Chronic Coronary Artery Disease Sergey Yalonetsky M.D. Ischemic




7340-stable_angina_2012.ppt
- Количество слайдов: 82
 Chronic Coronary Artery Disease Sergey Yalonetsky M.D.
Chronic Coronary Artery Disease Sergey Yalonetsky M.D.
 Ischemic Heart Disease Acute Myocardial Infarction Unstable AP Chronic Stable AP
Ischemic Heart Disease Acute Myocardial Infarction Unstable AP Chronic Stable AP
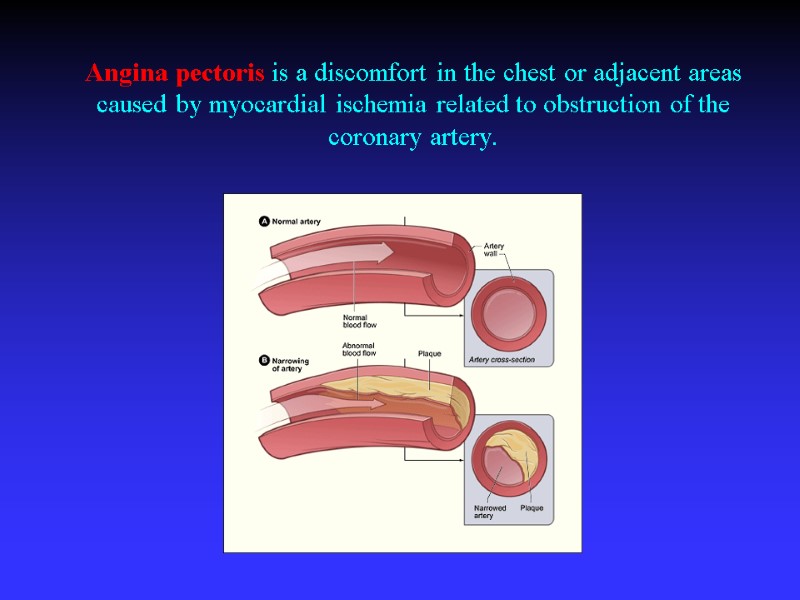
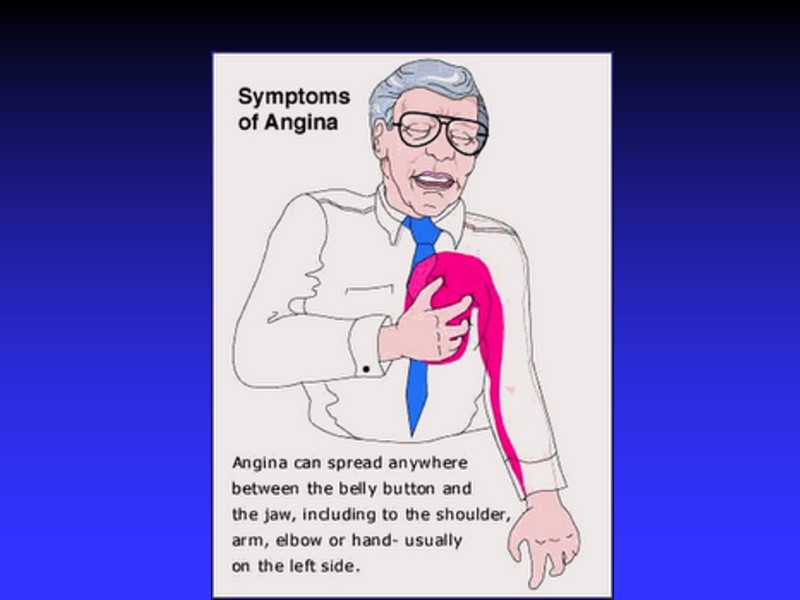
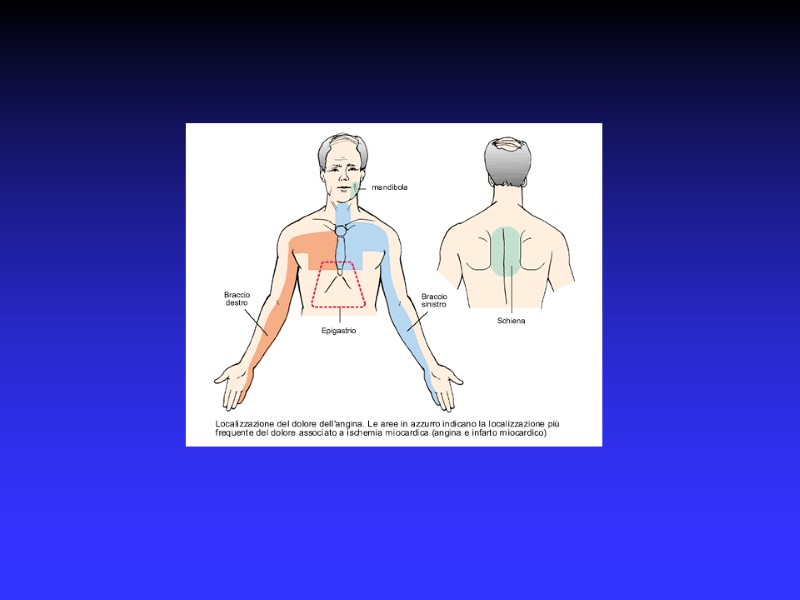
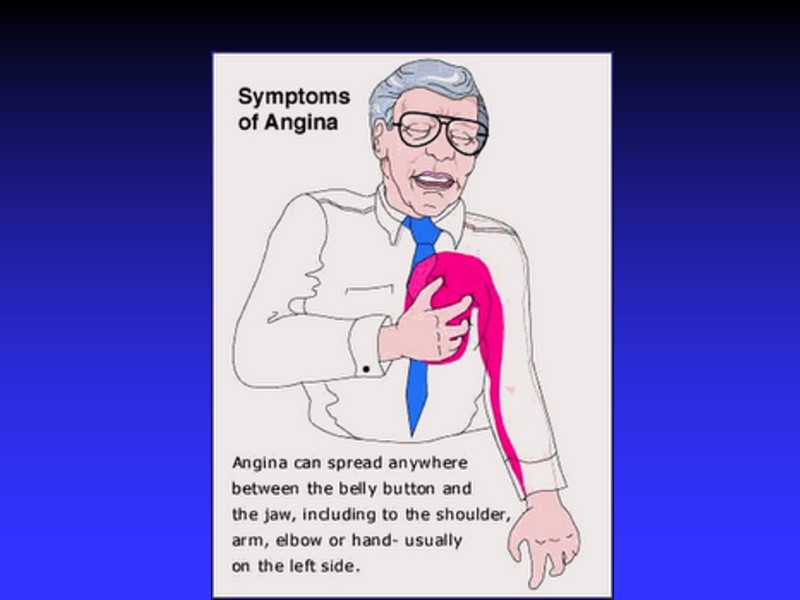
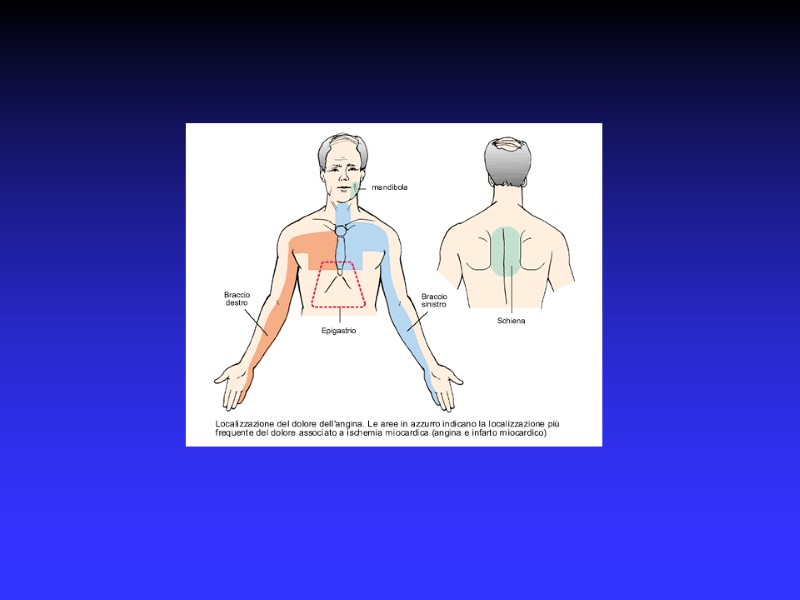
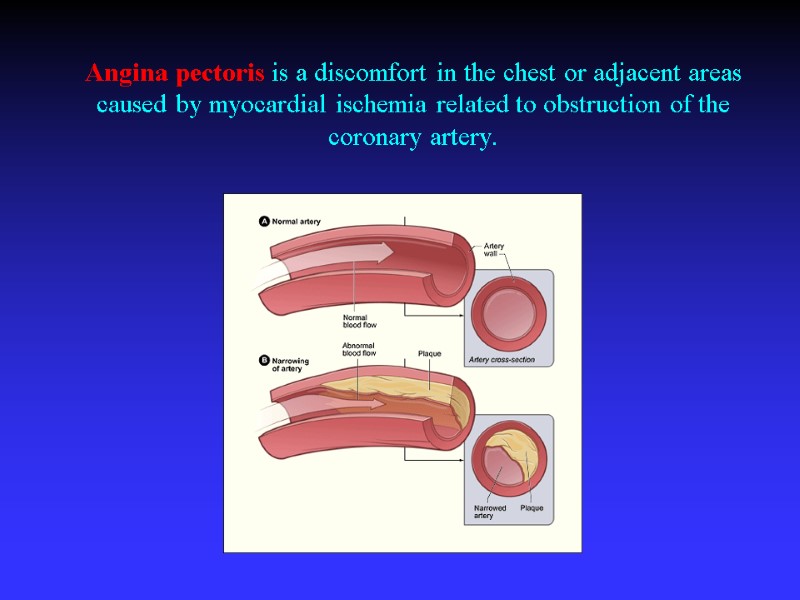 Angina pectoris is a discomfort in the chest or adjacent areas caused by myocardial ischemia related to obstruction of the coronary artery.
Angina pectoris is a discomfort in the chest or adjacent areas caused by myocardial ischemia related to obstruction of the coronary artery.
 Oxygen delivery-Oxygen demand
Oxygen delivery-Oxygen demand
 Coronary obstruction Atheromatous plaque Congenital abnormalities of the coronary vessels Myocardial bridging, Coronary arteritis in association with the systemic vasculitides, Radiation-induced coronary disease.
Coronary obstruction Atheromatous plaque Congenital abnormalities of the coronary vessels Myocardial bridging, Coronary arteritis in association with the systemic vasculitides, Radiation-induced coronary disease.
 Myocardial ischemia in the absence of obstructive CAD Aortic valve disease Hypertrophic cardiomyopathy
Myocardial ischemia in the absence of obstructive CAD Aortic valve disease Hypertrophic cardiomyopathy
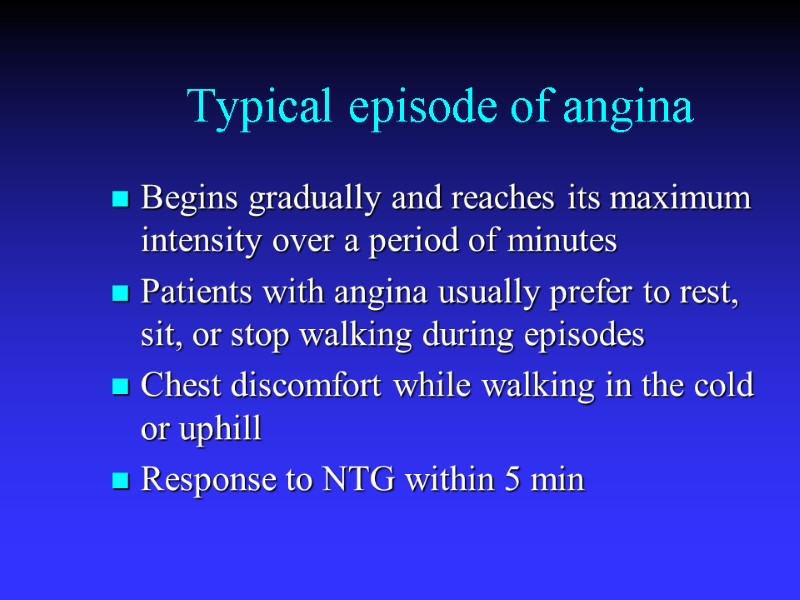
 Typical episode of angina Begins gradually and reaches its maximum intensity over a period of minutes Patients with angina usually prefer to rest, sit, or stop walking during episodes Chest discomfort while walking in the cold or uphill Response to NTG within 5 min
Typical episode of angina Begins gradually and reaches its maximum intensity over a period of minutes Patients with angina usually prefer to rest, sit, or stop walking during episodes Chest discomfort while walking in the cold or uphill Response to NTG within 5 min
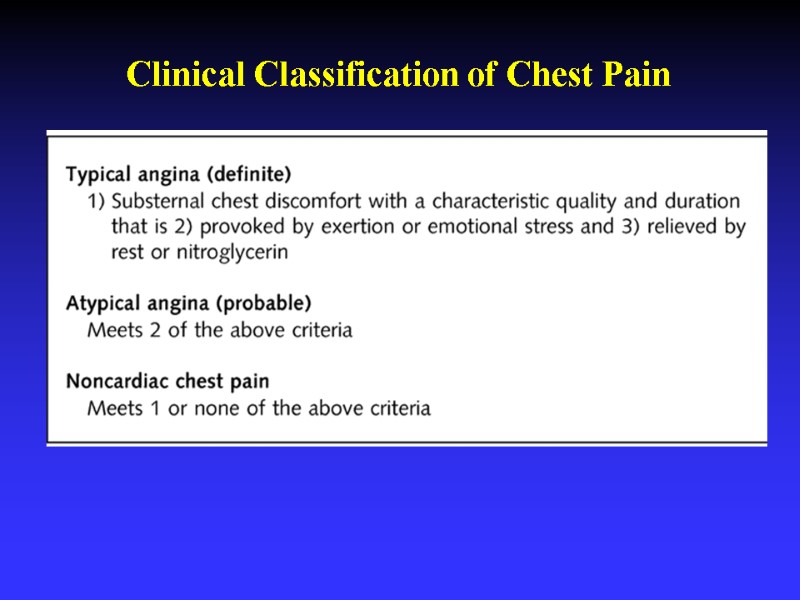
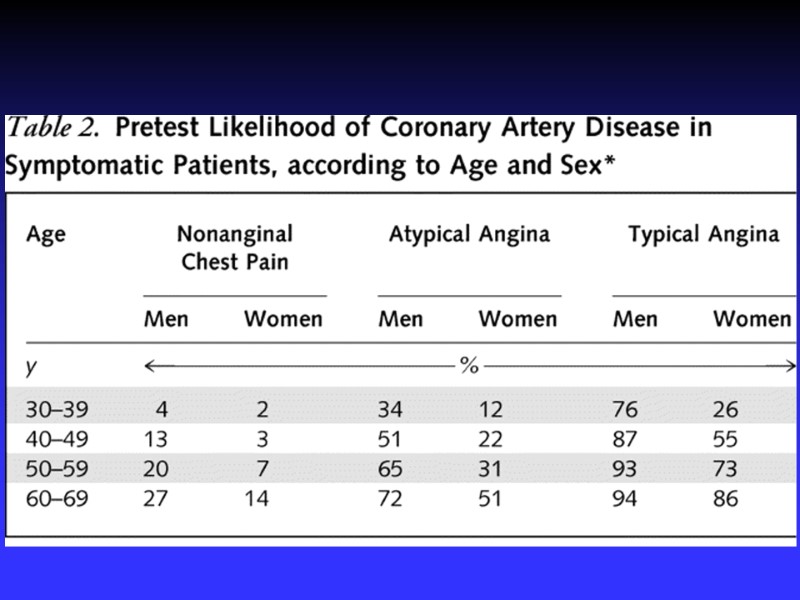
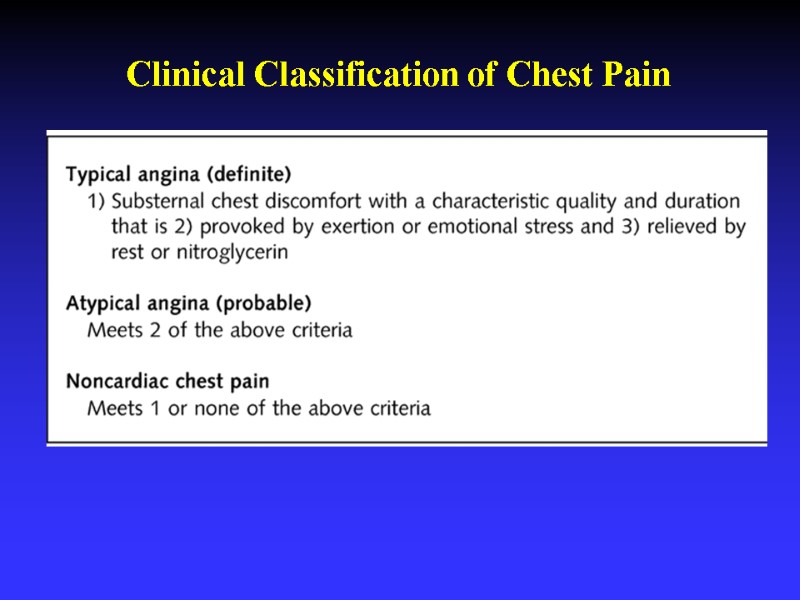 Clinical Classification of Chest Pain
Clinical Classification of Chest Pain
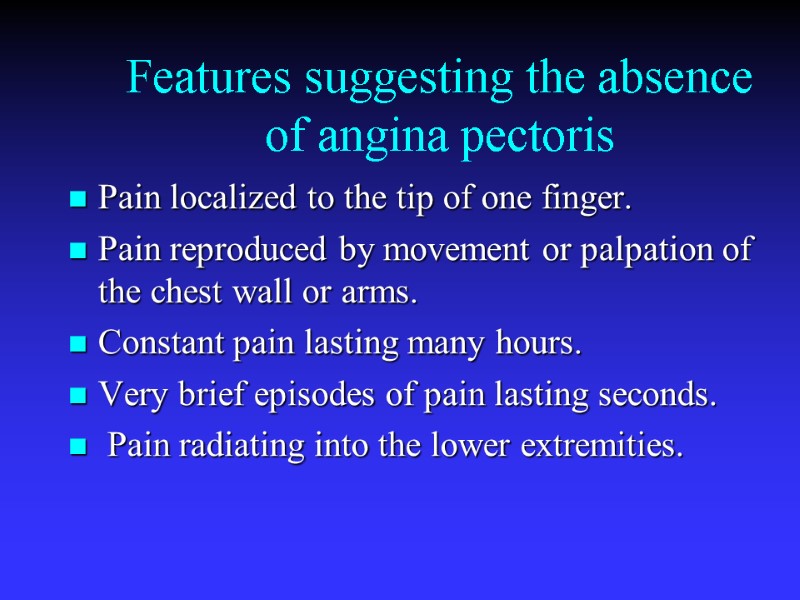
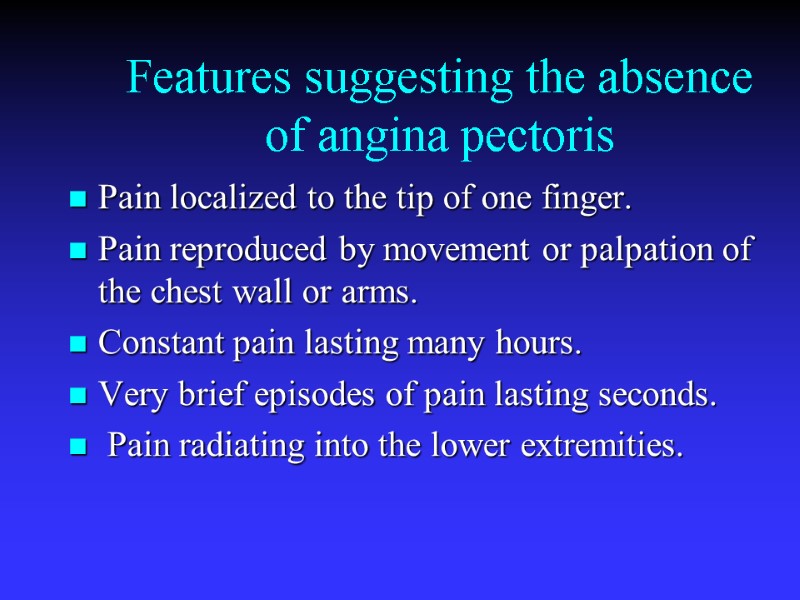 Features suggesting the absence of angina pectoris Pain localized to the tip of one finger. Pain reproduced by movement or palpation of the chest wall or arms. Constant pain lasting many hours. Very brief episodes of pain lasting seconds. Pain radiating into the lower extremities.
Features suggesting the absence of angina pectoris Pain localized to the tip of one finger. Pain reproduced by movement or palpation of the chest wall or arms. Constant pain lasting many hours. Very brief episodes of pain lasting seconds. Pain radiating into the lower extremities.
