
CHEMOTHERAPY 1. 2. 3. 4. 5. 6. Antibiotics Classification of antibacterial agents General principles of antibacterial therapy Antibiotic susceptibility testing Bacterial resistance to antibacterial agents Interferon and antiviral agents
ANTIBIOTICS (DEFINITIONS) • Antibiotics (anti-against, bios-life) are the substances able to inhibit microorganisms. • Antibacterial agents are any compounds natural, synthetic, or semisynthetic that are clinically useful in the treatment of bacterial infections. Antibiotics acting on bacteria causing them to expand burst
ANTIBIOTICS • Bacteriostatic agents (sulfonamides, chloramphenicol) inhibit bacterial growth • Bacteriocidal agents (penicillin, streptomycin) significantly reduce the number of viable bacteria in the culture. Bactericidal agents generally kill only growing organisms
ANTIBIOTICS • Narrow spectrum antibacterial agents are preferentially active against other Gram + or Gram- bacteria • Broad-spectrum antibacterial agents are active against Gr+ and Gr- bacteria
THE ACTIVITY OF ANTIBIOTICS • The activity of antibiotics is expressed in international unit (IU). IU of penicillin (oxford unit) is the smallest amount of preparation inhibiting the growth of a standard S. aureus strain. • One unit of activity (A. U. ) corresponds to the activity of 0. 6 micrograms (mg) of the chemically pure crystalline sodium salt of benzylpenicillin.
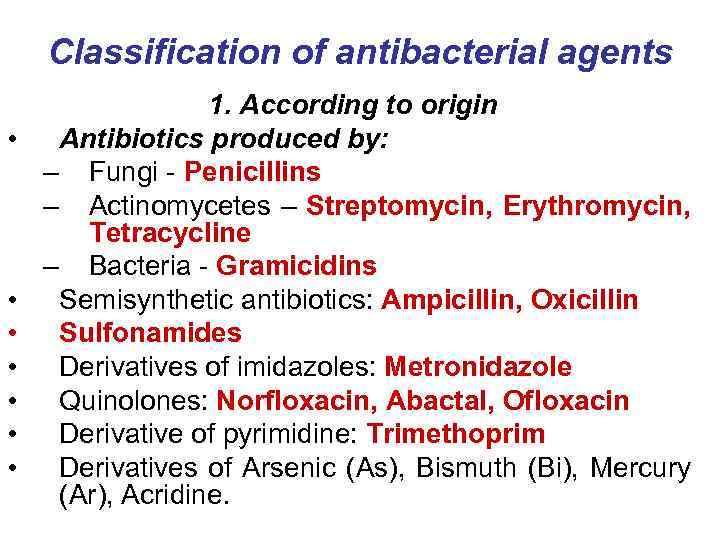
Classification of antibacterial agents • • 1. According to origin Antibiotics produced by: – Fungi - Penicillins – Actinomycetes – Streptomycin, Erythromycin, Tetracycline – Bacteria - Gramicidins Semisynthetic antibiotics: Ampicillin, Oxicillin Sulfonamides Derivatives of imidazoles: Metronidazole Quinolones: Norfloxacin, Abactal, Ofloxacin Derivative of pyrimidine: Trimethoprim Derivatives of Arsenic (As), Bismuth (Bi), Mercury (Ar), Acridine.
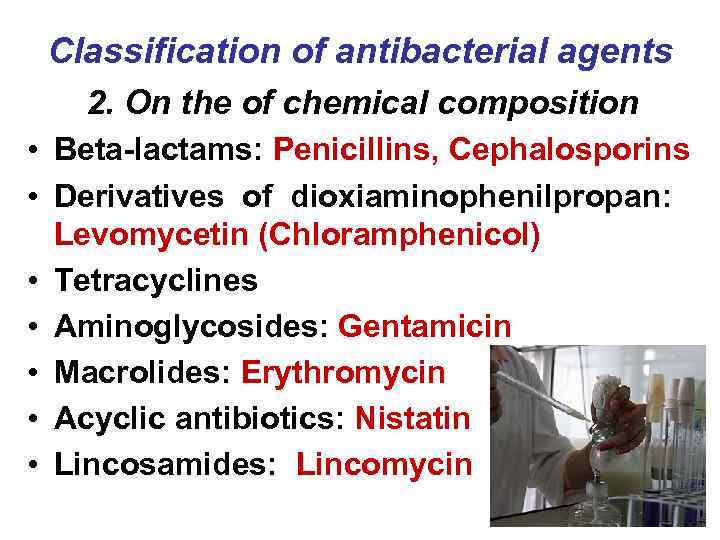
Classification of antibacterial agents 2. On the of chemical composition • Beta-lactams: Penicillins, Cephalosporins • Derivatives of dioxiaminophenilpropan: Levomycetin (Chloramphenicol) • Tetracyclines • Aminoglycosides: Gentamicin • Macrolides: Erythromycin • Acyclic antibiotics: Nistatin • Lincosamides: Lincomycin

Classification of antibacterial agents A. Inhibitors cell wall synthesis • B-lactams (Penicillins, Cephalosporins) • Other inhibitors of bacterial cell wall synthesis: Cycloserine, Vancomycin, Bacitracin B. Inhibitors nucleotide synthesis • Sulfonamides: Trimethoprim, Sulfamethoxazole-trimethoprim.
