ed9c6157b6cdf317c6107cf982eba10b.ppt
- Количество слайдов: 71

Childhood Disability
Aims n n n What is childhood disability? Common causes of and disordered development, learning difficulties and disability and how to assess these children Cerebral palsy u Causes u Classification u Areas to be assessed at diagnosis
What do you understand by: n. Disorder n. Impairment n. Disability n. Handicap
Disorder n Medically definable condition or disease
Impairment n Loss or abnormality of psychological, physiological or anatomical structure of function
Disability n Any restriction of lack (resulting from an impairment) of ability to perform an activity in the manner or within the range considered normal for a child of that age
Handicap – social mod n The impact of the impairment or disability on the person’s pursuits or achievement of goals that are desired by him/her or expected by him/her by society.
But this is now out of date International classification of function - ICF Runs alongside ICD-10 Disease does not predict difficulty In all lives we will at times have difficulties in function Standard language classify function Joins together medical and social model
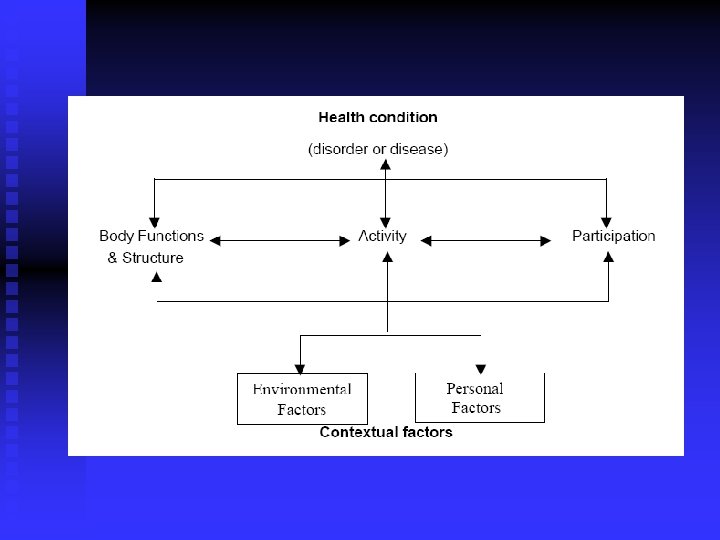
Disorder or disease
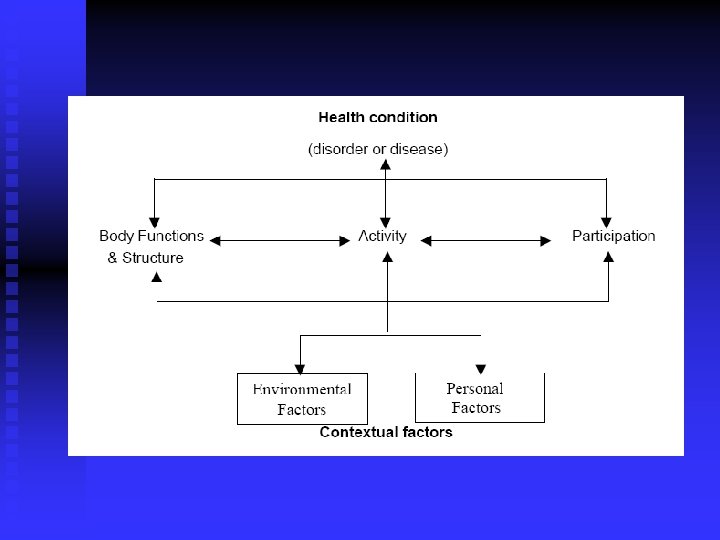
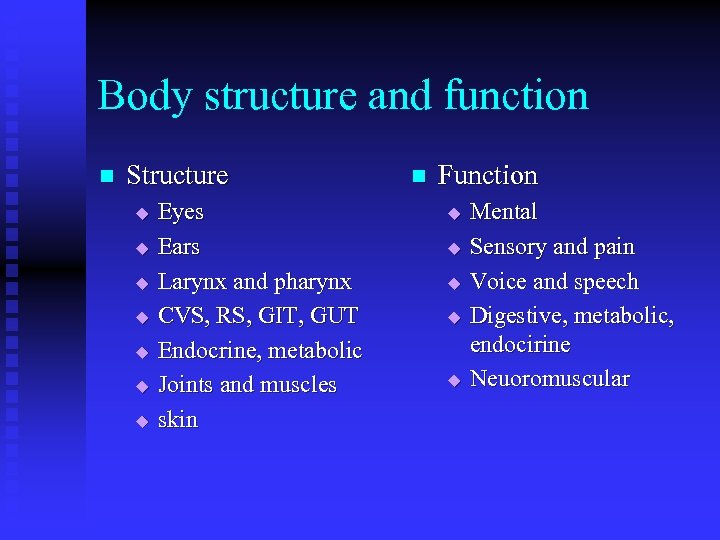
Body structure and function n Structure u u u u Eyes Ears Larynx and pharynx CVS, RS, GIT, GUT Endocrine, metabolic Joints and muscles skin n Function u u u Mental Sensory and pain Voice and speech Digestive, metabolic, endocirine Neuoromuscular
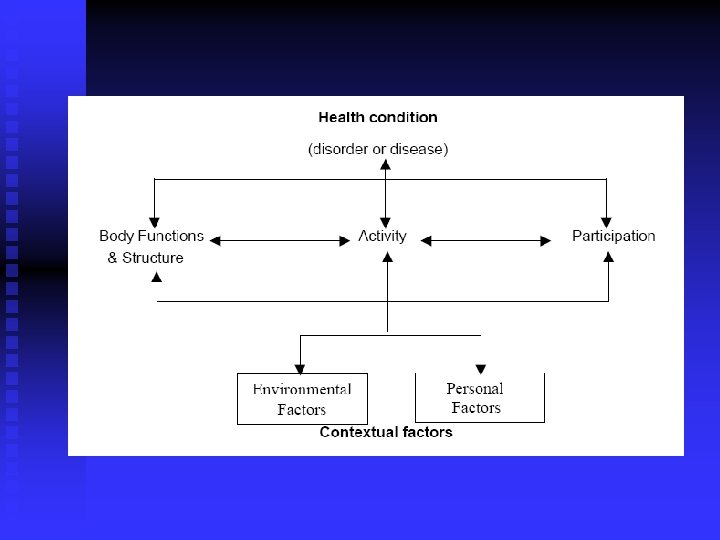
