2fca1025c3ffaee1b71685f4adda9966.ppt
- Количество слайдов: 71
Chest Radiography for the NICU Harbir Juj November, 2005
Introduction n n Basic radiographic principles in the NICU are similar to those elsewhere. However, there are unique disease processes and technical challenges in the NICU setting This presentation aims to offer a primer on key elements to consider when looking at chest radiographs in the NICU The presentation specifically addresses: n n n n n Features of normal neonatal CXR Lines and Tubes Respiratory Distress Syndrome Meconium Aspiration Syndrome Neonatal Pneumonia Transient Tachypnea of the Newborn Bronchopulmonary Dysplasia Air Leak Syndromes There are many other pulmonary, cardiac and congenital anomalies seen in NICU chest radiographs that are not addressed here
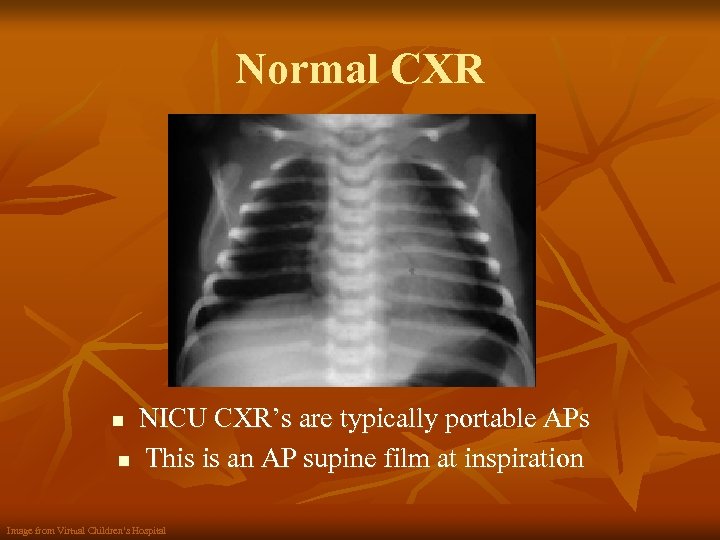
Normal CXR NICU CXR’s are typically portable APs n This is an AP supine film at inspiration n Image from Virtual Children’s Hospital
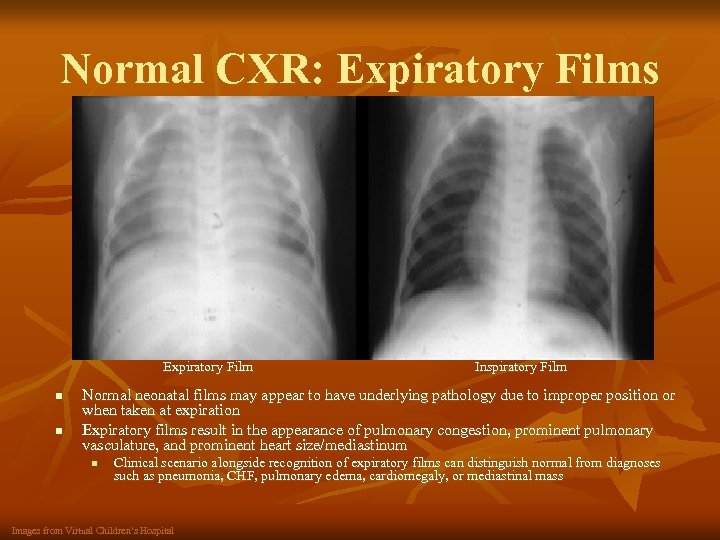
Normal CXR: Expiratory Films Expiratory Film n n Inspiratory Film Normal neonatal films may appear to have underlying pathology due to improper position or when taken at expiration Expiratory films result in the appearance of pulmonary congestion, prominent pulmonary vasculature, and prominent heart size/mediastinum n Clinical scenario alongside recognition of expiratory films can distinguish normal from diagnoses such as pneumonia, CHF, pulmonary edema, cardiomegaly, or mediastinal mass Images from Virtual Children’s Hospital
Normal CXR: Thymus n n n The thymus is a glandular organ located in the superior mediastinum, anterior to the heart and great vessels with variable size and contour In neonates and infants, a prominent thymus can give the semblance of pathology or even obscure an underlying abnormality The radiographs on the following slides are examples of normal thymic contour.
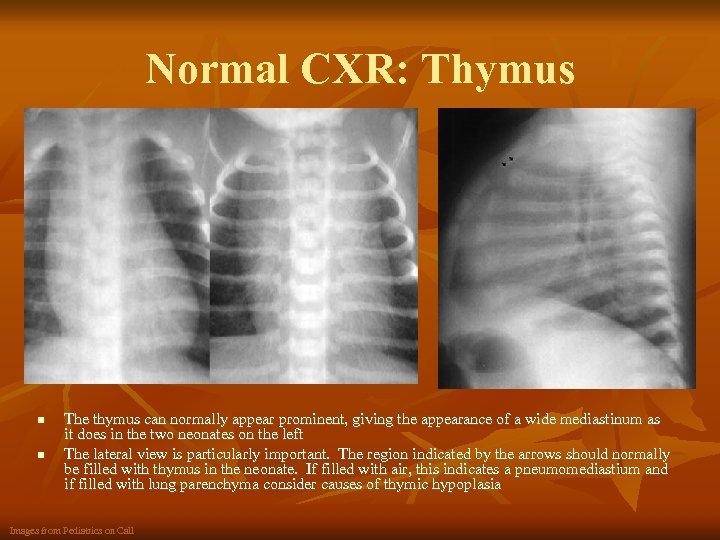
Normal CXR: Thymus n n The thymus can normally appear prominent, giving the appearance of a wide mediastinum as it does in the two neonates on the left The lateral view is particularly important. The region indicated by the arrows should normally be filled with thymus in the neonate. If filled with air, this indicates a pneumomediastium and if filled with lung parenchyma consider causes of thymic hypoplasia Images from Pediatrics on Call
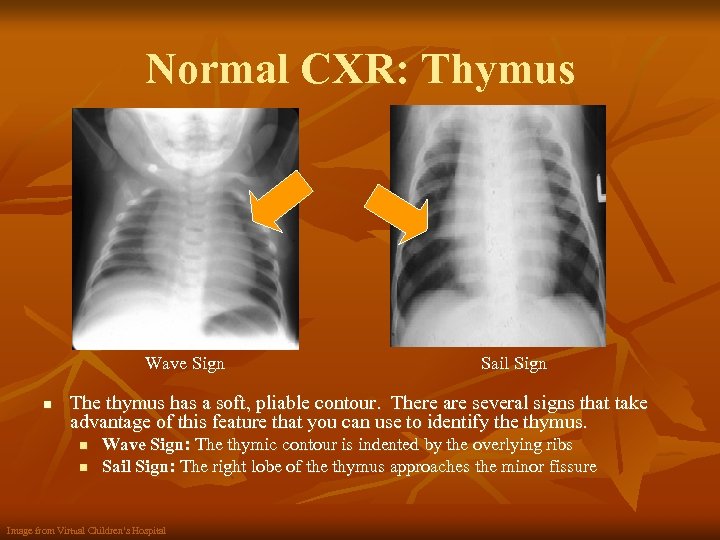
Normal CXR: Thymus Wave Sign n Sail Sign The thymus has a soft, pliable contour. There are several signs that take advantage of this feature that you can use to identify the thymus. n n Wave Sign: The thymic contour is indented by the overlying ribs Sail Sign: The right lobe of the thymus approaches the minor fissure Image from Virtual Children’s Hospital

Lines and Tubes n n It is important to evaluate each CXR for appropriate placement of lines and tubes The following slides address: n n Endotracheal tube Enteric tubes Umbilical artery catheter Umbilical vein catheter
Lines and Tubes ETT n n The ETT tip should be located halfway between the thoracic inlet and the carina Too low: the tip will usually enter the right mainstem bronchus n n Too high the tip will be above the clavicles n n May have asymmetric aeration with hyperaeration as well as atelectasis May have diffuse atelectasis Esophageal intubation n The tube may not match the trachea and there may be increased intestinal air proximally
Lines and Tubes Enteric Tubes n n The tip of the NGT or OGT should be in the body of the stomach Feeding tubes should terminate in the distal stomach or duodenum
