8233763ffd30010ed373978a7797414d.ppt
- Количество слайдов: 37
 Children and young people with long term medical conditions and their fathers & mothers: how do they learn to share the care of conditions with clinical teams?
Children and young people with long term medical conditions and their fathers & mothers: how do they learn to share the care of conditions with clinical teams?
 Background • Growing numbers of children and young people have a long term condition that needs regular treatments and special care • Children and young people are usually happier and grow and develop better at home rather than in hospital • The Department of Health (DH) therefore, encourages clinical teams, whenever possible, to help parents give treatments and special care at home • But this means parents: may perform the vast majority of care-giving, including tasks that are complex and demanding (DH 2006: 14)
Background • Growing numbers of children and young people have a long term condition that needs regular treatments and special care • Children and young people are usually happier and grow and develop better at home rather than in hospital • The Department of Health (DH) therefore, encourages clinical teams, whenever possible, to help parents give treatments and special care at home • But this means parents: may perform the vast majority of care-giving, including tasks that are complex and demanding (DH 2006: 14)
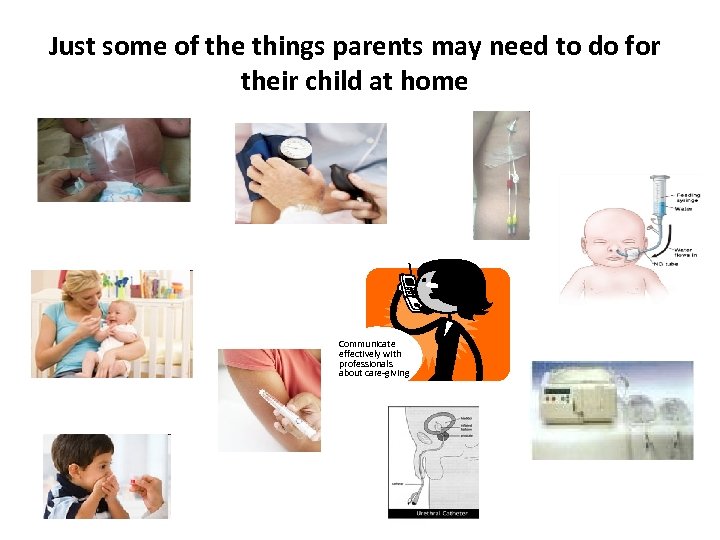 Just some of the things parents may need to do for their child at home Communicate effectively with professionals about care-giving
Just some of the things parents may need to do for their child at home Communicate effectively with professionals about care-giving
 Previous international research on childhood long term conditions • Generally, fewer fathers than mothers take part in research about parents’ roles in their child’s treatment and special care • Fathers are sometimes not invited to take part in research; some are invited but choose not to take part in the research • However, when fathers do take part in research the results suggest that children, parents and families can all benefit from fathers being involved in children’s treatments and special care giving
Previous international research on childhood long term conditions • Generally, fewer fathers than mothers take part in research about parents’ roles in their child’s treatment and special care • Fathers are sometimes not invited to take part in research; some are invited but choose not to take part in the research • However, when fathers do take part in research the results suggest that children, parents and families can all benefit from fathers being involved in children’s treatments and special care giving
 Our programme of research on ‘Family Learning in Long Term Conditions’ at the University of Manchester • By working with families of children with long term conditions and clinical teams in our research, we aim to find out more about the best ways to help parents learn to: – Share their child’s medical care with clinical teams – Give home-based treatments and special care to their child – Involve children in their own treatments and special care as they get older so they may eventually manage their own condition • The results will help clinical teams and parents to keep children and young people as well and as happy as possible
Our programme of research on ‘Family Learning in Long Term Conditions’ at the University of Manchester • By working with families of children with long term conditions and clinical teams in our research, we aim to find out more about the best ways to help parents learn to: – Share their child’s medical care with clinical teams – Give home-based treatments and special care to their child – Involve children in their own treatments and special care as they get older so they may eventually manage their own condition • The results will help clinical teams and parents to keep children and young people as well and as happy as possible