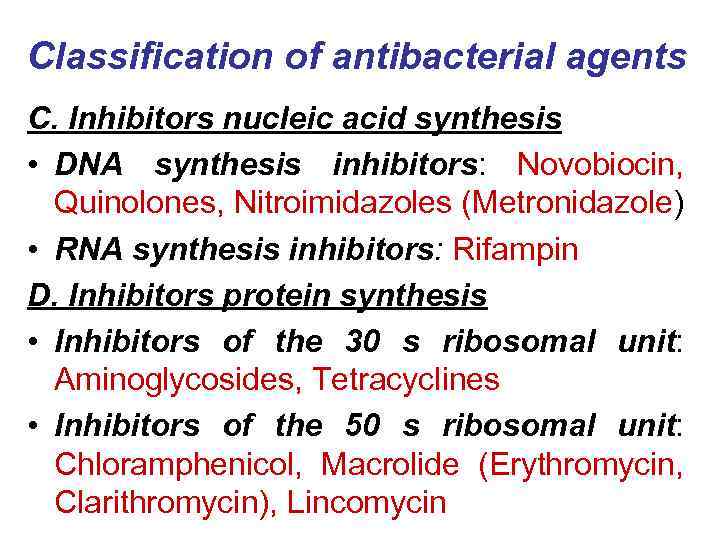
Classification of antibacterial agents C. Inhibitors nucleic acid synthesis • DNA synthesis inhibitors: Novobiocin, Quinolones, Nitroimidazoles (Metronidazole) • RNA synthesis inhibitors: Rifampin D. Inhibitors protein synthesis • Inhibitors of the 30 s ribosomal unit: Aminoglycosides, Tetracyclines • Inhibitors of the 50 s ribosomal unit: Chloramphenicol, Macrolide (Erythromycin, Clarithromycin), Lincomycin
General principles of effective antibacterial therapy 1. The choice of antibacterial agent should be based on susceptibility 2. When the infection is life-threatening or when early treatment is extremely important, treatment is initiated with broad-spectrum antibiotics without detection susceptibility
General principles of effective antibacterial therapy 3. Early treatment usually involves short-term therapy, which has the advantage of reducing the possibility of superinfection. 4. Infections of poorly vascularized tissues (e. g. Endocarditis, Osteomyelitis) should be treated with bactericidal antibiotics.
Antibiotic susceptibility testing allows the choice of the best antibiotic with the narrowest spectrum and highest effectiveness against the isolated bacteria 1. Tube dilution test 2. The agar diffusion test (Bauer-Kirby test) 3. E-test method 4. Automated tests
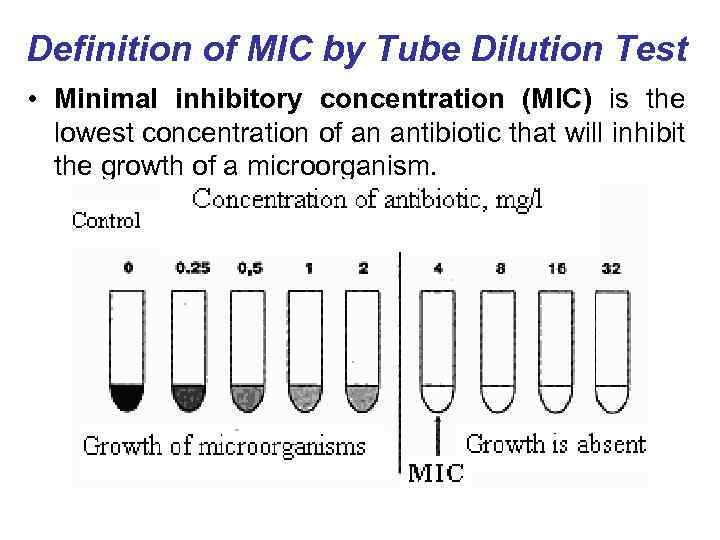
Definition of MIC by Tube Dilution Test • Minimal inhibitory concentration (MIC) is the lowest concentration of an antibiotic that will inhibit the growth of a microorganism.