Lines and Tubes UAC and UVC n UAC: can be placed “high” or “low” (based on institutional preference) n n High: tip between T 6 -T 9 Low: tip between L 3 -L 5 UVC: tip at junction of RA-IVC; just above diaphragm In order to determine appropriate line placement, it is necessary to distinguish between the UAC and UVC: n UAC: n n n Turns downward, then upward as it enters cord enroute to aorta on AP Generally projects on the left side of the spine on the AP UVC: n n Only projects in a cephalad direction on the AP Generally projects on the right side of the spine on the AP
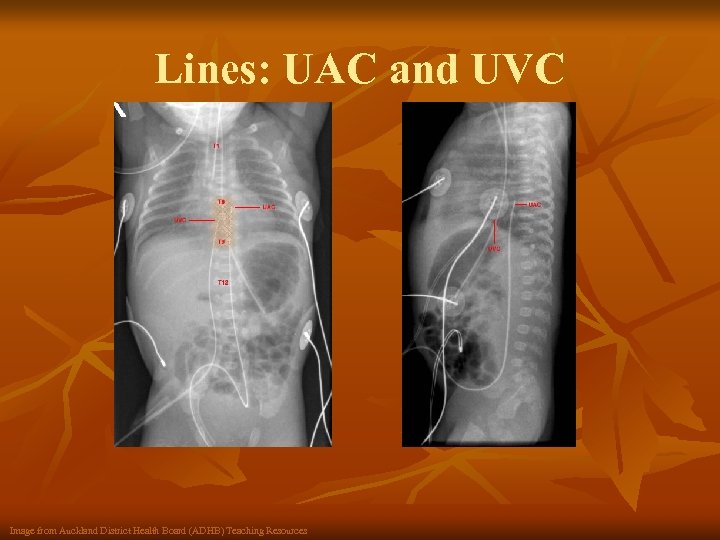
Lines: UAC and UVC Image from Auckland District Health Board (ADHB) Teaching Resources
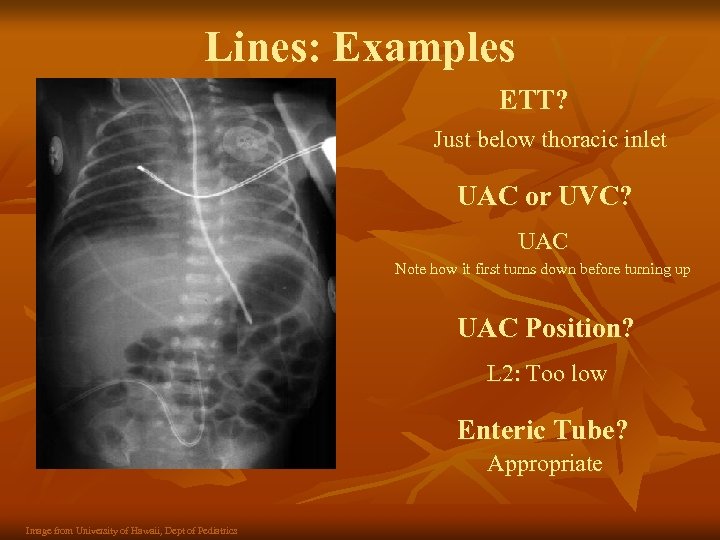
Lines: Examples ETT? Just below thoracic inlet UAC or UVC? UAC Note how it first turns down before turning up UAC Position? L 2: Too low Enteric Tube? Appropriate Image from University of Hawaii, Dept of Pediatrics
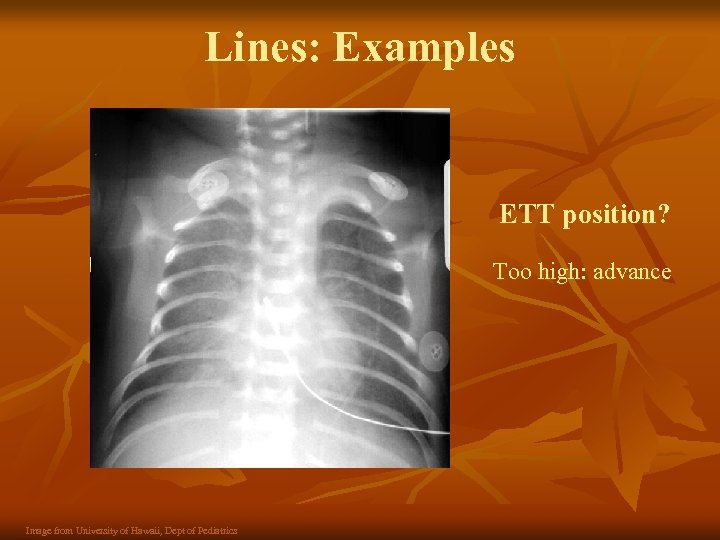
Lines: Examples ETT position? Too high: advance Image from University of Hawaii, Dept of Pediatrics
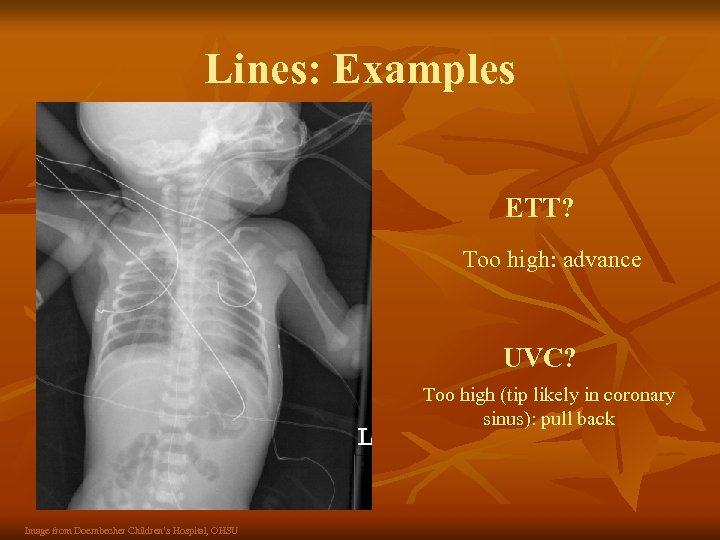
Lines: Examples ETT? Too high: advance UVC? Too high (tip likely in coronary sinus): pull back Image from Doernbecher Children’s Hospital, OHSU
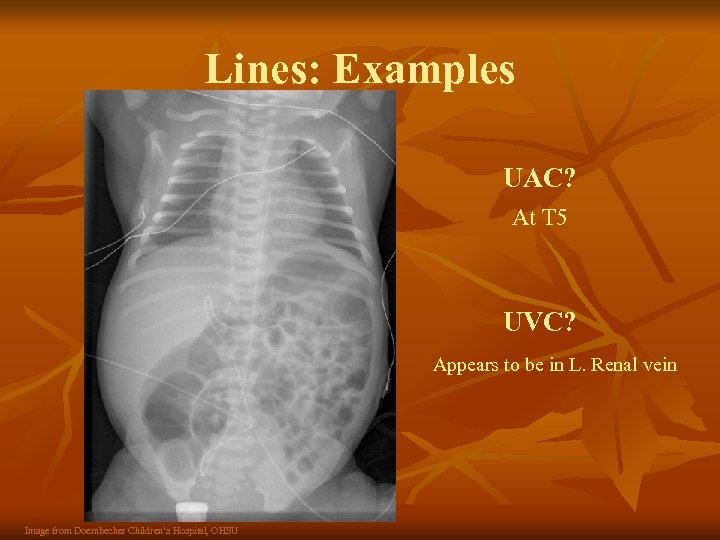
Lines: Examples UAC? At T 5 UVC? Appears to be in L. Renal vein Image from Doernbecher Children’s Hospital, OHSU
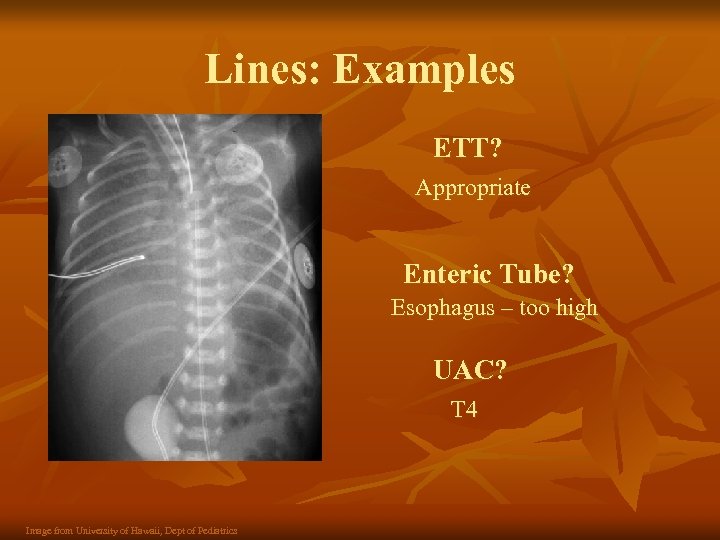
Lines: Examples ETT? Appropriate Enteric Tube? Esophagus – too high UAC? T 4 Image from University of Hawaii, Dept of Pediatrics

Neonatal Lung Pathology n n In addition to tube and line placement, the neonatal CXR can be used to identify any lung, cardiac, congenital, and even abdominal abnormalities. The subsequent slides focus specifically on some common lung pathologies seen in the NICU: n n n Respiratory Distress Syndrome (RDS) Meconium Aspiration Syndrome (MAS) Pneumonia Transient Tachypnea of the Newborn (TTN) Bronchopulmonary Dysplasia (BPD) Air Leak Syndromes
Respiratory Distress Syndrome “hyaline membrane disease” n n Common condition in premature neonates attributable to surfactant deficiency Pathophysiology n Surfactant is produced by the type II pneumocytes n n n Cell line differentiates at 24 -28 weeks gestation but sufficient amounts of surfactant are not present until 34 -36 weeks gestation Cell line is susceptible to various perinatal insults (e. g. ↑ insulin, asphyxia) Normally surfactant coats the alveoli, decreases surface tension, and prevents atelectasis by allowing the alveoli to stay open Without surfactant, the small airways collapse and there is progressive atelectasis with each expiration, decreased FRC, hypoxemia and respiratory distress. Risk Factors n n Increased Risk: prematurity, low birthweight, males, C-section, perinatal asyphyxia, chorioamnionitis, hydrops, maternal diabetes Decreased Risk: chronic intrauterine stress, PROM, maternal htn, narcotic/cocaine use, IUGR/SGA, steroids, thyroid hormone, tocolytics
Respiratory Distress Syndrome n Clinical Presentation n n Onset is typically 0 -7 hours after birth, and characteristically worsens during the first 72 hours and then spontaneously improves Signs of respiratory distress: tachypnea, grunting, nasal flaring, chest wall retractions, cyanosis Hypoxemia, hypercapnea, acidosis Radiographic Manifestations n n Low lung volumes Bilateral and uniform ground-glass n n Prominence of peripheral air bronchograms n n There are collapsed alveoli interspersed with open alveoli This occurs because the larger bronchi do not collapse Diffuse lung opacity n n In severe RDS, where the majority of alveoli collapse, the granular opacities can coalesce. This could also represent a superimposed pneumonia, aspiration, pulmonary hemorrhage, or CHF