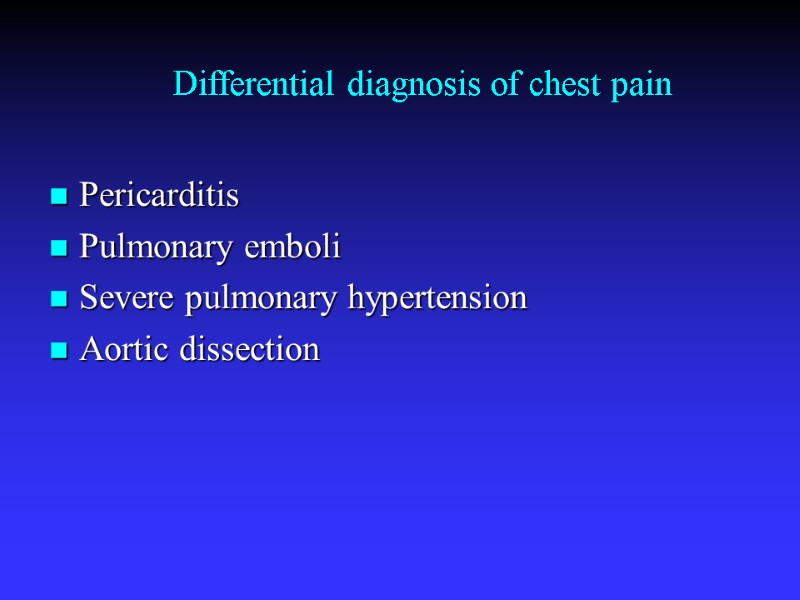 Differential diagnosis of chest pain Pericarditis Pulmonary emboli Severe pulmonary hypertension Aortic dissection
Differential diagnosis of chest pain Pericarditis Pulmonary emboli Severe pulmonary hypertension Aortic dissection
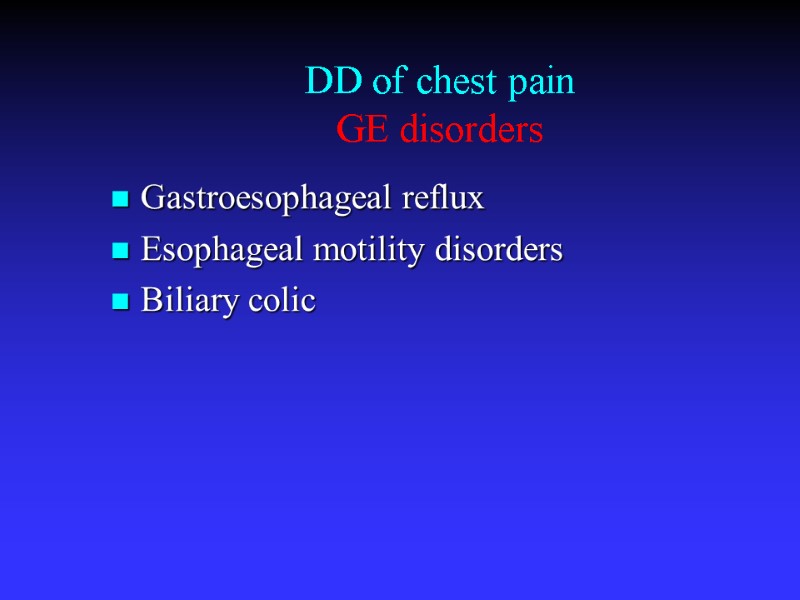 DD of chest pain GE disorders Gastroesophageal reflux Esophageal motility disorders Biliary colic
DD of chest pain GE disorders Gastroesophageal reflux Esophageal motility disorders Biliary colic
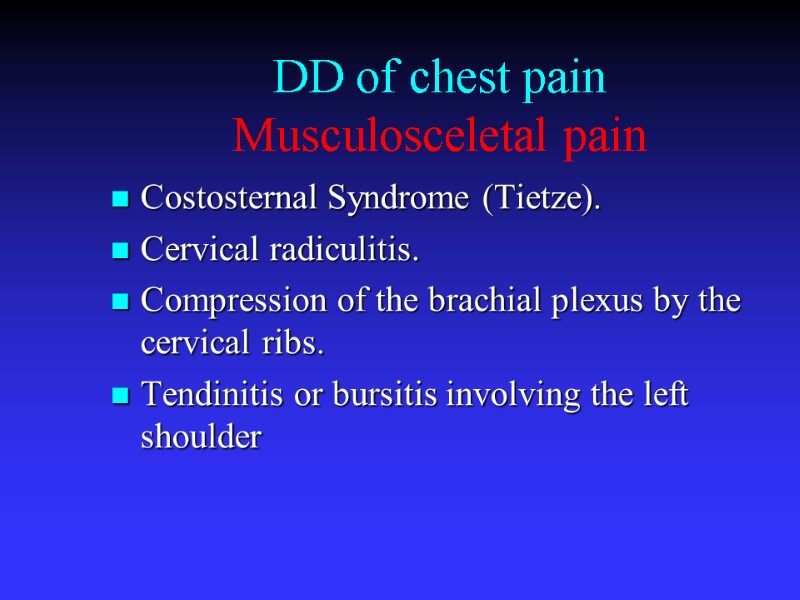 DD of chest pain Musculosceletal pain Costosternal Syndrome (Tietze). Cervical radiculitis. Compression of the brachial plexus by the cervical ribs. Tendinitis or bursitis involving the left shoulder
DD of chest pain Musculosceletal pain Costosternal Syndrome (Tietze). Cervical radiculitis. Compression of the brachial plexus by the cervical ribs. Tendinitis or bursitis involving the left shoulder
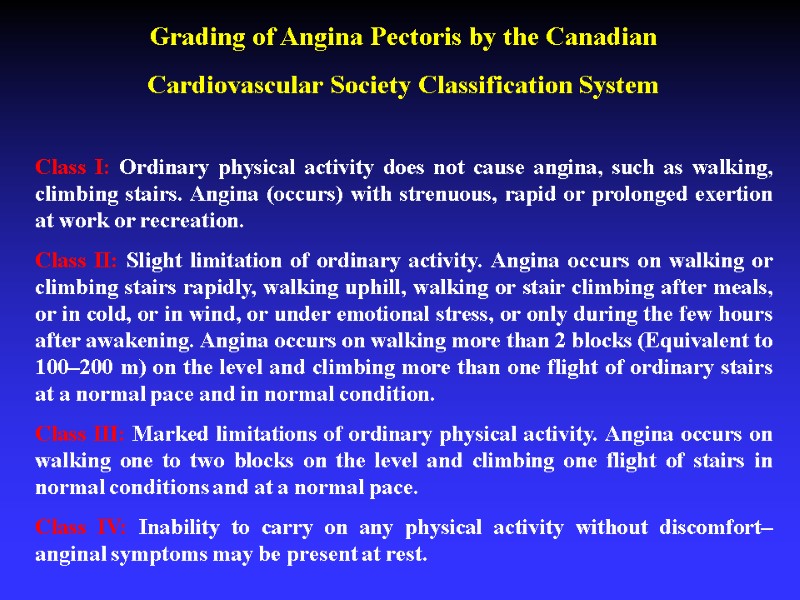
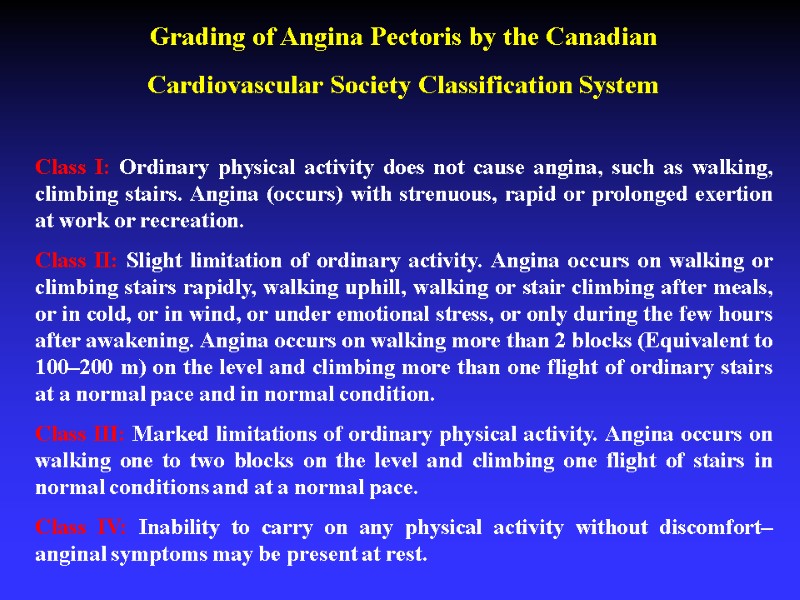 Grading of Angina Pectoris by the Canadian Cardiovascular Society Classification System Class I: Ordinary physical activity does not cause angina, such as walking, climbing stairs. Angina (occurs) with strenuous, rapid or prolonged exertion at work or recreation. Class II: Slight limitation of ordinary activity. Angina occurs on walking or climbing stairs rapidly, walking uphill, walking or stair climbing after meals, or in cold, or in wind, or under emotional stress, or only during the few hours after awakening. Angina occurs on walking more than 2 blocks (Equivalent to 100–200 m) on the level and climbing more than one flight of ordinary stairs at a normal pace and in normal condition. Class III: Marked limitations of ordinary physical activity. Angina occurs on walking one to two blocks on the level and climbing one flight of stairs in normal conditions and at a normal pace. Class IV: Inability to carry on any physical activity without discomfort–anginal symptoms may be present at rest.
Grading of Angina Pectoris by the Canadian Cardiovascular Society Classification System Class I: Ordinary physical activity does not cause angina, such as walking, climbing stairs. Angina (occurs) with strenuous, rapid or prolonged exertion at work or recreation. Class II: Slight limitation of ordinary activity. Angina occurs on walking or climbing stairs rapidly, walking uphill, walking or stair climbing after meals, or in cold, or in wind, or under emotional stress, or only during the few hours after awakening. Angina occurs on walking more than 2 blocks (Equivalent to 100–200 m) on the level and climbing more than one flight of ordinary stairs at a normal pace and in normal condition. Class III: Marked limitations of ordinary physical activity. Angina occurs on walking one to two blocks on the level and climbing one flight of stairs in normal conditions and at a normal pace. Class IV: Inability to carry on any physical activity without discomfort–anginal symptoms may be present at rest.
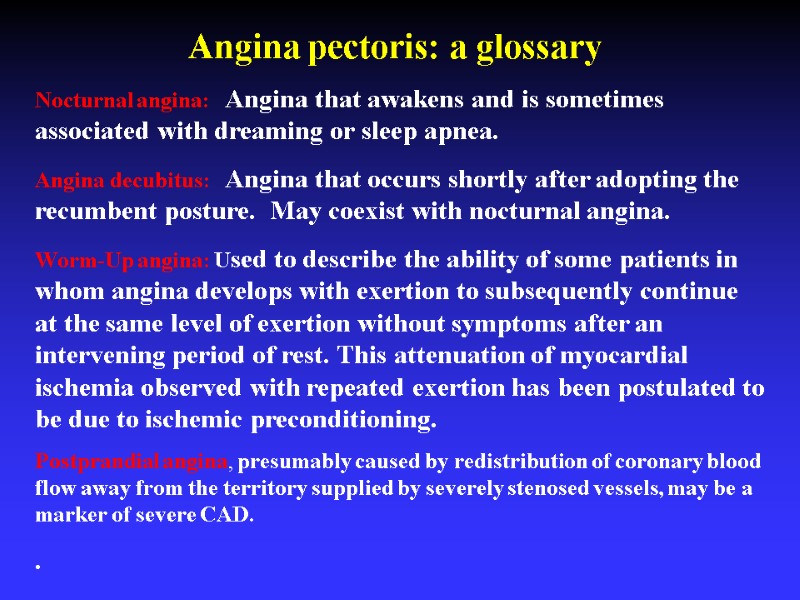 Nocturnal angina: Angina that awakens and is sometimes associated with dreaming or sleep apnea. Angina decubitus: Angina that occurs shortly after adopting the recumbent posture. May coexist with nocturnal angina. Worm-Up angina: Used to describe the ability of some patients in whom angina develops with exertion to subsequently continue at the same level of exertion without symptoms after an intervening period of rest. This attenuation of myocardial ischemia observed with repeated exertion has been postulated to be due to ischemic preconditioning. Postprandial angina, presumably caused by redistribution of coronary blood flow away from the territory supplied by severely stenosed vessels, may be a marker of severe CAD. . Angina pectoris: a glossary
Nocturnal angina: Angina that awakens and is sometimes associated with dreaming or sleep apnea. Angina decubitus: Angina that occurs shortly after adopting the recumbent posture. May coexist with nocturnal angina. Worm-Up angina: Used to describe the ability of some patients in whom angina develops with exertion to subsequently continue at the same level of exertion without symptoms after an intervening period of rest. This attenuation of myocardial ischemia observed with repeated exertion has been postulated to be due to ischemic preconditioning. Postprandial angina, presumably caused by redistribution of coronary blood flow away from the territory supplied by severely stenosed vessels, may be a marker of severe CAD. . Angina pectoris: a glossary
 Angina equivalents Symptoms other than pain or discomfort that are ischemic related and serve as angina surrogates, e.g., dyspnea, diaphoresis, fatigue, or light-headedness
Angina equivalents Symptoms other than pain or discomfort that are ischemic related and serve as angina surrogates, e.g., dyspnea, diaphoresis, fatigue, or light-headedness
 Physical Examination
Physical Examination
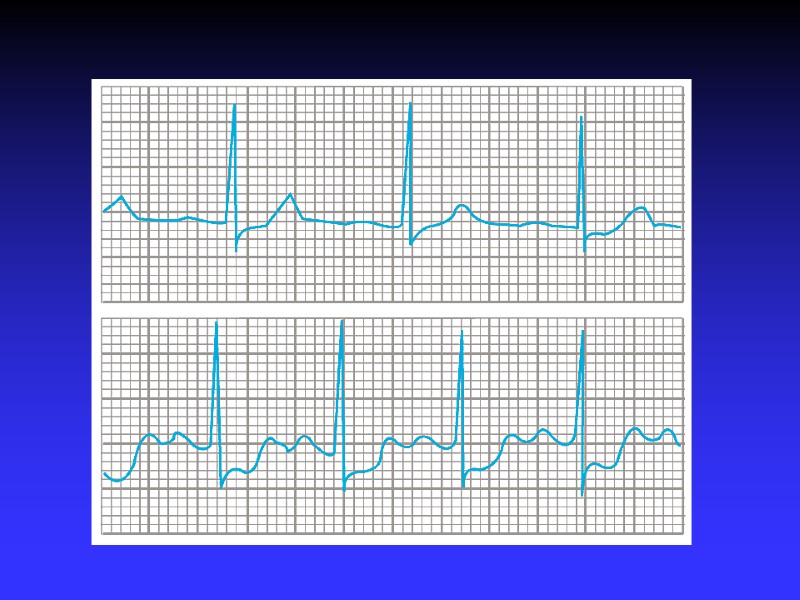
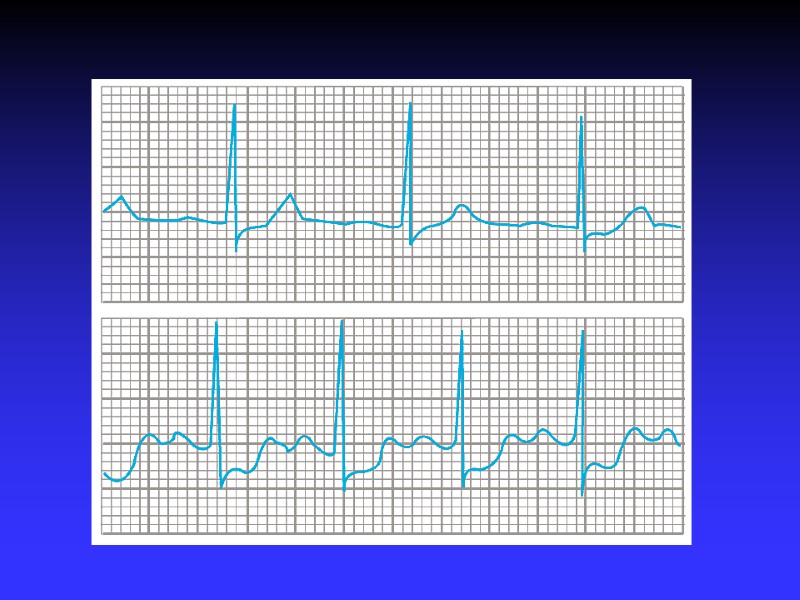
 ECG Rest ECG is normal in 50 % even in presence of severe CAD ST-T findings are the most common changes During an episode of angina pectoris, the ECG becomes abnormal in 50% or more of patients with normal resting ECGs
ECG Rest ECG is normal in 50 % even in presence of severe CAD ST-T findings are the most common changes During an episode of angina pectoris, the ECG becomes abnormal in 50% or more of patients with normal resting ECGs
 ECG (2) Look for: - Q waves - LBBB or LAHB - “pseudonormalization” - LVH signs
ECG (2) Look for: - Q waves - LBBB or LAHB - “pseudonormalization” - LVH signs
 ECG (3) DD of ST-T changes: - LVH - electrolyte abnormalities, - neurogenic effects -antiarrhythmic drugs
ECG (3) DD of ST-T changes: - LVH - electrolyte abnormalities, - neurogenic effects -antiarrhythmic drugs
 Prognostic significance of the rest ECG Normal resting ECG is a favorable long-term prognostic sign in patients with suspected or definite CAD. LV hypertrophy on the ECG is an indicator of worse prognosis in patients with chronic stable angina
Prognostic significance of the rest ECG Normal resting ECG is a favorable long-term prognostic sign in patients with suspected or definite CAD. LV hypertrophy on the ECG is an indicator of worse prognosis in patients with chronic stable angina