Activities and Participation Communication n Mobility n Self care n Domestic life n Interpersonal interactions and relationships n Learning and applying knowledge n Community, social and civic life n
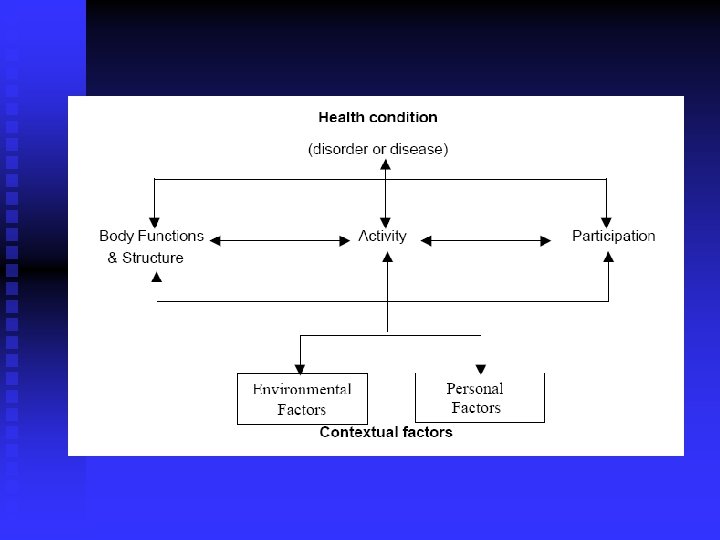
Contextural factors n Environment u u u Natural environment Man made environment Products and technology Support and relationships Services and policies Attitudes n Personal Factors u u u Mental health IQ Resilience
Examples n n Health Condition Impairment Activity Limitation Participation restrictions n n CP ASC Sensorineural deafness Diabetes mellitus

How can we use ICF? Individual n Service providers n Society n Policy development n Economic analysis n Research n
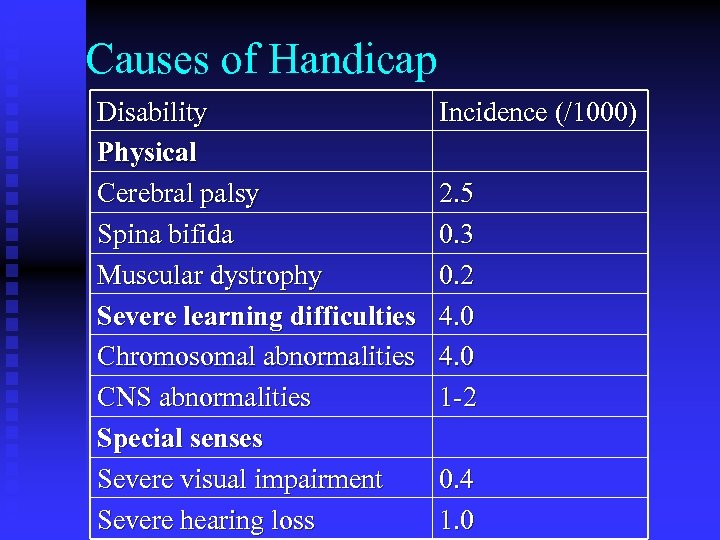
Causes of Handicap Disability Physical Cerebral palsy Spina bifida Muscular dystrophy Severe learning difficulties Chromosomal abnormalities CNS abnormalities Special senses Severe visual impairment Severe hearing loss Incidence (/1000) 2. 5 0. 3 0. 2 4. 0 1 -2 0. 4 1. 0
Presentation Antenatal concerns n At time of birth n Due to screening programmes n Family concerns n After acute severe illness n
Delayed development - warning signs n n At any age u Parental concern u Regression 10 weeks u not smiling

6 months warning signs Persistent primative reflexes u Persistent squint u Hand preference u Little interest in people, toys, noises u
10 -12 month warning signs Not sitting u No double syllable babble u No pincer grasp u
18 month warning signs n n n Not walking independently Fewer than 6 words Persistent mouthing / drooling
2 ½ year warning signs n No 2 -3 word sentences
4 year old Unintelligible speech
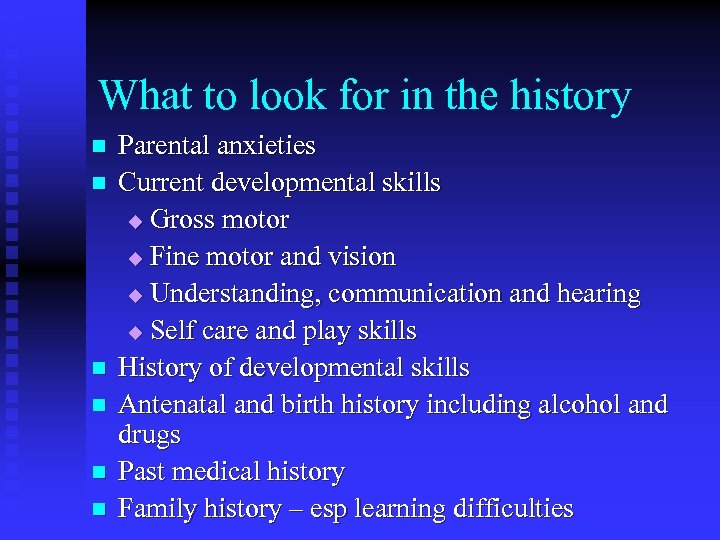