Respiratory Distress Syndrome n Differential Diagnosis: n Neonatal pneumonia n n n Meconium Aspiration Syndrome n n n Antenatal steroids Surfactant replacement Assess fetal lung maturity if preterm birth Tocolytics Close fetal monitoring Treatment Air Leaks Airway obstruction Congenital anomalies: cardiac disease, pulmonary hypoplasia, congenital diaphragmatic hernia, etc. Metabolic abnormalities Polycythemia, severe anemia Sepsis n n n n Nodular, non-homogenous densities May have pleural effusions Increased lung volumes n n Non-homogenous densities May have pleural fluid Normal lung volumes Non-homogenous densities May have pleural fluid Prevention n Transient tachypnea of newborn n n Surfactant replacement Supportive respiratory care: MV, CPAP Empiric antibiotics until r/o pneumonia or sepsis NPO while in respiratory distress (enteric tube feeding, parenteral)
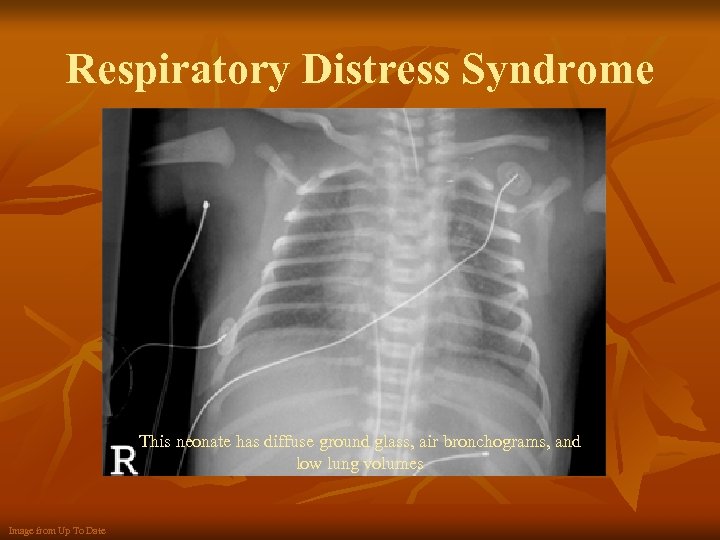
Respiratory Distress Syndrome This neonate has diffuse ground glass, air bronchograms, and low lung volumes Image from Up To Date
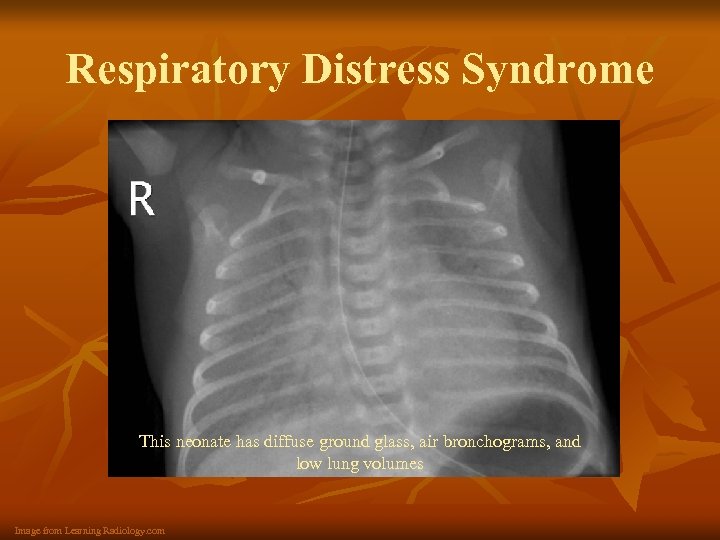
Respiratory Distress Syndrome This neonate has diffuse ground glass, air bronchograms, and low lung volumes Image from Learning Radiology. com
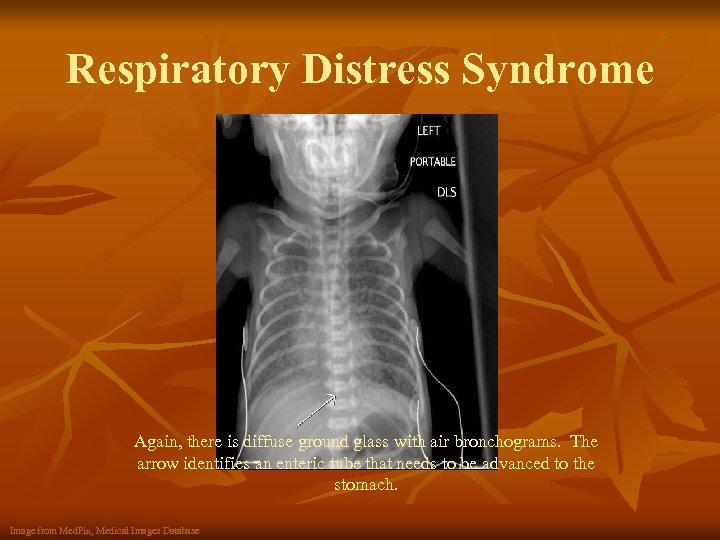
Respiratory Distress Syndrome Again, there is diffuse ground glass with air bronchograms. The arrow identifies an enteric tube that needs to be advanced to the stomach. Image from Med. Pix, Medical Images Database
Respiratory Distress Syndrome n It is important to know that the classic findings of RDS can change once treatment is initiated n n n CPAP/MV: normal lung volumes Surfactant: less homogenous/symmetric appearance Complications from interventions may include: n n Air leaks: pneumothorax, pneumomediastinum, etc Bronchopulmonary dysplasia
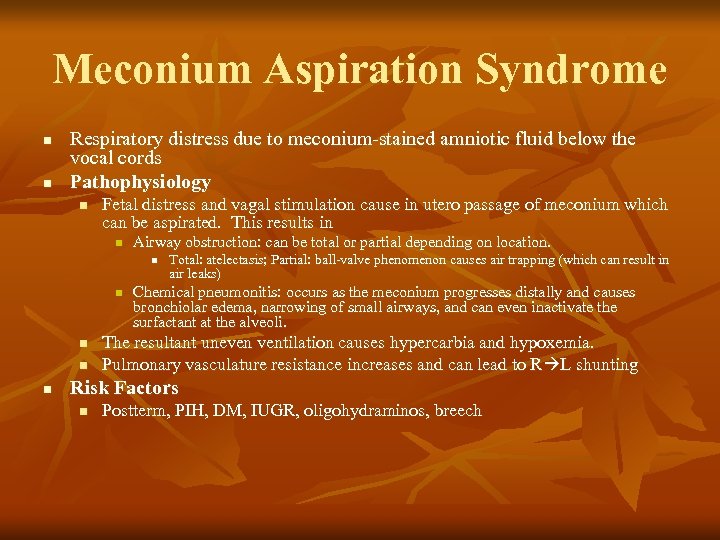
Meconium Aspiration Syndrome n n Respiratory distress due to meconium-stained amniotic fluid below the vocal cords Pathophysiology n Fetal distress and vagal stimulation cause in utero passage of meconium which can be aspirated. This results in n Airway obstruction: can be total or partial depending on location. n n n Total: atelectasis; Partial: ball-valve phenomenon causes air trapping (which can result in air leaks) Chemical pneumonitis: occurs as the meconium progresses distally and causes bronchiolar edema, narrowing of small airways, and can even inactivate the surfactant at the alveoli. The resultant uneven ventilation causes hypercarbia and hypoxemia. Pulmonary vasculature resistance increases and can lead to R L shunting Risk Factors n Postterm, PIH, DM, IUGR, oligohydraminos, breech
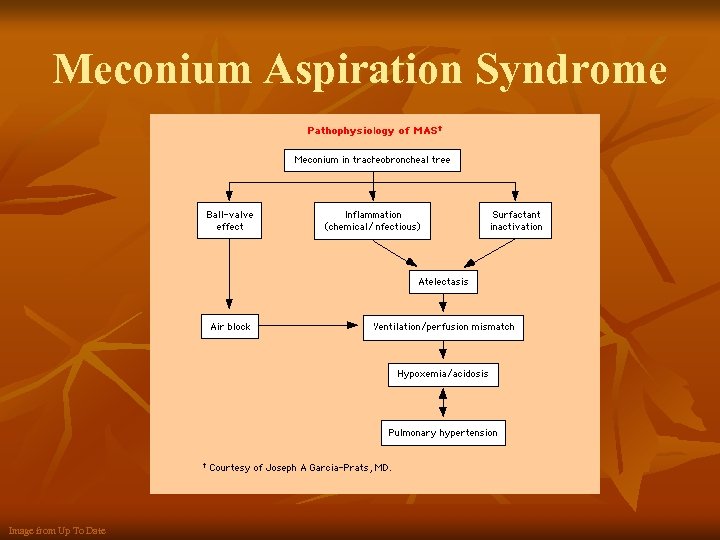
Meconium Aspiration Syndrome Image from Up To Date
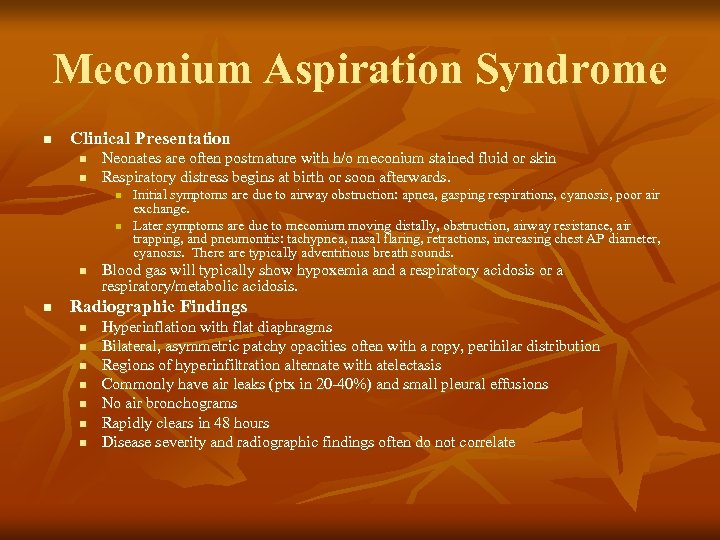
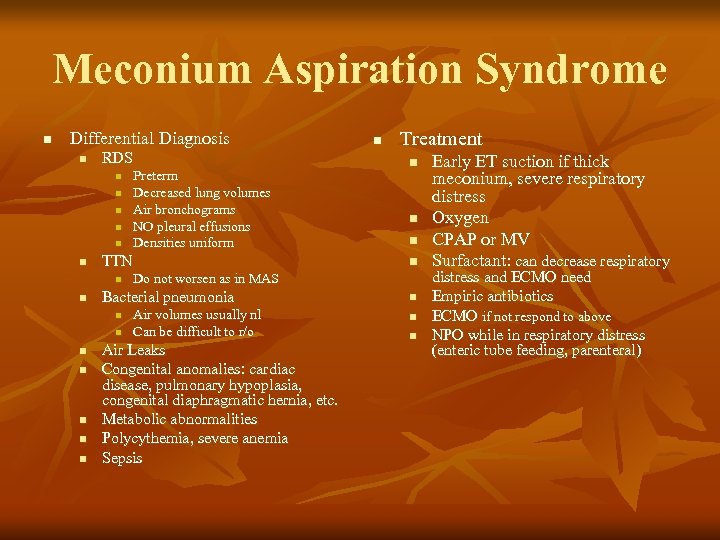
Meconium Aspiration Syndrome n Clinical Presentation n n Neonates are often postmature with h/o meconium stained fluid or skin Respiratory distress begins at birth or soon afterwards. n n Initial symptoms are due to airway obstruction: apnea, gasping respirations, cyanosis, poor air exchange. Later symptoms are due to meconium moving distally, obstruction, airway resistance, air trapping, and pneumonitis: tachypnea, nasal flaring, retractions, increasing chest AP diameter, cyanosis. There are typically adventitious breath sounds. Blood gas will typically show hypoxemia and a respiratory acidosis or a respiratory/metabolic acidosis. Radiographic Findings n n n n Hyperinflation with flat diaphragms Bilateral, asymmetric patchy opacities often with a ropy, perihilar distribution Regions of hyperinfiltration alternate with atelectasis Commonly have air leaks (ptx in 20 -40%) and small pleural effusions No air bronchograms Rapidly clears in 48 hours Disease severity and radiographic findings often do not correlate
