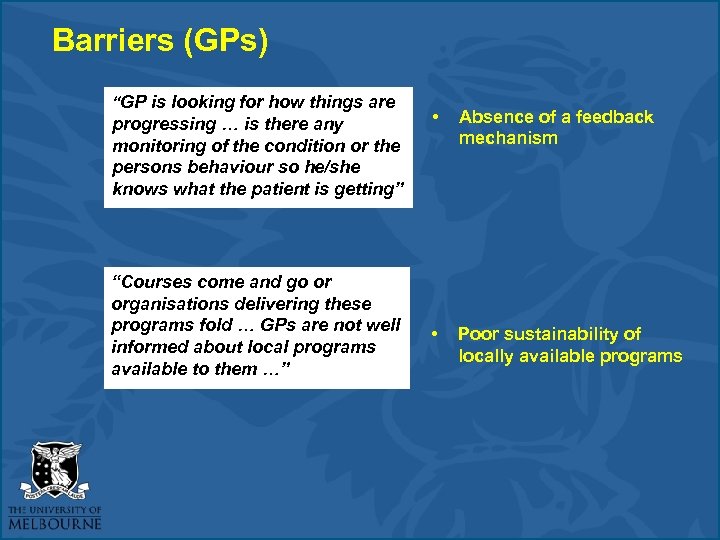 Barriers (GPs) “GP is looking for how things are progressing … is there any monitoring of the condition or the persons behaviour so he/she knows what the patient is getting” “Courses come and go or organisations delivering these programs fold … GPs are not well informed about local programs available to them …” • Absence of a feedback mechanism • Poor sustainability of locally available programs
Barriers (GPs) “GP is looking for how things are progressing … is there any monitoring of the condition or the persons behaviour so he/she knows what the patient is getting” “Courses come and go or organisations delivering these programs fold … GPs are not well informed about local programs available to them …” • Absence of a feedback mechanism • Poor sustainability of locally available programs
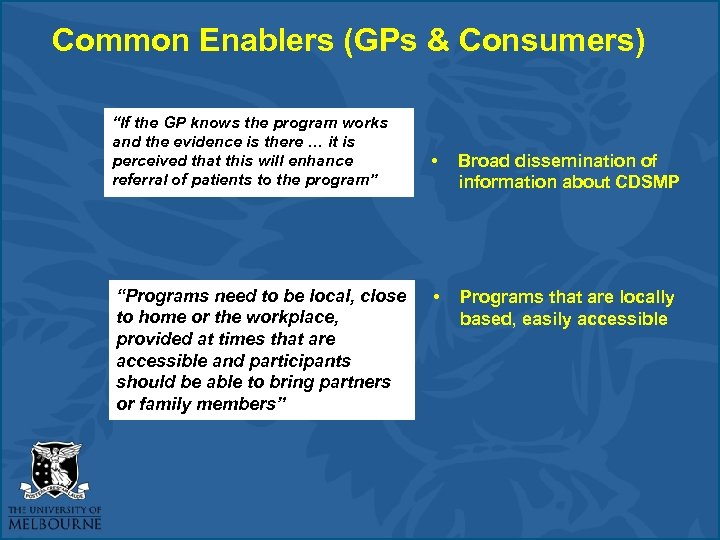 Common Enablers (GPs & Consumers) “If the GP knows the program works and the evidence is there … it is perceived that this will enhance referral of patients to the program” “Programs need to be local, close to home or the workplace, provided at times that are accessible and participants should be able to bring partners or family members” • Broad dissemination of information about CDSMP • Programs that are locally based, easily accessible
Common Enablers (GPs & Consumers) “If the GP knows the program works and the evidence is there … it is perceived that this will enhance referral of patients to the program” “Programs need to be local, close to home or the workplace, provided at times that are accessible and participants should be able to bring partners or family members” • Broad dissemination of information about CDSMP • Programs that are locally based, easily accessible