 Non-invasive stress testing To establish diagnosis To asses prognosis
Non-invasive stress testing To establish diagnosis To asses prognosis
 Non-invasive stress imaging Stress echocardiography Nuclear stress imaging Stress MRI
Non-invasive stress imaging Stress echocardiography Nuclear stress imaging Stress MRI
 Exercise echocardiography
Exercise echocardiography
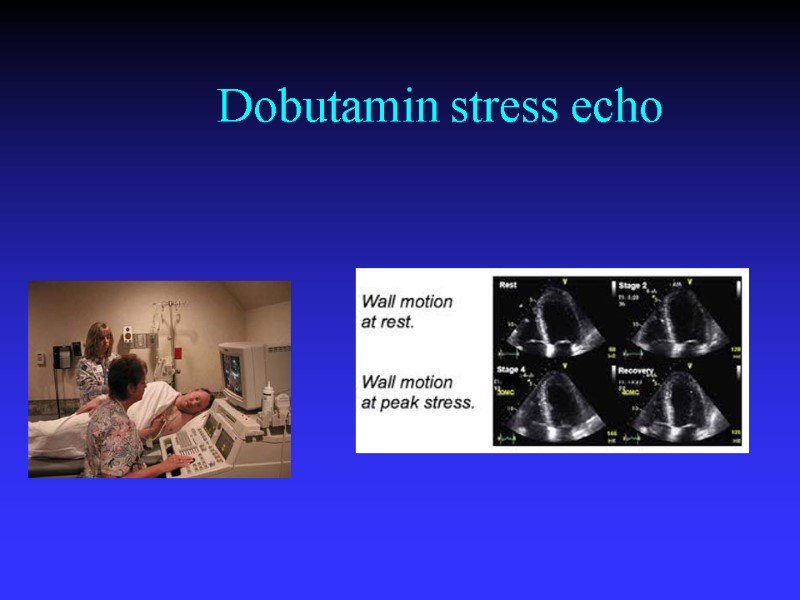
 Dobutamin stress echo
Dobutamin stress echo
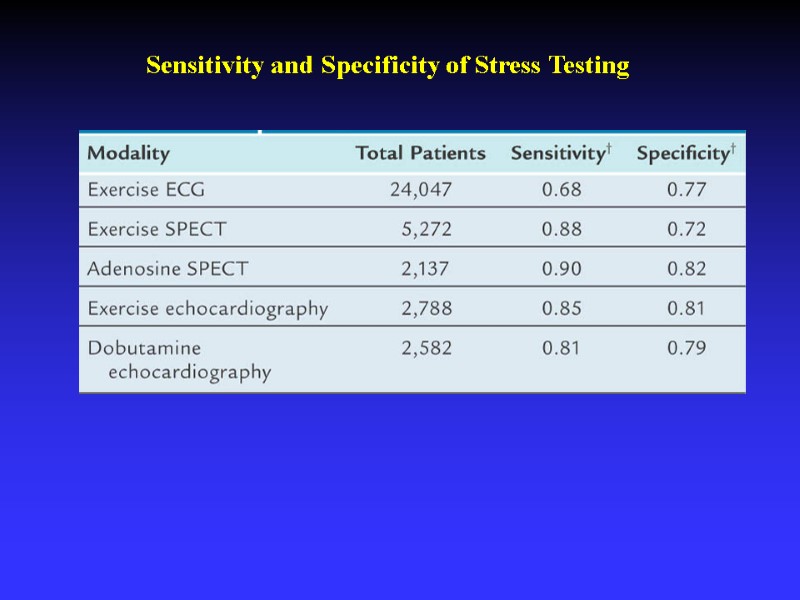
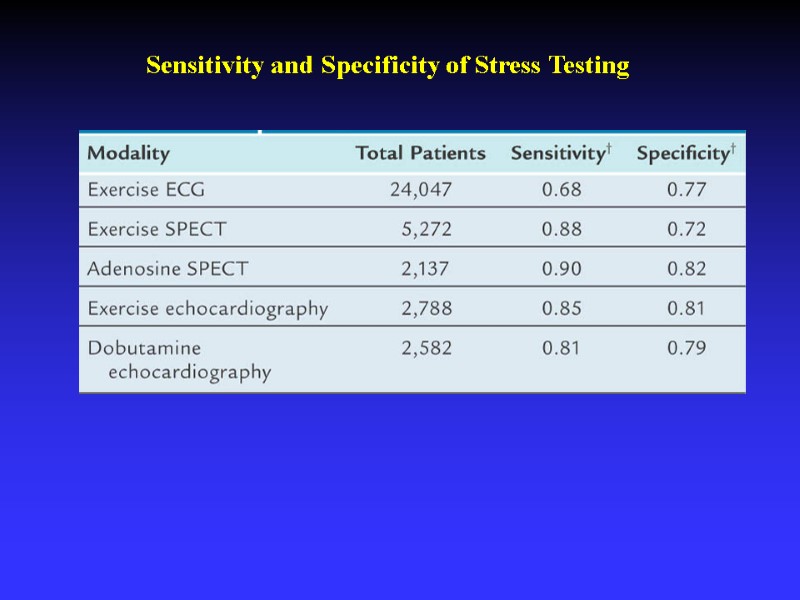 Sensitivity and Specificity of Stress Testing
Sensitivity and Specificity of Stress Testing
 RISK STRATIFICATION in stable AP The rationale is to identify high risk patients in whom coronary angiography and subsequent revascularization might improve survival
RISK STRATIFICATION in stable AP The rationale is to identify high risk patients in whom coronary angiography and subsequent revascularization might improve survival
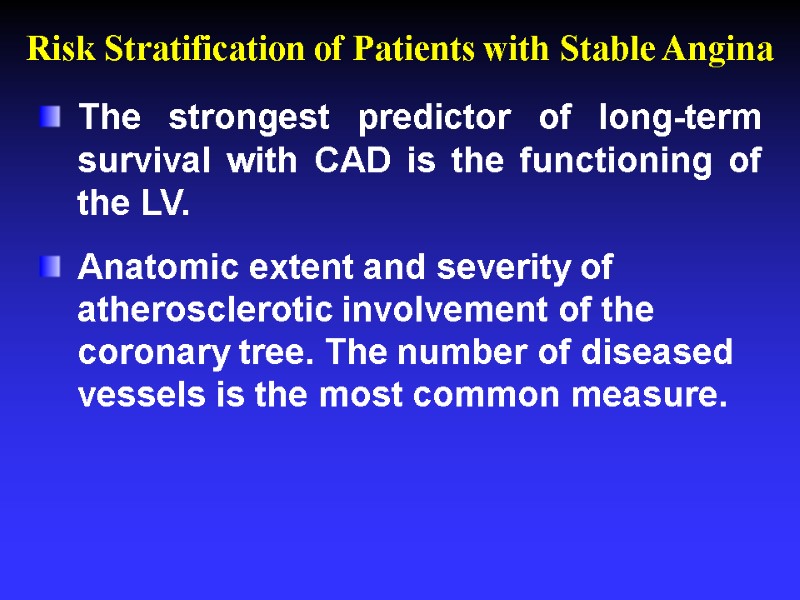 The strongest predictor of long-term survival with CAD is the functioning of the LV. Anatomic extent and severity of atherosclerotic involvement of the coronary tree. The number of diseased vessels is the most common measure. Risk Stratification of Patients with Stable Angina
The strongest predictor of long-term survival with CAD is the functioning of the LV. Anatomic extent and severity of atherosclerotic involvement of the coronary tree. The number of diseased vessels is the most common measure. Risk Stratification of Patients with Stable Angina
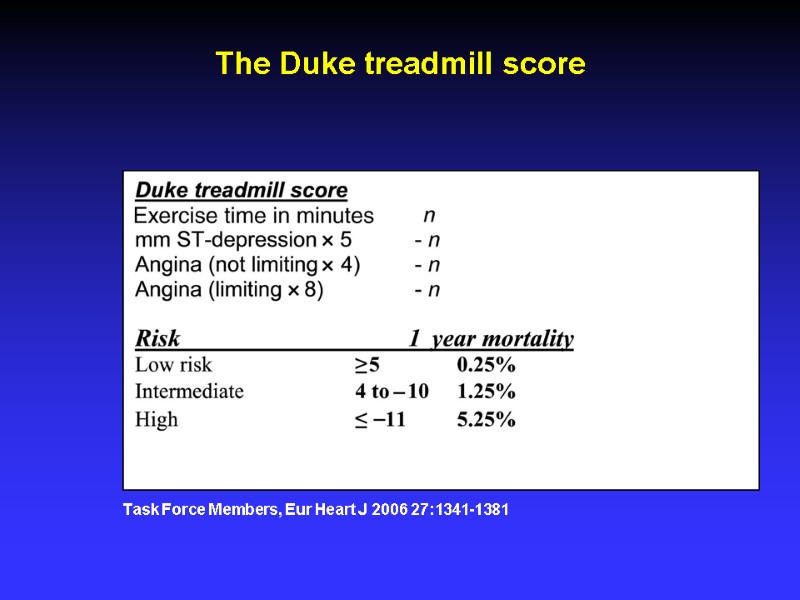
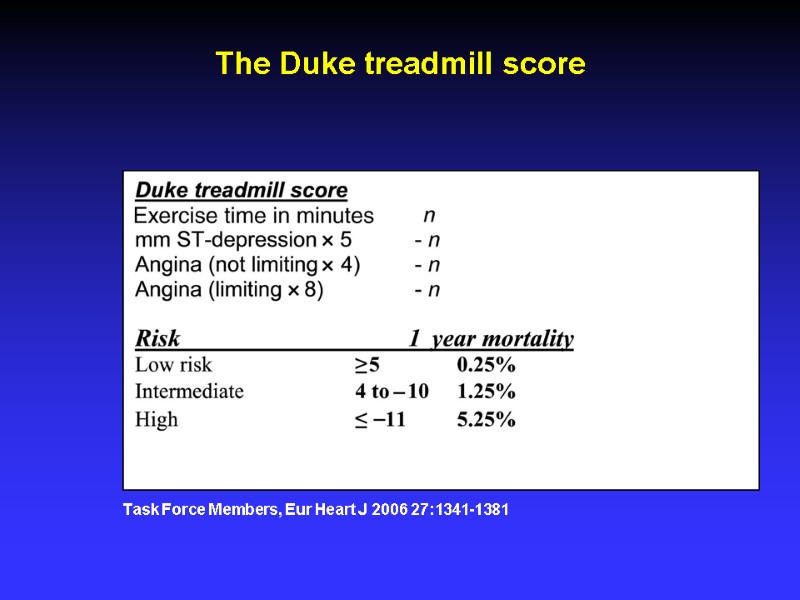 Task Force Members, Eur Heart J 2006 27:1341-1381 The Duke treadmill score
Task Force Members, Eur Heart J 2006 27:1341-1381 The Duke treadmill score
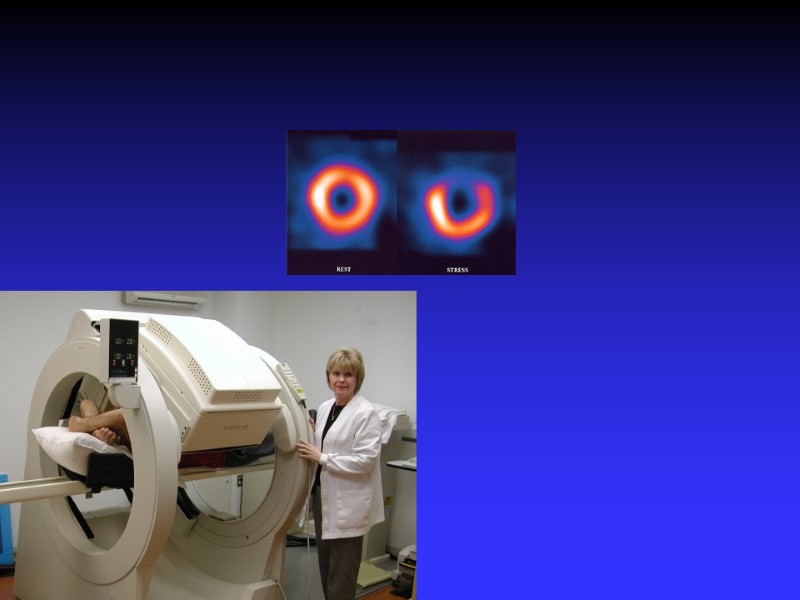
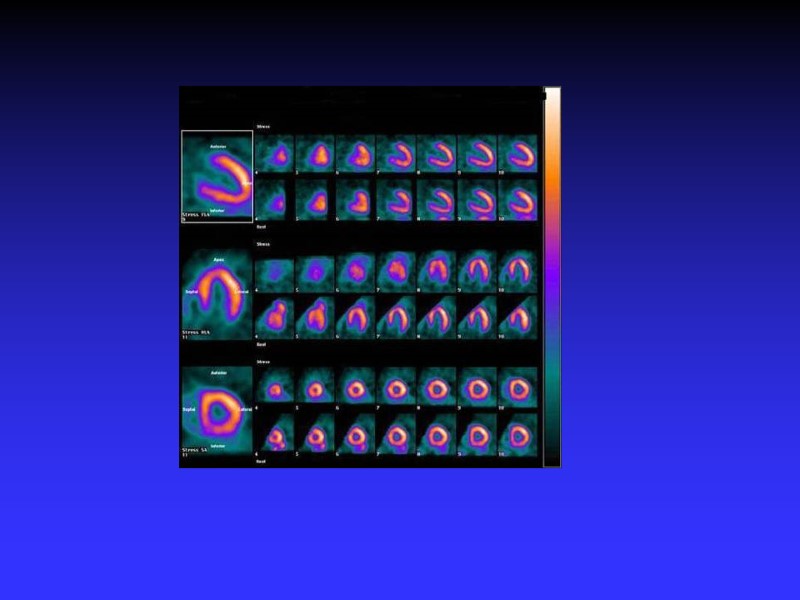
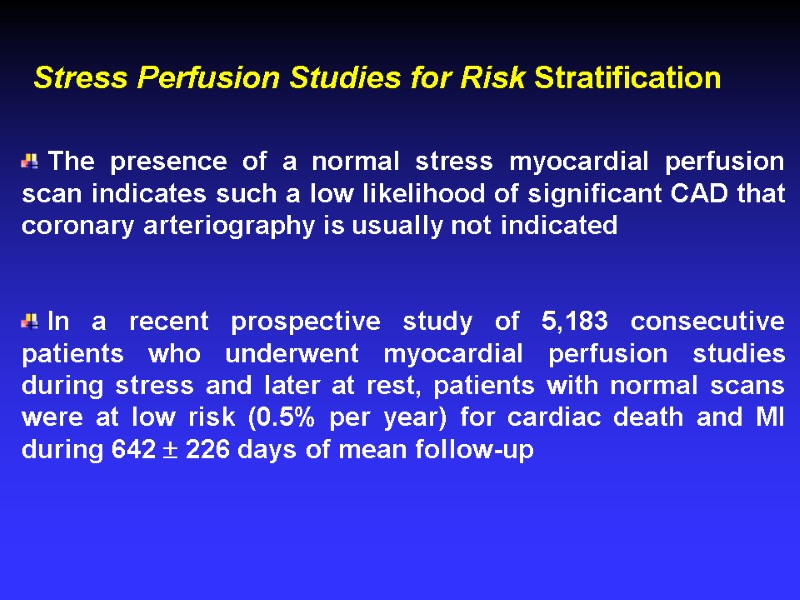
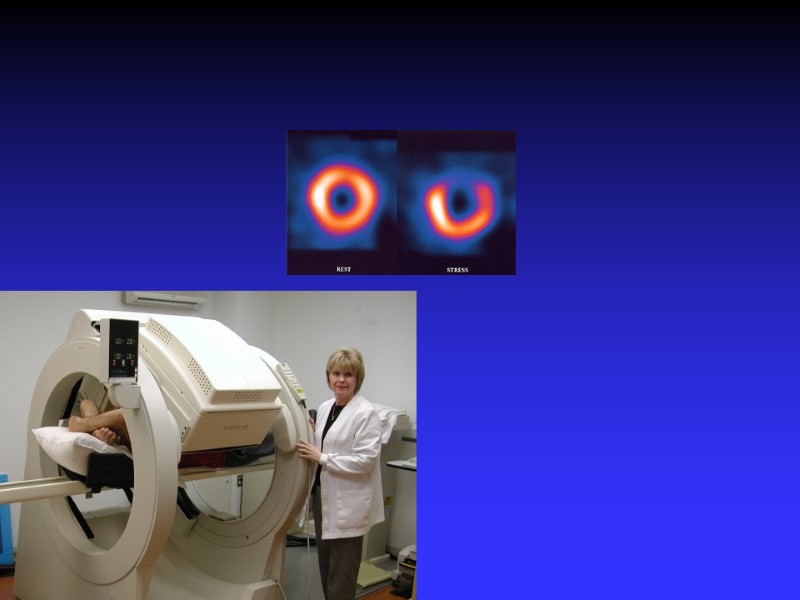
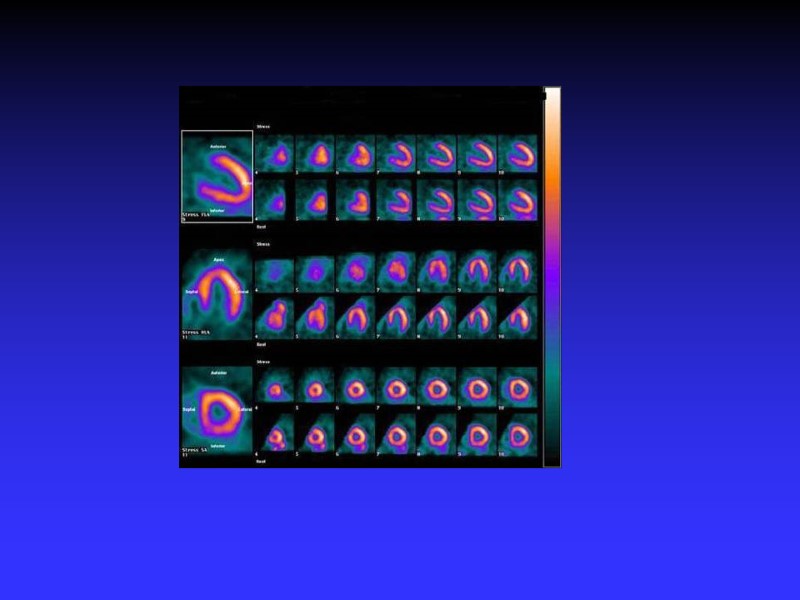
 The presence of a normal stress myocardial perfusion scan indicates such a low likelihood of significant CAD that coronary arteriography is usually not indicated In a recent prospective study of 5,183 consecutive patients who underwent myocardial perfusion studies during stress and later at rest, patients with normal scans were at low risk (0.5% per year) for cardiac death and MI during 642 226 days of mean follow-up Stress Perfusion Studies for Risk Stratification
The presence of a normal stress myocardial perfusion scan indicates such a low likelihood of significant CAD that coronary arteriography is usually not indicated In a recent prospective study of 5,183 consecutive patients who underwent myocardial perfusion studies during stress and later at rest, patients with normal scans were at low risk (0.5% per year) for cardiac death and MI during 642 226 days of mean follow-up Stress Perfusion Studies for Risk Stratification
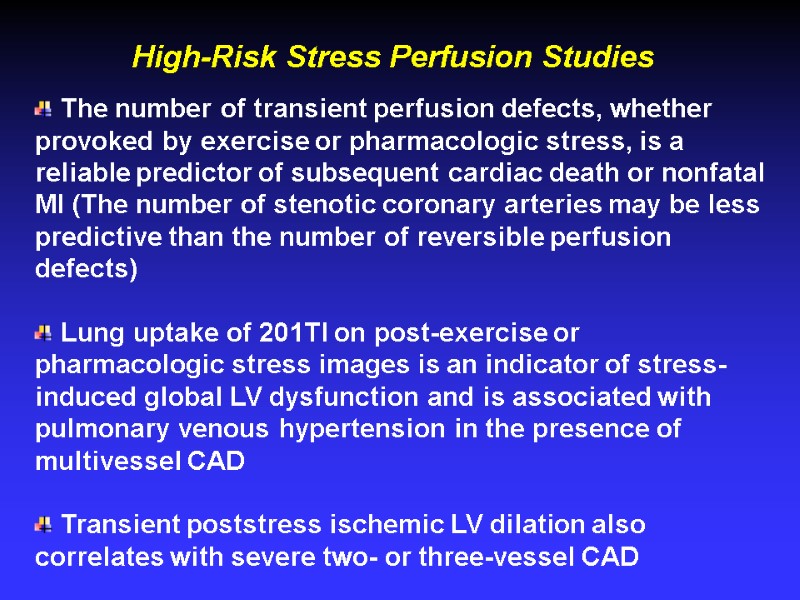
 High-Risk Stress Perfusion Studies The number of transient perfusion defects, whether provoked by exercise or pharmacologic stress, is a reliable predictor of subsequent cardiac death or nonfatal MI (The number of stenotic coronary arteries may be less predictive than the number of reversible perfusion defects) Lung uptake of 201Tl on post-exercise or pharmacologic stress images is an indicator of stress-induced global LV dysfunction and is associated with pulmonary venous hypertension in the presence of multivessel CAD Transient poststress ischemic LV dilation also correlates with severe two- or three-vessel CAD
High-Risk Stress Perfusion Studies The number of transient perfusion defects, whether provoked by exercise or pharmacologic stress, is a reliable predictor of subsequent cardiac death or nonfatal MI (The number of stenotic coronary arteries may be less predictive than the number of reversible perfusion defects) Lung uptake of 201Tl on post-exercise or pharmacologic stress images is an indicator of stress-induced global LV dysfunction and is associated with pulmonary venous hypertension in the presence of multivessel CAD Transient poststress ischemic LV dilation also correlates with severe two- or three-vessel CAD
 Symptomatic patients with suspected or known CAD should usually undergo exercise testing to assess the risk of future cardiac events unless they have confounding features on the rest ECG. Furthermore, documentation of exercise-induced ischemia is desirable for most patients who are being evaluated for revascularization. Determination of CAD Severity
Symptomatic patients with suspected or known CAD should usually undergo exercise testing to assess the risk of future cardiac events unless they have confounding features on the rest ECG. Furthermore, documentation of exercise-induced ischemia is desirable for most patients who are being evaluated for revascularization. Determination of CAD Severity
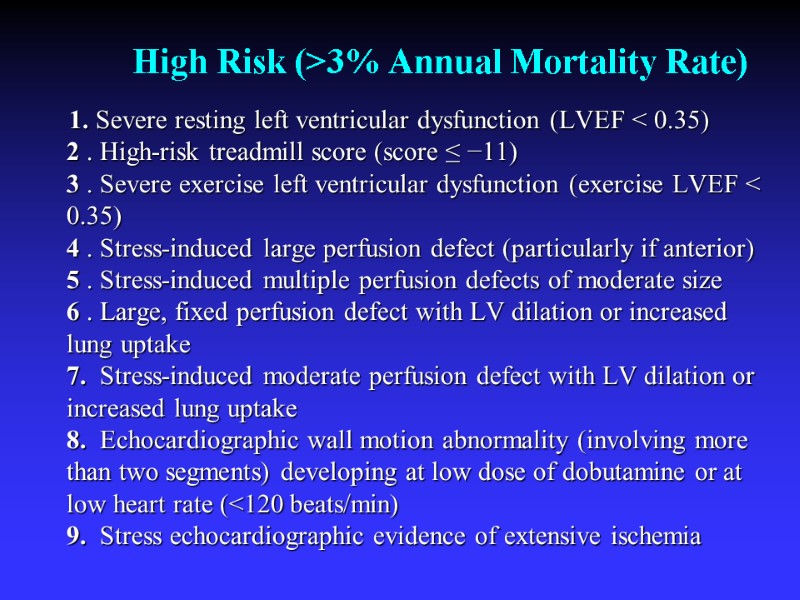
 High Risk (>3% Annual Mortality Rate) 1. Severe resting left ventricular dysfunction (LVEF < 0.35) 2 . High-risk treadmill score (score ≤ −11) 3 . Severe exercise left ventricular dysfunction (exercise LVEF < 0.35) 4 . Stress-induced large perfusion defect (particularly if anterior) 5 . Stress-induced multiple perfusion defects of moderate size 6 . Large, fixed perfusion defect with LV dilation or increased lung uptake 7. Stress-induced moderate perfusion defect with LV dilation or increased lung uptake 8. Echocardiographic wall motion abnormality (involving more than two segments) developing at low dose of dobutamine or at low heart rate (<120 beats/min) 9. Stress echocardiographic evidence of extensive ischemia
High Risk (>3% Annual Mortality Rate) 1. Severe resting left ventricular dysfunction (LVEF < 0.35) 2 . High-risk treadmill score (score ≤ −11) 3 . Severe exercise left ventricular dysfunction (exercise LVEF < 0.35) 4 . Stress-induced large perfusion defect (particularly if anterior) 5 . Stress-induced multiple perfusion defects of moderate size 6 . Large, fixed perfusion defect with LV dilation or increased lung uptake 7. Stress-induced moderate perfusion defect with LV dilation or increased lung uptake 8. Echocardiographic wall motion abnormality (involving more than two segments) developing at low dose of dobutamine or at low heart rate (<120 beats/min) 9. Stress echocardiographic evidence of extensive ischemia