Meconium Aspiration Syndrome n Differential Diagnosis n RDS n n n TTN n n n n Treatment n n Do not worsen as in MAS Bacterial pneumonia n n Preterm Decreased lung volumes Air bronchograms NO pleural effusions Densities uniform n Air volumes usually nl Can be difficult to r/o Air Leaks Congenital anomalies: cardiac disease, pulmonary hypoplasia, congenital diaphragmatic hernia, etc. Metabolic abnormalities Polycythemia, severe anemia Sepsis n n n Early ET suction if thick meconium, severe respiratory distress Oxygen CPAP or MV Surfactant: can decrease respiratory distress and ECMO need Empiric antibiotics ECMO if not respond to above NPO while in respiratory distress (enteric tube feeding, parenteral)
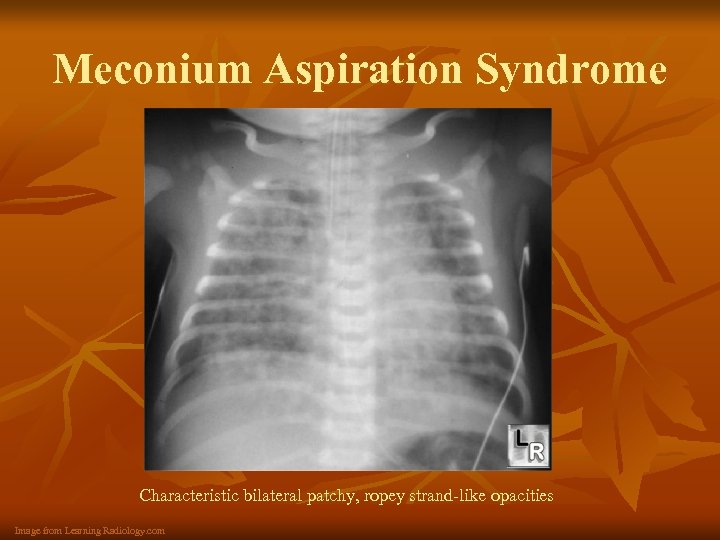
Meconium Aspiration Syndrome Characteristic bilateral patchy, ropey strand-like opacities Image from Learning Radiology. com
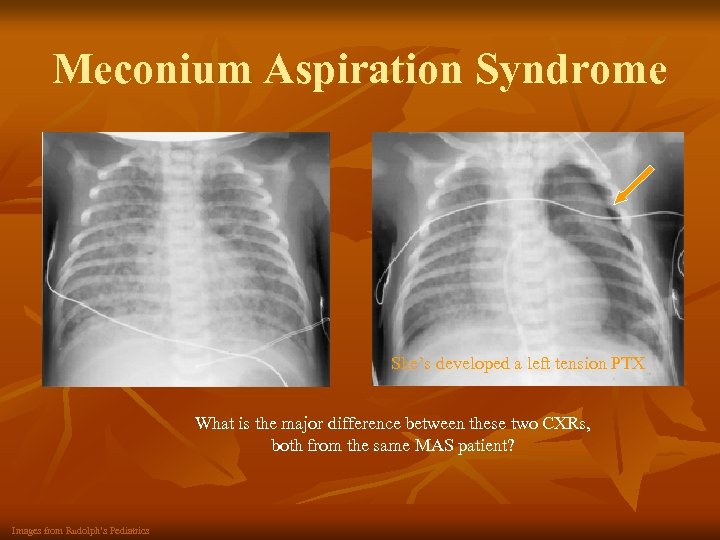
Meconium Aspiration Syndrome She’s developed a left tension PTX What is the major difference between these two CXRs, both from the same MAS patient? Images from Rudolph’s Pediatrics
Neonatal Pneumonia n There are many causes of neonatal pneumonia which are typically divided into two groups by time: n Early Onset n n n Late Onset n n n Symptoms begin at 0 -3 days Pathogens acquired by intrauterine aspiration of amniotic fluid, transplacental transmission, aspiration during/after birth of microbes in amniotic fluid/birth canal Symptoms develop later during hospital stay or after discharge Pathogens are acquired from colonizing flora on neonate or nosocomially Aspiration Pneumonia should also be considered in the NICU
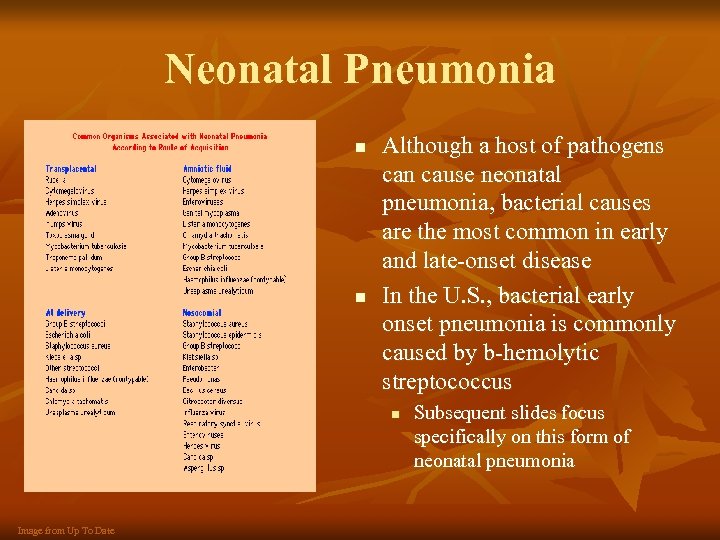
Neonatal Pneumonia n n Although a host of pathogens can cause neonatal pneumonia, bacterial causes are the most common in early and late-onset disease In the U. S. , bacterial early onset pneumonia is commonly caused by b-hemolytic streptococcus n Image from Up To Date Subsequent slides focus specifically on this form of neonatal pneumonia
GBS Neonatal Pneumonia n Pathophysiology n GBS can cause a host of infections throughout the neonatal period. There are three ways to become infected: n n n In utero: ascending or transplacental infection (particularly in setting of PPROM or prolonged labor) During birth: classically infected during transit through birth canal Post natal acquisition (not as common with GBS) Infection cause alveolar collapse, though less uniform than RDS. There are cocci in the lungs as well as an interstitial inflammatory exudate Risk Factors n PROM, fever, chorioamnionitis, prematurity
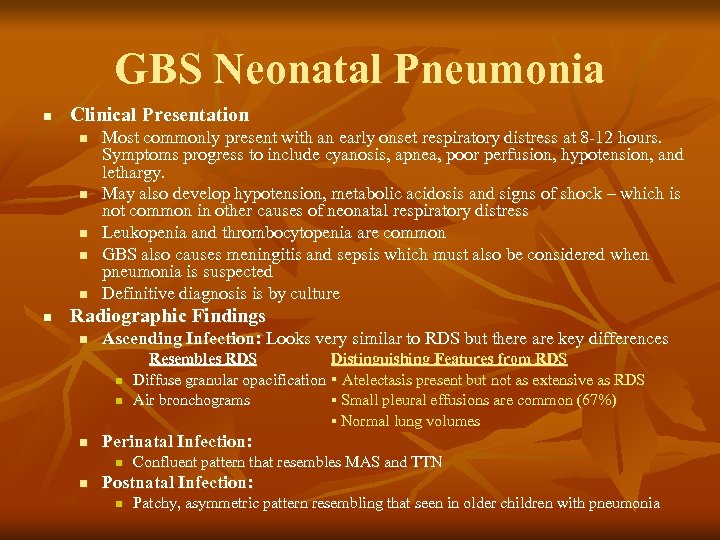
