be2949032b77cbe6b234b549e207b1dc.ppt
- Количество слайдов: 32
 Child Death Overview Panel and Rapid Response City and Hackney Dr Carla Stephen, Designated Dr for Child Death Children’s Services, Homerton University Hospital 22. 11. 13
Child Death Overview Panel and Rapid Response City and Hackney Dr Carla Stephen, Designated Dr for Child Death Children’s Services, Homerton University Hospital 22. 11. 13
 Aims of session At the end of this session you should be able to • Understand the role of your local CDOP • Understand the rapid response process and the contribution you can make • Be aware of the activity of your local CDOP
Aims of session At the end of this session you should be able to • Understand the role of your local CDOP • Understand the rapid response process and the contribution you can make • Be aware of the activity of your local CDOP
 Background • England is the first country to have national procedures for review of all child deaths. • Response to Inquiry into death of Victoria Climbie and the Every Child Matters Green Paper, 2003. • Introduced in Working Together to Safeguard Children, 2006.
Background • England is the first country to have national procedures for review of all child deaths. • Response to Inquiry into death of Victoria Climbie and the Every Child Matters Green Paper, 2003. • Introduced in Working Together to Safeguard Children, 2006.
 Background • Children Act 2004 & Working Together 2006 – Creation of Local Safeguarding Children Boards (LSCBs) by 2006 – LSCBs to review all child deaths in their area – LSCBs convene a CDOP for this purpose • Coroner’s Rules 1984 amendment in July 08 – Duty to notify deaths to LSCB – Power to provide information about deaths to LSCB
Background • Children Act 2004 & Working Together 2006 – Creation of Local Safeguarding Children Boards (LSCBs) by 2006 – LSCBs to review all child deaths in their area – LSCBs convene a CDOP for this purpose • Coroner’s Rules 1984 amendment in July 08 – Duty to notify deaths to LSCB – Power to provide information about deaths to LSCB