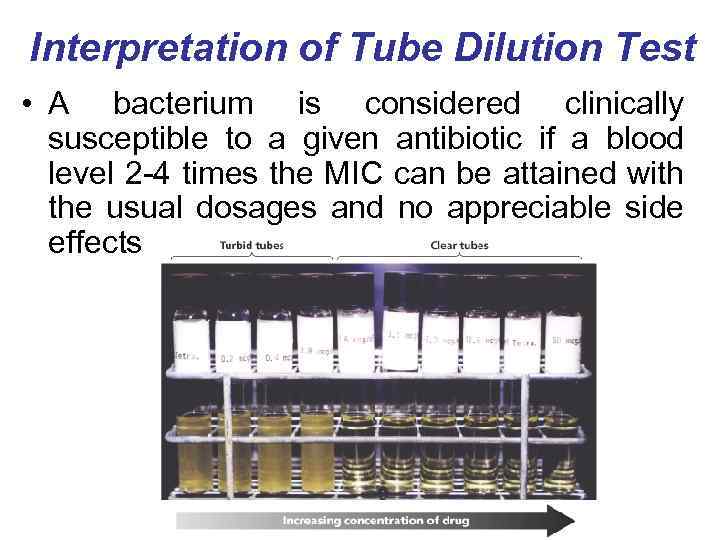
Interpretation of Tube Dilution Test • A bacterium is considered clinically susceptible to a given antibiotic if a blood level 2 -4 times the MIC can be attained with the usual dosages and no appreciable side effects
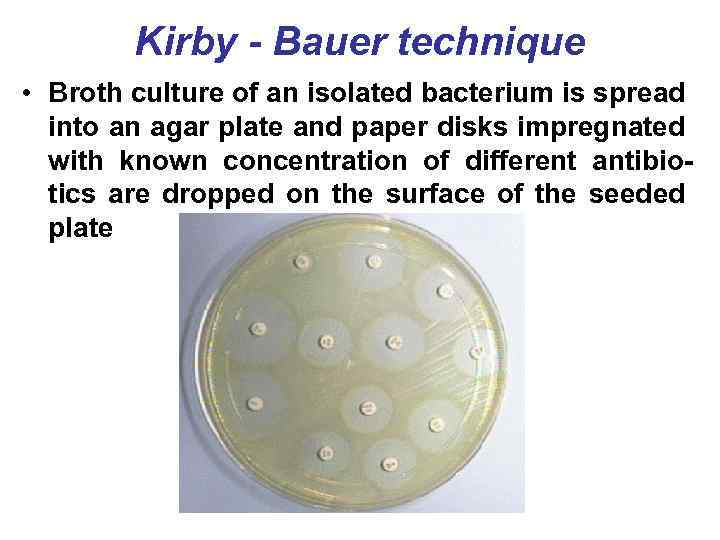
Kirby - Bauer technique • Broth culture of an isolated bacterium is spread into an agar plate and paper disks impregnated with known concentration of different antibiotics are dropped on the surface of the seeded plate
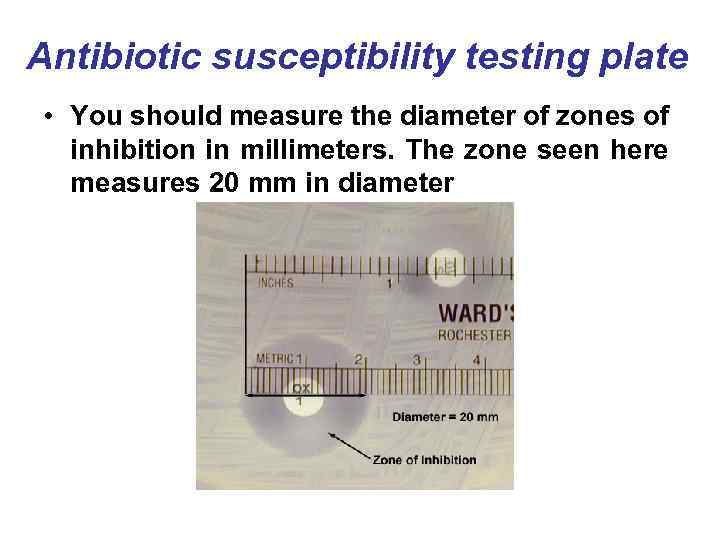
Antibiotic susceptibility testing plate • You should measure the diameter of zones of inhibition in millimeters. The zone seen here measures 20 mm in diameter
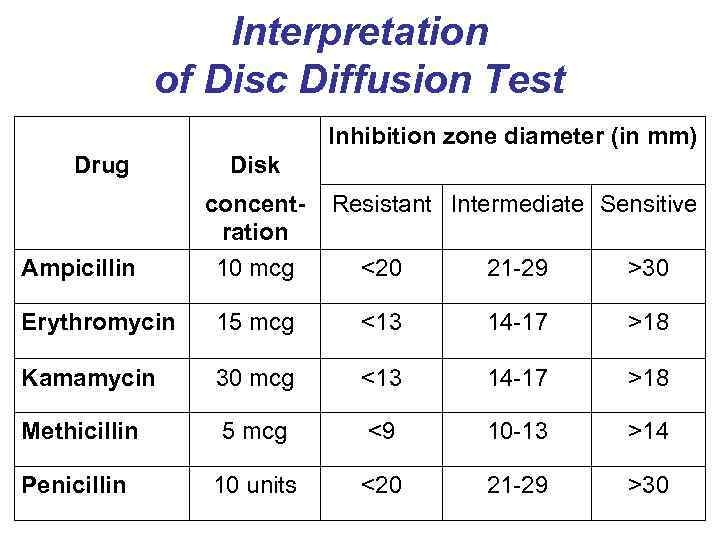