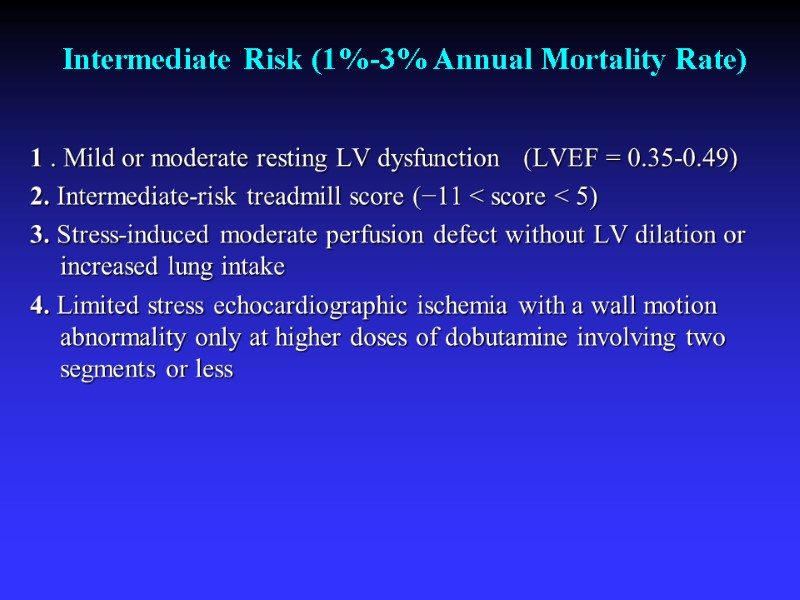
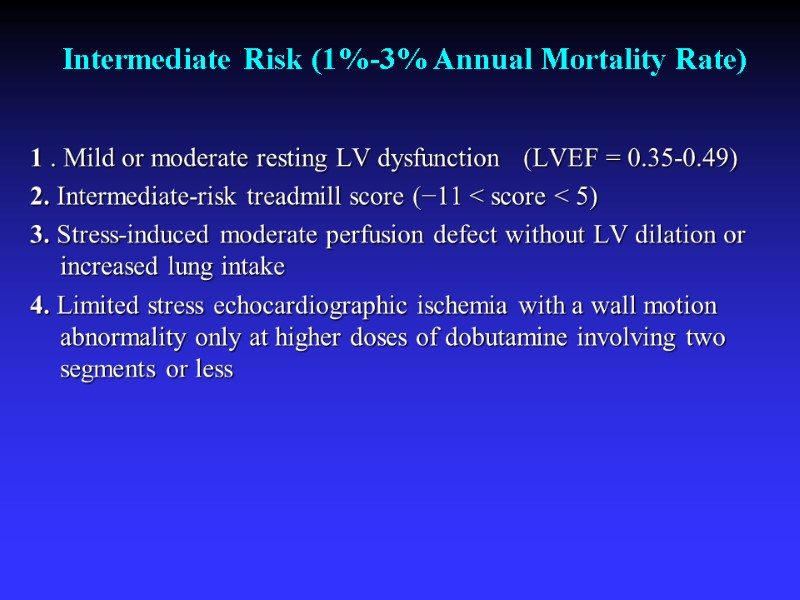 Intermediate Risk (1%-3% Annual Mortality Rate) 1 . Mild or moderate resting LV dysfunction (LVEF = 0.35-0.49) 2. Intermediate-risk treadmill score (−11 < score < 5) 3. Stress-induced moderate perfusion defect without LV dilation or increased lung intake 4. Limited stress echocardiographic ischemia with a wall motion abnormality only at higher doses of dobutamine involving two segments or less
Intermediate Risk (1%-3% Annual Mortality Rate) 1 . Mild or moderate resting LV dysfunction (LVEF = 0.35-0.49) 2. Intermediate-risk treadmill score (−11 < score < 5) 3. Stress-induced moderate perfusion defect without LV dilation or increased lung intake 4. Limited stress echocardiographic ischemia with a wall motion abnormality only at higher doses of dobutamine involving two segments or less
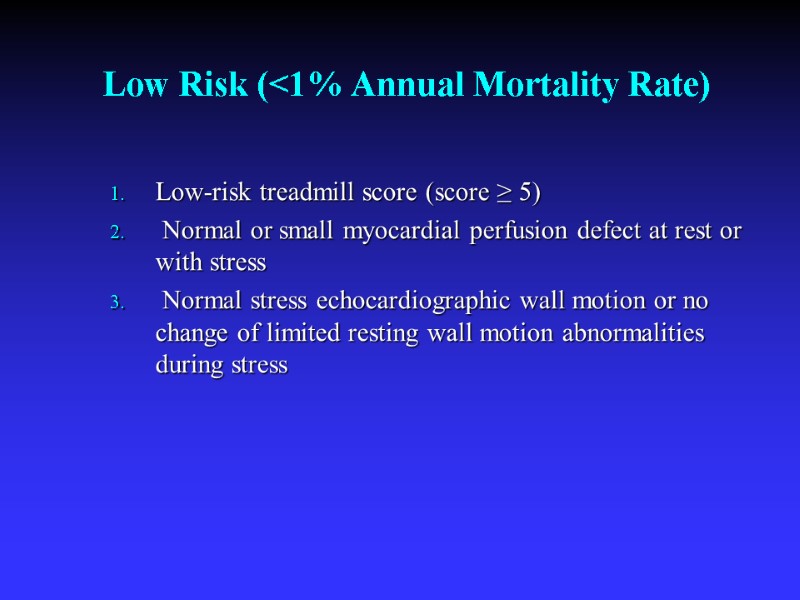
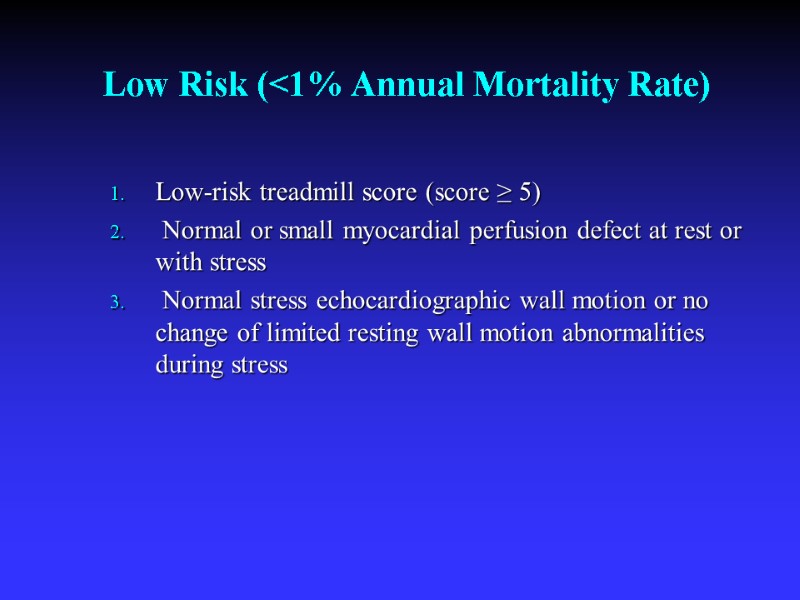 Low Risk (<1% Annual Mortality Rate) Low-risk treadmill score (score ≥ 5) Normal or small myocardial perfusion defect at rest or with stress Normal stress echocardiographic wall motion or no change of limited resting wall motion abnormalities during stress
Low Risk (<1% Annual Mortality Rate) Low-risk treadmill score (score ≥ 5) Normal or small myocardial perfusion defect at rest or with stress Normal stress echocardiographic wall motion or no change of limited resting wall motion abnormalities during stress
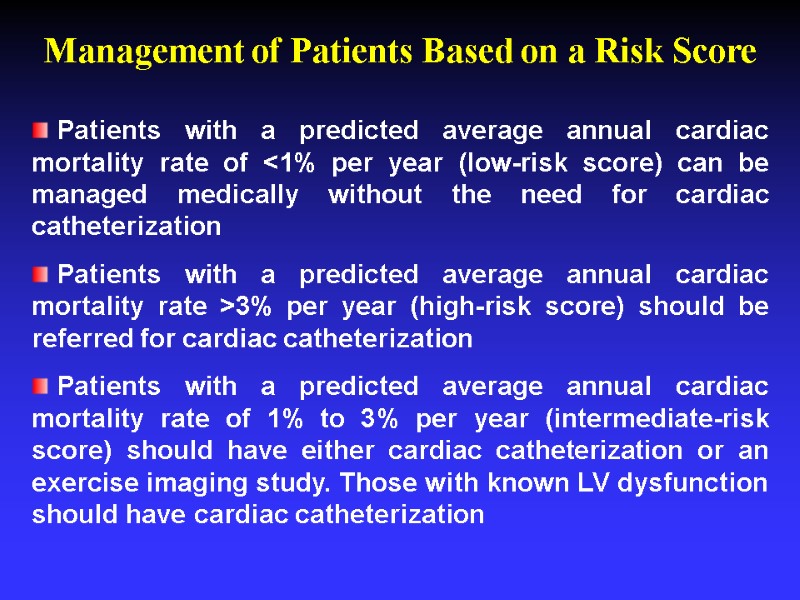
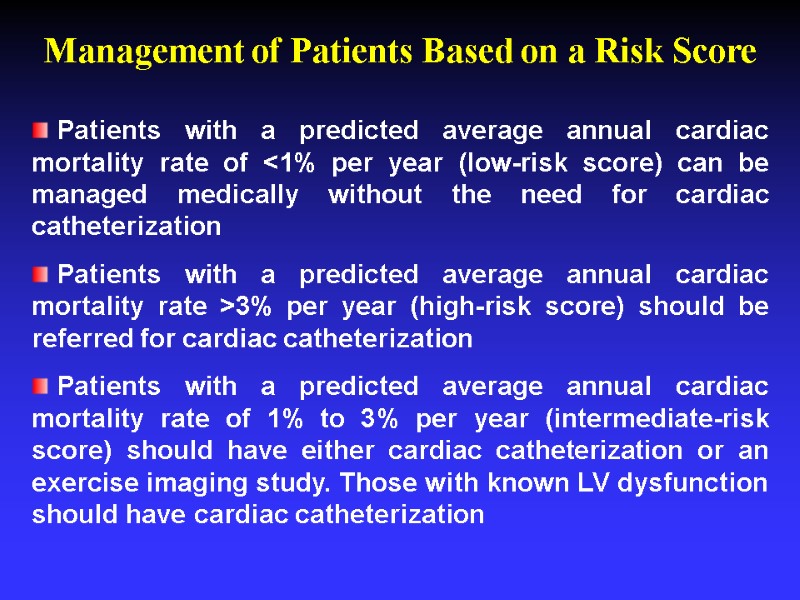 Patients with a predicted average annual cardiac mortality rate of <1% per year (low-risk score) can be managed medically without the need for cardiac catheterization Patients with a predicted average annual cardiac mortality rate >3% per year (high-risk score) should be referred for cardiac catheterization Patients with a predicted average annual cardiac mortality rate of 1% to 3% per year (intermediate-risk score) should have either cardiac catheterization or an exercise imaging study. Those with known LV dysfunction should have cardiac catheterization Management of Patients Based on a Risk Score
Patients with a predicted average annual cardiac mortality rate of <1% per year (low-risk score) can be managed medically without the need for cardiac catheterization Patients with a predicted average annual cardiac mortality rate >3% per year (high-risk score) should be referred for cardiac catheterization Patients with a predicted average annual cardiac mortality rate of 1% to 3% per year (intermediate-risk score) should have either cardiac catheterization or an exercise imaging study. Those with known LV dysfunction should have cardiac catheterization Management of Patients Based on a Risk Score
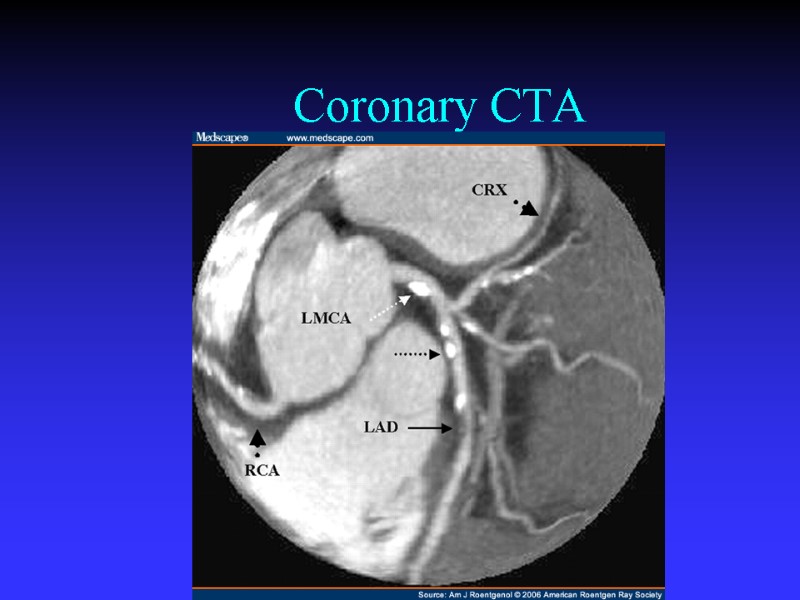
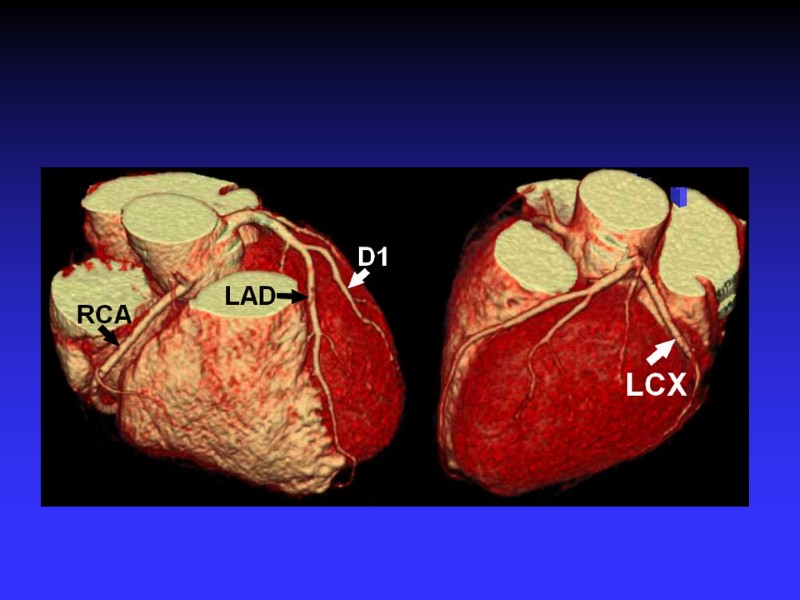
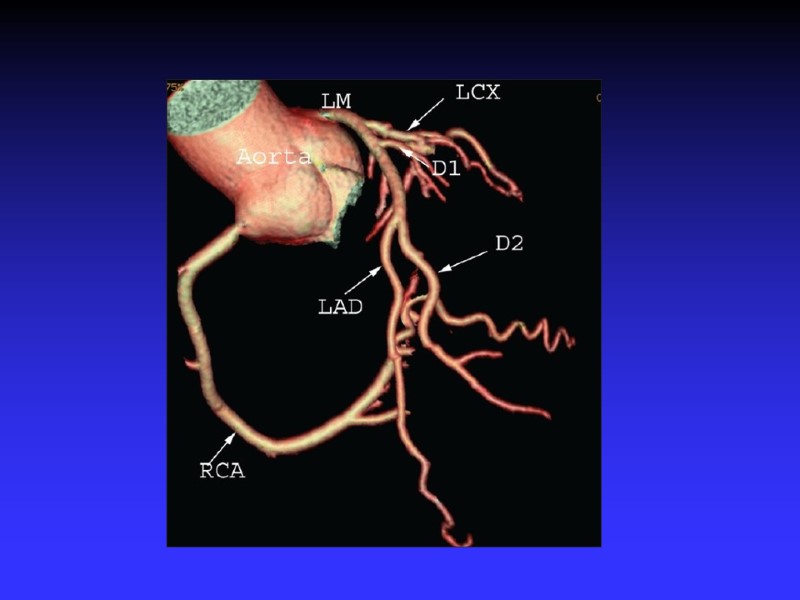
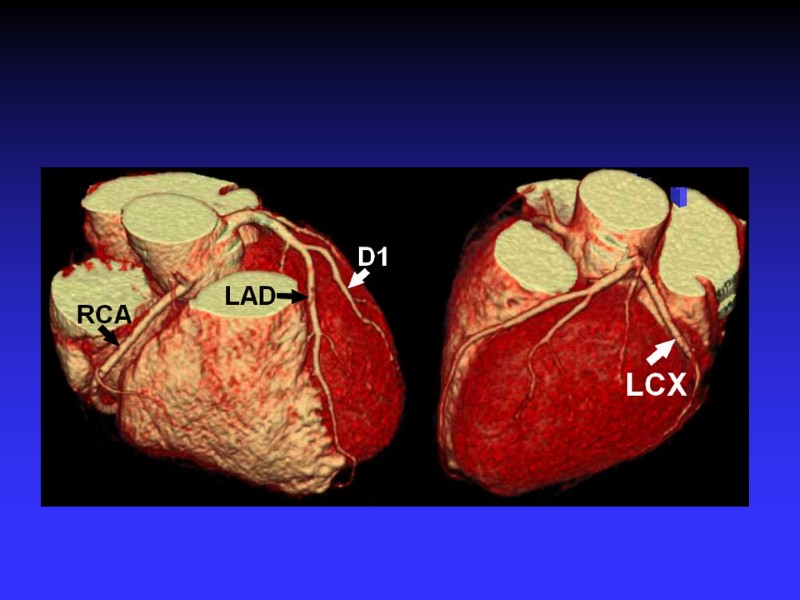
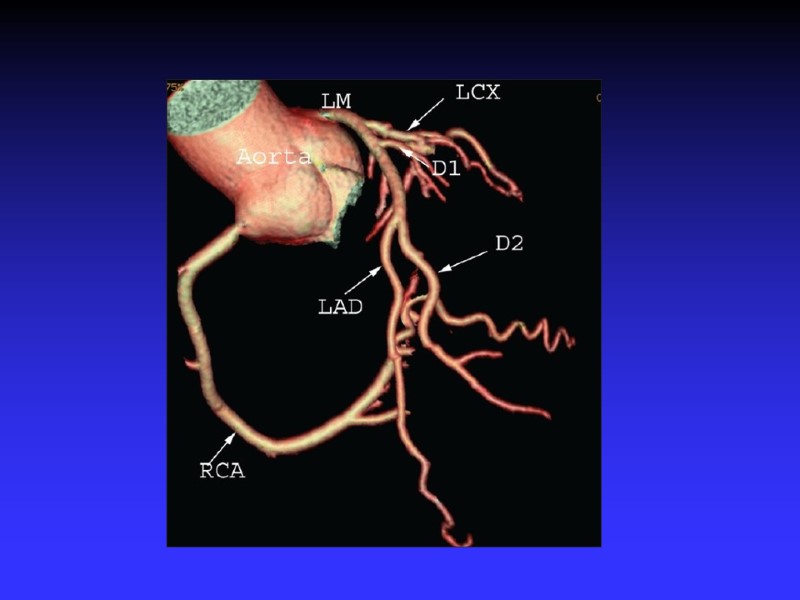
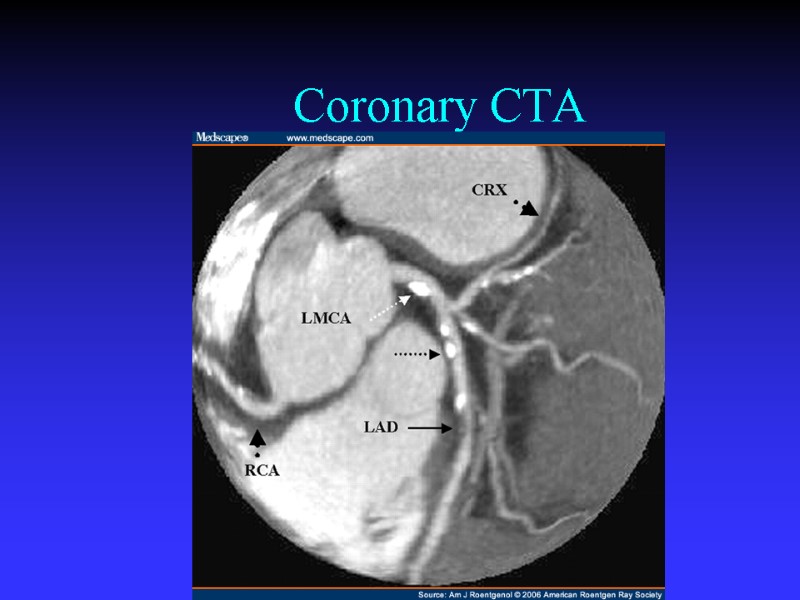 Coronary CTA
Coronary CTA

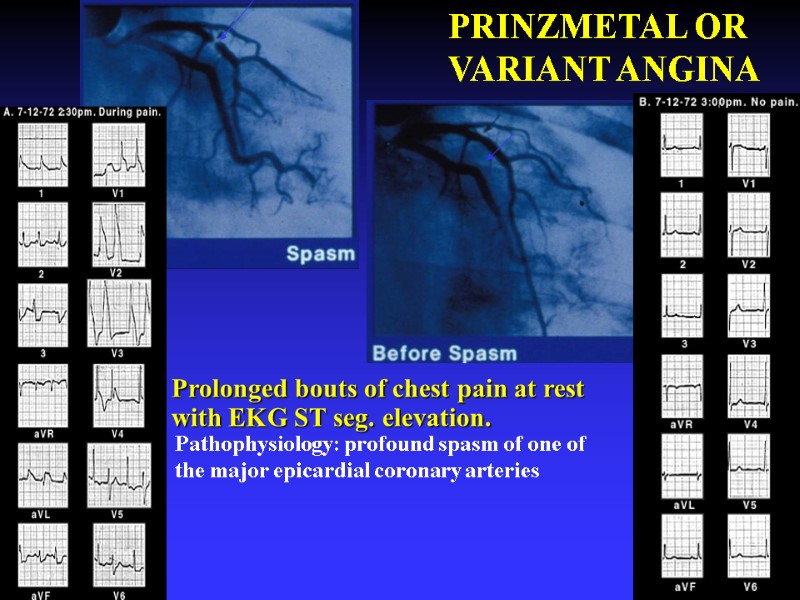
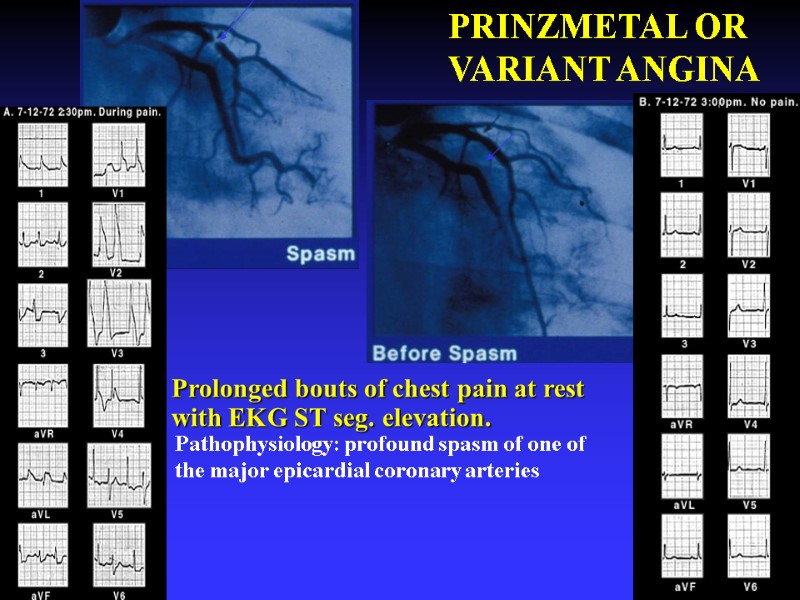 46 Prolonged bouts of chest pain at rest with EKG ST seg. elevation. PRINZMETAL OR VARIANT ANGINA Pathophysiology: profound spasm of one of the major epicardial coronary arteries
46 Prolonged bouts of chest pain at rest with EKG ST seg. elevation. PRINZMETAL OR VARIANT ANGINA Pathophysiology: profound spasm of one of the major epicardial coronary arteries
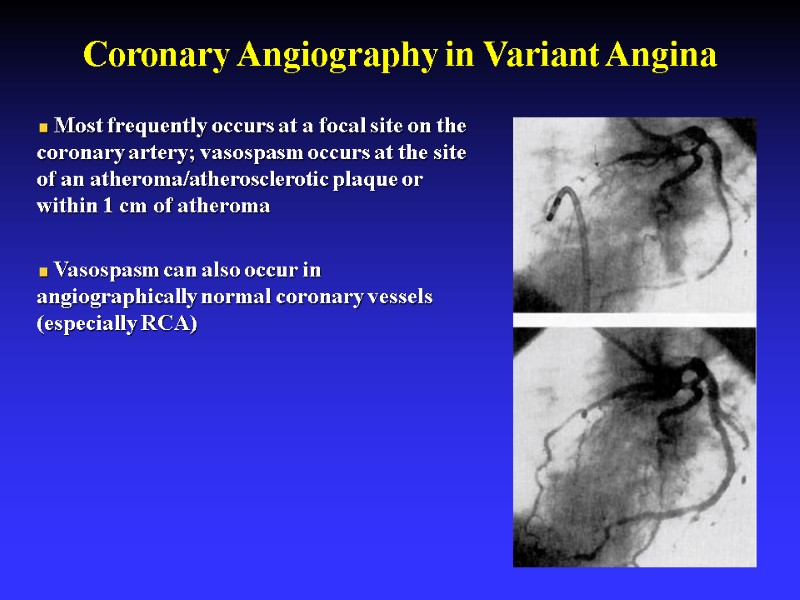
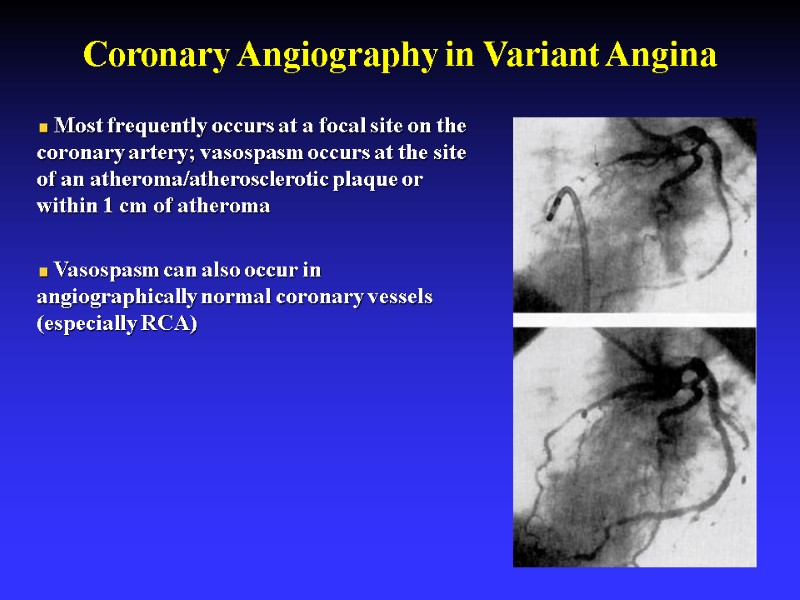 Coronary Angiography in Variant Angina Most frequently occurs at a focal site on the coronary artery; vasospasm occurs at the site of an atheroma/atherosclerotic plaque or within 1 cm of atheroma Vasospasm can also occur in angiographically normal coronary vessels (especially RCA)
Coronary Angiography in Variant Angina Most frequently occurs at a focal site on the coronary artery; vasospasm occurs at the site of an atheroma/atherosclerotic plaque or within 1 cm of atheroma Vasospasm can also occur in angiographically normal coronary vessels (especially RCA)
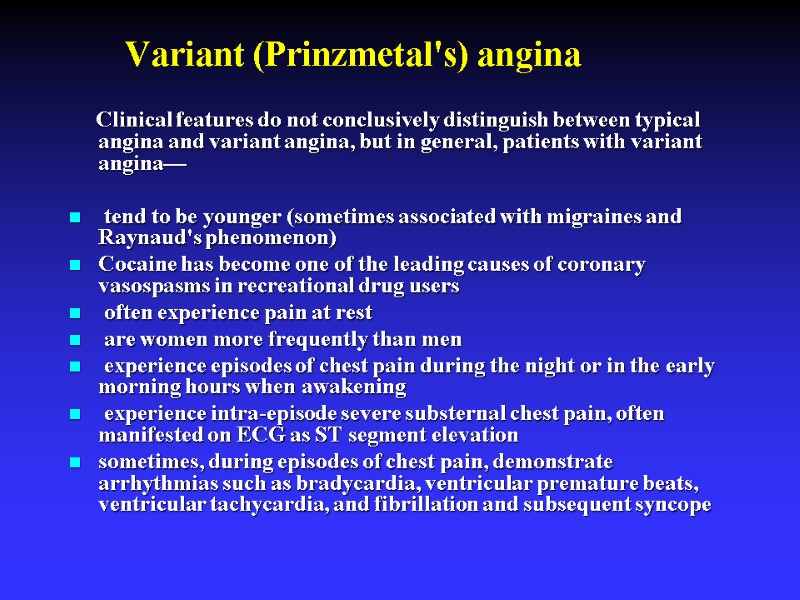 Clinical features do not conclusively distinguish between typical angina and variant angina, but in general, patients with variant angina— tend to be younger (sometimes associated with migraines and Raynaud's phenomenon) Cocaine has become one of the leading causes of coronary vasospasms in recreational drug users often experience pain at rest are women more frequently than men experience episodes of chest pain during the night or in the early morning hours when awakening experience intra-episode severe substernal chest pain, often manifested on ECG as ST segment elevation sometimes, during episodes of chest pain, demonstrate arrhythmias such as bradycardia, ventricular premature beats, ventricular tachycardia, and fibrillation and subsequent syncope Variant (Prinzmetal's) angina
Clinical features do not conclusively distinguish between typical angina and variant angina, but in general, patients with variant angina— tend to be younger (sometimes associated with migraines and Raynaud's phenomenon) Cocaine has become one of the leading causes of coronary vasospasms in recreational drug users often experience pain at rest are women more frequently than men experience episodes of chest pain during the night or in the early morning hours when awakening experience intra-episode severe substernal chest pain, often manifested on ECG as ST segment elevation sometimes, during episodes of chest pain, demonstrate arrhythmias such as bradycardia, ventricular premature beats, ventricular tachycardia, and fibrillation and subsequent syncope Variant (Prinzmetal's) angina
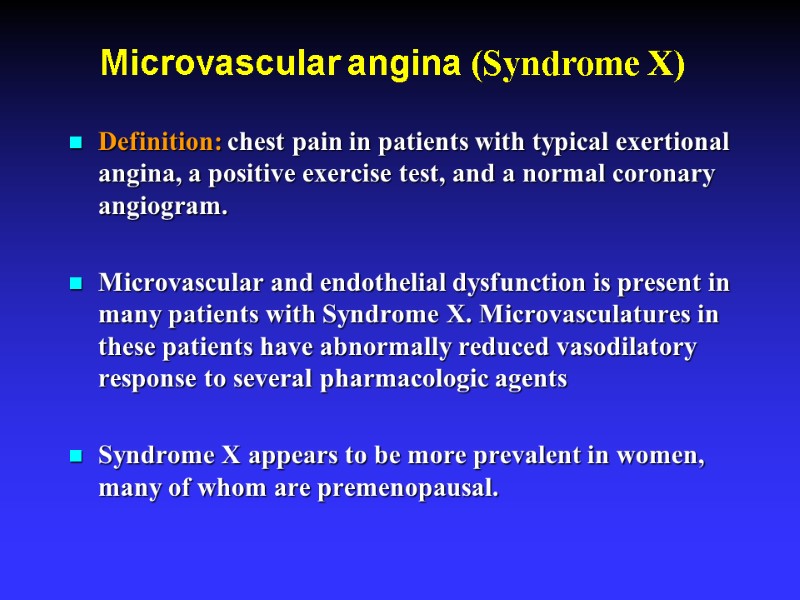 Microvascular angina (Syndrome X) Definition: chest pain in patients with typical exertional angina, a positive exercise test, and a normal coronary angiogram. Microvascular and endothelial dysfunction is present in many patients with Syndrome X. Microvasculatures in these patients have abnormally reduced vasodilatory response to several pharmacologic agents Syndrome X appears to be more prevalent in women, many of whom are premenopausal.