 The researchers Investigators: • Dr Veronica Swallow, Senior Lecturer in Children’s Nursing, University of Manchester • Dr Nick Webb, Consultant Paediatric Nephrologist & Mrs Trish Smith, Renal Nurse Specialist, Royal Manchester Children’s Hospital • Dr Heather Lambert, Consultant Paediatric Nephrologist; Dr Lucy Wirz, Consultant Renal Clinical Psychologist; Mrs Jean Crosier, Senior Renal Nurse Specialist & Ms Leila Qizalbash, Renal Dietician, The Great North Children’s Hospital, Newcastle upon Tyne • Mrs Ann Macfadyen, Principal Lecturer, Northumbria University • Professor Davina Allen, Director of Research, School of Nursing and Midwifery, Cardiff University • Professor Julian Williams, School of Education, University of Manchester • Professor Kathy Knafl, Associate Dean & Professor Sheila Santacroce, Associate Professor, School of Nursing, University of North Carolina at Chapel Hill, USA Advisers on current projects: • Dr. Kathy Hawley Independent Advisor Children's work, The Expert Patient Programme Community Interest Company (EPPCIC); Dr Jeremy Davies, Head of Communication, UK Fatherhood Institute; Dr Sara Ryan, Senior Qualitative Researcher, Department of Primary Health Care, Oxford University; Renal Patient View
The researchers Investigators: • Dr Veronica Swallow, Senior Lecturer in Children’s Nursing, University of Manchester • Dr Nick Webb, Consultant Paediatric Nephrologist & Mrs Trish Smith, Renal Nurse Specialist, Royal Manchester Children’s Hospital • Dr Heather Lambert, Consultant Paediatric Nephrologist; Dr Lucy Wirz, Consultant Renal Clinical Psychologist; Mrs Jean Crosier, Senior Renal Nurse Specialist & Ms Leila Qizalbash, Renal Dietician, The Great North Children’s Hospital, Newcastle upon Tyne • Mrs Ann Macfadyen, Principal Lecturer, Northumbria University • Professor Davina Allen, Director of Research, School of Nursing and Midwifery, Cardiff University • Professor Julian Williams, School of Education, University of Manchester • Professor Kathy Knafl, Associate Dean & Professor Sheila Santacroce, Associate Professor, School of Nursing, University of North Carolina at Chapel Hill, USA Advisers on current projects: • Dr. Kathy Hawley Independent Advisor Children's work, The Expert Patient Programme Community Interest Company (EPPCIC); Dr Jeremy Davies, Head of Communication, UK Fatherhood Institute; Dr Sara Ryan, Senior Qualitative Researcher, Department of Primary Health Care, Oxford University; Renal Patient View
 Our earlier research with families found that parents sometimes find it hard to: • Give treatments/special care if it upsets or hurts their child • Understand: – how to give treatments and special care – what each parents’ individual role in this is • Fit the treatments and special care into busy family life • Say if they find any of these things difficult in case the clinical team will think they are not good parents In addition: • Fathers’ & mothers’ views sometimes differed within couples
Our earlier research with families found that parents sometimes find it hard to: • Give treatments/special care if it upsets or hurts their child • Understand: – how to give treatments and special care – what each parents’ individual role in this is • Fit the treatments and special care into busy family life • Say if they find any of these things difficult in case the clinical team will think they are not good parents In addition: • Fathers’ & mothers’ views sometimes differed within couples
 Our earlier research with clinical teams found they sometimes want to know more about: • The types of teaching that work best for individual parents, children and young people and: – How much information or support they want – The types of information and support they would like
Our earlier research with clinical teams found they sometimes want to know more about: • The types of teaching that work best for individual parents, children and young people and: – How much information or support they want – The types of information and support they would like