Interpretation of Disc Diffusion Test Inhibition zone diameter (in mm) Drug Disk concentration Resistant Intermediate Sensitive Ampicillin 10 mcg <20 21 -29 >30 Erythromycin 15 mcg <13 14 -17 >18 Kamamycin 30 mcg <13 14 -17 >18 Methicillin 5 mcg <9 10 -13 >14 Penicillin 10 units <20 21 -29 >30
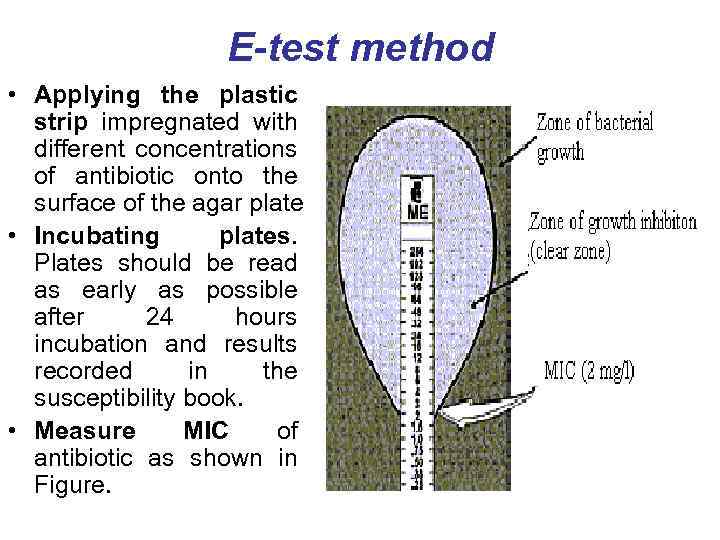
E-test method • Applying the plastic strip impregnated with different concentrations of antibiotic onto the surface of the agar plate • Incubating plates. Plates should be read as early as possible after 24 hours incubation and results recorded in the susceptibility book. • Measure MIC of antibiotic as shown in Figure.

E-test method Definition of susceptibility of microorganisms to antibiotics by E-test
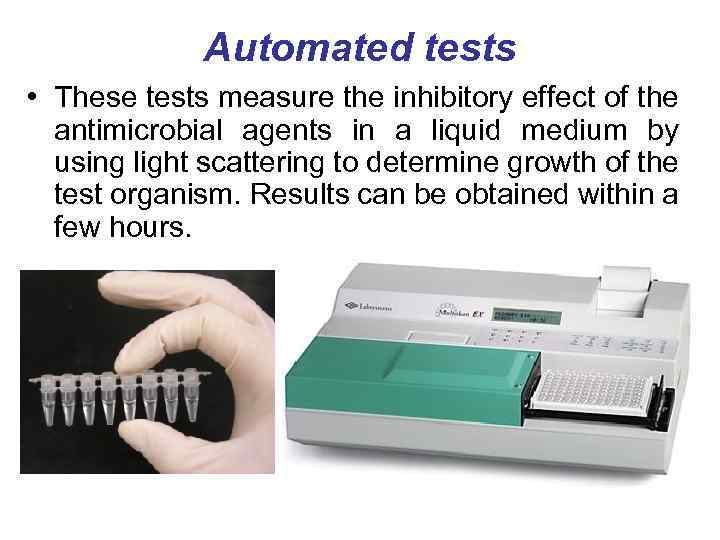
Automated tests • These tests measure the inhibitory effect of the antimicrobial agents in a liquid medium by using light scattering to determine growth of the test organism. Results can be obtained within a few hours.