What to look for in the history n n n Parental anxieties Current developmental skills u Gross motor u Fine motor and vision u Understanding, communication and hearing u Self care and play skills History of developmental skills Antenatal and birth history including alcohol and drugs Past medical history Family history – esp learning difficulties
Examination n n Dysmorphic features Growth including head circumference General examination Neurological exam including fundi Current developmental skills u Gross motor u Fine motor and vision u Understanding, communication and hearing u Self care and play skills
What you might find: n Downs
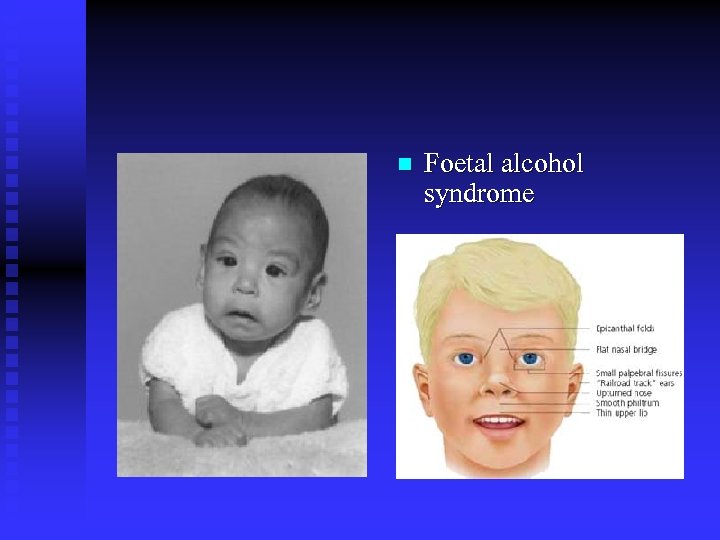
n Foetal alcohol syndrome
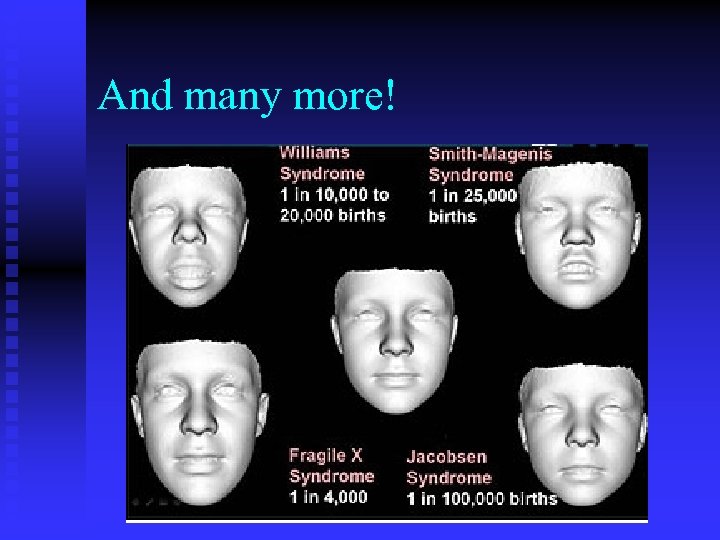
And many more!
Cerebral Palsy 2 -2. 5 children /1000
Aims What is CP n How do you classify CP n What Causes CP n Medical approach to a child with possible CP n
Cerebral palsy - definition Cerebral palsy (CP) describes a group of disorders of the development of movement and posture, causing activity limitation, that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain. The motor disorders of cerebral palsy are often accompanied by disturbances of sensation, cognition, communication, perception, and/or behaviour, and/or by a seizure disorder.
Cerebral palsy classification Motor impairment n Functional impairment n Associated impairments n Anatomical and radiological changes n Aetiology n
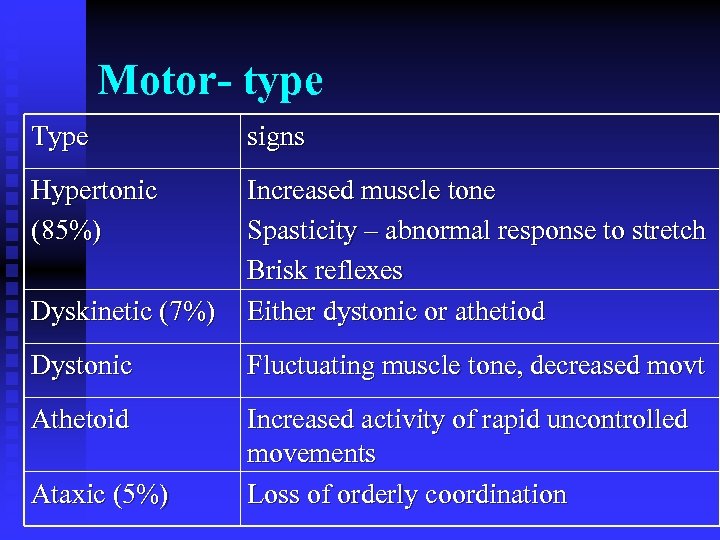
Motor- type Type signs Hypertonic (85%) Dyskinetic (7%) Increased muscle tone Spasticity – abnormal response to stretch Brisk reflexes Either dystonic or athetiod Dystonic Fluctuating muscle tone, decreased movt Athetoid Increased activity of rapid uncontrolled movements Loss of orderly coordination Ataxic (5%)