Microvascular angina (Syndrome X) Definition: chest pain in patients with typical exertional angina, a positive exercise test, and a normal coronary angiogram. Microvascular and endothelial dysfunction is present in many patients with Syndrome X. Microvasculatures in these patients have abnormally reduced vasodilatory response to several pharmacologic agents Syndrome X appears to be more prevalent in women, many of whom are premenopausal.
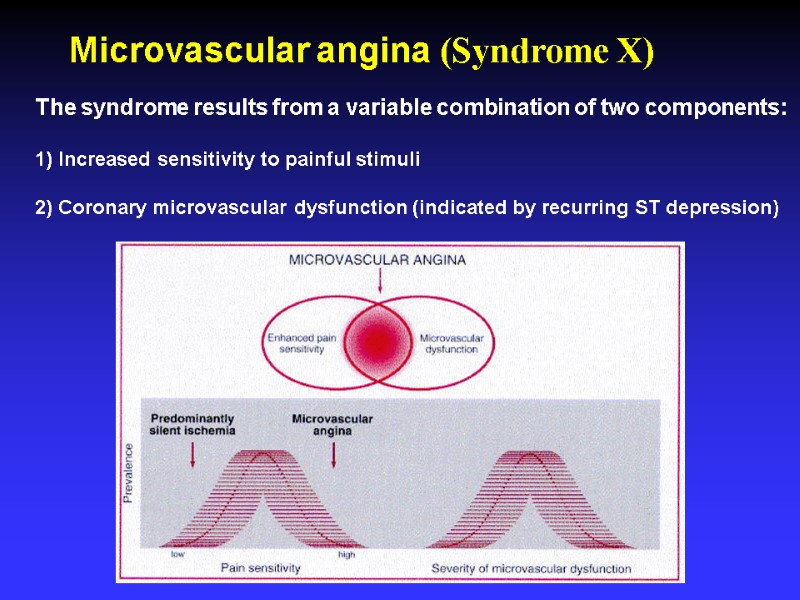
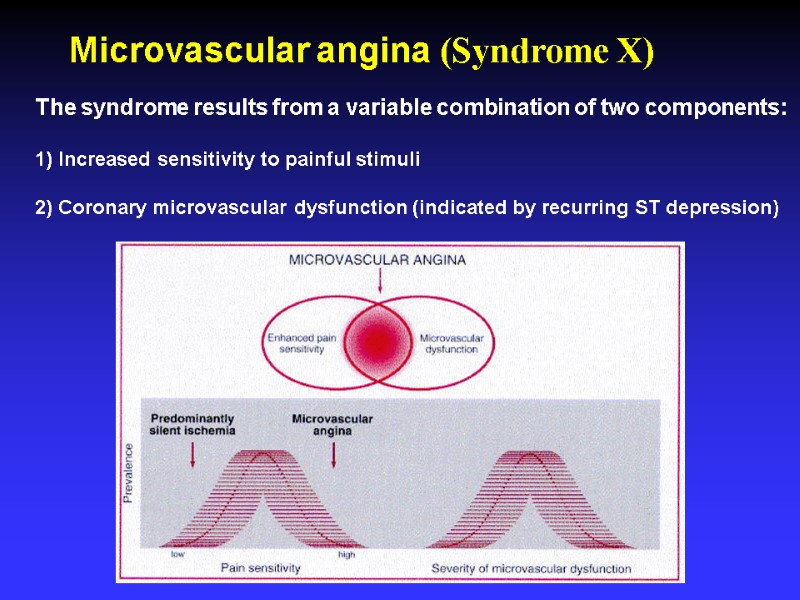 Microvascular angina (Syndrome X) The syndrome results from a variable combination of two components: 1) Increased sensitivity to painful stimuli 2) Coronary microvascular dysfunction (indicated by recurring ST depression)
Microvascular angina (Syndrome X) The syndrome results from a variable combination of two components: 1) Increased sensitivity to painful stimuli 2) Coronary microvascular dysfunction (indicated by recurring ST depression)
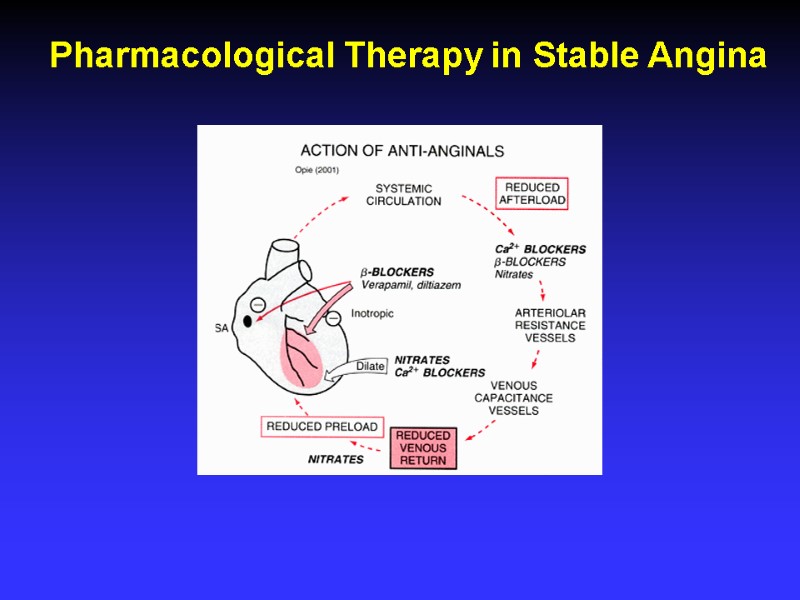
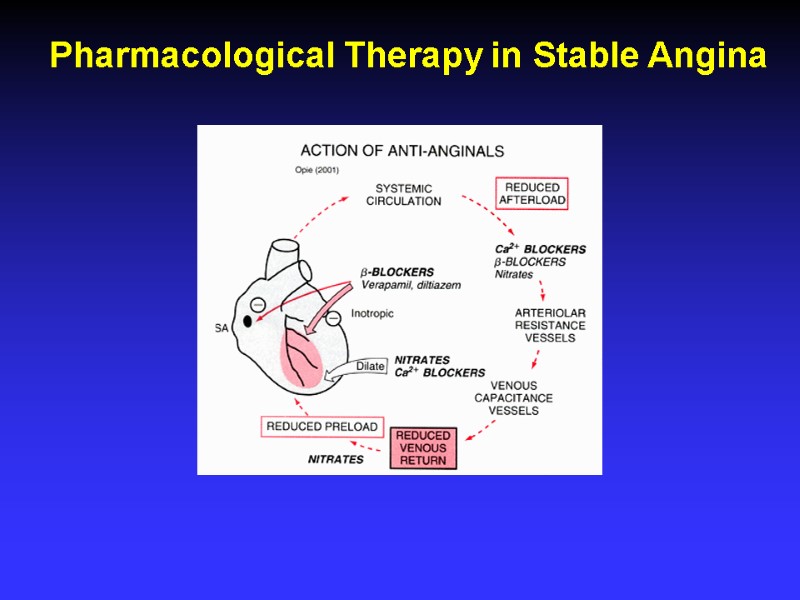 Pharmacological Therapy in Stable Angina
Pharmacological Therapy in Stable Angina
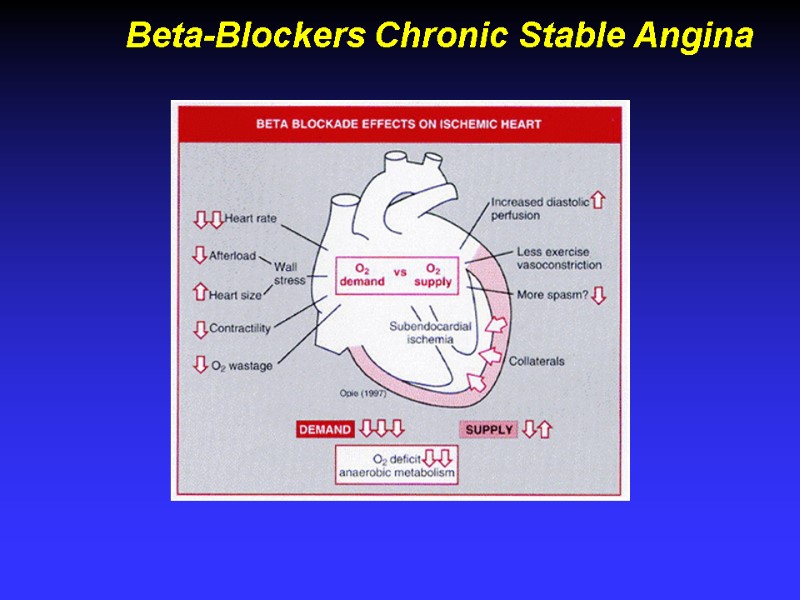
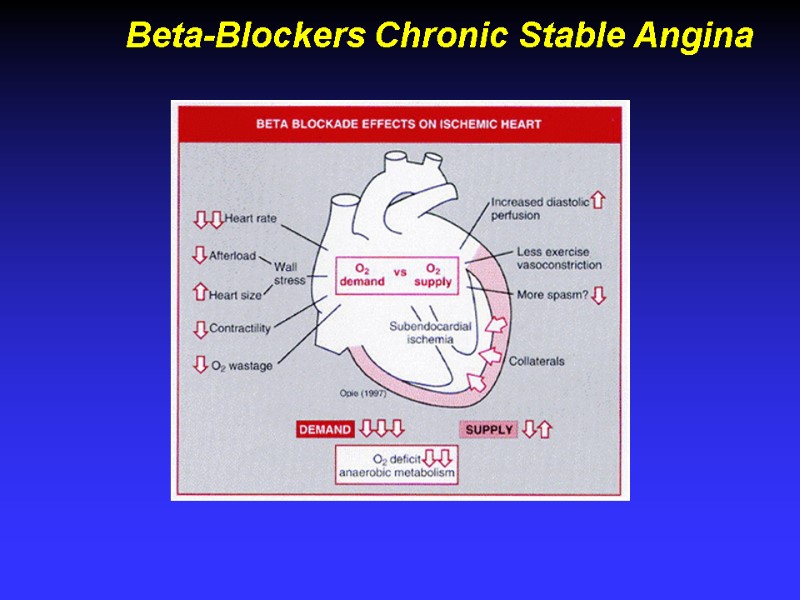 Beta-Blockers Chronic Stable Angina
Beta-Blockers Chronic Stable Angina
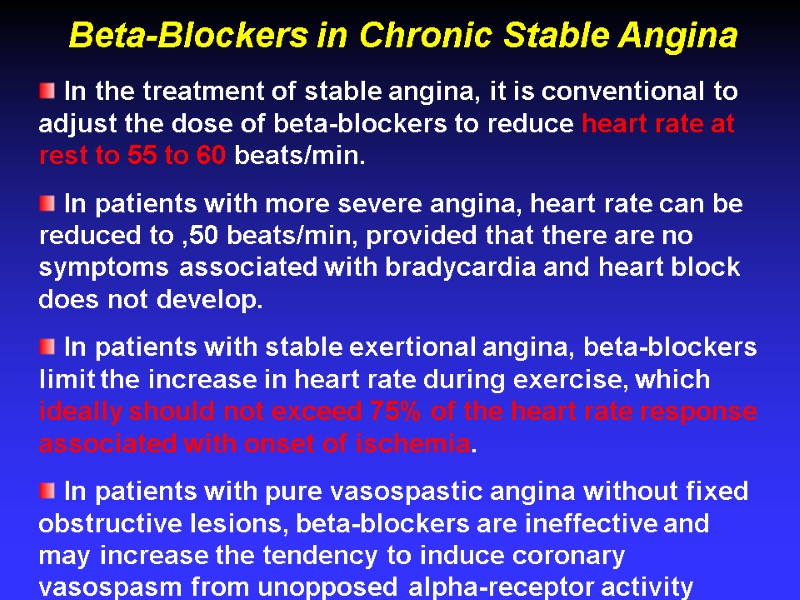
 In the treatment of stable angina, it is conventional to adjust the dose of beta-blockers to reduce heart rate at rest to 55 to 60 beats/min. In patients with more severe angina, heart rate can be reduced to ,50 beats/min, provided that there are no symptoms associated with bradycardia and heart block does not develop. In patients with stable exertional angina, beta-blockers limit the increase in heart rate during exercise, which ideally should not exceed 75% of the heart rate response associated with onset of ischemia. In patients with pure vasospastic angina without fixed obstructive lesions, beta-blockers are ineffective and may increase the tendency to induce coronary vasospasm from unopposed alpha-receptor activity Beta-Blockers in Chronic Stable Angina
In the treatment of stable angina, it is conventional to adjust the dose of beta-blockers to reduce heart rate at rest to 55 to 60 beats/min. In patients with more severe angina, heart rate can be reduced to ,50 beats/min, provided that there are no symptoms associated with bradycardia and heart block does not develop. In patients with stable exertional angina, beta-blockers limit the increase in heart rate during exercise, which ideally should not exceed 75% of the heart rate response associated with onset of ischemia. In patients with pure vasospastic angina without fixed obstructive lesions, beta-blockers are ineffective and may increase the tendency to induce coronary vasospasm from unopposed alpha-receptor activity Beta-Blockers in Chronic Stable Angina
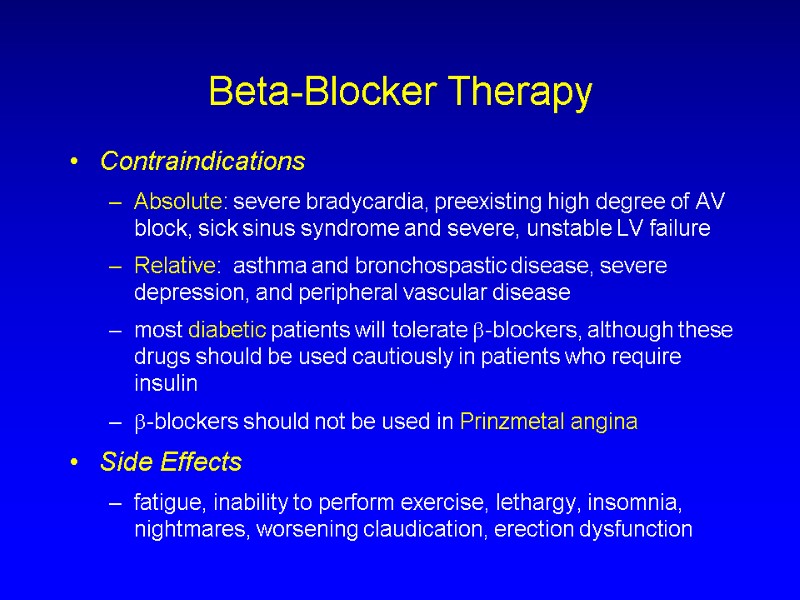
 Beta-Blocker Therapy Contraindications Absolute: severe bradycardia, preexisting high degree of AV block, sick sinus syndrome and severe, unstable LV failure Relative: asthma and bronchospastic disease, severe depression, and peripheral vascular disease most diabetic patients will tolerate -blockers, although these drugs should be used cautiously in patients who require insulin -blockers should not be used in Prinzmetal angina Side Effects fatigue, inability to perform exercise, lethargy, insomnia, nightmares, worsening claudication, erection dysfunction
Beta-Blocker Therapy Contraindications Absolute: severe bradycardia, preexisting high degree of AV block, sick sinus syndrome and severe, unstable LV failure Relative: asthma and bronchospastic disease, severe depression, and peripheral vascular disease most diabetic patients will tolerate -blockers, although these drugs should be used cautiously in patients who require insulin -blockers should not be used in Prinzmetal angina Side Effects fatigue, inability to perform exercise, lethargy, insomnia, nightmares, worsening claudication, erection dysfunction
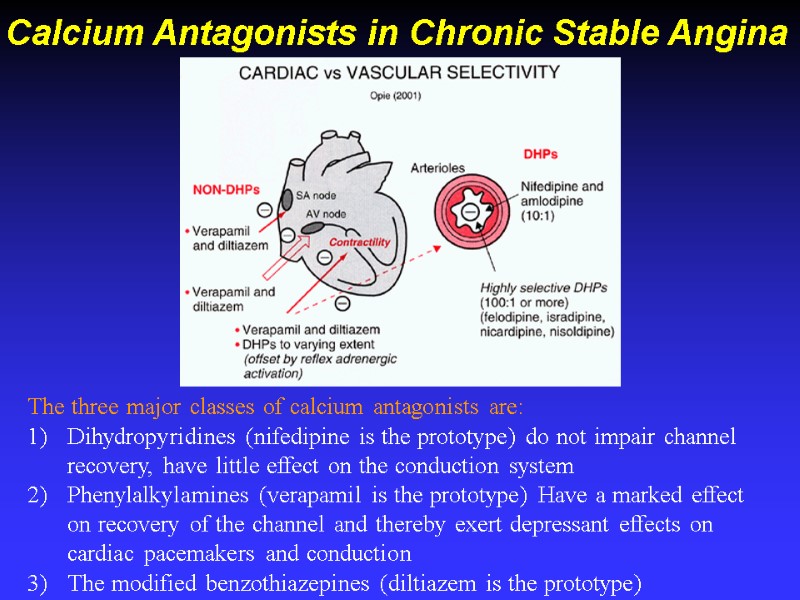
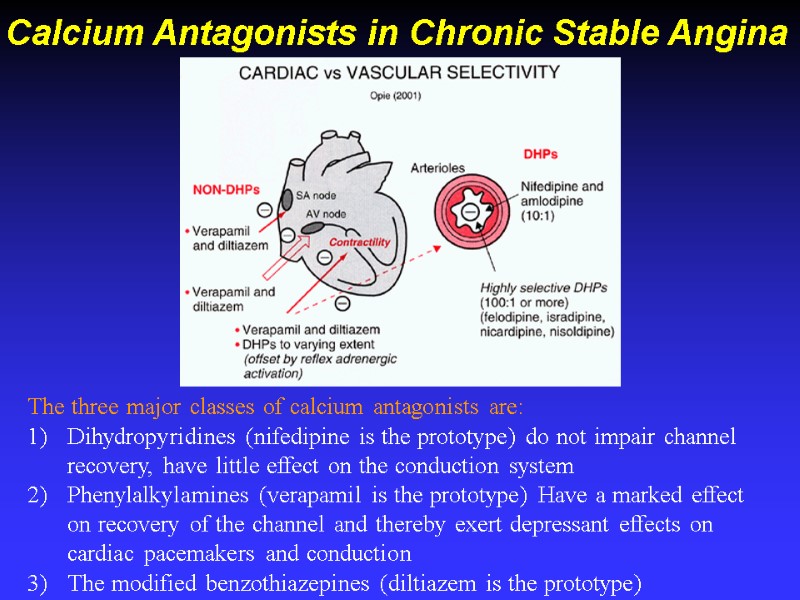 Calcium Antagonists in Chronic Stable Angina The three major classes of calcium antagonists are: Dihydropyridines (nifedipine is the prototype) do not impair channel recovery, have little effect on the conduction system Phenylalkylamines (verapamil is the prototype) Have a marked effect on recovery of the channel and thereby exert depressant effects on cardiac pacemakers and conduction The modified benzothiazepines (diltiazem is the prototype)
Calcium Antagonists in Chronic Stable Angina The three major classes of calcium antagonists are: Dihydropyridines (nifedipine is the prototype) do not impair channel recovery, have little effect on the conduction system Phenylalkylamines (verapamil is the prototype) Have a marked effect on recovery of the channel and thereby exert depressant effects on cardiac pacemakers and conduction The modified benzothiazepines (diltiazem is the prototype)
 Randomized clinical trials comparing calcium antagonists and beta blockers have demonstrated that calcium antagonists are generally equally as effective as beta-blockers in relieving angina and improving exercise time to onset of angina or ischemia. The clinical effectiveness of calcium antagonists was evident with both dihydropyridine and nondihydropyridine agents and various dosing regimens. In patients with vasospastic angina, calcium antagonists have been shown to be effective in reducing the incidence of angina. Short-acting nifedipine, diltiazem, and verapamil all appeared to completely abolish the recurrence of angina in approximately 70% of patients; in another 20% of patients, the frequency of angina was reduced substantially. Calcium Antagonists in Stable Angina
Randomized clinical trials comparing calcium antagonists and beta blockers have demonstrated that calcium antagonists are generally equally as effective as beta-blockers in relieving angina and improving exercise time to onset of angina or ischemia. The clinical effectiveness of calcium antagonists was evident with both dihydropyridine and nondihydropyridine agents and various dosing regimens. In patients with vasospastic angina, calcium antagonists have been shown to be effective in reducing the incidence of angina. Short-acting nifedipine, diltiazem, and verapamil all appeared to completely abolish the recurrence of angina in approximately 70% of patients; in another 20% of patients, the frequency of angina was reduced substantially. Calcium Antagonists in Stable Angina
 Ca channel blocker or beta blocker ? Calcium antagonists are the preferred agents in patients with a history of asthma or chronic obstructive lung disease with wheezing on clinical examination, in whom beta blockers, even relatively selective agents, are contraindicated. Consideration to a trial of beta blockers should be given if the patient has a history of prior MI. Calcium antagonists are clearly preferred for patients with suspected Prinzmetal (variant) angina beta blockers may even aggravate angina under these circumstances. Calcium antagonists may be preferred over beta blockers in patients with significant, symptomatic peripheral arterial disease because the latter may cause peripheral vasoconstriction. Beta blockers should usually be avoided in patients with a history of significant depressive illness and should be prescribed cautiously for patients with sexual dysfunction, sleep disturbance, nightmares, fatigue, or lethargy.