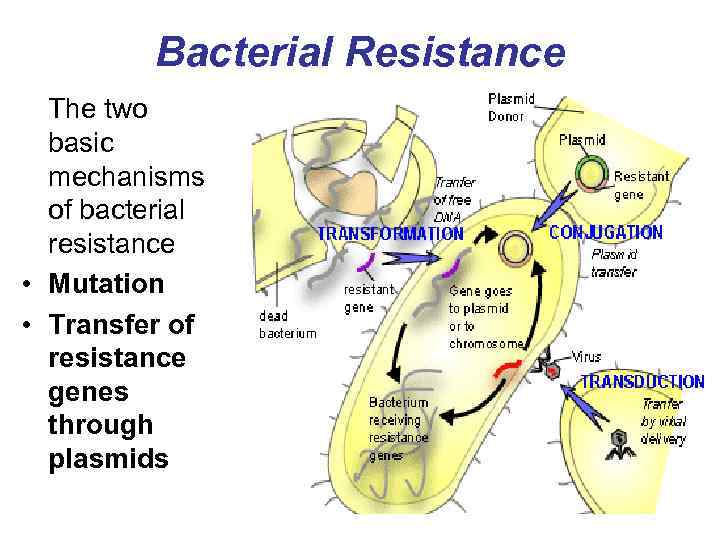
Bacterial Resistance The two basic mechanisms of bacterial resistance • Mutation • Transfer of resistance genes through plasmids
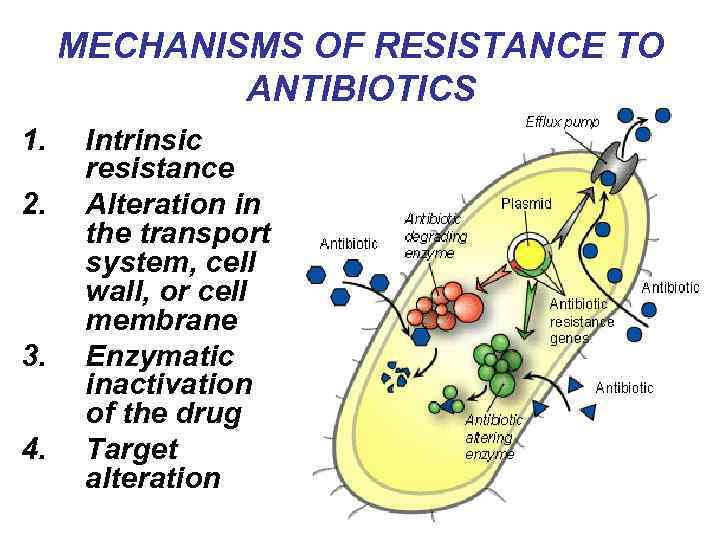
MECHANISMS OF RESISTANCE TO ANTIBIOTICS 1. 2. 3. 4. Intrinsic resistance Alteration in the transport system, cell wall, or cell membrane Enzymatic inactivation of the drug Target alteration
Why has antibiotic resistance occurred? • Pressure on doctors, by patients, to prescribe antibiotics even when they are not needed. • Patients being prescribed antibiotics without the doctor knowing the cause of the infection. • Use of antibiotics in animals for growth promotion and prophylaxis, which allows them to enter the human food chain.
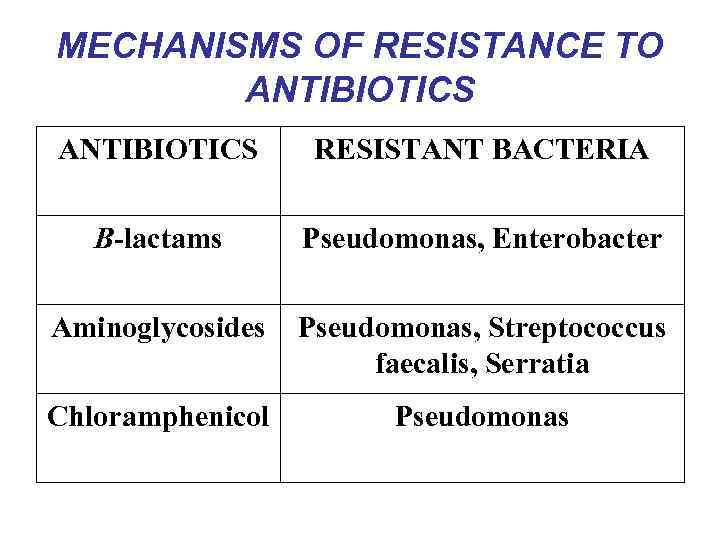
MECHANISMS OF RESISTANCE TO ANTIBIOTICS RESISTANT BACTERIA B-lactams Pseudomonas, Enterobacter Aminoglycosides Pseudomonas, Streptococcus faecalis, Serratia Chloramphenicol Pseudomonas
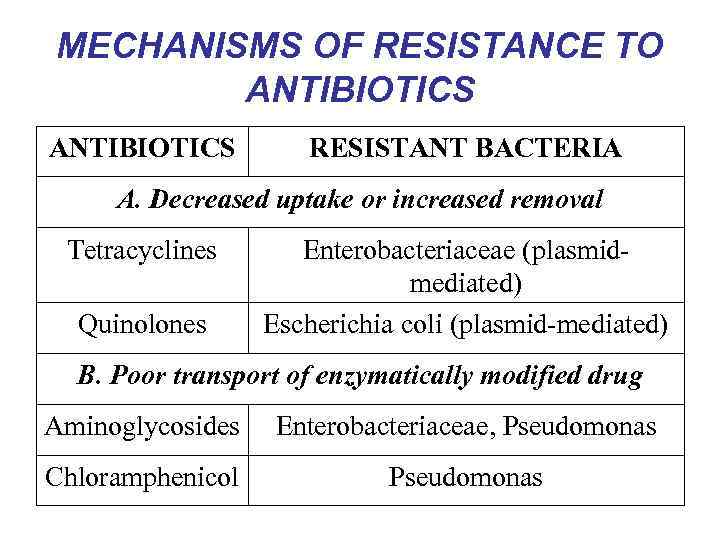
MECHANISMS OF RESISTANCE TO ANTIBIOTICS RESISTANT BACTERIA A. Decreased uptake or increased removal Tetracyclines Quinolones Enterobacteriaceae (plasmidmediated) Escherichia coli (plasmid-mediated) B. Poor transport of enzymatically modified drug Aminoglycosides Enterobacteriaceae, Pseudomonas Chloramphenicol Pseudomonas
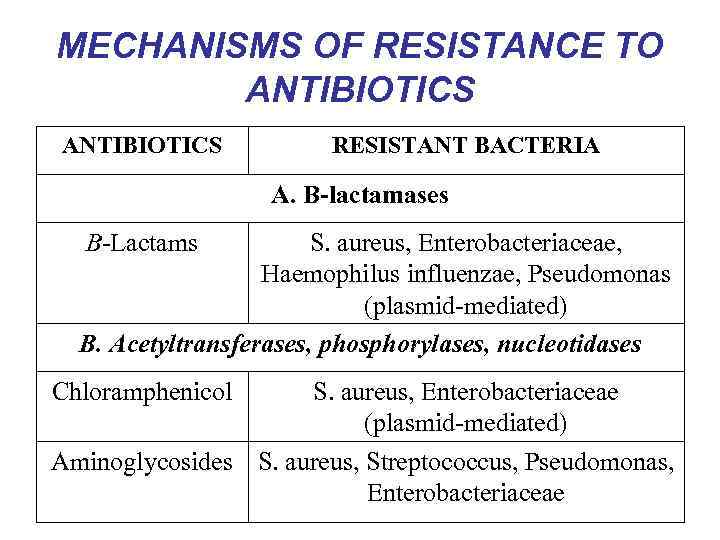