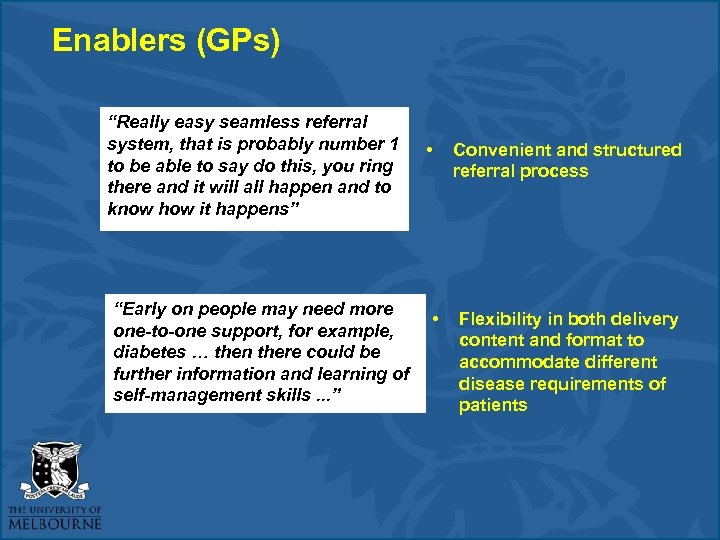 Enablers (GPs) “Really easy seamless referral system, that is probably number 1 to be able to say do this, you ring there and it will all happen and to know how it happens” “Early on people may need more one-to-one support, for example, diabetes … then there could be further information and learning of self-management skills. . . ” • • Convenient and structured referral process Flexibility in both delivery content and format to accommodate different disease requirements of patients
Enablers (GPs) “Really easy seamless referral system, that is probably number 1 to be able to say do this, you ring there and it will all happen and to know how it happens” “Early on people may need more one-to-one support, for example, diabetes … then there could be further information and learning of self-management skills. . . ” • • Convenient and structured referral process Flexibility in both delivery content and format to accommodate different disease requirements of patients
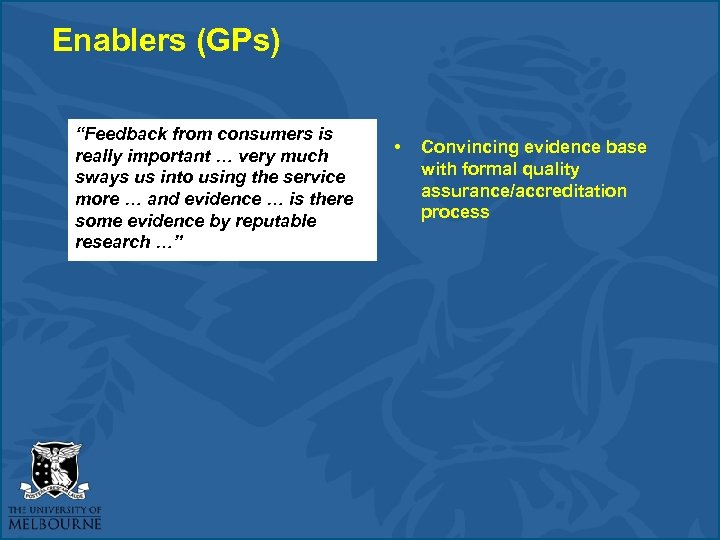 Enablers (GPs) “Feedback from consumers is really important … very much sways us into using the service more … and evidence … is there some evidence by reputable research …” • Convincing evidence base with formal quality assurance/accreditation process
Enablers (GPs) “Feedback from consumers is really important … very much sways us into using the service more … and evidence … is there some evidence by reputable research …” • Convincing evidence base with formal quality assurance/accreditation process