 To build on previous research and find out more about fathers’ and mothers’ individual views • The British Renal Society funded our recent Fathers and Mothers Study • We asked 14 couples (parents of 15 children with a long term kidney condition) to take part in taperecorded research interviews – First we listened to each father and mother separately – Next we listened to each couple jointly Grateful thanks to : • The parents who took part • The British Renal Society (Grant 06 -017) and • The Children’s Kidney Unit Fund, Royal Victoria Infirmary, Newcastle upon Tyne
To build on previous research and find out more about fathers’ and mothers’ individual views • The British Renal Society funded our recent Fathers and Mothers Study • We asked 14 couples (parents of 15 children with a long term kidney condition) to take part in taperecorded research interviews – First we listened to each father and mother separately – Next we listened to each couple jointly Grateful thanks to : • The parents who took part • The British Renal Society (Grant 06 -017) and • The Children’s Kidney Unit Fund, Royal Victoria Infirmary, Newcastle upon Tyne
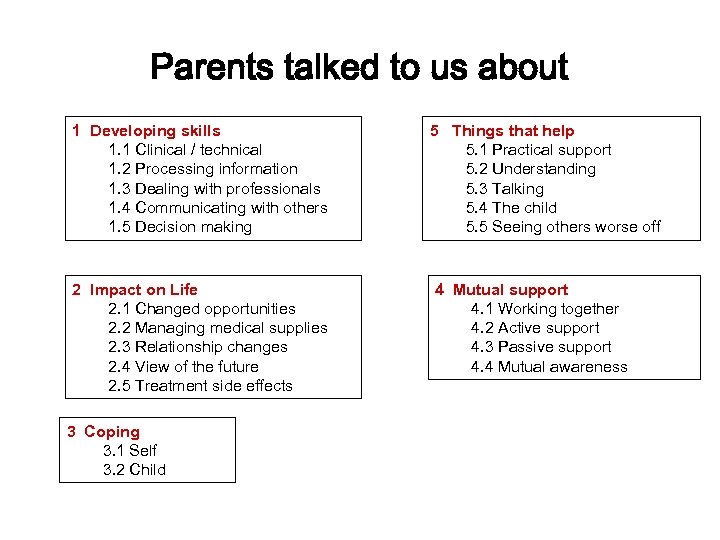 Parents talked to us about 1 Developing skills 1. 1 Clinical / technical 1. 2 Processing information 1. 3 Dealing with professionals 1. 4 Communicating with others 1. 5 Decision making 2 Impact on Life 2. 1 Changed opportunities 2. 2 Managing medical supplies 2. 3 Relationship changes 2. 4 View of the future 2. 5 Treatment side effects 3 Coping 3. 1 Self 3. 2 Child 5 Things that help 5. 1 Practical support 5. 2 Understanding 5. 3 Talking 5. 4 The child 5. 5 Seeing others worse off 4 Mutual support 4. 1 Working together 4. 2 Active support 4. 3 Passive support 4. 4 Mutual awareness
Parents talked to us about 1 Developing skills 1. 1 Clinical / technical 1. 2 Processing information 1. 3 Dealing with professionals 1. 4 Communicating with others 1. 5 Decision making 2 Impact on Life 2. 1 Changed opportunities 2. 2 Managing medical supplies 2. 3 Relationship changes 2. 4 View of the future 2. 5 Treatment side effects 3 Coping 3. 1 Self 3. 2 Child 5 Things that help 5. 1 Practical support 5. 2 Understanding 5. 3 Talking 5. 4 The child 5. 5 Seeing others worse off 4 Mutual support 4. 1 Working together 4. 2 Active support 4. 3 Passive support 4. 4 Mutual awareness
 More on our findings: • with the exception of situations where one parent worked away from home, both were involved in giving treatments and special care at some time • no mothers said that they were left with the bulk of care giving • some unexpected findings from our research include:
More on our findings: • with the exception of situations where one parent worked away from home, both were involved in giving treatments and special care at some time • no mothers said that they were left with the bulk of care giving • some unexpected findings from our research include:
 Some parents (particularly mothers) gave vivid accounts of the physical and emotional effects on themselves of giving treatments and special care: I mean I used to sit there and my heart was going and I was hyperventilating and I was feeling sick…it was horrible … trying to control that and learning not to panic I don’t think I ever actually mastered that. (Mother)
Some parents (particularly mothers) gave vivid accounts of the physical and emotional effects on themselves of giving treatments and special care: I mean I used to sit there and my heart was going and I was hyperventilating and I was feeling sick…it was horrible … trying to control that and learning not to panic I don’t think I ever actually mastered that. (Mother)
 Some fathers I think the hardest thing commented on the for me was probably effect that giving trying to come to treatments and terms with your special care had on reaction and dealing with you. their relationship with the mother, and the (father to mother in joint family as a whole, one interview) said:
Some fathers I think the hardest thing commented on the for me was probably effect that giving trying to come to treatments and terms with your special care had on reaction and dealing with you. their relationship with the mother, and the (father to mother in joint family as a whole, one interview) said:
 There were some differences in the ways mothers and fathers processed information Fathers tended to want the bigger picture, as this quotation from the father of a child who had a kidney transplant shows: That is what I liked about it really, we seemed to know from day one what was going to happen with all the procedures, what would happen if it didn’t work (Father) And generally took a long term view: It’s [son’s condition] a bomb ticking away in the background. . . you wonder what he’ll be like in 10, 15, 18 years (Father)
There were some differences in the ways mothers and fathers processed information Fathers tended to want the bigger picture, as this quotation from the father of a child who had a kidney transplant shows: That is what I liked about it really, we seemed to know from day one what was going to happen with all the procedures, what would happen if it didn’t work (Father) And generally took a long term view: It’s [son’s condition] a bomb ticking away in the background. . . you wonder what he’ll be like in 10, 15, 18 years (Father)
 Mothers wanted to understand what the impact would be on day to day life, one said: I still don’t think long term. . . he [child’s father] wonders more about what’s going to happen later; I’m more here and now.
Mothers wanted to understand what the impact would be on day to day life, one said: I still don’t think long term. . . he [child’s father] wonders more about what’s going to happen later; I’m more here and now.
 I think the driving back Some fathers said it home [from the hospital helped them to go quiet, have some space where his child was being treated initially and the or ‘disengage’ from mother was resident at care-giving for a short time to think about what the hospital] sometimes helped, just the drive, was happening. because I was on my own and I didn’t have One father, for instance, information being thrown said new information at me… either from what I could be overwhelming: saw or heard or people speaking to me about stuff.
I think the driving back Some fathers said it home [from the hospital helped them to go quiet, have some space where his child was being treated initially and the or ‘disengage’ from mother was resident at care-giving for a short time to think about what the hospital] sometimes helped, just the drive, was happening. because I was on my own and I didn’t have One father, for instance, information being thrown said new information at me… either from what I could be overwhelming: saw or heard or people speaking to me about stuff.
 We asked about this in later, joint interviews; if the father said he found it helped to disengage, the interviewer asked: What is it you are doing when you are quiet? In one joint interview the mother said: Oh I would like to know that! The father explained: I don’t know, you just think about what could happen, what is happening, how long is it going to take for the results to come through? . . . I think there a million things going through your head. You think of every possibility” This may indicate that mothers and fathers process the same thoughts about health care in different ways and warrants further investigation.
We asked about this in later, joint interviews; if the father said he found it helped to disengage, the interviewer asked: What is it you are doing when you are quiet? In one joint interview the mother said: Oh I would like to know that! The father explained: I don’t know, you just think about what could happen, what is happening, how long is it going to take for the results to come through? . . . I think there a million things going through your head. You think of every possibility” This may indicate that mothers and fathers process the same thoughts about health care in different ways and warrants further investigation.