MECHANISMS OF RESISTANCE TO ANTIBIOTICS RESISTANT BACTERIA A. B-lactamases B-Lactams S. aureus, Enterobacteriaceae, Haemophilus influenzae, Pseudomonas (plasmid-mediated) B. Acetyltransferases, phosphorylases, nucleotidases Chloramphenicol S. aureus, Enterobacteriaceae (plasmid-mediated) Aminoglycosides S. aureus, Streptococcus, Pseudomonas, Enterobacteriaceae
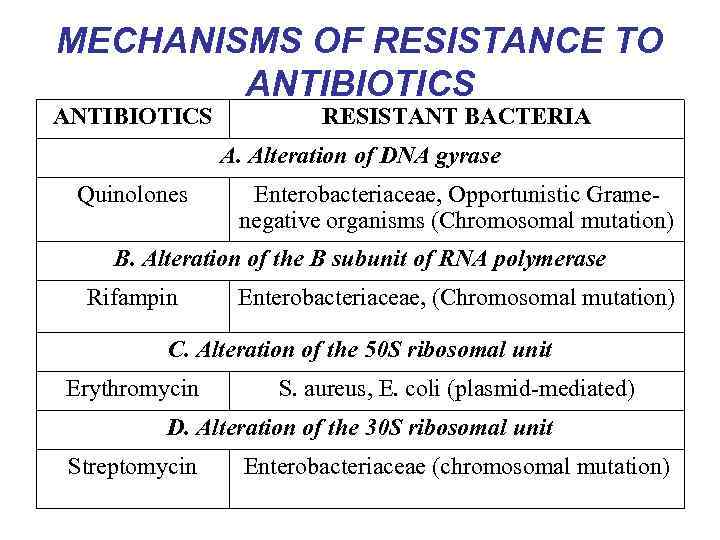
MECHANISMS OF RESISTANCE TO ANTIBIOTICS RESISTANT BACTERIA A. Alteration of DNA gyrase Quinolones Enterobacteriaceae, Opportunistic Gramenegative organisms (Chromosomal mutation) B. Alteration of the B subunit of RNA polymerase Rifampin Enterobacteriaceae, (Chromosomal mutation) C. Alteration of the 50 S ribosomal unit Erythromycin S. aureus, E. coli (plasmid-mediated) D. Alteration of the 30 S ribosomal unit Streptomycin Enterobacteriaceae (chromosomal mutation)
SIDE EFFECTS OF ANTIBIOTICS • 1. Organotoxic action: neurotoxic (Streptomycin); toxic action on the haematopoietic system (Tetracyclines). • 2. Allergic reactions: angioneurotic oedema, anaphylactic shock, allergic asthma, contact dermatitis (Penicillin).

SIDE EFFECTS OF ANTIBIOTICS • 3. Development of resistant strains of microorganisms which cause various complications • 4. Dysbacteriosis - disorders of normal flora of intestine and appears of infections. • 5. Immunosupression action.