GBS Neonatal Pneumonia n Clinical Presentation n n n Most commonly present with an early onset respiratory distress at 8 -12 hours. Symptoms progress to include cyanosis, apnea, poor perfusion, hypotension, and lethargy. May also develop hypotension, metabolic acidosis and signs of shock – which is not common in other causes of neonatal respiratory distress Leukopenia and thrombocytopenia are common GBS also causes meningitis and sepsis which must also be considered when pneumonia is suspected Definitive diagnosis is by culture Radiographic Findings n Ascending Infection: Looks very similar to RDS but there are key differences n n n Perinatal Infection: n n Resembles RDS Distinguishing Features from RDS Diffuse granular opacification ▪ Atelectasis present but not as extensive as RDS Air bronchograms ▪ Small pleural effusions are common (67%) ▪ Normal lung volumes Confluent pattern that resembles MAS and TTN Postnatal Infection: n Patchy, asymmetric pattern resembling that seen in older children with pneumonia
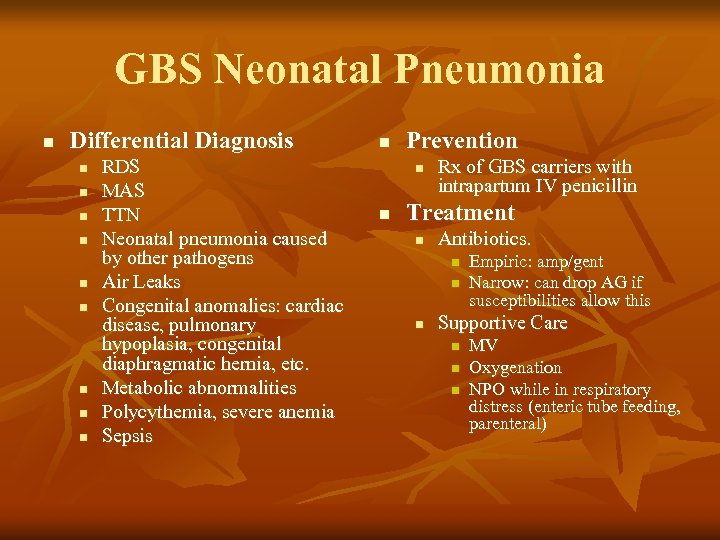
GBS Neonatal Pneumonia n Differential Diagnosis n n n n n RDS MAS TTN Neonatal pneumonia caused by other pathogens Air Leaks Congenital anomalies: cardiac disease, pulmonary hypoplasia, congenital diaphragmatic hernia, etc. Metabolic abnormalities Polycythemia, severe anemia Sepsis n Prevention n n Rx of GBS carriers with intrapartum IV penicillin Treatment n Antibiotics. n n n Empiric: amp/gent Narrow: can drop AG if susceptibilities allow this Supportive Care n n n MV Oxygenation NPO while in respiratory distress (enteric tube feeding, parenteral)
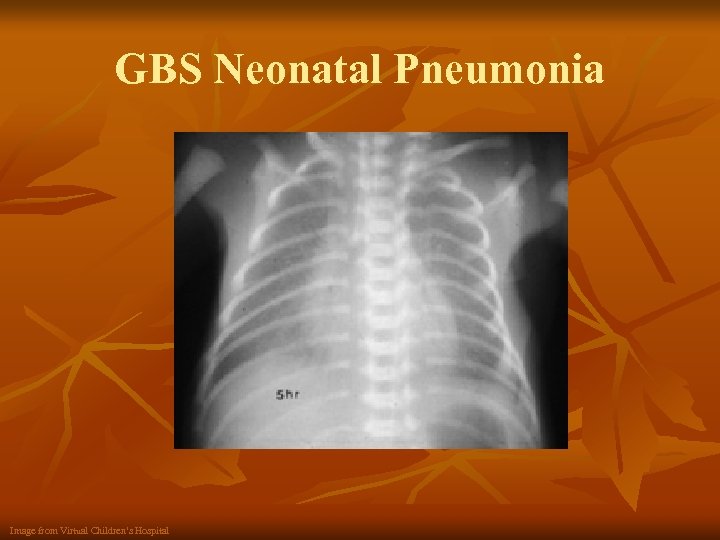
GBS Neonatal Pneumonia Image from Virtual Children’s Hospital
Transient Tachypnea of the Newborn “wet lung” n n Benign, time-limited respiratory distress in term/large preemies that resolves by 3 -5 days Pathophysiology n Unknown etiology but hypotheses include: n n Delayed resorption of fetal lung fluid from the pulmonary lymphatics. Increased fluid volume decreased lung compliance, increased airway resistance respiratory distress Pulmonary immaturity? Mild surfactant deficiency? Risk Factors n Elective c-section/C-section without trial of labor, birth asphyxia, males, breech, excess maternal sedation, maternal DM
Transient Tachypnea of Newborn n Clinical Presentation n n n Respiratory distress begins at 2 -6 hours, and usually resolves by 12 -24 hours (but can last up to 72 hours) Major respiratory sign is tachypnea. But may also have mild cyanosis, nasal flaring, or retractions. (Cyanosis should be responsive to 30 -40% oxygen). Breath sounds are clear Can have a barrel-chest, or increased AP diameter May have tachycardia with normal BP NO signs of sepsis Radiographic Findings n Variable findings but include a combination of: n n n n Symmetric pattern of pulmonary congestion with bilateral reticulonodular densities that are particularly prominent in the perihilar region Mild-moderate cardiomegaly Fluid in minor fissure Peripheral air trapping causes increased lung volumes Flat diaphragms on lateral Air leaks are rare CXR returns to normal in 48 -72 hours
Transient Tachypnea of Newborn n Differential Diagnosis n n n n RDS MAS Neonatal pneumonia Sepsis Congenital heart disease Polycythemia Metabolic disorders n Treatment n n n Oxygenation Empiric abx: until r/o pna, sepsis NPO if RR>60 to minimize aspiration risk Maintain hydration Diuretics: not helpful
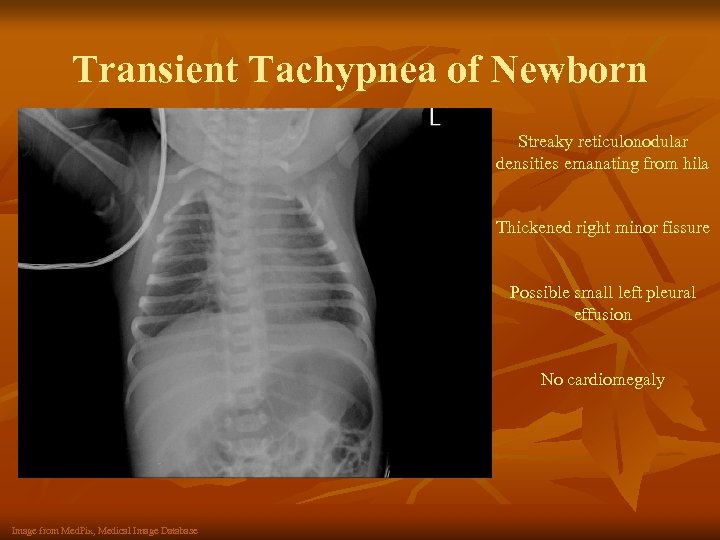
Transient Tachypnea of Newborn Streaky reticulonodular densities emanating from hila Thickened right minor fissure Possible small left pleural effusion No cardiomegaly Image from Med. Pix, Medical Image Database
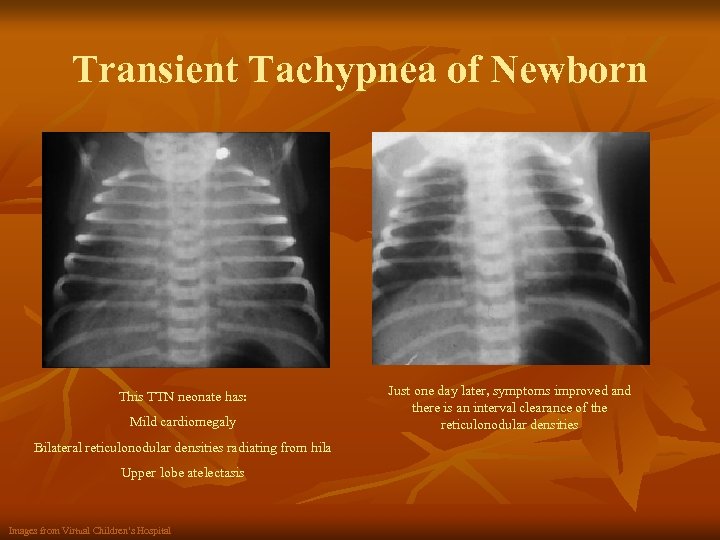
Transient Tachypnea of Newborn This TTN neonate has: Mild cardiomegaly Bilateral reticulonodular densities radiating from hila Upper lobe atelectasis Images from Virtual Children’s Hospital Just one day later, symptoms improved and there is an interval clearance of the reticulonodular densities
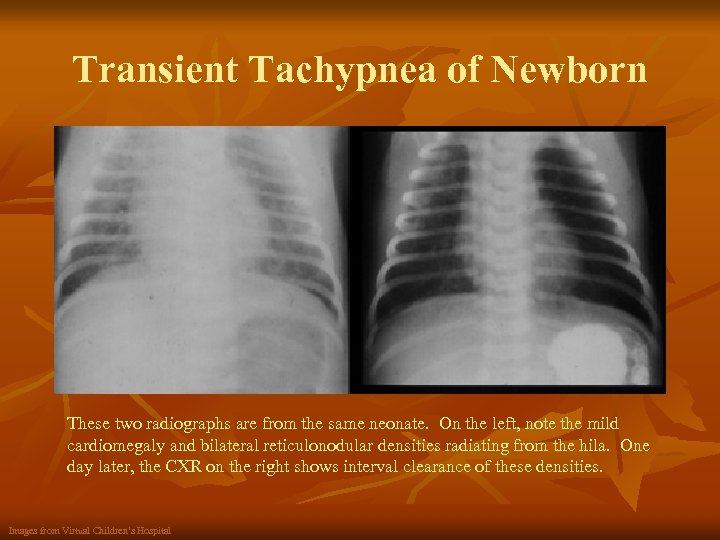