 We also reviewed results from 29 other research studies in health care that did involve some fathers These studies took place in Australia, Canada, China, Israel, Taiwan, the UK & the USA Our review tells us more about: 1. the impact of long-term conditions on fathers’ ability to promote their child's well-being 2. factors influencing fathers’ involvement in health care 3. personal growth ⁄ beneficial effects for fathers 4. the impact of fathers’ involvement on family functioning 5. strategies that increase fathers’ participation in their child's health care and in research investigating fathers participation
We also reviewed results from 29 other research studies in health care that did involve some fathers These studies took place in Australia, Canada, China, Israel, Taiwan, the UK & the USA Our review tells us more about: 1. the impact of long-term conditions on fathers’ ability to promote their child's well-being 2. factors influencing fathers’ involvement in health care 3. personal growth ⁄ beneficial effects for fathers 4. the impact of fathers’ involvement on family functioning 5. strategies that increase fathers’ participation in their child's health care and in research investigating fathers participation
 Helen and Graeme Walker are one couple who took part in our Fathers and Mothers study In the next 16 slides they introduce their daughter Alex and talk about their family’s experience of health care
Helen and Graeme Walker are one couple who took part in our Fathers and Mothers study In the next 16 slides they introduce their daughter Alex and talk about their family’s experience of health care
 Alex Walker: 4 th October 1990 • Alex was a perfectly healthy, normal baby • No complications during pregnancy • No problems with her birth
Alex Walker: 4 th October 1990 • Alex was a perfectly healthy, normal baby • No complications during pregnancy • No problems with her birth
 Alex through the ages! • Alex aged approx 5 months • Still no indication of kidney problems • She had a talent for projectile vomiting! • Doctors told us this was nothing to worry about
Alex through the ages! • Alex aged approx 5 months • Still no indication of kidney problems • She had a talent for projectile vomiting! • Doctors told us this was nothing to worry about
 Toddlerhood – All is still well!
Toddlerhood – All is still well!
 Infant school years – Still apparently OK
Infant school years – Still apparently OK
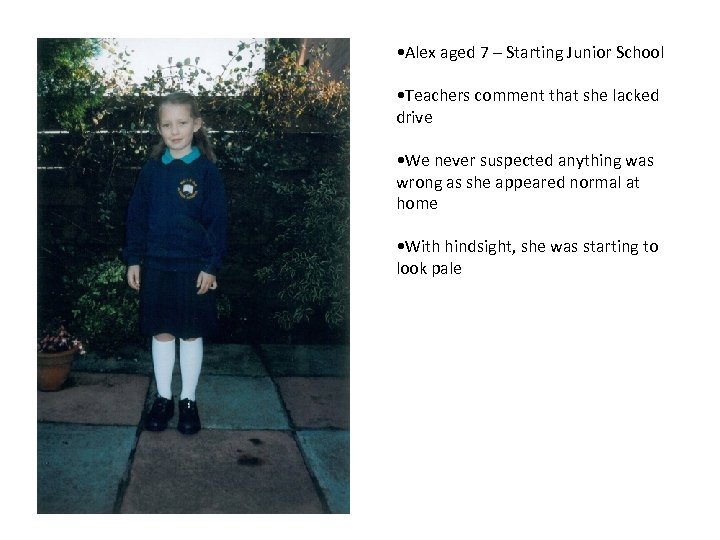 • Alex aged 7 – Starting Junior School • Teachers comment that she lacked drive • We never suspected anything was wrong as she appeared normal at home • With hindsight, she was starting to look pale
• Alex aged 7 – Starting Junior School • Teachers comment that she lacked drive • We never suspected anything was wrong as she appeared normal at home • With hindsight, she was starting to look pale
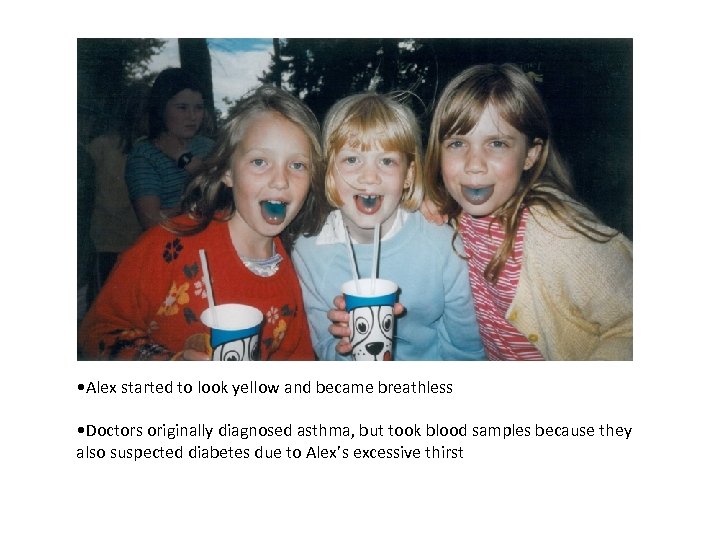 • Alex started to look yellow and became breathless • Doctors originally diagnosed asthma, but took blood samples because they also suspected diabetes due to Alex’s excessive thirst
• Alex started to look yellow and became breathless • Doctors originally diagnosed asthma, but took blood samples because they also suspected diabetes due to Alex’s excessive thirst