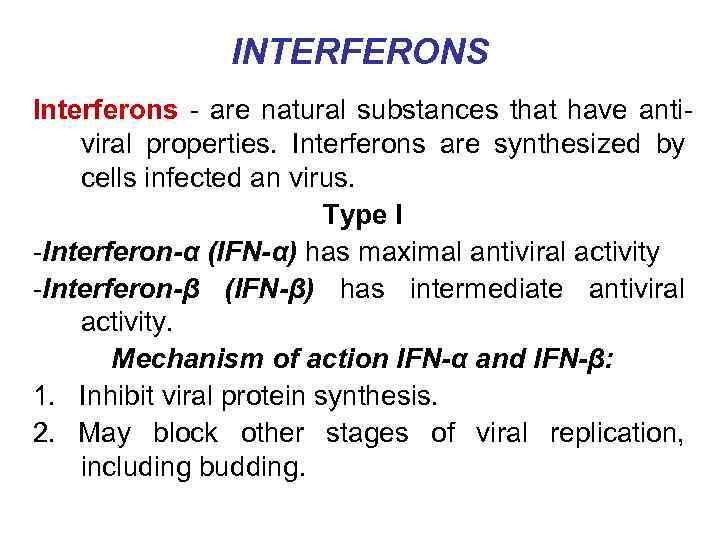
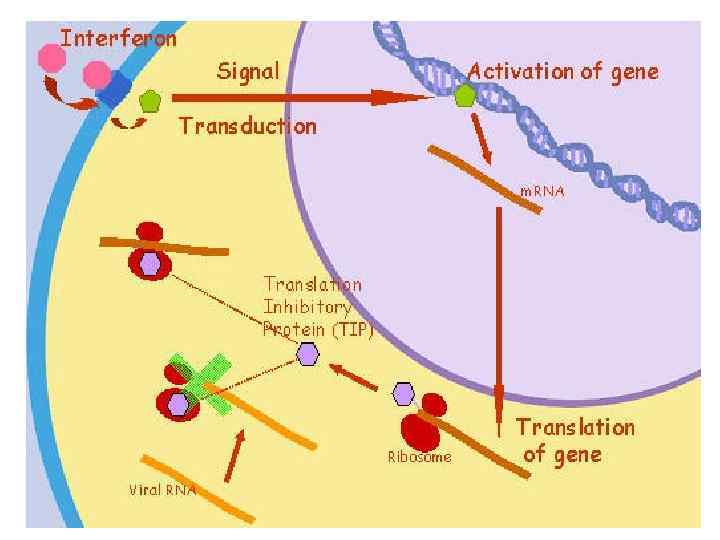
INTERFERONS Interferons - are natural substances that have antiviral properties. Interferons are synthesized by cells infected an virus. Type I -Interferon-α (IFN-α) has maximal antiviral activity -Interferon-β (IFN-β) has intermediate antiviral activity. Mechanism of action IFN-α and IFN-β: 1. Inhibit viral protein synthesis. 2. May block other stages of viral replication, including budding.
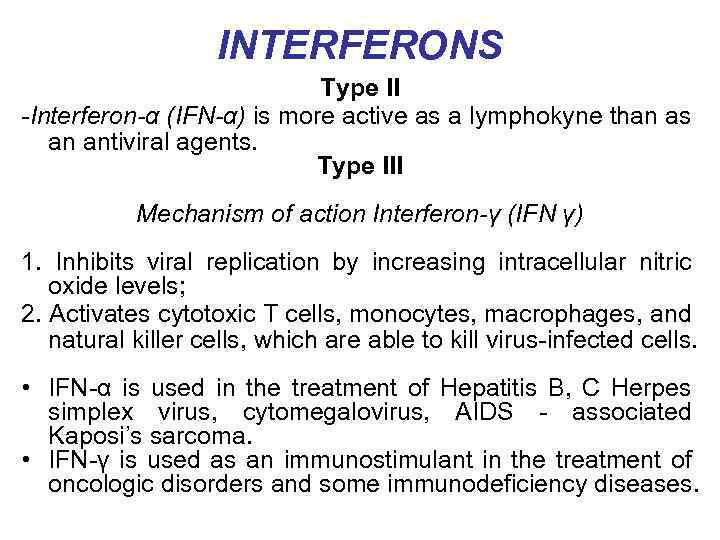
INTERFERONS Type II -Interferon-α (IFN-α) is more active as a lymphokyne than as an antiviral agents. Type III Mechanism of action Interferon-γ (IFN γ) 1. Inhibits viral replication by increasing intracellular nitric oxide levels; 2. Activates cytotoxic T cells, monocytes, macrophages, and natural killer cells, which are able to kill virus-infected cells. • IFN-α is used in the treatment of Hepatitis B, C Herpes simplex virus, cytomegalovirus, AIDS - associated Kaposi’s sarcoma. • IFN-γ is used as an immunostimulant in the treatment of oncologic disorders and some immunodeficiency diseases.