Transient Tachypnea of Newborn These two radiographs are from the same neonate. On the left, note the mild cardiomegaly and bilateral reticulonodular densities radiating from the hila. One day later, the CXR on the right shows interval clearance of these densities. Images from Virtual Children’s Hospital
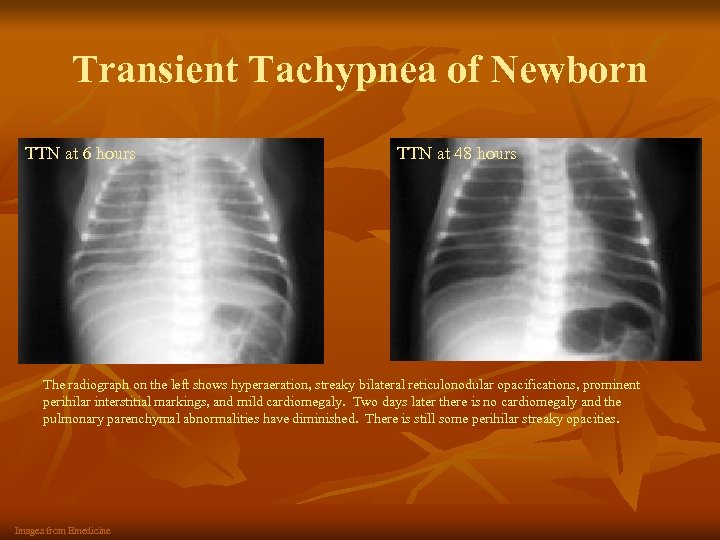
Transient Tachypnea of Newborn TTN at 6 hours TTN at 48 hours The radiograph on the left shows hyperaeration, streaky bilateral reticulonodular opacifications, prominent perihilar interstitial markings, and mild cardiomegaly. Two days later there is no cardiomegaly and the pulmonary parenchymal abnormalities have diminished. There is still some perihilar streaky opacities. Images from Emedicine
Bronchopulmonary Dysplasia n n BPD is a chronic lung disease of prematurity. Classically it follows a course of primary lung disease (RDS, MAS, etc) that requires exposure to mechanical ventilation and high oxygen concentration. Pathophysiology n n Alveolar stage of lung development begins at 36 weeks and continues postnatally. BPD occurs when insults result in defective repair, impede alveolarization, and cause vascular dysgenesis. Classically, BPD results from a primary lung disease (often RDS) requiring long-term mechanical ventilation or exposure to high oxygen concentration. It can occur without antecedent illness, particularly in the setting of extreme prematurity or sepsis. Key contributors to BPD: n n Oxygen exposure: decreased alveolar septation (causing fewer, larger alveoli), alveolar vascularization, increases lung fibrosis and inhibits lung growth. Mechanical ventiliation: Barotrauma and bacterial colonization from ETT can cause lung injury Inflammation: Those who later develop BPD have been shown to have an early exaggerated inflammatory response in the lungs. Risk Factors n Lung immaturity, low birthweight, prematurity, MV, exposure to high oxygen concentration, males
Bronchopulmonary Dysplasia n Clinical Presentation n n Progressive, idiopathic pulmonary deterioration in susceptible neonates: increased WOB, oxygen dependence, retractions, diffuse rales/wheeze, hypoxemia, hypercapnea, compensatory metabolic alkalosis May develop right sided heart failure Poor weight gain with increased energy intake Radiographic Findings n n Four orderly stages have been described, but often not seen and not currently thought to be clinically useful. Still, there is a progression of radiographic findings. Variable presentations are seen, but can include: n n n Initial homogenous ground glass appearance of RDS At 1 -2 weeks, will have “white-out” or a complete opacification of lungs Over weeks-months, small cystic lucencies of uniform size/distribution develop which give a characteristic “bubbly” appearance to the CXR. There may also be coarse lung markings and asymmetric aeration. Months later, lung volumes increase, the cystic lucencies coalesce By 2 -3 years of age the radiologic signs of BPD will often resolve
Bronchopulmonary Dysplasia n Differential Diagnosis n n n Cardiovascular anomalies Airway obstruction Tracheomalacia Immunodeficiency Aspiration, reflux Cystic fibrosis n Treatment n n n Maintain oxygenation PPV Fluid restriction Diuretic therapy Bronchodilation Corticosteroids
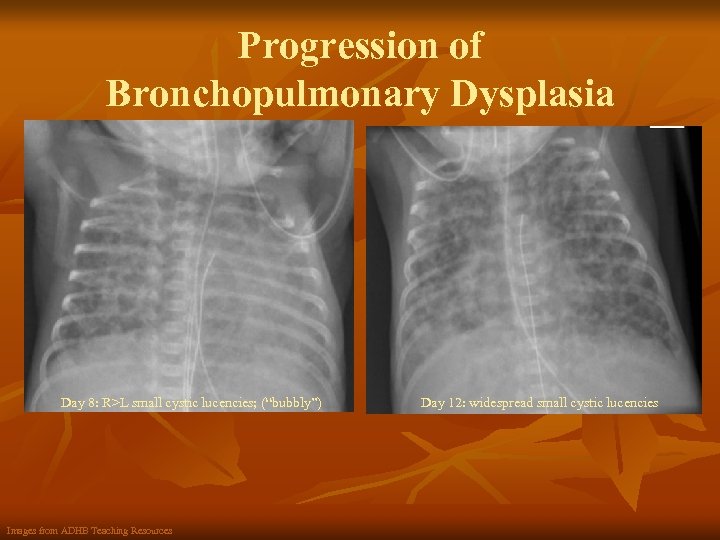
Progression of Bronchopulmonary Dysplasia Day 8: R>L small cystic lucencies; (“bubbly”) Images from ADHB Teaching Resources Day 12: widespread small cystic lucencies
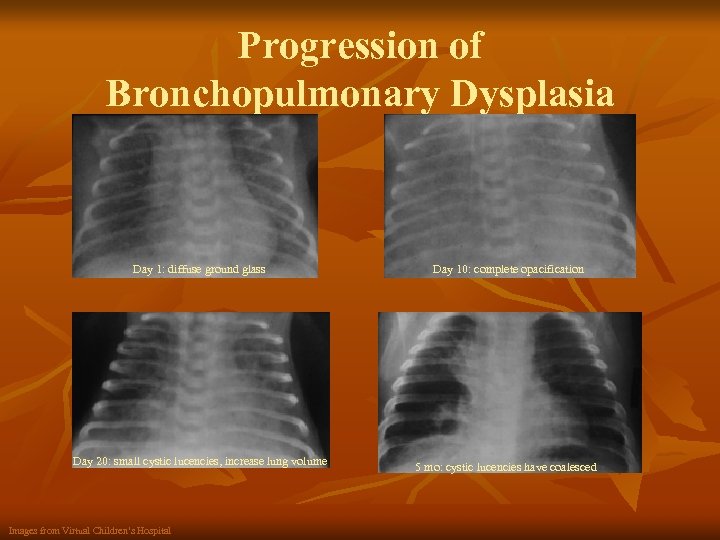
Progression of Bronchopulmonary Dysplasia Day 1: diffuse ground glass Day 10: complete opacification Day 20: small cystic lucencies, increase lung volume 5 mo: cystic lucencies have coalesced Images from Virtual Children’s Hospital