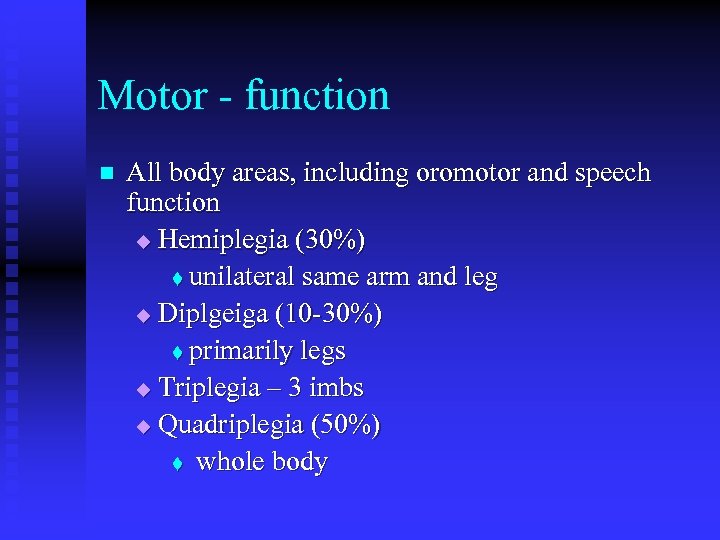
Motor - function n All body areas, including oromotor and speech function u Hemiplegia (30%) t unilateral same arm and leg u Diplgeiga (10 -30%) t primarily legs u Triplegia – 3 imbs u Quadriplegia (50%) t whole body
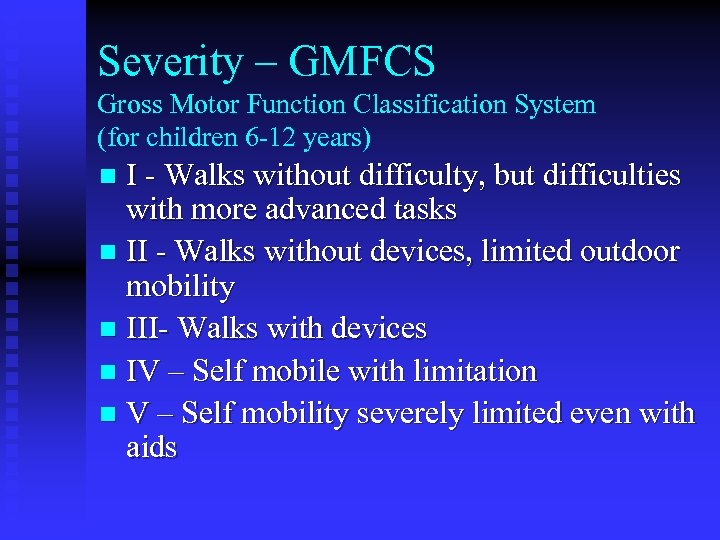
Severity – GMFCS Gross Motor Function Classification System (for children 6 -12 years) I - Walks without difficulty, but difficulties with more advanced tasks n II - Walks without devices, limited outdoor mobility n III- Walks with devices n IV – Self mobile with limitation n V – Self mobility severely limited even with aids n
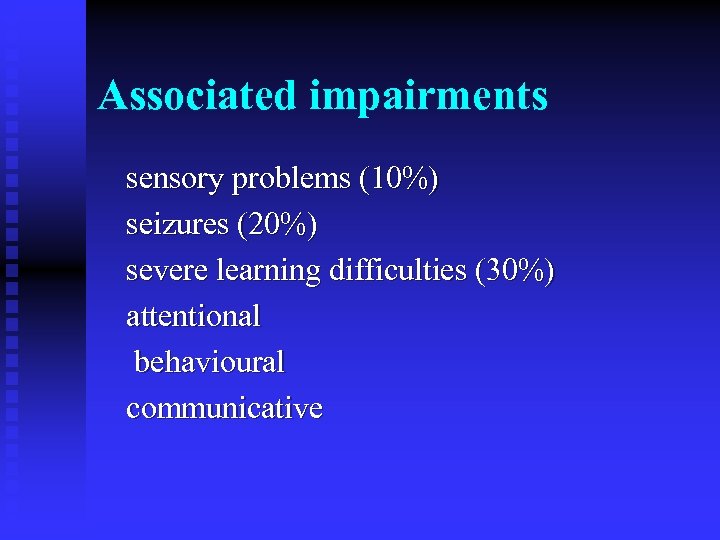
Associated impairments sensory problems (10%) seizures (20%) severe learning difficulties (30%) attentional behavioural communicative
Anatomical and radiological findings n Proposed anatomical site n Radiological findings: the neuroanatomic findings on computed tomography or magnetic resonance imaging, such as ventricular enlargement, white matter loss, or brain anomaly
Causation and timing Underlying cause if known e. g. meningitis / head injury/ brain malformation n Presumed timing n
Aetiology Over emphasis on intra partum asphyxia as a cause n 68% of children with CP have normal Apgar score and neuro neonatal exam (Nelson & n Ellenberg 1988) n 13% of those with CP had Apgar<5 and all had abnormal neuro exam