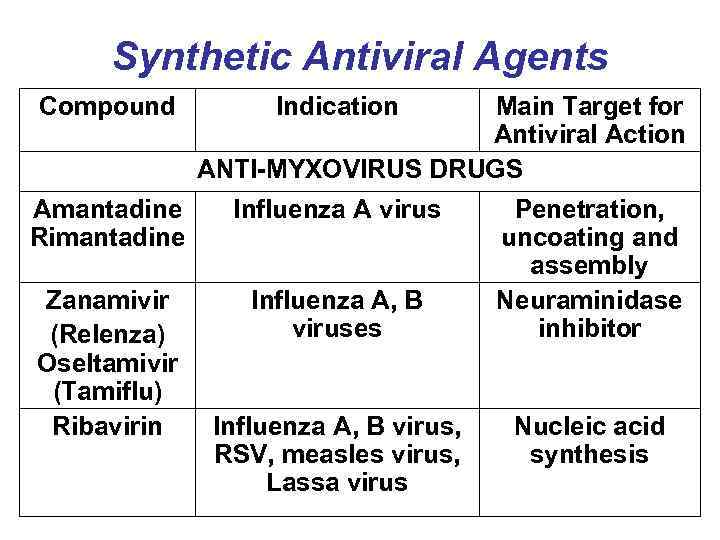
Synthetic Antiviral Agents Compound Indication Main Target for Antiviral Action ANTI-MYXOVIRUS DRUGS Amantadine Rimantadine Influenza A virus Zanamivir (Relenza) Oseltamivir (Tamiflu) Ribavirin Influenza A, B viruses Influenza A, B virus, RSV, measles virus, Lassa virus Penetration, uncoating and assembly Neuraminidase inhibitor Nucleic acid synthesis
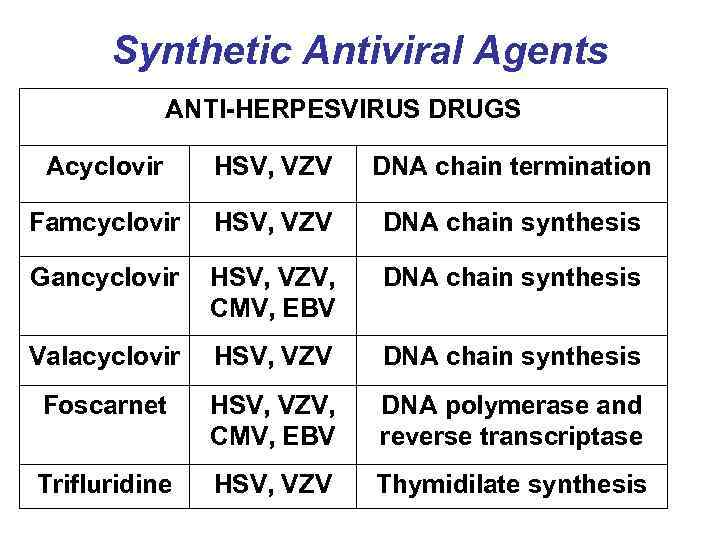
Synthetic Antiviral Agents ANTI-HERPESVIRUS DRUGS Acyclovir HSV, VZV DNA chain termination Famcyclovir HSV, VZV DNA chain synthesis Gancyclovir HSV, VZV, CMV, EBV DNA chain synthesis Valacyclovir HSV, VZV DNA chain synthesis Foscarnet HSV, VZV, CMV, EBV DNA polymerase and reverse transcriptase Trifluridine HSV, VZV Thymidilate synthesis
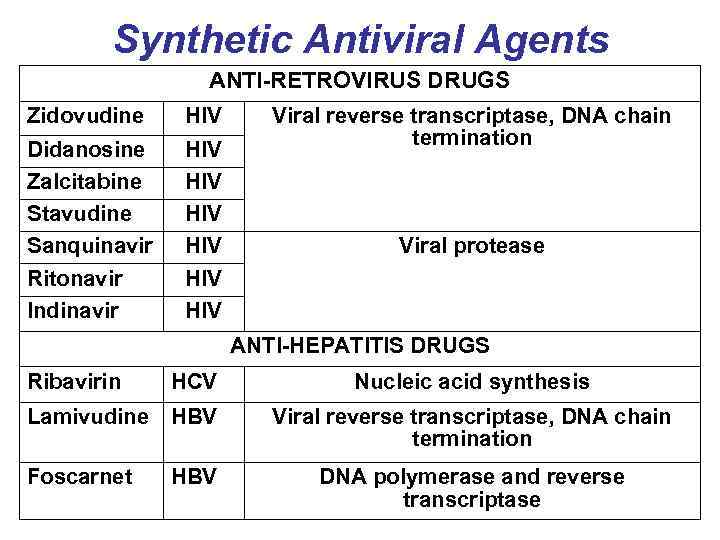
Synthetic Antiviral Agents ANTI-RETROVIRUS DRUGS Zidovudine HIV Didanosine Zalcitabine Stavudine Sanquinavir Ritonavir Indinavir HIV HIV HIV Viral reverse transcriptase, DNA chain termination Viral protease ANTI-HEPATITIS DRUGS Ribavirin HCV Lamivudine HBV Foscarnet HBV Nucleic acid synthesis Viral reverse transcriptase, DNA chain termination DNA polymerase and reverse transcriptase