Ca channel blocker or beta blocker ? Calcium antagonists are the preferred agents in patients with a history of asthma or chronic obstructive lung disease with wheezing on clinical examination, in whom beta blockers, even relatively selective agents, are contraindicated. Consideration to a trial of beta blockers should be given if the patient has a history of prior MI. Calcium antagonists are clearly preferred for patients with suspected Prinzmetal (variant) angina beta blockers may even aggravate angina under these circumstances. Calcium antagonists may be preferred over beta blockers in patients with significant, symptomatic peripheral arterial disease because the latter may cause peripheral vasoconstriction. Beta blockers should usually be avoided in patients with a history of significant depressive illness and should be prescribed cautiously for patients with sexual dysfunction, sleep disturbance, nightmares, fatigue, or lethargy.
 Nifedipine (long-acting), amlodipine, and nicardipine are the calcium antagonists of choice in patients with chronic stable angina and sick sinus syndrome, sinus bradycardia, or significant AV conduction disturbances, whereas beta blockers and verapamil should be used only with great caution in such patients. In patients with symptomatic conduction disease, neither a beta blocker nor a calcium channel blocker should be used unless a pacemaker is in place. If a beta blocker is required in patients with asymptomatic evidence of conduction disease, pindolol, which has the greatest ISA, is useful. Short-acting nifedipine should not be used because the reflex-mediated tachycardia may aggravate ischemia.
Nifedipine (long-acting), amlodipine, and nicardipine are the calcium antagonists of choice in patients with chronic stable angina and sick sinus syndrome, sinus bradycardia, or significant AV conduction disturbances, whereas beta blockers and verapamil should be used only with great caution in such patients. In patients with symptomatic conduction disease, neither a beta blocker nor a calcium channel blocker should be used unless a pacemaker is in place. If a beta blocker is required in patients with asymptomatic evidence of conduction disease, pindolol, which has the greatest ISA, is useful. Short-acting nifedipine should not be used because the reflex-mediated tachycardia may aggravate ischemia.
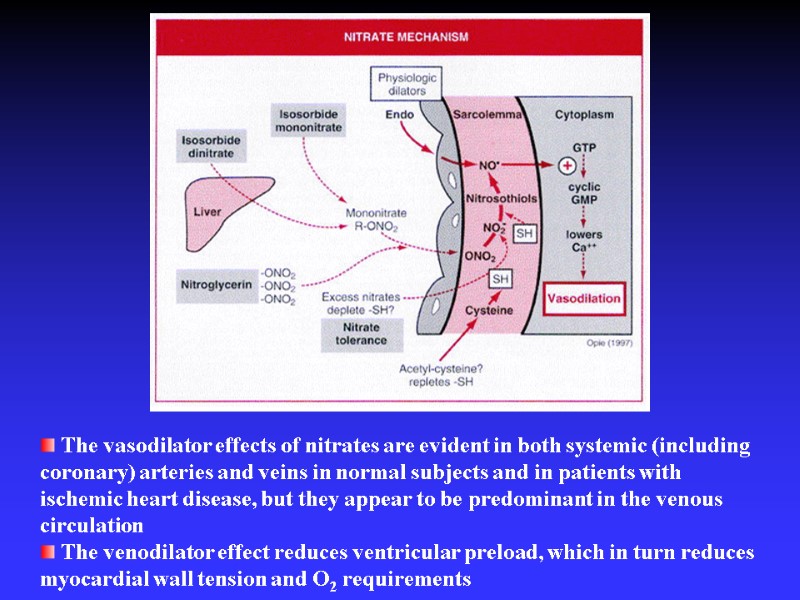
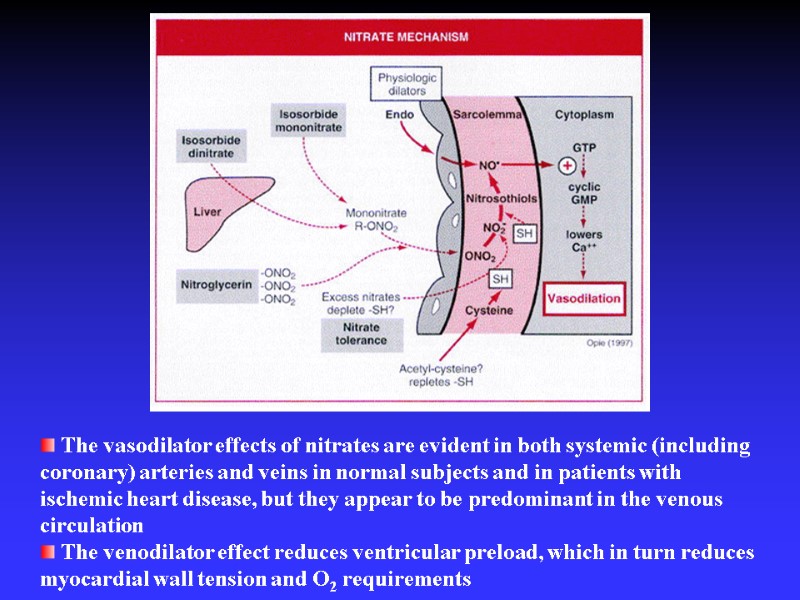 The vasodilator effects of nitrates are evident in both systemic (including coronary) arteries and veins in normal subjects and in patients with ischemic heart disease, but they appear to be predominant in the venous circulation The venodilator effect reduces ventricular preload, which in turn reduces myocardial wall tension and O2 requirements
The vasodilator effects of nitrates are evident in both systemic (including coronary) arteries and veins in normal subjects and in patients with ischemic heart disease, but they appear to be predominant in the venous circulation The venodilator effect reduces ventricular preload, which in turn reduces myocardial wall tension and O2 requirements
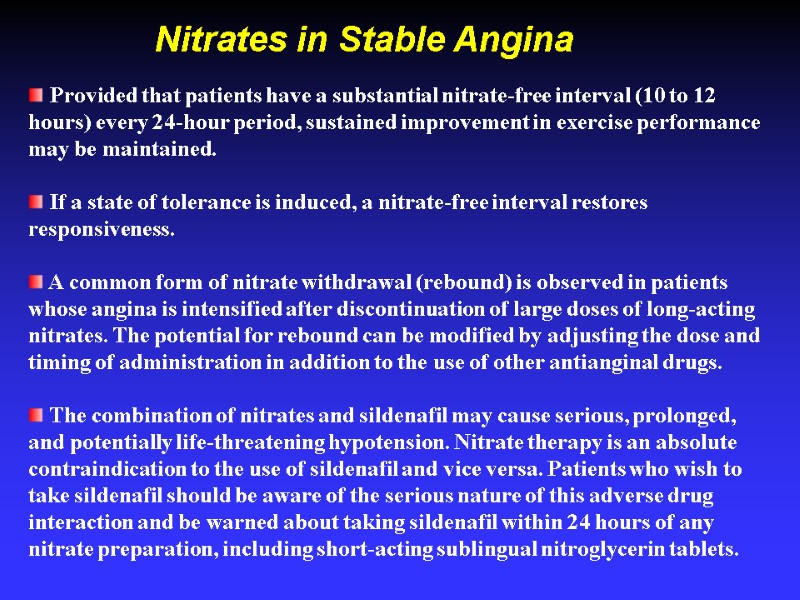
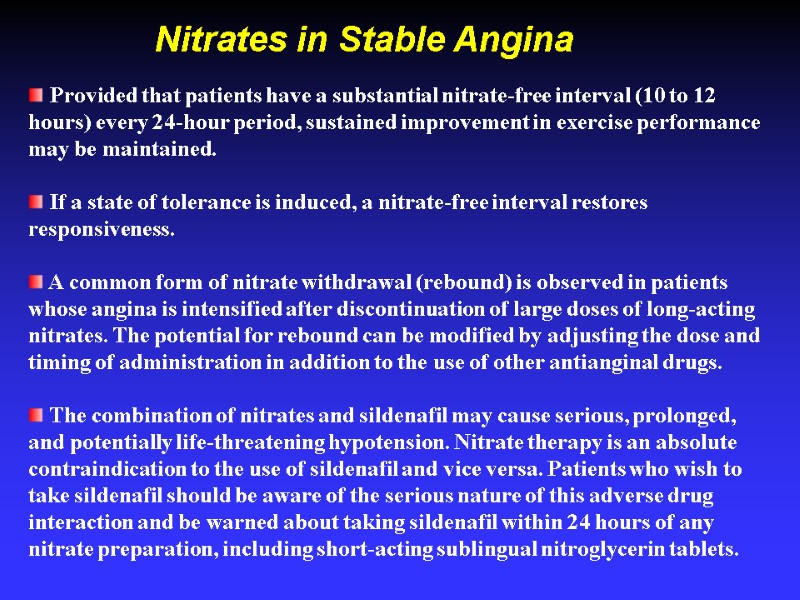 Provided that patients have a substantial nitrate-free interval (10 to 12 hours) every 24-hour period, sustained improvement in exercise performance may be maintained. If a state of tolerance is induced, a nitrate-free interval restores responsiveness. A common form of nitrate withdrawal (rebound) is observed in patients whose angina is intensified after discontinuation of large doses of long-acting nitrates. The potential for rebound can be modified by adjusting the dose and timing of administration in addition to the use of other antianginal drugs. The combination of nitrates and sildenafil may cause serious, prolonged, and potentially life-threatening hypotension. Nitrate therapy is an absolute contraindication to the use of sildenafil and vice versa. Patients who wish to take sildenafil should be aware of the serious nature of this adverse drug interaction and be warned about taking sildenafil within 24 hours of any nitrate preparation, including short-acting sublingual nitroglycerin tablets. Nitrates in Stable Angina
Provided that patients have a substantial nitrate-free interval (10 to 12 hours) every 24-hour period, sustained improvement in exercise performance may be maintained. If a state of tolerance is induced, a nitrate-free interval restores responsiveness. A common form of nitrate withdrawal (rebound) is observed in patients whose angina is intensified after discontinuation of large doses of long-acting nitrates. The potential for rebound can be modified by adjusting the dose and timing of administration in addition to the use of other antianginal drugs. The combination of nitrates and sildenafil may cause serious, prolonged, and potentially life-threatening hypotension. Nitrate therapy is an absolute contraindication to the use of sildenafil and vice versa. Patients who wish to take sildenafil should be aware of the serious nature of this adverse drug interaction and be warned about taking sildenafil within 24 hours of any nitrate preparation, including short-acting sublingual nitroglycerin tablets. Nitrates in Stable Angina
 Treatment of precipitating factors Anemia TTX Uncontrolled hypertension Tachyarrhythmias, Uncontrolled heart failure, Concomitant valvular heart disease.
Treatment of precipitating factors Anemia TTX Uncontrolled hypertension Tachyarrhythmias, Uncontrolled heart failure, Concomitant valvular heart disease.
 Risk factor modification Smoking cessation Healthy life style Diabetic control Weight loss Statins for hyperlipidemia (LDL<70mg/dl)