Aetiology n n Cause of most CP unknown but in 70 -80% cases due to pre- natal factors Intra partum asphyxia can & does occur in 1020%, causing hypoxic ischaemic brain injury (HIBI) u If this occurs <20 wks 27 -30 wks n migrational defects PVL 34 -40 wks parasagittal injury Although obstetric & neonatal care has improved, rates of CP have not fallen
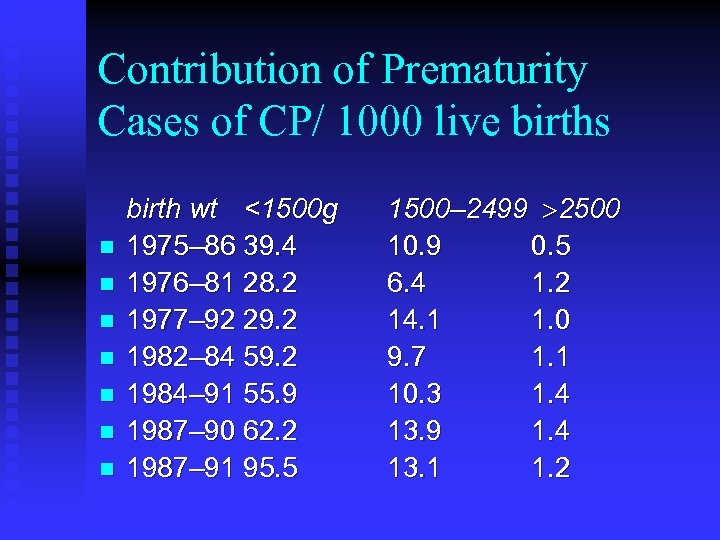
Contribution of Prematurity Cases of CP/ 1000 live births n n n n birth wt <1500 g 1975– 86 39. 4 1976– 81 28. 2 1977– 92 29. 2 1982– 84 59. 2 1984– 91 55. 9 1987– 90 62. 2 1987– 91 95. 5 1500– 2499 >2500 10. 9 0. 5 6. 4 1. 2 14. 1 1. 0 9. 7 1. 1 10. 3 1. 4 13. 9 1. 4 13. 1 1. 2
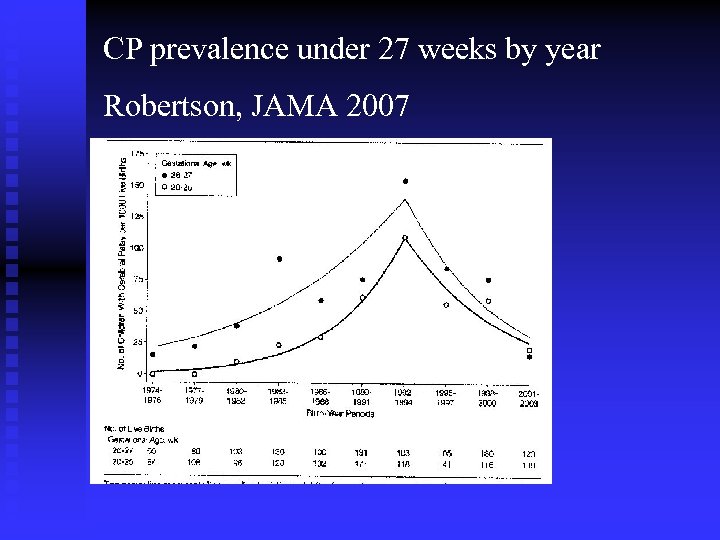
CP prevalence under 27 weeks by year Robertson, JAMA 2007
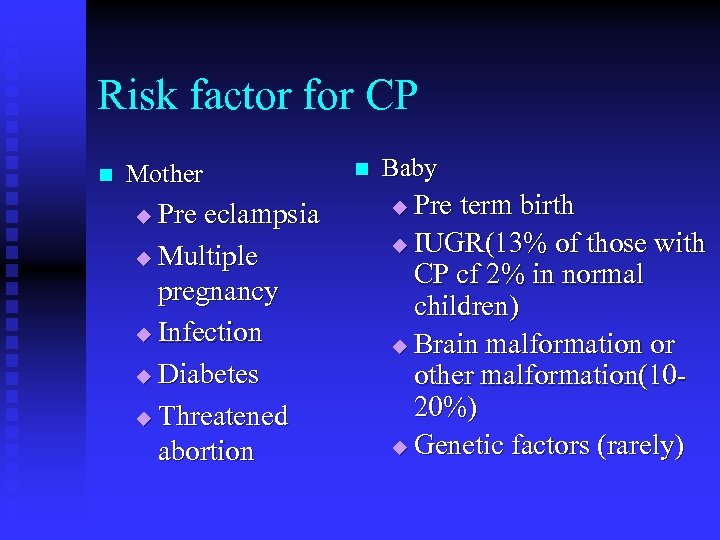
Risk factor for CP n Mother Pre eclampsia u Multiple pregnancy u Infection u Diabetes u Threatened abortion u n Baby Pre term birth u IUGR(13% of those with CP cf 2% in normal children) u Brain malformation or other malformation(1020%) u Genetic factors (rarely) u
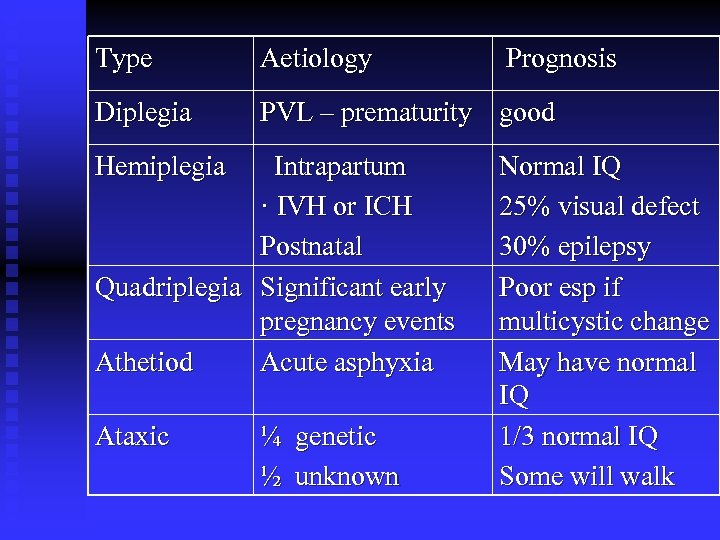
Type Aetiology Diplegia PVL – prematurity good Hemiplegia Intrapartum · IVH or ICH Postnatal Quadriplegia Significant early pregnancy events Athetiod Acute asphyxia Ataxic ¼ genetic ½ unknown Prognosis Normal IQ 25% visual defect 30% epilepsy Poor esp if multicystic change May have normal IQ 1/3 normal IQ Some will walk
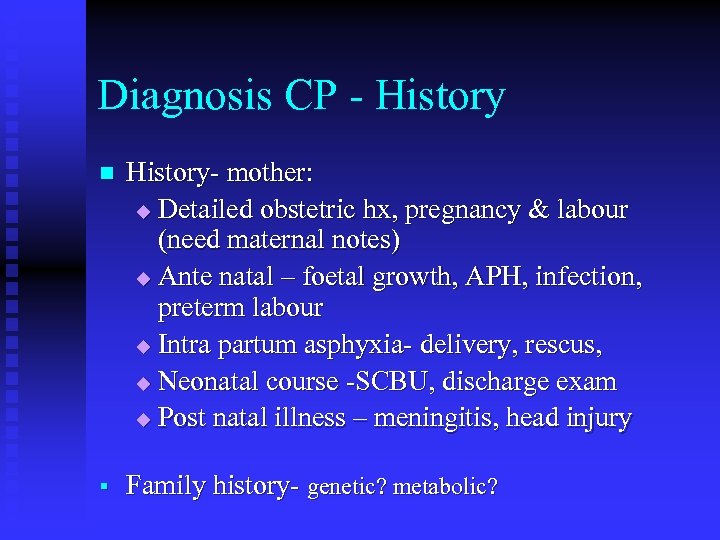
Diagnosis CP - History n History- mother: u Detailed obstetric hx, pregnancy & labour (need maternal notes) u Ante natal – foetal growth, APH, infection, preterm labour u Intra partum asphyxia- delivery, rescus, u Neonatal course -SCBU, discharge exam u Post natal illness – meningitis, head injury § Family history- genetic? metabolic?