 Background • Children and Young Persons Act 2008 – Registrars given duty to inform LSCB of death certificate information – Registrar General given duty to inform Secretary of State of all child deaths whether here or abroad • These powers allow for flow of information but their use depends on interpretation
Background • Children and Young Persons Act 2008 – Registrars given duty to inform LSCB of death certificate information – Registrar General given duty to inform Secretary of State of all child deaths whether here or abroad • These powers allow for flow of information but their use depends on interpretation
 Why review all deaths? • Evidence based interventions to prevent child deaths • Public health information about patterns of child death • Interagency working to safeguard children and promote their welfare • Statutory requirement, moral imperative and public expectation to promote learning and transparency
Why review all deaths? • Evidence based interventions to prevent child deaths • Public health information about patterns of child death • Interagency working to safeguard children and promote their welfare • Statutory requirement, moral imperative and public expectation to promote learning and transparency
 CDOP City and Hackney CDOP • • Subcommittee of CHSCB Operating 6 yrs Reviewed total of 153 deaths Deaths of all children under 18 yrs resident in Hackney reviewed – includes <23/40 gest • Determines any modifiable factors in prevention of death • Standardised national dataset
CDOP City and Hackney CDOP • • Subcommittee of CHSCB Operating 6 yrs Reviewed total of 153 deaths Deaths of all children under 18 yrs resident in Hackney reviewed – includes <23/40 gest • Determines any modifiable factors in prevention of death • Standardised national dataset
 CDOP Multidisciplinary panel • Independent chair –Dep Dir Public Health • • Paediatrics, Neonates, Paediatric Pathology, General Practice, mental health, safeguarding, nursing and midwifery Social care – Children’s Social Care Police - CAIT Education - HLT Youth crime reduction Coordinator
CDOP Multidisciplinary panel • Independent chair –Dep Dir Public Health • • Paediatrics, Neonates, Paediatric Pathology, General Practice, mental health, safeguarding, nursing and midwifery Social care – Children’s Social Care Police - CAIT Education - HLT Youth crime reduction Coordinator