Risk factor modification Smoking cessation Healthy life style Diabetic control Weight loss Statins for hyperlipidemia (LDL<70mg/dl)
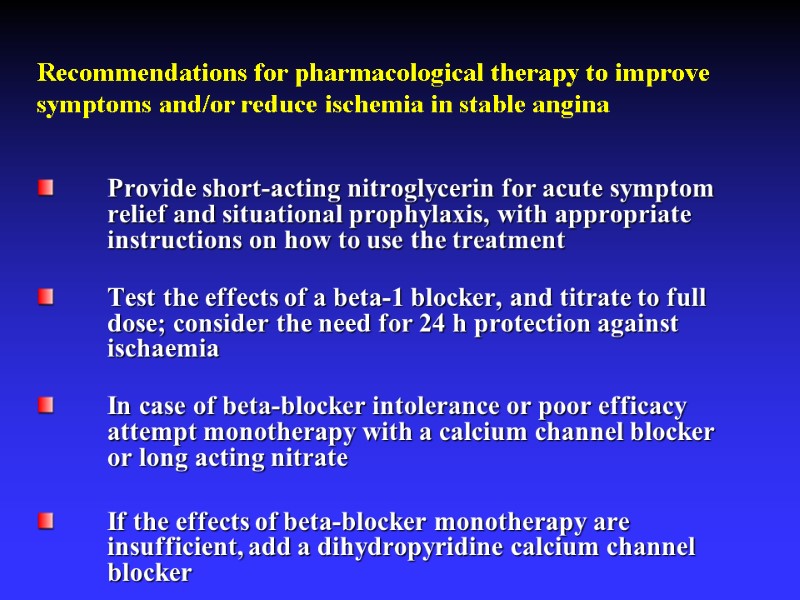
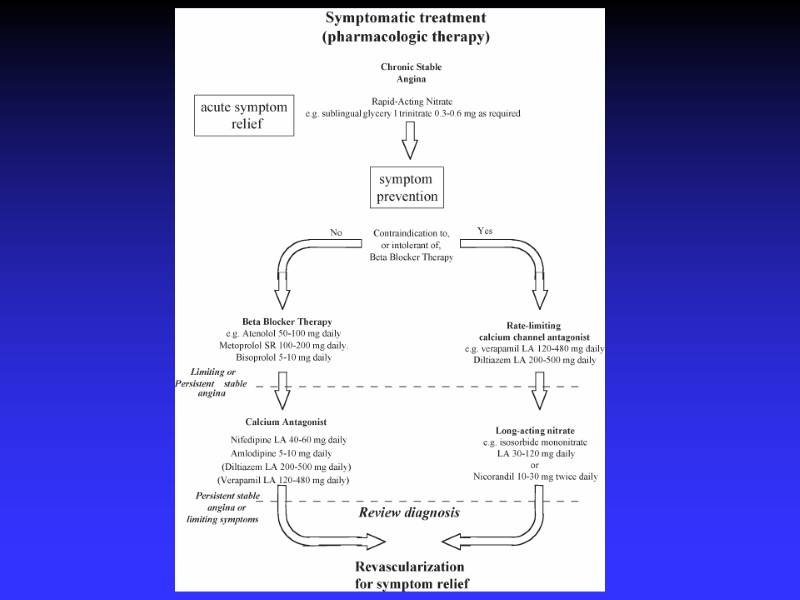
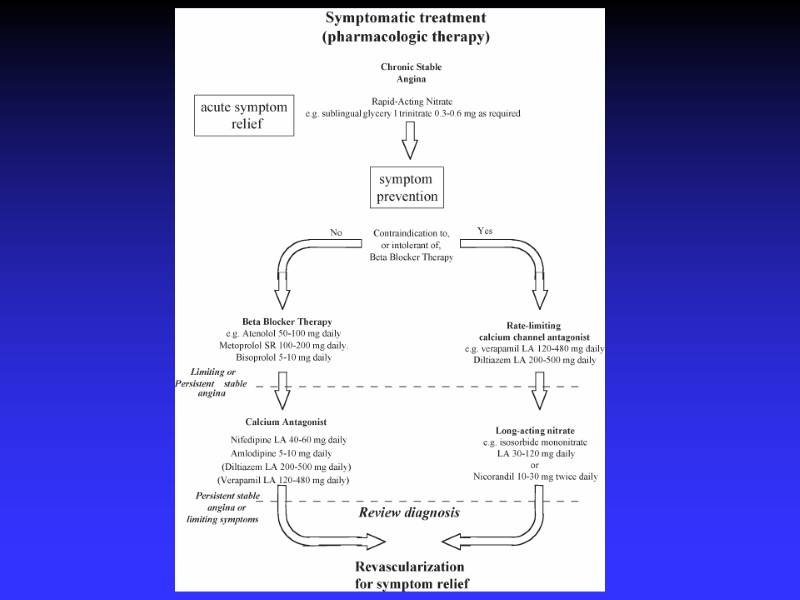
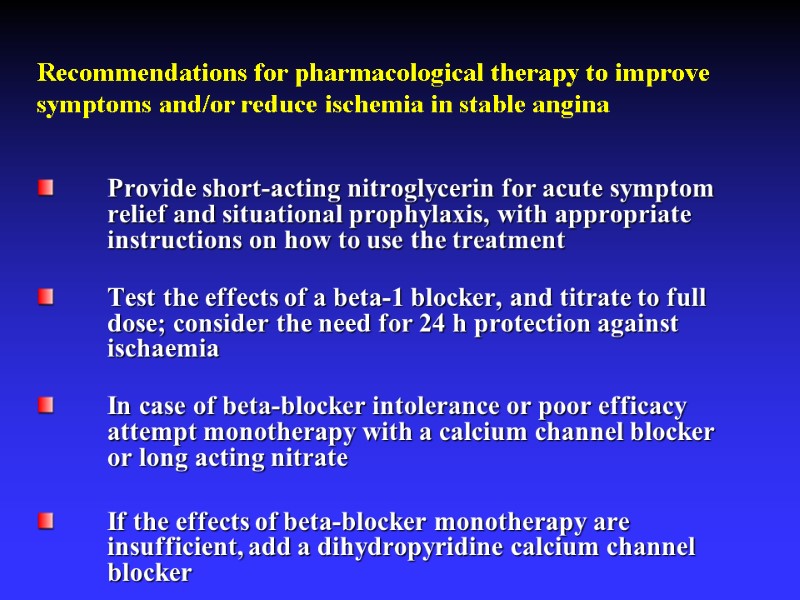 Recommendations for pharmacological therapy to improve symptoms and/or reduce ischemia in stable angina Provide short-acting nitroglycerin for acute symptom relief and situational prophylaxis, with appropriate instructions on how to use the treatment Test the effects of a beta-1 blocker, and titrate to full dose; consider the need for 24 h protection against ischaemia In case of beta-blocker intolerance or poor efficacy attempt monotherapy with a calcium channel blocker or long acting nitrate If the effects of beta-blocker monotherapy are insufficient, add a dihydropyridine calcium channel blocker
Recommendations for pharmacological therapy to improve symptoms and/or reduce ischemia in stable angina Provide short-acting nitroglycerin for acute symptom relief and situational prophylaxis, with appropriate instructions on how to use the treatment Test the effects of a beta-1 blocker, and titrate to full dose; consider the need for 24 h protection against ischaemia In case of beta-blocker intolerance or poor efficacy attempt monotherapy with a calcium channel blocker or long acting nitrate If the effects of beta-blocker monotherapy are insufficient, add a dihydropyridine calcium channel blocker
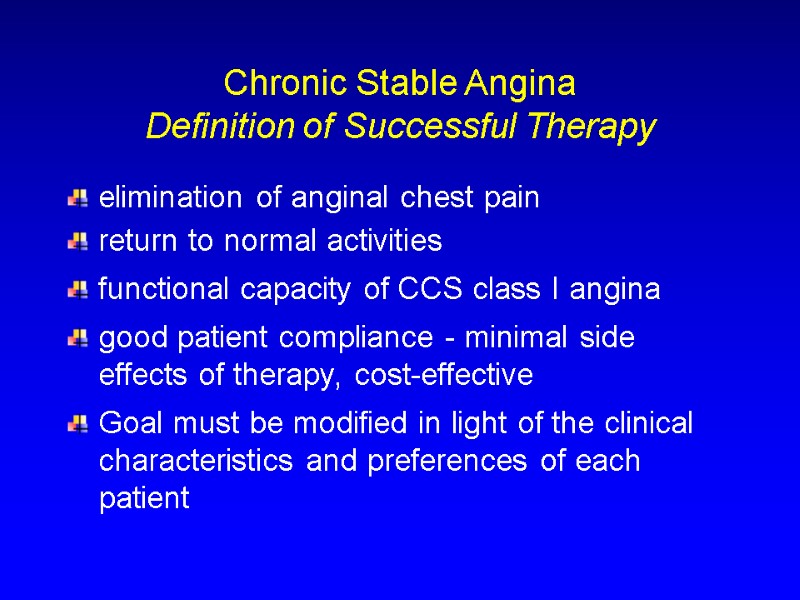
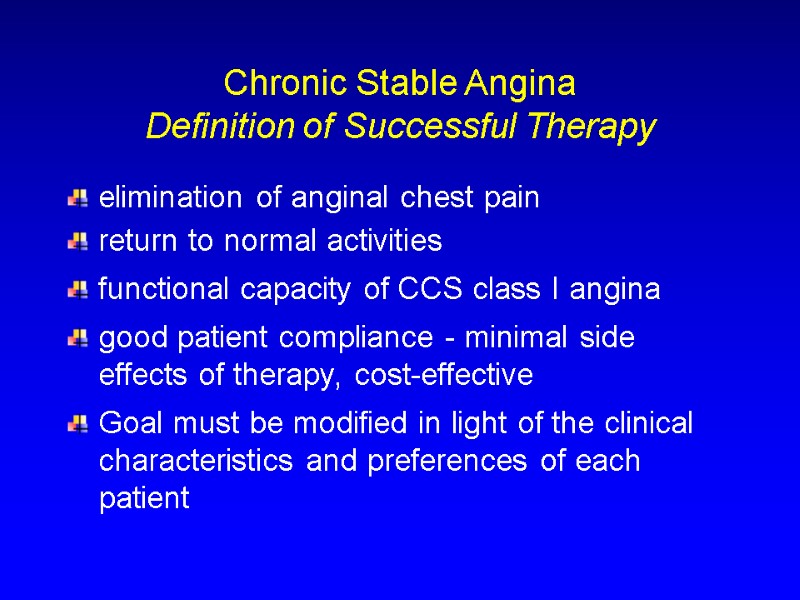 elimination of anginal chest pain return to normal activities functional capacity of CCS class I angina good patient compliance - minimal side effects of therapy, cost-effective Goal must be modified in light of the clinical characteristics and preferences of each patient Chronic Stable Angina Definition of Successful Therapy
elimination of anginal chest pain return to normal activities functional capacity of CCS class I angina good patient compliance - minimal side effects of therapy, cost-effective Goal must be modified in light of the clinical characteristics and preferences of each patient Chronic Stable Angina Definition of Successful Therapy
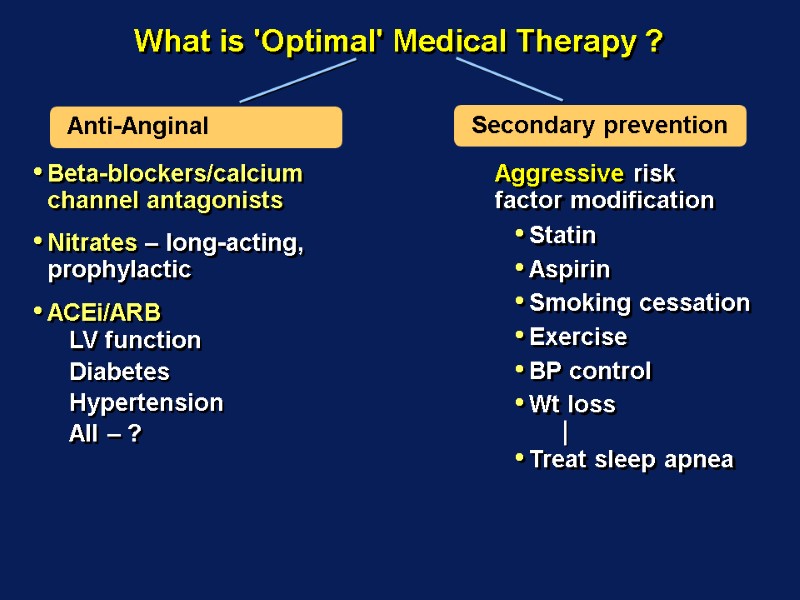
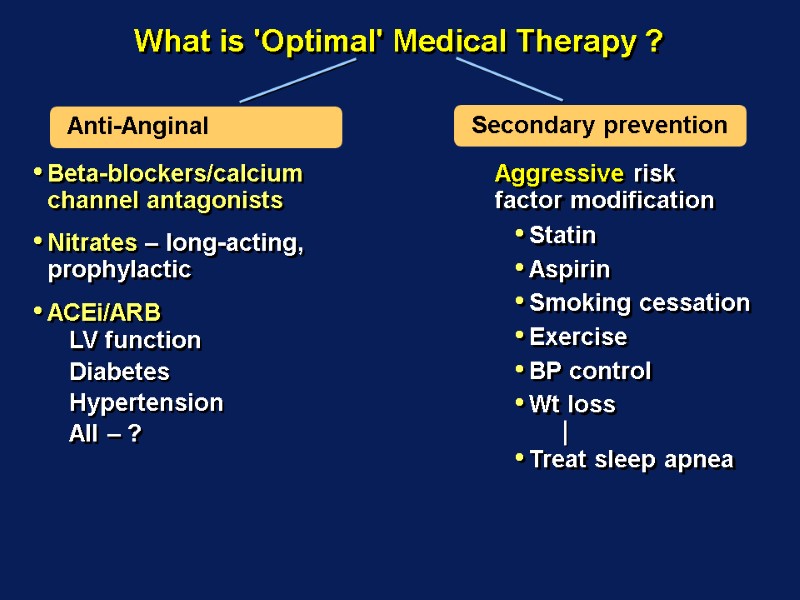 What is 'Optimal' Medical Therapy ? Beta-blockers/calcium channel antagonists Nitrates – long-acting, prophylactic ACEi/ARB LV function Diabetes Hypertension All – ? Aggressive risk factor modification Statin Aspirin Smoking cessation Exercise BP control Wt loss Treat sleep apnea
What is 'Optimal' Medical Therapy ? Beta-blockers/calcium channel antagonists Nitrates – long-acting, prophylactic ACEi/ARB LV function Diabetes Hypertension All – ? Aggressive risk factor modification Statin Aspirin Smoking cessation Exercise BP control Wt loss Treat sleep apnea
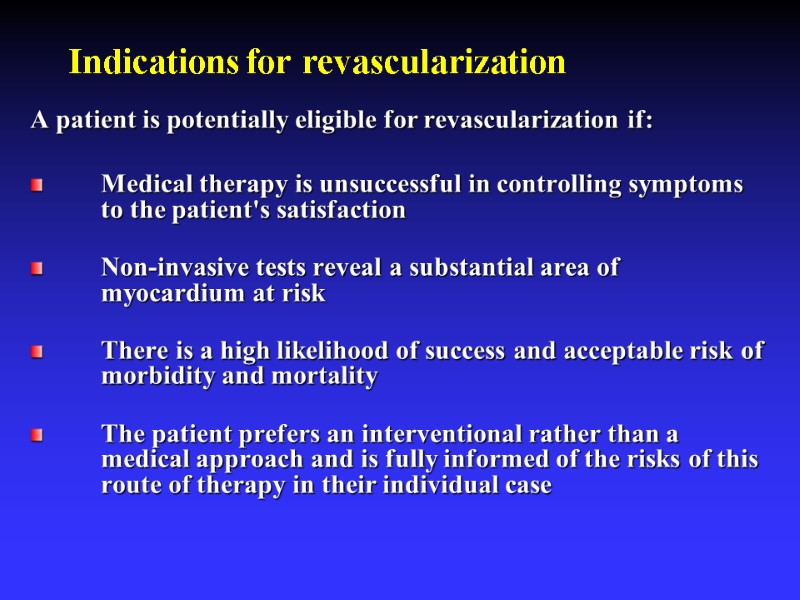 Indications for revascularization A patient is potentially eligible for revascularization if: Medical therapy is unsuccessful in controlling symptoms to the patient's satisfaction Non-invasive tests reveal a substantial area of myocardium at risk There is a high likelihood of success and acceptable risk of morbidity and mortality The patient prefers an interventional rather than a medical approach and is fully informed of the risks of this route of therapy in their individual case
Indications for revascularization A patient is potentially eligible for revascularization if: Medical therapy is unsuccessful in controlling symptoms to the patient's satisfaction Non-invasive tests reveal a substantial area of myocardium at risk There is a high likelihood of success and acceptable risk of morbidity and mortality The patient prefers an interventional rather than a medical approach and is fully informed of the risks of this route of therapy in their individual case
 Revascularization PCI CABG
Revascularization PCI CABG
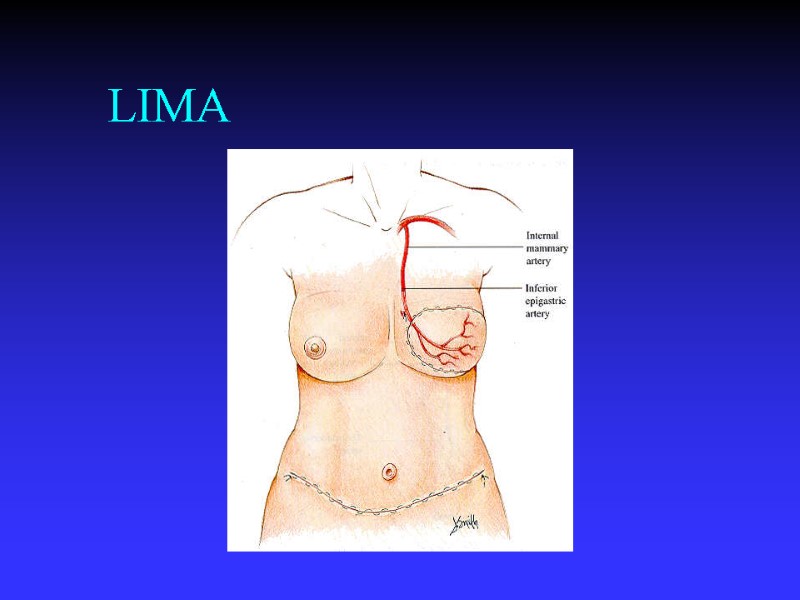
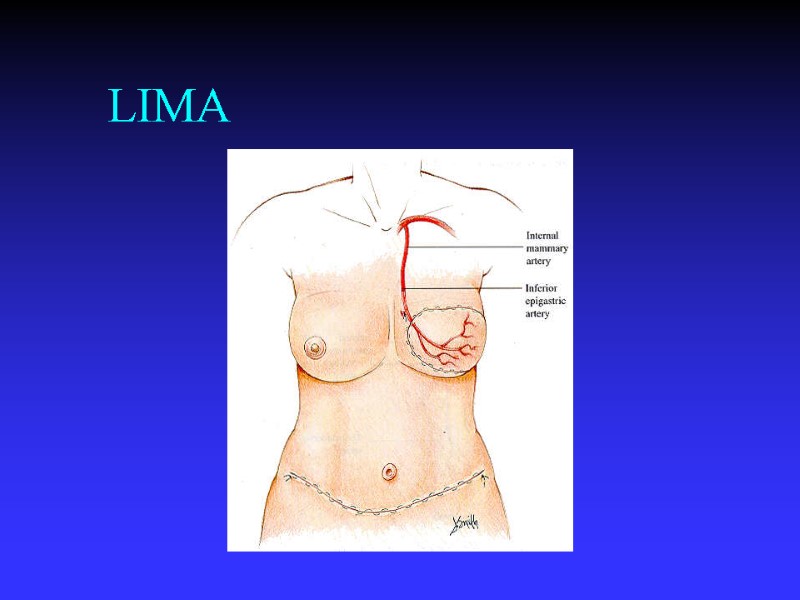 LIMA
LIMA
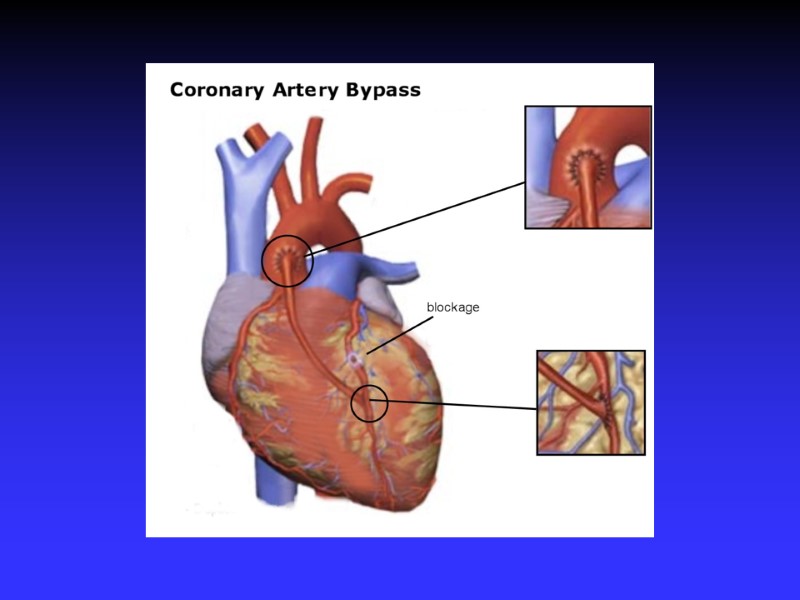
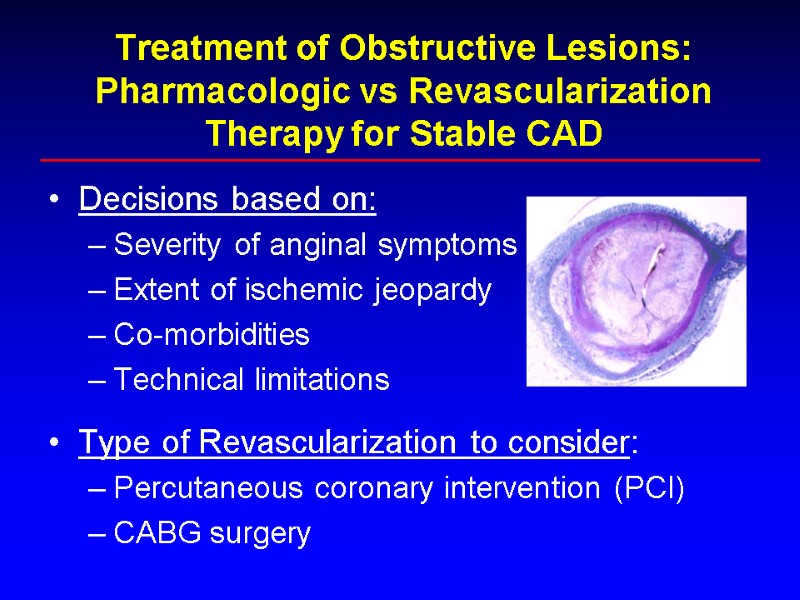 Treatment of Obstructive Lesions: Pharmacologic vs Revascularization Therapy for Stable CAD Decisions based on: Severity of anginal symptoms Extent of ischemic jeopardy Co-morbidities Technical limitations Type of Revascularization to consider: Percutaneous coronary intervention (PCI) CABG surgery
Treatment of Obstructive Lesions: Pharmacologic vs Revascularization Therapy for Stable CAD Decisions based on: Severity of anginal symptoms Extent of ischemic jeopardy Co-morbidities Technical limitations Type of Revascularization to consider: Percutaneous coronary intervention (PCI) CABG surgery
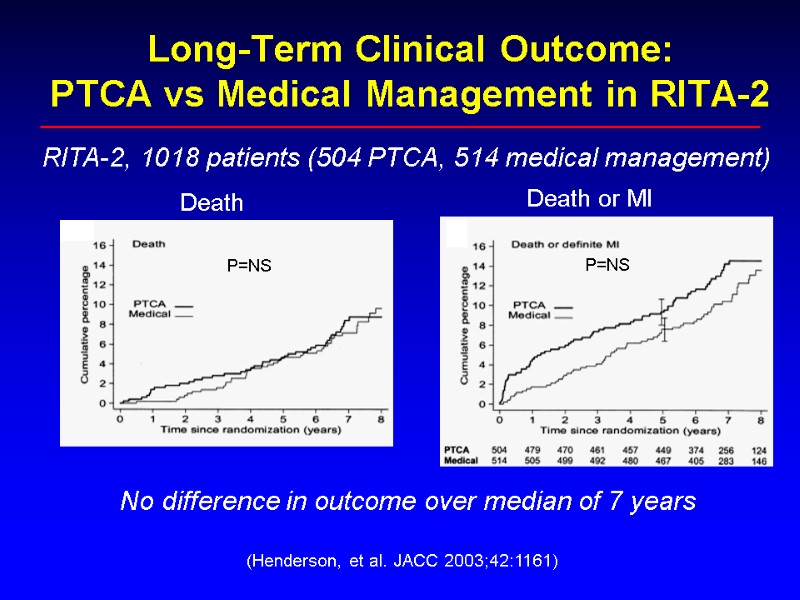
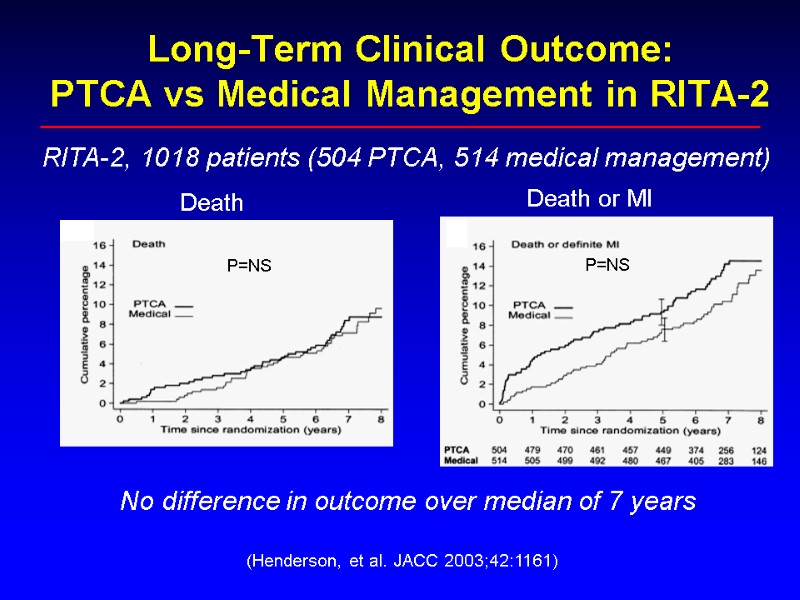 Long-Term Clinical Outcome: PTCA vs Medical Management in RITA-2 (Henderson, et al. JACC 2003;42:1161) P=NS P=NS No difference in outcome over median of 7 years RITA-2, 1018 patients (504 PTCA, 514 medical management) Death Death or MI
Long-Term Clinical Outcome: PTCA vs Medical Management in RITA-2 (Henderson, et al. JACC 2003;42:1161) P=NS P=NS No difference in outcome over median of 7 years RITA-2, 1018 patients (504 PTCA, 514 medical management) Death Death or MI
 Value of Optimal Medical Therapy: The COURAGE Trial 2,287 patients with objective evidence of myocardial ischemia and significant CAD in U.S. and Canada (1999-2004) All patients received max medical therapy (β-blockers, Ca++ blockers, nitrates, statins, ASA, ACEI/ARB) 1,149 underwent PCI in addition to optimal med therapy 1,138 received optimal medical therapy alone Followup 4.6 years (median) Primary endpoint = composite of death/non-fatal MI (Boden, et al. NEJM 2007;356:1503)