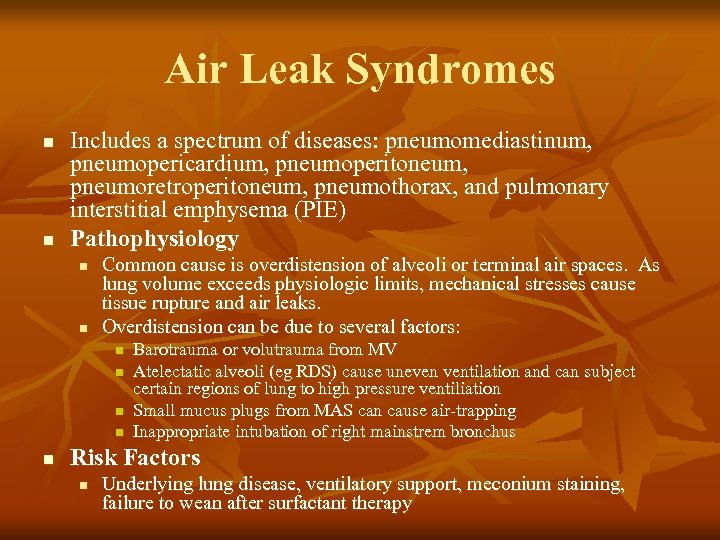
Air Leak Syndromes n n Includes a spectrum of diseases: pneumomediastinum, pneumopericardium, pneumoperitoneum, pneumoretroperitoneum, pneumothorax, and pulmonary interstitial emphysema (PIE) Pathophysiology n n Common cause is overdistension of alveoli or terminal air spaces. As lung volume exceeds physiologic limits, mechanical stresses cause tissue rupture and air leaks. Overdistension can be due to several factors: n n n Barotrauma or volutrauma from MV Atelectatic alveoli (eg RDS) cause uneven ventilation and can subject certain regions of lung to high pressure ventiliation Small mucus plugs from MAS can cause air-trapping Inappropriate intubation of right mainstrem bronchus Risk Factors n Underlying lung disease, ventilatory support, meconium staining, failure to wean after surfactant therapy
Air Leak Syndromes n Clinical Presentation n Although presentation is unique for each specific disease process, generally present with respiratory distress and worsening clinical course Potentially lethal Radiographic Findings n Definitive diagnosis in all is made with CXR
Air Leak Syndromes: Pneumomediastinum n n Air in the mediastinum from ruptured alveolar air that has traversed fascial planes. Clinical Presentation: n n Often preceded by pulmonary interstitial emphysema Can be completely asymptomatic Increased AP diameter, distant heart sounds Radiographic Findings: n n n Air in mediastinum – usually anterior, middle Thymus is well-outlined by air and may be elevated off heart May have “continuous diaphragm sign: ” retrocardiac air outlines diaphragm under the heart
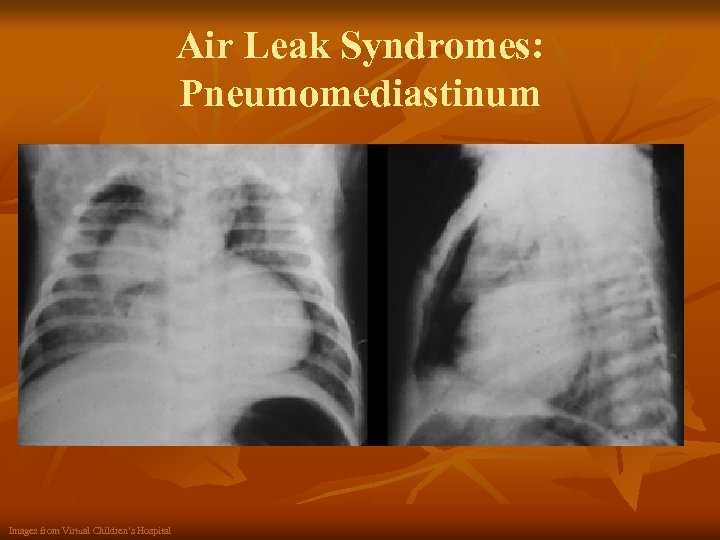
Air Leak Syndromes: Pneumomediastinum Images from Virtual Children’s Hospital
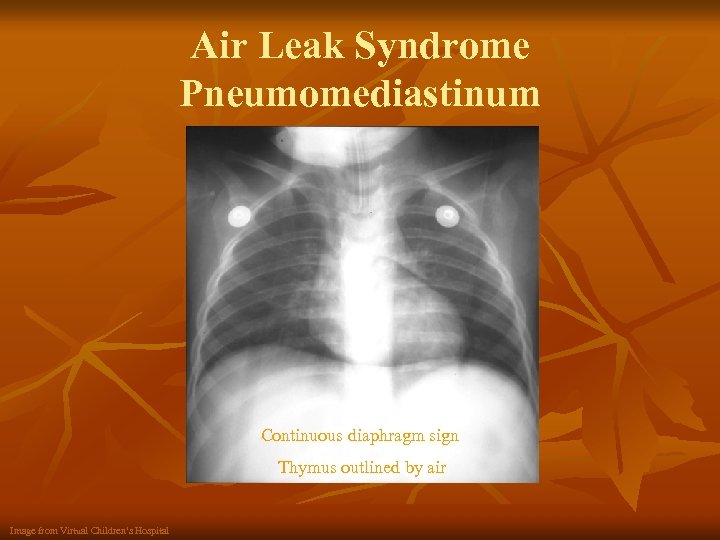
Air Leak Syndrome Pneumomediastinum Continuous diaphragm sign Thymus outlined by air Image from Virtual Children’s Hospital
Air Leak Syndromes: Pneumopericardium n n Air in the pericardial sac Clinical Presentation n Asymptomatic to cardiac tamponade Hypotension, decreased pulse pressure, tachycardia, distant heart sounds Radiographic Findings n “Halo sign: ” broad radiolucent halo surrounds heart and its diaphragmatic surface. n n Continuous diaphragm sign as in pneumomediastinum Unlike pneumomediastinum, does not extend beyond great vessels
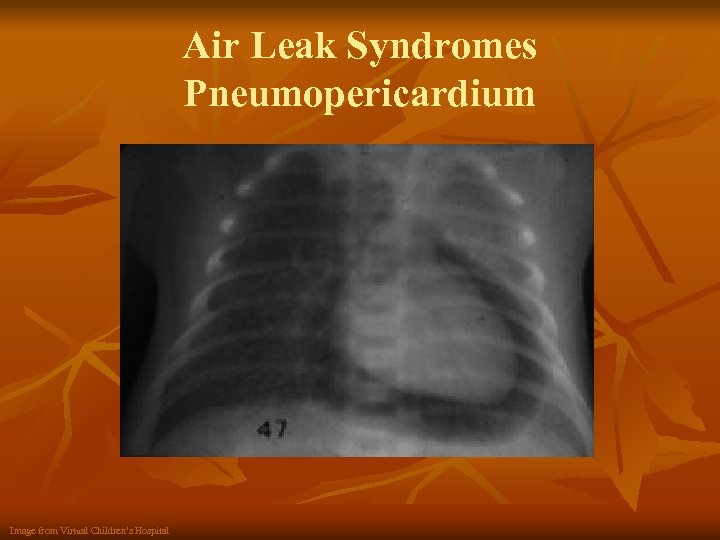
Air Leak Syndromes Pneumopericardium Image from Virtual Children’s Hospital
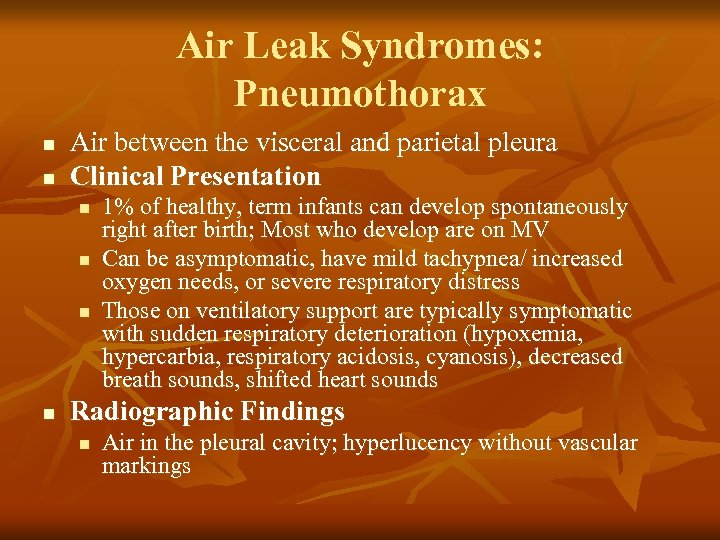
Air Leak Syndromes: Pneumothorax n n Air between the visceral and parietal pleura Clinical Presentation n n 1% of healthy, term infants can develop spontaneously right after birth; Most who develop are on MV Can be asymptomatic, have mild tachypnea/ increased oxygen needs, or severe respiratory distress Those on ventilatory support are typically symptomatic with sudden respiratory deterioration (hypoxemia, hypercarbia, respiratory acidosis, cyanosis), decreased breath sounds, shifted heart sounds Radiographic Findings n Air in the pleural cavity; hyperlucency without vascular markings
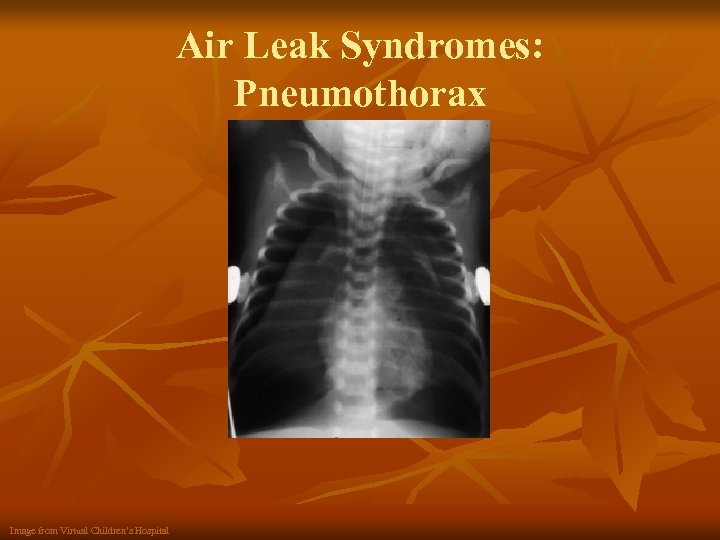
Air Leak Syndromes: Pneumothorax Image from Virtual Children’s Hospital
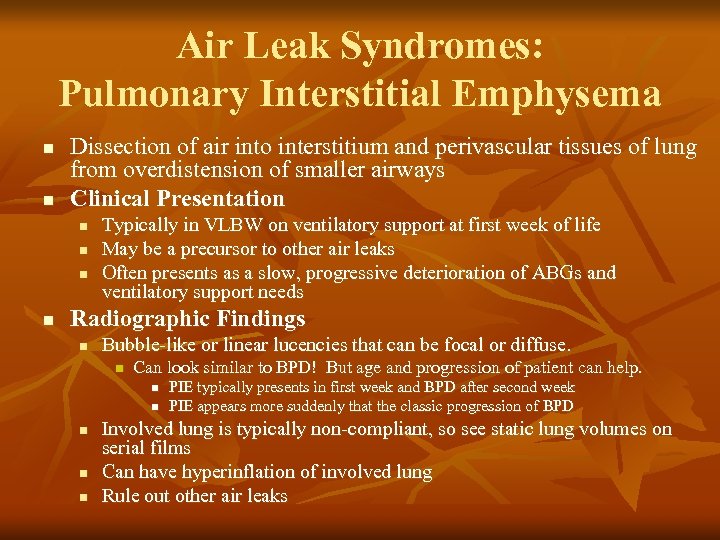