 • February 2000 – Rushed to hospital with suspected end stage renal failure • Stabilised in Carlisle before being transferred to the RVI in Newcastle • Diagnosis confirmed. Hopes that this was a short term problem were dashed. • We did not realise the enormity of what was to come
• February 2000 – Rushed to hospital with suspected end stage renal failure • Stabilised in Carlisle before being transferred to the RVI in Newcastle • Diagnosis confirmed. Hopes that this was a short term problem were dashed. • We did not realise the enormity of what was to come
 • Fitted with Tenchkoff catheter and started dialysis • Three operations to get the catheter working correctly took an emotional toll on the whole family. • Meanwhile we were taught how to do dialysis at home • A six week stay in hospital and we were competent but going home did not equate to going back to normality. It’s never normal.
• Fitted with Tenchkoff catheter and started dialysis • Three operations to get the catheter working correctly took an emotional toll on the whole family. • Meanwhile we were taught how to do dialysis at home • A six week stay in hospital and we were competent but going home did not equate to going back to normality. It’s never normal.
 • Stable on dialysis but cloudy fluid on the first drain after a night off meant many late night trips across to Newcastle • Sleepovers with friends had to be planned well in advance • Dietary constraints were always at the front of our minds • We tried to make life as normal as possible. Halloween doesn’t stop just because of dialysis.
• Stable on dialysis but cloudy fluid on the first drain after a night off meant many late night trips across to Newcastle • Sleepovers with friends had to be planned well in advance • Dietary constraints were always at the front of our minds • We tried to make life as normal as possible. Halloween doesn’t stop just because of dialysis.
 • Physically, Alex’s condition was being managed, but the emotional side was something we weren’t prepared for • Alex would sometimes hide in the bathroom to avoid being connected up for dialysis. Early on, it had caused extreme pain. • As her parents, we found this emotionally draining and each had to find our own way of coping and supporting each other
• Physically, Alex’s condition was being managed, but the emotional side was something we weren’t prepared for • Alex would sometimes hide in the bathroom to avoid being connected up for dialysis. Early on, it had caused extreme pain. • As her parents, we found this emotionally draining and each had to find our own way of coping and supporting each other
 • 10 months of dialysis and routine was established • Alex did EPO injections herself, despite becoming quite phobic of needles • Calcium carbonate tablets with every meal could be an issue at times • She undertook her own catheter care and even put herself on dialysis with dad’s supervision (mum didn’t know!)
• 10 months of dialysis and routine was established • Alex did EPO injections herself, despite becoming quite phobic of needles • Calcium carbonate tablets with every meal could be an issue at times • She undertook her own catheter care and even put herself on dialysis with dad’s supervision (mum didn’t know!)