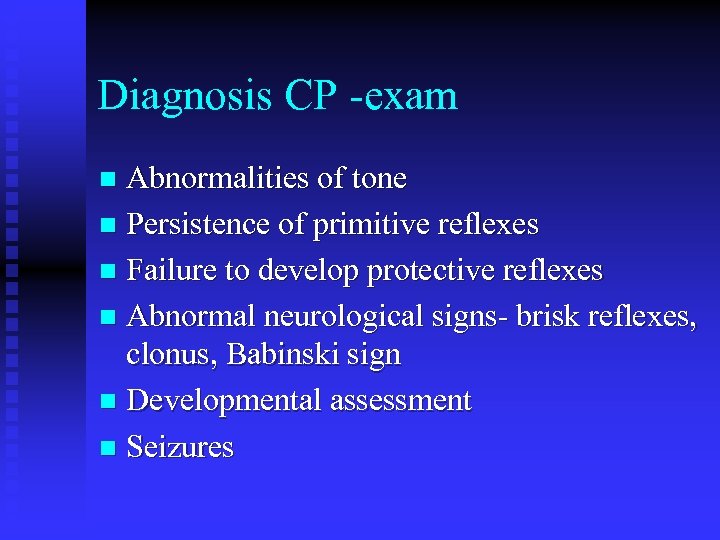
Diagnosis CP -exam Abnormalities of tone n Persistence of primitive reflexes n Failure to develop protective reflexes n Abnormal neurological signs- brisk reflexes, clonus, Babinski sign n Developmental assessment n Seizures n
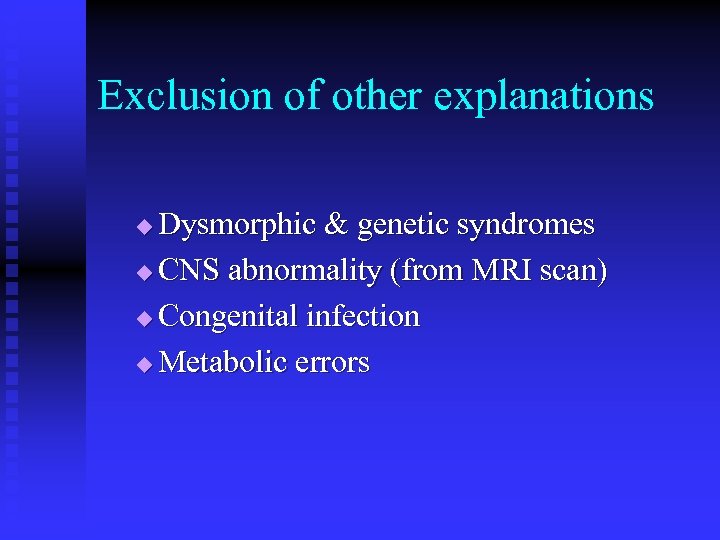
Exclusion of other explanations Dysmorphic & genetic syndromes u CNS abnormality (from MRI scan) u Congenital infection u Metabolic errors u
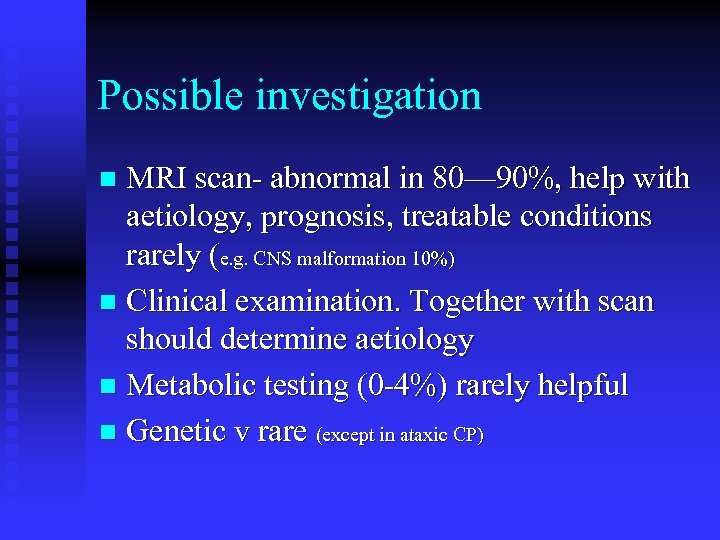
Possible investigation MRI scan- abnormal in 80— 90%, help with aetiology, prognosis, treatable conditions rarely (e. g. CNS malformation 10%) n Clinical examination. Together with scan should determine aetiology n Metabolic testing (0 -4%) rarely helpful n Genetic v rare (except in ataxic CP) n
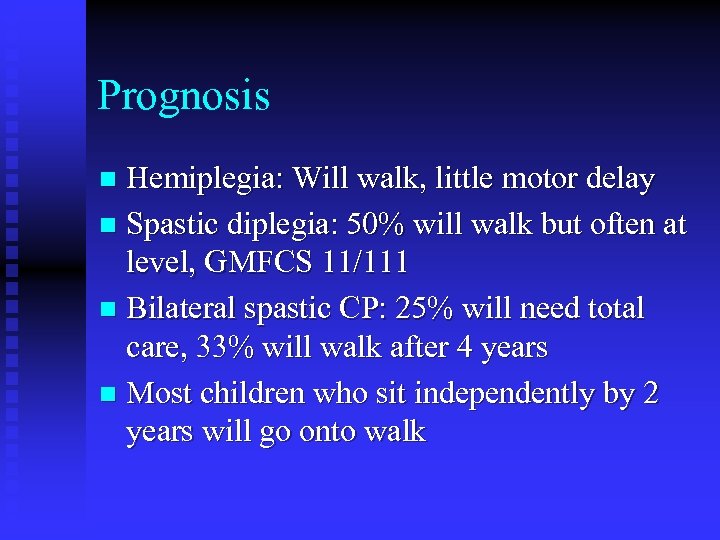
Prognosis Hemiplegia: Will walk, little motor delay n Spastic diplegia: 50% will walk but often at level, GMFCS 11/111 n Bilateral spastic CP: 25% will need total care, 33% will walk after 4 years n Most children who sit independently by 2 years will go onto walk n
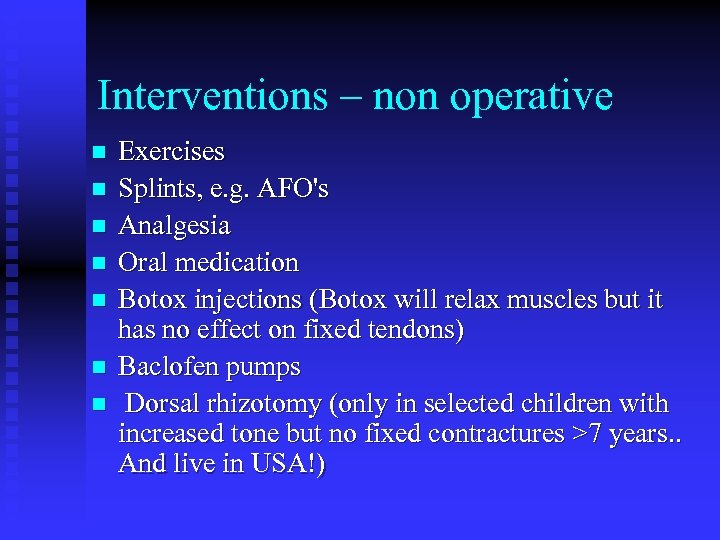
Interventions – non operative n n n n Exercises Splints, e. g. AFO's Analgesia Oral medication Botox injections (Botox will relax muscles but it has no effect on fixed tendons) Baclofen pumps Dorsal rhizotomy (only in selected children with increased tone but no fixed contractures >7 years. . And live in USA!)