Air Leak Syndromes: Pulmonary Interstitial Emphysema n n Dissection of air into interstitium and perivascular tissues of lung from overdistension of smaller airways Clinical Presentation n n Typically in VLBW on ventilatory support at first week of life May be a precursor to other air leaks Often presents as a slow, progressive deterioration of ABGs and ventilatory support needs Radiographic Findings n Bubble-like or linear lucencies that can be focal or diffuse. n Can look similar to BPD! But age and progression of patient can help. n n n PIE typically presents in first week and BPD after second week PIE appears more suddenly that the classic progression of BPD Involved lung is typically non-compliant, so see static lung volumes on serial films Can have hyperinflation of involved lung Rule out other air leaks
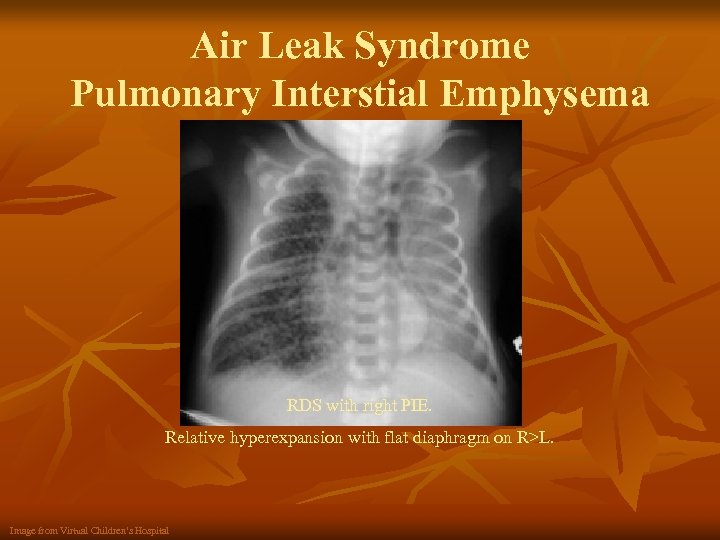
Air Leak Syndrome Pulmonary Interstial Emphysema RDS with right PIE. Relative hyperexpansion with flat diaphragm on R>L. Image from Virtual Children’s Hospital
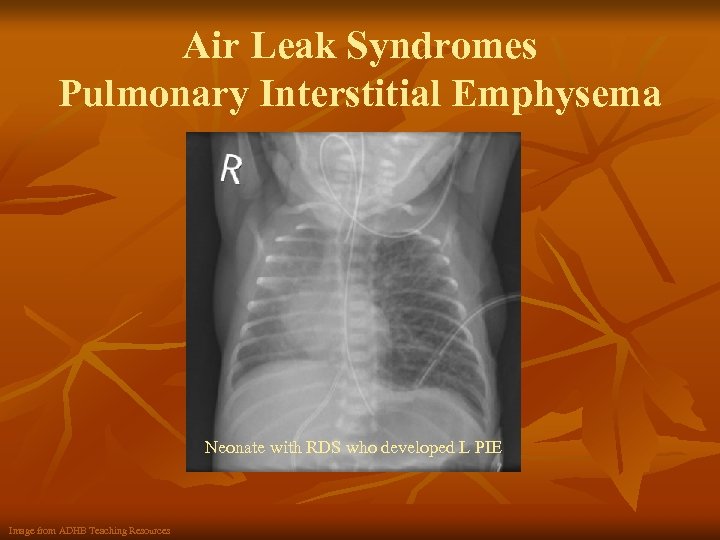
Air Leak Syndromes Pulmonary Interstitial Emphysema Neonate with RDS who developed L PIE Image from ADHB Teaching Resources
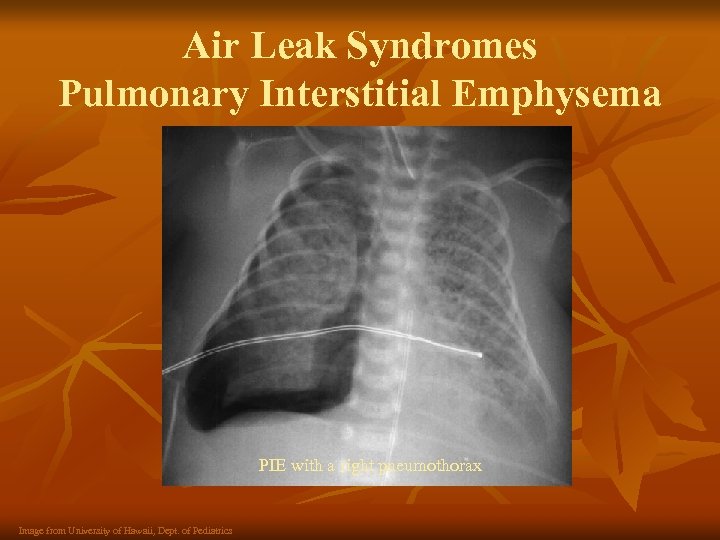
Air Leak Syndromes Pulmonary Interstitial Emphysema PIE with a right pneumothorax Image from University of Hawaii, Dept. of Pediatrics
References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. Alessandro, Michael. Neonatal Chest Disease. December 17, 1997 http: //www. vh. org/pediatric/provider/radiology/PAP/Neonatal. Chest. Diseases/Neonatal. Chest. Dis. Index. html Pediatrics on Call. Seizure and VSD in a 2 month infant. 2000. http: //www. pediatriconcall. com/fordoctor/casereports/Seizureand. VSD. asp Auckland District Health Board. Radiology Image Archive. Ocotber 4, 2004 http: //www. adhb. govt. nz/newborn/Teaching. Resources/Radiology. htm Yamamoto, Lauren. Radiology Cases in Neonatolgy. 1996 http: //www. hawaii. edu/medicine/pediatrics/neoxray. html Welty, Stephen. Pathophysiology and clinical manifestations of respiratory distress syndrome in the newborn. September 15, 2005 http: //www. utdol. com/application/topic. asp? file=neonatol/6415&type=P&selected. Title=6~12 Learning. Radiology. com. Hyaline Membrane Disease; Respiratory Distress Syndrome (of the Newborn). 2004 http: //www. learningradiology. com/notes/chestnotes/hyalinemembranepage. htm Med. Pix Pediatric Radiology Teaching File. Respiratory Distress Syndrome of Prematurity. 2005 http: //rad. usuhs. mil/medpix. html? mode=search_slides#top Garcia-Prats, Joseph. Clinical Features and Diagnosis of Meconium Aspiration Syndrome. August 8, 2005. http: //www. utdol. com/application/topic. asp? file=neonatol/14567&type=P&selected. Title=5~10 Learning. Radiology. com Meconium Aspiration Syndrome. 2004. http: //www. learningradiology. com/archives 04/COW%20089 -Meconium%20 aspiration/meconaspirationcorrect. htm Bancalari, Edward. Meconium Aspiration Syndrome in Rudolph’s Pediatrics, 21 st edition. 2003. http: //online. statref. com/Document. aspx? Doc. Id=78&Fx. Id=13&Session. Id=5 A 165 BKQWSENBJTU&Scroll=1&Index=1 Speer, Michael. Neonatal Pneumonia. June 13, 2005. http: //www. utdol. com/application/topic. asp? file=neonatol/2537&type=P&selected. Title=2~11 Asenjo, Magarita. Transient Tachypnea of the Newborn. May 6, 2003. http: //www. emedicine. com/radio/topic 710. htm Donnelly, Lane. Fundamentals of Pediatric Radiology. Philadelphia: WB Saunders, 2001. Behrman, Richard and Kliegman, Robert. Nelson Essentials of Pediatrics. Philadephia: WB Saunders, 2002. Gomella, Tricia. Neonataology: Management, Procedures, On-call Problems, Diseases, and Drugs. New York: Lange Medical Books, 2004. Division of Neonatology, Doernbecher Children’s Hospital. Neonatal Resident Training Manual. 2005.

2fca1025c3ffaee1b71685f4adda9966.ppt