 CDOP Core Functions • • Prevent future deaths Id risks and trends assoc with child death Timely, accurate cause of death reporting Ensure rapid response for unexpected deaths • Liaise with agencies about preventable factors and lessons learned
CDOP Core Functions • • Prevent future deaths Id risks and trends assoc with child death Timely, accurate cause of death reporting Ensure rapid response for unexpected deaths • Liaise with agencies about preventable factors and lessons learned
 CDOP Core Functions • Advise CHSCB re training/resources for interagency working • Share information with Police and Coroner • Notify CHSCB if s 47 or SCR needed • Collate and submit minimum datasets • Locally implement regional/national initiatives
CDOP Core Functions • Advise CHSCB re training/resources for interagency working • Share information with Police and Coroner • Notify CHSCB if s 47 or SCR needed • Collate and submit minimum datasets • Locally implement regional/national initiatives
 CDOP Procedure • • • Notification of death to SPOC (Kerry Littleford) Notification protocol – multiagency Form A Request for information via Form B Form C prepared by SPOC Unexpected deaths managed through RR Expected deaths discussed at quarterly CDOP meetings • Deaths classified and modifiable factors det. • Publication in anonymised form annually
CDOP Procedure • • • Notification of death to SPOC (Kerry Littleford) Notification protocol – multiagency Form A Request for information via Form B Form C prepared by SPOC Unexpected deaths managed through RR Expected deaths discussed at quarterly CDOP meetings • Deaths classified and modifiable factors det. • Publication in anonymised form annually
 Rapid Response • Subcommittee of CDOP which considers all unexpected child deaths i. e. not expected within previous 24 hrs or unanticipated collapse leading to death • Functions – – – Enquire into reasons and circumstances of death Identify and safeguard other children in the home Understand challenge organisation’s roles Bereavement support for family Collect standardised data set and report to CDOP