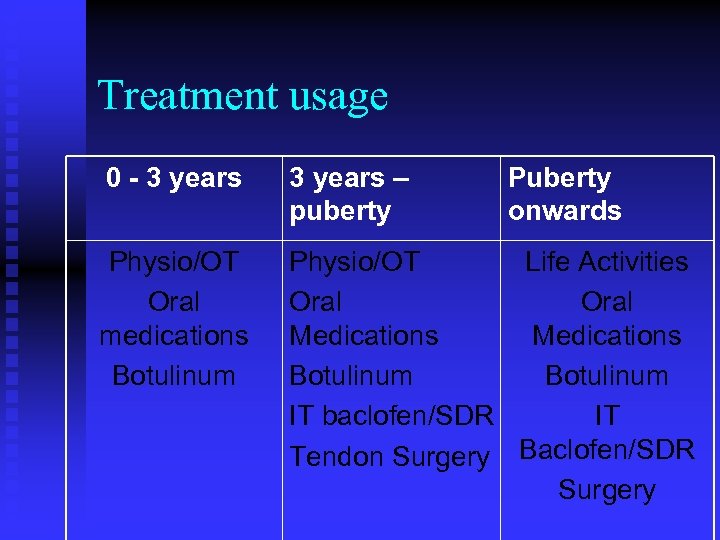
Treatment usage 0 - 3 years – puberty Physio/OT Oral medications Botulinum Physio/OT Life Activities Oral Medications Botulinum IT baclofen/SDR IT Tendon Surgery Baclofen/SDR Surgery Puberty onwards
CP- Orthopaedic complications Contractures n Dislocated hips n Scoliosis n
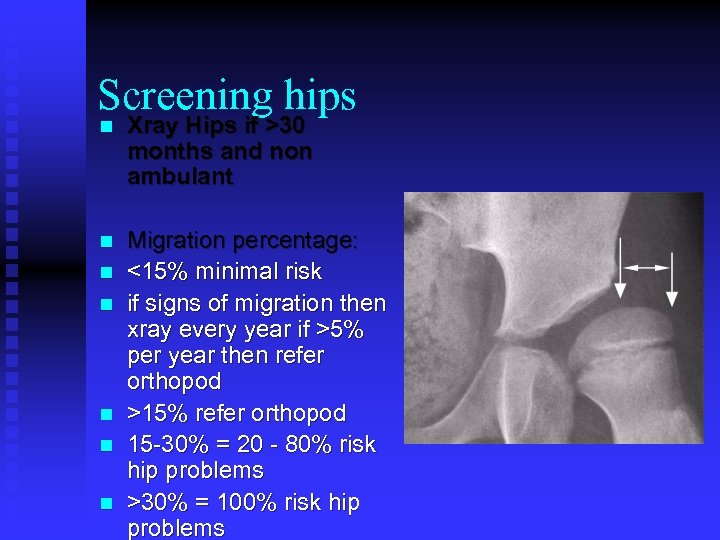
Screening hips n Xray Hips if >30 months and non ambulant n Migration percentage: <15% minimal risk if signs of migration then xray every year if >5% per year then refer orthopod >15% refer orthopod 15 -30% = 20 - 80% risk hip problems >30% = 100% risk hip problems n n n
Interventions – operative Aim of moving up one functional level Hips – when >30% subluxed n Soft tissues around hips / knees / ankles n Occasionally upper limbs / feet n Rarely the Spine n
Interventions - operative Realistic about outcome n Realistic about pain and difficulties and post op therapy n Realistic about the risks - there is a 1% mortality risk of surgery in cases of severe CP. n Optimise nutritional status n
This just thinks about the motor dificulties
Secondary disabilities Vision n Hearing n Learning (30% severe LD with 4 limb CP) n Behaviour n Sleep n
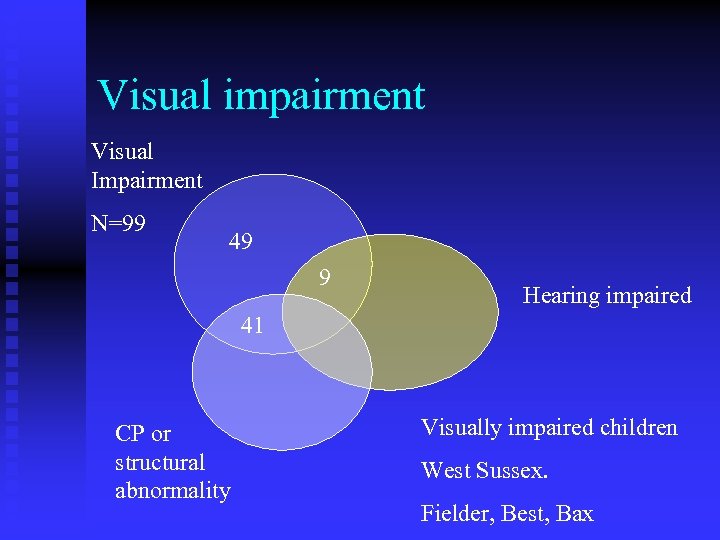
Visual impairment Visual Impairment N=99 49 9 Hearing impaired 41 CP or structural abnormality Visually impaired children West Sussex. Fielder, Best, Bax
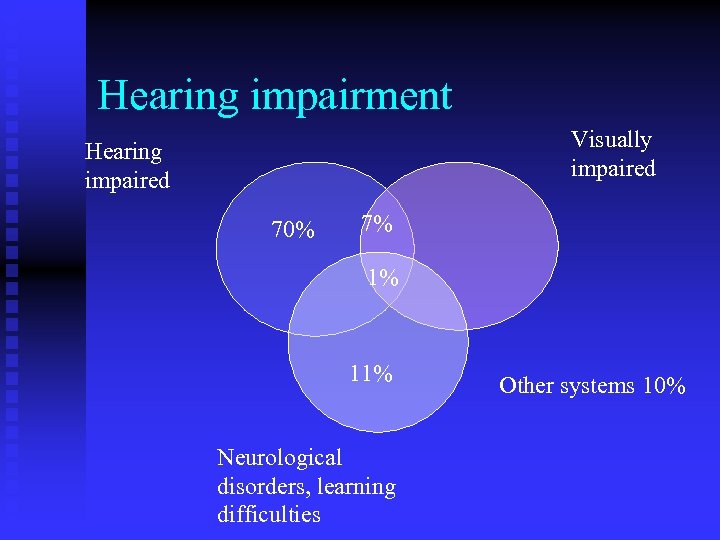
Hearing impairment Visually impaired Hearing impaired 70% 7% 1% 11% Neurological disorders, learning difficulties Other systems 10%