 Enablers (Consumers) Key factor for consumer participation is recommendation from health professional “Well I think all GPs should know about it and then the GP, if they know their patient well enough and have a good rapport should be able to say I think this should benefit you and should encourage you to go along … really that is the basis for that, you go to a GP who is the first port of call …”
Enablers (Consumers) Key factor for consumer participation is recommendation from health professional “Well I think all GPs should know about it and then the GP, if they know their patient well enough and have a good rapport should be able to say I think this should benefit you and should encourage you to go along … really that is the basis for that, you go to a GP who is the first port of call …”
 What needs to be done to take self-management forward? SELF-MANAGEMENT SERVICE IMPROVEMENT FRAMEWORK
What needs to be done to take self-management forward? SELF-MANAGEMENT SERVICE IMPROVEMENT FRAMEWORK
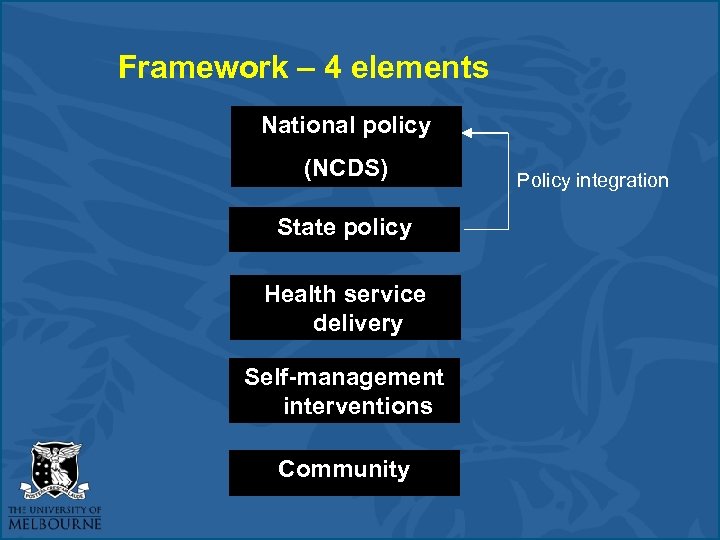 Framework – 4 elements National policy (NCDS) State policy Health service delivery Self-management interventions Community Policy integration
Framework – 4 elements National policy (NCDS) State policy Health service delivery Self-management interventions Community Policy integration
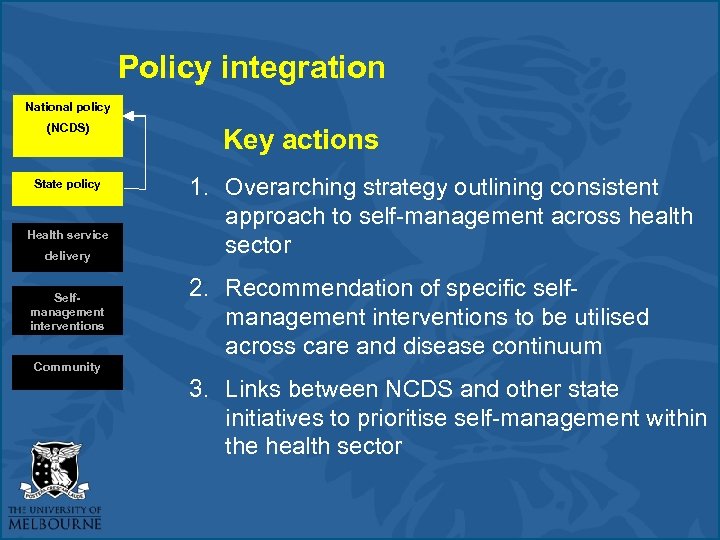 Policy integration National policy (NCDS) State policy Health service delivery Selfmanagement interventions Key actions 1. Overarching strategy outlining consistent approach to self-management across health sector 2. Recommendation of specific selfmanagement interventions to be utilised across care and disease continuum Community 3. Links between NCDS and other state initiatives to prioritise self-management within the health sector