Rapid Response • Subcommittee of CDOP which considers all unexpected child deaths i. e. not expected within previous 24 hrs or unanticipated collapse leading to death • Functions – – – Enquire into reasons and circumstances of death Identify and safeguard other children in the home Understand challenge organisation’s roles Bereavement support for family Collect standardised data set and report to CDOP
 Rapid Response Procedure • • Notification of death to SPOC Notification of death to local agencies by protocol Request for information from agencies- Form B Decision taken by Designated Dr for Child Death to call a Rapid Response meeting – usually within 1 wk of notification. • Submission of information about child and family held by agencies to SPOC and CDOP • Coroner investigates death and post mortem carried out as appropriate
Rapid Response Procedure • • Notification of death to SPOC Notification of death to local agencies by protocol Request for information from agencies- Form B Decision taken by Designated Dr for Child Death to call a Rapid Response meeting – usually within 1 wk of notification. • Submission of information about child and family held by agencies to SPOC and CDOP • Coroner investigates death and post mortem carried out as appropriate
 Rapid Response Procedure • Meeting chaired by Des. Dr for Child Death • Professionals meet to share information and discuss post mortem preliminary results if available • Whole life history of child and family considered • Areas of risk/concern identified and recommendations made • Minutes circulated and further information gathered • Second meeting may be called to discuss final post mortem results • Findings submitted to CDOP for classification. • Referral for SCR made to SCR Subc where needed
Rapid Response Procedure • Meeting chaired by Des. Dr for Child Death • Professionals meet to share information and discuss post mortem preliminary results if available • Whole life history of child and family considered • Areas of risk/concern identified and recommendations made • Minutes circulated and further information gathered • Second meeting may be called to discuss final post mortem results • Findings submitted to CDOP for classification. • Referral for SCR made to SCR Subc where needed