 Transplant – 4 th January 2001 • Alex had a kidney transplant after 11 months on dialysis • The practicalities of life returned to a more normal level • BUT… • There were still drugs • There were still doctors • There were still uncertainties about the future
Transplant – 4 th January 2001 • Alex had a kidney transplant after 11 months on dialysis • The practicalities of life returned to a more normal level • BUT… • There were still drugs • There were still doctors • There were still uncertainties about the future
 Alexwas little brother and • Stephen was 6 when Alex diagnosed • Kidney disease affects the whole family • Stephen stayed with grandparents when Alex was first admitted to hospital • When Alex had her transplant he came with us. We couldn’t be separated again.
Alexwas little brother and • Stephen was 6 when Alex diagnosed • Kidney disease affects the whole family • Stephen stayed with grandparents when Alex was first admitted to hospital • When Alex had her transplant he came with us. We couldn’t be separated again.
 Alex grows up! • Alex hasn’t let any of this hold her back • She is proud of her transplant scar and doesn’t regret anything that has happened • As parents, we have sometimes found it difficult to let Alex take responsibility for her own health, but that is what you have to do
Alex grows up! • Alex hasn’t let any of this hold her back • She is proud of her transplant scar and doesn’t regret anything that has happened • As parents, we have sometimes found it difficult to let Alex take responsibility for her own health, but that is what you have to do
 • The transition to Adult Services meant that we had to train a new team of health professionals to give us the information we need • We still ask her if she has taken her tablets, even though she never misses. It’s hard to stop!
• The transition to Adult Services meant that we had to train a new team of health professionals to give us the information we need • We still ask her if she has taken her tablets, even though she never misses. It’s hard to stop!
 • Alex is now a student Children’s Nurse at Northumbria University and she works at the hospital where she had her transplant • Her kidney might not last forever. She doesn’t let it worry her • We do! • She still celebrates Halloween in style!
• Alex is now a student Children’s Nurse at Northumbria University and she works at the hospital where she had her transplant • Her kidney might not last forever. She doesn’t let it worry her • We do! • She still celebrates Halloween in style!
 So what next? Building on previous research we have two more projects underway that involve children, young people, fathers, mothers and health professionals: 1. Teaching parents to become home-based care-givers of children’s longterm kidney conditions: a mixed methods survey of Children’s Kidney Units in England, Scotland Wales. We are grateful to Kids Kidney Research UK for funding this work 2. The OPIS (On-line Parent Information and Support) project: Meeting mothers' and fathers' information and support needs for home-based management of childhood chronic kidney disease. We are grateful to the National Institute of Health Research (NIHR) Research for Patient Benefit Programme for funding this work We are also grateful to the Greater Manchester, Lancashire and S. Cumbria Medicines for Children Research Network for supporting these studies
So what next? Building on previous research we have two more projects underway that involve children, young people, fathers, mothers and health professionals: 1. Teaching parents to become home-based care-givers of children’s longterm kidney conditions: a mixed methods survey of Children’s Kidney Units in England, Scotland Wales. We are grateful to Kids Kidney Research UK for funding this work 2. The OPIS (On-line Parent Information and Support) project: Meeting mothers' and fathers' information and support needs for home-based management of childhood chronic kidney disease. We are grateful to the National Institute of Health Research (NIHR) Research for Patient Benefit Programme for funding this work We are also grateful to the Greater Manchester, Lancashire and S. Cumbria Medicines for Children Research Network for supporting these studies