Policy integration National policy (NCDS) State policy Health service delivery Selfmanagement interventions Key actions 1. Overarching strategy outlining consistent approach to self-management across health sector 2. Recommendation of specific selfmanagement interventions to be utilised across care and disease continuum Community 3. Links between NCDS and other state initiatives to prioritise self-management within the health sector
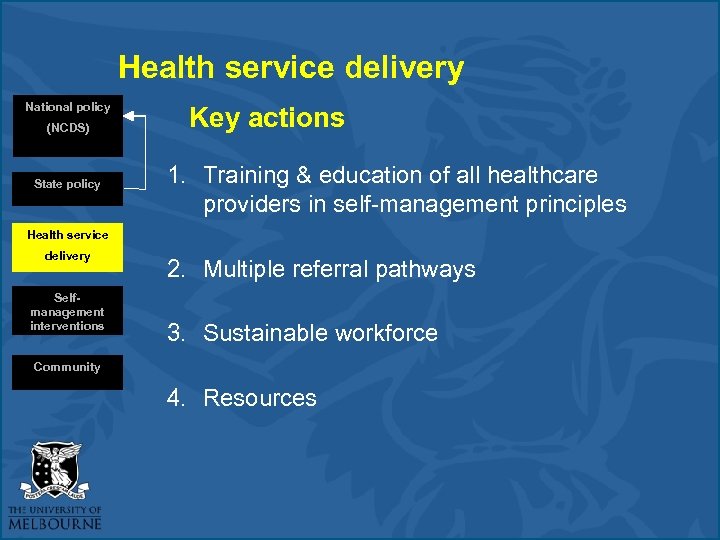 Health service delivery National policy (NCDS) State policy Key actions 1. Training & education of all healthcare providers in self-management principles Health service delivery Selfmanagement interventions 2. Multiple referral pathways 3. Sustainable workforce Community 4. Resources
Health service delivery National policy (NCDS) State policy Key actions 1. Training & education of all healthcare providers in self-management principles Health service delivery Selfmanagement interventions 2. Multiple referral pathways 3. Sustainable workforce Community 4. Resources
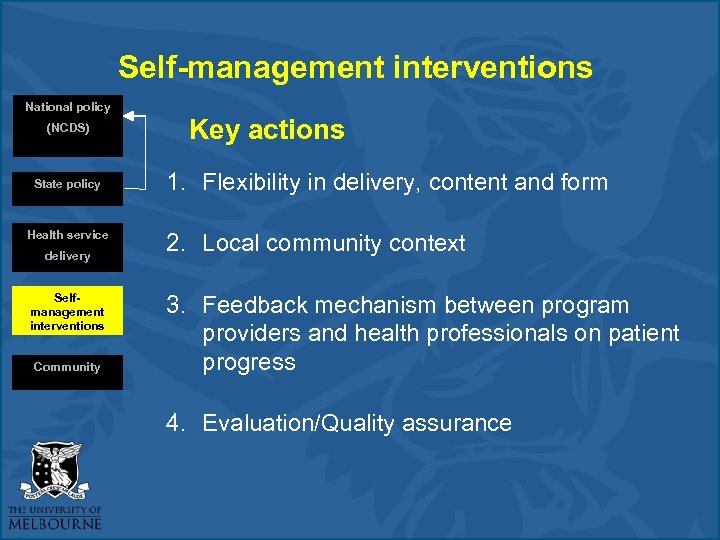 Self-management interventions National policy (NCDS) State policy Health service delivery Selfmanagement interventions Community Key actions 1. Flexibility in delivery, content and form 2. Local community context 3. Feedback mechanism between program providers and health professionals on patient progress 4. Evaluation/Quality assurance
Self-management interventions National policy (NCDS) State policy Health service delivery Selfmanagement interventions Community Key actions 1. Flexibility in delivery, content and form 2. Local community context 3. Feedback mechanism between program providers and health professionals on patient progress 4. Evaluation/Quality assurance