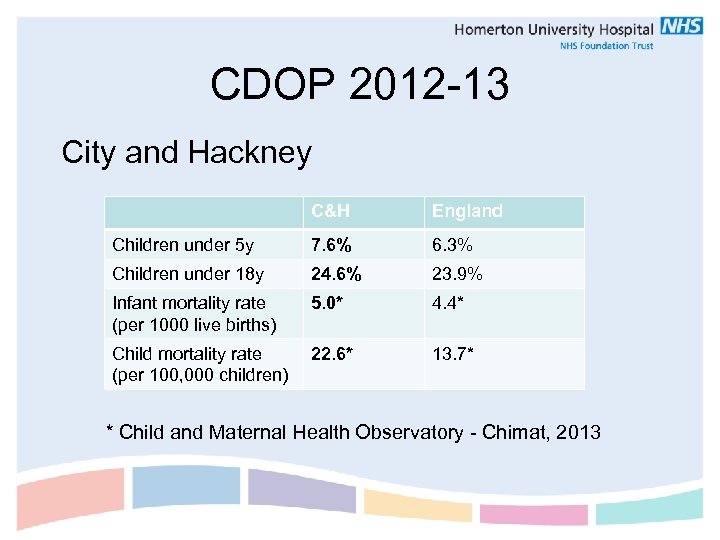 CDOP 2012 -13 City and Hackney C&H England Children under 5 y 7. 6% 6. 3% Children under 18 y 24. 6% 23. 9% Infant mortality rate (per 1000 live births) 5. 0* 4. 4* Child mortality rate (per 100, 000 children) 22. 6* 13. 7* * Child and Maternal Health Observatory - Chimat, 2013
CDOP 2012 -13 City and Hackney C&H England Children under 5 y 7. 6% 6. 3% Children under 18 y 24. 6% 23. 9% Infant mortality rate (per 1000 live births) 5. 0* 4. 4* Child mortality rate (per 100, 000 children) 22. 6* 13. 7* * Child and Maternal Health Observatory - Chimat, 2013
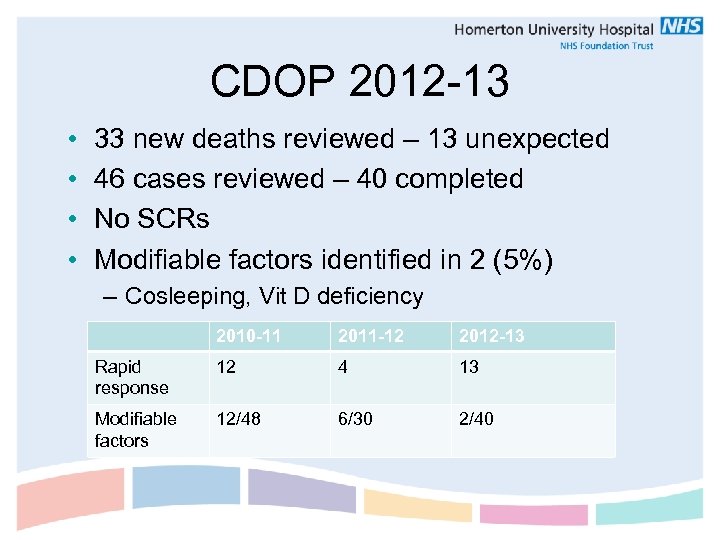 CDOP 2012 -13 • • 33 new deaths reviewed – 13 unexpected 46 cases reviewed – 40 completed No SCRs Modifiable factors identified in 2 (5%) – Cosleeping, Vit D deficiency 2010 -11 2011 -12 2012 -13 Rapid response 12 4 13 Modifiable factors 12/48 6/30 2/40
CDOP 2012 -13 • • 33 new deaths reviewed – 13 unexpected 46 cases reviewed – 40 completed No SCRs Modifiable factors identified in 2 (5%) – Cosleeping, Vit D deficiency 2010 -11 2011 -12 2012 -13 Rapid response 12 4 13 Modifiable factors 12/48 6/30 2/40
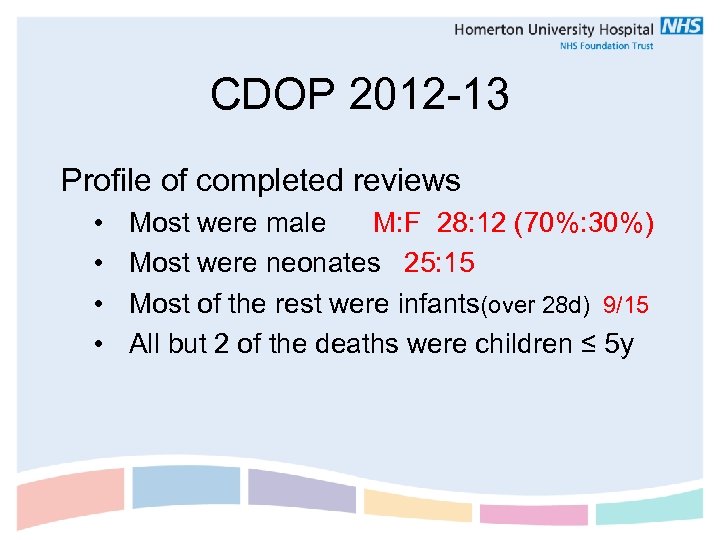 CDOP 2012 -13 Profile of completed reviews • • Most were male M: F 28: 12 (70%: 30%) Most were neonates 25: 15 Most of the rest were infants(over 28 d) 9/15 All but 2 of the deaths were children ≤ 5 y
CDOP 2012 -13 Profile of completed reviews • • Most were male M: F 28: 12 (70%: 30%) Most were neonates 25: 15 Most of the rest were infants(over 28 d) 9/15 All but 2 of the deaths were children ≤ 5 y
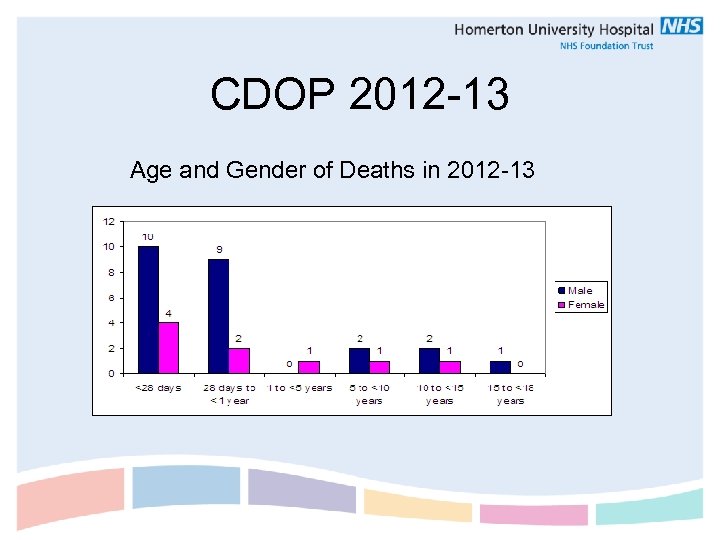 CDOP 2012 -13 Age and Gender of Deaths in 2012 -13
CDOP 2012 -13 Age and Gender of Deaths in 2012 -13
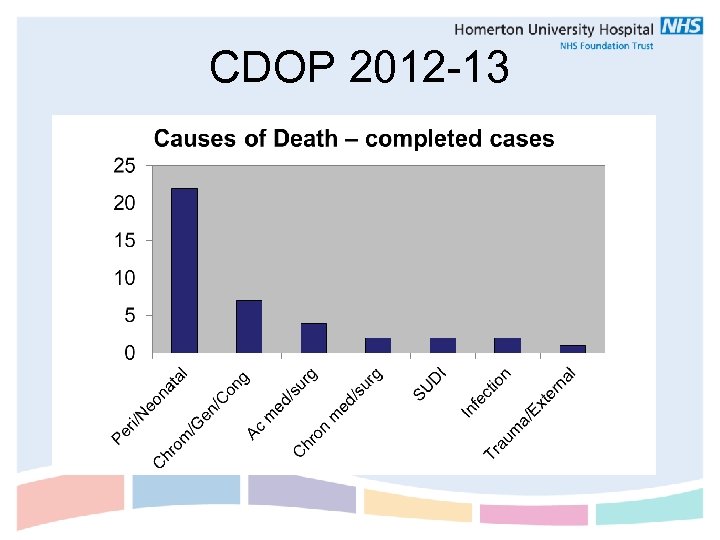
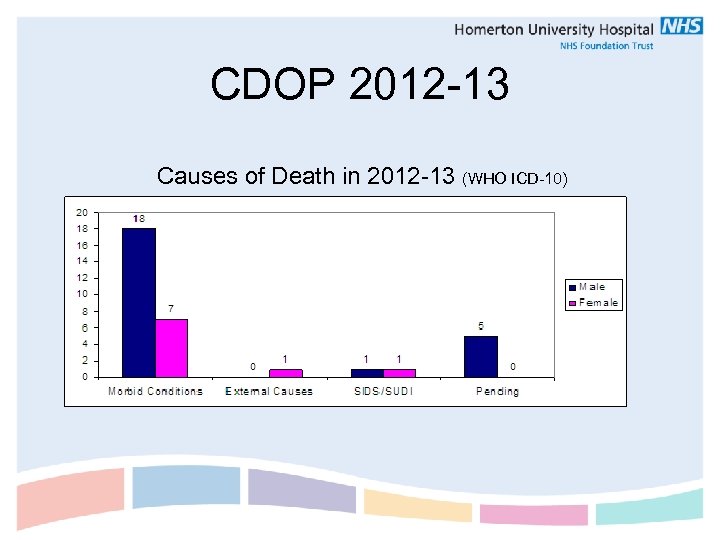 CDOP 2012 -13 Causes of Death in 2012 -13 (WHO ICD-10)
CDOP 2012 -13 Causes of Death in 2012 -13 (WHO ICD-10)
 CDOP 2012 -13
CDOP 2012 -13
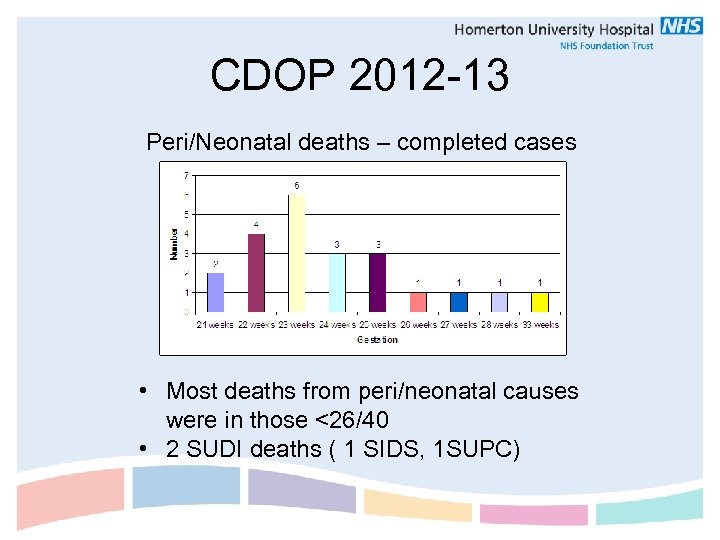 CDOP 2012 -13 Peri/Neonatal deaths – completed cases • Most deaths from peri/neonatal causes were in those <26/40 • 2 SUDI deaths ( 1 SIDS, 1 SUPC)
CDOP 2012 -13 Peri/Neonatal deaths – completed cases • Most deaths from peri/neonatal causes were in those <26/40 • 2 SUDI deaths ( 1 SIDS, 1 SUPC)