 Some references: Swallow V, Macfadyen A, Lambert H, Santacroce S. Fathers’ contributions to management of their children’s long-term medical conditions: a narrative review of the literature. Health Expectations. 2011 http: //dx. doi. org/10. 1111/j. 1369 -7625. 2011. 00674. x Swallow V, Lambert H, Santacroce S, Macfadyen A. Fathers and mothers developing skills in managing children’s long-term medical conditions : how do their qualitative accounts compare? Child: Care Health & Development. 2011 http: //dx. doi. org/10. 1111/j. 1365 -2214. 2011. 01219. x Swallow V, Macfadyen A, Forrester T (2011) Teenagers’ and parents’ views of a short break service for children with lifelimiting conditions: a qualitative study http: //dx. doi. org/http: //pmj. sagepub. com/content/early/2011/04/07/0269216311401947 Macfadyen A, Swallow V, Santacroce S, Lambert H (2011) Involving fathers in research. Jn. for Specialists in Pediatric Nursing http: //dx. doi. org/10. 1111/j. 1744 -6155. 2011. 00287. x Knafl K, Deatrick JA, Gallo A, Dixon J, Grey M, Knafl G, O'Malley J: Assessment of the Psychometric Properties of the Family Management Measure. J Pediatr Psychol 2009: 36, 6: Swallow V, Clarke C, Campbell S, Lambert H. Nurses as family learning brokers: shared management in childhood chronic kidney disease. Journal of Nursing and Healthcare of Chronic Illness. 2009; 1: 49 -59 Swallow V, Lambert H, Clarke C, Campbell S, Jacoby A. Childhood chronic-kidney-disease: A longitudinal-qualitative study of families learning to share management Patient Education & Counseling. 2008; 73: 354 -62 http: //dx. doi. org/10. 1016/j. pec. 2008. 07. 052 Swallow V. An exploration of mothers' and fathers' views of their identities in chronic-kidney-disease management: parents as students? Journal of Clinical Nursing. 2008; 17: 3177 -86 http: //dx. doi. org/10. 1111/j. 1365 -2702. 2008. 02642. x DOH. National Service Framework for Renal Services: Working for Children and Young People. London 2006: 14 Gavin, L. and T. Wysocki (2006). "Associations of paternal involvement in disease management with maternal and family outcomes in families of children with chronic illnesses. " Journal of Pediatric Psychology 31(5): 481 -489
Some references: Swallow V, Macfadyen A, Lambert H, Santacroce S. Fathers’ contributions to management of their children’s long-term medical conditions: a narrative review of the literature. Health Expectations. 2011 http: //dx. doi. org/10. 1111/j. 1369 -7625. 2011. 00674. x Swallow V, Lambert H, Santacroce S, Macfadyen A. Fathers and mothers developing skills in managing children’s long-term medical conditions : how do their qualitative accounts compare? Child: Care Health & Development. 2011 http: //dx. doi. org/10. 1111/j. 1365 -2214. 2011. 01219. x Swallow V, Macfadyen A, Forrester T (2011) Teenagers’ and parents’ views of a short break service for children with lifelimiting conditions: a qualitative study http: //dx. doi. org/http: //pmj. sagepub. com/content/early/2011/04/07/0269216311401947 Macfadyen A, Swallow V, Santacroce S, Lambert H (2011) Involving fathers in research. Jn. for Specialists in Pediatric Nursing http: //dx. doi. org/10. 1111/j. 1744 -6155. 2011. 00287. x Knafl K, Deatrick JA, Gallo A, Dixon J, Grey M, Knafl G, O'Malley J: Assessment of the Psychometric Properties of the Family Management Measure. J Pediatr Psychol 2009: 36, 6: Swallow V, Clarke C, Campbell S, Lambert H. Nurses as family learning brokers: shared management in childhood chronic kidney disease. Journal of Nursing and Healthcare of Chronic Illness. 2009; 1: 49 -59 Swallow V, Lambert H, Clarke C, Campbell S, Jacoby A. Childhood chronic-kidney-disease: A longitudinal-qualitative study of families learning to share management Patient Education & Counseling. 2008; 73: 354 -62 http: //dx. doi. org/10. 1016/j. pec. 2008. 07. 052 Swallow V. An exploration of mothers' and fathers' views of their identities in chronic-kidney-disease management: parents as students? Journal of Clinical Nursing. 2008; 17: 3177 -86 http: //dx. doi. org/10. 1111/j. 1365 -2702. 2008. 02642. x DOH. National Service Framework for Renal Services: Working for Children and Young People. London 2006: 14 Gavin, L. and T. Wysocki (2006). "Associations of paternal involvement in disease management with maternal and family outcomes in families of children with chronic illnesses. " Journal of Pediatric Psychology 31(5): 481 -489