 Evaluation & Quality Assurance • Health Education Impact Questionnaire (hei. Q) • Piloted as national quality and monitoring system across self-management programs in Australia • Broad range of self-management education interventions • Benchmark and provide national data on effectiveness of programs
Evaluation & Quality Assurance • Health Education Impact Questionnaire (hei. Q) • Piloted as national quality and monitoring system across self-management programs in Australia • Broad range of self-management education interventions • Benchmark and provide national data on effectiveness of programs

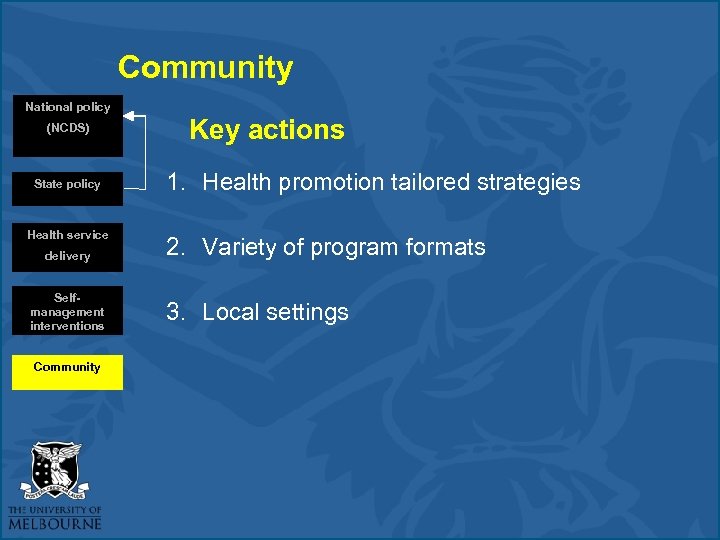 Community National policy (NCDS) State policy Health service delivery Selfmanagement interventions Community Key actions 1. Health promotion tailored strategies 2. Variety of program formats 3. Local settings
Community National policy (NCDS) State policy Health service delivery Selfmanagement interventions Community Key actions 1. Health promotion tailored strategies 2. Variety of program formats 3. Local settings
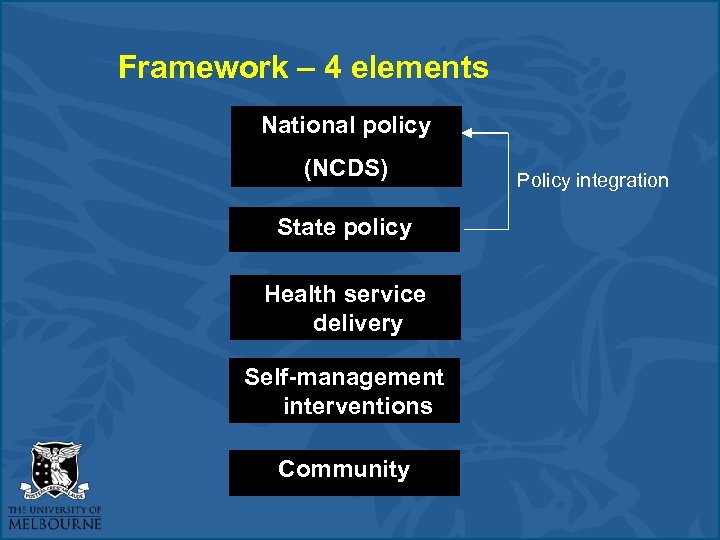 Framework – 4 elements National policy (NCDS) State policy Health service delivery Self-management interventions Community Policy integration
Framework – 4 elements National policy (NCDS) State policy Health service delivery Self-management interventions Community Policy integration
 Policy Recommendations
Policy Recommendations
 Acknowledgements • • Joan Nankervis Bella Laidlaw Dr Caroline Brand (principal investigator) Dr Richard Osborne (principal investigator)
Acknowledgements • • Joan Nankervis Bella Laidlaw Dr Caroline Brand (principal investigator) Dr Richard Osborne (principal investigator)
 Thank you jjordan@unimelb. edu. au
Thank you jjordan@unimelb. edu. au