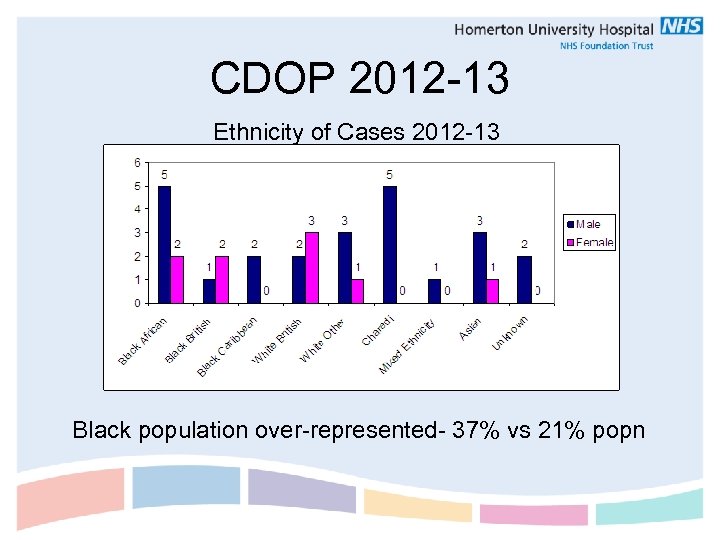 CDOP 2012 -13 Ethnicity of Cases 2012 -13 Black population over-represented- 37% vs 21% popn
CDOP 2012 -13 Ethnicity of Cases 2012 -13 Black population over-represented- 37% vs 21% popn
 CDOP 2012 -13 Geographical variation • City of London – 0 deaths • Hackney – no statistical difference between areas of varying Multiple Deprivation scores Seasonal variability • Slight increase in spring and autumn but not statistically significant
CDOP 2012 -13 Geographical variation • City of London – 0 deaths • Hackney – no statistical difference between areas of varying Multiple Deprivation scores Seasonal variability • Slight increase in spring and autumn but not statistically significant
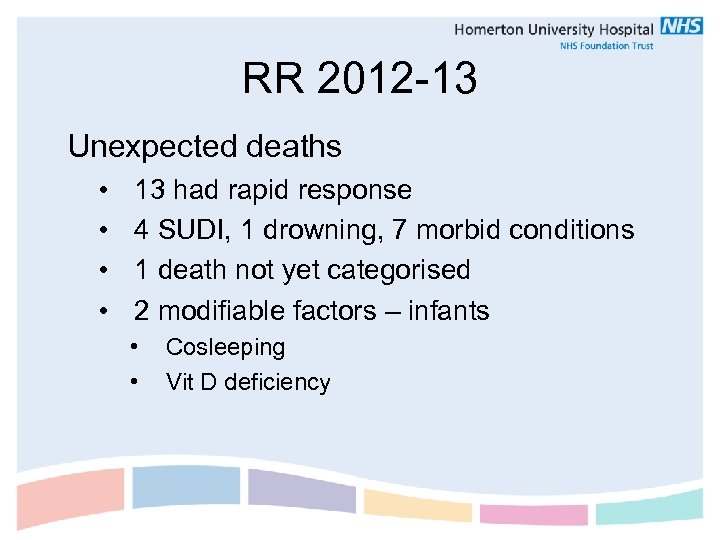 RR 2012 -13 Unexpected deaths • • 13 had rapid response 4 SUDI, 1 drowning, 7 morbid conditions 1 death not yet categorised 2 modifiable factors – infants • • Cosleeping Vit D deficiency
RR 2012 -13 Unexpected deaths • • 13 had rapid response 4 SUDI, 1 drowning, 7 morbid conditions 1 death not yet categorised 2 modifiable factors – infants • • Cosleeping Vit D deficiency
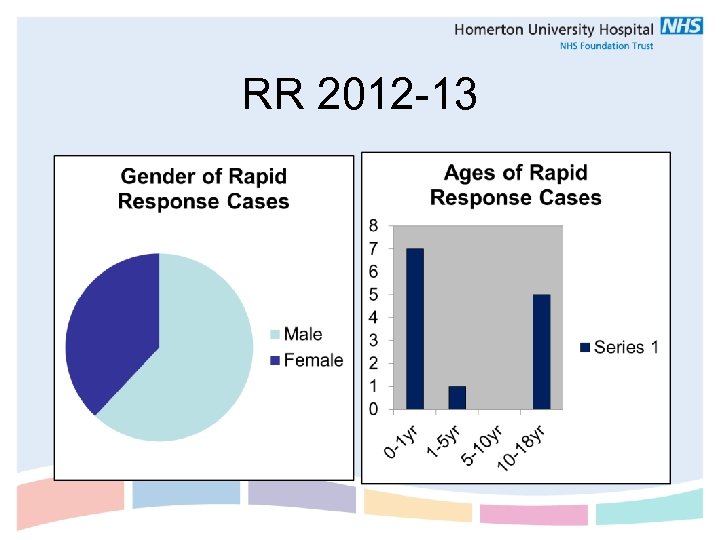 RR 2012 -13
RR 2012 -13
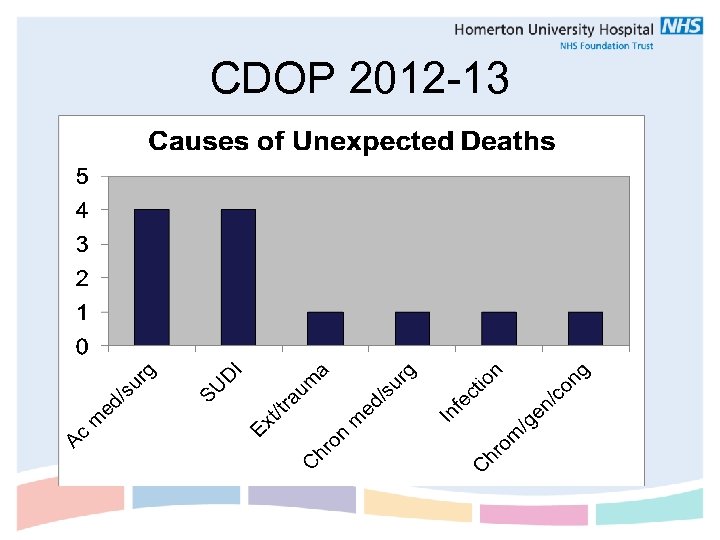 CDOP 2012 -13
CDOP 2012 -13
 CDOP 2012 -13 • Cardiac deaths - 4 • Cardiomyopathy, MI post transplant, HLH • • Asthma TTP Infection in child with cong. neuro abn SUDI • 3 SIDS, 1 SUPC
CDOP 2012 -13 • Cardiac deaths - 4 • Cardiomyopathy, MI post transplant, HLH • • Asthma TTP Infection in child with cong. neuro abn SUDI • 3 SIDS, 1 SUPC
 CDOP Recommendations • Sharing hospital discharge summaries with Community services • Ensuring family referral for genetic counselling where appropriate • Completed review of A&E fever management policy for premature infants • SIDS staff training via FSID and in children’s centre staff newsletter • Asthma integrated care pathway • Universal Vit D supplements via Healthy Start
CDOP Recommendations • Sharing hospital discharge summaries with Community services • Ensuring family referral for genetic counselling where appropriate • Completed review of A&E fever management policy for premature infants • SIDS staff training via FSID and in children’s centre staff newsletter • Asthma integrated care pathway • Universal Vit D supplements via Healthy Start