Value of Optimal Medical Therapy: The COURAGE Trial 2,287 patients with objective evidence of myocardial ischemia and significant CAD in U.S. and Canada (1999-2004) All patients received max medical therapy (β-blockers, Ca++ blockers, nitrates, statins, ASA, ACEI/ARB) 1,149 underwent PCI in addition to optimal med therapy 1,138 received optimal medical therapy alone Followup 4.6 years (median) Primary endpoint = composite of death/non-fatal MI (Boden, et al. NEJM 2007;356:1503)
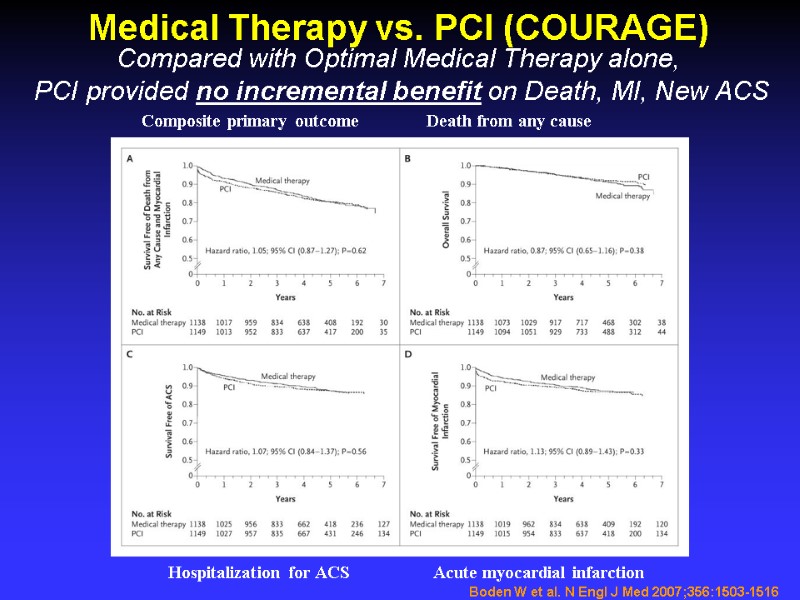
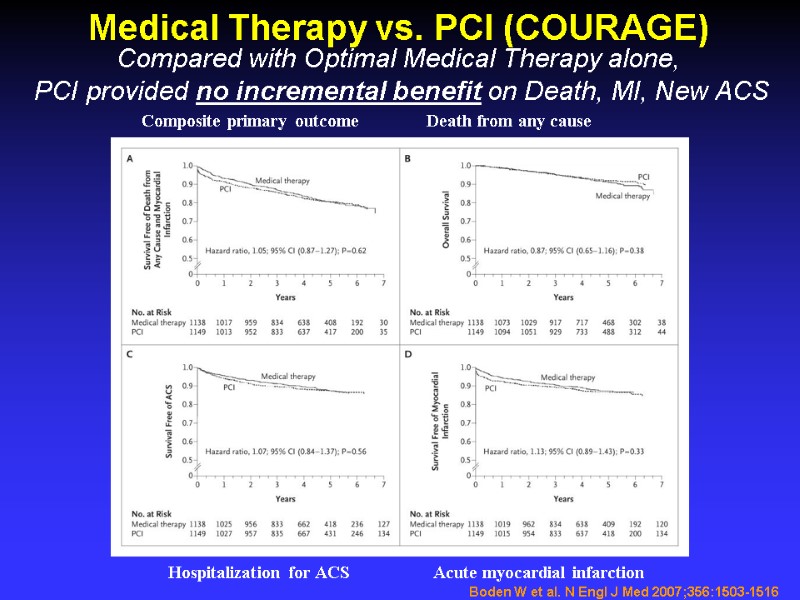 Boden W et al. N Engl J Med 2007;356:1503-1516 Medical Therapy vs. PCI (COURAGE) Composite primary outcome Death from any cause Hospitalization for ACS Acute myocardial infarction Compared with Optimal Medical Therapy alone, PCI provided no incremental benefit on Death, MI, New ACS
Boden W et al. N Engl J Med 2007;356:1503-1516 Medical Therapy vs. PCI (COURAGE) Composite primary outcome Death from any cause Hospitalization for ACS Acute myocardial infarction Compared with Optimal Medical Therapy alone, PCI provided no incremental benefit on Death, MI, New ACS
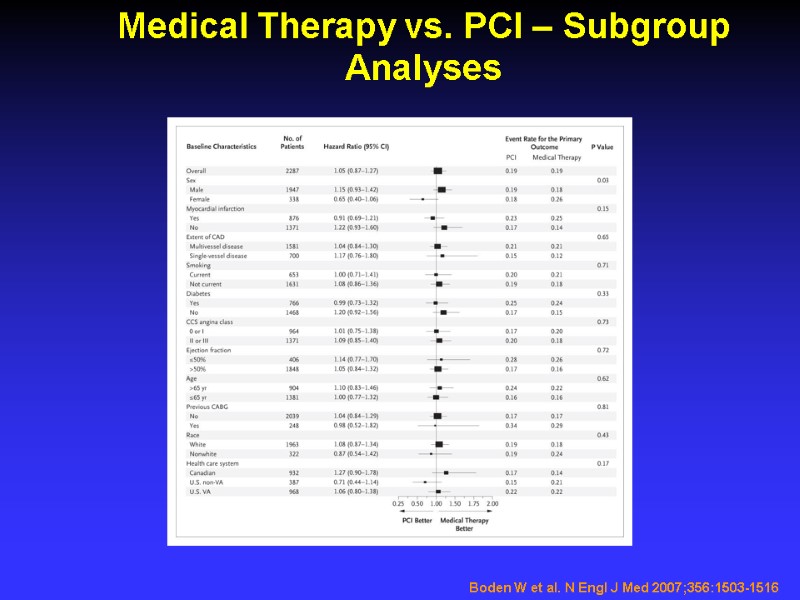
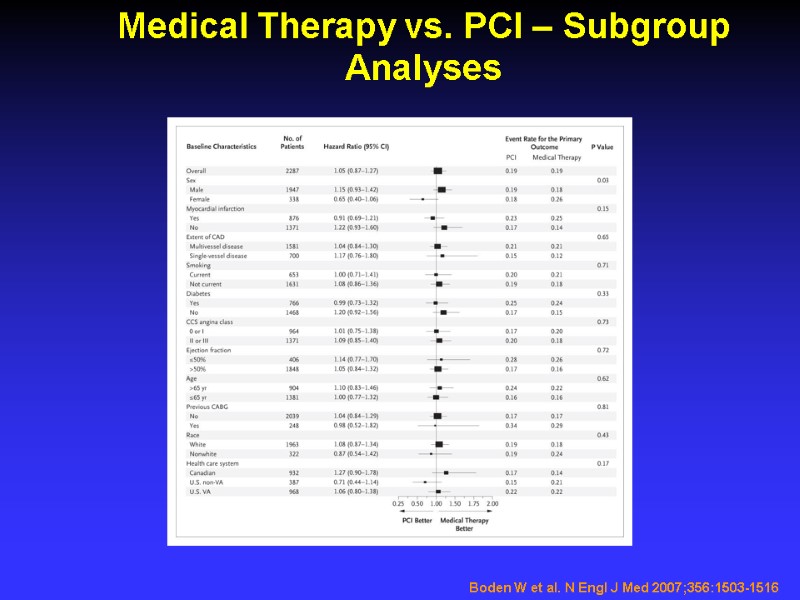 Medical Therapy vs. PCI – Subgroup Analyses Boden W et al. N Engl J Med 2007;356:1503-1516
Medical Therapy vs. PCI – Subgroup Analyses Boden W et al. N Engl J Med 2007;356:1503-1516
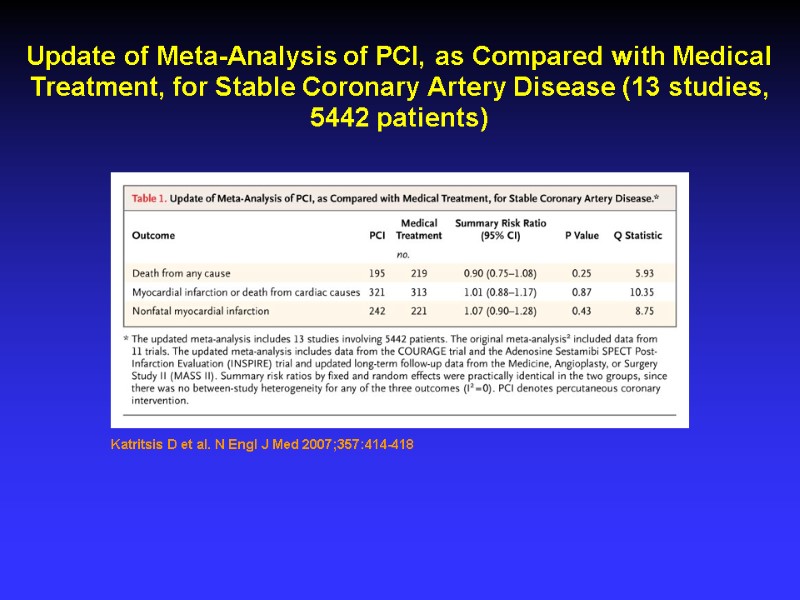
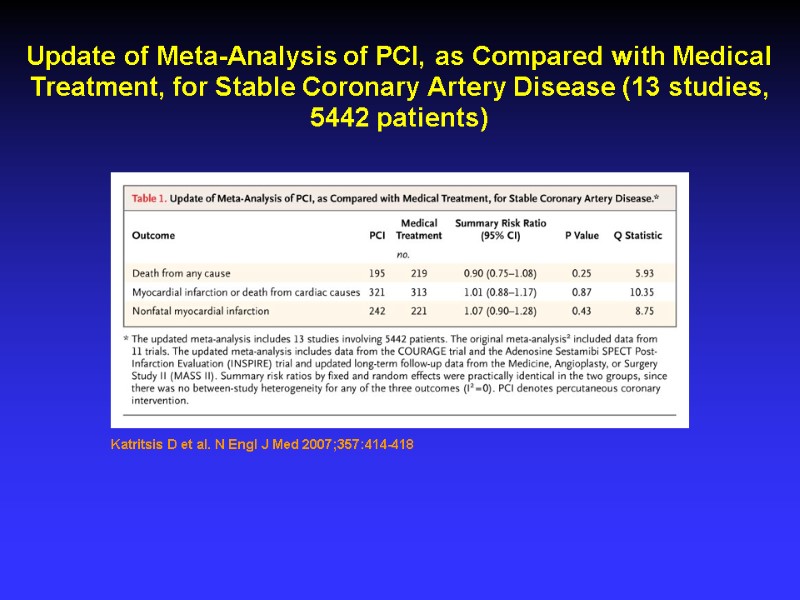 Katritsis D et al. N Engl J Med 2007;357:414-418 Update of Meta-Analysis of PCI, as Compared with Medical Treatment, for Stable Coronary Artery Disease (13 studies, 5442 patients)
Katritsis D et al. N Engl J Med 2007;357:414-418 Update of Meta-Analysis of PCI, as Compared with Medical Treatment, for Stable Coronary Artery Disease (13 studies, 5442 patients)
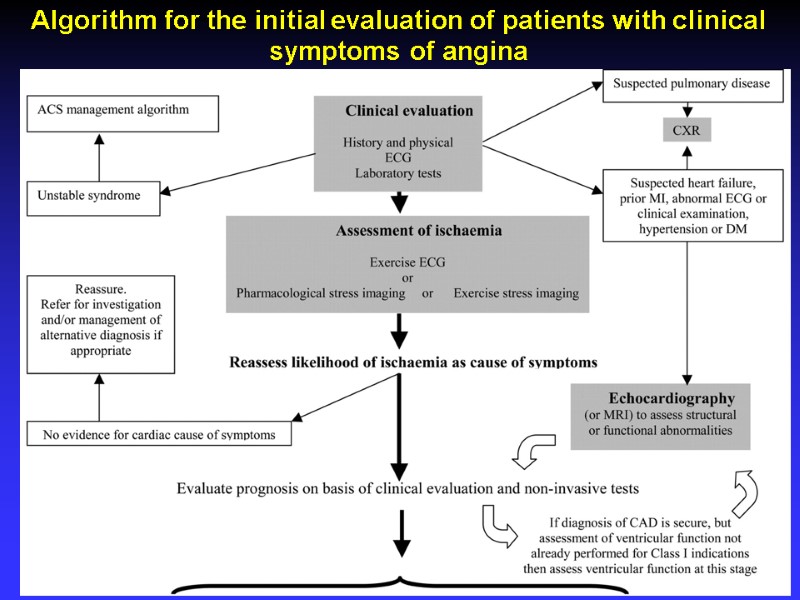
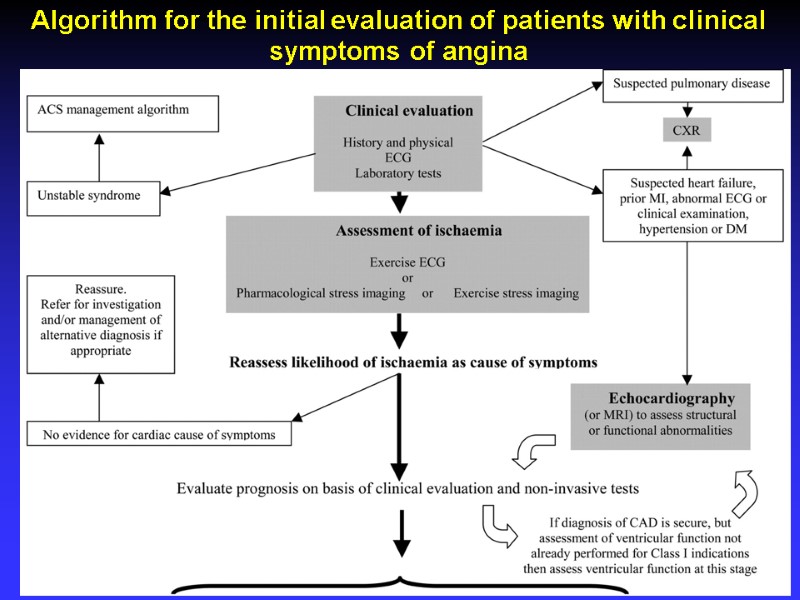 Algorithm for the initial evaluation of patients with clinical symptoms of angina
Algorithm for the initial evaluation of patients with clinical symptoms of angina
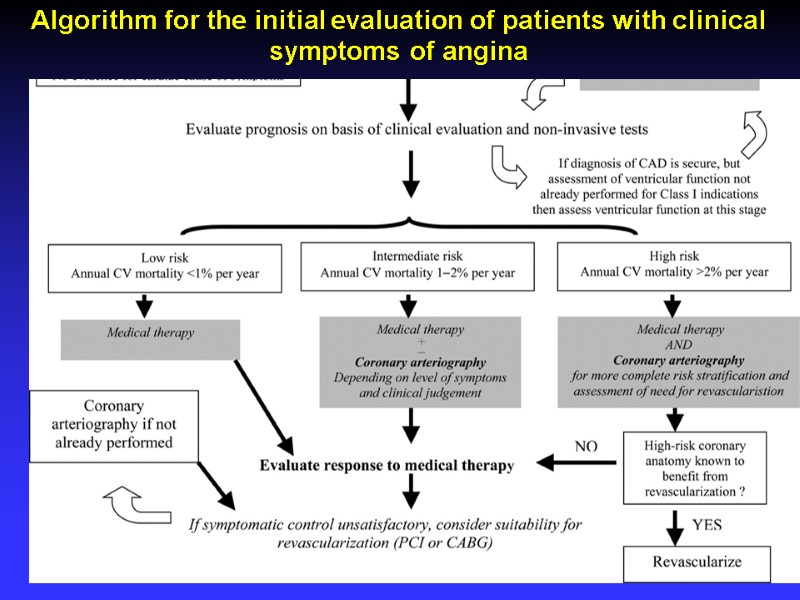
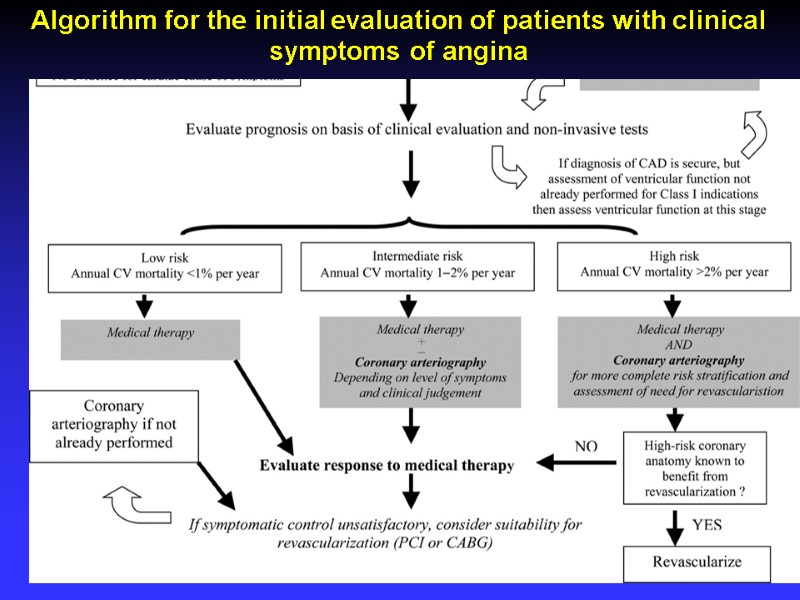 Algorithm for the initial evaluation of patients with clinical symptoms of angina
Algorithm for the initial evaluation of patients with clinical symptoms of angina
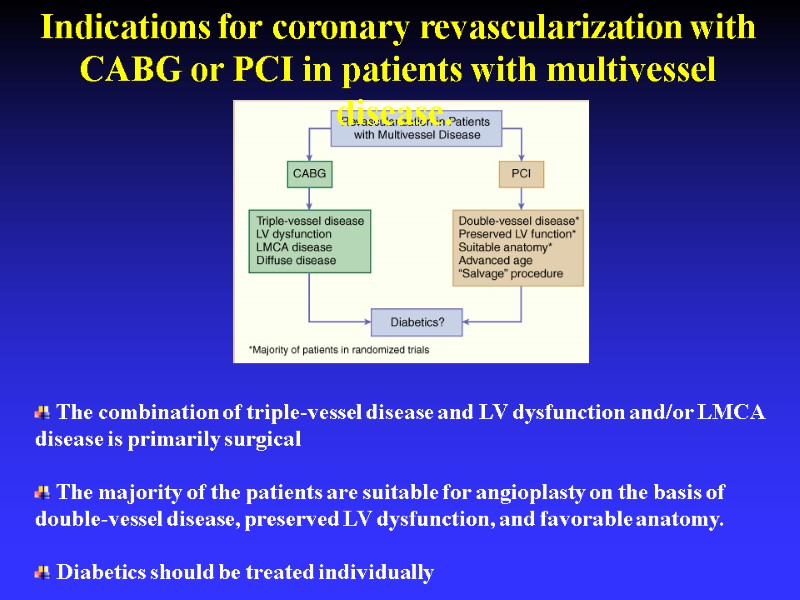
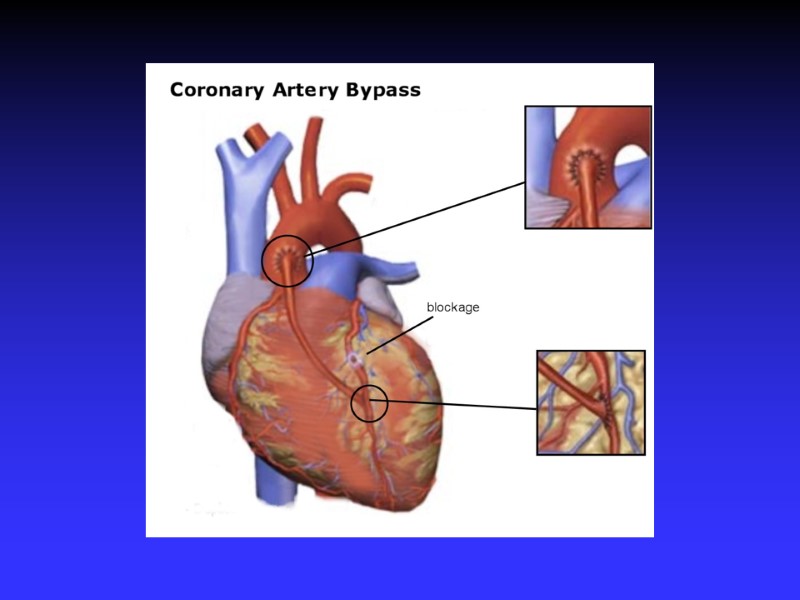
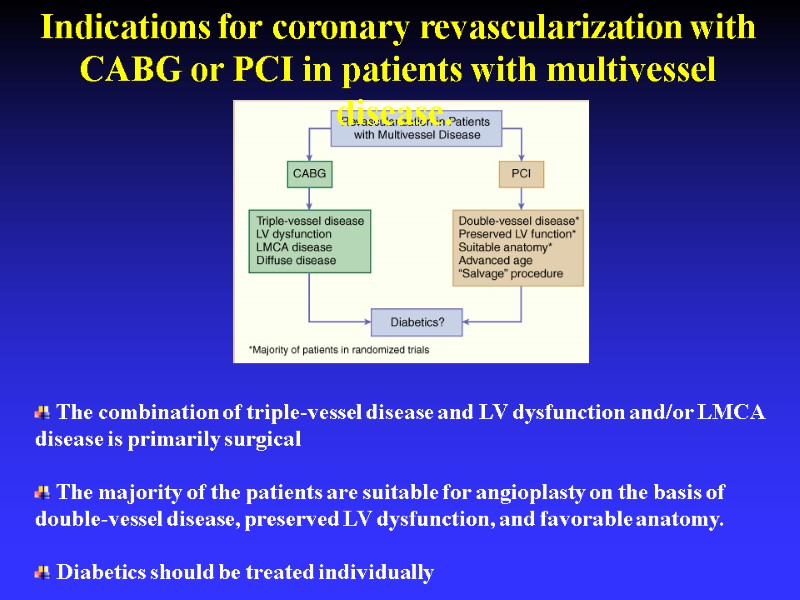 Indications for coronary revascularization with CABG or PCI in patients with multivessel disease. The combination of triple-vessel disease and LV dysfunction and/or LMCA disease is primarily surgical The majority of the patients are suitable for angioplasty on the basis of double-vessel disease, preserved LV dysfunction, and favorable anatomy. Diabetics should be treated individually
Indications for coronary revascularization with CABG or PCI in patients with multivessel disease. The combination of triple-vessel disease and LV dysfunction and/or LMCA disease is primarily surgical The majority of the patients are suitable for angioplasty on the basis of double-vessel disease, preserved LV dysfunction, and favorable anatomy. Diabetics should be treated individually
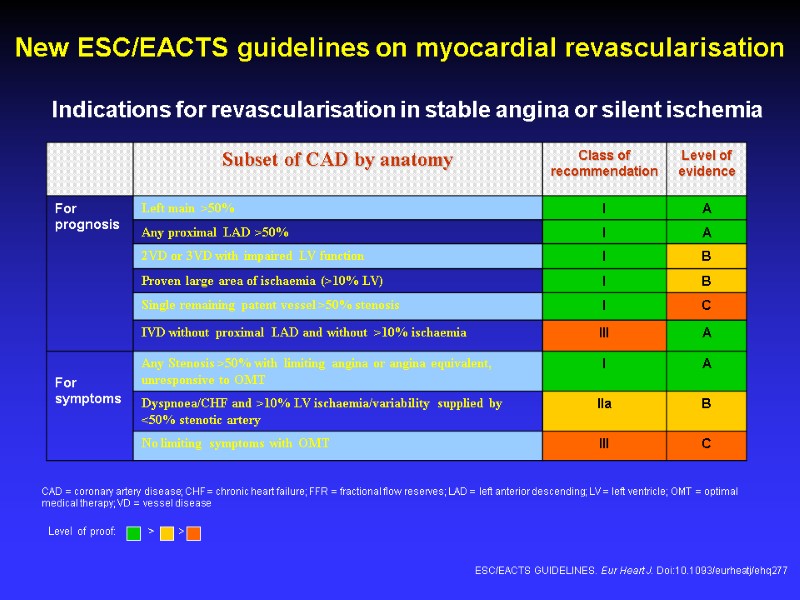
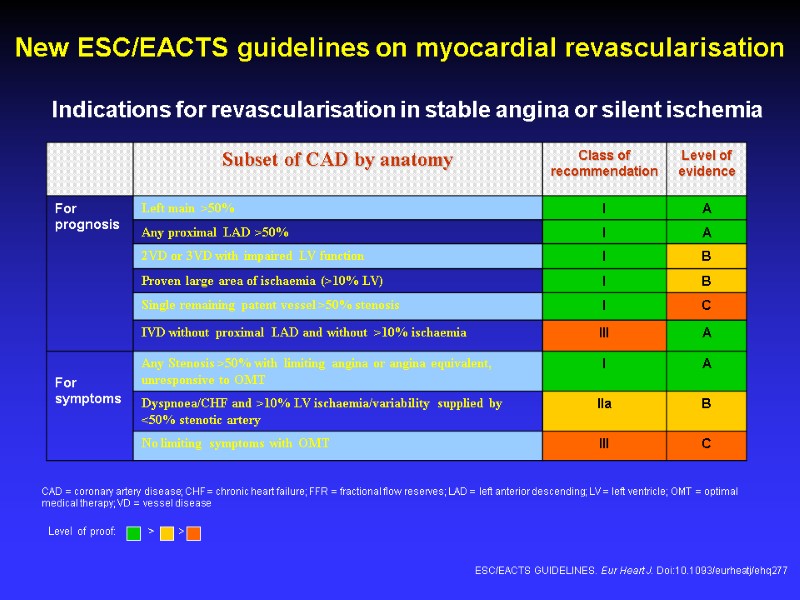 Indications for revascularisation in stable angina or silent ischemia CAD = coronary artery disease; CHF = chronic heart failure; FFR = fractional flow reserves; LAD = left anterior descending; LV = left ventricle; OMT = optimal medical therapy; VD = vessel disease New ESC/EACTS guidelines on myocardial revascularisation ESC/EACTS GUIDELINES. Eur Heart J. Doi:10.1093/eurheatj/ehq277 Level of proof: > >
Indications for revascularisation in stable angina or silent ischemia CAD = coronary artery disease; CHF = chronic heart failure; FFR = fractional flow reserves; LAD = left anterior descending; LV = left ventricle; OMT = optimal medical therapy; VD = vessel disease New ESC/EACTS guidelines on myocardial revascularisation ESC/EACTS GUIDELINES. Eur Heart J. Doi:10.1093/eurheatj/ehq277 Level of proof: > >
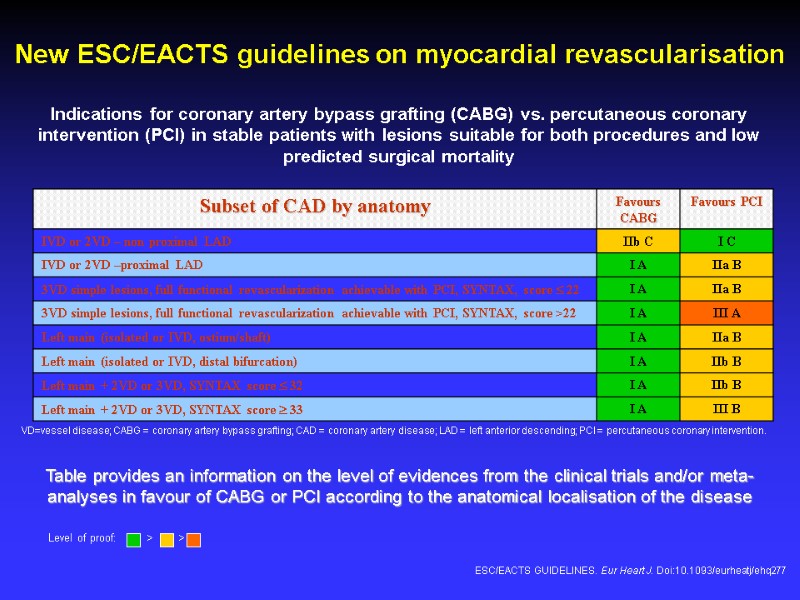
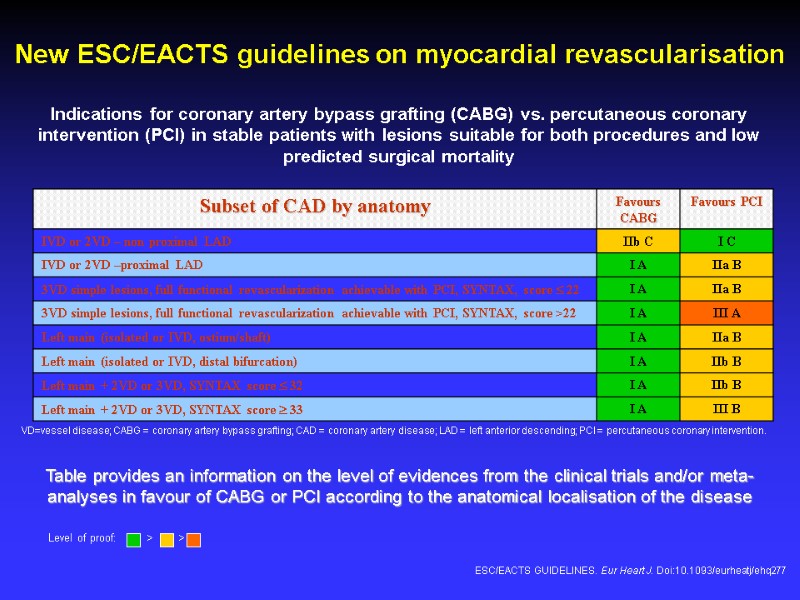 New ESC/EACTS guidelines on myocardial revascularisation Indications for coronary artery bypass grafting (CABG) vs. percutaneous coronary intervention (PCI) in stable patients with lesions suitable for both procedures and low predicted surgical mortality VD=vessel disease; CABG = coronary artery bypass grafting; CAD = coronary artery disease; LAD = left anterior descending; PCI = percutaneous coronary intervention. Table provides an information on the level of evidences from the clinical trials and/or meta-analyses in favour of CABG or PCI according to the anatomical localisation of the disease ESC/EACTS GUIDELINES. Eur Heart J. Doi:10.1093/eurheatj/ehq277 Level of proof: > >
New ESC/EACTS guidelines on myocardial revascularisation Indications for coronary artery bypass grafting (CABG) vs. percutaneous coronary intervention (PCI) in stable patients with lesions suitable for both procedures and low predicted surgical mortality VD=vessel disease; CABG = coronary artery bypass grafting; CAD = coronary artery disease; LAD = left anterior descending; PCI = percutaneous coronary intervention. Table provides an information on the level of evidences from the clinical trials and/or meta-analyses in favour of CABG or PCI according to the anatomical localisation of the disease ESC/EACTS GUIDELINES. Eur Heart J. Doi:10.1093/eurheatj/ehq277 Level of proof: > >