40% of children with learning disabilities have a diagnosable mental health problem
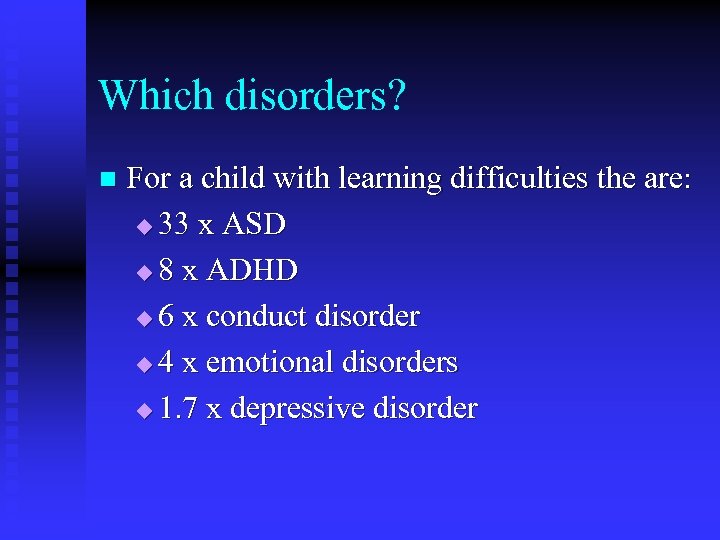
Which disorders? n For a child with learning difficulties the are: u 33 x ASD u 8 x ADHD u 6 x conduct disorder u 4 x emotional disorders u 1. 7 x depressive disorder
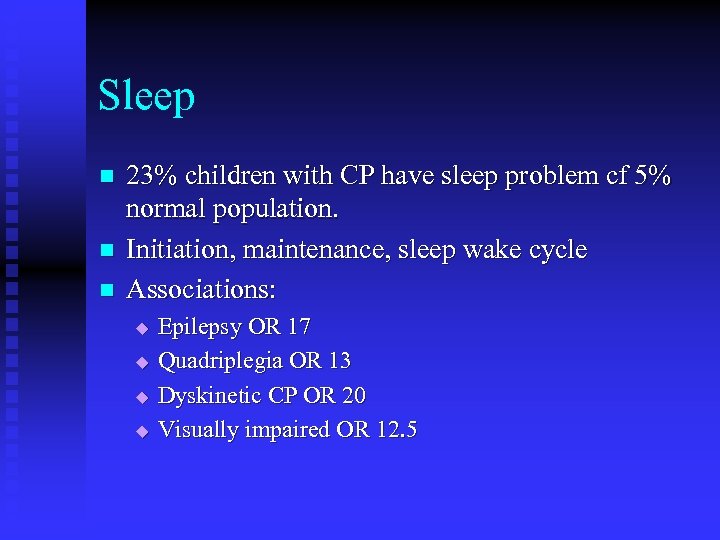
Sleep n n n 23% children with CP have sleep problem cf 5% normal population. Initiation, maintenance, sleep wake cycle Associations: u u Epilepsy OR 17 Quadriplegia OR 13 Dyskinetic CP OR 20 Visually impaired OR 12. 5
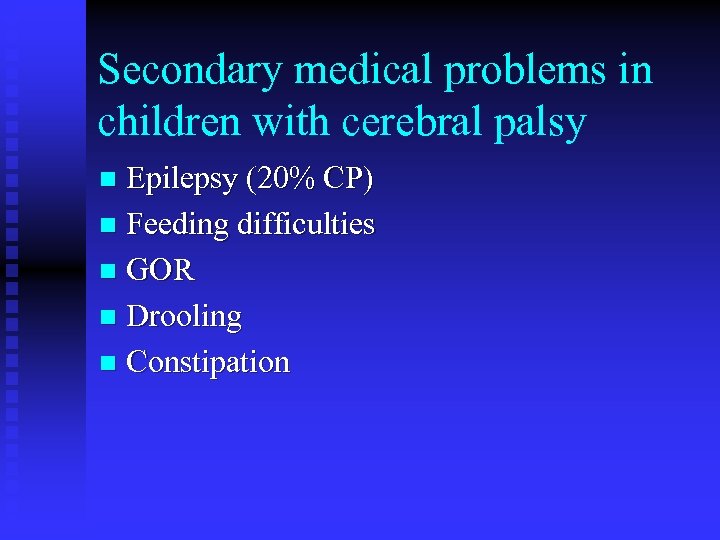
Secondary medical problems in children with cerebral palsy Epilepsy (20% CP) n Feeding difficulties n GOR n Drooling n Constipation n
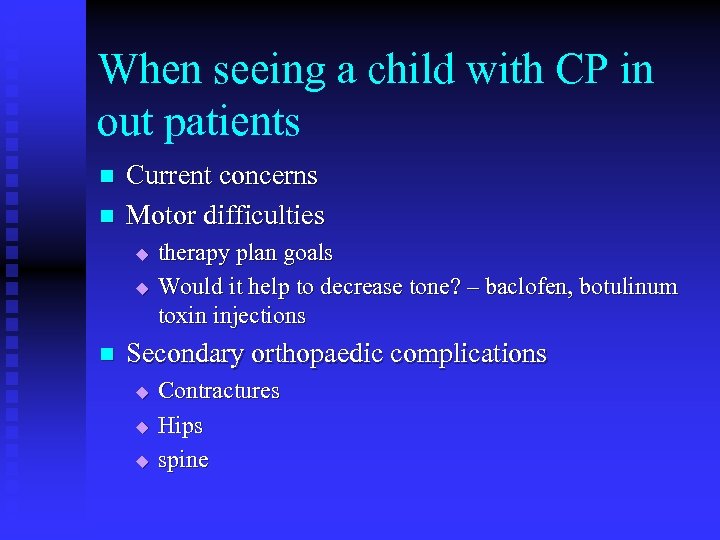
When seeing a child with CP in out patients n n Current concerns Motor difficulties u u n therapy plan goals Would it help to decrease tone? – baclofen, botulinum toxin injections Secondary orthopaedic complications u u u Contractures Hips spine
n Co-morbidities u u n Feeding / reflux constipation Seizures VP shunt Current function u u Vision / hearing communication Behaviour Sleep
n Situtation at home and school u Aids inc splints and wheelchair u Adaptations – home / school u Benefits u Support organisations u Short term breaks – if appropriate
Summary Many causes of cerebral palsy n Underlying cause cannot be treated n n It is important to address the other issues and complications so these children and families can lead normal lives

ed9c6157b6cdf317c6107cf982eba10b.ppt