 Your Contribution as GP • Provide information about child and family (Form B) • general health, specialist input, antenatal info, compliance (medication, vaccines), mental health of parents, family dynamics, safeguarding concerns You may know that family the best! • • Attending rapid response meeting Bereavement support Arranging referrals/screening for family Implementing learning into practice
Your Contribution as GP • Provide information about child and family (Form B) • general health, specialist input, antenatal info, compliance (medication, vaccines), mental health of parents, family dynamics, safeguarding concerns You may know that family the best! • • Attending rapid response meeting Bereavement support Arranging referrals/screening for family Implementing learning into practice
 “…. . Every family has the right to have their child’s death properly investigated. Families desperately want to know what happened, how the events could have occurred, what the cause of death was, and whether it could have been prevented. This is important in terms of grieving”. Baroness Helena Kennedy QC, 2007.
“…. . Every family has the right to have their child’s death properly investigated. Families desperately want to know what happened, how the events could have occurred, what the cause of death was, and whether it could have been prevented. This is important in terms of grieving”. Baroness Helena Kennedy QC, 2007.
 Useful contacts Marcia Smikle, Head of Nursing – Community marcia. smikle@homerton. nhs. uk Tel: 0207 683 4691/4314 Kerry Littleford, CDOP Coordinator and SPOC kerry. littleford@hackney. gov. uk Tel: 0208 356 4175 Dr Carla Stephen, Designated Dr for Child Death carla. stephen@homerton. nhs. uk Tel: 0207 683 4772
Useful contacts Marcia Smikle, Head of Nursing – Community marcia. smikle@homerton. nhs. uk Tel: 0207 683 4691/4314 Kerry Littleford, CDOP Coordinator and SPOC kerry. littleford@hackney. gov. uk Tel: 0208 356 4175 Dr Carla Stephen, Designated Dr for Child Death carla. stephen@homerton. nhs. uk Tel: 0207 683 4772


